Team Strategies and Tools to Enhance Performance and









- Slides: 57
Team Strategies and Tools to Enhance Performance and Patient Safety
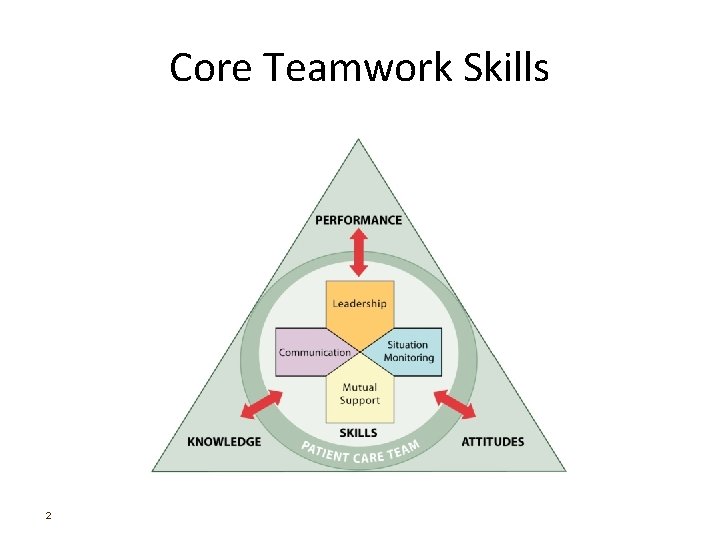
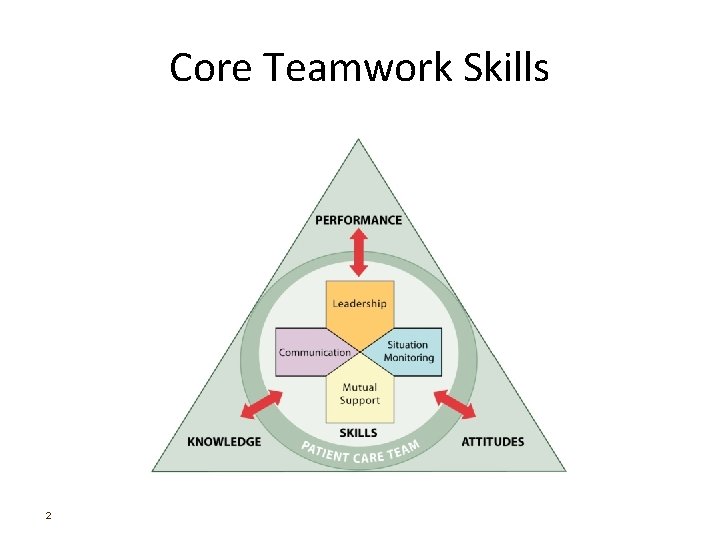
Core Teamwork Skills 2
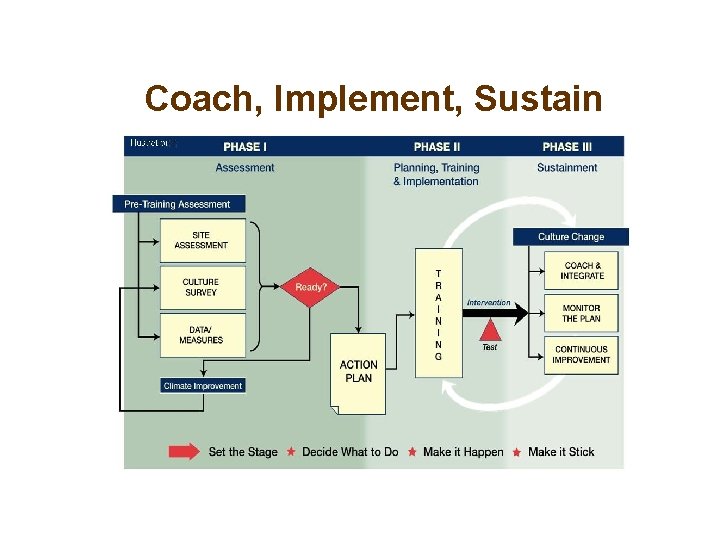
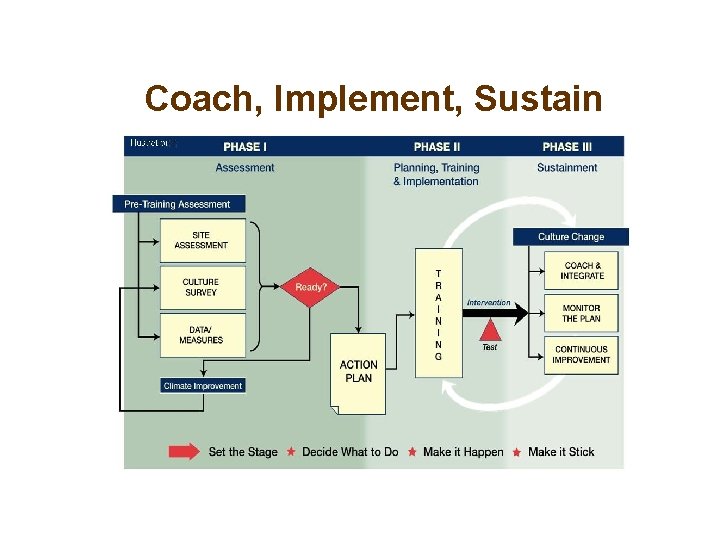
Coach, Implement, Sustain
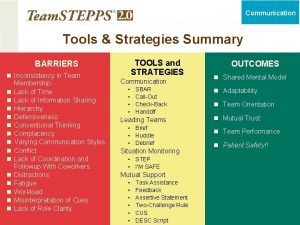
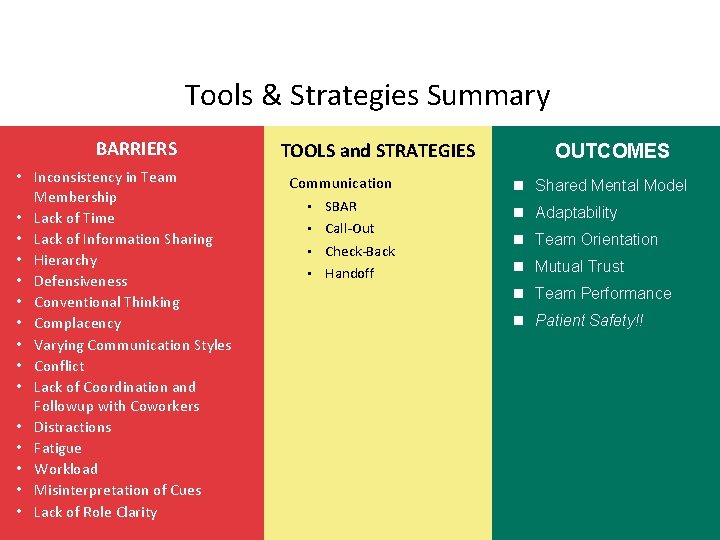
Barriers to Team Performance • Inconsistency in team membership • Lack of time • Lack of information sharing • Hierarchy • Defensiveness • Conventional thinking • Varying communication styles 4 • Conflict • Lack of coordination and followup • Distractions • Fatigue • Workload • Misinterpretation of cues • Lack of role clarity
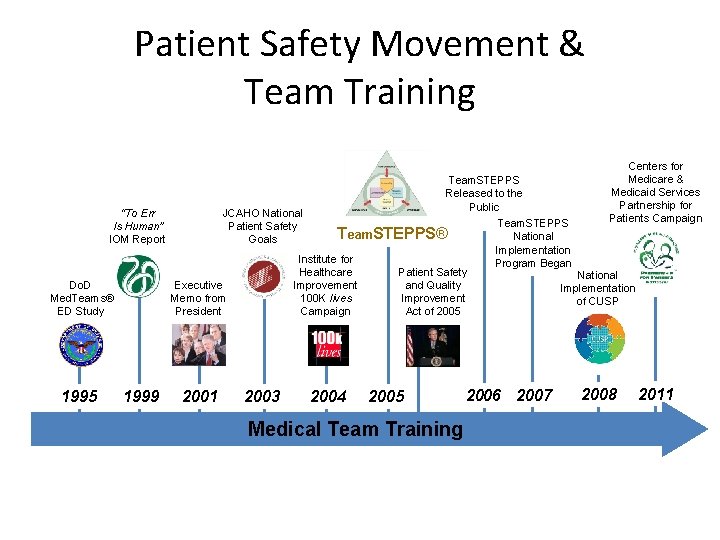
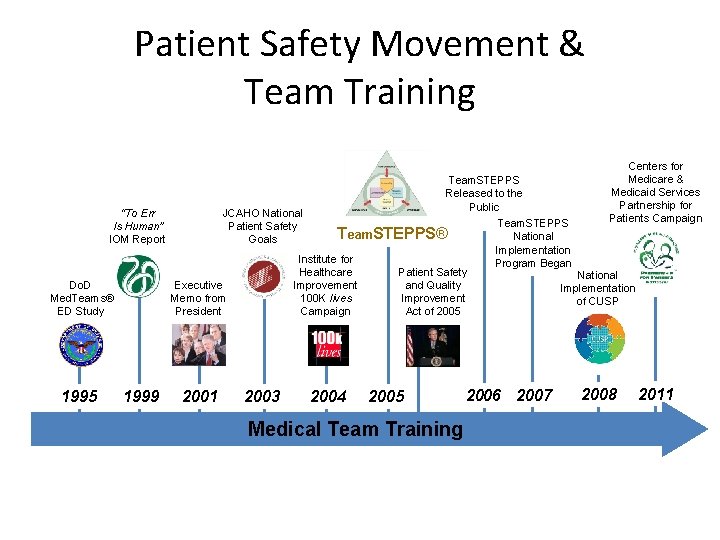
Patient Safety Movement & Team Training “To Err Is Human” IOM Report Do. D Med. Teams® ED Study 1995 JCAHO National Patient Safety Goals 2001 Team. STEPPS® Institute for Healthcare Improvement 100 K lives Campaign Executive Memo from President 1999 Team. STEPPS Released to the Public 2003 2004 Patient Safety and Quality Improvement Act of 2005 Medical Team Training Team. STEPPS National Implementation Program Began 2006 2007 Centers for Medicare & Medicaid Services Partnership for Patients Campaign National Implementation of CUSP 2008 2011
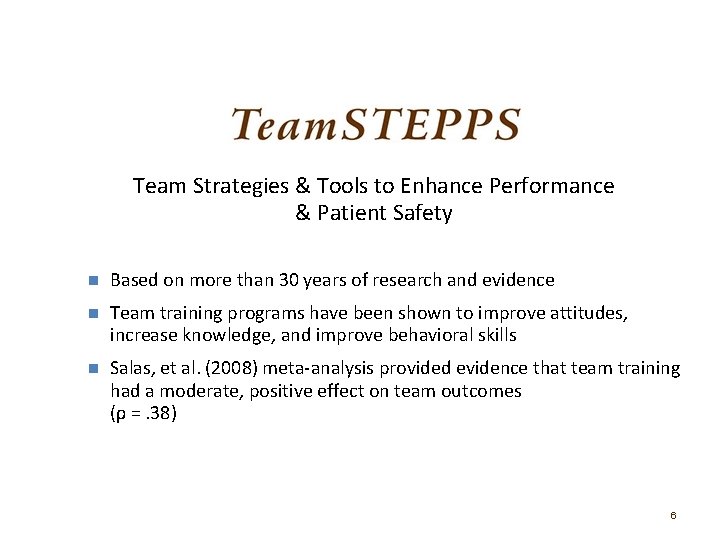
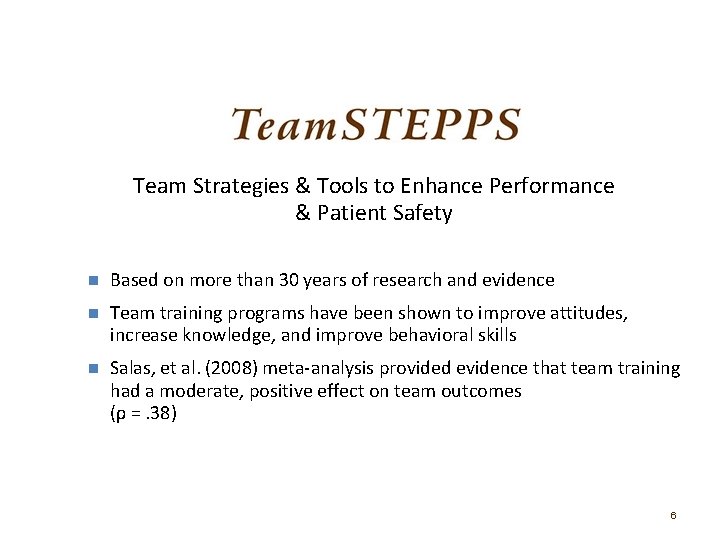
Team Strategies & Tools to Enhance Performance & Patient Safety n Based on more than 30 years of research and evidence n Team training programs have been shown to improve attitudes, increase knowledge, and improve behavioral skills n Salas, et al. (2008) meta-analysis provided evidence that team training had a moderate, positive effect on team outcomes (ρ =. 38) 6
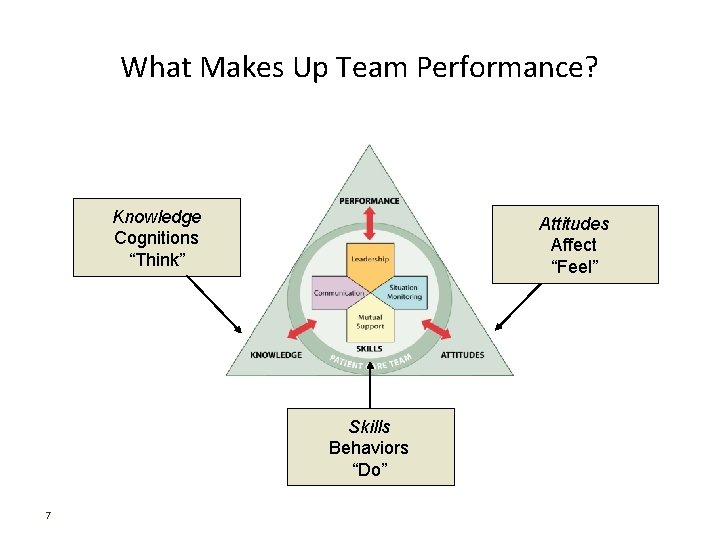
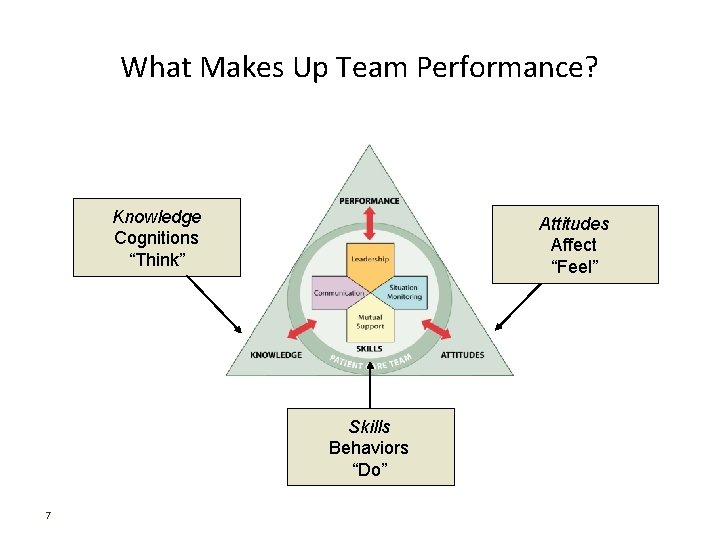
What Makes Up Team Performance? Knowledge Cognitions “Think” Attitudes Affect “Feel” Skills Behaviors “Do” 7
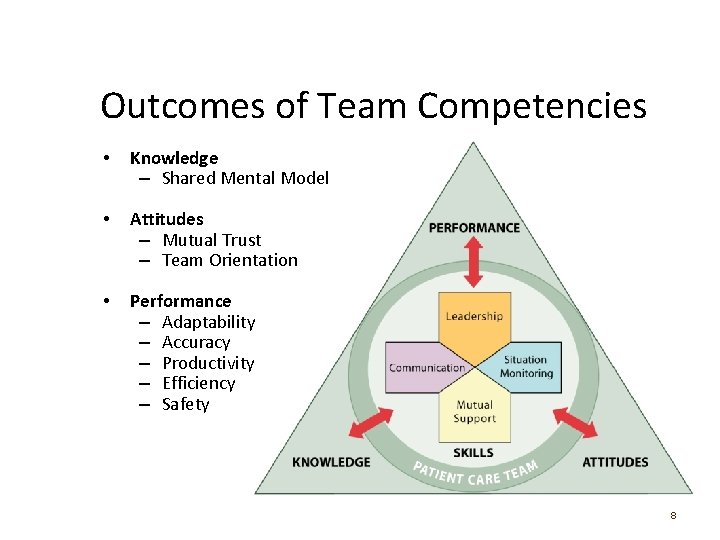
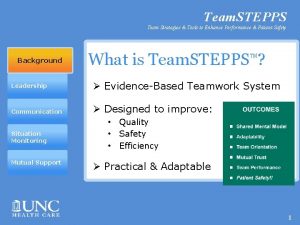
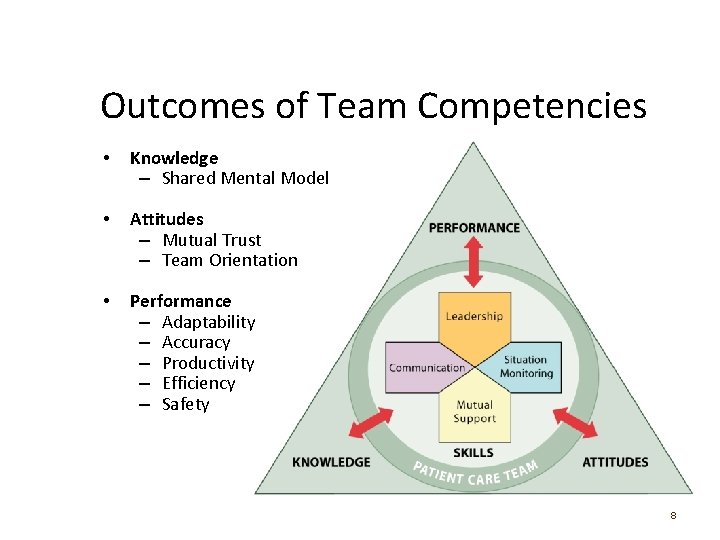
Outcomes of Team Competencies • Knowledge – Shared Mental Model • Attitudes – Mutual Trust – Team Orientation • Performance – Adaptability – Accuracy – Productivity – Efficiency – Safety 8
High-Performing Teams that perform well: – Hold shared mental models – Have clear roles and responsibilities – Have clear, valued, and shared vision – Optimize resources – Have strong team leadership – Engage in a regular discipline of feedback – Develop a strong sense of collective trust and confidence – Create mechanisms to cooperate and coordinate – Manage and optimize performance outcomes (Salas, et al. , 2004) 9
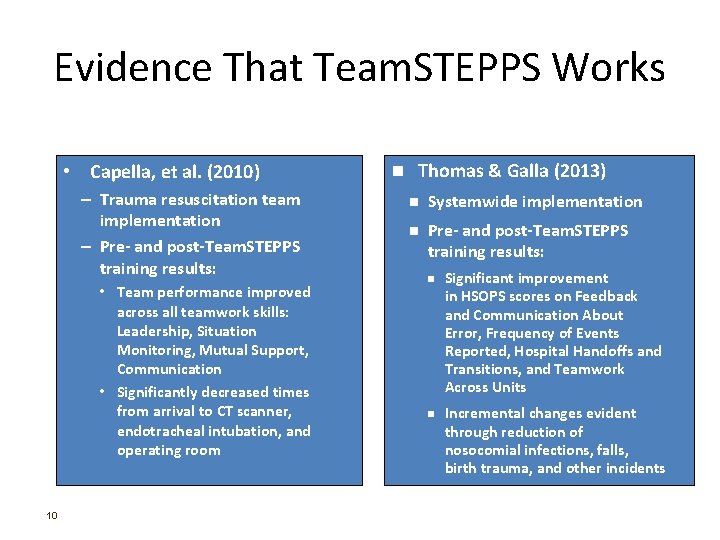
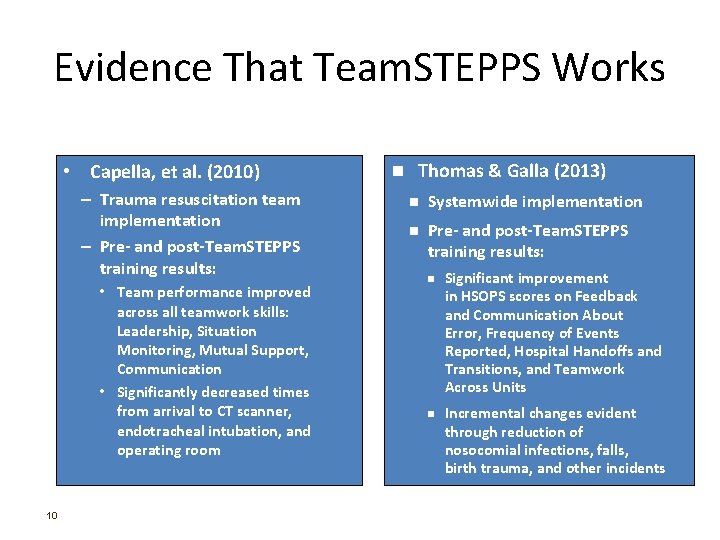
Evidence That Team. STEPPS Works • Capella, et al. (2010) – Trauma resuscitation team implementation – Pre- and post-Team. STEPPS training results: • Team performance improved across all teamwork skills: Leadership, Situation Monitoring, Mutual Support, Communication • Significantly decreased times from arrival to CT scanner, endotracheal intubation, and operating room 10 n Thomas & Galla (2013) n Systemwide implementation n Pre- and post-Team. STEPPS training results: n n Significant improvement in HSOPS scores on Feedback and Communication About Error, Frequency of Events Reported, Hospital Handoffs and Transitions, and Teamwork Across Units Incremental changes evident through reduction of nosocomial infections, falls, birth trauma, and other incidents
What is the patient safety issue your organization is facing that is linked to a problem with teamwork

Write down the names (or positions) of the people in your immediate work area or unit who contribute to successful patient care.






Team Structure Video
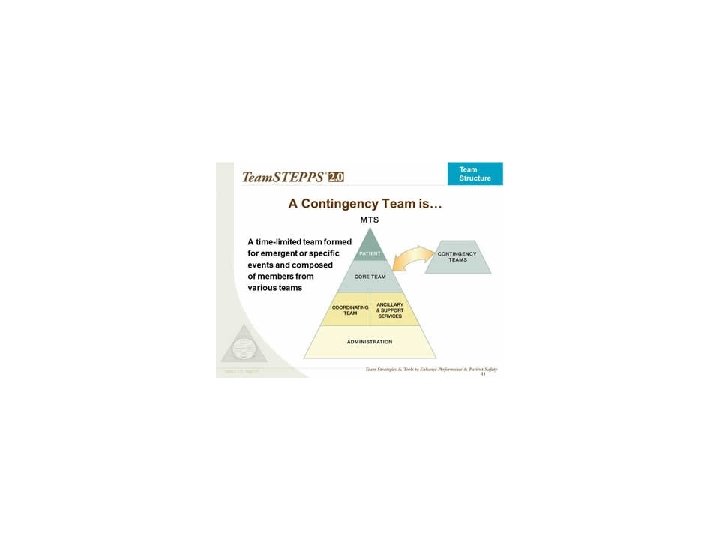
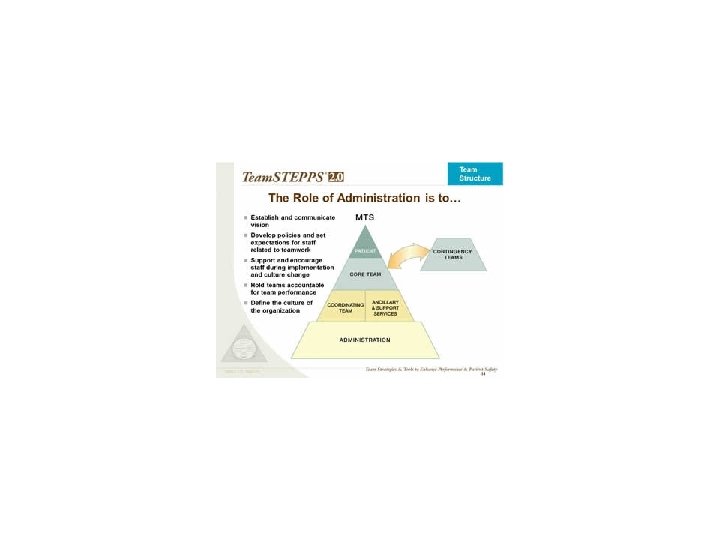
Video Analysis • What members of the following teams were involved in the scenario? – Core team. – Coordinating team. – Contingency team. – Ancillary and support services. • Where did the breakdowns occur between the components of this multi-team system? • What could the individuals involved in this scenario have done differently to produce a better outcome?

Communication Assumptions Fatigue Distractions HIPAA
Objectives • Describe how communication affects team processes and outcomes • Define effective communication • Identify communication challenges • Identify Team. STEPPS tools and strategies that can improve a team’s communication 28
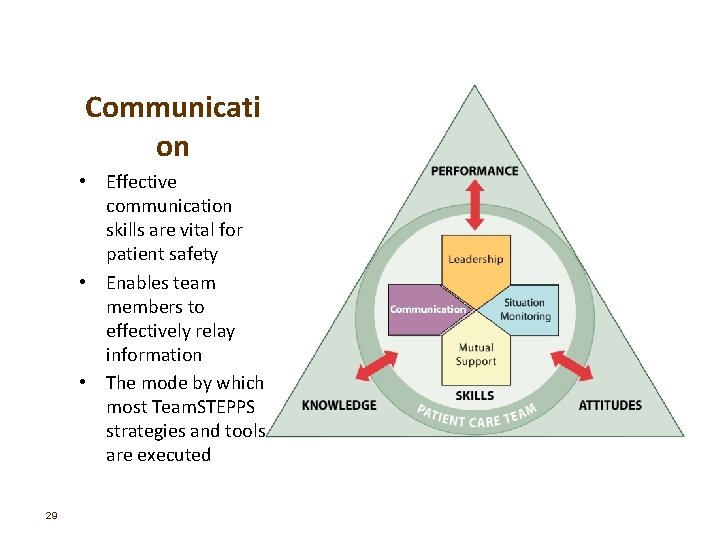
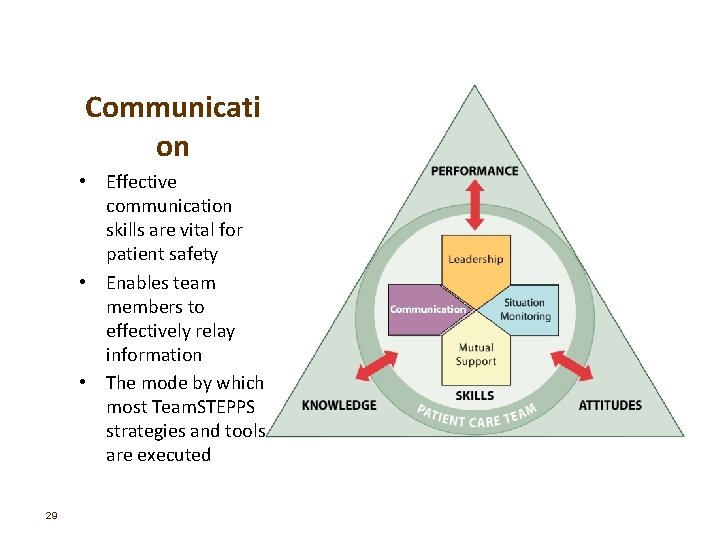
Communicati on • Effective communication skills are vital for patient safety • Enables team members to effectively relay information • The mode by which most Team. STEPPS strategies and tools are executed 29
Importance of Communication • Joint Commission data continues to demonstrate the importance of communication in patient safety – 1995 - 2005: Ineffective communication identified as root cause for nearly 66 percent of all reported sentinel events* – 2010 - 2013: Ineffective communication among top 3 root causes of sentinel events reported** * (JC Root Causes and Percentages for Sentinel Events (All Categories) January 1995−December 2005) ** (JC Sentinel Event Data (Root Causes by Event Type) 2004 -2012) 30
Communication is… • The process by which information is exchanged between individuals, departments, or organizations • The lifeline of the Core Team • Effective when it permeates every aspect of an organization Assumptions Fatigue Distractions HIPAA 31
Brief Clear Timely 32
Communication Challenges • • • 33 Language barrier Distractions Physical proximity Personalities Workload Varying communication styles Conflict Lack of information verification Shift change
Information Exchange Strategies • Situation – Background – Assessment – Recommendation (SBAR) • Call-Out • Check-Back • Handoffs 34
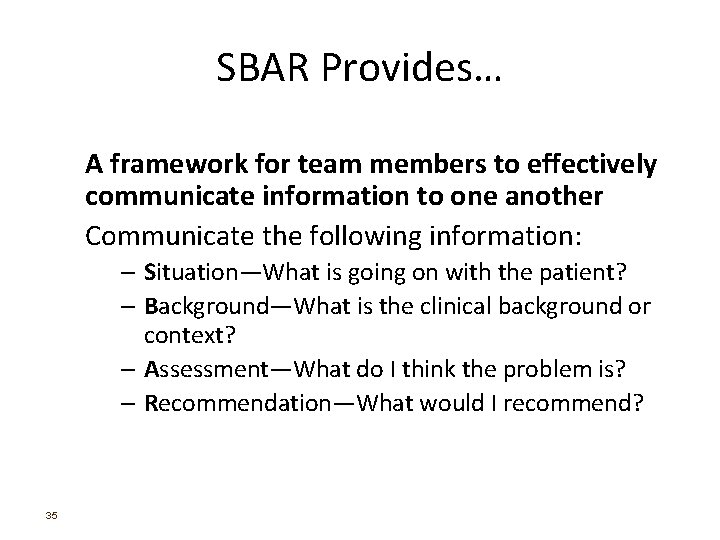
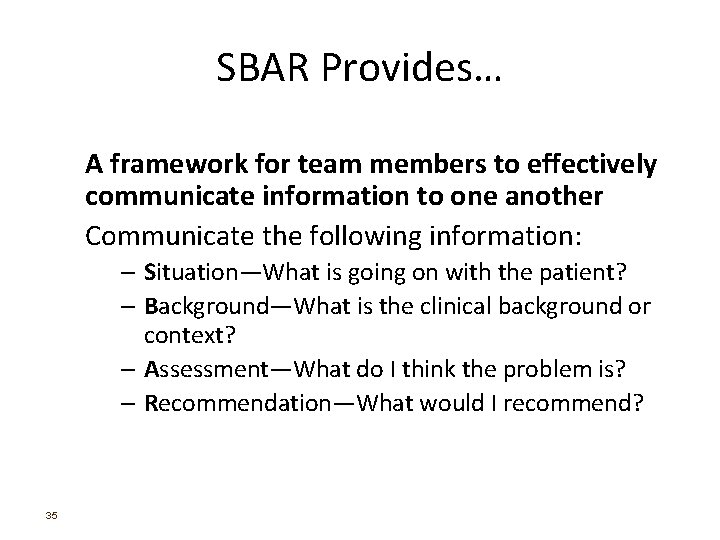
SBAR Provides… A framework for team members to effectively communicate information to one another Communicate the following information: – Situation―What is going on with the patient? – Background―What is the clinical background or context? – Assessment―What do I think the problem is? – Recommendation―What would I recommend? 35
Call-Out is… A strategy used to communicate important or critical information – It informs all team members simultaneously during emergency situations – It helps team members anticipate next steps 36
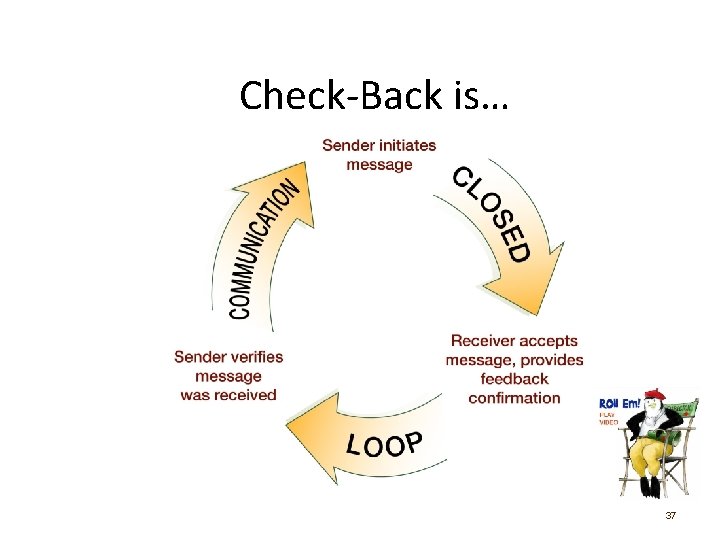
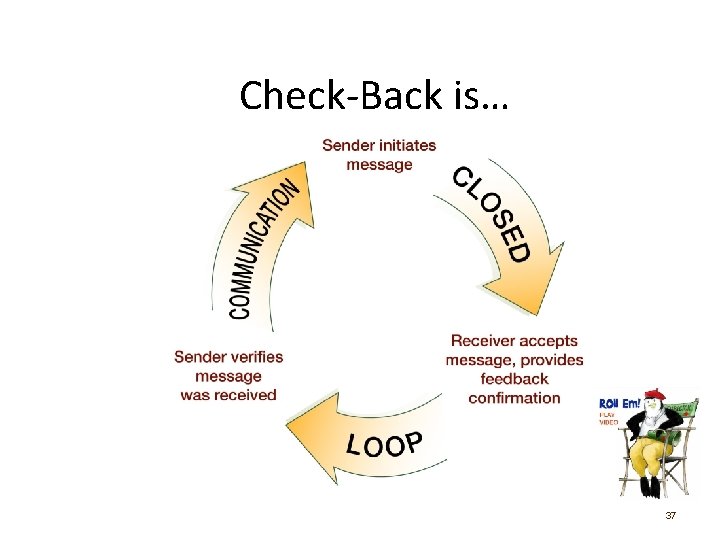
Check-Back is… 37

Handoff is… • The transfer of information during transitions in care across the continuum – Includes an opportunity to ask questions, clarify, and confirm 38
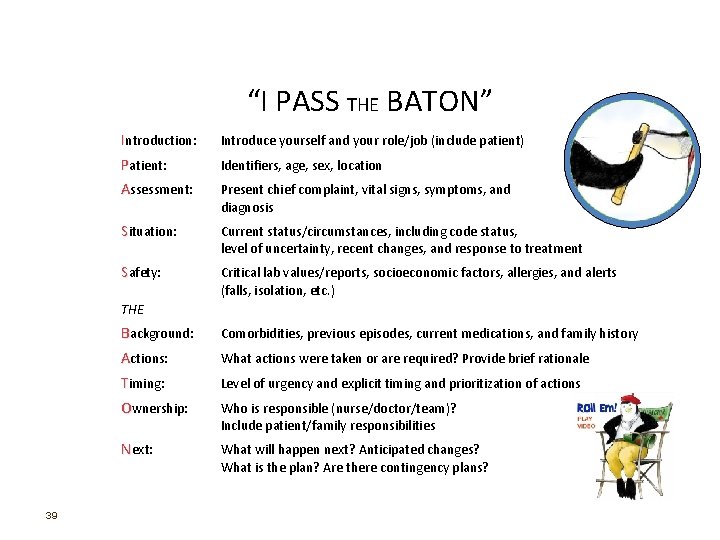
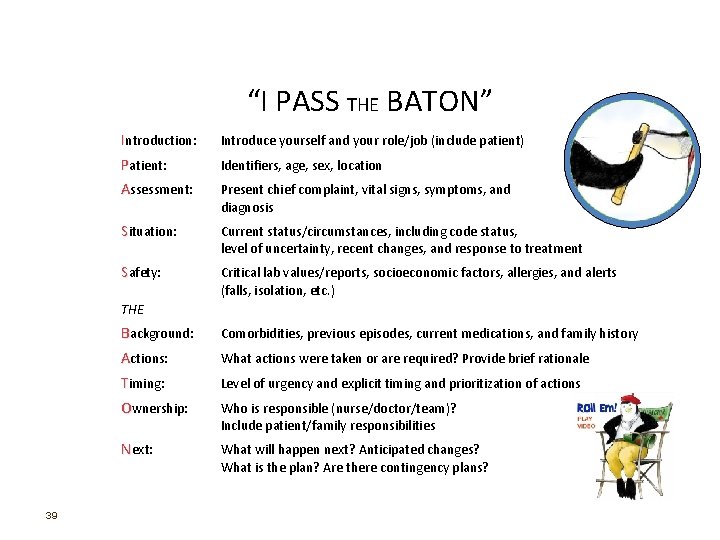
“I PASS THE BATON” Introduction: Introduce yourself and your role/job (include patient) Patient: Identifiers, age, sex, location Assessment: Present chief complaint, vital signs, symptoms, and diagnosis Situation: Current status/circumstances, including code status, level of uncertainty, recent changes, and response to treatment Safety: Critical lab values/reports, socioeconomic factors, allergies, and alerts (falls, isolation, etc. ) THE 39 Background: Comorbidities, previous episodes, current medications, and family history Actions: What actions were taken or are required? Provide brief rationale Timing: Level of urgency and explicit timing and prioritization of actions Ownership: Who is responsible (nurse/doctor/team)? Include patient/family responsibilities Next: What will happen next? Anticipated changes? What is the plan? Are there contingency plans?
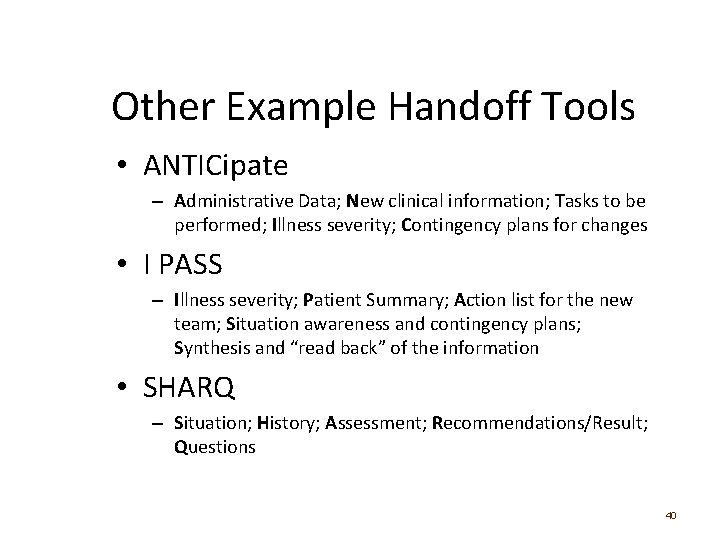
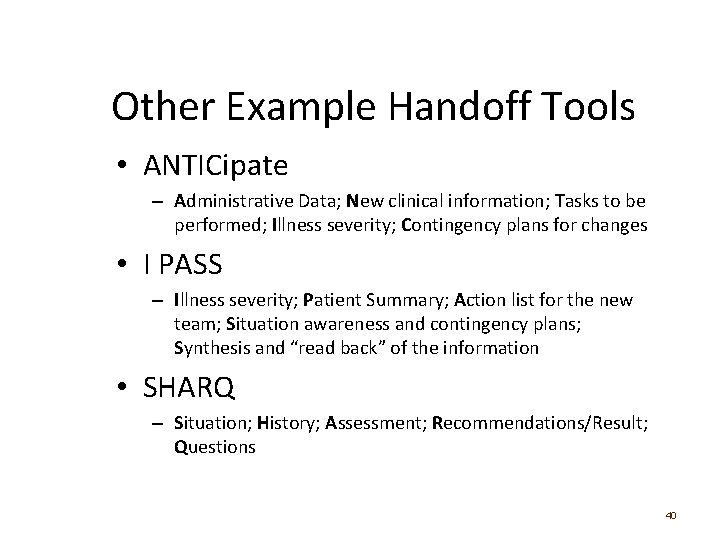
Other Example Handoff Tools • ANTICipate – Administrative Data; New clinical information; Tasks to be performed; Illness severity; Contingency plans for changes • I PASS – Illness severity; Patient Summary; Action list for the new team; Situation awareness and contingency plans; Synthesis and “read back” of the information • SHARQ – Situation; History; Assessment; Recommendations/Result; Questions 40
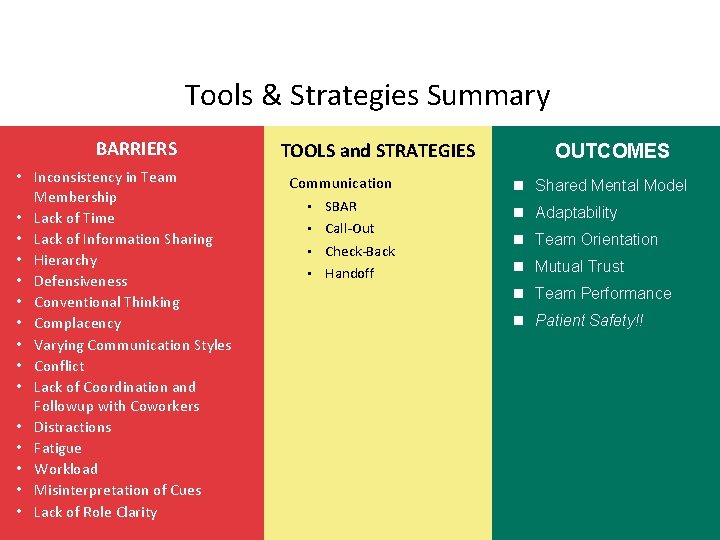
Tools & Strategies Summary BARRIERS • Inconsistency in Team Membership • Lack of Time • Lack of Information Sharing • Hierarchy • Defensiveness • Conventional Thinking • Complacency • Varying Communication Styles • Conflict • Lack of Coordination and Followup with Coworkers • Distractions • Fatigue • Workload • Misinterpretation of Cues • Lack of Role Clarity 41 TOOLS and STRATEGIES Communication • SBAR • Call-Out • Check-Back • Handoff OUTCOMES n Shared Mental Model n Adaptability n Team Orientation n Mutual Trust n Team Performance n Patient Safety!!
Applying Team. STEPPS Exercise 1. Is your teamwork issue related to communication? 2. If yes, what is the communication issue? 3. Which Team. STEPPS tools and/or strategies might you consider implementing to address the issue? 42
Leading Teams
Objectives • Describe how leadership affects team processes and outcomes • Identify different types of team leaders • Describe the activities involved in successfully leading teams • Describe the tools for leading teams, including briefs, huddles, and debriefs • Apply the tools for leading teams to specific clinical scenarios 44
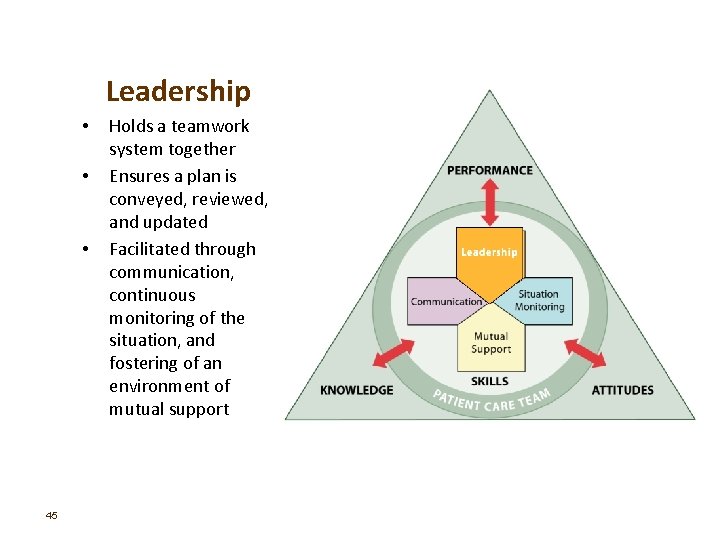
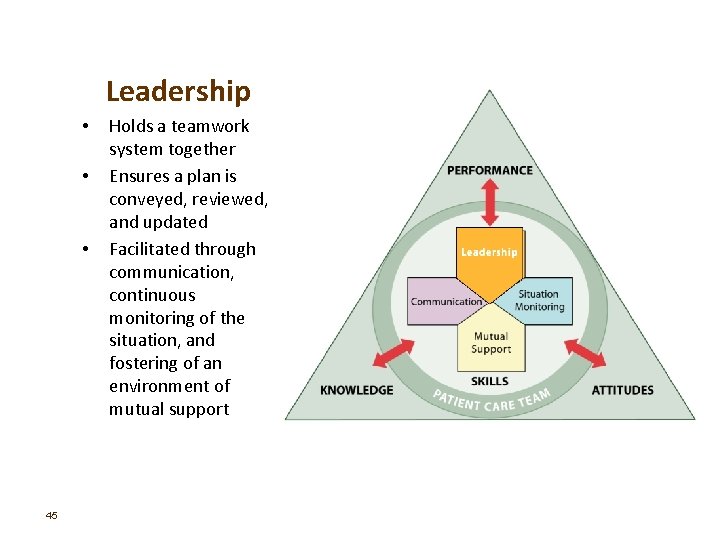
Leadership • • • 45 Holds a teamwork system together Ensures a plan is conveyed, reviewed, and updated Facilitated through communication, continuous monitoring of the situation, and fostering of an environment of mutual support
Types of Team Leaders • Designated – The person assigned to lead and organize a team, establish clear goals, and facilitate open communication and teamwork among team members • Situational – Any team member who has the skills to manage the situation at hand 46
Effective Team Leaders • • • 47 Define, assign, share, monitor, and modify a plan Review the team’s performance Establish “rules of engagement” Manage and allocate resources effectively Provide feedback regarding assigned responsibilities and progress toward the goal Facilitate information sharing Encourage team members to assist one another Facilitate conflict resolution Model effective teamwork
Defining the Plan • When developing a plan, team leaders should consider: – Time – How much time is available to complete all the necessary tasks and activities? – People – Do the available staff have the necessary knowledge and skills to perform their roles? – Equipment – Is the necessary equipment available and working? – Information – Has all of the necessary information been collected and reviewed? 48
Case Study Discussion After attending Team. STEPPS Master Training, a physician and nurse leader in a Level I Trauma Center decide that trauma resuscitations could be more effectively conducted. Currently, when a trauma alert is called to indicate the pending arrival of a severely injured patient, more staff show up to the trauma bay than needed, necessary equipment is sometimes missing or not functioning properly, and the lead trauma physician often shows up just as EMS is bringing the patient into the trauma bay. The newly trained Master Trainers observe that these practices have led to confusion and chaos that put patients at risk and result in valuable time being lost. 49
Assigning Tasks and Responsibilities • Determine the tasks and roles to be assigned • Determine which roles must be filled and allocate tasks appropriately • Communicate clear expectations of what team members need to do • Request feedback 50
Sharing the Plan: Briefs • A team briefing is an effective strategy for sharing the plan • Briefs should help: – Form the team – Designate team roles and responsibilities – Establish climate and goals – Engage team in short- and long-term planning 51
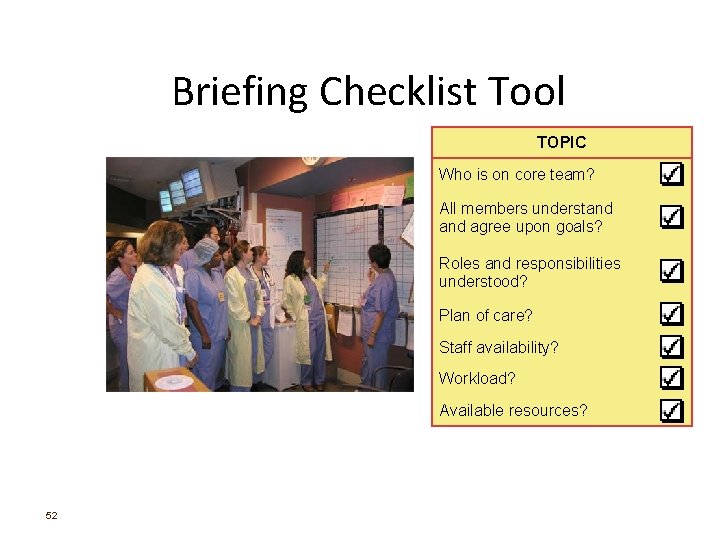
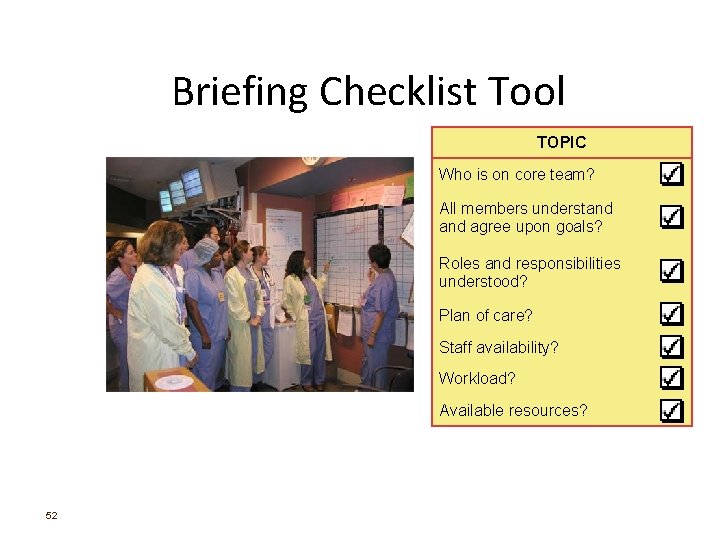
Briefing Checklist Tool TOPIC Who is on core team? All members understand agree upon goals? Roles and responsibilities understood? Plan of care? Staff availability? Workload? Available resources? 52
Exercise: Briefing INSTRUCTIONS: 1. Identify core group members within your work area, or organization. 2. Identify when, why, and where briefings might be conducted. Note who should lead the brief and who should participate. 3. Develop a checklist for guiding the brief. 4. Discuss what outcomes you expect to see as a result of implementing briefs. 5. At the end of the exercise, present and discuss your plans with the group. 53
Monitoring & Modifying the Plan: Huddle Problem Solving – Hold ad hoc, “touch base” meetings to regain situation awareness – Discuss critical issues and emerging events – Anticipate outcomes and likely contingencies – Assign resources – Express concerns 54
Reviewing the Team’s Performance: Debrief Process Improvement • • Brief, informal information exchange and feedback sessions Occur after an event or shift Designed to improve teamwork skills Designed to improve outcomes – – 55 An accurate recounting of key events Analysis of why the event occurred Discussion of lessons learned and reinforcement of successes Revised plan to incorporate lessons learned
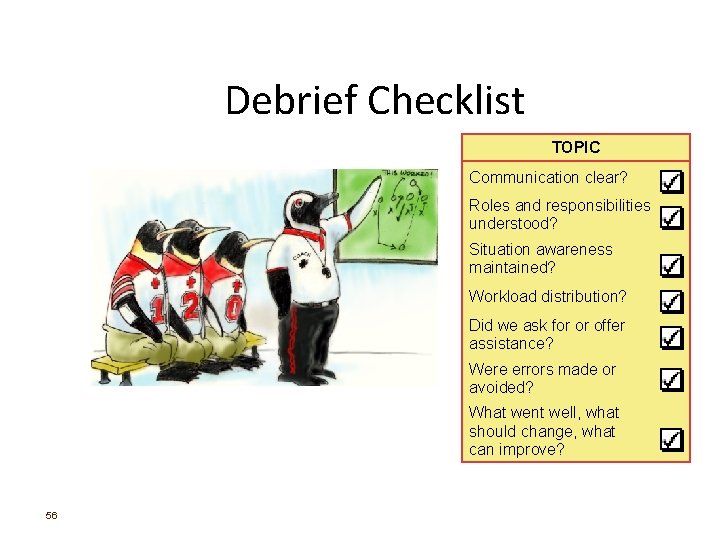
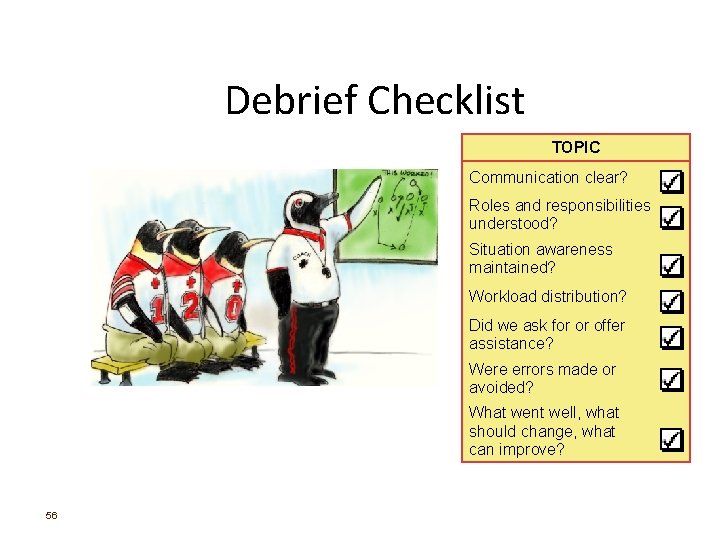
Debrief Checklist TOPIC Communication clear? Roles and responsibilities understood? Situation awareness maintained? Workload distribution? Did we ask for or offer assistance? Were errors made or avoided? What went well, what should change, what can improve? 56
Debrief Video 57
 Grammar to enrich and enhance writing
Grammar to enrich and enhance writing Fashion cycle
Fashion cycle Enhance an image
Enhance an image Cspnet
Cspnet Vcosmetics
Vcosmetics Enhance an image
Enhance an image Enhance life
Enhance life Enhance life
Enhance life A salad that stimulates appetite
A salad that stimulates appetite Can hypnosis enhance recall of forgotten events
Can hypnosis enhance recall of forgotten events Writing assessment strategies
Writing assessment strategies Team problem solving strategies
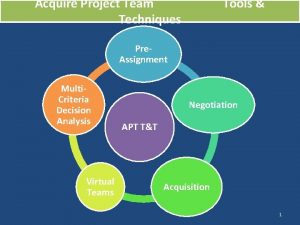
Team problem solving strategies Acquire resources tools and techniques
Acquire resources tools and techniques Going native project management
Going native project management Team spirit becomes team infatuation
Team spirit becomes team infatuation The white team cheers for the blue team, just like
The white team cheers for the blue team, just like Spms cycle
Spms cycle Team performance definition
Team performance definition Team performance models
Team performance models Sewing tools measuring tools
Sewing tools measuring tools Oracle performance tuning tutorial
Oracle performance tuning tutorial Network performance measurement tools
Network performance measurement tools Siebel performance monitoring
Siebel performance monitoring Network performance measurement tools
Network performance measurement tools Star error prevention tool
Star error prevention tool Performance engineering tools
Performance engineering tools Behaviorally anchored rating scale
Behaviorally anchored rating scale Performance appraisal process
Performance appraisal process All performance attributes designated as joint performance
All performance attributes designated as joint performance Translation loss definition
Translation loss definition New product development and product life cycle strategies
New product development and product life cycle strategies Security strategies in windows platforms and applications
Security strategies in windows platforms and applications Security strategies in windows platforms and applications
Security strategies in windows platforms and applications Types of readings
Types of readings Chapter 17 promotional concepts and strategies
Chapter 17 promotional concepts and strategies Procurement and outsourcing strategies
Procurement and outsourcing strategies Factors contributing to organizational politics
Factors contributing to organizational politics Direct investment and collaborative strategies
Direct investment and collaborative strategies What is intensive reading
What is intensive reading Examples of ifsp outcomes and strategies
Examples of ifsp outcomes and strategies Writing strategies and ethical considerations
Writing strategies and ethical considerations Chapter 7 strategic management
Chapter 7 strategic management Mis issues in strategy implementation
Mis issues in strategy implementation Implementing strategies: management and operations issues
Implementing strategies: management and operations issues Price signaling in mature industries happens when:
Price signaling in mature industries happens when: Packaging different products or services together
Packaging different products or services together The central instrument for directing and coordinating
The central instrument for directing and coordinating Intensive integrative and diversification growth strategies
Intensive integrative and diversification growth strategies Pricing and distribution strategies
Pricing and distribution strategies Contrast trade promotions and consumer sales promotions
Contrast trade promotions and consumer sales promotions Developing price strategies and programs
Developing price strategies and programs Licensing franchising and other contractual strategies
Licensing franchising and other contractual strategies Toyota brand hierarchy
Toyota brand hierarchy Designing and implementing brand marketing programs
Designing and implementing brand marketing programs Counseling strategies and techniques
Counseling strategies and techniques Aggregate planning strategies
Aggregate planning strategies Worldwide product division structure
Worldwide product division structure Toeic reading strategies
Toeic reading strategies