Syntactic Interoperability and the Role of Standards PERTEMUAN
Syntactic Interoperability and the Role of Standards PERTEMUAN Ke - 8 Taufik Rendi Anggara. , MT Manajemen Informasi Kesehatan Fakultas Ilmu Kesehatan
LEARNING OBJECTIVES • List and describe the different levels of interoperability and the role of each in health information exchange (HIE). • Describe the principles of messaging and its role in HIE. • Categorize messaging standards and distinguish their application in health care. • Describe the process for developing standards in health care. • Identify and describe available resources and services for organizations seeking to implement standards.
SYNTACTIC INTEROPERABILITY Schemas and templates constrain the vast array of possible message types and information that could potentially be put into any given message. Being compliant with constraints leads to robust and standard messages the facilitate interoperability. Fig. 1. 1 presents a section of HL 7 v 3 message that defines the guardian or caretaker for a patient. There are specific tags, enclosed in < >, for each type of information (eg, id, name, etc. ) in the section. There is also a structure to the section as indicated by the indentation as well as the color coding inside the tags. We can infer from this section that John Doe is the guardian and his telephone number is 555 -5001. Complete messages in health care much more complex, but they are constructed using these basic “building blocks. ”
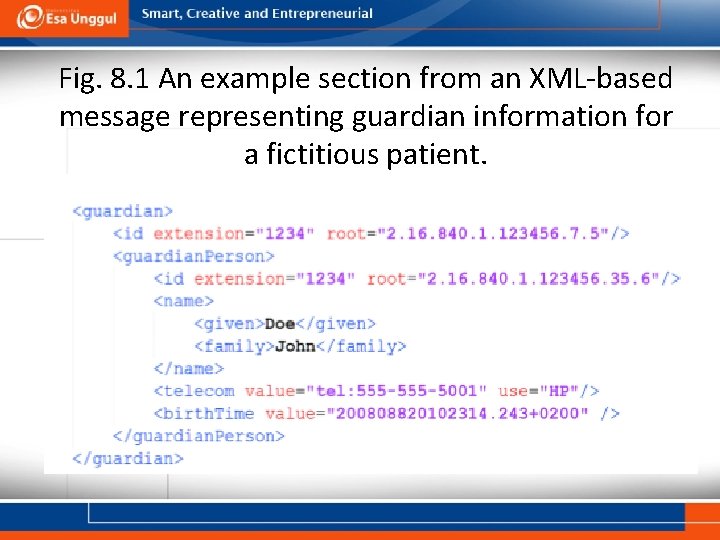
Fig. 8. 1 An example section from an XML-based message representing guardian information for a fictitious patient.
HEALTH INFORMATION MESSAGING STANDARDS Syntactic interoperability is achieved through the use of standards. Standards in health IT are broadly organized in four categories: • Vocabulary/code sets/terminology (semantic interoperability) • Structure and Content (syntactic interoperability) • Transport (foundational interoperability) • Services (syntactic interoperability)
Structure and Content Standards Health Level Seven (HL 7) is the leading and most widely recognized syntactic standard in health IT. The “level 7” in its name refers to the application layer of the OSI (Open Systems Interconnection) model, a conceptual model that characterizes and standardizes interactions within a computer system regardless of its underlying technology. The seventh layer of the OSI model describes application-layer functions that typically includes synchronizing communication between computer systems. HL 7 is an event trigger model in which the sending application transmits a message after a trigger is fired. The main cause for a trigger is a health-care event, such as the registration of a patient at a primary care clinic, discharge of a patient from an acute care hospital, or completion of a laboratory test for the presence of a disease. Receiving systems can then act upon the message, inferring the action that occurred based on the message type and responding to that action. For example, an A 01 message indicates the registration of a patient. A computer system that receives an A 01 message could respond by querying the HIE network for recent information on the patient available at other institutions for presentation to a clinician prior to the clinical encounter. The receipt of an ORU message for a laboratory result in which a test for the presence of Methicillin-resistant Staphylococcus aureus could cause a different computer system to examine the value of the result and alert a clinician to review the result or an infection preventionist to initiate an isolation protocol.
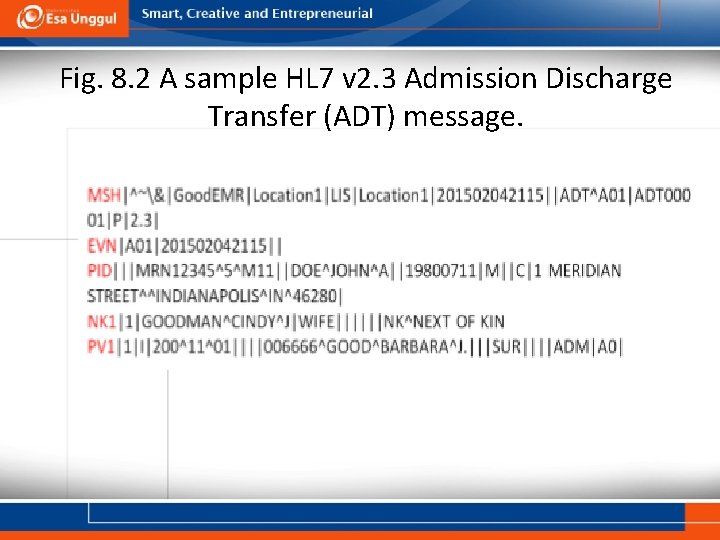
Fig. 8. 2 A sample HL 7 v 2. 3 Admission Discharge Transfer (ADT) message.
Benefits of V 3 as Provided on The HL 7 • Focuses on semantic interoperability by specifying that information be presented in a complete clinical context that assures that the sending and receiving systems share the meaning (semantics) of the information being exchanged. • Provides consistent representation of data laterally across the various HL 7 domains of interest and longitudinally over time as new requirements arise and new fields of clinical endeavor are addressed. • Designed for universal application so that the standards can have the broadest possible global impact and yet be adapted to meet local and regional requirements.
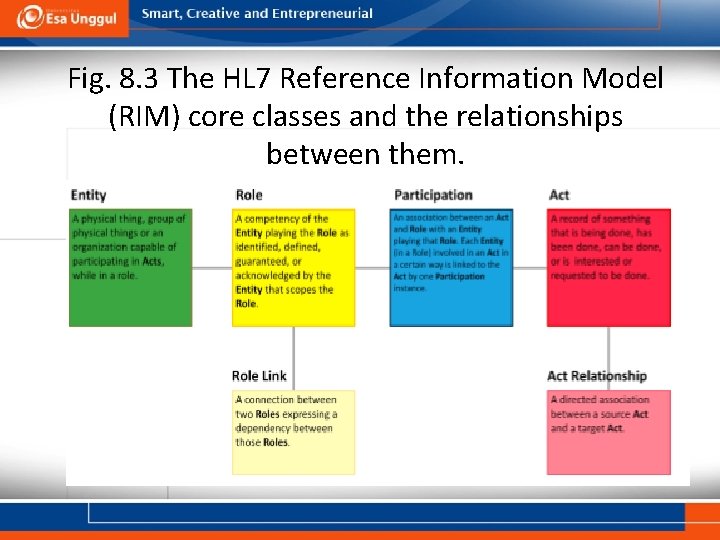
Fig. 8. 3 The HL 7 Reference Information Model (RIM) core classes and the relationships between them.
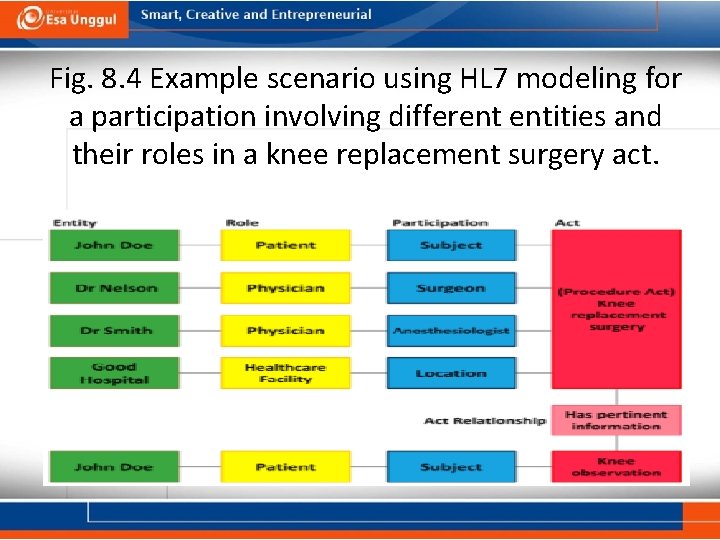
Fig. 8. 4 Example scenario using HL 7 modeling for a participation involving different entities and their roles in a knee replacement surgery act.
Digital Imaging and Communications in Medicine (DICOM (Digital Imaging and Communications in Medicine) is the most widely adopted standard in the world for the exchange and management of medical images. Since introducing DICOM in 1993, providers have been able to use fully digital images with high resolution instead of physical X-ray films. Using DICOM, images generated by different types of medical imaging devices (eg, X -ray, CT, MRI, ultrasound) can be integrated into picture archiving and communication systems (PACS) and they can be exchanged in HIE networks. The DICOM standard not only encodes the image but also a set of metadata and attributes that describe the image and can be used by other applications in health-care delivery.
National Council for Prescription Drug Programs (NCPDP) The National Council for Prescription Drug Programs (NCPDP) standardizes electronic exchange of data for prescribing, dispensing, monitoring, managing, and paying for medications and pharmacy services. Currently there are 26 different standards developed by NCPDP; yet only three of them are endorsed for implementation (Telecommunication, SCRIPT, and Manufacturer Rebate). The NCPDP telecommunication standard provides a structure to electronically submit third-party drug claims as well as perform eligibility verification and prior authorization. SCRIPT supports transmitting prescription information electronically in support of fulfilling new prescriptions, prescription refill requests, relaying medication history, and transactions for long-term care.
Standards for HIE Services A valid, well-constructed message is a major step towards HIE, yet it is only one component of syntactic interoperability. To successfully exchange information, one also needs syntactic standards for the envelope and transactions that will move valid messages from Hospital A to Hospital B. In this section of the chapter, we review existing, mature efforts that support HIE implementers’ efforts to establish interoperable exchange of information. While some may not consider these initiatives to be true technical standards, they provide guidance and support for standardizing transactions, in many ways helping to provide the extra 20% effort needed to achieve interoperability.
Integrating the Health-Care Enterprise (IHE) There are four major services provided by IHE to address interoperability issues in health care globally: • Problem Identification: Many clinical and IT experts gather together and identify different use cases and scenarios in health care that require HIE. These experts focus on certain domains and extract the needs for interoperability as well as clinical workflow. • Profile Specification: After identifying the gaps and challenges in health information interoperability, the experts focus on identifying established standards for communication among systems in these use cases to develop HIE Profiles. HIE profiles describe, in detail, how to use different messaging, terminology, and technical standards to enable HIS to communicate. Vendors in health IT use these profiles to address interoperability challenges in critical areas in health-care settings.
Cont. • Connectathon Testing: After developing systems using IHE profiles, vendors participate in a carefully planned and supervised event called the IHE Connectathon to test their application and exchange data with other vendors’ products to evaluate the level of interoperability and assess the maturity and accuracy of their implementation. • Integration Statements: After testing their systems at the IHE Connectathon, vendors publish IHE Integration Statements to state that their product is tested based on IHE guidelines and they are compliant with IHE Profiles. Integration Statements demonstrate that a given application supports IHE profiles and facilitates the process of product acquisition in health-care facilities.
e. Health Exchange The e. Health Exchange formerly known as the Nationwide Health Information Network (Nw. HIN) is the foundation for national health interoperability in the United States. Unlike IHE, the e. Health Exchange is itself an HIE network. The network consists of state and regional HIE networks as well as federal agencies such as the Social Security Administration and Department of Veterans Affairs. The e. Health Exchange functions as a federated network in which health information is maintained at the source and queried when it is needed. Supporting its transactions is a framework of technical standards carefully selected and supported by the e. Health Exchange. Thus the e. Health Exchange provides HIE services for its members rather than technical infrastructure or data.
Standards & Interoperability (S&I) Framework The Standards & Interoperability (S&I) Framework, established by ONC, provides a collaborative environment in the United States among public and private sectors to develop tools, services, and guidelines to facilitate interoperability in health care. Like IHE, the S&I Framework brings clinical subject matter experts and health IT professionals together to focus on a singular challenge in health care for which a robust “profile” can be developed. Through a well-defined process, a group of stakeholders can define a narrow use case, identify available standards, and create implementation guidance that enables adoption of the standards. However, unlike IHE, the S&I Framework also asks its teams to then take the next steps of creating a reference implementation of the profile, then facilitate pilot projects that test the use case in a few communities, and then develop HIS certification and testing criteria to support scaling HIE across the nation. S&I Framework as well as the various products it has created to date can be found on its website: http: //www. siframework. org/.
SUMMARY Technical standards provide a foundation for interoperability in HIE. While necessary, standards are not sufficient for achieving the goal of seamless HIE among health-care stakeholders. Additional effort is necessary to integrate complex HIS, which requires collaboration among providers, vendors, and other stakeholders. Integration profiles and IGs, created by multistakeholder groups, are required to fully connect systems in support of interoperability. Work continues to evolve standards, refine IGs, and support implementation of standards in many countries. While the road ahead is long, the end result will be more efficient health systems that support better outcomes for both patients and populations.
- Slides: 18