TCT 2012 Hypothermia in STEMI CRT 2013 Washington
















- Slides: 48

TCT 2012 Hypothermia in STEMI, CRT 2013 Washington. Therapeutic DC Cardiac Arrest and Cardiogenic Shock Michael R. Mooney MD, FACC Director Interventional Cardiology Minneapolis Heart Institute AMI David Hildebrandt, RN Director, CV Emergencies MHI ACS/AMI - Update on Drugs, Devices and Approaches Michael R. Mooney, MD, FACC Director, Interventional Cardiology

Michael R. Mooney, MD I/we have no real or apparent conflicts of interest to report.
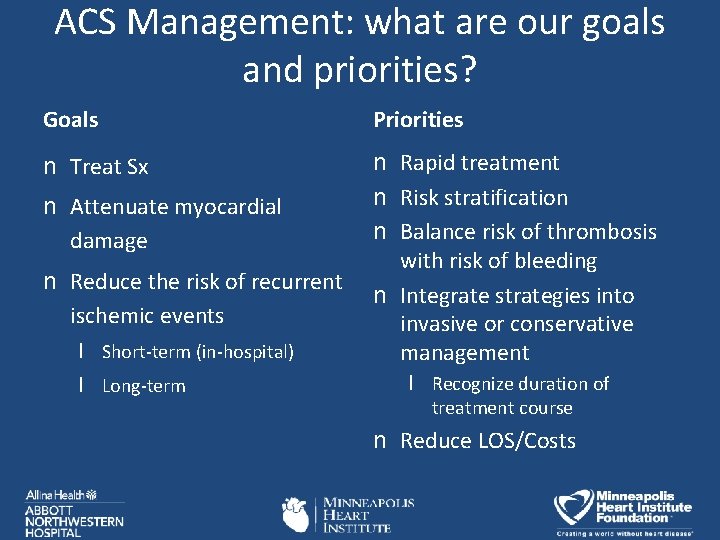
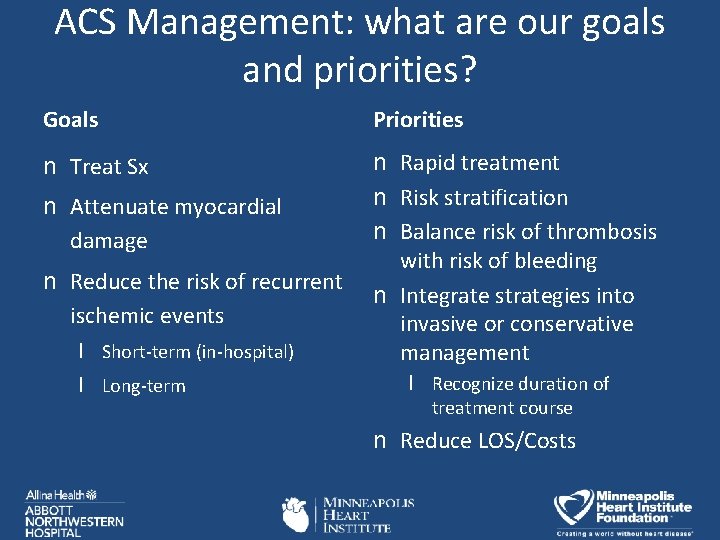
ACS Management: what are our goals and priorities? Goals Priorities n Treat Sx n Rapid treatment n Risk stratification n Balance risk of thrombosis with risk of bleeding n Integrate strategies into invasive or conservative management n Attenuate myocardial damage n Reduce the risk of recurrent ischemic events l Short-term (in-hospital) l Long-term l Recognize duration of treatment course n Reduce LOS/Costs
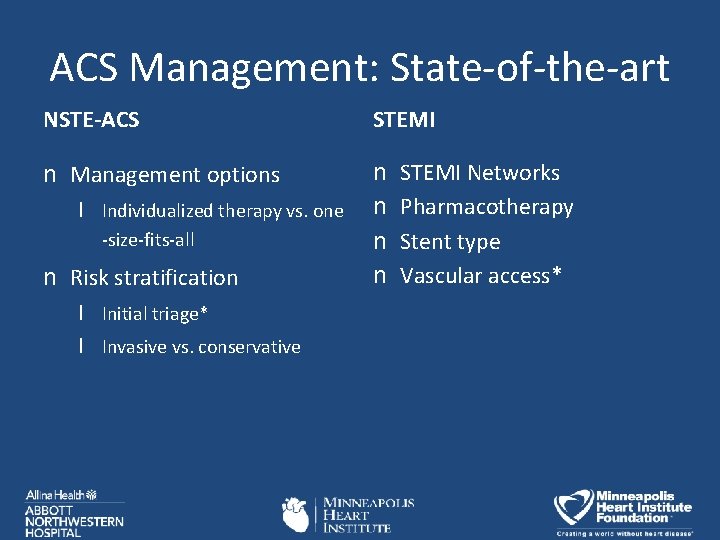
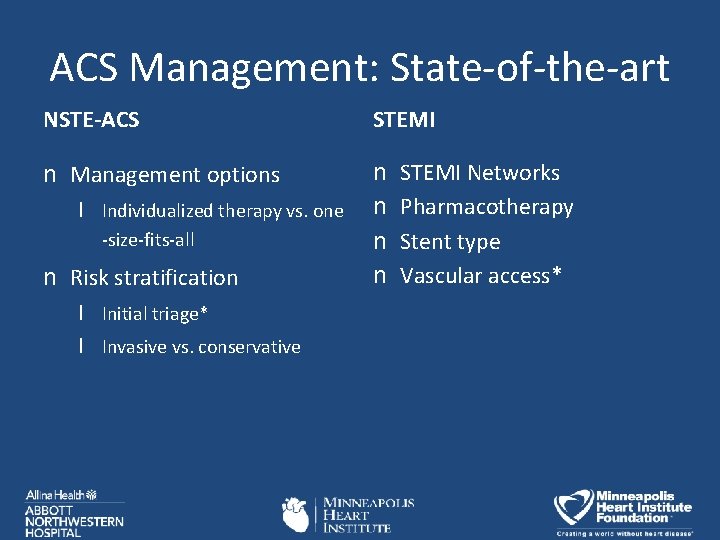
ACS Management: State-of-the-art NSTE-ACS STEMI n Management options n n l Individualized therapy vs. one -size-fits-all n Risk stratification l Initial triage* l Invasive vs. conservative STEMI Networks Pharmacotherapy Stent type Vascular access*
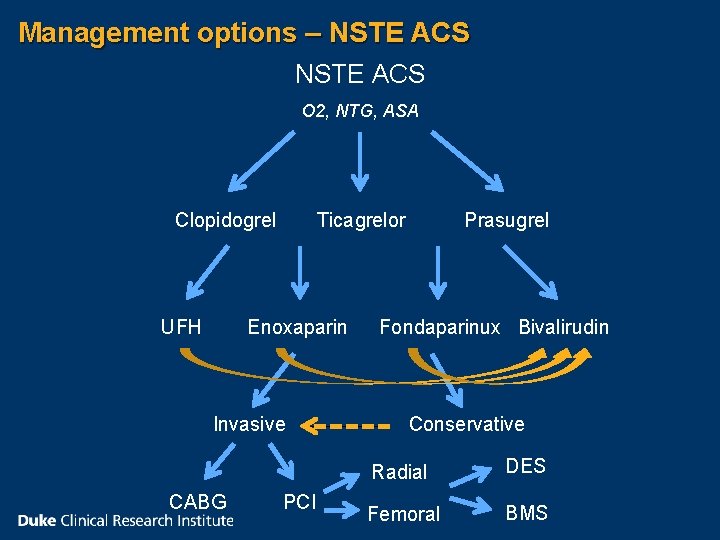
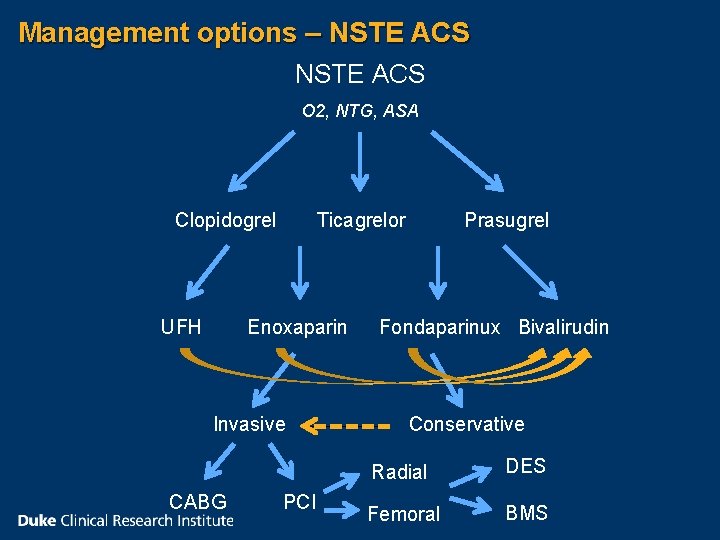
Management options – NSTE ACS O 2, NTG, ASA Clopidogrel UFH Ticagrelor Enoxaparin Invasive CABG PCI Prasugrel Fondaparinux Bivalirudin Conservative Radial DES Femoral BMS
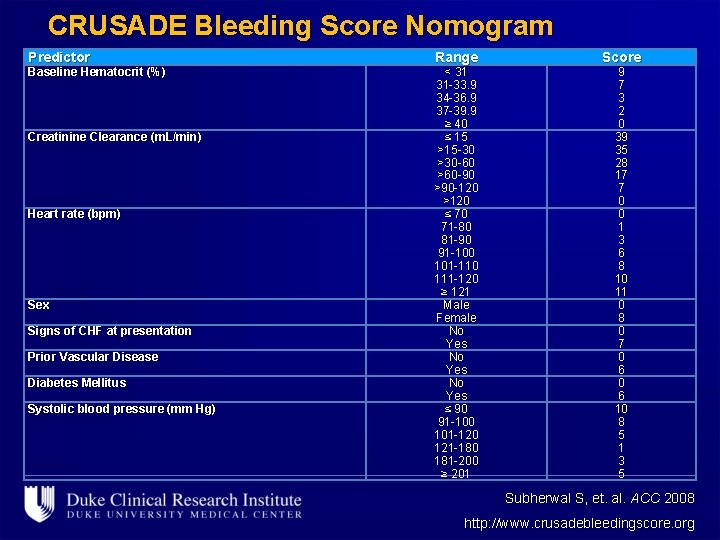
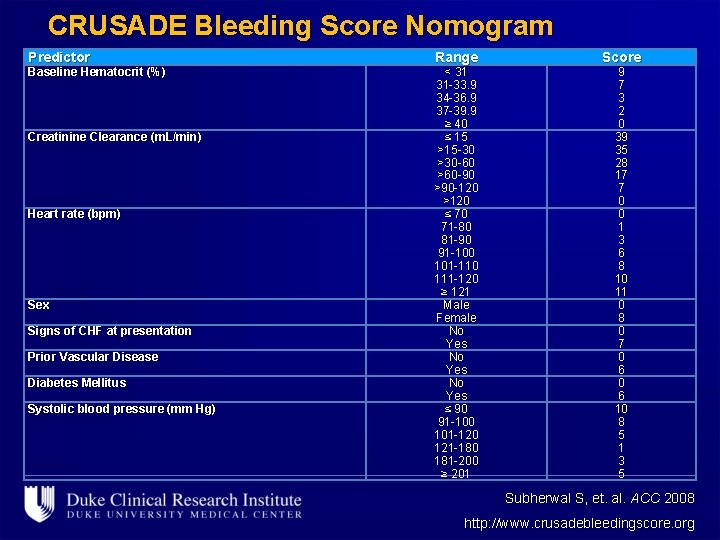
CRUSADE Bleeding Score Nomogram Predictor Baseline Hematocrit (%) Creatinine Clearance (m. L/min) Heart rate (bpm) Sex Signs of CHF at presentation Prior Vascular Disease Diabetes Mellitus Systolic blood pressure (mm Hg) Range < 31 31 -33. 9 34 -36. 9 37 -39. 9 ≥ 40 ≤ 15 >15 -30 >30 -60 >60 -90 >90 -120 >120 ≤ 70 71 -80 81 -90 91 -100 101 -110 111 -120 ≥ 121 Male Female No Yes ≤ 90 91 -100 101 -120 121 -180 181 -200 ≥ 201 Score 9 7 3 2 0 39 35 28 17 7 0 0 1 3 6 8 10 11 0 8 0 7 0 6 10 8 5 1 3 5 Subherwal S, et. al. ACC 2008 http: //www. crusadebleedingscore. org
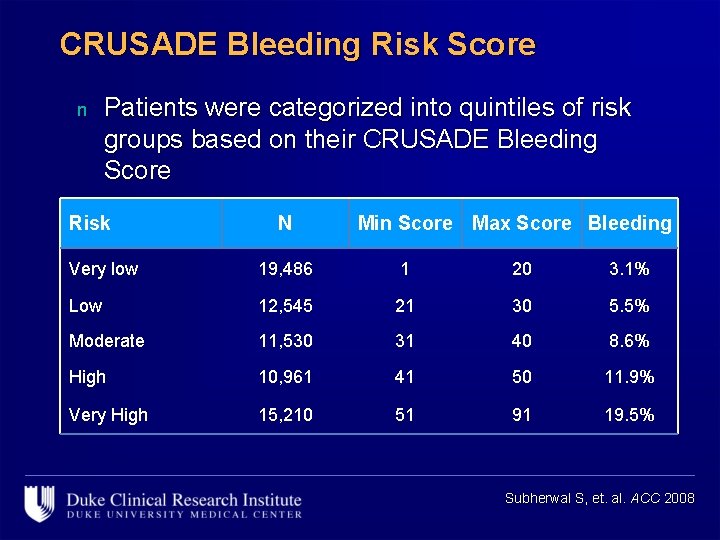
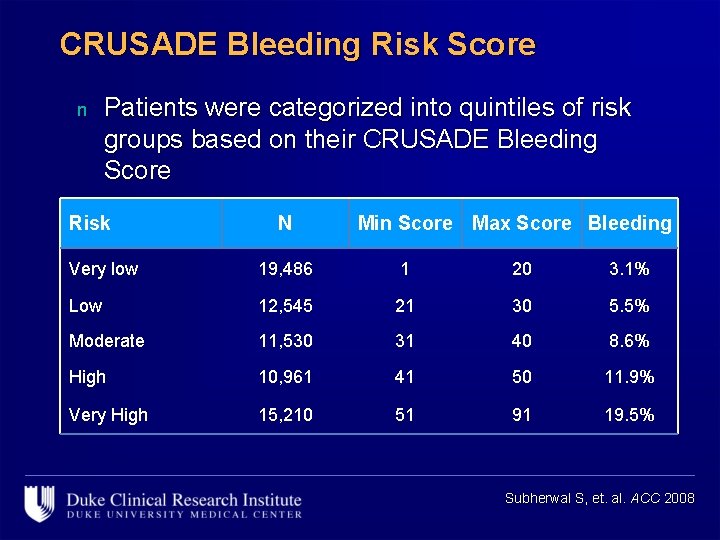
CRUSADE Bleeding Risk Score n Patients were categorized into quintiles of risk groups based on their CRUSADE Bleeding Score Risk N Min Score Max Score Bleeding Very low 19, 486 1 20 3. 1% Low 12, 545 21 30 5. 5% Moderate 11, 530 31 40 8. 6% High 10, 961 41 50 11. 9% Very High 15, 210 51 91 19. 5% Subherwal S, et. al. ACC 2008
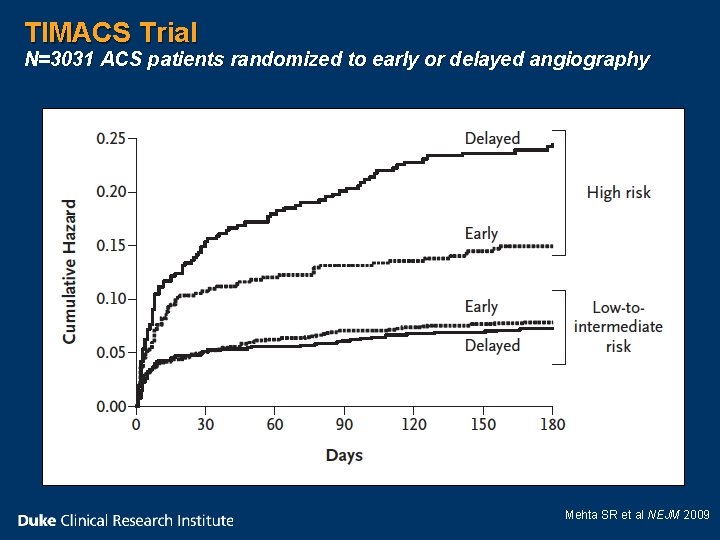
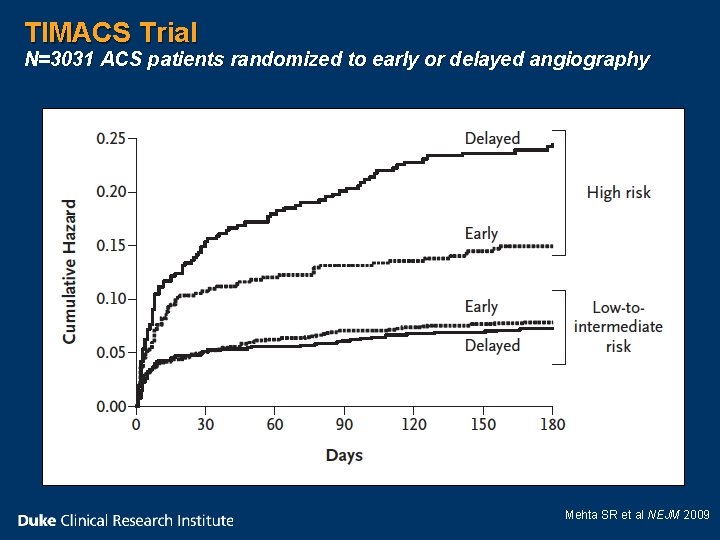
TIMACS Trial N=3031 ACS patients randomized to early or delayed angiography Mehta SR et al NEJM 2009
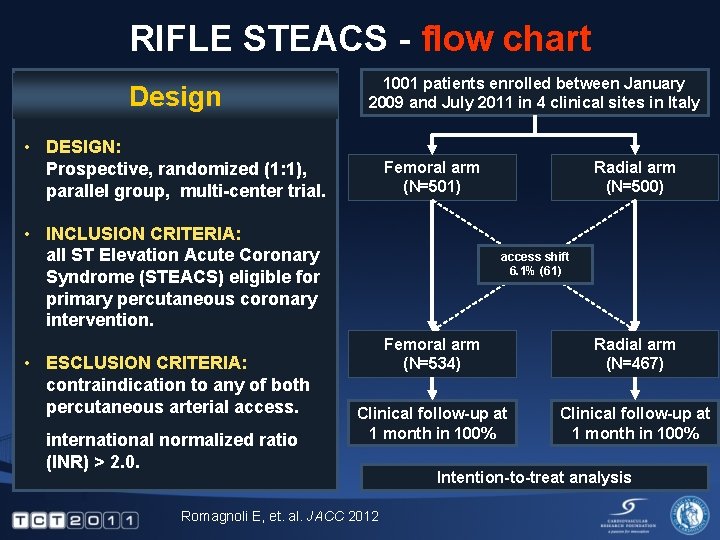
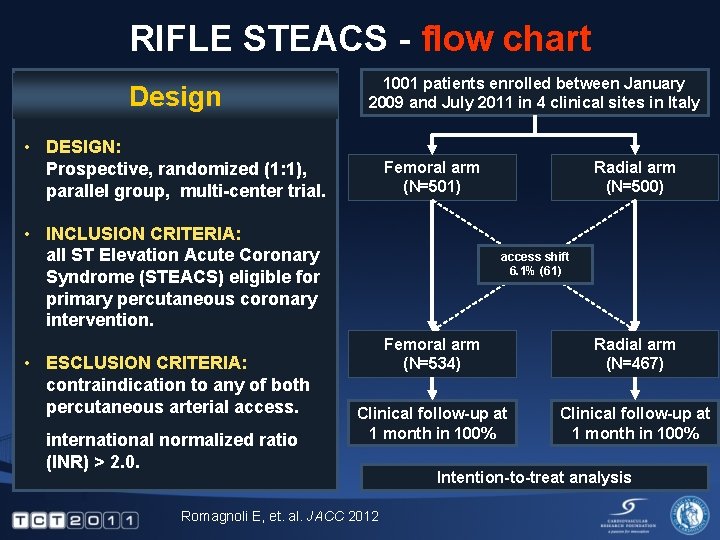
RIFLE STEACS - flow chart Design 1001 patients enrolled between January 2009 and July 2011 in 4 clinical sites in Italy • DESIGN: Prospective, randomized (1: 1), parallel group, multi-center trial. Femoral arm (N=501) • INCLUSION CRITERIA: all ST Elevation Acute Coronary Syndrome (STEACS) eligible for primary percutaneous coronary intervention. • ESCLUSION CRITERIA: contraindication to any of both percutaneous arterial access. international normalized ratio (INR) > 2. 0. Radial arm (N=500) access shift 6. 1% (61) Femoral arm (N=534) Radial arm (N=467) Clinical follow-up at 1 month in 100% Romagnoli E, et. al. JACC 2012 Intention-to-treat analysis
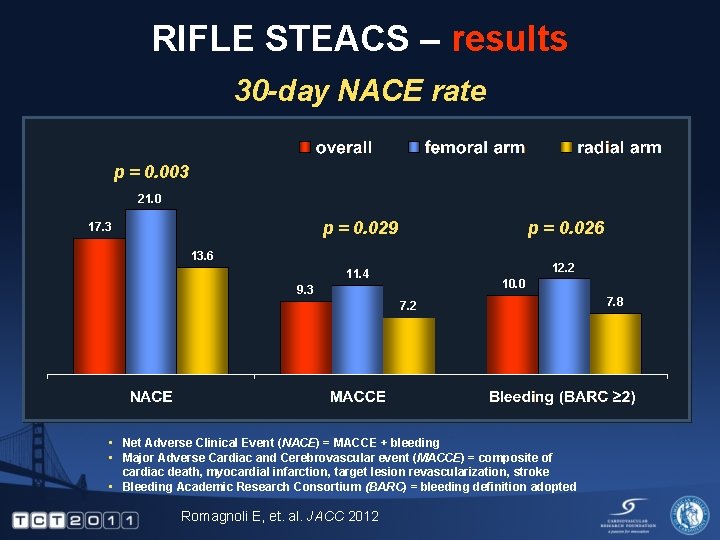
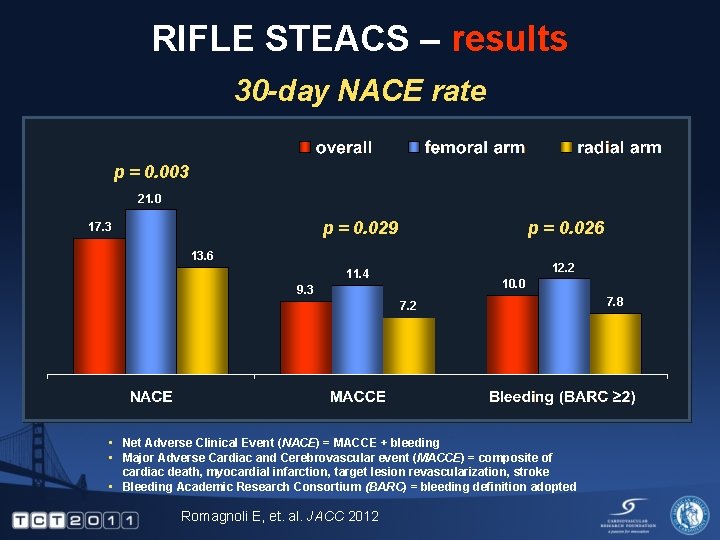
RIFLE STEACS – results 30 -day NACE rate p = 0. 003 21. 0 17. 3 p = 0. 029 p = 0. 026 11. 4 12. 2 13. 6 10. 0 9. 3 7. 2 • Net Adverse Clinical Event (NACE) = MACCE + bleeding • Major Adverse Cardiac and Cerebrovascular event (MACCE) = composite of cardiac death, myocardial infarction, target lesion revascularization, stroke • Bleeding Academic Research Consortium (BARC) = bleeding definition adopted Romagnoli E, et. al. JACC 2012 7. 8

RIFLE STEACS – results 30 -day MACCE rate p = 0. 020 9. 2 7. 2 5. 2 p = 1. 000 1. 3 1. 4 1. 2 Romagnoli E, et. al. JACC 2012 p = 0. 604 1. 5 1. 8 1. 2 p = 0. 725 0. 7 0. 6 0. 8
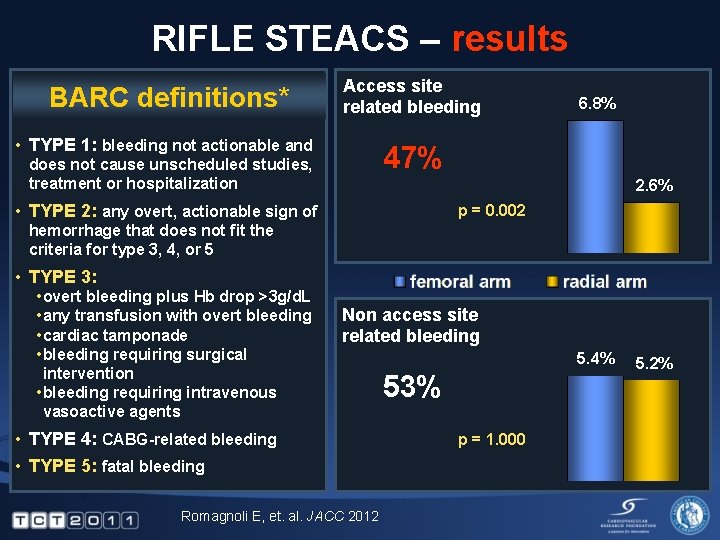
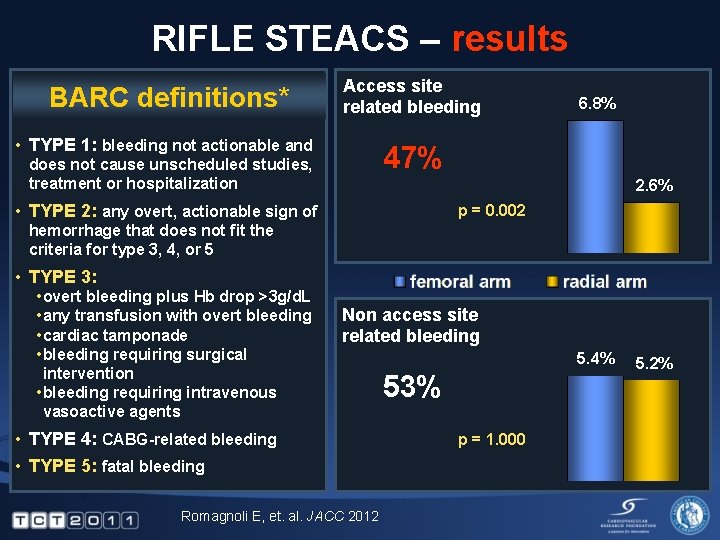
RIFLE STEACS – results BARC definitions* Access site related bleeding • TYPE 1: bleeding not actionable and 47% does not cause unscheduled studies, treatment or hospitalization 6. 8% 2. 6% • TYPE 2: any overt, actionable sign of p = 0. 002 hemorrhage that does not fit the criteria for type 3, 4, or 5 • TYPE 3: • overt bleeding plus Hb drop >3 g/d. L • any transfusion with overt bleeding • cardiac tamponade • bleeding requiring surgical intervention • bleeding requiring intravenous vasoactive agents Non access site related bleeding • TYPE 4: CABG-related bleeding • TYPE 5: fatal bleeding Romagnoli E, et. al. JACC 2012 5. 4% 53% p = 1. 000 5. 2%
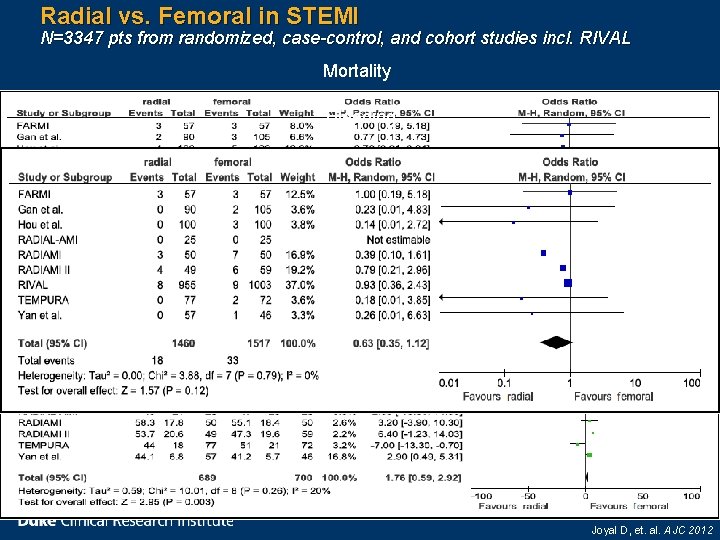
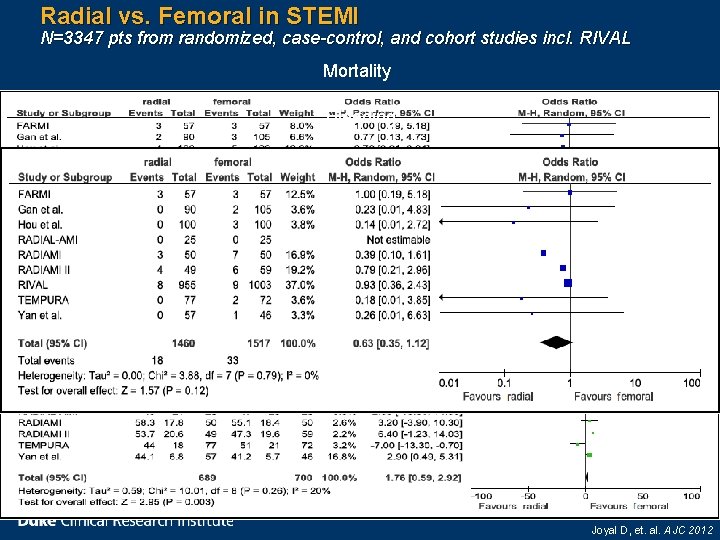
Radial vs. Femoral in STEMI N=3347 pts from randomized, case-control, and cohort studies incl. RIVAL Mortality Bleeding Procedure time (min) Joyal D, et. al. AJC 2012
ESC Updated STEMI Guidelines n The guidelines also support the use of transradial primary PCI over the use of transfemoral, but only in the hands of experienced operators… Steg PG, James SK, Atar D, et. al. EHJ 2012

ACS: State-of-the-art n Accelerated developments in ACS management make the “optimal” strategy a constantly moving target l The benefit-risk ratio of the chosen strategy may be influenced by the patient’s baseline risk n Nomograms to assess a patient’s risk of death, death/MI, and bleeding in the short- and intermediateterm are available n STEMI care has improved significantly l n The future is to reduce complications (bleeding, vascular), develop networks, STE-No. MI? Radial approach supported by trials, observational data, and guidelines l l No D 2 B consistently reported, mechanism of benefit unclear Need a large multicenter trial that reports clinical outcomes and D 2 B

Challenges to Rapid Triage and Transport in the US and Data/Trial Interpretation
TYPES OF HEMODYNAMIC SUPPORT • Intra Aortic Balloon Pump (IABP) • Percutaneous Left Ventricular Assist Devices – Impella LP – Tandem Heart • Extra corporeal Life support (ECMO)

IABP-SHOCK II Trial The use of IABP did not significantly reduce 30 day mortality in patients with cardiogenic shock complicating STEMI Thiele H et al. N Engl J Med 2012; 367: 1287 -1296
When Might We Consider Hemodynamic Support for STEMI? • Severe LV dysfunction: • Large Ischemic burden • Compromise of coronary flow • High risk of no reflow (i. e. , SVGs, Rota, STEMI) • Cardiogenic shock • Cardiac arrest

Anemia and Prognosis in ACS Patients Meta Analysis of 241, 293 patients OR 95%CI Short term mortality 2. 77 2. 09 -3. 65 Long term mortality 2. 03 1. 52 -2. 71 Heart failure 1. 96 1. 47 -2. 62 Cardiogenic shock 1. 95 1. 04 -2. 64 Major bleeding 4. 28 1. 05 -17. 14 Liu et al J Int Med Res 2012; 40(1) 43 -55
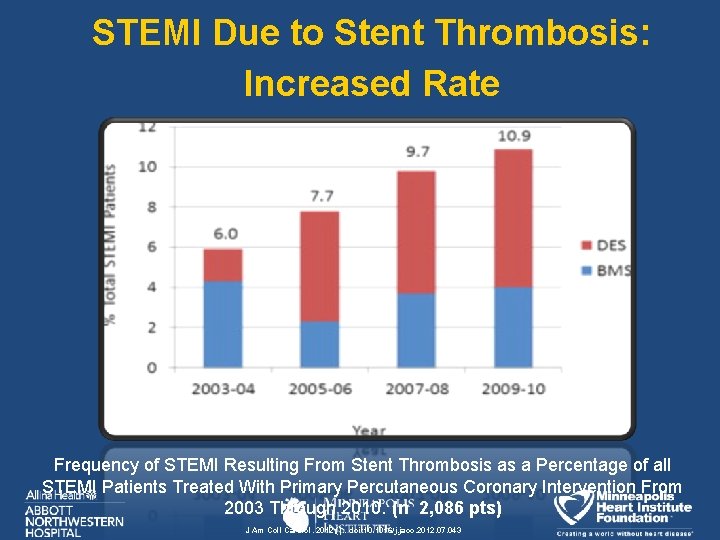
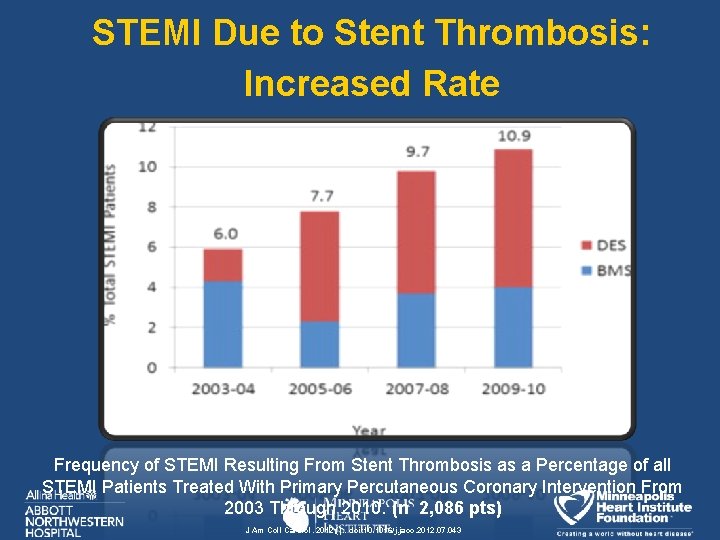
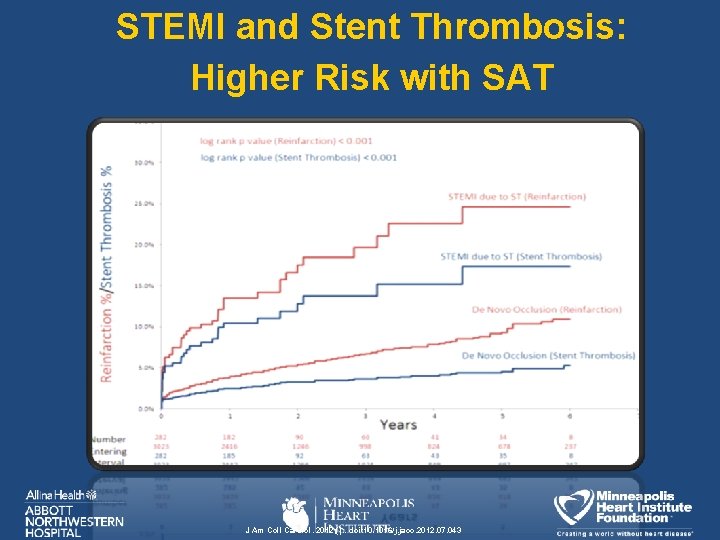
STEMI Due to Stent Thrombosis: Increased Rate Frequency of STEMI Resulting From Stent Thrombosis as a Percentage of all STEMI Patients Treated With Primary Percutaneous Coronary Intervention From 2003 Through 2010. (n 2, 086 pts) J Am Coll Cardiol. 2012; (): . doi: 10. 1016/j. jacc. 2012. 07. 043
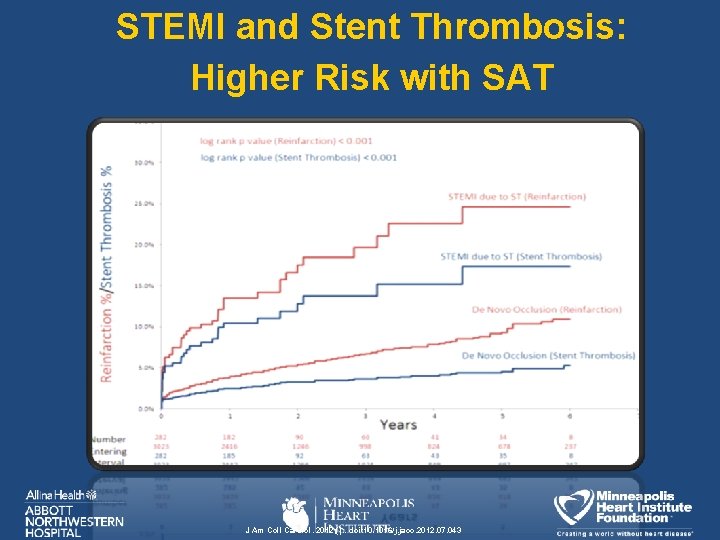
STEMI and Stent Thrombosis: Higher Risk with SAT J Am Coll Cardiol. 2012; (): . doi: 10. 1016/j. jacc. 2012. 07. 043
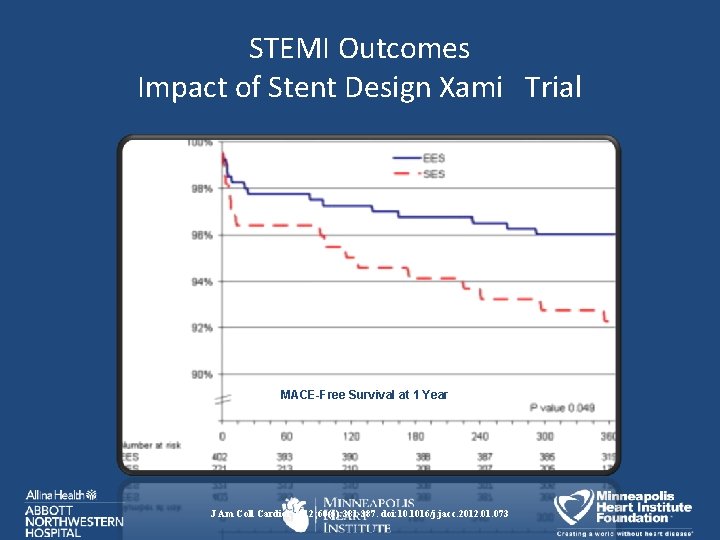
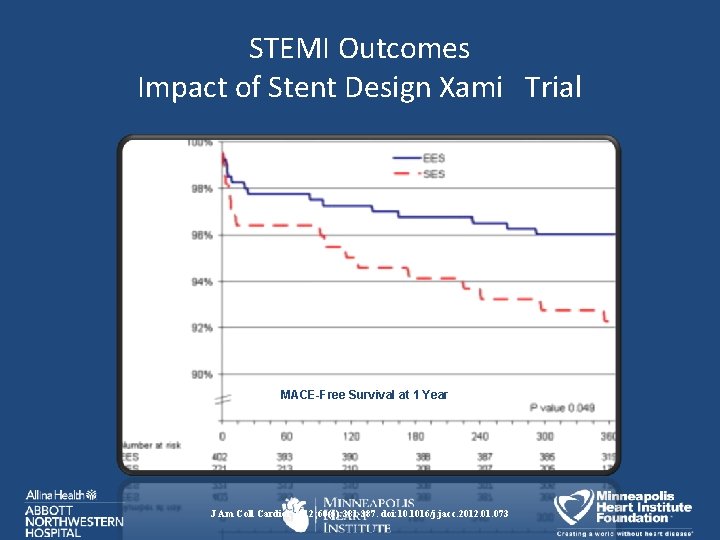
STEMI Outcomes Impact of Stent Design Xami Trial MACE-Free Survival at 1 Year J Am Coll Cardiol. 2012; 60(5): 381 -387. doi: 10. 1016/j. jacc. 2012. 01. 073
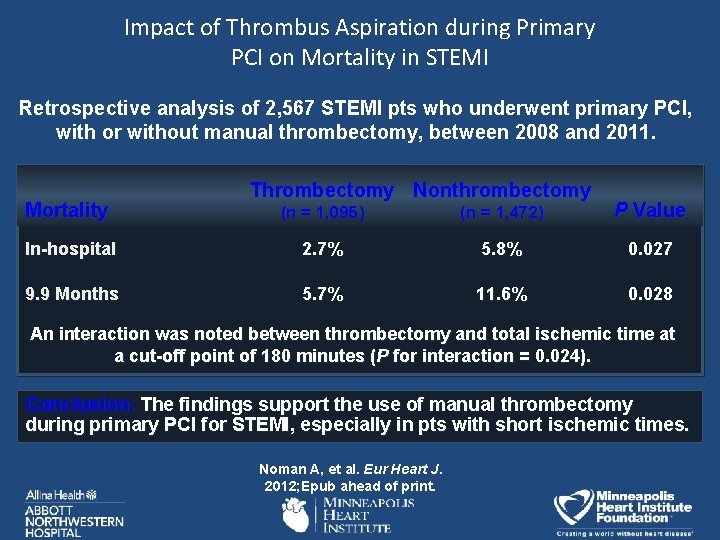
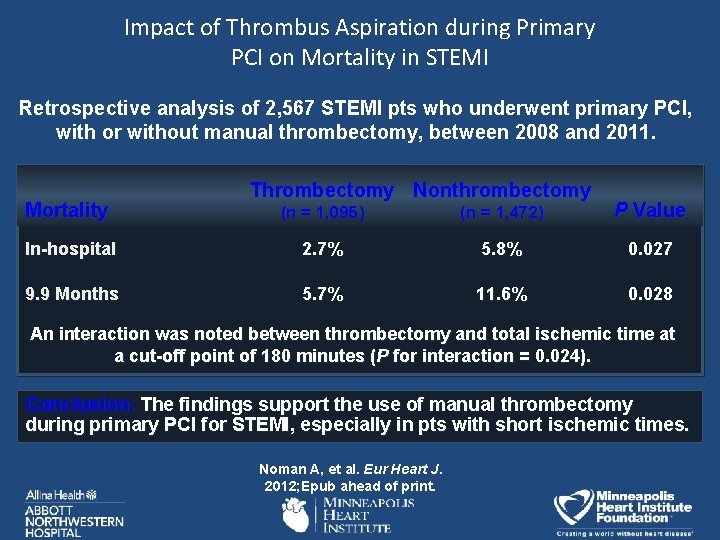
Impact of Thrombus Aspiration during Primary PCI on Mortality in STEMI Retrospective analysis of 2, 567 STEMI pts who underwent primary PCI, with or without manual thrombectomy, between 2008 and 2011. Mortality Thrombectomy Nonthrombectomy (n = 1, 095) (n = 1, 472) P Value In-hospital 2. 7% 5. 8% 0. 027 9. 9 Months 5. 7% 11. 6% 0. 028 An interaction was noted between thrombectomy and total ischemic time at a cut-off point of 180 minutes (P for interaction = 0. 024). Conclusion: The findings support the use of manual thrombectomy during primary PCI for STEMI, especially in pts with short ischemic times. Noman A, et al. Eur Heart J. 2012; Epub ahead of print.
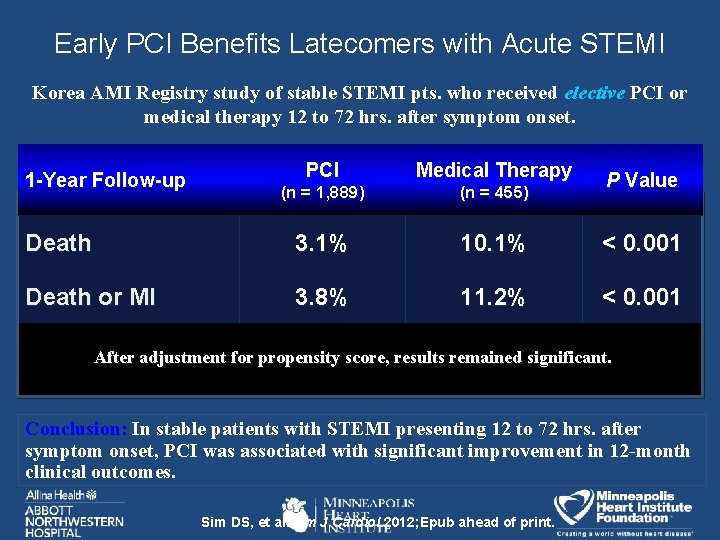
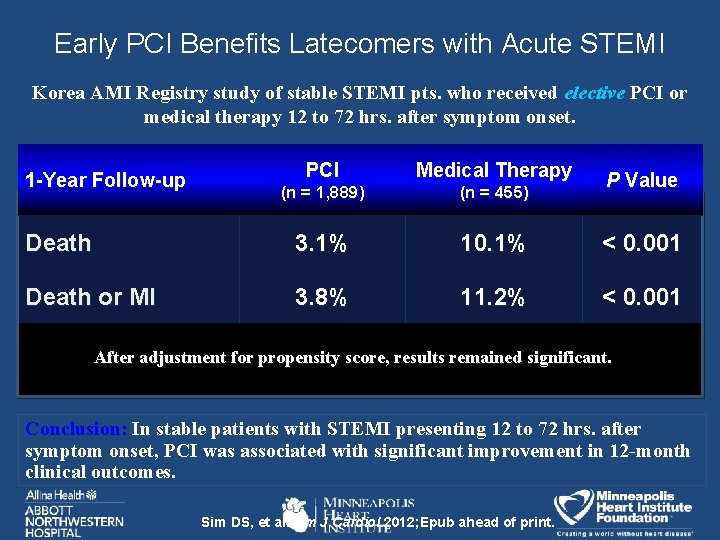
Early PCI Benefits Latecomers with Acute STEMI Korea AMI Registry study of stable STEMI pts. who received elective PCI or medical therapy 12 to 72 hrs. after symptom onset. PCI Medical Therapy (n = 1, 889) (n = 455) Death 3. 1% 10. 1% < 0. 001 Death or MI 3. 8% 11. 2% < 0. 001 1 -Year Follow-up P Value After adjustment for propensity score, results remained significant. Conclusion: In stable patients with STEMI presenting 12 to 72 hrs. after symptom onset, PCI was associated with significant improvement in 12 -month clinical outcomes. Sim DS, et al. Am J Cardiol. 2012; Epub ahead of print.

Improving Door to Balloon Time Pre Hospital EKG m. Visum STEMI Alert System by m. Visum, Inc. No STEMI (n = 9, 328) vs. STEMI J Am Coll Cardiol. 2012; 60(9): 806 -811. doi: 10. 1016/j. jacc. 2012. 03. 071 patients (n = 303) SRB TCT 2012

ST-Segment Resolution as a Predictor of Death and MACE after Primary PCI in STEMI: The HORIZONS-AMI Trial 2, 484 pts with interpretable baseline and 60 -minute post-PCI ECGs ST-segment resolution > 70% ST-segment resolution 30 -70% ST-segment resolution < 30% 30 ST resolution at 60’ Partial (30%-70%) 712 (28. 7%) Absent (<30%) 514 (20. 7%) Death (%) Complete (>70%) 1, 258 (50. 5%) 25 20 15 10 P=0. 03 5 0 0 Number at Risk >70% 1258 30 -70% 712 <30% 514 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36 Time in Months 1213 690 484 1203 682 483 1188 678 480 1173 669 465 Farkouh ME et al from Stone 2012. 1167 665 461 1154 659 457 1129 645 445 1119 641 443 744 445 327

ACS Admissions in the US SRB TCT 2012
What About STEMI and TH?
Therapeutic Hypothermia (TH): • The gold standard treatment for reperfusion injury • Reperfusion injury is important in both cardiac arrest/anoxic encephalopathy and acute MI • TH is pluripotent • TH is standard of care for CA • TH is an emerging treatment for Acute MI • TH may have efficacy in post MI cardiogenic shock • TH is markedly underutilized
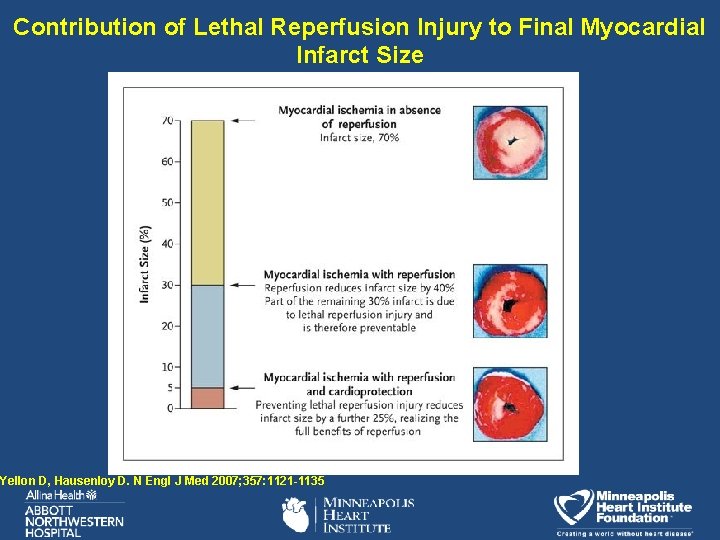
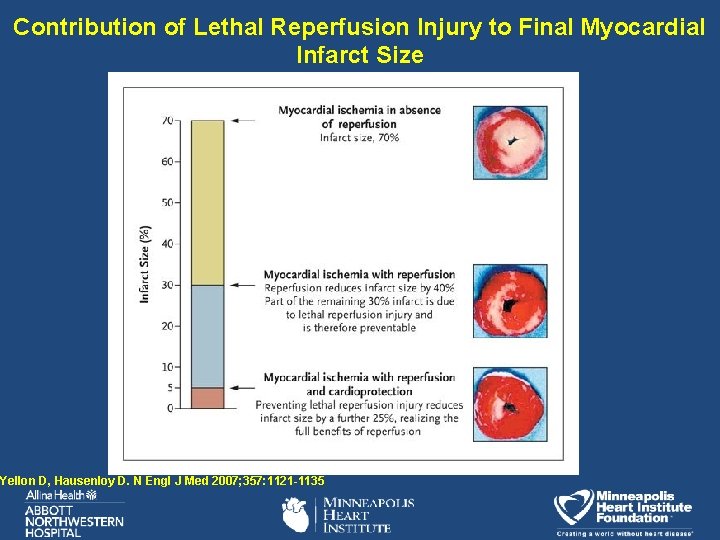
Contribution of Lethal Reperfusion Injury to Final Myocardial Infarct Size Yellon D, Hausenloy D. N Engl J Med 2007; 357: 1121 -1135
Major Mediators of Lethal Reperfusion Injury • reactive oxygen species • oxygen paradox • Ca paradox - sarcolemma • cytokines • activated complement • activated mitocondrial PTPpermeability transition pore accelerated by Ca. • neutrophil vascular plugging • hypercontractile myocyte • uncoupled oxidative-phos • all leading to lethal reperfusion Injury Yellon D, Hausenloy D. N Engl J Med 2007; 357: 1121 -1135

Anterior Myocardial Infarct Size vs Temp at Reperfusion Source- O’Neill, “Novel Myocardial Preservation Therapies: Past Frustrations and Future Promise”, TCT 2006
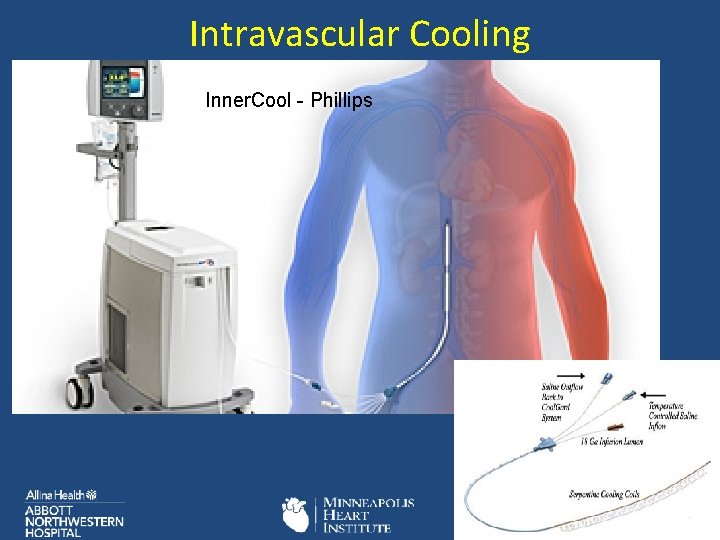
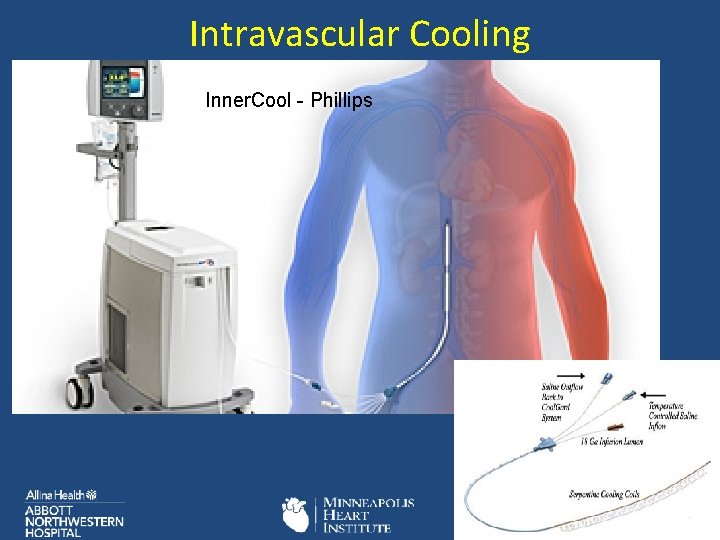
Intravascular Cooling Inner. Cool - Phillips

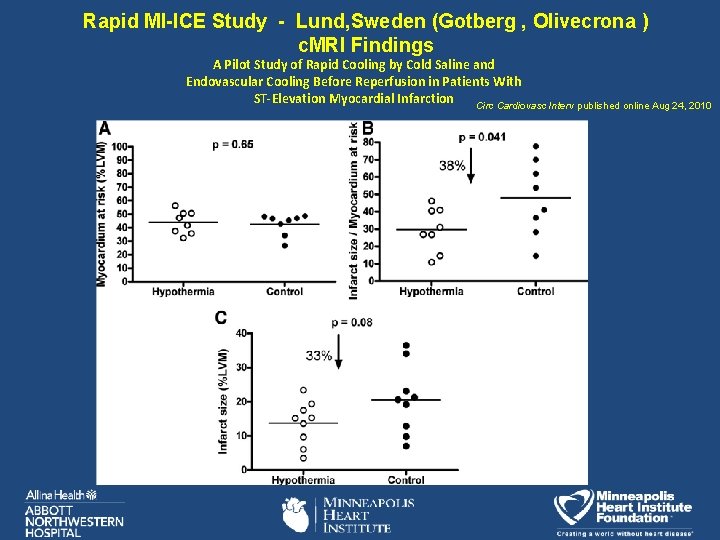
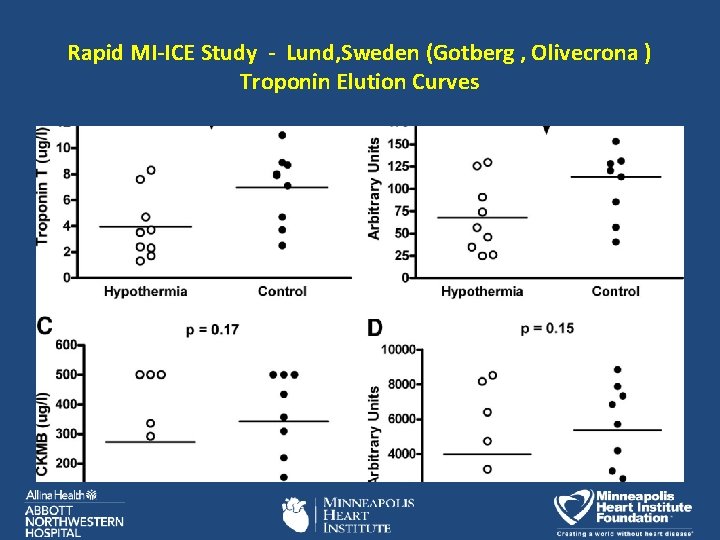
Rapid MI-ICE study summary • 20 pts w/ STEMI randomized iced saline and intravascular cooling v. control (Innercool) • Core temp <35 in 40 min D 2 B 43 min • 1500 cc 4 deg. Saline. Demerol , buspirone, Bear Hugger , intravascular cooling • Day 4 - c. MRI T 2 v. Gadolinium -- Hedstrom E, J Am. Coll Cardiovasc Imaging. 2009; 2: 569 – 576. • Troponin T elution curves • No difference in clinical outcomes
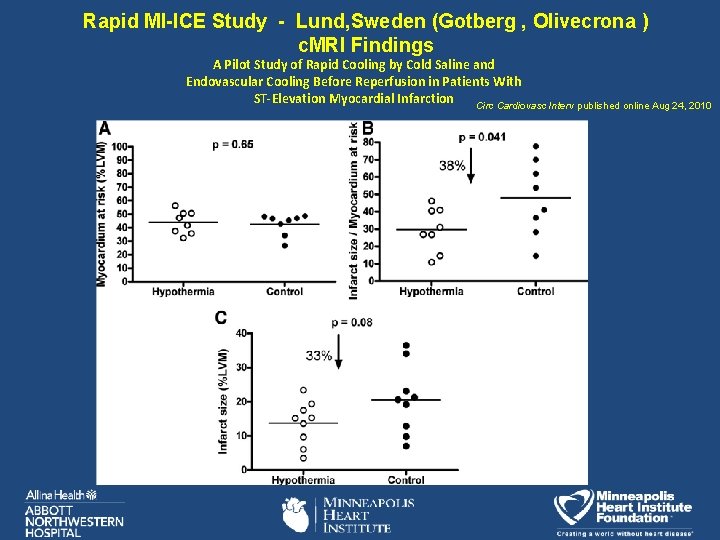
Rapid MI-ICE Study - Lund, Sweden (Gotberg , Olivecrona ) c. MRI Findings A Pilot Study of Rapid Cooling by Cold Saline and Endovascular Cooling Before Reperfusion in Patients With ST-Elevation Myocardial Infarction Circ Cardiovasc Interv published online Aug 24, 2010
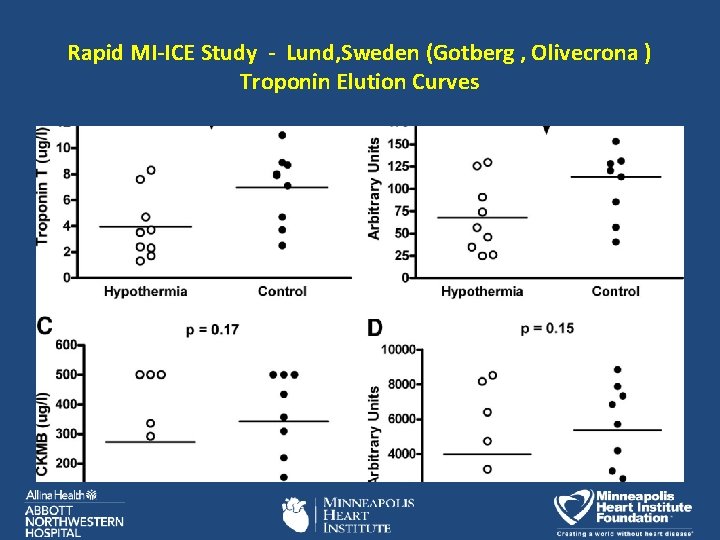
Rapid MI-ICE Study - Lund, Sweden (Gotberg , Olivecrona ) Troponin Elution Curves

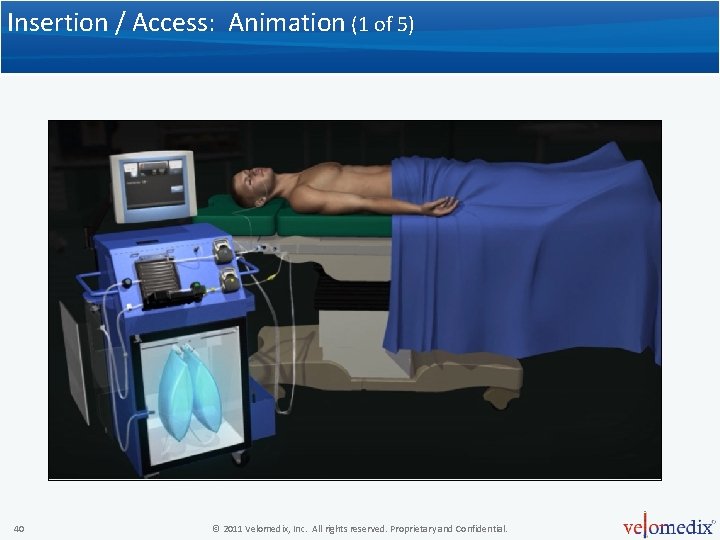
Peritoneal Cooling - Velomedix™, Inc Automated Peritoneal Lavage System (APLS) • Efficient heat exchange • Tight control for cooling and warming • Does not restrict access • Fully automated system

Why Use the Peritoneal Cavity? • Efficient heat exchange – > 50% of total blood flow – Large surface area • Time to target (10 - 15 minutes to 34°C) • Eliminates femoral access interference • Eliminates upper chest and neck area interference
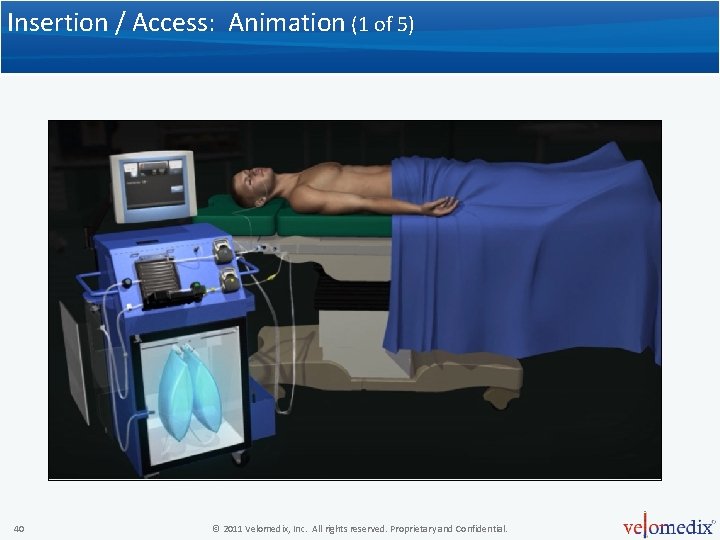
Insertion / Access: Animation (1 of 5) 40 © 2011 Velomedix, Inc. All rights reserved. Proprietary and Confidential.

Insertion / Access: Animation (2 of 5) 41 © 2011 Velomedix, Inc. All rights reserved. Proprietary and Confidential.
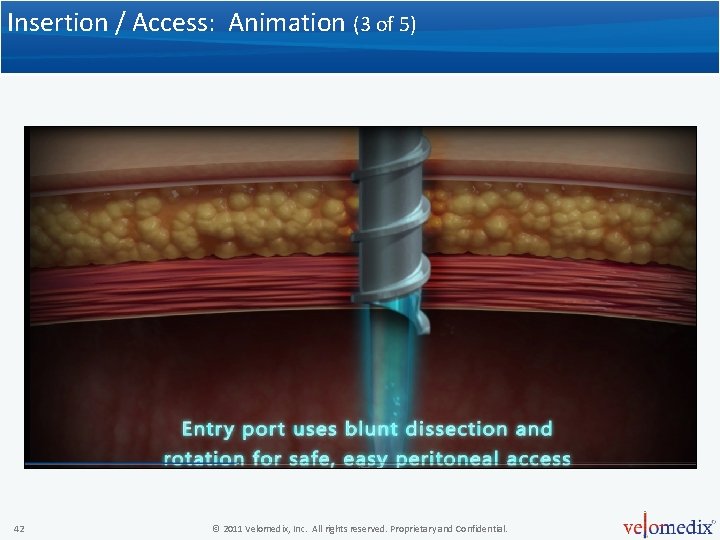
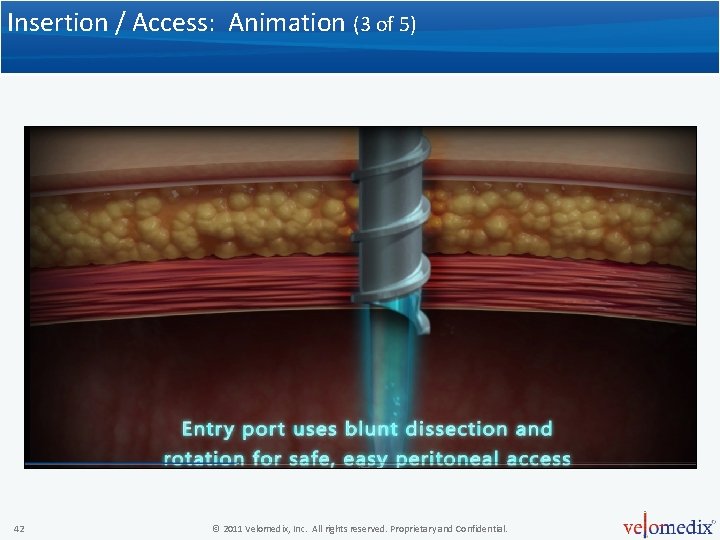
Insertion / Access: Animation (3 of 5) 42 © 2011 Velomedix, Inc. All rights reserved. Proprietary and Confidential.
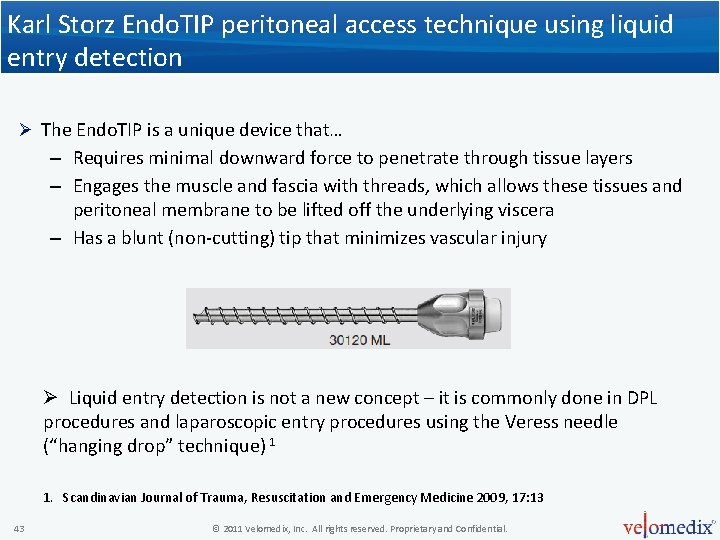
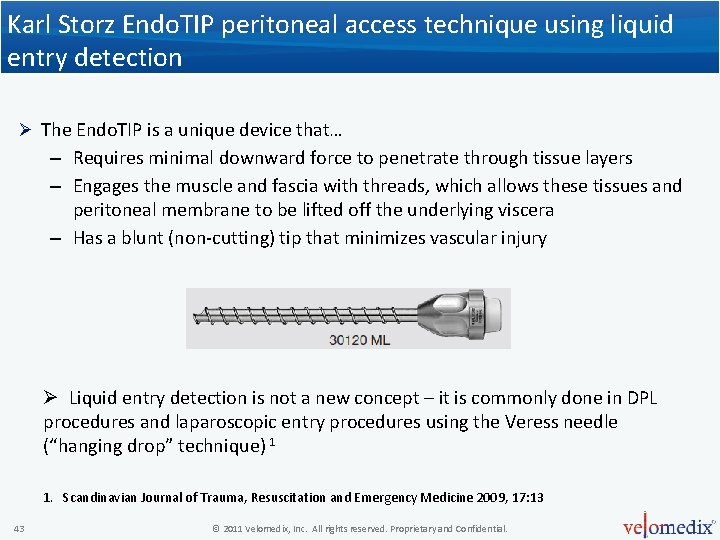
Karl Storz Endo. TIP peritoneal access technique using liquid entry detection Ø The Endo. TIP is a unique device that… – Requires minimal downward force to penetrate through tissue layers – Engages the muscle and fascia with threads, which allows these tissues and peritoneal membrane to be lifted off the underlying viscera – Has a blunt (non-cutting) tip that minimizes vascular injury Ø Liquid entry detection is not a new concept – it is commonly done in DPL procedures and laparoscopic entry procedures using the Veress needle (“hanging drop” technique) 1 1. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2009, 17: 13 43 © 2011 Velomedix, Inc. All rights reserved. Proprietary and Confidential.
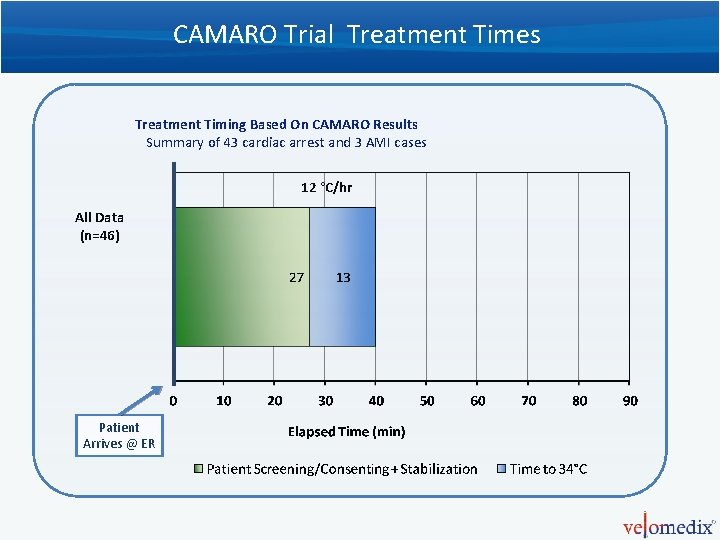
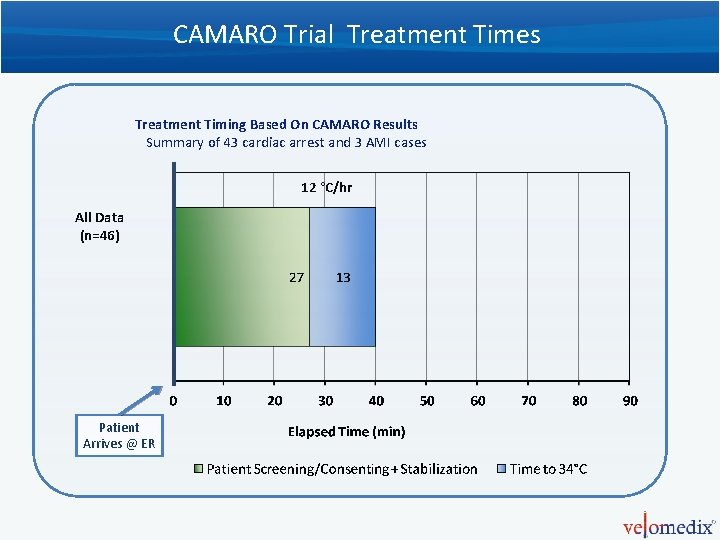
CAMARO Trial Treatment Times Treatment Timing Based On CAMARO Results Summary of 43 cardiac arrest and 3 AMI cases 12 °C/hr All Data (n=46) Patient Arrives @ ER
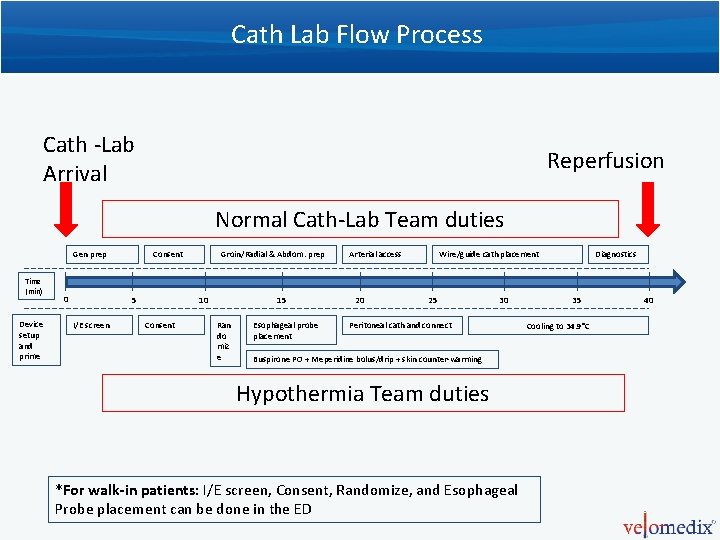
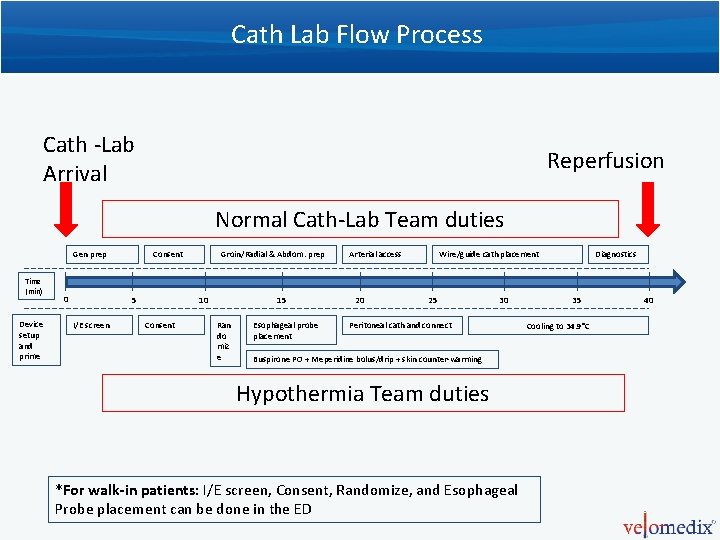
Cath Lab Flow Process Cath -Lab Arrival Reperfusion Normal Cath-Lab Team duties Gen prep Time (min) Device setup and prime 0 Consent 5 I/E screen Groin/Radial & Abdom. prep 10 Consent 15 Ran do miz e Esophageal probe placement Arterial access 20 Wire/guide cath placement 25 30 Peritoneal cath and connect Buspirone PO + Meperidine bolus/drip + skin counter-warming Hypothermia Team duties *For walk-in patients: I/E screen, Consent, Randomize, and Esophageal Probe placement can be done in the ED Diagnostics 35 Cooling to 34. 9°C 40
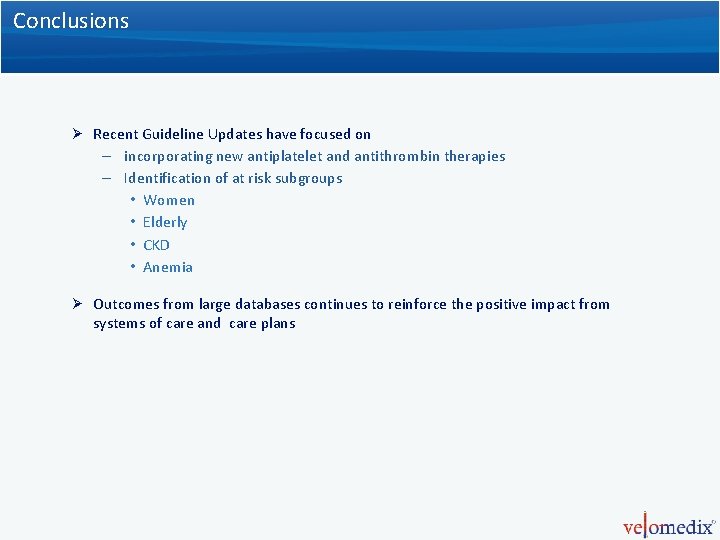
Conclusions Ø Recent Guideline Updates have focused on – incorporating new antiplatelet and antithrombin therapies – Identification of at risk subgroups • Women • Elderly • CKD • Anemia Ø Outcomes from large databases continues to reinforce the positive impact from systems of care and care plans
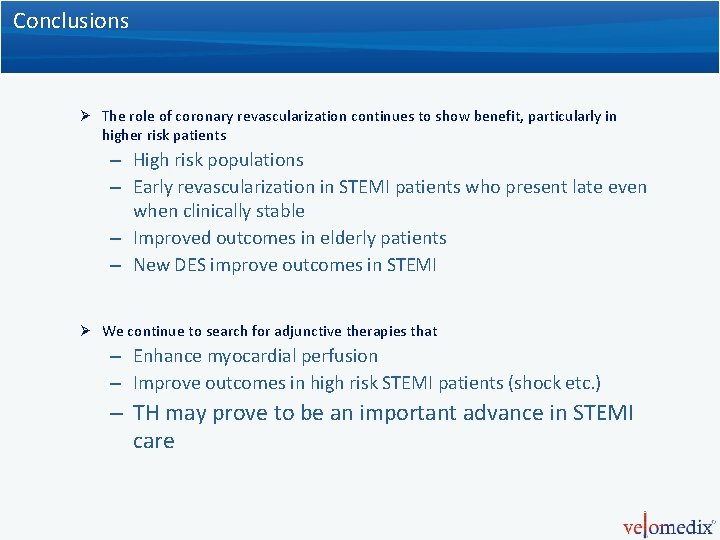
Conclusions Ø The role of coronary revascularization continues to show benefit, particularly in higher risk patients – High risk populations – Early revascularization in STEMI patients who present late even when clinically stable – Improved outcomes in elderly patients – New DES improve outcomes in STEMI Ø We continue to search for adjunctive therapies that – Enhance myocardial perfusion – Improve outcomes in high risk STEMI patients (shock etc. ) – TH may prove to be an important advance in STEMI care

Thank You
 Tct 2013
Tct 2013 Tct scan
Tct scan Difference between frostbite and trench foot
Difference between frostbite and trench foot Tct
Tct Temperature hypothermia
Temperature hypothermia Hypothermia suffix
Hypothermia suffix Tct congress 2018
Tct congress 2018 Nstemi
Nstemi Pvc bigemini
Pvc bigemini Ace inhibitors in stemi
Ace inhibitors in stemi Stemi chain of survival
Stemi chain of survival Complicated plaque
Complicated plaque Reem alzahrani
Reem alzahrani Stemi
Stemi Stemi imposters
Stemi imposters Stemi
Stemi Dtu stemi trial
Dtu stemi trial Crt monitor
Crt monitor Nrt vs crt
Nrt vs crt Introduction of cro
Introduction of cro Assessment process in special education
Assessment process in special education Crt diagram
Crt diagram Sentinel device
Sentinel device Example of nrt and crt
Example of nrt and crt Goldmemory test
Goldmemory test Crt micron manuale italiano
Crt micron manuale italiano Difference between crt and dvst
Difference between crt and dvst Crts ryles tube
Crts ryles tube Lcd led crt
Lcd led crt Purdue owl literary theory
Purdue owl literary theory Crt
Crt Crt display technology
Crt display technology Monitor crt partes
Monitor crt partes Pokupka
Pokupka Budowa kineskopu
Budowa kineskopu Crt 2010
Crt 2010 Uses crt;
Uses crt; Crt roanne
Crt roanne Critical race theory curriculum examples
Critical race theory curriculum examples Plasma panel display in computer graphics
Plasma panel display in computer graphics Salivary reductase test
Salivary reductase test Crt monitor aufbau
Crt monitor aufbau Angel
Angel Primary output device in a graphics system
Primary output device in a graphics system Crt
Crt Ventajas del monitor crt
Ventajas del monitor crt Pengertian monitor crt
Pengertian monitor crt Uses crt;
Uses crt; Crt 2017
Crt 2017