TCT 2011 PROFI A Prospective Randomized Trial of

- Slides: 21
TCT 2011 PROFI: A Prospective, Randomized Trial of Proximal Balloon Occlusion vs. Filter Embolic Protection in Patients Undergoing Carotid Stenting Klaudija Bijuklic Fadija Hazizi, Andreas Wandler, Joachim Schofer Medical Care Center Prof. Mathey, Prof. Schofer Hamburg University Cardiovascular Center Germany
Disclosure Statement of Financial Interest I, Klaudija Bijuklic, DO NOT have a financial interest/arrangement or affiliation with one or more organizations that could be perceived as a real or apparent conflict of interest in the context of the subject of this presentation.
Background Randomized trials revealed a higher periprocedural stroke rate after filter protected Carotid Artery Stenting (CAS) compared to carotid endarterectomy. Brott TG et al. N Engl J Med 2010; 363: 11 -23 Mas JL et al. Stroke 2004; 35: 18 -20
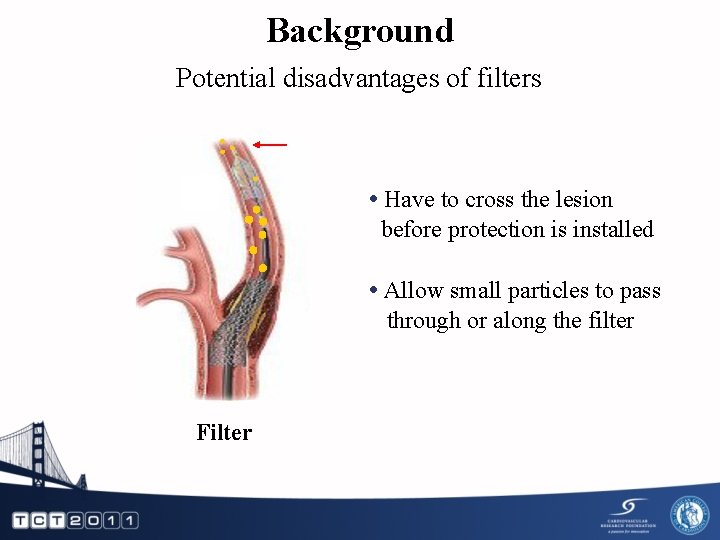
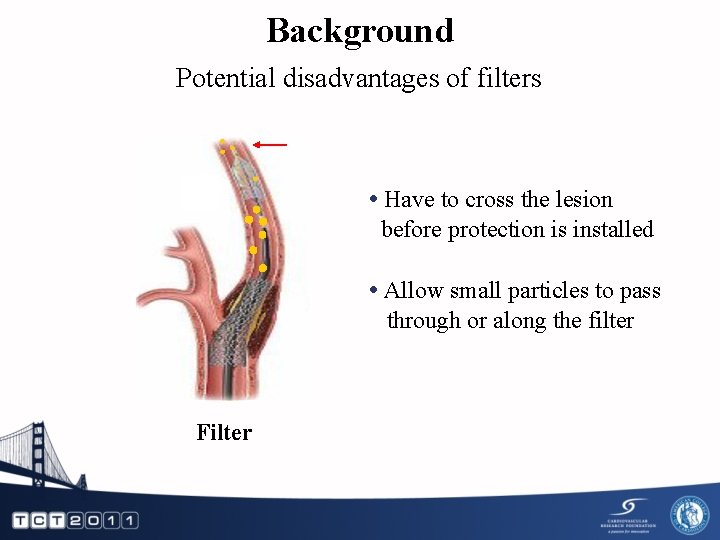
Background Potential disadvantages of filters • Have to cross the lesion before protection is installed • Allow small particles to pass through or along the filter Filter
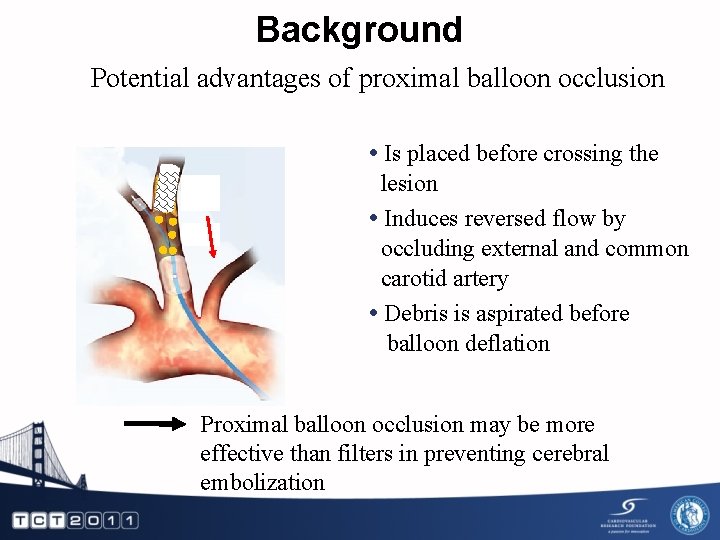
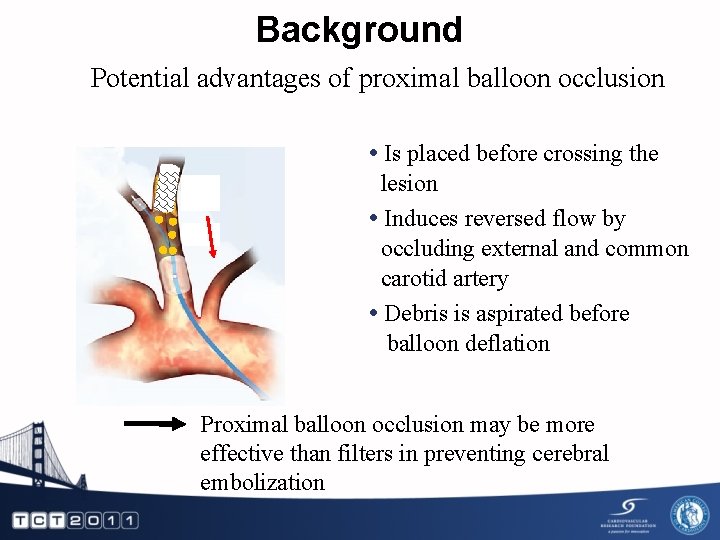
Background Potential advantages of proximal balloon occlusion • Is placed before crossing the lesion • Induces reversed flow by occluding external and common carotid artery • Debris is aspirated before balloon deflation Proximal balloon occlusion may be more effective than filters in preventing cerebral embolization
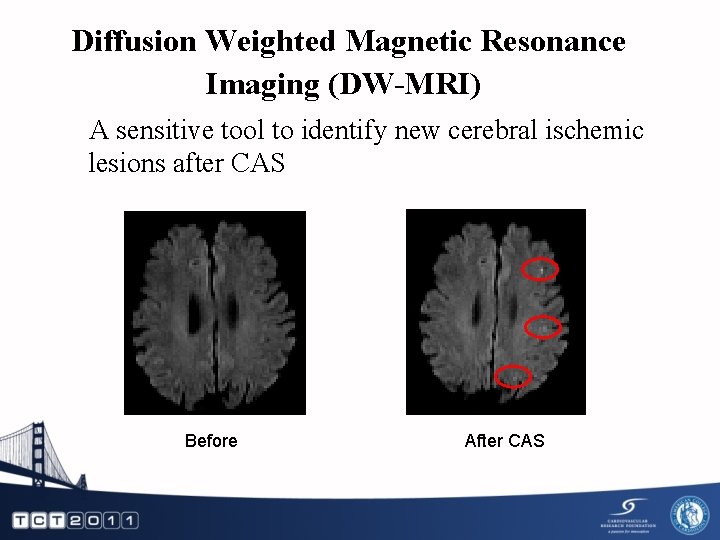
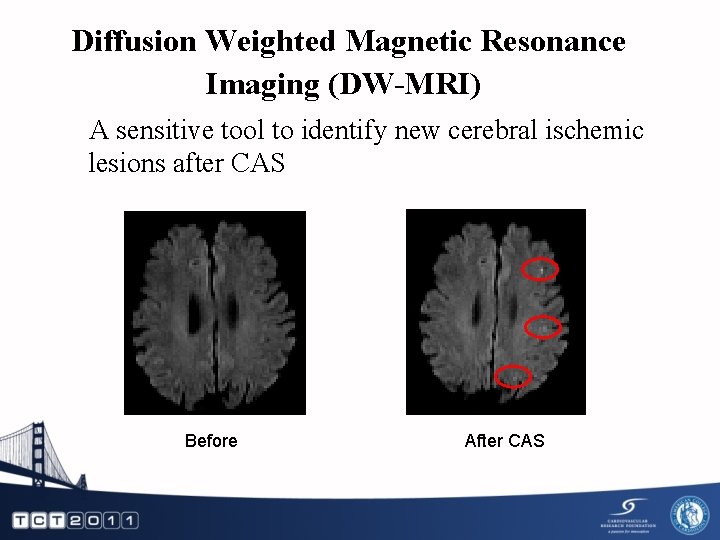
Diffusion Weighted Magnetic Resonance Imaging (DW-MRI) A sensitive tool to identify new cerebral ischemic lesions after CAS Before After CAS
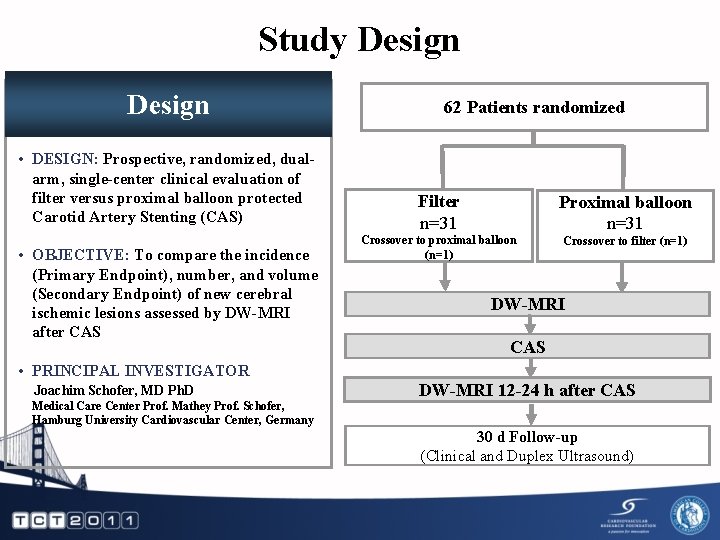
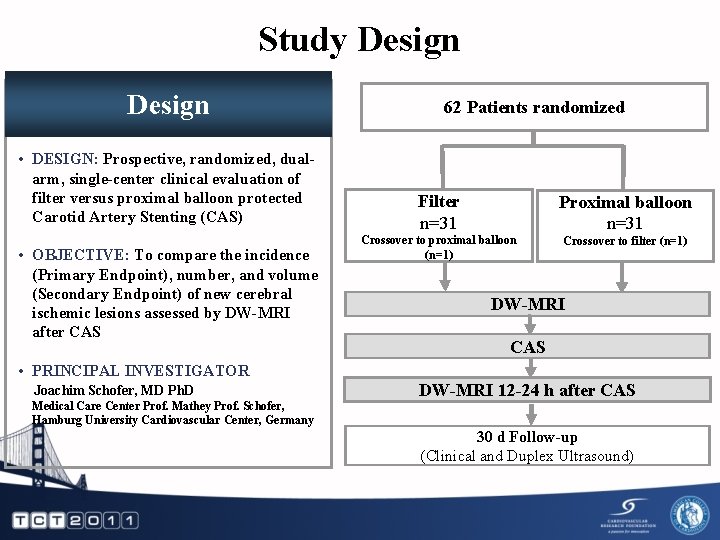
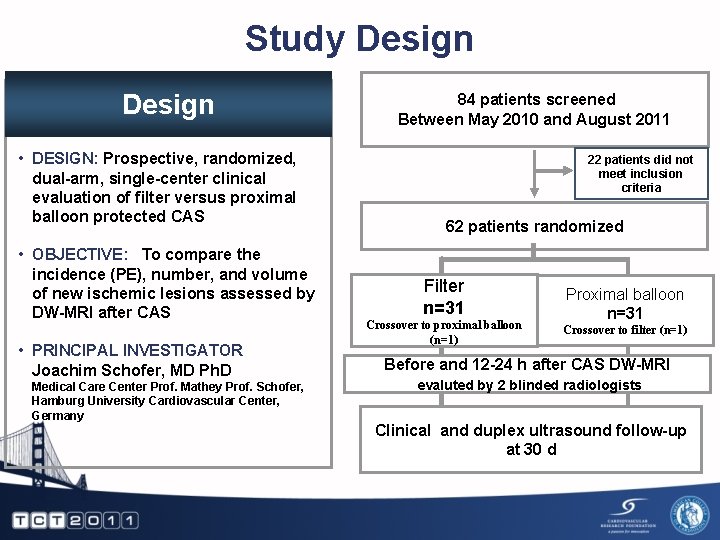
Study Design • DESIGN: Prospective, randomized, dualarm, single-center clinical evaluation of filter versus proximal balloon protected Carotid Artery Stenting (CAS) • OBJECTIVE: To compare the incidence (Primary Endpoint), number, and volume (Secondary Endpoint) of new cerebral ischemic lesions assessed by DW-MRI after CAS 62 Patients randomized Filter n=31 Proximal balloon n=31 Crossover to proximal balloon (n=1) Crossover to filter (n=1) DW-MRI CAS • PRINCIPAL INVESTIGATOR Joachim Schofer, MD Ph. D Medical Care Center Prof. Mathey Prof. Schofer, Hamburg University Cardiovascular Center, Germany DW-MRI 12 -24 h after CAS 30 d Follow-up (Clinical and Duplex Ultrasound)
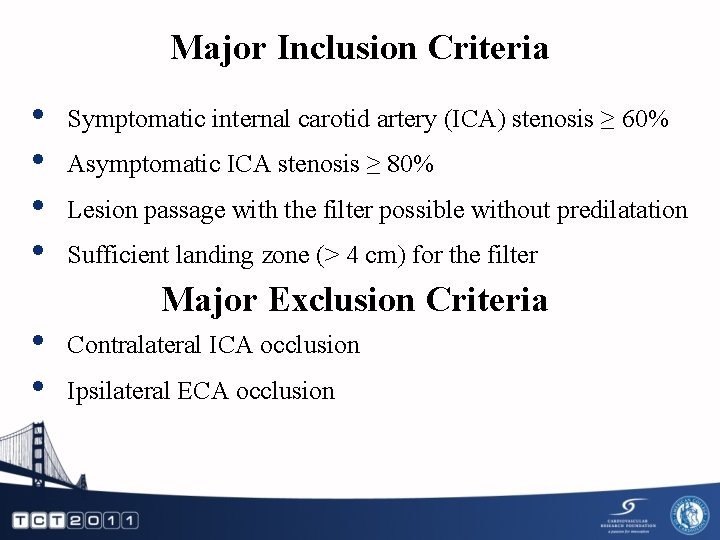
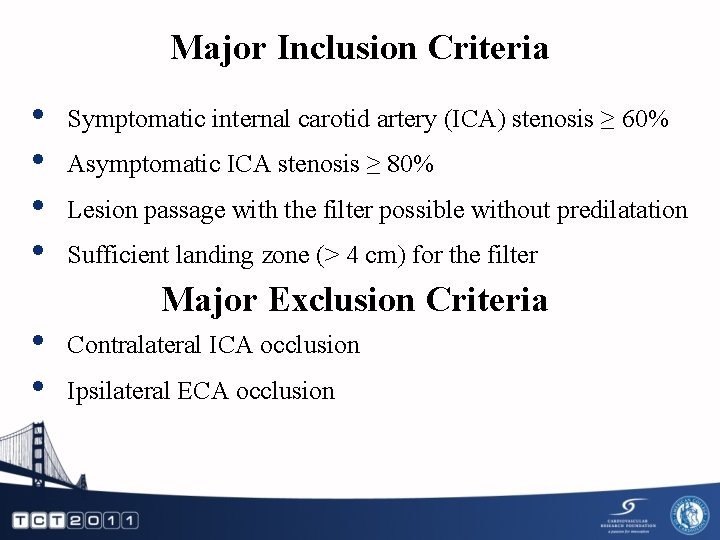
Major Inclusion Criteria • • • Symptomatic internal carotid artery (ICA) stenosis ≥ 60% Asymptomatic ICA stenosis ≥ 80% Lesion passage with the filter possible without predilatation Sufficient landing zone (> 4 cm) for the filter Major Exclusion Criteria Contralateral ICA occlusion Ipsilateral ECA occlusion
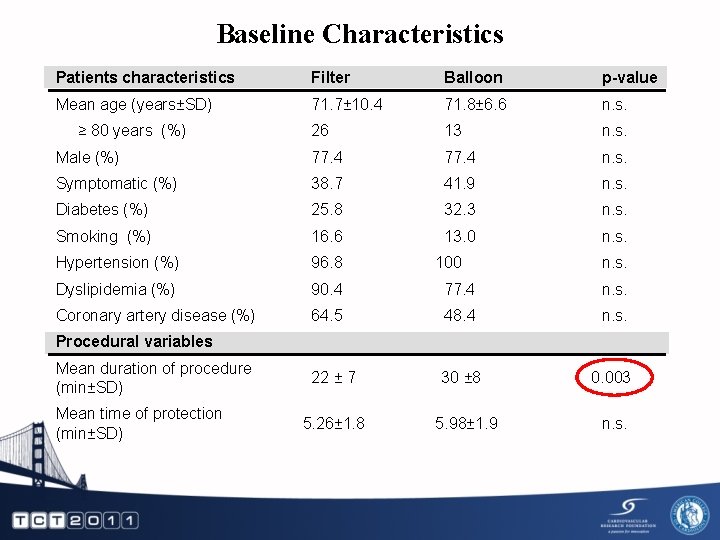
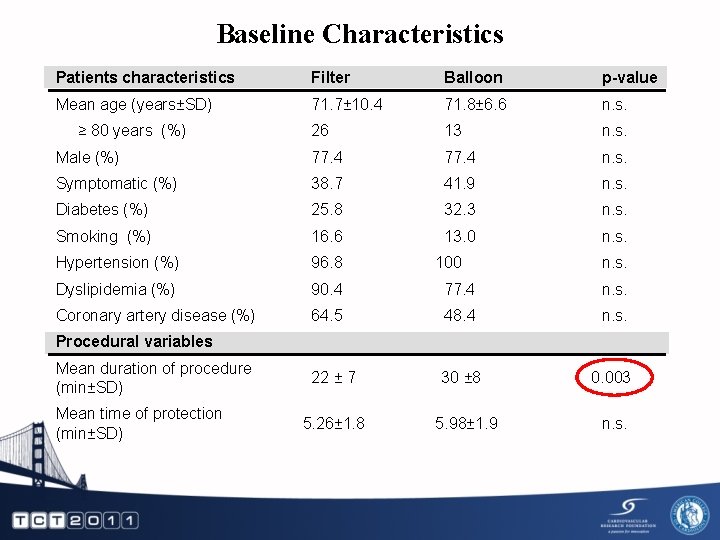
Baseline Characteristics Patients characteristics Filter Balloon p-value Mean age (years±SD) 71. 7± 10. 4 71. 8± 6. 6 n. s. 26 13 n. s. Male (%) 77. 4 n. s. Symptomatic (%) 38. 7 41. 9 n. s. Diabetes (%) 25. 8 32. 3 n. s. Smoking (%) 16. 6 13. 0 n. s. Hypertension (%) 96. 8 Dyslipidemia (%) 90. 4 77. 4 n. s. Coronary artery disease (%) 64. 5 48. 4 n. s. 22 ± 7 30 ± 8 0. 003 ≥ 80 years (%) 100 n. s. Procedural variables Mean duration of procedure (min±SD) Mean time of protection (min±SD) 5. 26± 1. 8 5. 98± 1. 9 n. s.
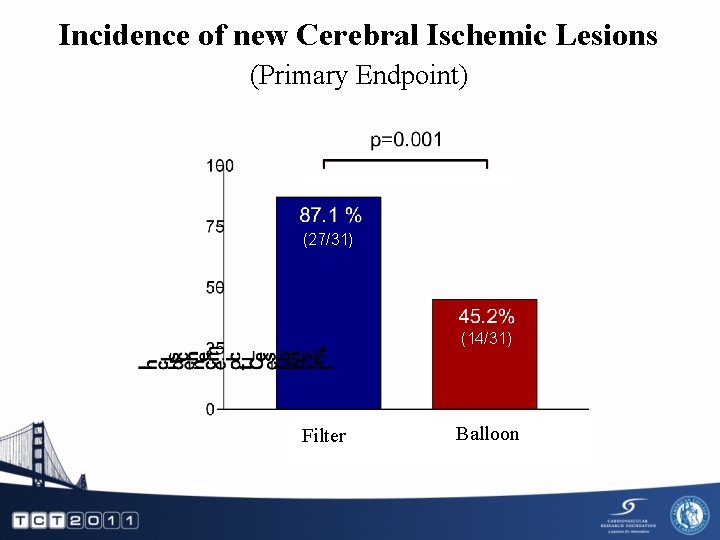
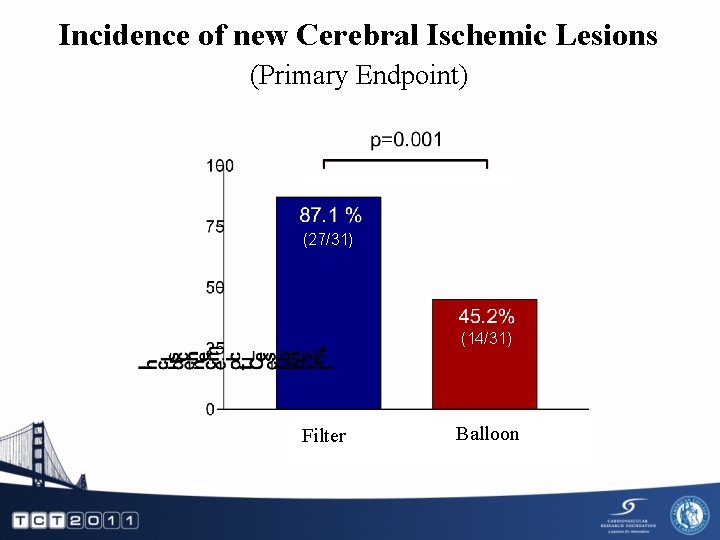
Incidence of new Cerebral Ischemic Lesions (Primary Endpoint) (27/31) (14/31) Filter Balloon
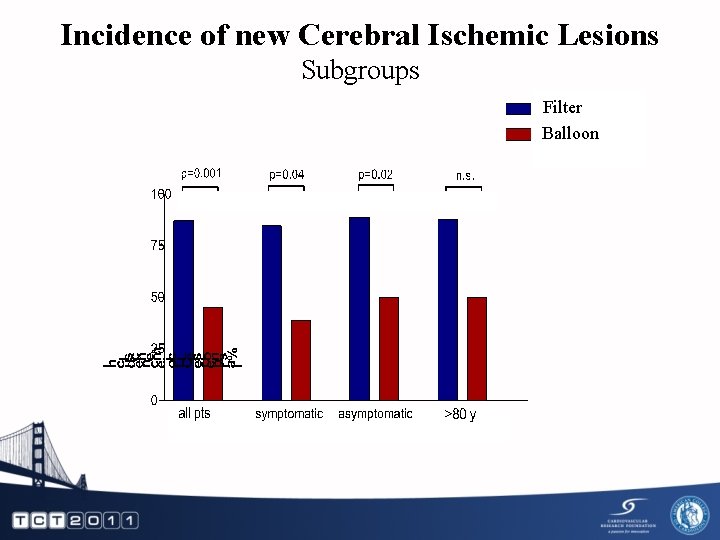
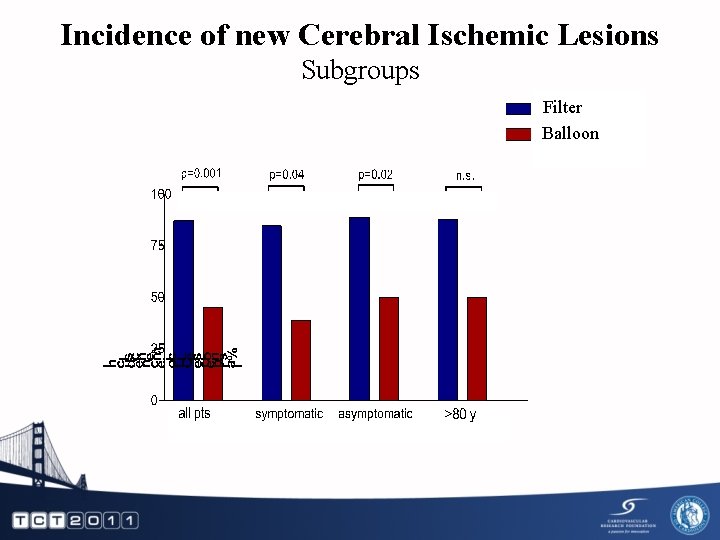
Incidence of new Cerebral Ischemic Lesions Subgroups Filter Balloon 12
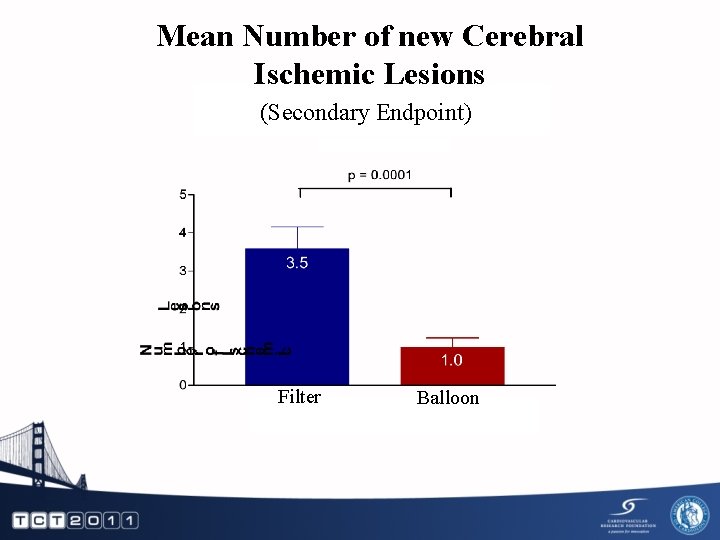
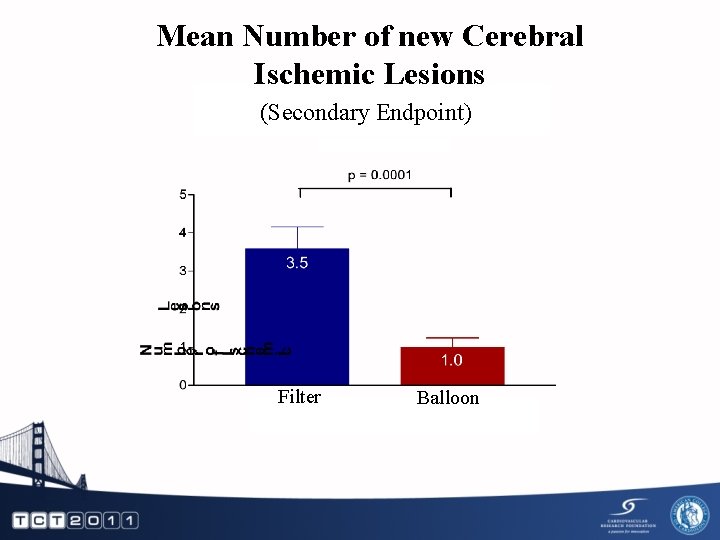
Mean Number of new Cerebral Ischemic Lesions (Secondary Endpoint) Filter Balloon
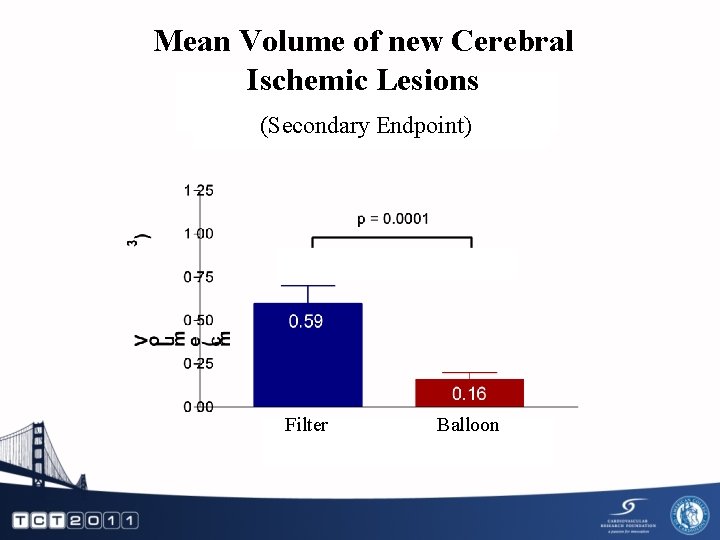
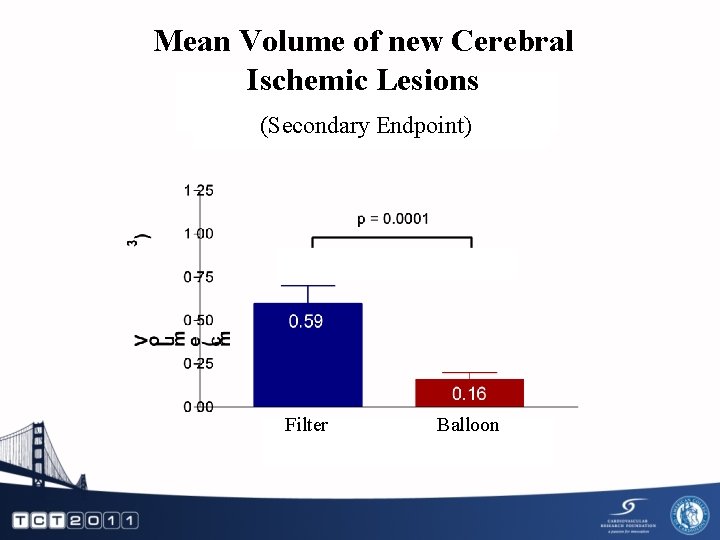
Mean Volume of new Cerebral Ischemic Lesions (Secondary Endpoint) Filter Balloon
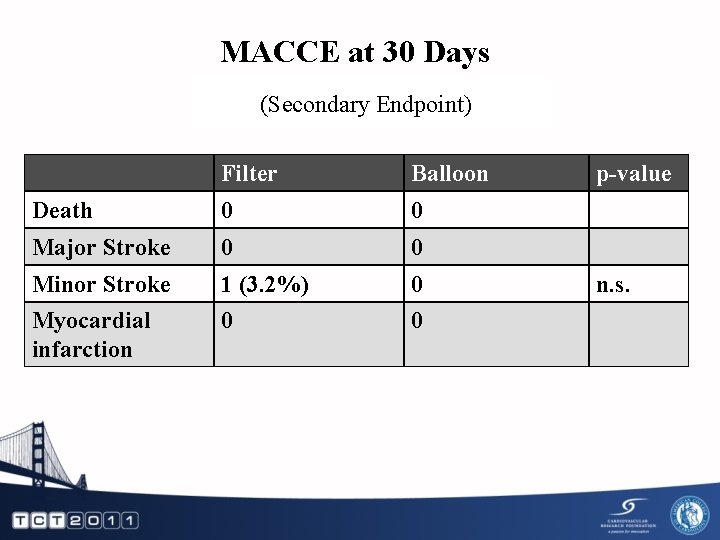
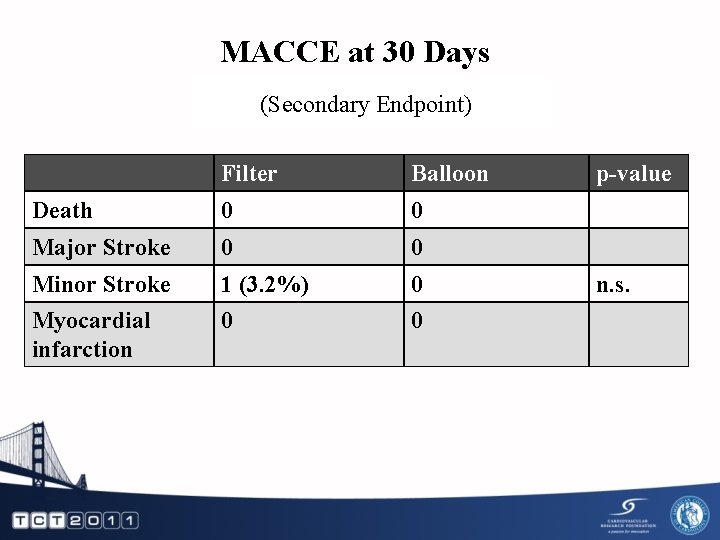
MACCE at 30 Days (Secondary Endpoint) Filter Balloon Death 0 0 Major Stroke 0 0 Minor Stroke 1 (3. 2%) 0 Myocardial infarction 0 0 p-value n. s.
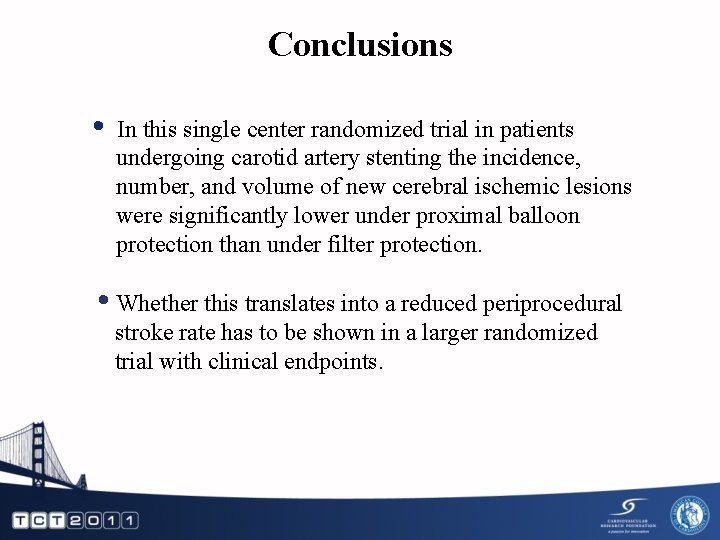
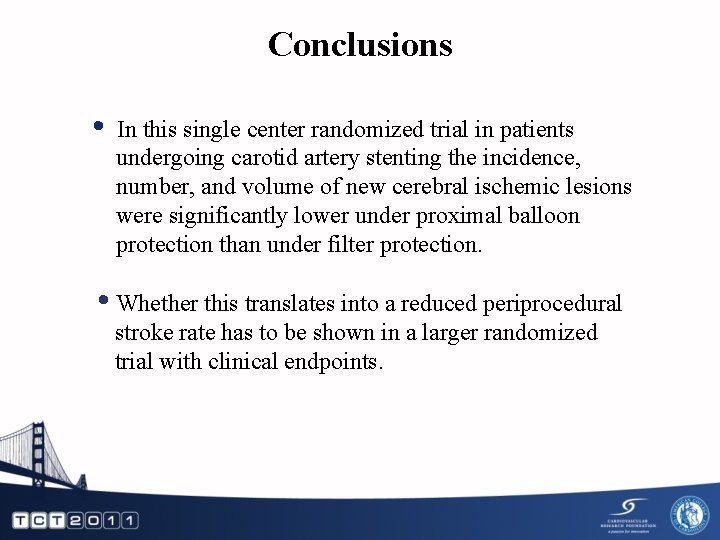
Conclusions • In this single center randomized trial in patients undergoing carotid artery stenting the incidence, number, and volume of new cerebral ischemic lesions were significantly lower under proximal balloon protection than under filter protection. • Whether this translates into a reduced periprocedural stroke rate has to be shown in a larger randomized trial with clinical endpoints.

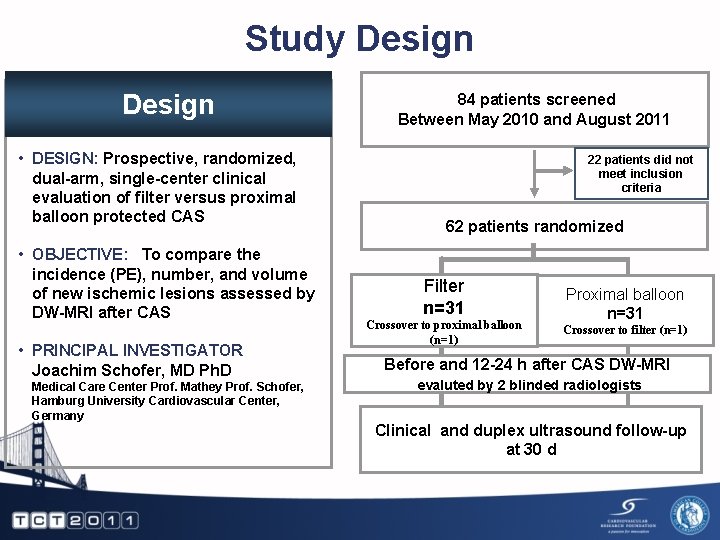
Study Design • DESIGN: Prospective, randomized, dual-arm, single-center clinical evaluation of filter versus proximal balloon protected CAS • OBJECTIVE: To compare the incidence (PE), number, and volume of new ischemic lesions assessed by DW-MRI after CAS • PRINCIPAL INVESTIGATOR Joachim Schofer, MD Ph. D Medical Care Center Prof. Mathey Prof. Schofer, Hamburg University Cardiovascular Center, Germany 84 patients screened Between May 2010 and August 2011 22 patients did not meet inclusion criteria 62 patients randomized Filter n=31 Crossover to proximal balloon (n=1) Proximal balloon n=31 Crossover to filter (n=1) Before and 12 -24 h after CAS DW-MRI evaluted by 2 blinded radiologists Clinical and duplex ultrasound follow-up at 30 d
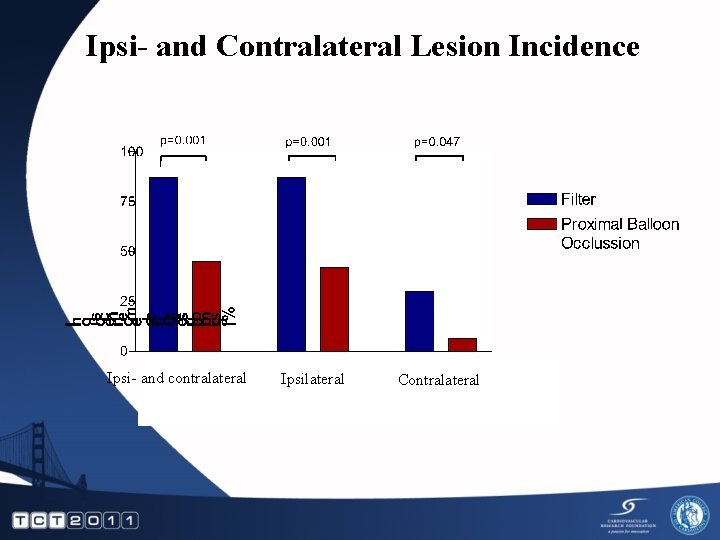
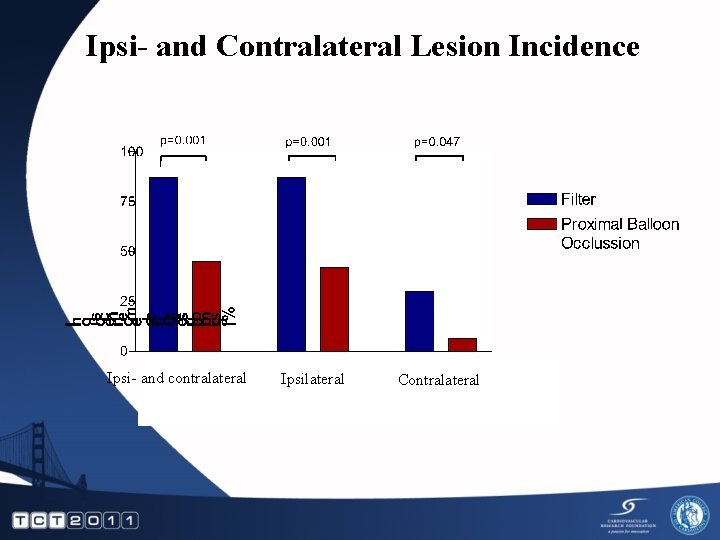
Ipsi- and Contralateral Lesion Incidence Ipsi- and contralateral Ipsilateral Contralateral
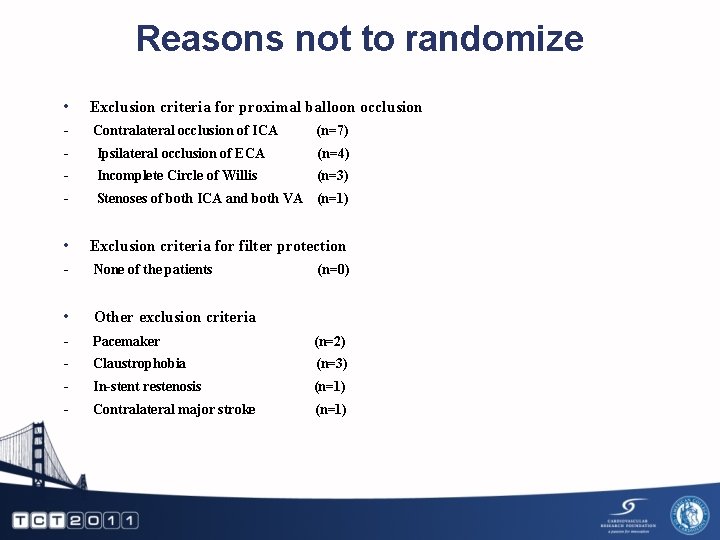
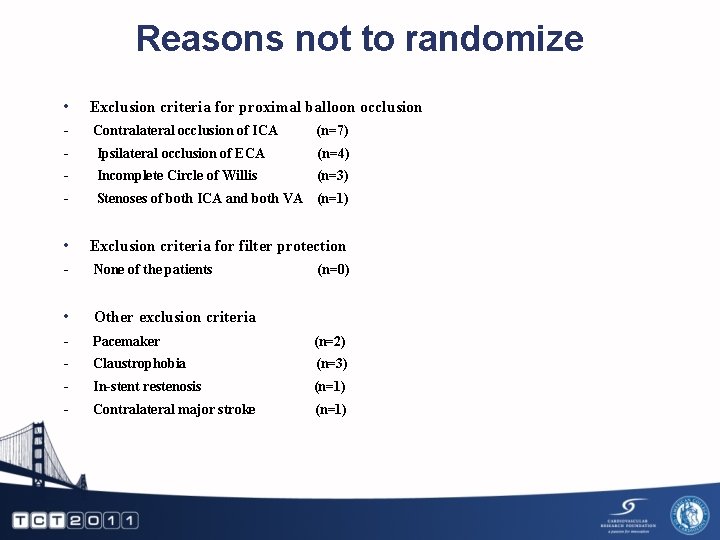
Reasons not to randomize • Exclusion criteria for proximal balloon occlusion - Contralateral occlusion of ICA (n=7) Ipsilateral occlusion of ECA (n=4) Incomplete Circle of Willis (n=3) Stenoses of both ICA and both VA (n=1) • Exclusion criteria for filter protection - None of the patients • Other exclusion criteria - Pacemaker (n=2) Claustrophobia (n=3) In-stent restenosis (n=1) Contralateral major stroke (n=1) (n=0)
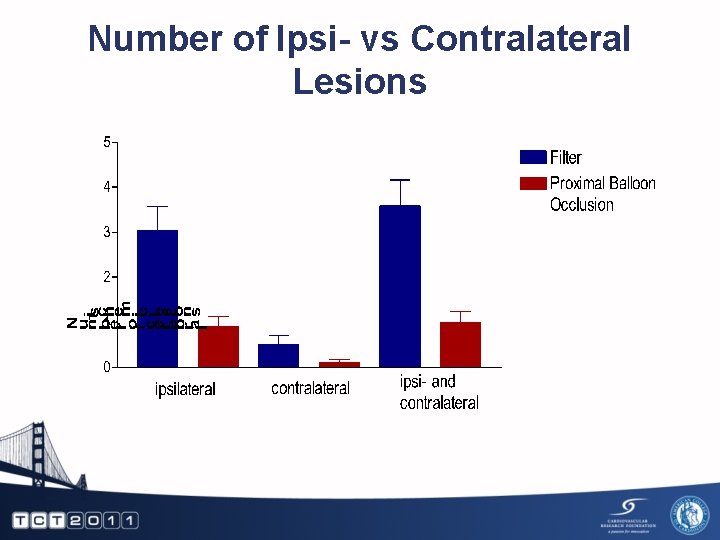
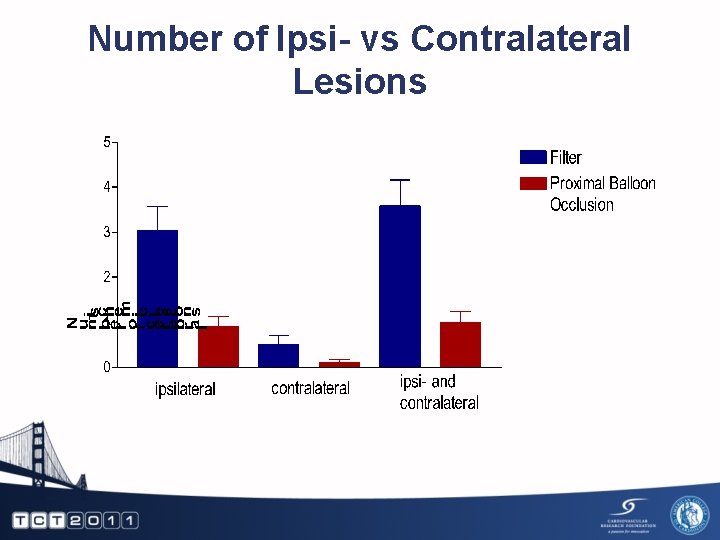
Number of Ipsi- vs Contralateral Lesions
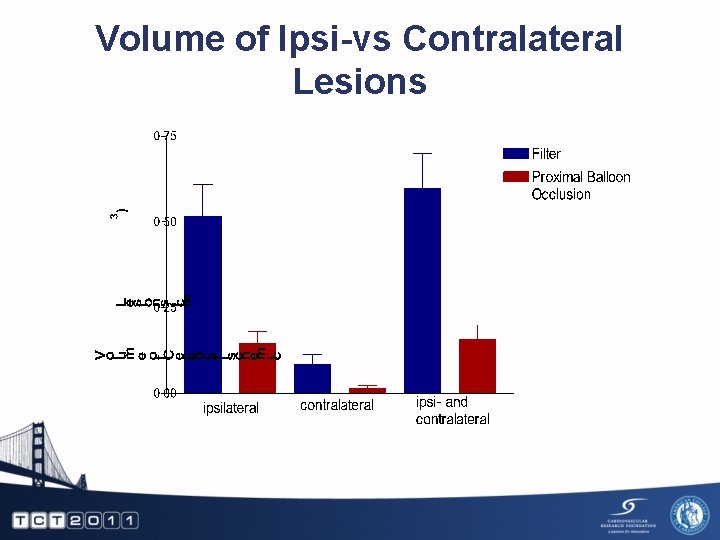
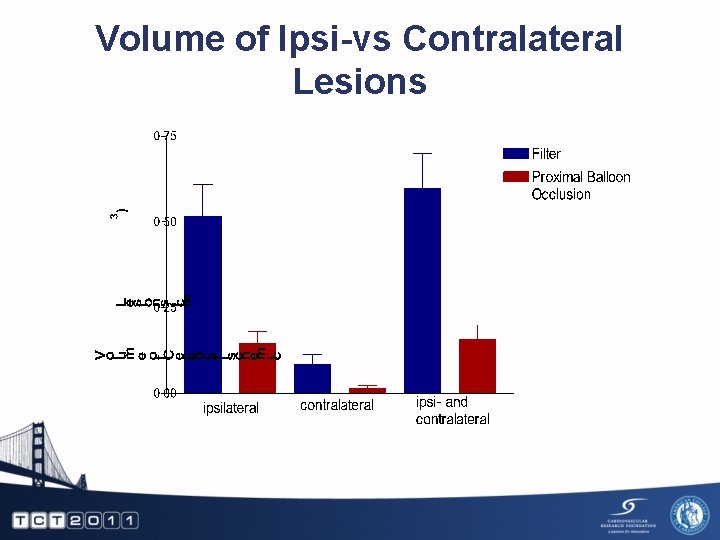
Volume of Ipsi-vs Contralateral Lesions