SymptoThermal Method of Natural Family Planning 2003 Northwest



- Slides: 39
Sympto-Thermal Method of Natural Family Planning © 2003, Northwest Family Services. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any electronic or mechanical or any other method, including photography, recording, or any information s retrieval system now known or to be invented, without written permission of the publisher.
Session One • Basic Reproductive Anatomy and Physiology • The Menstrual Cycle as a Whole • Charting the Waking Temperature • Evaluating the Temperature Pattern • Charting the Cervical Mucus by Tissue and Sensation • Setting Peak Day
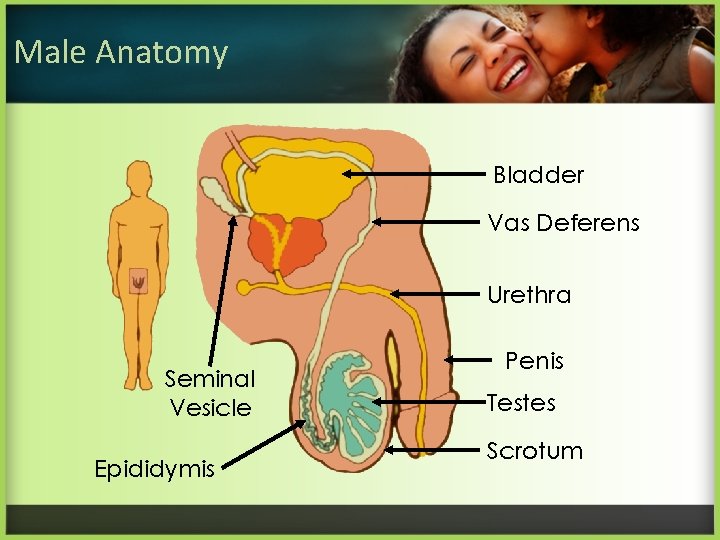
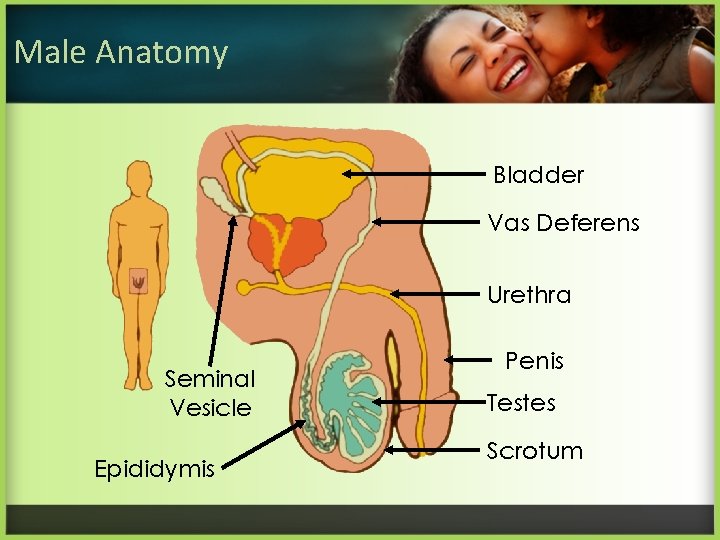
Male Anatomy Bladder Vas Deferens Urethra Seminal Vesicle Epididymis Penis Testes Scrotum

Male Fertility Sperm found in the epididymis Sperm in transit
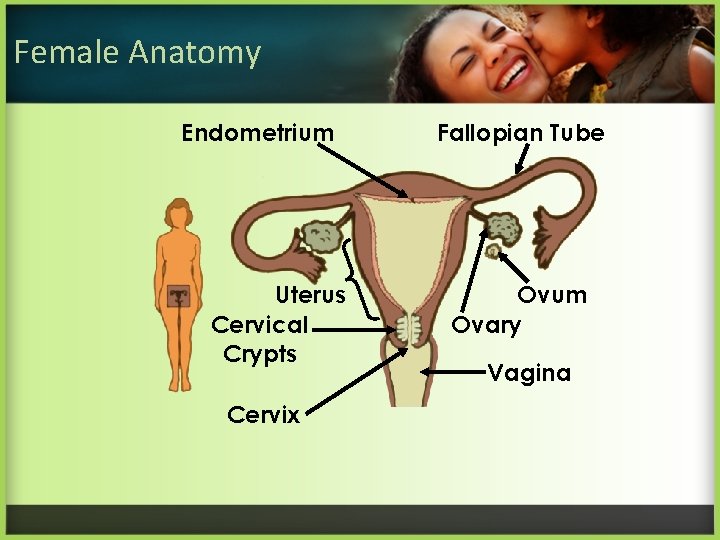
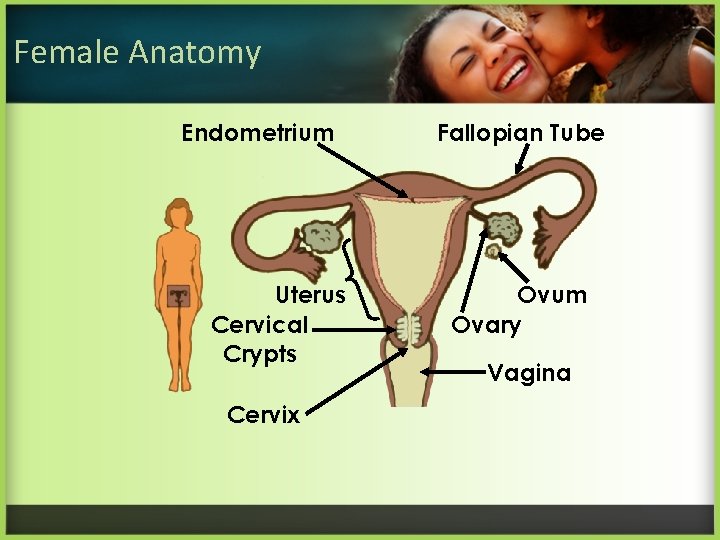
Female Anatomy Endometrium Uterus Cervical Crypts Cervix Fallopian Tube Ovum Ovary Vagina

Female Fertility Egg cell at ovulation Egg cell traveling in the fallopian tube
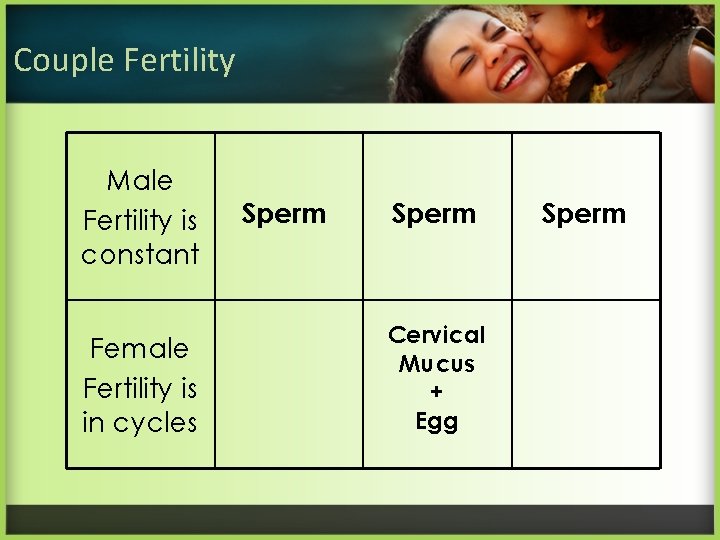
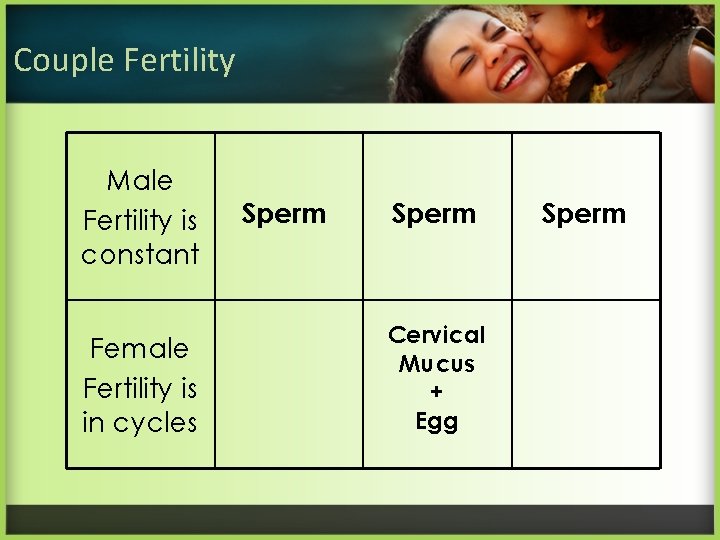
Couple Fertility Male Fertility is constant Female Fertility is in cycles Sperm Cervical Mucus + Egg Sperm
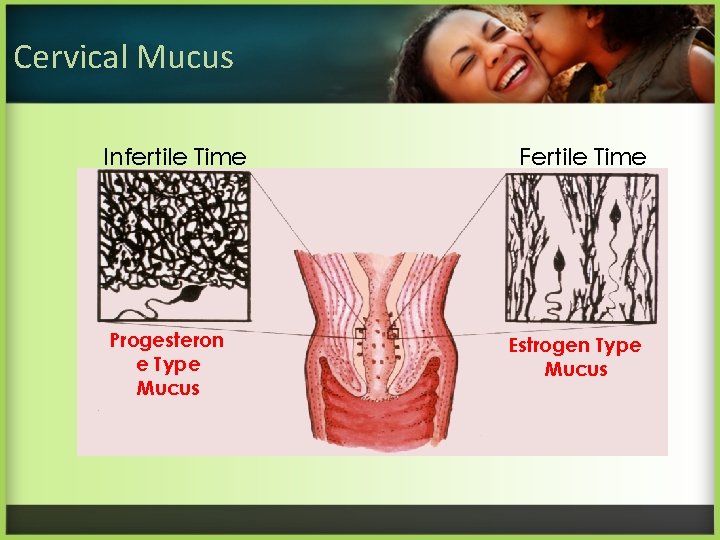
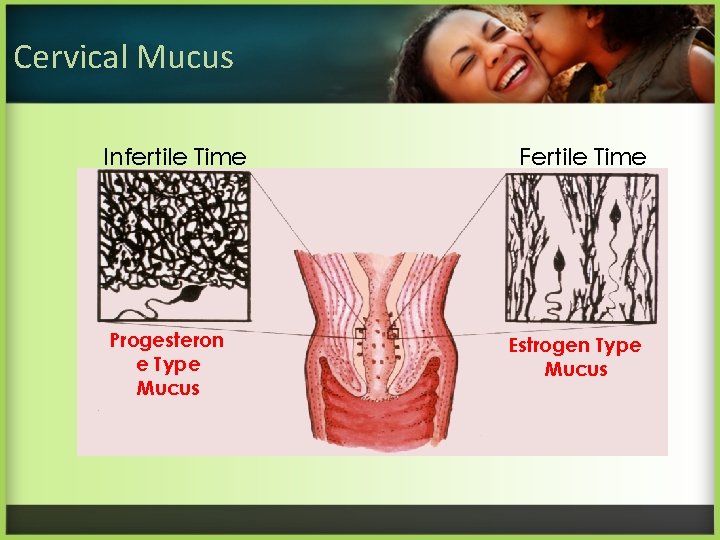
Cervical Mucus Infertile Time Progesteron e Type Mucus Fertile Time Estrogen Type Mucus
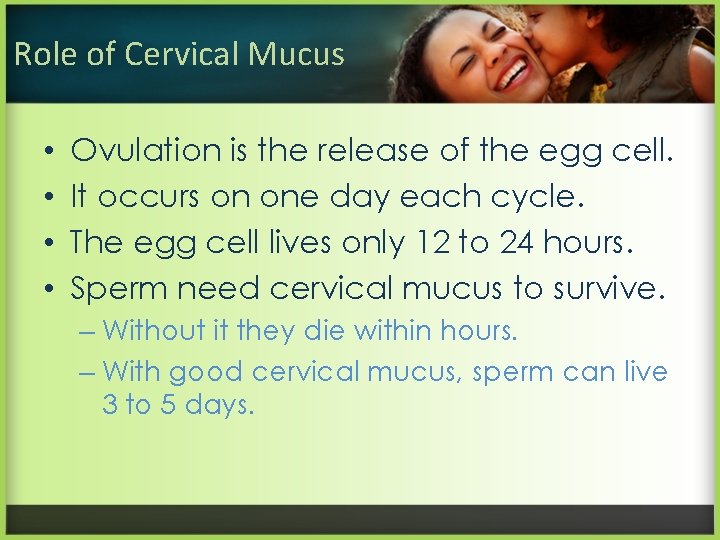
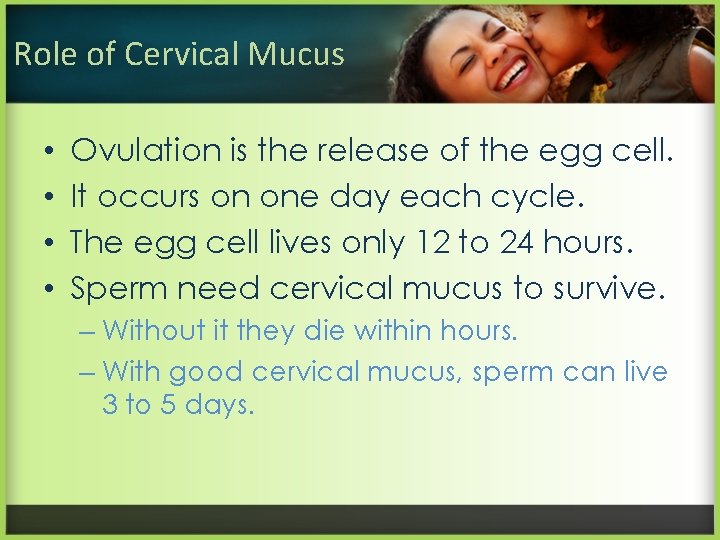
Role of Cervical Mucus • • Ovulation is the release of the egg cell. It occurs on one day each cycle. The egg cell lives only 12 to 24 hours. Sperm need cervical mucus to survive. – Without it they die within hours. – With good cervical mucus, sperm can live 3 to 5 days.
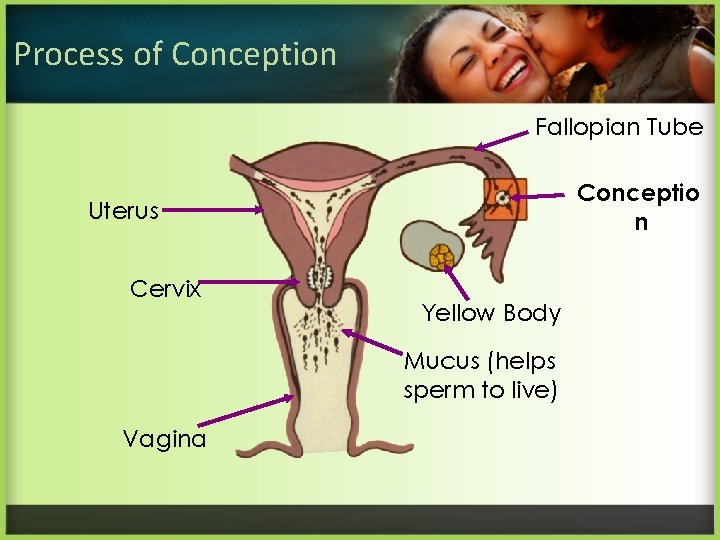
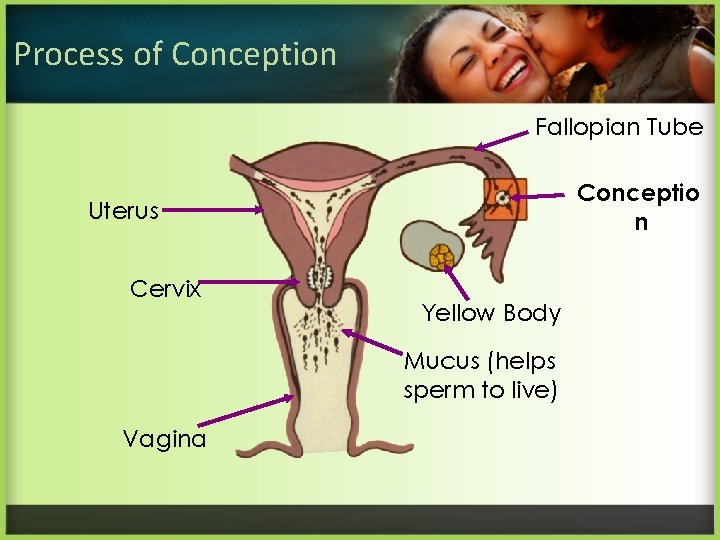
Process of Conception Fallopian Tube Conceptio n Uterus Cervix Yellow Body Mucus (helps sperm to live) Vagina

Images of Conception Egg and sperm before conception Fertilization and new life begins
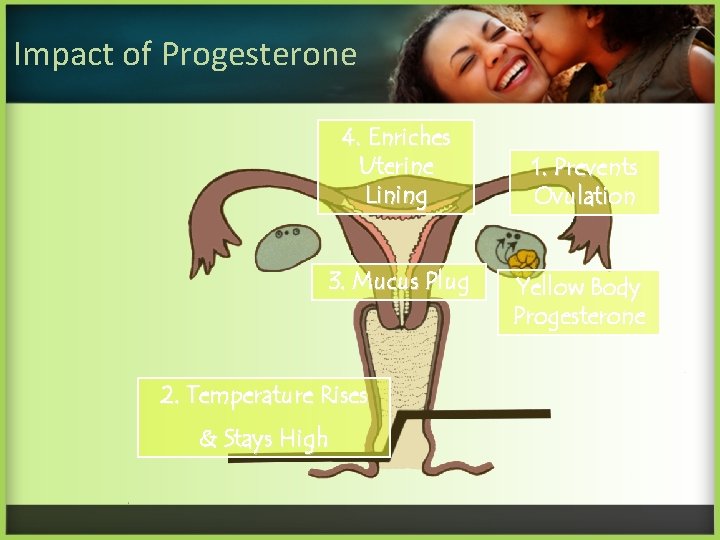
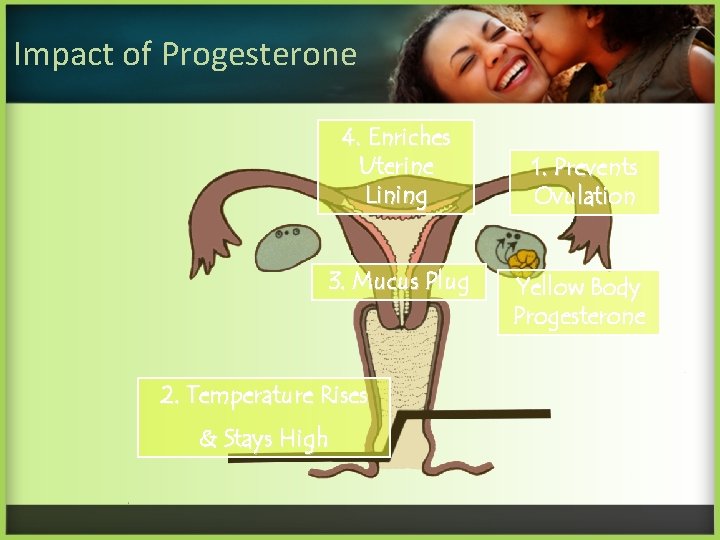
Impact of Progesterone 4. Enriches Uterine Lining 3. Mucus Plug 2. Temperature Rises & Stays High 1. Prevents Ovulation Yellow Body Progesterone
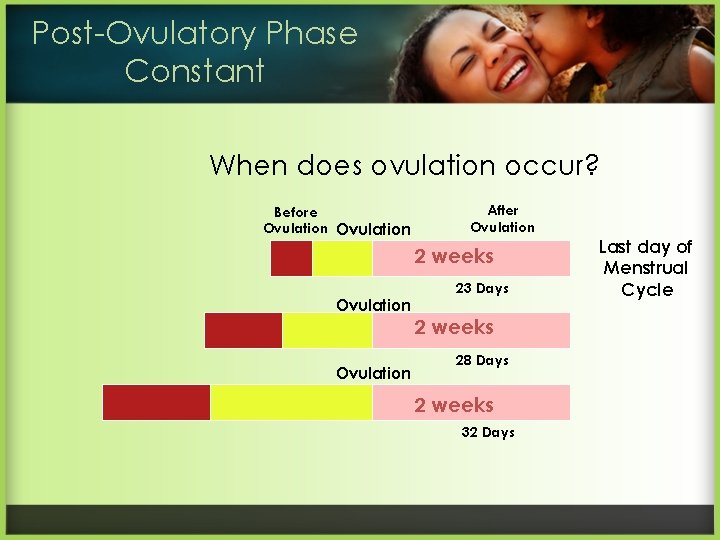
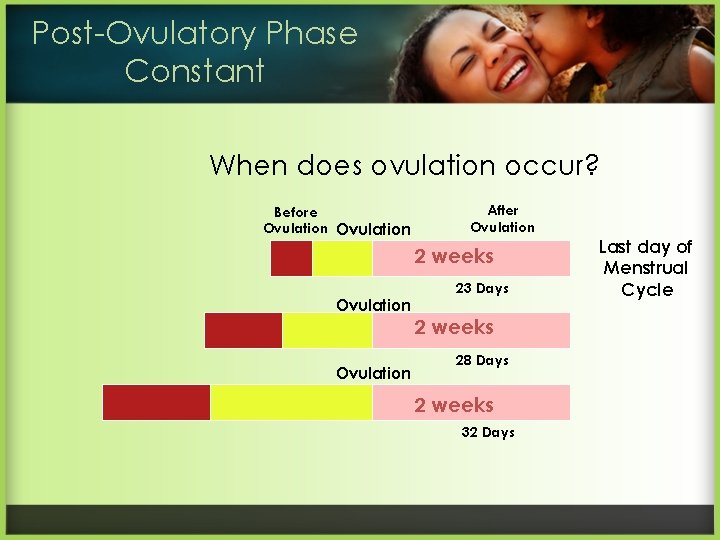
Post-Ovulatory Phase Constant When does ovulation occur? Before Ovulation After Ovulation 2 weeks Ovulation 23 Days 2 weeks 28 Days 2 weeks 32 Days Last day of Menstrual Cycle
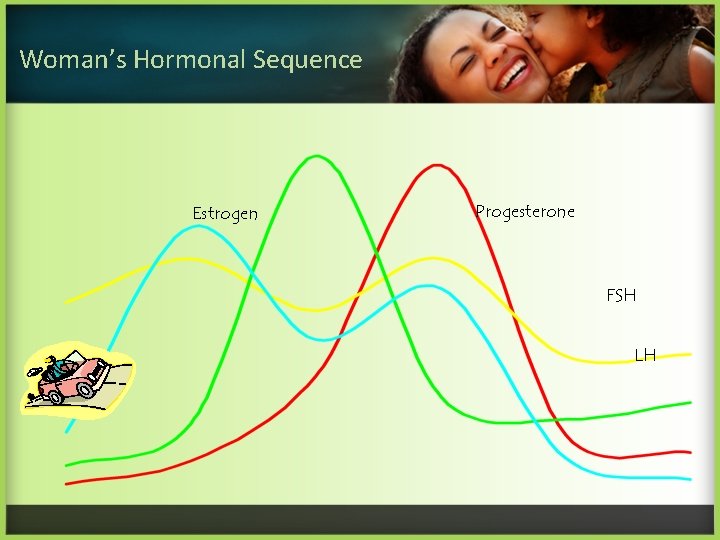
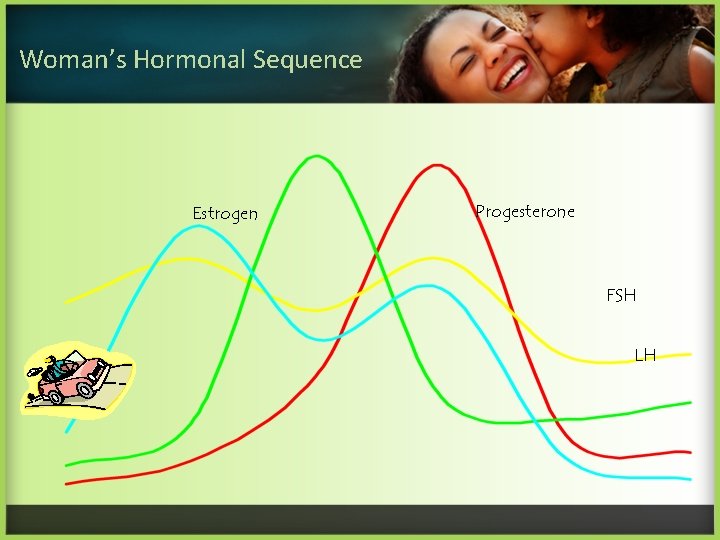
Woman’s Hormonal Sequence Estrogen Progesterone FSH LH
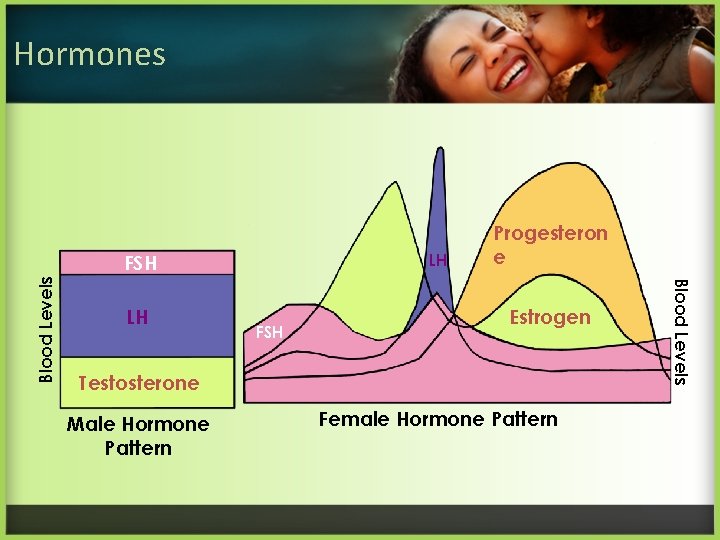
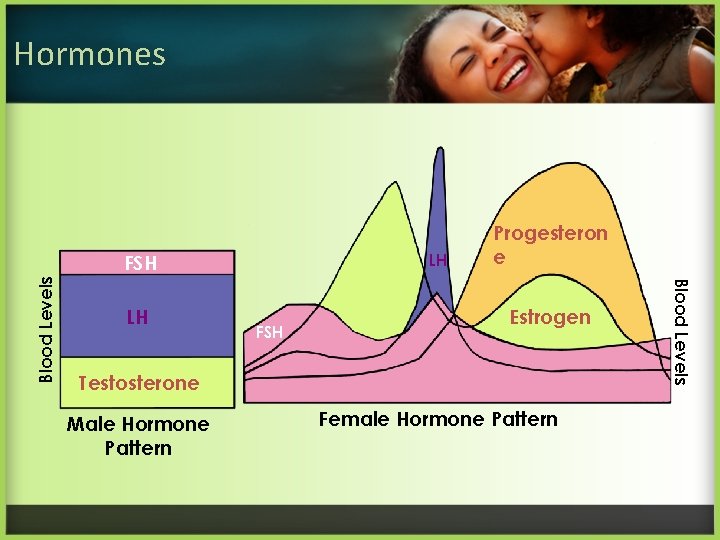
Hormones LH LH FSH Estrogen Testosterone Male Hormone Pattern Female Hormone Pattern Blood Levels FSH Progesteron e
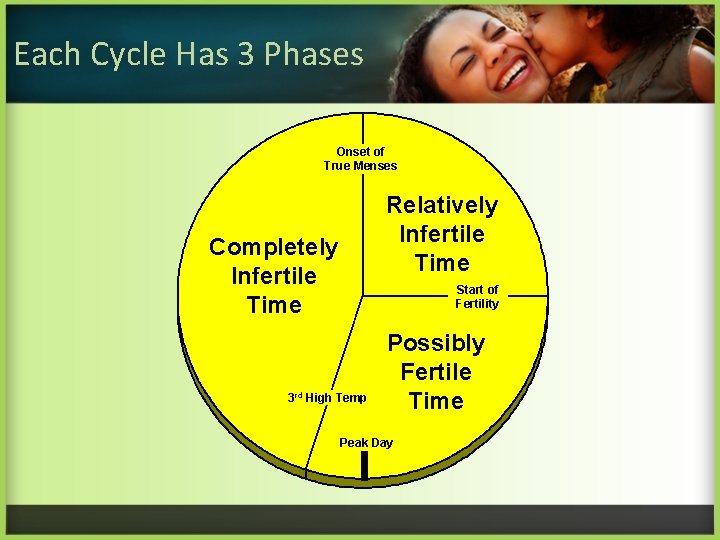
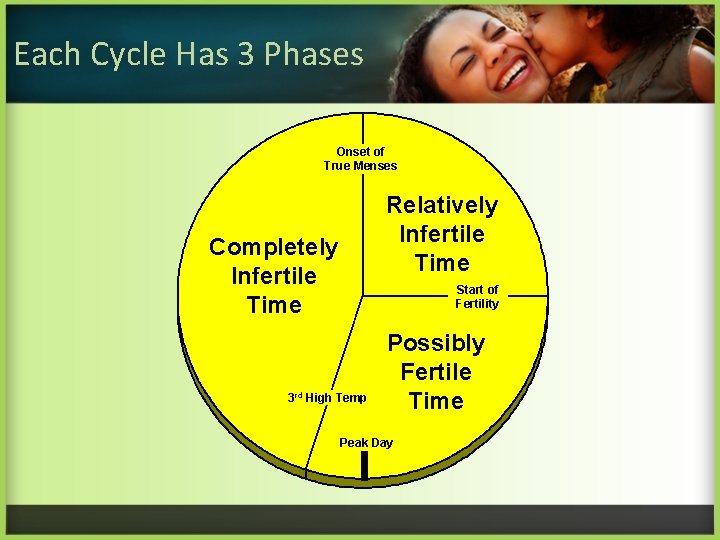
Each Cycle Has 3 Phases Onset of True Menses Relatively Infertile Time Completely Infertile Time Start of Fertility 3 rd High Temp Possibly Fertile Time Peak Day
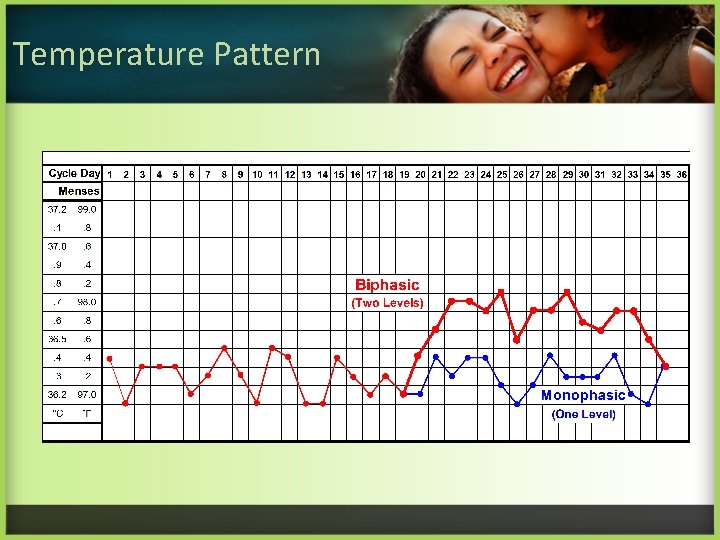
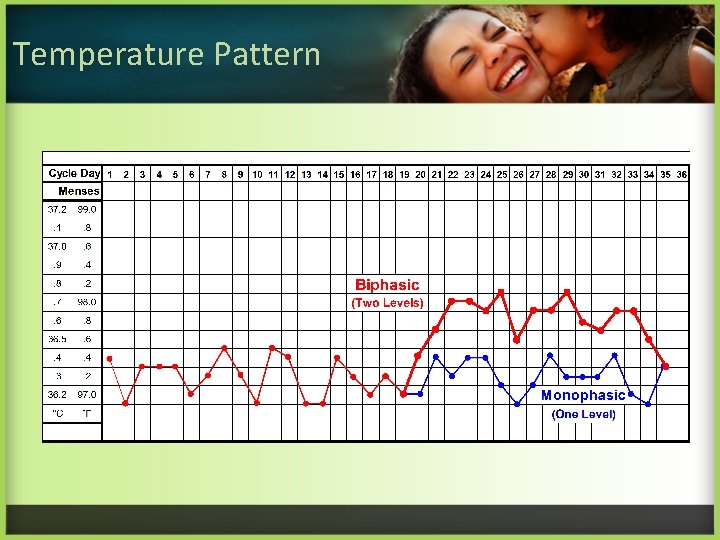
Temperature Pattern
Do Activity #2 • Use pages 5 and 6 in your activity packet. Record the readings from thermometers on page 6 day-by-day on the graph displayed on page 5.
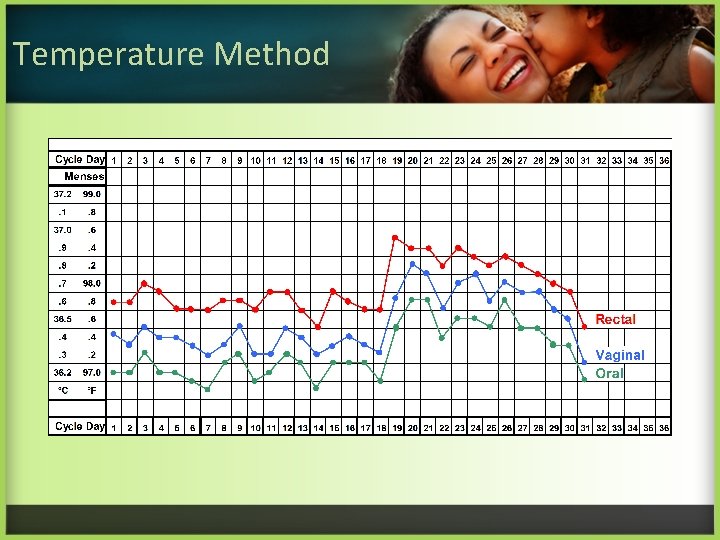
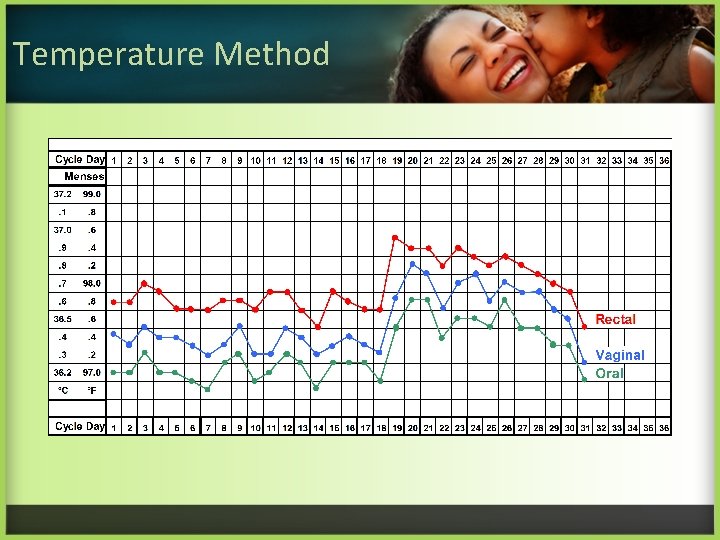
Temperature Method
Temperature Taking Technique • Consistency is essential • Body rhythms are a factor • Chart disturbances
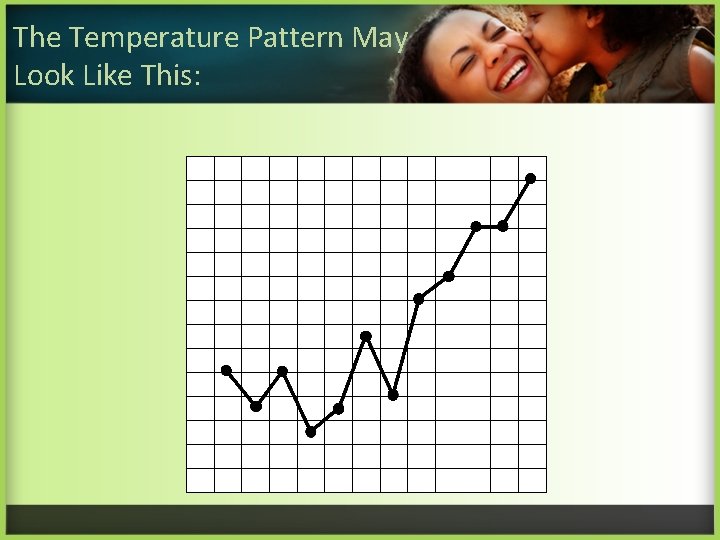
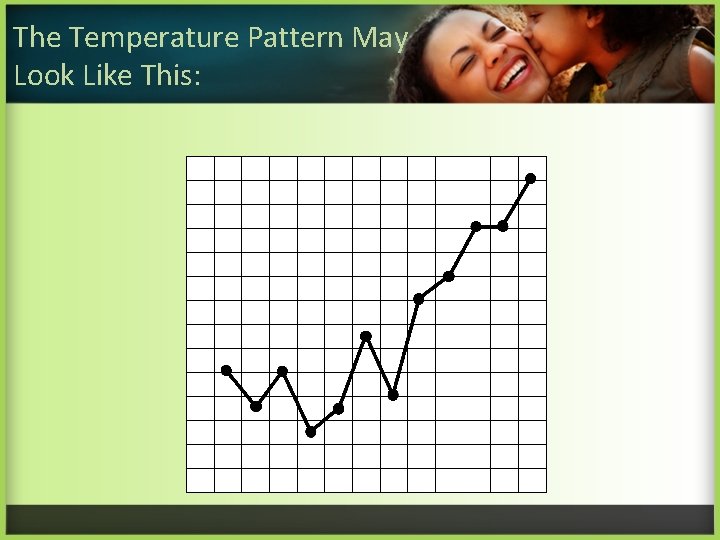
The Temperature Pattern May Look Like This:
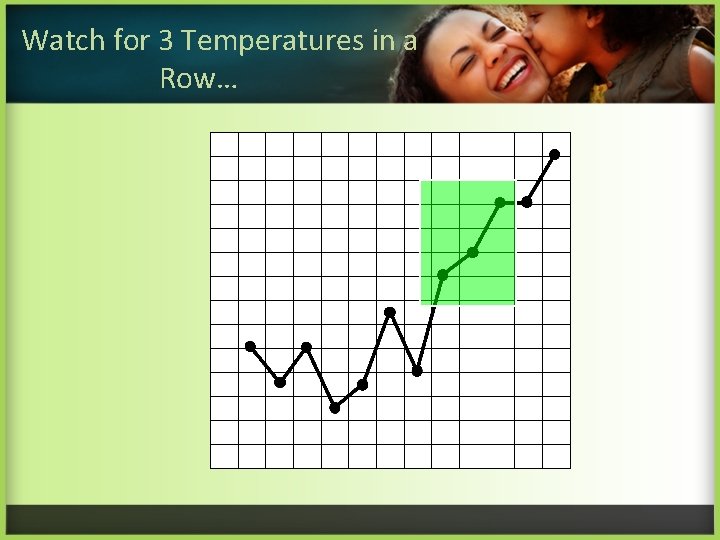
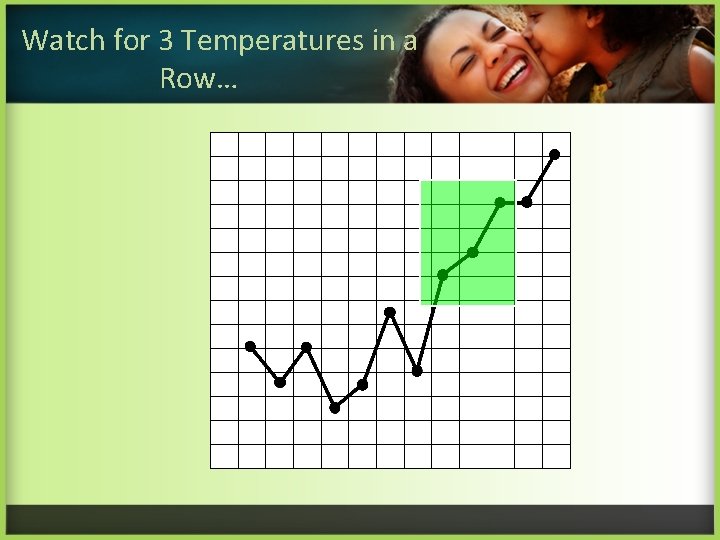
Watch for 3 Temperatures in a Row…
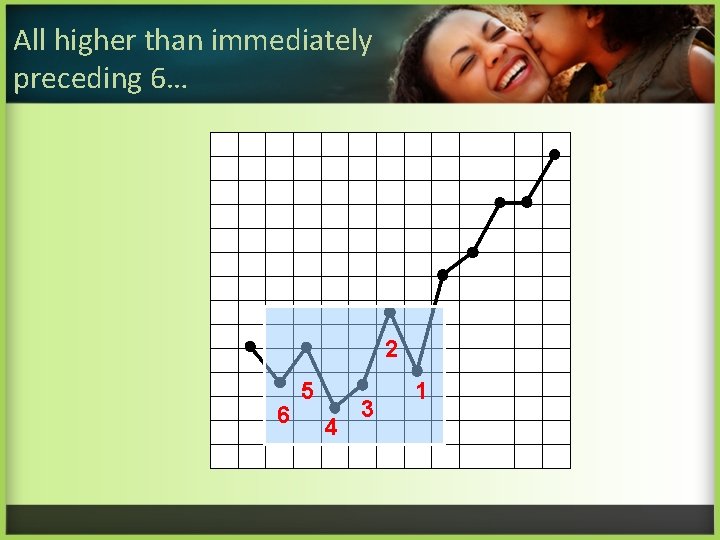
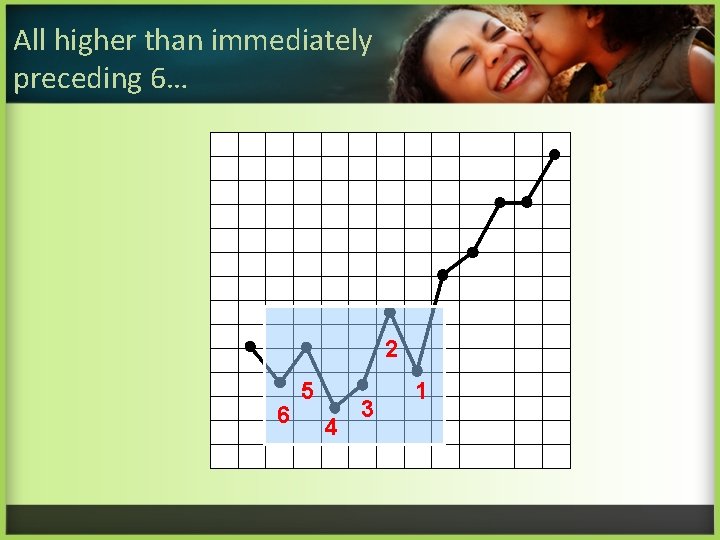
All higher than immediately preceding 6… 2 6 5 4 3 1
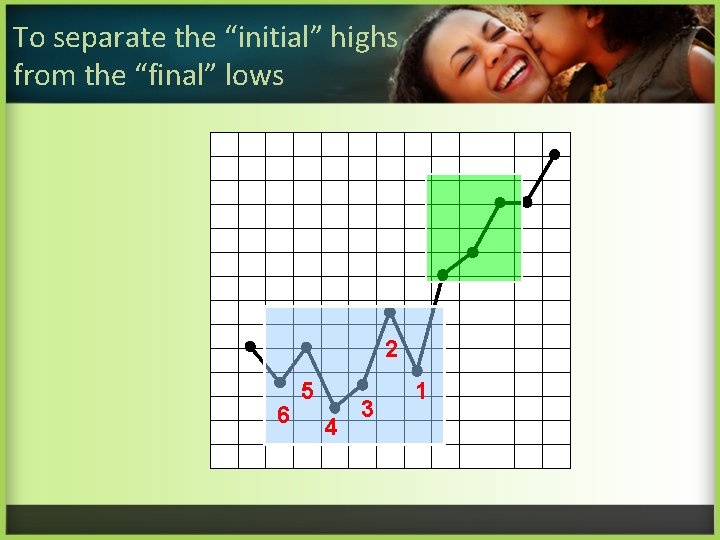
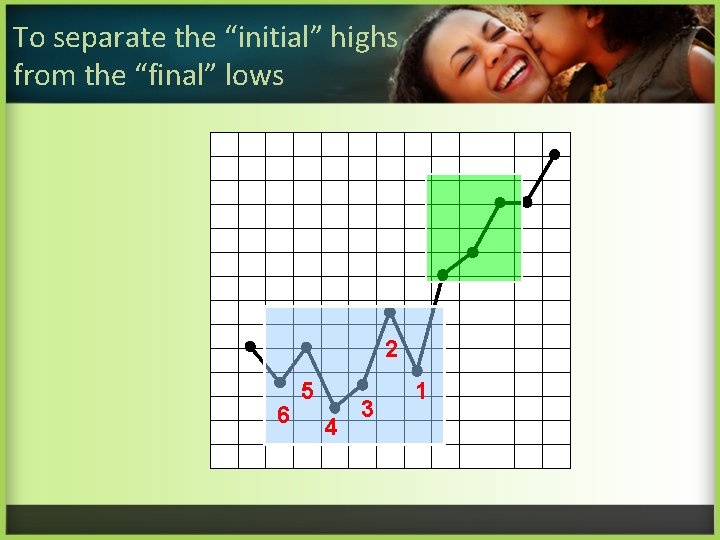
To separate the “initial” highs from the “final” lows 2 6 5 4 3 1
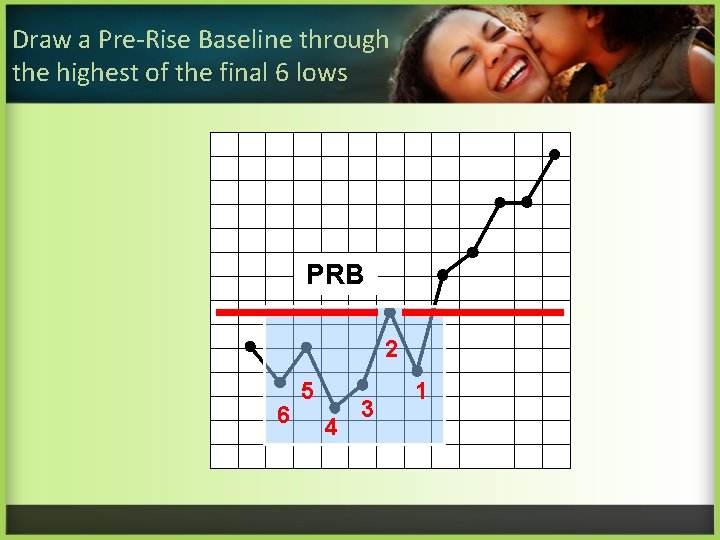
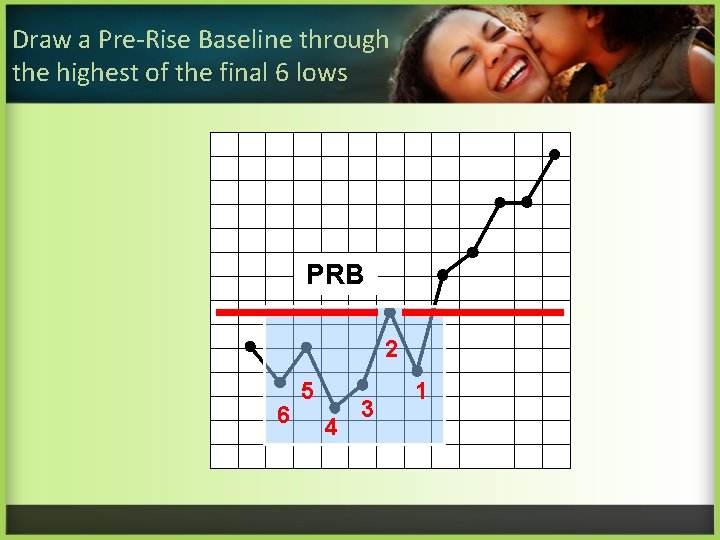
Draw a Pre-Rise Baseline through the highest of the final 6 lows PRB 2 6 5 4 3 1
Do Activity #3 • Establishing a Pre-Rise Baseline. See pages 7 and 8.
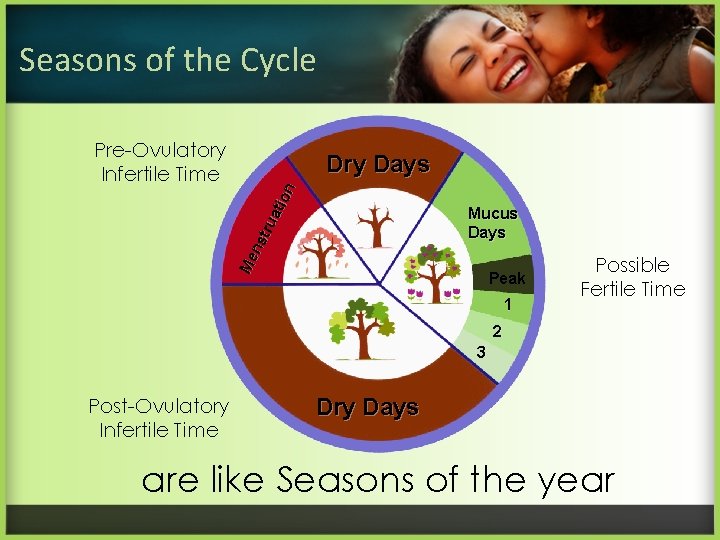
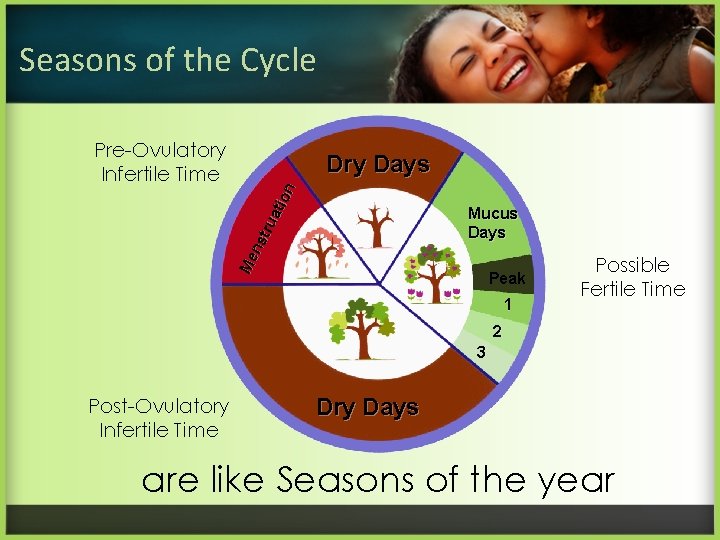
Seasons of the Cycle Pre-Ovulatory Infertile Time Me ns tru ati on Dry Days Mucus Days Peak 1 Possible Fertile Time 2 3 Post-Ovulatory Infertile Time Dry Days are like Seasons of the year
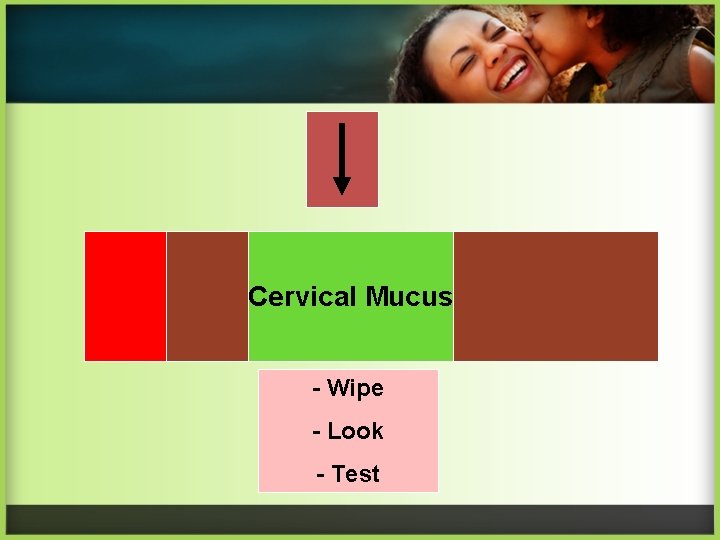
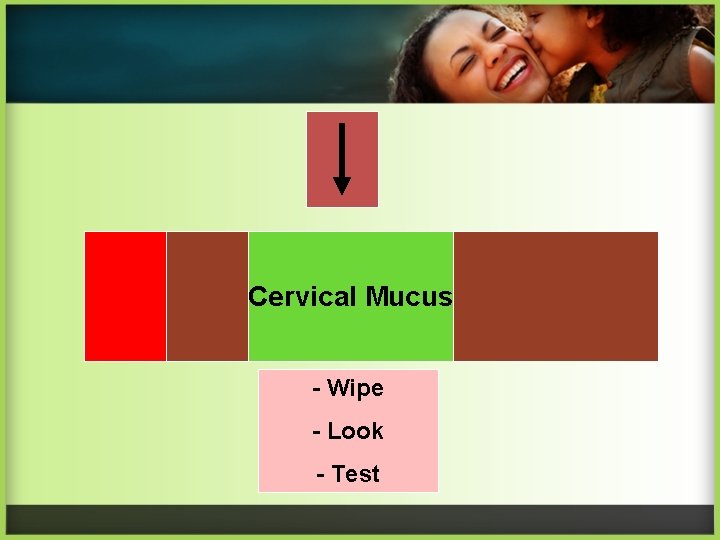
Cervical Mucus - Wipe - Look - Test
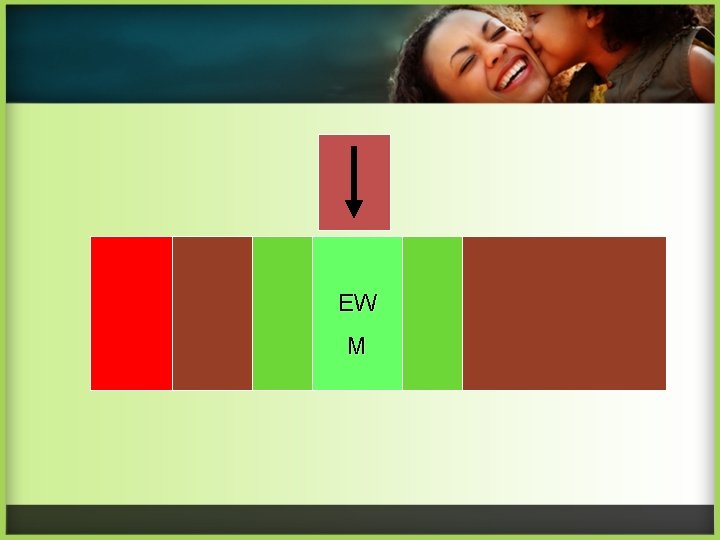
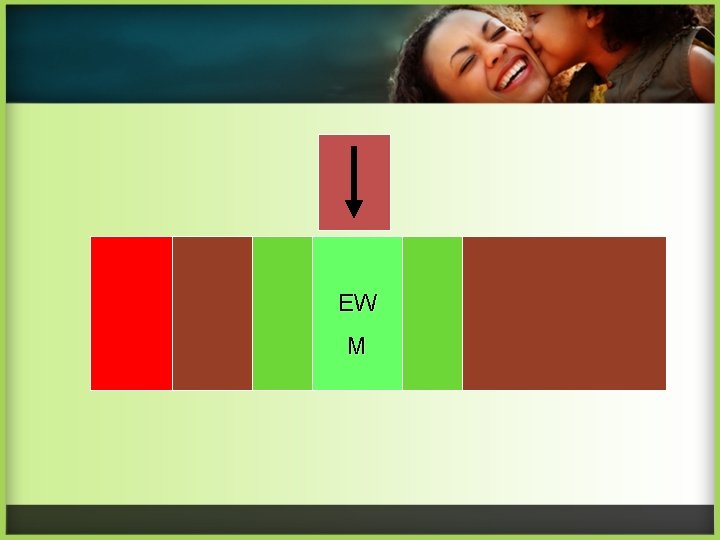
EW M
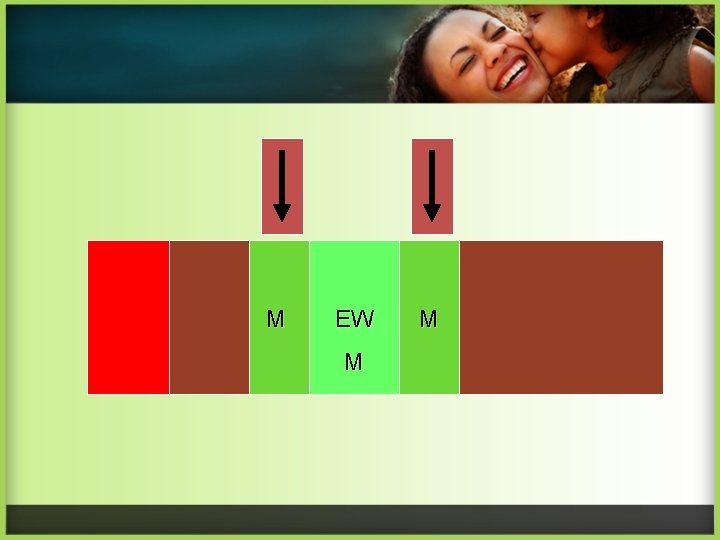
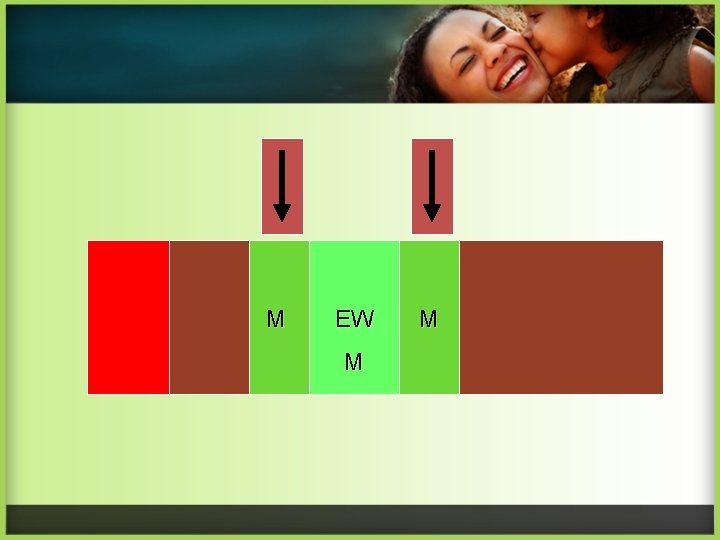
M EW M M
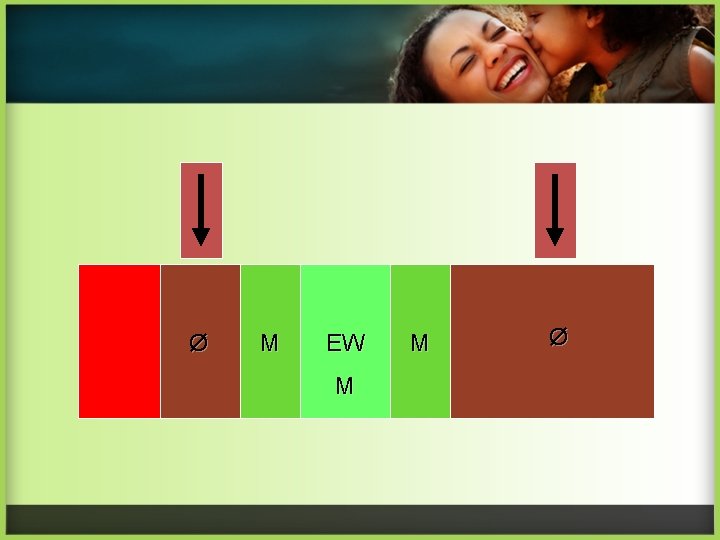
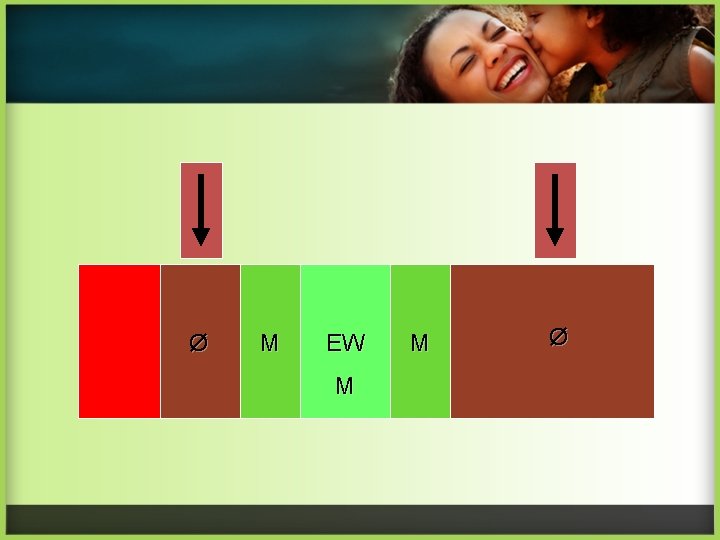
Ø M EW M M Ø
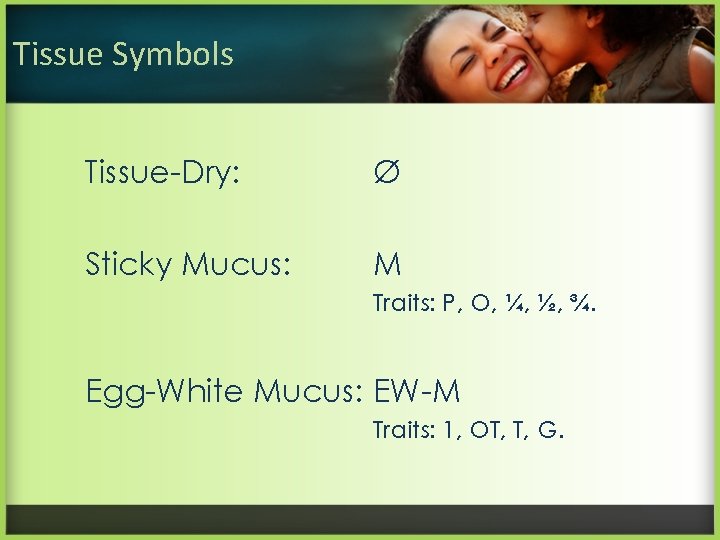
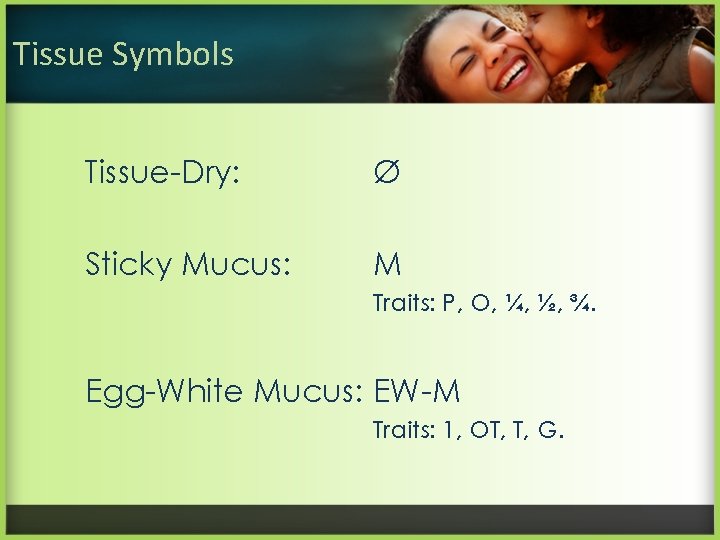
Tissue Symbols Tissue-Dry: Ø Sticky Mucus: M Traits: P, O, ¼, ½, ¾. Egg-White Mucus: EW-M Traits: 1, OT, T, G.
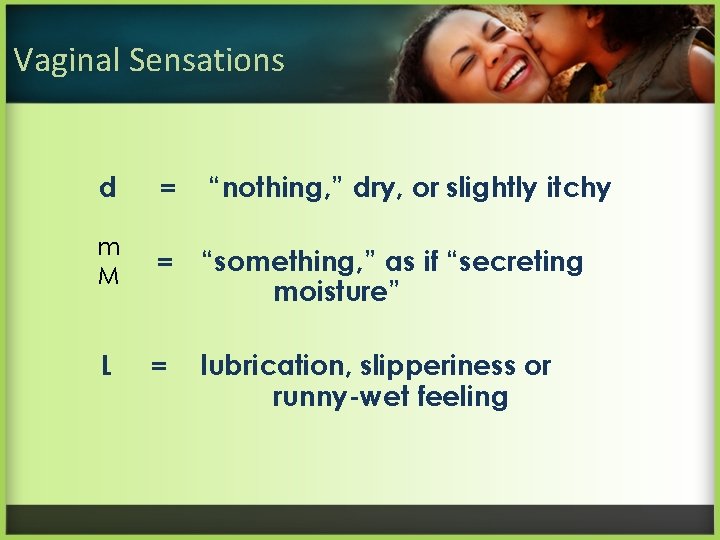
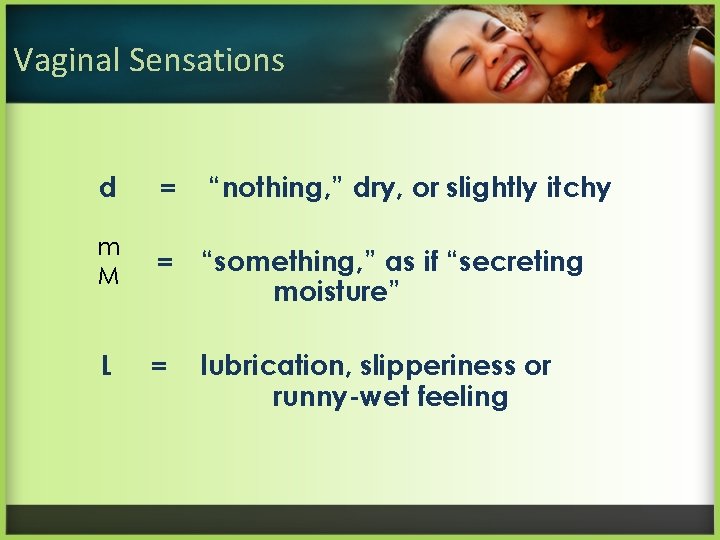
Vaginal Sensations d = “nothing, ” dry, or slightly itchy m M = “something, ” as if “secreting moisture” L = lubrication, slipperiness or runny-wet feeling
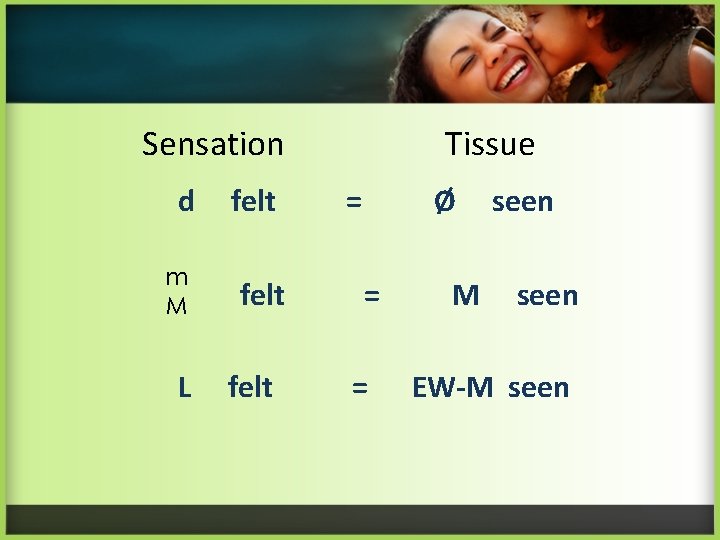
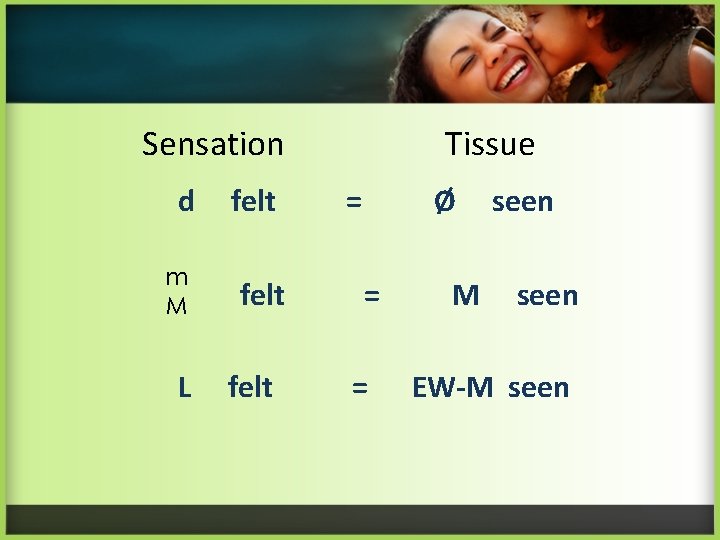
Sensation d m M L felt Tissue = Ø = = M seen EW-M seen
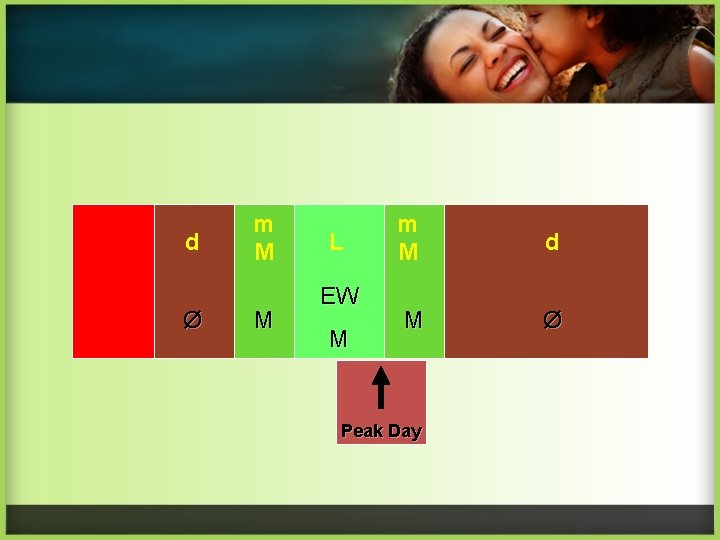
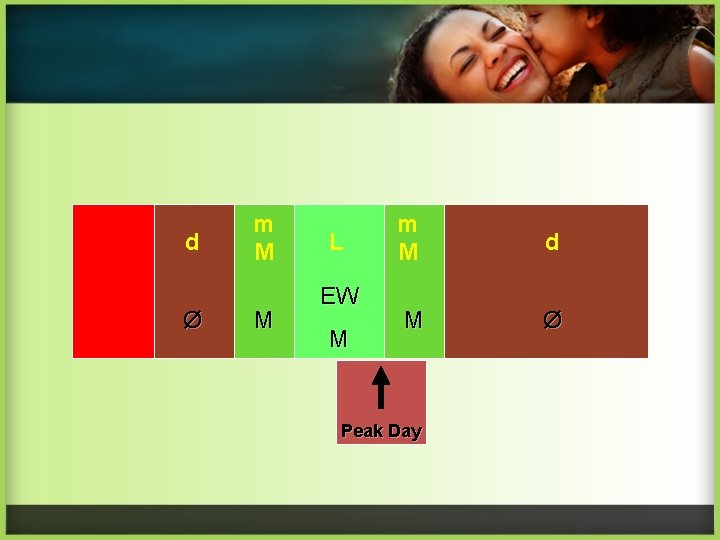
d Ø m M M L EW M m M d M Ø Peak Day
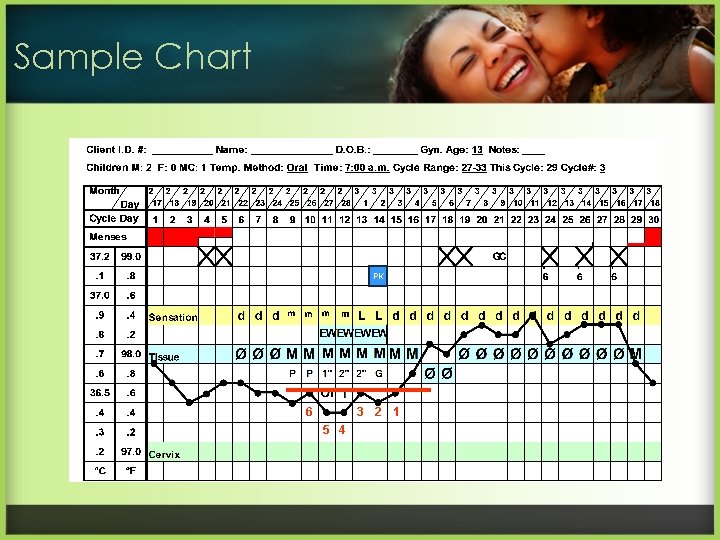
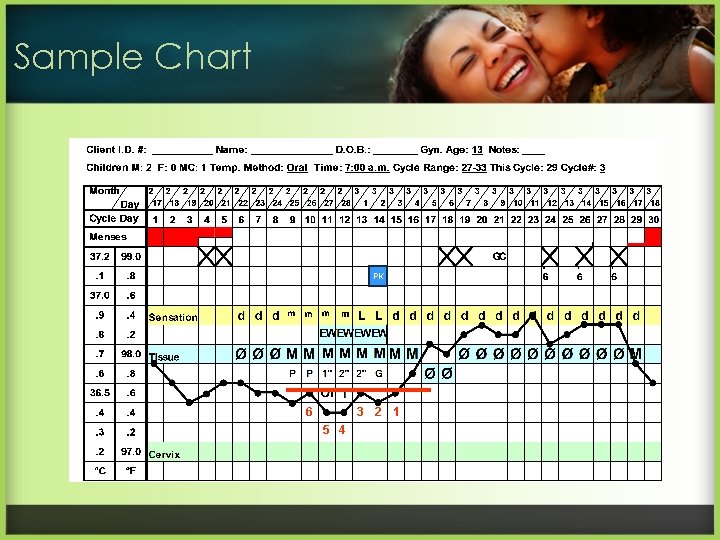
Sample Chart PK 6 3 5 4 2 1
Do Activity #4 • Using the graph on page 5 of the activity packet and the “fertility” diary on page 9, fill in the symbols, the traits, and Peak Day.
Be Sure to Chart • Every day at the end of the day. • The most fertile sign of the day. • What you actually observe.
Factors Disturbing the Cervical Mucus Observation • • • Douching and vaginal sprays. Scented tampons and sanitary napkins. Fabric softeners used in the dryer. Synthetic underwear. Medications such as steroids or antihistamines. Presence of an IUD. Hormonal products or contraceptives. Withdrawal or barrier contraceptives. Seminal fluid.