Syncope A work up for Internists and Hospitalists
- Slides: 51
Syncope A work up for Internists and Hospitalists Philip Dittmar January 31, 2014
• I have no conflicts of interest to disclose.
Syncope • The current state in healthcare • Classification of syncope • Costs of a “typical” work up • Ways to provide “High Value Cost Conscious Care”
Syncope • Transient loss of consciousness due to transient global cerebral hypoperfusion characterized by rapid onset, short duration, and spontaneous complete recovery. Moya A, Eur Heart J 2009
What we want to know? • What caused it to happen? • Will it happen again? • Is this a sign of other things? • Is it deadly?
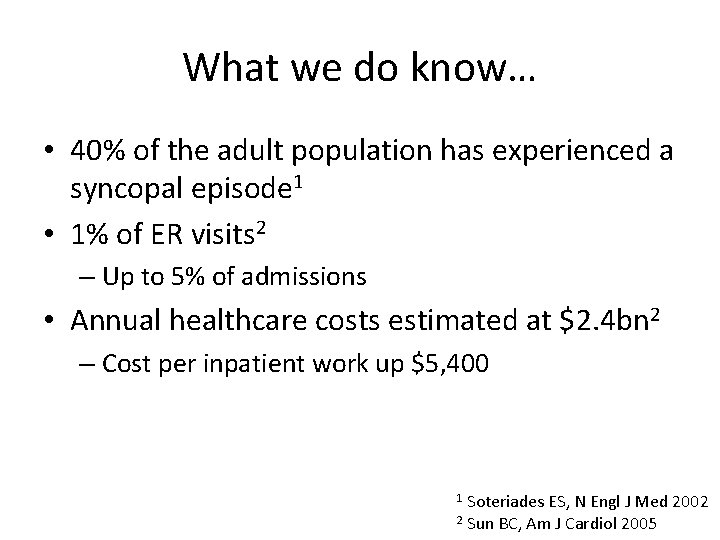
What we do know… • 40% of the adult population has experienced a syncopal episode 1 • 1% of ER visits 2 – Up to 5% of admissions • Annual healthcare costs estimated at $2. 4 bn 2 – Cost per inpatient work up $5, 400 Soteriades ES, N Engl J Med 2002 2 Sun BC, Am J Cardiol 2005 1
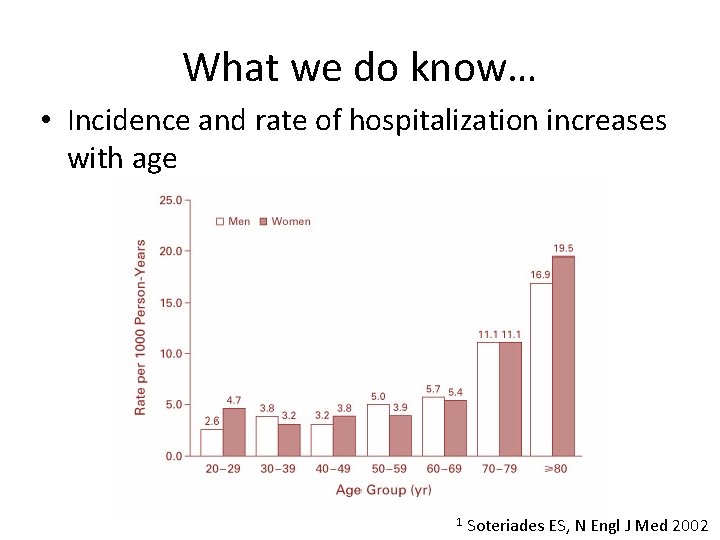
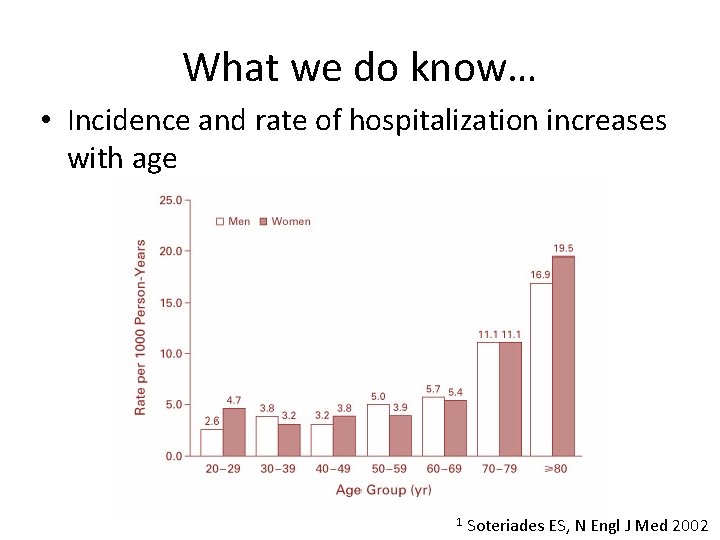
What we do know… • Incidence and rate of hospitalization increases with age 1 Soteriades ES, N Engl J Med 2002
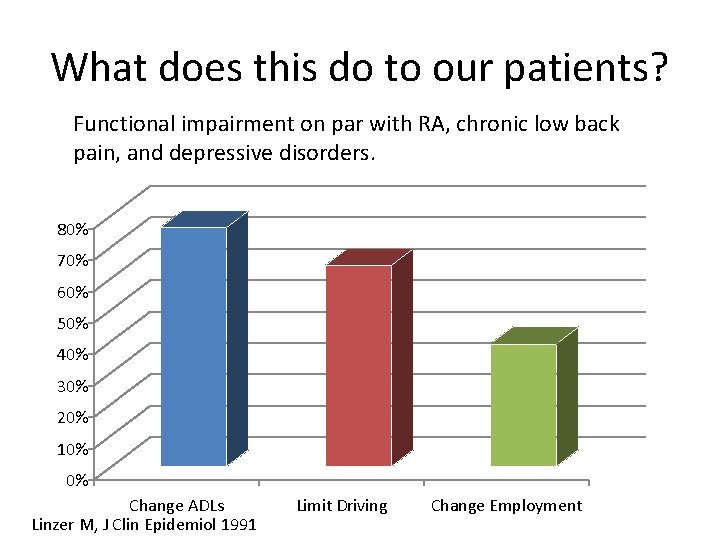
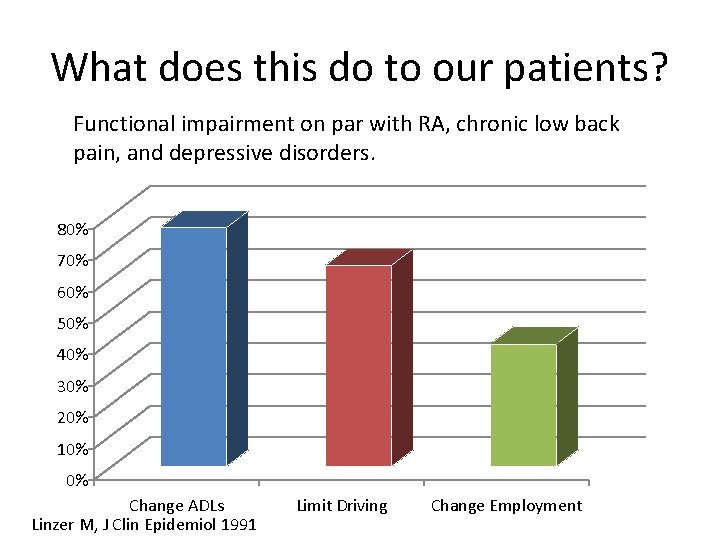
What does this do to our patients? Functional impairment on par with RA, chronic low back pain, and depressive disorders. 80% 70% 60% 50% 40% 30% 20% 10% 0% Change ADLs Linzer M, J Clin Epidemiol 1991 Limit Driving Change Employment
Syncope • The current state in healthcare • Classification of syncope • Costs of a “typical” work up • Ways to provide “High Value Care”
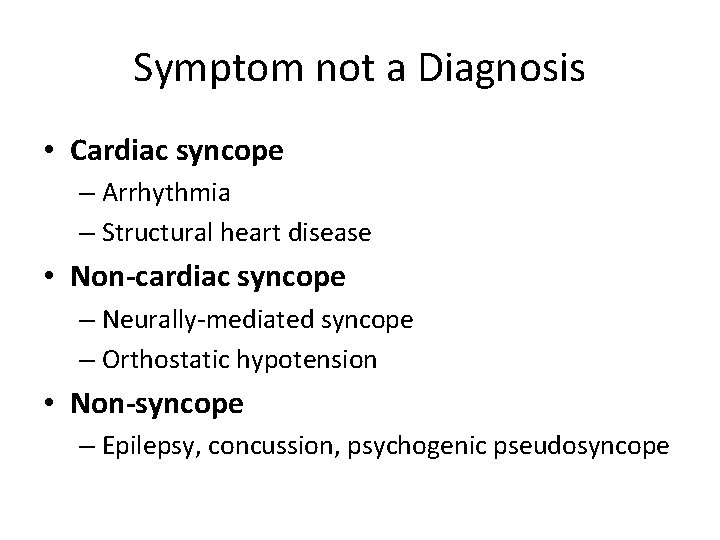
Symptom not a Diagnosis • Cardiac syncope – Arrhythmia – Structural heart disease • Non-cardiac syncope – Neurally-mediated syncope – Orthostatic hypotension • Non-syncope – Epilepsy, concussion, psychogenic pseudosyncope
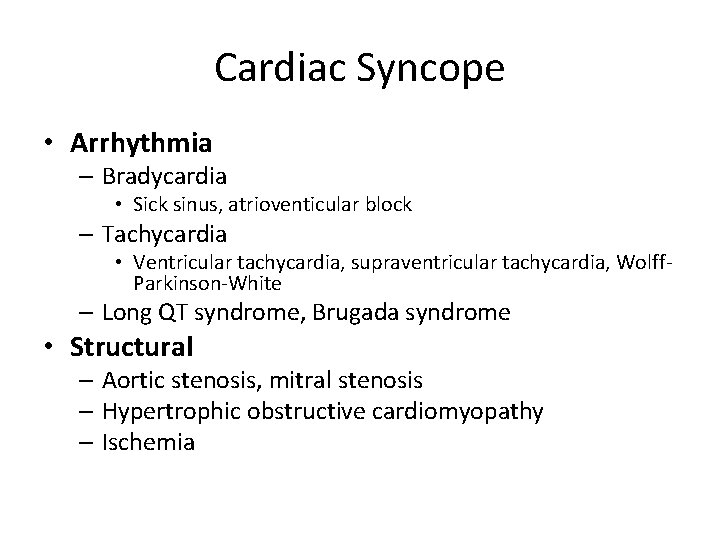
Cardiac Syncope • Arrhythmia – Bradycardia • Sick sinus, atrioventicular block – Tachycardia • Ventricular tachycardia, supraventricular tachycardia, Wolff. Parkinson-White – Long QT syndrome, Brugada syndrome • Structural – Aortic stenosis, mitral stenosis – Hypertrophic obstructive cardiomyopathy – Ischemia
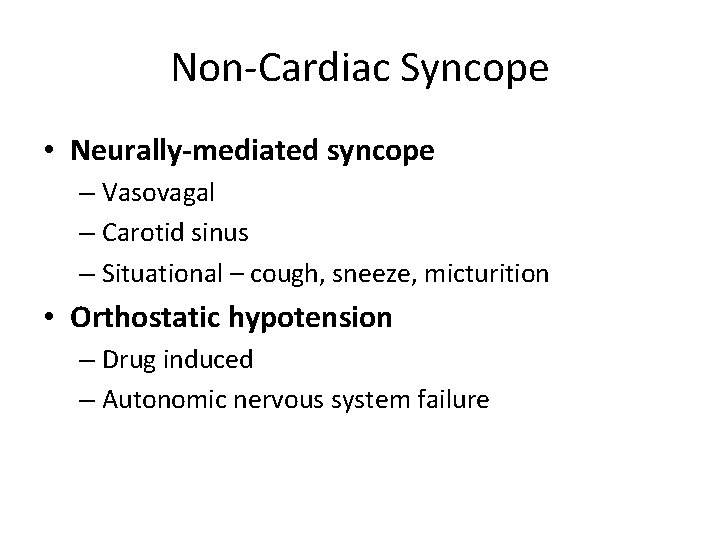
Non-Cardiac Syncope • Neurally-mediated syncope – Vasovagal – Carotid sinus – Situational – cough, sneeze, micturition • Orthostatic hypotension – Drug induced – Autonomic nervous system failure
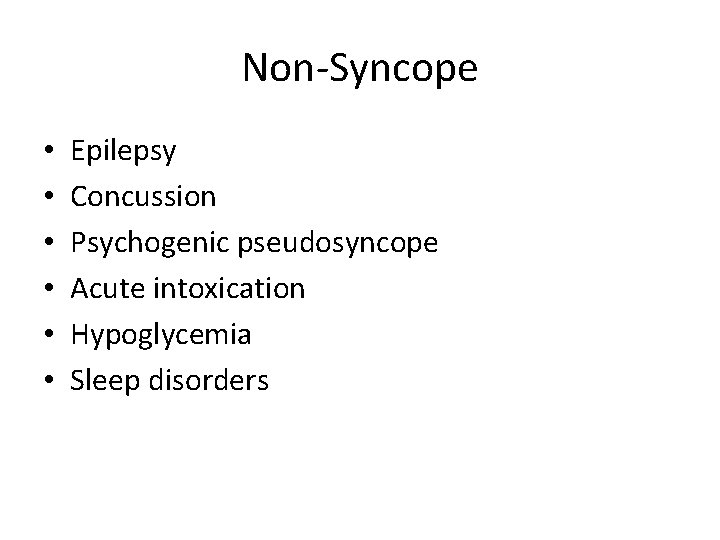
Non-Syncope • • • Epilepsy Concussion Psychogenic pseudosyncope Acute intoxication Hypoglycemia Sleep disorders
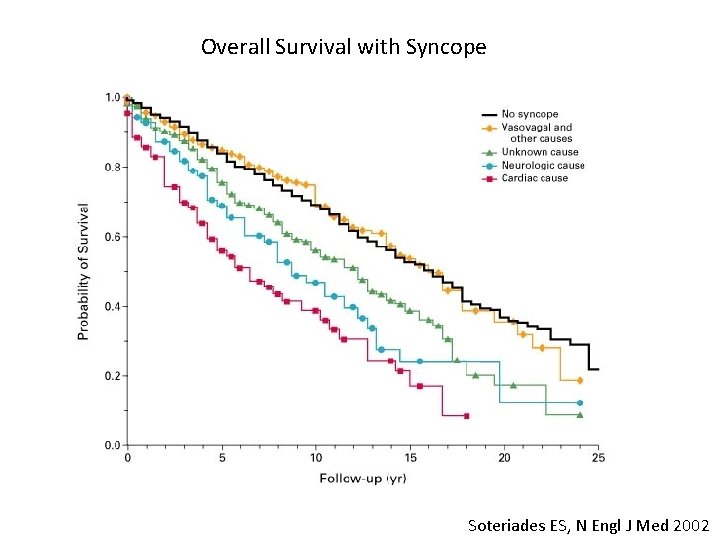
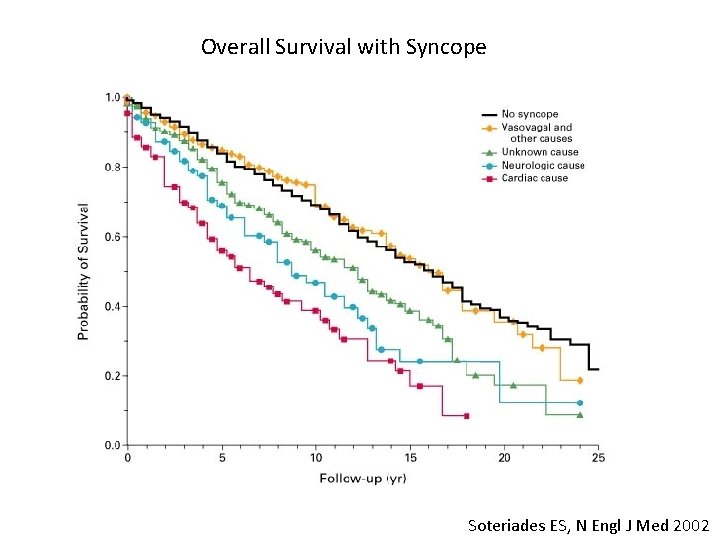
Overall Survival with Syncope Soteriades ES, N Engl J Med 2002
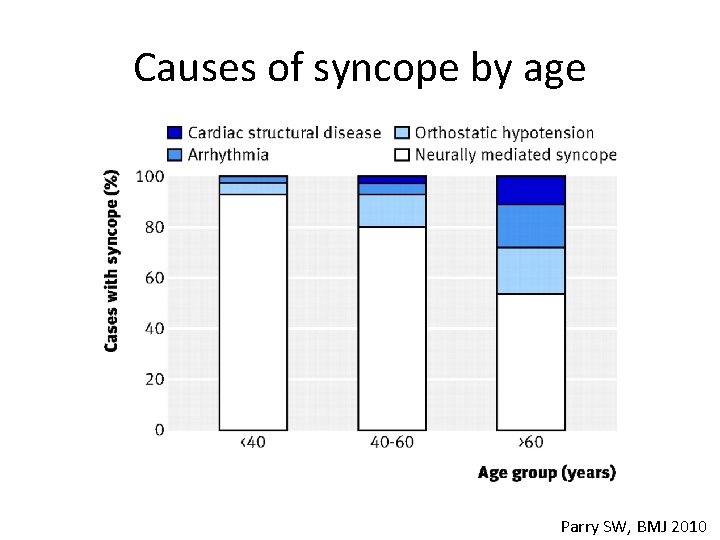
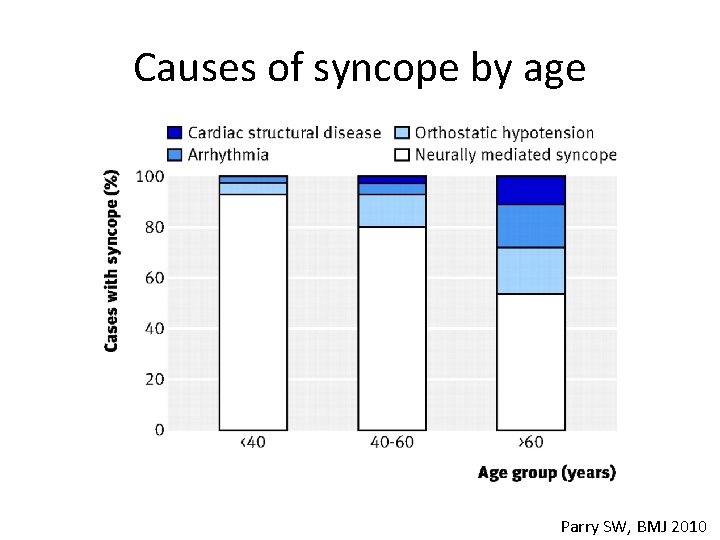
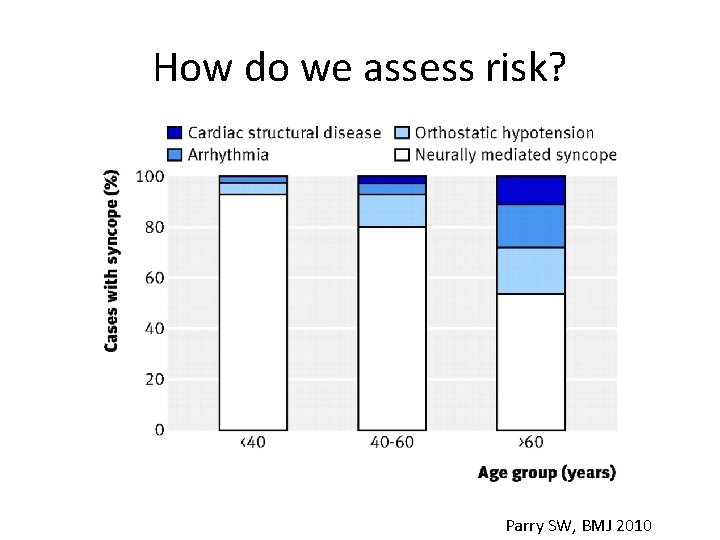
Causes of syncope by age Parry SW, BMJ 2010
Syncope • The current state in healthcare • Classification of syncope • Costs of a “typical” work up • Ways to provide “High Value Cost Conscious Care”
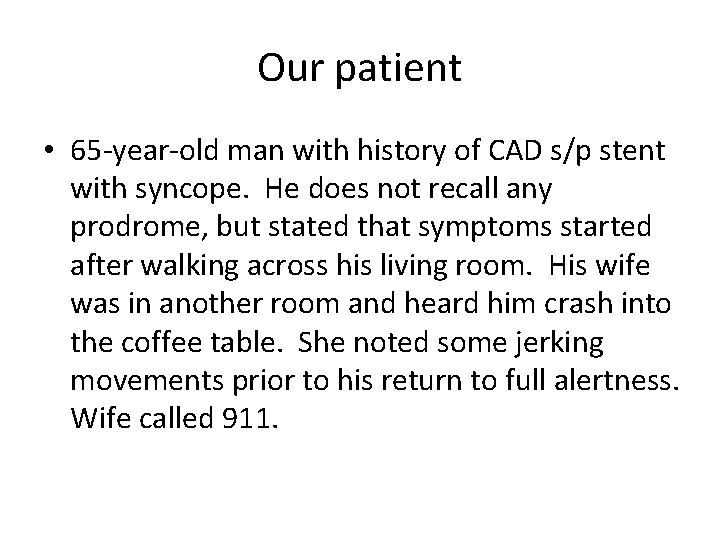
Our patient • 65 -year-old man with history of CAD s/p stent with syncope. He does not recall any prodrome, but stated that symptoms started after walking across his living room. His wife was in another room and heard him crash into the coffee table. She noted some jerking movements prior to his return to full alertness. Wife called 911.
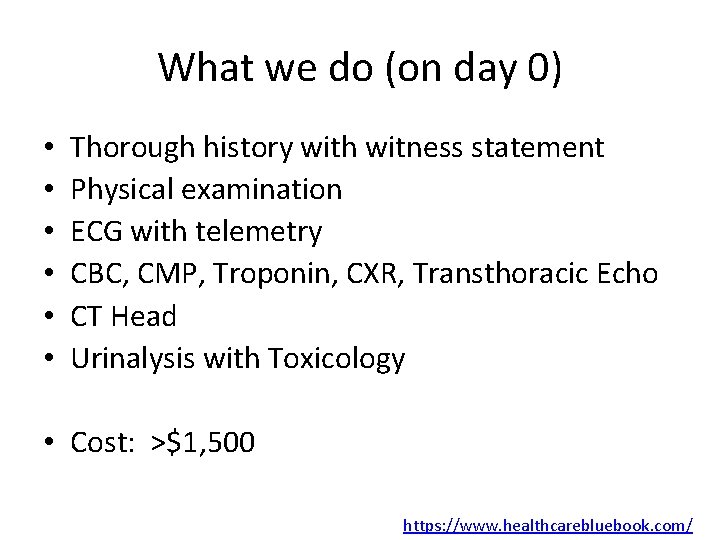
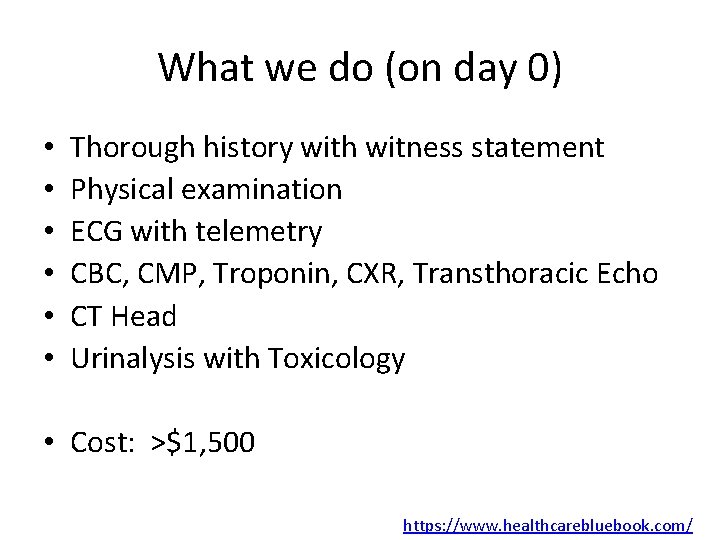
What we do (on day 0) • • • Thorough history with witness statement Physical examination ECG with telemetry CBC, CMP, Troponin, CXR, Transthoracic Echo CT Head Urinalysis with Toxicology • Cost: >$1, 500 https: //www. healthcarebluebook. com/
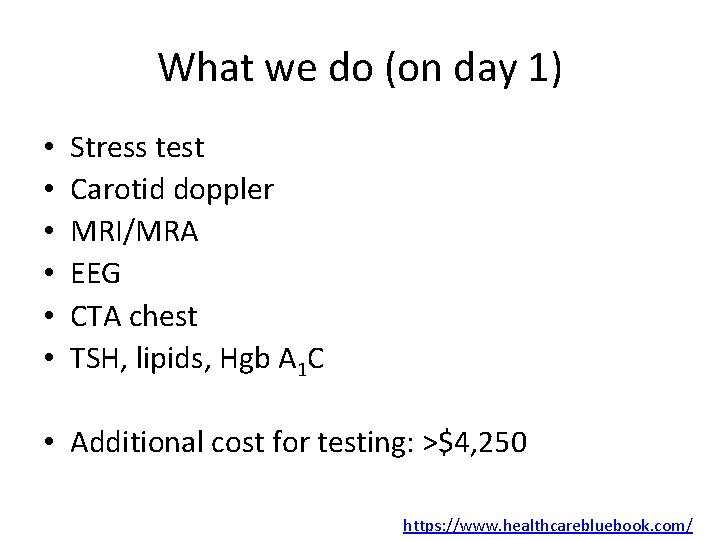
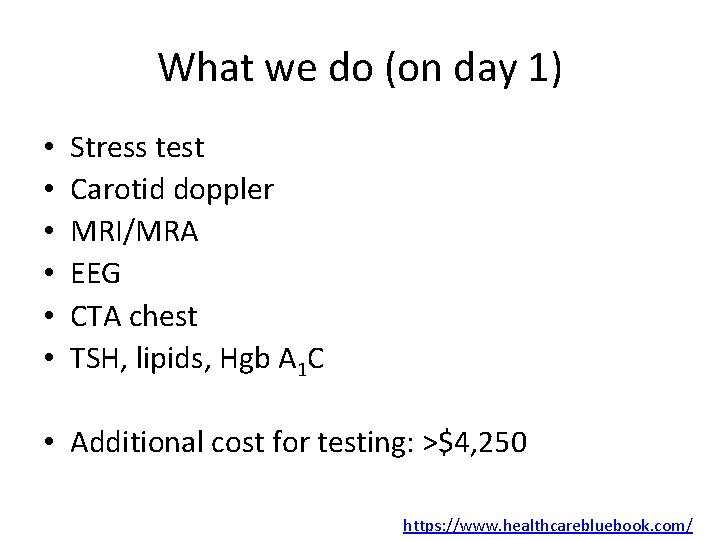
What we do (on day 1) • • • Stress test Carotid doppler MRI/MRA EEG CTA chest TSH, lipids, Hgb A 1 C • Additional cost for testing: >$4, 250 https: //www. healthcarebluebook. com/
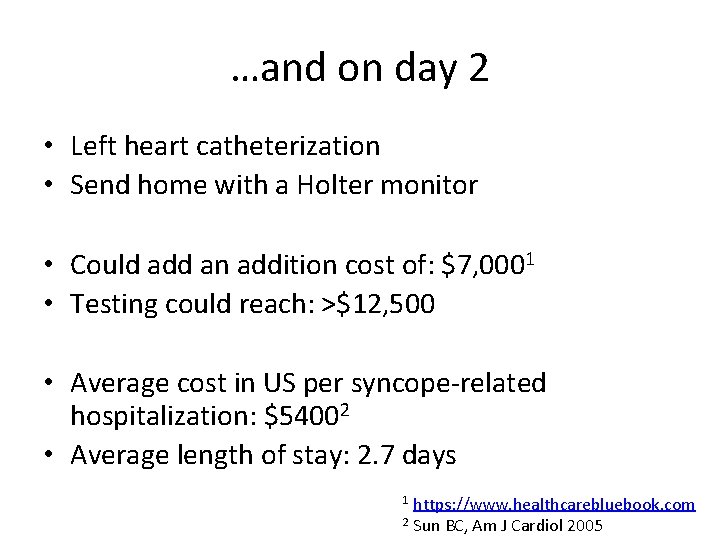
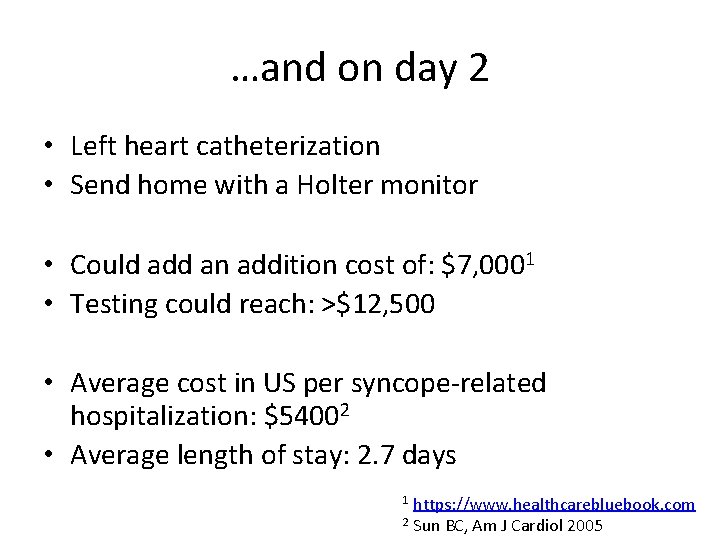
…and on day 2 • Left heart catheterization • Send home with a Holter monitor • Could add an addition cost of: $7, 0001 • Testing could reach: >$12, 500 • Average cost in US per syncope-related hospitalization: $54002 • Average length of stay: 2. 7 days https: //www. healthcarebluebook. com 2 Sun BC, Am J Cardiol 2005 1
Syncope • The current state in healthcare • Classification of syncope • Costs of a “typical” work up • Ways to provide “High Value, Cost Conscious Care”
How can we do this better? • Syncope. Cost-effective patient workup. – Radack KL, Postgrad Med 1986. • A cost effective approach to the investigation of syncope: relative merit of different diagnostic strategies – Simpson CS, Can J Cardiol 1999.
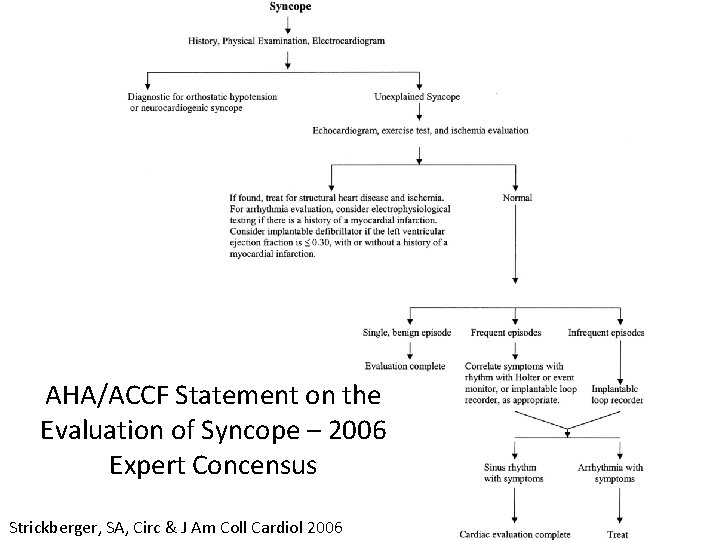
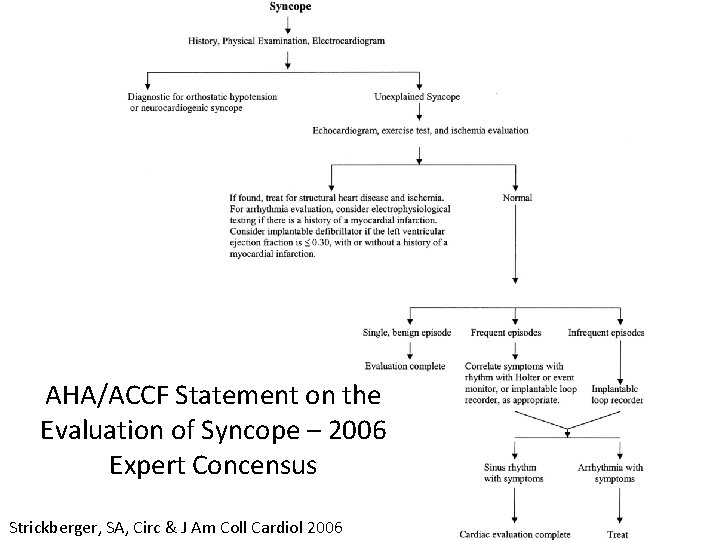
AHA/ACCF Statement on the Evaluation of Syncope – 2006 Expert Concensus Strickberger, SA, Circ & J Am Coll Cardiol 2006
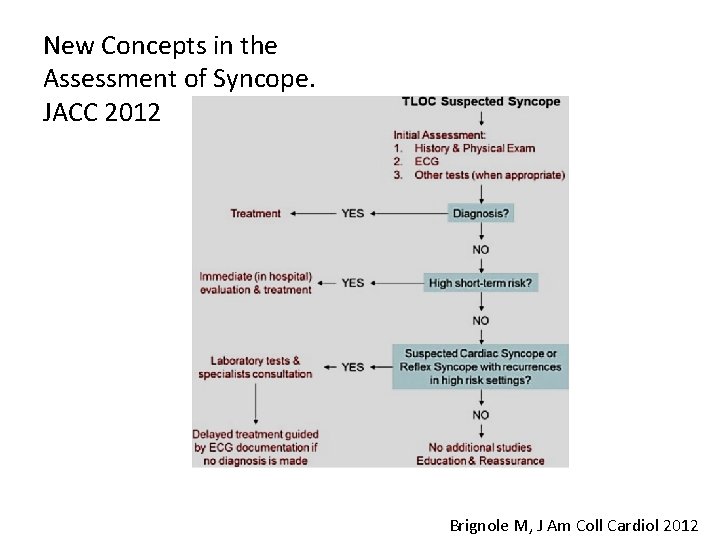
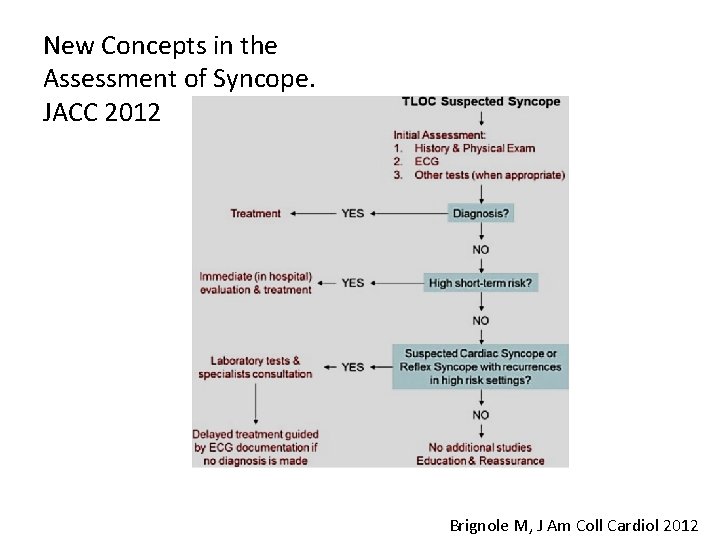
New Concepts in the Assessment of Syncope. JACC 2012 Brignole M, J Am Coll Cardiol 2012
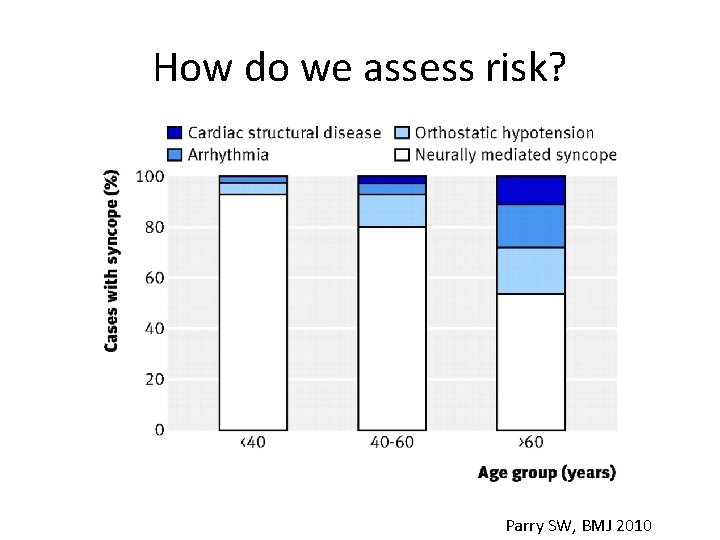
How do we assess risk? Parry SW, BMJ 2010
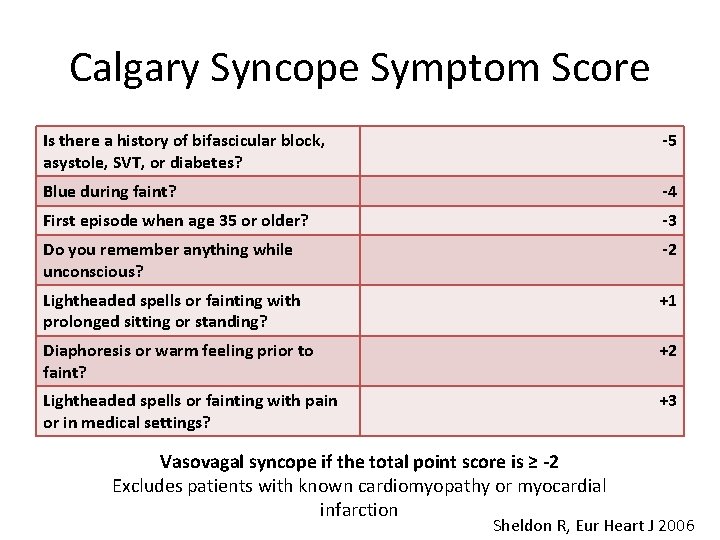
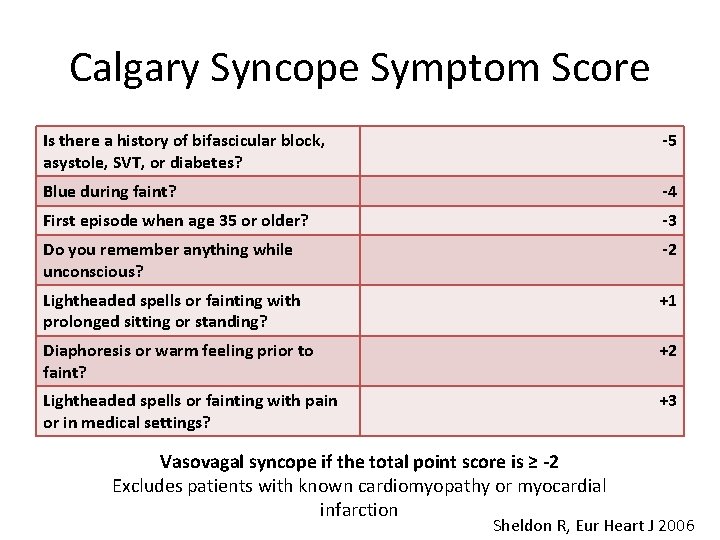
Calgary Syncope Symptom Score Is there a history of bifascicular block, asystole, SVT, or diabetes? -5 Blue during faint? -4 First episode when age 35 or older? -3 Do you remember anything while unconscious? -2 Lightheaded spells or fainting with prolonged sitting or standing? +1 Diaphoresis or warm feeling prior to faint? +2 Lightheaded spells or fainting with pain or in medical settings? +3 Vasovagal syncope if the total point score is ≥ -2 Excludes patients with known cardiomyopathy or myocardial infarction Sheldon R, Eur Heart J 2006
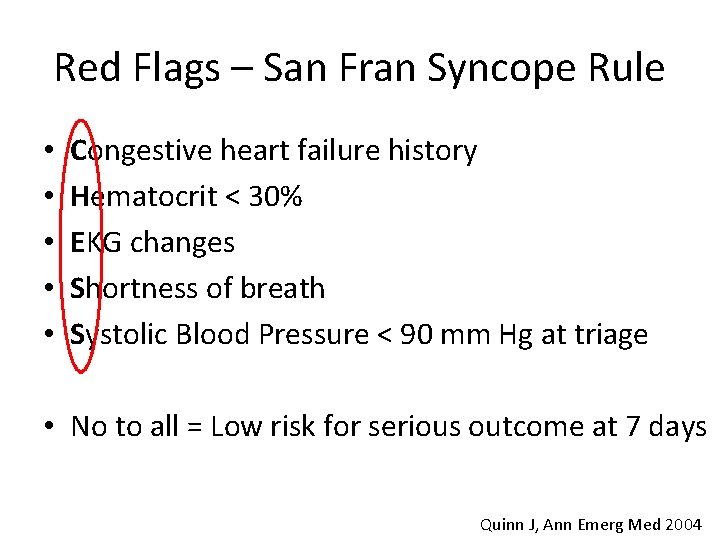
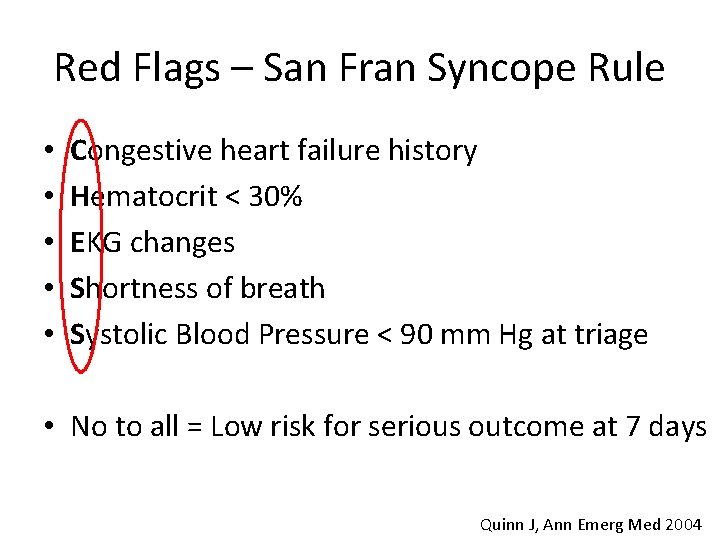
Red Flags – San Fran Syncope Rule • • • Congestive heart failure history Hematocrit < 30% EKG changes Shortness of breath Systolic Blood Pressure < 90 mm Hg at triage • No to all = Low risk for serious outcome at 7 days Quinn J, Ann Emerg Med 2004
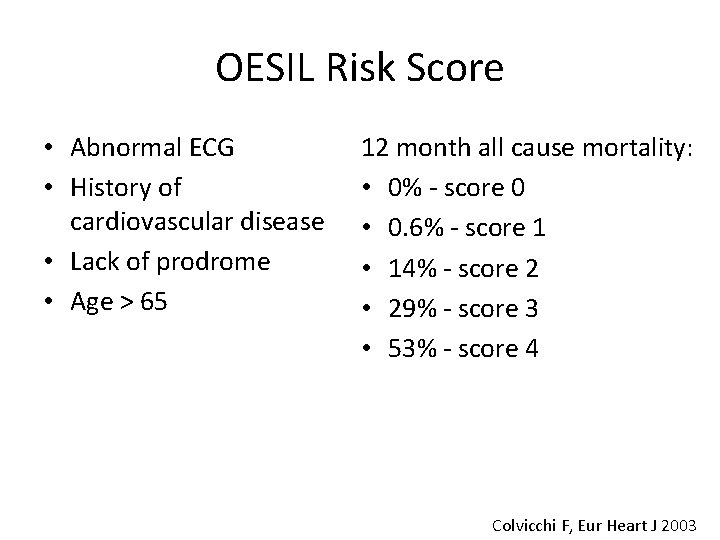
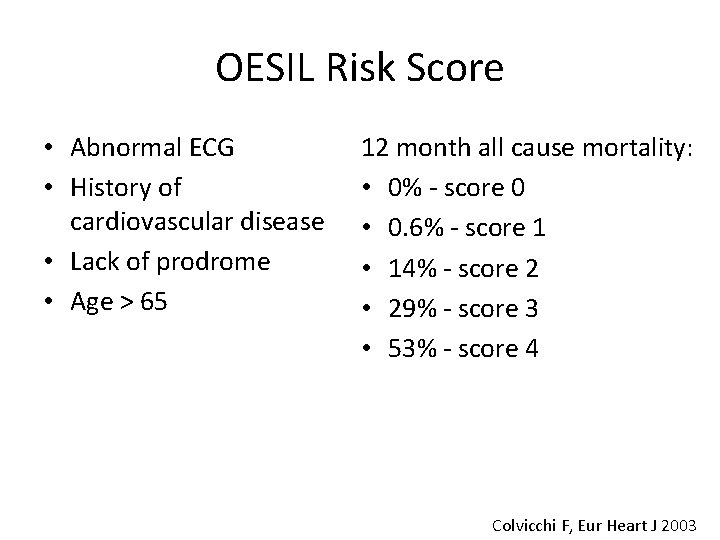
OESIL Risk Score • Abnormal ECG • History of cardiovascular disease • Lack of prodrome • Age > 65 12 month all cause mortality: • 0% - score 0 • 0. 6% - score 1 • 14% - score 2 • 29% - score 3 • 53% - score 4 Colvicchi F, Eur Heart J 2003
Recap of Risk Factors • • • Age Known cardiac disease Abnormal ECG Lack of prodrome Associated chest pain or shortness of breath
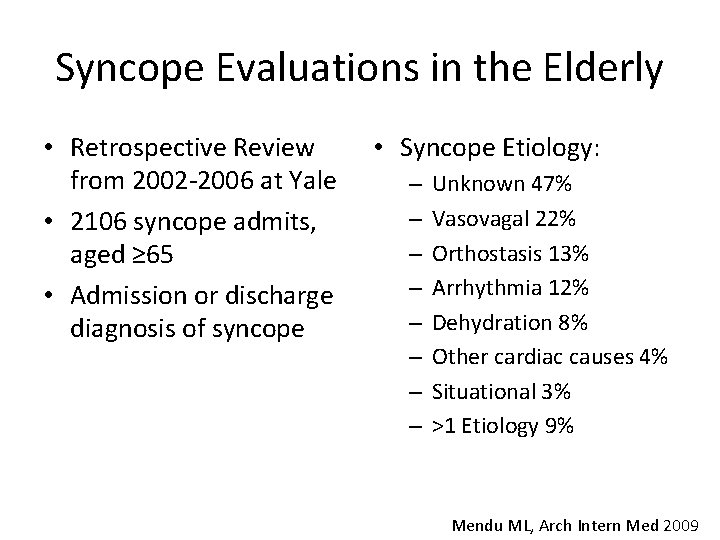
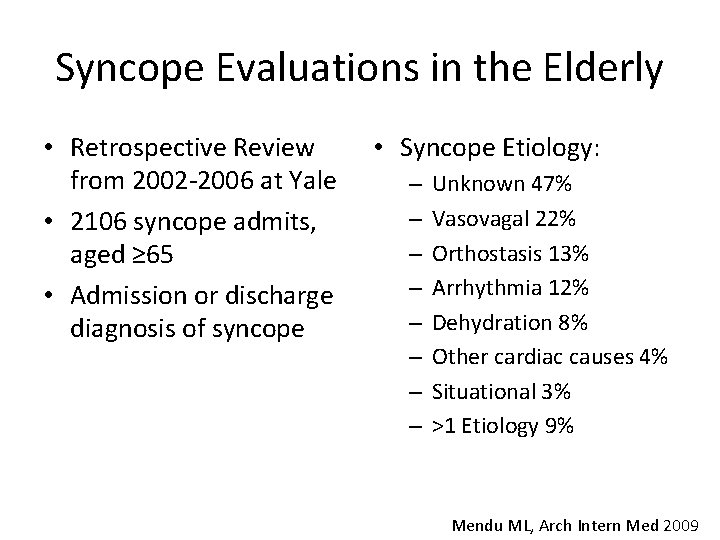
Syncope Evaluations in the Elderly • Retrospective Review from 2002 -2006 at Yale • 2106 syncope admits, aged ≥ 65 • Admission or discharge diagnosis of syncope • Syncope Etiology: – – – – Unknown 47% Vasovagal 22% Orthostasis 13% Arrhythmia 12% Dehydration 8% Other cardiac causes 4% Situational 3% >1 Etiology 9% Mendu ML, Arch Intern Med 2009
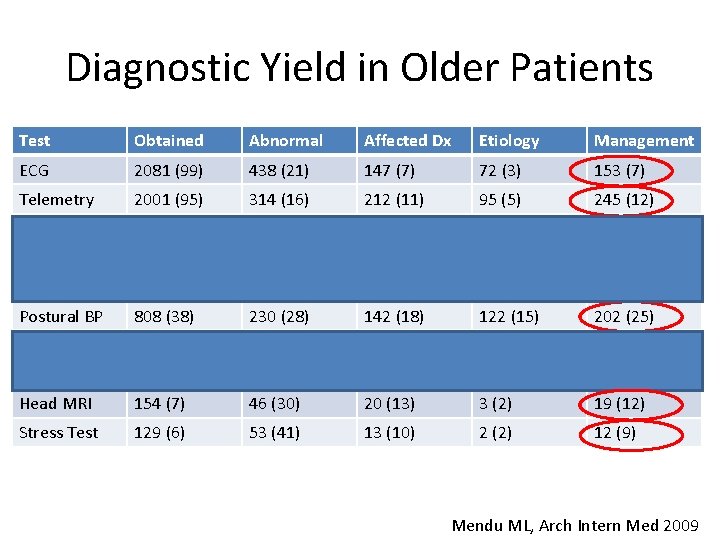
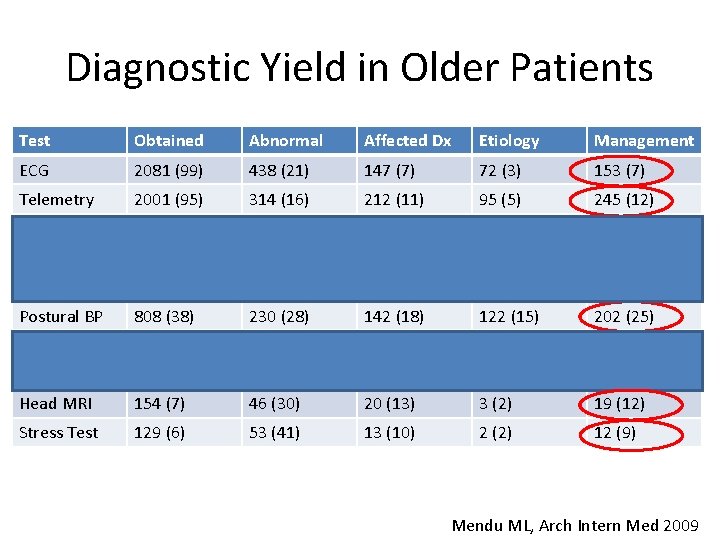
Diagnostic Yield in Older Patients Test Obtained Abnormal Affected Dx Etiology Management ECG 2081 (99) 438 (21) 147 (7) 72 (3) 153 (7) Telemetry 2001 (95) 314 (16) 212 (11) 95 (5) 245 (12) Enzymes 1991 (95) 108 (5) 31 (2) 9 (0. 5) 29 (1) Head CT 1327 (63) 138 (10) 28 (2) 7 (0. 5) 28 (2) TTE 821 (39) 516 (63) 35 (4) 13 (2) 36 (4) Postural BP 808 (38) 230 (28) 142 (18) 122 (15) 202 (25) Carotid US 267 (13) 122 (46) 2 (1) 2 (0. 8) 6 (2) EEG 174 (8) 68 (39) 2 (1) 1 (0. 6) 2 (1) Head MRI 154 (7) 46 (30) 20 (13) 3 (2) 19 (12) Stress Test 129 (6) 53 (41) 13 (10) 2 (2) 12 (9) Mendu ML, Arch Intern Med 2009
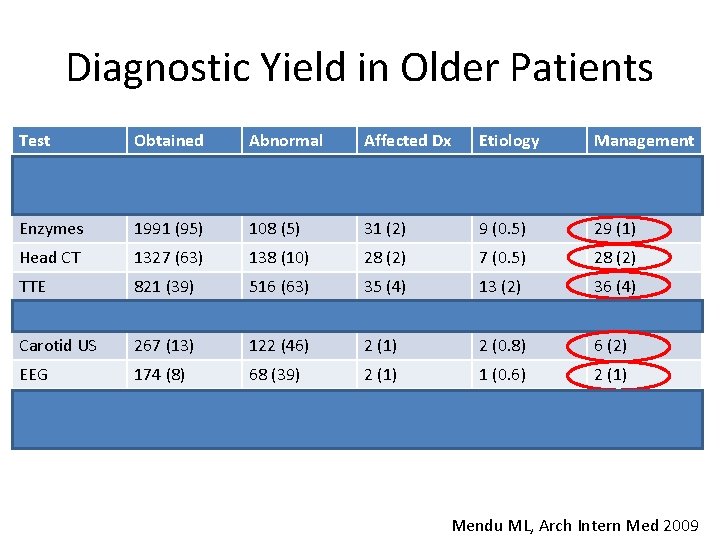
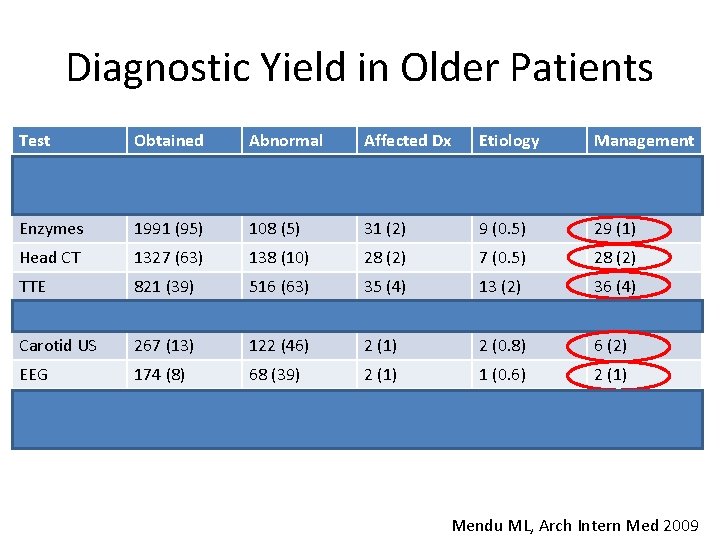
Diagnostic Yield in Older Patients Test Obtained Abnormal Affected Dx Etiology Management ECG 2081 (99) 438 (21) 147 (7) 72 (3) 153 (7) Telemetry 2001 (95) 314 (16) 212 (11) 95 (5) 245 (12) Enzymes 1991 (95) 108 (5) 31 (2) 9 (0. 5) 29 (1) Head CT 1327 (63) 138 (10) 28 (2) 7 (0. 5) 28 (2) TTE 821 (39) 516 (63) 35 (4) 13 (2) 36 (4) Postural BP 808 (38) 230 (28) 142 (18) 122 (15) 202 (25) Carotid US 267 (13) 122 (46) 2 (1) 2 (0. 8) 6 (2) EEG 174 (8) 68 (39) 2 (1) 1 (0. 6) 2 (1) Head MRI 154 (7) 46 (30) 20 (13) 3 (2) 19 (12) Stress Test 129 (6) 53 (41) 13 (10) 2 (2) 12 (9) Mendu ML, Arch Intern Med 2009
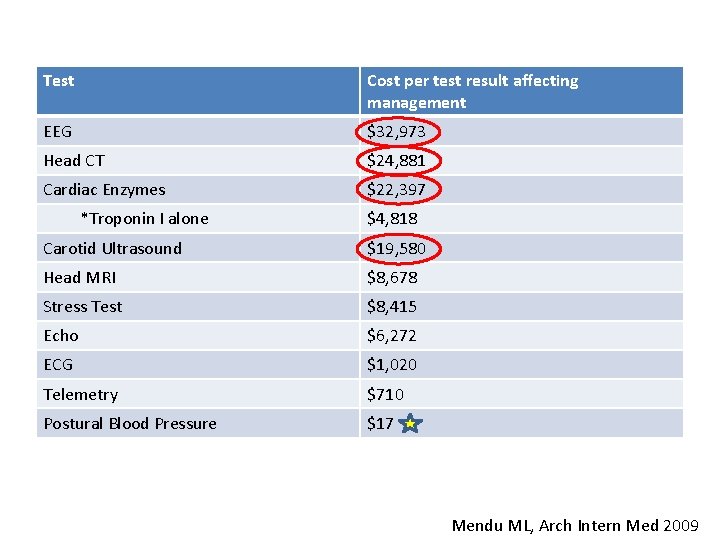
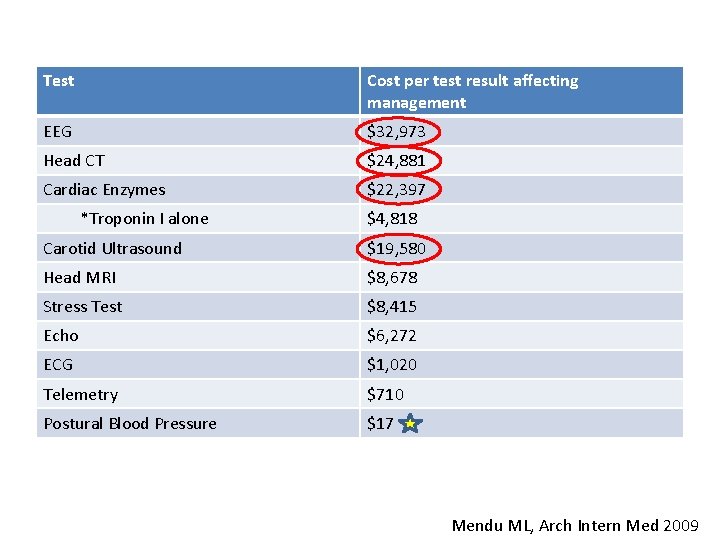
Test Cost per test result affecting management EEG $32, 973 Head CT $24, 881 Cardiac Enzymes $22, 397 *Troponin I alone $4, 818 Carotid Ultrasound $19, 580 Head MRI $8, 678 Stress Test $8, 415 Echo $6, 272 ECG $1, 020 Telemetry $710 Postural Blood Pressure $17 Mendu ML, Arch Intern Med 2009
What is NOT helpful? • • EEG Head CT Cardiac Enzymes Carotid US
EEG and Syncope • Myoclonic jerks associated with true syncope – Can be mistaken for seizure activity • Ictal asystole is a rare but severe complication of epileptic seizures • 828 patients admitted for presurgery video EEG monitoring between 2003 -2013. – 9 (1. 08%) had ictal asystole – Lasting 13 +/- 7 seconds – Mostly asymptomatic Nguyen-Michel VH, Epilepsia 2014
Head CT and Syncope • Of 293 ED syncope patients, 113 underwent CT head – 5% had abnormal head findings • 2 with subarachnoid hemorrhage • 2 with cerebral hemorrhage • 1 with stroke • Abnormal CTs associated with: – Focal neurological findings, headache, or trauma • Only half of patients undergoing CT had any neurological findings, headache, trauma above the clavicles, or coumadin use. Grossman SA, Intern Emerg Med 2007
Cardiac Enzymes and Syncope • Troponin unlikely to be beneficial unless other signs or symptoms point to MI. • Copeptin – surrogate marker for Vasopressin – Studied in Acute Myocardial Infarction – Small studies have found increased levels in patients with positive head up tilt test. 1 1 Lagi A, Int J Clin Pract 2013
Carotid US and Syncope • Choosing Wisely Recommendation #2: – Don’t perform imaging of the carotid arteries for simple syncope without other neurologic symptoms. Langer-Gould AM, Neuro 2013
What does work? • Thorough history with collateral information from witness • Physical examination • Postural blood pressure • ECG • Cost = $435 https: //www. healthcarebluebook. com/
Take a good history! • “ 5 Ps” – – – Precipitants Prodrome Palpitations Position Post-event phenomena Appearance Abnormal Movements Eyes open or closed Mental State Incontinence/Tongue Biting • Chronic medical issues • Family history of SCD • • • Parry SW, BMJ 2010
ECG and Telemetry • ECGs are relatively cheap and informative • Structural Heart Disease – Q-waves (infarct) – ST segment changes (ischemia) • Conduction System Disease – Bundle branch block – Atrioventricular (AV) block • Electrical Disease – Wolff-Parkinson-White (WPW) syndrome – Brugada syndrome – Long QT syndrome Marine JE, J Electrocardiol, 2013
Outpatient ECG Monitoring • Holter Monitor – daily syncopal episodes • Event Recorder – weekly syncopal episodes • Implantable Loop Recorder – monthly syncopal episodes
Postural Blood Pressure • • • Have the patient lie supine for 10 minutes Measure blood pressure and pulse Have the patient stand Inquire about symptoms Repeat blood pressure after 1 and 3 minutes • Classical Orthostatic Hypotension is defined by: – Drop in SBP >20 mm Hg or DBP >10 mm Hg within 3 minutes of standing
Carotid Sinus Syncope • Carotid Sinus Massage – 10 second sequential (right then left) with patient supine and erect • Hypersensitivity defined by: – Ventricular pause lasting >3 seconds – Fall in systolic BP >50 mm Hg • Carotid Sinus Syncope define by hypersensitivity in the presence of syncope
Post - H&P, ECG, and Postural BP • You should be able to answer: – Syncope or not? – Etiology determined based on the above? – High risk of cardiovascular events or death?
Echocardiogram and Syncope • Echo is helpful to confirm or refute suspicion of cardiac disease after the basics • Not indicated for syncope without suspicion of cardiac disease – Must have 2 nd diagnosis
Advanced Cardiac Testing • Stress testing and Left Heart Catheterization – If concern for ischemia • EP study – If concern for tachyarrhythmia • Tilt test – For diagnostic dilemma or if it will affect treatment
Tilt Table Testing • An effective technique for providing direct diagnostic evidence indicating susceptibility to vasovagal syncope • Utilizes a drug-free tilt lasting 45 minutes and pharmacologic provocation (Isoproterenol) • Monitor heart rate and blood pressure – Positive test with provocation of neurally-mediated hypotension or bradycardia (or both) Benditt DG, JACC, 1996
General Concepts • Perform a comprehensive history and physical examination using evidence based tools • Routinely obtain an ECG • Utilize EEG, Head CT, or MRI only with clinical suspicion of focal neurological deficit or seizure • Consider Holter, event recorder, or implantable loop recorders if an arrythmia is suspected, depending on frequency of events • Utilize cardiac imaging only with clinical suspicion of structural or valvular heart disease • Perform invasive EP study only with clinical suspicion of a tachyarrhythmia • Obtain a Tilt test only for diagnostic dilemma and if it will affect treatment and/or outcome
Do’s and Don’ts • Do every time: – H&P, ECG, Postural Blood Pressure • Try to avoid: – EEG, Cardiac Enzymes, Head CT, Carotid US • Other testing as indicated based on findings – Try to avoid the shot gun approach
• • • • • Bibliography Moya A, Sutton R, Ammirati F, Blanc JJ, Brignole M, Dahm JB, et al. Guidelines for the diagnosis and management of syncope (version 2009): the task force for the diagnosis and management of syncope of the European Society of Cardiology (ESC). Eur Heart J 2009; 30: 2631 -71. Soteriades ES, Evans JC, Larson MG, Chen MH, Chen L, Benjamin EJ, et al. Incidence and prognosis of syncope. N Eng J Med 2002; 347: 878 -85. Sun BC, Emond JA, Camargo CA Jr. Direct medical costs of syncope-related hospitalizations in the United States. Am J Cardiol 2005; 95: 668 -71. Linzer M, Pontinen M, Gold DT, Divine GW, Felder A, Brooks WB. Impairment of physical and psychosocial function in recurrent syncope. J Clin Epidemiol 1991; 44: 1037 -43. Rosanio S, Schwarz ER, Ware DL, Vitarelli A. Syncope in adults: systematic review and proposal of a diagnostic and therapeutic algorithm. Int J Cardiol 2013; 162(3): 149 -57. Parry SW, Tan MP. An approach to the evaluation and management of syncope in adults. BMJ 2010; 340: c 880. https: //www. healthcarebluebook. com/ Radack KL. Syncope. Cost-effective patient workup. Postgrad Med 1986; 80(8): 169 -76. Simpson CS, Krahn AD, Klein GJ, Yee R, Skanes AC, Manda V, Norris C. A cost effective approach to the investigation of syncope: relative merit of different diagnostic strategies. Can J Cardiol 1999; 15(5): 579 -84. Strickberger, SA, Benson DW, Biaggioni I, Callans DJ, Cohen MI, Ellenbogen KA, et al. AHA/ACCF scientific statement on the evaluation of syncope: from the American Heart Association Councils on Clinical Cardiology, Cardiovascular Nursing, Cardiovascular Disease in the Young, and Stroke, and the Quality of Care and Outcomes Research Interdisciplinary Working Group; and the American College of Cardiology Foundation: in collaboration with the Heart Rhythm Society: endorsed by the American Autonomic Society. Circulation 2006; 113(2): 316 -27. Brignole M, Hamdan MH. New concepts in the assessment of syncope. J Am Coll Cardiol 2012; 59(18): 1583 -91. Sheldon R, Rose S, Connolly S, Ritchie D, Koshman ML, Frenneaux M. Diagnostic criteria for vasovagal syncope based on a quantitative history. Eur Heart J 2006; 27(3): 344 -50. Quinn JV, Stiell IG, Mc. Dermott DA, Sellers KL, Kohn MA, Wells GA. Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Ann Emerg Med 2004; 43(2): 224 -32. Colvicchi F, Ammirati F, Melina D, Guido V, Imperoli G, Santini M, et al. Development and prospective validation of a risk stratification system for patients with syncope in the emergency department: the OESIL risk score. Eur Heart J 2003; 24: 811 -9. Mendu ML, Mc. Avay G, Lampert R, Stoehr J, Tinetti ME. Yield of diagnostic tests in evaluating syncopal episodes in older patients. Arch Intern Med 2009; 164(14): 1299 -1305. Nguyen-Michel VH, Adam C, Dinkelacker V, Pichit P, Boudali Y, Baulac M, et al. Characterization of seizure-induced syncopes: EEG, ECG, and clinical features. Epilepsia 2014; 55(1): 146 -55. Grossman SA, Fischer C, Bar JL, Lipsitz LA, Mottley L, Sands K, et al. The yield of head CT in syncope: a pilot study. Intern Emerg Med 2007; 2(1): 46 -9. Lagi A, Cuomo A, Veneziani F, Cencetti S. Copeptin: a blood test marker of syncope. Int J Clin Pract 2013; 67(6): 512 -5. Langer-Gould AM, Anderson WE, Armstrong MJ, Cohen AB, Eccher MA, et al. The American Academy of Neurology’s top five choosing wisely recommendations. Neurology 2013; 81(11): 1004 -11. Marine JE. ECG features that suggest a potentially life-threatening arrhythmia as the cause for syncope. J Electrocardiol 2013; 46(6): 561 -8.