Terminal Agitation Martlets hospice What this talk will

- Slides: 17
Terminal Agitation Martlets hospice
What this talk will cover • Definition of terminal agitation, how common is it • Symptoms and signs • Risk factors for more severe terminal agitation • Causes • General management • Management with medications • Delirium in COVID-19 patients • Summary • Opportunity for questions
What is terminal agitation? • Also known as terminal restlessness, terminal delirium • Anxious, restless and / or distressed behaviour that can occur at the end of life • Patient shows signs of anxiety, agitation and cognitive decline in the days leading up to death • Affects nearly 50% of all people who are dying • 80 -90% cancer patients become agitated
Recognition of Dying • Difficulty swallowing meds • Only manage sips • Bedbound • Decreased conscious level • Patient talks about dying, ready to die, premonition e. g. date of death, calls out to loved ones already dead • Profound fatigue – physical and mental • Change in cognition/delirium (preterm/terminal agitation)
Recognition of Dying • Art and science • Knowing the patient • Understanding the disease trajectory – cancer vs non-cancer • Liaising with colleagues – MDT • Pattern recognition • Listening to nurses, family, patient
Symptoms / Signs of Terminal Agitation • Calling out / shouting / screaming • Angry outbursts • Difficulty sitting still, trying to get out of bed • Unable to concentrate or relax • Fidgeting – picking at clothes, sheets • Can’t get comfortable • Confusion • Sleeping in day, active at night • Hallucinations
Increased Risk for severe terminal agitation • unfulfilled spiritual/emotional needs • armed forces veterans • parents with young children • young adults • victims of abuse/torture • those in denial of dying
Causes • unfulfilled spiritual/emotional needs • urinary retention • UTI, sepsis • Uncontrolled pain, nausea • Constipation • Hypoxia • Hypercalcaemia • Nicotine/alcohol/cannabis withdrawal • Cerebral oedema – brain tumour or metastases
General Management • Acknowledge their distress ‘I can see you are having distressing thoughts’ • Calm and safe environment • Avoid environmental triggers – noise, glare, back round distraction • Gentle music • Hold hand, gentle physical contact • Familiar objects, photos • Explain to family what is happening
Management - check no reversible issues • Review medications such as steroids • Review pain relief • Catheterise if suspect urinary retention • Nicotine patch if previously heavy smoker • Oxygen if hypoxia making agitation worse • Support from chaplain if available
Management with Medication • Medications – lower conscious level so they are calmer or asleep • Ask if they mind being a bit more sleepy • Involve family in discussion, make them aware their relative will be less able to communicate but they will be less distressed • Do not hasten death but can bring relief from distressing symptoms and allow a more peaceful death • Usually patients approaching end of life will have these medications prescribed as ‘just in case’ medications
Medication - Benzodiazepines • Midazolam • Stat subcutaneous dose 2. 5 -5 mg PRN hourly • Can increase up to 10 mg PRN • Syringe driver (CSCI) 10 -60 mg/24 hours
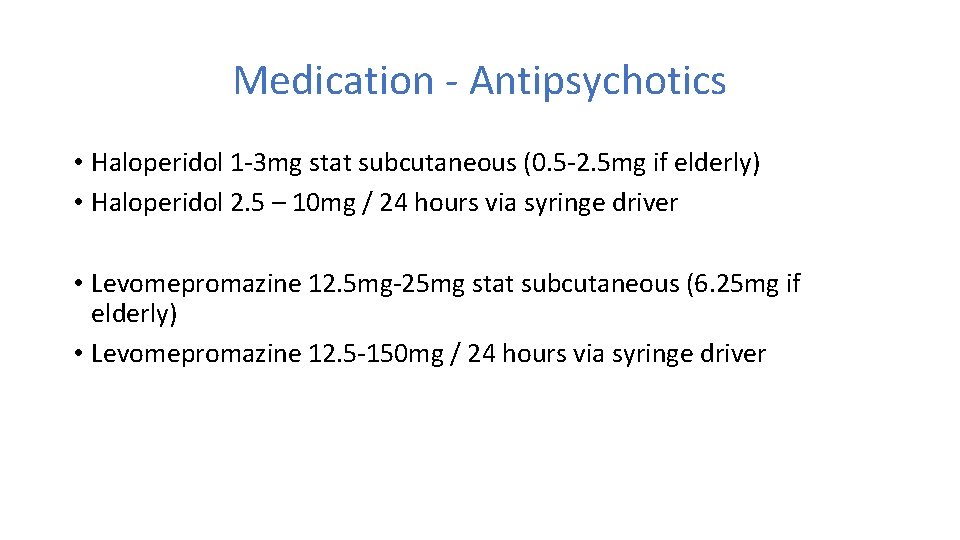
Medication - Antipsychotics • Haloperidol 1 -3 mg stat subcutaneous (0. 5 -2. 5 mg if elderly) • Haloperidol 2. 5 – 10 mg / 24 hours via syringe driver • Levomepromazine 12. 5 mg-25 mg stat subcutaneous (6. 25 mg if elderly) • Levomepromazine 12. 5 -150 mg / 24 hours via syringe driver
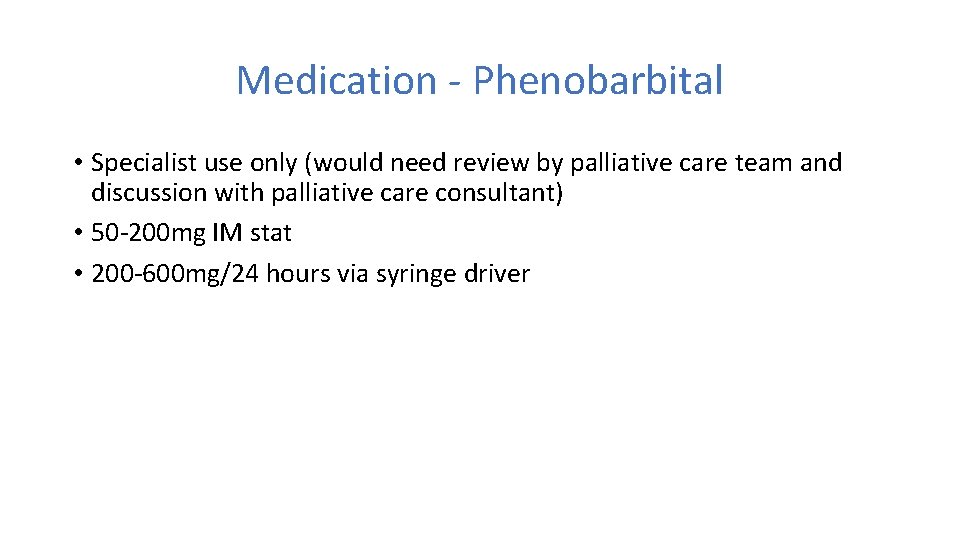
Medication - Phenobarbital • Specialist use only (would need review by palliative care team and discussion with palliative care consultant) • 50 -200 mg IM stat • 200 -600 mg/24 hours via syringe driver
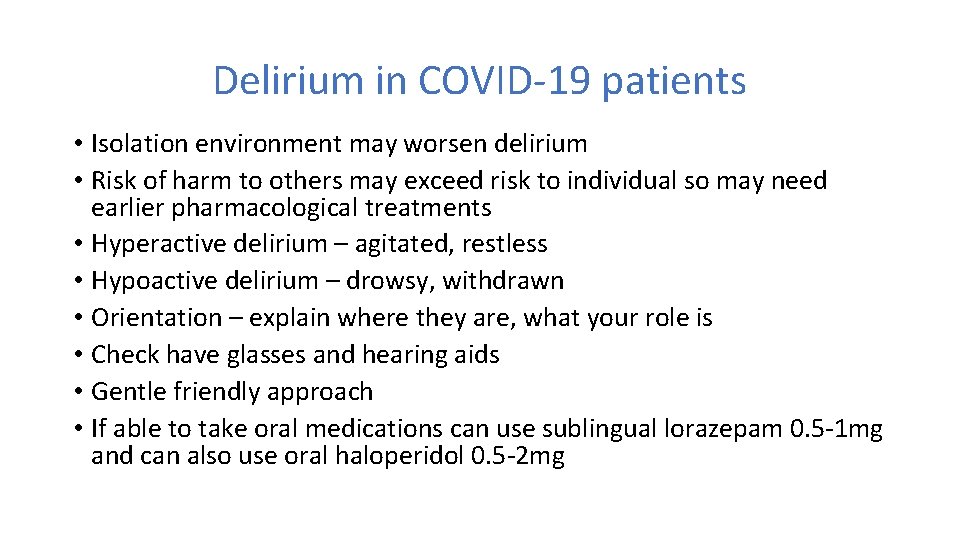
Delirium in COVID-19 patients • Isolation environment may worsen delirium • Risk of harm to others may exceed risk to individual so may need earlier pharmacological treatments • Hyperactive delirium – agitated, restless • Hypoactive delirium – drowsy, withdrawn • Orientation – explain where they are, what your role is • Check have glasses and hearing aids • Gentle friendly approach • If able to take oral medications can use sublingual lorazepam 0. 5 -1 mg and can also use oral haloperidol 0. 5 -2 mg
Summary • Terminal agitation is common at the end of life • Patients appear restless and unsettled • Check for any reversible causes such as pain, urinary retention • Calm environment important, acknowledge the distress • Medications also important to allow peaceful death • Start with midazolam, then consider haloperidol or levomepromazine

Thank you for listening!