Talking Space Talking Health The IAPT service Oxfordshire




- Slides: 26

Talking. Space & Talking. Health The IAPT service, Oxfordshire and Buckinghamshire NHS Foundation Trust Christina Surawy: Oxford Mindfulness Centre, Oxford University Department of Psychiatry With thanks to: Emma Evans, Clinical Supervisor and Clinical Psychologist
Outline of the session n n Overview of Talking. Space Talking. Health: Services for people with longterm health conditions MBCT within IAPT Questions and answers
Referrals to Talking. Space n n n TS receives 6500 referrals a year Primarily self-referral The service is meeting nationally agreed recovery rates (40 -50%)
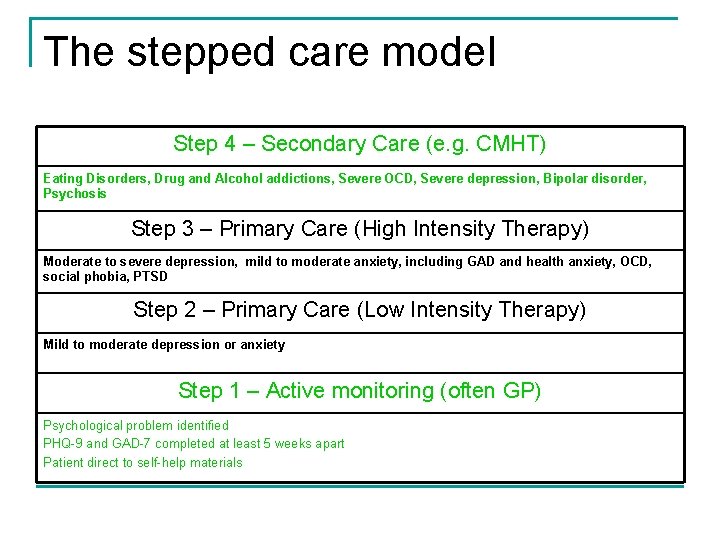
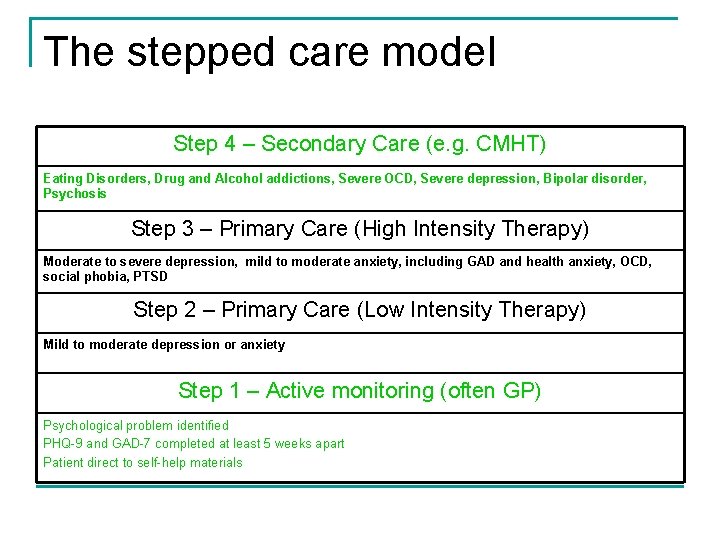
The stepped care model Step 4 – Secondary Care (e. g. CMHT) Eating Disorders, Drug and Alcohol addictions, Severe OCD, Severe depression, Bipolar disorder, Psychosis Step 3 – Primary Care (High Intensity Therapy) Moderate to severe depression, mild to moderate anxiety, including GAD and health anxiety, OCD, social phobia, PTSD Step 2 – Primary Care (Low Intensity Therapy) Mild to moderate depression or anxiety Step 1 – Active monitoring (often GP) Psychological problem identified PHQ-9 and GAD-7 completed at least 5 weeks apart Patient direct to self-help materials
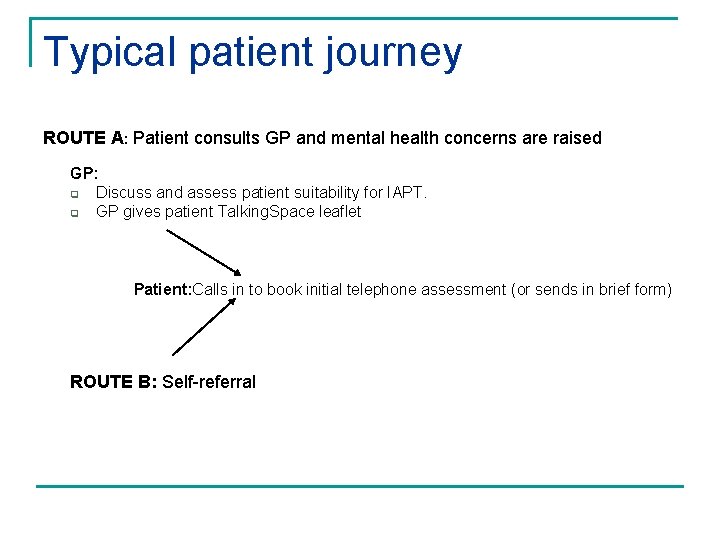
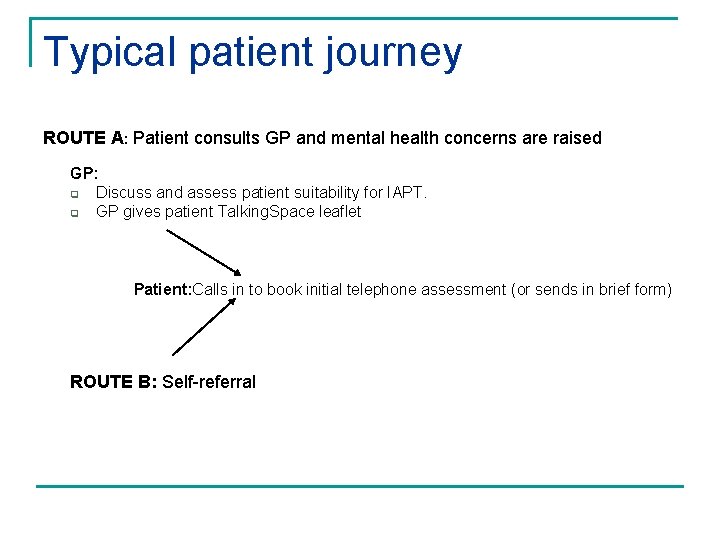
Typical patient journey ROUTE A: Patient consults GP and mental health concerns are raised GP: q Discuss and assess patient suitability for IAPT. q GP gives patient Talking. Space leaflet Patient: Calls in to book initial telephone assessment (or sends in brief form) ROUTE B: Self-referral
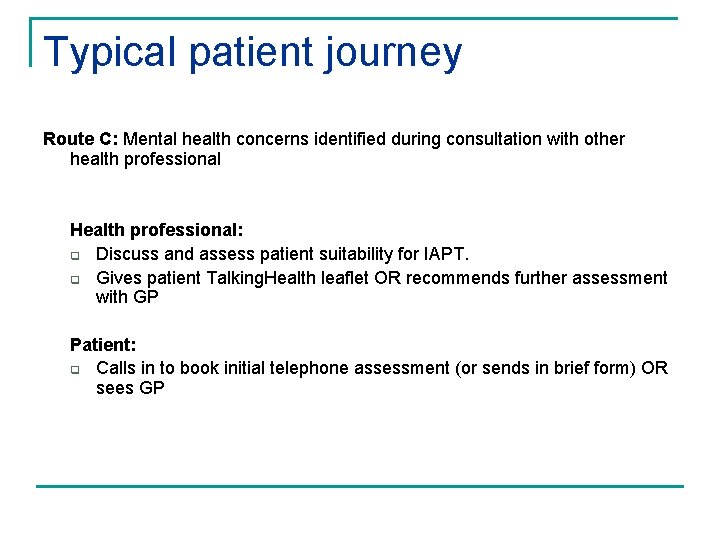
Typical patient journey Route C: Mental health concerns identified during consultation with other health professional Health professional: q Discuss and assess patient suitability for IAPT. q Gives patient Talking. Health leaflet OR recommends further assessment with GP Patient: q Calls in to book initial telephone assessment (or sends in brief form) OR sees GP
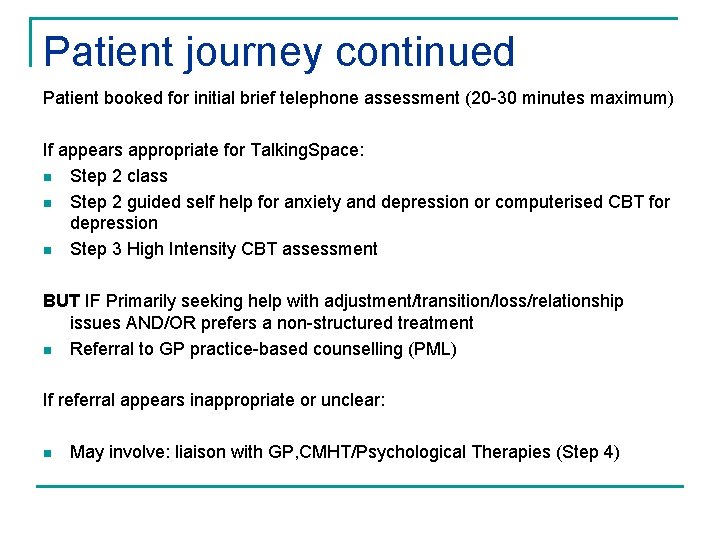
Patient journey continued Patient booked for initial brief telephone assessment (20 -30 minutes maximum) If appears appropriate for Talking. Space: n Step 2 class n Step 2 guided self help for anxiety and depression or computerised CBT for depression n Step 3 High Intensity CBT assessment BUT IF Primarily seeking help with adjustment/transition/loss/relationship issues AND/OR prefers a non-structured treatment n Referral to GP practice-based counselling (PML) If referral appears inappropriate or unclear: n May involve: liaison with GP, CMHT/Psychological Therapies (Step 4)
Treatments offered Step 2 (LI) n n n Psychoeducation courses – anxiety, depression, insomnia, emotional well being in diabetes Information giving Bibliotherapy & Guided-self help Computerised CBT (Beating the Blues) 3 -month follow ups as standard

Psychoeducation courses n n n Offered in various locations throughout Oxfordshire Depression, anxiety or insomnia Four sessions (five for insomnia) Stand-alone treatment or an introduction to CBT skills 1 month follow up call
Psychoeducation classes: patient comments n n n It would do a majority of people good. It’s really helpful/reassuring to meet other people suffering from the same thing. It’s nice to talk within a group and not just one to one which is quite intense. Excellent and friendly presentation. Useful and informative. Has certainly helped me to overcome some of my problems.
Treatments offered Step 3 (High Intensity) n Groups – depression, OCD, anxiety (transdiagnostic), carers’ groups for people caring for people with dementia n Individual CBT n Mindfulness Based CT group for depression (relapse prevention) n Mindfulness Based CT group for long-term conditions n IPT (Interpersonal therapy) n DIPT (Brief Dynamic Interpersonal Therapy)
Additional interventions and services n Employment support (Restore) to liaise, provide signposting and support for people struggling to stay in employment
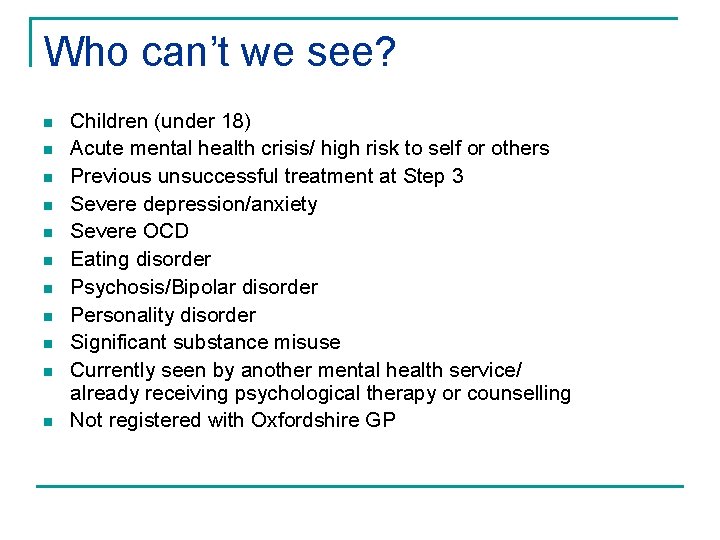
Who can’t we see? n n n Children (under 18) Acute mental health crisis/ high risk to self or others Previous unsuccessful treatment at Step 3 Severe depression/anxiety Severe OCD Eating disorder Psychosis/Bipolar disorder Personality disorder Significant substance misuse Currently seen by another mental health service/ already receiving psychological therapy or counselling Not registered with Oxfordshire GP
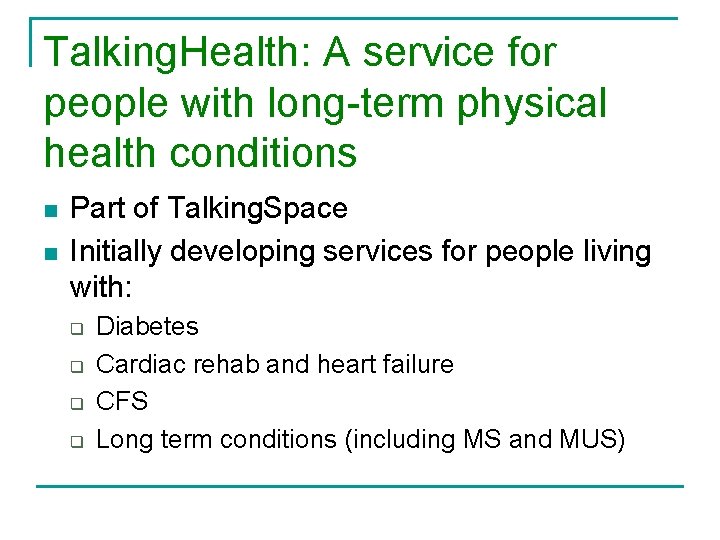
Talking. Health: A service for people with long-term physical health conditions n n Part of Talking. Space Initially developing services for people living with: q q Diabetes Cardiac rehab and heart failure CFS Long term conditions (including MS and MUS)
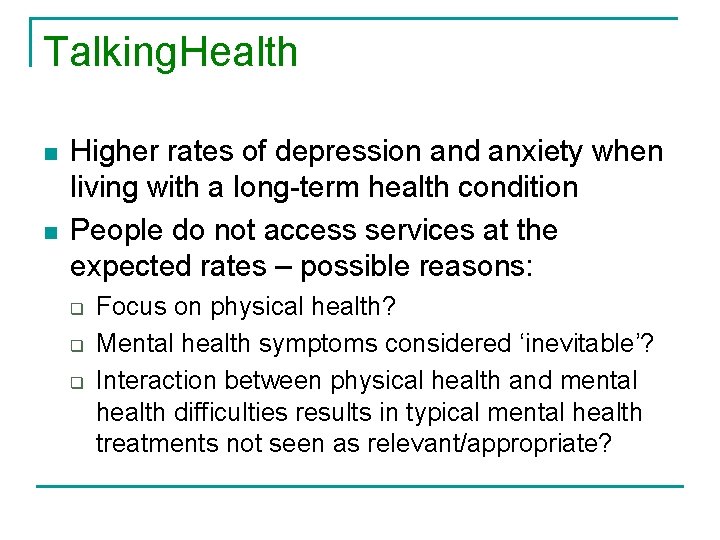
Talking. Health n n Higher rates of depression and anxiety when living with a long-term health condition People do not access services at the expected rates – possible reasons: q q q Focus on physical health? Mental health symptoms considered ‘inevitable’? Interaction between physical health and mental health difficulties results in typical mental health treatments not seen as relevant/appropriate?
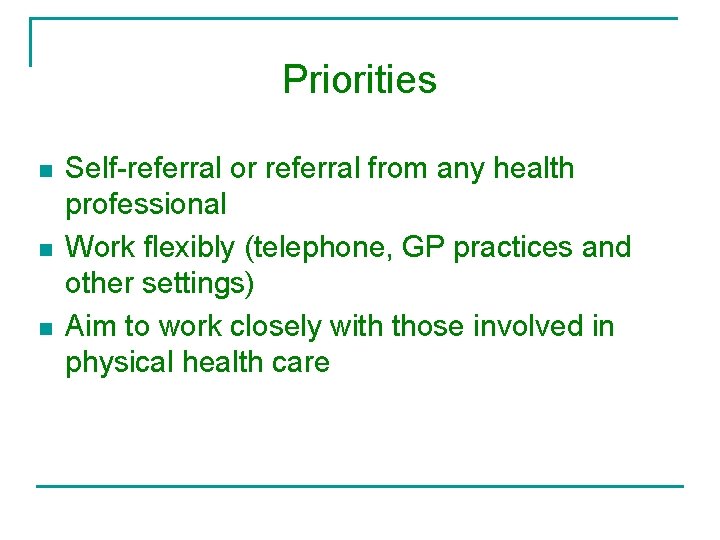
Priorities n n n Self-referral or referral from any health professional Work flexibly (telephone, GP practices and other settings) Aim to work closely with those involved in physical health care
Cardiac services n n n Input to classes run by nursing staff (psychoeducation) Guided self help (step 2) Individual CBT and staff supervision groups (step 3)
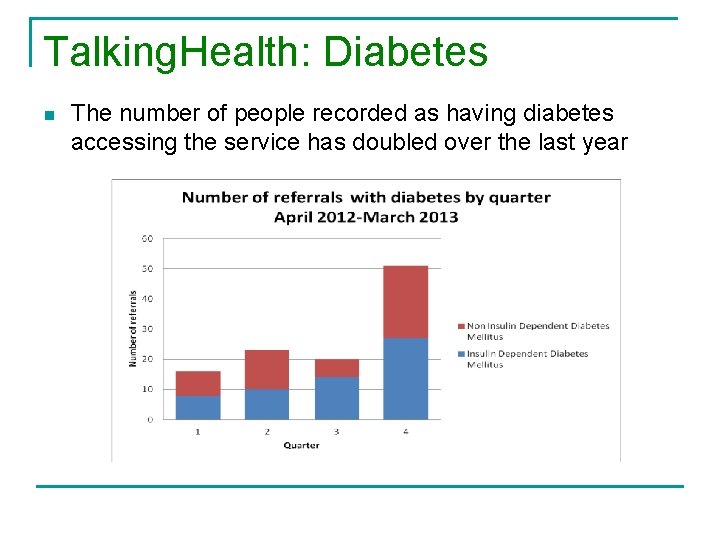
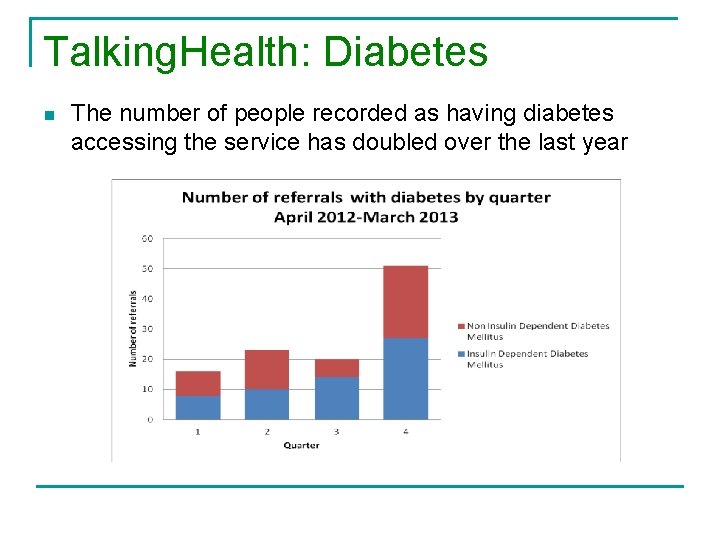
Talking. Health: Diabetes n The number of people recorded as having diabetes accessing the service has doubled over the last year
Emotional well-being in diabetes course n n n Four session psychoeducation group for people with diabetes and depression. CBT based Adapted from step 2 class ‘Managing your mood’ Looks at interaction between physical and mental health Topics covers: q q Behavioural activation Problem solving Goal setting Cognitive challenging
Evidence to support a course Initial outcomes suggest: n n Greater improvements in mood (PHQ-9) than in standard class Improvements in physical health (HBA 1 c)
MBCT in Talking. Space and Talking. Health n n n OMC have undertaken to train step 3 IAPT practitioners to deliver MBCT for recurrent depression and anxiety (TS) and LTC’s including MUS). Also a specific MBCT course for CFS Hoffman et al. (2011) showed that MBCT reduces anxiety and depression across a range of physical diagnoses So far 8 courses have run Average no. of participants in TS= 16 Fewer in talking health
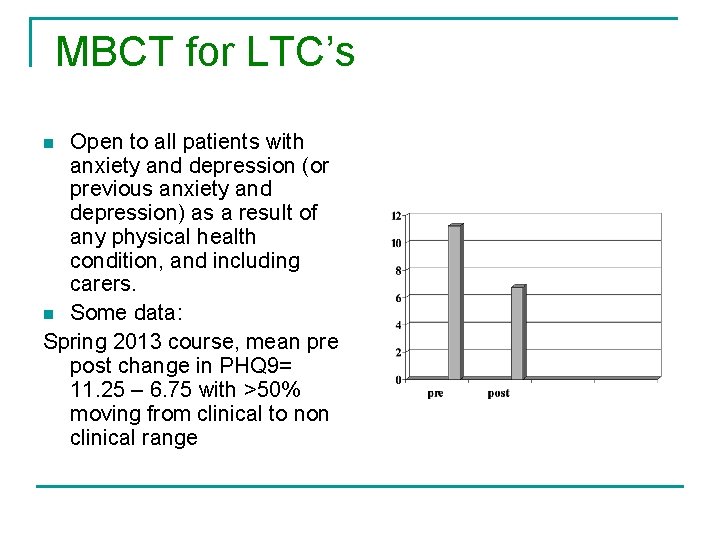
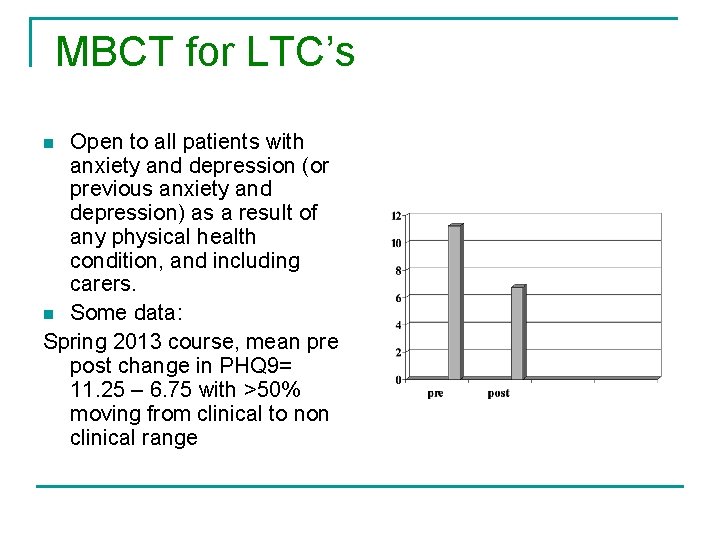
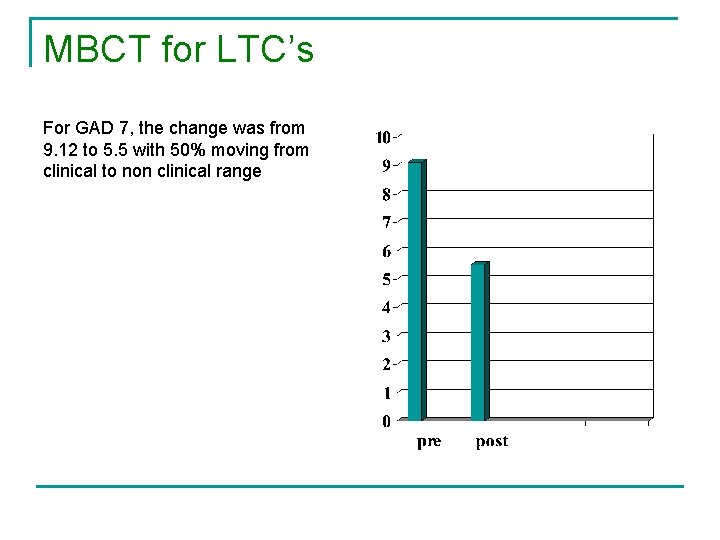
MBCT for LTC’s Open to all patients with anxiety and depression (or previous anxiety and depression) as a result of any physical health condition, and including carers. n Some data: Spring 2013 course, mean pre post change in PHQ 9= 11. 25 – 6. 75 with >50% moving from clinical to non clinical range n
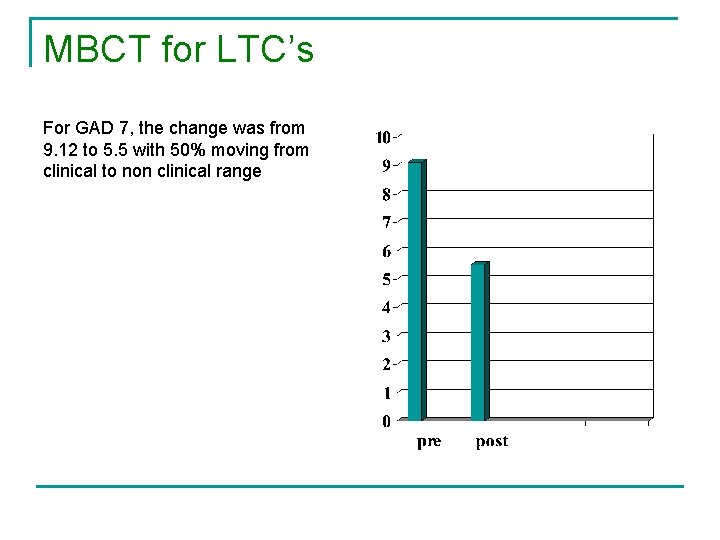
MBCT for LTC’s For GAD 7, the change was from 9. 12 to 5. 5 with 50% moving from clinical to non clinical range

Case example – Bill n n n 66 year old male Physical health: Multiple sclerosis (diagnosed 25 years), neuropathic pain, referred by pain clinic Mental health: Low mood, self-critical, frustration, tense, restless, body/pain the enemy (constant battle) Treatment: Mindfulness based cognitive therapy group (8 week programme) Outcome: improved mood, more relaxed, not fighting pain/body, reduced scores on PHQ-9 & GAD-7
Future directions n n n Continue to adapt and develop MBCT for LTC’s and MUS Individualised measures Developing links with pain services

Questions?
 Oxfordshire talking space
Oxfordshire talking space Oxfordshire cricket association
Oxfordshire cricket association Cpre oxfordshire
Cpre oxfordshire Oxfordshire safeguarding adults board
Oxfordshire safeguarding adults board Trafford iapt
Trafford iapt Joint space vs cartesian space
Joint space vs cartesian space Space junk the space age began
Space junk the space age began Camera space to world space
Camera space to world space Cartesian space vs joint space
Cartesian space vs joint space Ndc to screen space
Ndc to screen space Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Glasgow thang điểm
Glasgow thang điểm Hát lên người ơi alleluia
Hát lên người ơi alleluia Các môn thể thao bắt đầu bằng tiếng nhảy
Các môn thể thao bắt đầu bằng tiếng nhảy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Phép trừ bù
Phép trừ bù độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật