TEACHING FILES Dr Mayur R 2 Dr Payal









- Slides: 107
TEACHING FILES Dr Mayur R 2, Dr Payal R 1 Dept of Radiodiagnosis Medical College & S S G Hospital, Baroda ( 31 -12 -07 )
CASE 1
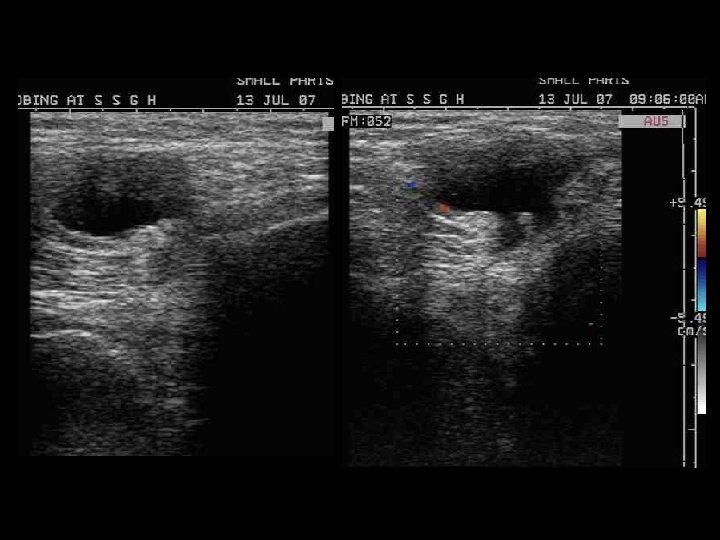
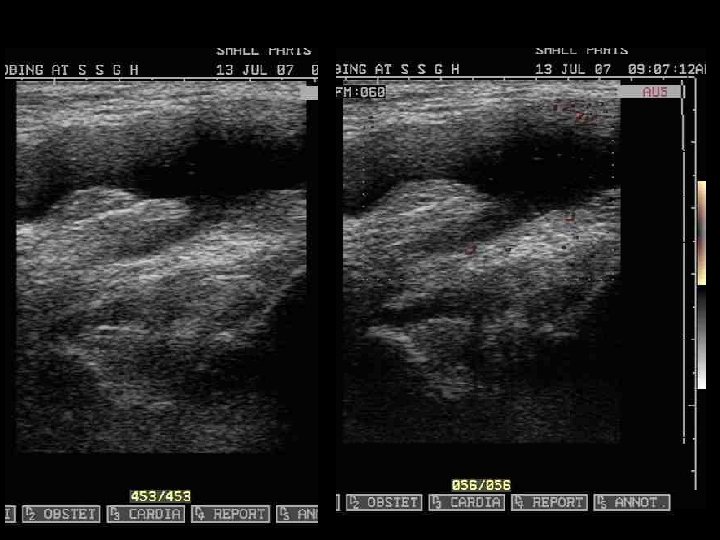
56 yr M, presented with a gradually progressing swelling in posterior region of knee & discomfort.
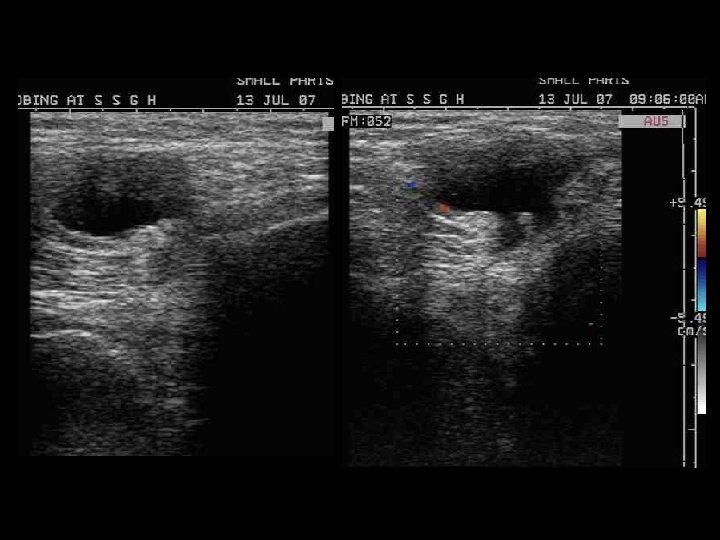
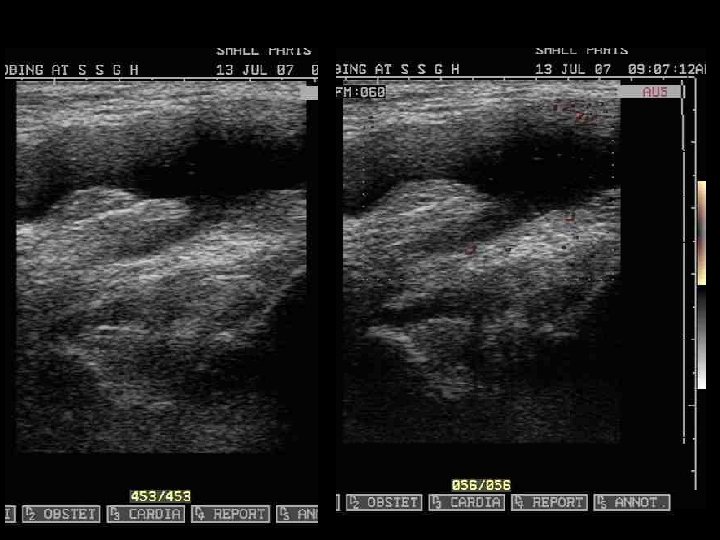
D/D OF CYSTIC LESION AROUND THE KNEE 1. Baker’s cyst 2. Popliteal aneurysm 3. Ganglion 4. Meniscal cysts 5. Collection or abscess
Backer or Popliteal cyst • It represents fluid distention of a bursa (gastrocnemiosemimembranosus bursa) between the gastrocnemius and semimembranosus tendons via a communication with the knee joint. • Although c/as the gastrocnemiosemimembranosus bursa, it represents a composite of two bursae: – a bursa anterior to the medial gastrocnemius tendon (the subgastrocnemius bursa) and – a bursa between the tendons of the gastrocnemius and semimembranosus tendons
• most common associations include joint effusion, meniscal tear, and degenerative joint disease • MRI gives the typical appearance of the fluid containing structure, with low SI on T 1 W & high SI on T 2 W. • Occasionally the cyst can leak fluid into the calf and cause calf swelling, tightness & pain ( rupture backer cyst ). This may even simulate a calf DVT (deep vein thrombosis). It is easily diagnosed by a careful examination and an ultrasound scan or on MRI.
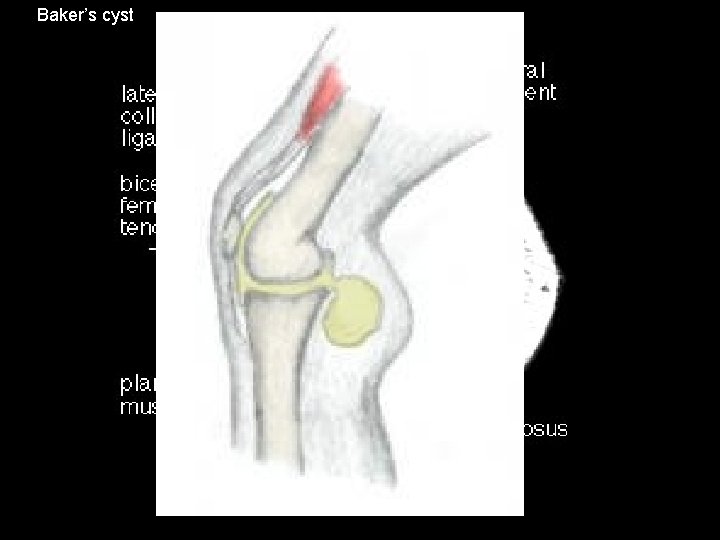
Baker’s cyst
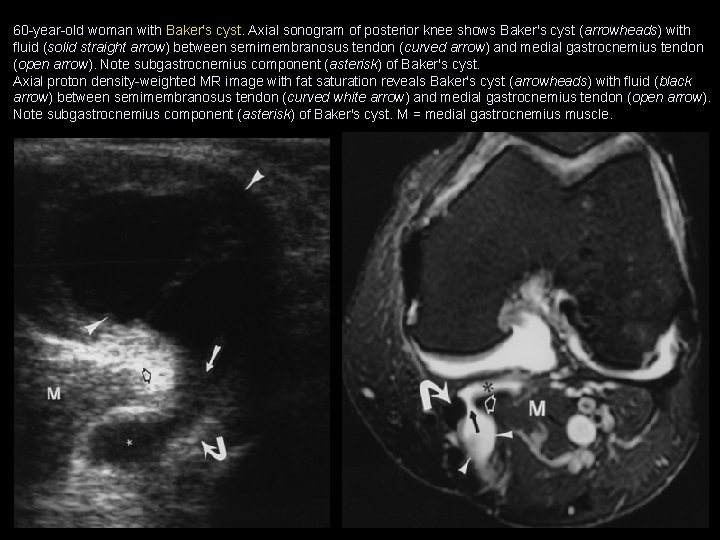
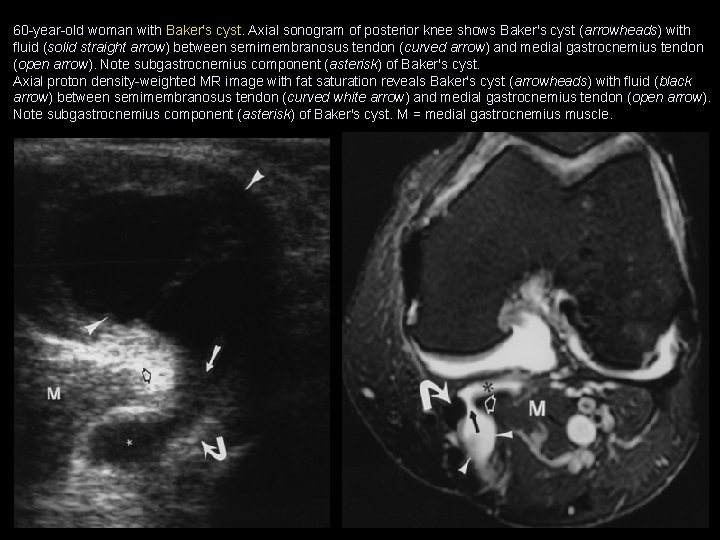
60 -year-old woman with Baker's cyst. Axial sonogram of posterior knee shows Baker's cyst (arrowheads) with fluid (solid straight arrow) between semimembranosus tendon (curved arrow) and medial gastrocnemius tendon (open arrow). Note subgastrocnemius component (asterisk) of Baker's cyst. Axial proton density-weighted MR image with fat saturation reveals Baker's cyst (arrowheads) with fluid (black arrow) between semimembranosus tendon (curved white arrow) and medial gastrocnemius tendon (open arrow). Note subgastrocnemius component (asterisk) of Baker's cyst. M = medial gastrocnemius muscle.
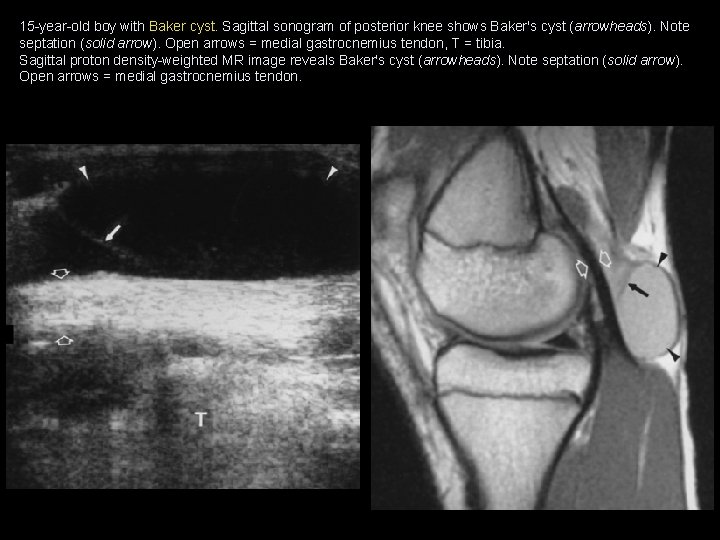
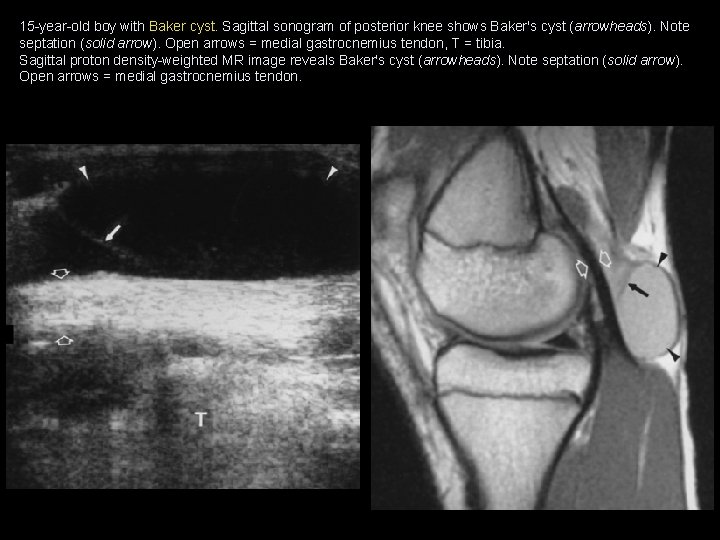
15 -year-old boy with Baker cyst. Sagittal sonogram of posterior knee shows Baker's cyst (arrowheads). Note septation (solid arrow). Open arrows = medial gastrocnemius tendon, T = tibia. Sagittal proton density-weighted MR image reveals Baker's cyst (arrowheads). Note septation (solid arrow). Open arrows = medial gastrocnemius tendon.
Meniscal cysts • It is a accumulation of fluid in association with an adjacent meniscus tear extending from the joint surface to its outer border. • Joint fluid is forced in to the cyst when patient walks & accumulates at the meniscocapsular margins. • When a Meniscal cysts is incidentally detected on the MRI, a careful attention must be paid to the adjacent meniscus.

13 -year-old girl with meniscal cyst. Sagittal proton density-weighted MR image reveals meniscal cyst (curved arrow) in continuity with meniscal tear (straight arrow). Axial proton density-weighted MR image with fat saturation reveals meniscal cyst (curved arrow) with signal intensity of fluid without extension between semimembranosus tendon (undulating arrow) and medial gastrocnemius tendon (arrowhead).
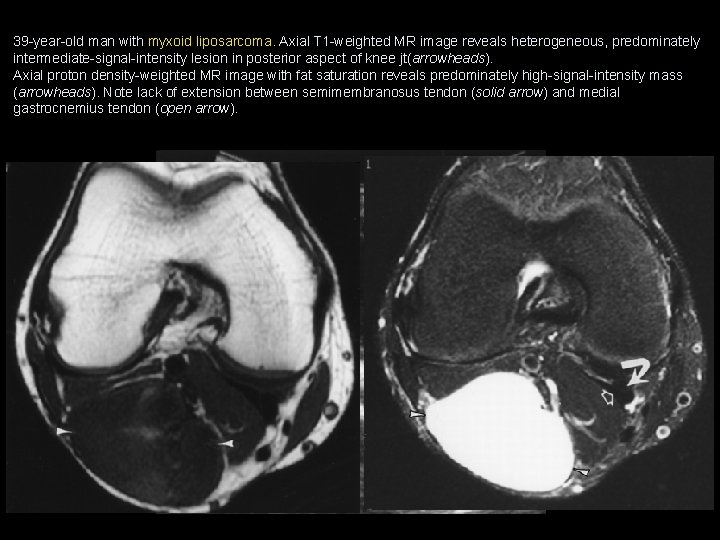
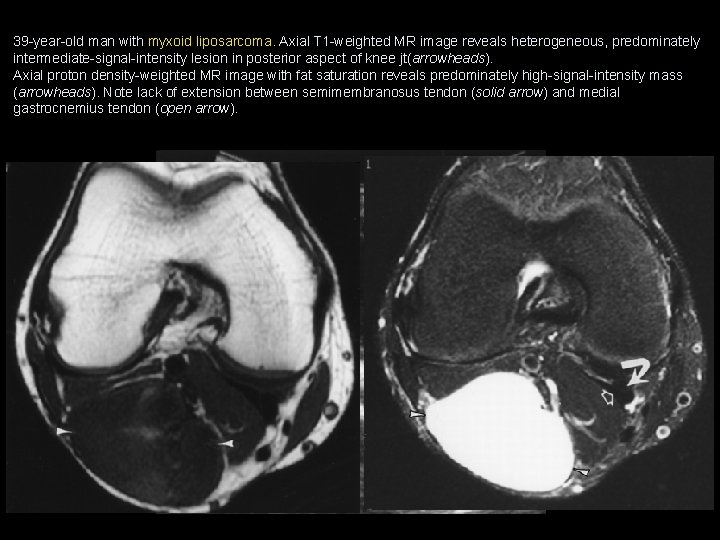
39 -year-old man with myxoid liposarcoma. Axial T 1 -weighted MR image reveals heterogeneous, predominately intermediate-signal-intensity lesion in posterior aspect of knee jt(arrowheads). Axial proton density-weighted MR image with fat saturation reveals predominately high-signal-intensity mass (arrowheads). Note lack of extension between semimembranosus tendon (solid arrow) and medial gastrocnemius tendon (open arrow).
Treatment • It is best treated by treating the cause of the excess fluid (fixing the cartilage tear or arthritis) and then the Bakers cyst usually fades away. • A large and persistent Bakers cyst may require surgical removal which is done through an incision across the back of the knee, although it can sometimes be removed by arthroscopic surgery.
CASE 2
• 25 years old female. • H/O Primary infertility, referred for pelvic ultrasound. • No other complaints. • Past & family histories are not significant. • P/V : NAD
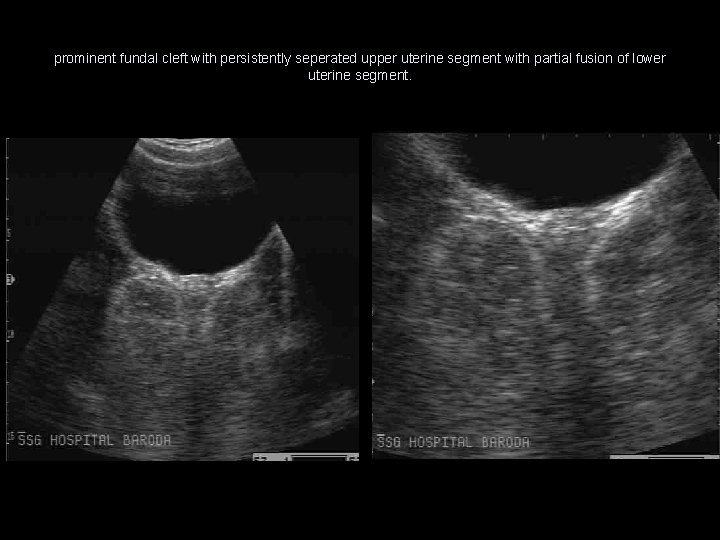
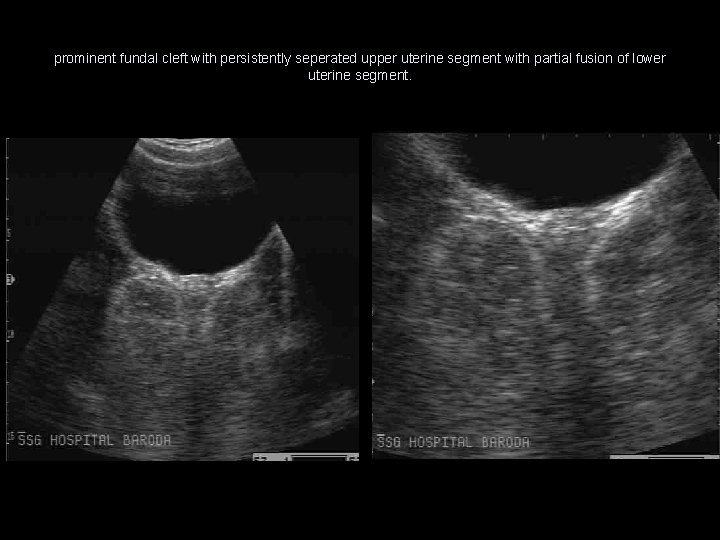
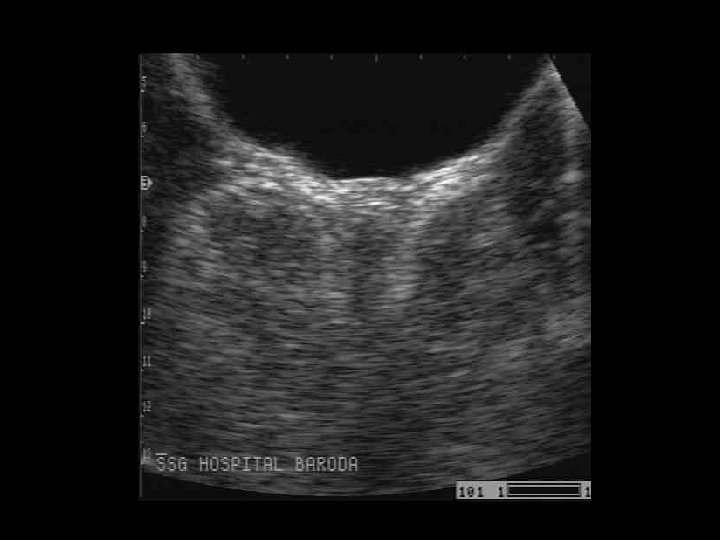
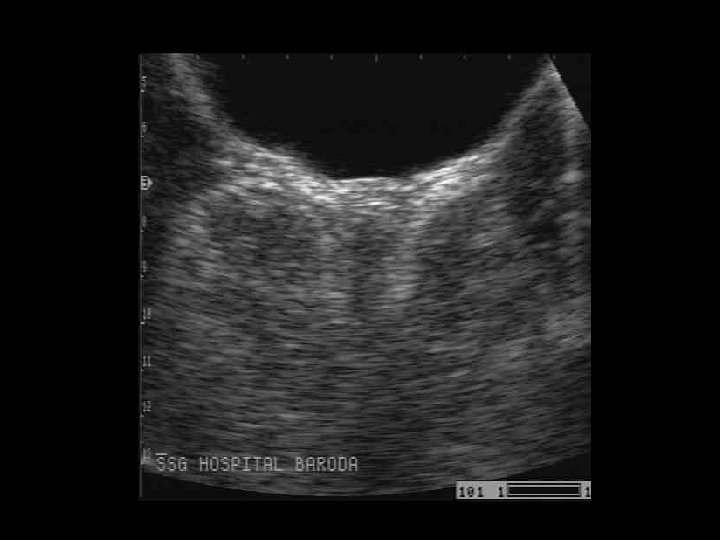
prominent fundal cleft with persistently seperated upper uterine segment with partial fusion of lower uterine segment.
Diagnosis • Uterus bicornis unicollis

Discussing the Müllerian duct anomalies • Two paired müllerian ducts ultimately develop into the structures of the female reproductive tract. • The structures include the fallopian tubes, uterus, cervix, and upper two thirds of the vagina. • The ovaries and lower one third of the vagina have separate embryologic origins not derived from the müllerian system. • Müllerian duct anomalies are categorized most commonly into 7 classes according to the American Fertility Society (AFS) Classification Scheme as follows:
Class I (hypoplasia/agenesis) • It includes uterine/cervical agenesis or hypoplasia. • The most common form is the Mayer-Rokitansky-Kuster. Hauser syndrome, which is combined agenesis of the uterus, cervix, and upper portion of the vagina. • Patients have no reproductive potential. • On USG & MRI: – Findings of agenesis include absence of the cervix and/or uterus with a blind-ending vagina. In uterine hypoplasia, the endometrial cavity is small with a reduced intercornual distance (<2 cm).
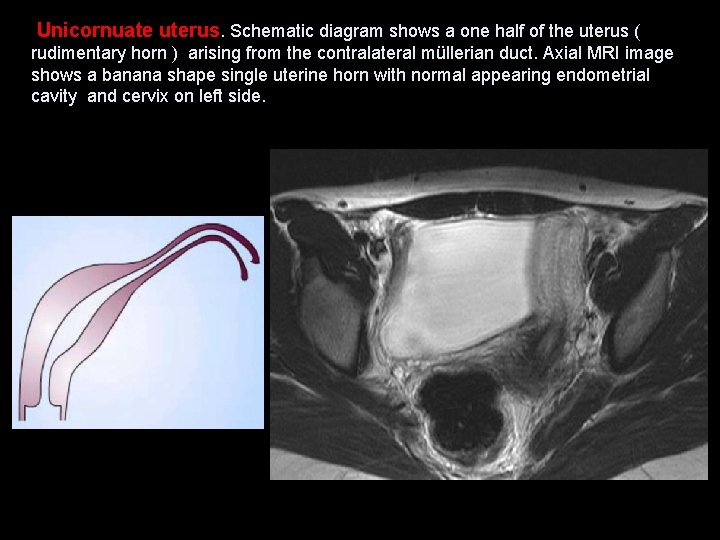
Class II (unicornuate uterus) • Result of complete, or almost complete, arrest of development of one of the müllerian duct. • On USG & MRI: – The unicornuate uterus appears banana shaped without the usual rounded fundal contour and triangular appearance of the fundal cavity. Uterine zonal anatomy is normal. – If obstructed, a rudimentary horn with functioning endometrium may present as a complex hemorrhagic cystic structure. ( blood or blood products on MRI )
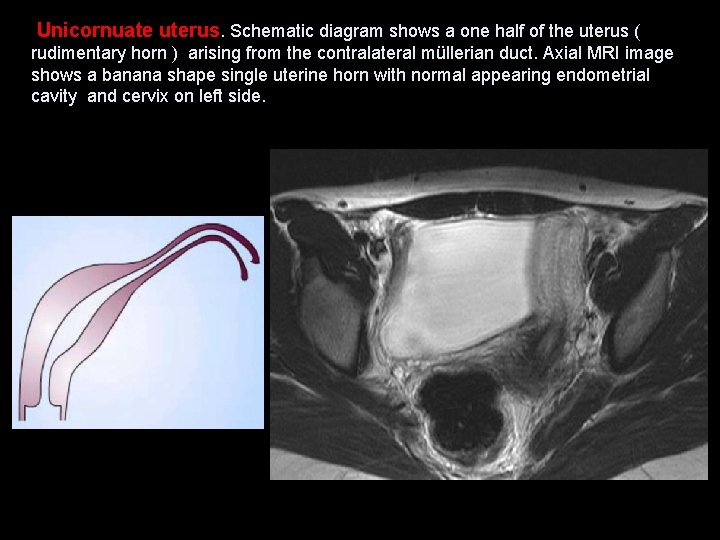
Unicornuate uterus. Schematic diagram shows a one half of the uterus ( rudimentary horn ) arising from the contralateral müllerian duct. Axial MRI image shows a banana shape single uterine horn with normal appearing endometrial cavity and cervix on left side.
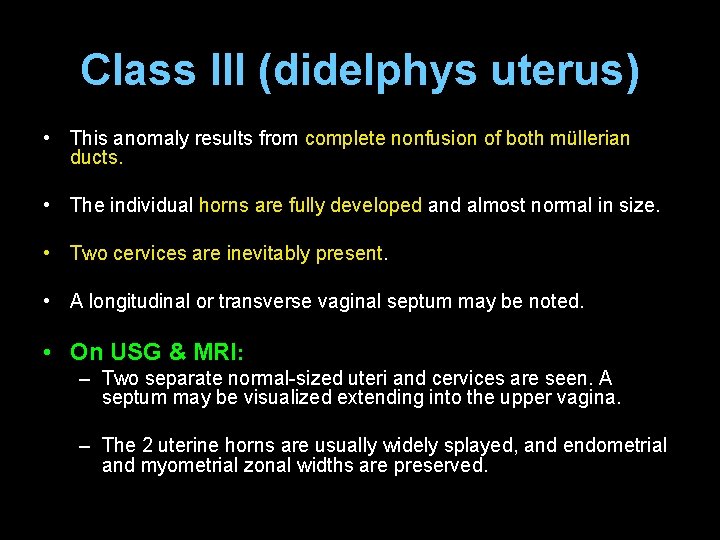
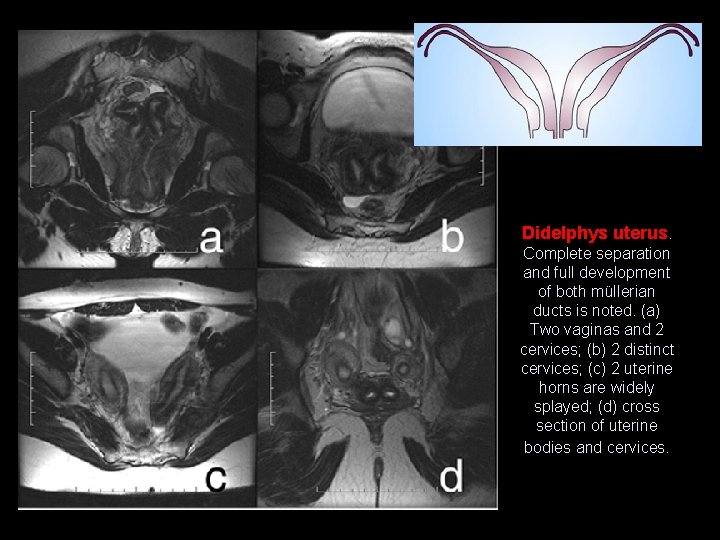
Class III (didelphys uterus) • This anomaly results from complete nonfusion of both müllerian ducts. • The individual horns are fully developed and almost normal in size. • Two cervices are inevitably present. • A longitudinal or transverse vaginal septum may be noted. • On USG & MRI: – Two separate normal-sized uteri and cervices are seen. A septum may be visualized extending into the upper vagina. – The 2 uterine horns are usually widely splayed, and endometrial and myometrial zonal widths are preserved.
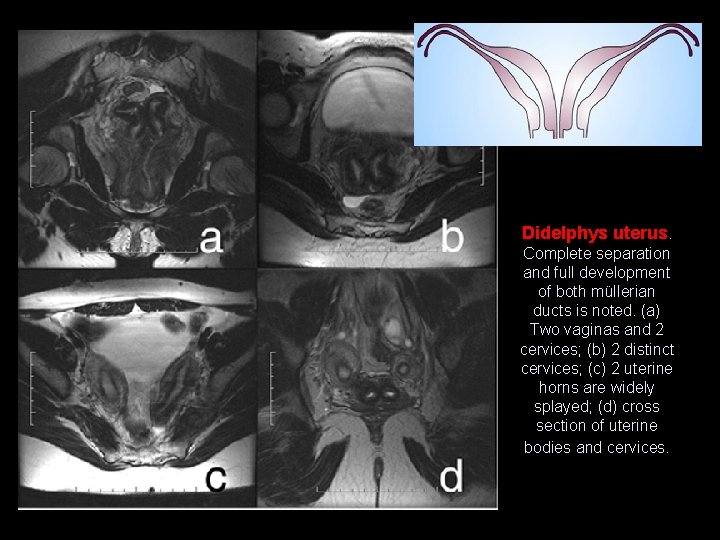
Didelphys uterus. Complete separation and full development of both müllerian ducts is noted. (a) Two vaginas and 2 cervices; (b) 2 distinct cervices; (c) 2 uterine horns are widely splayed; (d) cross section of uterine bodies and cervices.
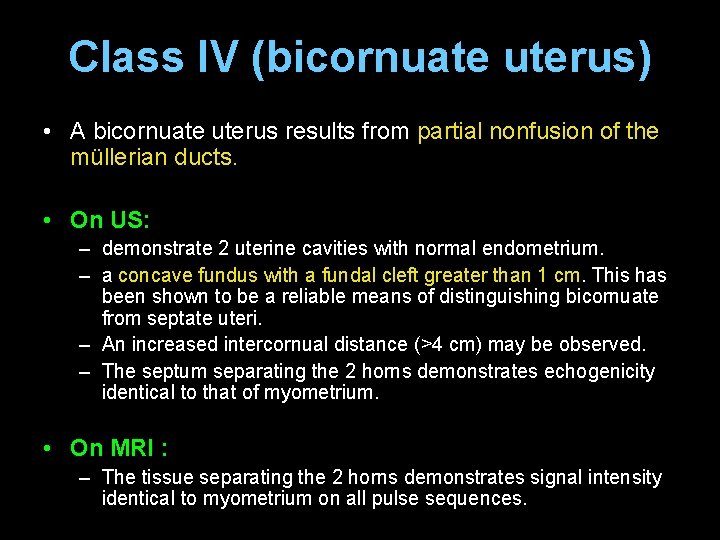
Class IV (bicornuate uterus) • A bicornuate uterus results from partial nonfusion of the müllerian ducts. • On US: – demonstrate 2 uterine cavities with normal endometrium. – a concave fundus with a fundal cleft greater than 1 cm. This has been shown to be a reliable means of distinguishing bicornuate from septate uteri. – An increased intercornual distance (>4 cm) may be observed. – The septum separating the 2 horns demonstrates echogenicity identical to that of myometrium. • On MRI : – The tissue separating the 2 horns demonstrates signal intensity identical to myometrium on all pulse sequences.
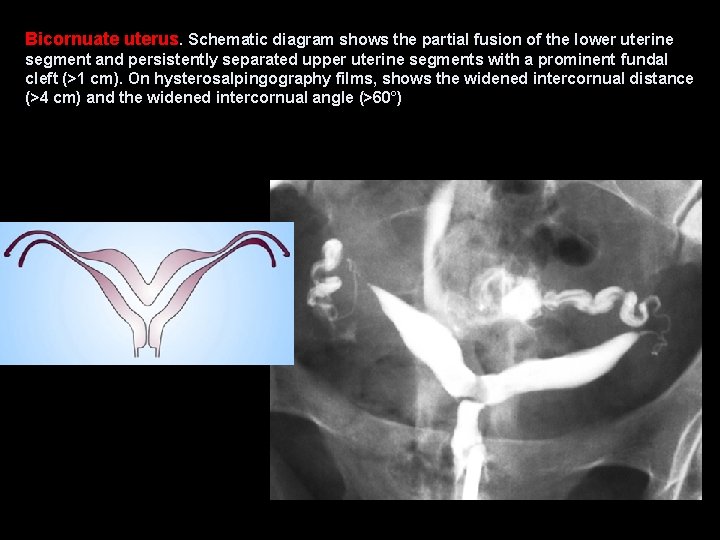
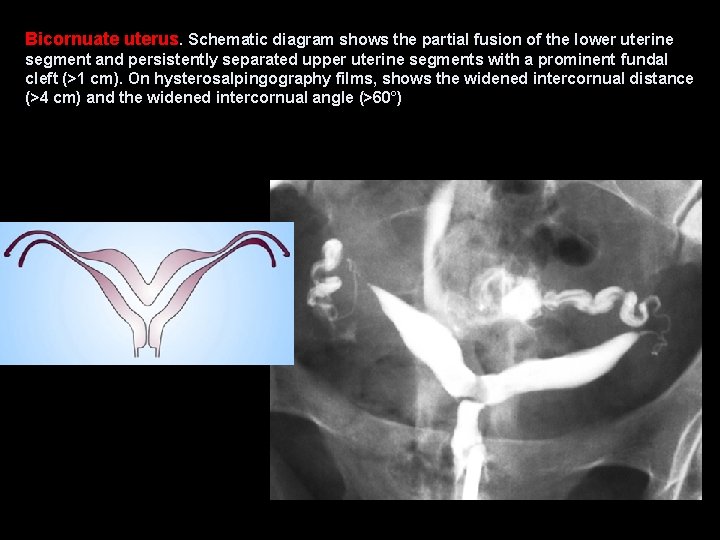
Bicornuate uterus. Schematic diagram shows the partial fusion of the lower uterine segment and persistently separated upper uterine segments with a prominent fundal cleft (>1 cm). On hysterosalpingography films, shows the widened intercornual distance (>4 cm) and the widened intercornual angle (>60°)
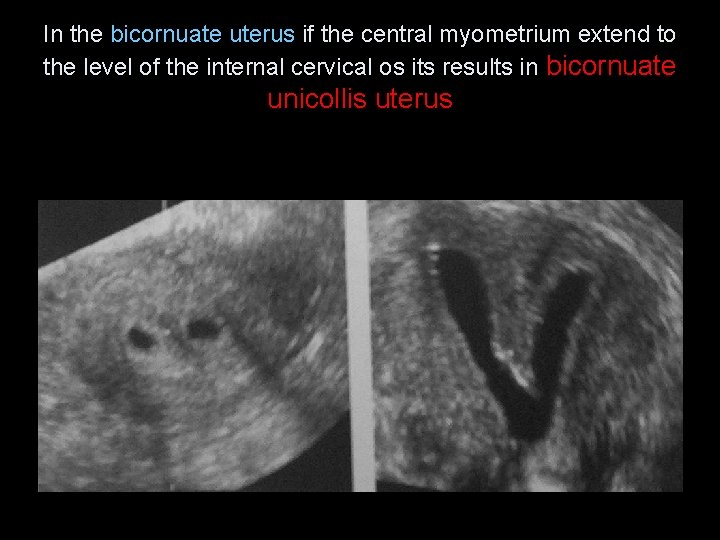
In the bicornuate uterus if the central myometrium extend to the level of the internal cervical os its results in bicornuate unicollis uterus
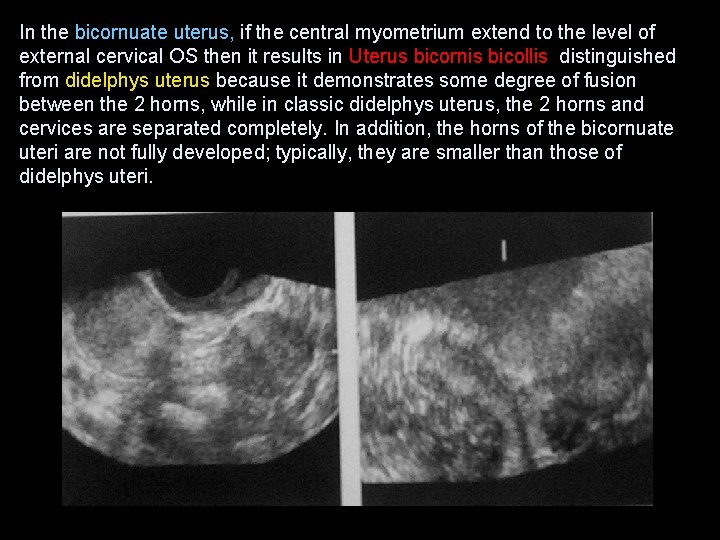
In the bicornuate uterus, if the central myometrium extend to the level of external cervical OS then it results in Uterus bicornis bicollis distinguished from didelphys uterus because it demonstrates some degree of fusion between the 2 horns, while in classic didelphys uterus, the 2 horns and cervices are separated completely. In addition, the horns of the bicornuate uteri are not fully developed; typically, they are smaller than those of didelphys uteri.
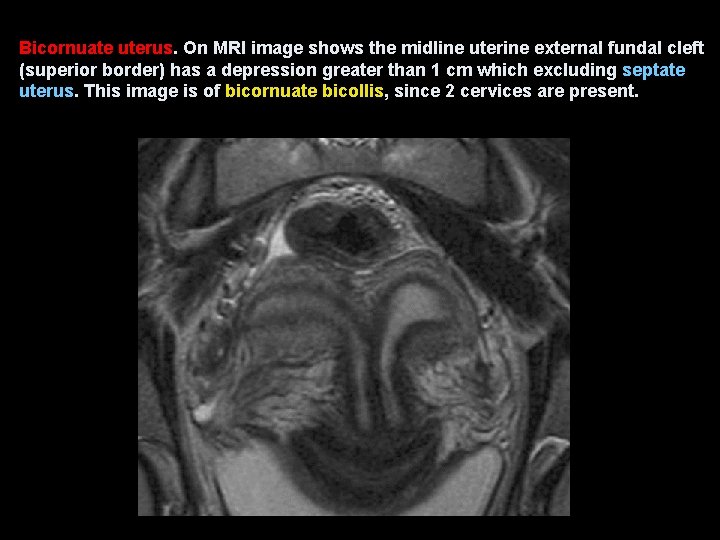
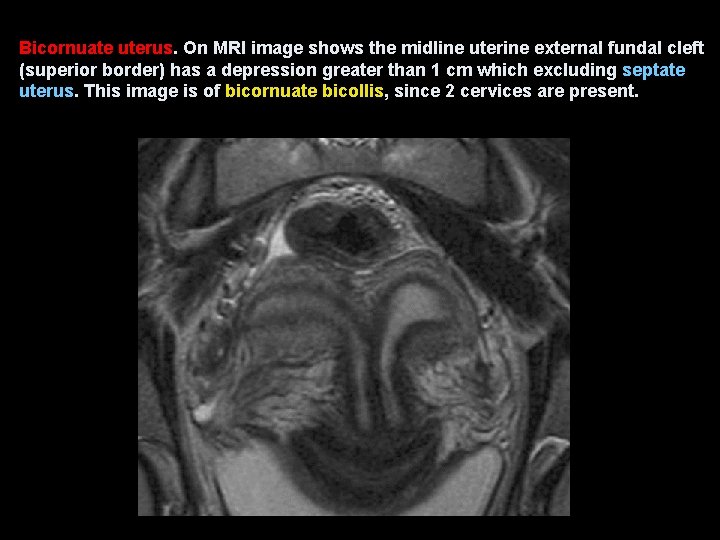
Bicornuate uterus. On MRI image shows the midline uterine external fundal cleft (superior border) has a depression greater than 1 cm which excluding septate uterus. This image is of bicornuate bicollis, since 2 cervices are present.
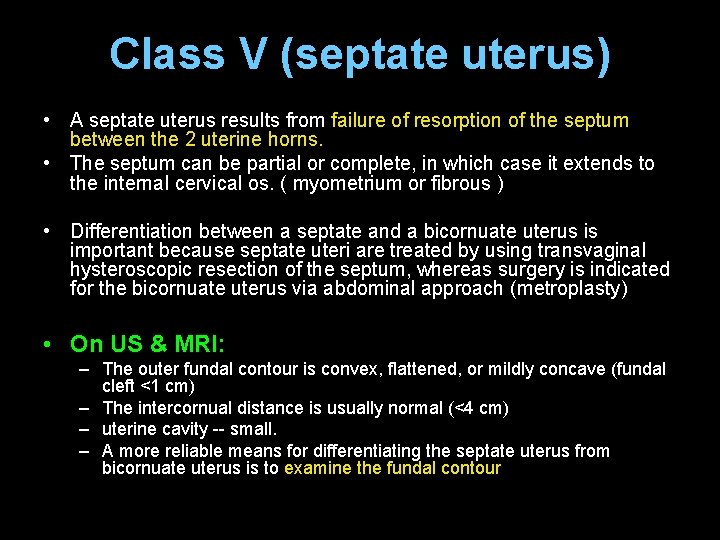
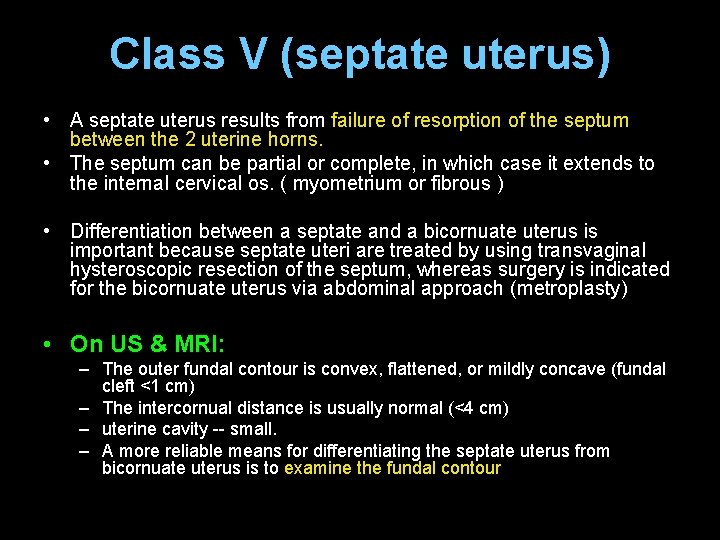
Class V (septate uterus) • A septate uterus results from failure of resorption of the septum between the 2 uterine horns. • The septum can be partial or complete, in which case it extends to the internal cervical os. ( myometrium or fibrous ) • Differentiation between a septate and a bicornuate uterus is important because septate uteri are treated by using transvaginal hysteroscopic resection of the septum, whereas surgery is indicated for the bicornuate uterus via abdominal approach (metroplasty) • On US & MRI: – The outer fundal contour is convex, flattened, or mildly concave (fundal cleft <1 cm) – The intercornual distance is usually normal (<4 cm) – uterine cavity -- small. – A more reliable means for differentiating the septate uterus from bicornuate uterus is to examine the fundal contour
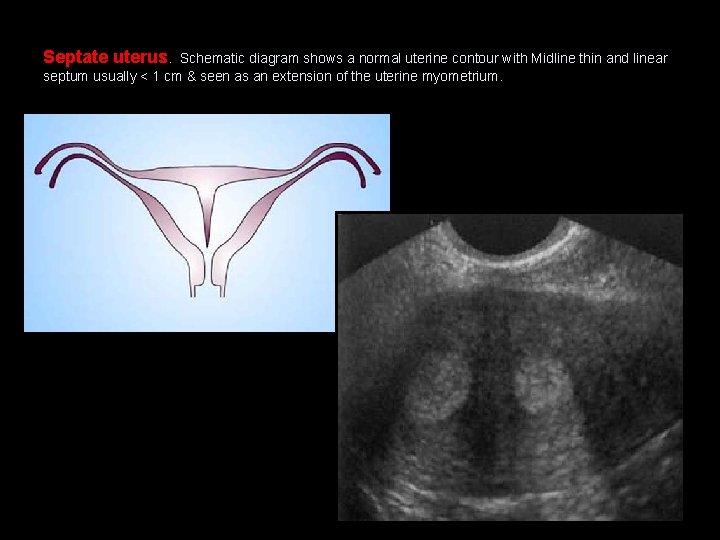
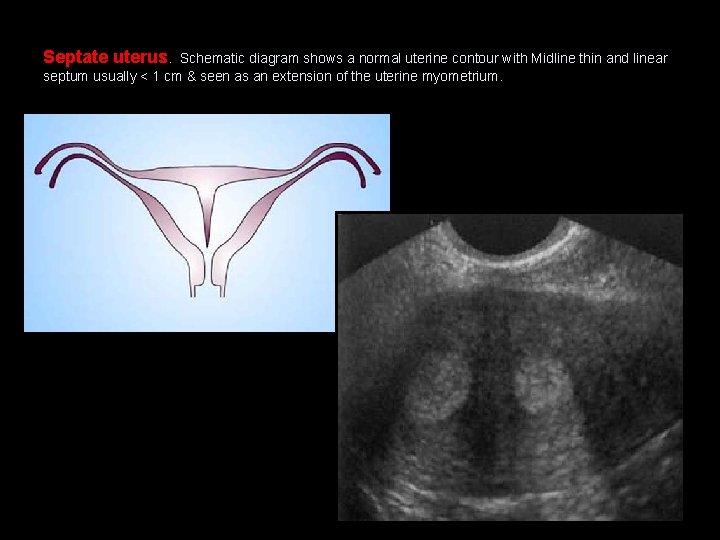
Septate uterus. Schematic diagram shows a normal uterine contour with Midline thin and linear septum usually < 1 cm & seen as an extension of the uterine myometrium.
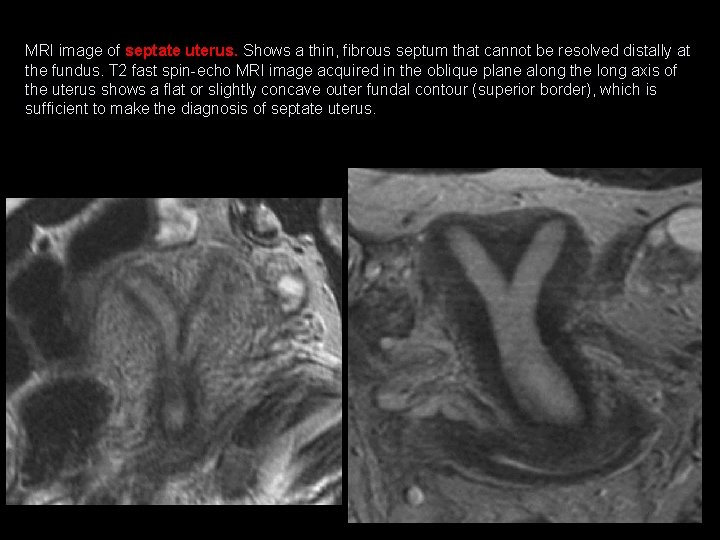
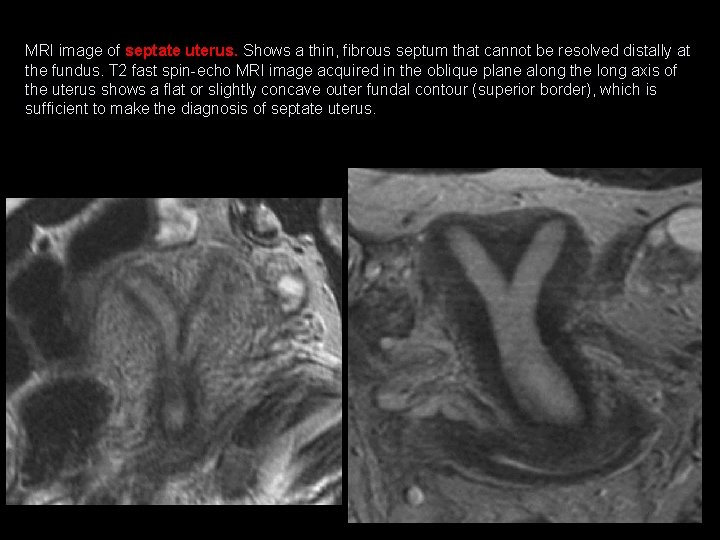
MRI image of septate uterus. Shows a thin, fibrous septum that cannot be resolved distally at the fundus. T 2 fast spin-echo MRI image acquired in the oblique plane along the long axis of the uterus shows a flat or slightly concave outer fundal contour (superior border), which is sufficient to make the diagnosis of septate uterus.
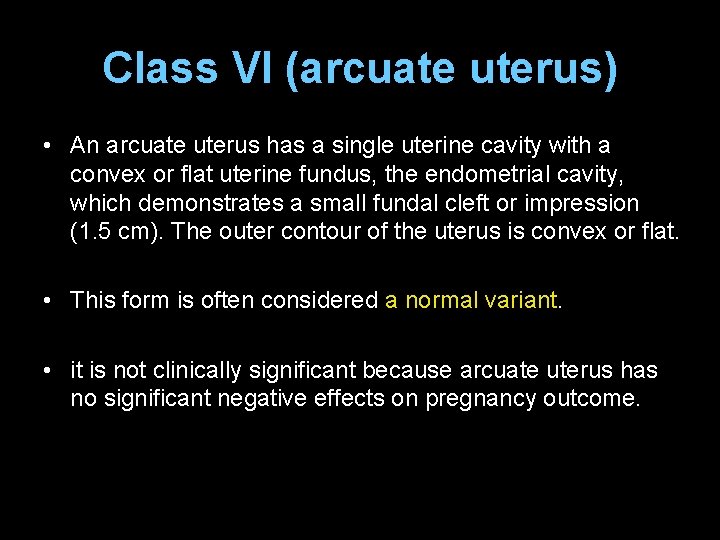
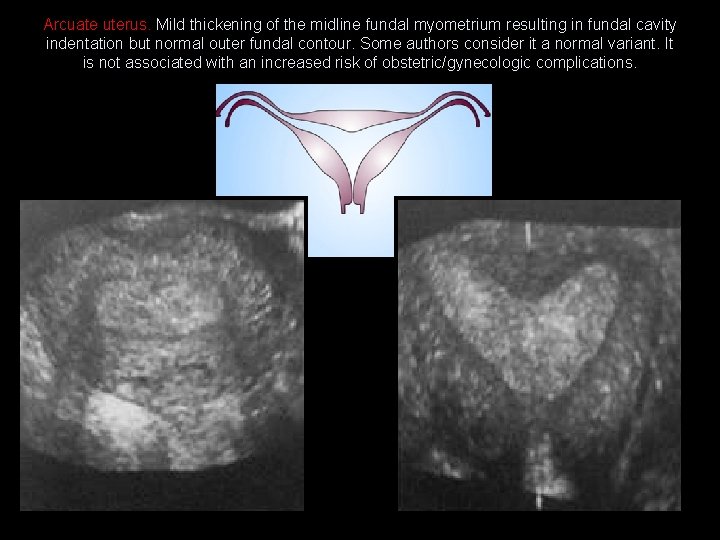
Class VI (arcuate uterus) • An arcuate uterus has a single uterine cavity with a convex or flat uterine fundus, the endometrial cavity, which demonstrates a small fundal cleft or impression (1. 5 cm). The outer contour of the uterus is convex or flat. • This form is often considered a normal variant. • it is not clinically significant because arcuate uterus has no significant negative effects on pregnancy outcome.
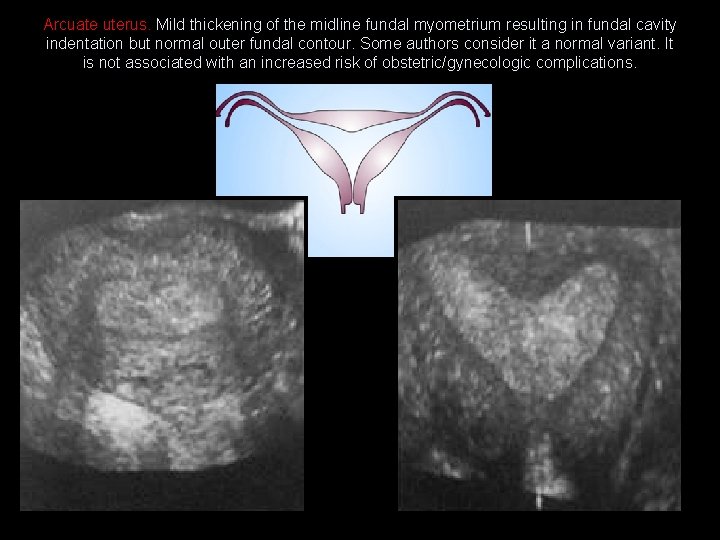
Arcuate uterus. Mild thickening of the midline fundal myometrium resulting in fundal cavity indentation but normal outer fundal contour. Some authors consider it a normal variant. It is not associated with an increased risk of obstetric/gynecologic complications.
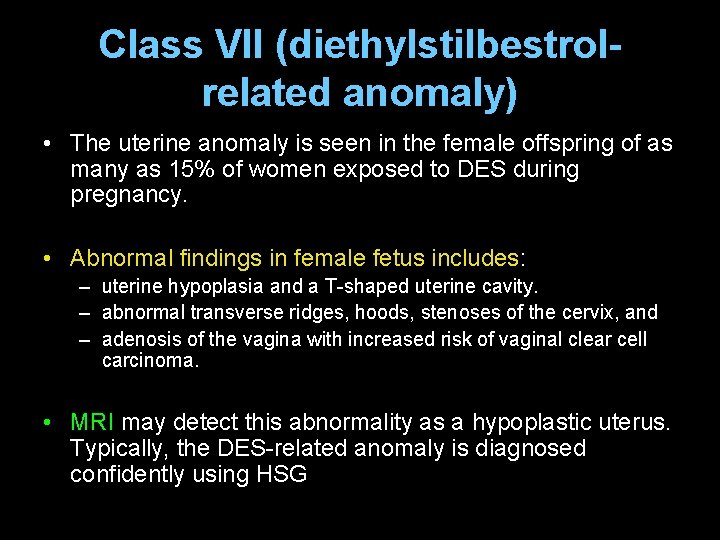
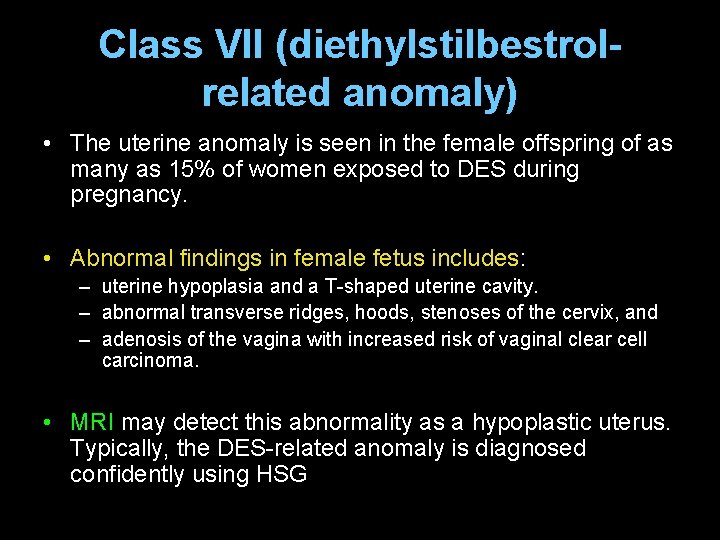
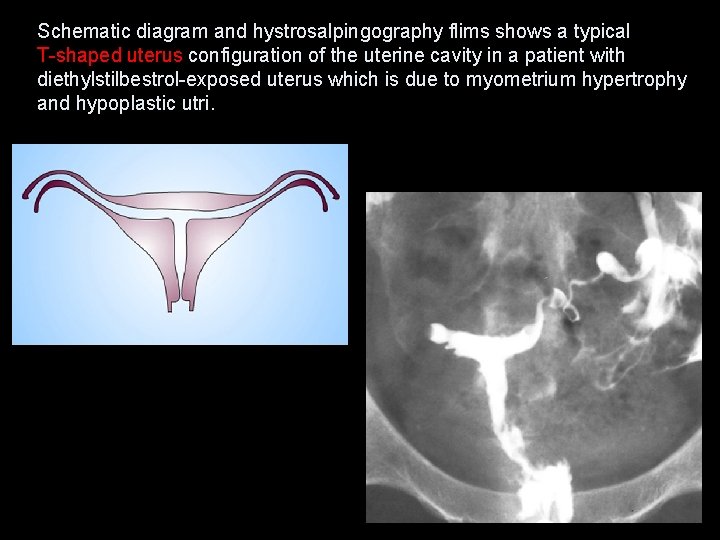
Class VII (diethylstilbestrolrelated anomaly) • The uterine anomaly is seen in the female offspring of as many as 15% of women exposed to DES during pregnancy. • Abnormal findings in female fetus includes: – uterine hypoplasia and a T-shaped uterine cavity. – abnormal transverse ridges, hoods, stenoses of the cervix, and – adenosis of the vagina with increased risk of vaginal clear cell carcinoma. • MRI may detect this abnormality as a hypoplastic uterus. Typically, the DES-related anomaly is diagnosed confidently using HSG
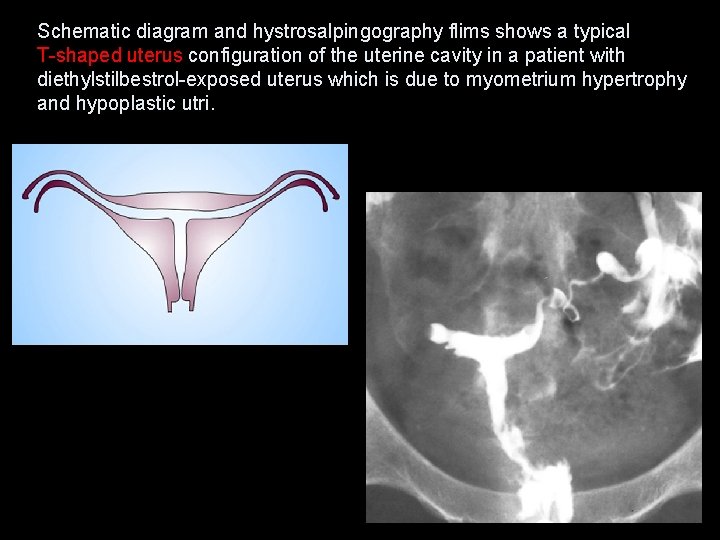
Schematic diagram and hystrosalpingography flims shows a typical T-shaped uterus configuration of the uterine cavity in a patient with diethylstilbestrol-exposed uterus which is due to myometrium hypertrophy and hypoplastic utri.
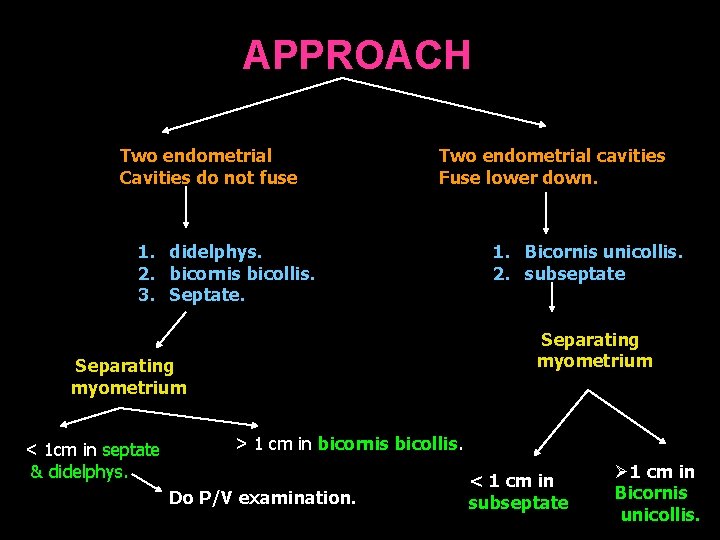
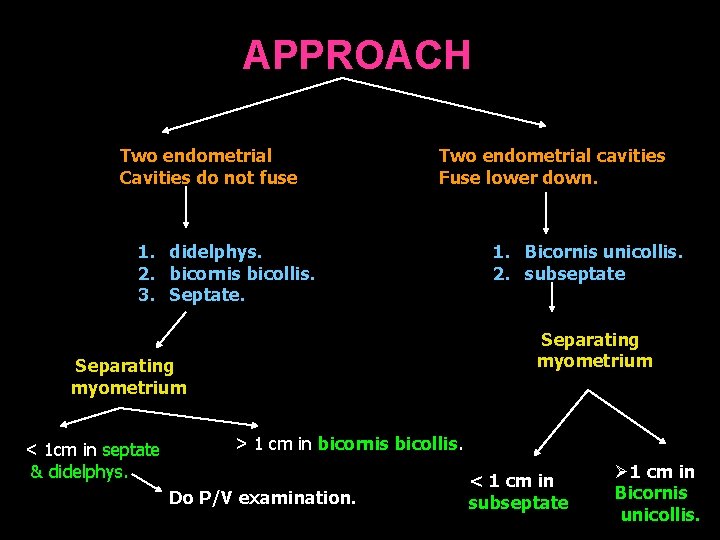
APPROACH Two endometrial Cavities do not fuse Two endometrial cavities Fuse lower down. 1. didelphys. 2. bicornis bicollis. 3. Septate. Separating myometrium < 1 cm in septate & didelphys. 1. Bicornis unicollis. 2. subseptate > 1 cm in bicornis bicollis. Do P/V examination. < 1 cm in subseptate Ø 1 cm in Bicornis unicollis.
CASE 3
• A 5 yr old girl presented with a h/o lethargy & cough since 4 mth. • On examination pt was anaemic and PEM gr 3. • Has a raised ESR.

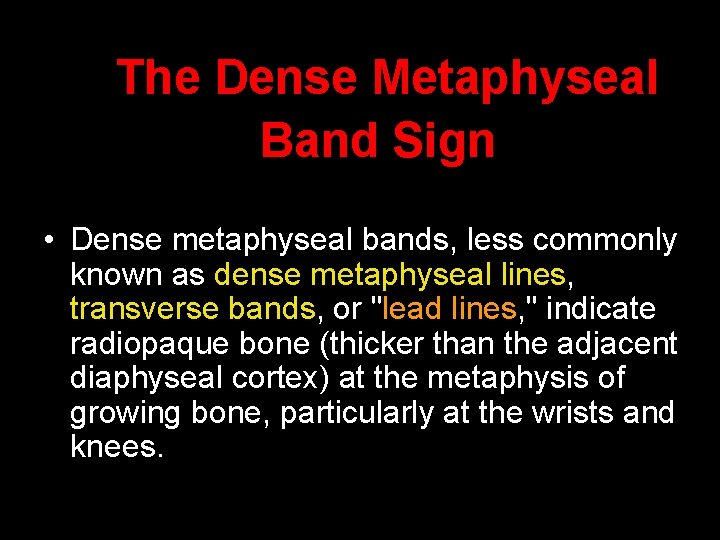
The Dense Metaphyseal Band Sign • Dense metaphyseal bands, less commonly known as dense metaphyseal lines, transverse bands, or "lead lines, " indicate radiopaque bone (thicker than the adjacent diaphyseal cortex) at the metaphysis of growing bone, particularly at the wrists and knees.

Anteroposterior radiograph of the wrist obtained in a 2 -year-old boy reveals a dense metaphyseal band (arrow) in the distal radius, without flaring or cupping. The distal ulna is unremarkable. By excluding more serious causes, this finding was proved to be a normal variant.
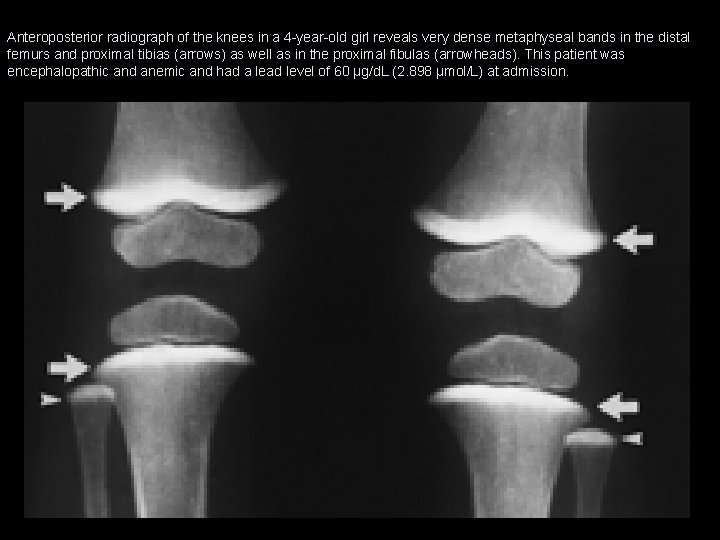
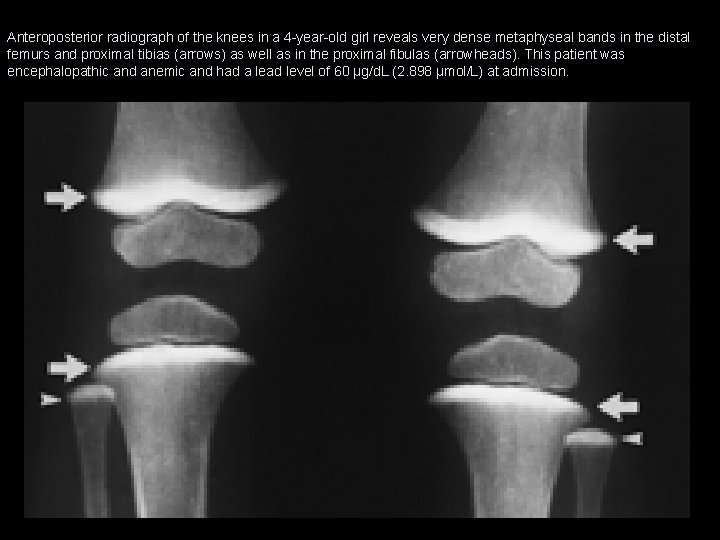
Anteroposterior radiograph of the knees in a 4 -year-old girl reveals very dense metaphyseal bands in the distal femurs and proximal tibias (arrows) as well as in the proximal fibulas (arrowheads). This patient was encephalopathic and anemic and had a lead level of 60 µg/d. L (2. 898 µmol/L) at admission.
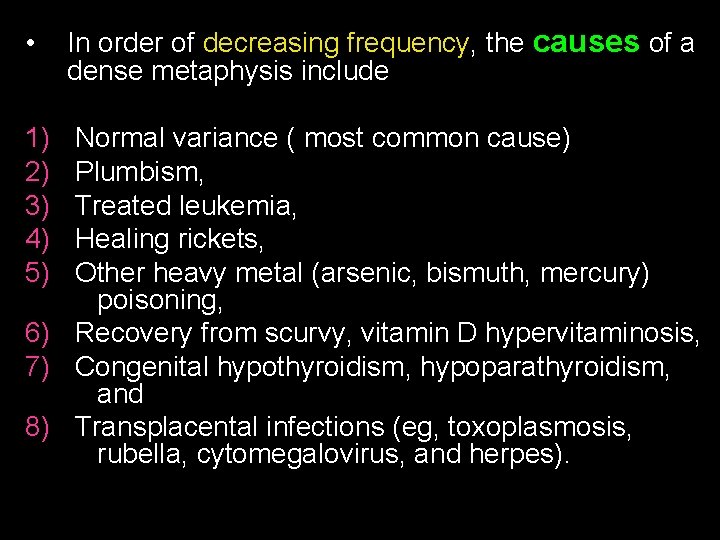
• 1) 2) 3) 4) 5) In order of decreasing frequency, the causes of a dense metaphysis include Normal variance ( most common cause) Plumbism, Treated leukemia, Healing rickets, Other heavy metal (arsenic, bismuth, mercury) poisoning, 6) Recovery from scurvy, vitamin D hypervitaminosis, 7) Congenital hypothyroidism, hypoparathyroidism, and 8) Transplacental infections (eg, toxoplasmosis, rubella, cytomegalovirus, and herpes).
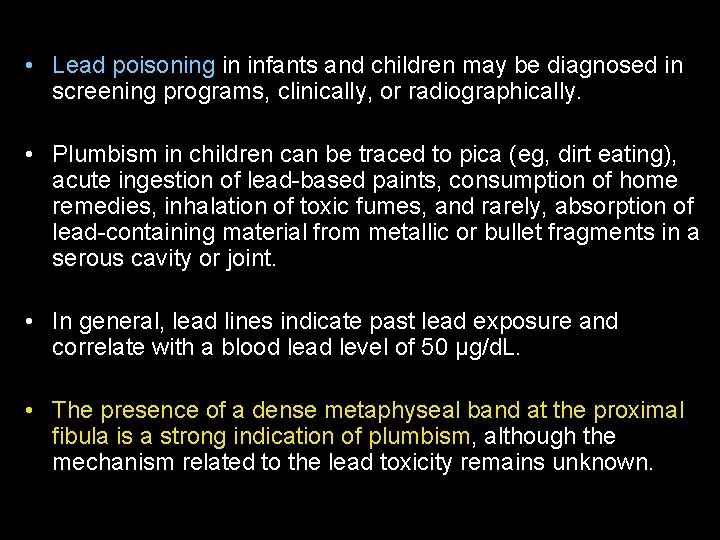
• Lead poisoning in infants and children may be diagnosed in screening programs, clinically, or radiographically. • Plumbism in children can be traced to pica (eg, dirt eating), acute ingestion of lead-based paints, consumption of home remedies, inhalation of toxic fumes, and rarely, absorption of lead-containing material from metallic or bullet fragments in a serous cavity or joint. • In general, lead lines indicate past lead exposure and correlate with a blood lead level of 50 µg/d. L. • The presence of a dense metaphyseal band at the proximal fibula is a strong indication of plumbism, although the mechanism related to the lead toxicity remains unknown.
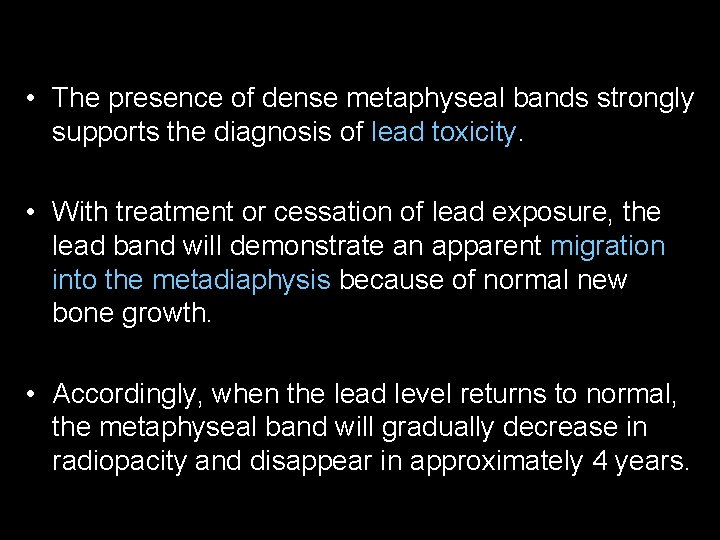
• The presence of dense metaphyseal bands strongly supports the diagnosis of lead toxicity. • With treatment or cessation of lead exposure, the lead band will demonstrate an apparent migration into the metadiaphysis because of normal new bone growth. • Accordingly, when the lead level returns to normal, the metaphyseal band will gradually decrease in radiopacity and disappear in approximately 4 years.
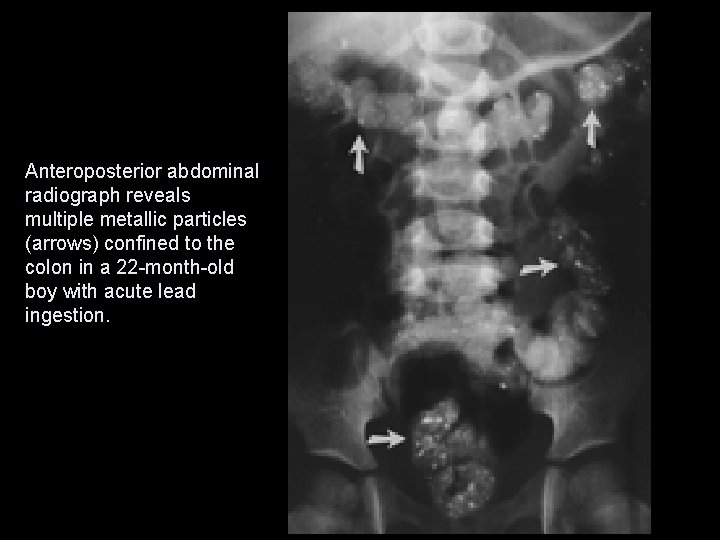
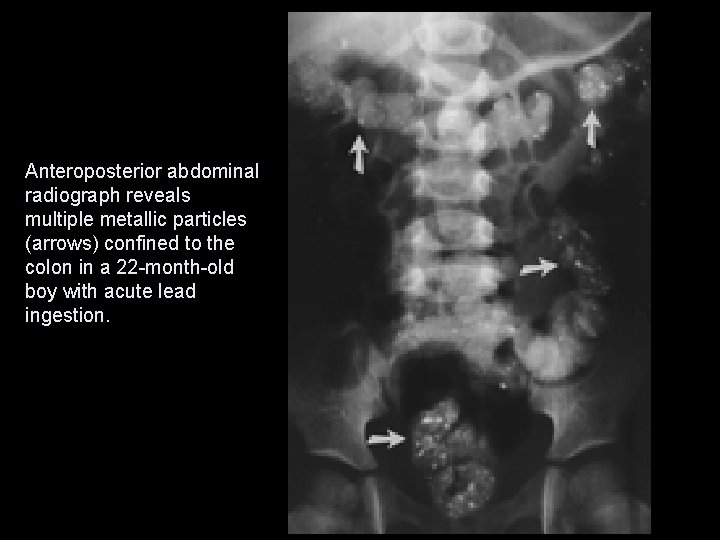
Anteroposterior abdominal radiograph reveals multiple metallic particles (arrows) confined to the colon in a 22 -month-old boy with acute lead ingestion.
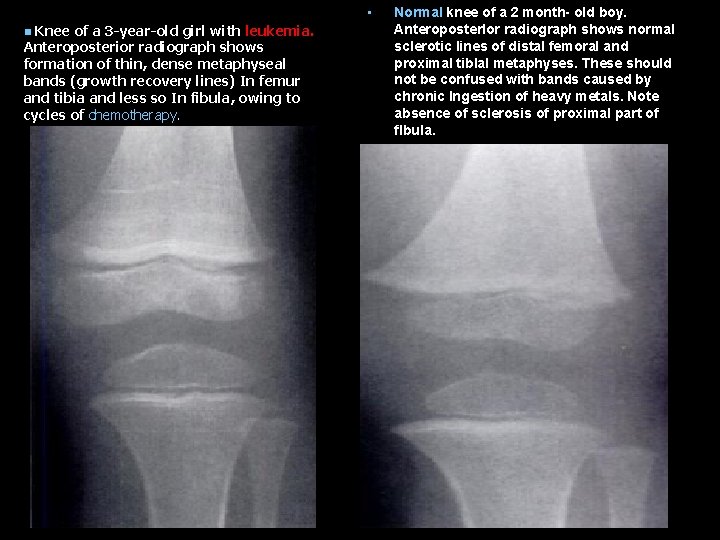
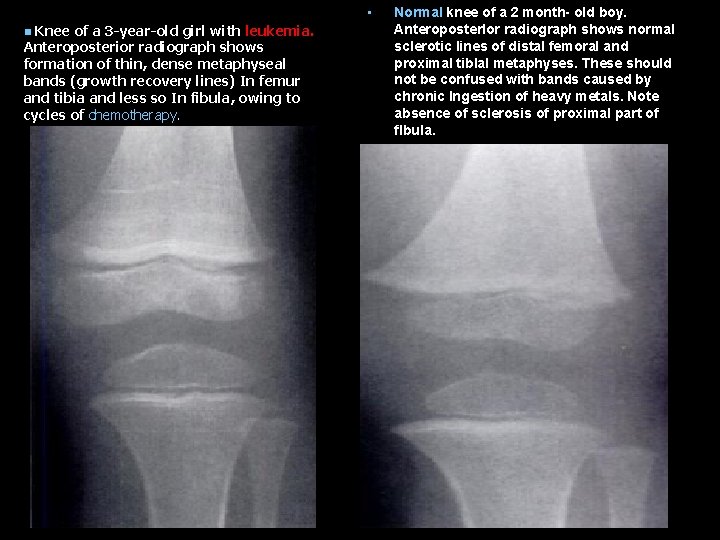
• Knee of a 3 -year-old girl with leukemia. Anteroposterior radiograph shows formation of thin, dense metaphyseal bands (growth recovery lines) In femur and tibia and less so In fibula, owing to cycles of chemotherapy. n Normal knee of a 2 month- old boy. Anteroposterlor radiograph shows normal sclerotic lines of distal femoral and proximal tiblal metaphyses. These should not be confused with bands caused by chronic Ingestion of heavy metals. Note absence of sclerosis of proximal part of flbula.
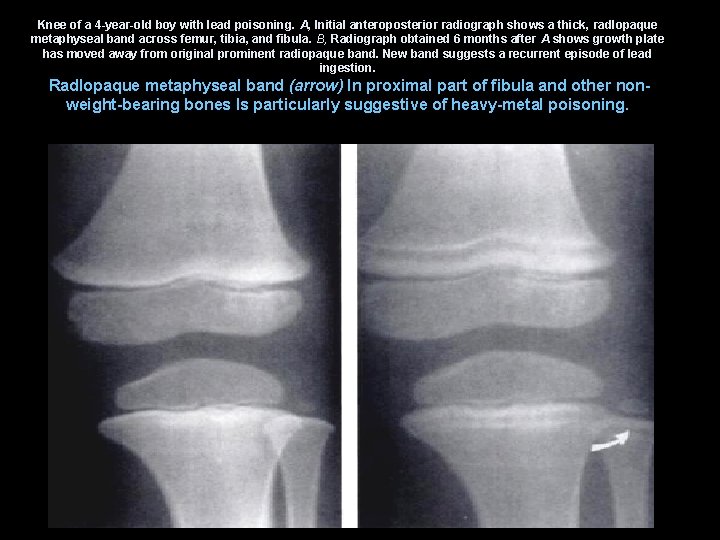
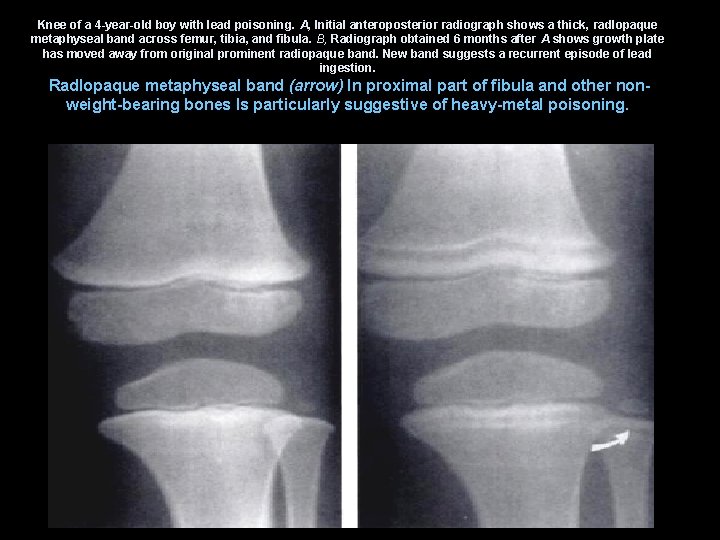
Knee of a 4 -year-old boy with lead poisoning. A, Initial anteroposterior radiograph shows a thick, radlopaque metaphyseal band across femur, tibia, and fibula. B, Radiograph obtained 6 months after A shows growth plate has moved away from original prominent radiopaque band. New band suggests a recurrent episode of lead ingestion. Radlopaque metaphyseal band (arrow) In proximal part of fibula and other nonweight-bearing bones Is particularly suggestive of heavy-metal poisoning.
CASE 4
• A 22 year female presented with abdominal pain, nausea, vomiting. • Clinical examination reveals epigastric mass and tenderness. • Female was knows to have psychological disturbances.
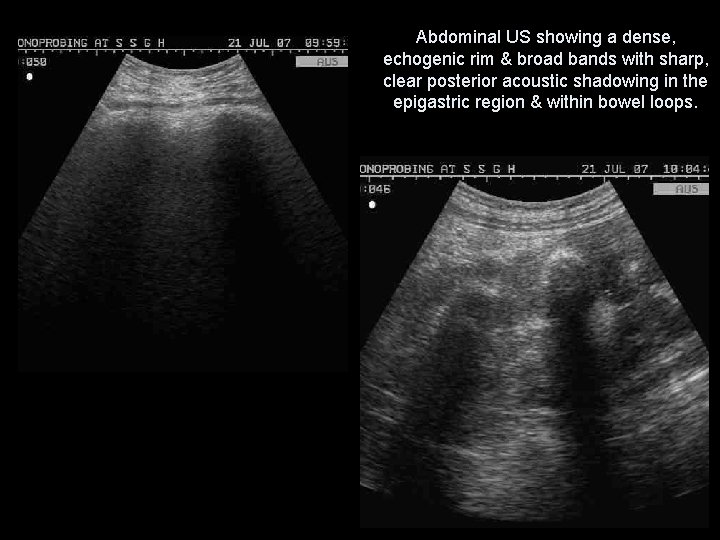
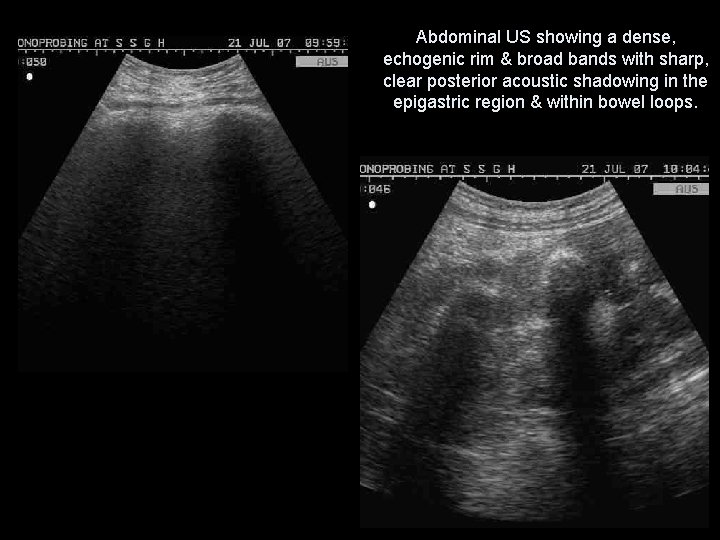
Abdominal US showing a dense, echogenic rim & broad bands with sharp, clear posterior acoustic shadowing in the epigastric region & within bowel loops.

• US, demonstrates a superficially located broad band of high amplitude echoes along the anterior wall of the mass with sharp, clean posterior acoustic shadowing. • This characteristic appearance persists irrespective of the angulation of the transducer, alteration of position of the patient and the administration of clear water. • This can be attributed to multiple tiny interfaces between the smooth, compressed, compact mass and the entrapped air and food debris.
• This specific US appearance excludes the clinical possibility of a pancreatic pseudocyst, splenic or renal mass, non-calcified gastric tumor, gastric duplication cyst and gastric outlet obstruction. • However a heavily calcified mass such as teratoma, neuroblastoma or impacted mass of feces may produce a similar US image. • The sharp, clean margins of the acoustic shadow rule out the possibility of gas and which produce "dirty" shadowing.
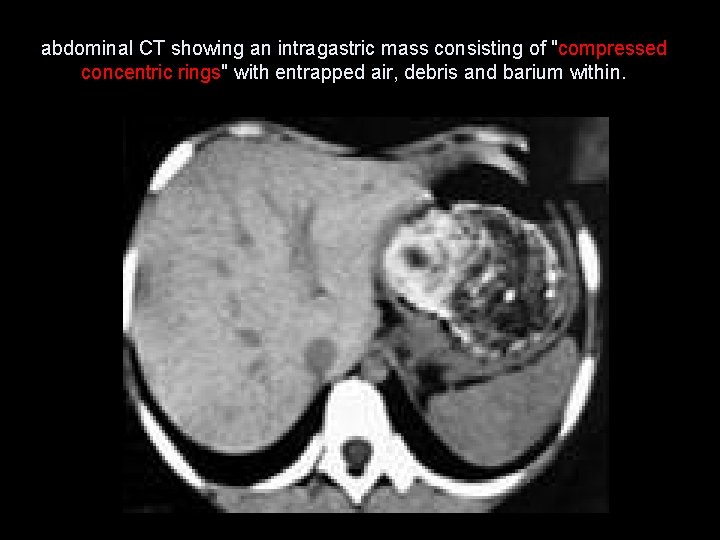
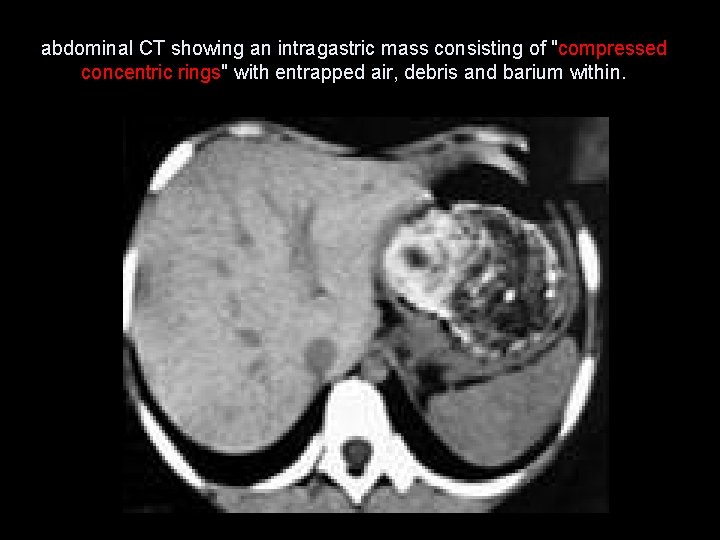
abdominal CT showing an intragastric mass consisting of "compressed concentric rings" with entrapped air, debris and barium within.
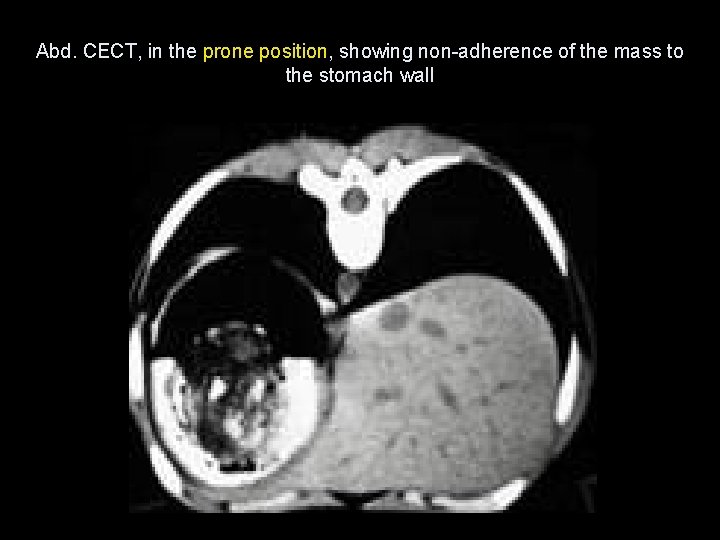
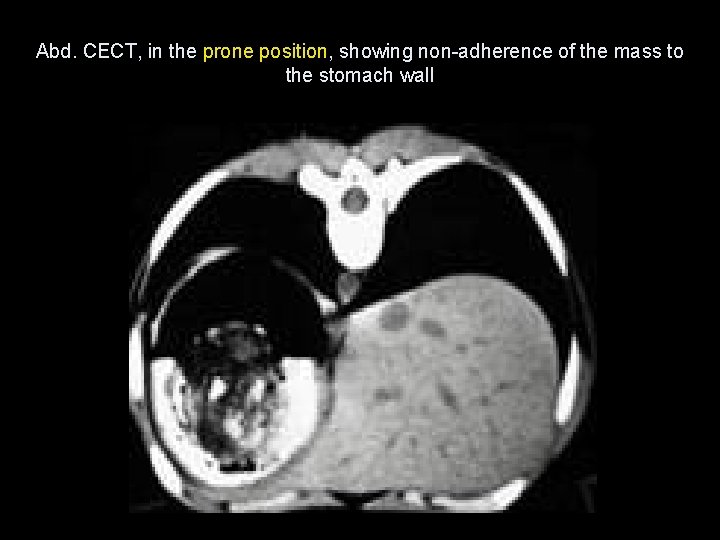
Abd. CECT, in the prone position, showing non-adherence of the mass to the stomach wall
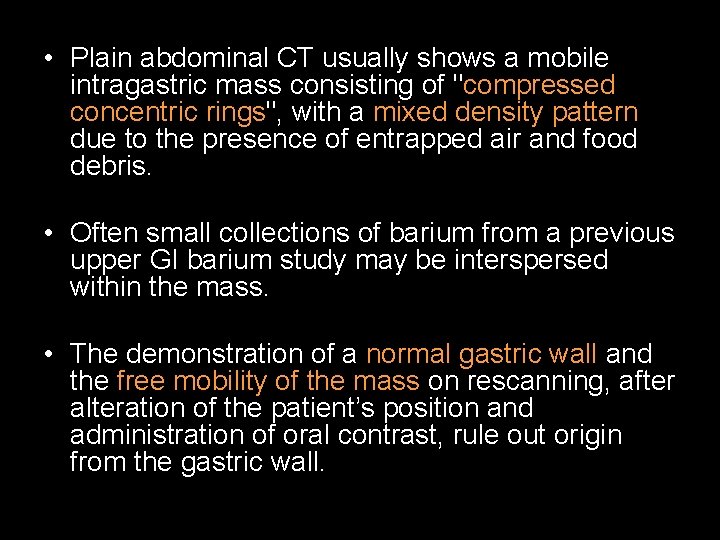
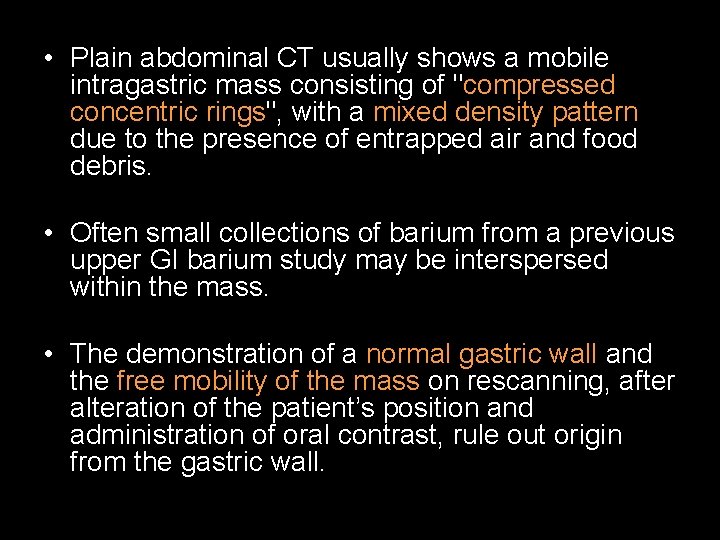
• Plain abdominal CT usually shows a mobile intragastric mass consisting of "compressed concentric rings", with a mixed density pattern due to the presence of entrapped air and food debris. • Often small collections of barium from a previous upper GI barium study may be interspersed within the mass. • The demonstration of a normal gastric wall and the free mobility of the mass on rescanning, after alteration of the patient’s position and administration of oral contrast, rule out origin from the gastric wall.

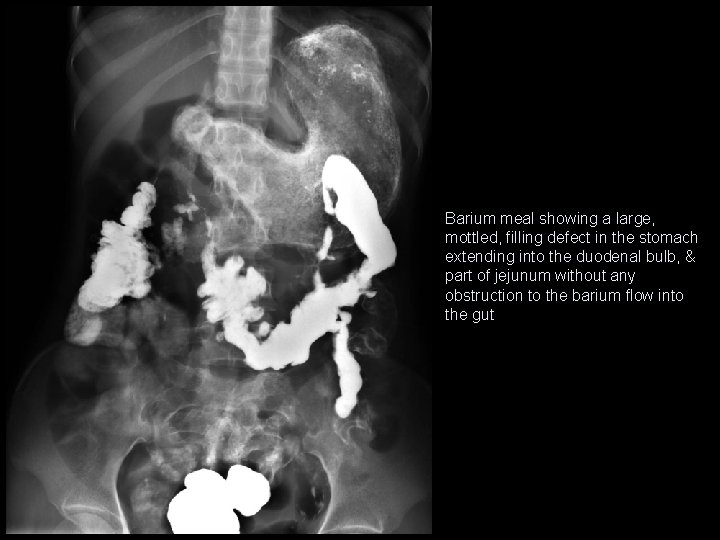
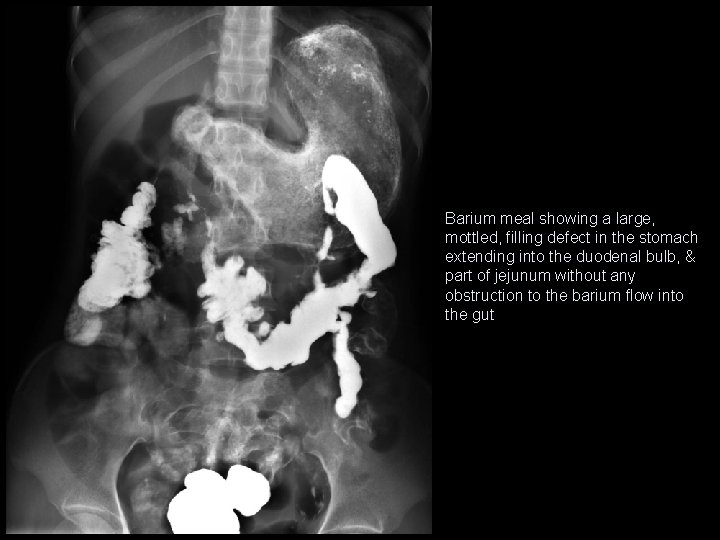
Barium meal showing a large, mottled, filling defect in the stomach extending into the duodenal bulb, & part of jejunum without any obstruction to the barium flow into the gut
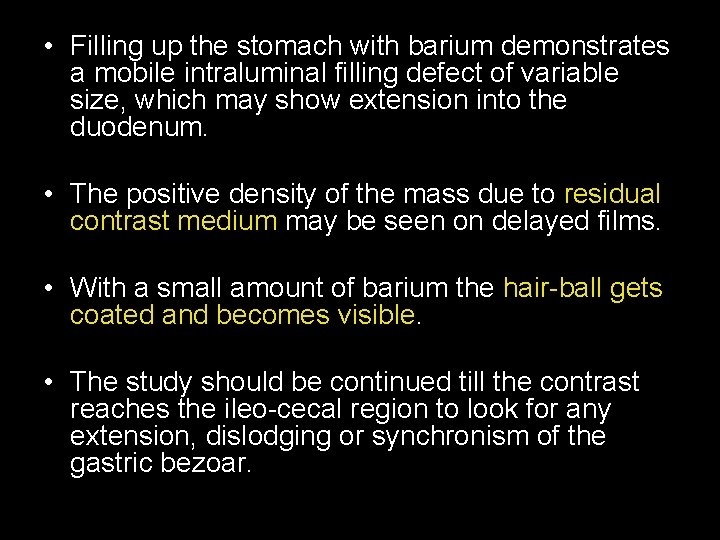
• Filling up the stomach with barium demonstrates a mobile intraluminal filling defect of variable size, which may show extension into the duodenum. • The positive density of the mass due to residual contrast medium may be seen on delayed films. • With a small amount of barium the hair-ball gets coated and becomes visible. • The study should be continued till the contrast reaches the ileo-cecal region to look for any extension, dislodging or synchronism of the gastric bezoar.
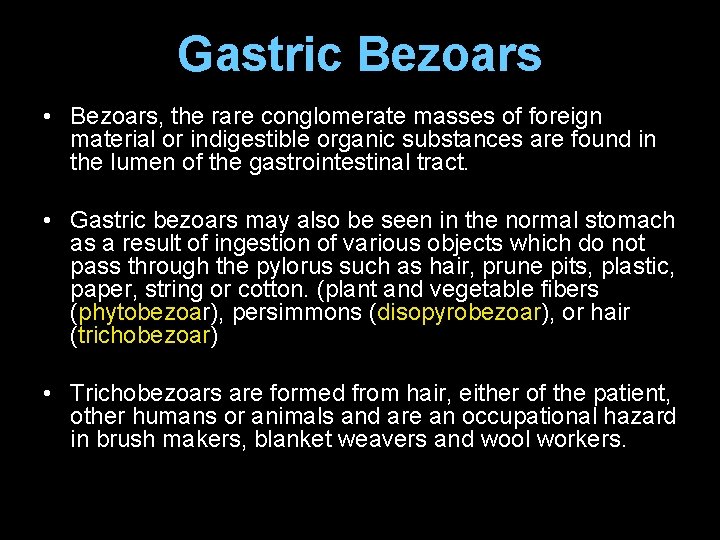
Gastric Bezoars • Bezoars, the rare conglomerate masses of foreign material or indigestible organic substances are found in the lumen of the gastrointestinal tract. • Gastric bezoars may also be seen in the normal stomach as a result of ingestion of various objects which do not pass through the pylorus such as hair, prune pits, plastic, paper, string or cotton. (plant and vegetable fibers (phytobezoar), persimmons (disopyrobezoar), or hair (trichobezoar) • Trichobezoars are formed from hair, either of the patient, other humans or animals and are an occupational hazard in brush makers, blanket weavers and wool workers.
Clinical Presentation • 80% of bezoars occur before the age of 30 years and more than 90% occur in women. • Trichobezoars are comparatively rare in children, whereas lactobezoars have become more common in infants. • An underlying psychological disturbance is common and a history of trichophagy or trichotillomania can occasionally be elicited. • Gastric bezoars may cause dyspepsia, nausea and vomiting (64%), colicky abdominal pain (70%), alteration of bowel habits (32%), and anorexia, weakness and weight loss.
• An erect abdominal radiograph and a supine radiograph may also show a prominent gastric outline with an intragastric mottled mass, outlined by gas in the distended stomach, mimicking a food-filled stomach. • The majority of the gastric bezoars are preoperatively diagnosed or confirmed on upper GI barium study. • Herein, patient underwent surgery, the mass was found to be a large collections of hair tufts with undigested food particles.

Thank you….
CASE 2
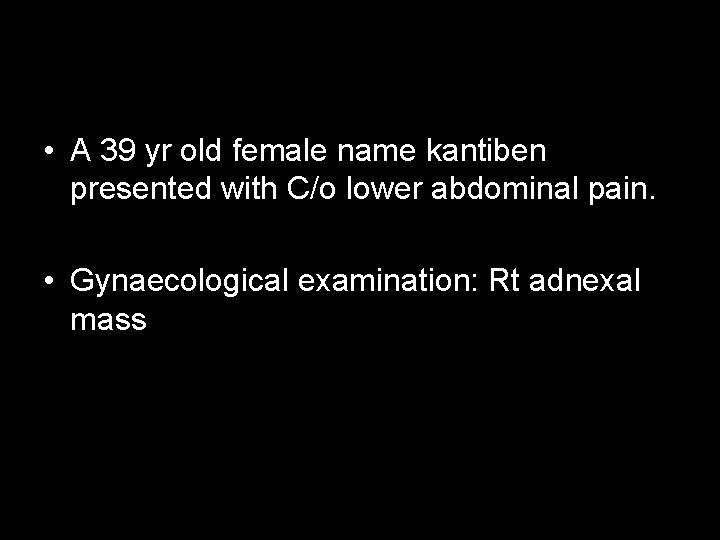
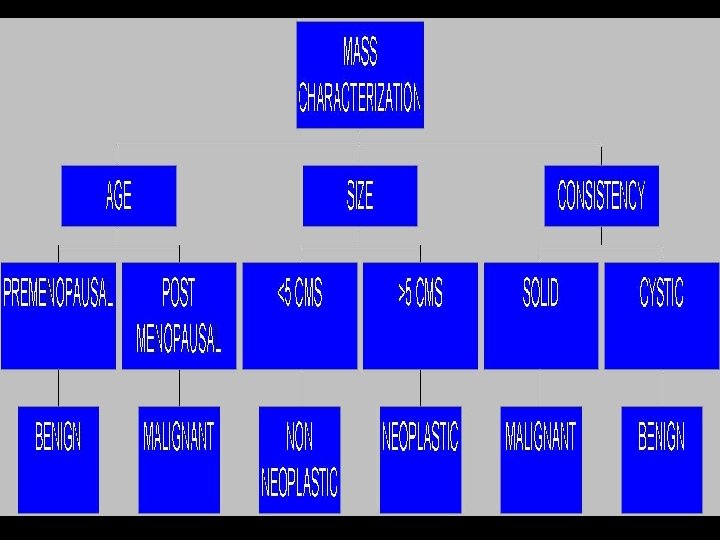
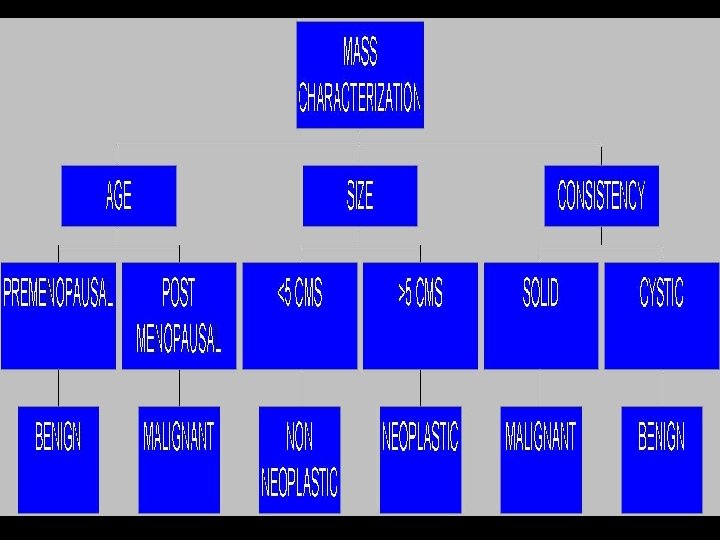
• A 39 yr old female name kantiben presented with C/o lower abdominal pain. • Gynaecological examination: Rt adnexal mass
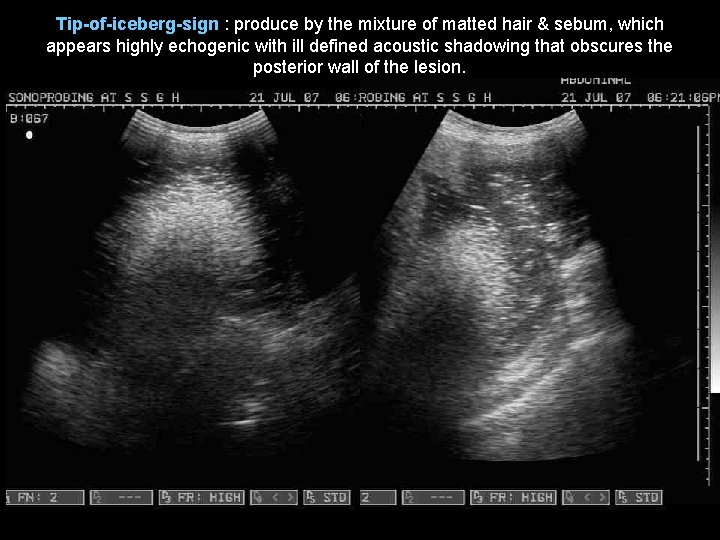
Tip-of-iceberg-sign : produce by the mixture of matted hair & sebum, which appears highly echogenic with ill defined acoustic shadowing that obscures the posterior wall of the lesion.
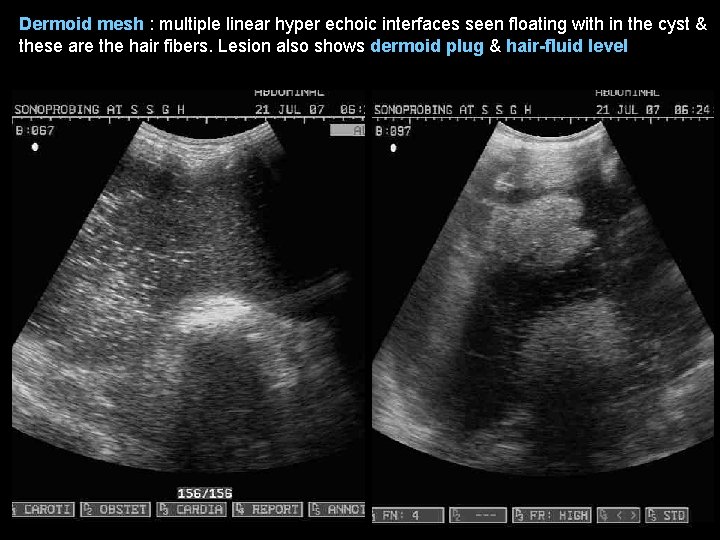
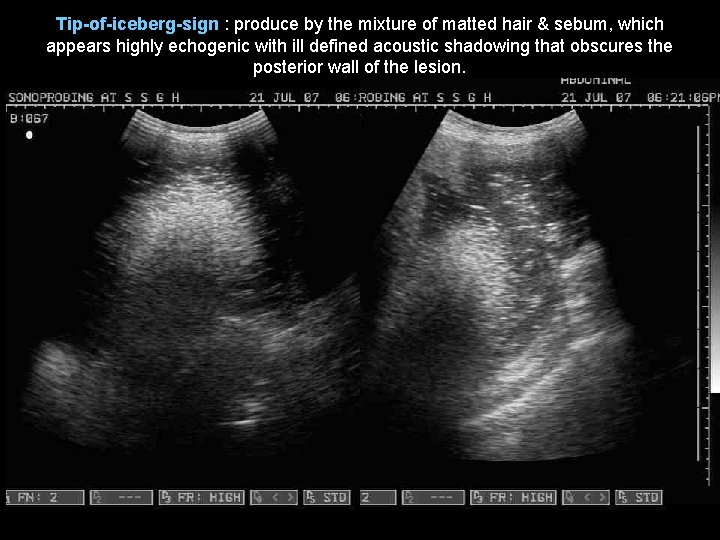
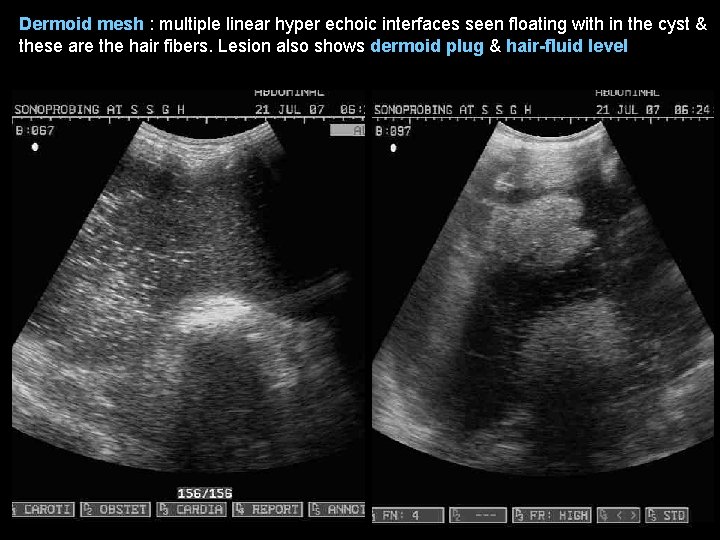
Dermoid mesh : multiple linear hyper echoic interfaces seen floating with in the cyst & these are the hair fibers. Lesion also shows dermoid plug & hair-fluid level
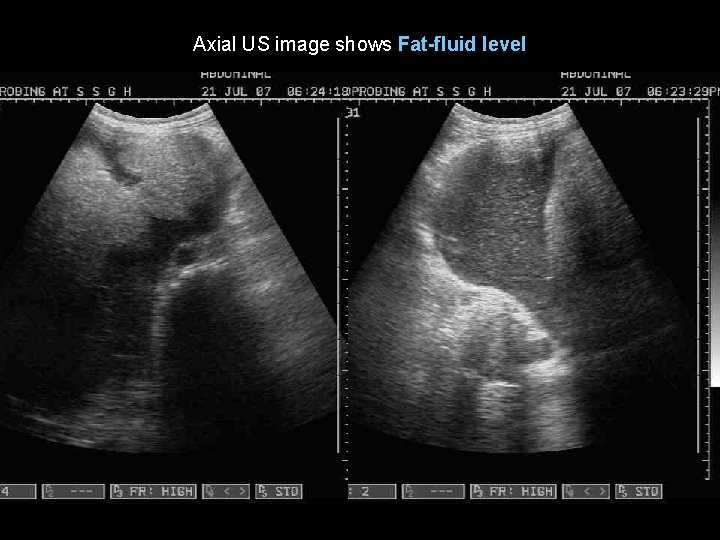
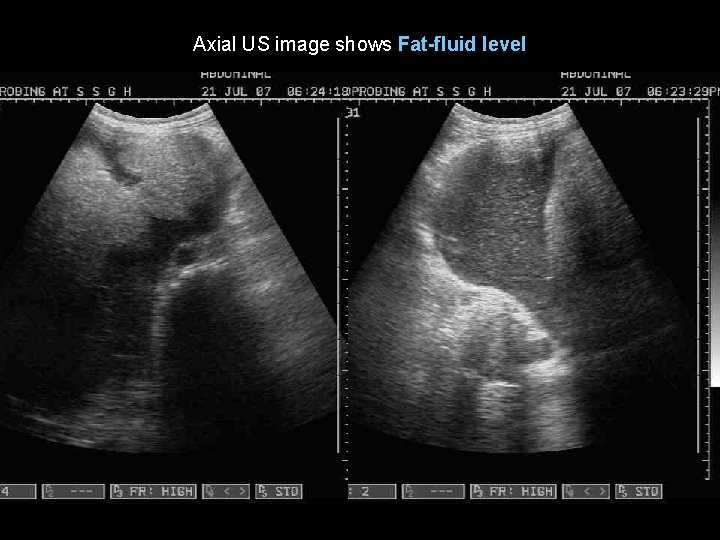
Axial US image shows Fat-fluid level
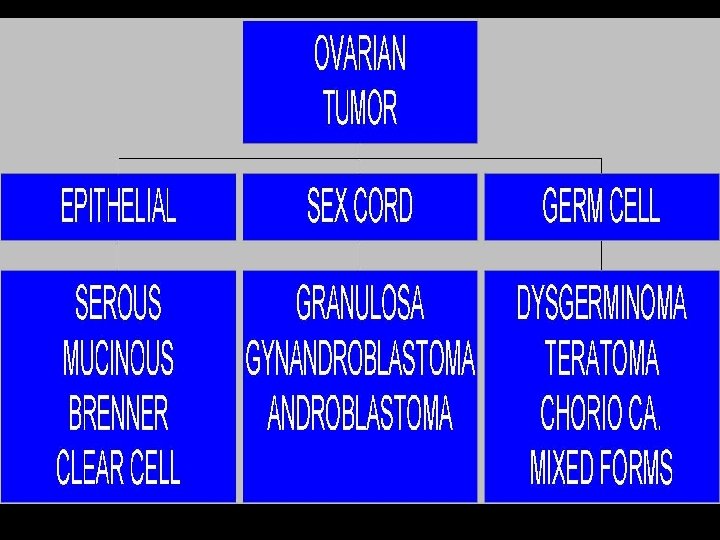
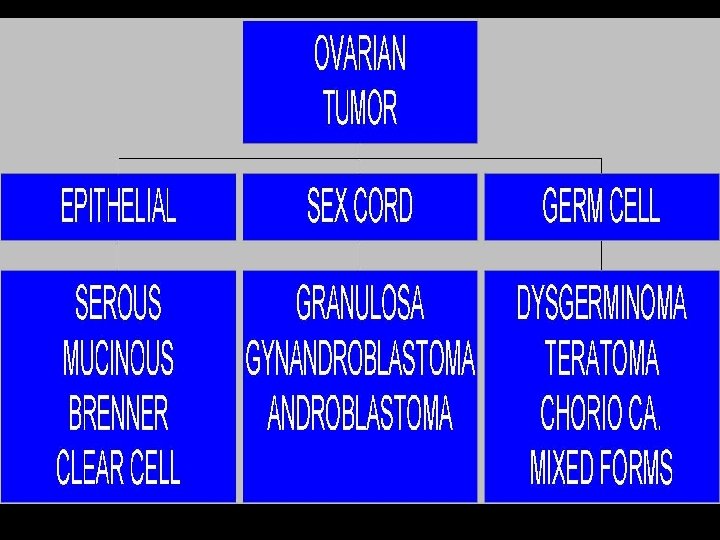
Discussion • Dermoid cyst, also referred as benign/mature cystic teratoma, arises from germ cells of the ovary and it is composed of a combination of well-differentiated ectodetermal, mesodermal and endodermal elements. • Dermoid cyst is the most common type of germ cell tumor. • It represents 25% of all ovarian tumors. The majority occur during the reproductive years. Malignant degeneration is seen in 1 -2%.
On USG • completely anechoic to hyperechoic appearance large cystic lesion. • highly echogenic dermoid plug (Rokitansky nodule), which is the solid element within the cyst that contains hair follicles, sebaceous glands, fat, and calcified elements. • Mixture of hair & sebum is highly echogenic and produces ill-defined acoustic shadowing which obscures the post wall of the lesion, k/a “ tip of the iceberg sign”. • Multiple linear hyperechoic interface seen floating within the cyst, k/a “dermoid mesh”. • Fat-fluid or hair-fluid level may be seen.
• On CT scan: – fat attenuation within a cyst, with or without calcification in the wall, is diagnostic for ovarian dermoid cysts. • On MRI: – On T 1 W : high SI ( due to sebaceous component of dermoid cysts) – On T 2 W : variable SI of the sebaceous component – Chemical-shift artifacts in the frequencyencoding direction can also be used to detect fat and distinguish it from a hemorrhage.
Differential diagnosis on ultrasound • Tubo-ovarian abscesses ( which can also contain fluid levels and echogenic pus that can produce acoustic shadowing caused by gas formation) • Benign or malignant ovarian neoplasms • Ovarian cystadenoma • Ectopic pregnancies ( also demonstrate shadowing from bone and contain echogenic hemorrhage) • • • endometriomas, pedunculated uterine fibroids hydrosalpinges, pelvic kidneys, and peritoneal cysts
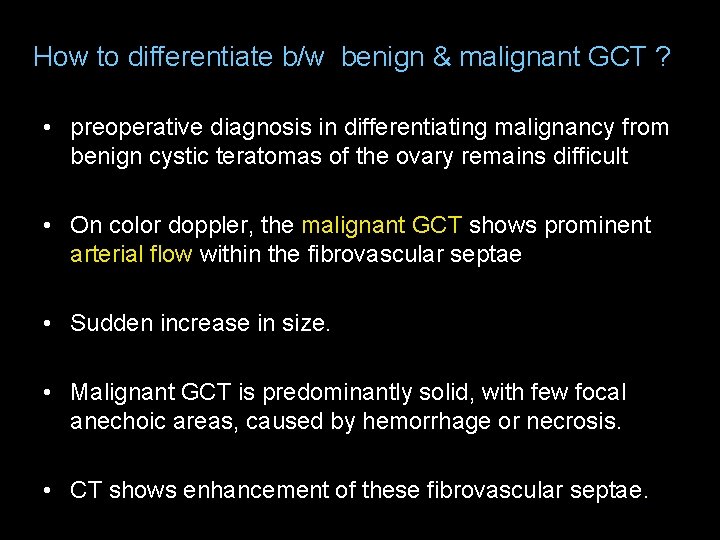
How to differentiate b/w benign & malignant GCT ? • preoperative diagnosis in differentiating malignancy from benign cystic teratomas of the ovary remains difficult • On color doppler, the malignant GCT shows prominent arterial flow within the fibrovascular septae • Sudden increase in size. • Malignant GCT is predominantly solid, with few focal anechoic areas, caused by hemorrhage or necrosis. • CT shows enhancement of these fibrovascular septae.
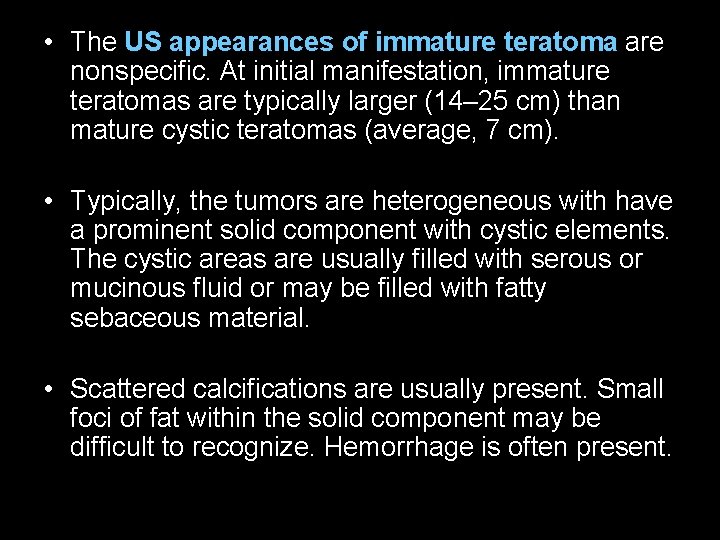
• The US appearances of immature teratoma are nonspecific. At initial manifestation, immature teratomas are typically larger (14– 25 cm) than mature cystic teratomas (average, 7 cm). • Typically, the tumors are heterogeneous with have a prominent solid component with cystic elements. The cystic areas are usually filled with serous or mucinous fluid or may be filled with fatty sebaceous material. • Scattered calcifications are usually present. Small foci of fat within the solid component may be difficult to recognize. Hemorrhage is often present.

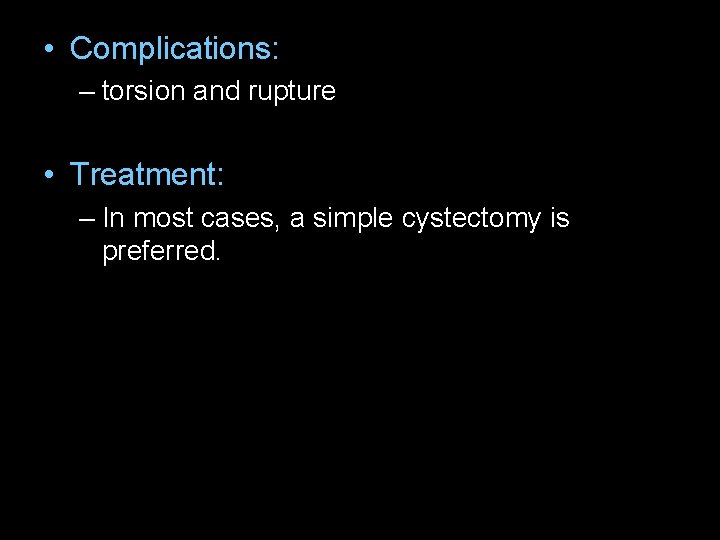
• Complications: – torsion and rupture • Treatment: – In most cases, a simple cystectomy is preferred.
Case 4
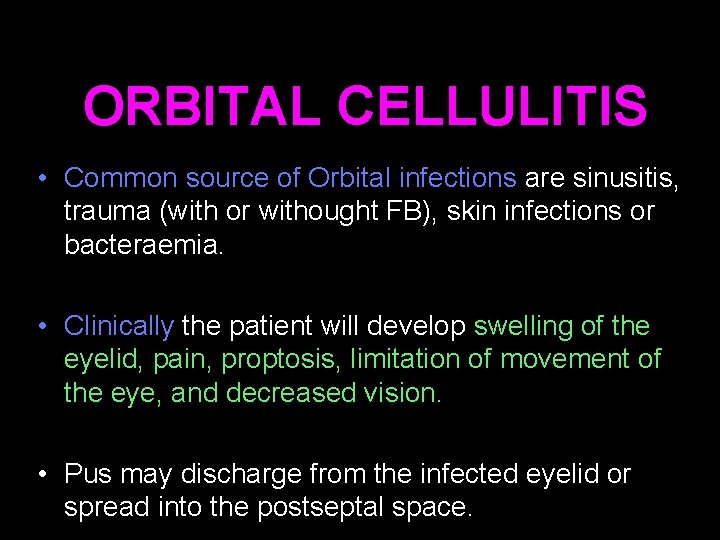
ORBITAL CELLULITIS • Common source of Orbital infections are sinusitis, trauma (with or withought FB), skin infections or bacteraemia. • Clinically the patient will develop swelling of the eyelid, pain, proptosis, limitation of movement of the eye, and decreased vision. • Pus may discharge from the infected eyelid or spread into the postseptal space.
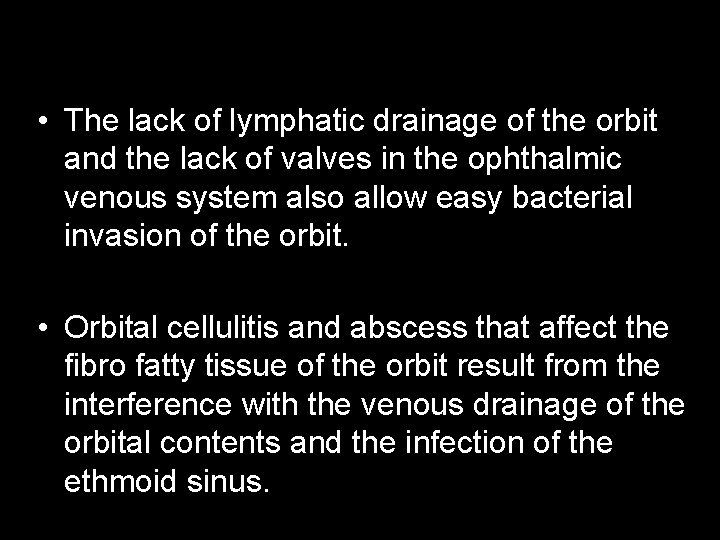
• The lack of lymphatic drainage of the orbit and the lack of valves in the ophthalmic venous system also allow easy bacterial invasion of the orbit. • Orbital cellulitis and abscess that affect the fibro fatty tissue of the orbit result from the interference with the venous drainage of the orbital contents and the infection of the ethmoid sinus.
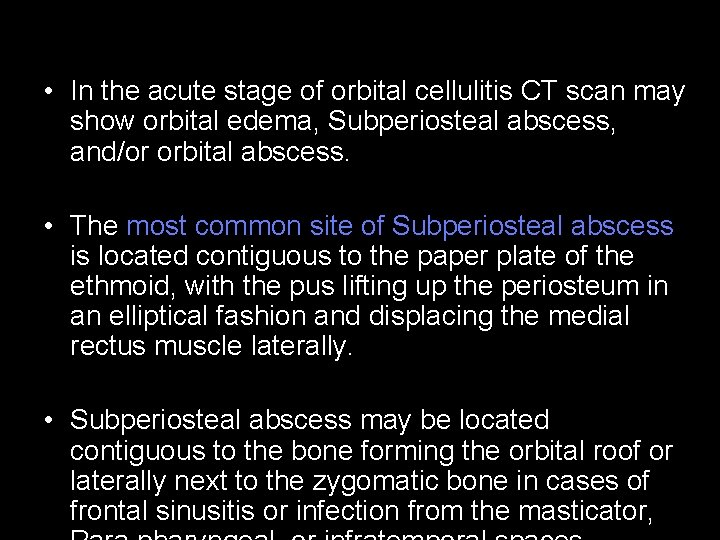
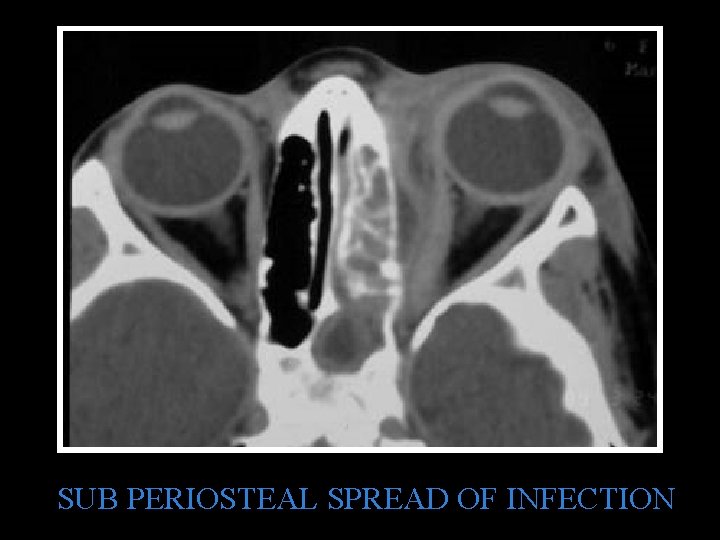
• In the acute stage of orbital cellulitis CT scan may show orbital edema, Subperiosteal abscess, and/or orbital abscess. • The most common site of Subperiosteal abscess is located contiguous to the paper plate of the ethmoid, with the pus lifting up the periosteum in an elliptical fashion and displacing the medial rectus muscle laterally. • Subperiosteal abscess may be located contiguous to the bone forming the orbital roof or laterally next to the zygomatic bone in cases of frontal sinusitis or infection from the masticator,
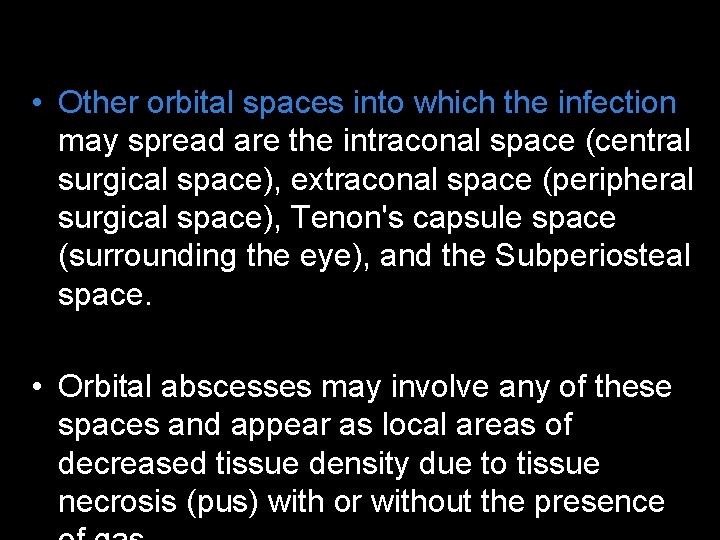
• Other orbital spaces into which the infection may spread are the intraconal space (central surgical space), extraconal space (peripheral surgical space), Tenon's capsule space (surrounding the eye), and the Subperiosteal space. • Orbital abscesses may involve any of these spaces and appear as local areas of decreased tissue density due to tissue necrosis (pus) with or without the presence
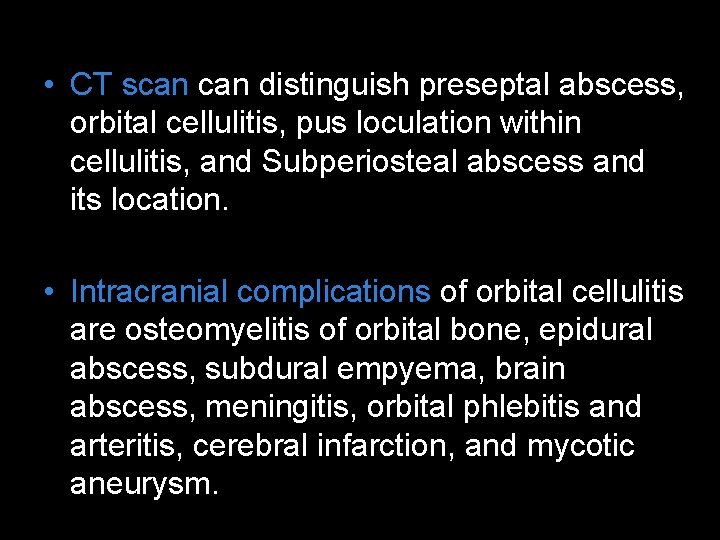
• CT scan distinguish preseptal abscess, orbital cellulitis, pus loculation within cellulitis, and Subperiosteal abscess and its location. • Intracranial complications of orbital cellulitis are osteomyelitis of orbital bone, epidural abscess, subdural empyema, brain abscess, meningitis, orbital phlebitis and arteritis, cerebral infarction, and mycotic aneurysm.
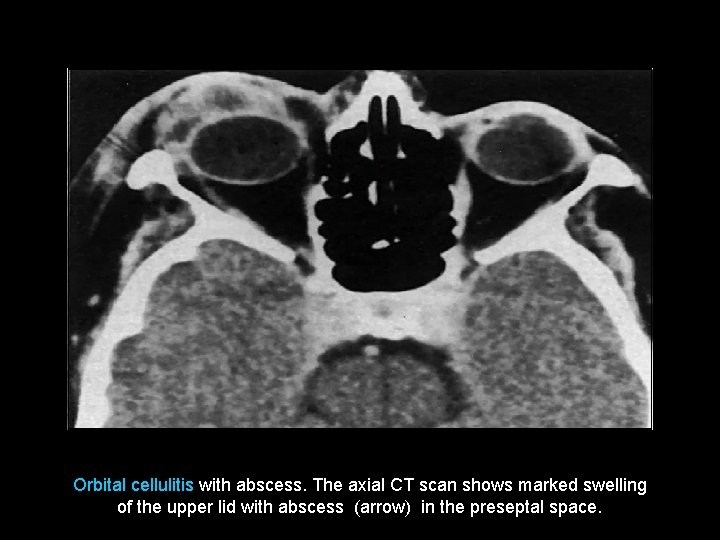
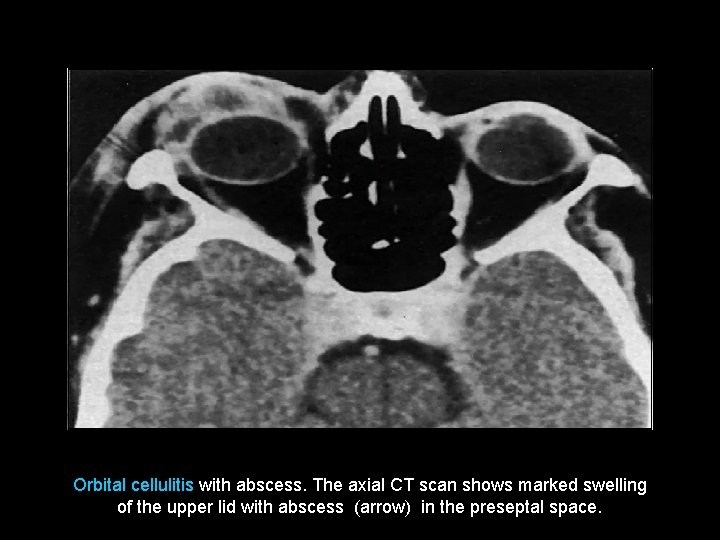
Orbital cellulitis with abscess. The axial CT scan shows marked swelling of the upper lid with abscess (arrow) in the preseptal space.
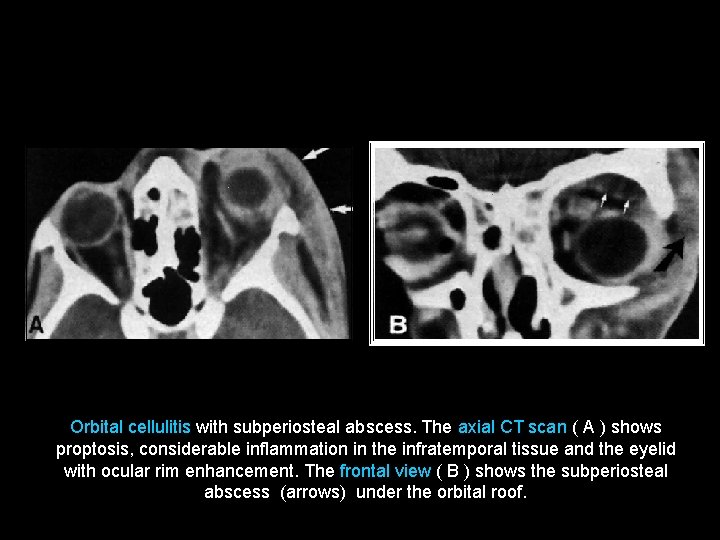
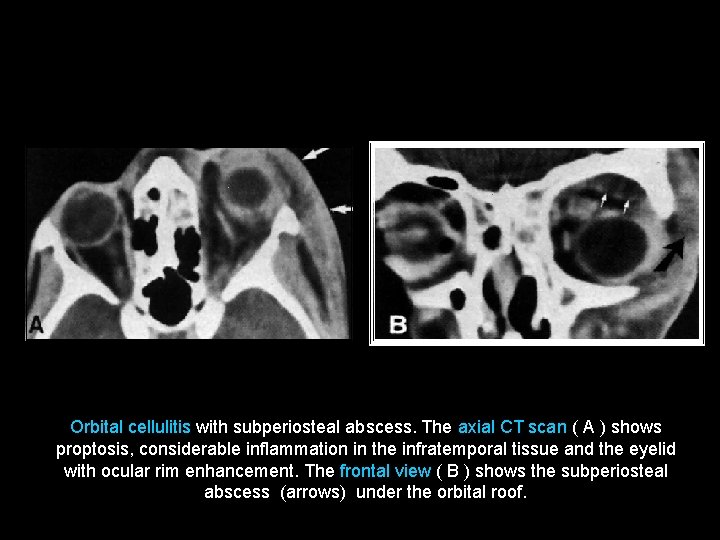
Orbital cellulitis with subperiosteal abscess. The axial CT scan ( A ) shows proptosis, considerable inflammation in the infratemporal tissue and the eyelid with ocular rim enhancement. The frontal view ( B ) shows the subperiosteal abscess (arrows) under the orbital roof.
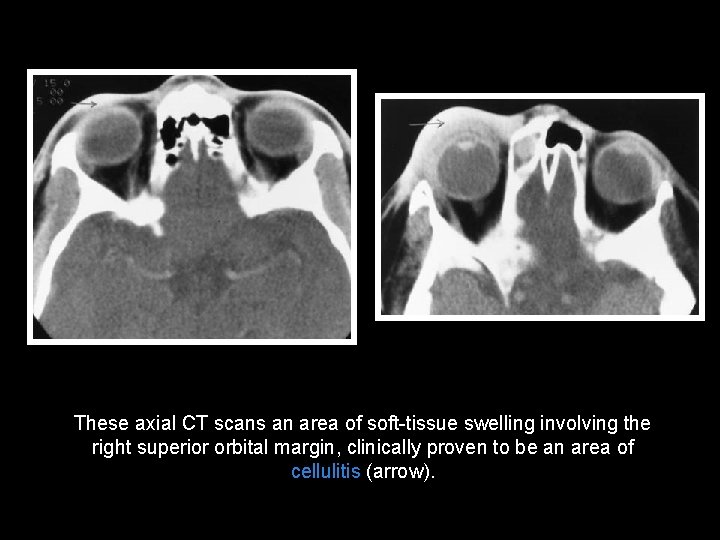
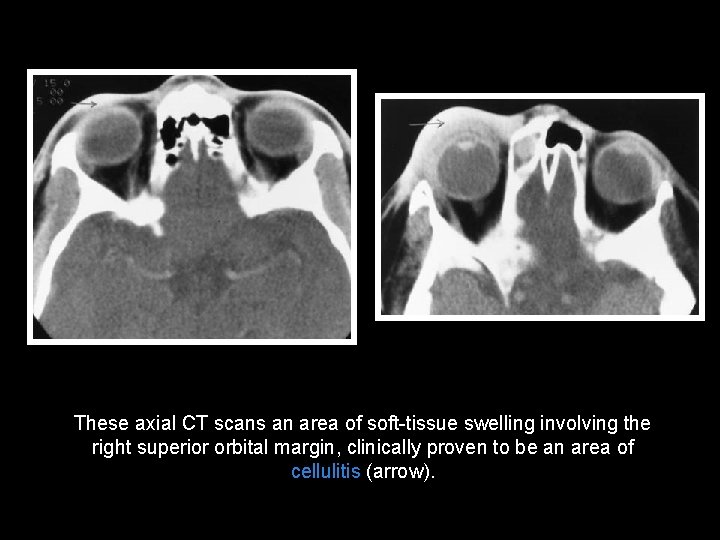
These axial CT scans an area of soft-tissue swelling involving the right superior orbital margin, clinically proven to be an area of cellulitis (arrow).
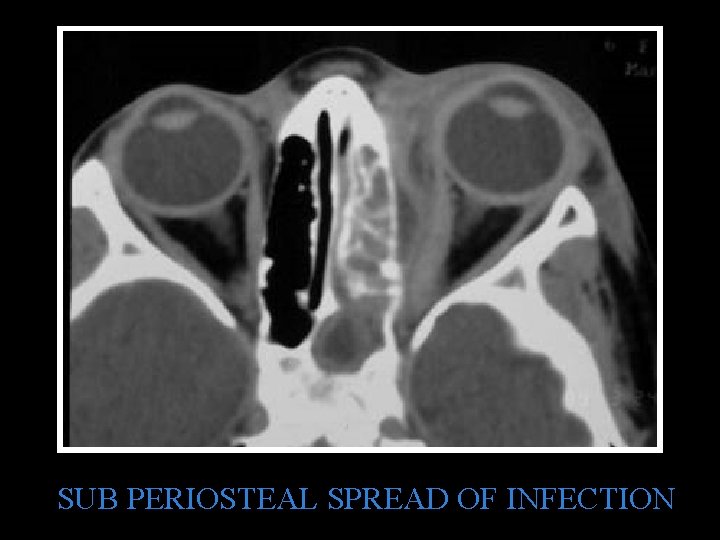
SUB PERIOSTEAL SPREAD OF INFECTION
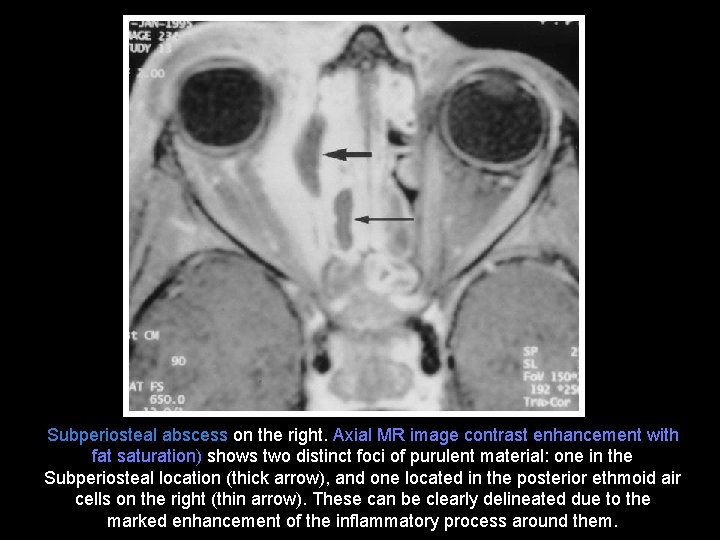
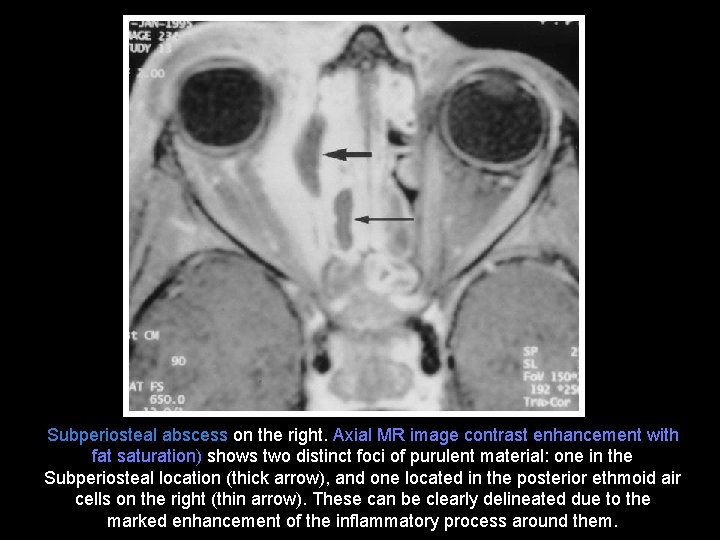
Subperiosteal abscess on the right. Axial MR image contrast enhancement with fat saturation) shows two distinct foci of purulent material: one in the Subperiosteal location (thick arrow), and one located in the posterior ethmoid air cells on the right (thin arrow). These can be clearly delineated due to the marked enhancement of the inflammatory process around them.
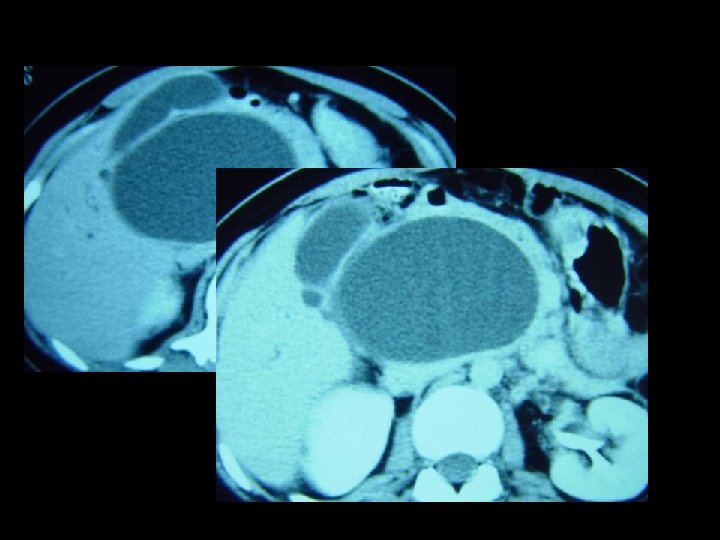
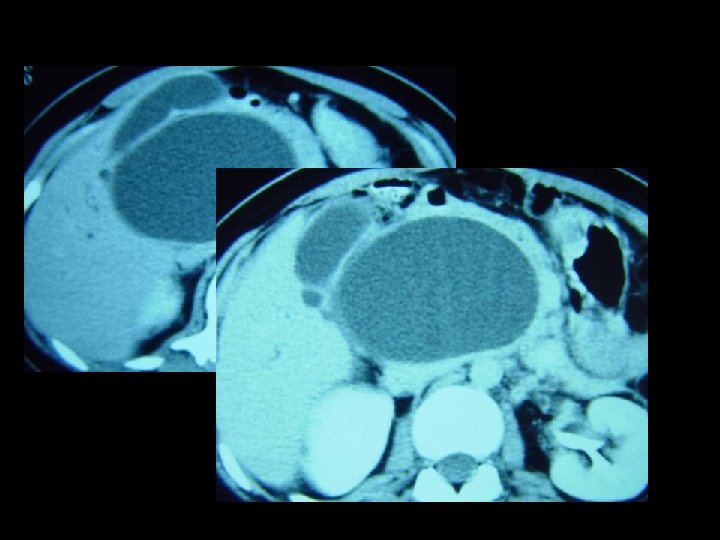
Case 5 • Choledocal cyst
EXPLANATION Dense metaphyseal line • Normal metaphyseal endochondral bone growth (in the zone of provisional calcification) requires the maintenance of a delicate balance between osteoblastic bone deposition and osteoclastic bone remodeling. • Whenever growing bone is subjected to toxic, metabolic, neoplastic, or infectious stressors, proper osteogenesis is compromised. • Stress on growing bone leads to poor endochondral bone formation. • In general, when the stress is eliminated, rapid deposition of new bone at the metaphysis produces dense bands.
• The result of osseous lead poisoning effectively illustrates a specific example of how the dense metaphyseal band sign is formed. • With lead toxicity, or plumbism, the lead ions deposit on the hydroxyapatite crystal but preferentially in the zone of provisional calcification. • Lead inhibits osteoclastic remodeling, but it has no effect on osteoblasts. The result is an increase in the thickness and number of trabeculae at the metaphysis. • The lead itself contributes very little to the metaphyseal density in plumbism. • Whenever growing bone recovers from any pathologic insult or becomes lead poisoned, exuberant calcium deposition in the zone of provisional calcification induces dense metaphyseal bands.
• ORBITAL CELLULITIS - divided into 3 groups 1) bacterial preseptal cellulitis 2) bacterial orbital cellulitis 3) fungal orbital cellulitis Preseptal Cellulitis - arises anterior to orbital septum - generally a function of direct inoculation from trauma and from nearby skin - severe upper lid edema, less edema of lower lid with minimal involvement of the globe Orbital Cellulitis - usually arises from paranasal sinus disease - Sx -> sign. proptosis of the eye, restricted eye movements with pain and periorbital involvement - Abscess formation is not uncommon Fungal Cellulitis - uncommon - two major types 1) Phycomycosis 2) Aspergillosis
• Orbital Cellulitis more about Orbital Cellulitis • Bacterial infections that affect the orbit and the structures surrounding the eyes • Because of the close proximity of the eye to the brain, orbital infections can be very dangerous. • • Fever • Redness or swollen eyelids and eyes. • A droop in the eyelids. • Pain around the eye and upon eye movement • Eyes may bulge forward • Headaches • Conjunctiva (the lining of the eye lids and the eye surface) may become red and begin to itch. • In severe cases, there may be a full or partial loss of vision (Optic neuritis). • Neck stiffness and pain, nausea, vomiting, delirium, and coma can occur with spread of infection to the brain. • • Infection can spread from the paranasal sinuses (air-filled cavities around the eyes), blood, teeth, or other sites in the body, to the tissues immediately surrounding the eyes. • Infection can also occur after eye injury. • The most common infections are due to bacteria – – – Staphylococcus aureus Streptococcus pyogenes and Streptococcus pneumoniae Mixed infections with different bacteria can also occur • In children under the age of 5, H. influenzae is the most common bacterium. Recent vaccinations with the HB vaccine are showing a drop in the number of cases. • Fungi are seen in those with a weak immune or body defense system. •
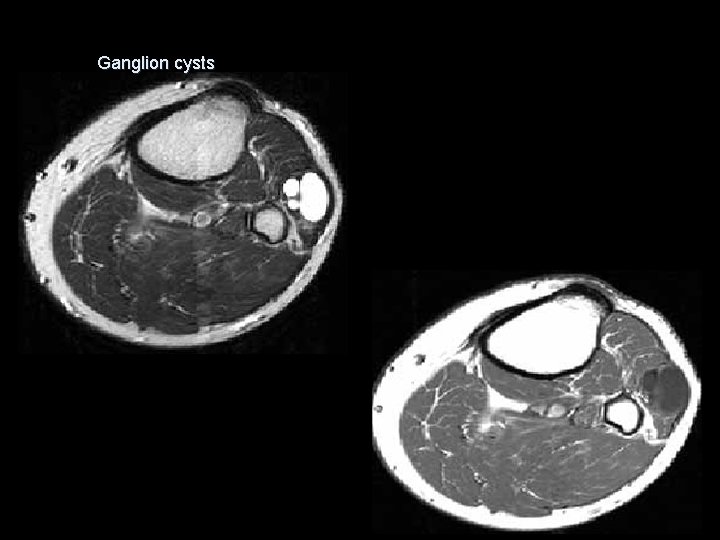
Ganglion cysts • Ganglion cysts are locular or multilocular benign, masses filled with mucinous material. • Ganglion cysts are commonly related to trauma and may arise from tendons, ligaments, bursa and joint capsules. • May present with compressive nerve palsy e. g. on the common peroneal nerve palsy when the ganglion arise near the proximal tibiofibular joint.
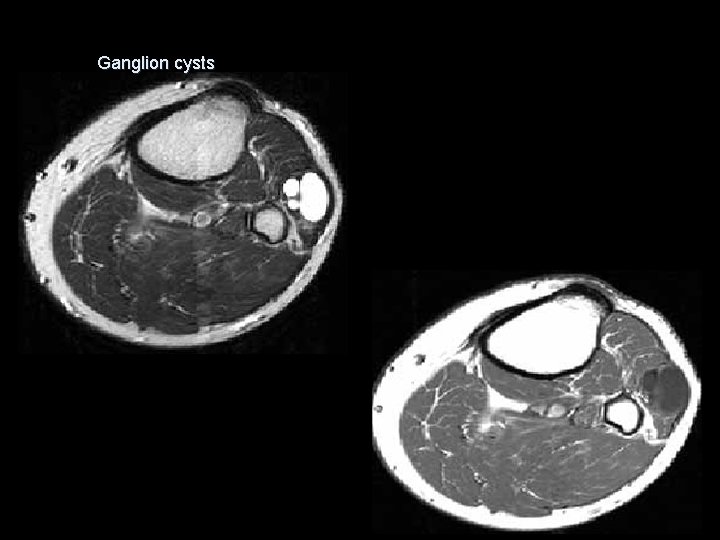
Ganglion cysts
