Systema genitale femininum Female genital system Anatomy Organa


- Slides: 60
Systema genitale femininum Female genital system Anatomy
Organa genitalia feminina interna Female internal genitalia • • • ovarium (= ovary) tuba uterina / salpinx (= uterine tube) uterus (= womb) vagina developmental rudiments (epoophoron, paroophoron)
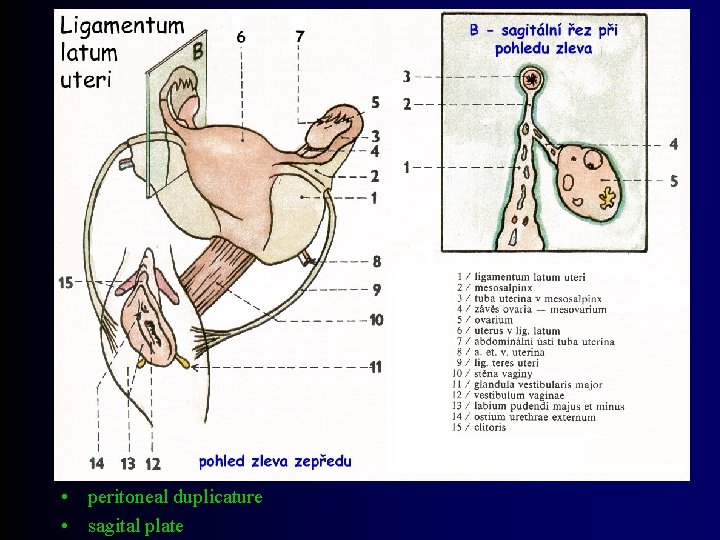
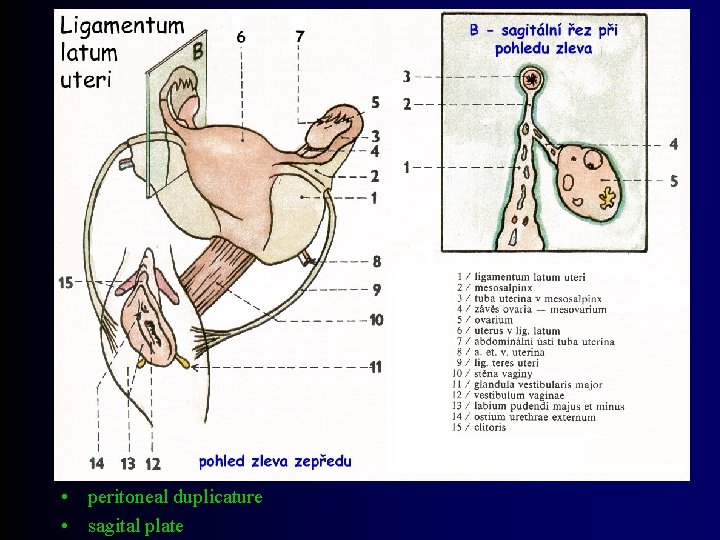
• peritoneal duplicature • sagital plate
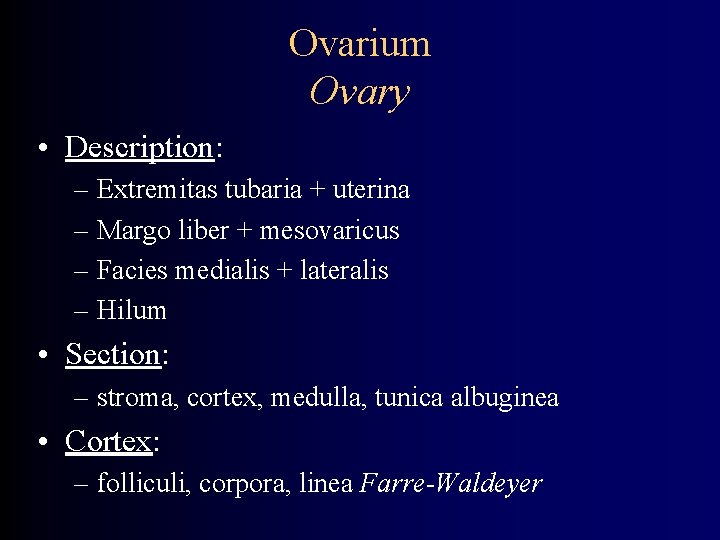
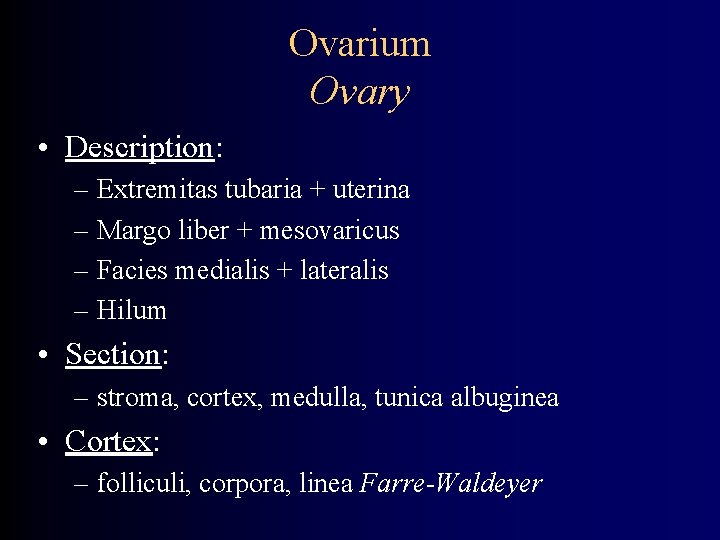
Ovarium Ovary • Description: – Extremitas tubaria + uterina – Margo liber + mesovaricus – Facies medialis + lateralis – Hilum • Section: – stroma, cortex, medulla, tunica albuginea • Cortex: – folliculi, corpora, linea Farre-Waldeyer
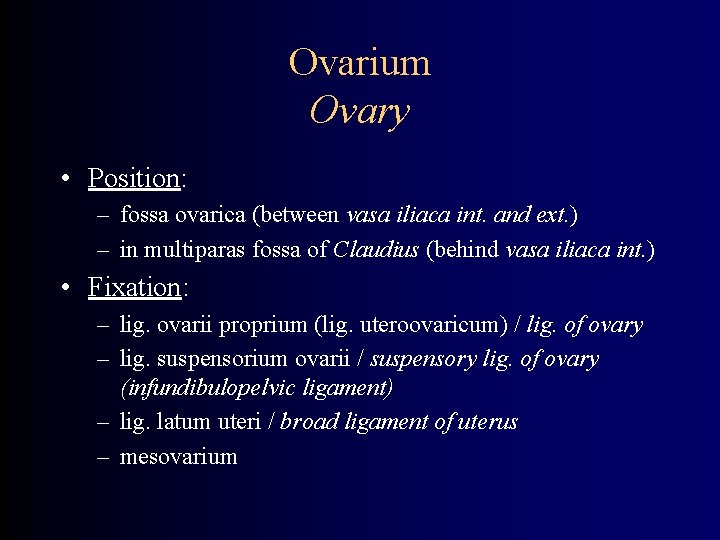
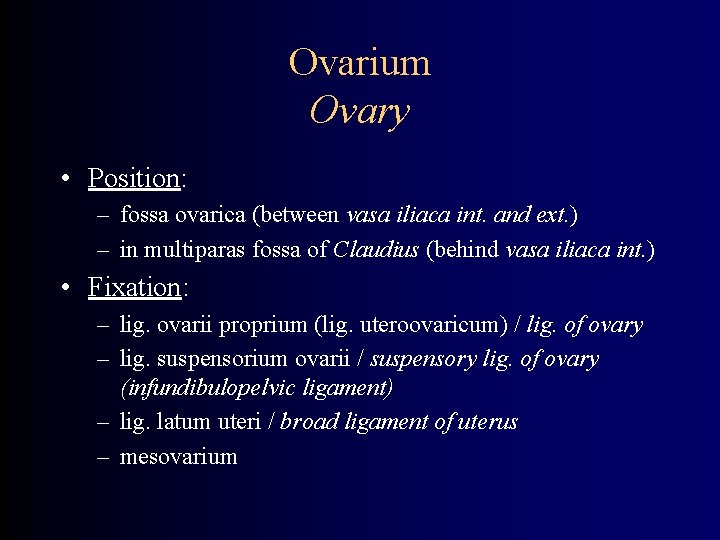
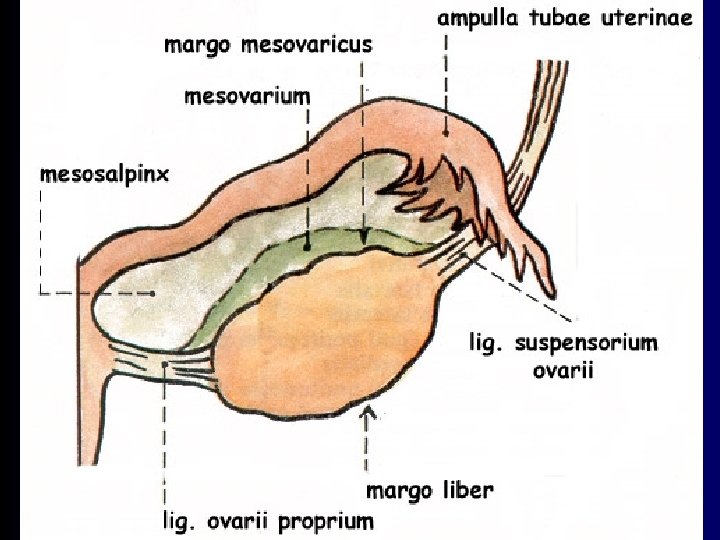
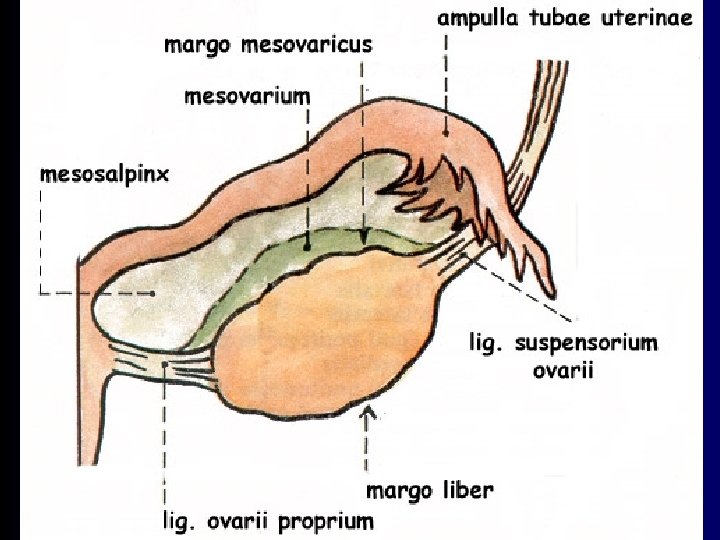
Ovarium Ovary • Position: – fossa ovarica (between vasa iliaca int. and ext. ) – in multiparas fossa of Claudius (behind vasa iliaca int. ) • Fixation: – lig. ovarii proprium (lig. uteroovaricum) / lig. of ovary – lig. suspensorium ovarii / suspensory lig. of ovary (infundibulopelvic ligament) – lig. latum uteri / broad ligament of uterus – mesovarium
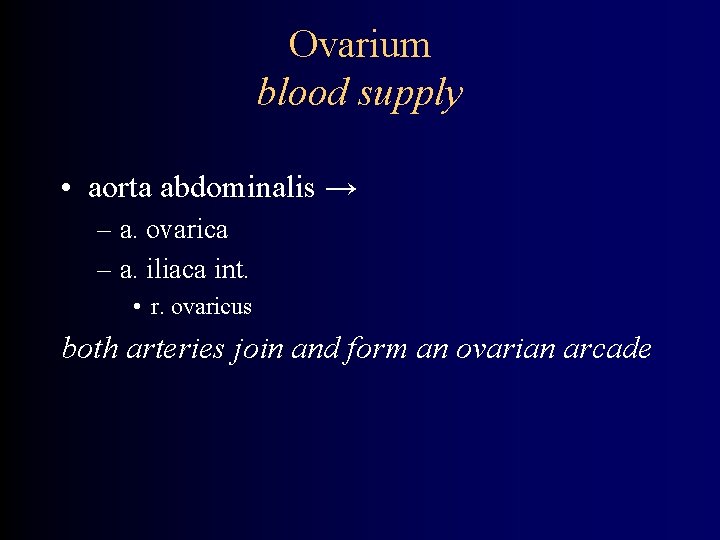
Ovarium blood supply • aorta abdominalis → – a. ovarica – a. iliaca int. • r. ovaricus both arteries join and form an ovarian arcade
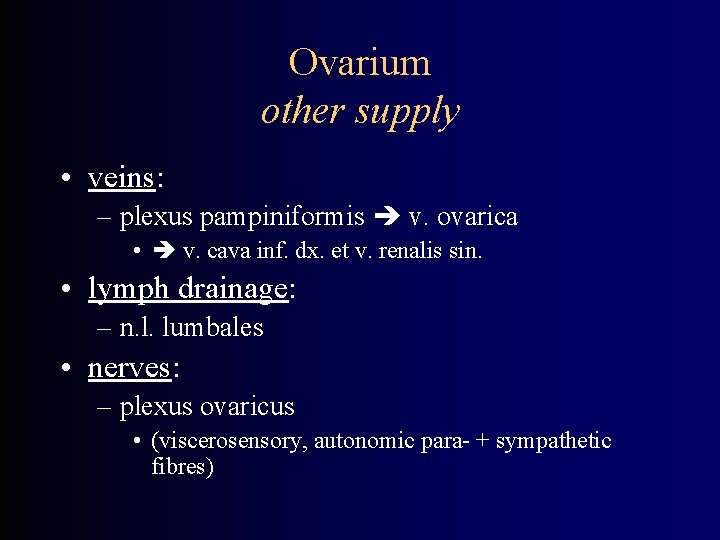
Ovarium other supply • veins: – plexus pampiniformis v. ovarica • v. cava inf. dx. et v. renalis sin. • lymph drainage: – n. l. lumbales • nerves: – plexus ovaricus • (viscerosensory, autonomic para- + sympathetic fibres)
Ovarium - histoloy • cortex (cortical zone) – simple cuboideal epithelium – tunica albuginea – loose connective tissue, fibroblasts, collagen and reticular fibres – ovarian follicles • medulla (vascular zone) – collagenous tissue, vessels, nerves
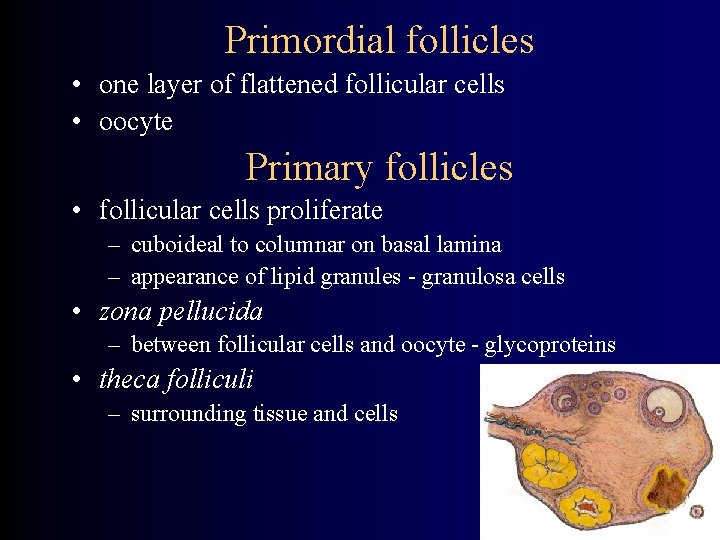
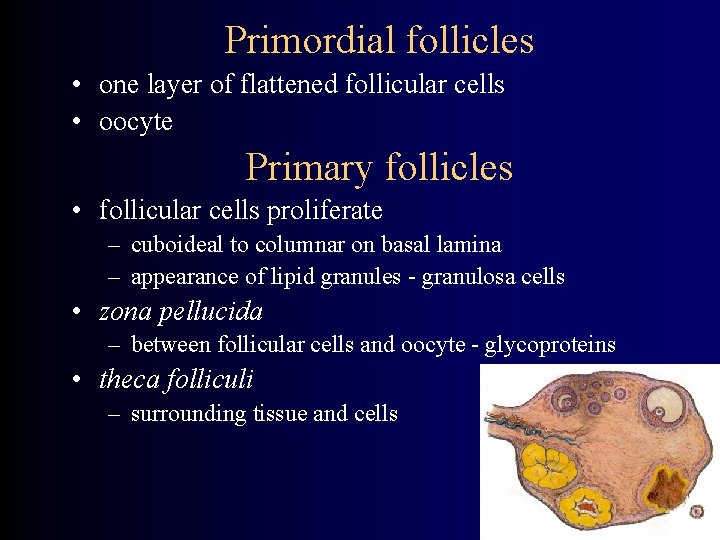
Primordial follicles • one layer of flattened follicular cells • oocyte Primary follicles • follicular cells proliferate – cuboideal to columnar on basal lamina – appearance of lipid granules - granulosa cells • zona pellucida – between follicular cells and oocyte - glycoproteins • theca folliculi – surrounding tissue and cells
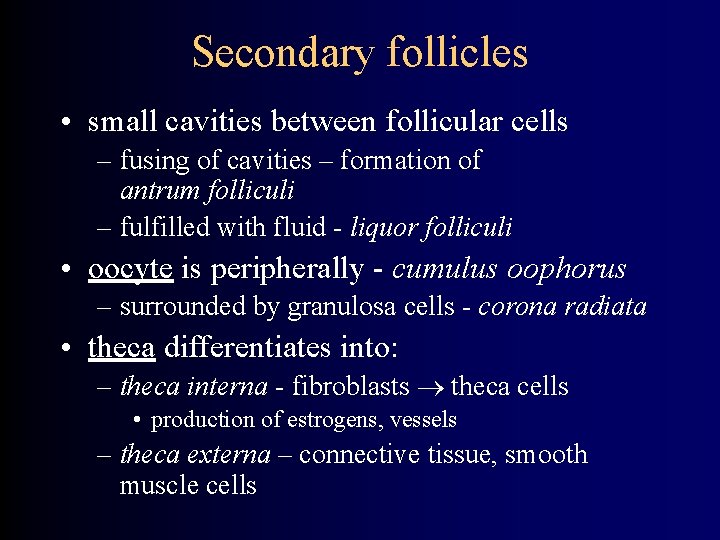
Secondary follicles • small cavities between follicular cells – fusing of cavities – formation of antrum folliculi – fulfilled with fluid - liquor folliculi • oocyte is peripherally - cumulus oophorus – surrounded by granulosa cells - corona radiata • theca differentiates into: – theca interna - fibroblasts theca cells • production of estrogens, vessels – theca externa – connective tissue, smooth muscle cells
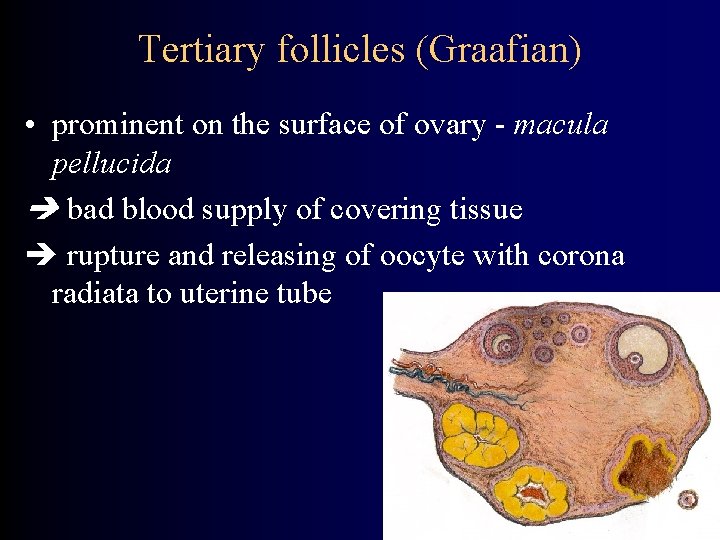
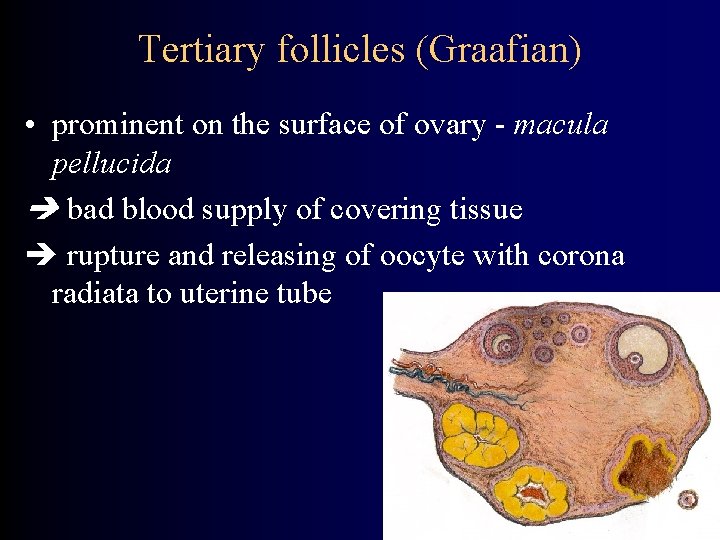
Tertiary follicles (Graafian) • prominent on the surface of ovary - macula pellucida bad blood supply of covering tissue rupture and releasing of oocyte with corona radiata to uterine tube
Corpus luteum • develops from empty Graafian follicle • corpus luteum graviditatis – in function till 4 th month of gravidity • corpus luteum menstruationis – functional for 10 -12 days (till 24 th-26 th day of cycle) • corpus luteum change to corpus albicans (connective tissue) – c. a. graviditatis – remains a recession on ovary surface – c. a. menstruationis – no traces
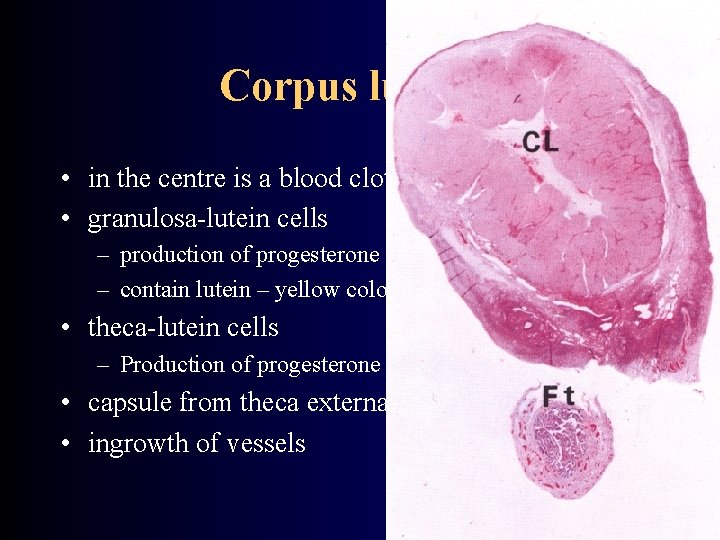
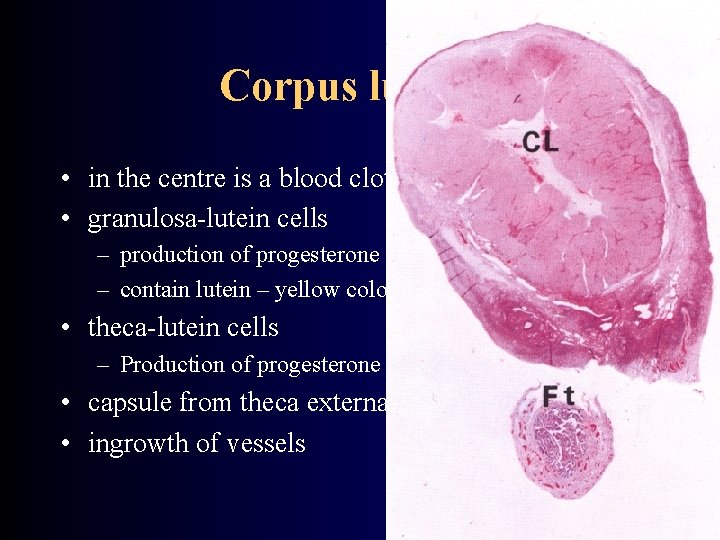
Corpus luteum • in the centre is a blood clot • granulosa-lutein cells – production of progesterone and estrogens – contain lutein – yellow color • theca-lutein cells – Production of progesterone androstedione • capsule from theca externa - septa • ingrowth of vessels
Ovary development • from 12 th week • primary sex cords disappear • development of cortical cords – surrounding the primordial germ cells – development of follicles with oogonia • surface epithelium – simple cuboideal mesovarium – tunica albuginea • relative descent (elongation of body) • gubernaculum lig. suspensorium ovarii, lig. teres uteri
Tuba uterina / salpinx Uterine tube (Falloppii) • Parts: – ostium abdominale – infundibulum – ampulla – isthmus – pars uterina (p. intramuralis) – ostium uterinum • Fimbriae – the longest ovarian fimbria reaching the ovary
Tuba uterina / salpinx Uterine tube (Falloppii) • Fixation: – mesosalpinx • Arteries: – r. tubarius a. uterinae – r. tubarius a. ovaricae • Veins: – vv. ovaricae, plexus venosus uterovaginalis • Lymph drainage: – n. l. lumbales
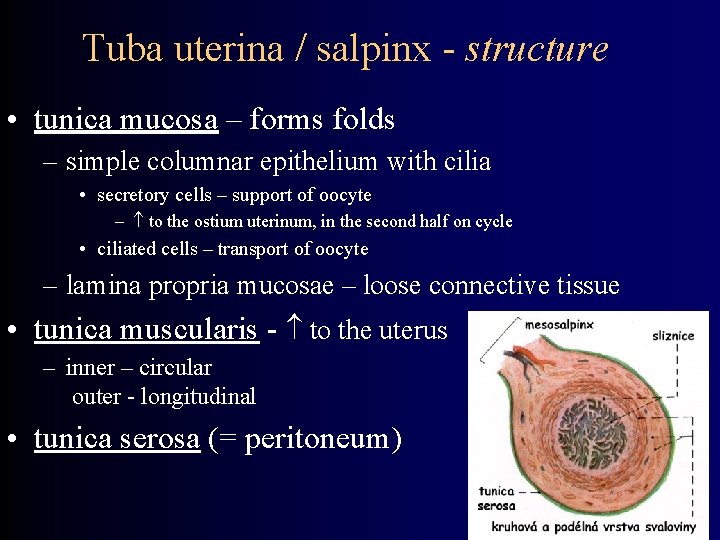
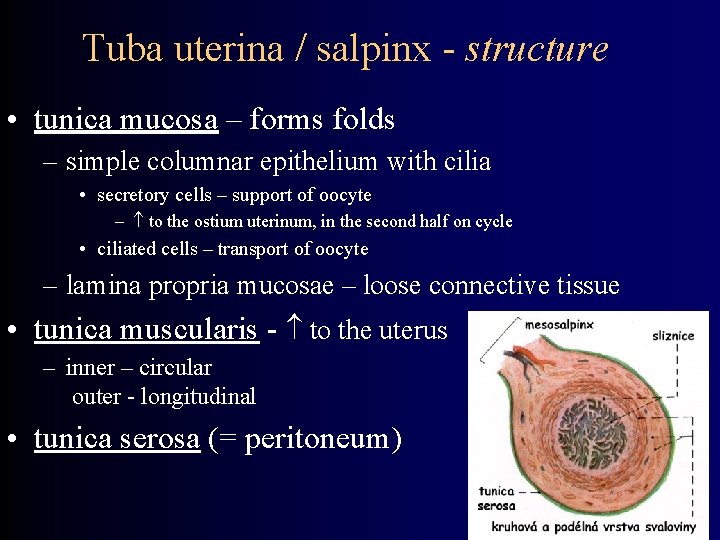
Tuba uterina / salpinx - structure • tunica mucosa – forms folds – simple columnar epithelium with cilia • secretory cells – support of oocyte – to the ostium uterinum, in the second half on cycle • ciliated cells – transport of oocyte – lamina propria mucosae – loose connective tissue • tunica muscularis - to the uterus – inner – circular outer - longitudinal • tunica serosa (= peritoneum)
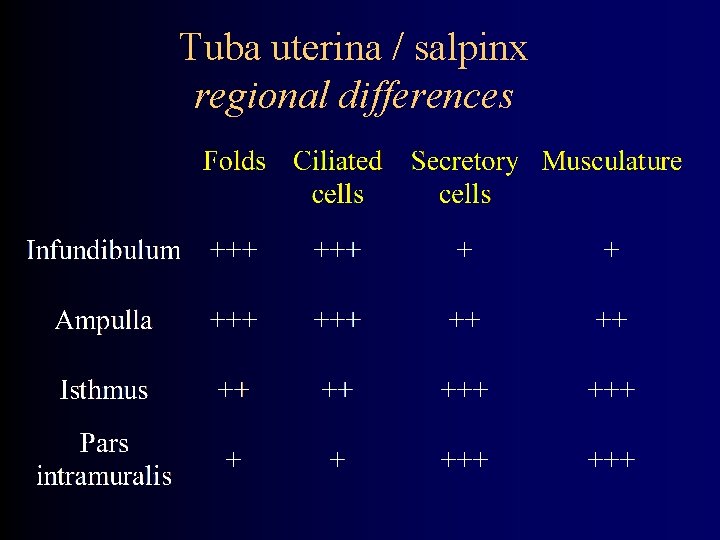
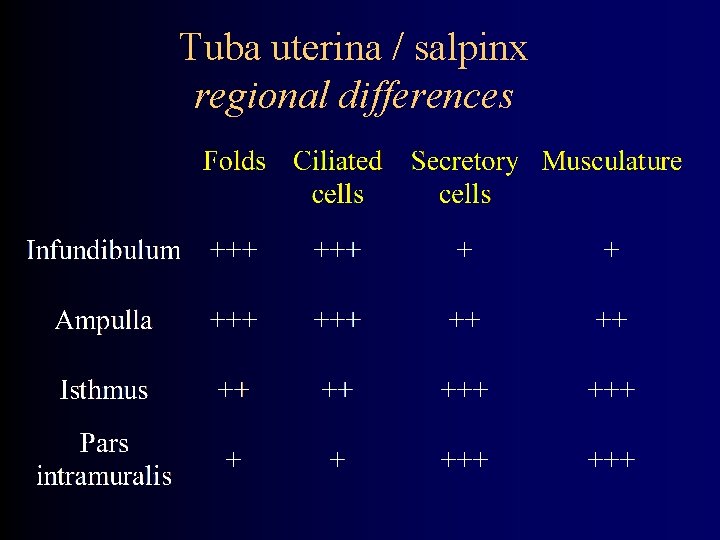
Tuba uterina / salpinx regional differences
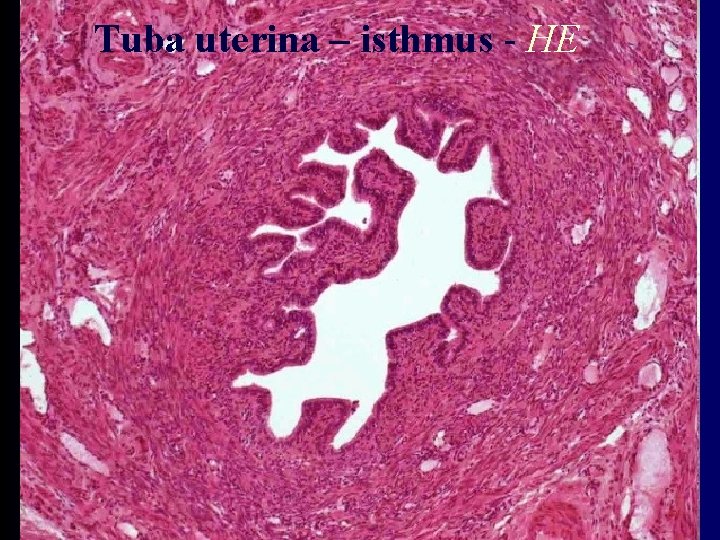
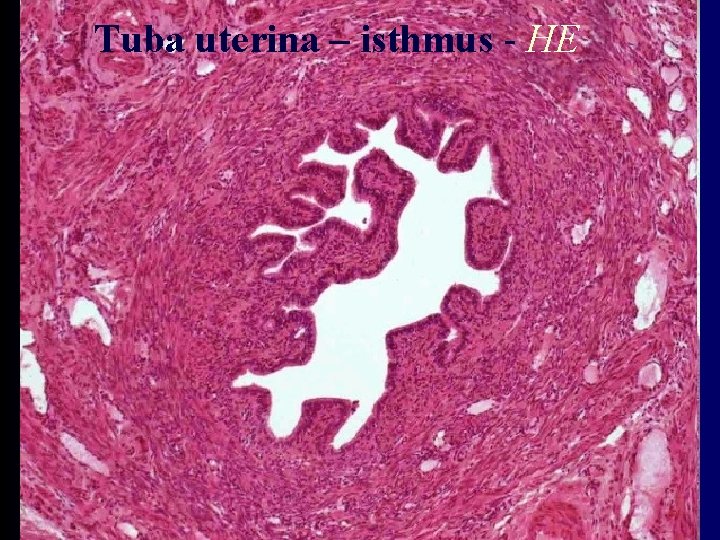
Tuba uterina – isthmus - HE

Tuba uterina – ampula - HE
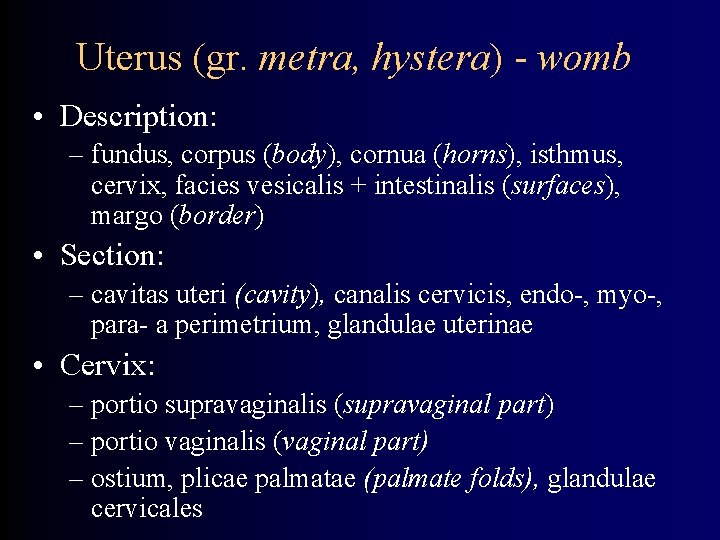
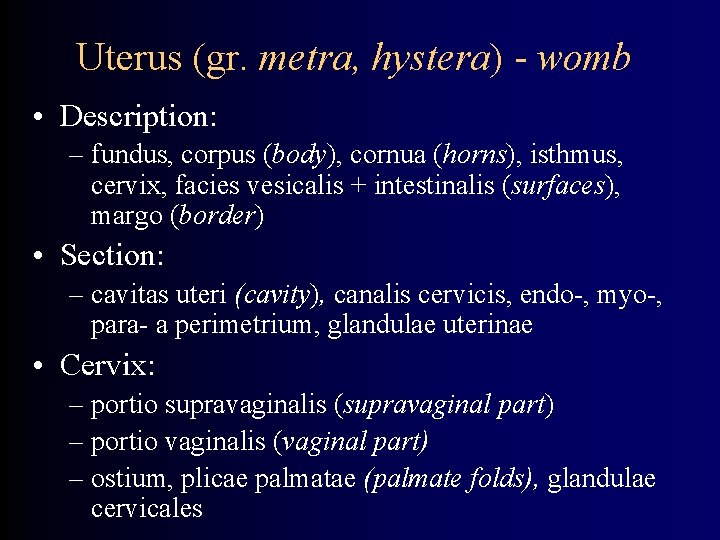
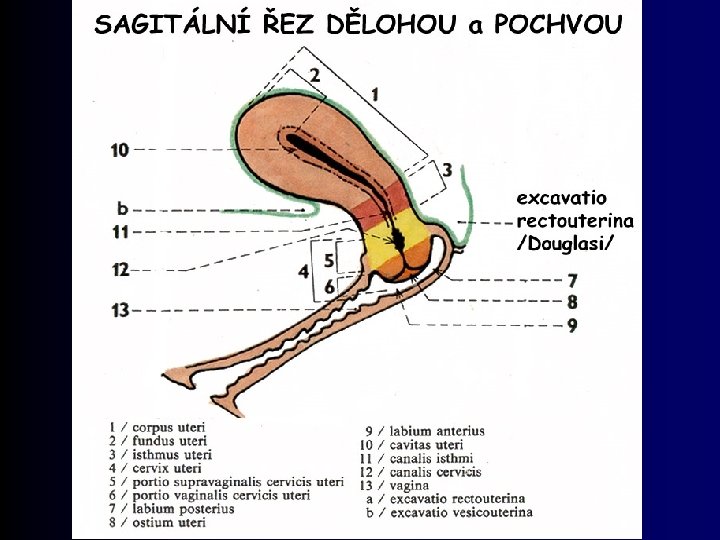
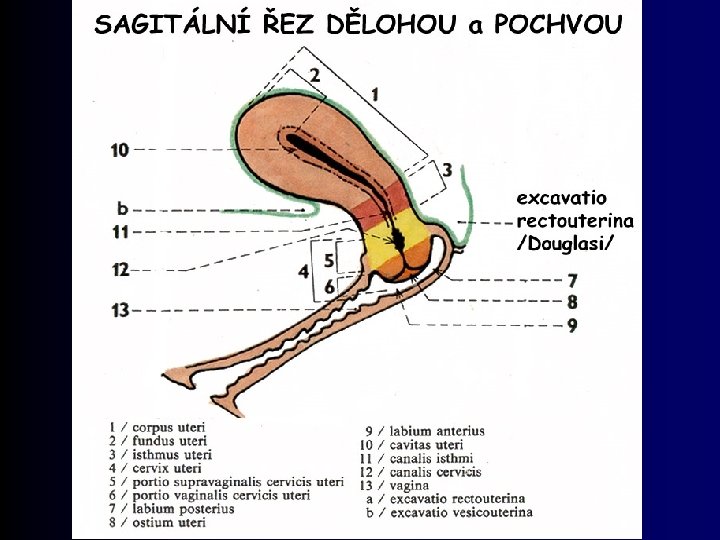
Uterus (gr. metra, hystera) - womb • Description: – fundus, corpus (body), cornua (horns), isthmus, cervix, facies vesicalis + intestinalis (surfaces), margo (border) • Section: – cavitas uteri (cavity), canalis cervicis, endo-, myo-, para- a perimetrium, glandulae uterinae • Cervix: – portio supravaginalis (supravaginal part) – portio vaginalis (vaginal part) – ostium, plicae palmatae (palmate folds), glandulae cervicales
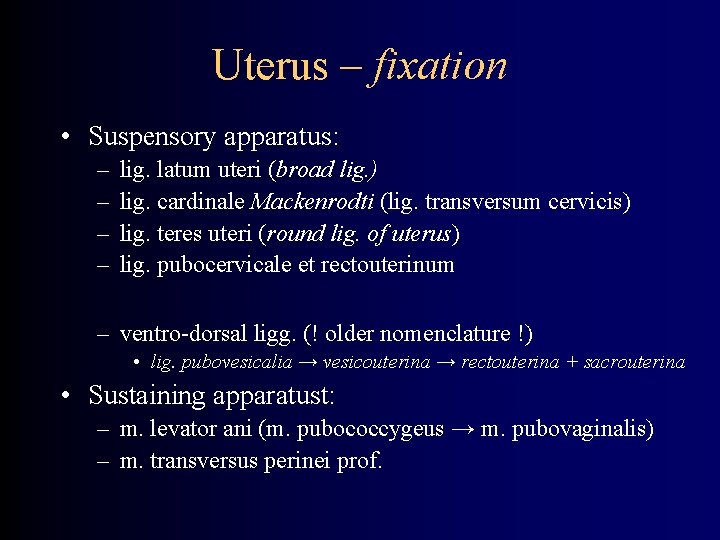
Uterus – fixation • Suspensory apparatus: – – lig. latum uteri (broad lig. ) lig. cardinale Mackenrodti (lig. transversum cervicis) lig. teres uteri (round lig. of uterus) lig. pubocervicale et rectouterinum – ventro-dorsal ligg. (! older nomenclature !) • lig. pubovesicalia → vesicouterina → rectouterina + sacrouterina • Sustaining apparatust: – m. levator ani (m. pubococcygeus → m. pubovaginalis) – m. transversus perinei prof.
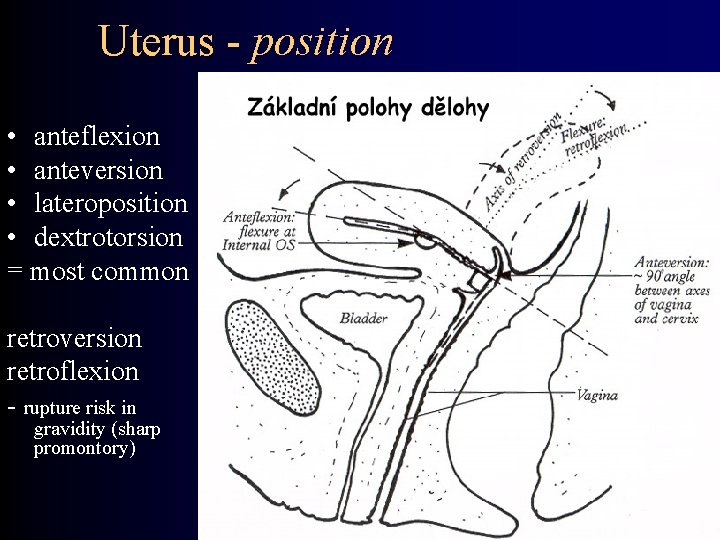
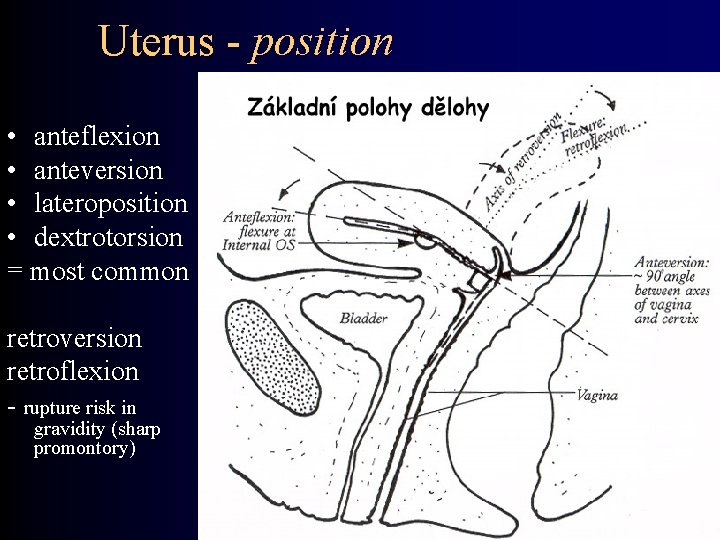
Uterus - position • anteflexion • anteversion • lateroposition • dextrotorsion = most common retroversion retroflexion - rupture risk in gravidity (sharp promontory)
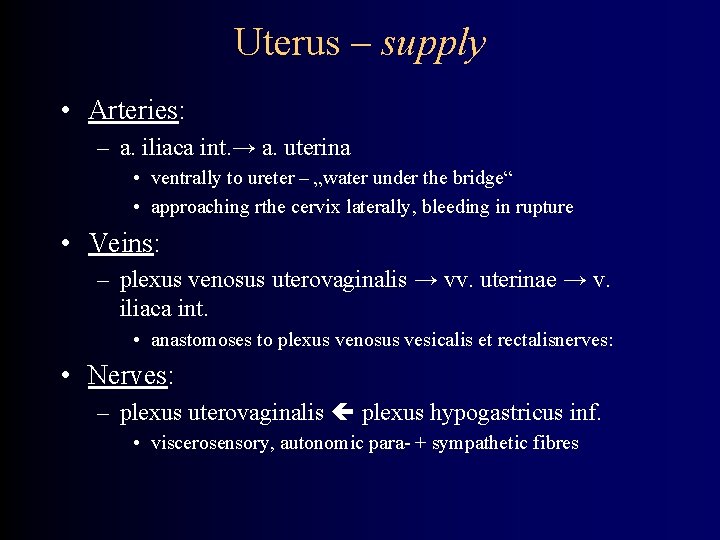
Uterus – supply • Arteries: – a. iliaca int. → a. uterina • ventrally to ureter – „water under the bridge“ • approaching rthe cervix laterally, bleeding in rupture • Veins: – plexus venosus uterovaginalis → vv. uterinae → v. iliaca int. • anastomoses to plexus venosus vesicalis et rectalisnerves: • Nerves: – plexus uterovaginalis plexus hypogastricus inf. • viscerosensory, autonomic para- + sympathetic fibres
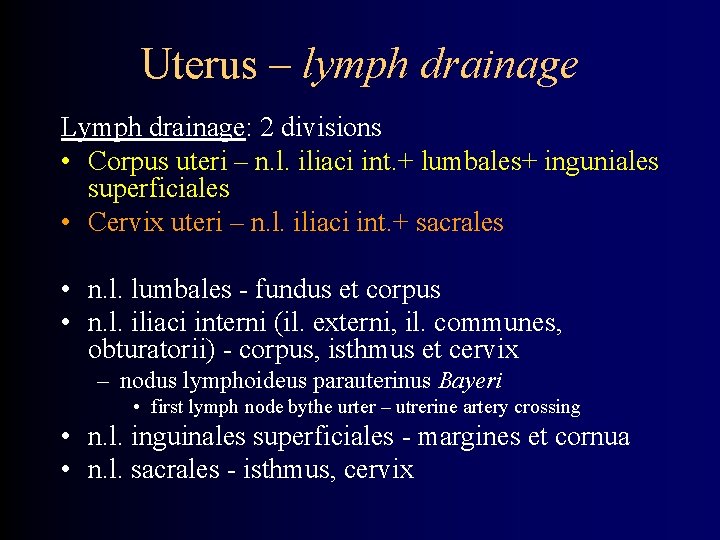
Uterus – lymph drainage Lymph drainage: 2 divisions • Corpus uteri – n. l. iliaci int. + lumbales+ inguniales superficiales • Cervix uteri – n. l. iliaci int. + sacrales • n. l. lumbales - fundus et corpus • n. l. iliaci interni (il. externi, il. communes, obturatorii) - corpus, isthmus et cervix – nodus lymphoideus parauterinus Bayeri • first lymph node bythe urter – utrerine artery crossing • n. l. inguinales superficiales - margines et cornua • n. l. sacrales - isthmus, cervix
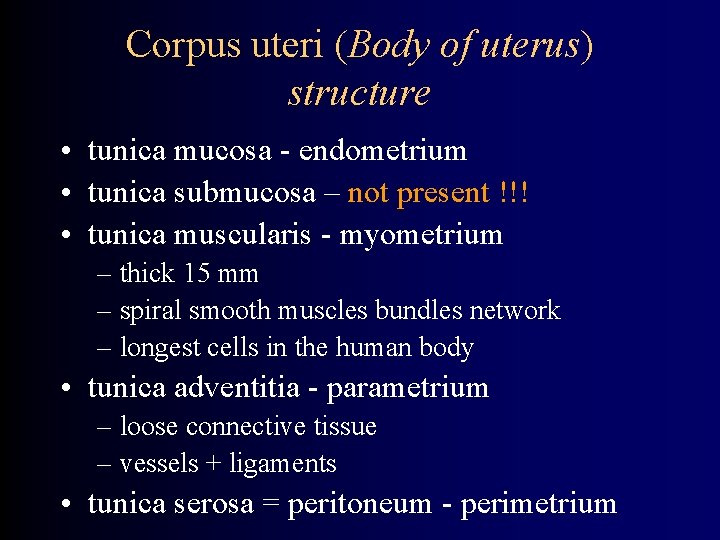
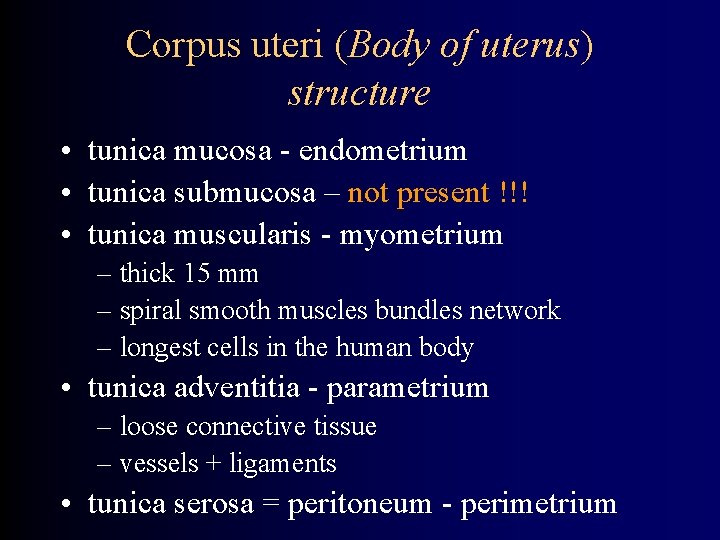
Corpus uteri (Body of uterus) structure • tunica mucosa - endometrium • tunica submucosa – not present !!! • tunica muscularis - myometrium – thick 15 mm – spiral smooth muscles bundles network – longest cells in the human body • tunica adventitia - parametrium – loose connective tissue – vessels + ligaments • tunica serosa = peritoneum - perimetrium
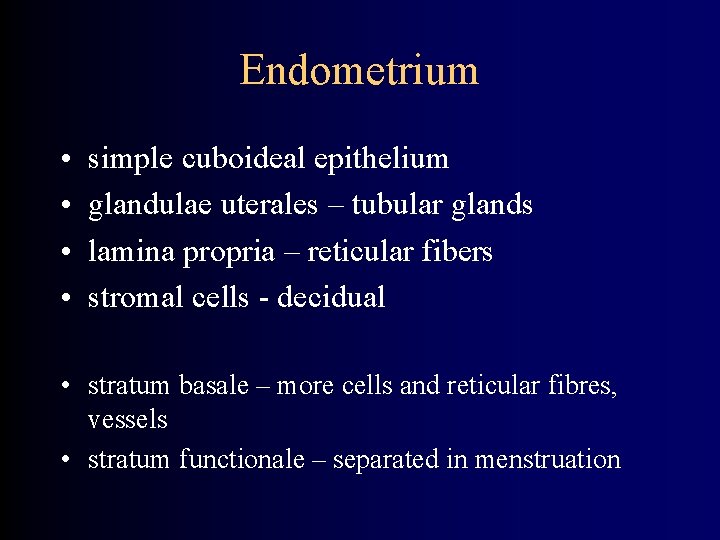
Endometrium • • simple cuboideal epithelium glandulae uterales – tubular glands lamina propria – reticular fibers stromal cells - decidual • stratum basale – more cells and reticular fibres, vessels • stratum functionale – separated in menstruation
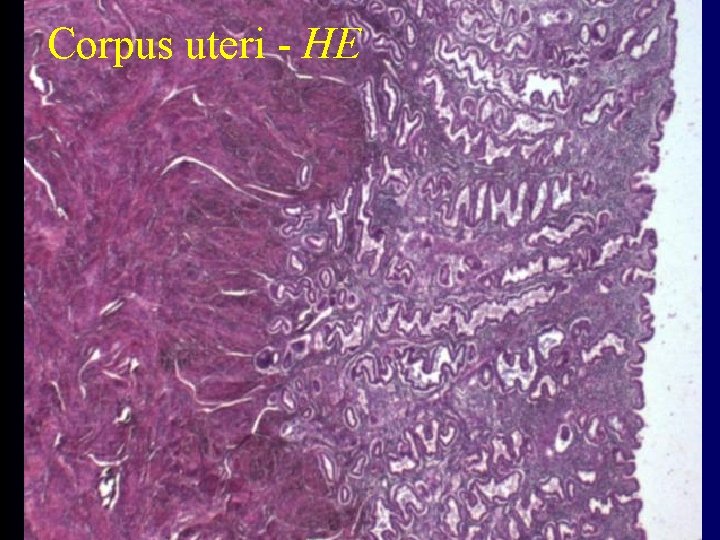
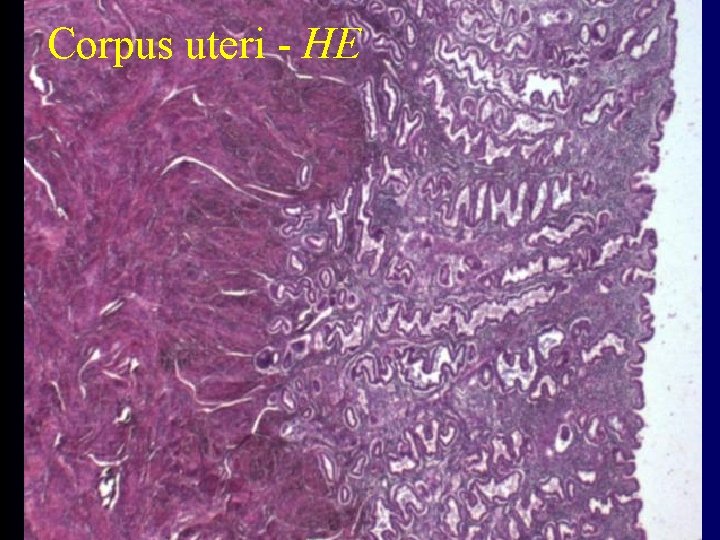
Corpus uteri - HE
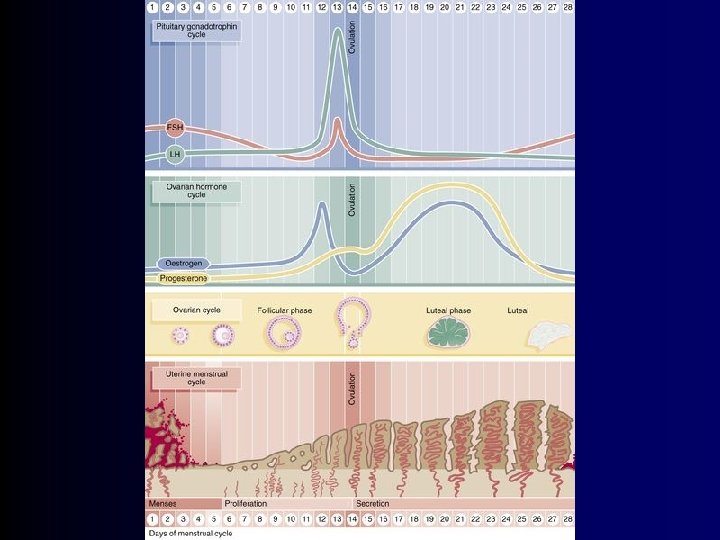
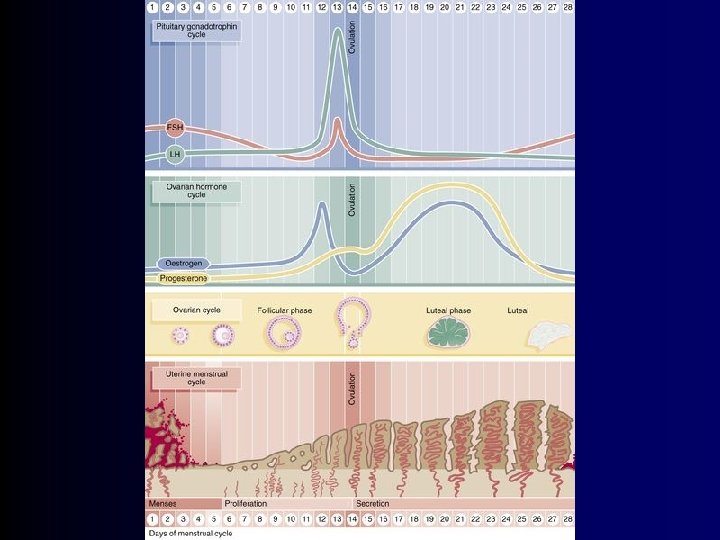
Menstrual cycle • menstrual phase (1 st – 4 th day) • proliferative phase (5 th – 14 th day) • secretory phase • ischemic phase (15 th – 28 th day) (28 th day)
Menstrual phase • releasing of functional layer • basal layer stays in place • epithelisation of surface – fisihed 5 th day = regeneration phase • menstruation blood – do not form clots – enzymes of mucosa – is mix of arterial and venous blood
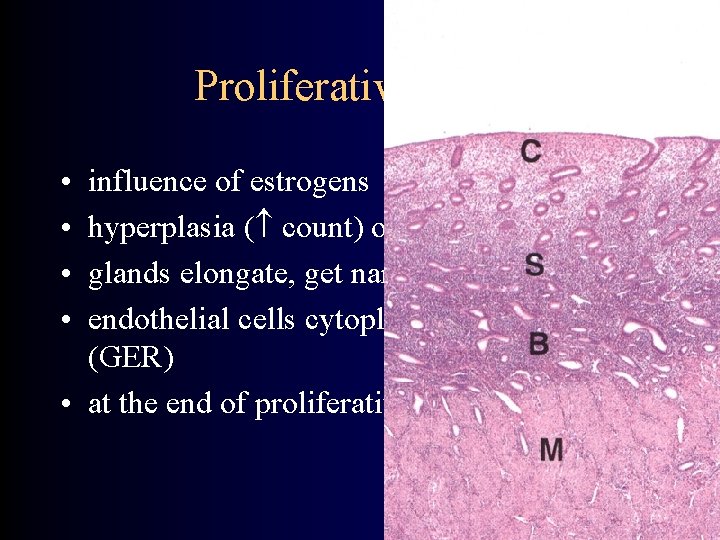
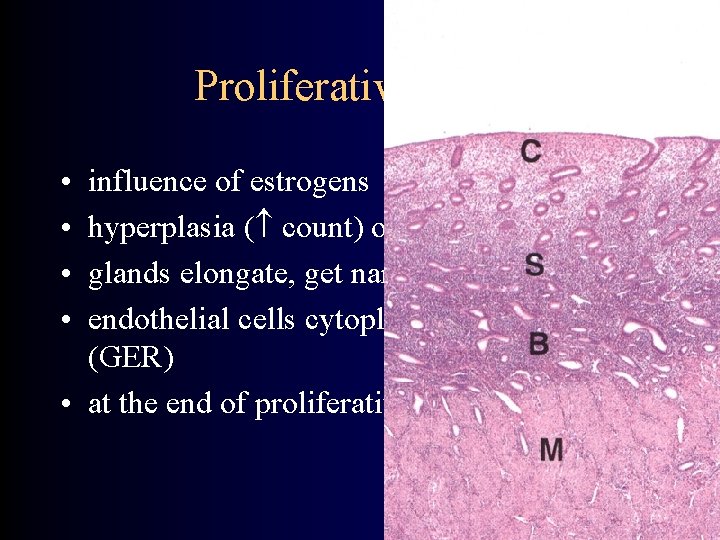
Proliferative phase • • influence of estrogens hyperplasia ( count) of functional layer glands elongate, get narrow with no lumen endothelial cells cytoplasma – basophile (GER) • at the end of proliferative phase – ovulation
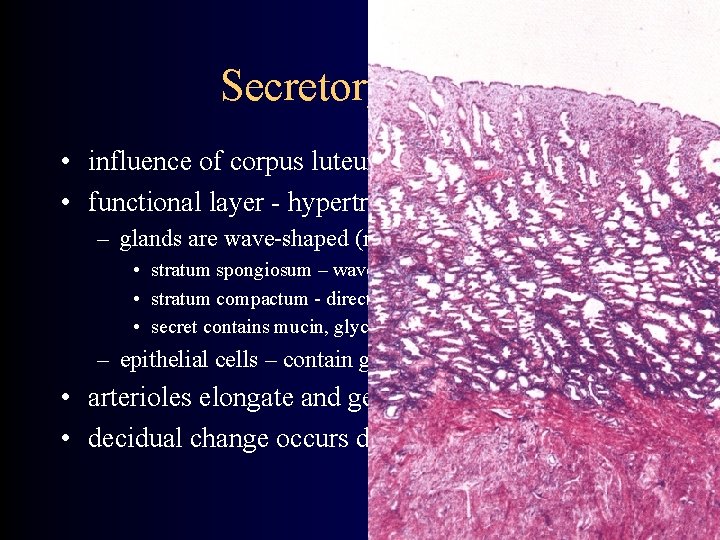
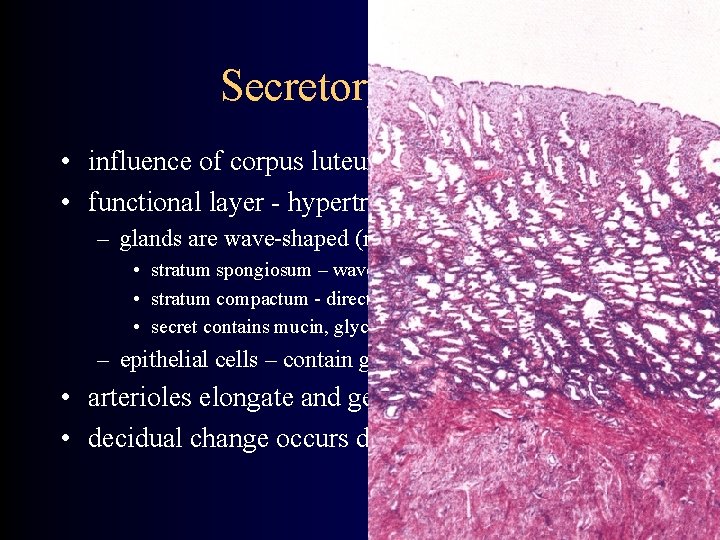
Secretory phase • influence of corpus luteum hormones • functional layer - hypertrophy ( size) – glands are wave-shaped (not in apical and basal parts) • stratum spongiosum – wave-shaped • stratum compactum - direct • secret contains mucin, glycogen and lipids – epithelial cells – contain glycogen and mucin • arterioles elongate and get wave-shaped • decidual change occurs during the nidation
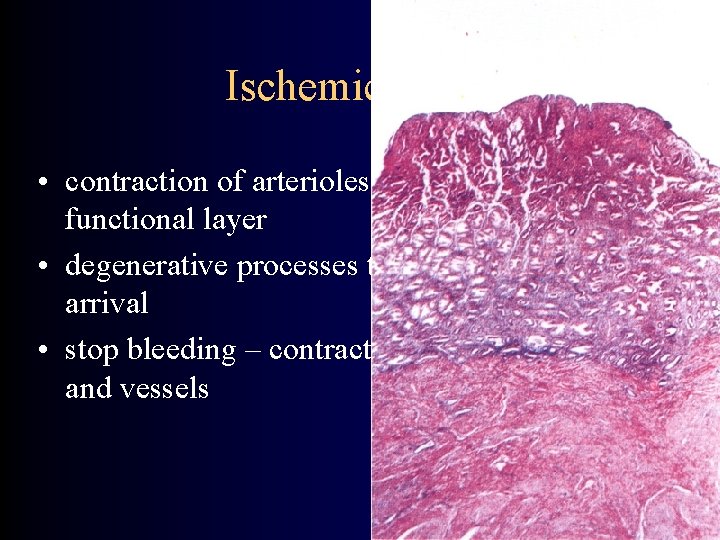
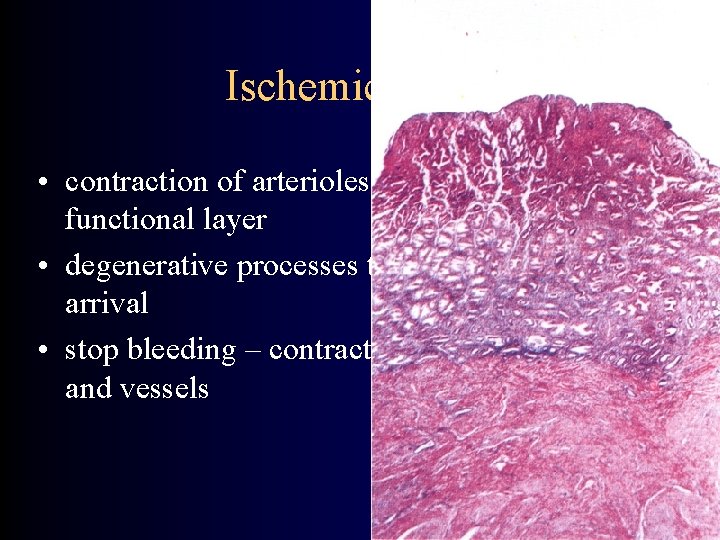
Ischemic phase • contraction of arterioles – ischemia of functional layer • degenerative processes thanks to leukocytes arrival • stop bleeding – contraction of myometrium and vessels
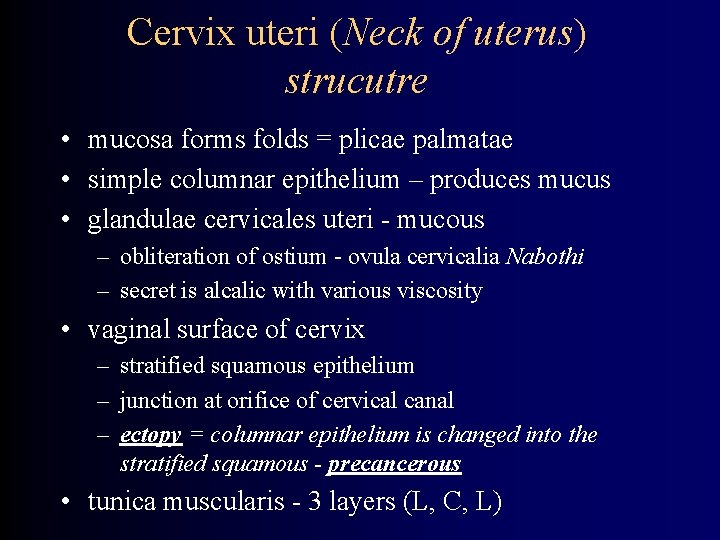
Cervix uteri (Neck of uterus) strucutre • mucosa forms folds = plicae palmatae • simple columnar epithelium – produces mucus • glandulae cervicales uteri - mucous – obliteration of ostium - ovula cervicalia Nabothi – secret is alcalic with various viscosity • vaginal surface of cervix – stratified squamous epithelium – junction at orifice of cervical canal – ectopy = columnar epithelium is changed into the stratified squamous - precancerous • tunica muscularis - 3 layers (L, C, L)

Cervix uteri - HE
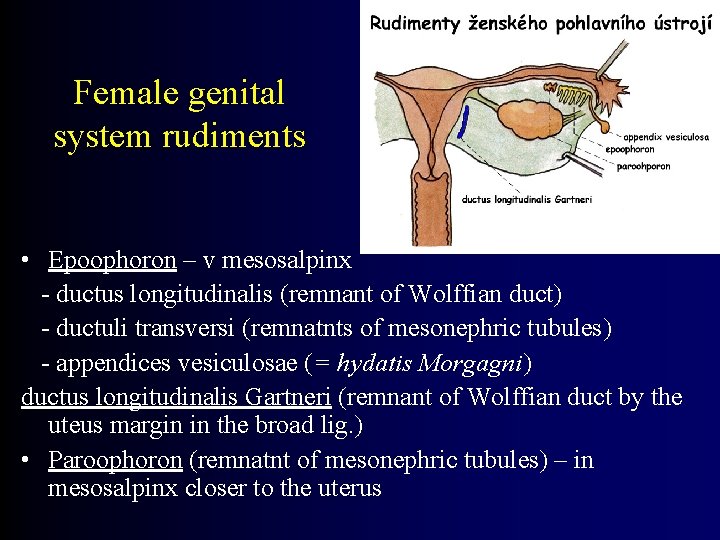
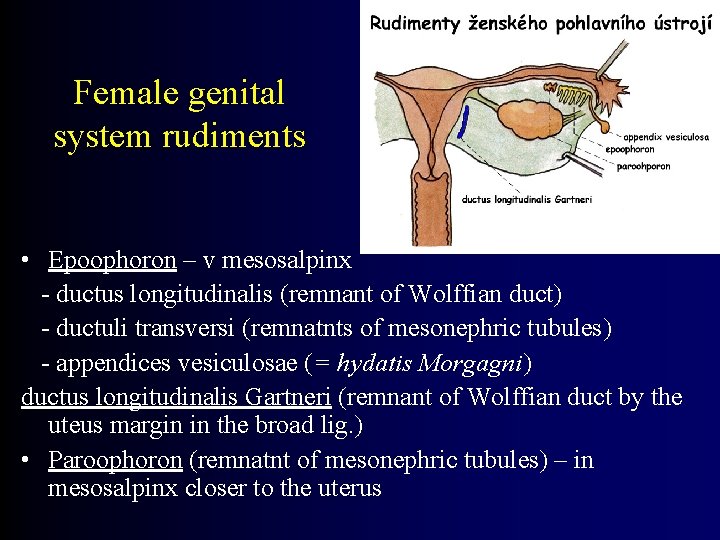
Female genital system rudiments • Epoophoron – v mesosalpinx - ductus longitudinalis (remnant of Wolffian duct) - ductuli transversi (remnatnts of mesonephric tubules) - appendices vesiculosae (= hydatis Morgagni) ductus longitudinalis Gartneri (remnant of Wolffian duct by the uteus margin in the broad lig. ) • Paroophoron (remnatnt of mesonephric tubules) – in mesosalpinx closer to the uterus
Vagina (gr. kolpos) • Description: – Fornix anterior, posterior, laterales – Paries (wall) anterior, posterior – Hymen • carunculae hymenales (remnants after defloration) • Section: – rugae – columnae rugarum (ant. + post. ), carina urethralis, area trigonalis Pawliki • Fixation and position: – septum urethrovaginale et rectovaginale – excavatio rectouterina – m. pubovaginalis
Vagina – blood supply • arteries: a. iliaca interna → a. vaginalis (sometimes missing) → a. uterina → r. vaginalis → a. rectalis media → r. vaginalis → a. pudenda int. → r. vaginalis • veins: → v. iliaca int. plexus venosus uterovaginalis → v. pudenda int. → v. uterina
Vagina – lymph drainage and nerves • lymph drainage: – n. l. iliaci int. + ext. – n. l. inguinales superficiales (caudally below hymen) • nerves: – nn. vaginales z plexus uterovaginalis plexus hypogastricus inf. – n. pudendus (caudally below hymen)
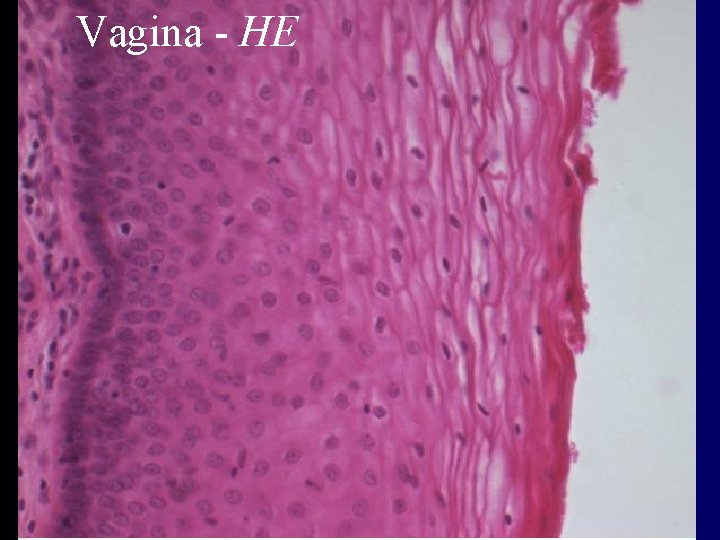
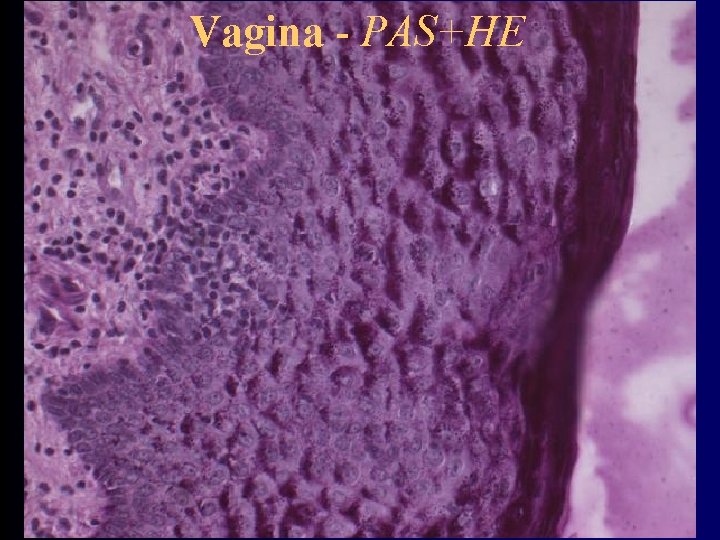
Vagina – inner structure • tunica mucosa – folds and columns - columna rugarum, rugae vaginales – epithelium – stratified squamous (? keratinizing ? ) • cells produce glycogen – acid environment – exfoliative cytology – lamina propria – loose connective tissue • no glands • tunica muscularis – inner - circular, outer - longitudinal • adventitia – dense connective tissue, vessels, nerves
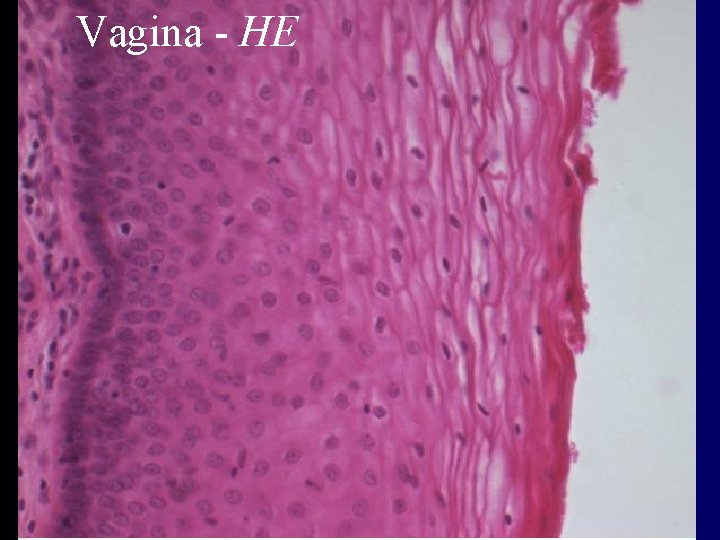
Vagina - HE
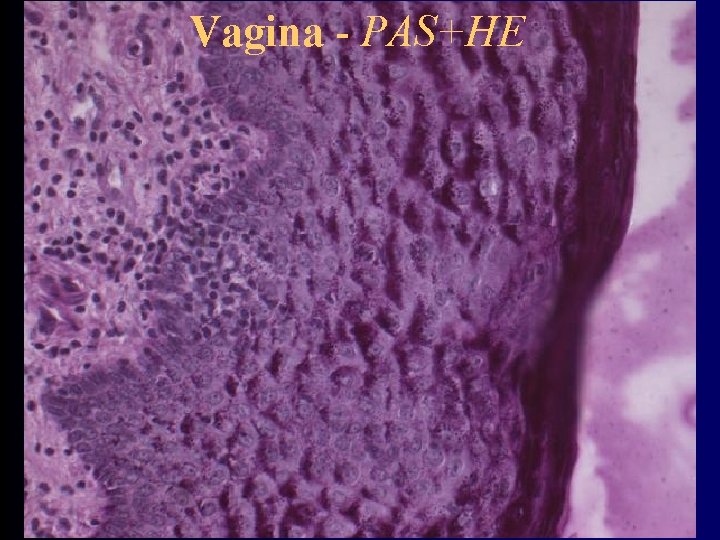
Vagina - PAS+HE
Exfoliative vaginal cytology • Proliferative phase – cells with acidophilic (= eosinophilic) cytoplasma • Secretory phase - cells with basophilic cytoplasma
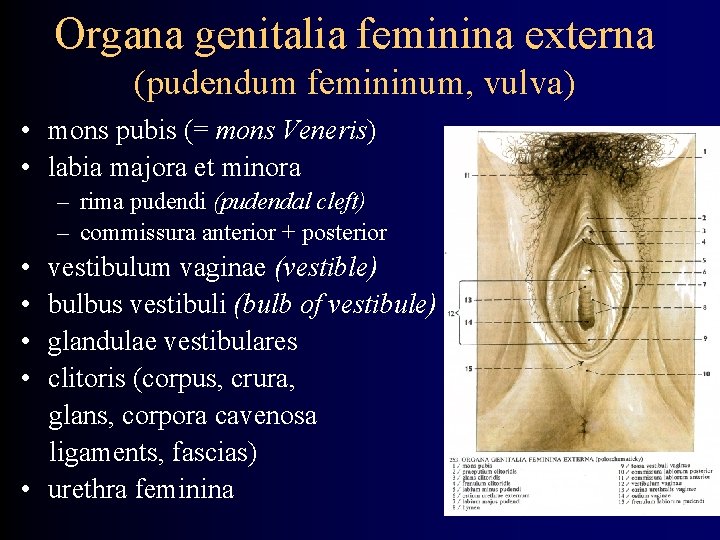
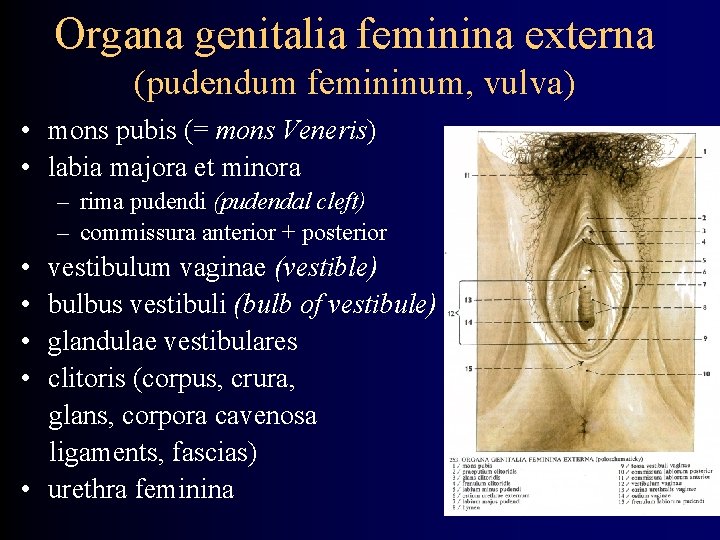
Organa genitalia feminina externa (pudendum femininum, vulva) • mons pubis (= mons Veneris) • labia majora et minora – rima pudendi (pudendal cleft) – commissura anterior + posterior • • vestibulum vaginae (vestible) bulbus vestibuli (bulb of vestibule) glandulae vestibulares clitoris (corpus, crura, glans, corpora cavenosa ligaments, fascias) • urethra feminina
Female external genitalia - structure • labia majora – connective tissue, adipose cells – outer surface – skin with hair follicles, sebaceous, apocrine and sweat glands – inner – no follicles, only sebaceous glands • labia minora – no adipose cells, no hair follicles – stratified squamous epithelium – slightly keratinizing – sebaceous gland - smegma praeputii
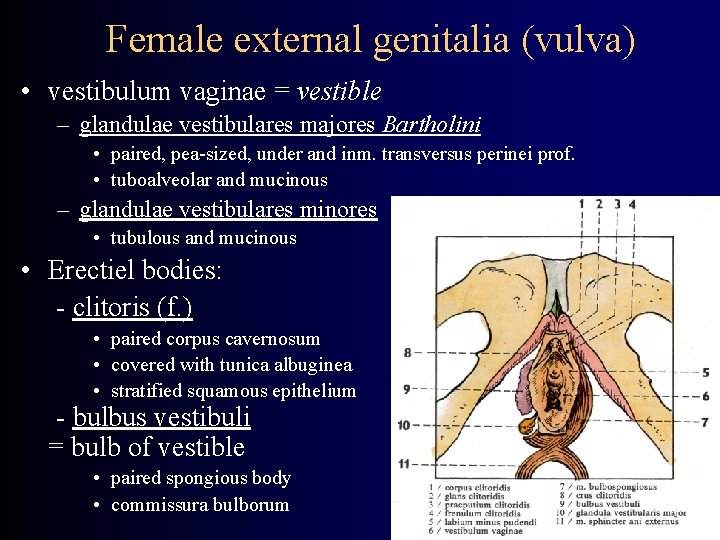
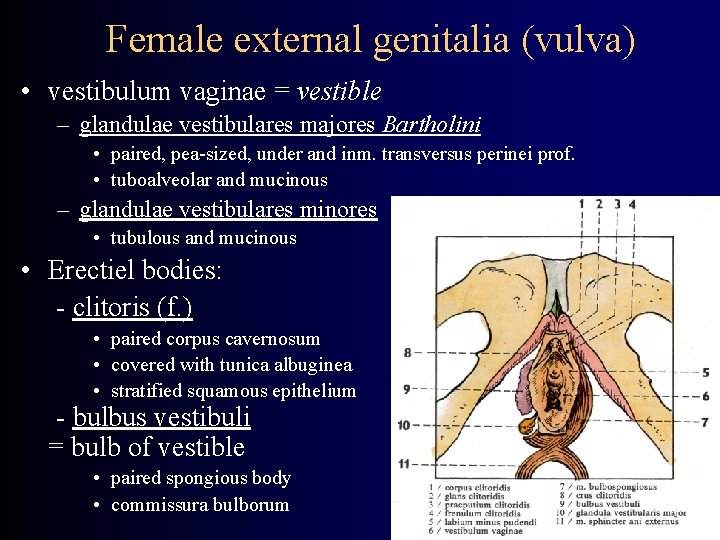
Female external genitalia (vulva) • vestibulum vaginae = vestible – glandulae vestibulares majores Bartholini • paired, pea-sized, under and inm. transversus perinei prof. • tuboalveolar and mucinous – glandulae vestibulares minores • tubulous and mucinous • Erectiel bodies: - clitoris (f. ) • paired corpus cavernosum • covered with tunica albuginea • stratified squamous epithelium - bulbus vestibuli = bulb of vestible • paired spongious body • commissura bulborum
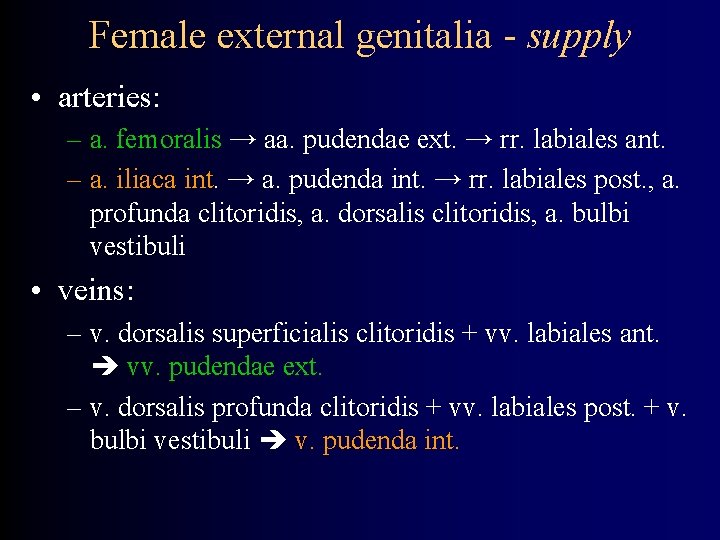
Female external genitalia - supply • arteries: – a. femoralis → aa. pudendae ext. → rr. labiales ant. – a. iliaca int. → a. pudenda int. → rr. labiales post. , a. profunda clitoridis, a. dorsalis clitoridis, a. bulbi vestibuli • veins: – v. dorsalis superficialis clitoridis + vv. labiales ant. vv. pudendae ext. – v. dorsalis profunda clitoridis + vv. labiales post. + v. bulbi vestibuli v. pudenda int.
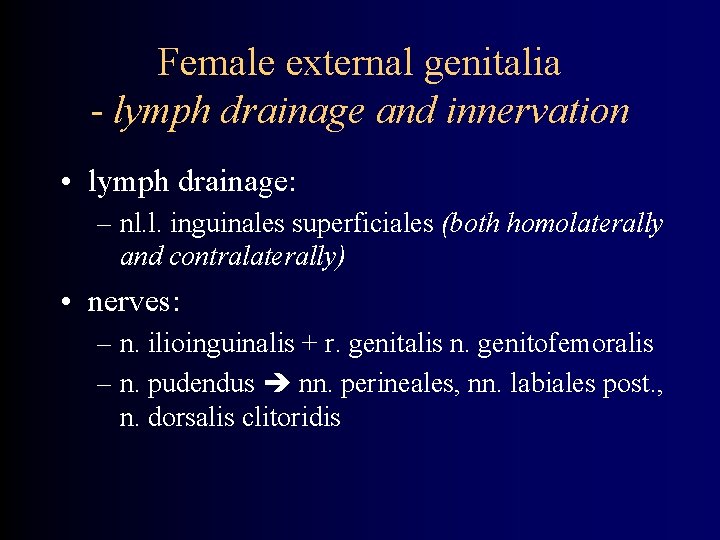
Female external genitalia - lymph drainage and innervation • lymph drainage: – nl. l. inguinales superficiales (both homolaterally and contralaterally) • nerves: – n. ilioinguinalis + r. genitalis n. genitofemoralis – n. pudendus nn. perineales, nn. labiales post. , n. dorsalis clitoridis
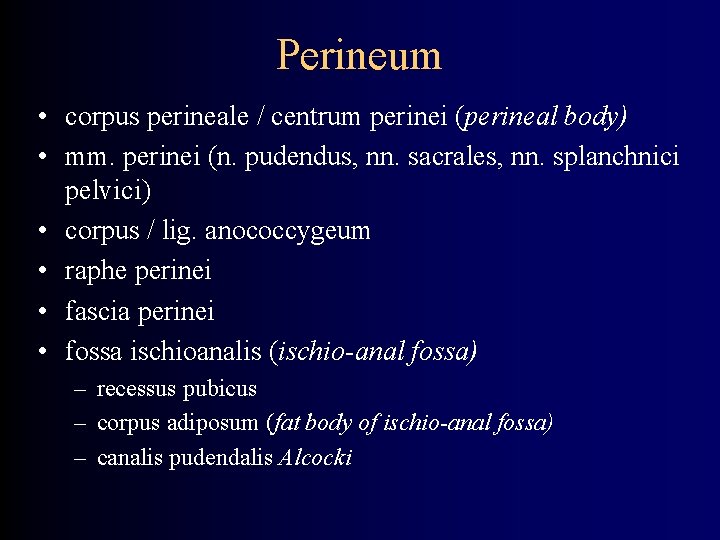
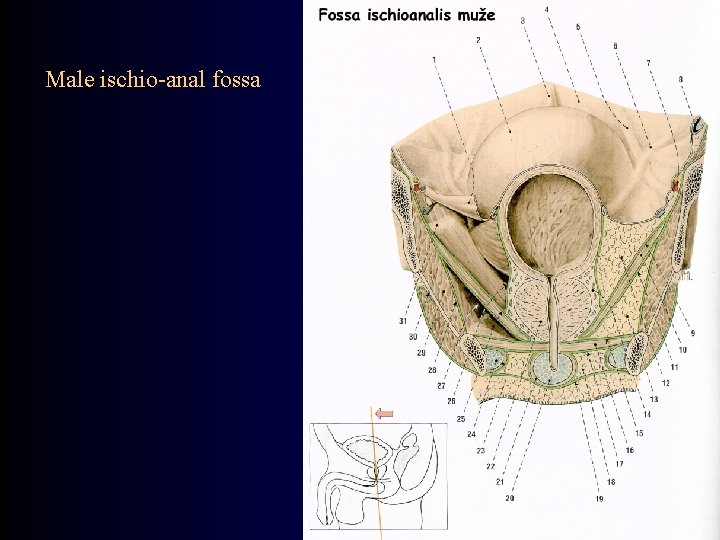
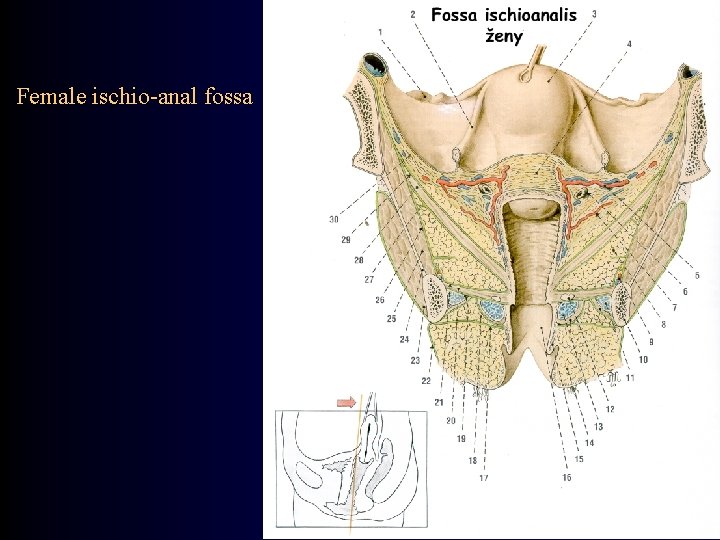
Perineum • corpus perineale / centrum perinei (perineal body) • mm. perinei (n. pudendus, nn. sacrales, nn. splanchnici pelvici) • corpus / lig. anococcygeum • raphe perinei • fascia perinei • fossa ischioanalis (ischio-anal fossa) – recessus pubicus – corpus adiposum (fat body of ischio-anal fossa) – canalis pudendalis Alcocki
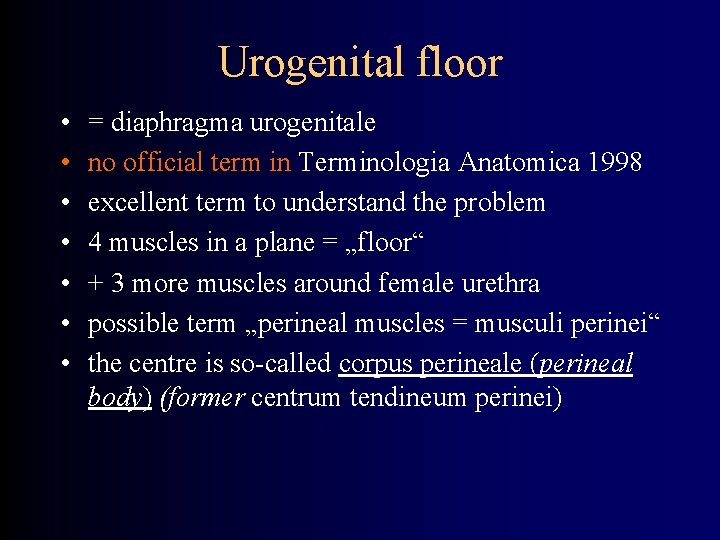
Urogenital floor • • = diaphragma urogenitale no official term in Terminologia Anatomica 1998 excellent term to understand the problem 4 muscles in a plane = „floor“ + 3 more muscles around female urethra possible term „perineal muscles = musculi perinei“ the centre is so-called corpus perineale (perineal body) (former centrum tendineum perinei)
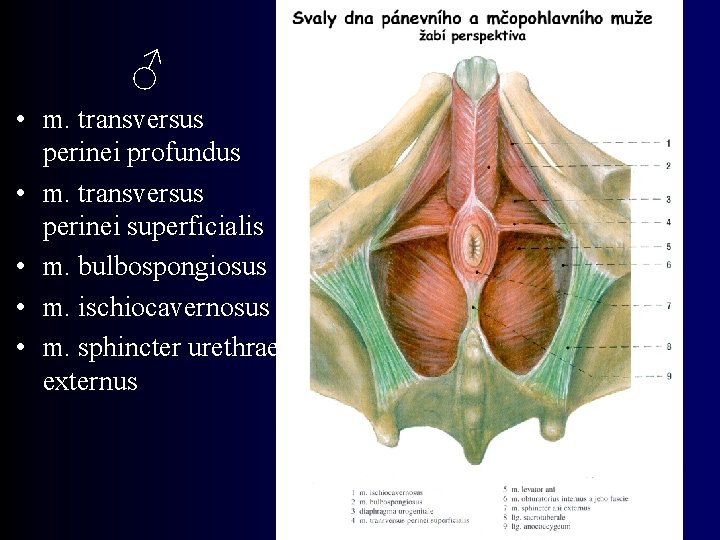
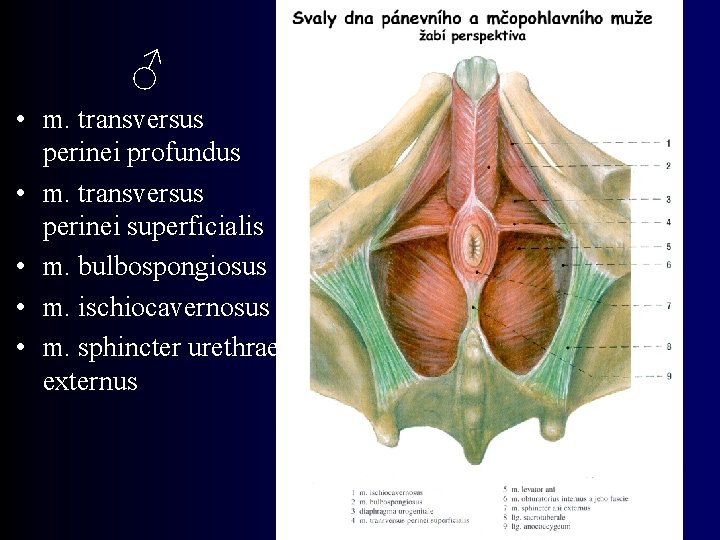
♂ • m. transversus perinei profundus • m. transversus perinei superficialis • m. bulbospongiosus • m. ischiocavernosus • m. sphincter urethrae externus
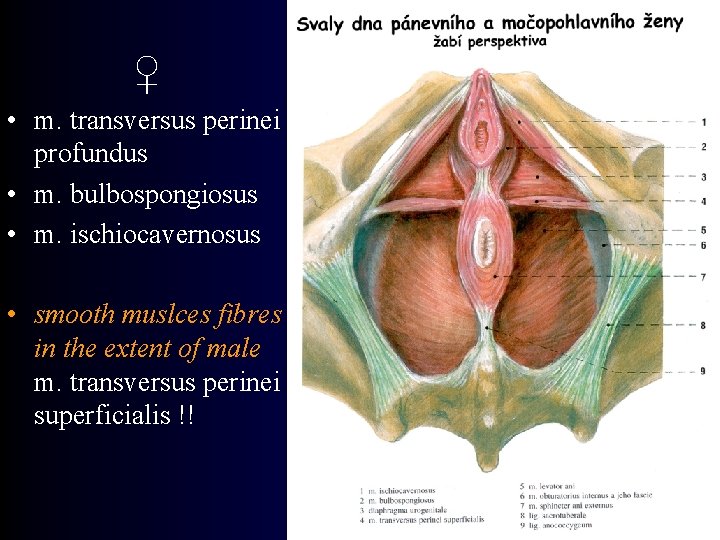
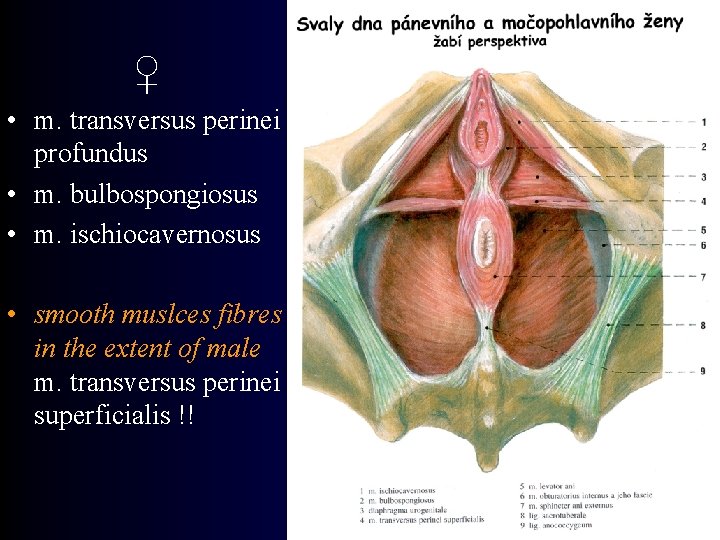
♀ • m. transversus perinei profundus • m. bulbospongiosus • m. ischiocavernosus • smooth muslces fibres in the extent of male m. transversus perinei superficialis !!
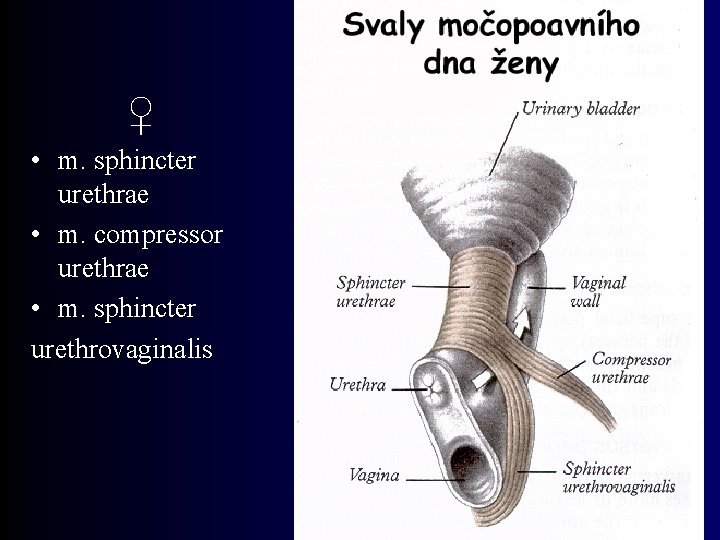
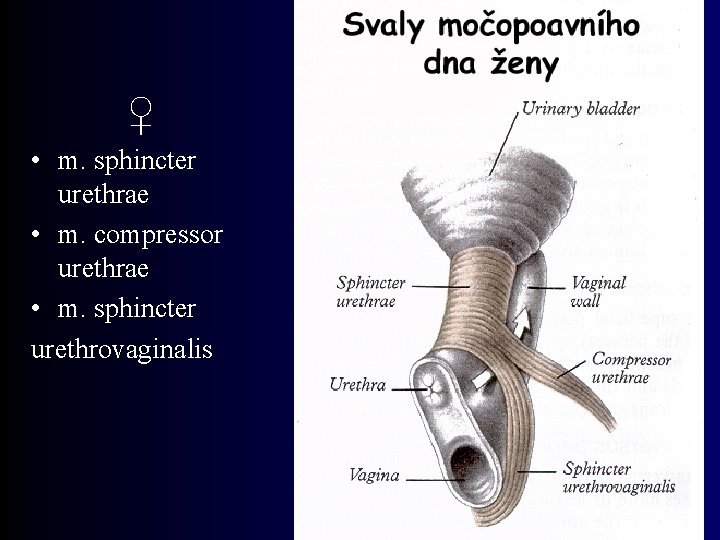
♀ • m. sphincter urethrae • m. compressor urethrae • m. sphincter urethrovaginalis
Urogenital floor - innervation • nn. perineales n. pudendi • rr. ventrales nn. sacralium • nn. splanchnici pelvici
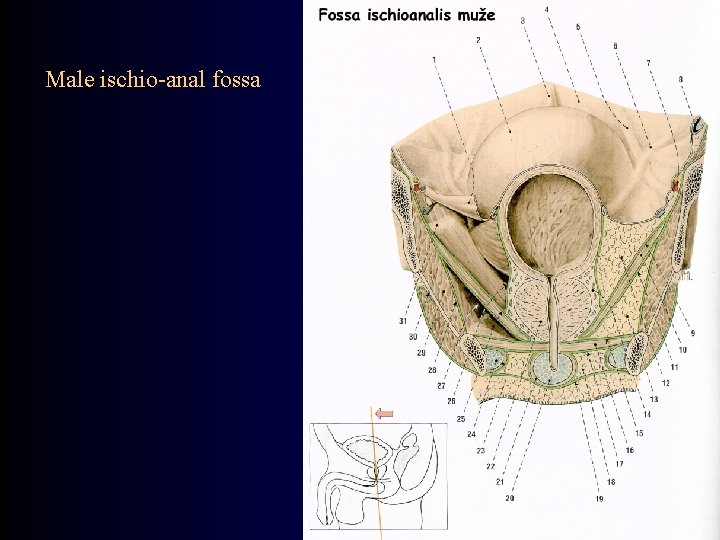
Male ischio-anal fossa
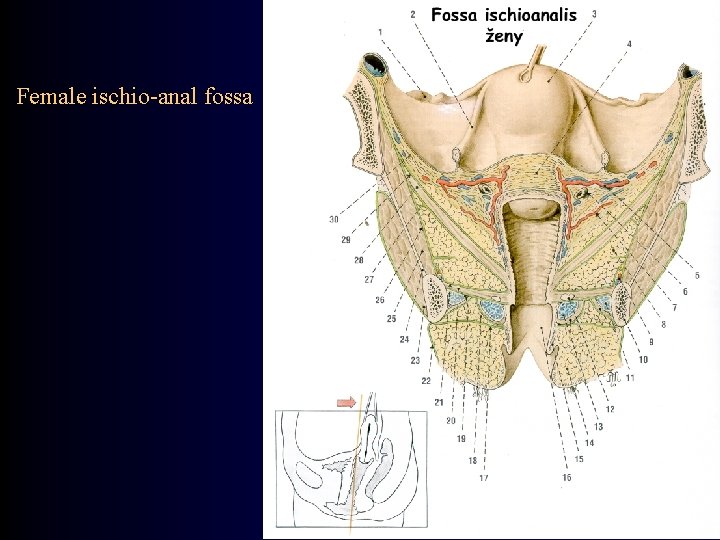
Female ischio-anal fossa