TEMPORARY TRANSVENOUS PACEMAKER INSERTION Return to Procedures Temporary










- Slides: 52

TEMPORARY TRANSVENOUS PACEMAKER INSERTION Return to Procedures
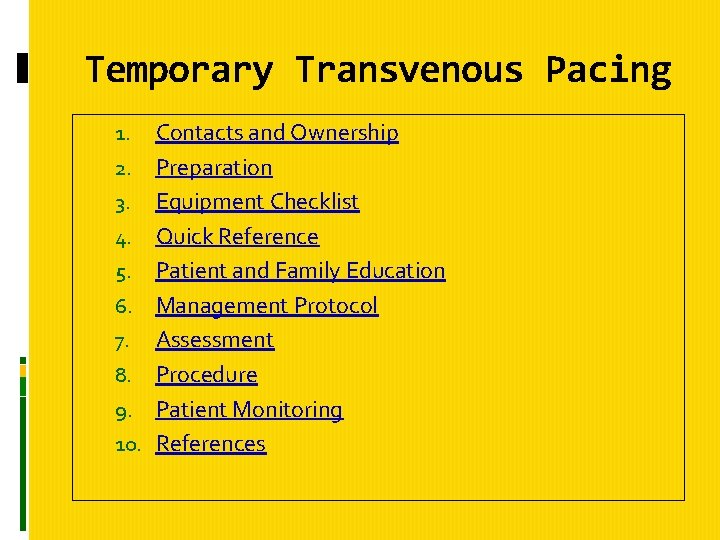
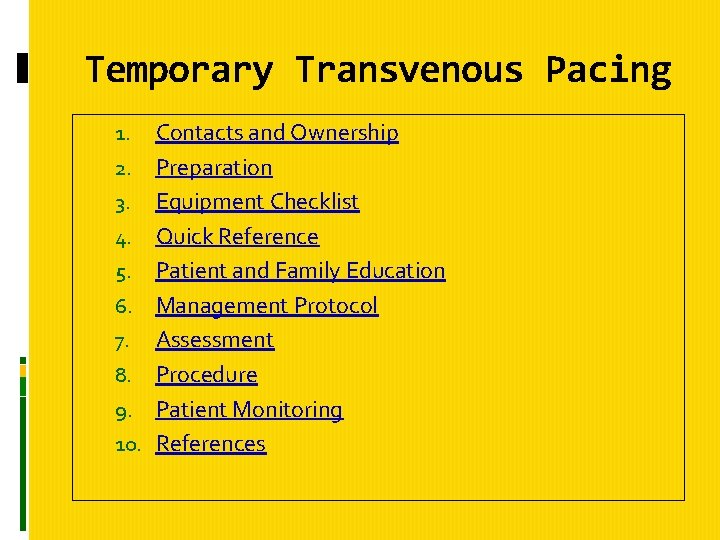
Temporary Transvenous Pacing 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Contacts and Ownership Preparation Equipment Checklist Quick Reference Patient and Family Education Management Protocol Assessment Procedure Patient Monitoring References
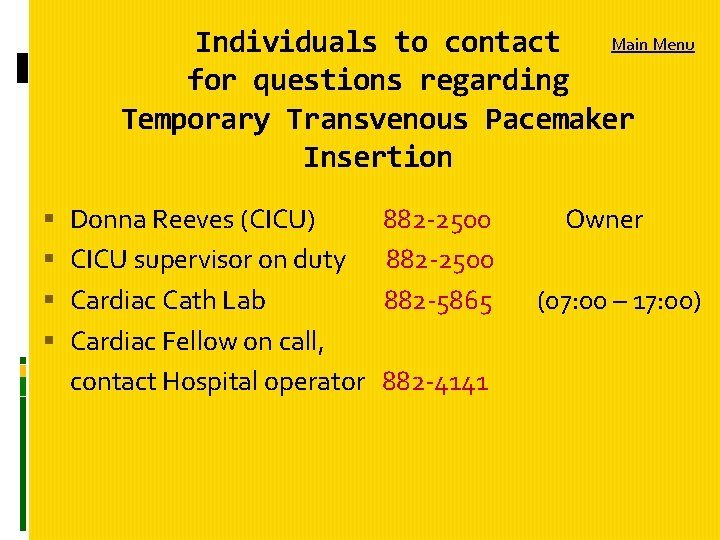
Main Menu Individuals to contact for questions regarding Temporary Transvenous Pacemaker Insertion Donna Reeves (CICU) 882 -2500 Owner CICU supervisor on duty 882 -2500 Cardiac Cath Lab 882 -5865 (07: 00 – 17: 00) Cardiac Fellow on call, contact Hospital operator 882 -4141
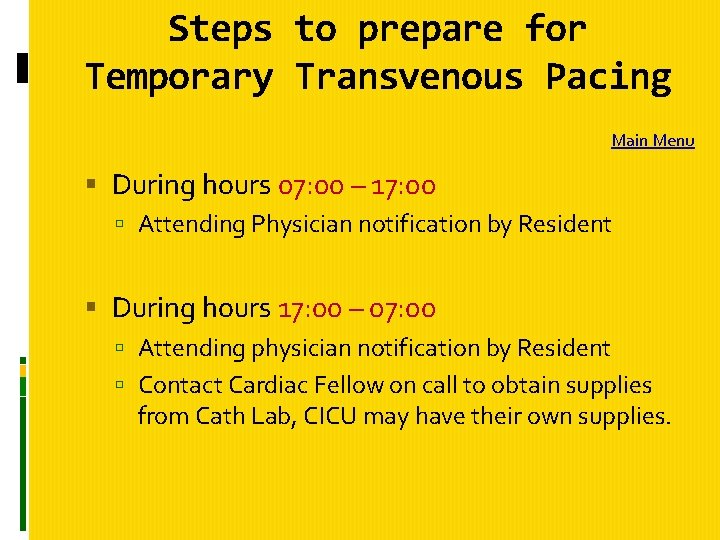
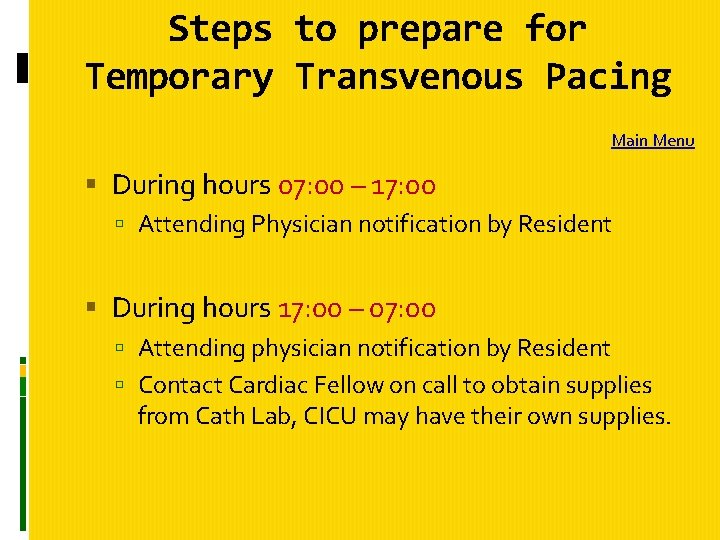
Steps to prepare for Temporary Transvenous Pacing Main Menu During hours 07: 00 – 17: 00 Attending Physician notification by Resident During hours 17: 00 – 07: 00 Attending physician notification by Resident Contact Cardiac Fellow on call to obtain supplies from Cath Lab, CICU may have their own supplies.
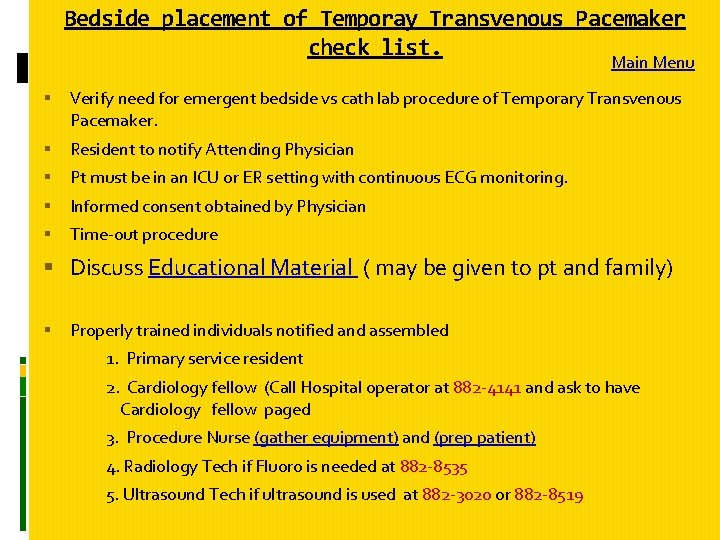
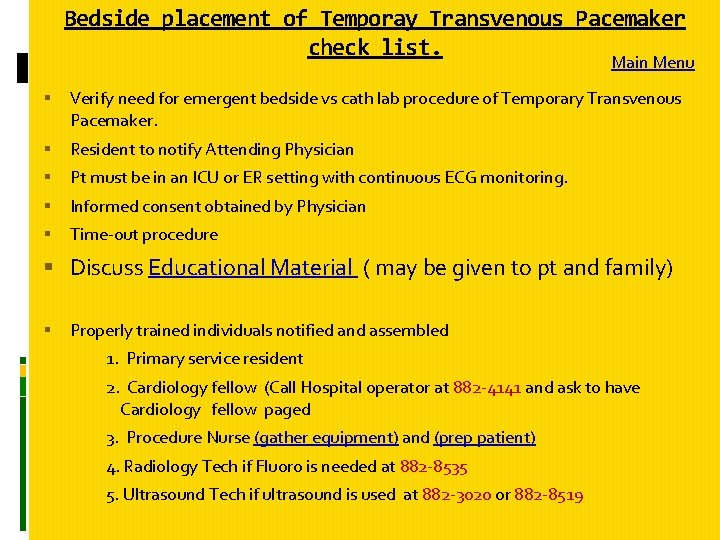
Bedside placement of Temporay Transvenous Pacemaker check list. Main Menu Verify need for emergent bedside vs cath lab procedure of Temporary Transvenous Pacemaker. Resident to notify Attending Physician Pt must be in an ICU or ER setting with continuous ECG monitoring. Informed consent obtained by Physician Time-out procedure Discuss Educational Material ( may be given to pt and family) Properly trained individuals notified and assembled 1. Primary service resident 2. Cardiology fellow (Call Hospital operator at 882 -4141 and ask to have Cardiology fellow paged 3. Procedure Nurse (gather equipment) and (prep patient) 4. Radiology Tech if Fluoro is needed at 882 -8535 5. Ultrasound Tech if ultrasound is used at 882 -3020 or 882 -8519
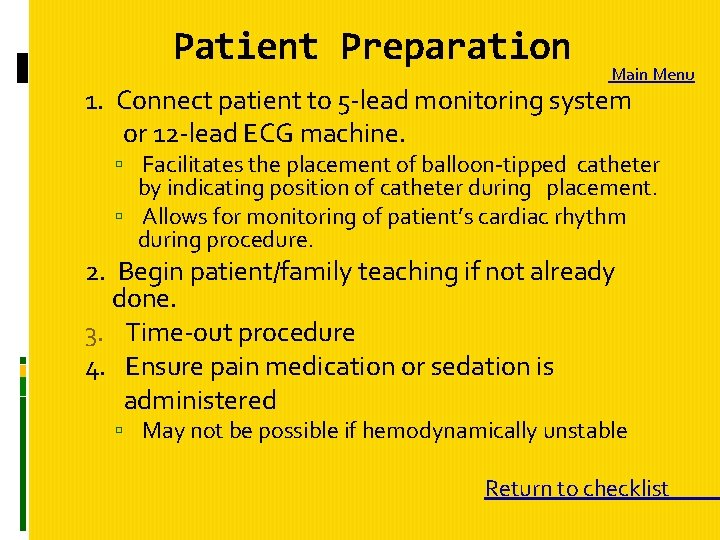
Patient Preparation Main Menu 1. Connect patient to 5 -lead monitoring system or 12 -lead ECG machine. Facilitates the placement of balloon-tipped catheter by indicating position of catheter during placement. Allows for monitoring of patient’s cardiac rhythm during procedure. 2. Begin patient/family teaching if not already done. 3. Time-out procedure 4. Ensure pain medication or sedation is administered May not be possible if hemodynamically unstable Return to checklist
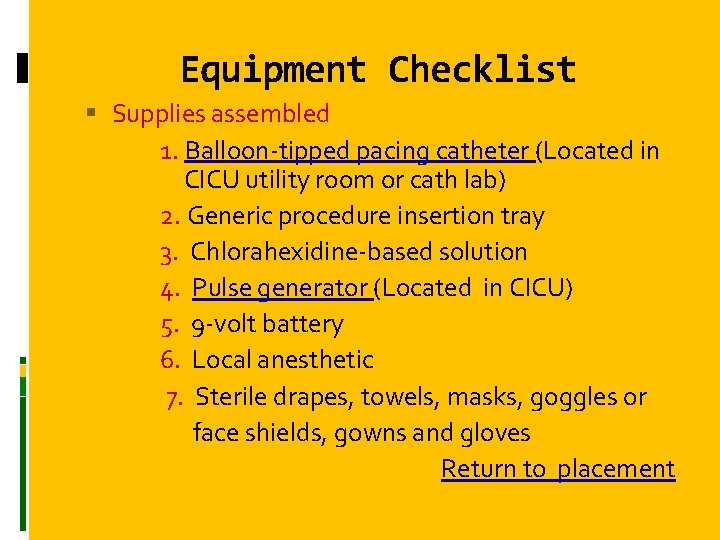
Equipment Checklist Supplies assembled 1. Balloon-tipped pacing catheter (Located in CICU utility room or cath lab) 2. Generic procedure insertion tray 3. Chlorahexidine-based solution 4. Pulse generator (Located in CICU) 5. 9 -volt battery 6. Local anesthetic 7. Sterile drapes, towels, masks, goggles or face shields, gowns and gloves Return to placement
8. Connecting cable (Located in CICU, or Cath Lab) 9. Percutaneous introducer needle comes in percutaneous sheath introducer set or can do individually 10. Introducer sheath with dilator (steri sleeve - if don't use kit) 11. Guide wire 12. Alligator clips or wire with connecting pins (Located in CICU or Cath Lab) 13. Suture with needle 2. 0 silk, syringes, needles 14. ECG monitor and recorder 15. Dressing supplies 16. Pain Medication / Sedation if ordered
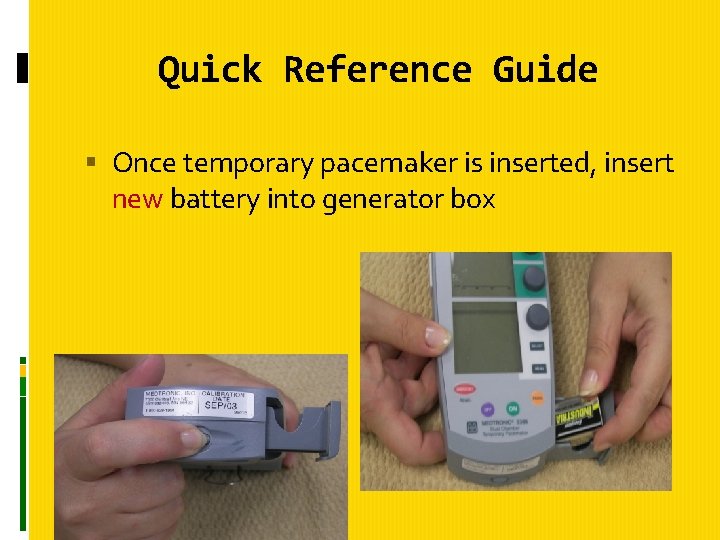
Additional Equipment that may be needed Main Menu • Emergency equipment (Crash Cart) • Fluoroscopy • Lead aprons or sheets • 12 -lead ECG machine • Transcutaneous ultrasound Place a new battery in the pulse generator
Quick Reference Guide for Nurses Main Menu Once temporary pacemaker inserted check its threshold parameters and assure proper functioning Mode of pacing set on: Demand Pacemaker senses heart’s impluses, paces when patient needs it. Asynchronous (Red button) Pacemaker fires at fixed rate. Return
Quick Reference Guide Set rate as prescribed. Set the stimulation threshold Set the sensitivity after determining the sensitivity threshold Pt should be transferred to an Adult ICU if not already there. Chart all of the above procedure and initiate the Temporary Transvenous pacemaker management protocol
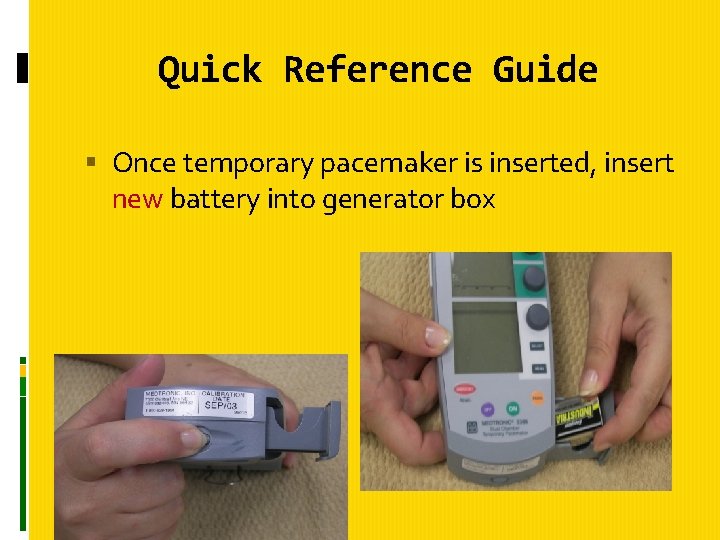
Quick Reference Guide Once temporary pacemaker is inserted, insert new battery into generator box

Quick Reference Guide Turn pacer on Select mode of pacing. Demand or asynchronous Return
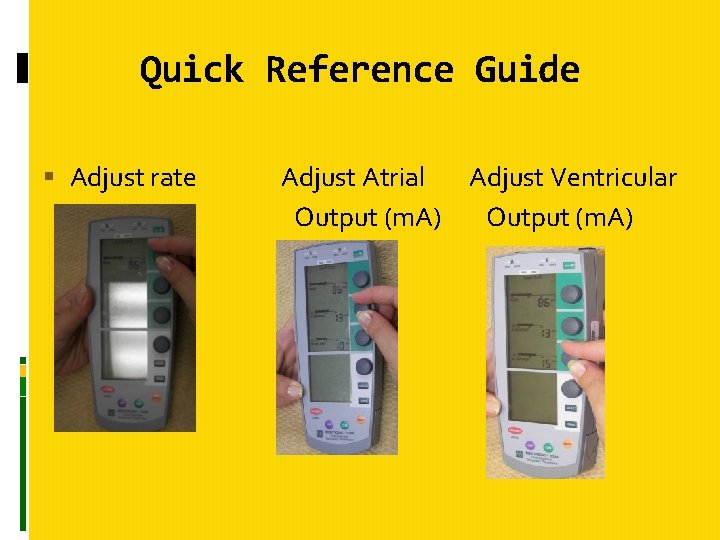
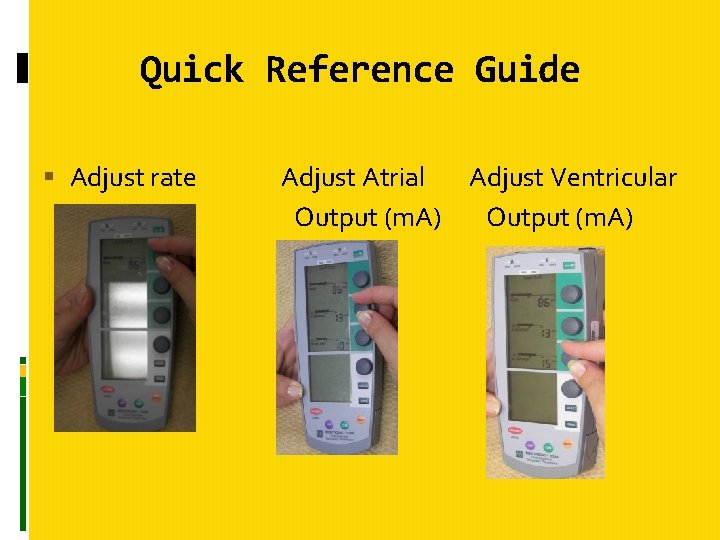
Quick Reference Guide Adjust rate Adjust Atrial Adjust Ventricular Output (m. A)
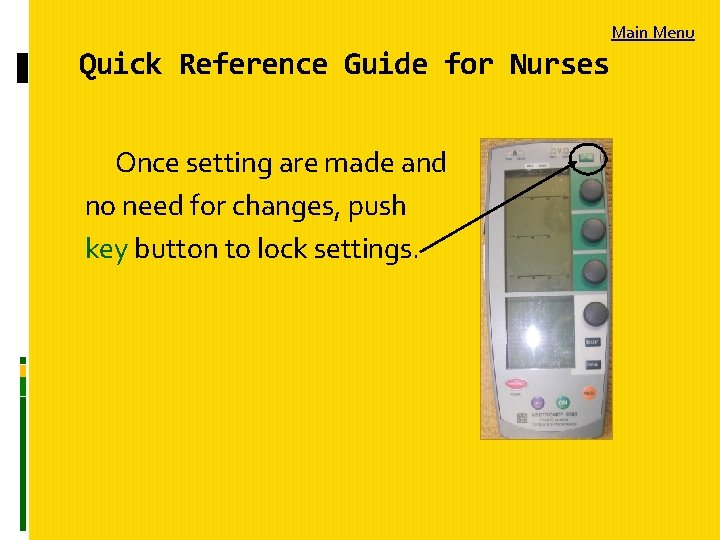
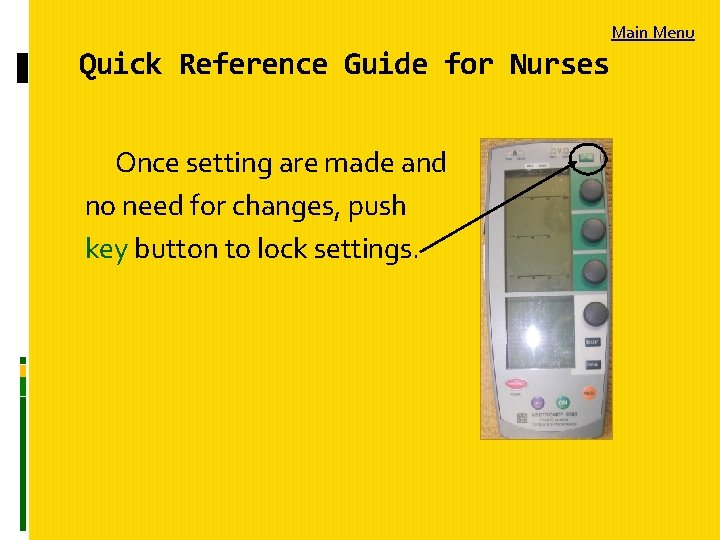
Main Menu Quick Reference Guide for Nurses Once setting are made and no need for changes, push key button to lock settings.
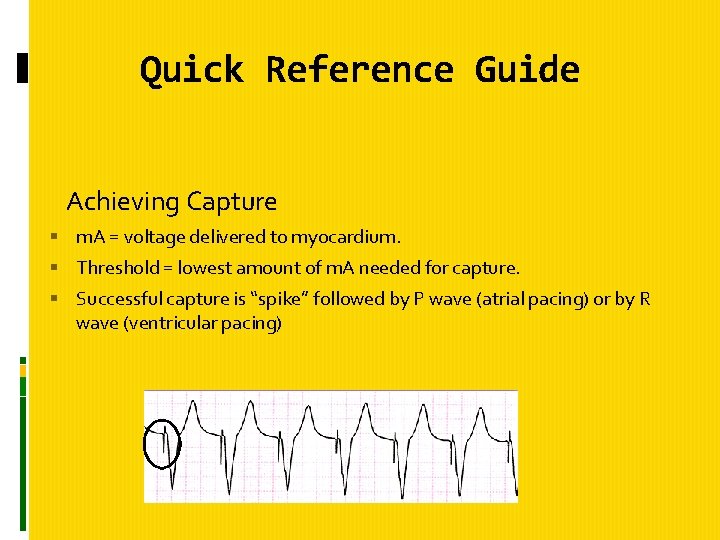
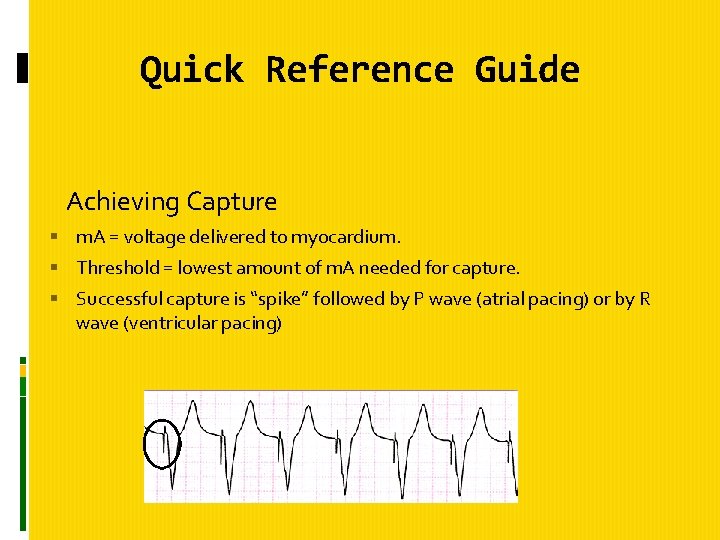
Quick Reference Guide Achieving Capture m. A = voltage delivered to myocardium. Threshold = lowest amount of m. A needed for capture. Successful capture is “spike” followed by P wave (atrial pacing) or by R wave (ventricular pacing)
Quick Reference Guide Stimulation Threshold Set in demand mode Set rate 10 bpm above patient’s rate. or as high as needed to see 100% capture. (spike with each beat) Slowly turn down m. A until 1: 1 capture is lost (EKG will show spikes without complexes following) Slowly turn up m. A until capture is regained.
Quick Reference Guide Sensing = ability of pacemaker to detect the heart’s own electrical activity and deliver paced beats only when needed. Set the rate 10 beats below patient’s inherent rate Contraindicated if patient has no intrinsic rate or symptomatic bradycardia Reduce m. A to lowest level (threshold) Turn sensitivity dial counterclockwise toward higher numerical setting (Sensing light, which flashes when sensing, will stop. ) Pacemaker is now less sensitive to patient’s heartbeat.

Quick Reference Guide Turn sensitivity dial clockwise until the sensing light starts flashing again. Sensitivity threshold. Set the sensitivity, (m. V = millivolts) at half the sensitivity threshold value obtained. (If sensitivity threshold is 4 you set dial on 2 m. V Restore m. A and rate to proper settings.
Quick Reference Guide Troubleshooting Check stimulation and sensitivity thresholds done daily if in demand mode. Failure to pace: No pacer spikes shown on ECG or telemetry strip Check batteries and replace if necessary (change every 2 – 3 days) Check to make sure all connections are tight If still no spikes, pacer may be oversensing Lower m. V on sensitivity dial

Quick Reference Guide Oversensing may be caused by electromechanical interference such as electric devices or muscle movement and artifact Undersensing : can be dangerous Pacer fails to sense the patient’s intrinsic beats Pacer spikes fire indiscriminately throughout cardiac cycle, can trigger lethal dysrhythmia if spike falls on T-wave. Lower pacemaker’s sensitivity to the heart by turning up the dial to higher m. V
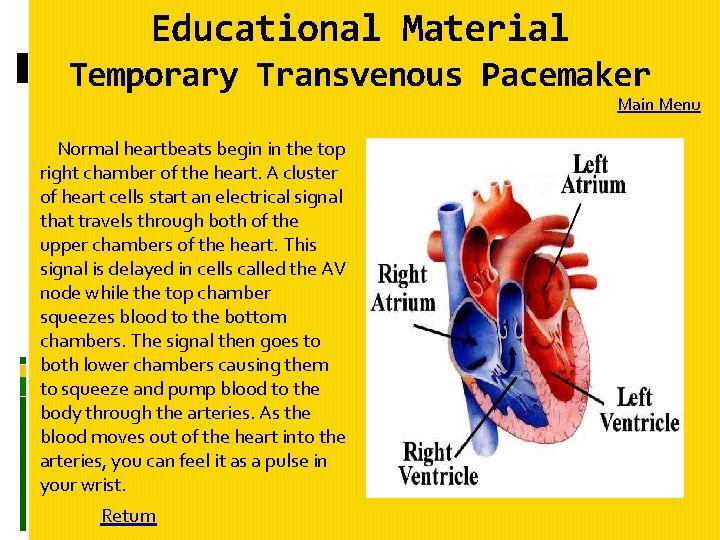
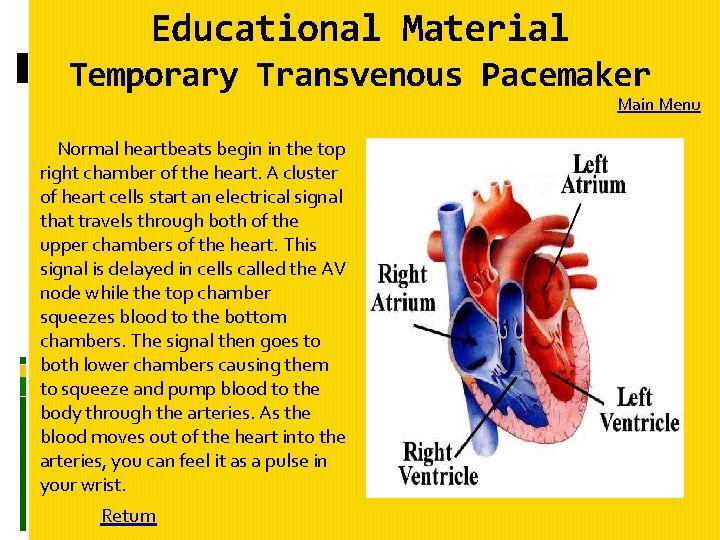
Educational Material Temporary Transvenous Pacemaker Normal heartbeats begin in the top right chamber of the heart. A cluster of heart cells start an electrical signal that travels through both of the upper chambers of the heart. This signal is delayed in cells called the AV node while the top chamber squeezes blood to the bottom chambers. The signal then goes to both lower chambers causing them to squeeze and pump blood to the body through the arteries. As the blood moves out of the heart into the arteries, you can feel it as a pulse in your wrist. Return Main Menu

Educational Material Normally the heart speeds up and slows down all the time as your activity changes. You need a faster heart beat when you are exercising to pump the blood faster through your body. When you are resting or sleeping, your heart rate slows. Unusually slow heartbeats can cause symptoms of weakness, shortness of breath, dizziness or even blackouts. Some of the time, a very slow heart beat is temporary. It may be caused from a side effect of a drug, blockage in one of the arteries of the heart or from another cause. A temporary pacemaker may be necessary to treat slow heart rates. A pacemaker is often the only way to get a steady, reliable heart rhythm.
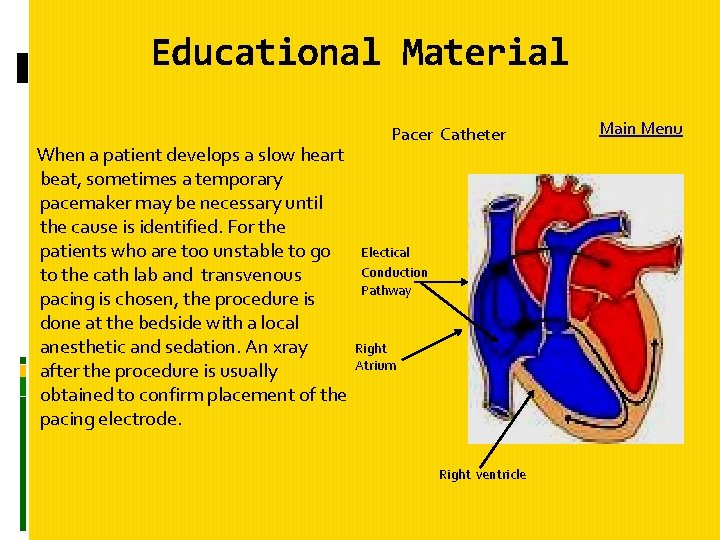
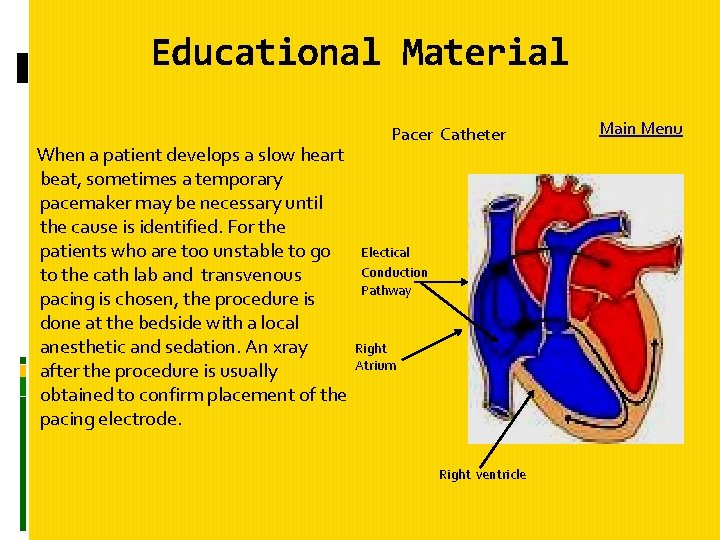
Educational Material Pacer Catheter When a patient develops a slow heart beat, sometimes a temporary pacemaker may be necessary until the cause is identified. For the patients who are too unstable to go Electical Conduction to the cath lab and transvenous Pathway pacing is chosen, the procedure is done at the bedside with a local Right anesthetic and sedation. An xray Atrium after the procedure is usually obtained to confirm placement of the pacing electrode. Right ventricle Main Menu

Educational Material How long should you expect the temporary pacemaker to remain in place? Temporary pacemakers are usually only left in place until the patient stabilizes enough by correcting the cause of the slow heartbeat or until they can be taken to the cath lab to have a permanent pacemaker placed.

Transvenous Pacemaker Management Protocol Return to Protocols
Transvenous Pacemaker Management Protocol
Transvenous Pacemaker Management Protocol Main Menu

Equipment for insertion Generic procedure insertion tray Chlorahexidine-based solution 9 -volt battery Local anesthetic, pain medication/sedation Sterile drapes, towels, masks, goggles or face shields, gowns, gloves. Suture with needle, syringes, needles Dressing supplies Guidewire
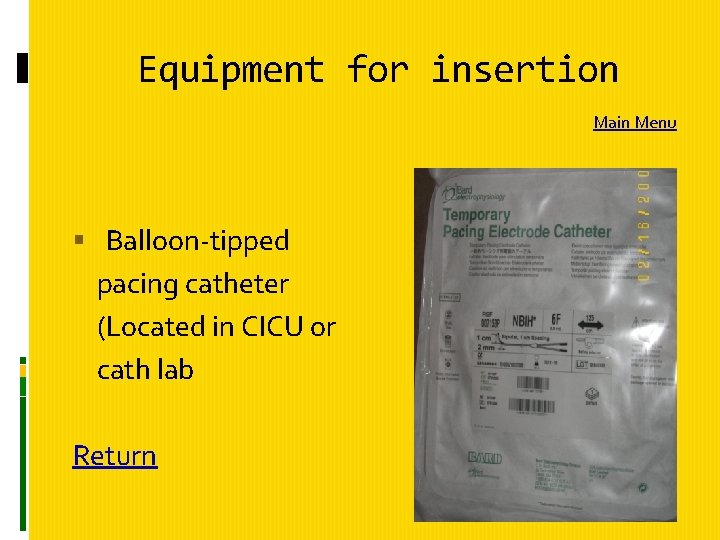
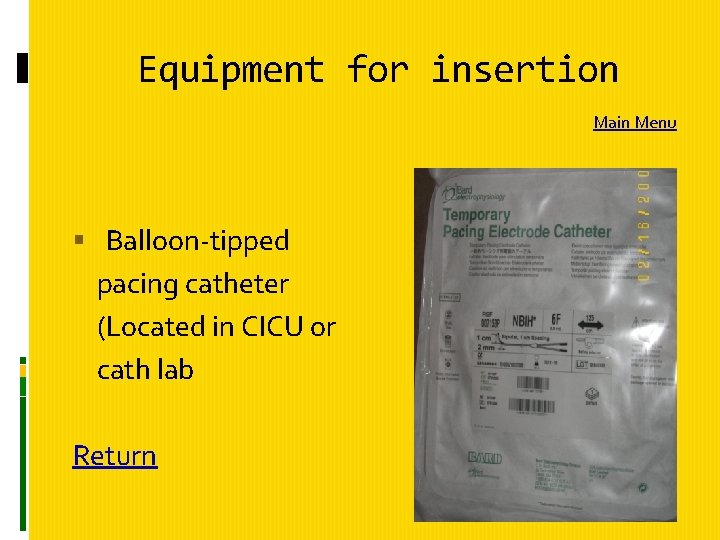
Equipment for insertion Main Menu Balloon-tipped pacing catheter (Located in CICU or cath lab Return

Equipment for insertion Pulse generator (Located in CICU, ICU or Cath Lab) Return
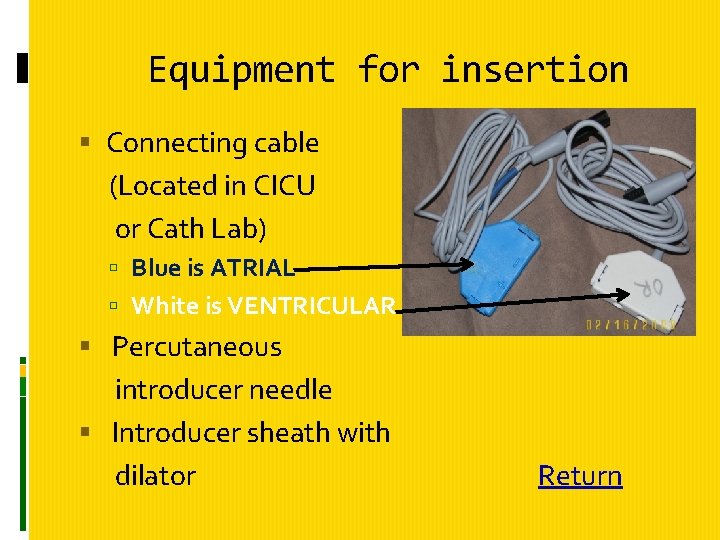
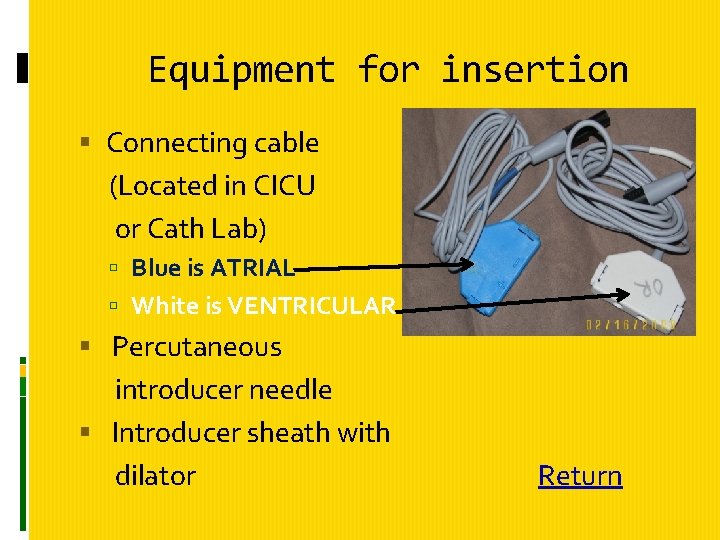
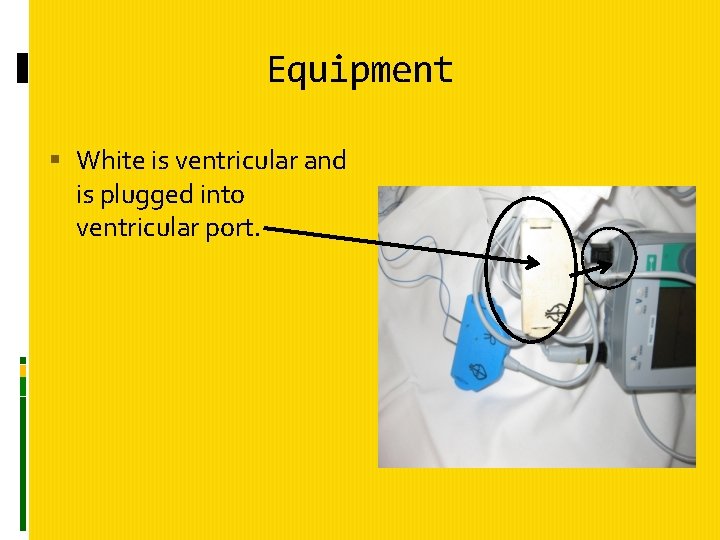
Equipment for insertion Connecting cable (Located in CICU or Cath Lab) Blue is ATRIAL White is VENTRICULAR Percutaneous introducer needle Introducer sheath with dilator Return
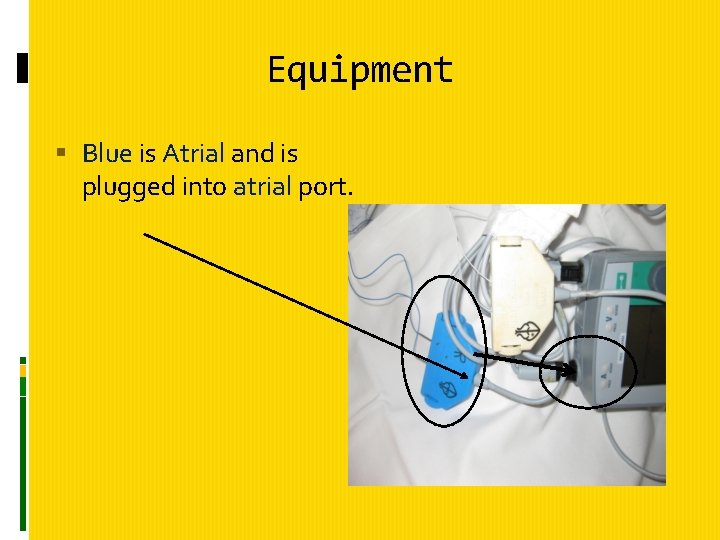
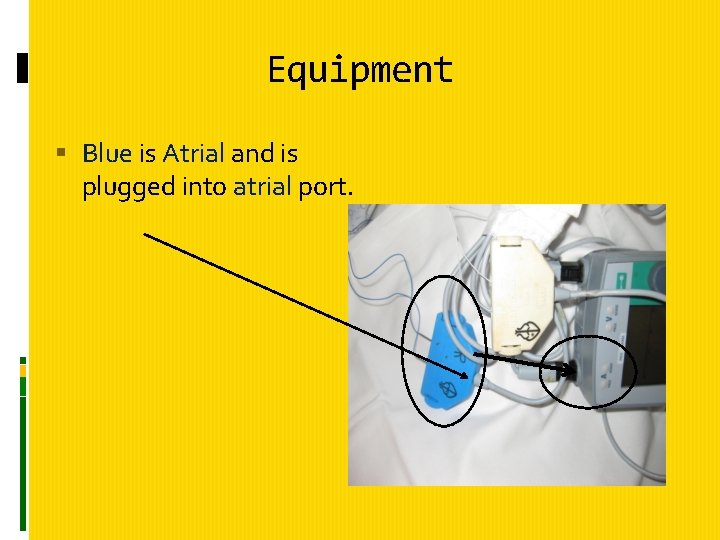
Equipment Blue is Atrial and is plugged into atrial port.
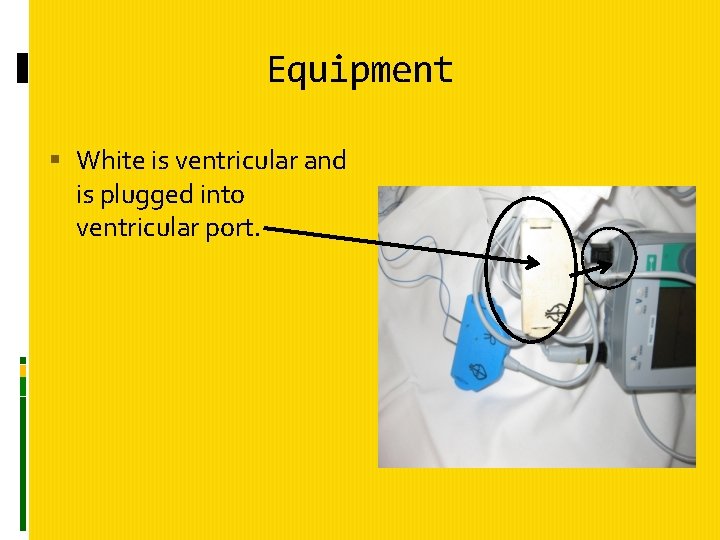
Equipment White is ventricular and is plugged into ventricular port.
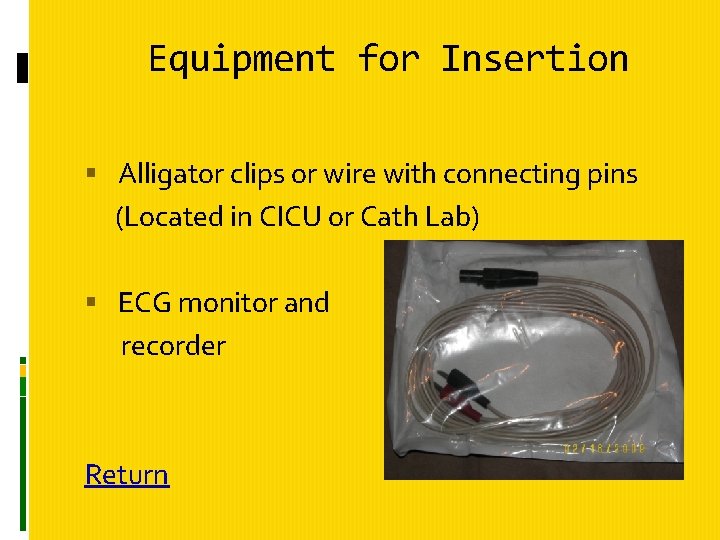
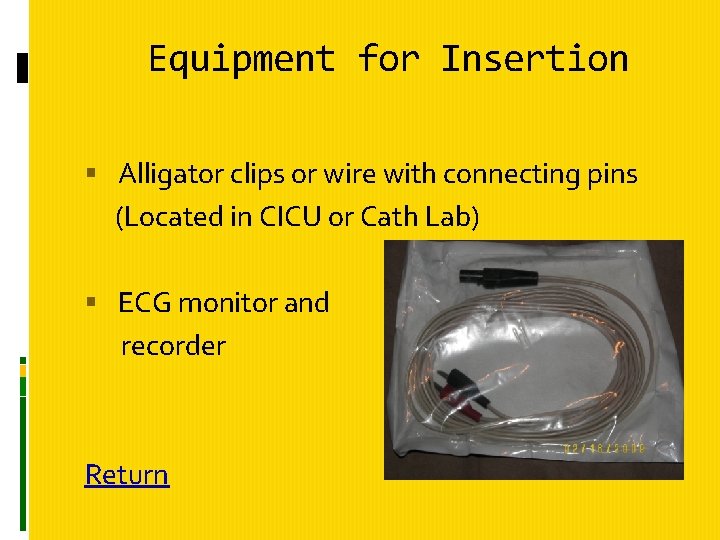
Equipment for Insertion Alligator clips or wire with connecting pins (Located in CICU or Cath Lab) ECG monitor and recorder Return
Additional Equipment that may be needed Emergency equipment 1. Crash cart 2. Intubation box 3. Drug box Fluoroscopy Lead aprons or sheets 12 -lead ECG machine Transcutaneous Ultasound Main Menu
Assessment Assess patient’s cardiac rhythm Determines need for invasive cardiac pacing. Assess patient’s hemodynamic response to dysrhythmia. Assessment determines the urgency of procedure. Review current medications Medications may be the cause of dysrhythmia Antidysrhythmics may alter the pacing threshold.
Assessment Review patient’s current laboratory studies including chemistry, electrolyte profile, arterial blood gasses, coagulation profile, platelet count and cardioactive medication levels. Determines if inserting pacemaker was precipitated by metabolic disturbances or medication toxicity.
Assessment Assess presence and position of central venous access Temporary transvenous pacing catheter is advanced through central venous circulation. If access already established, must ensure proper placement before pacing catheter advanced through circulatory system.
Assessment Main Menu Pre-procedure teaching to patient and family. Obtain informed consent In an emergency may not have time to obtain.
Procedure Connect patient to bedside monitoring system and monitor ECG continuously. Monitors intrinsic heart rate and rhythm to evaluate adequate rate and pacemaker function. Assess pacemaker functioning and insert new battery into generator. Attach connecting cable to pulse generator Connect “positive” cable to “positive “ on generator and “negative” cable to “negative” on generator.
Procedure Check placement of central venous access by x-ray before starting procedure. Time-out procedure Prepare insertion site by clipping hair close to skin in area surrounding insertion site. All personnel performing and assisting procedure should don masks, caps, goggles, sterile gowns and gloves. Gloves should be worn whenever the pacing electrodes are handled to prevent microshock.
Procedure Cleanse site with Chlorhexidine-based preparation Drape site with sterile drapes Administer local anesthetic to numb insertion site. Make percutaneous puncture through vein selected for procedure (jugular, subclavian, antecubital or femoral) Insert balloon-tipped catheter through introducer and advance pacing lead.

Procedure Inflate balloon when tip of pacing lead is in vena cava. Transcutaneous ultrasound or Fluoroscopy of chest during insertion procedure may assist in obtaining proper position. Advance pacing lead. Verify transvenous pacing lead placement by: �Use V lead of bedside monitor system �Connect patient to limb leads �Use an alligator clip or wire with connector pins.
Procedure Advance pacing lead Verify transvenous pacing lead placement by: Use V lead of bedside monitor or 12 -lead ECG Connect patient to limb leads Use alligator clip or wire with connector pins Attach V lead of ECG to negative electrode connector pin of pacing lead wire Set monitor system to record V lead continuously Observe ECG for ST-segment elevation in V lead Observe for left bundle-branch block pattern and left axis deviation.
Procedure After electrodes properly positioned, deflate balloon and connect external electrode pins to pulse generator via connecting cable. Positive and negative to respective terminals on generator. Set pacemaker settings and initiate pacing. See Quick Reference Guide for Nurses Physician orders desired rate Suture pacing lead in place to minimize risk of dislodgement. Apply sterile, occlusive dressing over site. Return
Procedure Main Menu Secure necessary equipment (hang generator on IV pole, strap to patient torso or hang from carrying device) Obtain chest x-ray. Pt needs to remain minimally active especially if lead is placed in extremity to avoid dislodgement of lead.
Patient Monitoring Monitor vital signs and hemodynamic response to pacing as patient condition warrants. Cardiac output should increase due to increasing heart rate or by overriding life-threatening dysrhythmias Evaluate ECG for presence of paced rhythm or resolution of initiating dyshythmia.
Patient Monitoring Monitor patient’s comfort. Administer analgesic or sedative as needed. Evaluate response to interventions Check and document sensitivity and threshold at least every 24 hours. Threshold should be checked by physician in high- risk patients. Ensures proper pacemaker functioning. Prevents unnecessarily high levels of energy delivery to myocardium.
Patient Monitoring Change dressing according to policy Use gloves to prevent microshock Cleanse with Chlorhexidine-based preparation. Apply dry, sterile dressing Record date of dressing change Monitor for other complications Embolus Thrombosis Perforation of myocardium Pneumothorax Hemothorax Phlebitis
Patient Monitioring Main Menu Monitor electrolytes Imbalances may precipitate dysrhythmias Ensure all connections are secure For proper sensing, impulse conduction, and to minimize risk of microshock conduction to heart. For questions or comments, please contact; Donna Reeves RN (CICU) or CICU supervisor/core 882 -2500
SOURCES 1. Diepenbrock, N. H. (2004). Quick reference to critical care (2 nd ed. ), (pp. 119 – 125). Philadelphia: Lippincott Williams & Wilkins. 2. Breuninger, C. , Follin, S. , et al. (Eds. ). (2001). Handbook of nursing procedures (pp. 603 – 604). Springhouse, PA: Springhouse Corporation. Main Menu