Terminal Agitation Managing Symptoms at the End of



- Slides: 35
Terminal Agitation: Managing Symptoms at the End of Life Gregg Vande. Kieft, MD, MA Washington State Hospice and Palliative Care Annual Meeting Chelan, WA October 12, 2015

Speaker Bio Gregg Vande. Kieft, MD, MA • System Lead Physician for Palliative Care, Providence Health and Services (PH&S), Renton, WA • Regional Medical Director for Palliative Care, PH&S Southwest Washington Region, Olympia, WA • Inpatient and Outpatient Palliative Care, Providence St. Peter Hospital, Olympia, WA • Formerly Hospice Medical Director, Providence Sound Home Care and Hospice, Olympia, WA gregg. vandekieft@providence. org Twitter: @vandekieftg
Disclosures Dr. Vande. Kieft has no commercial relationships or conflicts of interest to report.
Learning Objectives At the conclusion of this presentation, participants will be able to: • • Define delirium and terminal agitation List common causes of terminal agitation Describe the initial assessment for delirium Recommend non-pharmacologic interventions and medication management for delirium and terminal agitation
Reflection Do not go gentle into that good night, Old age should burn and rave at close of day; Rage, rage against the dying of the light. Dylan Thomas, 1947
Key Points Delirium is a medical condition, rather than a psychiatric condition If possible identify and treat the underlying cause; less practical in the actively dying Underlying dementia increases risk of delirium 2 -3 x Terminal agitation is very common, treatment is often non-pharmacological
Delirium A transient global disorder of cognition • not a disease but a syndrome - multiple causes that produce a similar array of symptoms A medical emergency • 10 -25% mortality in patients admitted with delirium • up to 75% mortality in patients who develop delirium during hospitalization • early diagnosis and treatment correlates to better outcomes
Terminal Agitation or Restlessness Clinical spectrum of unsettling behaviors and cognitive disturbance in the last hours to days of life • Symptoms include: irritability, anxiety, distress, inattention, hallucinations, paranoia • Signs include: restlessness, fidgeting, grimacing, moaning, attempts to get out of bed Increased risk with certain medications • Anticholinergics, opioids, benzodiazepines, steroids, antipsychotics, anticonvulsants
Delirium: DSM-5 Criteria �Disturbance in attention and awareness �Change in cognition not better accounted for by an established or evolving dementia. �Acute onset (hours to days) and fluctuates over the course of the day �History, exam, and/or labs indicate the disturbance is caused by a medical condition, intoxicating substance, medication, or more than one cause.
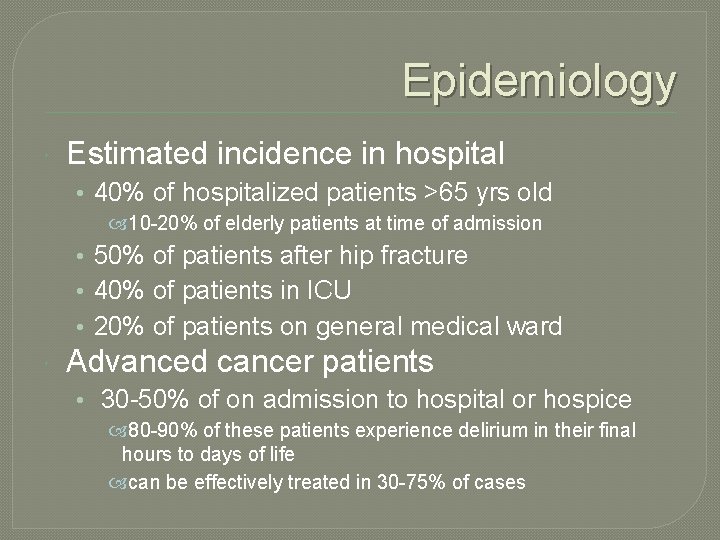
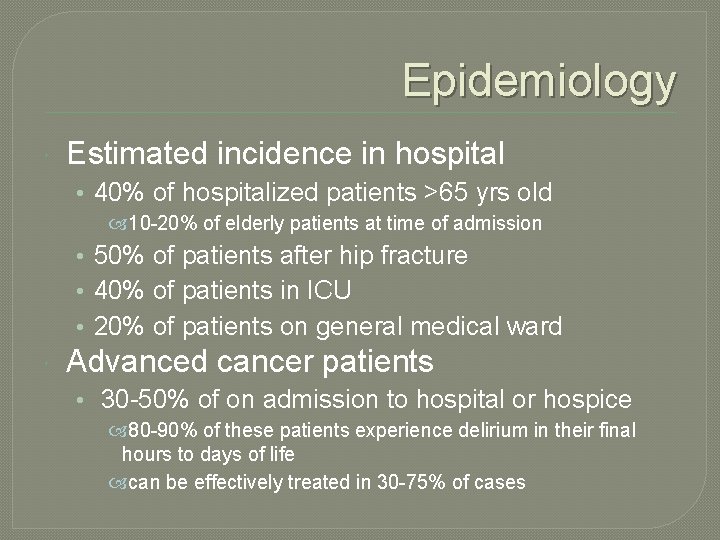
Epidemiology Estimated incidence in hospital • 40% of hospitalized patients >65 yrs old 10 -20% of elderly patients at time of admission • 50% of patients after hip fracture • 40% of patients in ICU • 20% of patients on general medical ward Advanced cancer patients • 30 -50% of on admission to hospital or hospice 80 -90% of these patients experience delirium in their final hours to days of life can be effectively treated in 30 -75% of cases
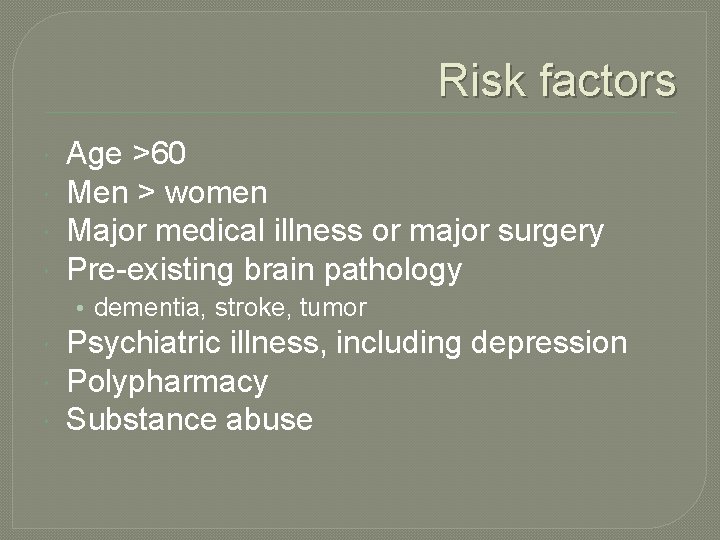
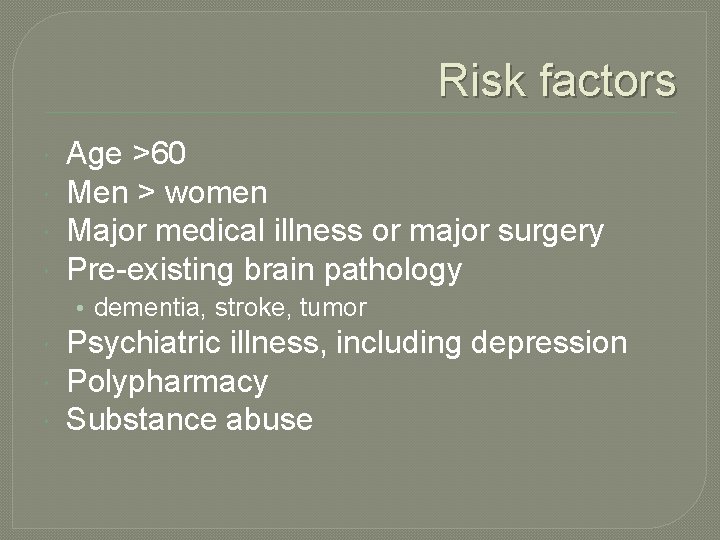
Risk factors Age >60 Men > women Major medical illness or major surgery Pre-existing brain pathology • dementia, stroke, tumor Psychiatric illness, including depression Polypharmacy Substance abuse
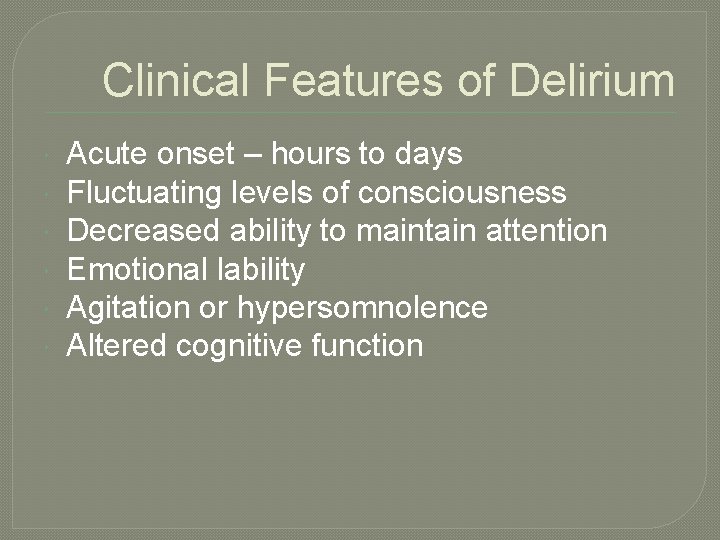
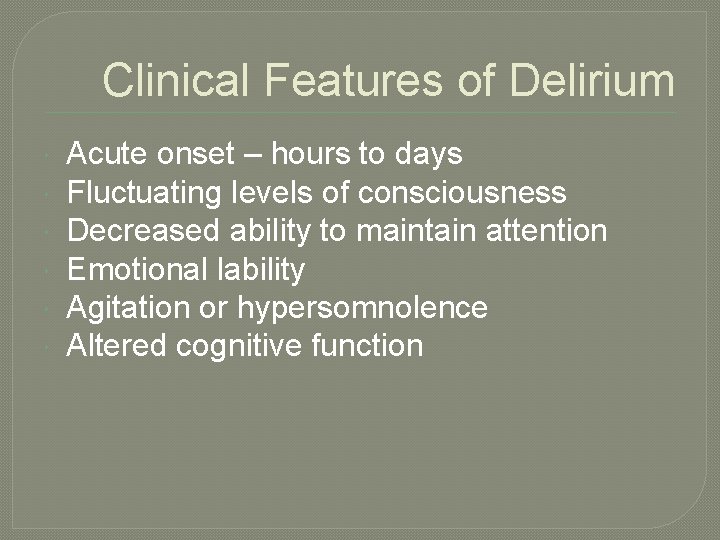
Clinical Features of Delirium Acute onset – hours to days Fluctuating levels of consciousness Decreased ability to maintain attention Emotional lability Agitation or hypersomnolence Altered cognitive function
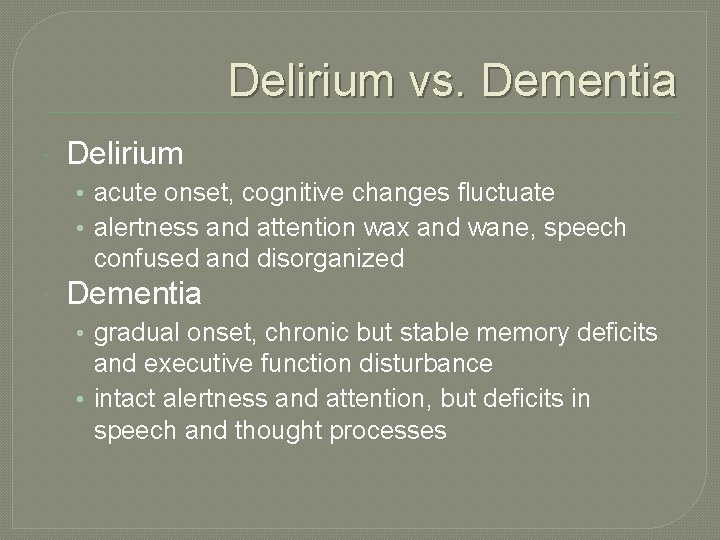
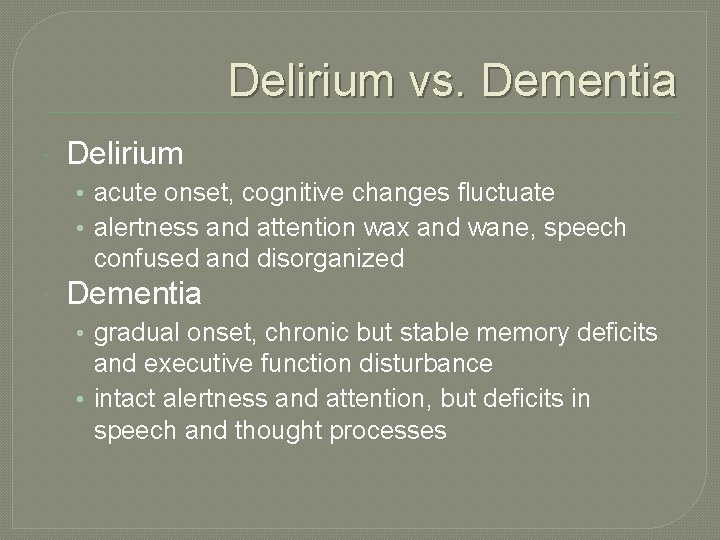
Delirium vs. Dementia Delirium • acute onset, cognitive changes fluctuate • alertness and attention wax and wane, speech confused and disorganized Dementia • gradual onset, chronic but stable memory deficits and executive function disturbance • intact alertness and attention, but deficits in speech and thought processes
Characteristic Cognitive Deficits Speech disturbance • slurred, mumbling, incoherent, disorganized Language impairments • word finding difficulty Memory dysfunction • short-term memory impaired; disoriented to persons, place, time Perceptual disturbance • delusions, hallucinations, misrepresentations
Clinical Case: Rose 76 year old woman with non-small cell lung cancer, metastatic to pelvis and spine • s/p chemo and radiation, now on hospice • no known psychiatric issues or dementia • neighbors called police after she wandered into their house confused – she became combative with the police • Paramedics bring her to ER for evaluation
Delirium in Oncology Patients �Direct effects of cancer on CNS • metastatic disease • higher circulating cytokine levels �Indirect effects of cancer • cancer related organ dysfunction - e. g. , liver • paraneoplastic syndromes • infections, electrolyte disturbance �Exogenous factors • chemotherapy, radiation therapy • opioids, polypharmacy
Differential Diagnosis � Brain metastasis • delirium not typically initial manifestation, but… � Medication reaction or interaction • very common – review med list, timing of medications relative to onset of symptoms • eliminate all meds that are not essential � Alcohol or drug withdrawal • consider Et. OH if onset 24 -48 hrs after hospital admit • has patient missed regular psychotropics or opioids? � Intracranial bleed • consider unwitnessed fall, especially for debilitated or thrombocytopenic patients
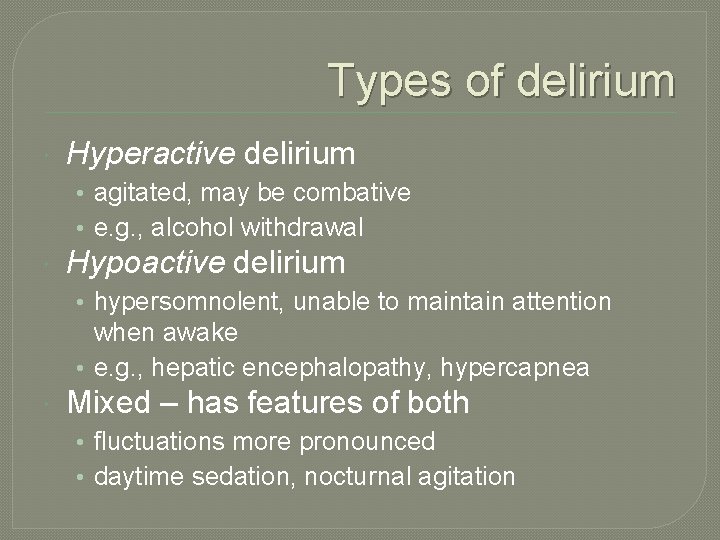
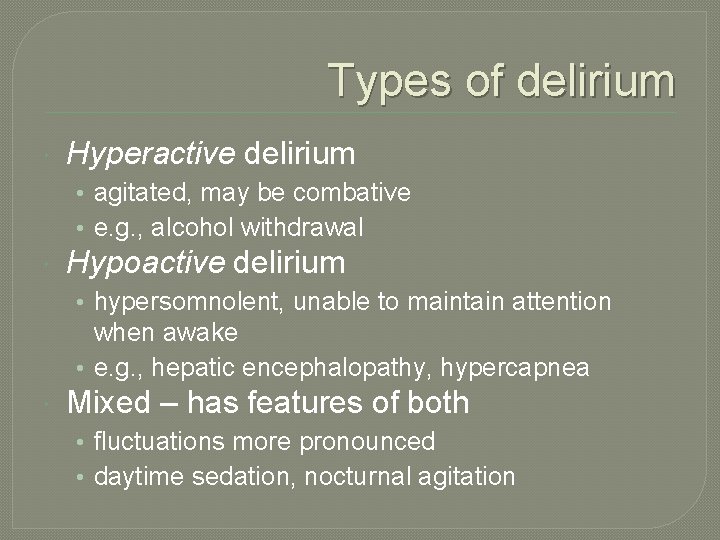
Types of delirium Hyperactive delirium • agitated, may be combative • e. g. , alcohol withdrawal Hypoactive delirium • hypersomnolent, unable to maintain attention when awake • e. g. , hepatic encephalopathy, hypercapnea Mixed – has features of both • fluctuations more pronounced • daytime sedation, nocturnal agitation
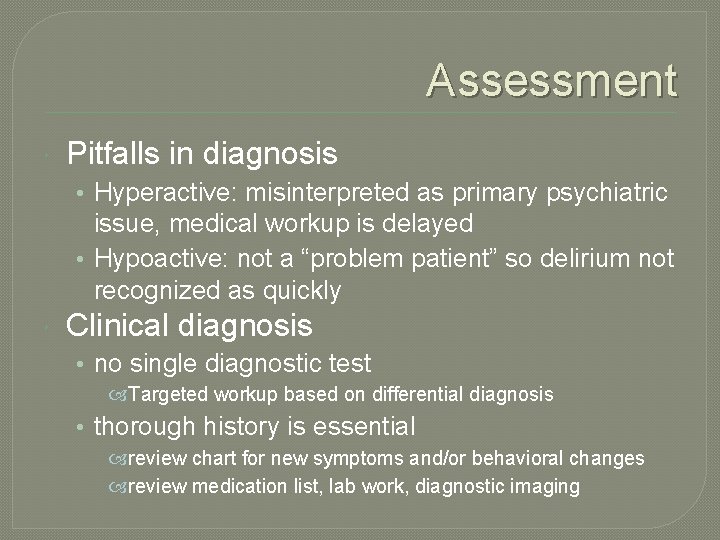
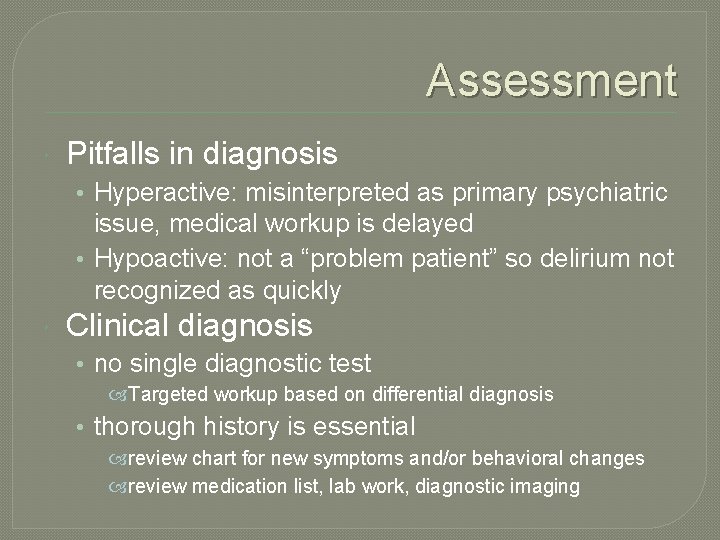
Assessment Pitfalls in diagnosis • Hyperactive: misinterpreted as primary psychiatric issue, medical workup is delayed • Hypoactive: not a “problem patient” so delirium not recognized as quickly Clinical diagnosis • no single diagnostic test Targeted workup based on differential diagnosis • thorough history is essential review chart for new symptoms and/or behavioral changes review medication list, lab work, diagnostic imaging
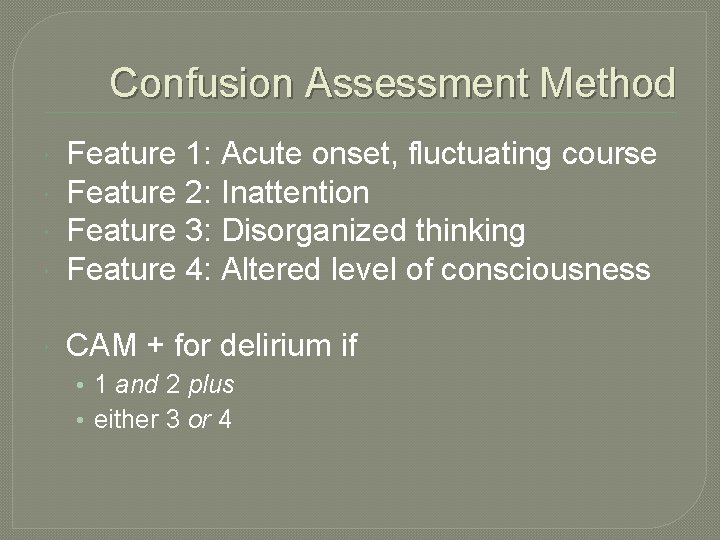
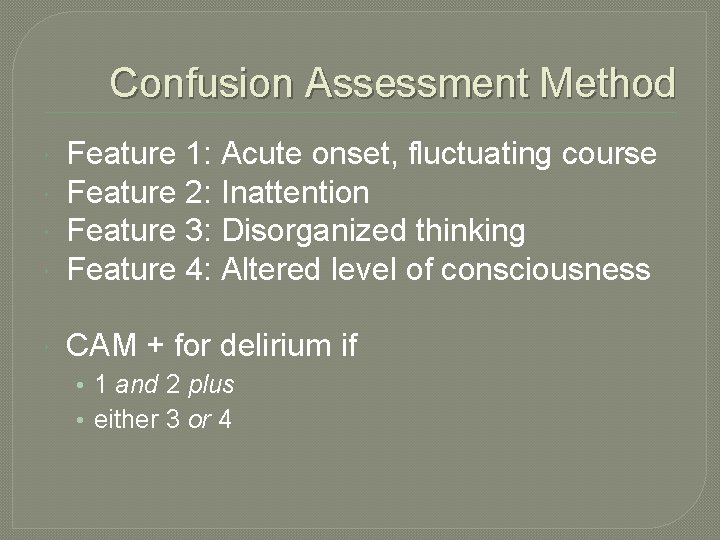
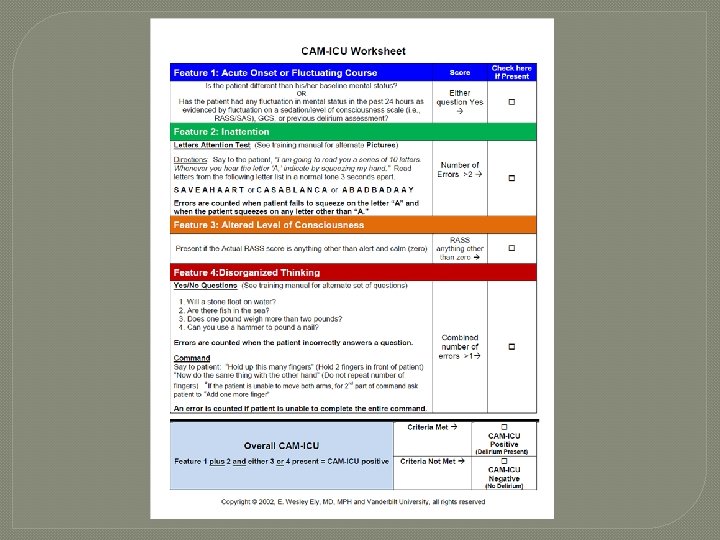
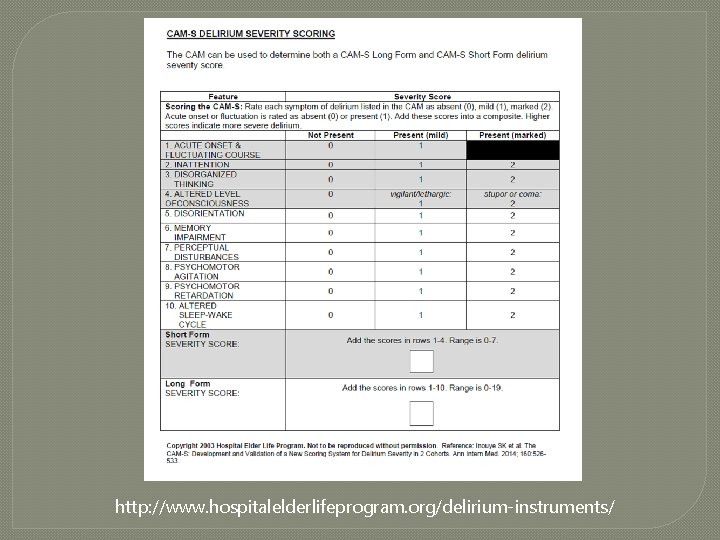
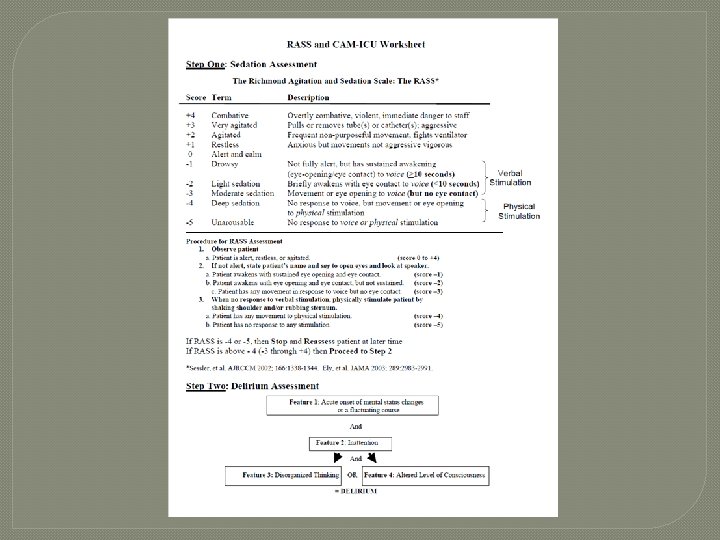
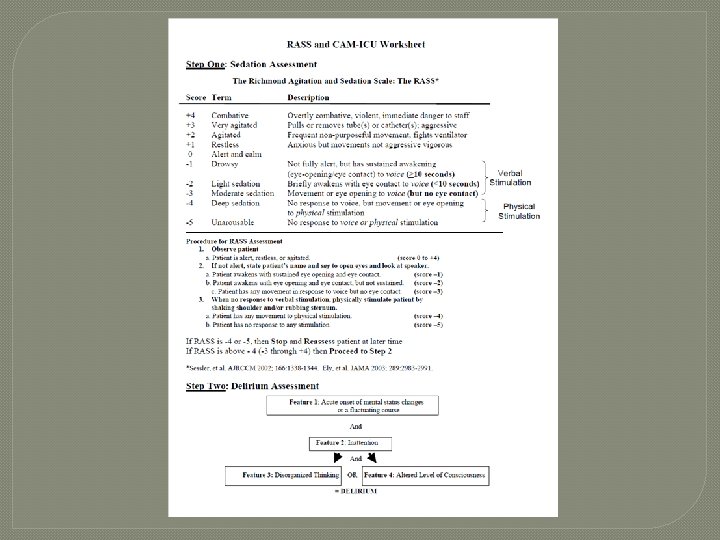
Confusion Assessment Method Feature 1: Acute onset, fluctuating course Feature 2: Inattention Feature 3: Disorganized thinking Feature 4: Altered level of consciousness CAM + for delirium if • 1 and 2 plus • either 3 or 4
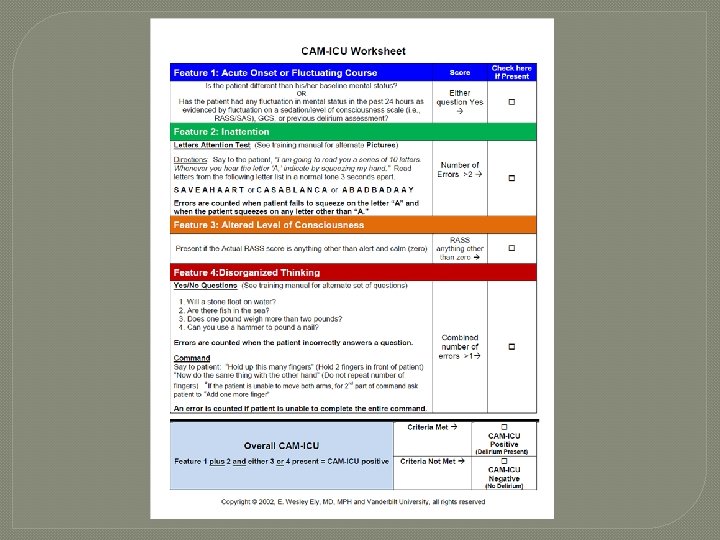
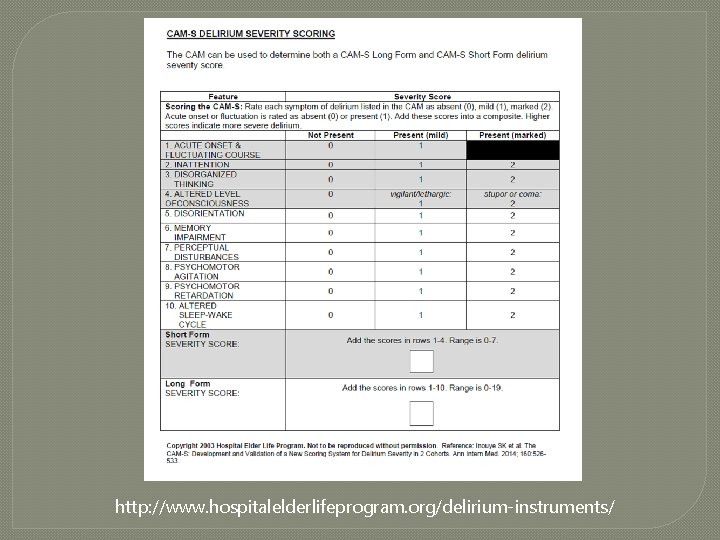
http: //www. hospitalelderlifeprogram. org/delirium-instruments/
Clinical Case (cont. ) In ER • Rose undergoes lab tests, receives IV fluids, electrolytes, meds, becomes marginally oriented • a mental health professional is consulted, determines she is able to make her own health care decisions and cannot be hospitalized against her wishes – she refuses admission and is discharged home against medical advice • the following day, her hospice nurse finds her covered with feces, rambling incoherently
Common Reversible Clinical Causes of Delirium Electrolyte disorders • hypercalcemia, hyponatremia, hyperkalemia Drug reactions, interactions, or toxicity • benzodiazepenes, opioids, anticholinergics, steroids, digoxin, Parkinsons meds, H 2 -blockers, alcohol Infection Hypoxemia Hyper- or hypoglycemia Hypotension Hepatic or renal encephalopathy Most cases are multifactorial
Causes of Terminal Agitation Biochemical abnormalities as organs fail • Hypercalcemia especially common in cancer Opioid or other drug toxicity Drug interactions Pain Fever, with or without infection Spiritual or existential distress Unresolved psychosocial issues
Obtain history Interview patient when possible • delirium covers a wide range of presentations, some patients can provide significant history If possible, talk to family or caregivers who know patient’s baseline • Review records carefully Typical tests of cognitive function (e. g. , MMSE) not very helpful in delirium • use tests that measure attention – e. g. , serial 7 s, spell world backward, or list months in reverse
Targeted workup For all studies, ask: Will it alter treatment? • how does test fit within broader context of illness trajectory and treatment goals? Brain mets: cranial CT or MRI Infection: CBC, UA, cultures, x-rays Electrolyte abnormalities: chem panel Liver failure: hepatic panel, ammonia Renal failure: BUN/Cr, monitor I/Os Respiratory failure: O 2 sat, ABGs
Clinical Case (cont. ) Rose is brought back to ER, remains disoriented, admitted Hospice GIP status • work-up showed UTI, possible pneumonia – started on IV antibiotics • required 1: 1 sitter due to behavioral outbursts • responded well to p. r. n. haloperidol … but no SNF would take her while she needed 1: 1 or was receiving haloperidol • risperidone added, good response, transferred to SNF, did well until she died 6 weeks later

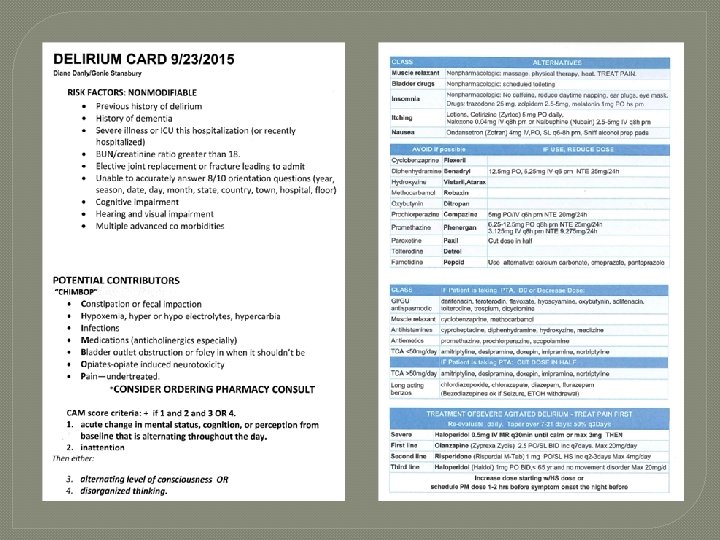
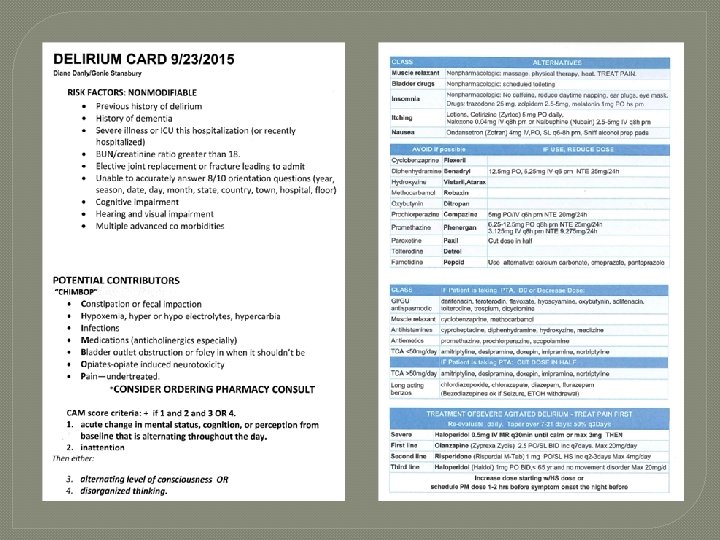
Treatment Identify and treat underlying cause, if able • Often not practical during actively dying phase • When etiology uncertain, treat symptoms Environmental therapy • Facilitate a quiet, peaceful setting • Provide cues: family photos, calendar, clock Address psychosocial issues, spiritual or existential concerns • Involve family, staff, spiritual care, music thanatology

Treatment (cont. ) “Pharmacologic debridement” • Review med profile, look for potential offending agents, eliminate all unnecessary meds Pharmacotherapy if non-pharmacologic interventions unsuccessful • Target patients who are severely agitated Behavior interferes with essential interventions or poses a safety hazard to self, family, staff • Avoid restraints! Usually worsens agitation
Medical Managment �Benzodiazepenes • generally avoid - can paradoxically worsen symptoms • helpful for alcohol withdrawal, anxiety �Conventional antipsychotics • haloperidol 1 st line in hospital or home, but usually not an option in nursing homes • IV or oral – onset of action 5 -20 min for IV route �Atypical antipsychotics • helpful for “maintenance” use, especially olanzapine or risperidone
Key Points Delirium is a medical condition, rather than a psychiatric condition If possible identify and treat the underlying cause; less practical in the actively dying Underlying dementia increases risk of delirium 2 -3 x Terminal agitation is very common, treatment is often non-pharmacological
Questions?