Systemic Retinoids in Dermatology By Dr Hassan Ibrahim
Systemic Retinoids in Dermatology
By Dr. Hassan Ibrahim Prepared by Soher Abd El -Hamid Ali M. B. , B. Ch Demonstrator at Qena Faculty of Medicine, South Valley University
WHAT WE WILL TAKE ABOUT? Definition. o Pharmacokinetics. o Phramacodynamic. o Safety profile of Retinoids. o Monitoring Guidelines. o Contraindications. o Retinoid drug interactions. o
WHAT ARE RETINOIDS? q The retinoids are a class of chemical compounds that are related chemically to vitamin A. Retinoids are used in medicine, primarily to regulate epithelial cell growth.
q Vitamin A cannot be syntheized in vivo must be acquired through diet. q It is important for vision, reproduction, regulation of emberyogenic development, promotion of general growth and modulation of immunoresponse. q Vitamin A deficiency induce epidermal hyperkeratosis, squamous metaplasia of mucous membranes, various keratinization disorders and certain precancerous conditions(Germain P et al. , 2006, Davidovici BB et al. , 2007).
q In mammals, vitamin A exists in interconvertible forms as Ø Retinol (vitamin A alcohol): the most potent vitamin A analog and represent the main dietary source, transport and storage form. Ø Retinal (vitamin A aldehyde): has role in visual cycle. Ø Retinoic acid (vitamin A acid): the most oxidized and water-soluble form, less toxic than its parent compound (Germain P et al. , 2006).
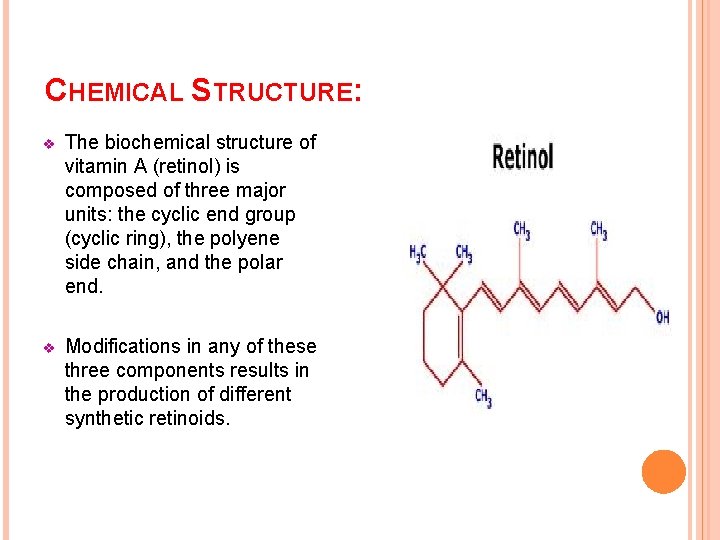
CHEMICAL STRUCTURE: v The biochemical structure of vitamin A (retinol) is composed of three major units: the cyclic end group (cyclic ring), the polyene side chain, and the polar end. v Modifications in any of these three components results in the production of different synthetic retinoids.
q o There are three generations of Retinoids: First generation retinoids (monoaromatic) : which include , tretinoin (all-trans RA), isotretinoin (13 -cis RA) and alitretinoin (9 -cis. RA). o Second generation (monoaromatic) retinoids: which include etretinate and its metabolite acitretin. o Third generation (polyaromatic) retinoids: which include tazarotene , bexarotene and Adapalene.
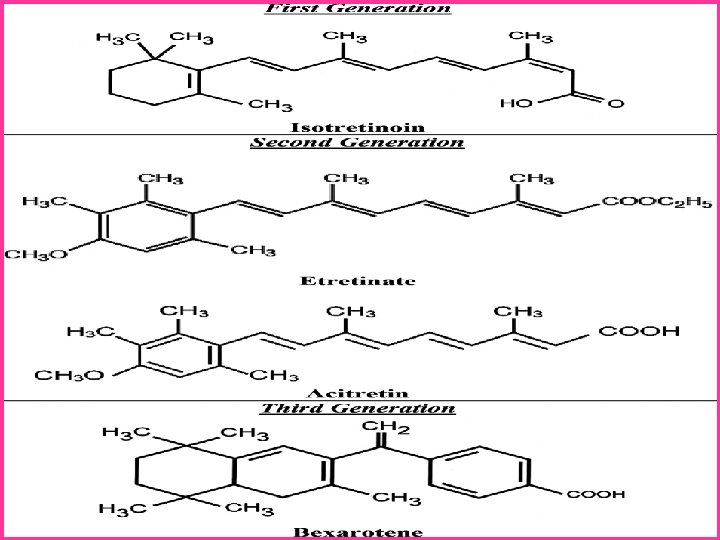
o First and Second generation retinoids are able to bind with several retinoid receptors due to the flexibility imparted by their alternating single and double bonds. o Third generation retinoids are less flexible than First and Second generation retinoids and therefore, interact with fewer retinoid receptors (Patton TJ et al. , 2007).
Pharmacokinetics
ABSORPTION AND DISTRIBUTION: o The oral bioavailability of retinoid is enhanced with food intake, effect of fatty meal is great with acitretin and bexarotene. o In serum, transported by plasma proteins. o Stored in liver. o Isotretinoin, acitretin and bexarotene are water soluble, there is very little lipid deposition, they are undetectable in serum within 1 month after stopping therapy.
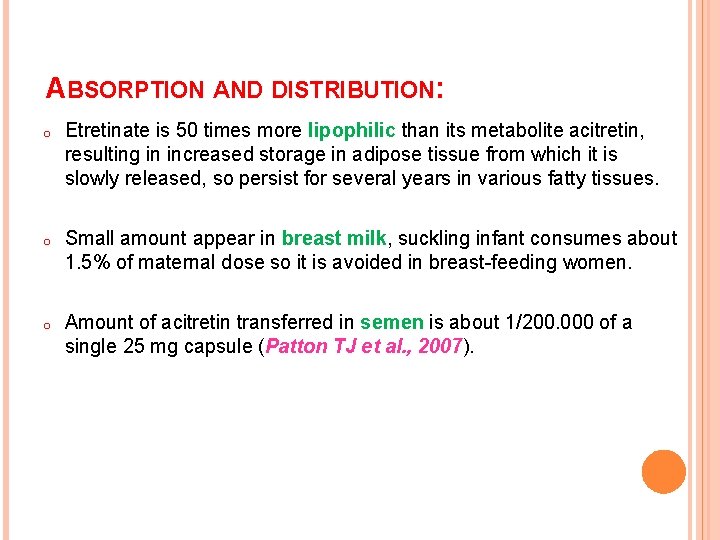
ABSORPTION AND DISTRIBUTION: o Etretinate is 50 times more lipophilic than its metabolite acitretin, resulting in increased storage in adipose tissue from which it is slowly released, so persist for several years in various fatty tissues. o Small amount appear in breast milk, suckling infant consumes about 1. 5% of maternal dose so it is avoided in breast-feeding women. o Amount of acitretin transferred in semen is about 1/200. 000 of a single 25 mg capsule (Patton TJ et al. , 2007).
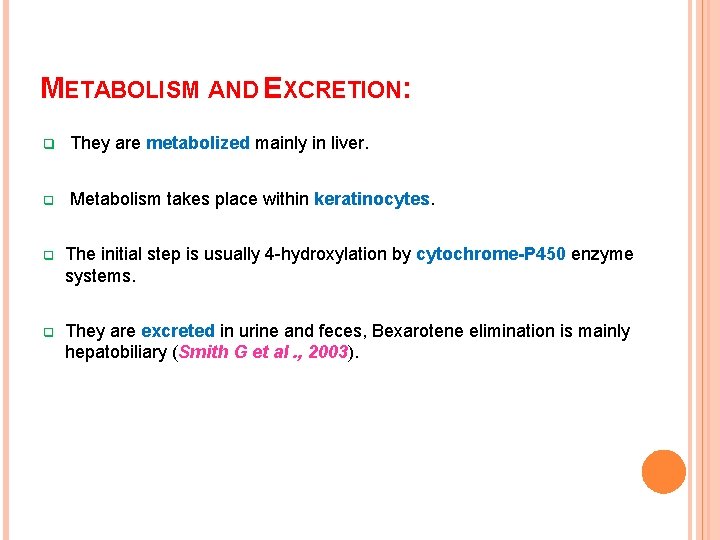
METABOLISM AND EXCRETION: q They are metabolized mainly in liver. q Metabolism takes place within keratinocytes. q The initial step is usually 4 -hydroxylation by cytochrome-P 450 enzyme systems. q They are excreted in urine and feces, Bexarotene elimination is mainly hepatobiliary (Smith G et al. , 2003).
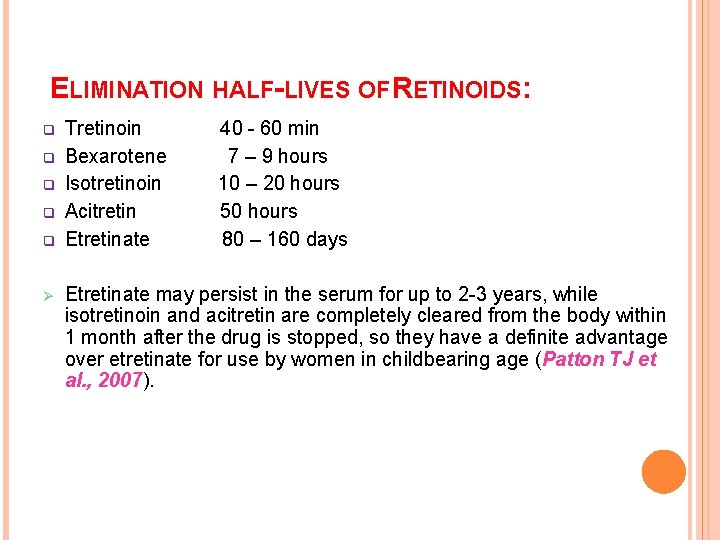
ELIMINATION HALF-LIVES OF RETINOIDS: q q q Ø Tretinoin Bexarotene Isotretinoin Acitretin Etretinate 40 - 60 min 7 – 9 hours 10 – 20 hours 50 hours 80 – 160 days Etretinate may persist in the serum for up to 2 -3 years, while isotretinoin and acitretin are completely cleared from the body within 1 month after the drug is stopped, so they have a definite advantage over etretinate for use by women in childbearing age (Patton TJ et al. , 2007).
Pharmacodynamic

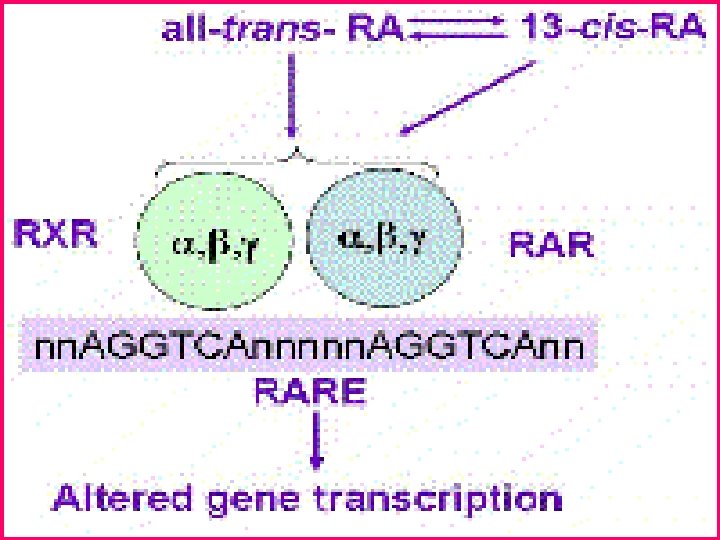
q Retinoids in general are lipoosoluble materials and they will pass easily through cell membranes. q Within the nucleus, retinoids bind to specific receptors, retinoic acid receptors (RAR α, β and γ) and retinoid X receptors (RXR α, β and γ). q Alternative splicing of each of these receptors generates further diversity (the subtypes being known as RAR-α 1, RAR-α 2 etc. ) (Craven NM et al. , 1996). q All-trans retinoic acid is the endogenous ligand for the RARs whilst 9 -cis retinoic acid is the endogenous ligand for the RXRs.
q These receptors bind to specific elements of DNA, known as response elements, within the regulatory regions of numerous genes; this interaction may increase or decrease transcription of the gene. q The end result of these processes acting on numerous different genes is that retinoids demonstrate a tendency to normalize keratinocyte differentiation in diverse circumstances where this is disturbed (Smith G et al. , 2003).
q The receptors most abundantly expressed in the epidermis are RAR-γ and RXR-α, while RAR-α and RXR-β are present at relatively low levels.
Retinoids in dermatology can be classified into: Topical Retinoids Systemic Retinoids
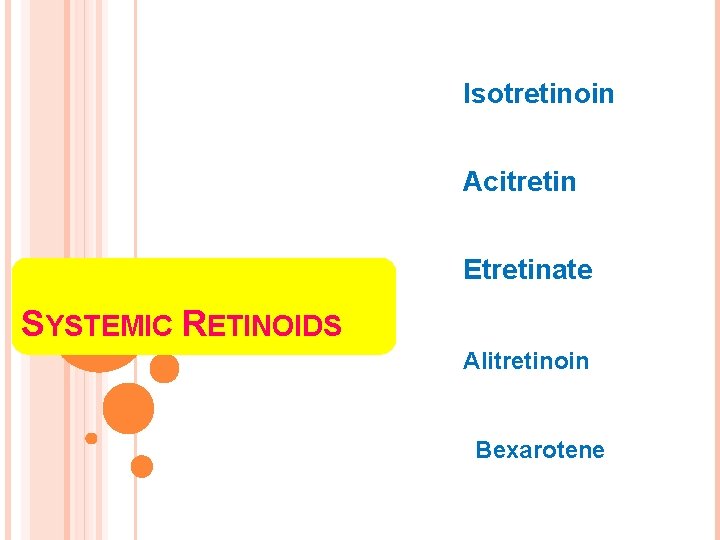
Isotretinoin Acitretin Etretinate SYSTEMIC RETINOIDS Alitretinoin Bexarotene
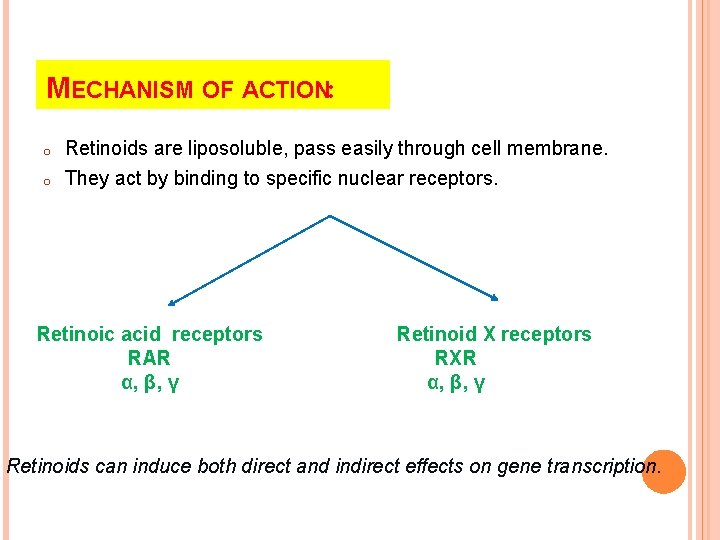
MECHANISM OF ACTION: o o Retinoids are liposoluble, pass easily through cell membrane. They act by binding to specific nuclear receptors. Retinoic acid receptors RAR α, β, γ Retinoid X receptors RXR α, β, γ Retinoids can induce both direct and indirect effects on gene transcription.
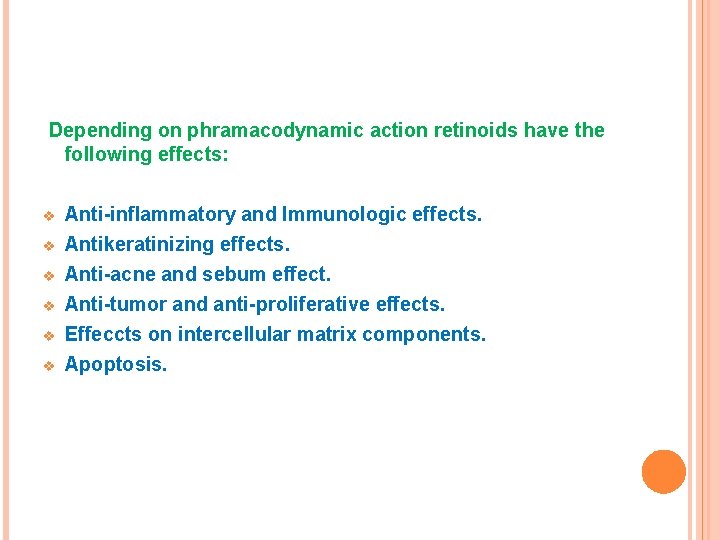
Depending on phramacodynamic action retinoids have the following effects: v v v Anti-inflammatory and Immunologic effects. Antikeratinizing effects. Anti-acne and sebum effect. Anti-tumor and anti-proliferative effects. Effeccts on intercellular matrix components. Apoptosis.
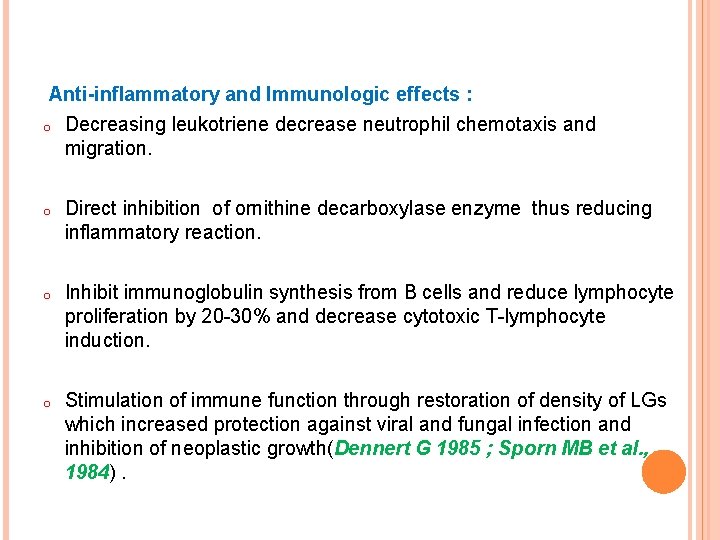
Anti-inflammatory and Immunologic effects : o Decreasing leukotriene decrease neutrophil chemotaxis and migration. o Direct inhibition of ornithine decarboxylase enzyme thus reducing inflammatory reaction. o Inhibit immunoglobulin synthesis from B cells and reduce lymphocyte proliferation by 20 -30% and decrease cytotoxic T-lymphocyte induction. o Stimulation of immune function through restoration of density of LGs which increased protection against viral and fungal infection and inhibition of neoplastic growth(Dennert G 1985 ; Sporn MB et al. , 1984).
Antikeratinizing effects: o Retinoids modulate the expression of keratin. o They down regulate the proliferative keratin K 6, K 16. o Decrease in epidermal thickness and keratinocyte proliferation. o Enhance keratinocyte differentiation. o Decreasing number of desmosomes (Elias PM et al. , 1981).
Anti-acne and sebum effect: o They inhibit sebocyte proliferation in a dose and time dependent manner. o Isotretinoin is the most potent inhibitor of lipid synthesis. o Isotretinoin produce 80% reduction in dihydrotestosterone.
Anti-acne and sebum effect: o Induce normalization of abnormal keratinization so decrease comedo formation. o Reduce sebum production so inhibit growth of propinobacterium acne. o Inhibit neutrophil chemotaxis (Dubertret L et al. , 1982 ; Orfanos CE et al. , 1983).
Apoptosis: o Retinoid-induced apoptosis involves regulation of expression of apoptosis-linked gene product BCL 2. o o Activation of tumor suppression proteins p 53. Activation of Caspase proteolytic activity. This is important antineoplastic role of retinoids (Fields AL et al. , 2007 ; Garattini E et al. , 2007).
Anti-tumor and anti-proliferative effects: o Retinoids directly inhibit ornithine decarboxylase enzyme and this decrease inflammatory hyperplasia. o Inhibit epidermal growth factor binding to keratinocytes so decrease their proliferation (Gouveia J et al. , 1982).
Effeccts on intercellular matrix components: o In normal skin, increase mucopolysaccharides, collagen, fibronectin synthesis, and decrease in collagenase production. o At nonphysiologic concentration, Retinoids inhibit fibroblast proliferation, decrease synthesis of type I and III collagen, so in high concentration may interfere with wound healing. o They inhibit collagenase activity which suggest theoretic efficacy in recessive DEB.
Other Retinoid effects: o Modulate infection caused by cytomegalovirus, Epstein Barr virus and human papilloma virus. o Retinoids have a role in hair growth.
ISOTRETINOIN Ø Isotretinoin is an RAR agonist. Clinical indications: Acne ü Severe forms of acne (such as nodular or conglobate acne or inflammatory acne at risk of permanent scarring, acne fulminans) and moderate acne. ü The recommended dose is 0. 5 -1 mg/kg bw/day for 4 -5 months with cumulative dose 120 -150 mg/kg (Layton AM et al 1993 ; Stainforth JM et al. , 1993).
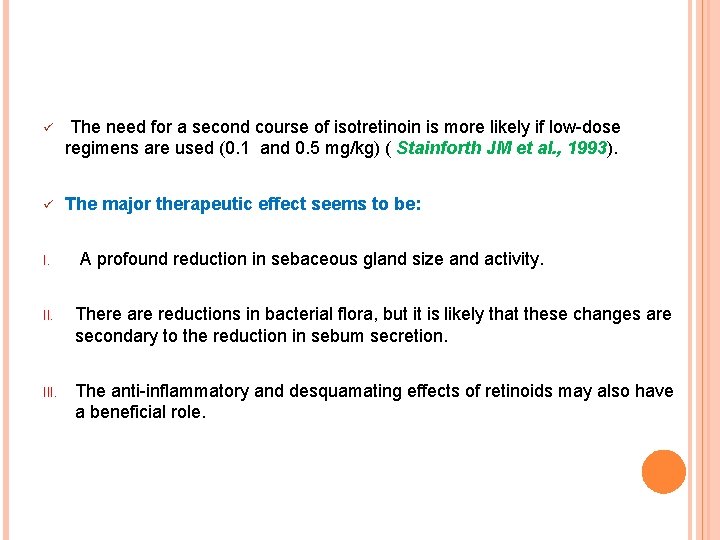
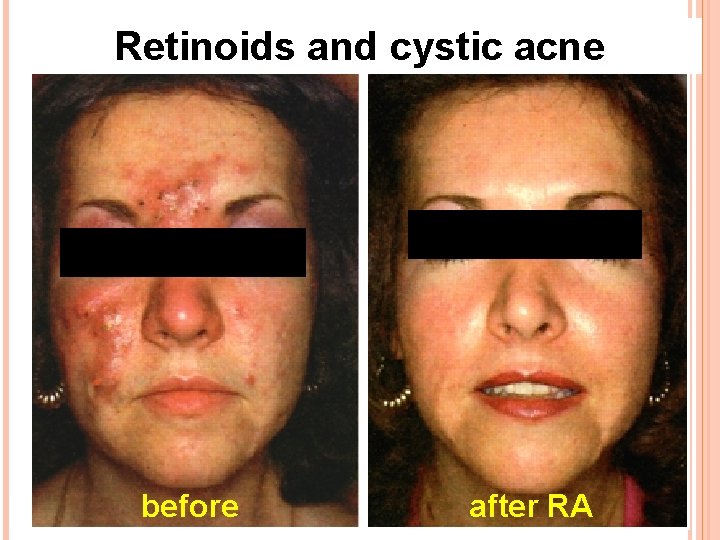
ü The need for a second course of isotretinoin is more likely if low-dose regimens are used (0. 1 and 0. 5 mg/kg) ( Stainforth JM et al. , 1993). ü The major therapeutic effect seems to be: I. A profound reduction in sebaceous gland size and activity. II. There are reductions in bacterial flora, but it is likely that these changes are secondary to the reduction in sebum secretion. III. The anti-inflammatory and desquamating effects of retinoids may also have a beneficial role.
Retinoids and cystic acne before after RA
Systemic dosing of RA and cystic acne before after RA
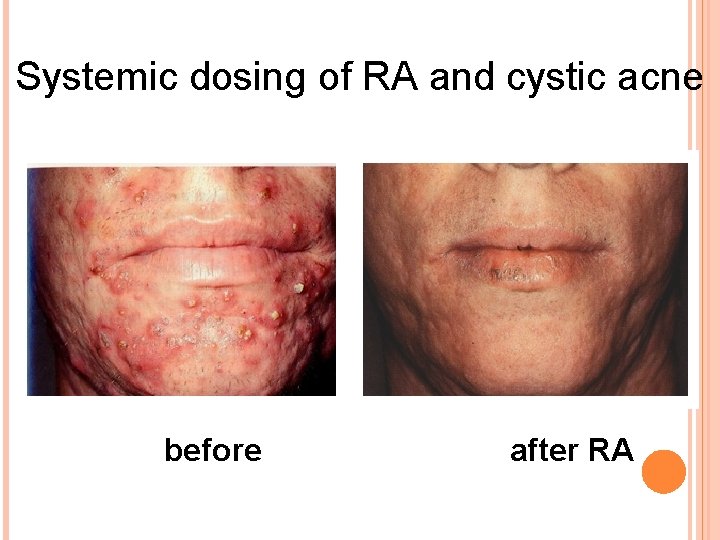
Rosacea and seborrhoea: ü Isotretinoin at a dose of 0. 5 mg/kg bw/day for 20 weeks, not only papules and pustules, but also seborrhoea, rhinophyma, oedema and erythema have been improved considerably ( Hoting E et al. , 1986). ü In severe seborrhoea : isotretinoin (5 mg/day or less) used ; mean sebaceous gland size and sebum production were both reduced 50% or more (Geissler SE et al. , 2003).
Gram-negative folliculitis: Isotretinoin is the treatment of choice for Gram-negative folliculitis (James WD et al. , 1985 ; Böni R et al. , 2003) Dissecting cellulitis of the scalp: ü Success has been observed in treating this refractory inflammatory scalp dermatosis with isotretinoin alone and in combination with rifampicin (Scerri L et al. , 1996 ; Georgala S et al. , 2008)
Disorders of keratinization: ü A wide range of disorders of keratinization has been found to be responsive to isotretinoin. ü In Europe, however, this group of disorders is now usually treated with acitretin. ü In women who may be contemplating future pregnancy, isotretinoin offers the advantage that it is cleared from the body much more quickly than acitretin and thus pregnancy need not be delayed for 2 to 3 years after discontinuing treatment. The management of Behçet's disease (Sharaquie KE et al. , 2013).
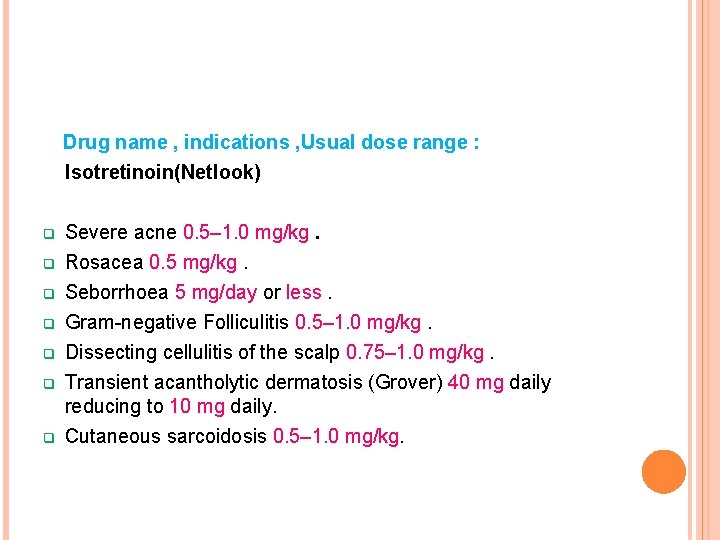
Drug name , indications , Usual dose range : Isotretinoin(Netlook) q q q q Severe acne 0. 5– 1. 0 mg/kg. Rosacea 0. 5 mg/kg. Seborrhoea 5 mg/day or less. Gram-negative Folliculitis 0. 5– 1. 0 mg/kg. Dissecting cellulitis of the scalp 0. 75– 1. 0 mg/kg. Transient acantholytic dermatosis (Grover) 40 mg daily reducing to 10 mg daily. Cutaneous sarcoidosis 0. 5– 1. 0 mg/kg.
ACITRETIN Ø Ø Acitretin, the hydrolysis product and active metabolite of etretinate, is an RAR agonist. Its activity is very similar to etretinate (Griffiths CEM et al. , 2000).
ETRETINATE (TEGASON) Ø Is 50 times more lipophilic than acitretin and, with an elimination half-life of more than 100 days (cf. 2 days for acitretin), can remain stored in body fat for up to 2 years after discontinuation of treatment. Because of the teratogenicity of retinoids this was a major disadvantage. Ø Because it is lipophilic , etretinate is sequestered into adipose tissue from which small amounts of drug is slowly released. Ø In contrast there is no indication that storge of etretinate occurs. Ø This difference in lipophilicity and in potential storage explains why elimination of etretinate is much slower than that of acitretin.
Ø Acitretin was developed in the hope that female patients would require to delay consideration of pregnancy for only a matter of weeks rather than years after completing a course of treatment. Ø However, there is reverse metabolism to etretinate (particularly in the presence of alcohol) and therefore it is advised that there should be a gap of at least 2 years (3 years in the US) between the end of a course and pregnancy ( Lee CS et al. , 2005). Ø The mechanism of metabolic process for conversion of acitretin to etretinate has not been fully defined. Ø It is unknown whether substances other than ethanol are associated with transesterification.
Ø In the absence of transesterification to etretinate > 98 of acitretin would be eliminated within 2 months. Ø Female patients must use 2 effective forms of contraception for at least 1 month prior to initiation of acitretin therapy during acitretin and for at least 3 years after discontinuing acitretin therapy.
ARE ACITRETIN AND ETRETINATE CLINICALLY IDENTICAL? v Acitretin is the major metabolite of etretinate. v Etretinate is an ethylester that undergoes extensive hydrolysis in the body to yield the corresponding acid metabolite. v From cellular and molecular pharmacology studies , it appears that pharmacologically active compound of etretinate is acitretin and therefore etretinate may be considered a prodrug. v The two drugs have been compared in several double-blind trials in psoriasis, palmoplanter pustulosis, darier disease. v The skin lesions improved to a similar extent and final outcome after a 3 months was identical in both treatment groups.
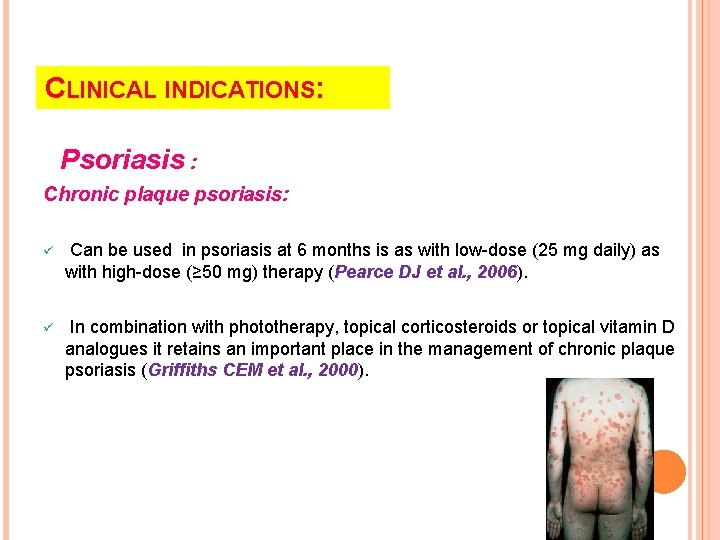
CLINICAL INDICATIONS: Psoriasis : Chronic plaque psoriasis: ü Can be used in psoriasis at 6 months is as with low-dose (25 mg daily) as with high-dose (≥ 50 mg) therapy (Pearce DJ et al. , 2006). ü In combination with phototherapy, topical corticosteroids or topical vitamin D analogues it retains an important place in the management of chronic plaque psoriasis (Griffiths CEM et al. , 2000).
Generalized pustular psoriasis: ü It is likely that inhibition of neutrophil migration plays a key role here. It was found that retinoid treatment was effective compared with methotrexate and ciclosporin (Ozawa A et al. , 1999).
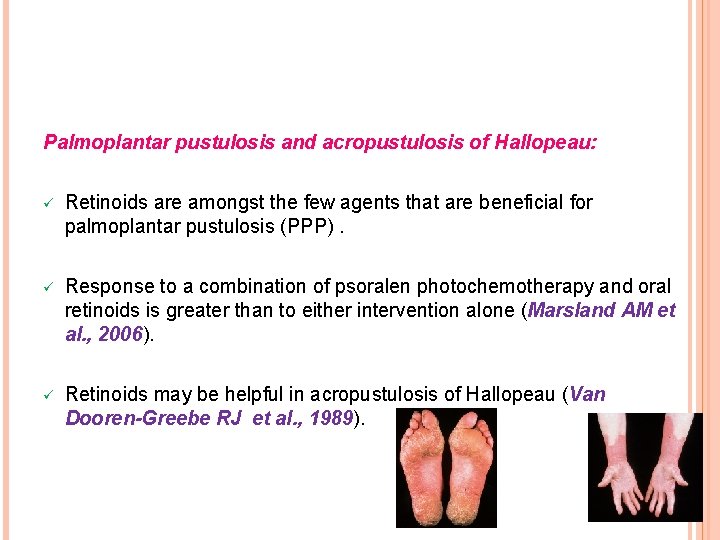
Palmoplantar pustulosis and acropustulosis of Hallopeau: ü Retinoids are amongst the few agents that are beneficial for palmoplantar pustulosis (PPP). ü Response to a combination of psoralen photochemotherapy and oral retinoids is greater than to either intervention alone (Marsland AM et al. , 2006). ü Retinoids may be helpful in acropustulosis of Hallopeau (Van Dooren-Greebe RJ et al. , 1989).
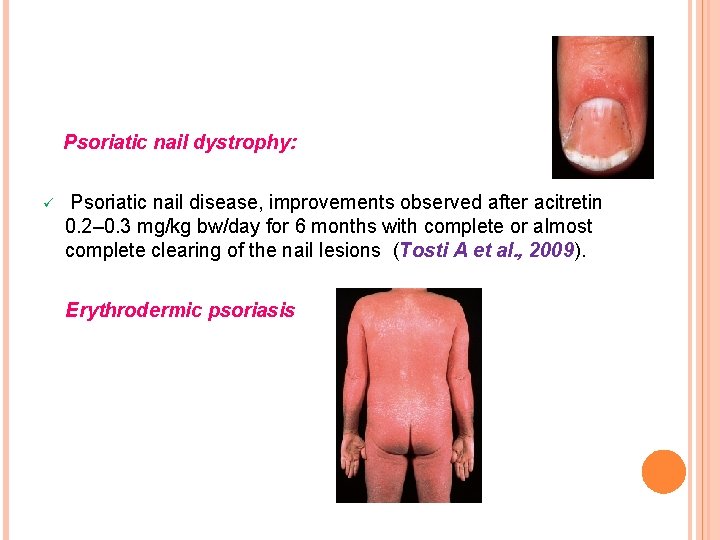
Psoriatic nail dystrophy: ü Psoriatic nail disease, improvements observed after acitretin 0. 2– 0. 3 mg/kg bw/day for 6 months with complete or almost complete clearing of the nail lesions (Tosti A et al. , 2009). Erythrodermic psoriasis
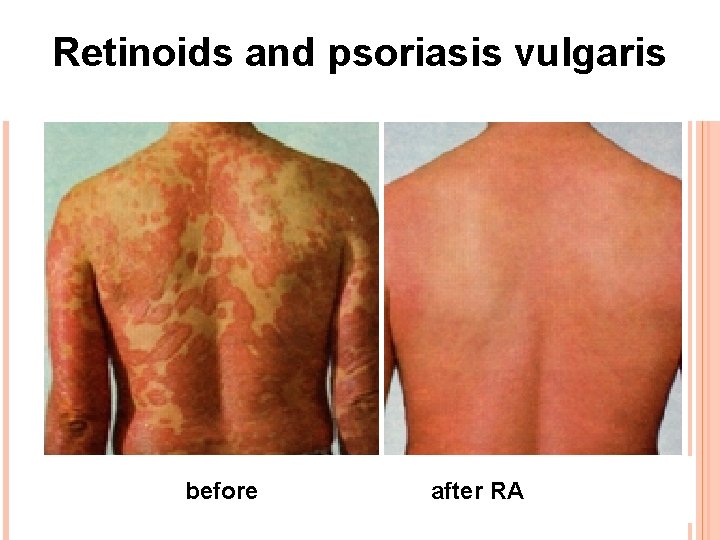
Retinoids and psoriasis vulgaris before after RA
Disorders of keratinization: ü Acitretin can dramatically ameliorate a number of generalized keratinizing disorders including : o Severe Darier’s disease (keratosisfollicularis)( Burge SM et al. , 1992). o Erythrokeratoderma variabilis ( Common JEA et al. , 2005). o lamellar ichthyosis. o Harlequin ichthyosis ( Lawlor F and Peiris S 1985). o Bullous ichthyosiform erythroderma (epidermolytic hyperkeratosis). o Palmoplantar keratodermas.

Severe Darier’s disease before after
Miscellaneous inflammatory dermatoses: ü Cutaneous and less convincingly, for erosive oral lichen planus (Cribier B et al. , 1998). ü Both chronic and subacute forms of cutaneous lupus erythematosus may respond to retinoid therapy. Both acitretin and isotretinoin appear to be beneficial (Ruzicka T et al. , 1988 ; Vena GA et al. , 1989).

a b A-29 -YEAR-OLD PATIENT WITH SUBACUTE CUTANEOUS LUPUS ERYTHEMATOSUS BEFORE THERAPY. B COMPLETE CLEARING OF SKIN LESIONS WITH EXTENSIVE DEPIGMENTATION TWO WEEKS AFTER THERAPY WITH ACITRETIN
Skin cancer chemoprophylaxis: ü Etretinate and acitretin have been used to reduce the rate of tumour formation in patients at high risk of development of skin cancer including : o Xeroderma pigmentosum. o o Naevoid basal cell carcinoma syndrome. Organ transplant recipients requiring long term immunosuppression (Campbell RM et al. , 2006).

Renal transplant recipient with multiple large SCCs and scars from previous SCCs.
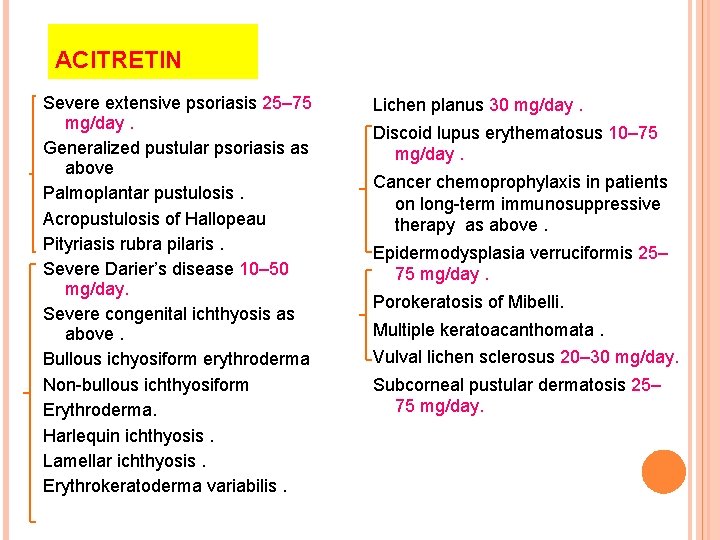
ACITRETIN Severe extensive psoriasis 25– 75 mg/day. Generalized pustular psoriasis as above Palmoplantar pustulosis. Acropustulosis of Hallopeau Pityriasis rubra pilaris. Severe Darier’s disease 10– 50 mg/day. Severe congenital ichthyosis as above. Bullous ichyosiform erythroderma Non-bullous ichthyosiform Erythroderma. Harlequin ichthyosis. Lamellar ichthyosis. Erythrokeratoderma variabilis. Lichen planus 30 mg/day. Discoid lupus erythematosus 10– 75 mg/day. Cancer chemoprophylaxis in patients on long-term immunosuppressive therapy as above. Epidermodysplasia verruciformis 25– 75 mg/day. Porokeratosis of Mibelli. Multiple keratoacanthomata. Vulval lichen sclerosus 20– 30 mg/day. Subcorneal pustular dermatosis 25– 75 mg/day.
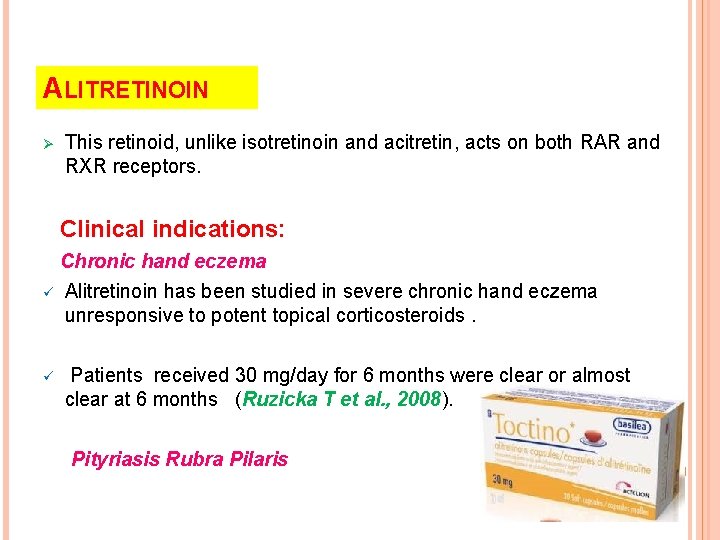
ALITRETINOIN Ø This retinoid, unlike isotretinoin and acitretin, acts on both RAR and RXR receptors. Clinical indications: Chronic hand eczema ü Alitretinoin has been studied in severe chronic hand eczema unresponsive to potent topical corticosteroids. ü Patients received 30 mg/day for 6 months were clear or almost clear at 6 months (Ruzicka T et al. , 2008). Pityriasis Rubra Pilaris
BEXAROTENE Ø A number of studies carried out in the 1980 showed some beneficial effect of RAR retinoids including etretinate and isotretinoin in cutaneous T-cell lymphoma (CTCL). Ø Bexarotene is an RXR-selective retinoid (rexinoid) which is licensed for the treatment of advanced CTCL Ø More recent research has focused on producing receptor specific retinoids with greater antitumour activity.
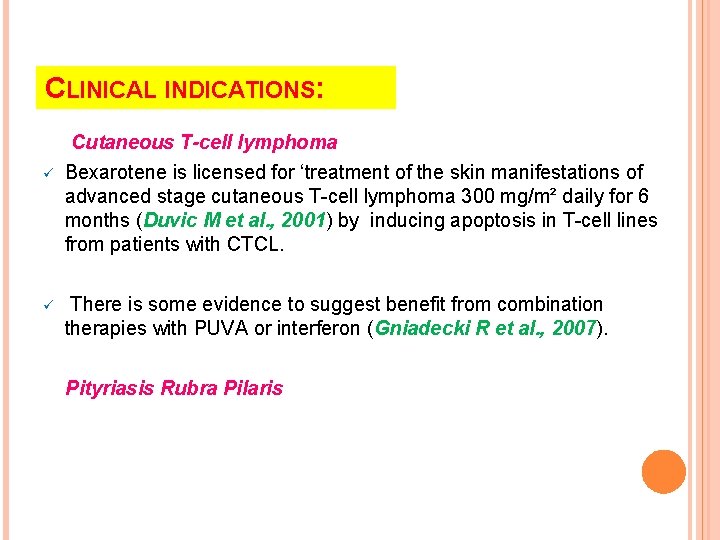
CLINICAL INDICATIONS: ü ü Cutaneous T-cell lymphoma Bexarotene is licensed for ‘treatment of the skin manifestations of advanced stage cutaneous T-cell lymphoma 300 mg/m² daily for 6 months (Duvic M et al. , 2001) by inducing apoptosis in T-cell lines from patients with CTCL. There is some evidence to suggest benefit from combination therapies with PUVA or interferon (Gniadecki R et al. , 2007). Pityriasis Rubra Pilaris

a b Palms before and after bexarotene treatment. A) Before treatment, confluent inflammatory hyperkeratosis with sparse fissuring. B) After treatment, reduced hyperkeratosis without fissuring or inflammation.
SAFETY PROFILE OF RETINOIDS: Mucocutaneous effects: v Cheilitis, dryness of mucous membranes , nasal colonization and epistaxis may occur. v Xerosis and skin peeling, palmoplantar desquamation, pruritus. v Increased incidence of vulvovaginal candidosis has been reported in patients receiving acitretin. v Photosensitivity due to reduction of thickness of stratum corneum. v Pyogenic granuloma-like proliferation of granulaion tissue occur early in therapy (Gollnick H et al. , 2003).
Liver toxicity: v Patients may develop abnormal liver enzyme levels during therapy with retinoids; not all values have returned to normal on cessation of the drug. v Retinoids may increase the hepatotoxicity of methotrexate. v Patients at risk of liver toxicity are those with diabetes mellitus, obesity, prior or concurrent methotrexate use, excess alcohol consumption, infectious hepatitis, and abnormal baseline LFTs (Kontaxakis VP et al. , 2009 ; Marqueling AL et al. , 2005).
Blood lipid abnormalities : v Increase in very-low-density lipoprotein (VLDL) cholesterol and reduction in high-density lipoprotein (HDL) cholesterol have been reported with retinoid therapy. v These levels have returned to normal on cessation of treatment. v The effect on lipids is greatest with bexarotene; 80% of patients develop hyperlipidaemia (Gniadecki R et al. , 2007).
CNS effects: v Changes of pseudotumor cerebi ( Intracranial hypertension )may occur and is a reason not to combine isotretinoin with tetracyclines. v Some patients may experience sensory changes , mood change including depression, aggressiveness and suicidal ideation while receiving isotretinoin. (Jick SS et al. , 2000 ; Kontaxakis VP et al. , 2009). Hematological effects: v Bexarotene induce reversible leukopenia. v The incidence is less frequent with first and second generation.
Bone effects: v Decalcificaition. v Cortical hyperostosis. v Epiphyseal closure. the possbility of premature closure in growing children should be carefully considered, particularly with high dose or planned long- term therapy with retinoids. v These drugs should only be given to younger children when there are sound indications. v It is important to ask patients about any skeletal pain or mobility restrictions( Carey BM et al. , 1988 ; Katz HI et al. , 1999 ; Gollnick H et al. , 2003)
Teratogenicity: v Maternal ingestion of retinoids early in pregnancy can lead to severe fetal abnormalities. It is important that women are not pregnant prior to starting treatment. Effective contraception is mandatory during and after a course of treatment. v Isotretinoin has a short half-life and therefore contraceptive measures need to be taken for only 1 month after cessation of treatment. v Because of the small risk of esterification of acitretin to etretinate (which has a very long half-life) it is recommended that attempts to conceive should be delayed for at least 2 years (3 years in US) after cessation of acitretin therapy. v Males can safely father children even when they are taking the drug. The most common malformations include those of the CNS ( hydrocephaly and cranial nerve abnormalities) , craniofacial anomalies : absent auditory canal, cardic , thymus anomalies (Rosa FW 1983 ; de la Cruz E et al. , 1984 ; Katz HI et al. , 1999)
Ocular effects: v Involve conjunctive (blepharoconjunctivitis ), cornea, lens , retina. many patients cannot tolerate contact lenses while receiving isotretinoin. Hair and nail effects: v Alopecia , the risk of telogen effluvium due to retinoids has been reported. The risk is greater for etretinate and acitretin. v Fragiale nails , nail dystrophy and onycholysis occur infrequently (Gollnick H et al. , 2003). Muscle effects: v Myalgia, arthralgia and lethargy (Gollnick H et al. , 2003).
ALSO REPORTED: v Decrease serum vitamin E levels in patients with acne while receving isotretinoin (Akturk AS et al. , 2013) v Decrease serum folic acid levels in patients with acne while receving isotretinoin (Javanbakht AM et al. , 2012). v Central hypothyroidism with systemic bexarotene (Gniadecki R et al. , 2007).
MONITORING GUIDELINES: Baseline Examination: q Ø Careful history and examination. Ø Identify those patients at increased risk of toxicity or adverse effects. Ø Document concomitant medications may interact with retinoids.
MONITORING GUIDELINES: q Ø Laboratory: Two serum or sensitive urine pregnancy tests. Ø Complete blood count. Ø Liver function test. Ø Lipid profile. Ø Renal function tests.
MONITORING GUIDELINES: q Special tests: Ø Baseline x-rays of wrist, ankles or thoracic spine if plan long term retinoid therapy. Ø Ophthalmologic examination if patient has history of cataract or retinopathy.
MONITORING GUIDELINES: q Follow up: Ø Examination: monthly for first 3 to then every 3 month. Ø Assessment of patient response, improvement, and complaints of adverse effects.
q Laboratory: monthly for first 3 , then every 3 month. Ø Complete blood count. Ø Liver function tests. Ø Fasting lipid studies. Ø Renal function tests. Ø Pregnancy tests monthly.
CONTRAINDICATIONS: q Absolute: 1) Pregnancy or woman who is likely to become pregnant. 2) Noncompliance with contraception. 3) Nursing mother.
q Relative: 1) Significant hepatic dysfunction. 2) Significant renal dysfunction. 3) Moderate to severe cholesterol or triglyceride elevation. 4) Patients at risk of coronary artery disease. 5) Chronic use in children. 6) Patients at risk of liver toxicity. 7) Leukopenia. 8) Hypothyroidism in bexarotene patients.
RETINOID DRUG INTERACTIONS: q Drugs increase the serum level of Retinoids: Ø Vitamin A. Ø Tetracycline, doxycycline and minocyclin increase risk of pseudotumor cerebri. Ø Macrolides, azoles inhibit cytochrome p. Ø Carbamazepine, Phenytoin , Phenobarbital Anticonvulsants
RETINOID DRUG INTERACTIONS: q Drugs decrease serum level of retinoids via CYP induction: Ø Antituberculous: rifampin. q Retinoids may increase drug level of: Ø Cyclosporine: competition for CYP metabolism.
q Retinoids decrease drug level of: Ø Progesterone only contraceptive pills: minipills. q Other potentially important drug interactions: Ø Methotrexate: increase risk of liver toxicity. Ø Alcohol: increase reverse metabolism of acitretin. Ø Oral antidiabetic increases risk of hypoglycemia. Ø Corticosteroids increase the risk of bone loss. Iranian Journal of Dermatology © 2013 Iranian Society of Dermatology
HOME MESSAGE v Systemic retinoids used mainly in sever forms of acne , disorders of kertinization and sever forms of psoriasis. v Investigations, follow up are mandatory when using systemic retinoids. v Systemic retinoids are contraindicated in pregnant women, children, hepatic and renal patients and patients with cholesterol or triglyceride elevation.


- Slides: 82