TBI Neuroanatomy of TBA Primary Effects Diffuse Axonal
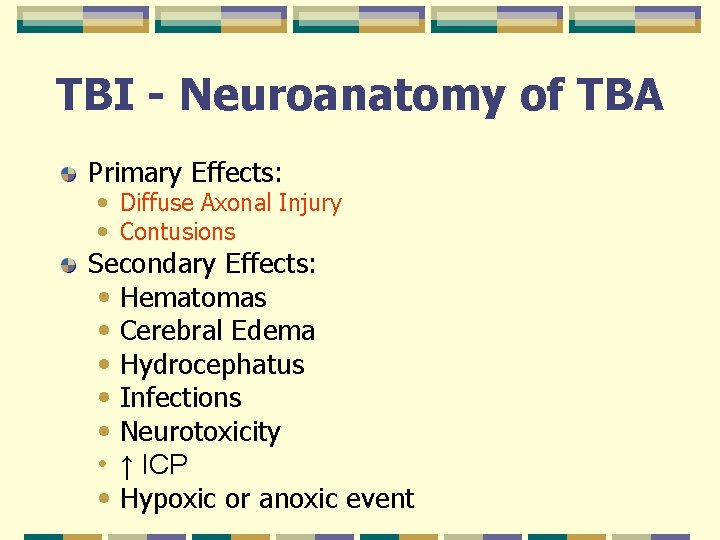
TBI - Neuroanatomy of TBA Primary Effects: • Diffuse Axonal Injury • Contusions Secondary Effects: • Hematomas • Cerebral Edema • Hydrocephatus • Infections • Neurotoxicity • ↑ ICP • Hypoxic or anoxic event

Prediction of Outcome after TBI Injury severity Duration of Post-Traumatic Amnesia Type of damage (contusion vs. DAI) Premorbid intelligence Alcohol intoxication at time of injury Premorbid OBS or history of substance abuse Premorbid psychiatric/behavioral history
TBI - Risk Factors for TBI Men 2: 1 15 -24 Years Old Alcohol Trauma

TBI - Personality Changes – Common Worsening of premorbid behavioral traits Childishness Disinhibition Social inappropriateness Restlessness Emotional lability Decreased social contact Less spontaneity/poverty of interest Decreased social interaction
TBI – Executive Function Changes – Decreased Mental Flexibility Decreased capacity to: • Concentrate • Use language • Abstract calculate • Reason remember • Plan • Access information
Post Concussion Syndrome and TBI Criteria: • Any period of LOC • Any loss of memory • Any alteration in mental status • Mild focal neurological deficits
Post Concussion and TBI Syndrome Somatic: HA, dizziness, fatigue, insomnia Cognitive: memory deficits, impaired concentration Perceptual: tinnitus, noise sensitivity, light sensitivity Emotional: depression, anxiety, irritability Other: decreased reasoning, information processing, verbal learning, attention
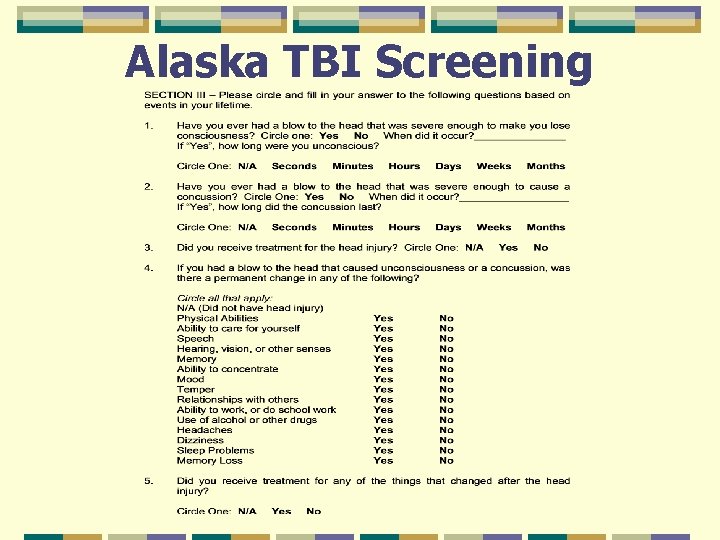
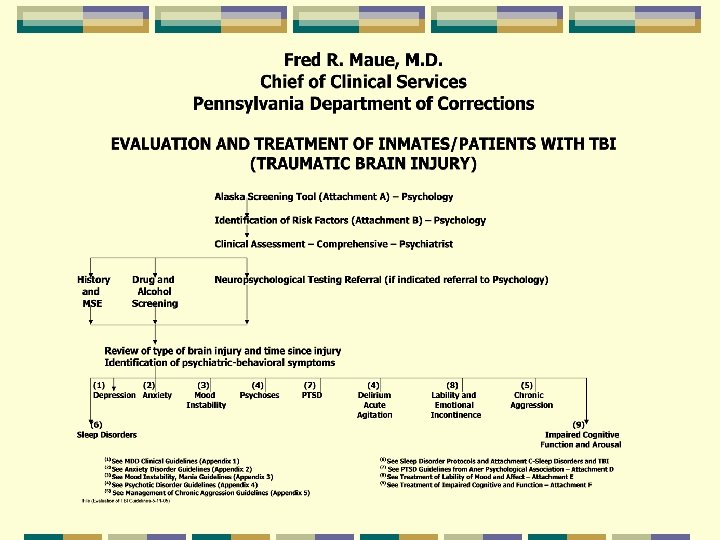
Alaska TBI Screening
TBI - Assessment Neuropsychological Testing: • Attention • Concentration • Memory • Verbal Capacity • Executive Functions: • Problem Solving • Reasoning Abilities • Abstract Thinking • Planning
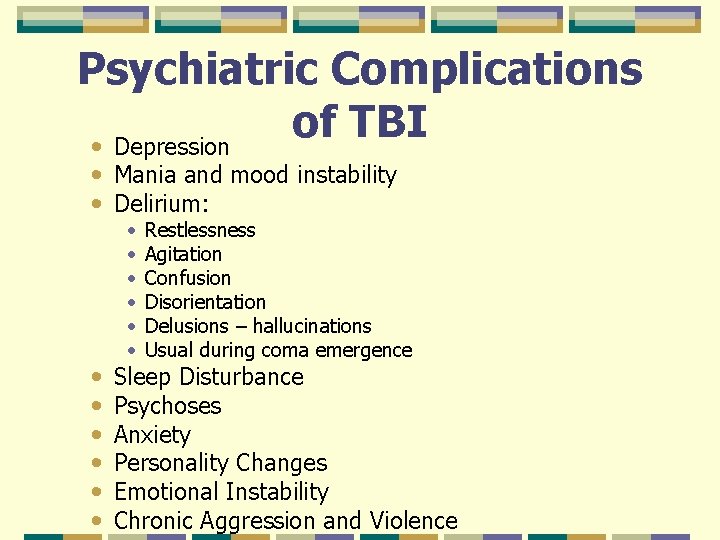
Psychiatric Complications of TBI • Depression • Mania and mood instability • Delirium: • • • Restlessness Agitation Confusion Disorientation Delusions – hallucinations Usual during coma emergence Sleep Disturbance Psychoses Anxiety Personality Changes Emotional Instability Chronic Aggression and Violence
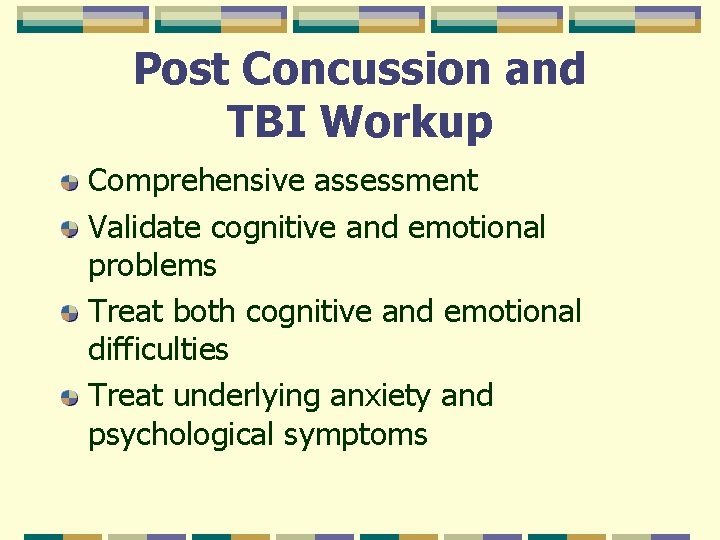
Post Concussion and TBI Workup Comprehensive assessment Validate cognitive and emotional problems Treat both cognitive and emotional difficulties Treat underlying anxiety and psychological symptoms
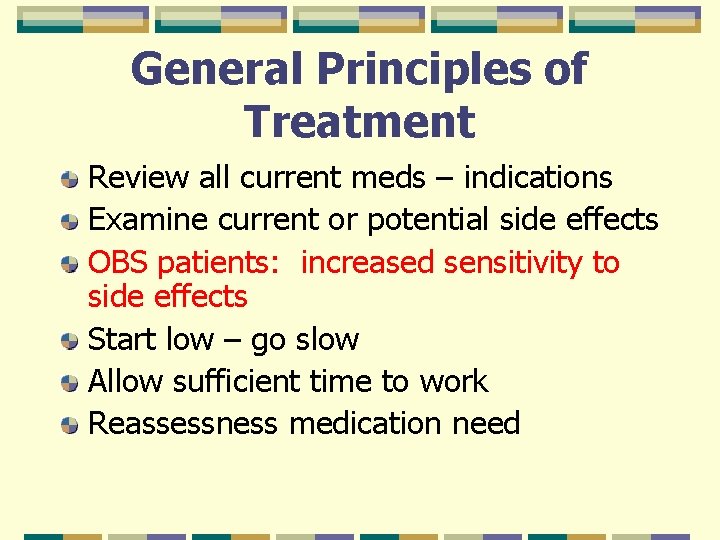
General Principles of Treatment Review all current meds – indications Examine current or potential side effects OBS patients: increased sensitivity to side effects Start low – go slow Allow sufficient time to work Reassessness medication need
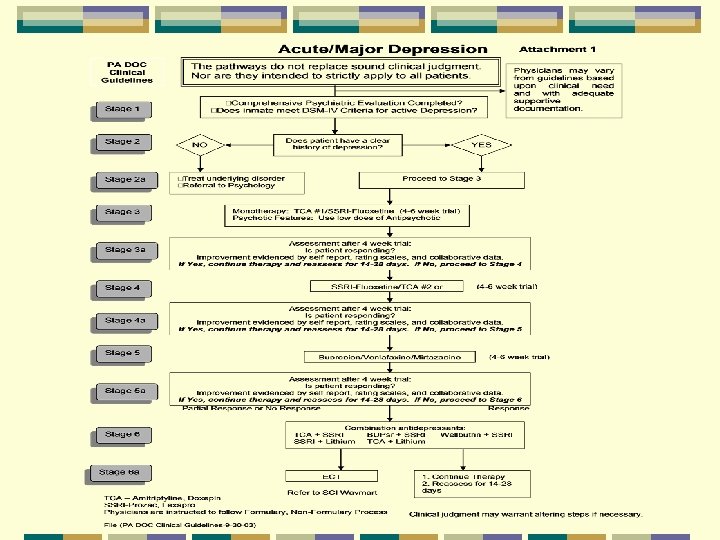
TBI - Treatment of Depression See Depression Guidelines for MDD and Bipolar Depression Tricyclic anticholinergic effects may impair cognition
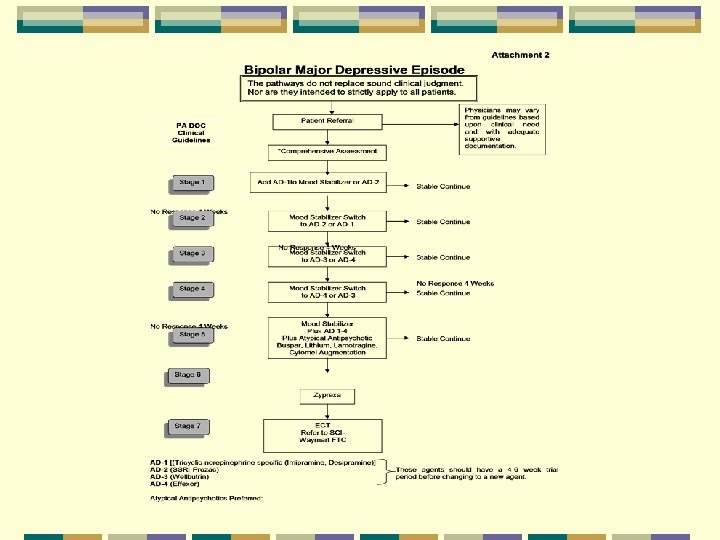
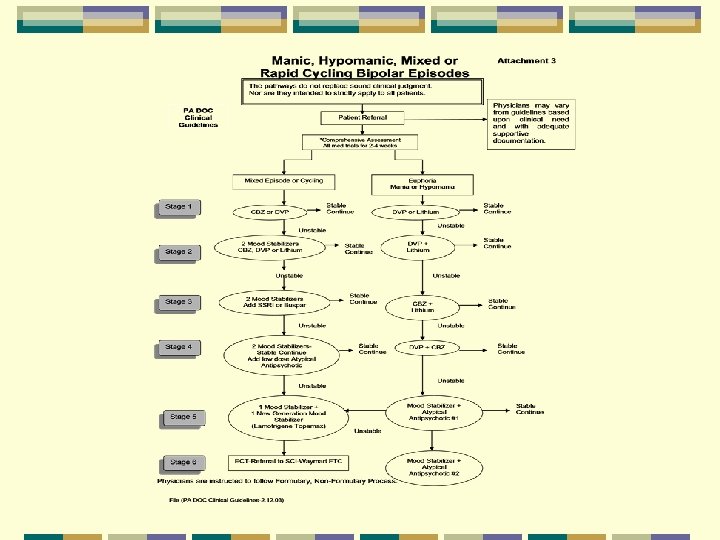
TBI - Treatment of Mood Instability – Mania, Hypomania, Mixed See Treatment Guidelines. Lithium levels – keep level less than 1. 0
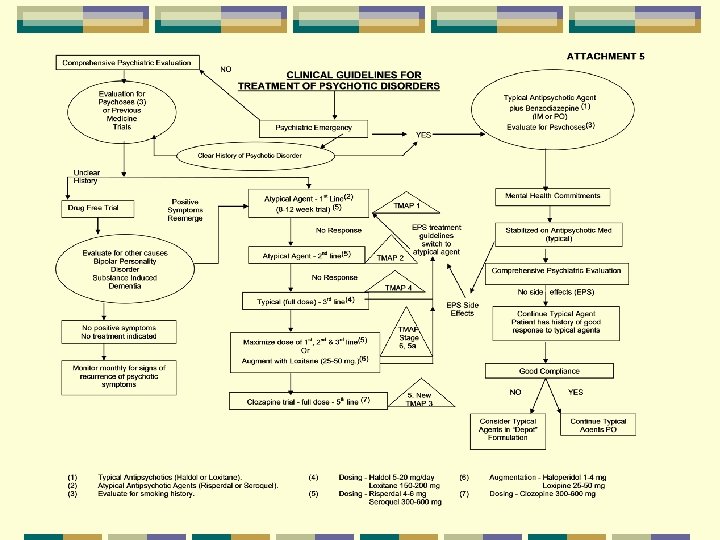
TBI - Treatment of Psychoses See Clinical Guidelines for Treatment of Psychoses. Increased sensitivity to EPS Atypicals – less EPS potential, greater metabolic side effects, OHD, CVA Risperdal – higher EPS
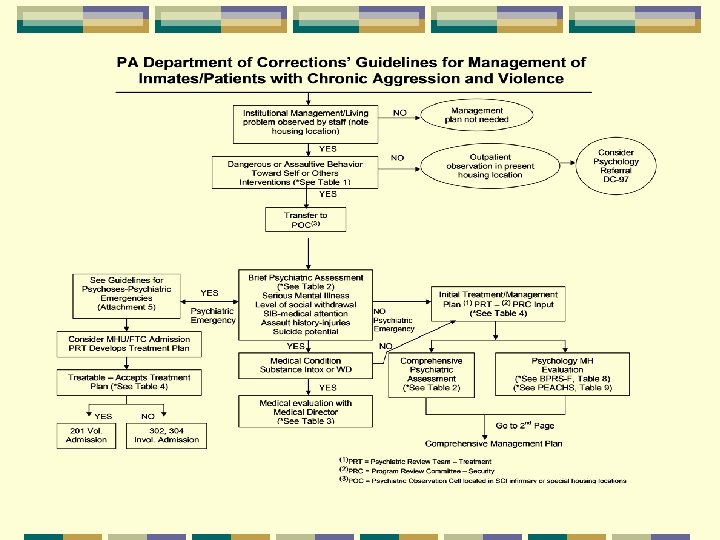
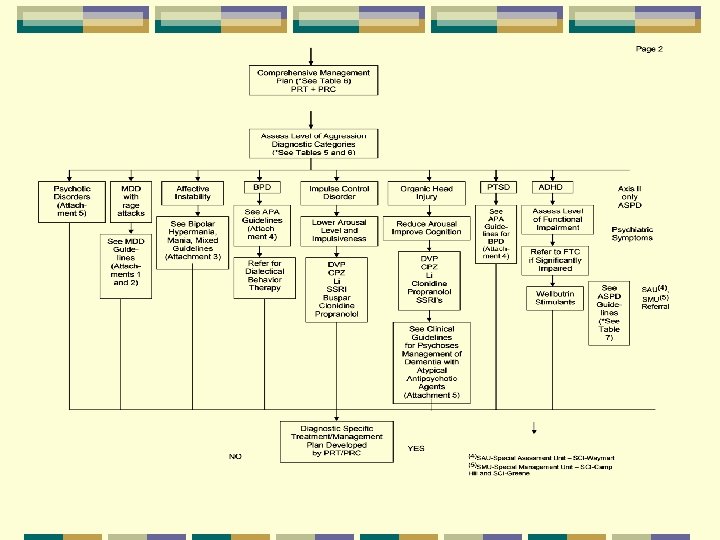
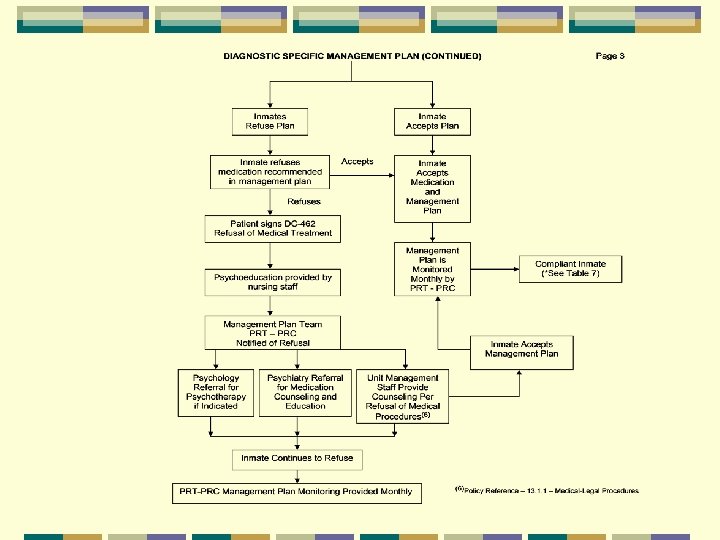
TBI -Treatment of Chronic Aggression – Episodic Dyscontrol See Management of Chronic Aggression Guidelines.
TBI - Treatment of Lability of Mood and Affect Emotional incontinence Antidepressants are best choice: • Fluoxetine (20 -80 mg/d) – Prozac • Sertraline (25 -150 mg/d) – Zoloft • Nortriptyline (50 -150 mg/d) – Pamelor • Effexor (150 -450 mg/day) – higher doses needed to get NE effect
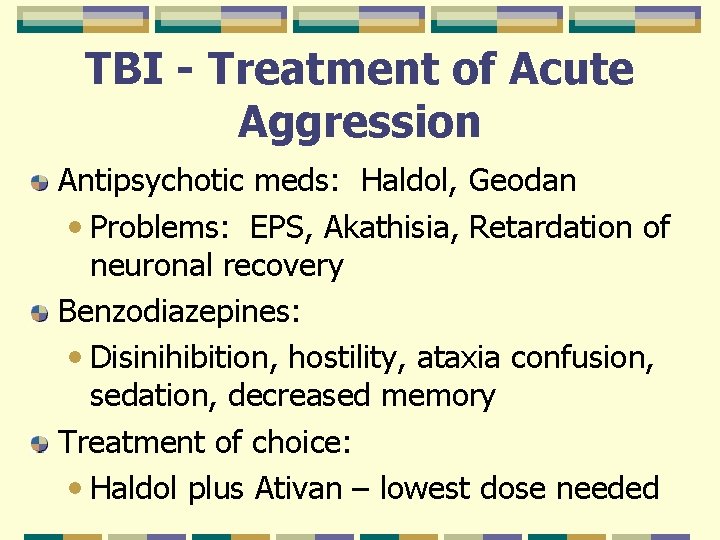
TBI - Treatment of Acute Aggression Antipsychotic meds: Haldol, Geodan • Problems: EPS, Akathisia, Retardation of neuronal recovery Benzodiazepines: • Disinihibition, hostility, ataxia confusion, sedation, decreased memory Treatment of choice: • Haldol plus Ativan – lowest dose needed
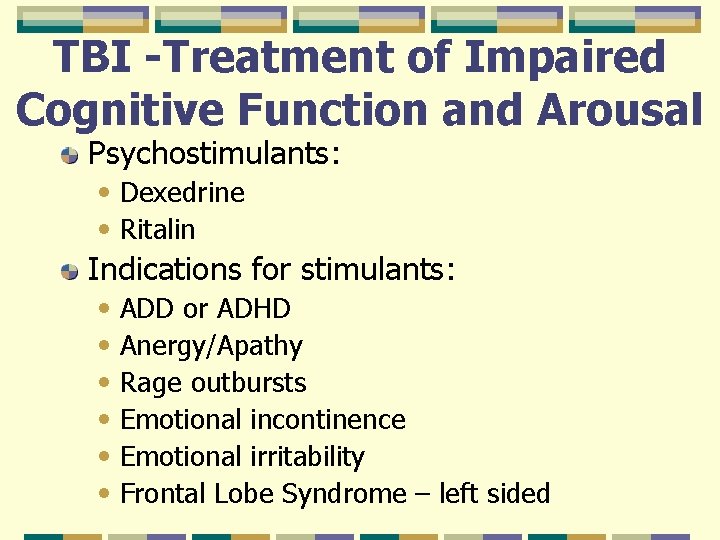
TBI -Treatment of Impaired Cognitive Function and Arousal Psychostimulants: • Dexedrine • Ritalin Indications for stimulants: • ADD or ADHD • Anergy/Apathy • Rage outbursts • Emotional incontinence • Emotional irritability • Frontal Lobe Syndrome – left sided
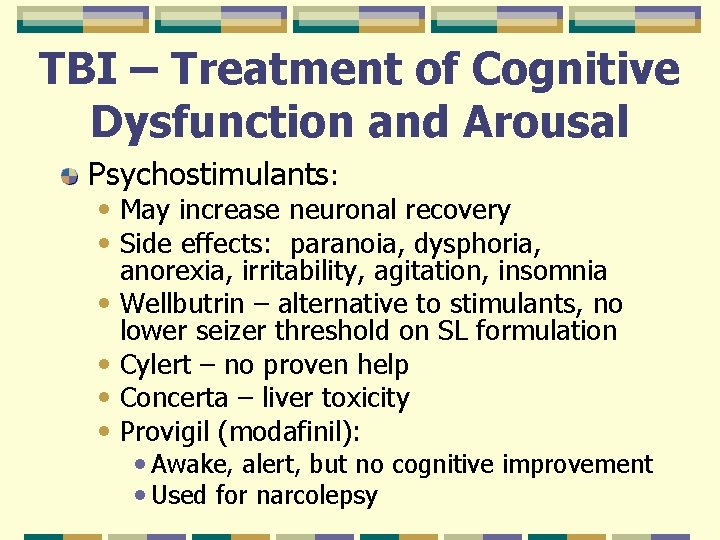
TBI – Treatment of Cognitive Dysfunction and Arousal Psychostimulants: • May increase neuronal recovery • Side effects: paranoia, dysphoria, • • anorexia, irritability, agitation, insomnia Wellbutrin – alternative to stimulants, no lower seizer threshold on SL formulation Cylert – no proven help Concerta – liver toxicity Provigil (modafinil): • Awake, alert, but no cognitive improvement • Used for narcolepsy
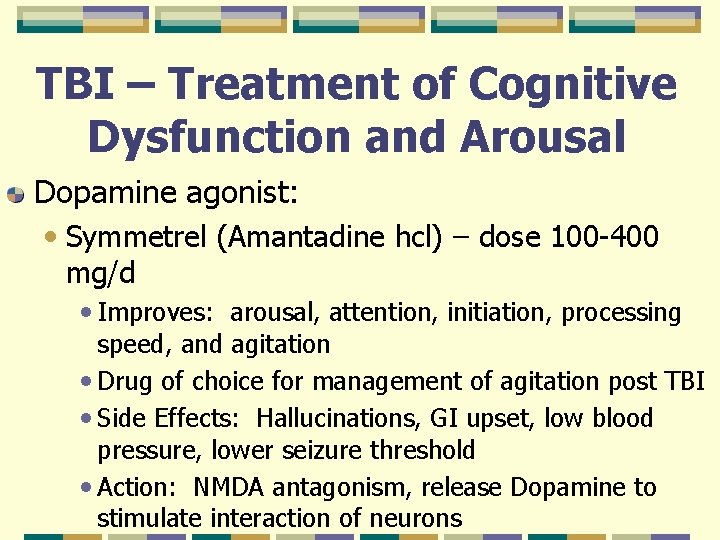
TBI – Treatment of Cognitive Dysfunction and Arousal Dopamine agonist: • Symmetrel (Amantadine hcl) – dose 100 -400 mg/d • Improves: arousal, attention, initiation, processing speed, and agitation • Drug of choice for management of agitation post TBI • Side Effects: Hallucinations, GI upset, low blood pressure, lower seizure threshold • Action: NMDA antagonism, release Dopamine to stimulate interaction of neurons
Sleep Disorders and TBI 50% of TBI patients with pain 27 -56% of all patients with TBI Common symptom of co-existing depression Acute phase of TBI – diffuse disruption of cerebral functioning, direct physical damage to brain, secondary neuropathological events Decreased REM and slow wave sleep Increase awakening at night Shortening of total sleep time: • Decrease or disappearance of deep sleep DIMS – common in recent injury
Treatment of Sleep Disorders in TBI Patients Melatonin – 3. 0 to 7. 5 mg at bedtime Ambien (5 to 20 mgs. ) – shorter activity, preserves REM sleep, decreased daytime effects Chloral Hydrate – rapid sleep induction, increases total sleep time, potential for tolerance, narrow therapeutic window Trazadone (Desyrel) – useful in depressed-TBI patients with insomnia
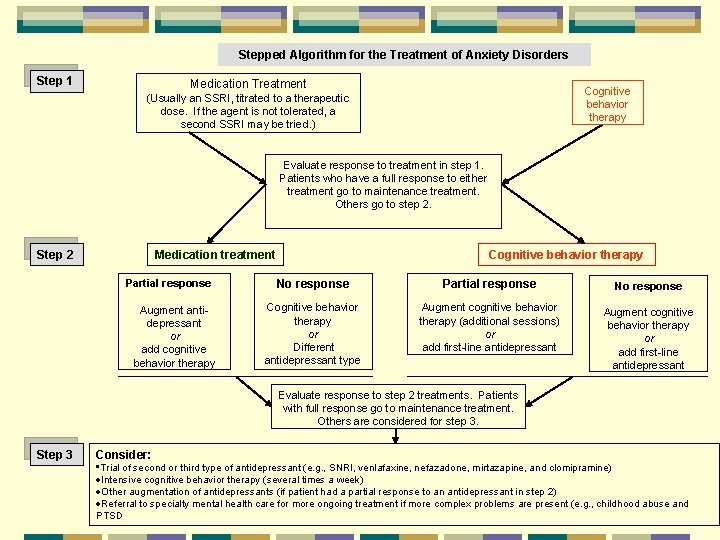
Stepped Algorithm for the Treatment of Anxiety Disorders Step 1 Medication Treatment Cognitive behavior therapy (Usually an SSRI, titrated to a therapeutic dose. If the agent is not tolerated, a second SSRI may be tried. ) Evaluate response to treatment in step 1. Patients who have a full response to either treatment go to maintenance treatment. Others go to step 2. Step 2 Medication treatment Partial response Augment antidepressant or add cognitive behavior therapy Cognitive behavior therapy No response Partial response No response Cognitive behavior therapy or Different antidepressant type Augment cognitive behavior therapy (additional sessions) or add first-line antidepressant Augment cognitive behavior therapy or add first-line antidepressant Evaluate response to step 2 treatments. Patients with full response go to maintenance treatment. Others are considered for step 3. Step 3 Consider: • Trial of second or third type of antidepressant (e. g. , SNRI, venlafaxine, nefazadone, mirtazapine, and clomipramine) ·Intensive cognitive behavior therapy (several times a week) ·Other augmentation of antidepressants (if patient had a partial response to an antidepressant in step 2) ·Referral to specialty mental health care for more ongoing treatment if more complex problems are present (e. g. , childhood abuse and PTSD
Alcohol TCU Screening Clinical Assessment CAGE
- Slides: 34