SYNDROME OF GOITER ANATOMY OF THE THYROID GLAND










- Slides: 74
SYNDROME OF GOITER


ANATOMY OF THE THYROID GLAND Location - neck, anterior to the trachea, between the cricoid cartilage and the suprasternal notch n Consists of two lobes connected by an isthmus n Normal weight in adults – 20 -30 g. n Highly vascular, and soft in consistency. n Innervations: sympathetic and parasympathetic nerves n
Function of thyroid gland Biosynthesis and production of two hormones: - thyroxine (T 4) - triiodothyronine (T 3)
REGULATION OF THE THYROID FUNCTION Hypothalamic thyrotropinereleasing hormone (TRH) stimulates pituitary production of thyroid-stimulating hormone (TSH) TSH stimulates thyroid hormone synthesis and secretion.
ENDOCRINE FEEDBACK LOOP Thyroid hormones inhibit TRH and TSH production n Reduced levels of thyroid hormone increase basal TSH production and enhance TRH-mediated stimulation of TSH n High thyroid hormone levels suppress TSH and inhibit TRH-mediated stimulation of TSH n
THYROID HORMONES PHYSIOLOGICAL EFFECTS Activation of sympathetic nervous system n Increase of metabolic rate n Increase of oxygen consumption (hypoxia, depletion of ATP) n Activation of oxidative phosphorylation n Stimulation of glycogenolysis n Stimulation of lipolysis n Stimulation of proteins synthesis and catabolism n
CLASSIFICATION OF THE DISORDERS OF THYROID GLAND I. Congenital a) aplasia and hypoplasia (with hypothyrosis) b) aberrant thyroid gland c) persistent thyroglossal ductus
CLASSIFICATION OF THE DISORDERS OF THYROID GLAND II. Iodine deficiency diseases Endemic goiter a) Degree of enlargement; 0; I; II b) Forms: diffuse; nodular; mixed c) Thyroid function: euthyrosis; hypothyrosis with cretinism; hyperthyrosis
CLASSIFICATION OF THE DISORDERS OF THYROID GLAND III. Sporadic goiter (degree of enlargement, forms, thyroid function) IV. Toxic adenoma ( solitary, multinodular) V Diffuse toxic goiter a) mild b) moderate c) severe
CLASSIFICATION OF THE DISORDERS OF THYROID GLAND VI. HYPOTHYROIDISM a) b) c) mild moderate severe
CLASSIFICATION OF THE DISORDERS OF THYROID GLAND VII. Inflammatory thyroid diseases a) Immune inflammation n acute thyroiditis (suppurative and non-suppurative) subacute thyroiditis (de Quervain's thyroiditis, granulomatous thyroiditis, or viral thyroiditis) chronic thyroiditis (Hashimoto's thyroiditis and Riedel's thyroiditis) b) Infectious inflammation (tuberculosis, syphilis, actinomycosis)
CLASSIFICATION OF THE DISORDERS OF THYROID GLAND VIII. Trauma of thyroid gland IX. Thyroid cancer
Diffuse toxic goiter (GRAVES' DISEASE) n This is the most common cause of hyperthyroidism and is due to autoimmune process. n 1835 - Robert Graves n 1840 – Karl Basedow
Diffuse toxic goiter (GRAVES' DISEASE) Epidemiology accounts for 60 to 80% of thyrotoxycosis. n occurs in up to 2% of women and in 0, 2% of men. n rarely begins before adolescence and typically occurs between 20 and 50 years of age, may also occurs in the elderly. n
Diffuse toxic goiter (Graves ′disease ) n Systemic autoimmune disease due to production of serum Ig G antibodies to the thyroid TSH receptor stimulating thyroid hormone production behaving like TSH. It's manifested by diffuse goiter and clinical syndrome of thyrotoxicosis.
Etiology of Graves ′disease n There is an association with HLA- В 8 , DR 3, and DR 2 and 50% concordance is seen among monozygotic twins with 5% concordance in dizygotic twins. n Provoking factors are stresses, infections, tobacco smoking, insolation.
Diffuse toxic goiter Pathogenesis The hyperthyroidism is caused by TSH-Rstimulating immunoglobulins that bind to the receptor and mimic the action of TSH thereby stimulating thyroid hormone synthesis and secretion. Other thyroid autoimmune responses coexist in these patients, and therefore there is no direct correlation between the levels of TSI and thyroid hormones.
Diffuse toxic goiter Clinical manifestations Main complains: n Hyperactivity, irritability, dysphoria n Palpitation n Weight loss with increased appetite n Proptosis n Tremor n Diarrhea n Sweating n Fatigue and weakness
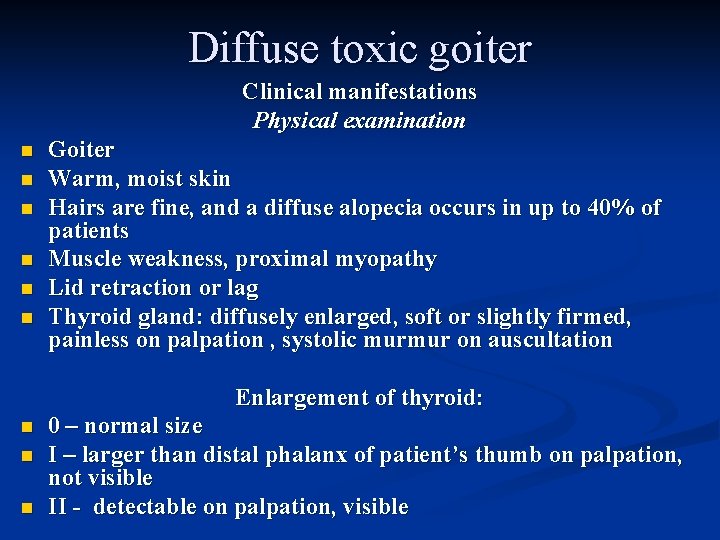
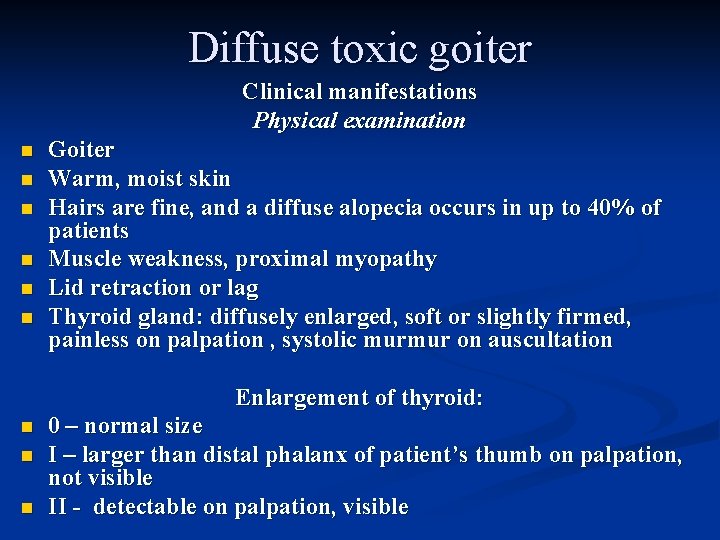
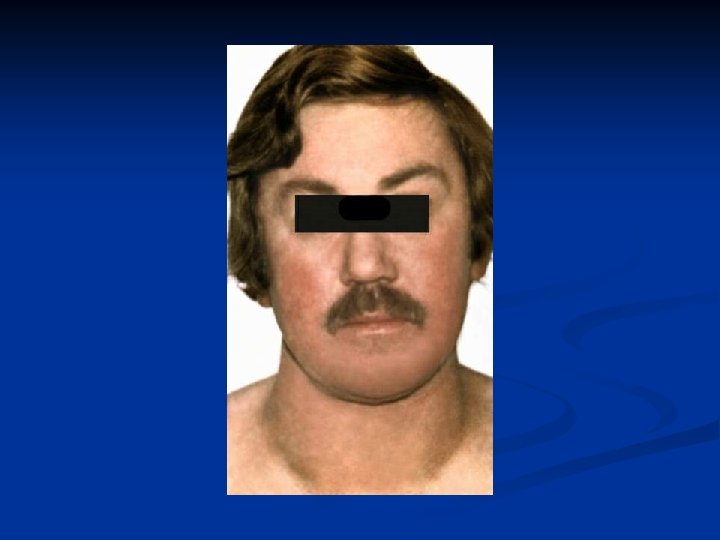
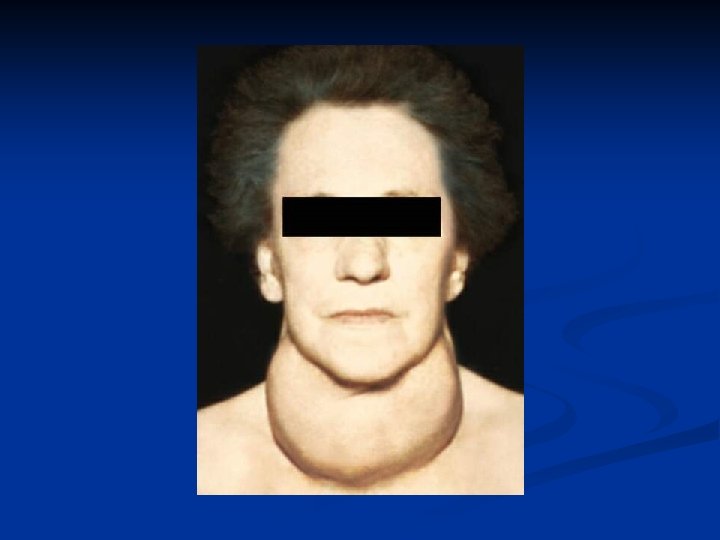
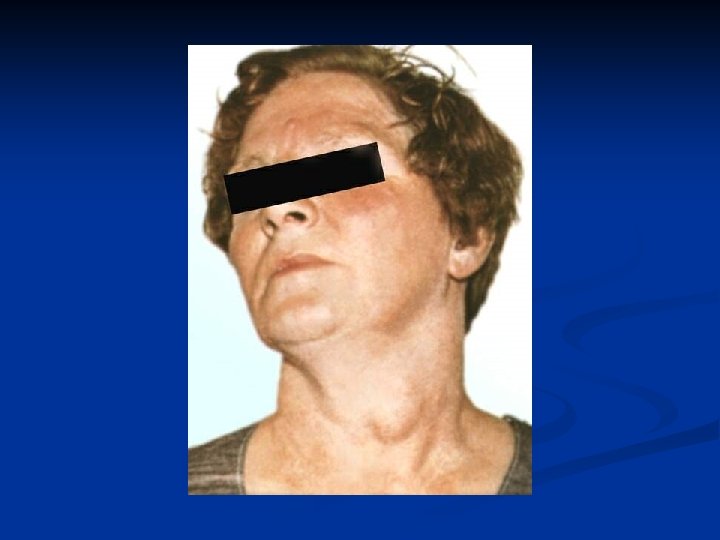
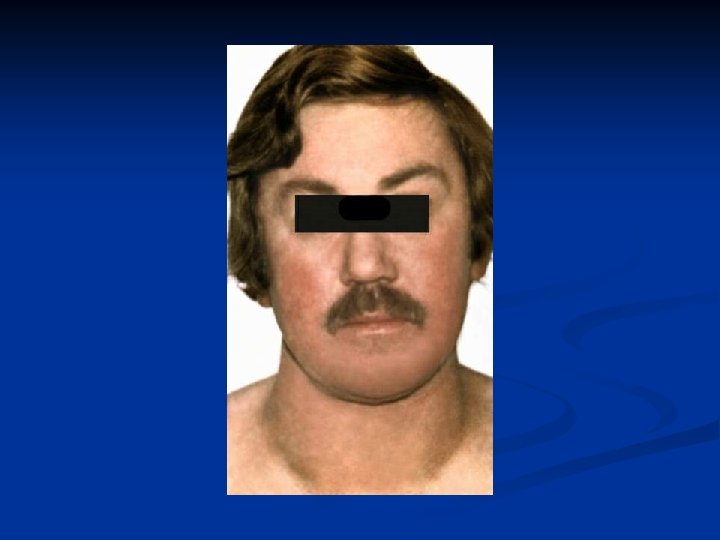
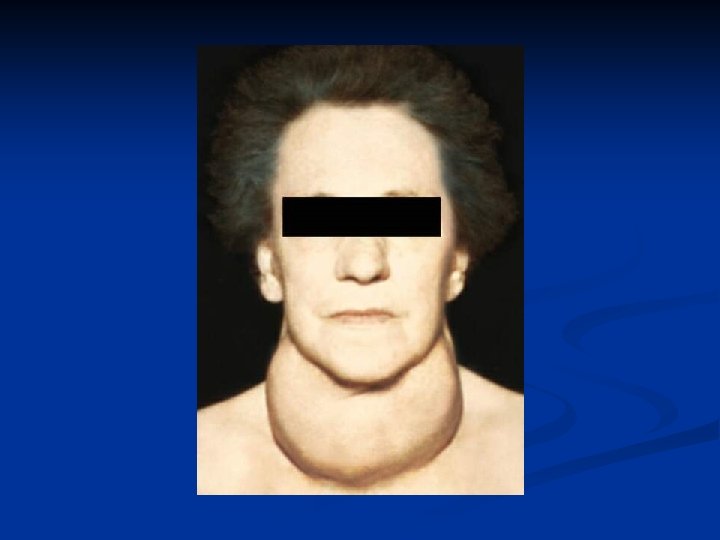
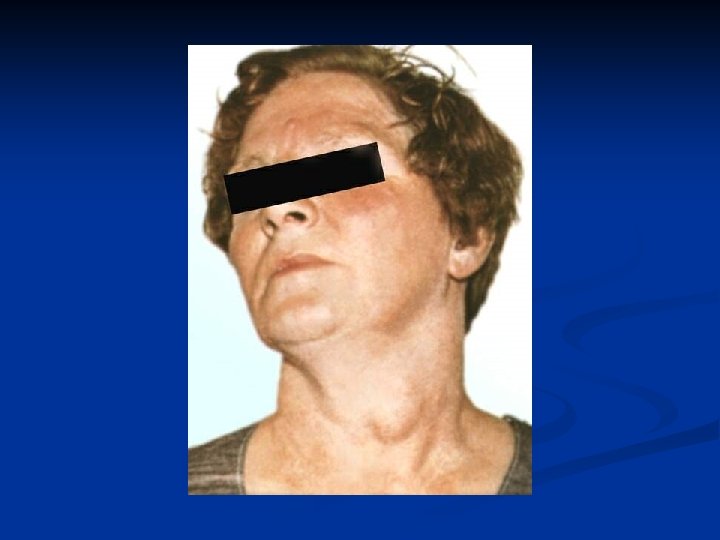
Diffuse toxic goiter Clinical manifestations Physical examination n n n Goiter Warm, moist skin Hairs are fine, and a diffuse alopecia occurs in up to 40% of patients Muscle weakness, proximal myopathy Lid retraction or lag Thyroid gland: diffusely enlarged, soft or slightly firmed, painless on palpation , systolic murmur on auscultation Enlargement of thyroid: n n n 0 – normal size I – larger than distal phalanx of patient’s thumb on palpation, not visible II - detectable on palpation, visible

Methods of thyroid gland palpation


Diffuse toxic goiter Laboratory evaluation T 4 and T 3 are increased n TSH is low n Determination of TSH-R-stimulating immunoglobulins n Determination of thyroid peroxidase (TPO) antibodies n
Diffuse toxic goiter THYROID SCANNING The thyroid gland selectively transports radioisotopes of iodine (123 I, 125 I, 131 I) and 99 m. Tc pertechnetate, allowing thyroid imaging and quantitation of radioactive tracer fractional uptake. Graves' disease is characterized by an enlarged gland increased tracer uptake that is distributed homogeneously.
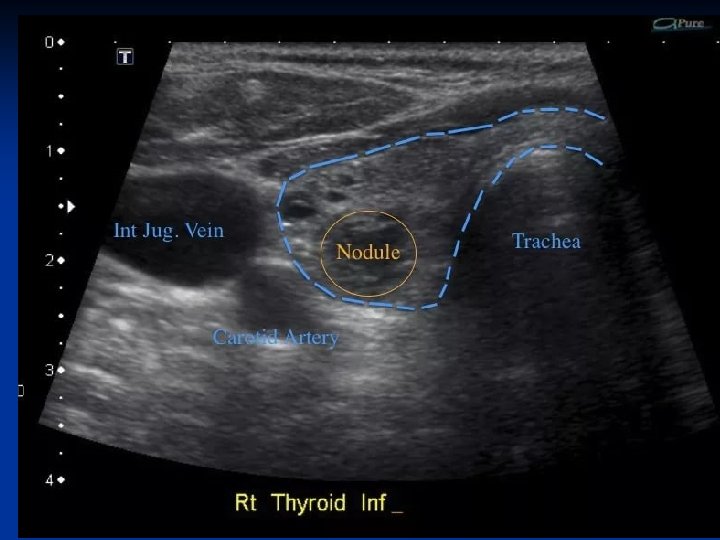
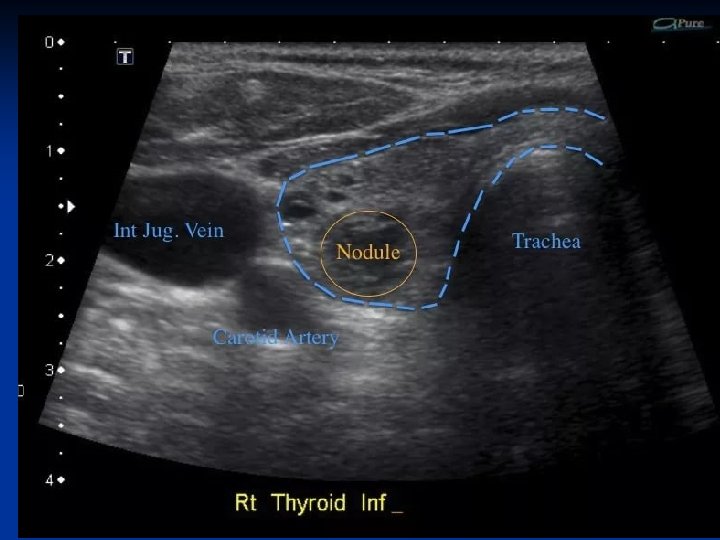
Diffuse toxic goiter THYROID ULTRASOUND Ultrasonography is used to assist in the diagnosis of nodular thyroid disease. In addition to detecting thyroid nodules, ultrasound is useful for monitoring nodule size, for guiding biopsies, and for the aspiration of cystic lesions.
Diffuse toxic goiter Diagnosis Biochemically confirmed thyrotoxicosis n Diffuse goiter on palpation n Ophthalmopathy n Positive thyroid peroxidase (TPO) antibodies n Positive TSH-R-stimulating immunoglobulins n
Diffuse toxic goiter Differential Diagnosis Diseases, that mimic thyrotoxicosis n Panic attacks n Mania n Pheochromocytoma n Weight loss associated with malignancy
Diffuse toxic goiter Differential Diagnosis Diseases, that cause thyrotoxicosis Nodular thyroid disease (palpation, radionuclide or ultrasound scan) Destructive thyroiditis (palpation, radionuclide or ultrasound scan) Ectopic thyroid tissue (palpation, radionuclide or ultrasound scan) Pituitary tumor secreting TSH (nonsuppressed TSH level, and the finding of a pituitary tumor on computed tomography (CT) or magnetic resonance imaging (MRI) scan).

Diffuse toxic goiter TREATMENT n Reducing thyroid hormone synthesis (antithyroid drugs, thyrostatics) n Reducing the amount of thyroid tissue (subtotal thyroidectomy or radioiodine (131 I) treatment)
DIFFUSE NONTOXIC (SIMPLE) GOITER endemic goiter (when it affects >5% of the population of the region) – iodine deficiency sporadic goiter – cause unknown
Endemic goiter Is present in 200 million people over the world Severe endemia – accounts more than 60% of population; 15% of them have nodular goiters; male/female ratio >1/3 (in nonendemic regions 1/10)
DIFFUSE NONTOXIC (SIMPLE) GOITER Clinical manifestations Goiter - symmetrically enlarged, nontender, generally soft gland without palpable nodules. n If the thyroid is markedly enlarged, it can cause tracheal or esophageal compression. n Substernal goiter may obstruct the thoracic inlet. n Thyroid function usually is preserved, but in some cases hypothyroidism occurs n
DIFFUSE NONTOXIC (SIMPLE) GOITER TREATMENT Iodine replacement Children, adolescents – 100 -200 μg daily Adults – 300 -500 μg daily until normalization of the size of goiter, after that – 150 -200 μg daily Thyroid hormone replacement If TSH level exceeds 0, 5 m. U/l. Dose of Levothyroxine is adjusted on the basis of TSH levels, with the goal of treatment to maintain TSH level within the range 0, 25 -0, 5 m. U/l Levothyroxine treatment is usually combined with iodine (150 μg daily) Duration of Levothyroxine treatment – 2 years and longer. After that - iodine (150 -200 μg daily)
THYROIDITES Classification Acute thyriodities: suppurative, nonsuppurative n Subacute (viral) thyroiditis (de Quervain thyroiditis) n n Chronic thyroiditis
Chronic thyroiditis n n n n Autoimmune hypertrophic thyroiditis (Hashimoto’s goiter) Autoimmune atrophic thyroiditis Asymptomatic thyroiditis Painless thyroiditis Postnatal Specific: tuberculous, syphilitic, septicomycotic Ridel’s fibrous thyroiditis (as a symptom of some systemic diseases)

Acute thyroiditis Etiology: bacterial infection, more frequently caused by Str. pyogenes, Staph. aureus. n Pathogenesis: the ways of infection are lymphogenic or haematogenic. Usually one lobe is affected. n Unsuppurative thyroiditis is caused by ionizing radiation (radiation thyroiditis). n
Clinical features of acute purulent thyroiditis n n n Acute onset, body temperature is above 38 -39°С, rigor, tachycardia. TG is expanded, algetic. Pain irradiates to an ear and a mandible. Complications: Abscess formation: symptom of fluctuation. Hyperemia of skin over the lesion focus. Fistulae may open to the front surface of a neck or to mediastinum (mediastinitis), phlegmon of a neck.
Clinical features of acute nonsuppurative thyroiditis. On palpation - tenderness in TG region. n Thyrotoxicosis signs. n
Addition methods of investigation n Clinical blood count shift to the left) n Ultrasound of TG. n Biopsy. (leukocytosis with
Treatment of acute thyroiditis n n Hospitalization to surgical department. Antibacterial therapy with broad spectrum antibiotics. Lancing and draining of abscess. ß-adrenoreceptor blockers ( propranolol 20 -40 mg 3 times a day till full liquidation of clinical manifestations will be obtained). Analgesics.
Subacute thyroiditis n n Granulematous, viral, de Quervain, giantcell. Etiology: Coxsackie viruses, adenoviruses, mumps viruses, flu viruses, Epstein-Barr viruses. Pathogenesis: Viral penetration → destruction of TG → Т 3, Т 4 releasing into blood, transient thyrothoxicosis. On the tissue level - focal granulomatous infiltration by neutrophils and histiocytes.

Clinical features of subacute thyroiditis n n ↑ body temperature to 38 -39° С after 2 -3 weeks from ARD (viral etiology). Pain is on the affected side of a front surface of a neck. Pain extends to an ear or to a mandible from the same side. Pain increases during swallowing or head rotation. Sometimes palpation of TG is impossible due to severe pain. There are 4 stages: TRANSIENT THYROTOXICOSIS (4 -6 WEEKS) , EUTHYROIDISM, HYPOTHYROIDISM (2 -3 MONTH), CONVALISCENCE.
Additional methods of investigation Clinical blood count: lymphocytosis, abrupt increasing of ESR. n Hyper-γ-globulinemia. n ↑ content of fibrinogen n ↑ Т 3, ↑ Т 4 , then ↓Т 3, ↓Т 4 n Autoantibodies to thyroglobulin and TPO. n US of TG: hypoechoic focal areas. n TG Scanning (if needed) – area of inflammation ( «cold» area). n
Treatment of subacute thyroiditis Hospitalization into an endocrinological department. n Antiinflammatory therapy: - NSAIDs; - Corticosteroids - Prednisolon 30 -60 mg daily per os. n
Chronic autoimmune thyroiditis The most common form of thyroiditis n Etiology: association with HLA antigenes: HLA DR 3 and DR 5. F: M – 10 -15: 1. n Pathogenesis: n AT –autoimmune inflammation of TG. ↓ Т- supressors → → Т- helpers interact with native antigenes of TG cells. It combines with other autoimmune diseases. n Lymphoid infiltration of TG. n
Clinical manifestations of chronic autoimmune thyroiditis Function of TG: gradual changes from thyrotoxicosis at the onset and consequent euthyroidism to hypothyroidism. n TG is enlarged on palpation, its structure is solid, heterogeneous. n Frequent combination with other autoimmune or TG diseases. n
Additional methods of investigation Thyroid hormones’ rate evaluation. n Indication of antibodies to TG tissues, TPO. n Ultrasound of TG (hypoechogenity). n Biopsy is needed for differential diagnostics with nodular goiter. n
Treatment of autoimmune thyroiditis Conservative: - Treatment of TG functional status disturbances. Hyperthyroid phase: ß-blockers Hypothyroid phase: adequate replacement therapy - Levothyroxine 1, 6 μg⁄kg or 100 -150 μg daily. n
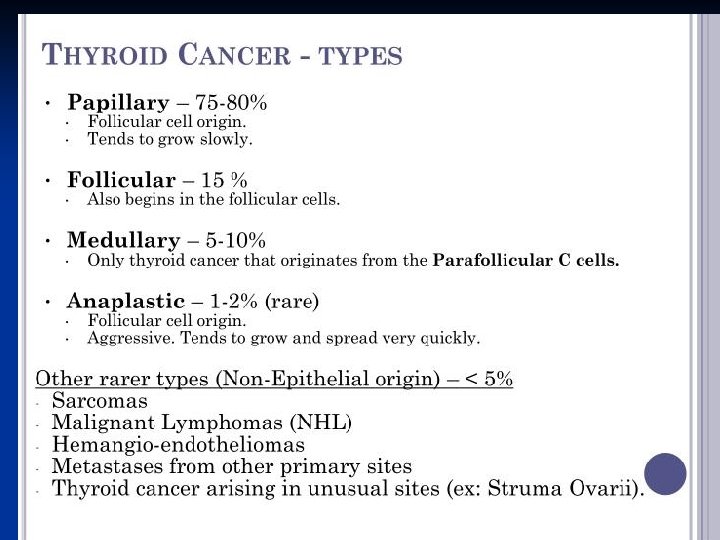
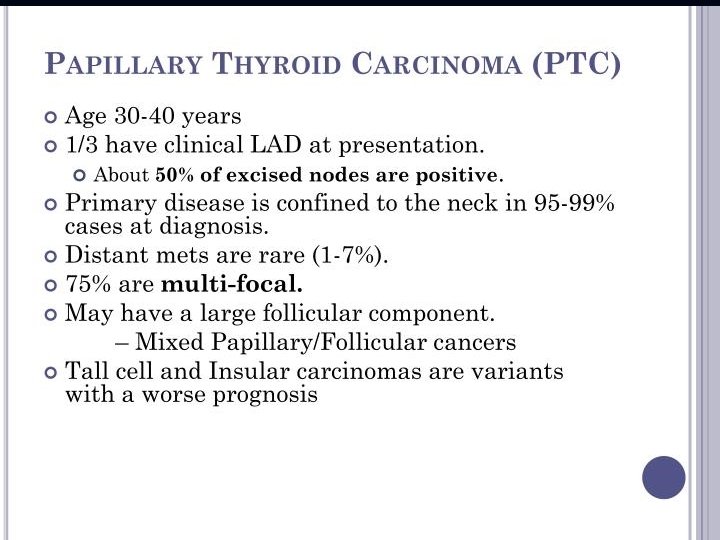
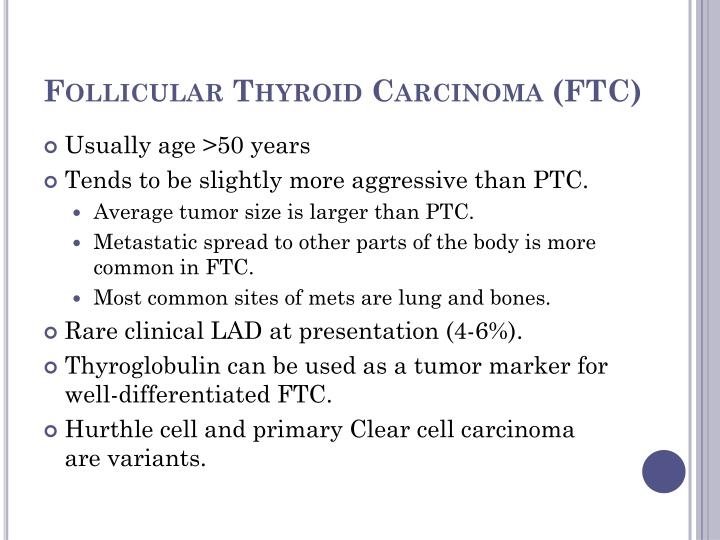
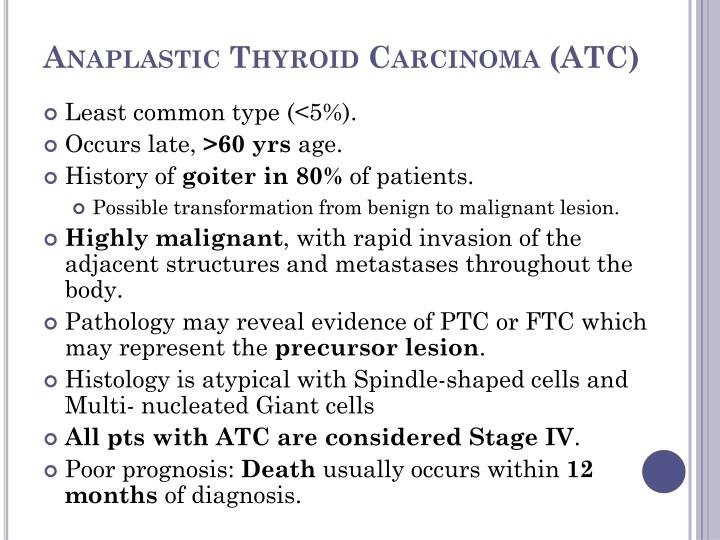
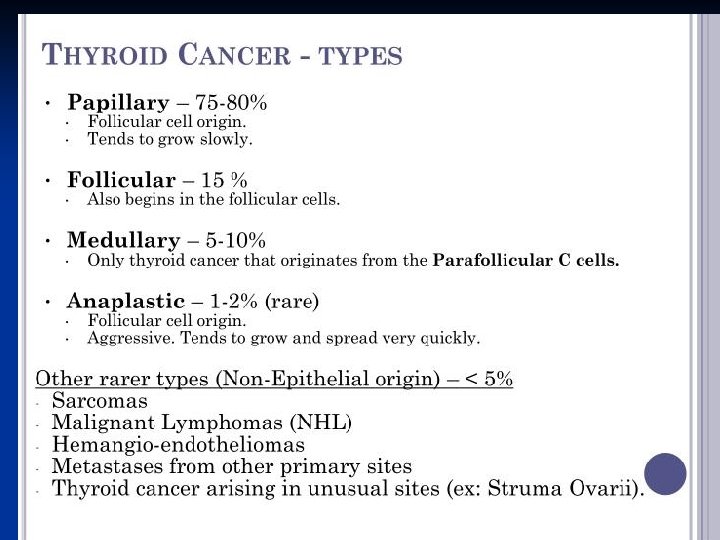
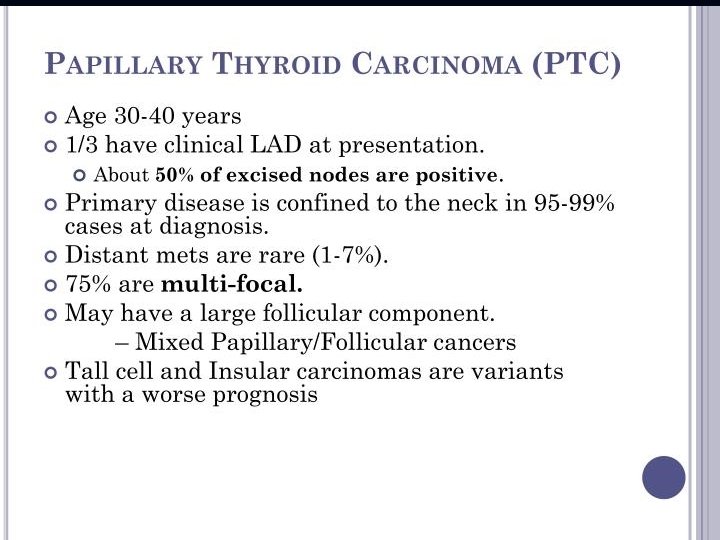
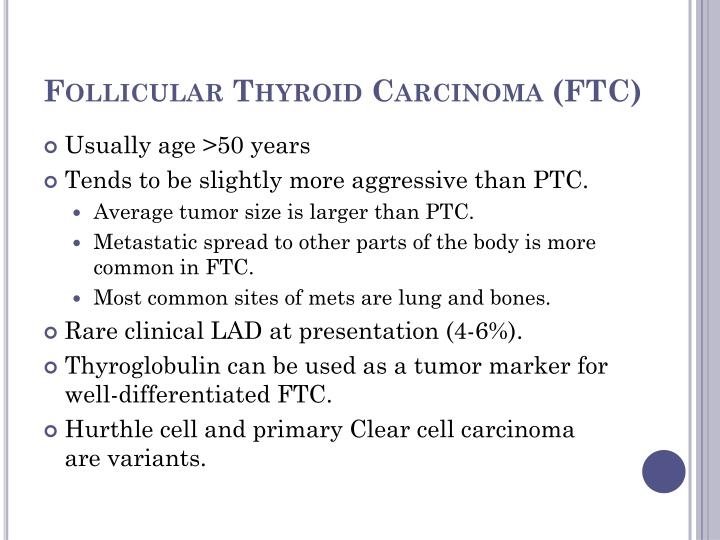
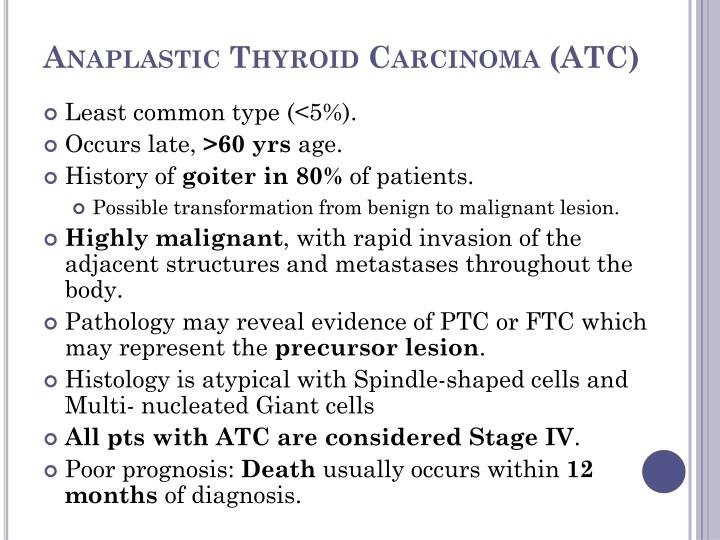
Tumors of thyroid gland
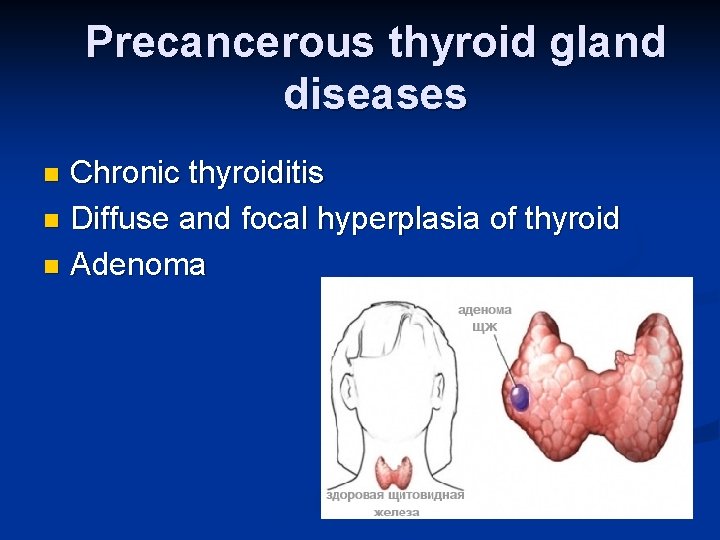
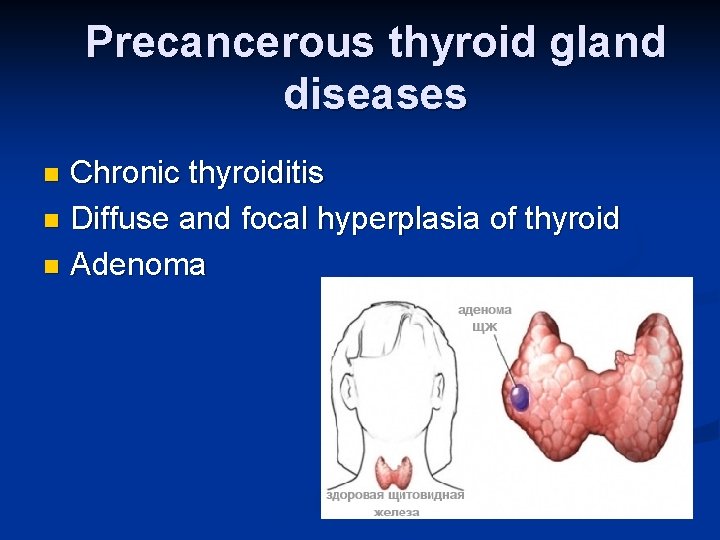
Precancerous thyroid gland diseases Chronic thyroiditis n Diffuse and focal hyperplasia of thyroid n Adenoma n