Syncope A Diagnostic and Treatment Strategy David G



- Slides: 105
Syncope A Diagnostic and Treatment Strategy David G. Benditt, M. D. Richard Sutton, DSc. Med University of Minnesota Medical School Minneapolis, MN USA Royal Brompton Hospital London, UK
Transient Loss of Consciousness (TLOC)
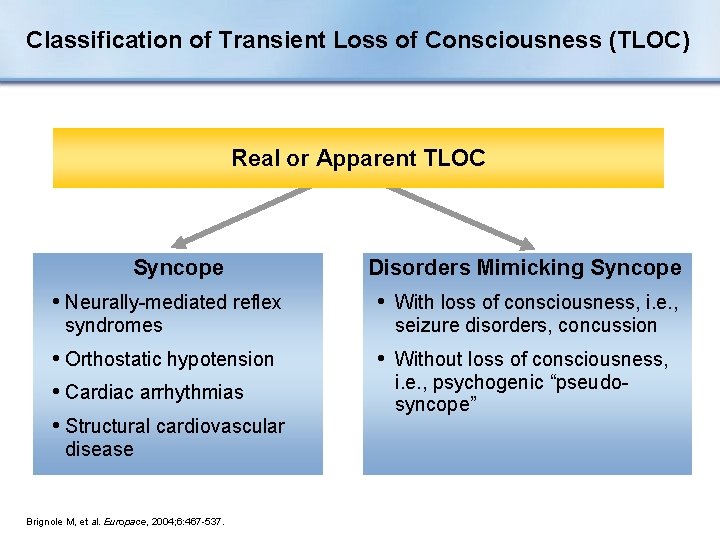
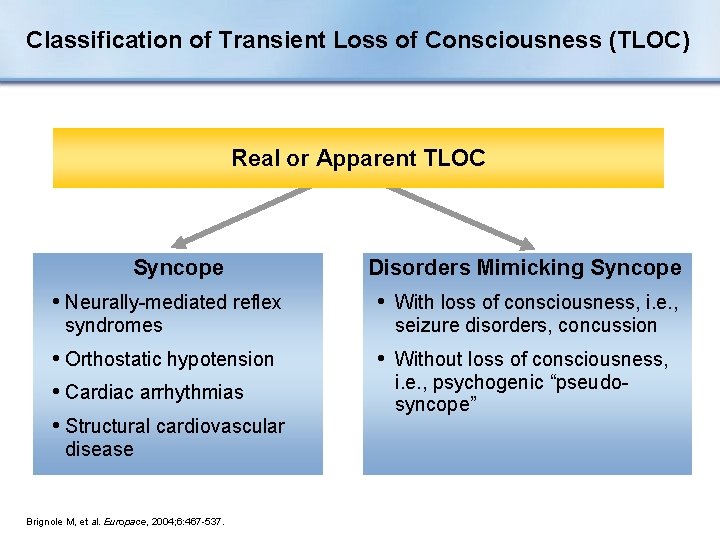
Classification of Transient Loss of Consciousness (TLOC) Real or Apparent TLOC Syncope Disorders Mimicking Syncope • Neurally-mediated reflex • With loss of consciousness, i. e. , • Orthostatic hypotension • Cardiac arrhythmias • Structural cardiovascular • Without loss of consciousness, syndromes disease Brignole M, et al. Europace, 2004; 6: 467 -537. seizure disorders, concussion i. e. , psychogenic “pseudosyncope”
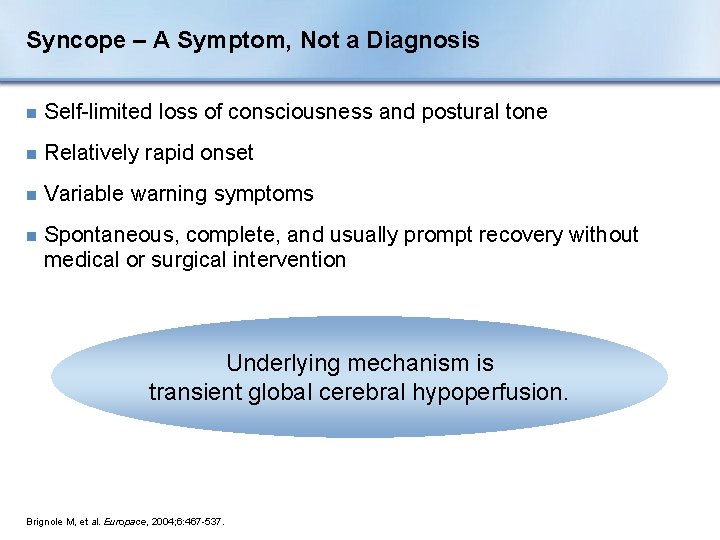
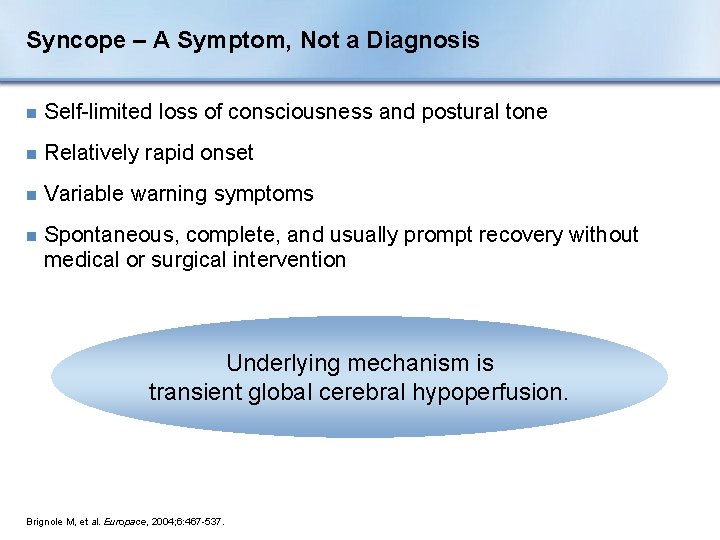
Syncope – A Symptom, Not a Diagnosis n Self-limited loss of consciousness and postural tone n Relatively rapid onset n Variable warning symptoms n Spontaneous, complete, and usually prompt recovery without medical or surgical intervention Underlying mechanism is transient global cerebral hypoperfusion. Brignole M, et al. Europace, 2004; 6: 467 -537.
Presentation Overview I. Etiology, Prevalence, Impact II. Diagnosis III. Specific Conditions and Treatment IV. Special Issues
Section I: Etiology, Prevalence, Impact
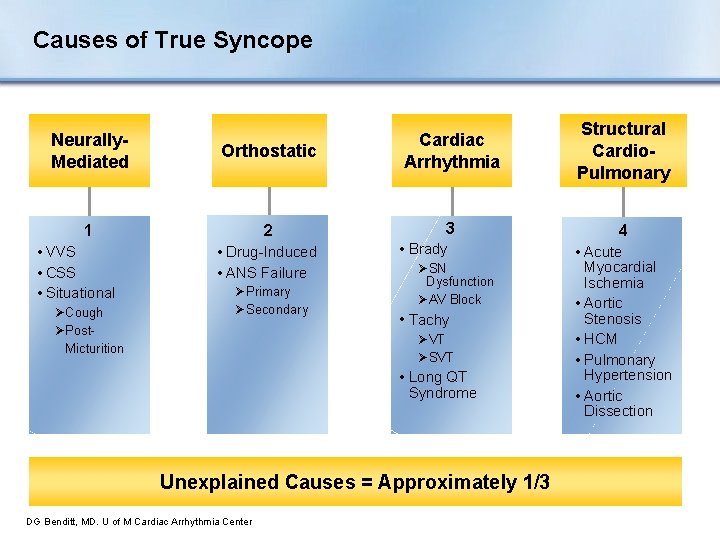
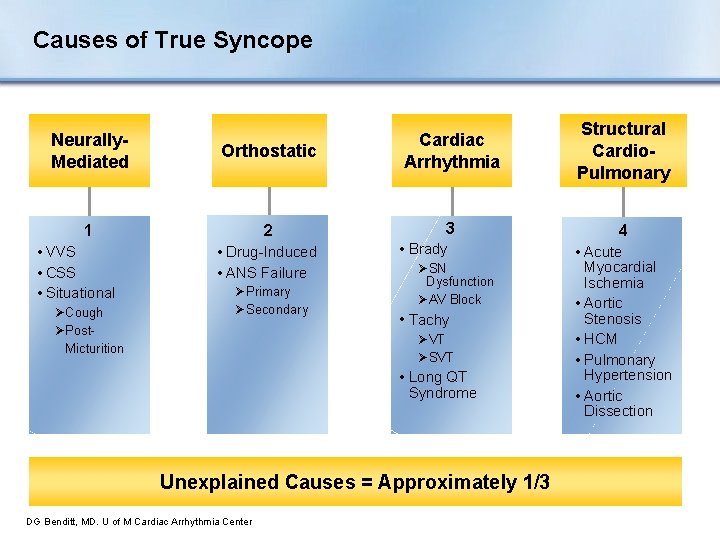
Causes of True Syncope Neurally. Mediated 1 • VVS • CSS • Situational ØCough ØPost. Micturition Orthostatic Cardiac Arrhythmia Structural Cardio. Pulmonary 2 3 4 • Drug-Induced • ANS Failure ØPrimary ØSecondary • Brady ØSN Dysfunction ØAV Block • Tachy ØVT ØSVT • Long QT Syndrome Unexplained Causes = Approximately 1/3 DG Benditt, MD. U of M Cardiac Arrhythmia Center • Acute Myocardial Ischemia • Aortic Stenosis • HCM • Pulmonary Hypertension • Aortic Dissection

Syncope Mimics n Acute intoxication (e. g. , alcohol) n Seizures n Sleep disorders n Somatization disorder (psychogenic pseudo-syncope) n Trauma/concussion n Hypoglycemia n Hyperventilation Brignole M, et al. Europace, 2004; 6: 467 -537.
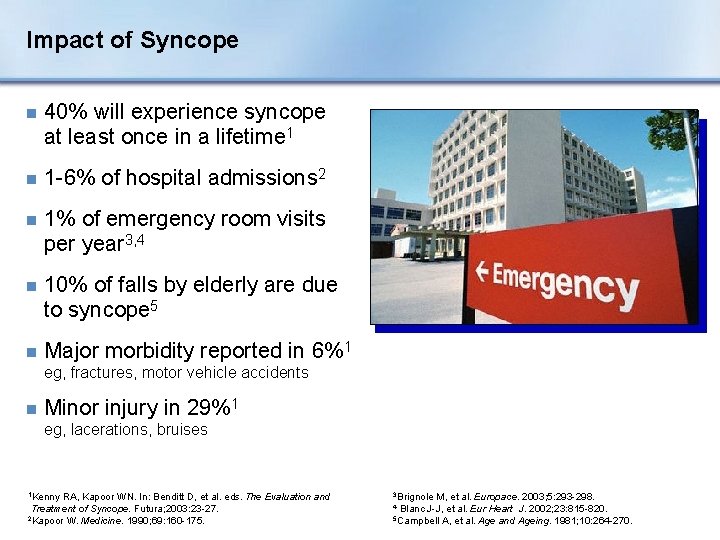
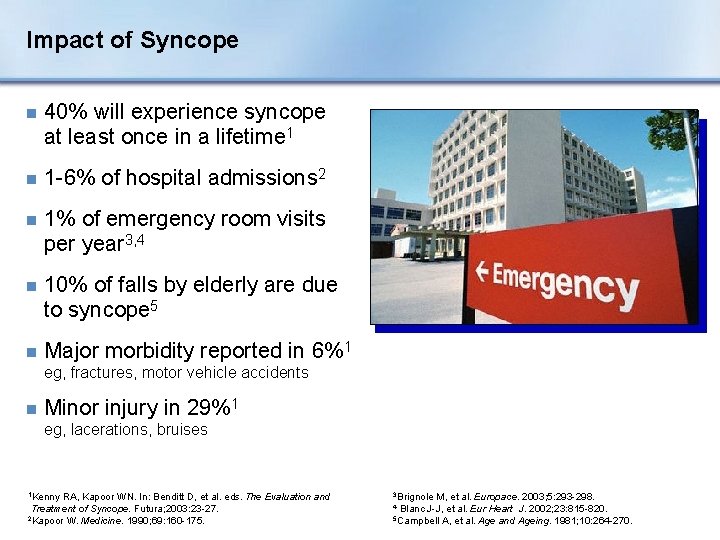
Impact of Syncope n 40% will experience syncope at least once in a lifetime 1 n 1 -6% of hospital admissions 2 n 1% of emergency room visits per year 3, 4 n 10% of falls by elderly are due to syncope 5 n Major morbidity reported in 6%1 eg, fractures, motor vehicle accidents n Minor injury in 29%1 eg, lacerations, bruises 1 Kenny RA, Kapoor WN. In: Benditt D, et al. eds. The Evaluation and Treatment of Syncope. Futura; 2003: 23 -27. 2 Kapoor W. Medicine. 1990; 69: 160 -175. 3 Brignole M, et al. Europace. 2003; 5: 293 -298. Blanc J-J, et al. Eur Heart J. 2002; 23: 815 -820. 5 Campbell A, et al. Age and Ageing. 1981; 10: 264 -270. 4
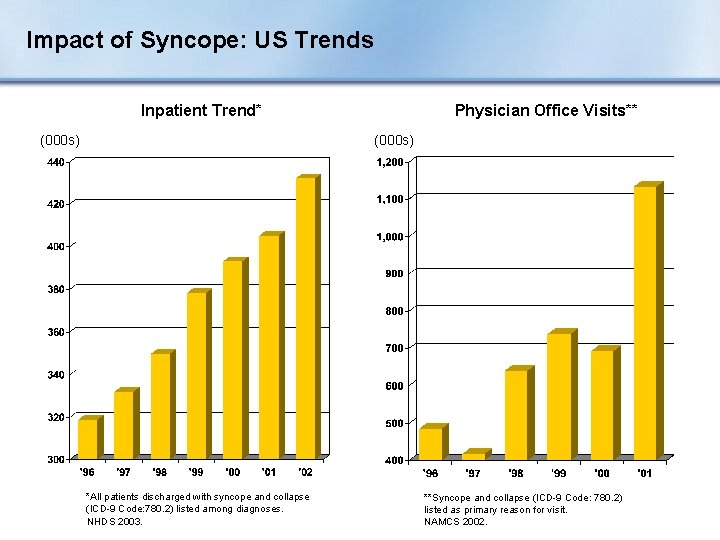
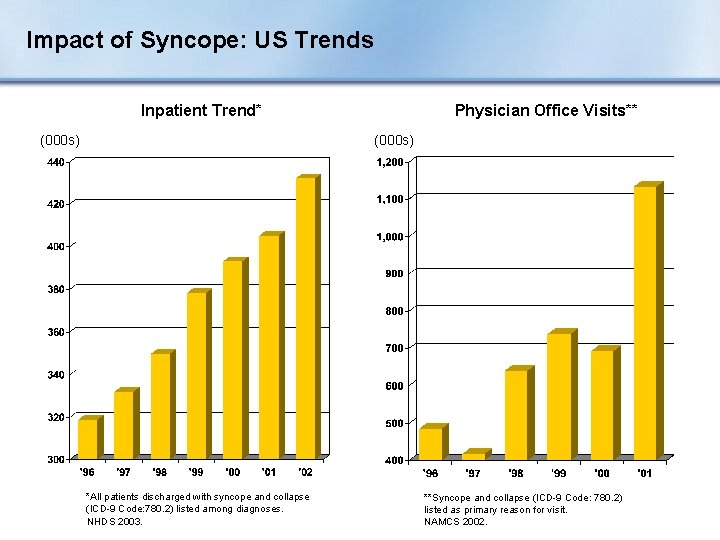
Impact of Syncope: US Trends Inpatient Trend* (000 s) Physician Office Visits** (000 s) *All patients discharged with syncope and collapse (ICD-9 Code: 780. 2) listed among diagnoses. NHDS 2003. **Syncope and collapse (ICD-9 Code: 780. 2) listed as primary reason for visit. NAMCS 2002.
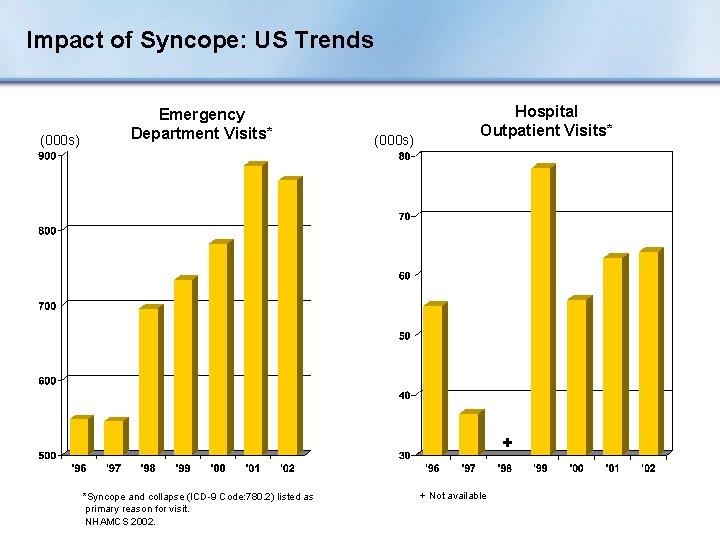
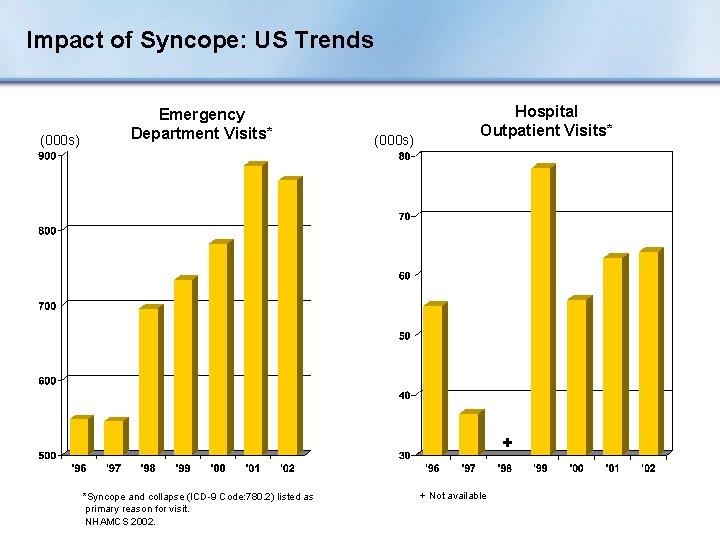
Impact of Syncope: US Trends (000 s) Emergency Department Visits* (000 s) Hospital Outpatient Visits* + *Syncope and collapse (ICD-9 Code: 780. 2) listed as primary reason for visit. NHAMCS 2002. + Not available
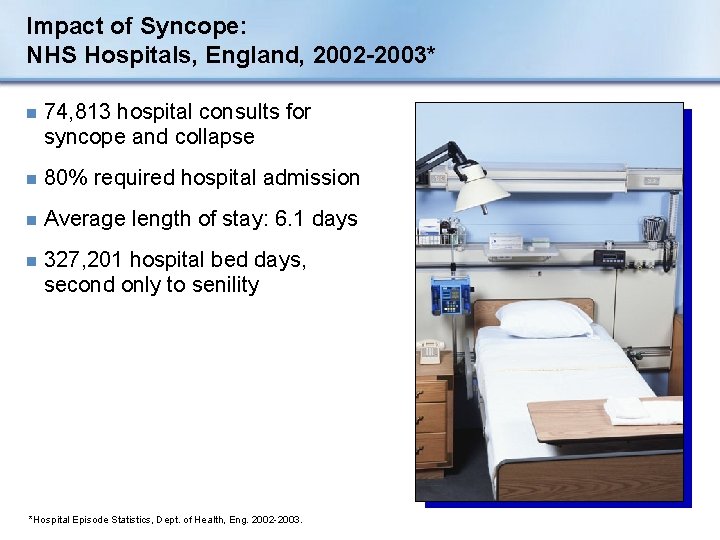
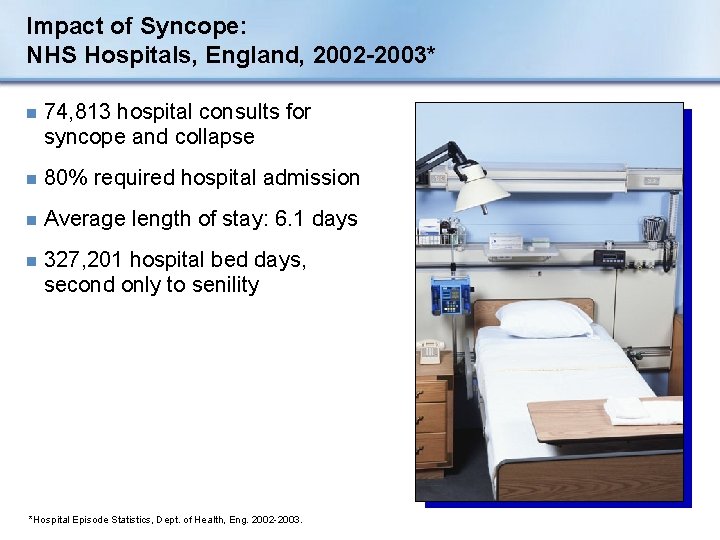
Impact of Syncope: NHS Hospitals, England, 2002 -2003* n 74, 813 hospital consults for syncope and collapse n 80% required hospital admission n Average length of stay: 6. 1 days n 327, 201 hospital bed days, second only to senility *Hospital Episode Statistics, Dept. of Health, Eng. 2002 -2003.
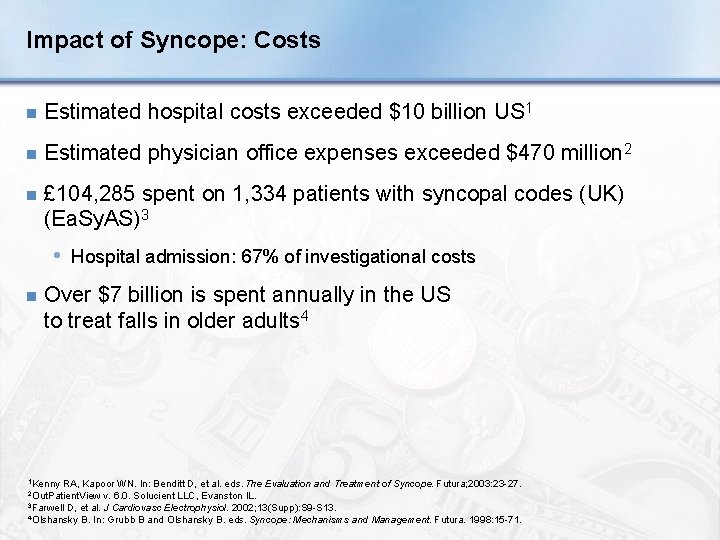
Impact of Syncope: Costs n Estimated hospital costs exceeded $10 billion US 1 n Estimated physician office expenses exceeded $470 million 2 n £ 104, 285 spent on 1, 334 patients with syncopal codes (UK) (Ea. Sy. AS)3 • Hospital admission: 67% of investigational costs n Over $7 billion is spent annually in the US to treat falls in older adults 4 1 Kenny RA, Kapoor WN. In: Benditt D, et al. eds. The Evaluation and Treatment of Syncope. Futura; 2003: 23 -27. v. 6. 0. Solucient LLC, Evanston IL. 3 Farwell D, et al. J Cardiovasc Electrophysiol. 2002; 13(Supp): S 9 -S 13. 4 Olshansky B. In: Grubb B and Olshansky B. eds. Syncope: Mechanisms and Management. Futura. 1998: 15 -71. 2 Out. Patient. View

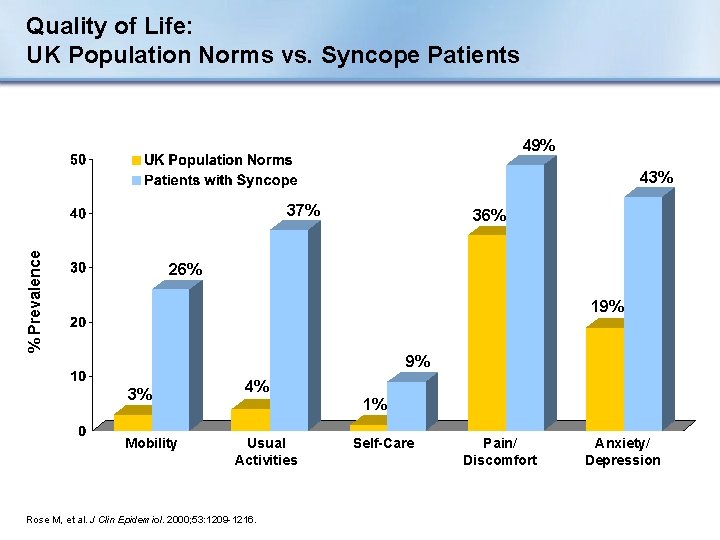
Impact of Syncope: Quality of Life Percent of Patients 73%1 60%2 37%2 Anxiety/ Depression 1 Linzer 2 Linzer 71%2 M. J Clin Epidemiol. 1991; 44: 1037. M. J Gen Int Med. 1994; 9: 181. Alter Daily Activities Restricted Driving Change Employment
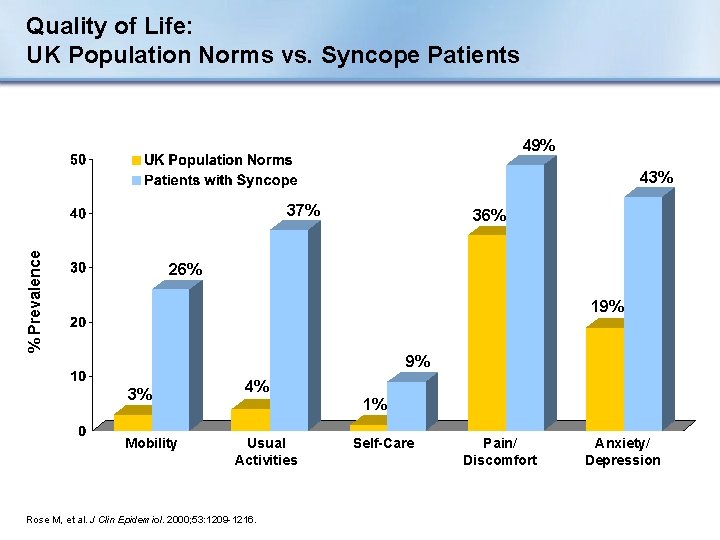
Quality of Life: UK Population Norms vs. Syncope Patients 49% 43% % Prevalence 37% 36% 26% 19% 9% 3% Mobility 4% Usual Activities Rose M, et al. J Clin Epidemiol. 2000; 53: 1209 -1216. 1% Self-Care Pain/ Discomfort Anxiety/ Depression
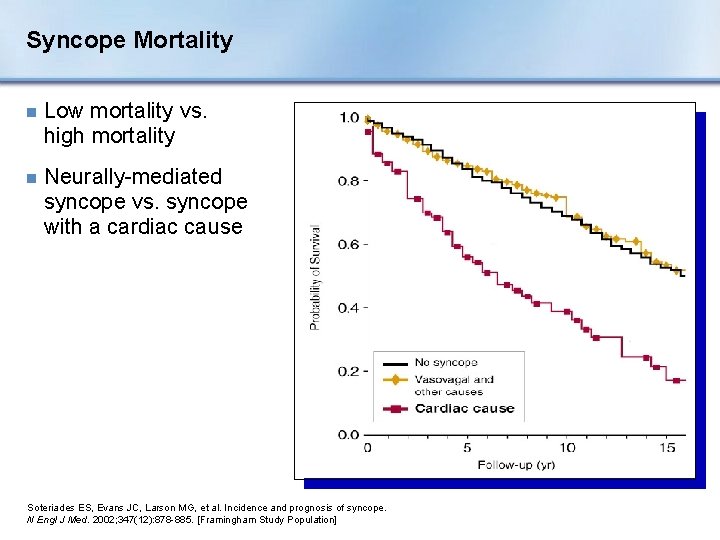
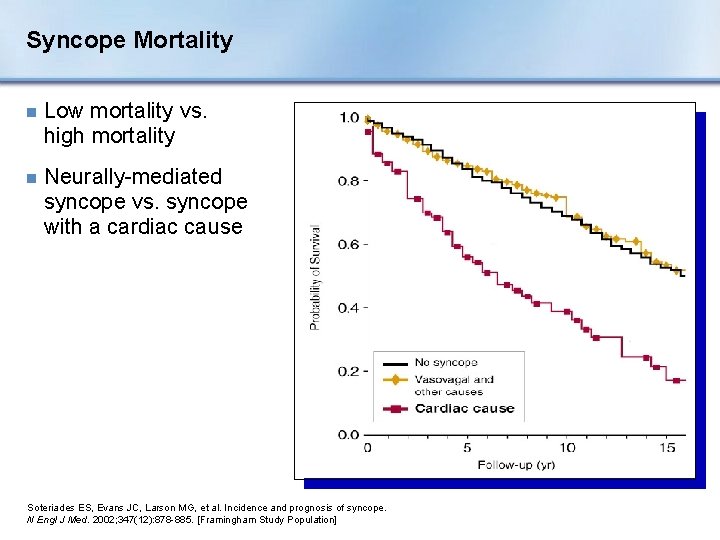
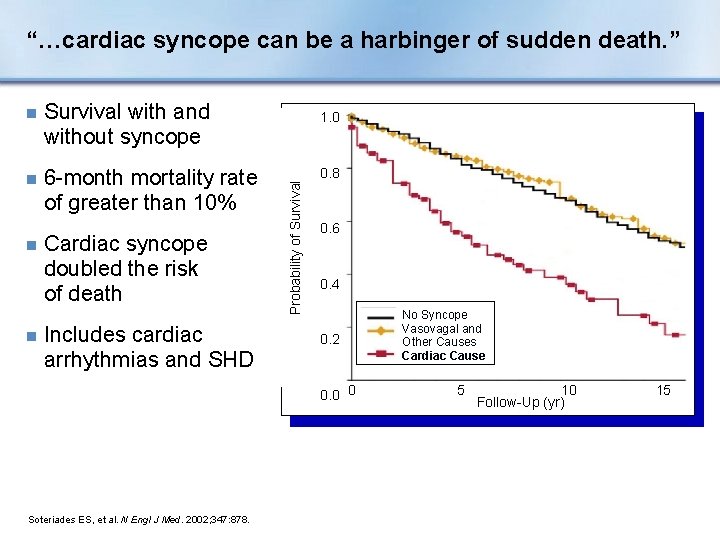
Syncope Mortality n Low mortality vs. high mortality n Neurally-mediated syncope vs. syncope with a cardiac cause Soteriades ES, Evans JC, Larson MG, et al. Incidence and prognosis of syncope. N Engl J Med. 2002; 347(12): 878 -885. [Framingham Study Population]
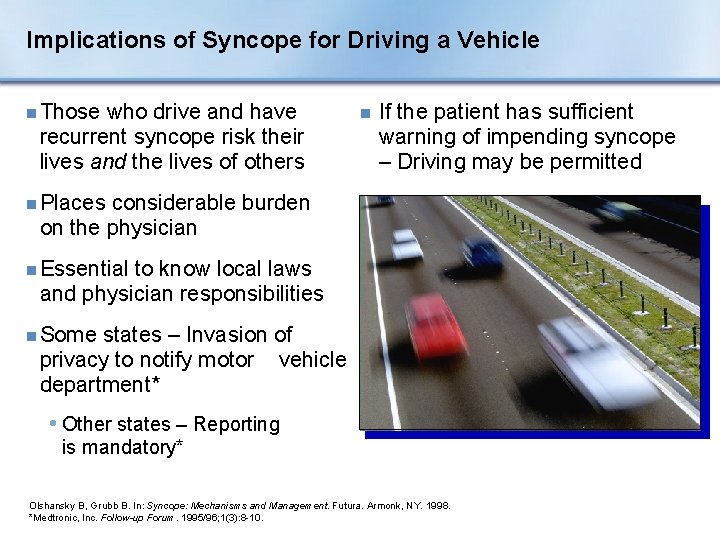
Implications of Syncope for Driving a Vehicle n Those who drive and have recurrent syncope risk their lives and the lives of others n If the patient has sufficient warning of impending syncope – Driving may be permitted n Places considerable burden on the physician n Essential to know local laws and physician responsibilities n Some states – Invasion of privacy to notify motor vehicle department* • Other states – Reporting is mandatory* Olshansky B, Grubb B. In: Syncope: Mechanisms and Management. Futura. Armonk, NY. 1998. *Medtronic, Inc. Follow-up Forum. 1995/96; 1(3): 8 -10.
Challenges of Syncope n Diagnosis • Complex n Quality of life implications • Work • Mobility (automobiles) • Psychological n Cost • Cost/year • Cost/diagnosis
Section II: Diagnosis
Diagnostic Objectives n Distinguish true syncope from syncope mimics n Determine presence of heart disease n Establish the cause of syncope with sufficient certainty to: • Assess prognosis confidently • Initiate effective preventive treatment
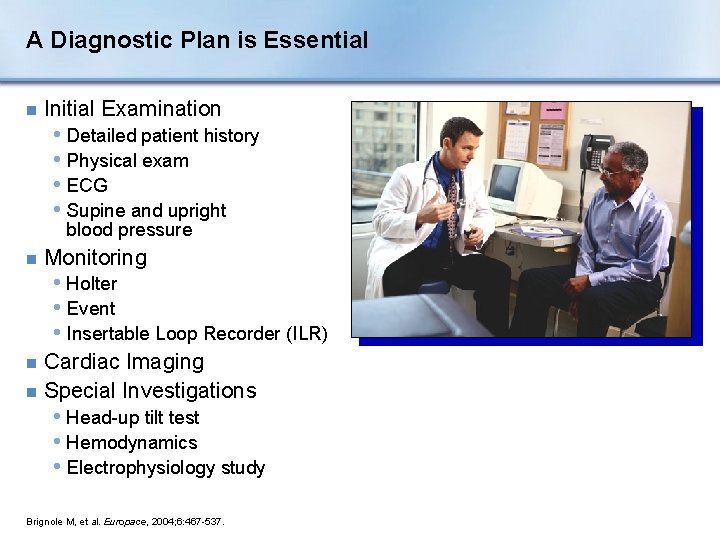
A Diagnostic Plan is Essential n Initial Examination • Detailed patient history • Physical exam • ECG • Supine and upright blood pressure n Monitoring • Holter • Event • Insertable Loop Recorder (ILR) Cardiac Imaging n Special Investigations n • Head-up tilt test • Hemodynamics • Electrophysiology study Brignole M, et al. Europace, 2004; 6: 467 -537.
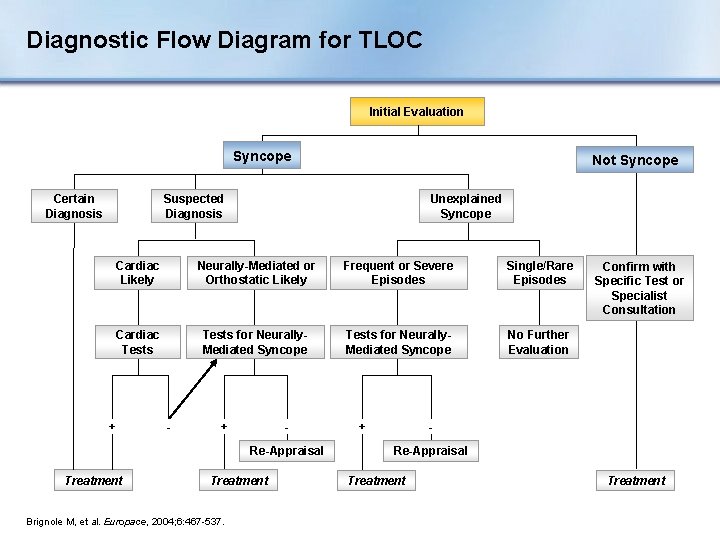
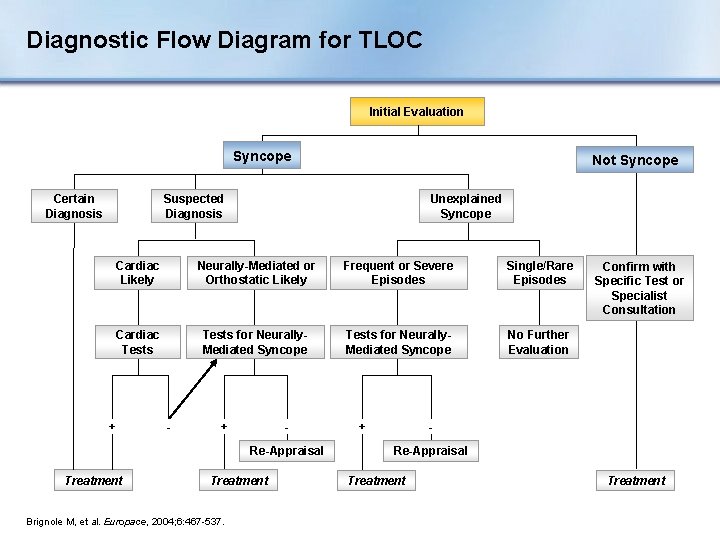
Diagnostic Flow Diagram for TLOC Initial Evaluation Syncope Certain Diagnosis Not Syncope Suspected Diagnosis Unexplained Syncope Cardiac Likely Neurally-Mediated or Orthostatic Likely Frequent or Severe Episodes Single/Rare Episodes Cardiac Tests for Neurally. Mediated Syncope No Further Evaluation + - + Re-Appraisal Treatment Brignole M, et al. Europace, 2004; 6: 467 -537. + Confirm with Specific Test or Specialist Consultation Re-Appraisal Treatment
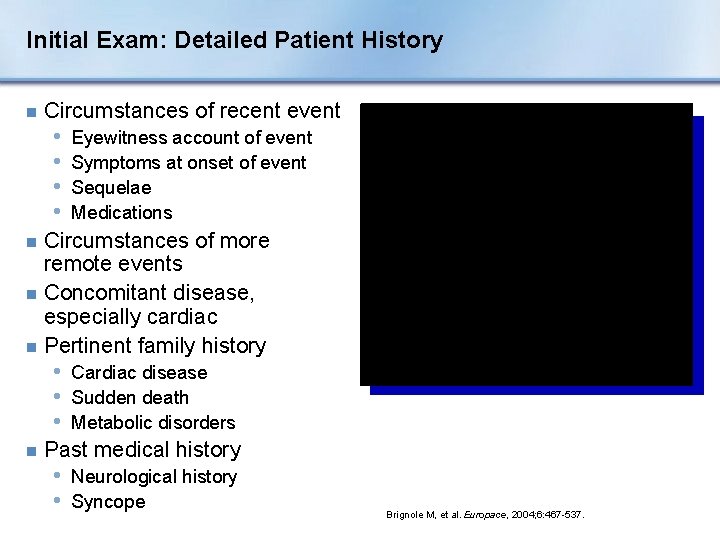
Initial Exam: Detailed Patient History n Circumstances of recent event • • Eyewitness account of event Symptoms at onset of event Sequelae Medications Circumstances of more remote events n Concomitant disease, especially cardiac n Pertinent family history n • Cardiac disease • Sudden death • Metabolic disorders n Past medical history • Neurological history • Syncope Brignole M, et al. Europace, 2004; 6: 467 -537.
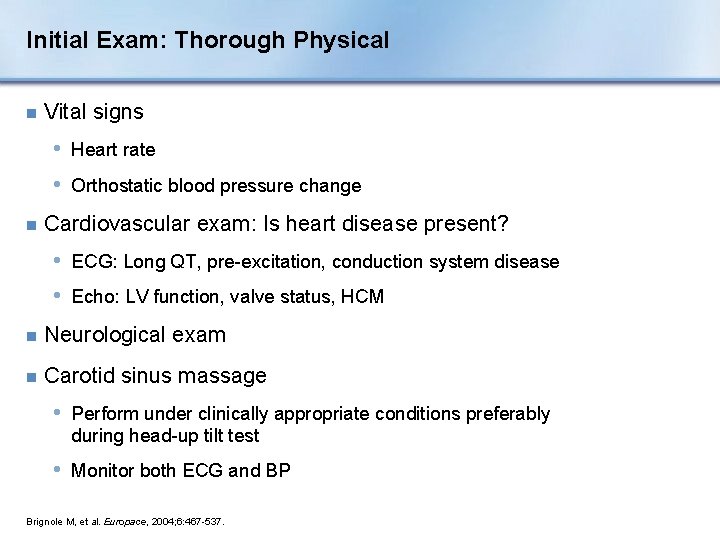
Initial Exam: Thorough Physical n Vital signs • Heart rate • Orthostatic blood pressure change n Cardiovascular exam: Is heart disease present? • ECG: Long QT, pre-excitation, conduction system disease • Echo: LV function, valve status, HCM n Neurological exam n Carotid sinus massage • Perform under clinically appropriate conditions preferably during head-up tilt test • Monitor both ECG and BP Brignole M, et al. Europace, 2004; 6: 467 -537.
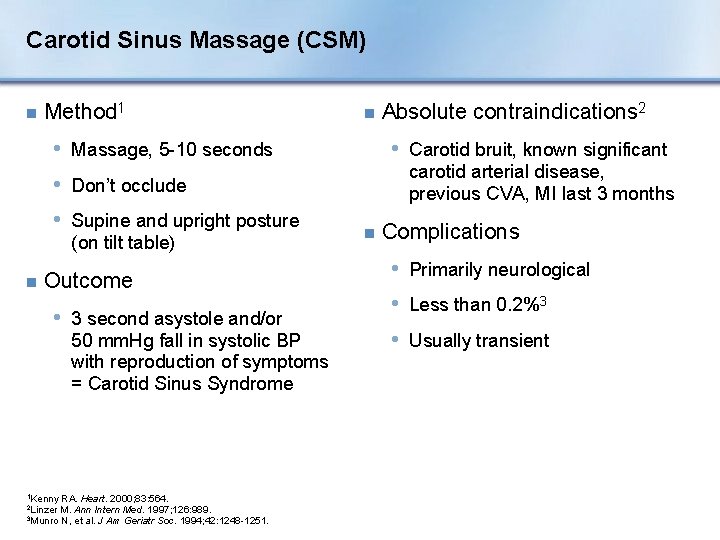
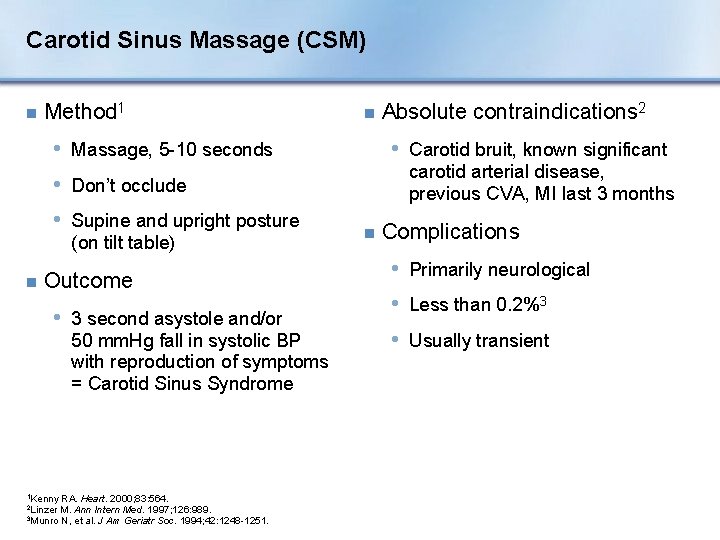
Carotid Sinus Massage (CSM) n Method 1 n • Massage, 5 -10 seconds • Carotid bruit, known significant carotid arterial disease, previous CVA, MI last 3 months • Don’t occlude • Supine and upright posture (on tilt table) n Outcome • 3 second asystole and/or 50 mm. Hg fall in systolic BP with reproduction of symptoms = Carotid Sinus Syndrome 1 Kenny RA. Heart. 2000; 83: 564. M. Ann Intern Med. 1997; 126: 989. 3 Munro N, et al. J Am Geriatr Soc. 1994; 42: 1248 -1251. 2 Linzer Absolute contraindications 2 n Complications • Primarily neurological • Less than 0. 2%3 • Usually transient
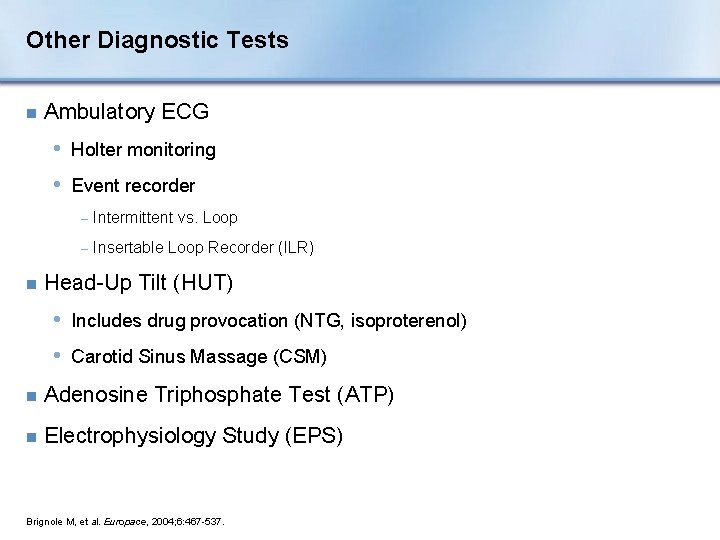
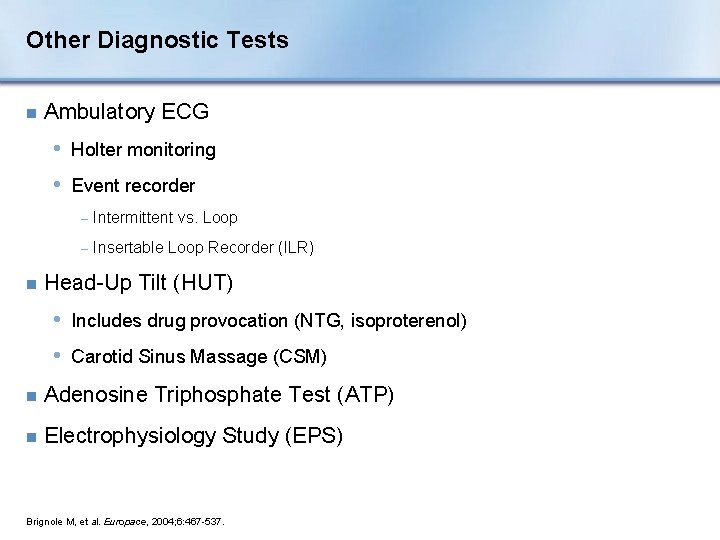
Other Diagnostic Tests n Ambulatory ECG • Holter monitoring • Event recorder n − Intermittent vs. Loop − Insertable Loop Recorder (ILR) Head-Up Tilt (HUT) • Includes drug provocation (NTG, isoproterenol) • Carotid Sinus Massage (CSM) n Adenosine Triphosphate Test (ATP) n Electrophysiology Study (EPS) Brignole M, et al. Europace, 2004; 6: 467 -537.
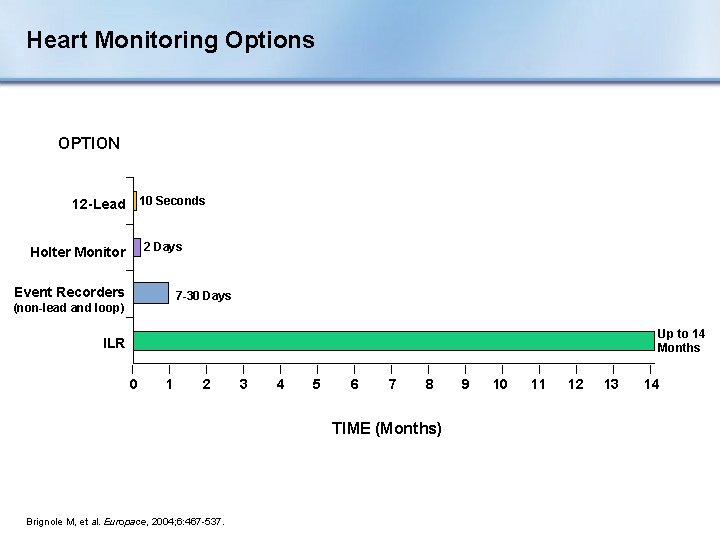
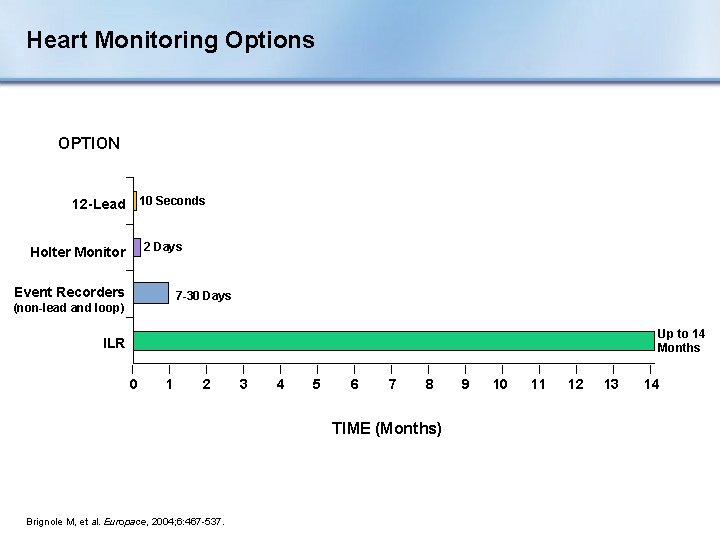
Heart Monitoring Options OPTION 10 Seconds 12 -Lead 2 Days Holter Monitor Event Recorders 7 -30 Days (non-lead and loop) Up to 14 Months ILR 0 1 2 3 4 5 6 7 8 TIME (Months) Brignole M, et al. Europace, 2004; 6: 467 -537. 9 10 11 12 13 14
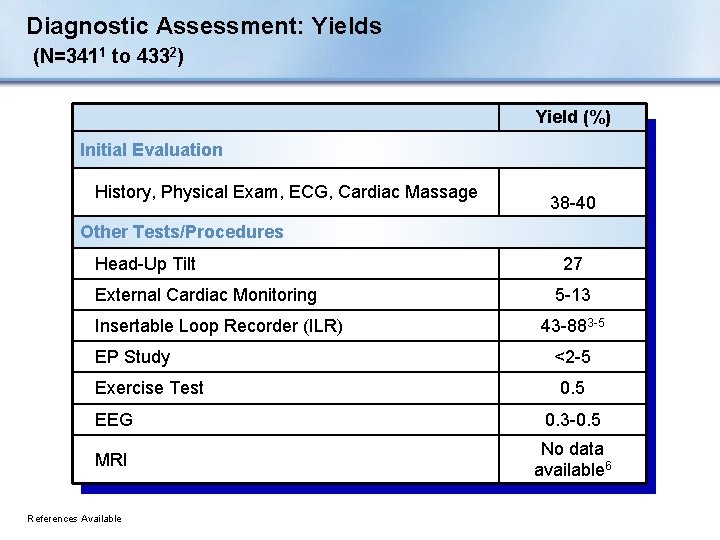
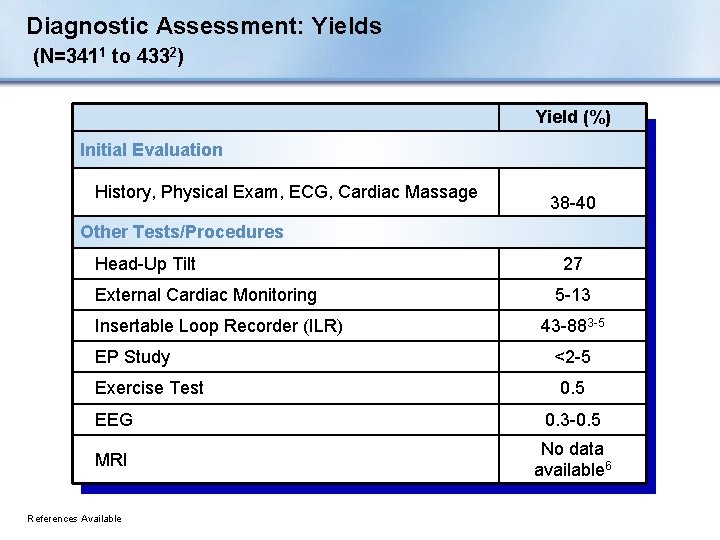
Diagnostic Assessment: Yields (N=3411 to 4332) Yield (%) Initial Evaluation History, Physical Exam, ECG, Cardiac Massage 38 -40 Other Tests/Procedures Head-Up Tilt External Cardiac Monitoring Insertable Loop Recorder (ILR) EP Study Exercise Test 27 5 -13 43 -883 -5 <2 -5 0. 5 EEG 0. 3 -0. 5 MRI No data available 6 References Available
Neurological Tests: Rarely Diagnostic for Syncope n EEG, Head CT, Head MRI n May help diagnose seizure Brignole M, et al. Europace. 2004; 6: 467 -537.
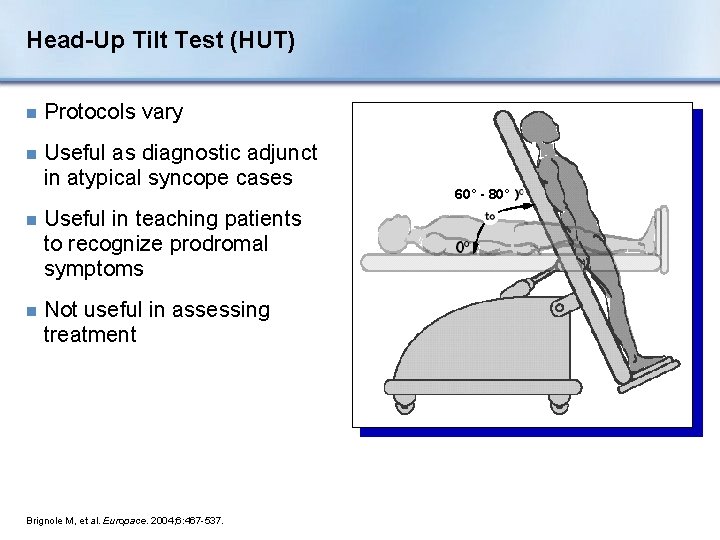
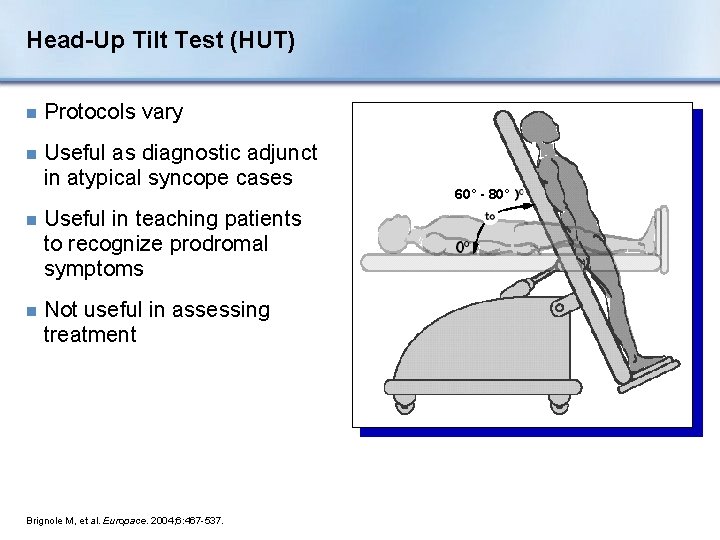
Head-Up Tilt Test (HUT) n Protocols vary n Useful as diagnostic adjunct in atypical syncope cases n Useful in teaching patients to recognize prodromal symptoms n Not useful in assessing treatment Brignole M, et al. Europace. 2004; 6: 467 -537. 60° - 80°
Head-up Tilt Test Click once on image to play video. Carlos Morillo, MD, FRCPC Professor, Faculty of Health Sciences Mc. Master University, Hamilton Ontario
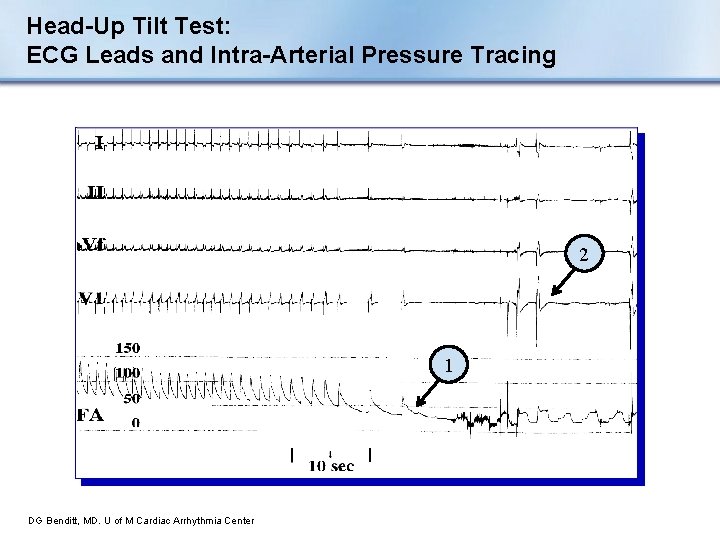
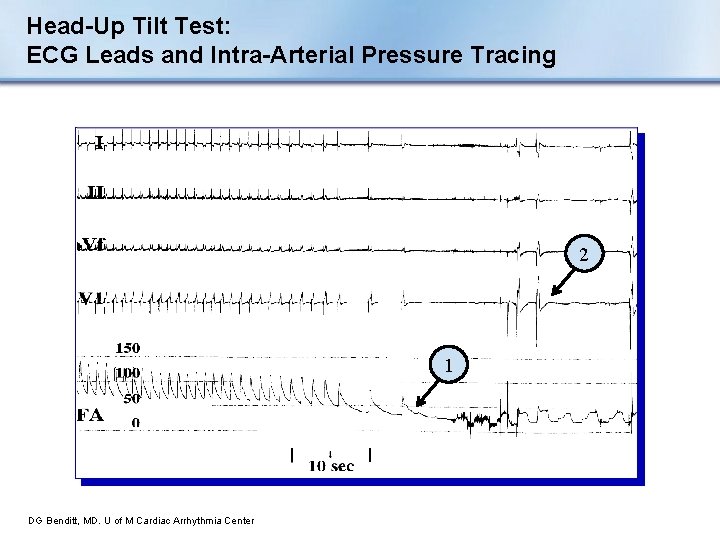
Head-Up Tilt Test: ECG Leads and Intra-Arterial Pressure Tracing 2 1 DG Benditt, MD. U of M Cardiac Arrhythmia Center
Adenosine Triphosphate (ATP) Test n Ongoing investigation in the US n Provokes a short and potent cardioinhibitory vasovagal response n Advantages • Simple • Inexpensive • Correlation with pacing benefit Brignole M. Heart. 2000; 83: 24 -28. Donateo P. J Am Coll Cardiol. 2003; 41: 93 -98. Flammang D. Circ. 1999; 99: 2427 -2433. n Seems to identify a unique mechanism of syncope found in patients with: • Advanced age • More hypertension • More ECG abnormalities
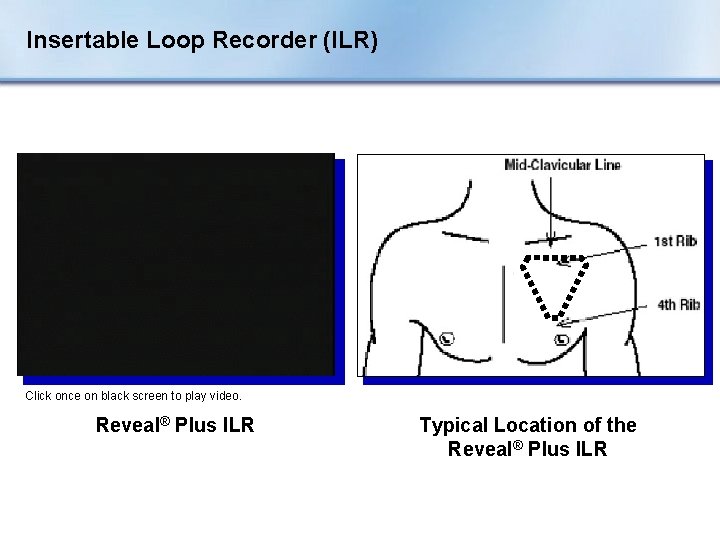
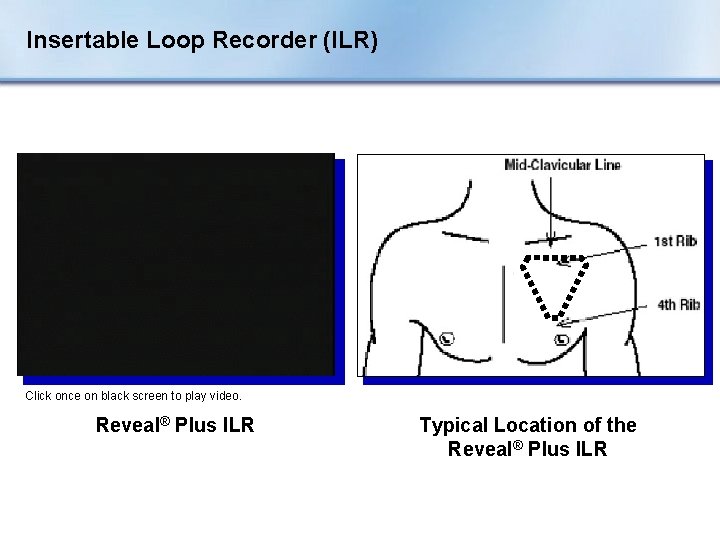
Insertable Loop Recorder (ILR) Click once on black screen to play video. Reveal® Plus ILR Typical Location of the Reveal® Plus ILR
Insertable Loop Recorder (ILR) The ILR is an implantable patient – and automatically – activated monitoring system that records subcutaneous ECG and is indicated for: n Patients with clinical syndromes or situations at increased risk of cardiac arrhythmias n Patients who experience transient symptoms that may suggest a cardiac arrhythmia
Insertable Loop Recorder (ILR) Click once on black screen to play video.
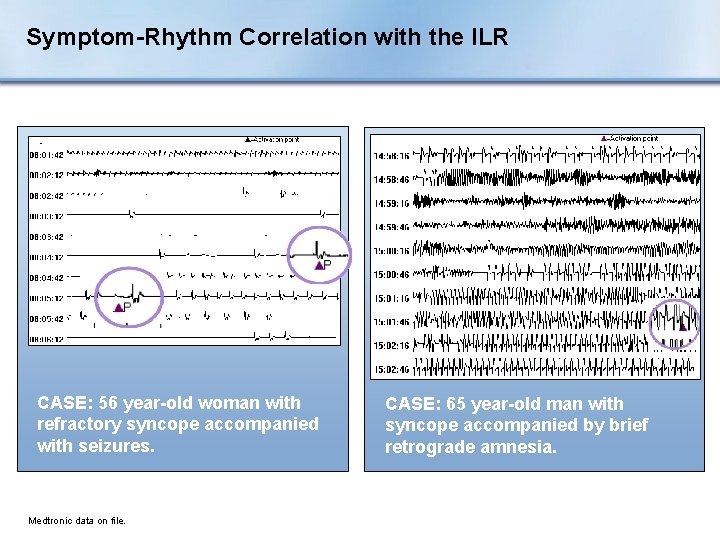
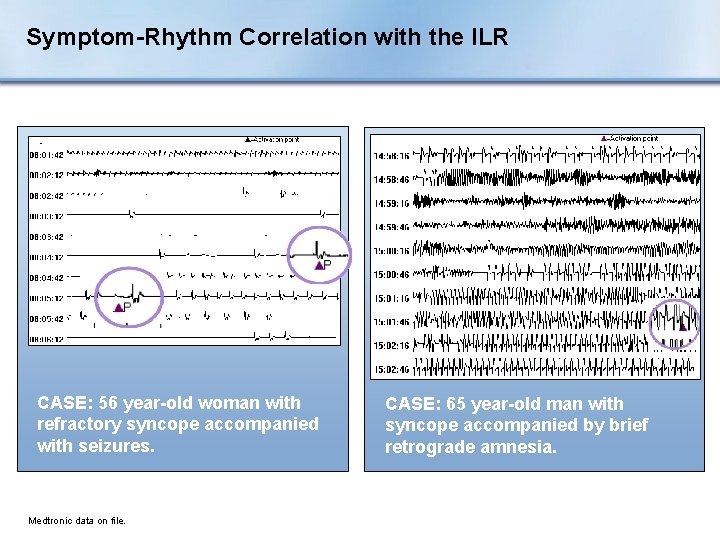
Symptom-Rhythm Correlation with the ILR CASE: 56 year-old woman with refractory syncope accompanied with seizures. Medtronic data on file. CASE: 65 year-old man with syncope accompanied by brief retrograde amnesia.
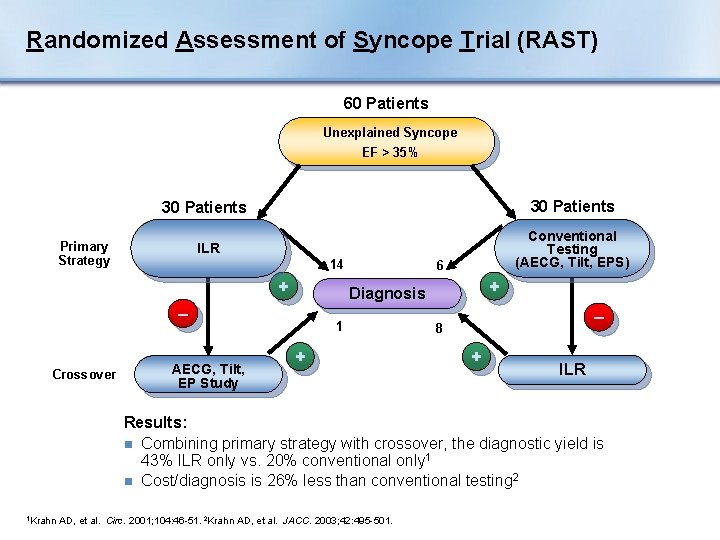
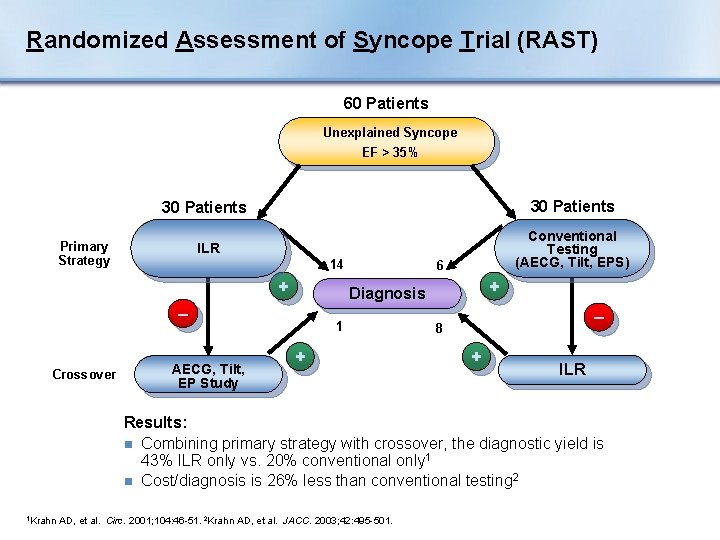
Randomized Assessment of Syncope Trial (RAST) 60 Patients Unexplained Syncope EF > 35% 30 Patients ILR Conventional Testing (AECG, Tilt, EPS) Primary Strategy 14 + Crossover + Diagnosis – AECG, Tilt, EP Study 6 1 + – 8 + ILR Results: n Combining primary strategy with crossover, the diagnostic yield is 43% ILR only vs. 20% conventional only 1 n Cost/diagnosis is 26% less than conventional testing 2 1 Krahn AD, et al. Circ. 2001; 104: 46 -51. 2 Krahn AD, et al. JACC. 2003; 42: 495 -501.
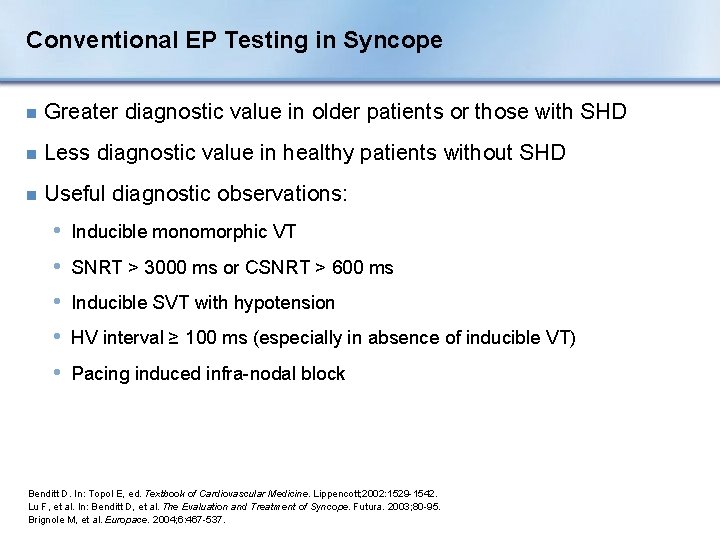
Conventional EP Testing in Syncope n Greater diagnostic value in older patients or those with SHD n Less diagnostic value in healthy patients without SHD n Useful diagnostic observations: • Inducible monomorphic VT • SNRT > 3000 ms or CSNRT > 600 ms • Inducible SVT with hypotension • HV interval ≥ 100 ms (especially in absence of inducible VT) • Pacing induced infra-nodal block Benditt D. In: Topol E, ed. Textbook of Cardiovascular Medicine. Lippencott; 2002: 1529 -1542. Lu F, et al. In: Benditt D, et al. The Evaluation and Treatment of Syncope. Futura. 2003; 80 -95. Brignole M, et al. Europace. 2004; 6: 467 -537.
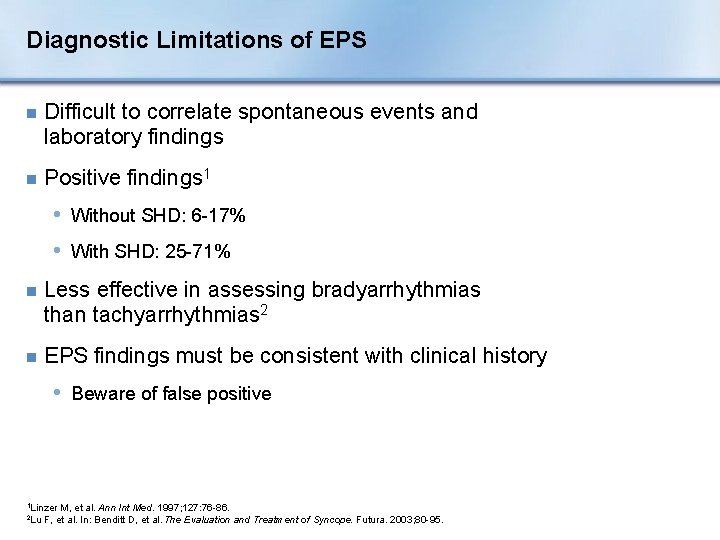
Diagnostic Limitations of EPS n Difficult to correlate spontaneous events and laboratory findings n Positive findings 1 • Without SHD: 6 -17% • With SHD: 25 -71% n Less effective in assessing bradyarrhythmias than tachyarrhythmias 2 n EPS findings must be consistent with clinical history • Beware of false positive 1 Linzer 2 Lu M, et al. Ann Int Med. 1997; 127: 76 -86. F, et al. In: Benditt D, et al. The Evaluation and Treatment of Syncope. Futura. 2003; 80 -95.
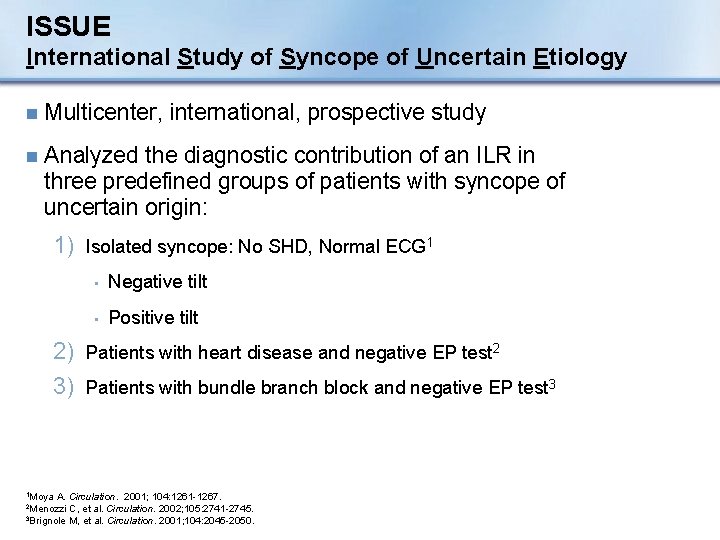
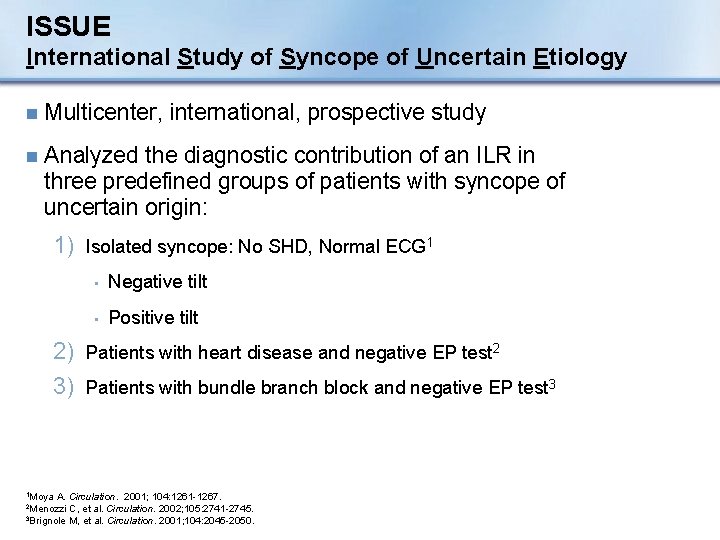
ISSUE International Study of Syncope of Uncertain Etiology n Multicenter, international, prospective study n Analyzed the diagnostic contribution of an ILR in three predefined groups of patients with syncope of uncertain origin: 1) Isolated syncope: No SHD, Normal ECG 1 • Negative tilt • Positive tilt 2) Patients with heart disease and negative EP test 2 3) Patients with bundle branch block and negative EP test 3 1 Moya A. Circulation. 2001; 104: 1261 -1267. C, et al. Circulation. 2002; 105: 2741 -2745. 3 Brignole M, et al. Circulation. 2001; 104: 2045 -2050. 2 Menozzi
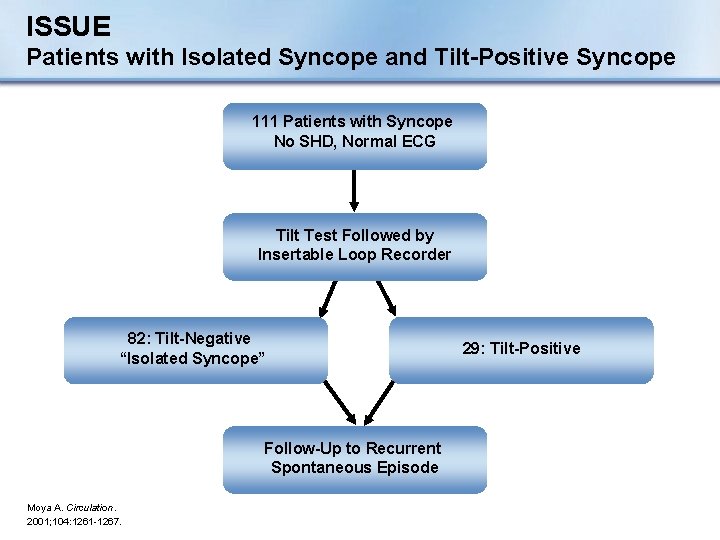
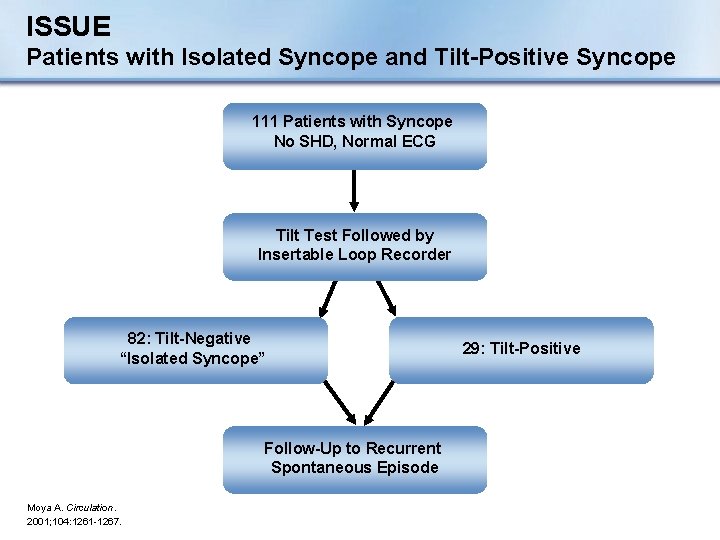
ISSUE Patients with Isolated Syncope and Tilt-Positive Syncope 111 Patients with Syncope No SHD, Normal ECG Tilt Test Followed by Insertable Loop Recorder 82: Tilt-Negative “Isolated Syncope” Follow-Up to Recurrent Spontaneous Episode Moya A. Circulation. 2001; 104: 1261 -1267. 29: Tilt-Positive
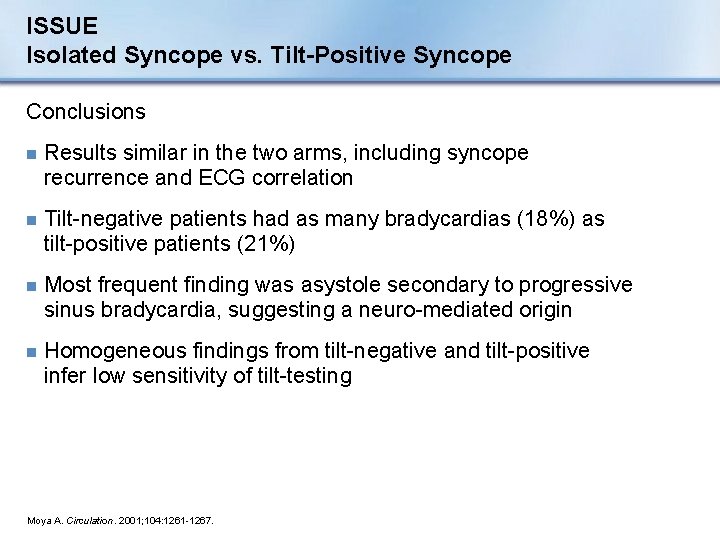
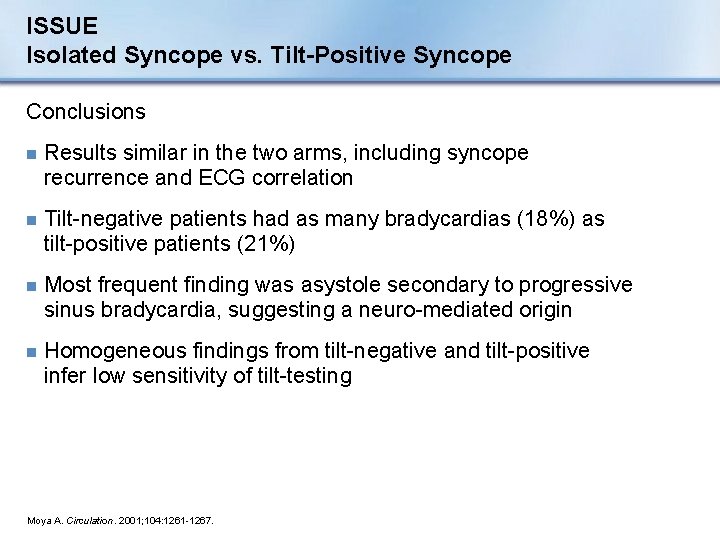
ISSUE Isolated Syncope vs. Tilt-Positive Syncope Conclusions n Results similar in the two arms, including syncope recurrence and ECG correlation n Tilt-negative patients had as many bradycardias (18%) as tilt-positive patients (21%) n Most frequent finding was asystole secondary to progressive sinus bradycardia, suggesting a neuro-mediated origin n Homogeneous findings from tilt-negative and tilt-positive infer low sensitivity of tilt-testing Moya A. Circulation. 2001; 104: 1261 -1267.
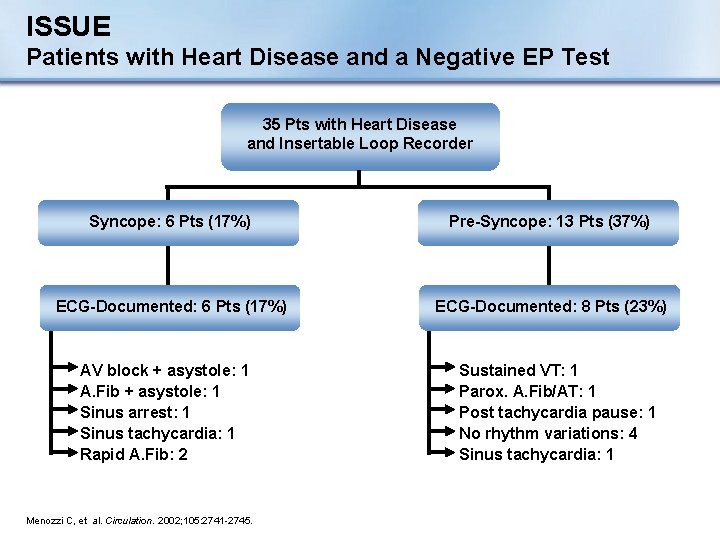
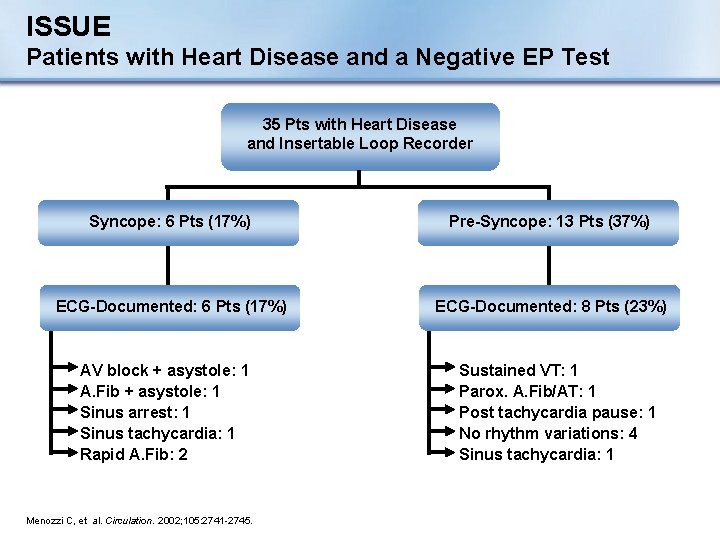
ISSUE Patients with Heart Disease and a Negative EP Test 35 Pts with Heart Disease and Insertable Loop Recorder Syncope: 6 Pts (17%) Pre-Syncope: 13 Pts (37%) ECG-Documented: 6 Pts (17%) ECG-Documented: 8 Pts (23%) AV block + asystole: 1 A. Fib + asystole: 1 Sinus arrest: 1 Sinus tachycardia: 1 Rapid A. Fib: 2 Menozzi C, et al. Circulation. 2002; 105: 2741 -2745. Sustained VT: 1 Parox. A. Fib/AT: 1 Post tachycardia pause: 1 No rhythm variations: 4 Sinus tachycardia: 1
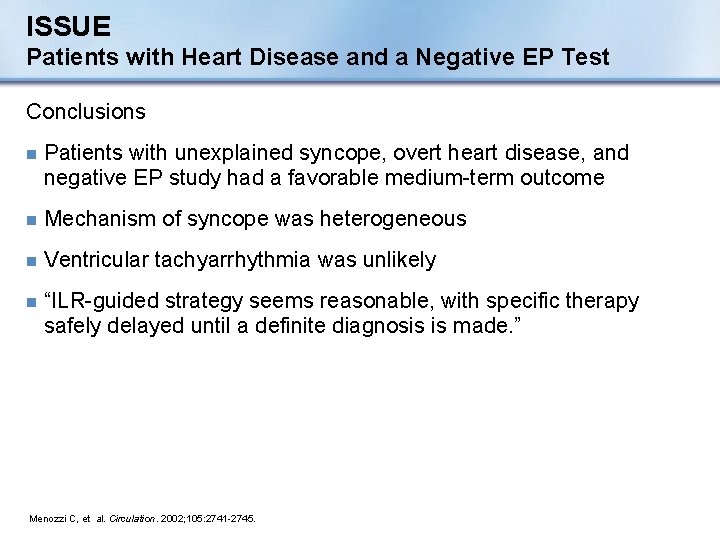
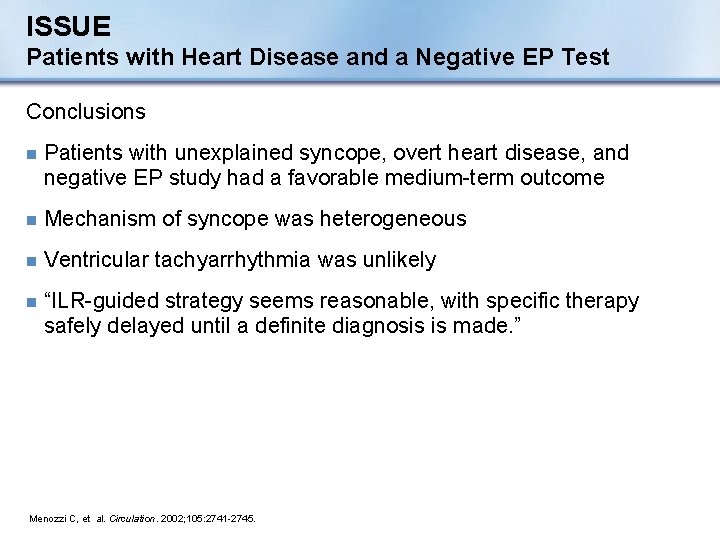
ISSUE Patients with Heart Disease and a Negative EP Test Conclusions n Patients with unexplained syncope, overt heart disease, and negative EP study had a favorable medium-term outcome n Mechanism of syncope was heterogeneous n Ventricular tachyarrhythmia was unlikely n “ILR-guided strategy seems reasonable, with specific therapy safely delayed until a definite diagnosis is made. ” Menozzi C, et al. Circulation. 2002; 105: 2741 -2745.
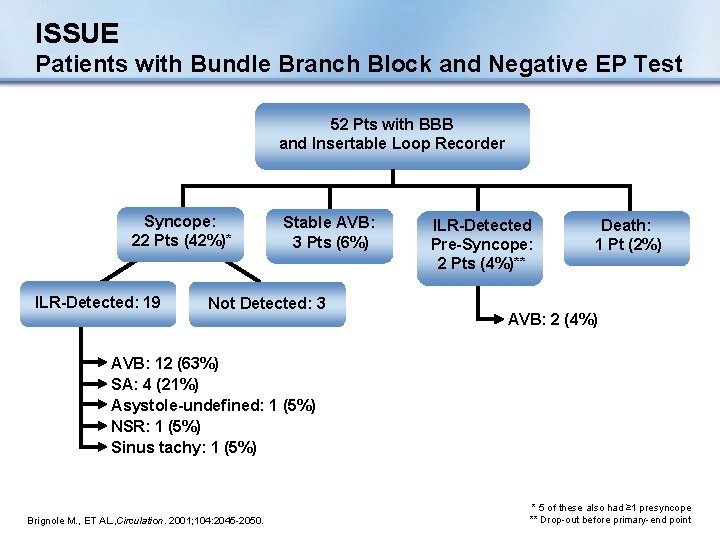
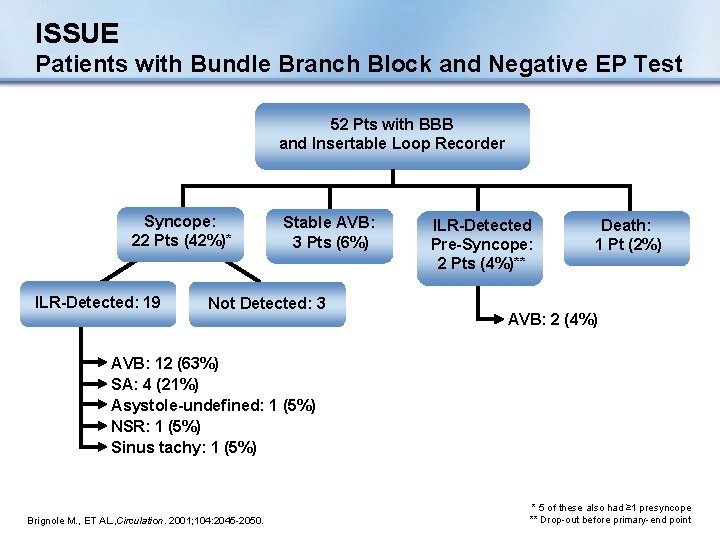
ISSUE Patients with Bundle Branch Block and Negative EP Test 52 Pts with BBB and Insertable Loop Recorder Syncope: 22 Pts (42%)* ILR-Detected: 19 Stable AVB: 3 Pts (6%) Not Detected: 3 ILR-Detected Pre-Syncope: 2 Pts (4%)** Death: 1 Pt (2%) AVB: 2 (4%) AVB: 12 (63%) SA: 4 (21%) Asystole-undefined: 1 (5%) NSR: 1 (5%) Sinus tachy: 1 (5%) Brignole M. , ET AL. , Circulation. 2001; 104: 2045 -2050. * 5 of these also had ≥ 1 presyncope ** Drop-out before primary-end point
ISSUE Patients with Bundle Branch Block and Negative EP Test Conclusion: n In patients with BBB and negative EP study, most syncopal recurrences have a homogeneous mechanism that is characterized by prolonged asystolic pauses mainly attributable to sudden-onset paroxysmal AV block Brignole M. Circulation. 2001; 104: 2045 -2050.
Section III: Specific Conditions and Treatment
Specific Conditions n Cardiac arrhythmia • Brady/Tachy • Long QT syndrome • Torsade de pointes • Brugada • Drug-induced n Structural cardio-pulmonary n Neurally-mediated • Vasovagal Syncope (VVS) • Carotid Sinus Syndrome (CSS) n Orthostatic
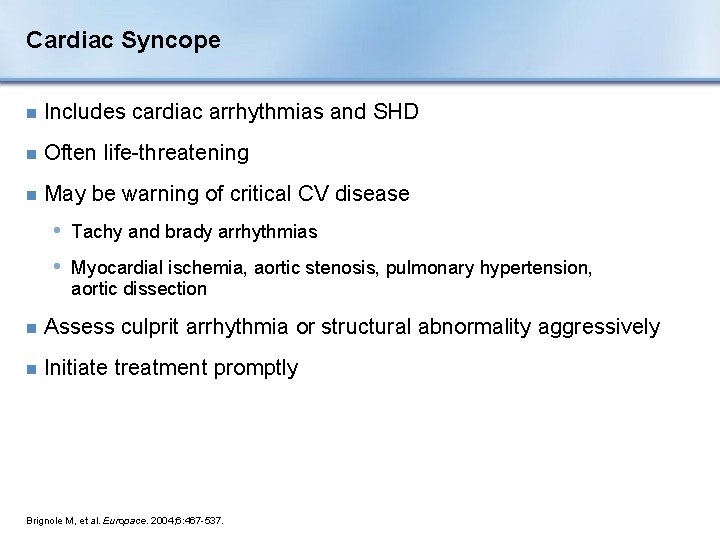
Cardiac Syncope n Includes cardiac arrhythmias and SHD n Often life-threatening n May be warning of critical CV disease • Tachy and brady arrhythmias • Myocardial ischemia, aortic stenosis, pulmonary hypertension, aortic dissection n Assess culprit arrhythmia or structural abnormality aggressively n Initiate treatment promptly Brignole M, et al. Europace. 2004; 6: 467 -537.
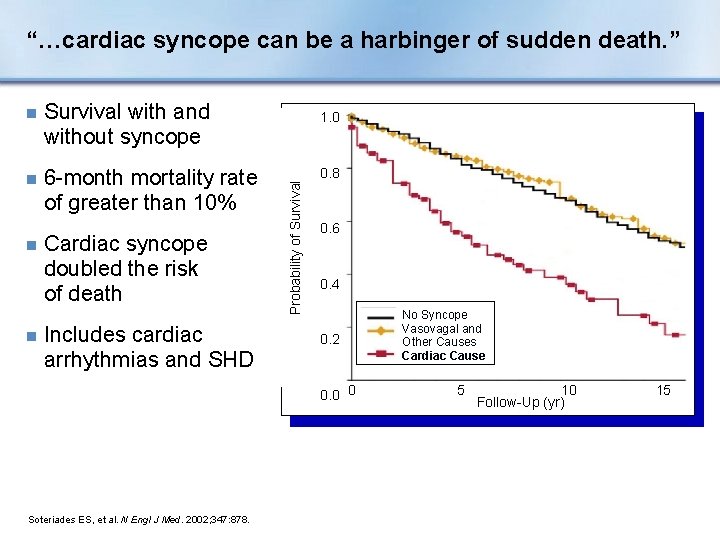
“…cardiac syncope can be a harbinger of sudden death. ” Survival with and without syncope n 6 -month mortality rate of greater than 10% n n Cardiac syncope doubled the risk of death Includes cardiac arrhythmias and SHD 1. 0 Probability of Survival n 0. 8 0. 6 0. 4 0. 2 0. 0 0 Soteriades ES, et al. N Engl J Med. 2002; 347: 878. No Syncope Vasovagal and Other Causes Cardiac Cause 5 10 Follow-Up (yr) 15
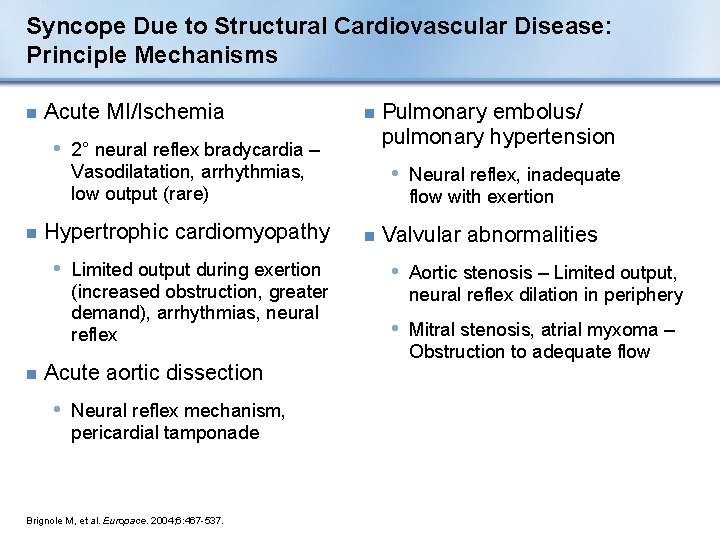
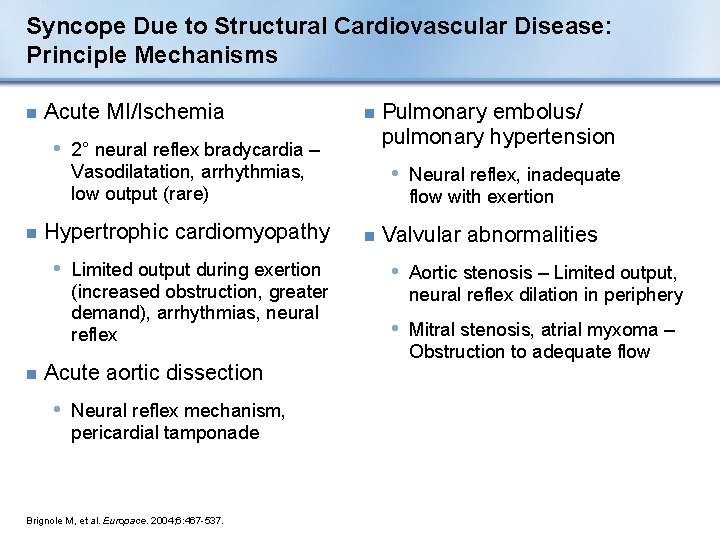
Syncope Due to Structural Cardiovascular Disease: Principle Mechanisms n Acute MI/Ischemia n • 2° neural reflex bradycardia – • Neural reflex, inadequate Vasodilatation, arrhythmias, low output (rare) n Hypertrophic cardiomyopathy • Limited output during exertion (increased obstruction, greater demand), arrhythmias, neural reflex n Acute aortic dissection • Neural reflex mechanism, pericardial tamponade Brignole M, et al. Europace. 2004; 6: 467 -537. Pulmonary embolus/ pulmonary hypertension flow with exertion n Valvular abnormalities • Aortic stenosis – Limited output, neural reflex dilation in periphery • Mitral stenosis, atrial myxoma – Obstruction to adequate flow
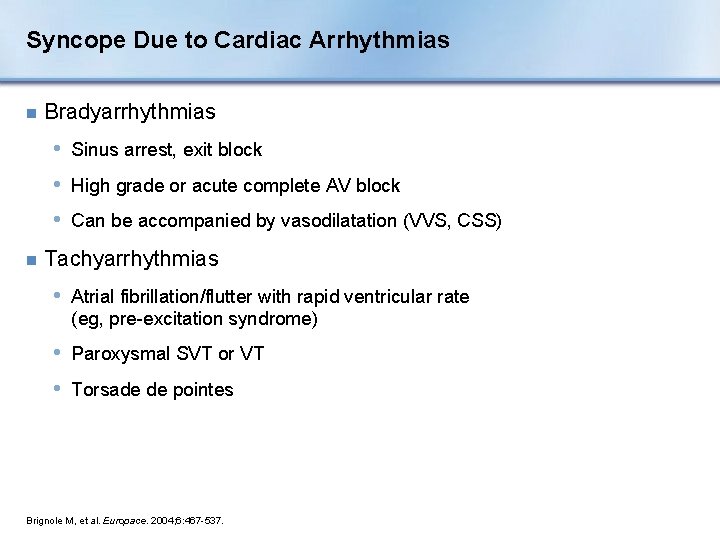
Syncope Due to Cardiac Arrhythmias n Bradyarrhythmias • Sinus arrest, exit block • High grade or acute complete AV block • Can be accompanied by vasodilatation (VVS, CSS) n Tachyarrhythmias • Atrial fibrillation/flutter with rapid ventricular rate (eg, pre-excitation syndrome) • Paroxysmal SVT or VT • Torsade de pointes Brignole M, et al. Europace. 2004; 6: 467 -537.
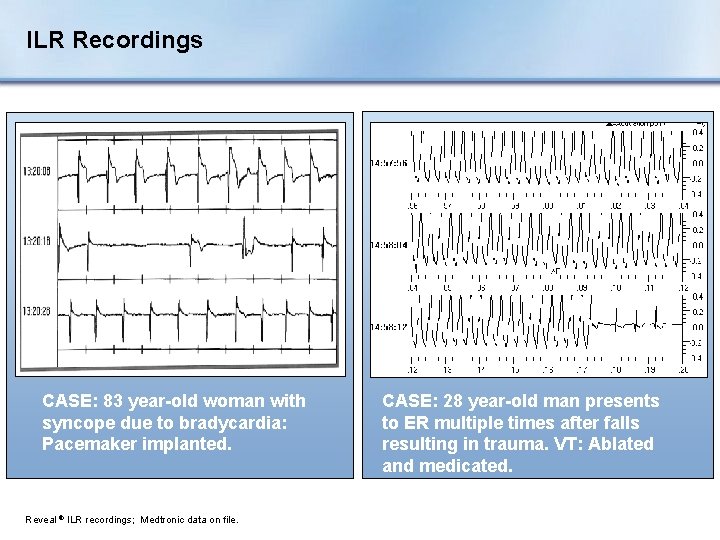
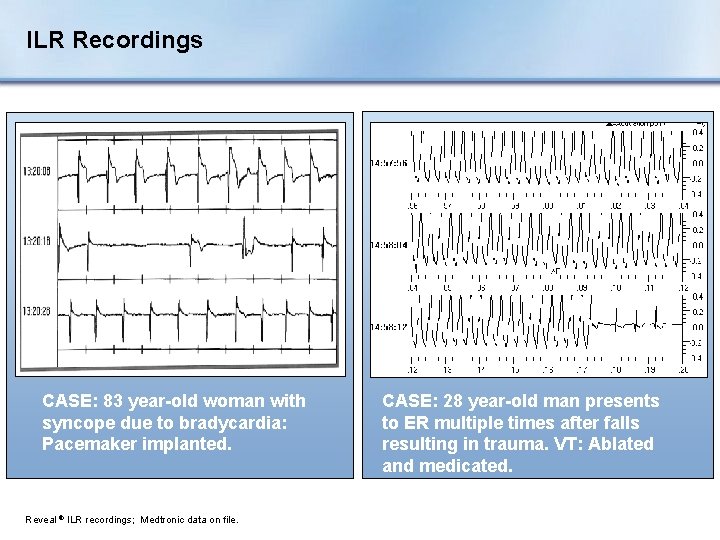
ILR Recordings CASE: 83 year-old woman with syncope due to bradycardia: Pacemaker implanted. Reveal ® ILR recordings; Medtronic data on file. CASE: 28 year-old man presents to ER multiple times after falls resulting in trauma. VT: Ablated and medicated.
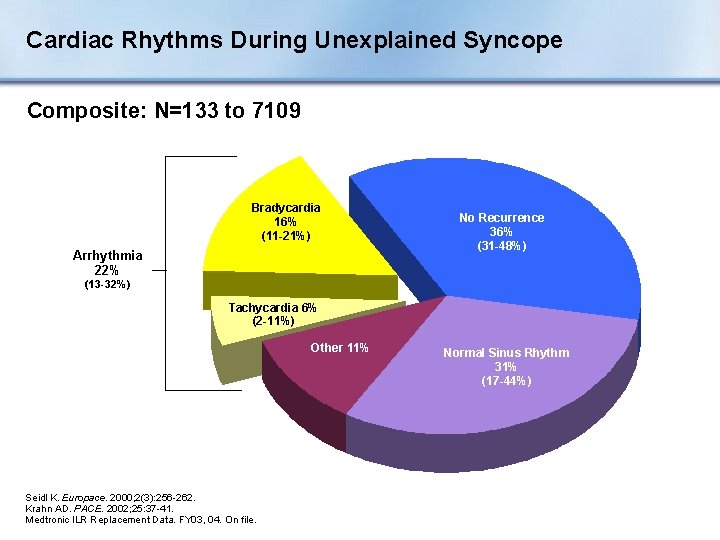
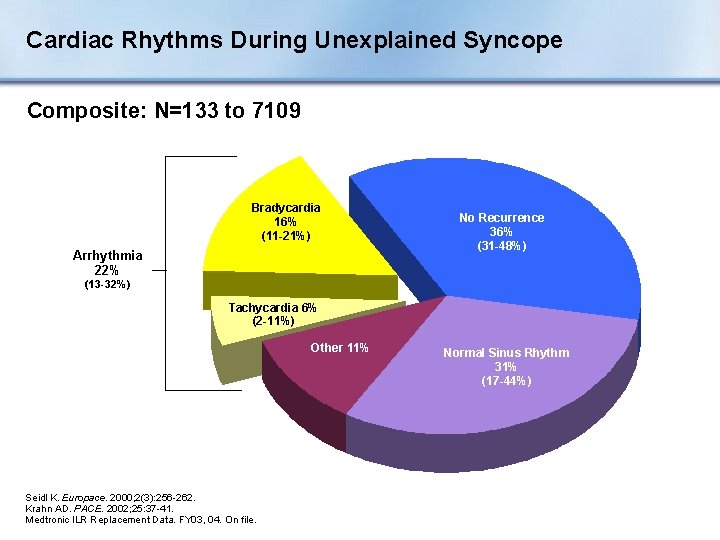
Cardiac Rhythms During Unexplained Syncope Composite: N=133 to 7109 Bradycardia 16% (11 -21%) Arrhythmia 22% No Recurrence 36% (31 -48%) (13 -32%) Tachycardia 6% (2 -11%) Other 11% Seidl K. Europace. 2000; 2(3): 256 -262. Krahn AD. PACE. 2002; 25: 37 -41. Medtronic ILR Replacement Data. FY 03, 04. On file. Normal Sinus Rhythm 31% (17 -44%)
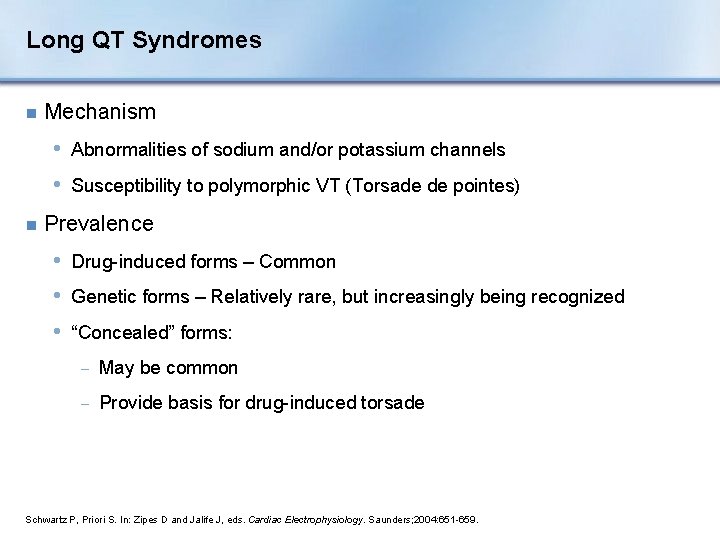
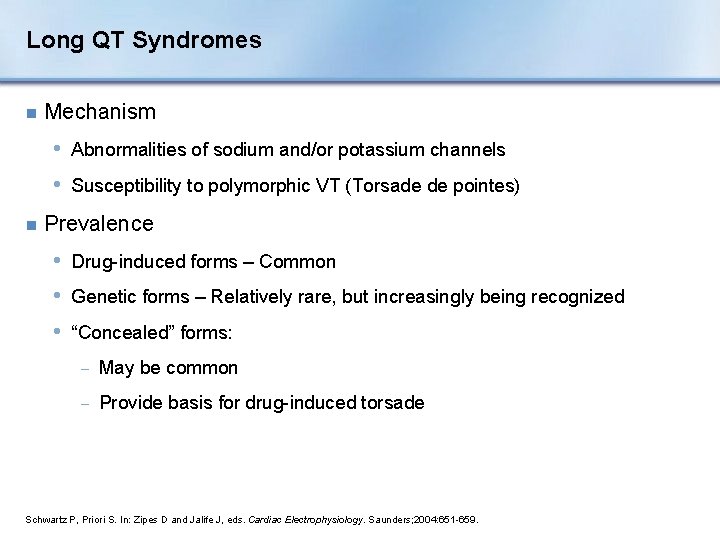
Long QT Syndromes n Mechanism • Abnormalities of sodium and/or potassium channels • Susceptibility to polymorphic VT (Torsade de pointes) n Prevalence • Drug-induced forms – Common • Genetic forms – Relatively rare, but increasingly being recognized • “Concealed” forms: − May be common − Provide basis for drug-induced torsade Schwartz P, Priori S. In: Zipes D and Jalife J, eds. Cardiac Electrophysiology. Saunders; 2004: 651 -659.
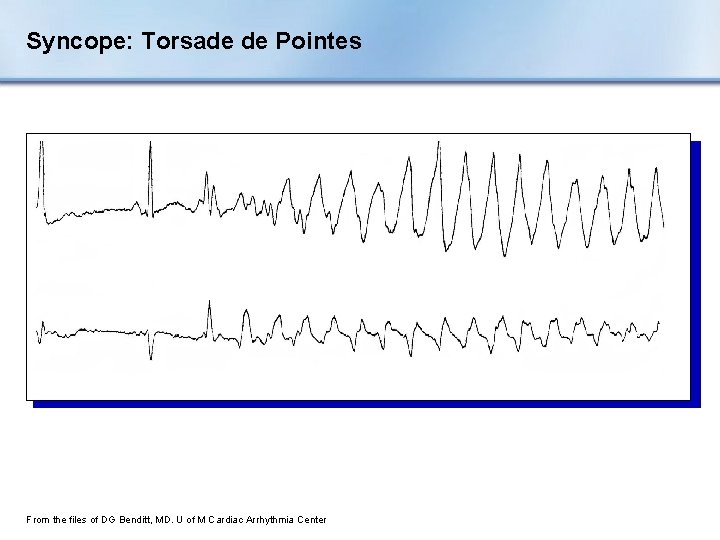
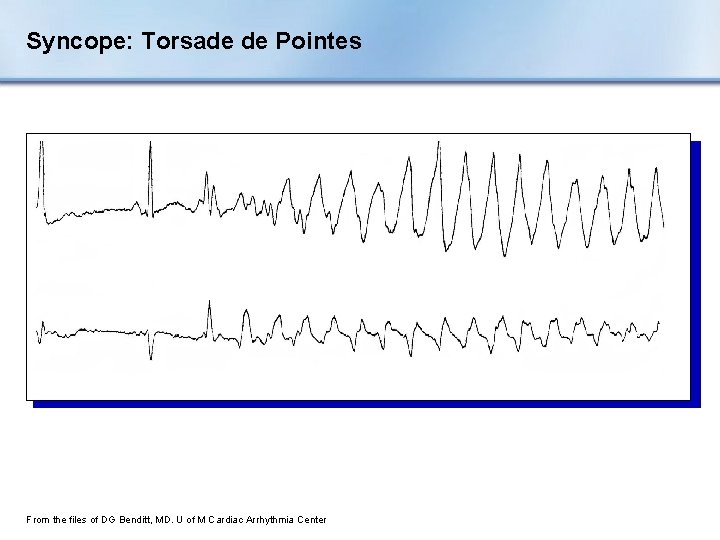
Syncope: Torsade de Pointes From the files of DG Benditt, MD. U of M Cardiac Arrhythmia Center
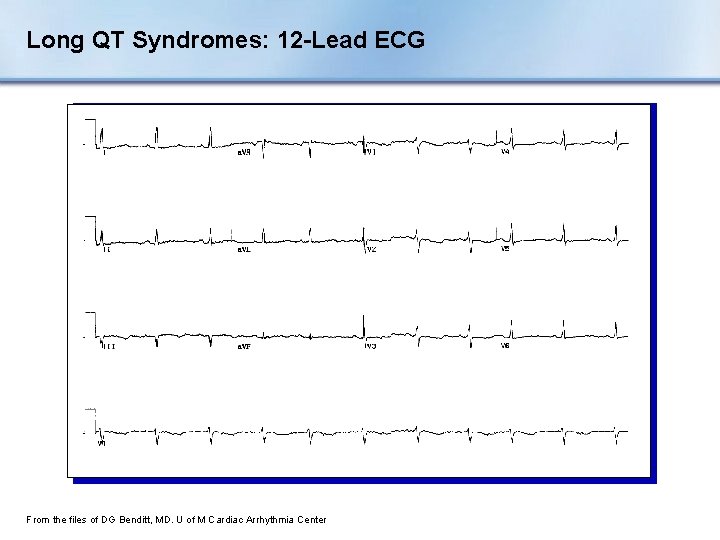
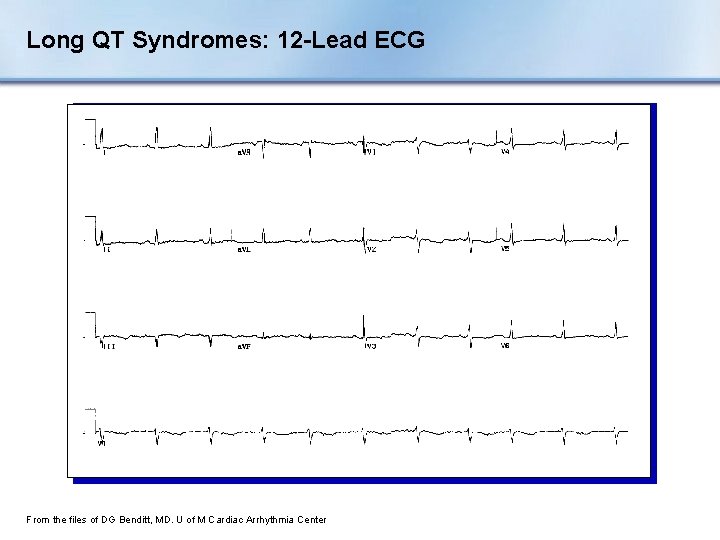
Long QT Syndromes: 12 -Lead ECG From the files of DG Benditt, MD. U of M Cardiac Arrhythmia Center
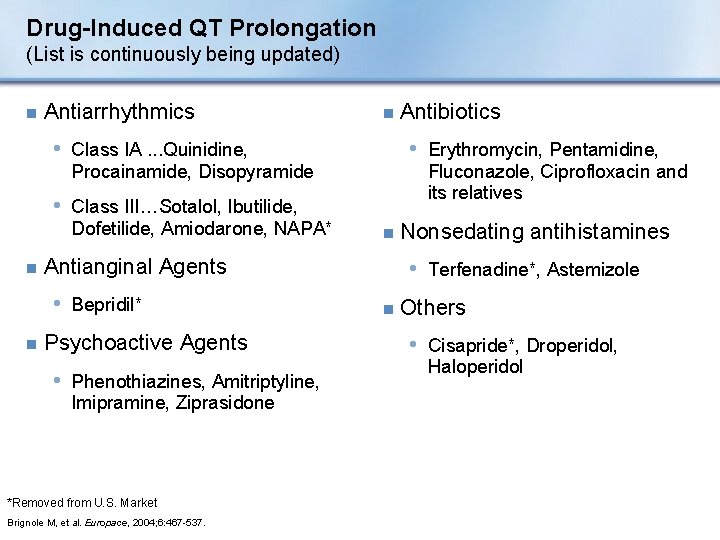
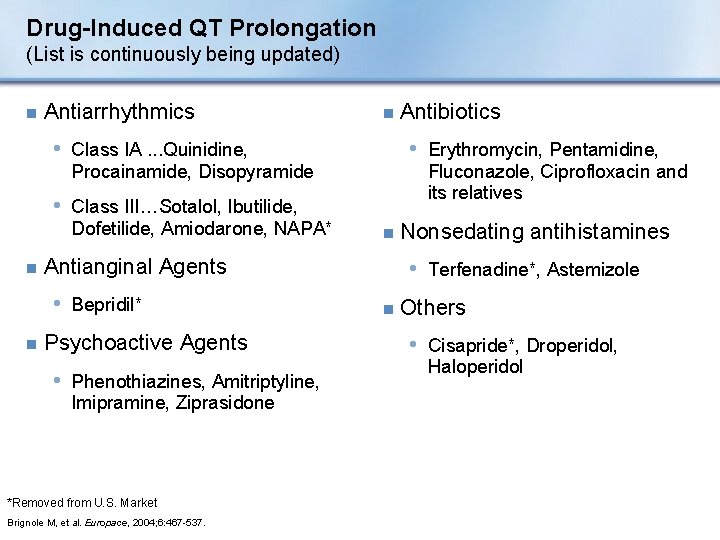
Drug-Induced QT Prolongation (List is continuously being updated) n Antiarrhythmics n • Erythromycin, Pentamidine, • Class IA. . . Quinidine, Fluconazole, Ciprofloxacin and its relatives Procainamide, Disopyramide • Class III…Sotalol, Ibutilide, Dofetilide, Amiodarone, NAPA* n n n Antianginal Agents • Bepridil* Psychoactive Agents • Phenothiazines, Amitriptyline, Imipramine, Ziprasidone *Removed from U. S. Market Brignole M, et al. Europace, 2004; 6: 467 -537. Antibiotics Nonsedating antihistamines • Terfenadine*, Astemizole n Others • Cisapride*, Droperidol, Haloperidol
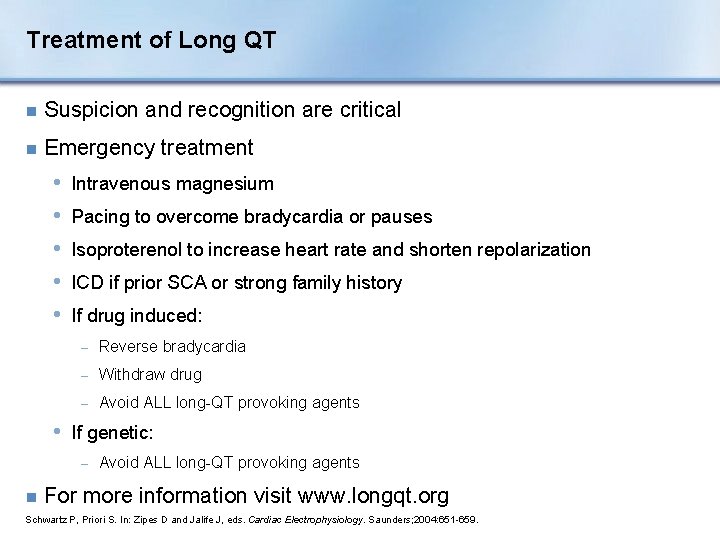
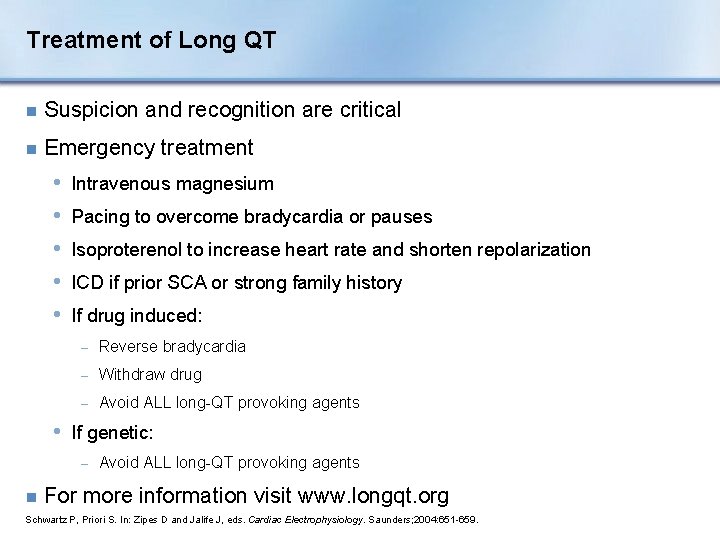
Treatment of Long QT n Suspicion and recognition are critical n Emergency treatment • • • Intravenous magnesium Pacing to overcome bradycardia or pauses Isoproterenol to increase heart rate and shorten repolarization ICD if prior SCA or strong family history If drug induced: − Reverse bradycardia − Withdraw drug − Avoid ALL long-QT provoking agents • If genetic: − n Avoid ALL long-QT provoking agents For more information visit www. longqt. org Schwartz P, Priori S. In: Zipes D and Jalife J, eds. Cardiac Electrophysiology. Saunders; 2004: 651 -659.
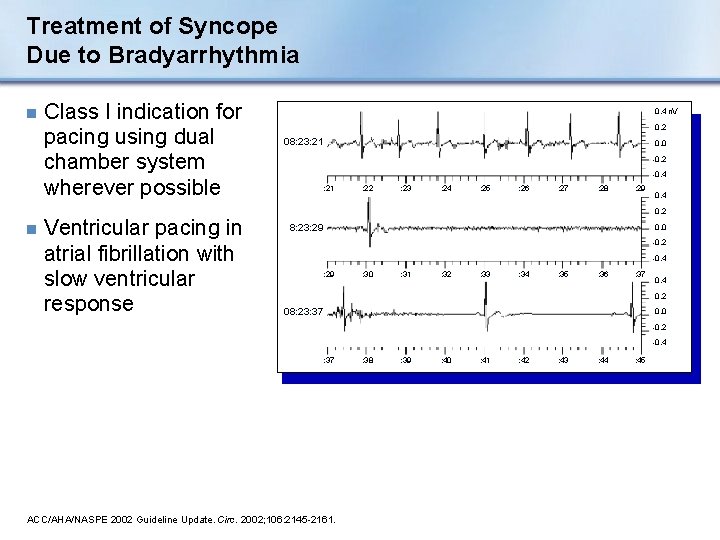
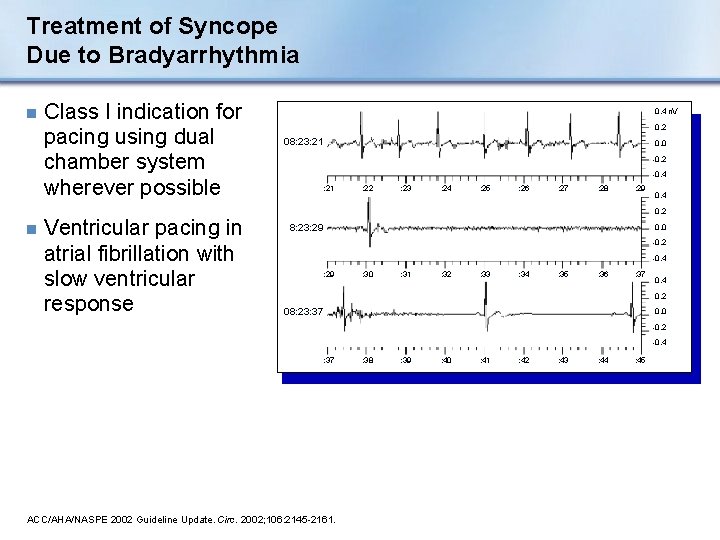
Treatment of Syncope Due to Bradyarrhythmia n n Class I indication for pacing using dual chamber system wherever possible Ventricular pacing in atrial fibrillation with slow ventricular response 0. 4 n. V 0. 2 08: 23: 21 0. 0 -0. 2 -0. 4 : 21 : 22 : 23 : 24 : 25 : 26 : 27 : 28 : 29 0. 4 0. 2 8: 23: 29 0. 0 -0. 2 -0. 4 : 29 : 30 : 31 : 32 : 33 : 34 : 35 : 36 : 37 0. 4 0. 2 08: 23: 37 0. 0 -0. 2 -0. 4 : 37 ACC/AHA/NASPE 2002 Guideline Update. Circ. 2002; 106: 2145 -2161. : 38 : 39 : 40 : 41 : 42 : 43 : 44 : 45
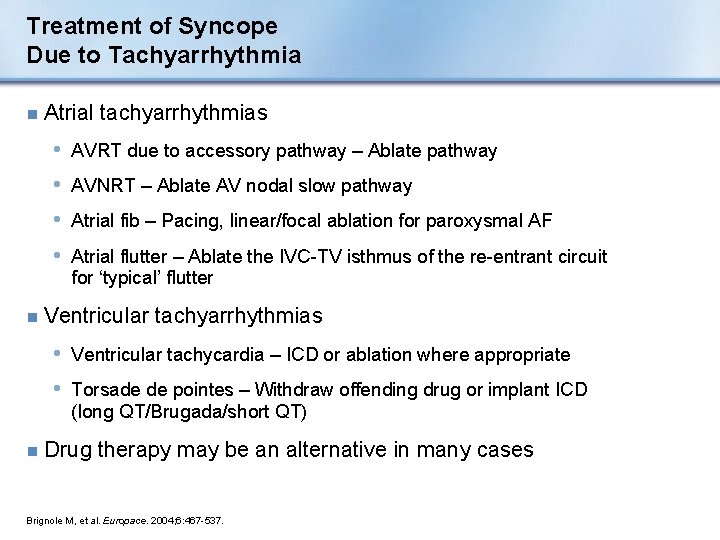
Treatment of Syncope Due to Tachyarrhythmia n Atrial tachyarrhythmias • AVRT due to accessory pathway – Ablate pathway • AVNRT – Ablate AV nodal slow pathway • Atrial fib – Pacing, linear/focal ablation for paroxysmal AF • Atrial flutter – Ablate the IVC-TV isthmus of the re-entrant circuit for ‘typical’ flutter n Ventricular tachyarrhythmias • Ventricular tachycardia – ICD or ablation where appropriate • Torsade de pointes – Withdraw offending drug or implant ICD (long QT/Brugada/short QT) n Drug therapy may be an alternative in many cases Brignole M, et al. Europace. 2004; 6: 467 -537.
Neurally-Mediated Reflex Syncope n Vasovagal Syncope (VVS) n Carotid Sinus Syndrome (CSS) n Situational syncope • Post-micturition • Cough • Swallow • Defecation • Blood drawing, etc. Brignole M, et al. Europace, 2004; 6: 467 -537.
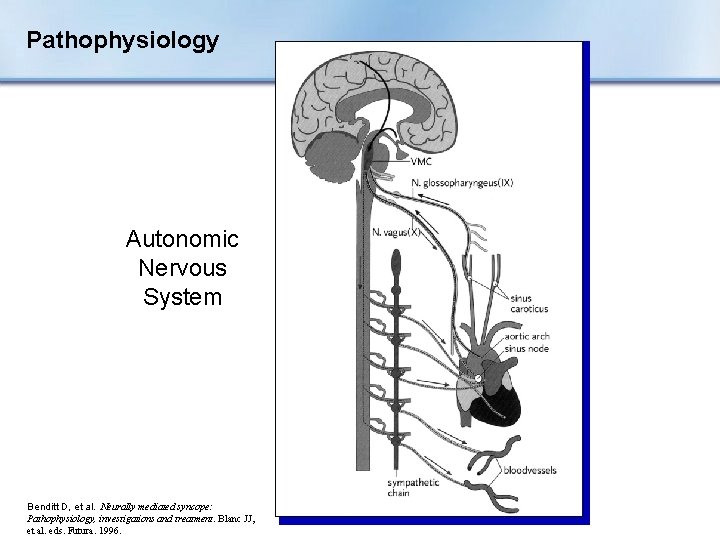
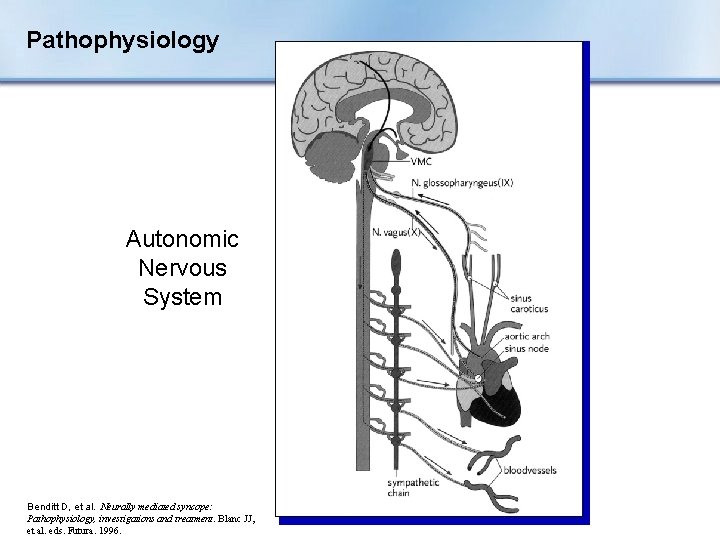
Pathophysiology Autonomic Nervous System Benditt D, et al. Neurally mediated syncope: Pathophysiology, investigations and treatment. Blanc JJ, et al. eds. Futura. 1996.
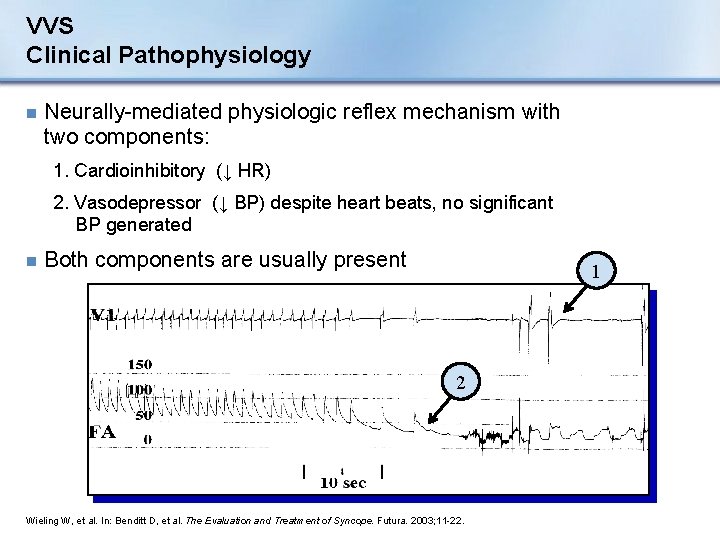
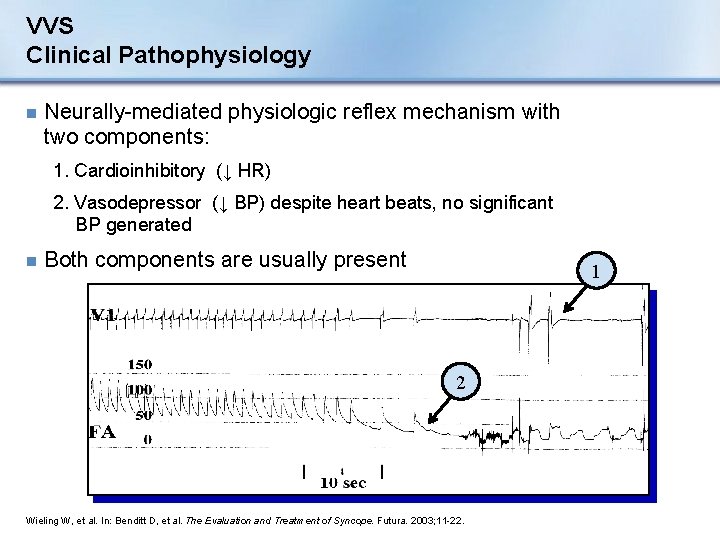
VVS Clinical Pathophysiology n Neurally-mediated physiologic reflex mechanism with two components: 1. Cardioinhibitory (↓ HR) 2. Vasodepressor (↓ BP) despite heart beats, no significant BP generated n Both components are usually present 1 2 Wieling W, et al. In: Benditt D, et al. The Evaluation and Treatment of Syncope. Futura. 2003; 11 -22.

VVS Incidence n Most common form of syncope • 8% to 37% (mean 18%) of syncope cases n Depends on population sampled • Young without SHD, ↑ incidence • Older with SHD, ↓ incidence Linzer M, et al. Ann Intern Med. 1997; 126: 989.
VVS vs. CSS n In general: • VVS patients younger than CSS patients • Ages range from adolescence to older adults (median 43 years) Linzer M, et al. Ann Intern Med. 1997; 126: 989.
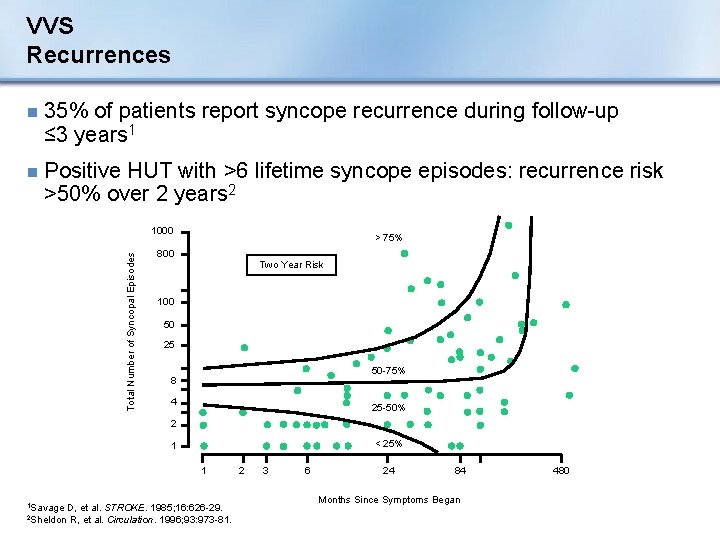
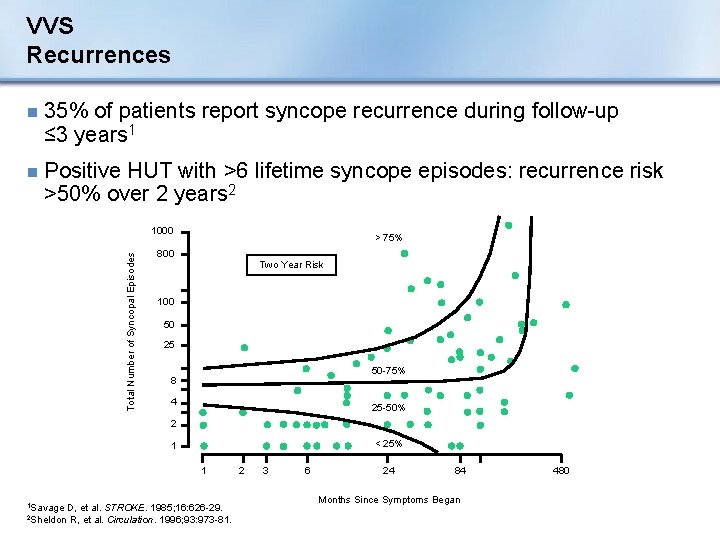
VVS Recurrences n 35% of patients report syncope recurrence during follow-up ≤ 3 years 1 n Positive HUT with >6 lifetime syncope episodes: recurrence risk >50% over 2 years 2 Total Number of Syncopal Episodes 1000 > 75% 800 Two Year Risk 100 50 25 50 -75% 8 4 25 -50% 2 < 25% 1 1 1 Savage D, et al. STROKE. 1985; 16: 626 -29. 2 Sheldon R, et al. Circulation. 1996; 93: 973 -81. 2 3 6 24 84 Months Since Symptoms Began 480
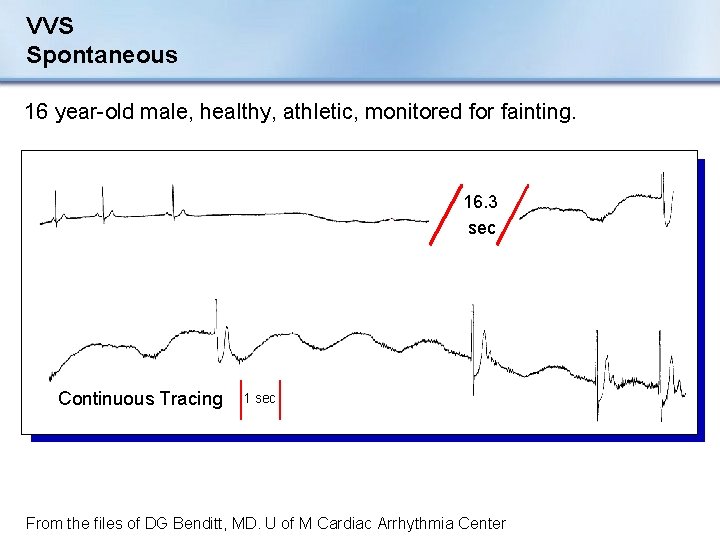
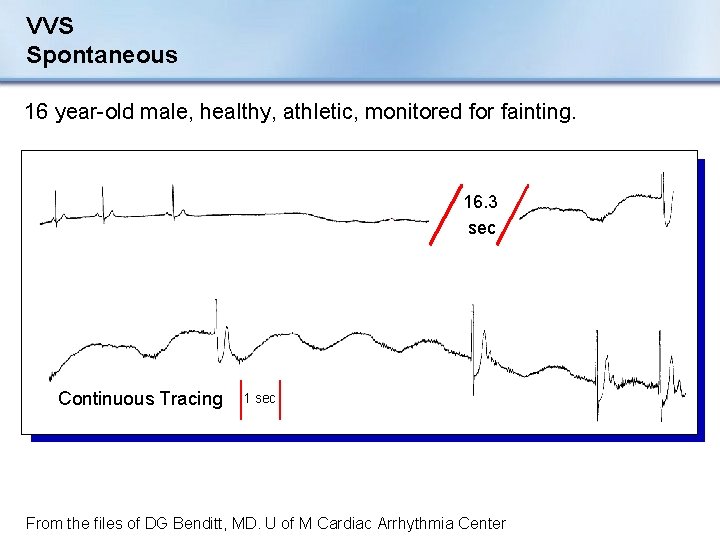
VVS Spontaneous 16 year-old male, healthy, athletic, monitored for fainting. 16. 3 sec Continuous Tracing 1 sec From the files of DG Benditt, MD. U of M Cardiac Arrhythmia Center
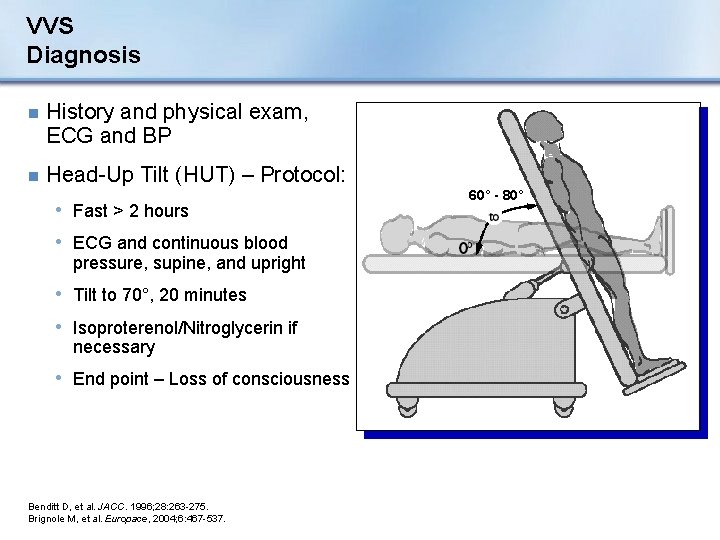
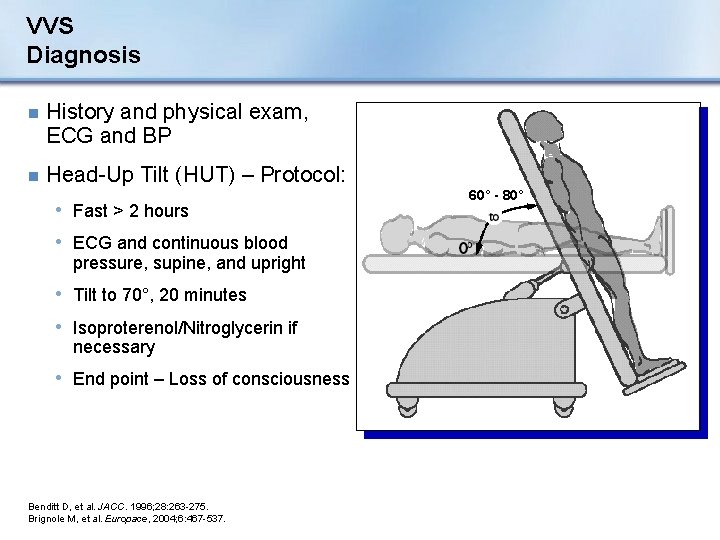
VVS Diagnosis n History and physical exam, ECG and BP n Head-Up Tilt (HUT) – Protocol: • Fast > 2 hours • ECG and continuous blood pressure, supine, and upright • Tilt to 70°, 20 minutes • Isoproterenol/Nitroglycerin if necessary • End point – Loss of consciousness Benditt D, et al. JACC. 1996; 28: 263 -275. Brignole M, et al. Europace, 2004; 6: 467 -537. 60° - 80°
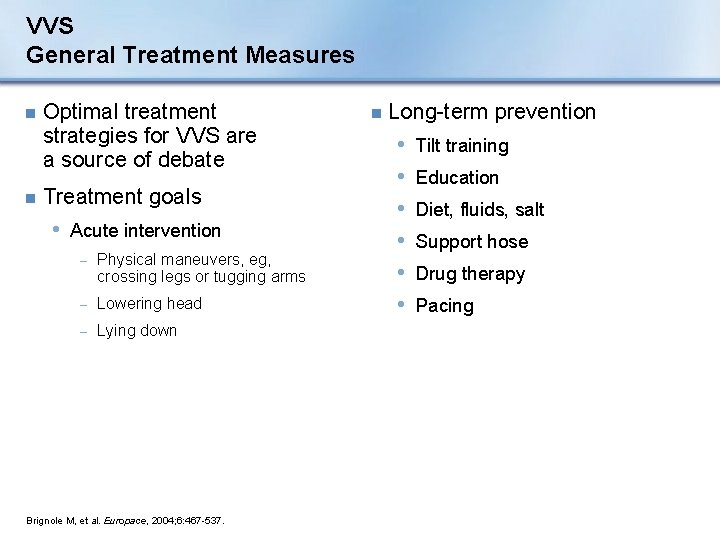
VVS General Treatment Measures n n Optimal treatment strategies for VVS are a source of debate Treatment goals • Acute intervention − Physical maneuvers, eg, crossing legs or tugging arms − Lowering head − Lying down Brignole M, et al. Europace, 2004; 6: 467 -537. n Long-term prevention • • • Tilt training Education Diet, fluids, salt Support hose Drug therapy Pacing
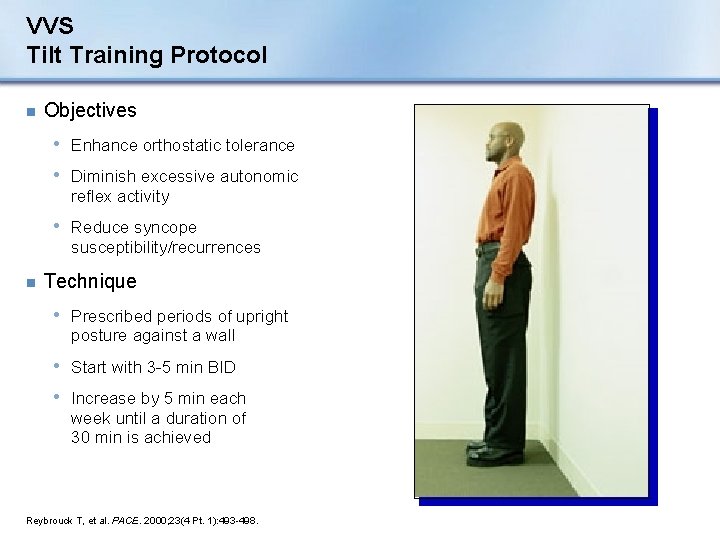
VVS Tilt Training Protocol n Objectives • Enhance orthostatic tolerance • Diminish excessive autonomic reflex activity • Reduce syncope susceptibility/recurrences n Technique • Prescribed periods of upright posture against a wall • Start with 3 -5 min BID • Increase by 5 min each week until a duration of 30 min is achieved Reybrouck T, et al. PACE. 2000; 23(4 Pt. 1): 493 -498.
VVS Tilt Training: Clinical Outcomes n Treatment of recurrent VVS n Reybrouck, et al. *: Long-term study • 38 patients performed home tilt training • After a period of regular tilt training, 82% remained free of syncope during the follow-up period • However, at the 43 -month follow-up, 29 patients had therapy • Conclusion: The abnormal autonomic reflex activity of VVS can be remedied. Compliance may be an issue. *Reybrouck T, et al. PACE. 2000; 23: 493 -498. abandoned
VVS Tilt Training: Clinical Outcomes n Foglia-Manzillo, et al. *: Short-term study • 68 patients • • – 35 tilt training – 33 no treatment (control) Tilt table test conducted after 3 weeks 19 (59%) of tilt trained and 18 (60%) of controls had a positive test Tilt training was not effective in reducing tilt testing positivity rate Poor compliance in the majority of patients with recurrent VVS *Foglio-Manzillo G, et al. Europace. 2004; 6: 199 -204.
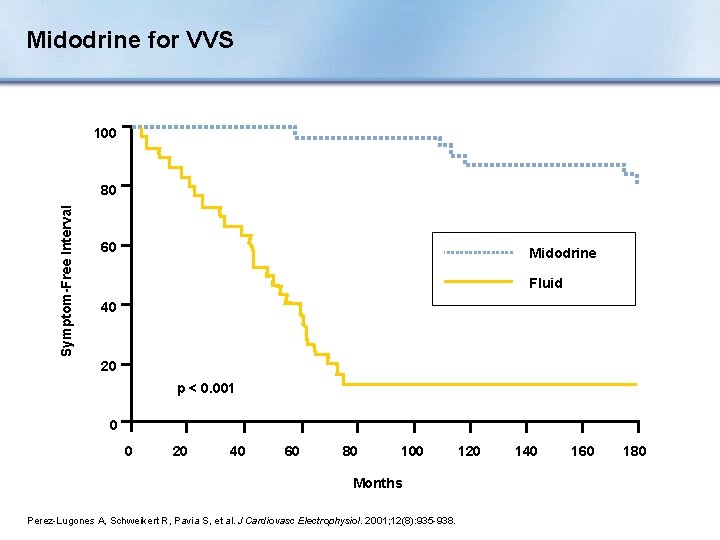
VVS Pharmacologic Treatment n Fludrocortisone n Beta-adrenergic blockers • Preponderance of clinical evidence suggests minimal benefit 1 n SSRI (Selective Serotonin Re-Uptake Inhibitor) • 1 small controlled trial 2 n Vasoconstrictors • 1 negative controlled trial (etilefrine)3 • 2 positive controlled trials (midodrine)4, 5 1 Brignole M, et al. Europace, 2004; 6: 467 -537. Girolamo E, et al. JACC. 1999; 33: 1227 -1230. 3 Raviele A, et al. Circ. 1999; 99: 1452 -1457. 2 Di 4 Ward C, et al. Heart. 1998; 79: 45 -49. A, et al. J Cardiovasc Electrophysiol. 2001; 12(8): 935 -938. 5 Perez-Lugones
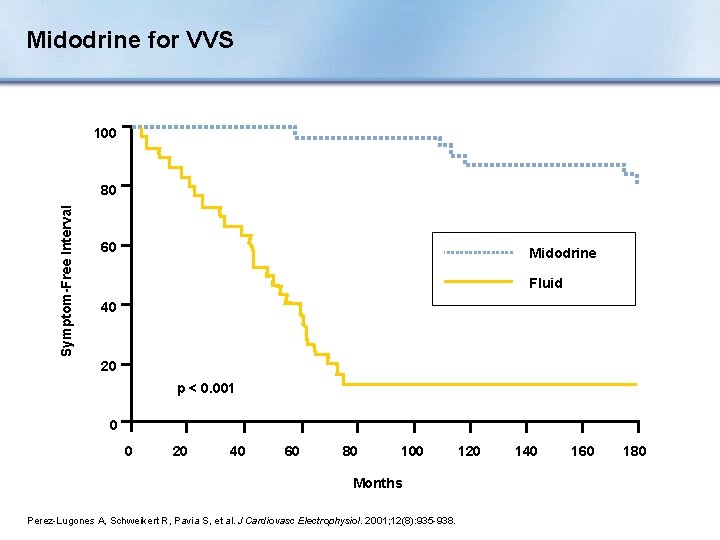
Midodrine for VVS 100 Symptom-Free Interval 80 60 Midodrine Fluid 40 20 p < 0. 001 0 0 20 40 60 80 100 Months Perez-Lugones A, Schweikert R, Pavia S, et al. J Cardiovasc Electrophysiol. 2001; 12(8): 935 -938. 120 140 160 180
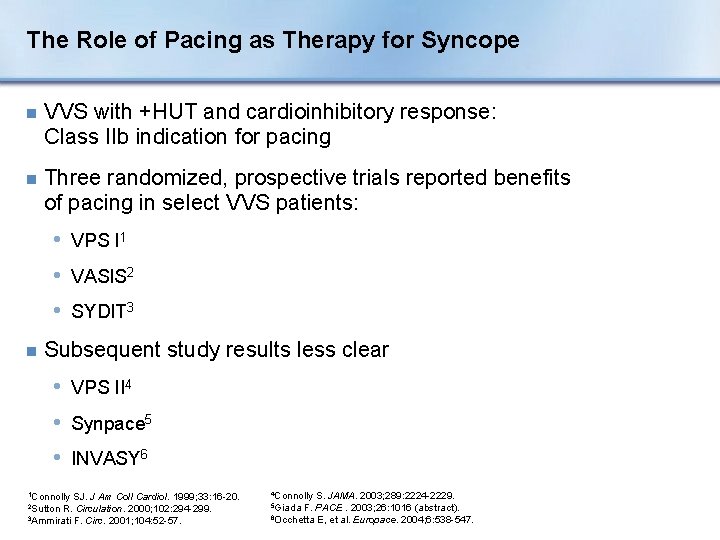
The Role of Pacing as Therapy for Syncope n VVS with +HUT and cardioinhibitory response: Class IIb indication for pacing n Three randomized, prospective trials reported benefits of pacing in select VVS patients: • VPS I 1 • VASIS 2 • SYDIT 3 n Subsequent study results less clear • VPS II 4 • Synpace 5 • INVASY 6 1 Connolly SJ. J Am Coll Cardiol. 1999; 33: 16 -20. 2 Sutton R. Circulation. 2000; 102: 294 -299. 3 Ammirati F. Circ. 2001; 104: 52 -57. 4 Connolly S. JAMA. 2003; 289: 2224 -2229. F. PACE. 2003; 26: 1016 (abstract). 6 Occhetta E, et al. Europace. 2004; 6: 538 -547. 5 Giada
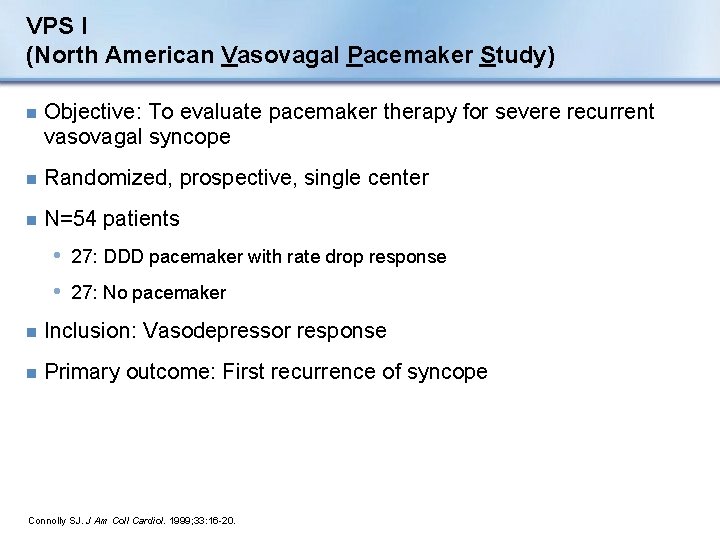
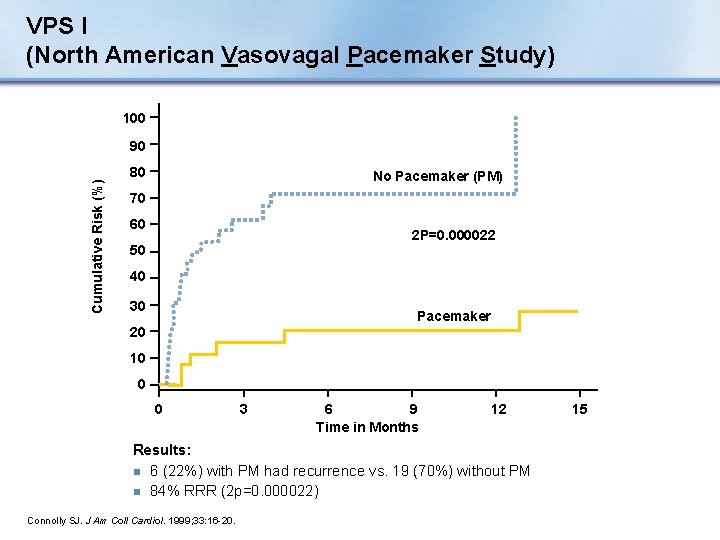
VPS I (North American Vasovagal Pacemaker Study) n Objective: To evaluate pacemaker therapy for severe recurrent vasovagal syncope n Randomized, prospective, single center n N=54 patients • 27: DDD pacemaker with rate drop response • 27: No pacemaker n Inclusion: Vasodepressor response n Primary outcome: First recurrence of syncope Connolly SJ. J Am Coll Cardiol. 1999; 33: 16 -20.
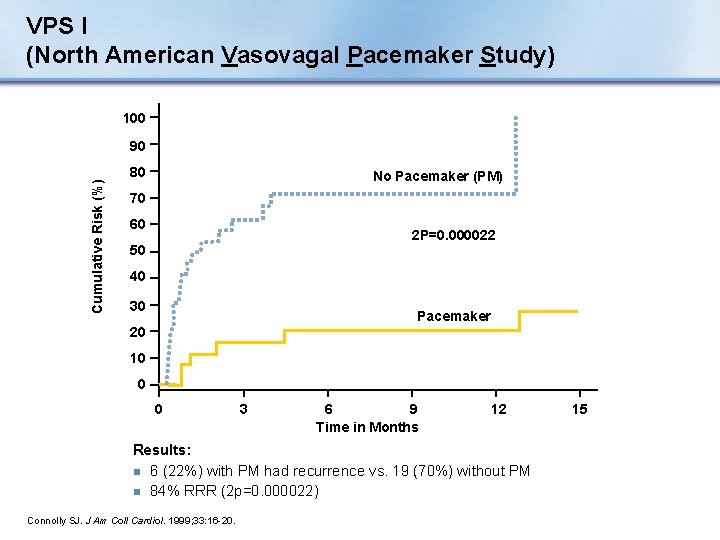
VPS I (North American Vasovagal Pacemaker Study) 100 Cumulative Risk (%) 90 80 No Pacemaker (PM) 70 60 2 P=0. 000022 50 40 30 Pacemaker 20 10 0 0 3 6 9 Time in Months 12 Results: n 6 (22%) with PM had recurrence vs. 19 (70%) without PM n 84% RRR (2 p=0. 000022) Connolly SJ. J Am Coll Cardiol. 1999; 33: 16 -20. 15
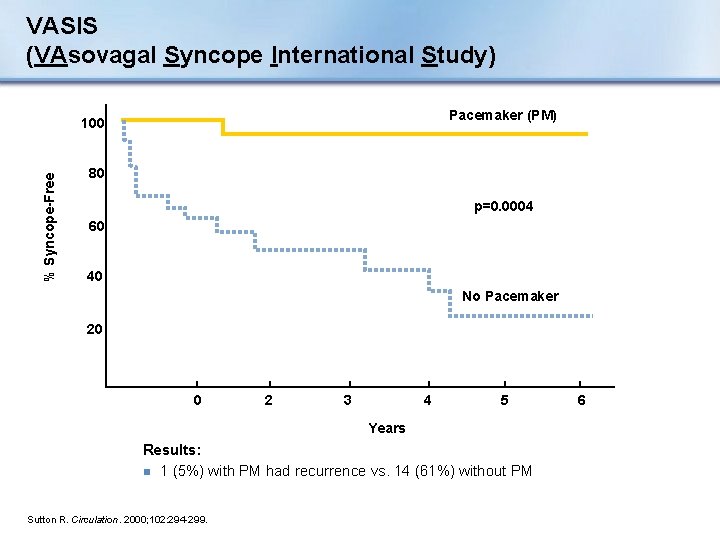
VASIS (VAsovagal Syncope International Study) n Objective: To evaluate pacemaker therapy for severe cardioinhibitory tilt-positive neurally mediated syncope n Randomized, prospective, multi-center n N=42 patients • 19: DDI pacemaker (80 bpm) with rate hysteresis (45 bpm) • 23: No pacemaker n Inclusion: Positive cardioinhibitory response n Primary outcome: First recurrence of syncope Sutton R. Circulation. 2000; 102: 294 -299.
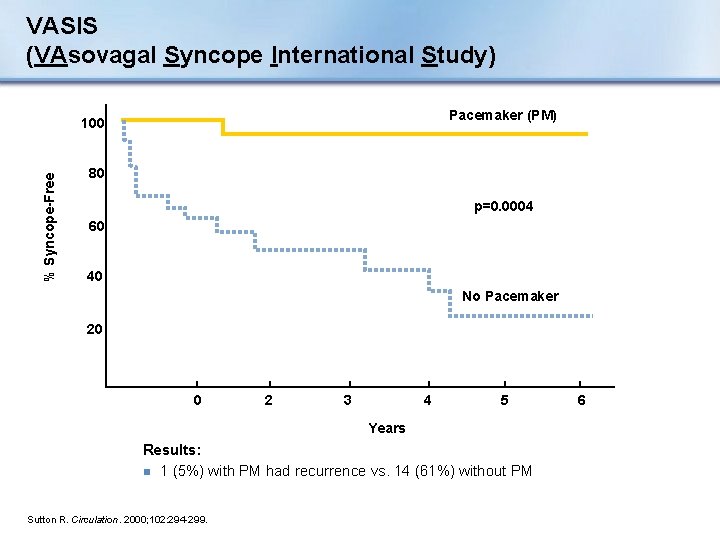
VASIS (VAsovagal Syncope International Study) Pacemaker (PM) % Syncope-Free 100 80 p=0. 0004 60 40 No Pacemaker 20 0 2 3 4 5 Years Results: n 1 (5%) with PM had recurrence vs. 14 (61%) without PM Sutton R. Circulation. 2000; 102: 294 -299. 6
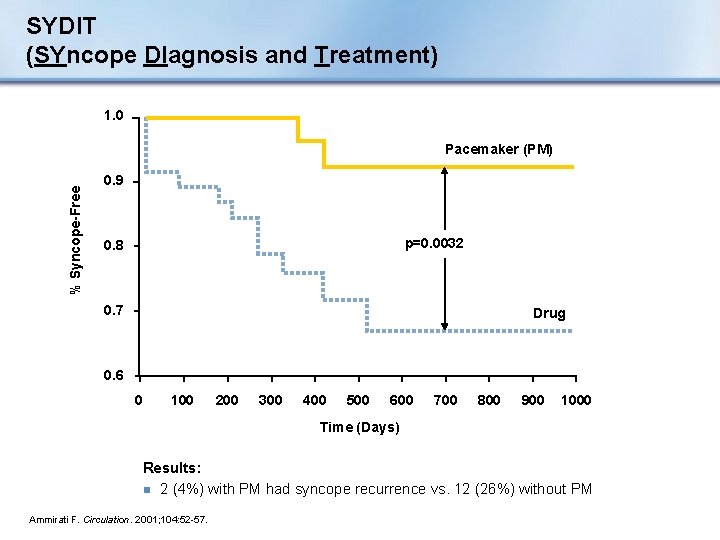
SYDIT (SYncope DIagnosis and Treatment) n Objective: To compare the effects of cardiac pacing with pharmacological therapy in patients with recurrent vasovagal syncope n Randomized, prospective, multi-center n N=93 patients • 46: DDD pacemaker with rate drop response • 47: Atenolol 100 mg/d n Inclusion: Positive HUT with relative bradycardia n Primary outcome: First recurrence of syncope Ammirati F. Circulation. 2001; 104: 52 -57.
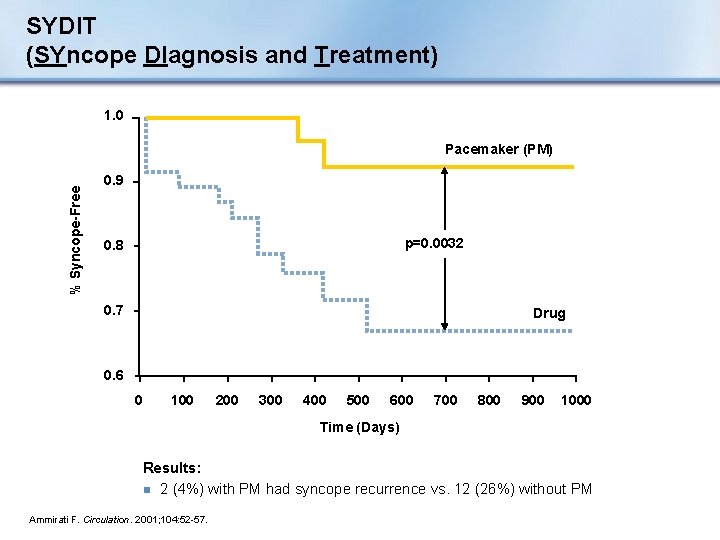
SYDIT (SYncope DIagnosis and Treatment) 1. 0 % Syncope-Free Pacemaker (PM) 0. 9 p=0. 0032 0. 8 0. 7 Drug 0. 6 0 100 200 300 400 500 600 700 800 900 1000 Time (Days) Results: n 2 (4%) with PM had syncope recurrence vs. 12 (26%) without PM Ammirati F. Circulation. 2001; 104: 52 -57.
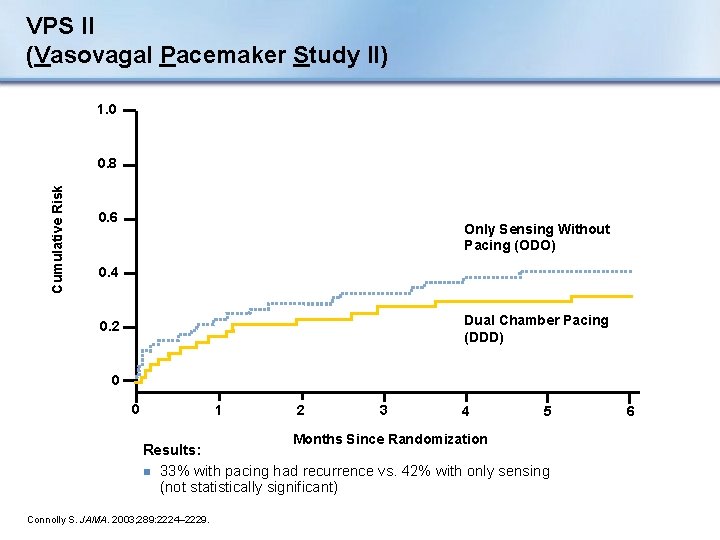
VPS II (Vasovagal Pacemaker Study II) n Objective: To determine if pacing therapy reduces the risk of syncope in patients with vasovagal syncope n Randomized, double-blind, prospective, multi-center n N=100 patients • 52: Only sensing without pacing • 48: DDD pacemaker with rate drop response n Inclusion: Positive HUT with (HRx. BP) < 6000/min x mm Hg n Primary outcome: First recurrence of syncope Connolly S. JAMA. 2003; 289: 2224 -2229.
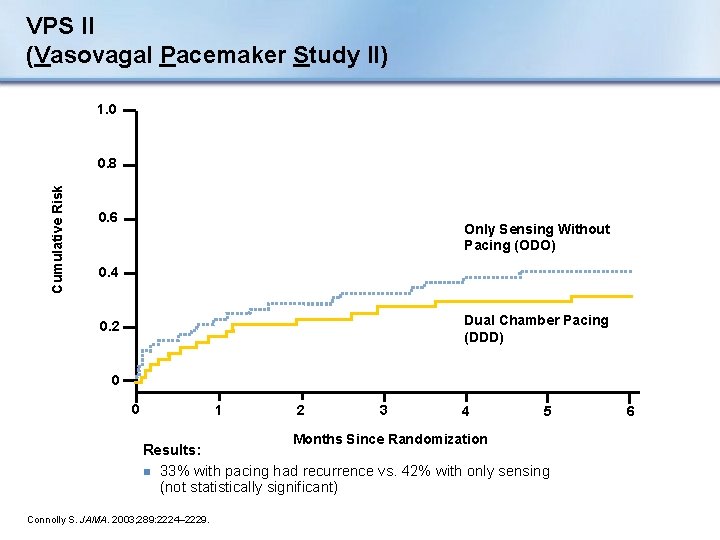
VPS II (Vasovagal Pacemaker Study II) 1. 0 Cumulative Risk 0. 8 0. 6 Only Sensing Without Pacing (ODO) 0. 4 Dual Chamber Pacing (DDD) 0. 2 0 0 1 2 3 4 Months Since Randomization 5 Results: n 33% with pacing had recurrence vs. 42% with only sensing (not statistically significant) Connolly S. JAMA. 2003; 289: 2224– 2229. 6
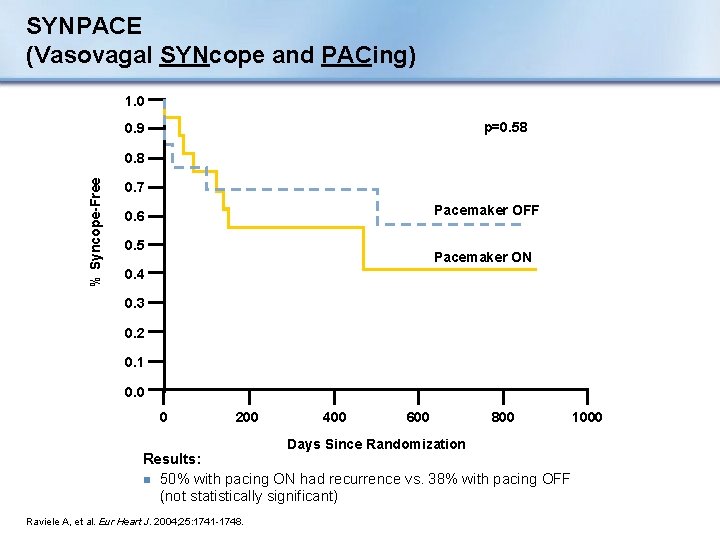
SYNPACE (Vasovagal SYNcope and PACing) n Objective: To determine if pacing therapy will reduce syncope relapses in patients with recurrent vasovagal syncope, compared to those with a pacemaker programmed to OFF n Randomized, double-blind, prospective, multi-center, placebo-controlled n N=29 patients • 16: DDD PM with rate drop response programmed ON • 13: PM programmed OFF (OOO mode) n Inclusion: Recurrent VVS and +HUT with asystolic or mixed response n Primary outcome: First recurrence of syncope Raviele A. . Europace. 2001; 3: 336– 341. Raviele A, et al. Eur Heart J. 2004; 25: 1741 -1748.
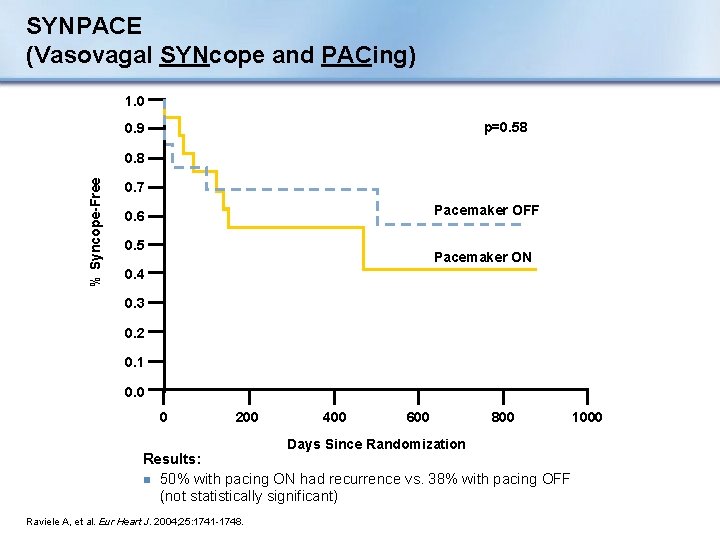
SYNPACE (Vasovagal SYNcope and PACing) 1. 0 p=0. 58 0. 9 % Syncope-Free 0. 8 0. 7 Pacemaker OFF 0. 6 0. 5 Pacemaker ON 0. 4 0. 3 0. 2 0. 1 0. 0 0 200 400 600 Days Since Randomization 800 Results: n 50% with pacing ON had recurrence vs. 38% with pacing OFF (not statistically significant) Raviele A, et al. Eur Heart J. 2004; 25: 1741 -1748. 1000
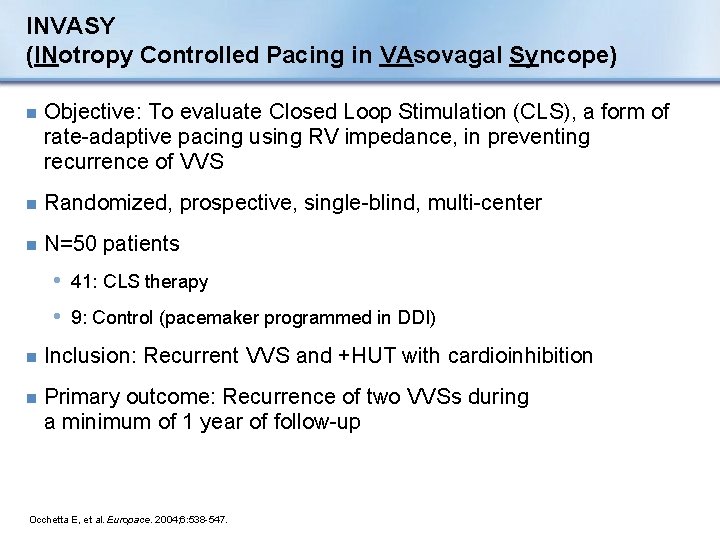
INVASY (INotropy Controlled Pacing in VAsovagal Syncope) n Objective: To evaluate Closed Loop Stimulation (CLS), a form of rate-adaptive pacing using RV impedance, in preventing recurrence of VVS n Randomized, prospective, single-blind, multi-center n N=50 patients • 41: CLS therapy • 9: Control (pacemaker programmed in DDI) n Inclusion: Recurrent VVS and +HUT with cardioinhibition n Primary outcome: Recurrence of two VVSs during a minimum of 1 year of follow-up Occhetta E, et al. Europace. 2004; 6: 538 -547.
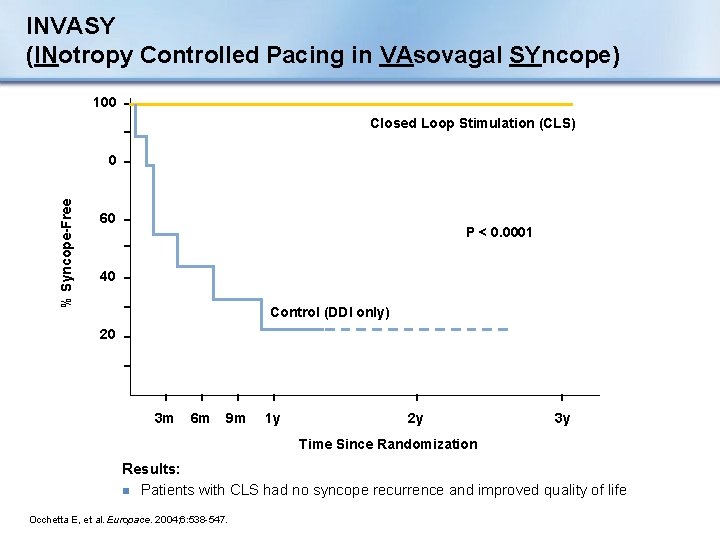
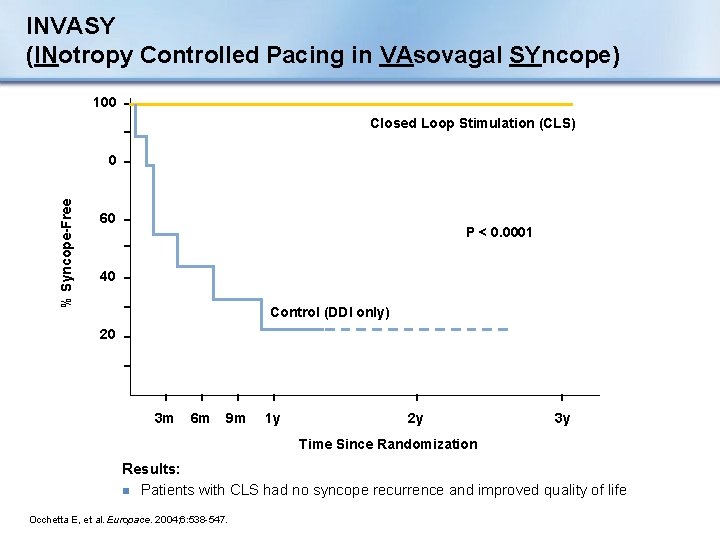
INVASY (INotropy Controlled Pacing in VAsovagal SYncope) 100 Closed Loop Stimulation (CLS) % Syncope-Free 0 60 P < 0. 0001 40 Control (DDI only) 20 3 m 6 m 9 m 1 y 2 y 3 y Time Since Randomization Results: n Patients with CLS had no syncope recurrence and improved quality of life Occhetta E, et al. Europace. 2004; 6: 538 -547.
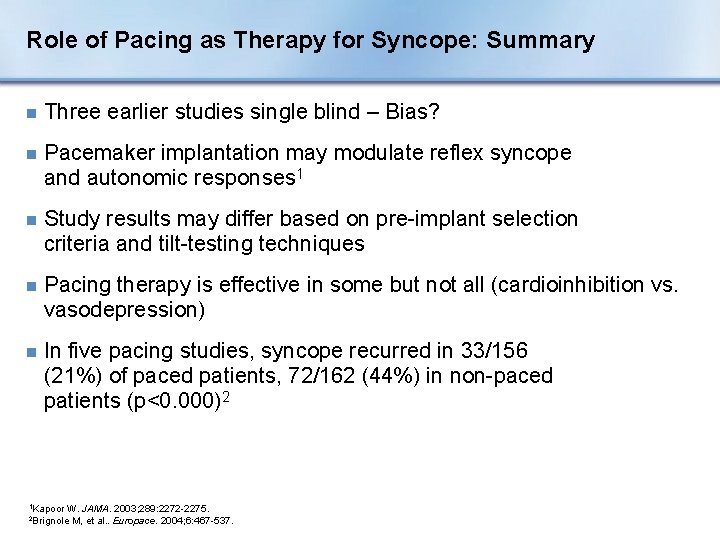
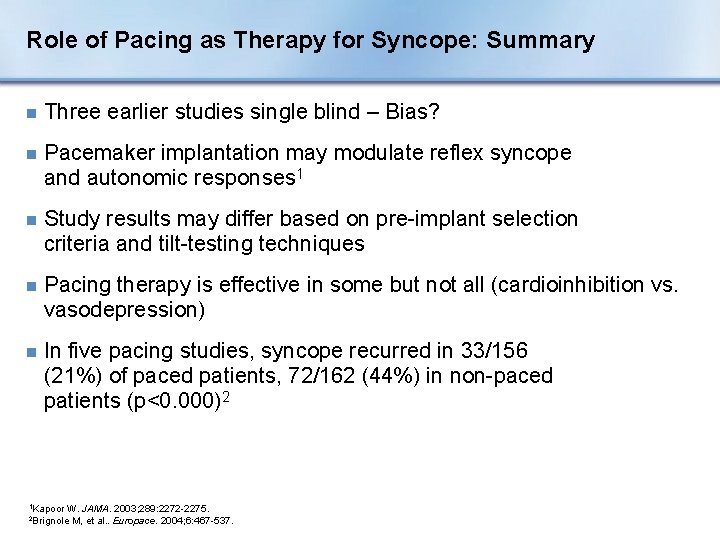
Role of Pacing as Therapy for Syncope: Summary n Three earlier studies single blind – Bias? n Pacemaker implantation may modulate reflex syncope and autonomic responses 1 n Study results may differ based on pre-implant selection criteria and tilt-testing techniques n Pacing therapy is effective in some but not all (cardioinhibition vs. vasodepression) n In five pacing studies, syncope recurred in 33/156 (21%) of paced patients, 72/162 (44%) in non-paced patients (p<0. 000)2 1 Kapoor W. JAMA. 2003; 289: 2272 -2275. M, et al. . Europace. 2004; 6: 467 -537. 2 Brignole
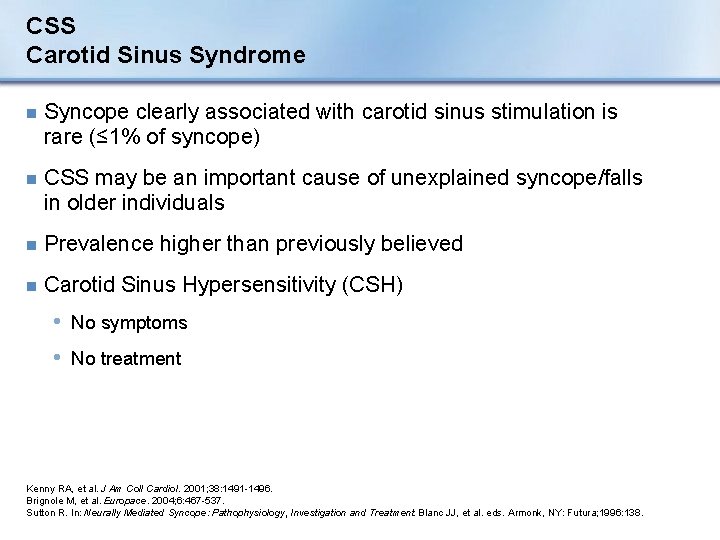
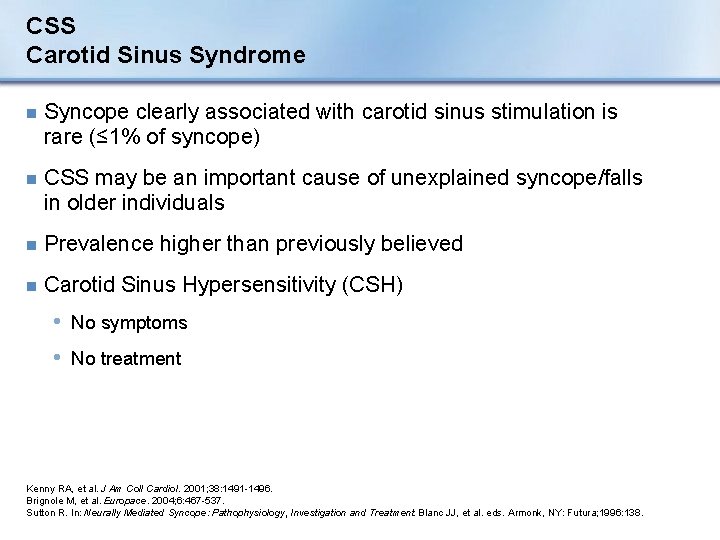
CSS Carotid Sinus Syndrome n Syncope clearly associated with carotid sinus stimulation is rare (≤ 1% of syncope) n CSS may be an important cause of unexplained syncope/falls in older individuals n Prevalence higher than previously believed n Carotid Sinus Hypersensitivity (CSH) • No symptoms • No treatment Kenny RA, et al. J Am Coll Cardiol. 2001; 38: 1491 -1496. Brignole M, et al. Europace. 2004; 6: 467 -537. Sutton R. In: Neurally Mediated Syncope: Pathophysiology, Investigation and Treatment. Blanc JJ, et al. eds. Armonk, NY: Futura; 1996: 138.
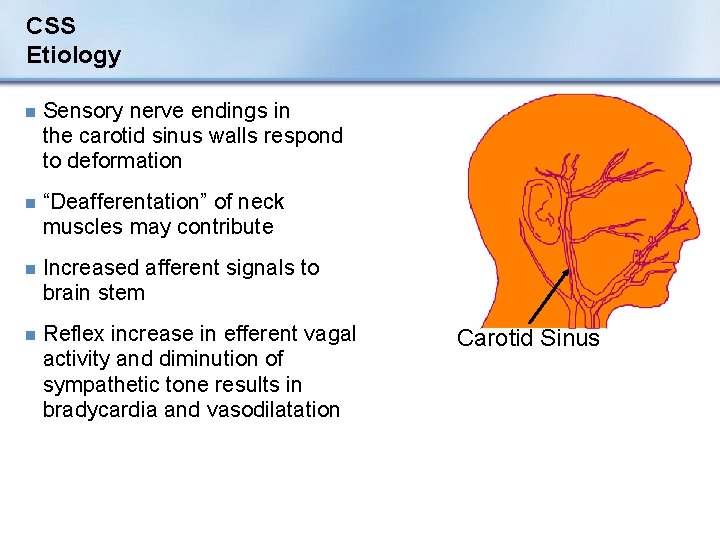
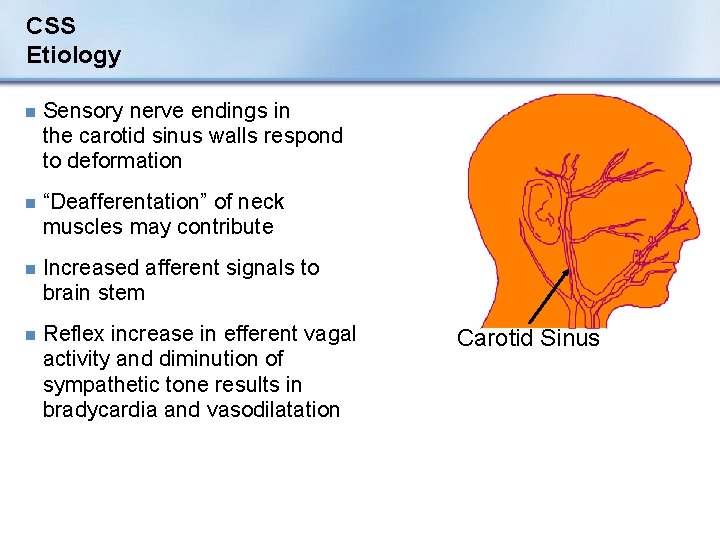
CSS Etiology n Sensory nerve endings in the carotid sinus walls respond to deformation n “Deafferentation” of neck muscles may contribute n Increased afferent signals to brain stem n Reflex increase in efferent vagal activity and diminution of sympathetic tone results in bradycardia and vasodilatation Carotid Sinus
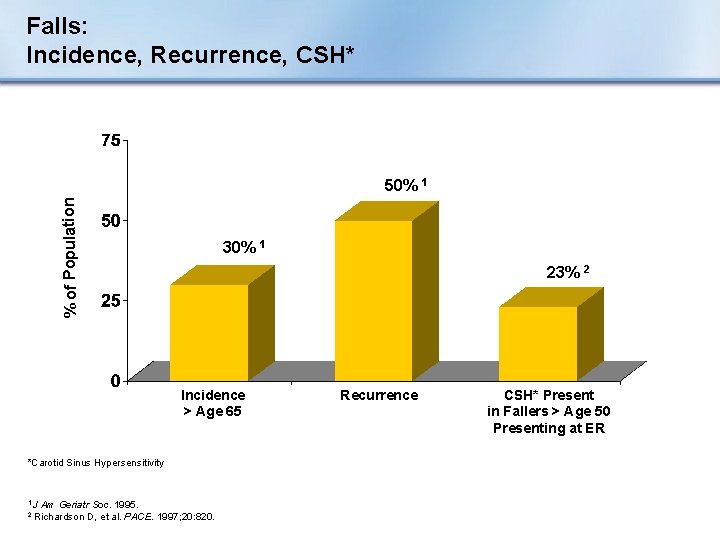
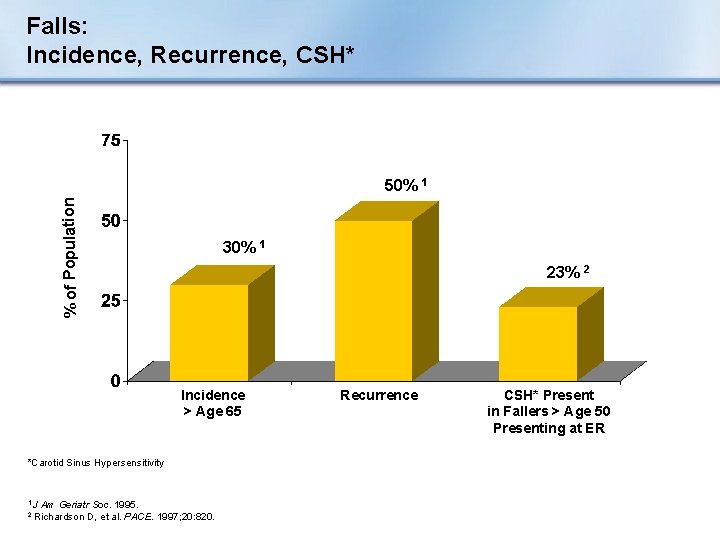
Falls: Incidence, Recurrence, CSH* % of Population 50% 1 30% 1 23% 2 Incidence > Age 65 *Carotid Sinus Hypersensitivity 1 J 2 Am Geriatr Soc. 1995. Richardson D, et al. PACE. 1997; 20: 820. Recurrence CSH* Present in Fallers > Age 50 Presenting at ER
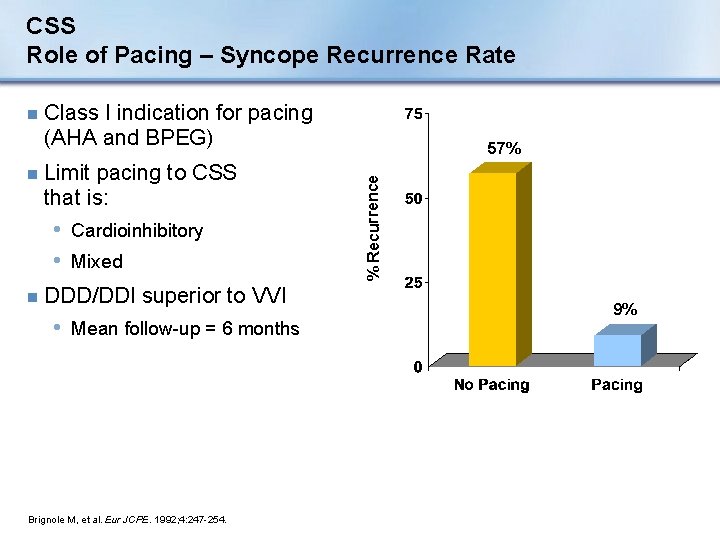
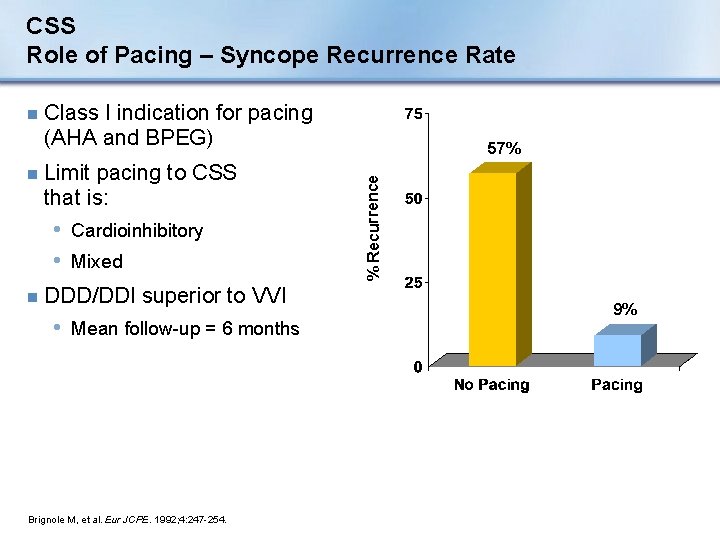
CSS Role of Pacing – Syncope Recurrence Rate Limit pacing to CSS that is: • Cardioinhibitory • Mixed n DDD/DDI superior to VVI • Mean follow-up = 6 months Brignole M, et al. Eur JCPE. 1992; 4: 247 -254. 57% % Recurrence n Class I indication for pacing (AHA and BPEG) %6 n
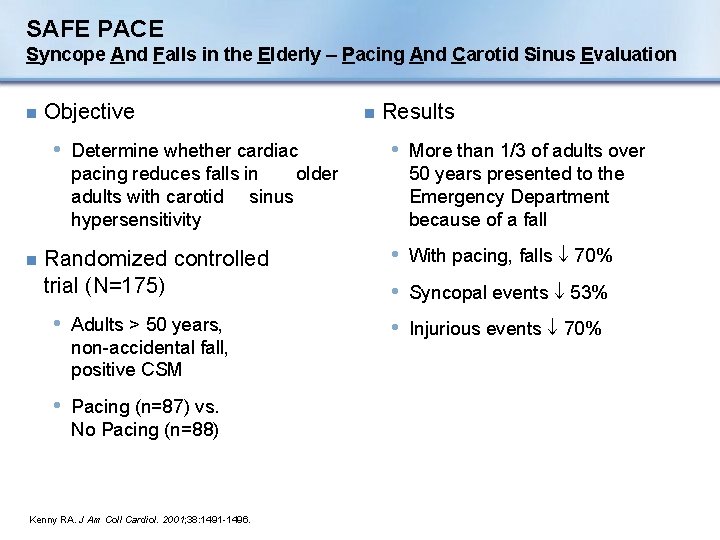
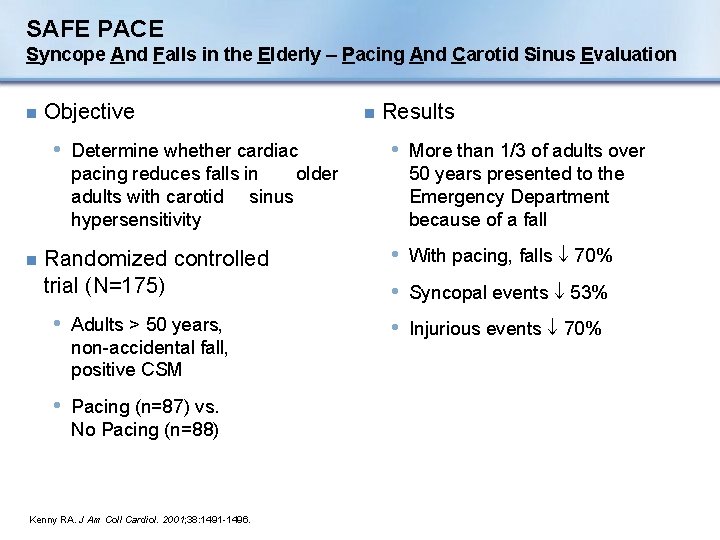
SAFE PACE Syncope And Falls in the Elderly – Pacing And Carotid Sinus Evaluation n Objective • Determine whether cardiac pacing reduces falls in older adults with carotid sinus hypersensitivity n Randomized controlled trial (N=175) • Adults > 50 years, non-accidental fall, positive CSM • Pacing (n=87) vs. No Pacing (n=88) Kenny RA. J Am Coll Cardiol. 2001; 38: 1491 -1496. n Results • More than 1/3 of adults over 50 years presented to the Emergency Department because of a fall • With pacing, falls 70% • Syncopal events 53% • Injurious events 70%
SAFE PACE n Conclusions • Strong association between non-accidental falls and cardioinhibitory CSH • These patients usually not referred for cardiac assessment • Cardiac pacing significantly reduced subsequent falls • CSH should be considered in all older adults who have non-accidental falls Kenny RA, J Am Coll Cardiol. 2001; 38: 1491 -1496.
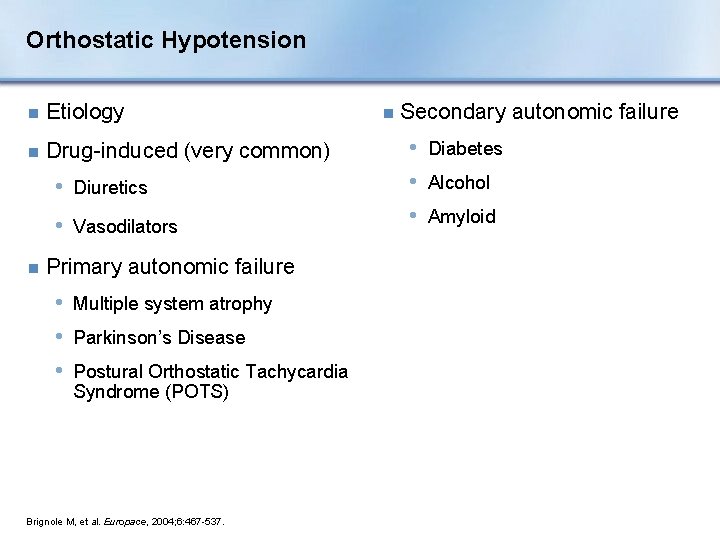
Orthostatic Hypotension n Etiology n Drug-induced (very common) • Diuretics • Vasodilators n Primary autonomic failure • Multiple system atrophy • Parkinson’s Disease • Postural Orthostatic Tachycardia Syndrome (POTS) Brignole M, et al. Europace, 2004; 6: 467 -537. n Secondary autonomic failure • Diabetes • Alcohol • Amyloid
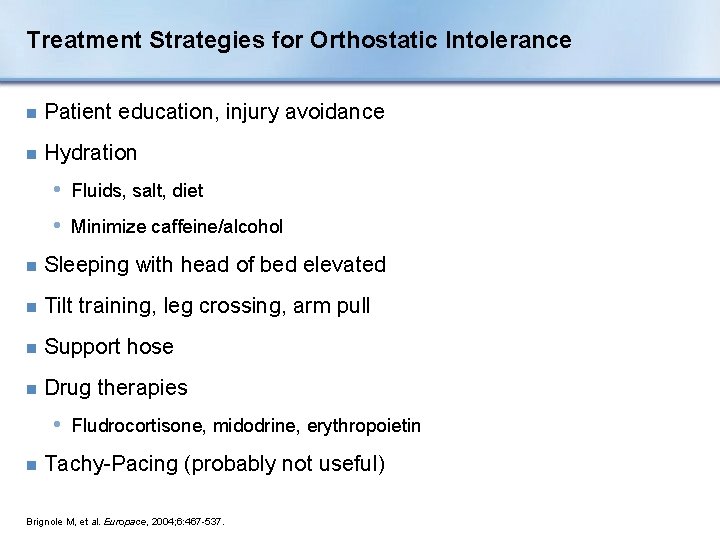
Treatment Strategies for Orthostatic Intolerance n Patient education, injury avoidance n Hydration • Fluids, salt, diet • Minimize caffeine/alcohol n Sleeping with head of bed elevated n Tilt training, leg crossing, arm pull n Support hose n Drug therapies • Fludrocortisone, midodrine, erythropoietin n Tachy-Pacing (probably not useful) Brignole M, et al. Europace, 2004; 6: 467 -537.
Section IV: Special Issues
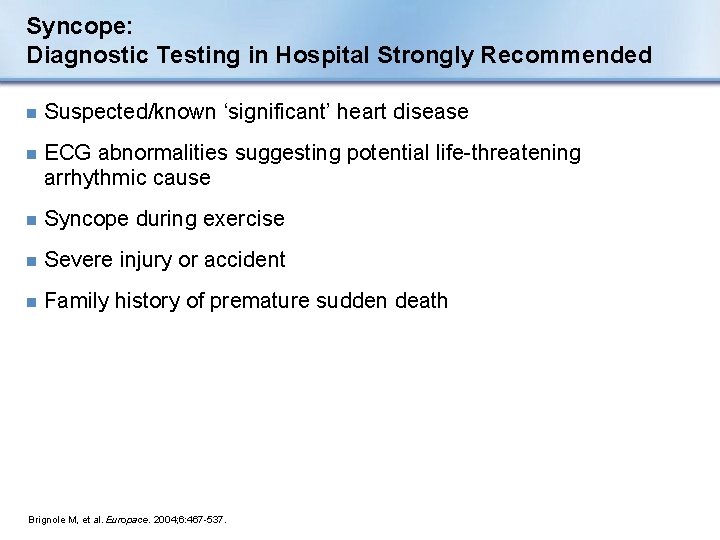
Syncope: Diagnostic Testing in Hospital Strongly Recommended n Suspected/known ‘significant’ heart disease n ECG abnormalities suggesting potential life-threatening arrhythmic cause n Syncope during exercise n Severe injury or accident n Family history of premature sudden death Brignole M, et al. Europace. 2004; 6: 467 -537.
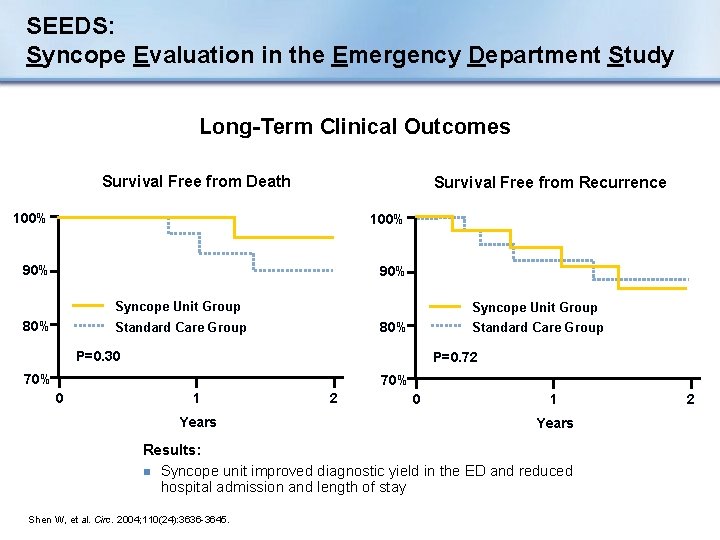
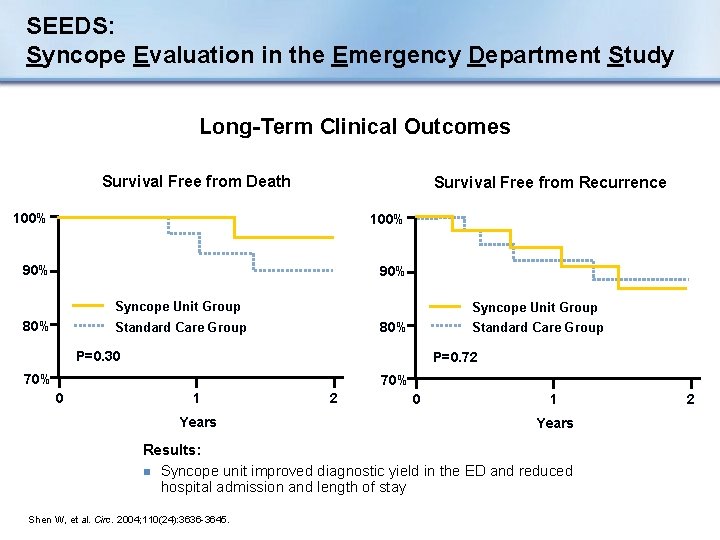
SEEDS: Syncope Evaluation in the Emergency Department Study Long-Term Clinical Outcomes Survival Free from Death Survival Free from Recurrence 100% 90% Syncope Unit Group 80% Standard Care Group P=0. 30 P=0. 72 70% 0 1 Years 2 0 1 Years Results: n Syncope unit improved diagnostic yield in the ED and reduced hospital admission and length of stay Shen W, et al. Circ. 2004; 110(24): 3636 -3645. 2
The Integrated Syncope Unit n To optimize the effectiveness of the evaluation and treatment of syncope patients at a given center n Best accomplished by: • Cohesive, structured care pathway • Multidisciplinary approach • Core equipment available • Preferential access to other tests or therapy n Majority of syncope evaluations – Out-patient or day cases 1 Kenny RA, Brignole M. In: Benditt D, et al. eds. The Evaluation and Treatment of Syncope. Futura; 2003: 55 -60. M, et al. Europace, 2004; 6: 467 -537. 2 Brignole
Conclusion n Syncope is a common symptom with many causes n Deserves thorough investigation and appropriate treatment n A disciplined approach is essential n ESC guidelines offer current best practices Brignole M, et al. Europace, 2004; 6: 467 -537.
Challenges of Syncope n Cost n Quality of life implications n Diagnosis and treatment • Diagnostic yield and repeatability of tests • Frequency and clustering of events • Difficulty in managing/treating/controlling future events • Appropriate risk stratification • Complex etiology Olshansky B. In: Grubb B and Olshansky B. eds. Syncope: Mechanisms and Management. Futura. 1998: 15 -71. Brignole M, et al. Europace, 2004; 6: 467 -537.
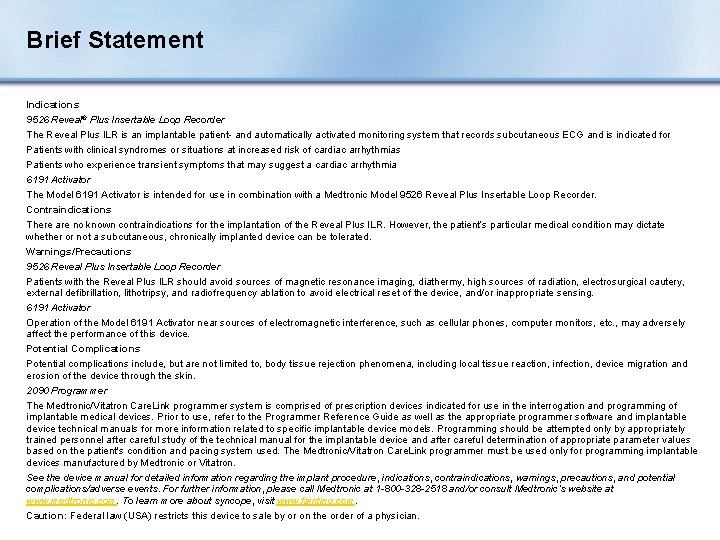
Brief Statement Indications 9526 Reveal® Plus Insertable Loop Recorder The Reveal Plus ILR is an implantable patient- and automatically activated monitoring system that records subcutaneous ECG and is indicated for Patients with clinical syndromes or situations at increased risk of cardiac arrhythmias Patients who experience transient symptoms that may suggest a cardiac arrhythmia 6191 Activator The Model 6191 Activator is intended for use in combination with a Medtronic Model 9526 Reveal Plus Insertable Loop Recorder. Contraindications There are no known contraindications for the implantation of the Reveal Plus ILR. However, the patient’s particular medical condition may dictate whether or not a subcutaneous, chronically implanted device can be tolerated. Warnings/Precautions 9526 Reveal Plus Insertable Loop Recorder Patients with the Reveal Plus ILR should avoid sources of magnetic resonance imaging, diathermy, high sources of radiation, electrosurgical cautery, external defibrillation, lithotripsy, and radiofrequency ablation to avoid electrical reset of the device, and/or inappropriate sensing. 6191 Activator Operation of the Model 6191 Activator near sources of electromagnetic interference, such as cellular phones, computer monitors, etc. , may adversely affect the performance of this device. Potential Complications Potential complications include, but are not limited to, body tissue rejection phenomena, including local tissue reaction, infection, device migration and erosion of the device through the skin. 2090 Programmer The Medtronic/Vitatron Care. Link programmer system is comprised of prescription devices indicated for use in the interrogation and programming of implantable medical devices. Prior to use, refer to the Programmer Reference Guide as well as the appropriate programmer software and implantable device technical manuals for more information related to specific implantable device models. Programming should be attempted only by appropriately trained personnel after careful study of the technical manual for the implantable device and after careful determination of appropriate parameter values based on the patient's condition and pacing system used. The Medtronic/Vitatron Care. Link programmer must be used only for programming implantable devices manufactured by Medtronic or Vitatron. See the device manual for detailed information regarding the implant procedure, indications, contraindications, warnings, precautions, and potential complications/adverse events. For further information, please call Medtronic at 1 -800 -328 -2518 and/or consult Medtronic’s website at www. medtronic. com. To learn more about syncope, visit www. fainting. com. Caution: Federal law (USA) restricts this device to sale by or on the order of a physician.