Taking Patient Observations National Early Warning Score NEWS

Taking Patient Observations
National Early Warning Score (NEWS 2)
Learning Outcomes • To develop a basic understanding of anatomy related to patient • • • observations Demonstrate accurate taking and recording of patient observations Demonstrate recording of patient observations using National Early Warning Score (NEWS 2) chart. Understand the importance of escalation of care in relation to patient observations and NEWS 2
Patient Observations • • • Respiratory rate Oxygen Saturations Pulse Blood Pressure (BP) Level of consciousness Temperature
Normal Parameters • RR: 12 -20 • Saturations: 96 or over in normal adults 88 – 92% in patients with COPD • BP: Systolic 111 - 219 mm. Hg • HR: 51 -90 bpm • Urine output in last 6 hours • Alert and Aware of surroundings • Temperature: 36 – 38°C
Taking Patient Observations • • • Airway Breathing Circulation Disability Exposure
Airway
Airway Assessment • Is the airway clear? • In a conscious patient ask them a question, if they can answer normally, their airway is clear • If the patient is unconscious or the airway is blocked or noisy you need to call for help urgently
Breathing
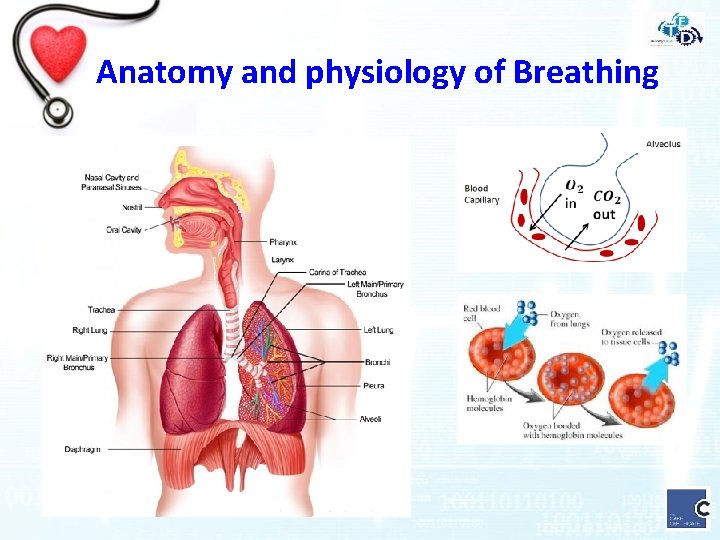
Anatomy and physiology of Breathing
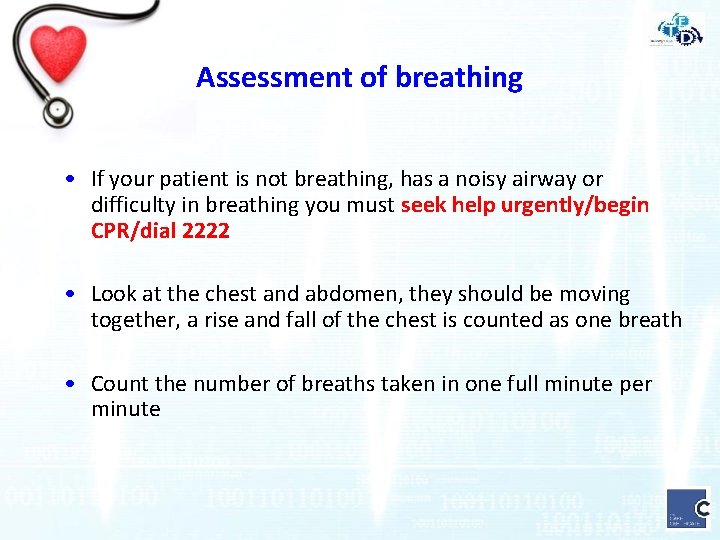
Assessment of breathing • If your patient is not breathing, has a noisy airway or difficulty in breathing you must seek help urgently/begin CPR/dial 2222 • Look at the chest and abdomen, they should be moving together, a rise and fall of the chest is counted as one breath • Count the number of breaths taken in one full minute per minute
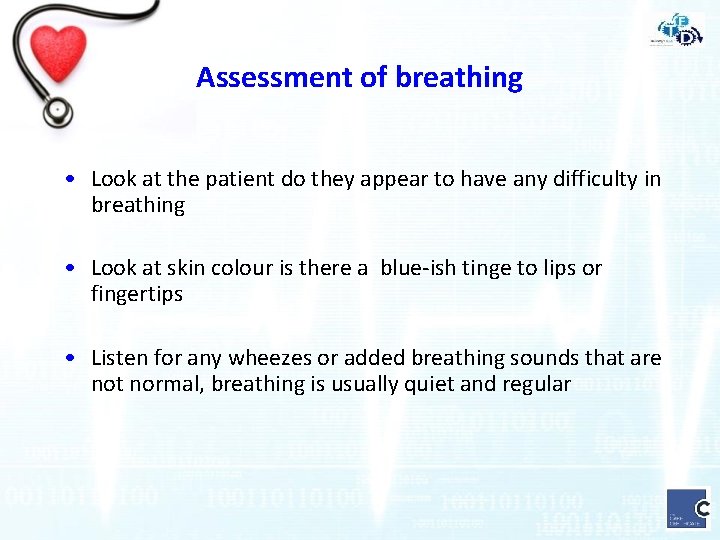
Assessment of breathing • Look at the patient do they appear to have any difficulty in breathing • Look at skin colour is there a blue-ish tinge to lips or fingertips • Listen for any wheezes or added breathing sounds that are not normal, breathing is usually quiet and regular
Assessment of Breathing - Respiratory Rate • Normal rate should be between 12 and 20 breaths per minute • If the patient has increased or decreased rate of breathing is an abnormal finding call for help urgently
Assessment of Breathing – Oxygen Saturations • Oxygen is carried in the blood attached to haemoglobin molecules. • Oxygen saturation is a measure of how much oxygen the blood is carrying and is recorded as a percentage (Sp 02) • Normal values: Over 96% in normal adults 88 – 92% in patients with COPD • Problems leading to unreliable readings are ambient light, nail polish, temperature and circulation of limbs
Circulation
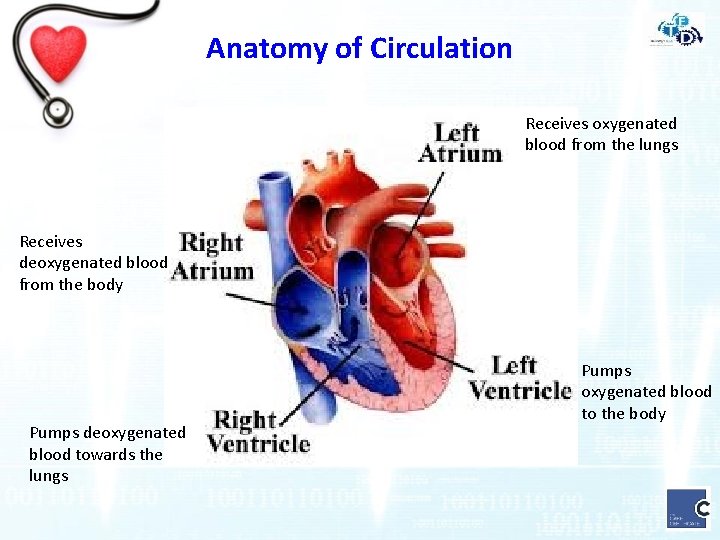
Anatomy of Circulation Receives oxygenated blood from the lungs Receives deoxygenated blood from the body Pumps deoxygenated blood towards the lungs Pumps oxygenated blood to the body
Anatomy of Circulation • The Circulatory system comprises of the heart and blood vessels it is a closed system • The contraction of the heart muscle pumps forces blood through blood vessels • Blood vessels allow blood to circulate to all parts of the body • The function of the circulatory system is to deliver oxygen and nutrients and to remove carbon dioxide and other waste products
Assessment of Circulation - Pulse · Pulse – pressure wave of blood following each contraction of the heart muscle (heartbeat) · Monitored at bony prominences where pulse is easily felt · The pulse (heart rate) should be monitored for 60 seconds · Always palpate the pulse for a full minute and note any irregular or missed heartbeats
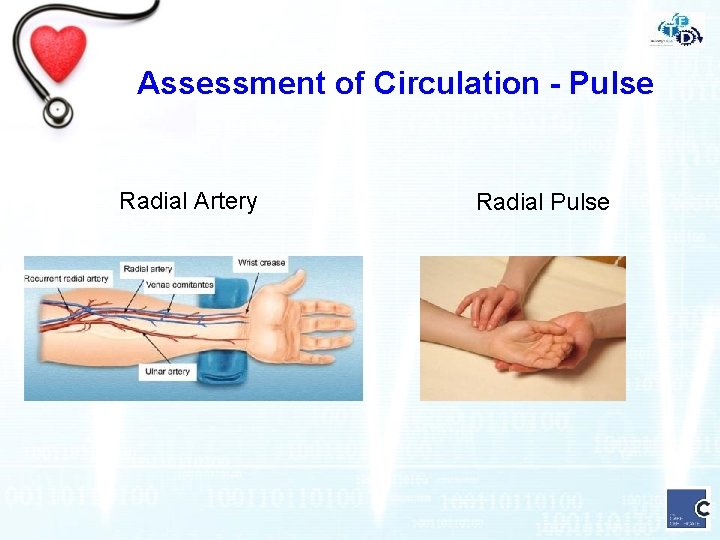
Assessment of Circulation - Pulse Radial Artery Radial Pulse
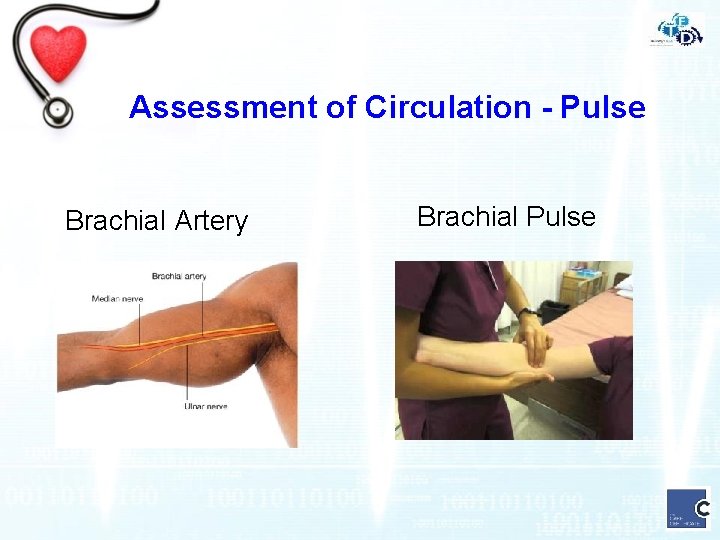
Assessment of Circulation - Pulse Brachial Artery Brachial Pulse
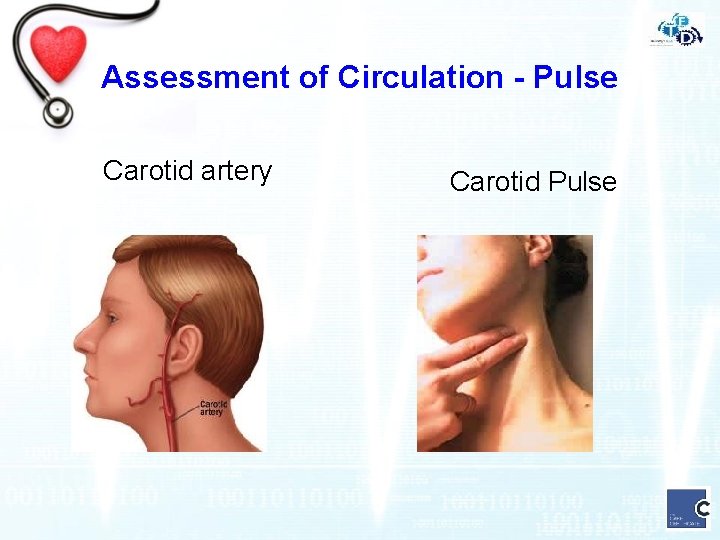
Assessment of Circulation - Pulse Carotid artery Carotid Pulse
Assessment of Circulation - Pulse • Normal ranges for adults is 51 – 90 beats per minute (bpm) • Bradycardia is a slower than normal pulse rate less than 50 bpm • Tachycardia is a faster than normal pulse rate more than 90 bpm • Always inform nursing staff if you patient has an abnormal heart rate as they may need an ECG recording
Assessment of Circulation – Blood Pressure • Blood pressure (BP) is the force exerted by blood against the walls of the vessels in which it is contained. • It is recorded as a figure: 120 80 Systole Diastole mm. Hg • Systolic pressure is the peak pressure of blood in the arteries and is caused by contraction of the ventricle. • Diastolic pressure is the minimum pressure of the blood against the wall of the vessel following closure of the aortic valve.
Assessment of Circulation – Blood Pressure • Adequate Blood Pressure is essential for delivery of O 2 and nutrients to the rest of the body. • Be aware of what is normal for patient • Always ask the patient if they have a Fistula, Lymphoedema, or Mastectomy, before you apply a blood pressure cuff • A low blood pressure is a late sign of deterioration
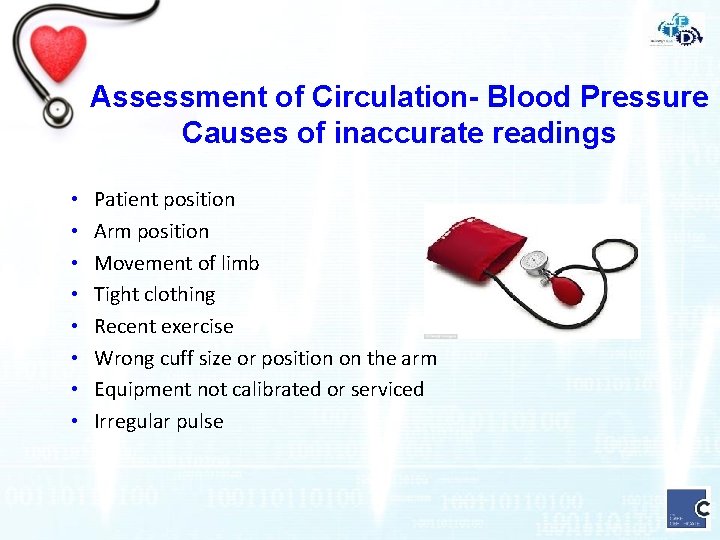
Assessment of Circulation- Blood Pressure Causes of inaccurate readings • • Patient position Arm position Movement of limb Tight clothing Recent exercise Wrong cuff size or position on the arm Equipment not calibrated or serviced Irregular pulse
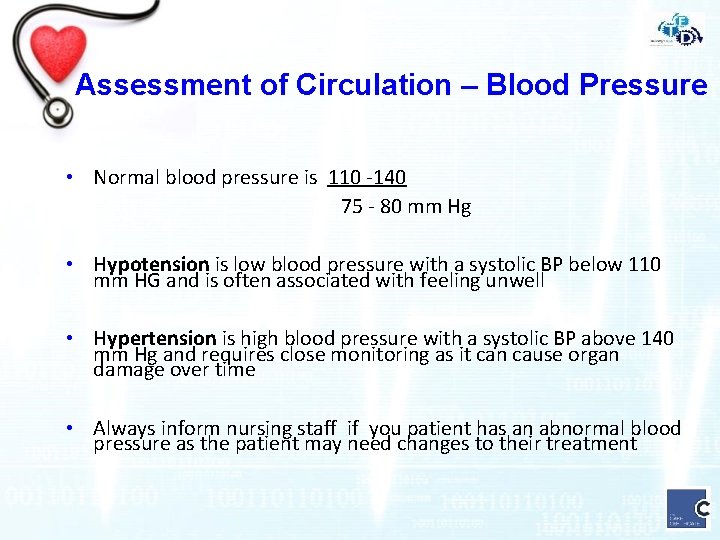
Assessment of Circulation – Blood Pressure • Normal blood pressure is 110 -140 75 - 80 mm Hg • Hypotension is low blood pressure with a systolic BP below 110 mm HG and is often associated with feeling unwell • Hypertension is high blood pressure with a systolic BP above 140 mm Hg and requires close monitoring as it can cause organ damage over time • Always inform nursing staff if you patient has an abnormal blood pressure as the patient may need changes to their treatment
Disability (Level of Consciousness)
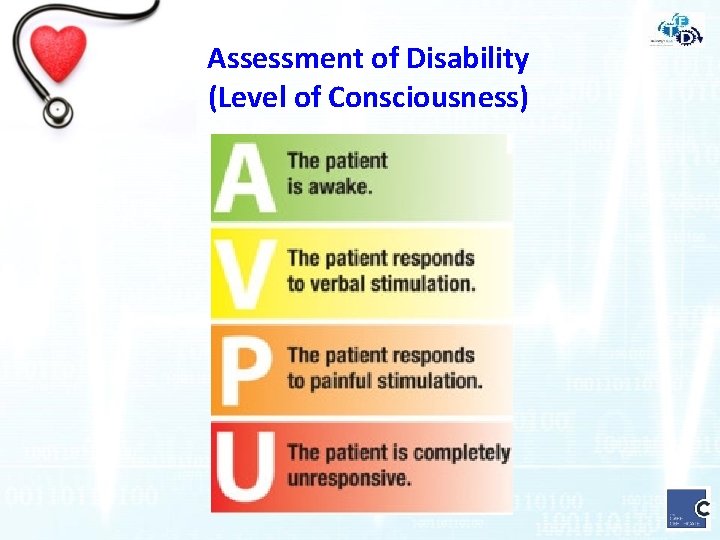
Assessment of Disability (Level of Consciousness)
Assessment of Disability (Level of Consciousness) • Consider what is normal for the patient e. g. Dementia • Things that affect a patients level of consciousness could include • Drugs prescribed and recreational • Alcohol • Blood Sugar • Head Injury • If your patient is unresponsive or only responding to pain seek help urgently and inform nursing staff • A more in depth assessment of consciousness using the Glasgow Coma Score will be required
Exposure (Temperature)
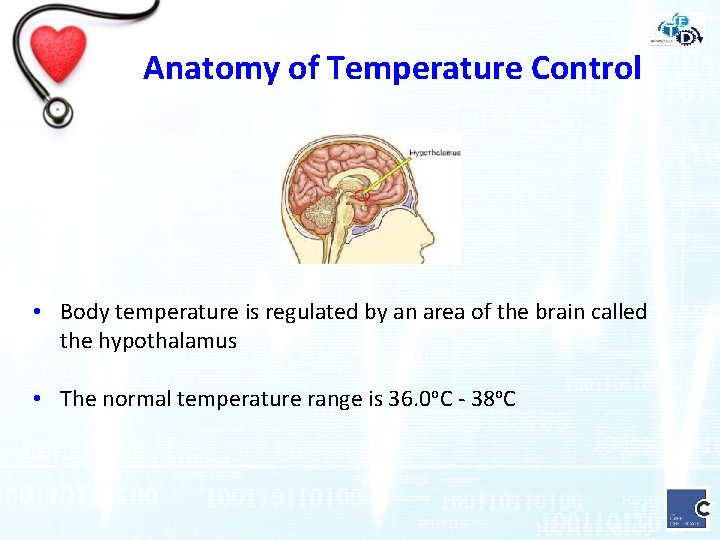
Anatomy of Temperature Control • Body temperature is regulated by an area of the brain called the hypothalamus • The normal temperature range is 36. 0 o. C - 38 o. C
Assessment of Temperature measurements can be taken • Orally (Mouth) • Rectally (Anus) • Axillary (Armpit) • Tympanic (Ear)
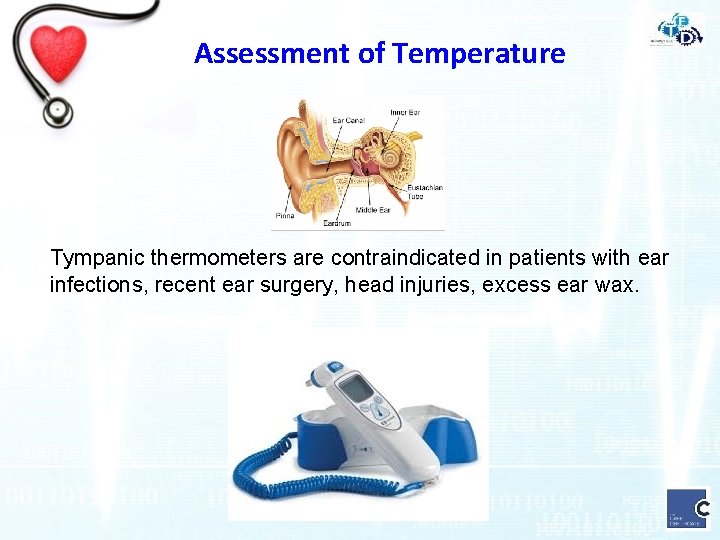
Assessment of Temperature Tympanic thermometers are contraindicated in patients with ear infections, recent ear surgery, head injuries, excess ear wax.
Assessment of Temperature • The normal temperature range is 36. 0 o. C - 38 o. C • Hypothermia is a low temperature below 35 o. C • Pyrexia is a high temperature 38 o. C - 40. 0 o. C • Hyperpyrexia is a high temperature above 40. 0 o. C • If your patient has hypothermia, pyrexia or hyperpyrexia inform nursing staff immediately
Exposure - Other considerations • Wounds • Bleeding • Pressure areas • Drains • Catheters
Patients who are at risk • • Immunosuppressed On Opioids Existing Co-morbidities Emergency Admissions Elderly ICU discharges Prolonged Hospital Stay
Soft Signs • • Colour of skin / sweating Unable to speak / out of breath Cold feet and legs / reduced mobility Change in bowel and bladder function Withdrawn/agitated/confused(new) Concern from family/relatives Increased pain Reduced appetite
Summary • A basic understanding of anatomy related to patient • • • observations Importance of accurate taking and recording of patient observations Accurately recording of patient observations using National Early Warning Score (NEWS 2) chart. Support the escalation of care in relation to patient observations and NEWS 2
Demonstration Welch Allyn Electronic Blood Pressure and Sp. O 2 device
Practical Assessment Please work in pairs: • Take a a full set of patient observations • Record observations on National Early Warning Score Chart
- Slides: 42