Systemic sclerosis scleroderma Systemic sclerosis SSc SSc is










- Slides: 19
Systemic sclerosis (scleroderma)
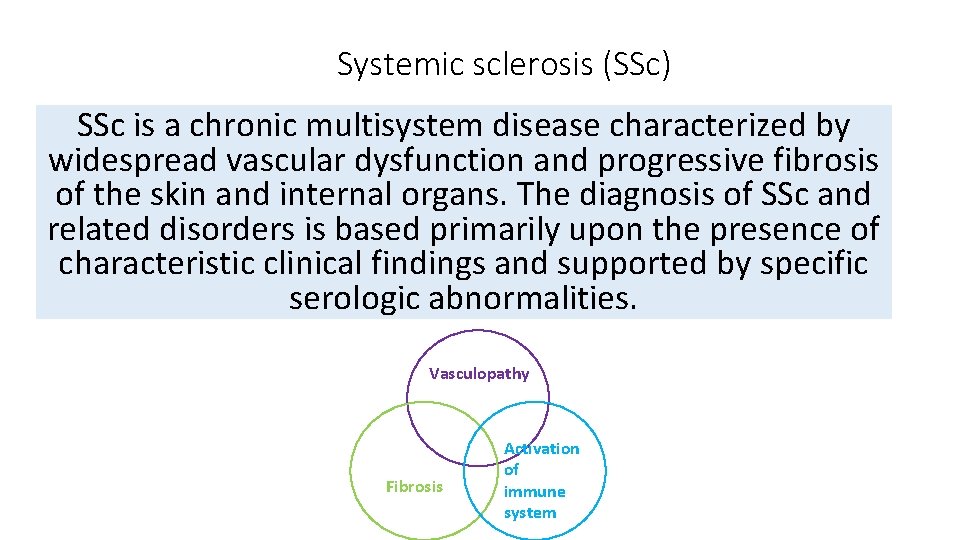
Systemic sclerosis (SSc) SSc is a chronic multisystem disease characterized by widespread vascular dysfunction and progressive fibrosis of the skin and internal organs. The diagnosis of SSc and related disorders is based primarily upon the presence of characteristic clinical findings and supported by specific serologic abnormalities. Vasculopathy Fibrosis Activation of immune system
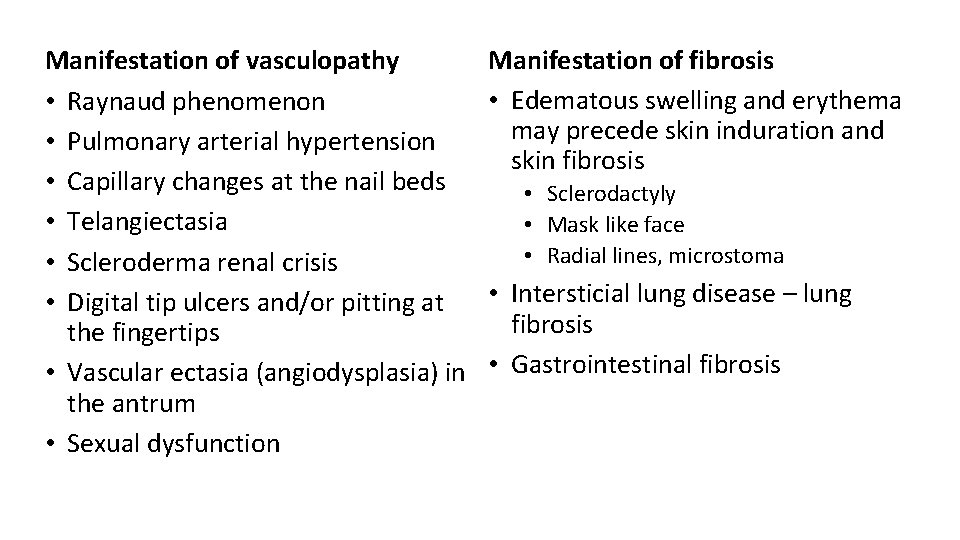
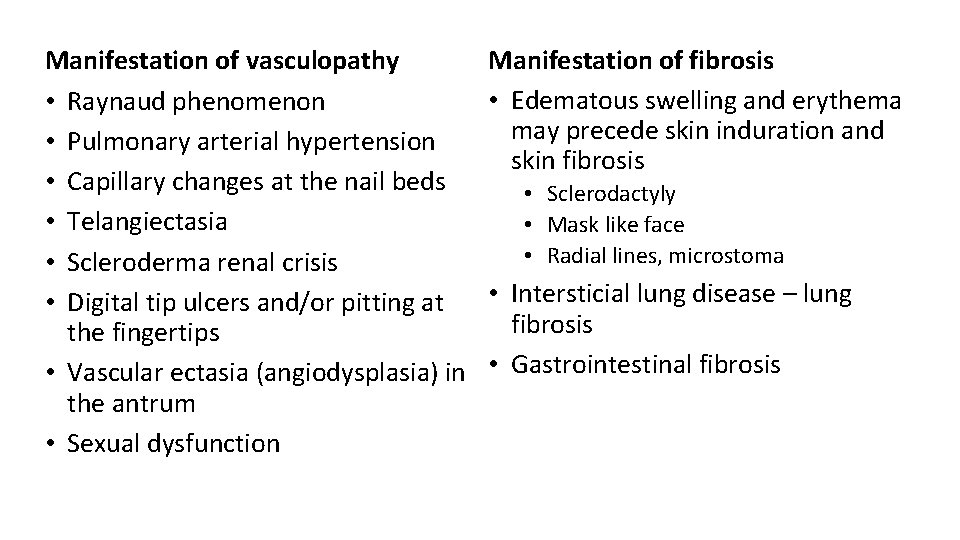
Manifestation of vasculopathy • Raynaud phenomenon • Pulmonary arterial hypertension • Capillary changes at the nail beds • Telangiectasia • Scleroderma renal crisis • Digital tip ulcers and/or pitting at the fingertips • Vascular ectasia (angiodysplasia) in the antrum • Sexual dysfunction Manifestation of fibrosis • Edematous swelling and erythema may precede skin induration and skin fibrosis • Sclerodactyly • Mask like face • Radial lines, microstoma • Intersticial lung disease – lung fibrosis • Gastrointestinal fibrosis
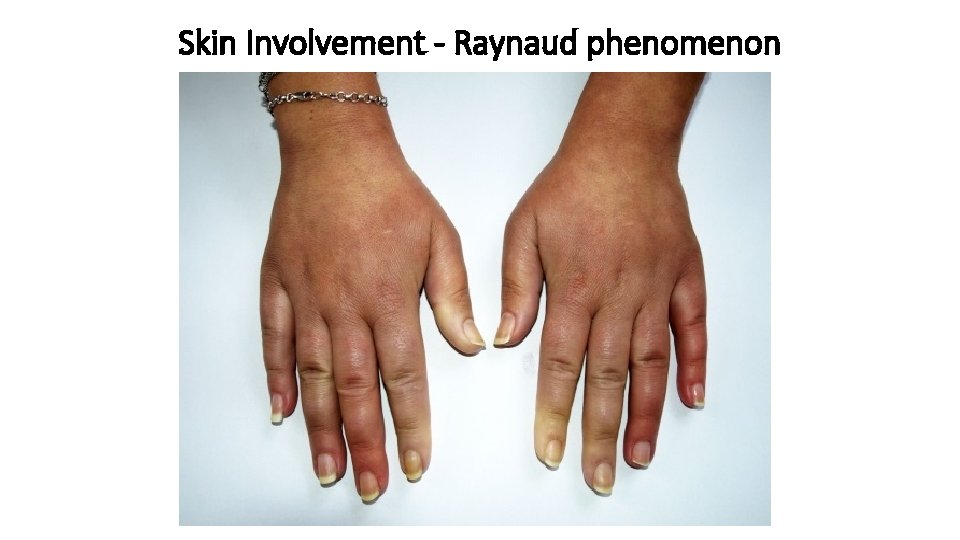
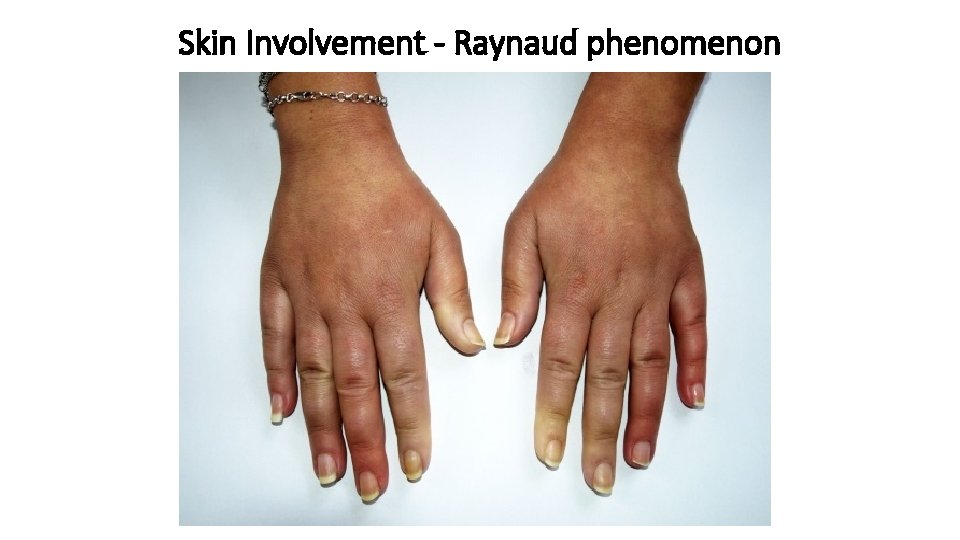
Skin Involvement - Raynaud phenomenon

Skin Involvement – Sclerodactyly, ulceration

Skin Involvement – Skin ulceration, amputation

Skin Involvement – mask face, radial lines, microstoma

Skin Involvement - Calcinosis cutis
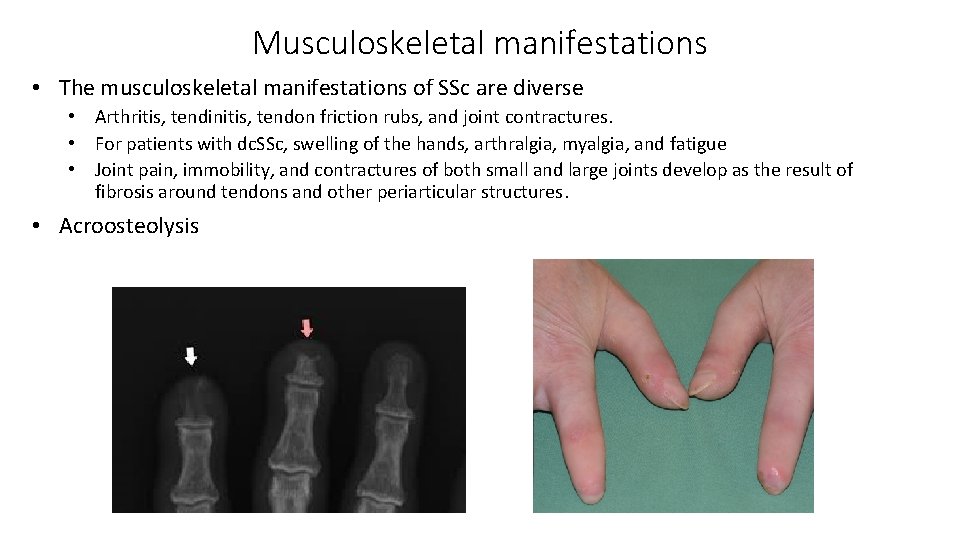
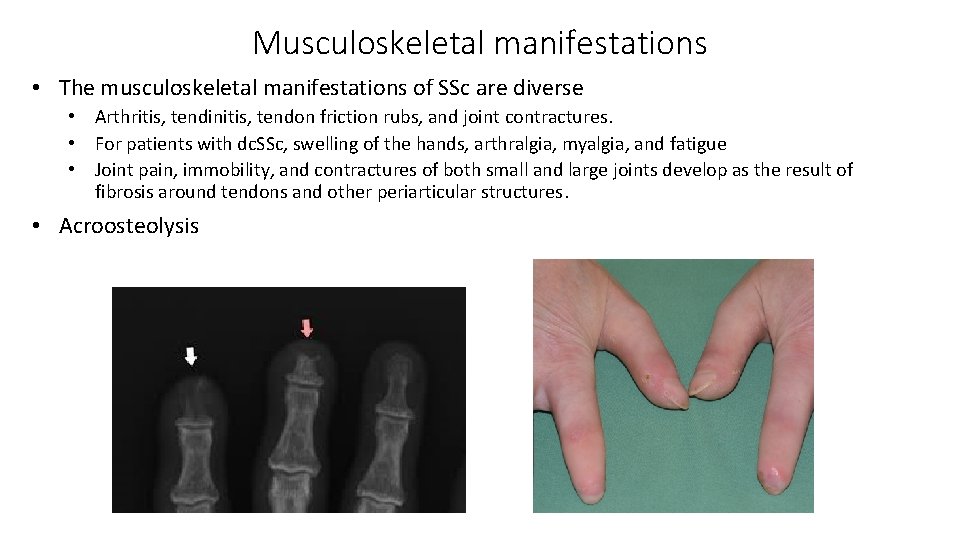
Musculoskeletal manifestations • The musculoskeletal manifestations of SSc are diverse • Arthritis, tendinitis, tendon friction rubs, and joint contractures. • For patients with dc. SSc, swelling of the hands, arthralgia, myalgia, and fatigue • Joint pain, immobility, and contractures of both small and large joints develop as the result of fibrosis around tendons and other periarticular structures. • Acroosteolysis
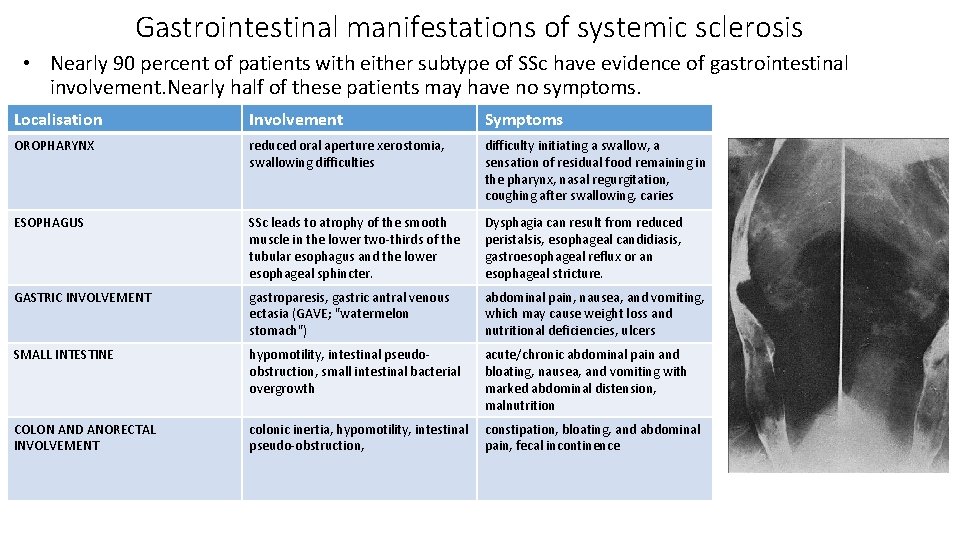
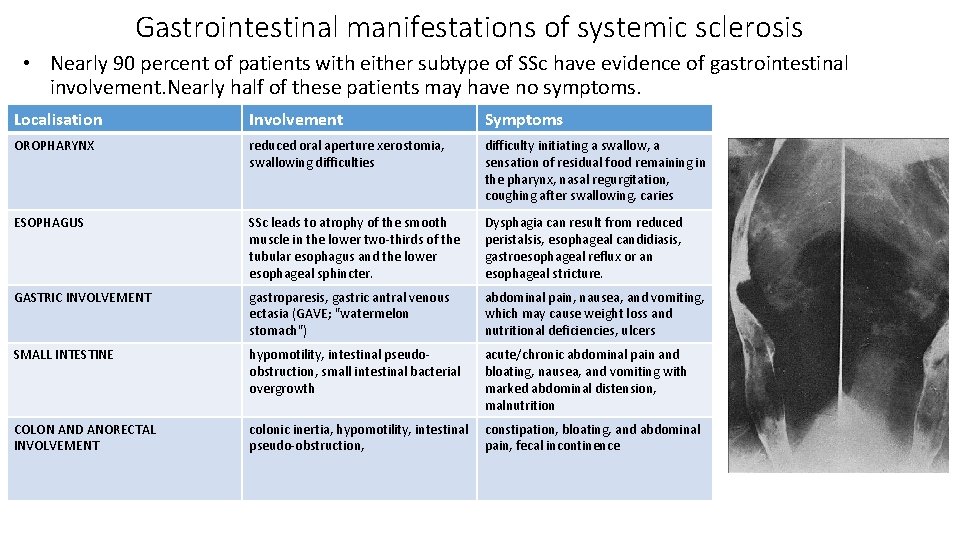
Gastrointestinal manifestations of systemic sclerosis • Nearly 90 percent of patients with either subtype of SSc have evidence of gastrointestinal involvement. Nearly half of these patients may have no symptoms. Localisation Involvement Symptoms OROPHARYNX reduced oral aperture xerostomia, swallowing difficulties difficulty initiating a swallow, a sensation of residual food remaining in the pharynx, nasal regurgitation, coughing after swallowing, caries ESOPHAGUS SSc leads to atrophy of the smooth muscle in the lower two-thirds of the tubular esophagus and the lower esophageal sphincter. Dysphagia can result from reduced peristalsis, esophageal candidiasis, gastroesophageal reflux or an esophageal stricture. GASTRIC INVOLVEMENT gastroparesis, gastric antral venous ectasia (GAVE; "watermelon stomach") abdominal pain, nausea, and vomiting, which may cause weight loss and nutritional deficiencies, ulcers SMALL INTESTINE hypomotility, intestinal pseudoobstruction, small intestinal bacterial overgrowth acute/chronic abdominal pain and bloating, nausea, and vomiting with marked abdominal distension, malnutrition COLON AND ANORECTAL INVOLVEMENT colonic inertia, hypomotility, intestinal pseudo-obstruction, constipation, bloating, and abdominal pain, fecal incontinence

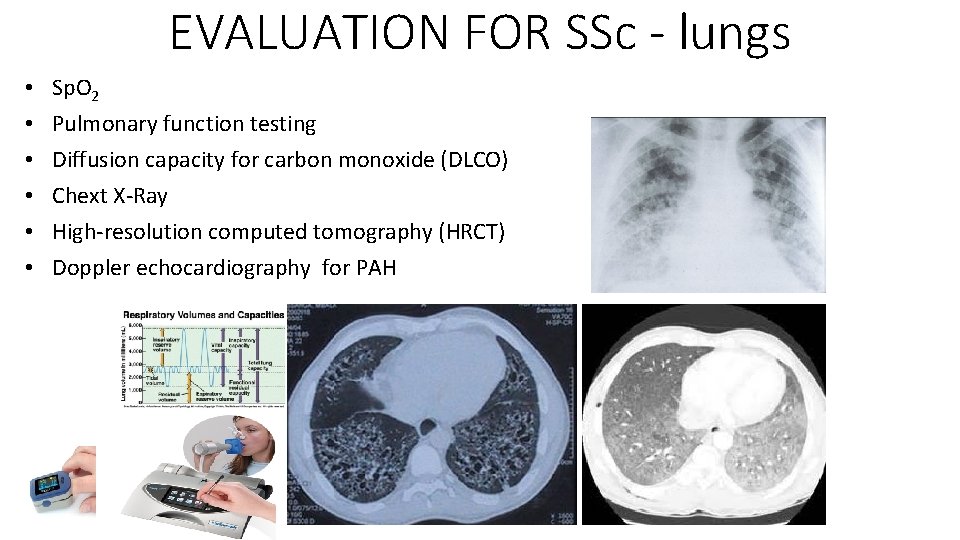
Pulmonary complications of systemic sclerosis • Pulmonary involvement occurs in over 70% percent of patients with systemic sclerosis • Interstitial lung disease - typically presents with the subacute onset of dyspnea on exertion and sometimes nonproductive cough • The radiographic, and pathologic features of SSc-associated ILD • nonspecific interstitial pneumonia (NSIP) • usual interstitial pneumonia (UIP) • Pulmonary fibrosis • Pulmonary arterial hypertension (5 -27%) • primary – without lung involvement • secondary associated with ILD • According the m. PAP: light 25 -35 mm Hg, medium 36 -45 mm Hg, severe above 45 mm Hg Among patients with SSc and PAH, dyspnea on exertion is the most common initial symptom, but early PAH can be asymptomatic. Patients with advanced PAH may have chest pain due to right ventricular angina, and near-syncope or syncope on exertion due to reduced cardiac reserve.

Renal disease in systemic sclerosis - scleroderma renal crisis • Scleroderma renal crisis 10% • Abrupt onset of moderate to severe hypertension that is typically associated with an increase in plasma renin activity • Acute kidney injury • Urinalysis that is normal or reveals only mild proteinuria with few cells or casts

Major disease subsets Disease subtype Diffuse cutaneous systemic sclerosis (dc. SSc) Limited cutaneous systemic sclerosis (lc. SSc) Systemic sclerosis sine scleroderma Systemic sclerosis with overlap syndrome Extent of skin involvement and the accompanying pattern of internal organ involvement Skin sclerosis extends proximally to the upper arms, thighs, and/or trunk. Patients are more likely to have a rapid progression of skin thickening, early development of lung fibrosis, increased risk of renal crisis and cardiac involvement. Skin sclerosis distal to the elbows and knees and to a lesser extent, the face and neck, while the trunk and proximal extremities are spared. Raynaud phenomenon, mucocutaneous telangiectasia followed by a later onset of PAH. Could be present CREST syndrome (Calcinosis cutis, Raynaud phenomenon, Esophageal dysmotility, Sclerodactyly, Telangiectasia). A small subset of patients have no detectable skin involvement but have clinical organ features of systemic sclerosis along with autoantibodies specific for SSc. Patients with SSc may have overlap or features of another systemic rheumatic disease such as systemic lupus erythematosus, rheumatoid arthritis, polymyositis or Sjögren's syndrome

Antibodies and phenotype of SSc Antigen Nucleus (ANA) Antitopoisomerase I (anti-Scl-70) Anticentromere antibody (ACA) Presence 95% Form SSc Association with clinical manifestation lc. SSc i dc. SSc 15% - 25% dc. SSc interstitial lung disease, heart involvement 10% - 20% lc. SSc PAH, CREST syndrome, calcinosis

EVALUATION FOR SSc – vasculopathy • Abnormal nailfold capillaroscopy with scleroderma pattern. This is particularly useful for clinicians skilled at identifying characteristic nailfold capillary abnormalities, such as dilated capillary loops, capillary dropout, microhemorrhages, and architectural derangement. • Raynaud phenomenon – cold test
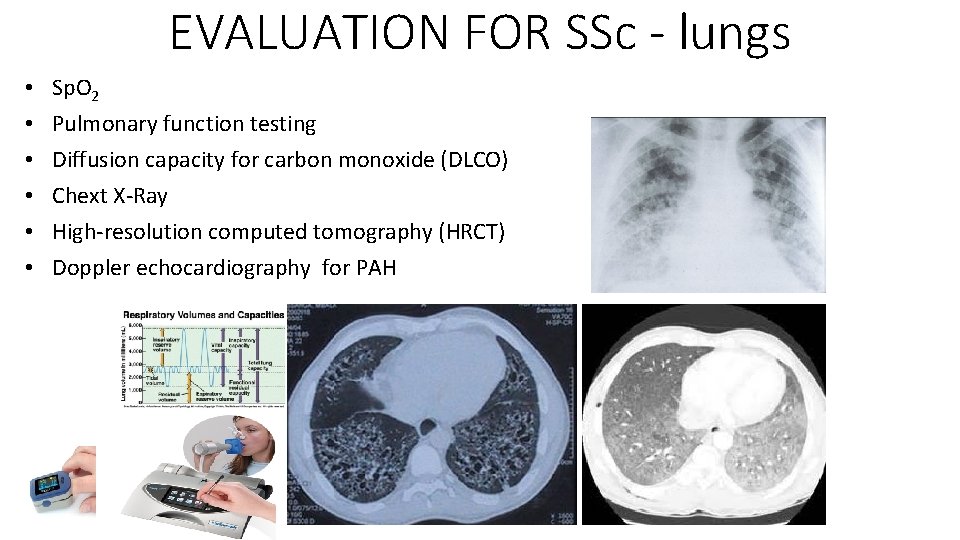
EVALUATION FOR SSc - lungs • • • Sp. O 2 Pulmonary function testing Diffusion capacity for carbon monoxide (DLCO) Chext X-Ray High-resolution computed tomography (HRCT) Doppler echocardiography for PAH
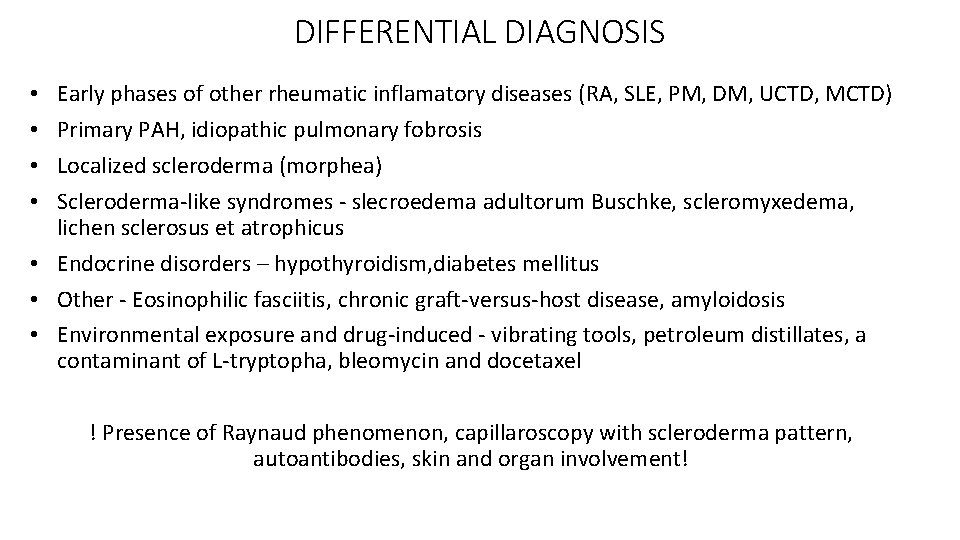
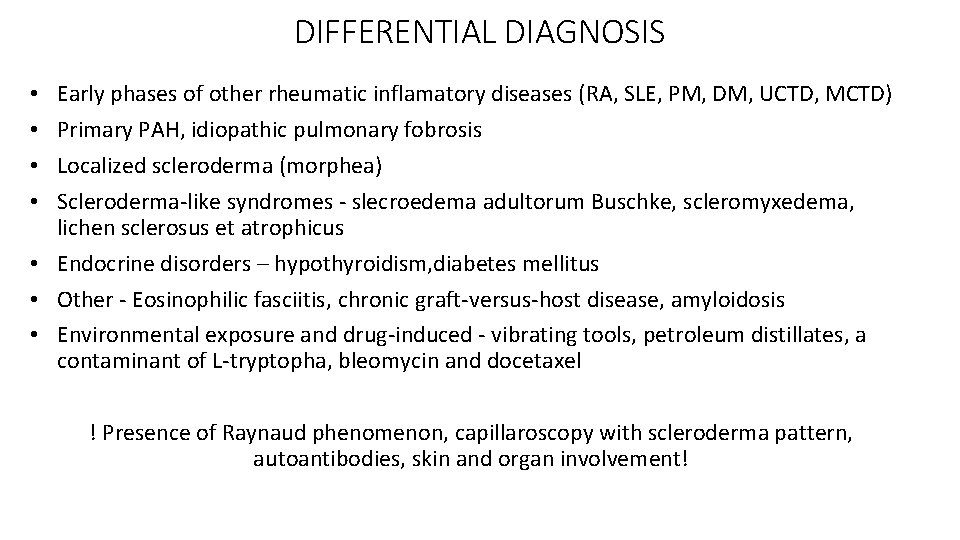
DIFFERENTIAL DIAGNOSIS Early phases of other rheumatic inflamatory diseases (RA, SLE, PM, DM, UCTD, MCTD) Primary PAH, idiopathic pulmonary fobrosis Localized scleroderma (morphea) Scleroderma-like syndromes - slecroedema adultorum Buschke, scleromyxedema, lichen sclerosus et atrophicus • Endocrine disorders – hypothyroidism, diabetes mellitus • Other - Eosinophilic fasciitis, chronic graft-versus-host disease, amyloidosis • Environmental exposure and drug-induced - vibrating tools, petroleum distillates, a contaminant of L-tryptopha, bleomycin and docetaxel • • ! Presence of Raynaud phenomenon, capillaroscopy with scleroderma pattern, autoantibodies, skin and organ involvement!
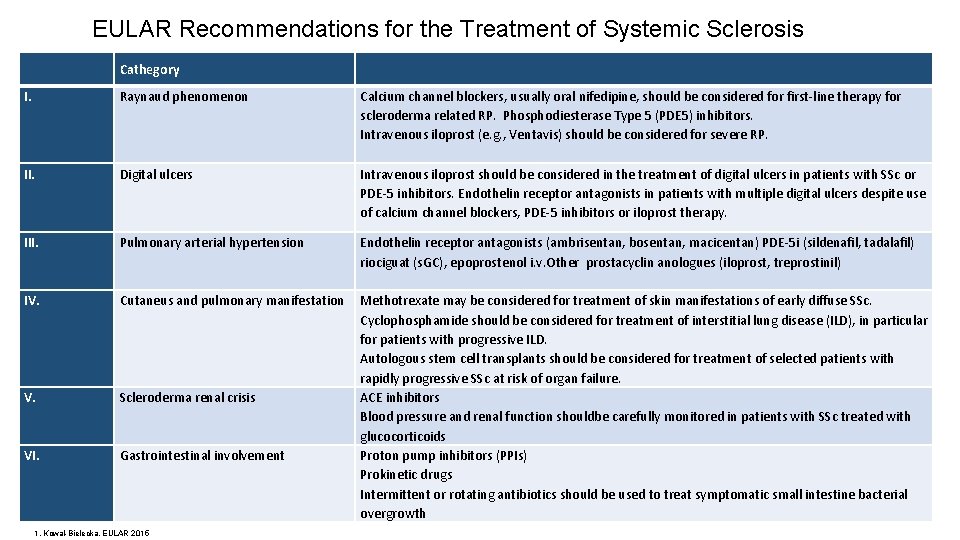
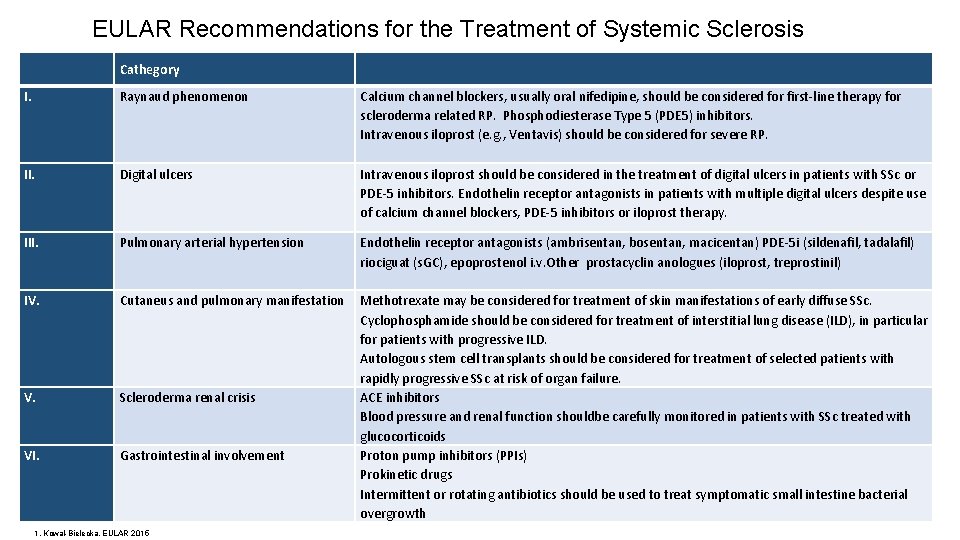
EULAR Recommendations for the Treatment of Systemic Sclerosis Cathegory I. Raynaud phenomenon Calcium channel blockers, usually oral nifedipine, should be considered for first-line therapy for scleroderma related RP. Phosphodiesterase Type 5 (PDE 5) inhibitors. Intravenous iloprost (e. g. , Ventavis) should be considered for severe RP. II. Digital ulcers Intravenous iloprost should be considered in the treatment of digital ulcers in patients with SSc or PDE-5 inhibitors. Endothelin receptor antagonists in patients with multiple digital ulcers despite use of calcium channel blockers, PDE-5 inhibitors or iloprost therapy. III. Pulmonary arterial hypertension Endothelin receptor antagonists (ambrisentan, bosentan, macicentan) PDE-5 i (sildenafil, tadalafil) riociguat (s. GC), epoprostenol i. v. Other prostacyclin anologues (iloprost, treprostinil) IV. Cutaneus and pulmonary manifestation V. Scleroderma renal crisis VI. Gastrointestinal involvement Methotrexate may be considered for treatment of skin manifestations of early diffuse SSc. Cyclophosphamide should be considered for treatment of interstitial lung disease (ILD), in particular for patients with progressive ILD. Autologous stem cell transplants should be considered for treatment of selected patients with rapidly progressive SSc at risk of organ failure. ACE inhibitors Blood pressure and renal function shouldbe carefully monitored in patients with SSc treated with glucocorticoids Proton pump inhibitors (PPIs) Prokinetic drugs Intermittent or rotating antibiotics should be used to treat symptomatic small intestine bacterial overgrowth 1. Kowal-Bielecka, EULAR 2015
