Table of Contents 1 Introduction 2 Main Changes
Table of Contents 1. Introduction 2. Main Changes 3. BLS in PALS 4. Algorithms 대한심폐소생협회
Introduction v In contrast to adults Ø Ø Ø Cardiac arrest is the terminal result of progressive respiratory failure or shock, also called an asphyxial arrest ith a variable period of systemic hypoxemia, hypercapnea, Asphyxia begins with a variable period of systemic hypoxemia, hypercapnea, and acidosis, progresses to bradycardia and hypotension, and culminates with cardiac arrest v VF or pulseless VT in children Ø Ø Approximately 5% to 15% of pediatric in-hospital and out-ofhospital cardiac arrests The incidence rises with age v Sudden Unexplained Deaths Ø Ø Sudden unexpected death in young people Channelopathy : myocyte ion channel abnormalities 대한심폐소생협회

Most Important Changes in PALS v Pulse check : deemphasized for healthcare providers v Cuffed endotracheal tube : safe and effective v Cricoid pressure : be modified or discontinued if it impedes ventilation v Monitoring capnography/capnometry Ø Ø To confirm proper endotracheal tube (and other advanced airway) position To assess and optimize quality of chest compressions v Dose of defibrillation : 2 J/kg initially, followed 4 J/kg v Oxygen : inspired oxygen should be titrated v New sections Ø Single ventricle, pulmonary hypertension v Victims of sudden death Ø Channelopathy 대한심폐소생협회

BLS during PALS v Chest compressions should be immediately started by one rescuer, while a second rescuer prepares to start ventilations with a bag and mask ventilation v The effectiveness of PALS is dependent on high-quality CPR, which requires an adequate compression rate (at least 100 compressions/min), an adequate compression depth (at least one third of the AP diameter of the chest or approximately 4 cm in infants and approximately 5 cm in children), allowing complete recoil of the chest after each compression, minimizing interruptions in compressions, and avoiding excessive ventilation v While one rescuer performs chest compressions and another performs ventilations, other rescuers should obtain a monitor/defibrillator, establish vascular access, and calculate and prepare the anticipated medications 대한심폐소생협회
Monitored Patients v Many in-hospital patients are monitored v Some have an advanced airway and are receiving mechanical ventilation v Indwelling arterial catheter Ø Ø Use the waveform as feedback to evaluate hand position and chest compression depth. Also be useful in identification of return of spontaneous circulation (ROSC) v End-tidal CO 2 (PETCO 2) Ø Ø Can be used to evaluate the quality of chest compressions Also provide an indication of ROSC 대한심폐소생협회
Respiratory Failure & Shock v Anticipate respiratory failure Ø Ø Ø Increased respiratory rate with signs of distress (eg, nasal flaring, retractions, seesaw breathing, or grunting) Inadequate respiratory rate, effort, or chest excursion (eg, diminished breath sounds or gasping) with depressed mentality Cyanosis with abnormal breathing with supplementary oxygen v Typical signs of compensated shock Ø Tachycardia, cool and pale distal extremities, prolonged (2 seconds) capillary refill (in warm ambient temperature), weak peripheral pulses compared with central pulses, normal SBP v Signs of inadequate end-organ perfusion develop Ø Depressed mental status, decreased urine output, metabolic acidosis, tachypnea, weak central pulses, deterioration in color (eg, mottling) 대한심폐소생협회
Hypotension v Hypotension Ø SBP less than 5 th percentile at various ages v SBP Ø Ø < < 60 70 70 90 mm mm Hg Hg in term neonates (0 to 28 days) in infants (1 month to 12 months) (2 age in years) in children 1 to 10 years in children 10 years of age 대한심폐소생협회
Airway v OPA or NPA Ø Ø Ø Help maintain an open airway by displacing the tongue or soft palate from the pharyngeal air passages Oropharyngeal airways are used in unresponsive victims who do not have a gag reflex Nasopharyngeal airways can be used in children who do have a gag reflex v LMA is acceptable when used by experienced providers to provide a patent airway and support ventilation v Oxygen Ø Ø Once the circulation is restored, monitor systemic oxygen saturation Titrate oxygen administration to maintain the oxyhemoglobin saturation 94% 대한심폐소생협회
Bag-Mask Ventilation v Effective, and safer than endotracheal tube ventilation for short periods during out-of-hospital resuscitation v Use the force and tidal volume to just make the chest rise visibly avoid excessive ventilation v Excessive ventilation Ø Ø Ø Increase intrathoracic pressure, impedes venous return, reducing CO and cerebral and coronary blood flow Cause air trapping/barotrauma in small airway obstruction Increase the risk of stomach inflation, regurgitation & aspiration. v Ventilate 1 breath every 6 to 8 seconds (8 to 10/minute) without interrupting compression for intubated child v With a perfusing rhythm and inadequate respiratory effort, give 1 breath every 3 to 5 seconds (12 to 20 breaths per minute), using the higher rate for the younger child 대한심폐소생협회
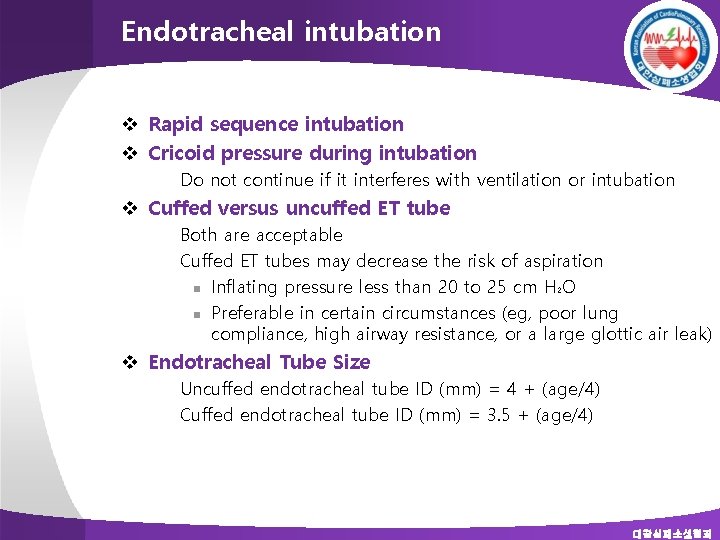
Endotracheal intubation v Rapid sequence intubation v Cricoid pressure during intubation Ø Do not continue if it interferes with ventilation or intubation v Cuffed versus uncuffed ET tube Ø Ø Both are acceptable Cuffed ET tubes may decrease the risk of aspiration n Inflating pressure less than 20 to 25 cm H 2 O n Preferable in certain circumstances (eg, poor lung compliance, high airway resistance, or a large glottic air leak) v Endotracheal Tube Size Ø Ø Uncuffed endotracheal tube ID (mm) = 4 + (age/4) Cuffed endotracheal tube ID (mm) = 3. 5 + (age/4) 대한심폐소생협회
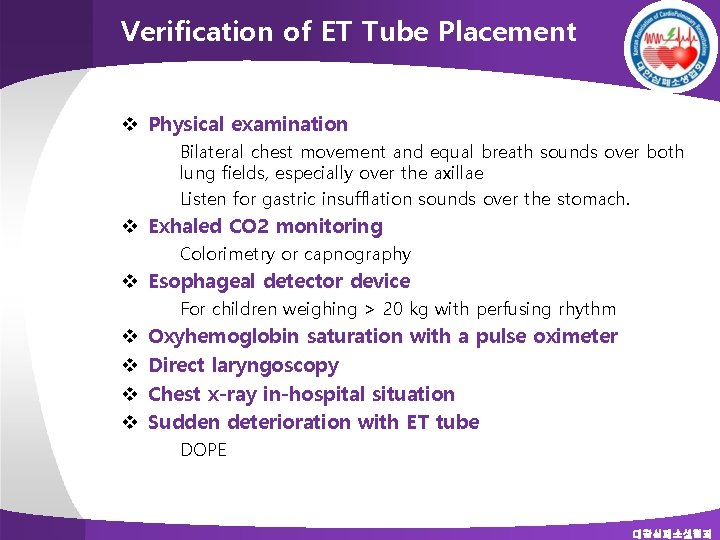
Verification of ET Tube Placement v Physical examination Ø Ø Bilateral chest movement and equal breath sounds over both lung fields, especially over the axillae Listen for gastric insufflation sounds over the stomach. v Exhaled CO 2 monitoring Ø Colorimetry or capnography v Esophageal detector device Ø v v For children weighing > 20 kg with perfusing rhythm Oxyhemoglobin saturation with a pulse oximeter Direct laryngoscopy Chest x-ray in-hospital situation Sudden deterioration with ET tube Ø DOPE 대한심폐소생협회
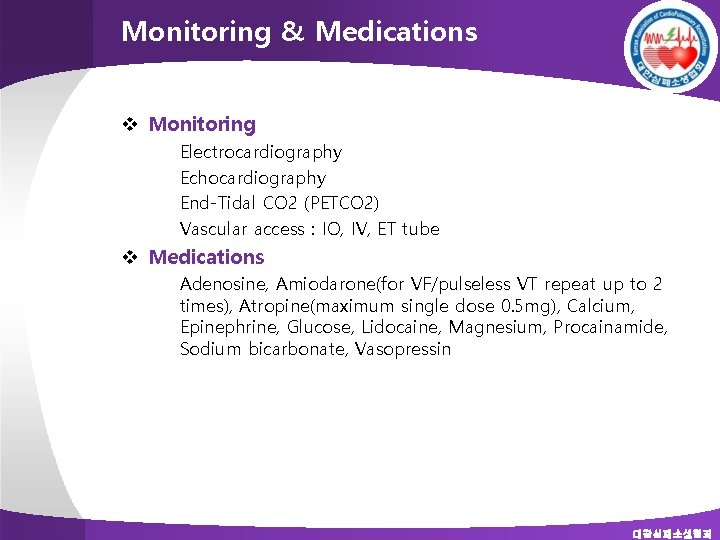
Monitoring & Medications v Monitoring Ø Ø Electrocardiography Echocardiography End-Tidal CO 2 (PETCO 2) Vascular access : IO, IV, ET tube v Medications Ø Adenosine, Amiodarone(for VF/pulseless VT repeat up to 2 times), Atropine(maximum single dose 0. 5 mg), Calcium, Epinephrine, Glucose, Lidocaine, Magnesium, Procainamide, Sodium bicarbonate, Vasopressin 대한심폐소생협회
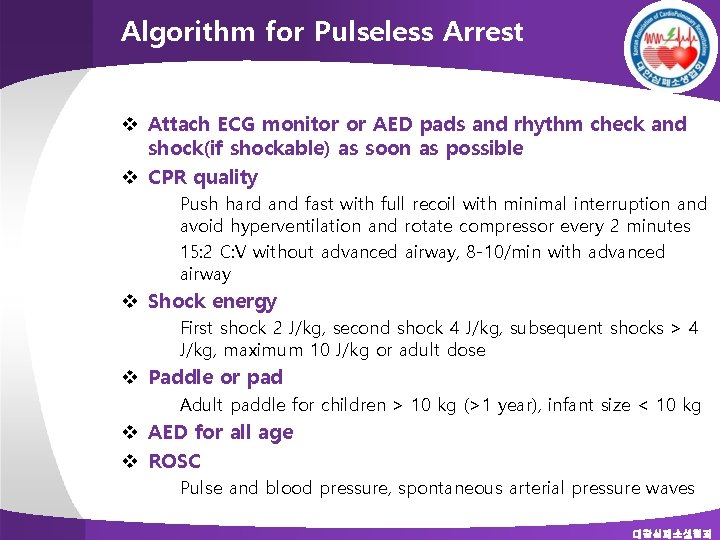
Algorithm for Pulseless Arrest v Attach ECG monitor or AED pads and rhythm check and shock(if shockable) as soon as possible v CPR quality Ø Ø Push hard and fast with full recoil with minimal interruption and avoid hyperventilation and rotate compressor every 2 minutes 15: 2 C: V without advanced airway, 8 -10/min with advanced airway v Shock energy Ø First shock 2 J/kg, second shock 4 J/kg, subsequent shocks > 4 J/kg, maximum 10 J/kg or adult dose v Paddle or pad Ø Adult paddle for children > 10 kg (>1 year), infant size < 10 kg v AED for all age v ROSC Ø Pulse and blood pressure, spontaneous arterial pressure waves 대한심폐소생협회
Algorithm for Tachycardia/Bradycardia v Cardiopulmonary compromise Ø Ø Ø Hypotension Acutely altered mental status Signs of shock v Bradycardia Ø Atropine for increased vagal tone or primary AV block n 0. 02 mg/kg(minimum 0. 1 maximum 0. 5 mg) n Repeat once v Criteria for QRS : 0. 09 second v For probable SVT Ø Adenosin 0. 1 mg/kg rapid bolus(maximum 6 mg) with second dose 0. 2 mg/kg(maximum 12 mg) 대한심폐소생협회
Special Resuscitation Situations v Septic shock Ø Ø Ø Isotonic crystalloid solution for initial fluid Central venous oxygen saturation 70% Early assited ventilation Etomidate : do not use routinely in septic shock Hypertonic saline ? v Single ventricle Ø Ø Ø Heparin may be considered with systemic-pulmonary shunt or RV-PA shunt Target saturation after CPR : 80% PETCO 2 may not be reliable v Pulmonary hypertension Ø Ø Reinstitute IV or inhaled medication for pulmonary HT i. NO or aerosolized prostacyclin 대한심폐소생협회
- Slides: 16