Teaching TraumaInformed Care Responding to Adverse Childhood Experiences


- Slides: 21
Teaching Trauma-Informed Care: Responding to Adverse Childhood Experiences (ACEs) in a Residency Setting Daniel J. Harkness, Ph. D, LMFT Stacey K. Neu, MD
Disclosures • We have no disclosures to report.

Who We Are

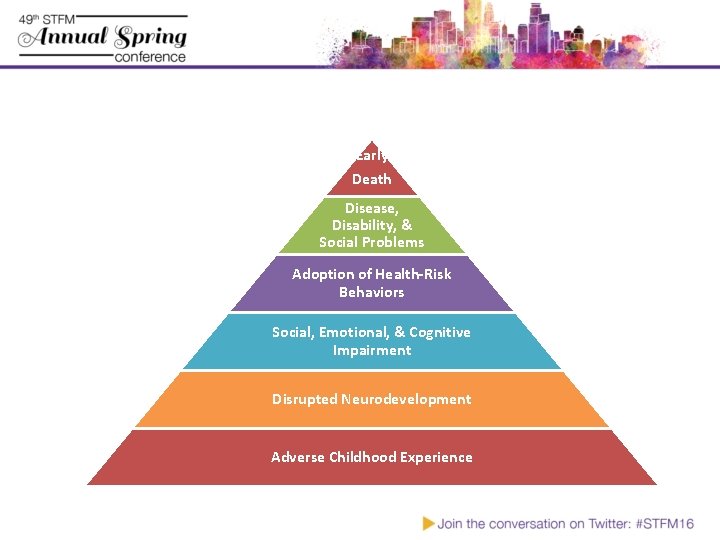
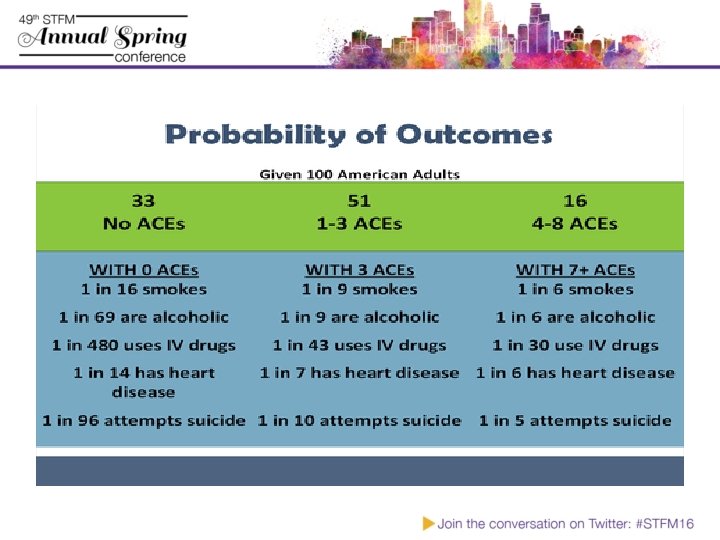
ACE Study • Kaiser Permanente • Drs. Felliti (Kaiser) and Anda (CDC) • More than 17, 000 participants completed a standardized physical examination. • General Findings: Childhood experiences are powerful determinants of who we become as adults. • Showed a linear correlation between ACEs and chronic disease states
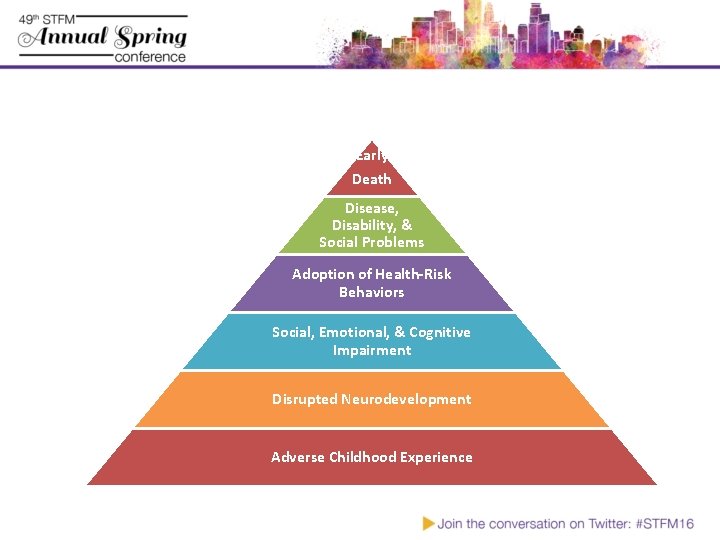
Early Death Disease, Disability, & Social Problems Adoption of Health-Risk Behaviors Social, Emotional, & Cognitive Impairment Disrupted Neurodevelopment Adverse Childhood Experience
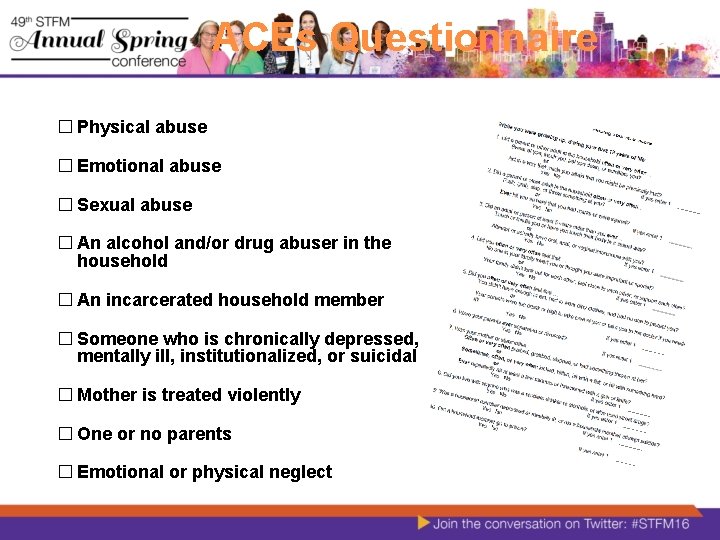
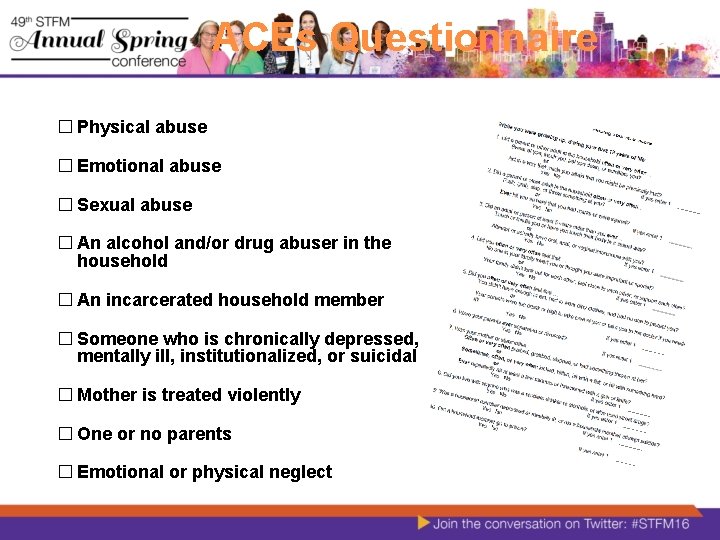
ACEs Questionnaire � Physical abuse � Emotional abuse � Sexual abuse � An alcohol and/or drug abuser in the household � An incarcerated household member � Someone who is chronically depressed, mentally ill, institutionalized, or suicidal � Mother is treated violently � One or no parents � Emotional or physical neglect
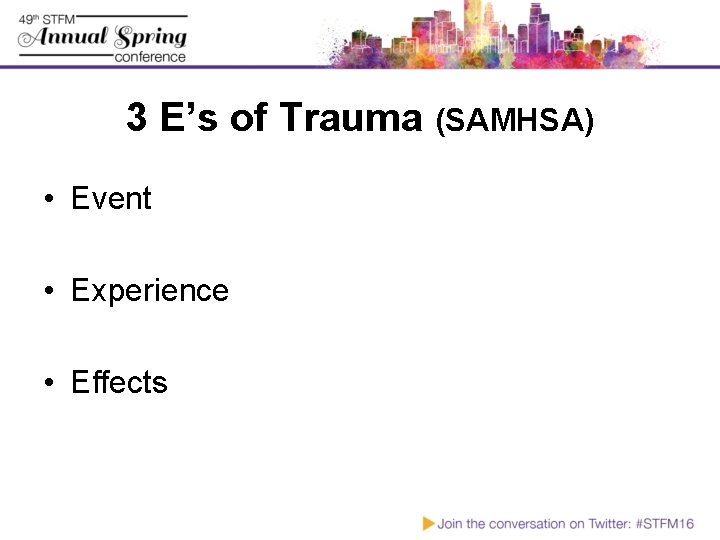
3 E’s of Trauma (SAMHSA) • Event • Experience • Effects
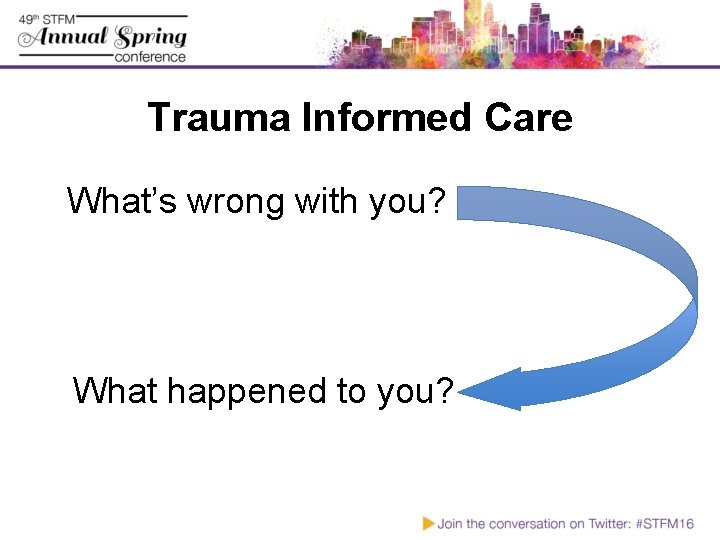
Trauma Informed Care What’s wrong with you? What happened to you?
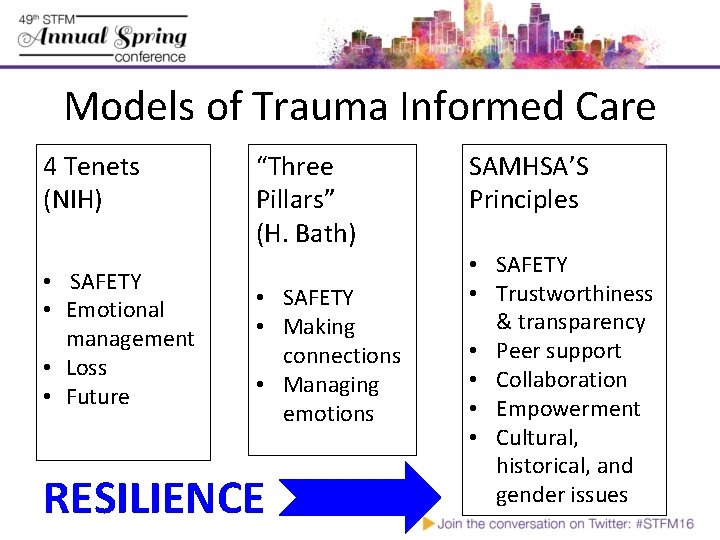
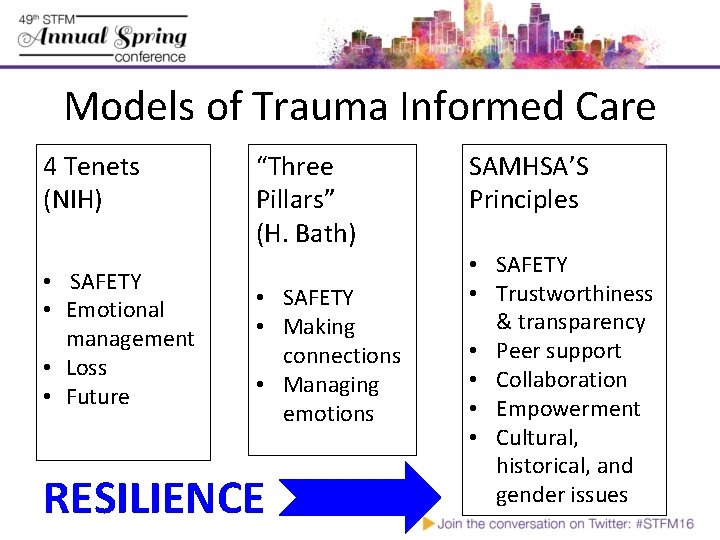
Models of Trauma Informed Care 4 Tenets (NIH) • SAFETY • Emotional management • Loss • Future “Three Pillars” (H. Bath) • SAFETY • Making connections • Managing emotions RESILIENCE SAMHSA’S Principles • SAFETY • Trustworthiness & transparency • Peer support • Collaboration • Empowerment • Cultural, historical, and gender issues
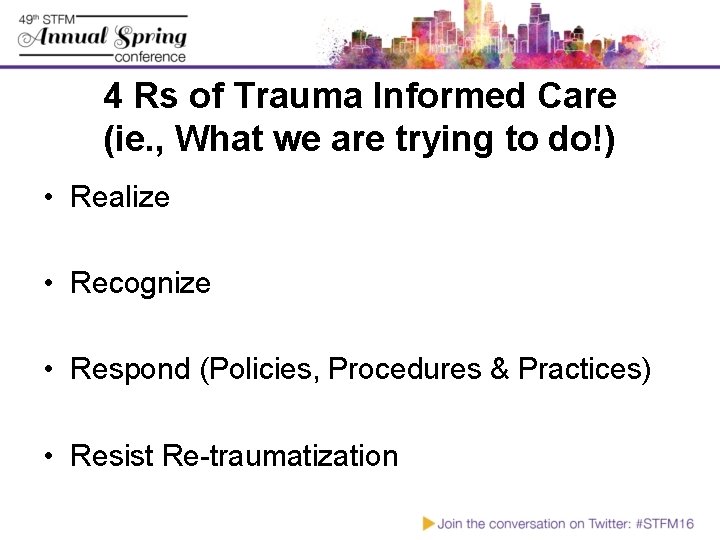
4 Rs of Trauma Informed Care (ie. , What we are trying to do!) • Realize • Recognize • Respond (Policies, Procedures & Practices) • Resist Re-traumatization
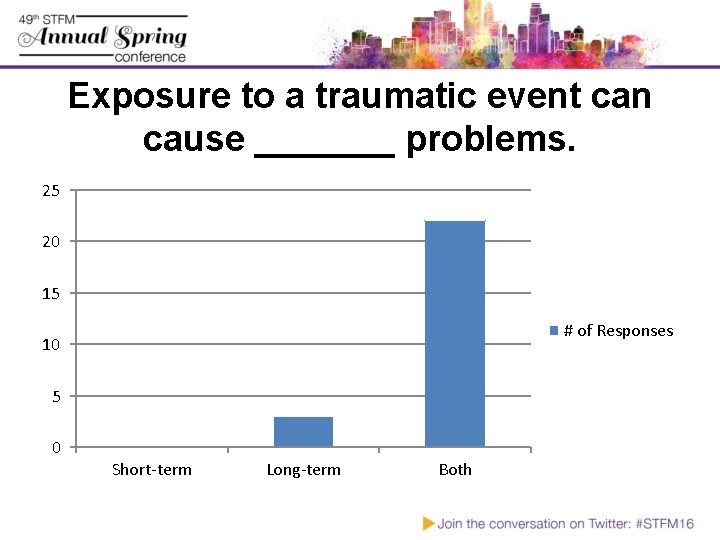
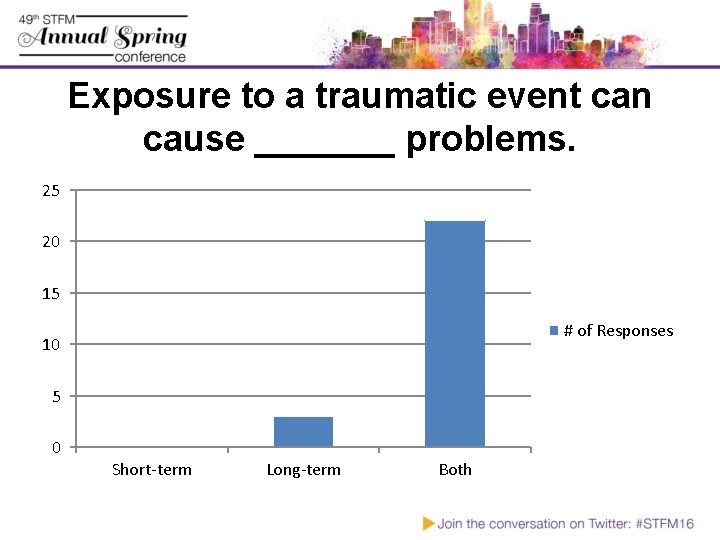
Exposure to a traumatic event can cause _______ problems. 25 20 15 # of Responses 10 5 0 Short-term Long-term Both
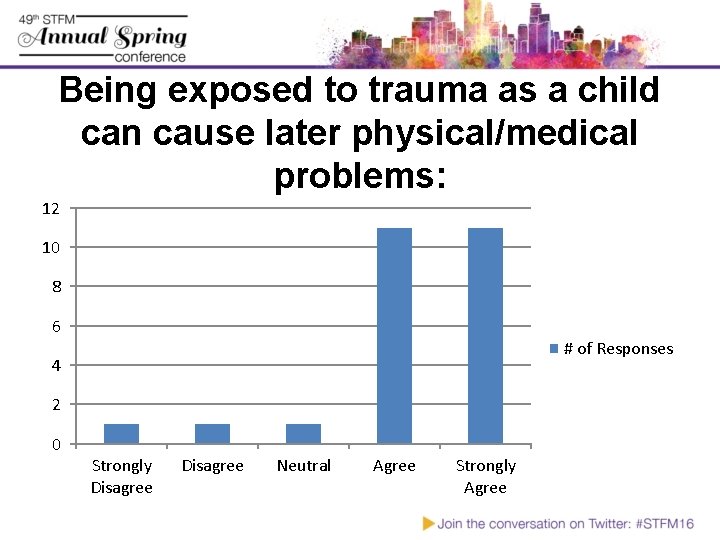
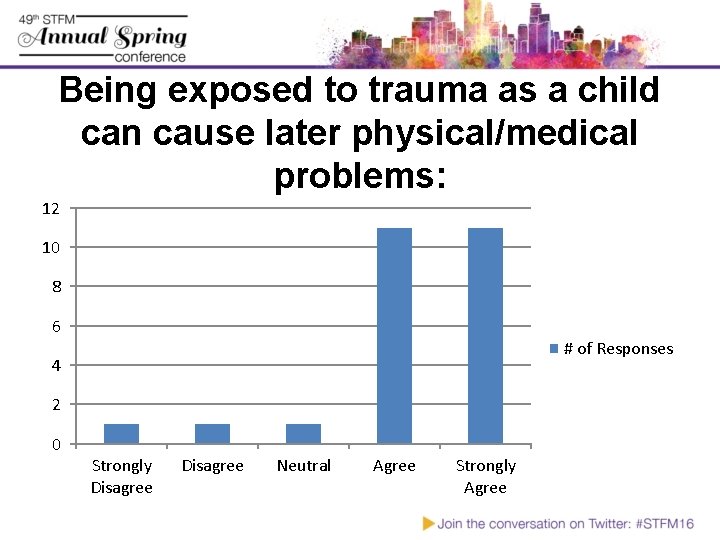
Being exposed to trauma as a child can cause later physical/medical problems: 12 10 8 6 # of Responses 4 2 0 Strongly Disagree Neutral Agree Strongly Agree
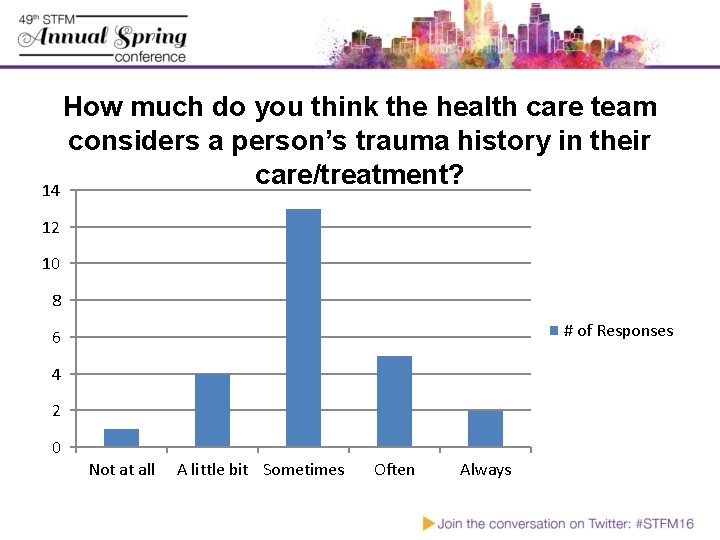
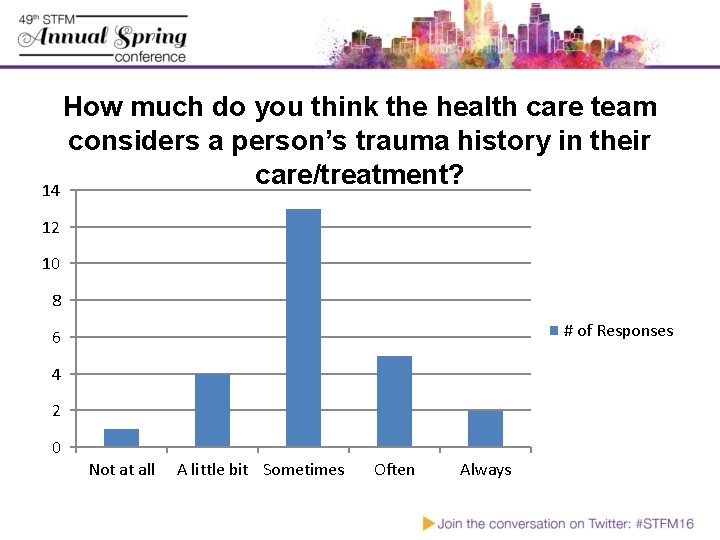
How much do you think the health care team considers a person’s trauma history in their care/treatment? 14 12 10 8 # of Responses 6 4 2 0 Not at all A little bit Sometimes Often Always
Progression of Project • Late Fall, 2014 – Summer, 2015 – Outline of prospective education – Completed pre-survey (a lot of info was not new to them because of ACEs) – Survey results informed content for education sessions – Created 6 brief sessions; taught at monthly staff meetings (next slide) – Reflected back to staff what was helpful • Late Fall, 2015 - Current – – – – November: 2 nd set of sessions began by reviewing previous topics December: Intro to ACEs & impact on health, economy and workforce January: Review TIC models; Queried staff on what they still needed. February: Clinic-based “self-assessment” March: Spring Break April: Resilience and plan from book “Childhood Disrupted” May: R 3 presents on attachment disorders r/t trauma
Monthly Curriculum (beg. 2014) 1. Introduction and defining trauma 2. ACEs & the relationship to high-risk behaviors and chronic disease development 3. Reviewing models of Trauma Informed Care (with a focus on a safe environment) 4. Taking their own ACE questionnaire and offering EAP services 5. Scenarios of traumatized individuals in a clinic setting 6. Hope and resilience
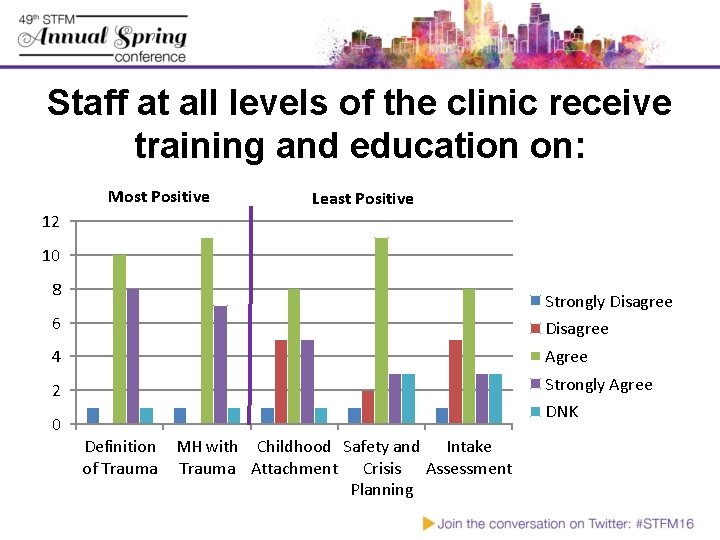
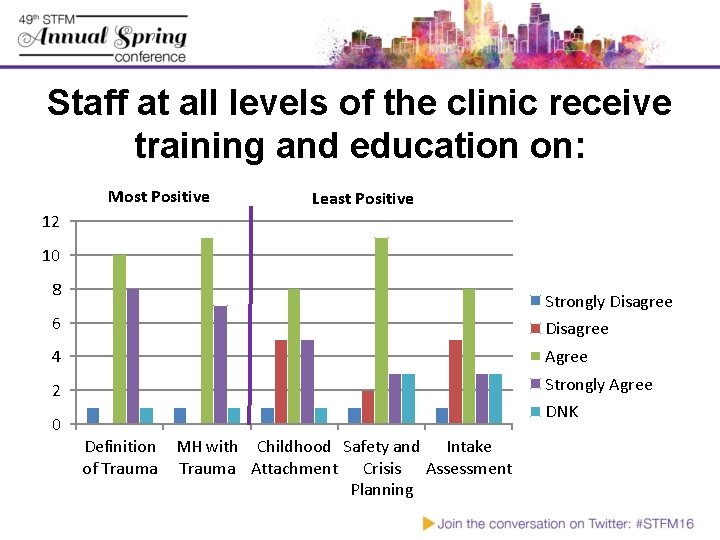
Staff at all levels of the clinic receive training and education on: Most Positive Least Positive 12 10 8 Strongly Disagree 6 Disagree 4 Agree 2 Strongly Agree 0 DNK Definition of Trauma MH with Childhood Safety and Intake Trauma Attachment Crisis Assessment Planning
Case Example • A long-time EDM patient calls in to the clinic asking to talk to a doctor or nurse immediately. This patient is well-known to providers and nurses as a high utilizer of healthcare services. His family members have been EDM patients for decades so you know history. He starts demanding his refills because they are due today but his physician is not in clinic today or the rest of the week. He sounds as if he is slurring his speech and you can hear his girlfriend yelling at him in the background. He says that if he cannot get his refill order, he will kill himself.
Trauma-Sensitive Practice • • • Respect Taking time Rapport Sharing information Sharing control Respecting boundaries Fostering mutual learning Understanding “non-linear” healing Demonstrating awareness and knowledge of trauma
Limitations • EPIC implemented May, 2015 • Didn’t finish 6 th educational session until August, 2015 • Significant staff turnover limited survey results and follow-up
Please evaluate this presentation using the conference mobile app! Simply click on the "clipboard" icon on the presentation page.