Team STEPPS Everywhere Implementing at the System Level















- Slides: 77
Team. STEPPS Everywhere: Implementing at the System Level Slides may not be reproduced without permission
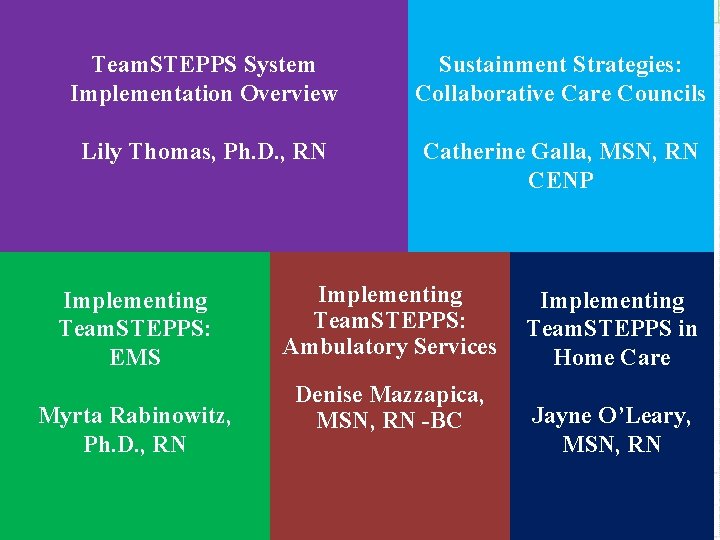
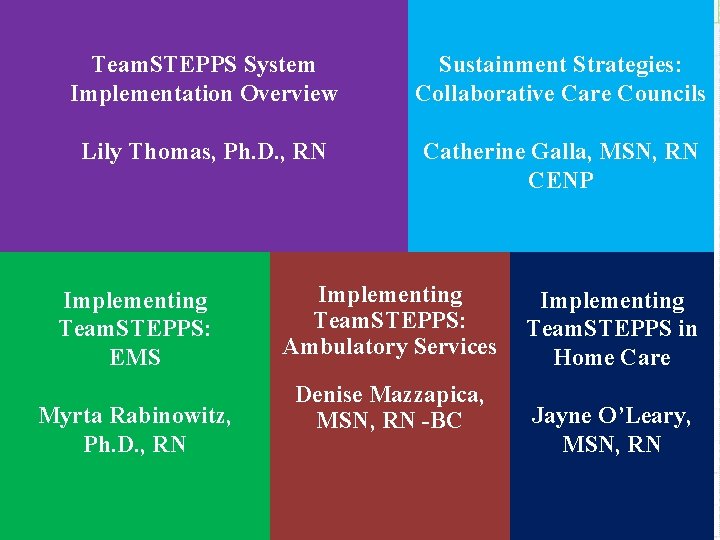
Team. STEPPS System Implementation Overview Sustainment Strategies: Collaborative Care Councils Lily Thomas, Ph. D. , RN Catherine Galla, MSN, RN CENP Implementing Team. STEPPS: EMS Myrta Rabinowitz, Ph. D. , RN Implementing Team. STEPPS: Ambulatory Services Denise Mazzapica, MSN, RN -BC Implementing Team. STEPPS in Home Care Jayne O’Leary, MSN, RN 2
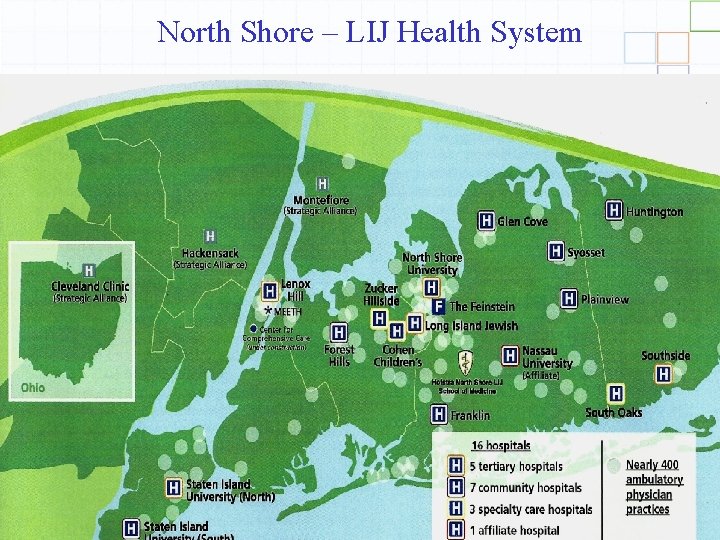
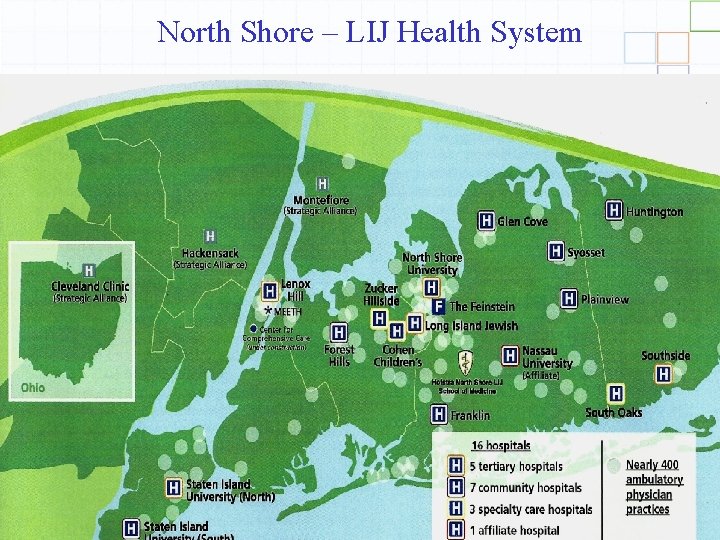
North Shore – LIJ Health System 3
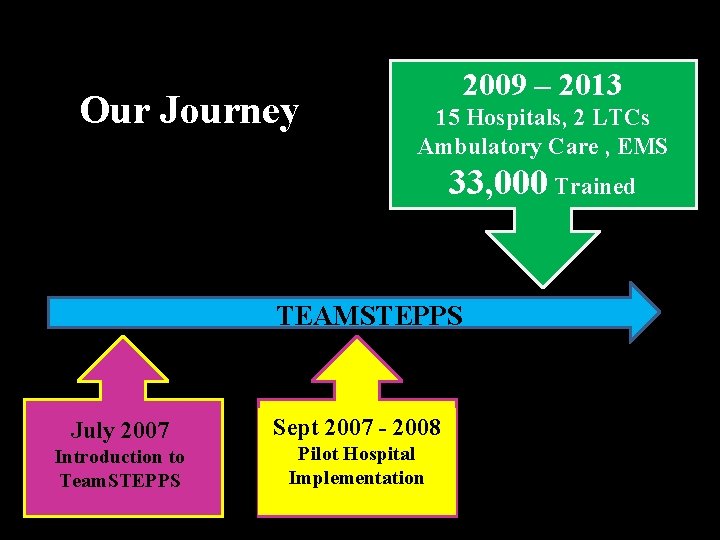
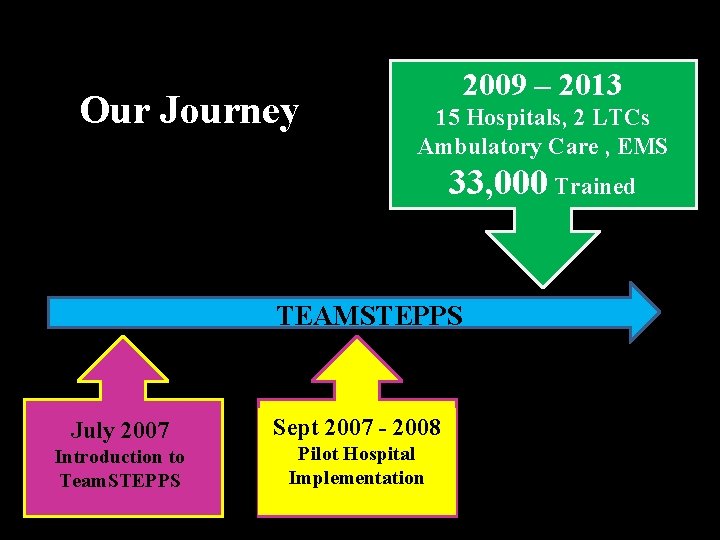
Our Journey 2009 – 2013 15 Hospitals, 2 LTCs Ambulatory Care , EMS 33, 000 Trained TEAMSTEPPS July 2007 Introduction to Team. STEPPS Sept 2007 - 2008 Pilot Hospital Implementation

NSLIJHS IFN 5
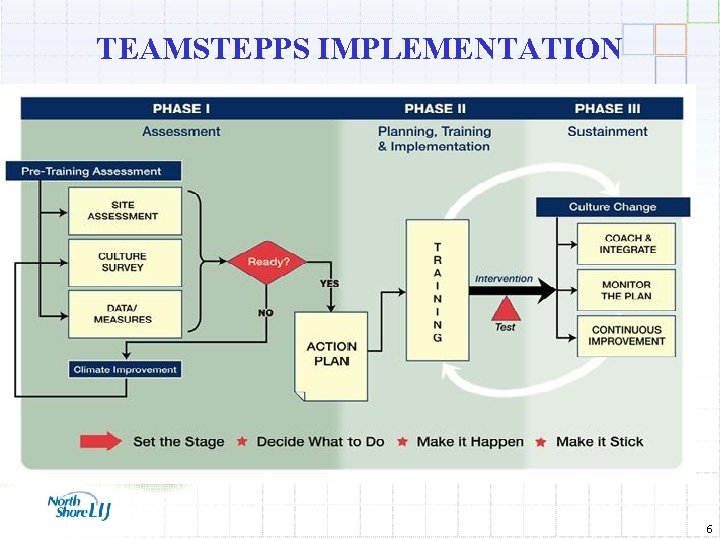
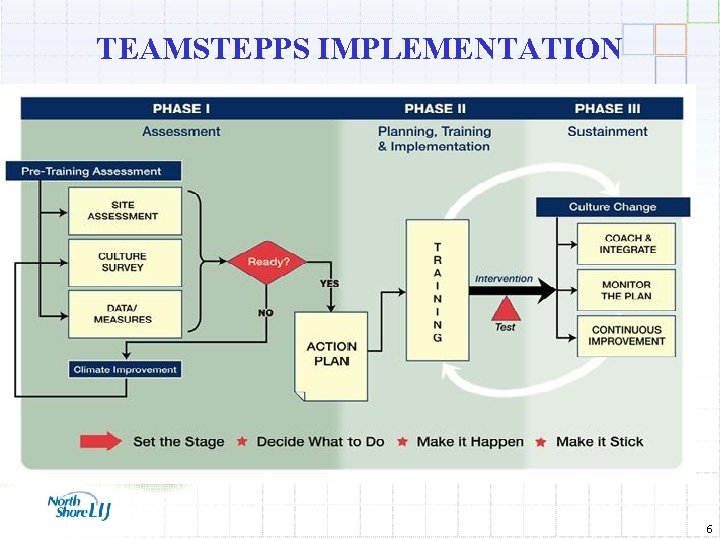
TEAMSTEPPS IMPLEMENTATION 6
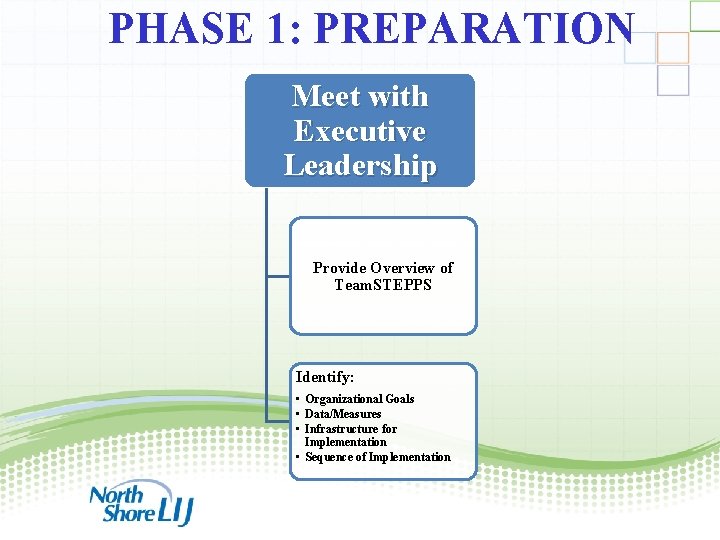
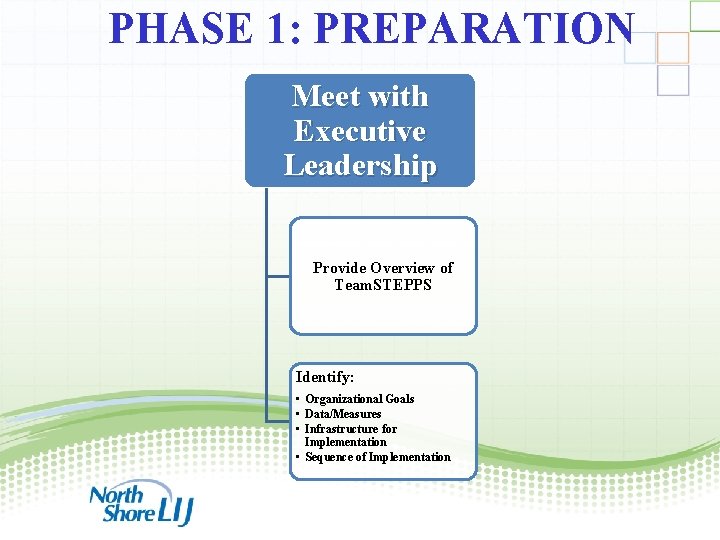
PHASE 1: PREPARATION Meet with Executive Leadership Provide Overview of Team. STEPPS Identify: • Organizational Goals • Data/Measures • Infrastructure for Implementation • Sequence of Implementation 7
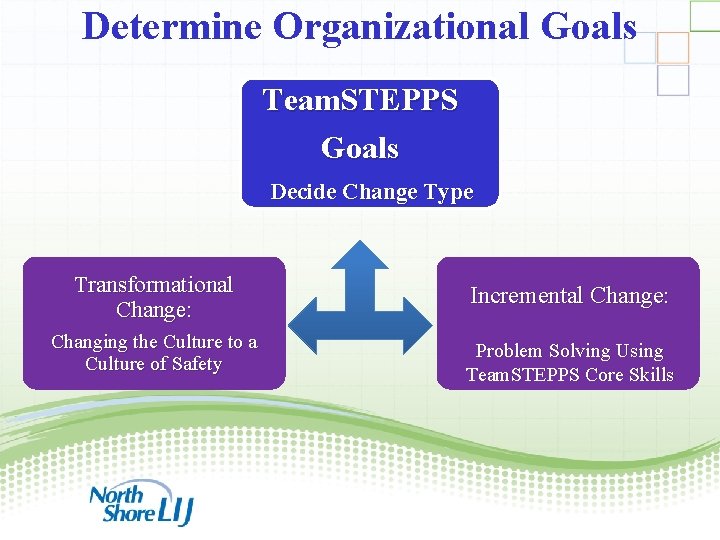
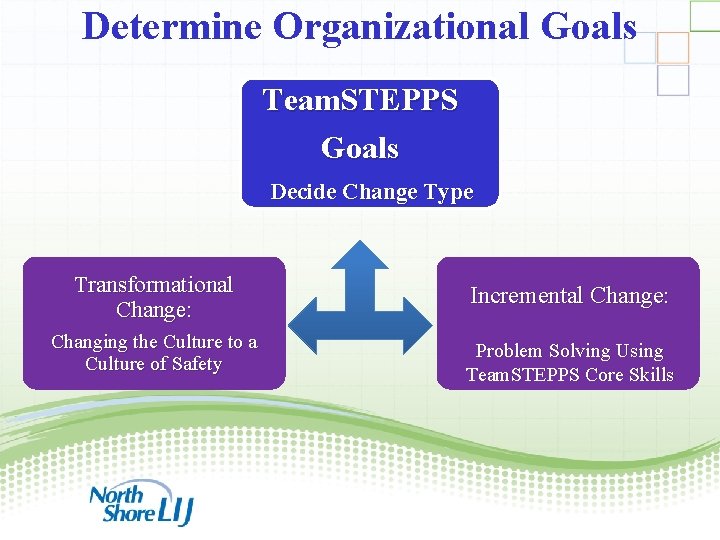
Determine Organizational Goals Team. STEPPS Goals Decide Change Type Transformational Change: Changing the Culture to a Culture of Safety Incremental Change: Problem Solving Using Team. STEPPS Core Skills 8
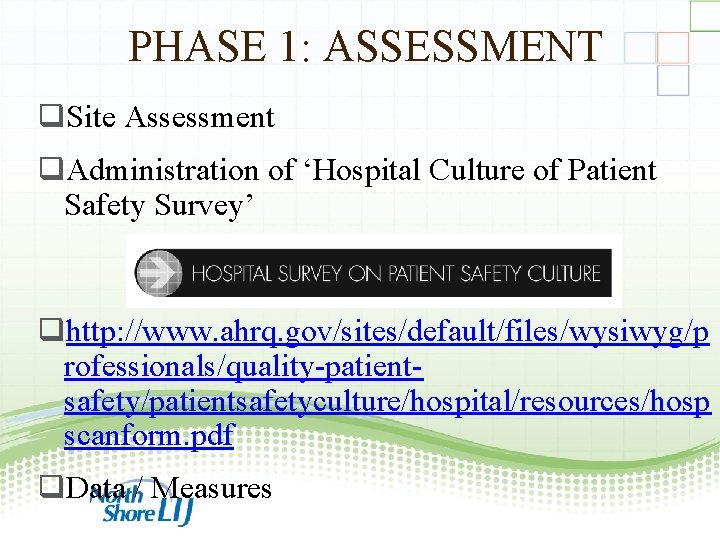
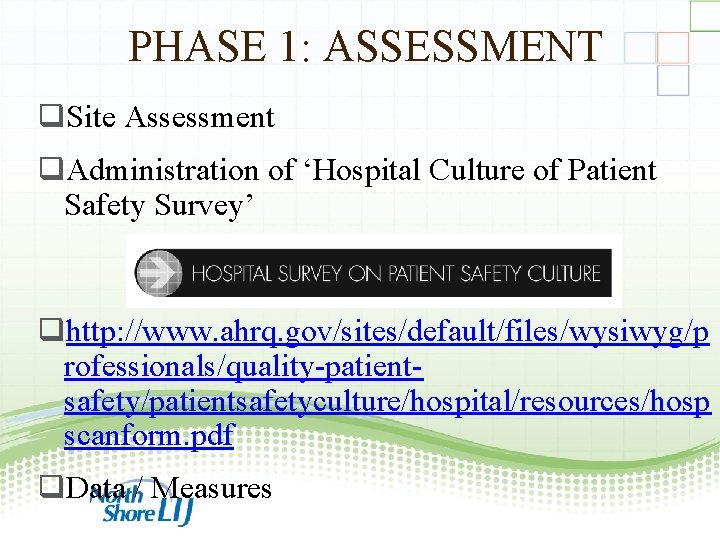
PHASE 1: ASSESSMENT q. Site Assessment q. Administration of ‘Hospital Culture of Patient Safety Survey’ qhttp: //www. ahrq. gov/sites/default/files/wysiwyg/p rofessionals/quality-patientsafety/patientsafetyculture/hospital/resources/hosp scanform. pdf q. Data / Measures 9
Begin with the End in Mind! 10
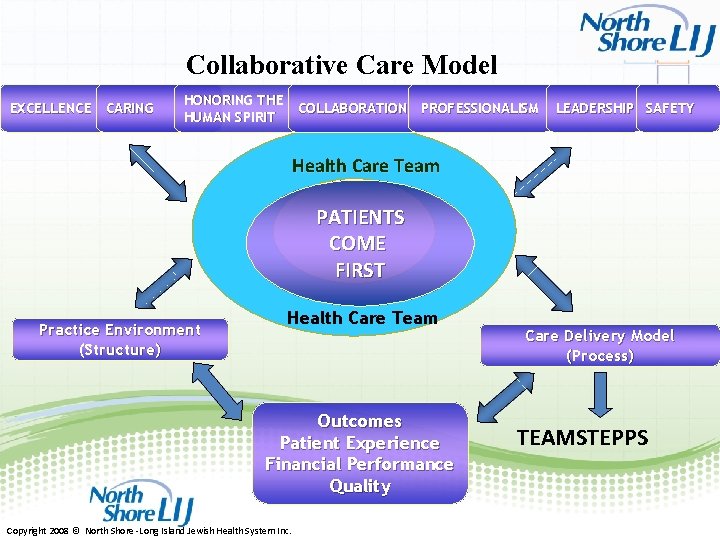
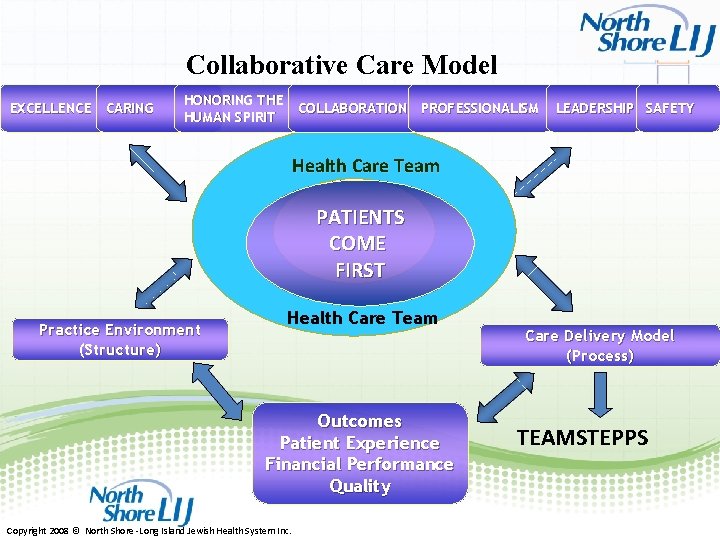
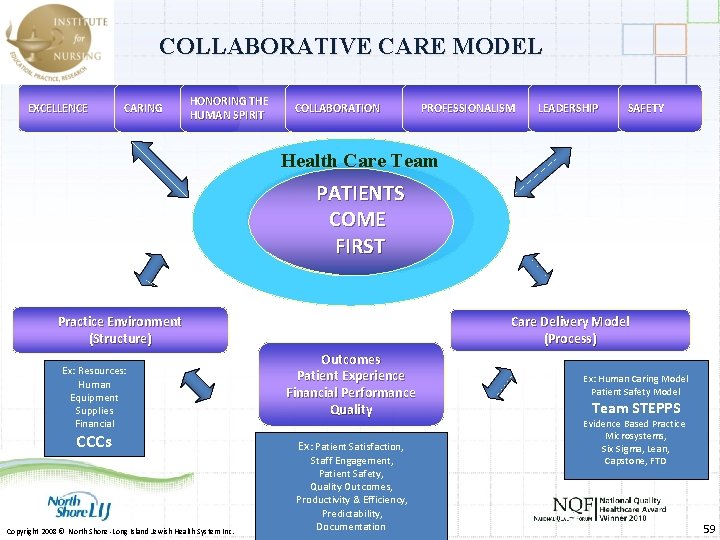
Collaborative Care Model EXCELLENCE CARING HONORING THE COLLABORATION PROFESSIONALISM HUMAN SPIRIT LEADERSHIP SAFETY Health Care Team PATIENTS COME FIRST Practice Environment (Structure) Health Care Team Outcomes Patient Experience Financial Performance Quality Copyright 2008 © North Shore -Long Island Jewish Health System Inc. Care Delivery Model (Process) TEAMSTEPPS 11
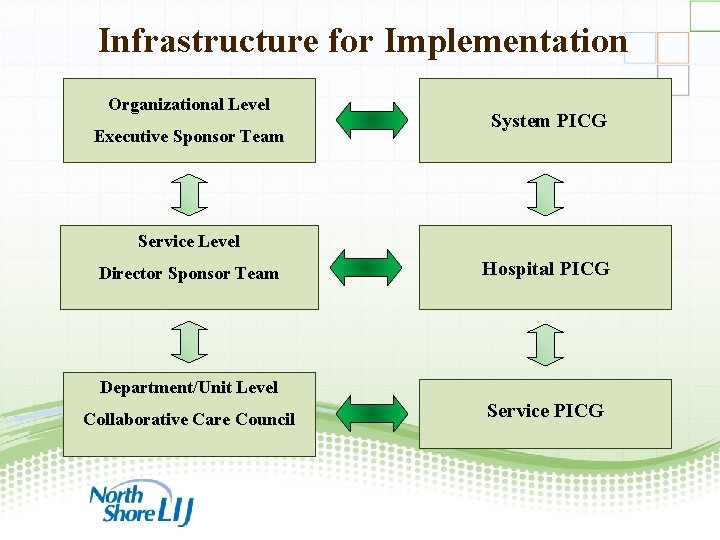
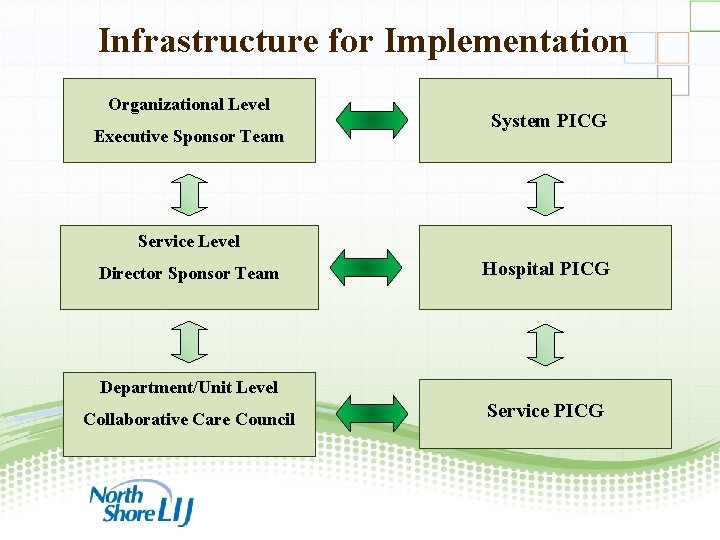
Infrastructure for Implementation Organizational Level Executive Sponsor Team System PICG Service Level Director Sponsor Team Hospital PICG Department/Unit Level Collaborative Care Council Service PICG 12

ACTION PLANNING & IMPLEMENTATION 13
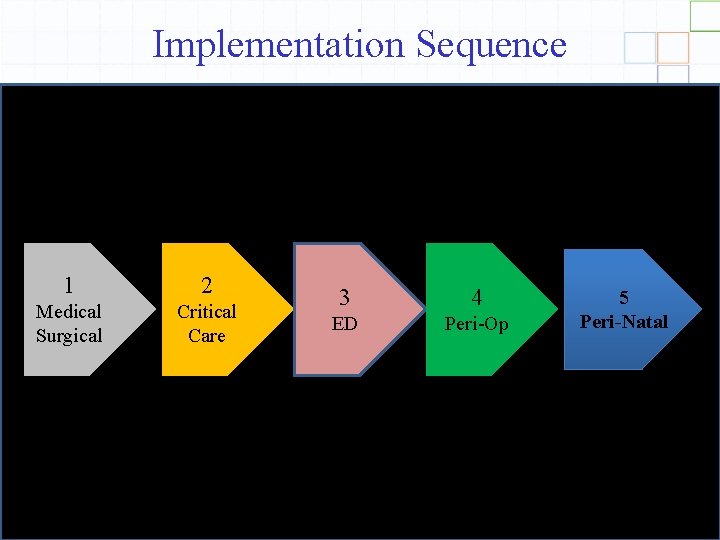
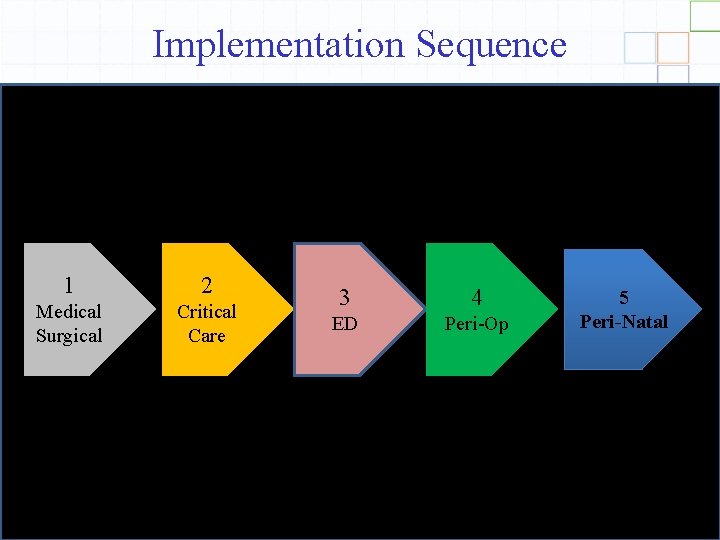
Implementation Sequence 1 2 Medical Surgical Critical Care 3 4 ED Peri-Op 5 Peri-Natal 14
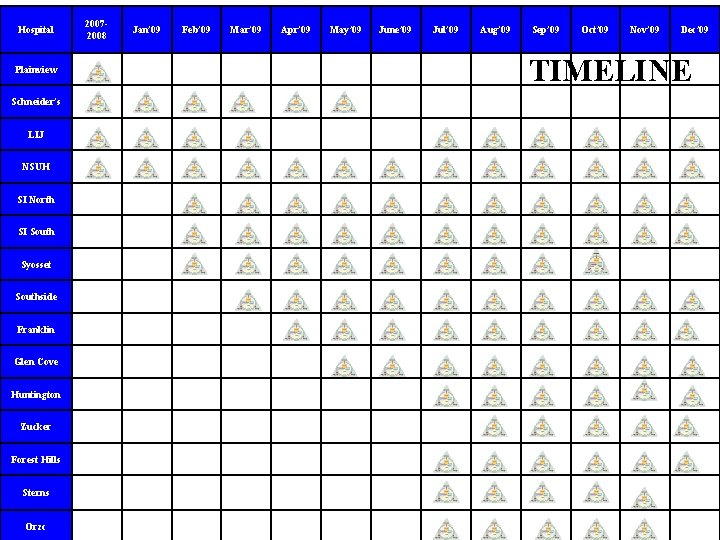
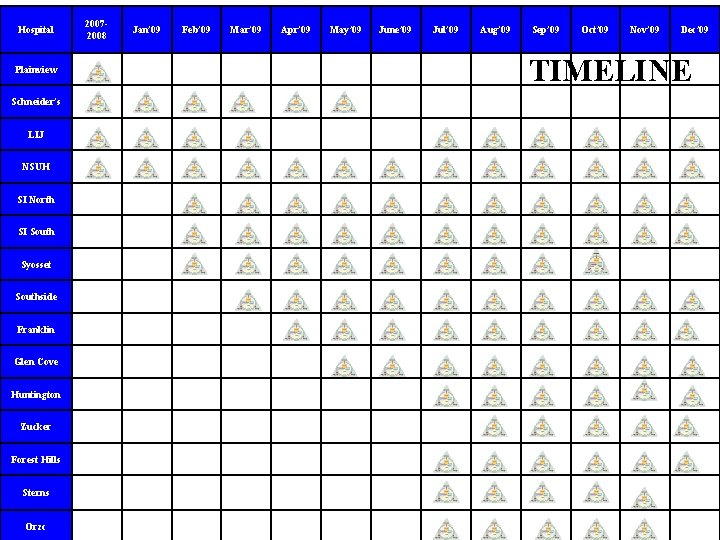
Hospital Plainview Schneider’s LIJ NSUH SI North SI South Syosset Southside Franklin Glen Cove Huntington Zucker Forest Hills Sterns Orzc 20072008 Jan’ 09 Feb’ 09 Mar’ 09 Apr’ 09 May’ 09 June’ 09 Jul’ 09 Aug’ 09 Sep’ 09 Oct’ 09 Nov’ 09 Dec’ 09 TIMELINE
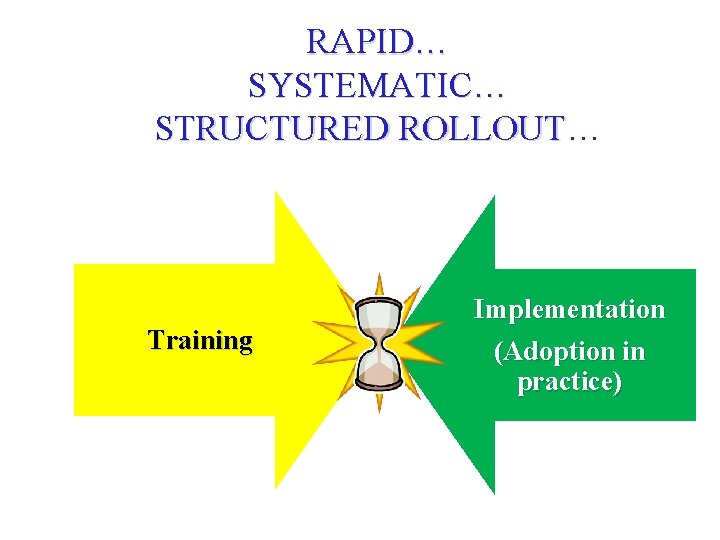
RAPID… SYSTEMATIC… STRUCTURED ROLLOUT Training Implementation (Adoption in practice)
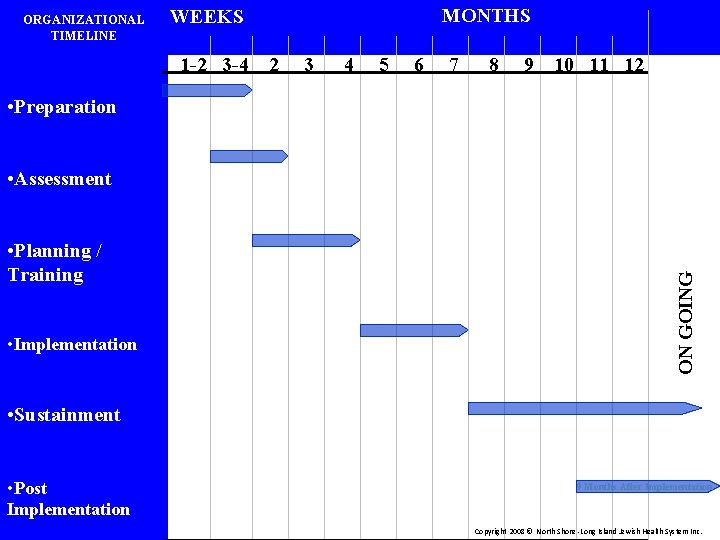
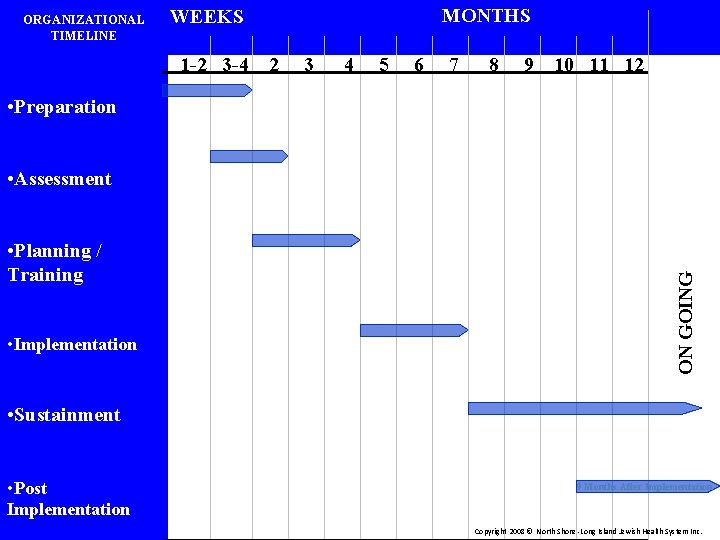
ORGANIZATIONAL TIMELINE MONTHS WEEKS 1 -2 3 -4 2 3 4 5 6 7 8 9 10 11 12 • Preparation • Planning / Training • Implementation ON GOING • Assessment • Sustainment • Post Implementation 9 Months After Implementation Copyright 2008 © North Shore -Long Island Jewish Health System Inc.
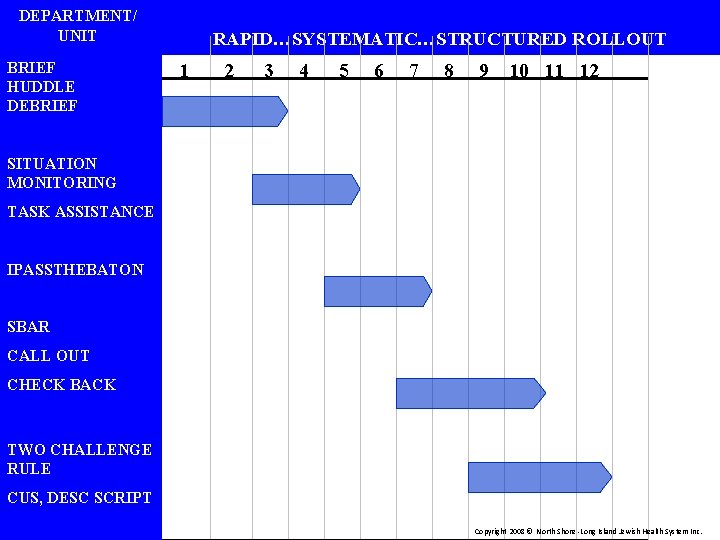
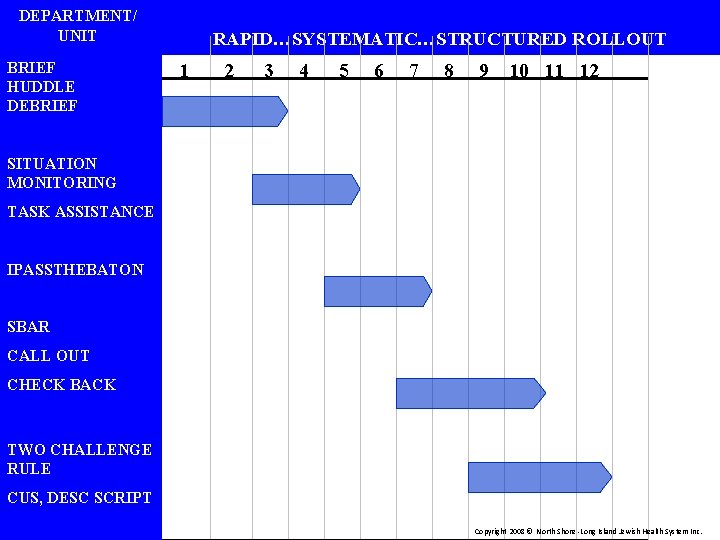
DEPARTMENT/ UNIT BRIEF HUDDLE DEBRIEF RAPID…SYSTEMATIC…STRUCTURED ROLLOUT 1 2 3 4 5 6 7 8 9 10 11 12 SITUATION MONITORING TASK ASSISTANCE IPASSTHEBATON SBAR CALL OUT CHECK BACK TWO CHALLENGE RULE CUS, DESC SCRIPT Copyright 2008 © North Shore -Long Island Jewish Health System Inc.
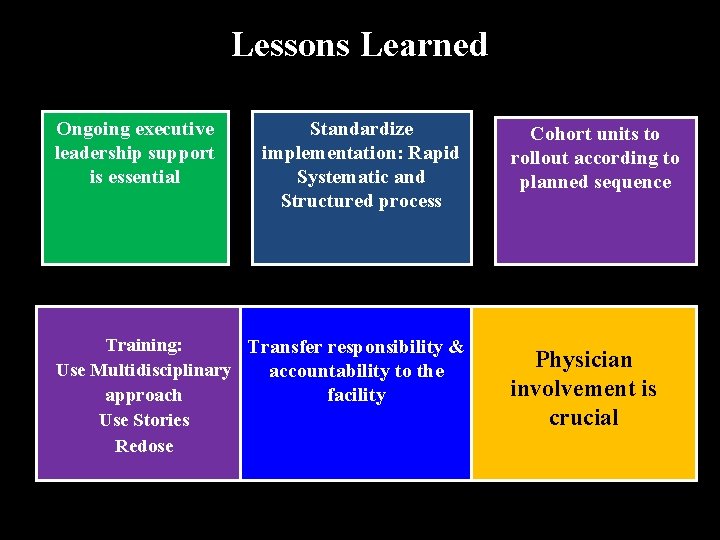
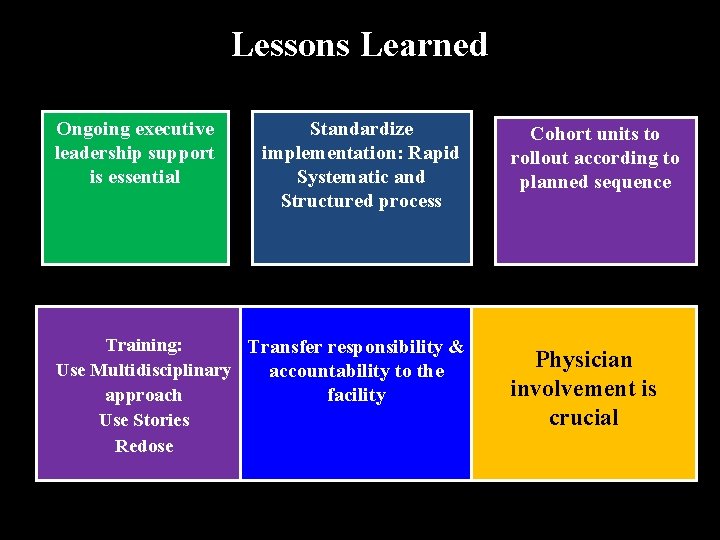
Lessons Learned Ongoing executive leadership support is essential Standardize implementation: Rapid Systematic and Structured process Training: Transfer responsibility & Use Multidisciplinary accountability to the facility approach Use Stories Redose Cohort units to rollout according to planned sequence Physician involvement is crucial
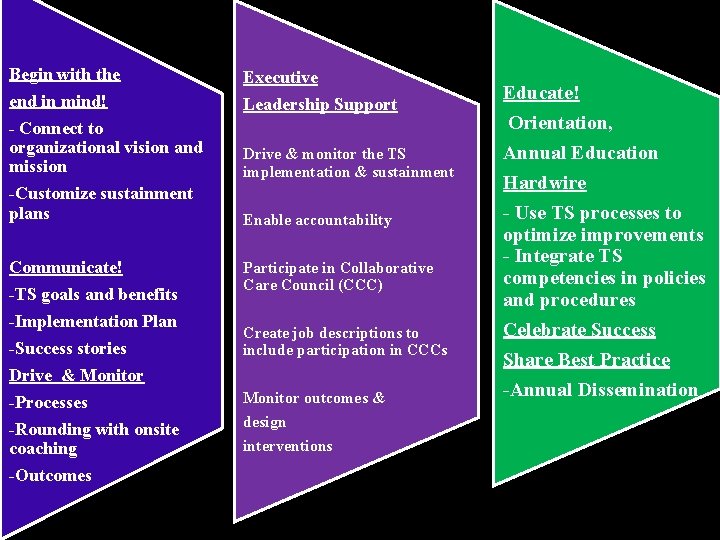
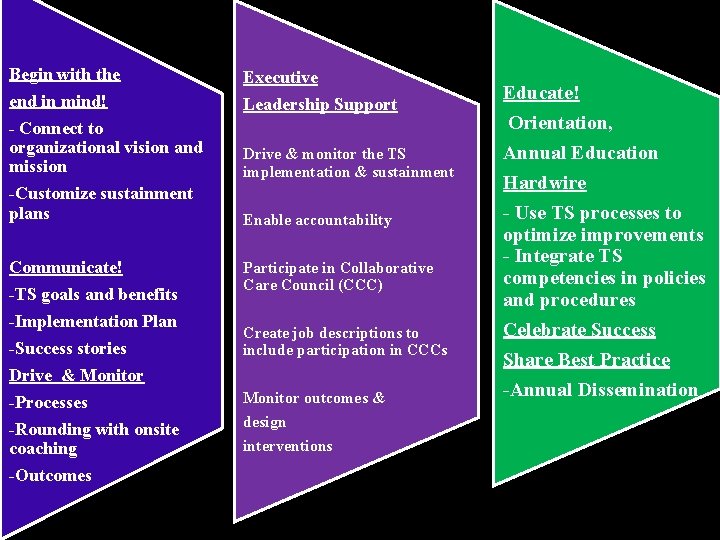
Begin with the end in mind! - Connect to organizational vision and mission -Customize sustainment plans Executive Communicate! -TS goals and benefits -Implementation Plan -Success stories Drive & Monitor -Processes -Rounding with onsite coaching -Outcomes Participate in Collaborative Care Council (CCC) Leadership Support Drive & monitor the TS implementation & sustainment Enable accountability Create job descriptions to include participation in CCCs Monitor outcomes & design interventions Educate! Orientation, Annual Education Hardwire - Use TS processes to optimize improvements - Integrate TS competencies in policies and procedures Celebrate Success Share Best Practice -Annual Dissemination SUSTAINMENT STRATEGIES 20

TRANSFORMATIONAL GOAL RESULTS: PILOT HOSPITAL 2011 2007 9 Domains 11 m Tea PPS E ST Domains Total = 12 Domains 21

TRANSFORMATIONAL GOAL RESULTS: Health System 2011 2009 9 Domains 7 m Tea PPS E ST Domains Total = 12 Domains 22
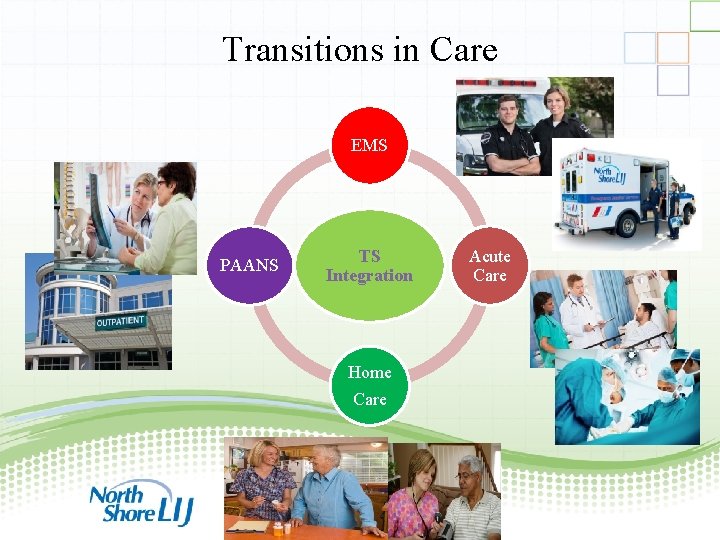
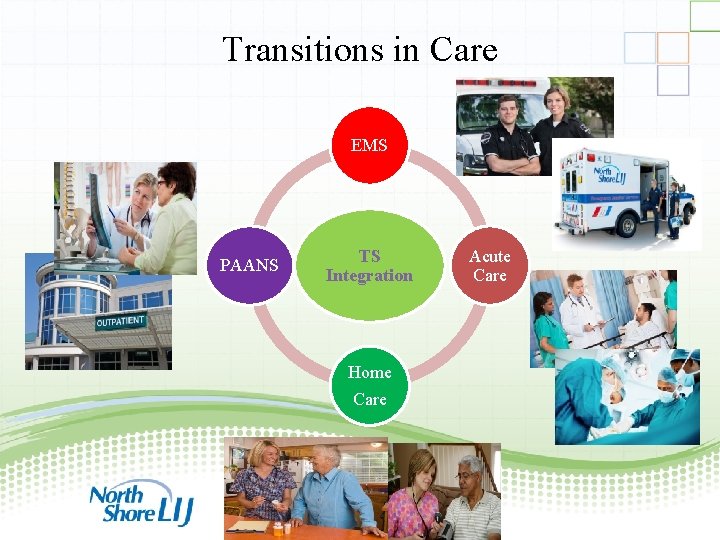
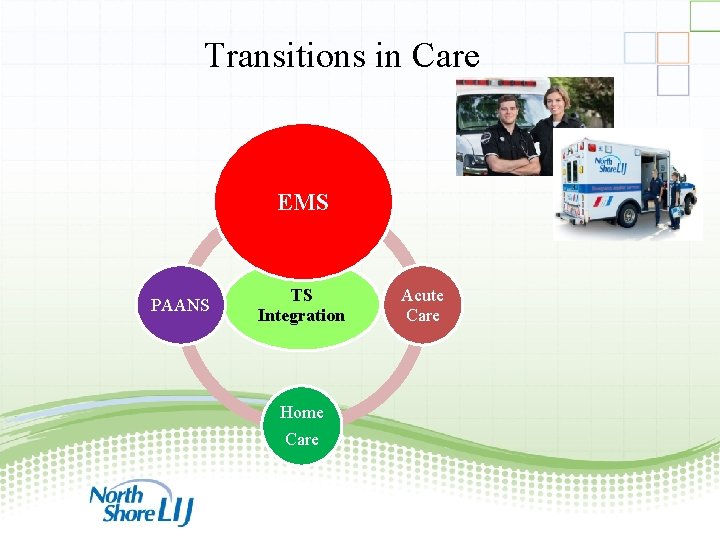
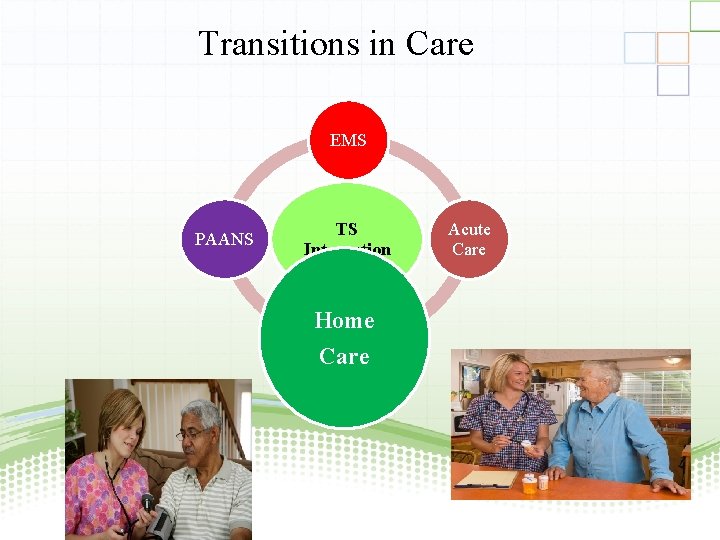
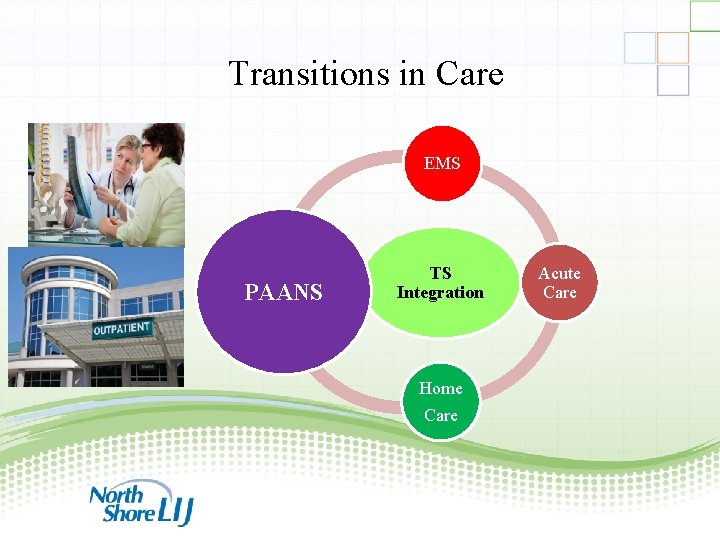
Transitions in Care EMS PAANS TS Integration Acute Care Home Care 23
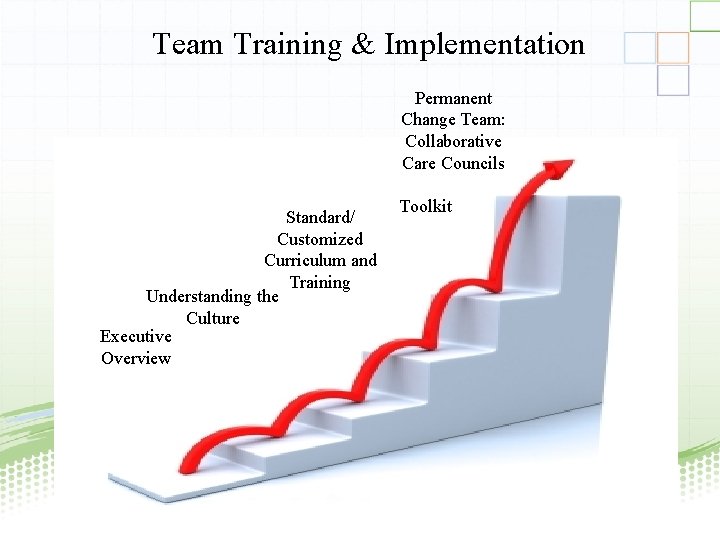
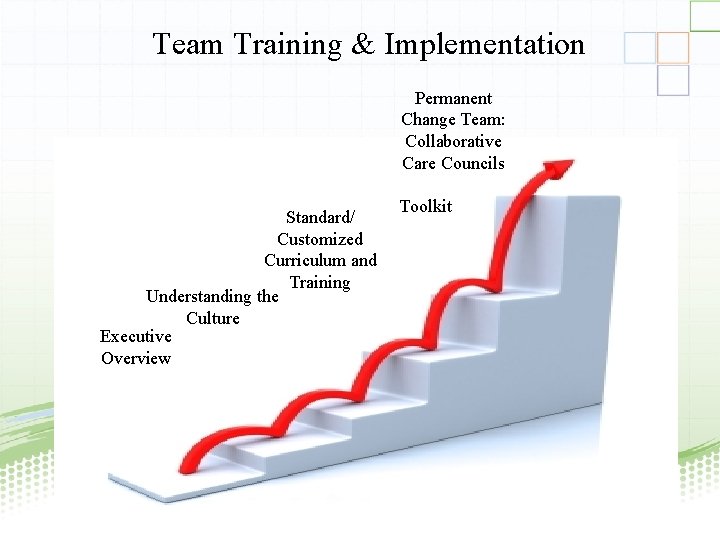
Team Training & Implementation Permanent Change Team: Collaborative Care Councils Standard/ Customized Curriculum and Training Understanding the Culture Executive Overview Toolkit 24

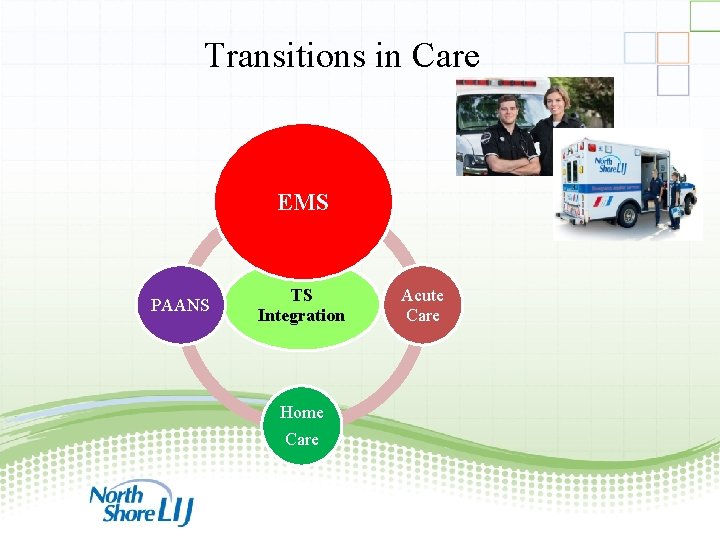
Transitions in Care EMS PAANS TS Integration Acute Care Home Care 25

Acute Care Toolkit • Standard TS Training • Standard Scenarios • Multi-Team System (MTS) • Briefing Template • Handoff • Collaborative Care Council 26
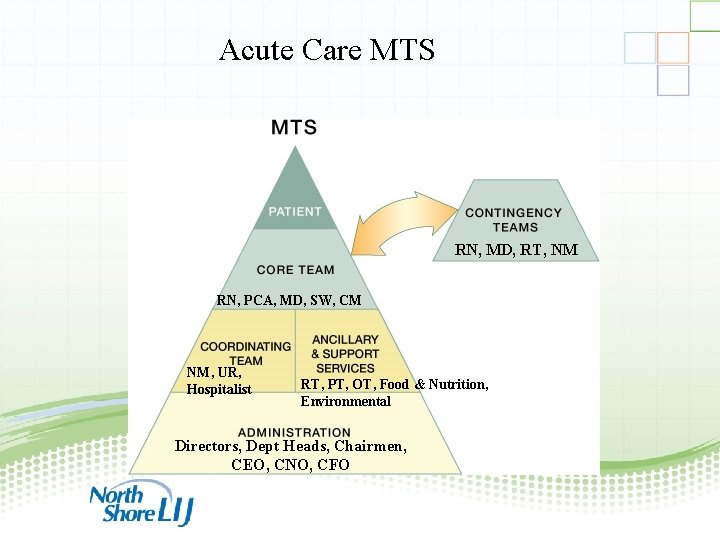
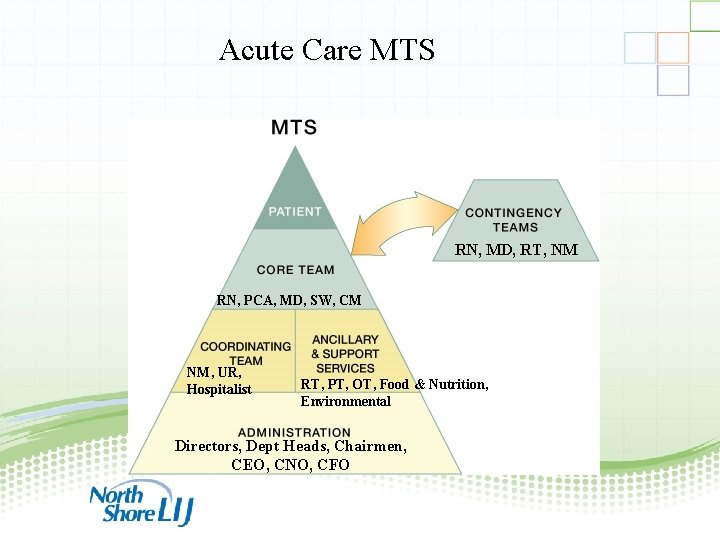
Acute Care MTS RN, MD, RT, NM RN, PCA, MD, SW, CM NM, UR, Hospitalist RT, PT, OT, Food & Nutrition, Environmental Directors, Dept Heads, Chairmen, CEO, CNO, CFO 27
Transitions in Care EMS PAANS TS Integration Acute Care Home Care 28

29

30
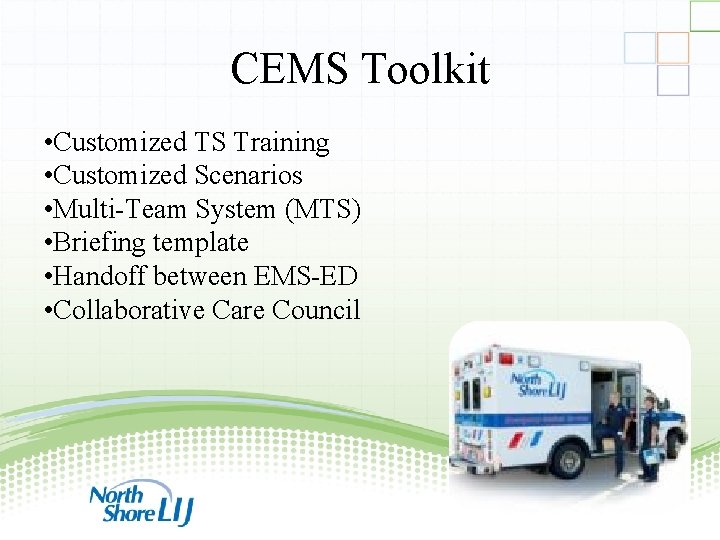
CEMS Toolkit • Customized TS Training • Customized Scenarios • Multi-Team System (MTS) • Briefing template • Handoff between EMS-ED • Collaborative Care Council 31
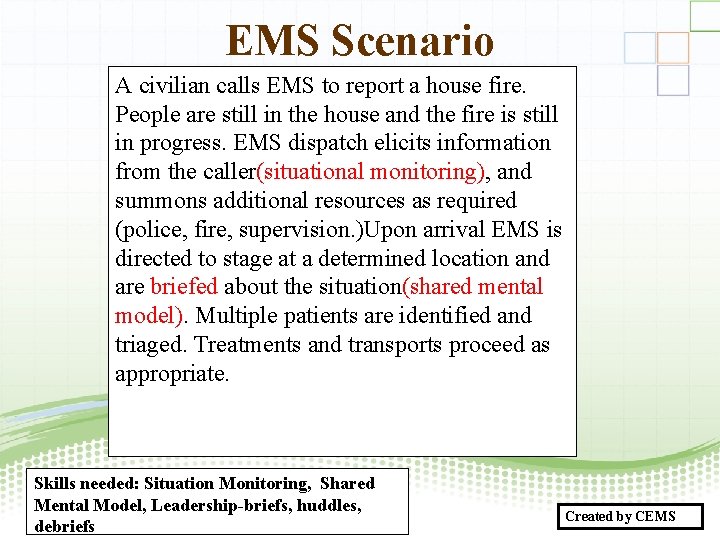
EMS Scenario A civilian calls EMS to report a house fire. People are still in the house and the fire is still in progress. EMS dispatch elicits information from the caller(situational monitoring), and summons additional resources as required (police, fire, supervision. )Upon arrival EMS is directed to stage at a determined location and are briefed about the situation(shared mental model). Multiple patients are identified and triaged. Treatments and transports proceed as appropriate. Skills needed: Situation Monitoring, Shared Mental Model, Leadership-briefs, huddles, debriefs Created by CEMS 32
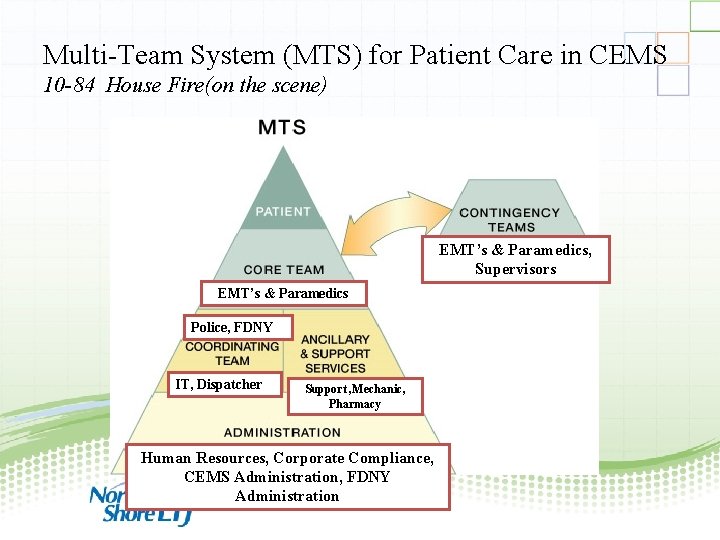
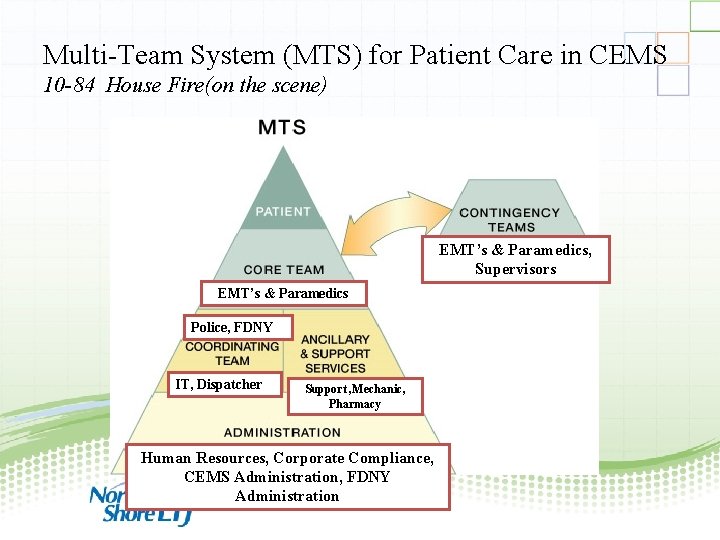
Multi-Team System (MTS) for Patient Care in CEMS 10 -84 House Fire(on the scene) EMT’s & Paramedics, Supervisors EMT’s & Paramedics Police, FDNY IT, Dispatcher Support , Mechanic, Pharmacy Human Resources, Corporate Compliance, CEMS Administration, FDNY Administration 33
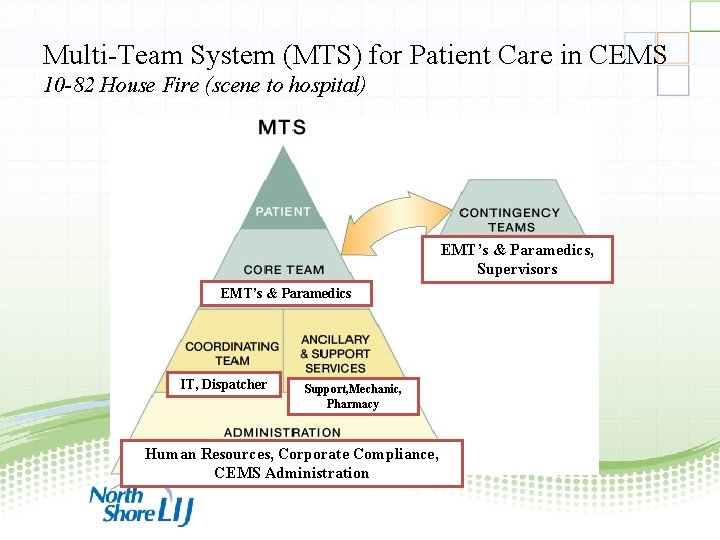
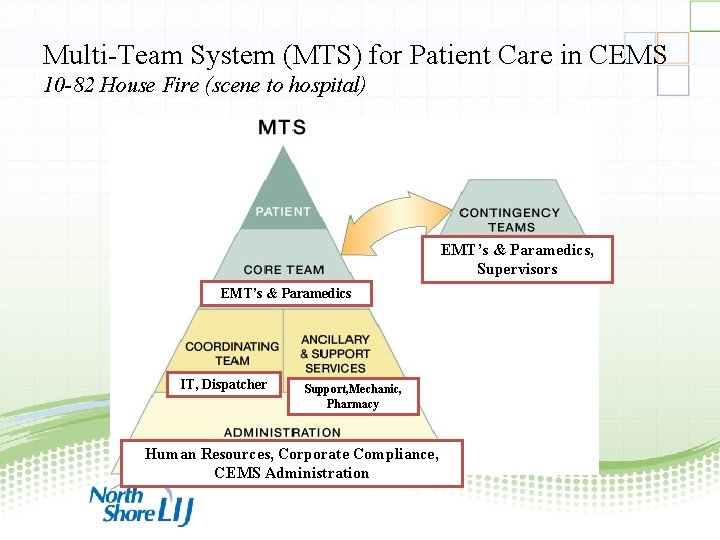
Multi-Team System (MTS) for Patient Care in CEMS 10 -82 House Fire (scene to hospital) EMT’s & Paramedics, Supervisors EMT’s & Paramedics IT, Dispatcher Support, Mechanic, Pharmacy Human Resources, Corporate Compliance, CEMS Administration 34
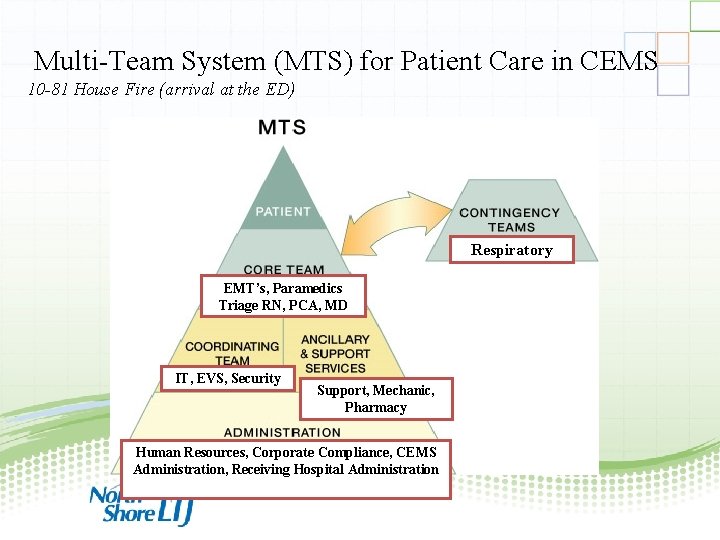
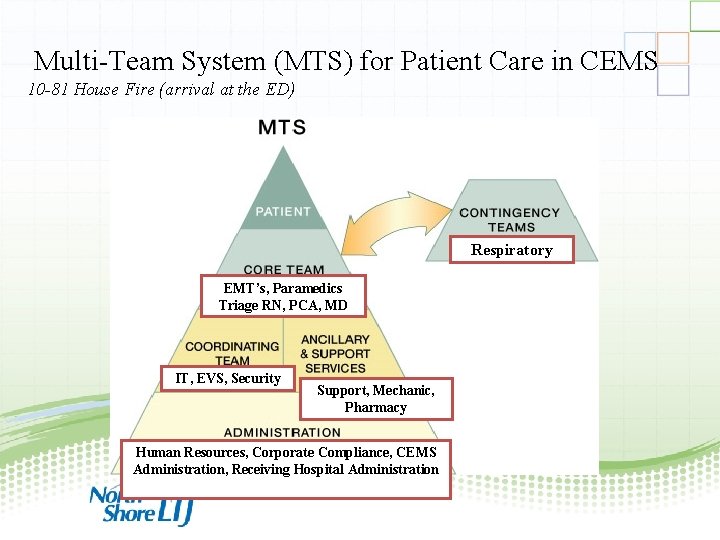
Multi-Team System (MTS) for Patient Care in CEMS 10 -81 House Fire (arrival at the ED) Respiratory EMT’s, Paramedics Triage RN, PCA, MD IT, EVS, Security Support, Mechanic, Pharmacy Human Resources, Corporate Compliance, CEMS Administration, Receiving Hospital Administration 35
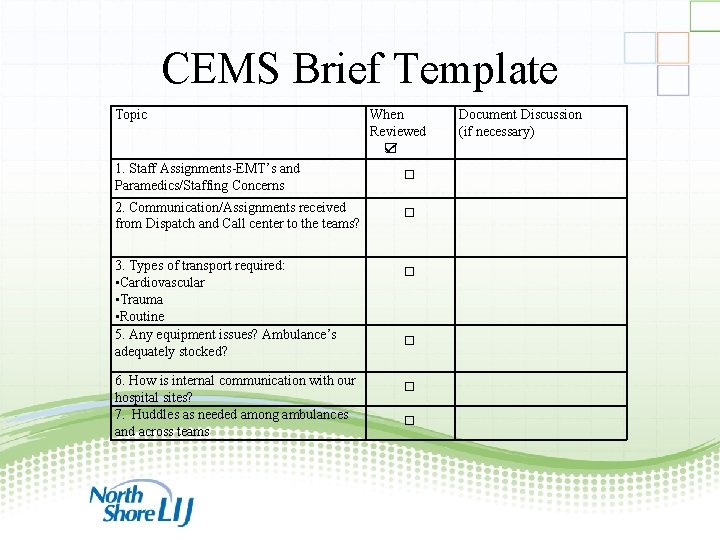
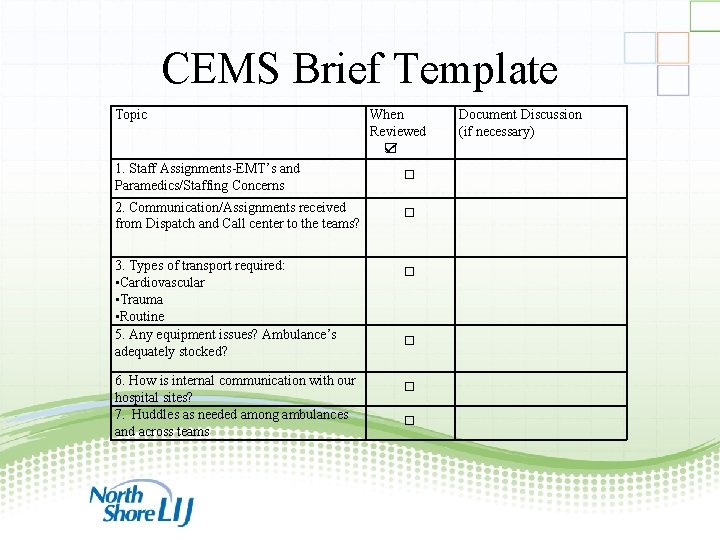
CEMS Brief Template Topic When Reviewed ☑ 1. Staff Assignments-EMT’s and Paramedics/Staffing Concerns □ 2. Communication/Assignments received from Dispatch and Call center to the teams? □ 3. Types of transport required: • Cardiovascular • Trauma • Routine 5. Any equipment issues? Ambulance’s adequately stocked? □ 6. How is internal communication with our hospital sites? 7. Huddles as needed among ambulances and across teams □ Document Discussion (if necessary) □ □ 36
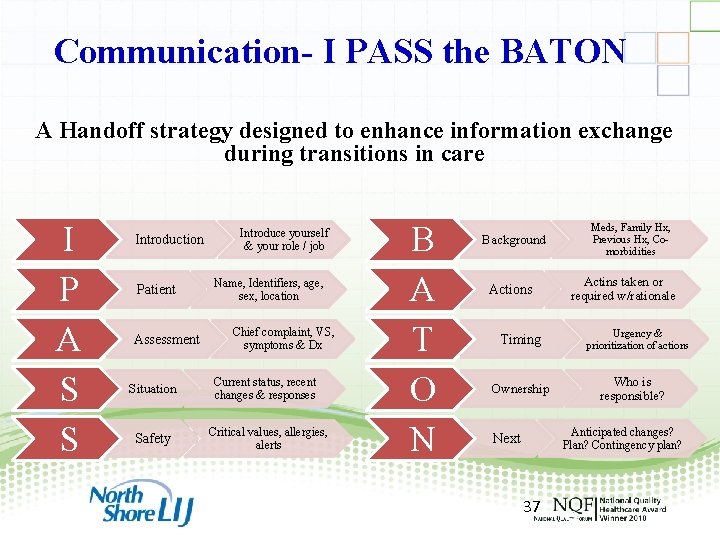
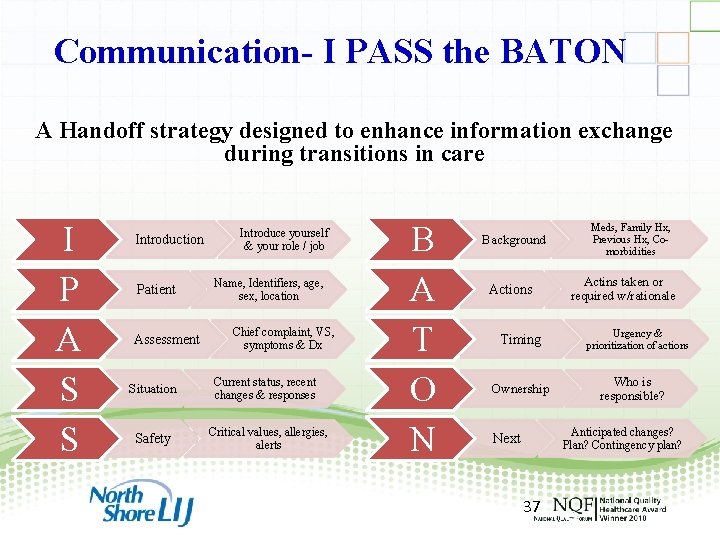
Communication- I PASS the BATON A Handoff strategy designed to enhance information exchange during transitions in care I P A S S Introduction Patient Assessment Situation Safety Introduce yourself & your role / job Name, Identifiers, age, sex, location Chief complaint, VS, symptoms & Dx Current status, recent changes & responses Critical values, allergies, alerts B A T O N Background Actions Timing Ownership Meds, Family Hx, Previous Hx, Comorbidities Actins taken or required w/rationale Urgency & prioritization of actions Who is responsible? Anticipated changes? Plan? Contingency plan? Next 37 37
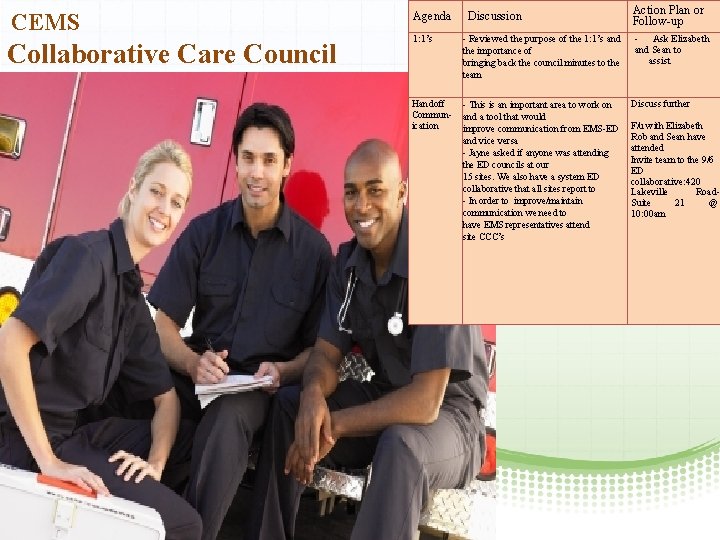
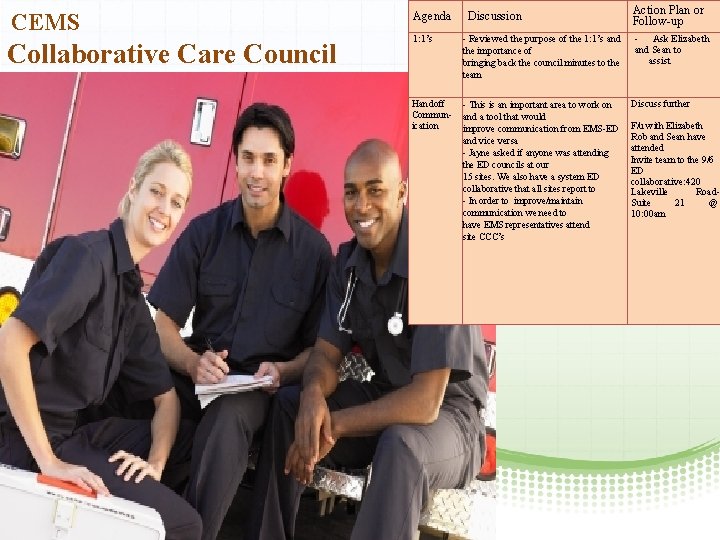
CEMS Collaborative Care Council Agenda Discussion 1: 1’s - Reviewed the purpose of the 1: 1’s and the importance of bringing back the council minutes to the team Handoff Communication - This is an important area to work on and a tool that would improve communication from EMS-ED and vice versa - Jayne asked if anyone was attending the ED councils at our 15 sites. We also have a system ED collaborative that all sites report to - In order to improve/maintain communication we need to have EMS representatives attend site CCC’s Action Plan or Follow-up - Ask Elizabeth and Sean to assist Discuss further F/u with Elizabeth Rob and Sean have attended Invite team to the 9/6 ED collaborative: 420 Lakeville Road. Suite 21 @ 10: 00 am 38
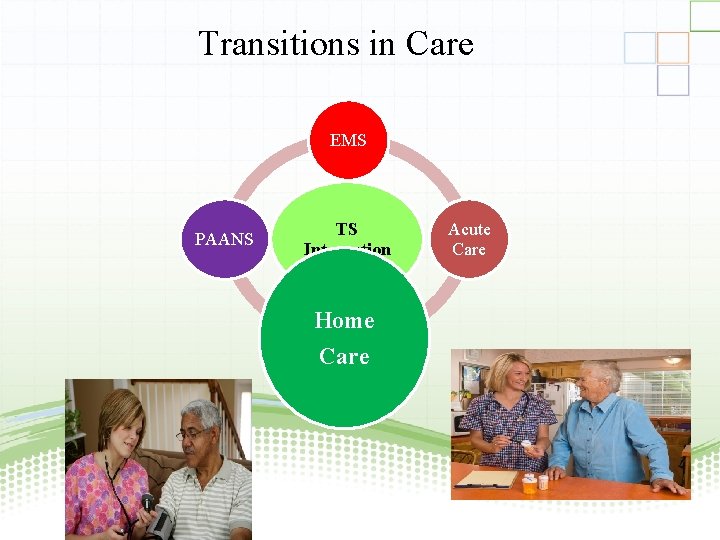
Transitions in Care EMS PAANS TS Integration Acute Care Home Care 39

Home Health Care 40
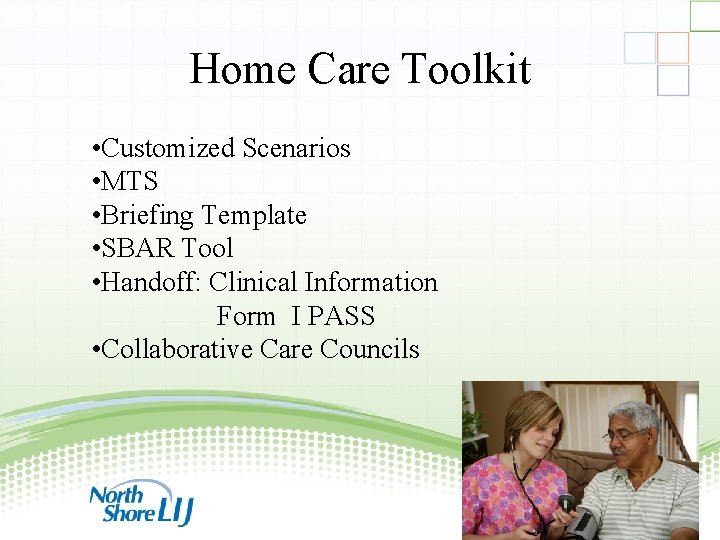
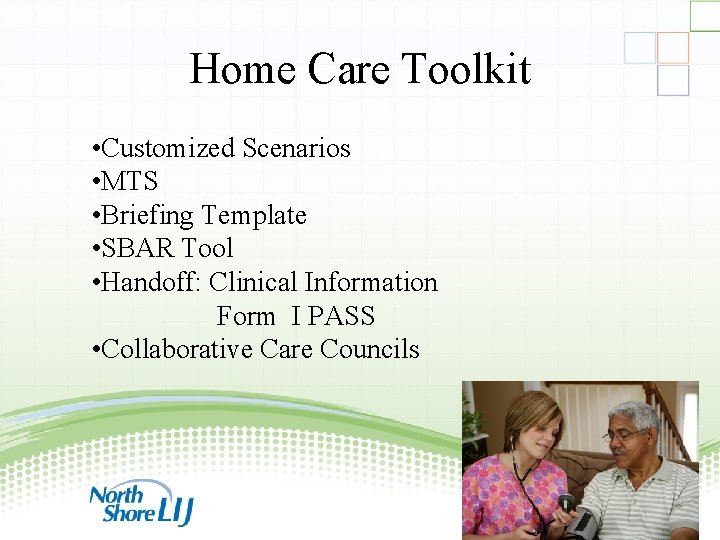
Home Care Toolkit • Customized Scenarios • MTS • Briefing Template • SBAR Tool • Handoff: Clinical Information Form I PASS • Collaborative Care Councils 41
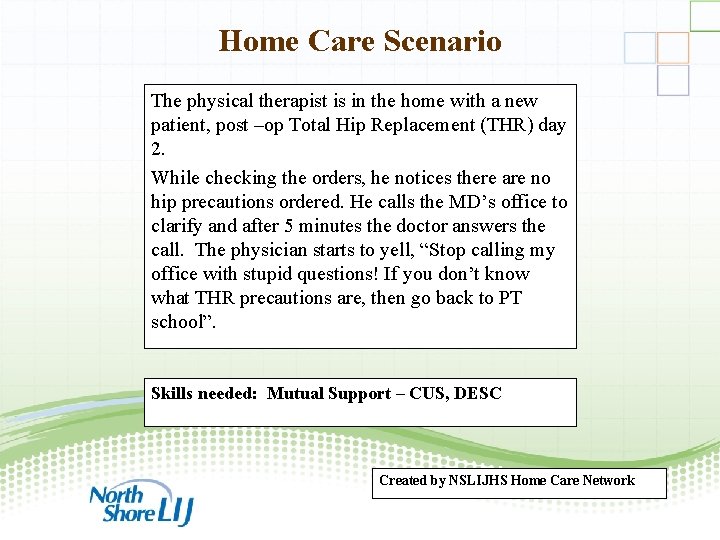
Home Care Scenario The physical therapist is in the home with a new patient, post –op Total Hip Replacement (THR) day 2. While checking the orders, he notices there are no hip precautions ordered. He calls the MD’s office to clarify and after 5 minutes the doctor answers the call. The physician starts to yell, “Stop calling my office with stupid questions! If you don’t know what THR precautions are, then go back to PT school”. Skills needed: Mutual Support – CUS, DESC Created by NSLIJHS Home Care Network 42
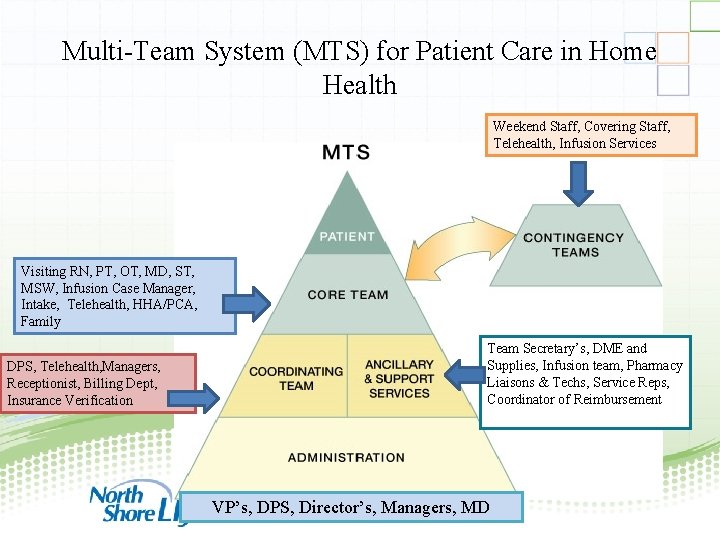
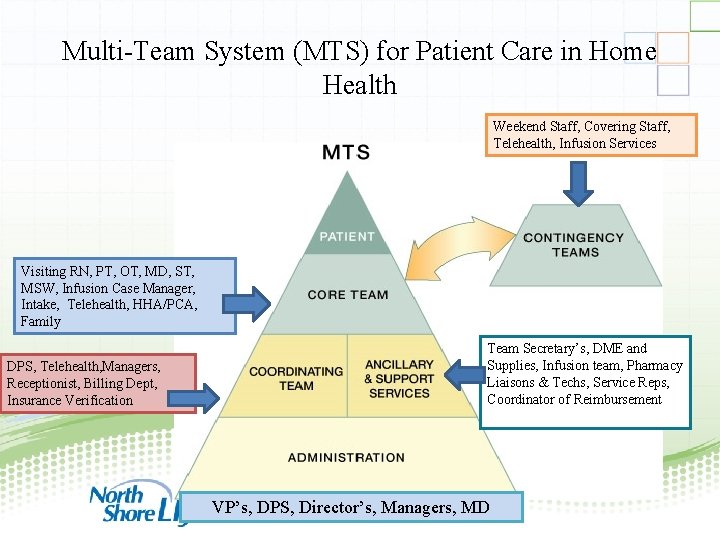
Multi-Team System (MTS) for Patient Care in Home Health Weekend Staff, Covering Staff, Telehealth, Infusion Services Visiting RN, PT, OT, MD, ST, MSW, Infusion Case Manager, Intake, Telehealth, HHA/PCA, Family DPS, Telehealth, Managers, Receptionist, Billing Dept, Insurance Verification Team Secretary’s, DME and Supplies, Infusion team, Pharmacy Liaisons & Techs, Service Reps, Coordinator of Reimbursement VP’s, DPS, Director’s, Managers, MD 43
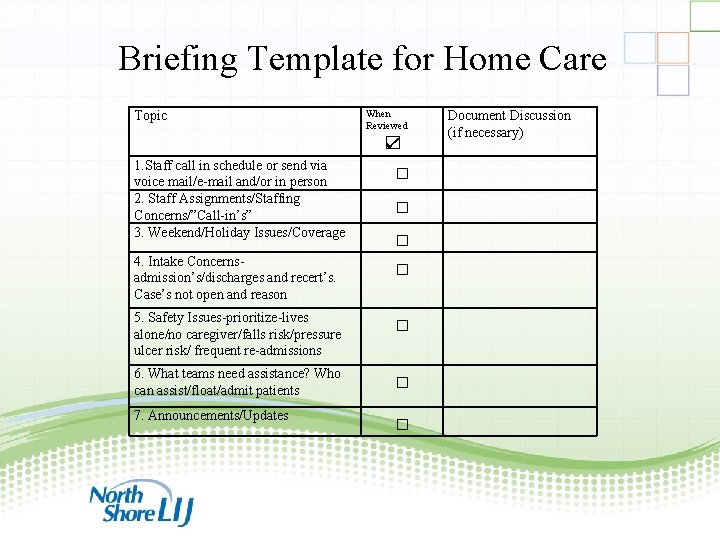
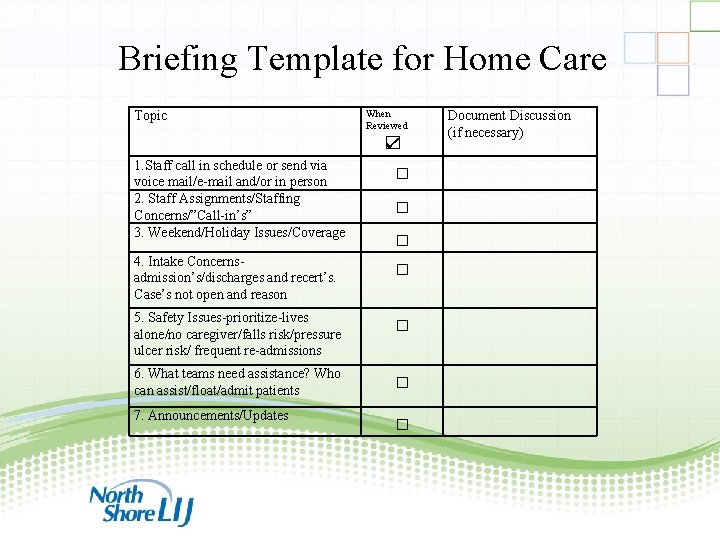
Briefing Template for Home Care Topic When Reviewed ☑ 1. Staff call in schedule or send via voice mail/e-mail and/or in person 2. Staff Assignments/Staffing Concerns/”Call-in’s” 3. Weekend/Holiday Issues/Coverage 4. Intake Concernsadmission’s/discharges and recert’s. Case’s not open and reason Document Discussion (if necessary) □ □ 5. Safety Issues-prioritize-lives alone/no caregiver/falls risk/pressure ulcer risk/ frequent re-admissions □ 6. What teams need assistance? Who can assist/float/admit patients □ 7. Announcements/Updates □ 44
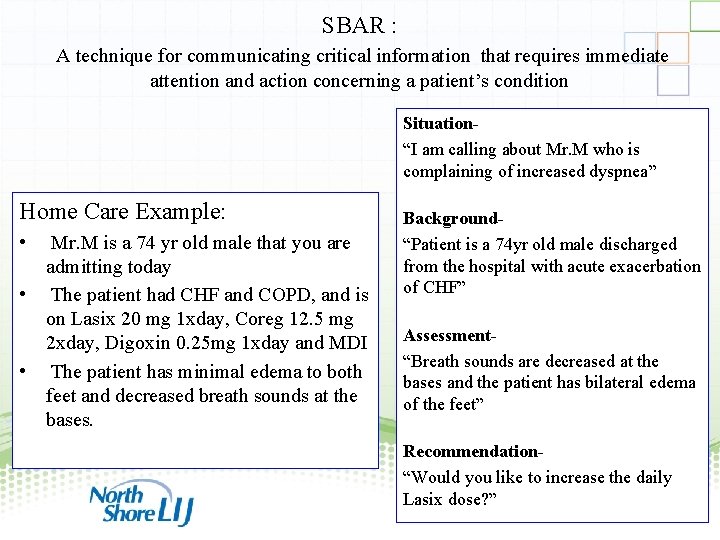
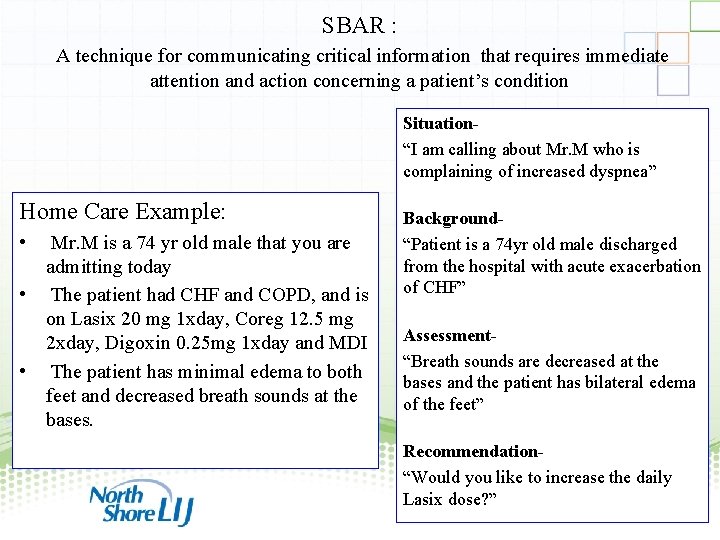
SBAR : A technique for communicating critical information that requires immediate attention and action concerning a patient’s condition Situation“I am calling about Mr. M who is complaining of increased dyspnea” Home Care Example: • Mr. M is a 74 yr old male that you are admitting today • The patient had CHF and COPD, and is on Lasix 20 mg 1 xday, Coreg 12. 5 mg 2 xday, Digoxin 0. 25 mg 1 xday and MDI • The patient has minimal edema to both feet and decreased breath sounds at the bases. Background“Patient is a 74 yr old male discharged from the hospital with acute exacerbation of CHF” Assessment“Breath sounds are decreased at the bases and the patient has bilateral edema of the feet” Recommendation“Would you like to increase the daily Lasix dose? ” 45
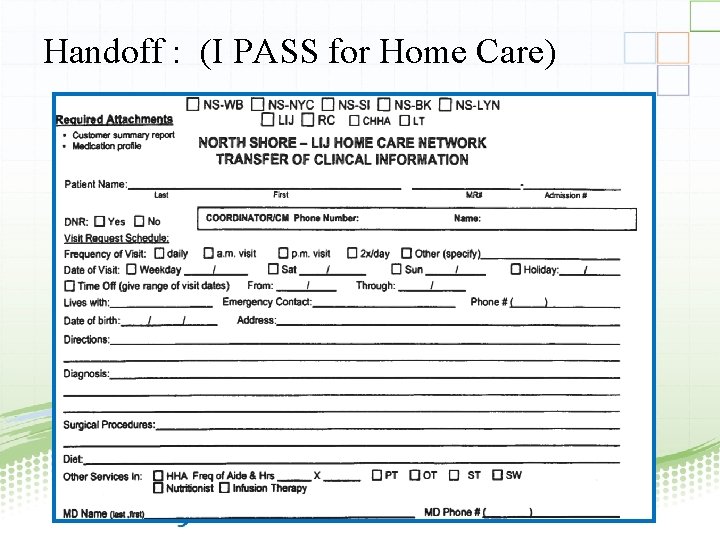
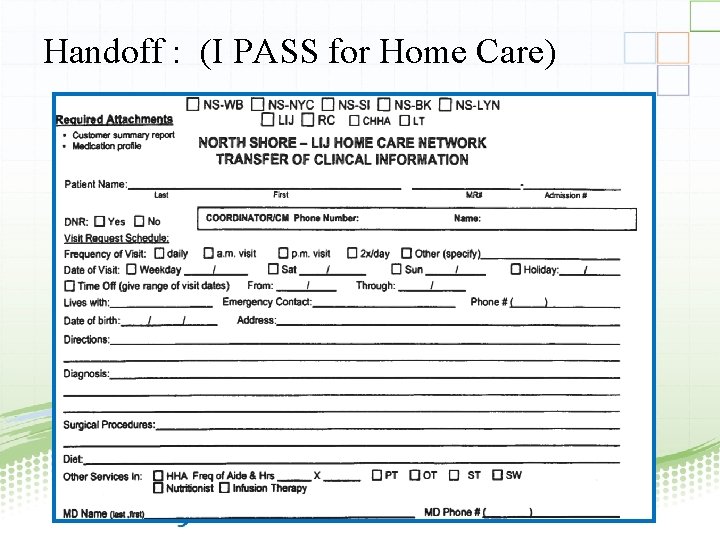
Handoff : (I PASS for Home Care) 46
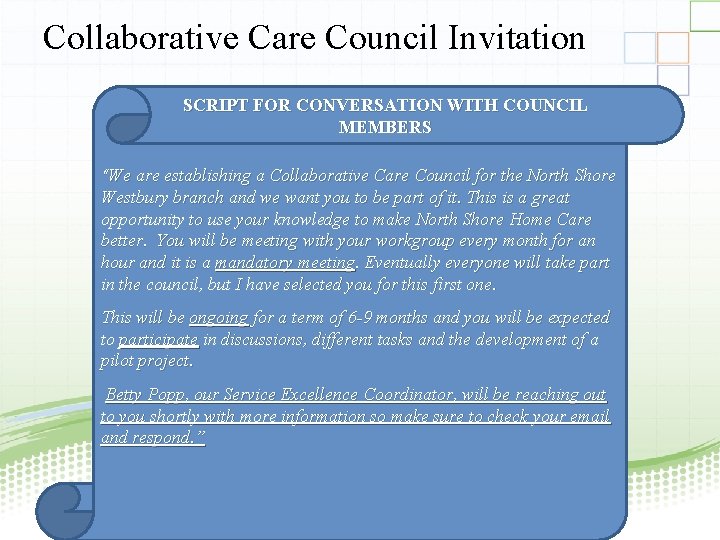
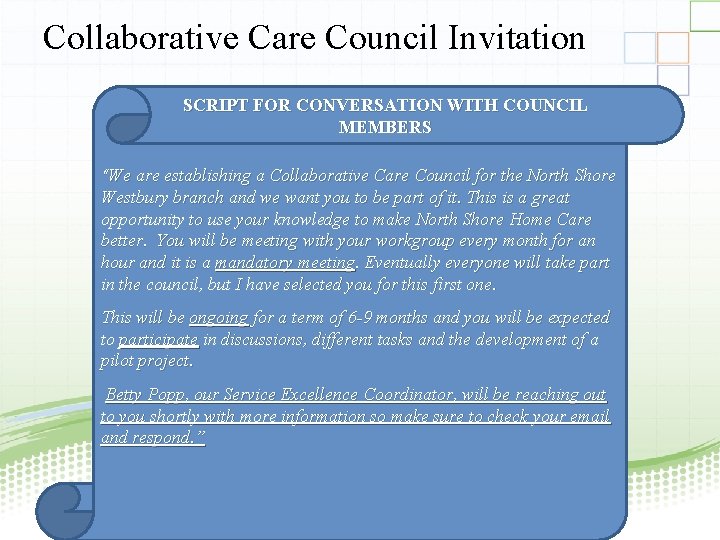
Collaborative Care Council Invitation SCRIPT FOR CONVERSATION WITH COUNCIL MEMBERS “We are establishing a Collaborative Care Council for the North Shore Westbury branch and we want you to be part of it. This is a great opportunity to use your knowledge to make North Shore Home Care better. You will be meeting with your workgroup every month for an hour and it is a mandatory meeting. Eventually everyone will take part in the council, but I have selected you for this first one. This will be ongoing for a term of 6 -9 months and you will be expected to participate in discussions, different tasks and the development of a pilot project. Betty Popp, our Service Excellence Coordinator, will be reaching out to you shortly with more information so make sure to check your email and respond. ” 47
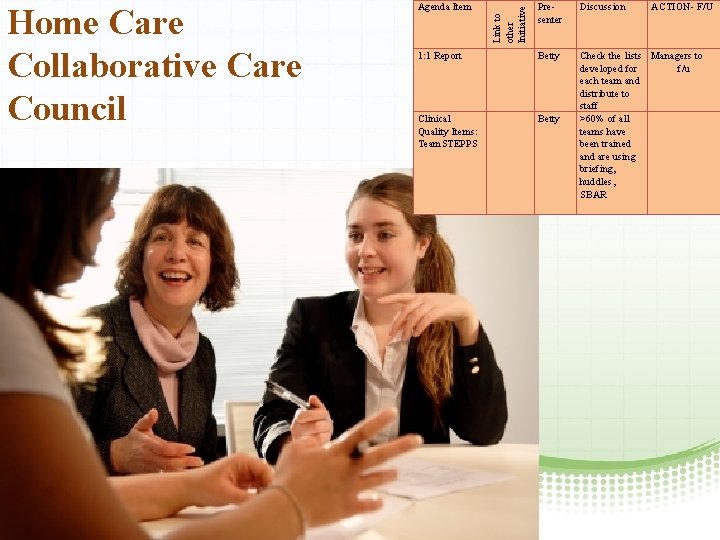
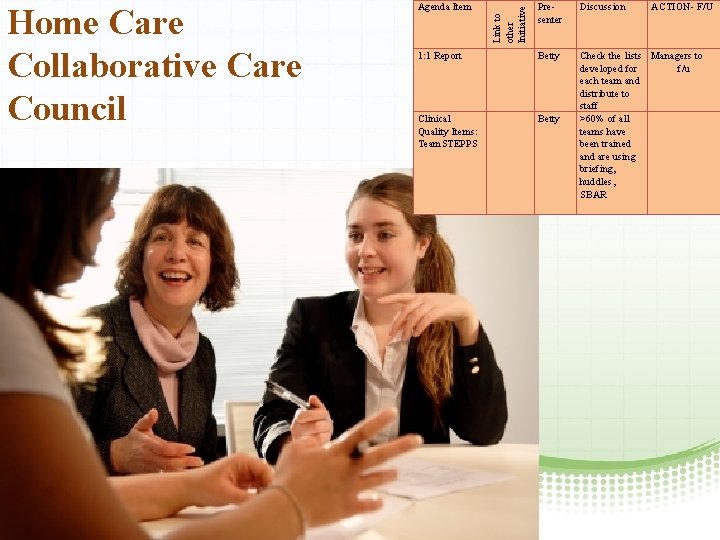
Presenter Discussion 1: 1 Report Betty Clinical Quality Items: Team. STEPPS Betty Check the lists Managers to developed for f/u each team and distribute to staff >60% of all teams have been trained and are using briefing, huddles, SBAR Link to other Initiative Home Care Collaborative Care Council Agenda Item ACTION- F/U 48
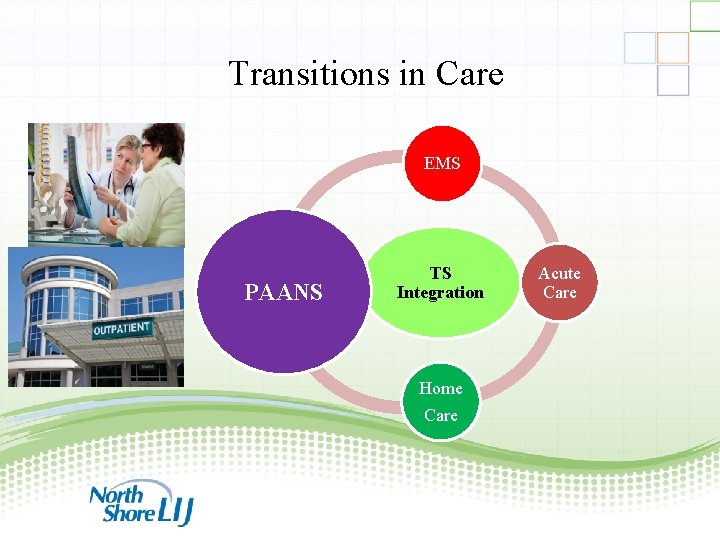
Transitions in Care EMS PAANS TS Integration Acute Care Home Care 49
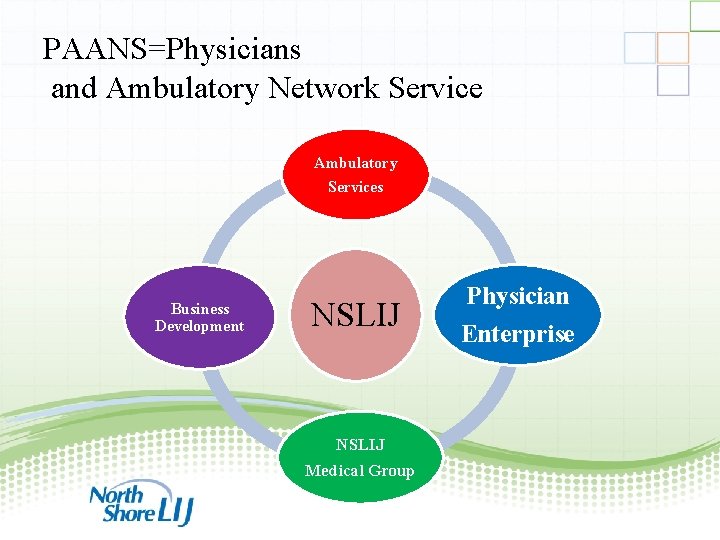
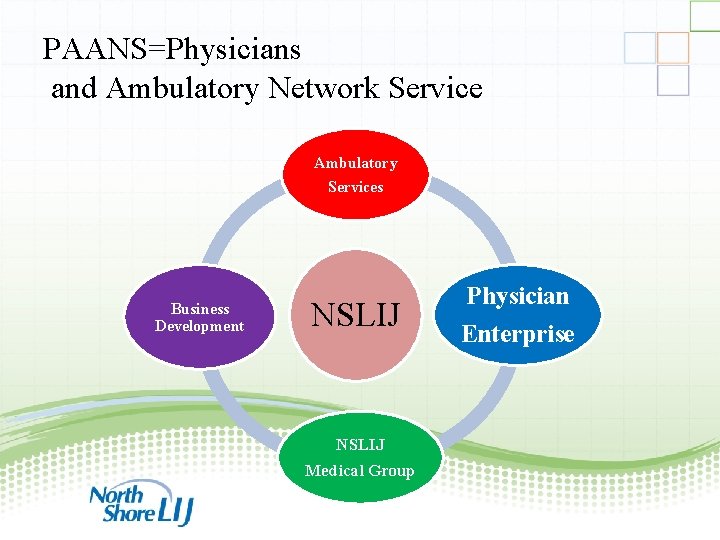
PAANS=Physicians and Ambulatory Network Service Ambulatory Services Business Development NSLIJ Physician Enterprise NSLIJ Medical Group 50

PAANS Toolkit • Customized Scenarios • MTS for Ambulatory Services • Briefing Template • SBAR 51
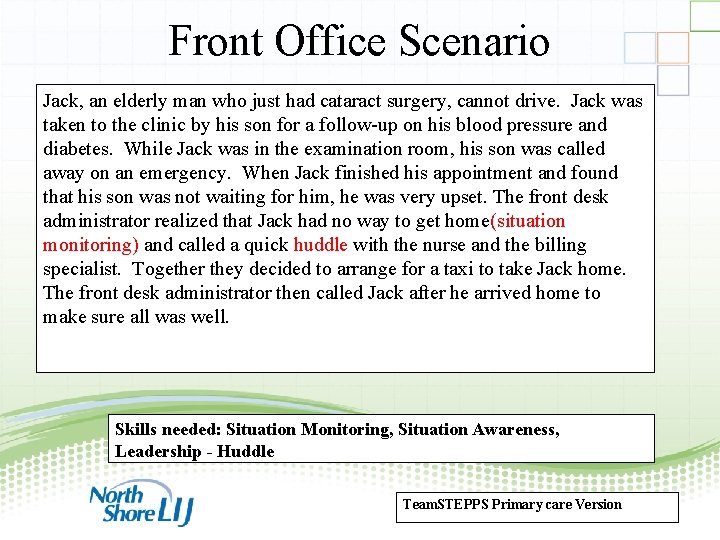
Front Office Scenario Jack, an elderly man who just had cataract surgery, cannot drive. Jack was taken to the clinic by his son for a follow-up on his blood pressure and diabetes. While Jack was in the examination room, his son was called away on an emergency. When Jack finished his appointment and found that his son was not waiting for him, he was very upset. The front desk administrator realized that Jack had no way to get home(situation monitoring) and called a quick huddle with the nurse and the billing specialist. Together they decided to arrange for a taxi to take Jack home. The front desk administrator then called Jack after he arrived home to make sure all was well. Skills needed: Situation Monitoring, Situation Awareness, Leadership - Huddle Team. STEPPS Primary care Version 52
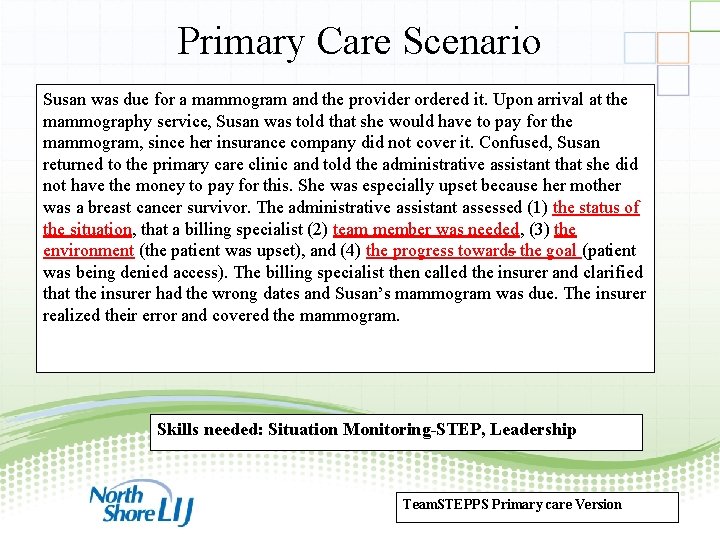
Primary Care Scenario Susan was due for a mammogram and the provider ordered it. Upon arrival at the mammography service, Susan was told that she would have to pay for the mammogram, since her insurance company did not cover it. Confused, Susan returned to the primary care clinic and told the administrative assistant that she did not have the money to pay for this. She was especially upset because her mother was a breast cancer survivor. The administrative assistant assessed (1) the status of the situation, that a billing specialist (2) team member was needed, (3) the environment (the patient was upset), and (4) the progress towards the goal (patient was being denied access). The billing specialist then called the insurer and clarified that the insurer had the wrong dates and Susan’s mammogram was due. The insurer realized their error and covered the mammogram. Skills needed: Situation Monitoring-STEP, Leadership Team. STEPPS Primary care Version 53
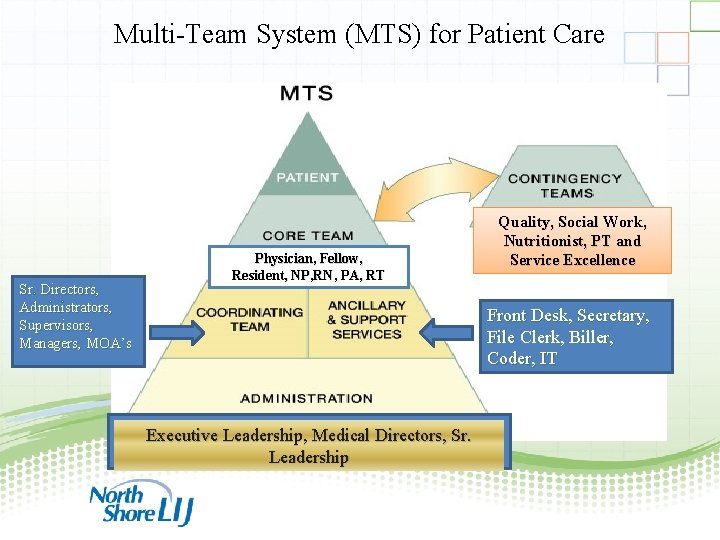
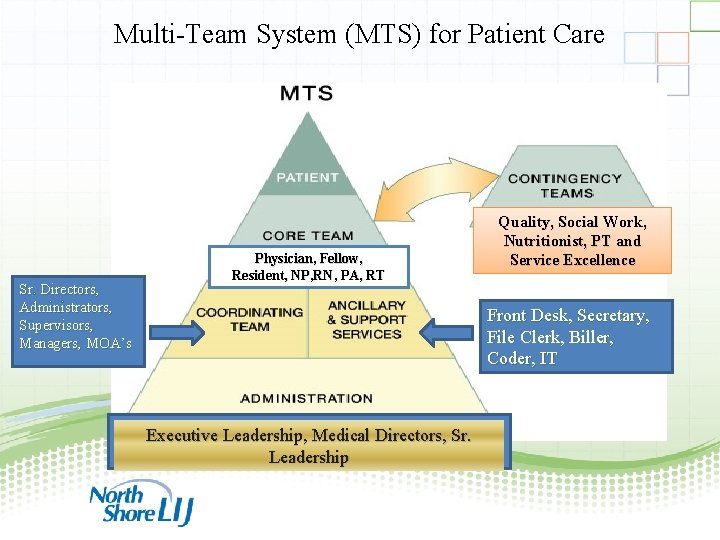
Multi-Team System (MTS) for Patient Care Sr. Directors, Administrators, Supervisors, Managers, MOA’s Physician, Fellow, Resident, NP, RN, PA, RT Quality, Social Work, Nutritionist, PT and Service Excellence Front Desk, Secretary, File Clerk, Biller, Coder, IT Executive Leadership, Medical Directors, Sr. Leadership 54
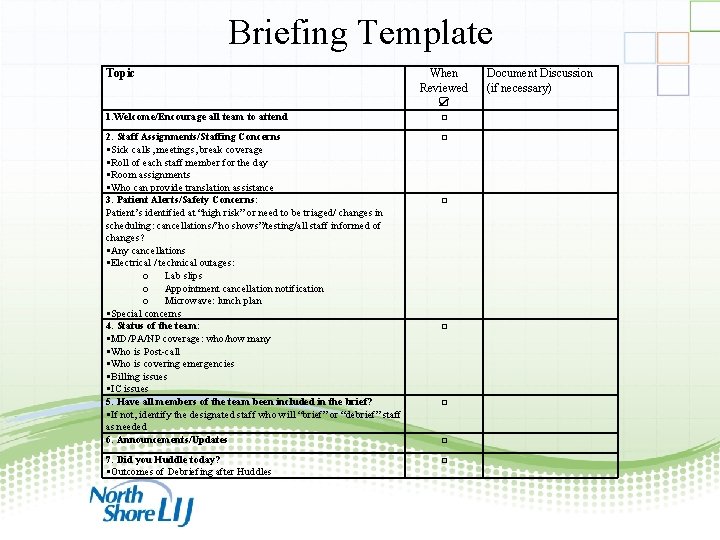
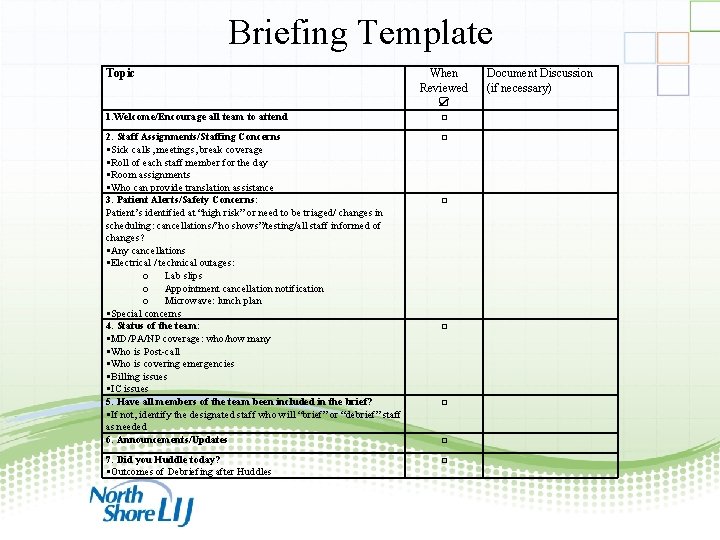
Briefing Template Topic When Reviewed ☑ 1. Welcome/Encourage all team to attend □ 2. Staff Assignments/Staffing Concerns Sick calls, meetings, break coverage Roll of each staff member for the day Room assignments Who can provide translation assistance 3. Patient Alerts/Safety Concerns: Patient’s identified at “high risk” or need to be triaged/ changes in scheduling: cancellations/”no shows”/testing/all staff informed of changes? Any cancellations Electrical / technical outages: o Lab slips o Appointment cancellation notification o Microwave: lunch plan Special concerns 4. Status of the team: MD/PA/NP coverage: who/how many Who is Post-call Who is covering emergencies Billing issues IC issues 5. Have all members of the team been included in the brief? If not, identify the designated staff who will “brief” or “debrief” staff as needed 6. Announcements/Updates □ 7. Did you Huddle today? Outcomes of Debriefing after Huddles □ Document Discussion (if necessary) □ □ 55
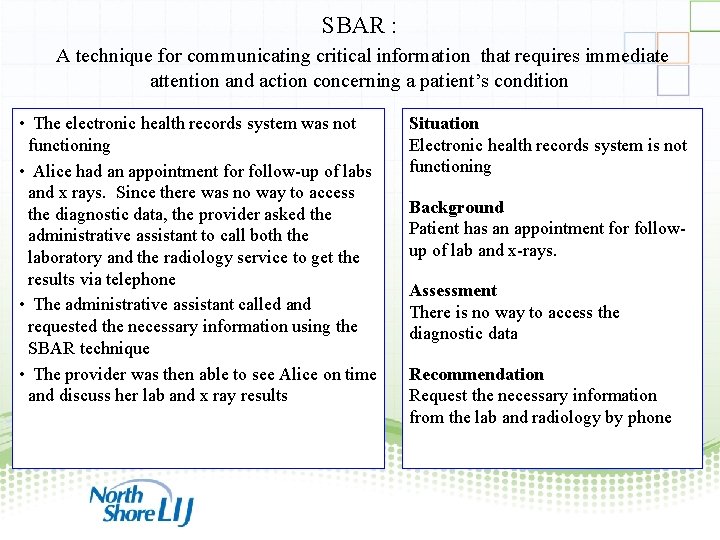
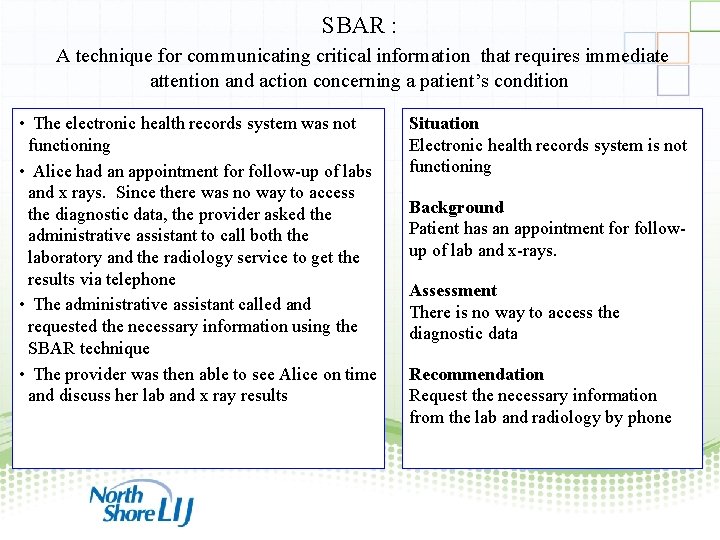
SBAR : A technique for communicating critical information that requires immediate attention and action concerning a patient’s condition • The electronic health records system was not functioning • Alice had an appointment for follow-up of labs and x rays. Since there was no way to access the diagnostic data, the provider asked the administrative assistant to call both the laboratory and the radiology service to get the results via telephone • The administrative assistant called and requested the necessary information using the SBAR technique • The provider was then able to see Alice on time and discuss her lab and x ray results Situation Electronic health records system is not functioning Background Patient has an appointment for followup of lab and x-rays. Assessment There is no way to access the diagnostic data Recommendation Request the necessary information from the lab and radiology by phone 56
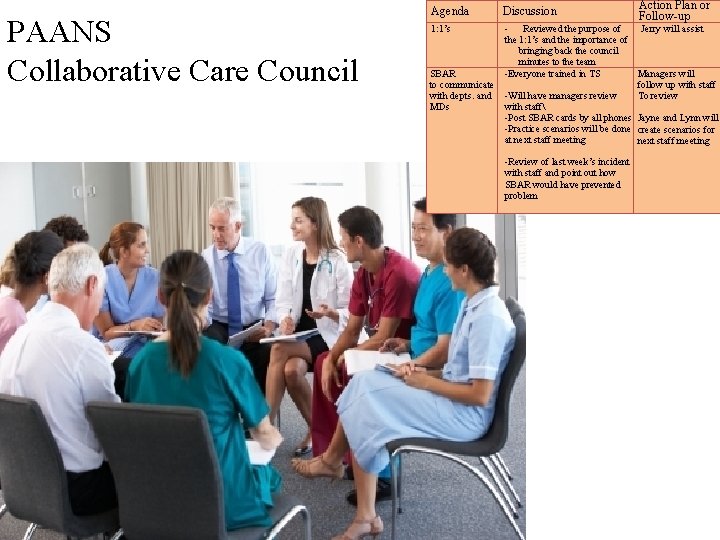
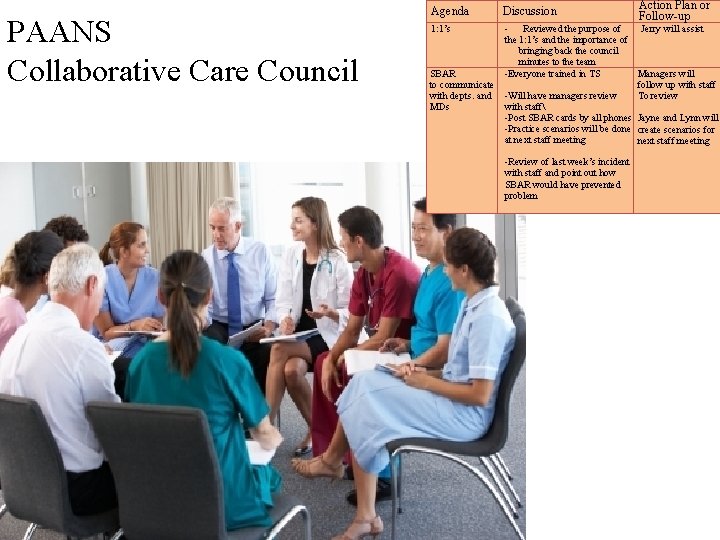
PAANS Collaborative Care Council Agenda Discussion 1: 1’s Action Plan or Follow-up - Reviewed the purpose of Jerry will assist the 1: 1’s and the importance of bringing back the council minutes to the team SBAR -Everyone trained in TS Managers will to communicate follow up with staff with depts. and -Will have managers review To review MDs with staff -Post SBAR cards by all phones Jayne and Lynn will -Practice scenarios will be done create scenarios for at next staff meeting -Review of last week’s incident with staff and point out how SBAR would have prevented problem
Begin with the end in mind! S Covey, The 7 Habits of Highly Effective People (Habit 2) - - Secret of Sustainment - - Connect Team. STEPPS to Organizational Vision & Mission 58
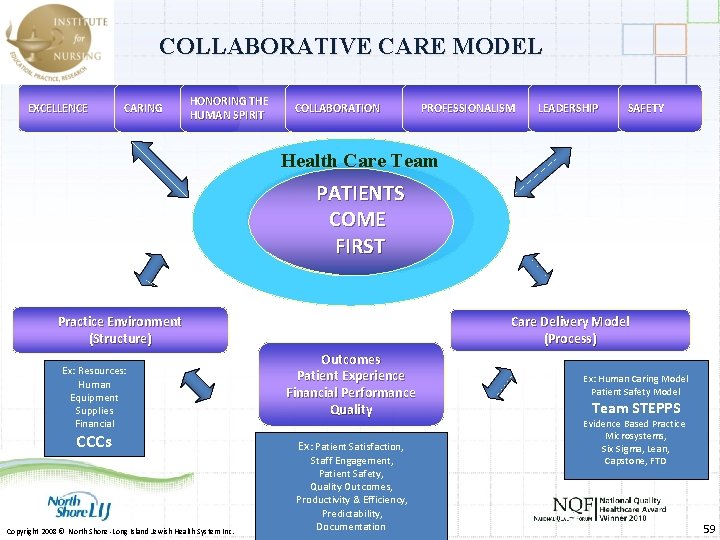
COLLABORATIVE CARE MODEL EXCELLENCE CARING HONORING THE HUMAN SPIRIT COLLABORATION PROFESSIONALISM LEADERSHIP SAFETY Health Care Team PATIENTS COME FIRST Practice Environment (Structure) Ex: Resources: Human Equipment Supplies Financial CCCs Copyright 2008 © North Shore -Long Island Jewish Health System Inc. Care Delivery Model (Process) Outcomes Patient Experience Financial Performance Quality Ex: Patient Satisfaction, Staff Engagement, Patient Safety, Quality Outcomes, Productivity & Efficiency, Predictability, Documentation Ex: Human Caring Model Patient Safety Model Team STEPPS Evidence Based Practice Microsystems, Six Sigma, Lean, Capstone, FTD 59
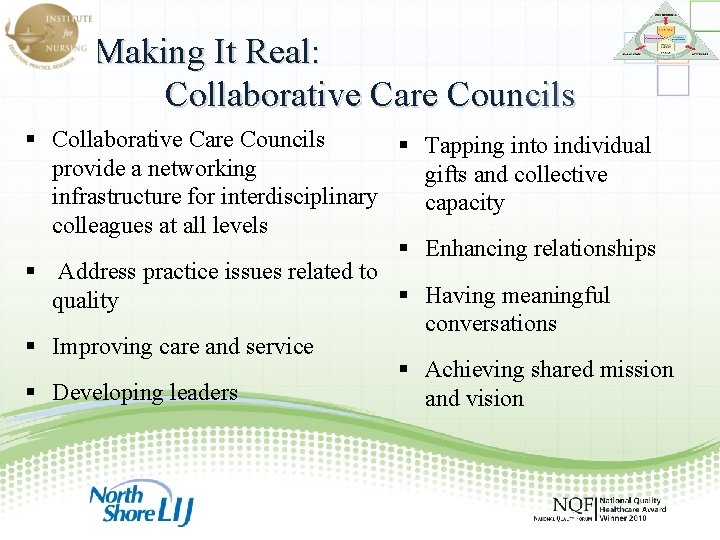
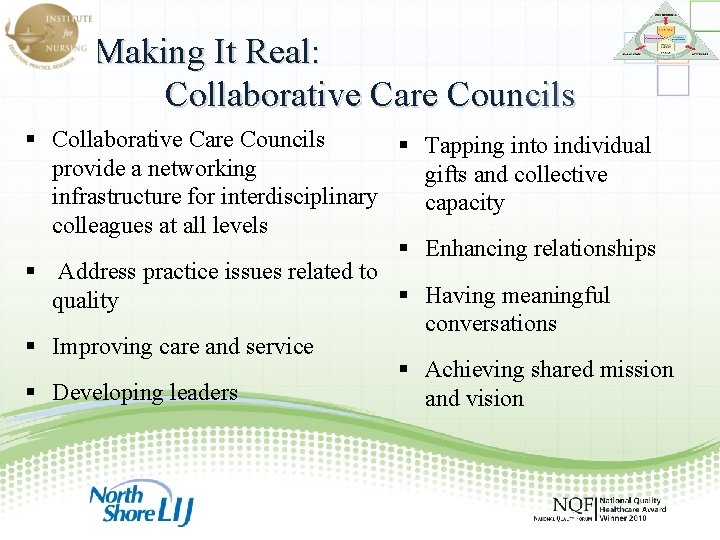
Making It Real: Collaborative Care Councils Tapping into individual provide a networking gifts and collective infrastructure for interdisciplinary capacity colleagues at all levels Enhancing relationships Address practice issues related to Having meaningful quality conversations Improving care and service Achieving shared mission Developing leaders and vision
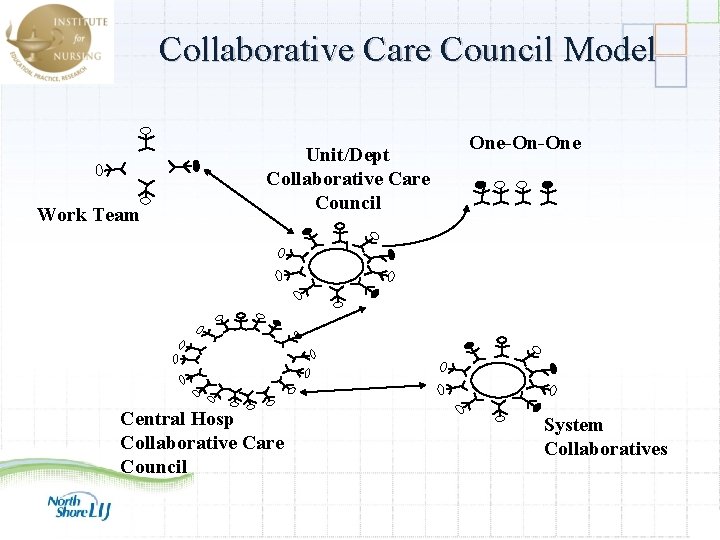
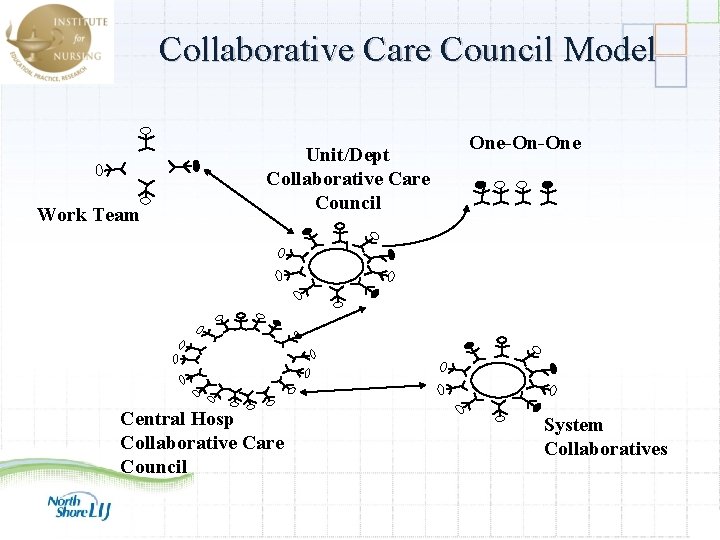
Collaborative Care Council Model Work Team Unit/Dept Collaborative Care Council One-On-One Central Hosp Collaborative Care Council System Collaboratives 61
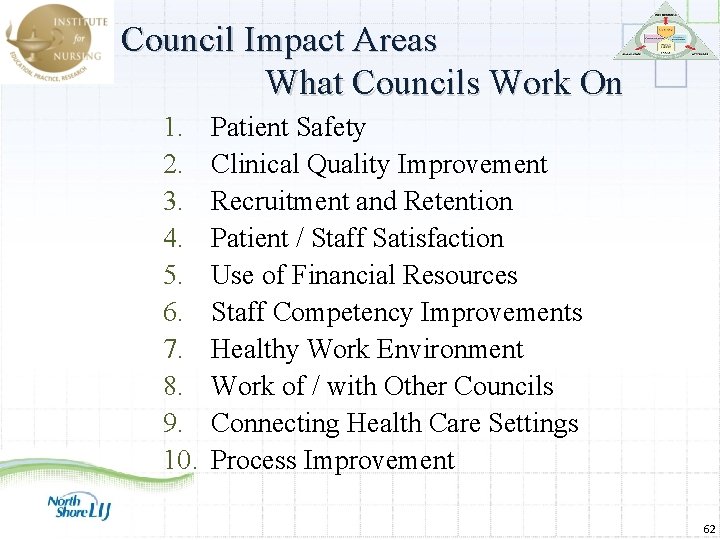
Council Impact Areas What Councils Work On 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Patient Safety Clinical Quality Improvement Recruitment and Retention Patient / Staff Satisfaction Use of Financial Resources Staff Competency Improvements Healthy Work Environment Work of / with Other Councils Connecting Health Care Settings Process Improvement 62

Key Council Success Strategies Multi-modal Communication plan Standardized Agenda Advanced scheduling of meetings 63
1: 1 Critical to Sustainability and Growth ØStaff build relationships one person at a time ØEnhances interpersonal relationships ØEveryone feels connected and a part of decisions ØAccountability increases - becomes “our decision” 64
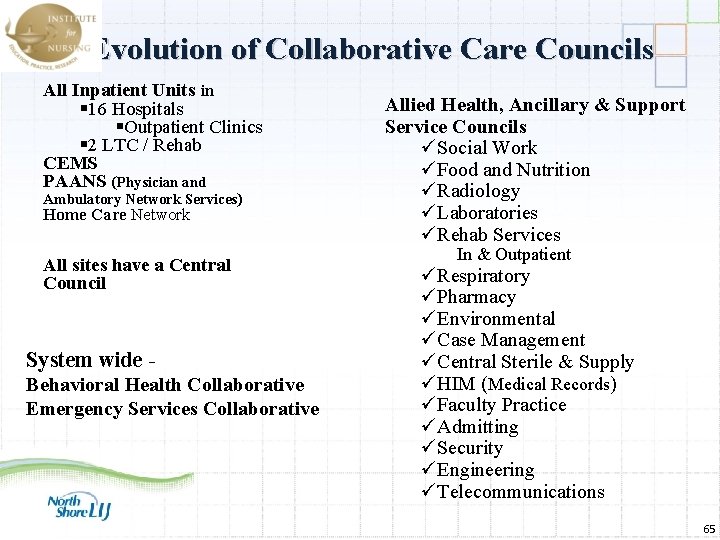
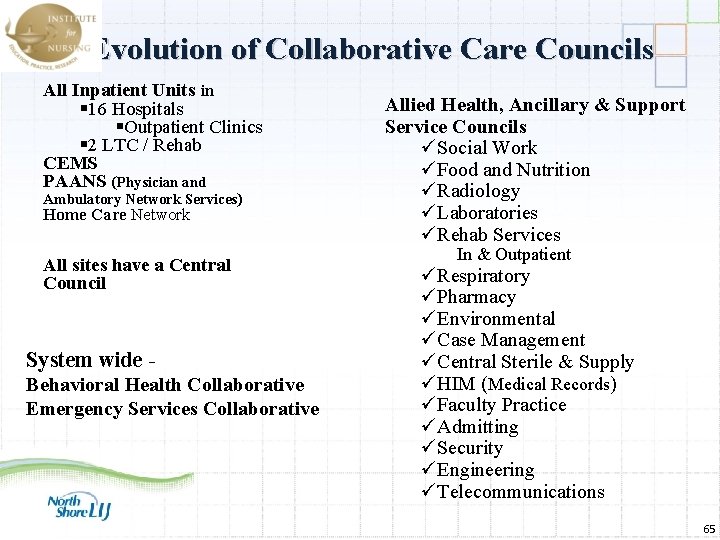
Evolution of Collaborative Care Councils All Inpatient Units in 16 Hospitals Outpatient Clinics 2 LTC / Rehab CEMS PAANS (Physician and Ambulatory Network Services) Home Care Network All sites have a Central Council System wide Behavioral Health Collaborative Emergency Services Collaborative Allied Health, Ancillary & Support Service Councils üSocial Work üFood and Nutrition üRadiology üLaboratories üRehab Services In & Outpatient üRespiratory üPharmacy üEnvironmental üCase Management üCentral Sterile & Supply üHIM (Medical Records) üFaculty Practice üAdmitting üSecurity üEngineering üTelecommunications 65
Team. STEPPS Showcases 66

Success Factors Unique to NSLIJ Implementation across a diverse care continuum 67
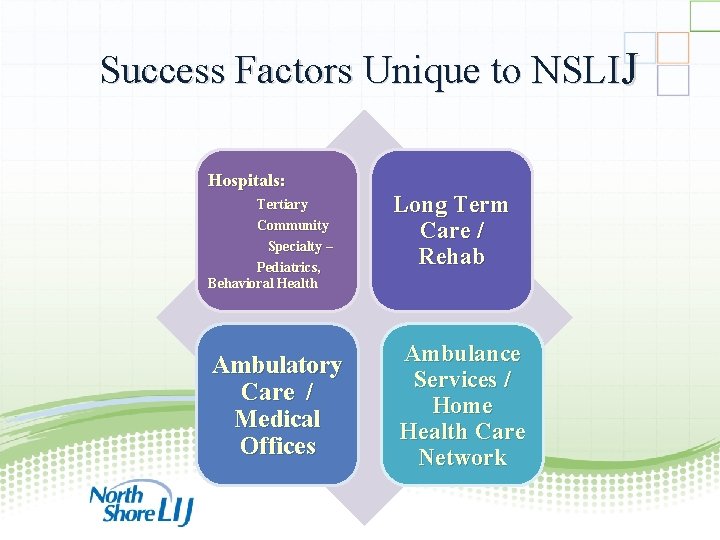
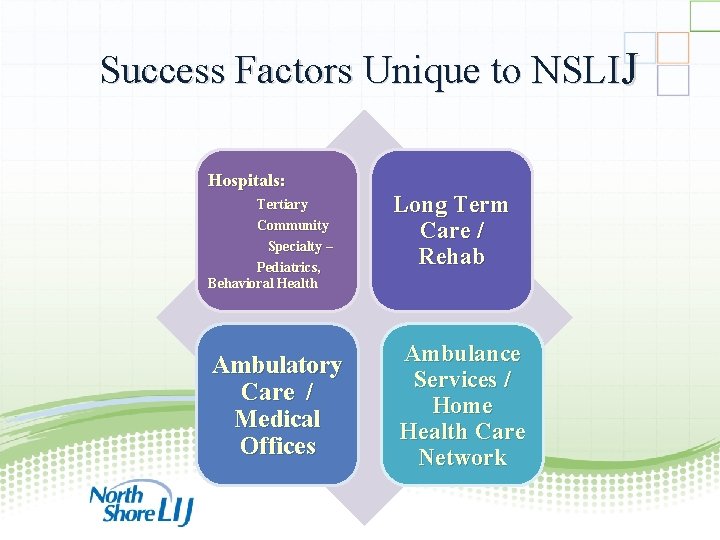
Success Factors Unique to NSLIJ Hospitals: Tertiary Community Specialty – Pediatrics, Behavioral Health Ambulatory Care / Medical Offices Long Term Care / Rehab Ambulance Services / Home Health Care Network 68

Unique to NSLIJ CCCs = Change Team is Permanent Videos Leaders Physicians & Staff Leadership Support & Engagement 69

Unique to NSLIJ All Clinical Leaders / Dept Heads attend Master Training All Clinical Leaders / Dept Heads become Trainers or Coaches System Policy / Procedure Human Resources Team. STEPPS Tools & Strategies anchored in daily practice … Orientation Simulation scenarios 70
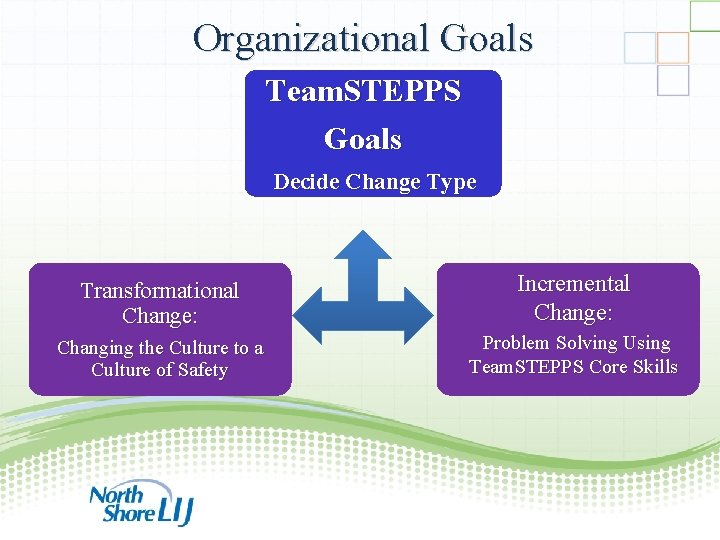
Organizational Goals Team. STEPPS Goals Decide Change Type Transformational Change: Changing the Culture to a Culture of Safety Incremental Change: Problem Solving Using Team. STEPPS Core Skills 71
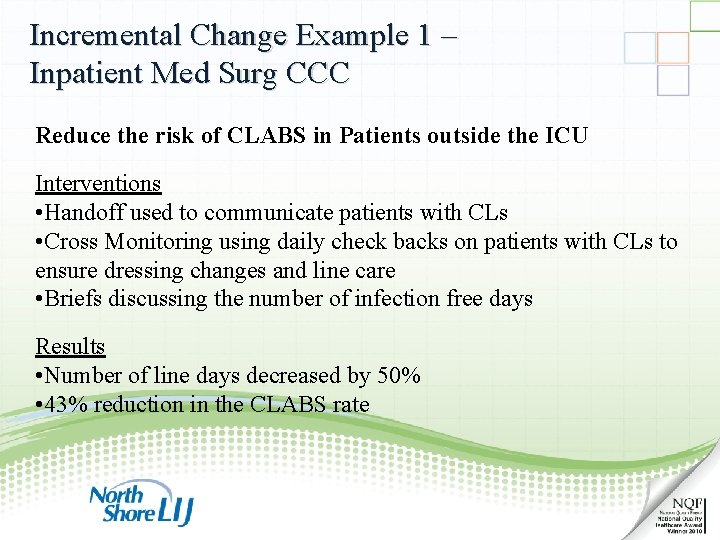
Incremental Change Example 1 – Inpatient Med Surg CCC Reduce the risk of CLABS in Patients outside the ICU Interventions • Handoff used to communicate patients with CLs • Cross Monitoring using daily check backs on patients with CLs to ensure dressing changes and line care • Briefs discussing the number of infection free days Results • Number of line days decreased by 50% • 43% reduction in the CLABS rate 72
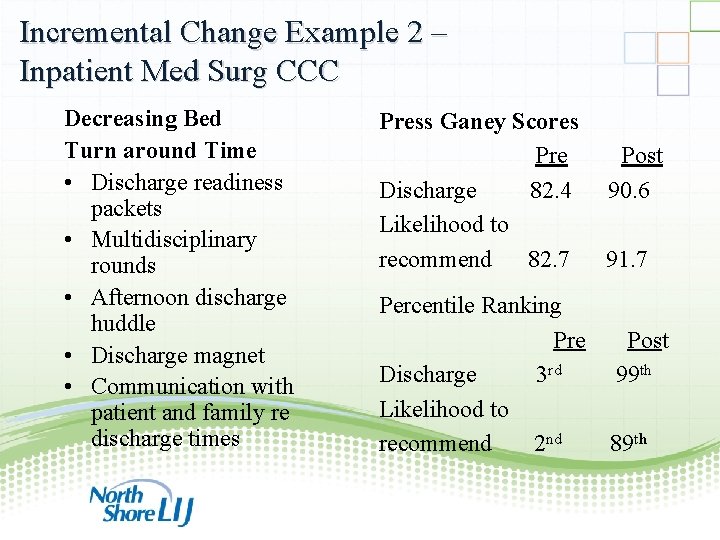
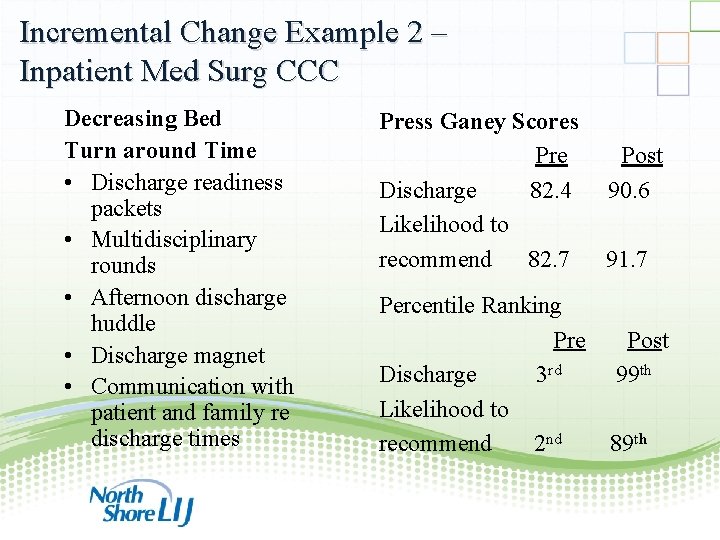
Incremental Change Example 2 – Inpatient Med Surg CCC Decreasing Bed Turn around Time • Discharge readiness packets • Multidisciplinary rounds • Afternoon discharge huddle • Discharge magnet • Communication with patient and family re discharge times Press Ganey Scores Pre Post Discharge 82. 4 90. 6 Likelihood to recommend 82. 7 91. 7 Percentile Ranking Pre Post Discharge 3 rd 99 th Likelihood to recommend 2 nd 89 th 73
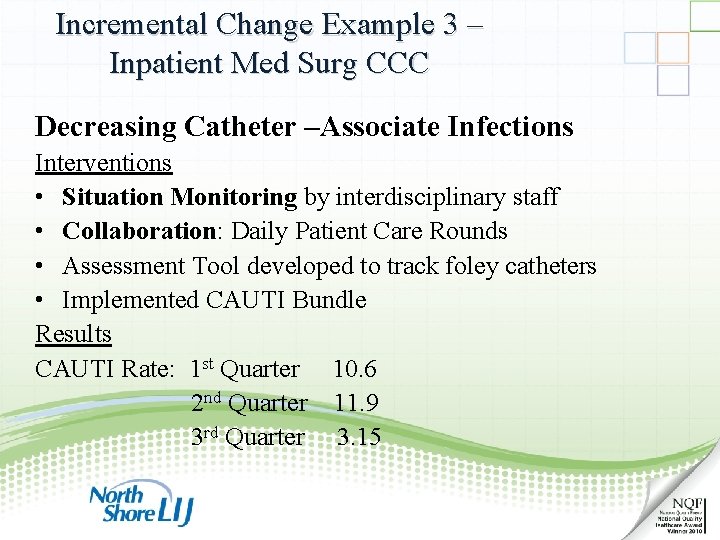
Incremental Change Example 3 – Inpatient Med Surg CCC Decreasing Catheter –Associate Infections Interventions • Situation Monitoring by interdisciplinary staff • Collaboration: Daily Patient Care Rounds • Assessment Tool developed to track foley catheters • Implemented CAUTI Bundle Results CAUTI Rate: 1 st Quarter 10. 6 2 nd Quarter 11. 9 3 rd Quarter 3. 15 74
Team. STEPPS: The glue that binds it all together… Tea m ST EP Acu te C are PS Ho m Ca e re CE MS Am bul ato r y 75
The only way to discover the limits of the possible is to go beyond them into the impossible. ~ Arthur C. Clarke 76

77