TAVR Addressing RealLife Issues CRT 2013 Washington DC








- Slides: 22
TAVR Addressing Real-Life Issues CRT 2013 Washington DC Marian Hawkey RN Center for Interventional Vascular Therapy New. York Presbyterian/Columbia University Medical Center New York, NY
Marian C. Hawkey, RN Within the past 12 months, I have had a financial interest/arrangement or affiliation with the organization(s) listed below. Affiliation/Financial Relationship: Consulting Fees/Honoraria Company: Edwards Lifesciences
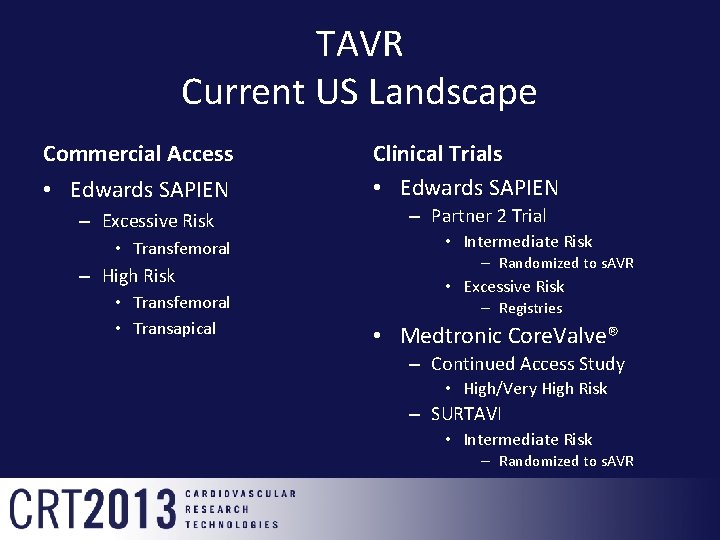
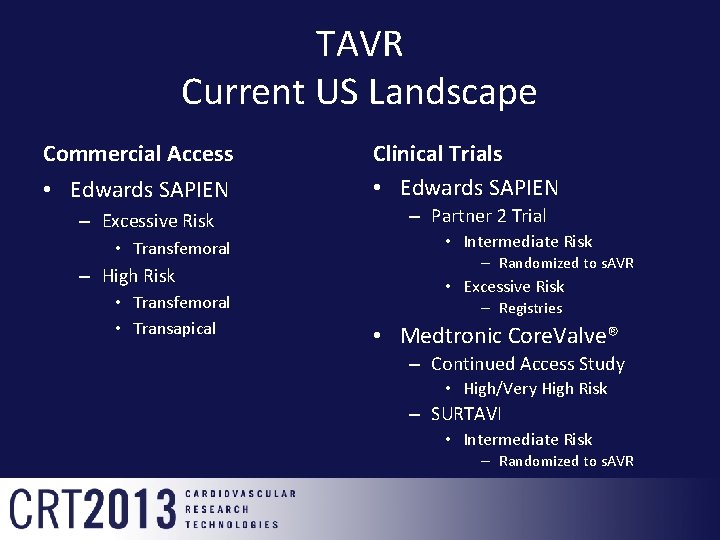
TAVR Current US Landscape Commercial Access • Edwards SAPIEN – Excessive Risk • Transfemoral – High Risk • Transfemoral • Transapical Clinical Trials • Edwards SAPIEN – Partner 2 Trial • Intermediate Risk – Randomized to s. AVR • Excessive Risk – Registries • Medtronic Core. Valve® – Continued Access Study • High/Very High Risk – SURTAVI • Intermediate Risk – Randomized to s. AVR
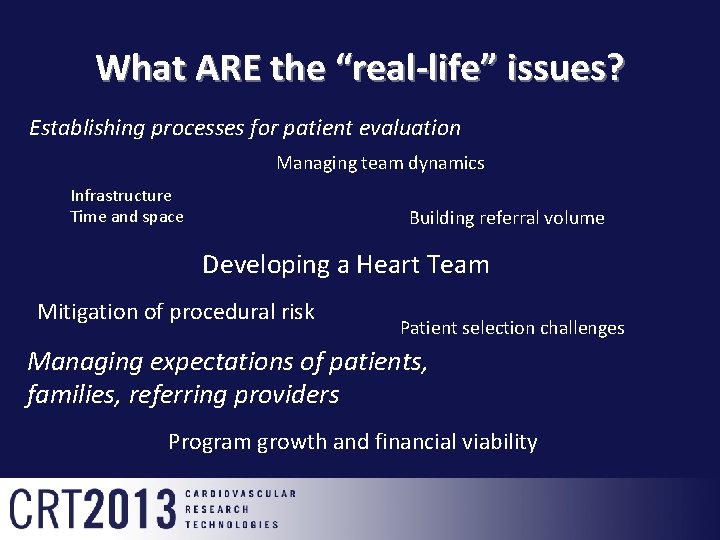
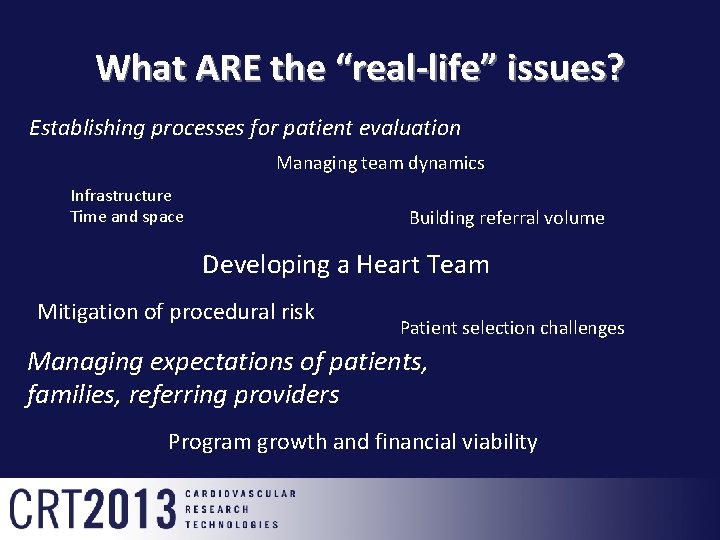
What ARE the “real-life” issues? Establishing processes for patient evaluation Managing team dynamics Infrastructure Time and space Building referral volume Developing a Heart Team Mitigation of procedural risk Patient selection challenges Managing expectations of patients, families, referring providers Program growth and financial viability

Embracing New Technology in the “Real World” • Making the transition from clinical research to clinical practice • STRONG institutional support • Collaborative team concept • Multiple moving parts • Developing a valve team (easier said than done) – Identification of key team players • Multidisciplinary clinical evaluation process • Technical expertise • Process development and implementation • Allow for growth and flexibility • Selecting the right patients
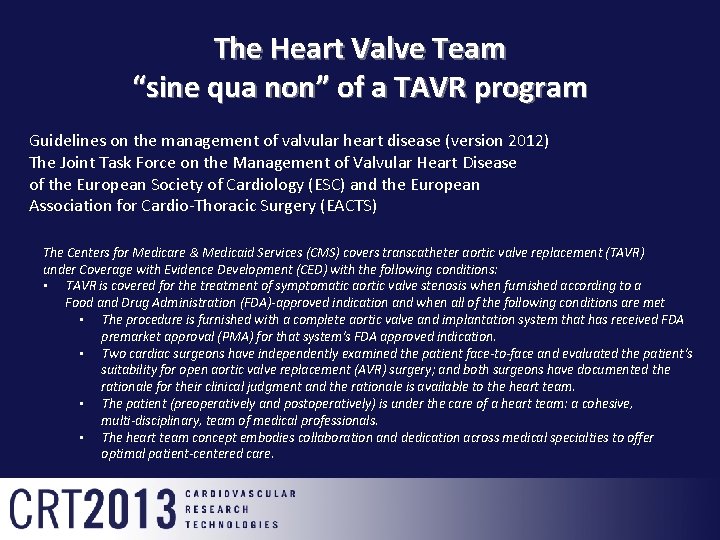
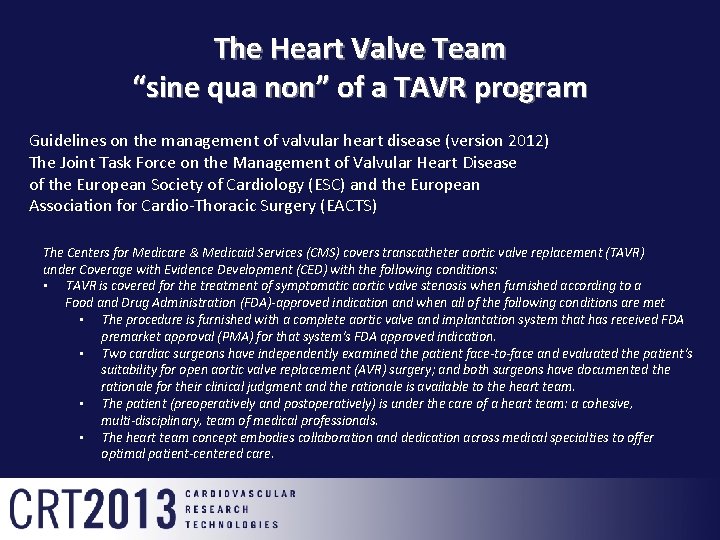
The Heart Valve Team “sine qua non” of a TAVR program Guidelines on the management of valvular heart disease (version 2012) The Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) The Centers for Medicare & Medicaid Services (CMS) covers transcatheter aortic valve replacement (TAVR) under Coverage with Evidence Development (CED) with the following conditions: • TAVR is covered for the treatment of symptomatic aortic valve stenosis when furnished according to a Food and Drug Administration (FDA)-approved indication and when all of the following conditions are met • The procedure is furnished with a complete aortic valve and implantation system that has received FDA premarket approval (PMA) for that system's FDA approved indication. • Two cardiac surgeons have independently examined the patient face-to-face and evaluated the patient's suitability for open aortic valve replacement (AVR) surgery; and both surgeons have documented the rationale for their clinical judgment and the rationale is available to the heart team. • The patient (preoperatively and postoperatively) is under the care of a heart team: a cohesive, multi-disciplinary, team of medical professionals. • The heart team concept embodies collaboration and dedication across medical specialties to offer optimal patient-centered care.
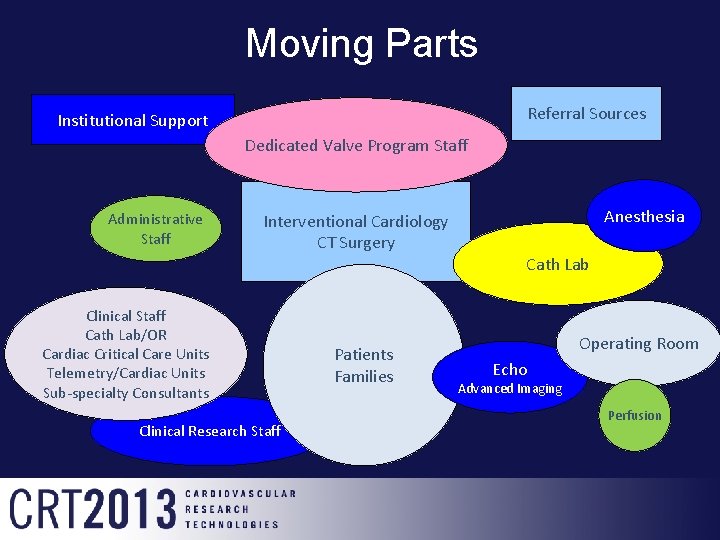
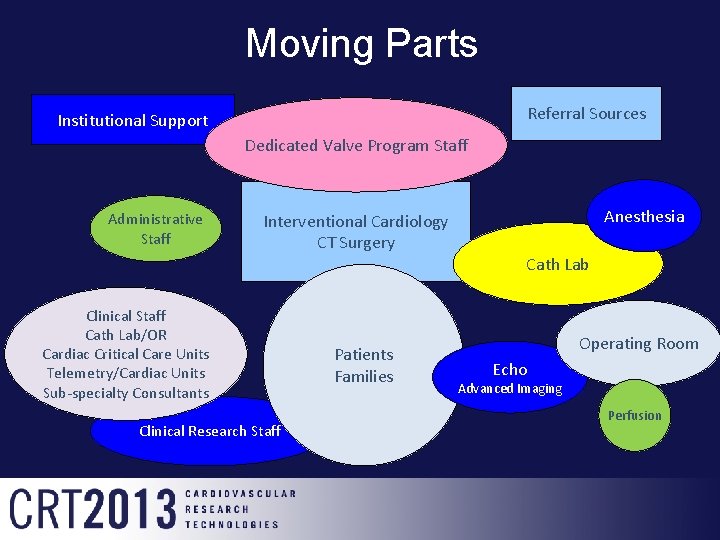
Moving Parts Referral Sources Institutional Support Dedicated Valve Program Staff Administrative Staff Interventional Cardiology CT Surgery Clinical Staff Cath Lab/OR Cardiac Critical Care Units Telemetry/Cardiac Units Sub-specialty Consultants Clinical Research Staff Patients Families Anesthesia Cath Lab Operating Room Echo Advanced Imaging Perfusion
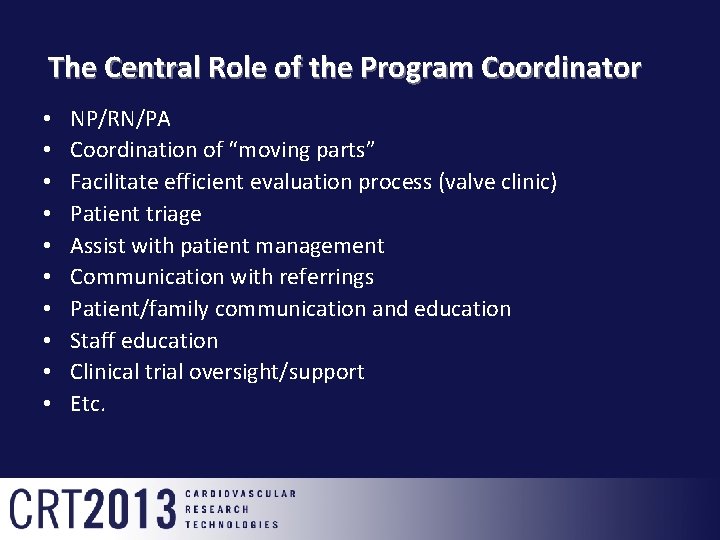
The Central Role of the Program Coordinator • • • NP/RN/PA Coordination of “moving parts” Facilitate efficient evaluation process (valve clinic) Patient triage Assist with patient management Communication with referrings Patient/family communication and education Staff education Clinical trial oversight/support Etc.

Marketing Development and of standardizedoutreach Data orders collection Communication with patients and families Deal with reimbursement Clinical Coordination issues assessment of diagnostic and triage work-up Consent Process Coordination of clinical Valve Clinic trials Schedule schedule and procedures operations Referrals and pre-op Program Intake Patient Coordination The voice of testing Development follow-up of heart team reason activities and Staff processes education Management Represent program to of Communication Waitlist patients, families, expectations with referring Management referrings etc. Patient and providers Fostering of essential family Process relationships education Development
Clinical Processes • Establish and maintain contact with referrings • Facilitate valve clinic appointments and scheduling/review of diagnostic testing • Inpatient service support • Key point of contact with patient and family – Provide “road map”/navigation – Manage expectations – Initiate consent process • Waitlist management • Keeping track of the “small” details

Developing and Sustaining The Heart Team and Program • “Face” of the program • Create communication pathways • Process development – Evaluation of processes • • Data management Clinical research operations and coordination Marketing and outreach Education
Patient-Centered Care • Represent program to patients and families – Familiarity with individual patients • Insights on patient selection • Making procedural information accessible and comprehensible • Understanding the needs of the patient population • Being an advocate for patients and families

Patient-Specific Considerations • • • Elderly Multiple comorbidities Sensory and/or cognitive deficits Mobility impairment Multiple family members involved in decision-making process Determining operability status – Risk assessment – Is TAVR technically feasible and safe? – Is TAVR appropriate for this patient?

Making Balanced Treatment Decisions Can we do this? Technical feasibility Utility vs. Futility Should we do this? Realistic posttreatment goals
Patients and Families Educational Imperatives • Complex nature of procedure-related information – In most cases, family involvement is essential • Awareness of sensory impairments • Awareness of cognitive impairments – Assessment of ability to provide consent • Utilization of educational tools i. e. procedure animations • Allow plenty of time for discussion and to obtain consent • Management of patient and family expectations – Addressing misperceptions
Peri-Procedural Processes • Keep referring practitioner in loop • Clinical trial vs. commercial procedures • Internal communication regarding schedule, logistics etc. • Integration of Cath Lab/OR staff • Device management • Creation of standardized orders • Facilitated discharge planning

Procedural Essentials • Hybrid OR and/or Cath Lab – Necessary surgical and interventional equipment must be available in either location – Cardiopulmonary bypass on stand-by • Staff education and training – Core group to “own” TAVR procedures – Inventory checklist – Cath lab/OR cross-training • Scrub/circulating nurse roles – Create familiar environment for staff – Worst-case scenario planning – Designation of primary procedure days
Integrating AS Patients Into Your Clinical Environment • How will these patients change the demographics, staffing ratio, length of stay etc. in your interventional cardiology step-down unit? – Adaptation of clinical staff • Expertise in care and management of patients with aortic stenosis – Key sub-specialty consultants on speed dial – Develop of competency assessment for nursing staff • Expertise in care and management of geriatric patients – Strong support from social workers, physical/occupational therapists etc.

Looking to the future • New devices and expanded indications • Ongoing challenges associated with complex patient populations • Relationships in the international transcatheter valve therapy nursing community will continue to play an essential role – Sharing of processes – Collaborative research – Expansion of our evidence-base for clinical practice
In Conclusion • Physician expertise is of critical importance • Of equal importance is engagement of experts (RN, NP, PA etc. ) who will: – Develop and implement processes for managing referrals, efficient patient evaluation, valve clinic operations – Foster essential relationships and educational opportunities – Take ownership for program growth – Know their patients (literally) inside and out

 Annular rupture tavr
Annular rupture tavr Tavr antiplatelet guidelines
Tavr antiplatelet guidelines Flat addressing vs hierarchical addressing
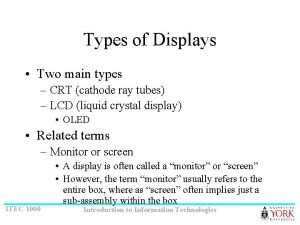
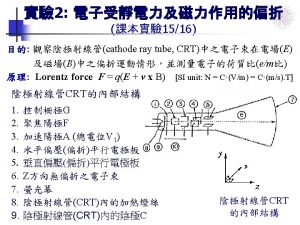
Flat addressing vs hierarchical addressing Uses crt
Uses crt Vertical sync
Vertical sync Lcd led crt
Lcd led crt Helmet mounted display crt
Helmet mounted display crt Crt topics
Crt topics Crt graphics
Crt graphics Crt 2017
Crt 2017 Crt monitor
Crt monitor Monitor crt zasada działania
Monitor crt zasada działania Uses crt
Uses crt Crt electron gun
Crt electron gun Cathode ray oscilloscope animation
Cathode ray oscilloscope animation Crt monitor
Crt monitor Cro cathode ray oscilloscope
Cro cathode ray oscilloscope Crt monitor vorteile nachteile
Crt monitor vorteile nachteile Nrt vs crt
Nrt vs crt Assessment process in special education
Assessment process in special education Angel computer graphics
Angel computer graphics Nrt and crt examples
Nrt and crt examples Převod vhs do pc
Převod vhs do pc