Swan Gantz Catherter and the Meaning of its
- Slides: 67
Swan Gantz Catherter and the Meaning of its Justin Chandler Readings Surgical Critical Care Fellow
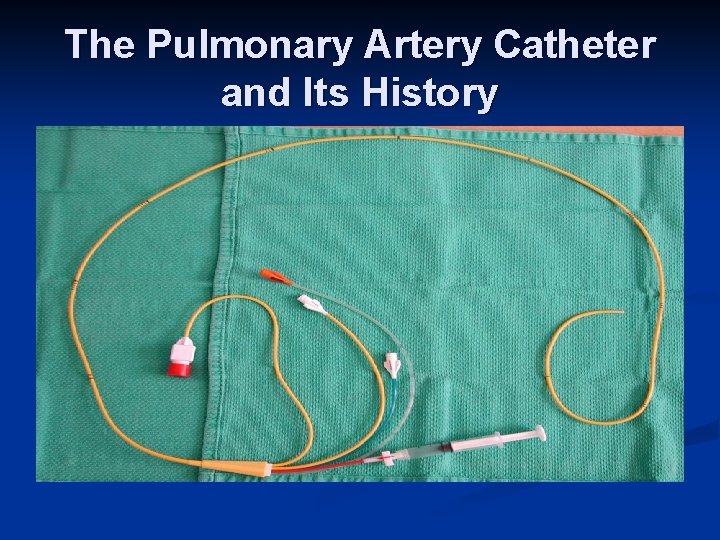
The Pulmonary Artery Catheter and Its History
The Pulmonary Artery Catheter and Its History n Cardiac catheterization dates back to Claude Bernard n n used it on animal models Clinical application begins with Werner Forssmann in the 1930 s n inserted a catheter into his own forearm, guided it fluoroscopically into his right atrium, and took an X-ray picture of it
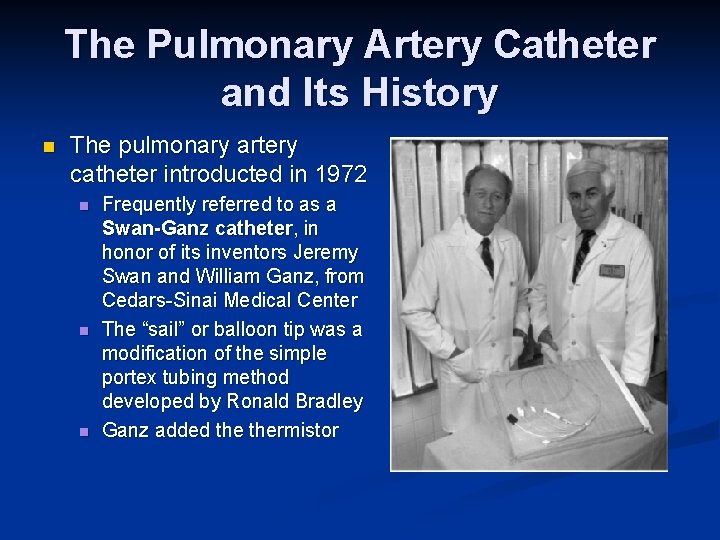
The Pulmonary Artery Catheter and Its History n The pulmonary artery catheter introducted in 1972 n n n Frequently referred to as a Swan-Ganz catheter, in honor of its inventors Jeremy Swan and William Ganz, from Cedars-Sinai Medical Center The “sail” or balloon tip was a modification of the simple portex tubing method developed by Ronald Bradley Ganz added thermistor
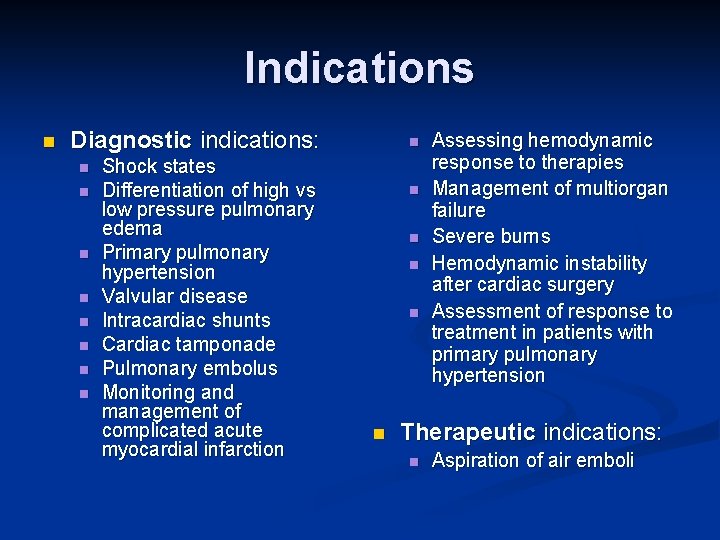
Indications n Diagnostic indications: n n n n Shock states Differentiation of high vs low pressure pulmonary edema Primary pulmonary hypertension Valvular disease Intracardiac shunts Cardiac tamponade Pulmonary embolus Monitoring and management of complicated acute myocardial infarction n n n Assessing hemodynamic response to therapies Management of multiorgan failure Severe burns Hemodynamic instability after cardiac surgery Assessment of response to treatment in patients with primary pulmonary hypertension Therapeutic indications: n Aspiration of air emboli
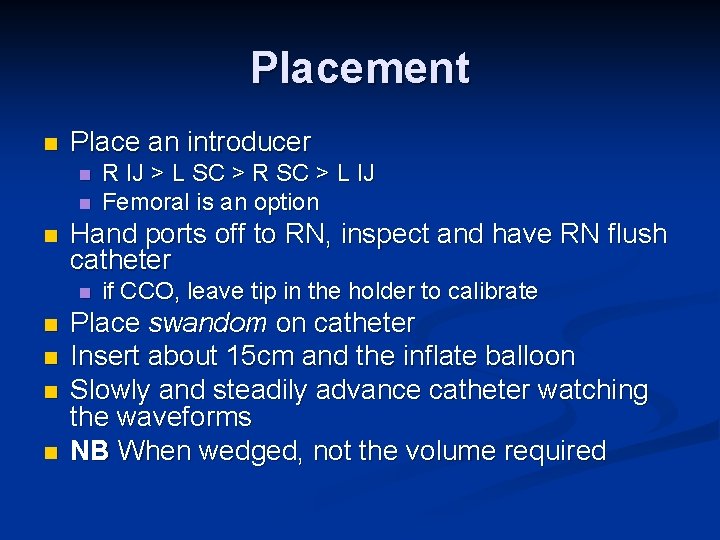
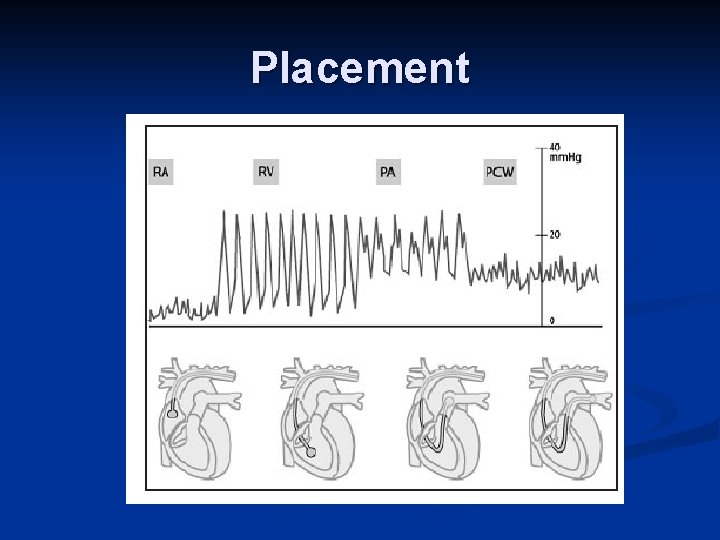
Placement n Place an introducer n n n Hand ports off to RN, inspect and have RN flush catheter n n n R IJ > L SC > R SC > L IJ Femoral is an option if CCO, leave tip in the holder to calibrate Place swandom on catheter Insert about 15 cm and the inflate balloon Slowly and steadily advance catheter watching the waveforms NB When wedged, not the volume required
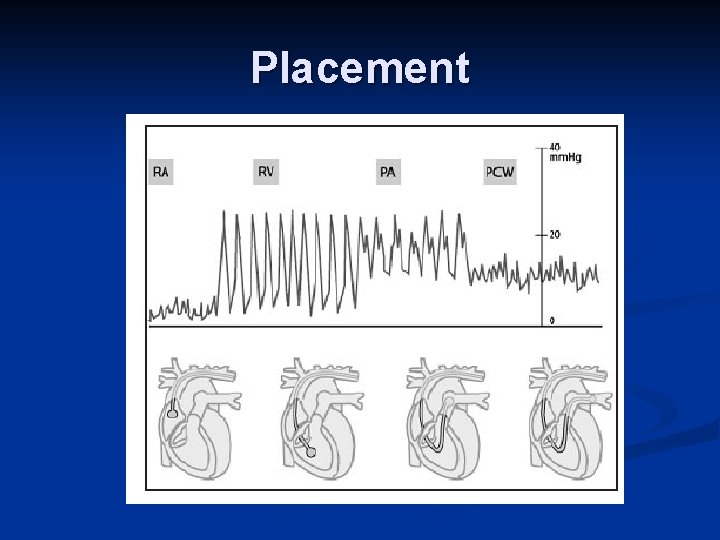
Placement
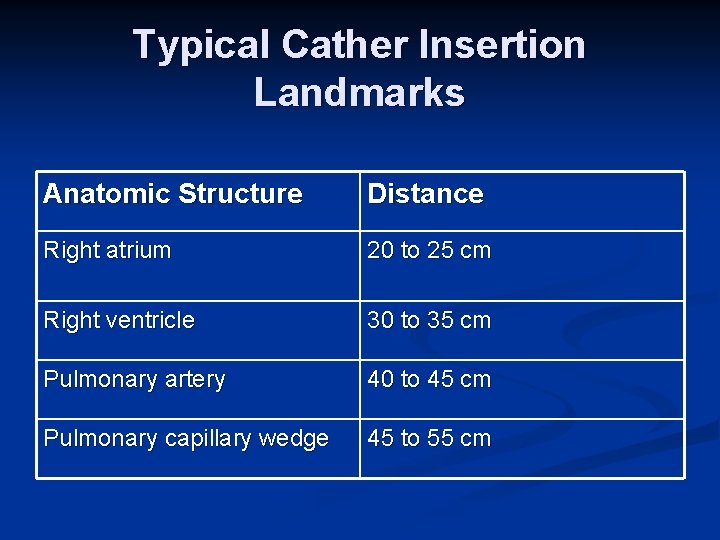
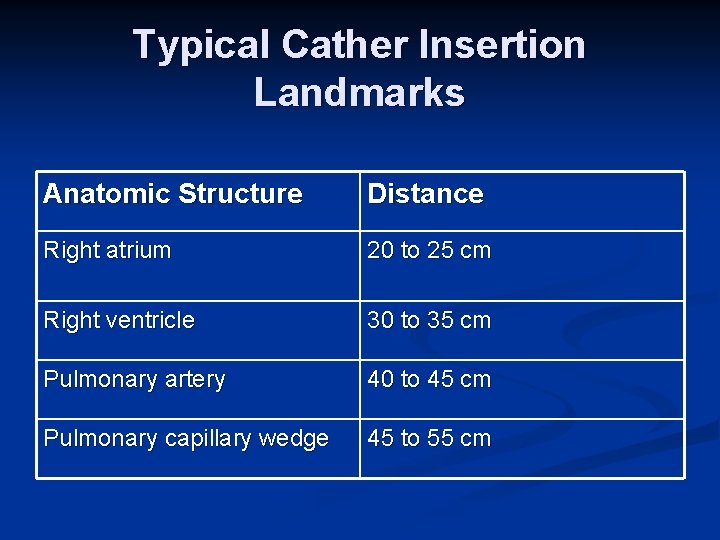
Typical Cather Insertion Landmarks Anatomic Structure Distance Right atrium 20 to 25 cm Right ventricle 30 to 35 cm Pulmonary artery 40 to 45 cm Pulmonary capillary wedge 45 to 55 cm
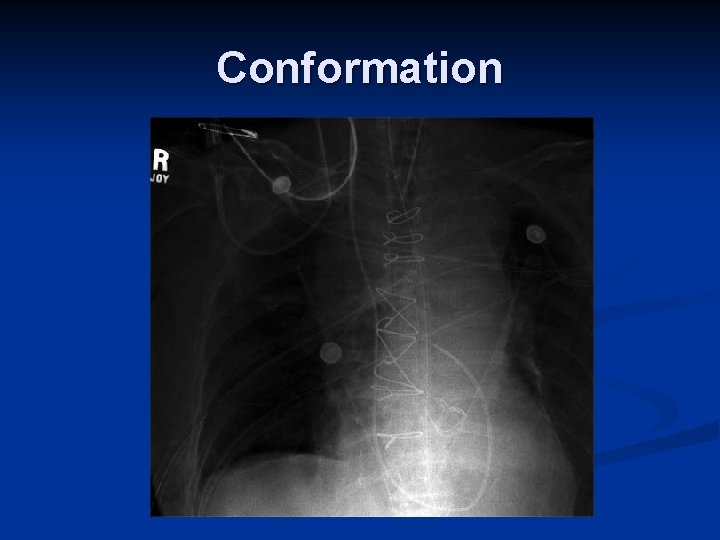
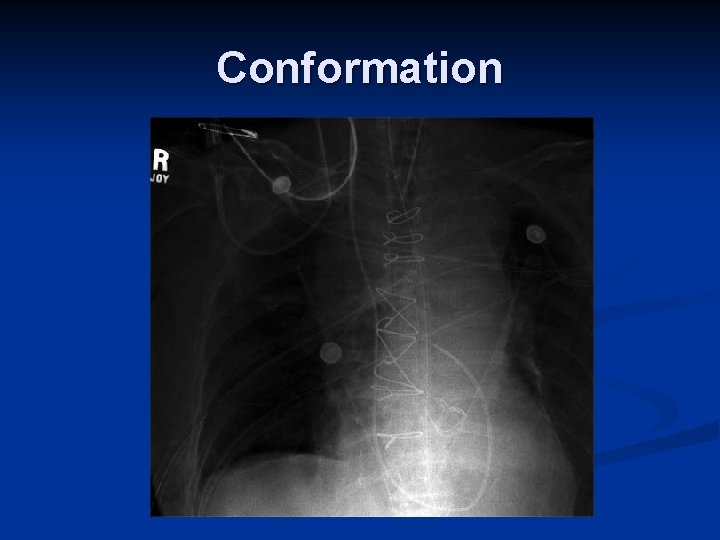
Conformation
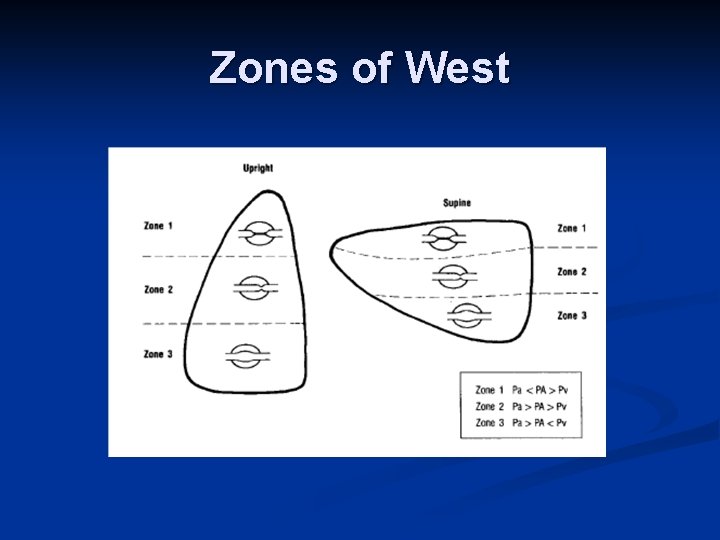
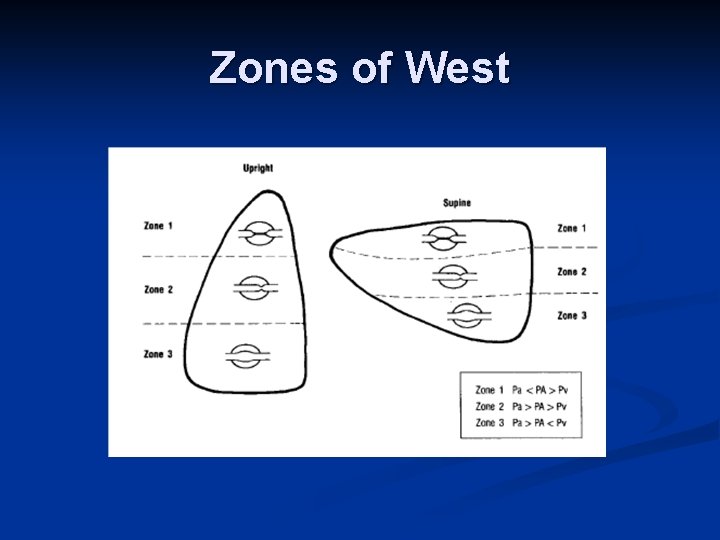
Zones of West
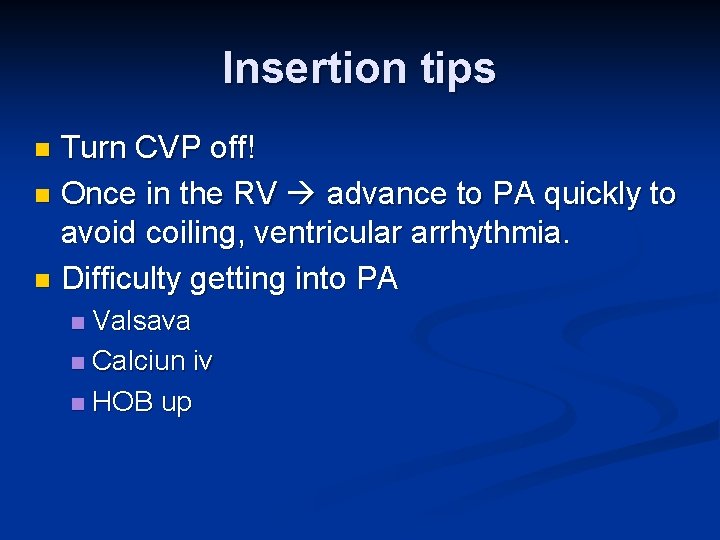
Insertion tips T u rn C V P o f f ! n Once in the RV advance to PA quickly to avoid coiling, ventricular arrhythmia. n Difficulty getting into PA n Valsava n Calciun iv n HO B up n
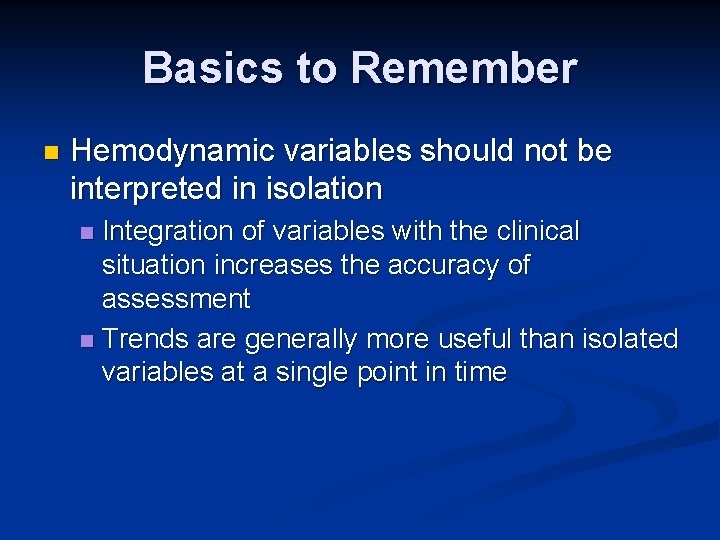
Basics to Remember n Hemodynamic variables should not be interpreted in isolation Integration of variables with the clinical situation increases the accuracy of assessment n Trends are generally more useful than isolated variables at a single point in time n
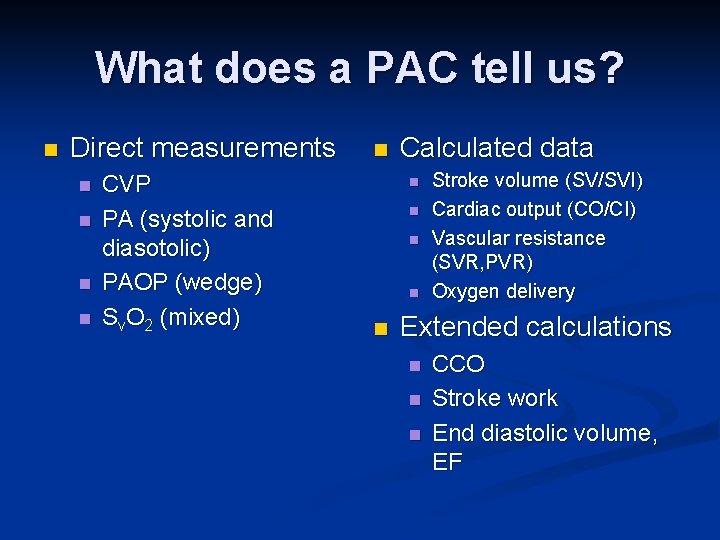
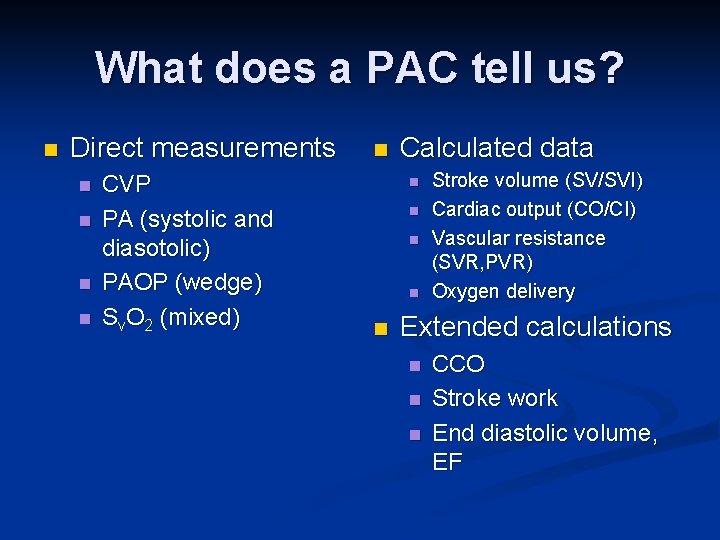
What does a PAC tell us? n Direct measurements n n CVP PA (systolic and diasotolic) PAOP (wedge) Sv. O 2 (mixed) n Calculated data n n n Stroke volume (SV/SVI) Cardiac output (CO/CI) Vascular resistance (SVR, PVR) Oxygen delivery Extended calculations n n n CCO Stroke work End diastolic volume, EF
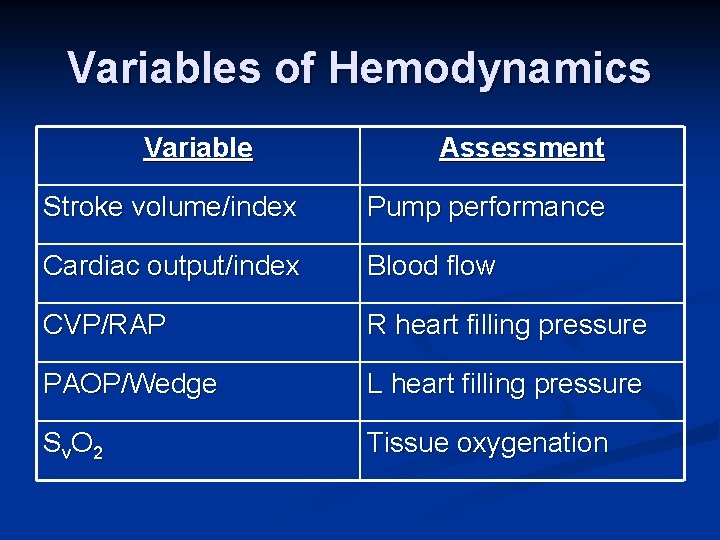
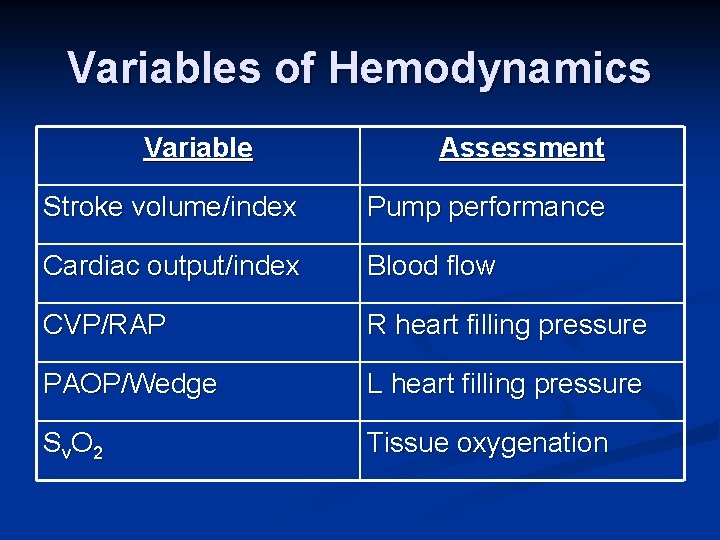
Variables of Hemodynamics Variable Assessment Stroke volume/index Pump performance Cardiac output/index Blood flow CVP/RAP R heart filling pressure PAOP/Wedge L heart filling pressure Sv. O 2 Tissue oxygenation
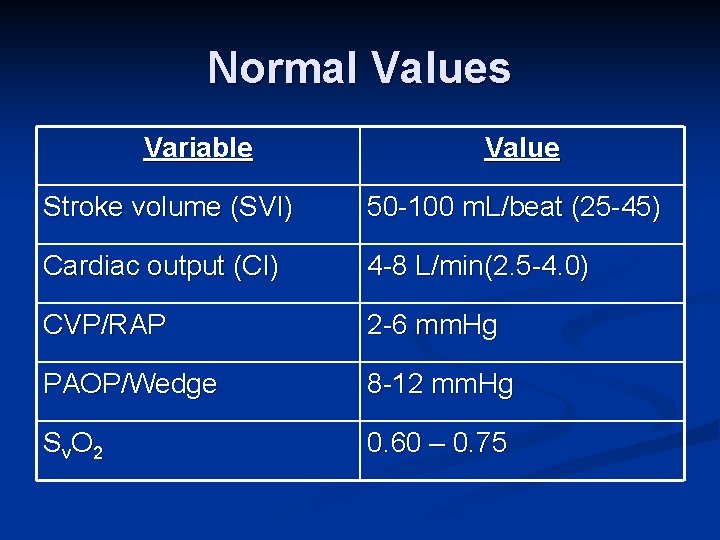
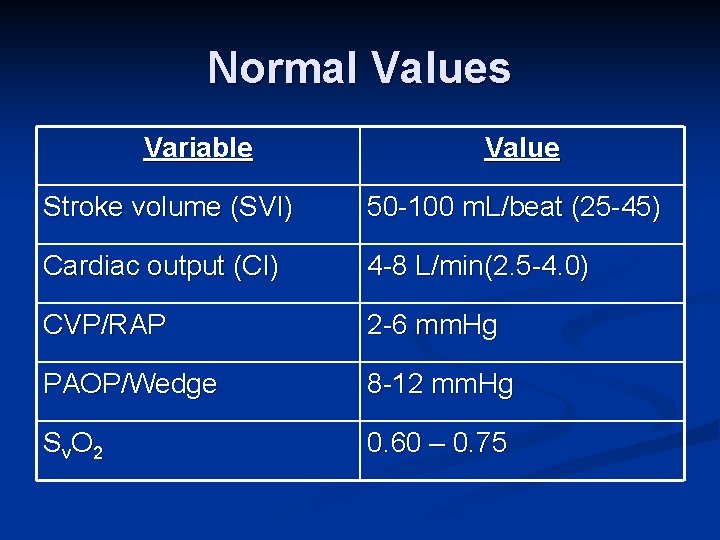
Normal Values Variable Value Stroke volume (SVI) 50 -100 m. L/beat (25 -45) Cardiac output (CI) 4 -8 L/min(2. 5 -4. 0) CVP/RAP 2 -6 mm. Hg PAOP/Wedge 8 -12 mm. Hg Sv. O 2 0. 60 – 0. 75
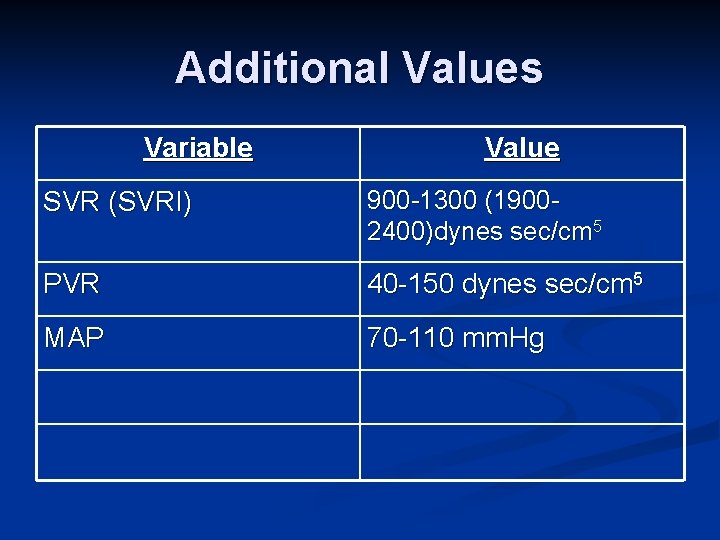
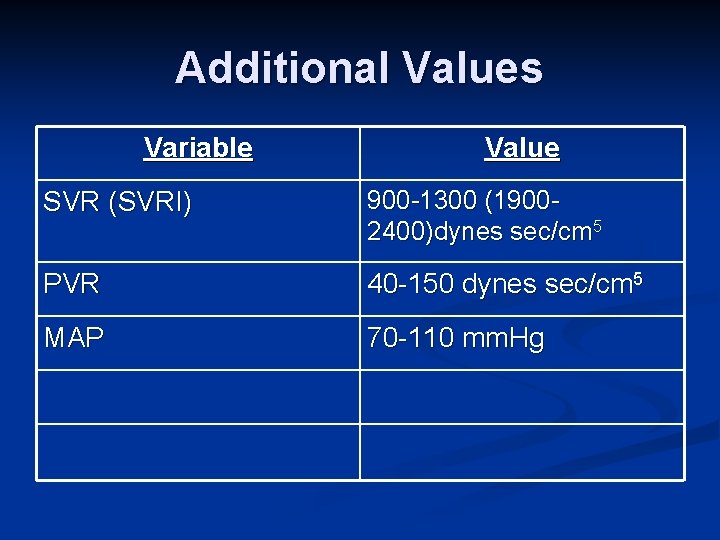
Additional Values Variable Value SVR (SVRI) 900 -1300 (19002400)dynes sec/cm 5 PVR 40 -150 dynes sec/cm 5 MAP 70 -110 mm. Hg
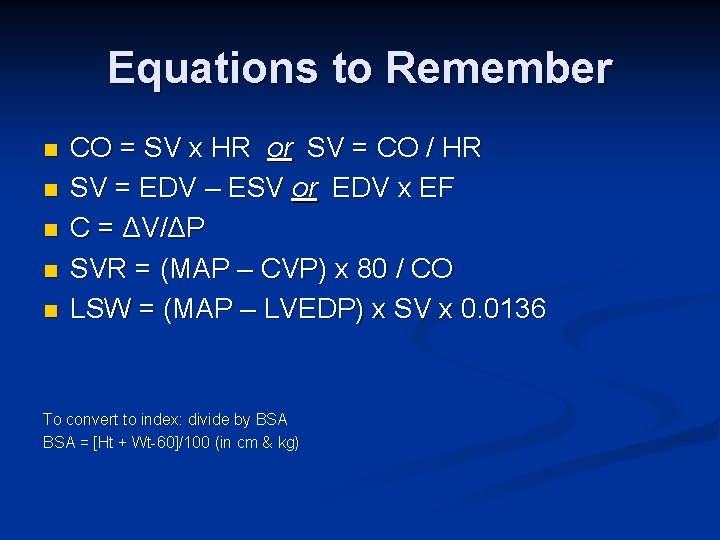
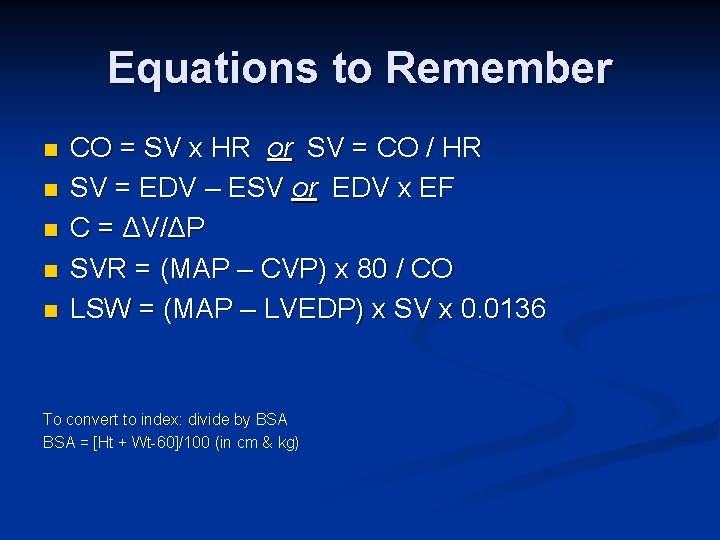
Equations to Remember n n n CO = SV x HR or SV = CO / HR SV = EDV – ESV or EDV x EF C = ΔV/ΔP SVR = (MAP – CVP) x 80 / CO LSW = (MAP – LVEDP) x SV x 0. 0136 To convert to index: divide by BSA = [Ht + Wt-60]/100 (in cm & kg)
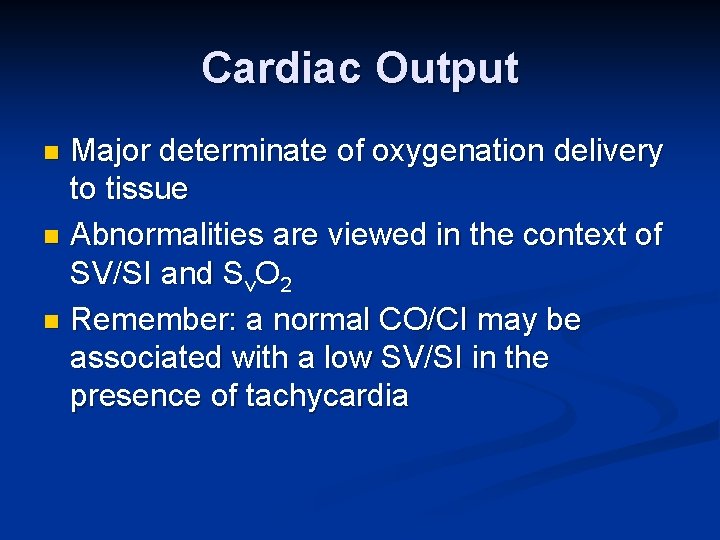
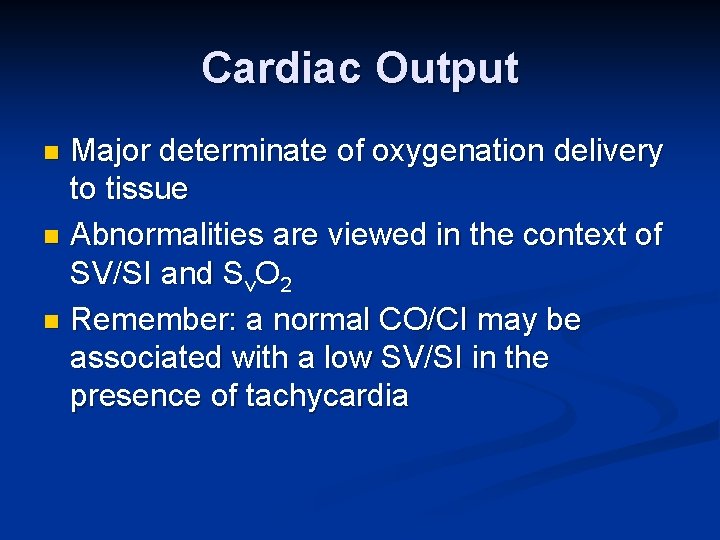
Cardiac Output Major determinate of oxygenation delivery to tissue n Abnormalities are viewed in the context of SV/SI and Sv. O 2 n Remember: a normal CO/CI may be associated with a low SV/SI in the presence of tachycardia n
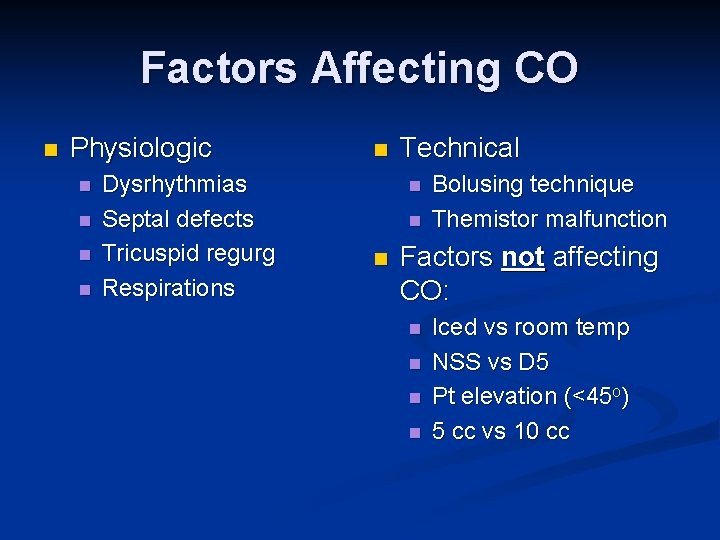
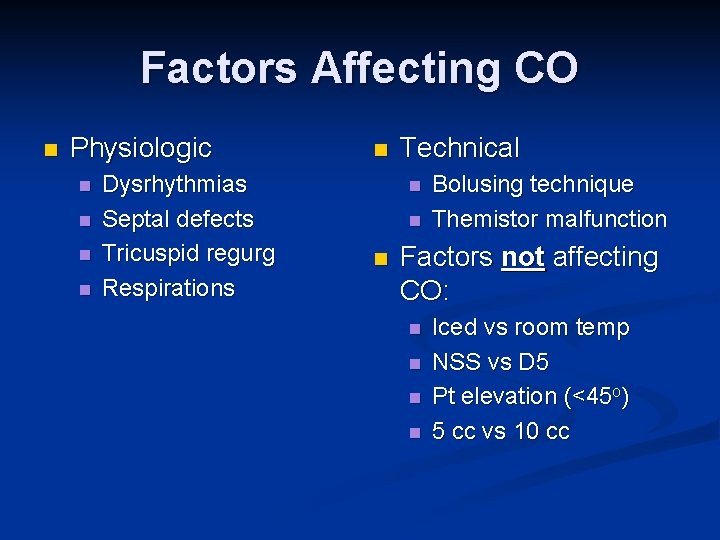
Factors Affecting CO n Physiologic n n Dysrhythmias Septal defects Tricuspid regurg Respirations n Technical n n n Bolusing technique Themistor malfunction Factors not affecting CO: n n Iced vs room temp NSS vs D 5 Pt elevation (<45 o) 5 cc vs 10 cc
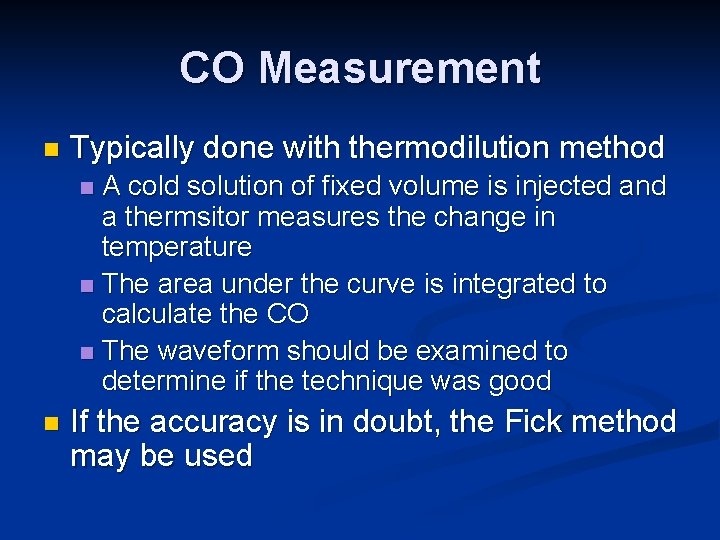
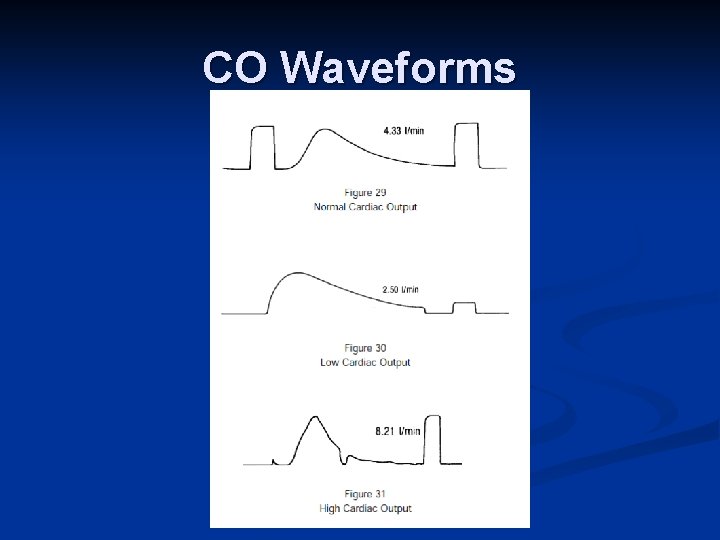
CO Measurement n Typically done with thermodilution method A cold solution of fixed volume is injected and a thermsitor measures the change in temperature n The area under the curve is integrated to calculate the CO n The waveform should be examined to determine if the technique was good n n If the accuracy is in doubt, the Fick method may be used
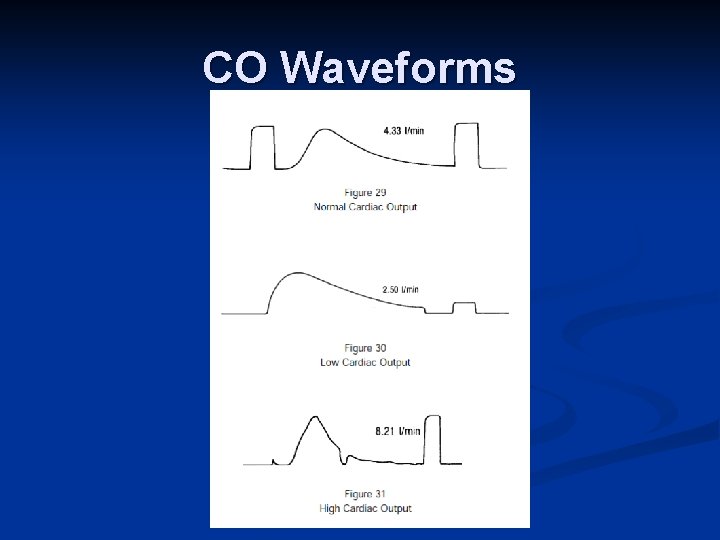
CO Waveforms
Fick Method n CO = VO 2 / [Ca. O 2 – Cv. O 2] * 10 n Sa. O 2 and Sv. O 2 often substituted n CO = VO 2 / [Sa. O 2 – Sv. O 2] * Hgb * 1. 34* 10 n VO 2 is not usually measured n Can use 3. 5 m. L/kg or 125 m. L/m 2 n If metabolic rate is abnormal, the calculation may be incorrect
Stroke volume n If low Inadequate volume (hypovolemia) n Impaired ventricular contraction (ischemia/infarction) n Increased SVR (drugs) n Valve dysfunction (MVR) n n If high n Low vascular resistance (sepsis, drugs)
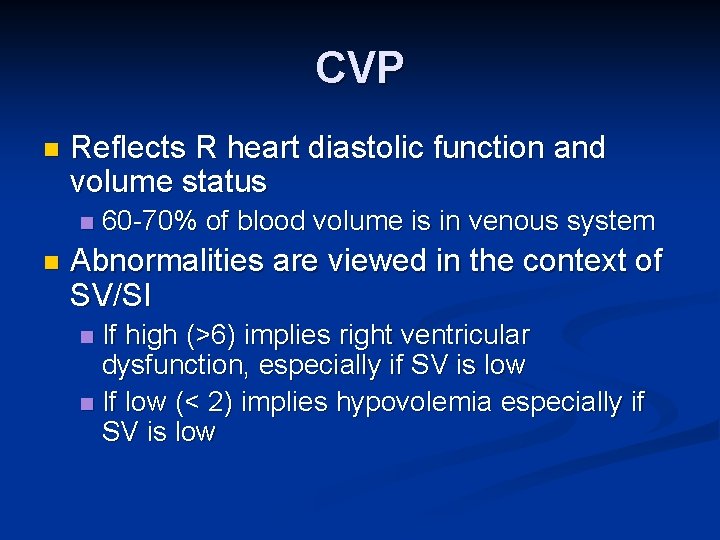
CVP n Reflects R heart diastolic function and volume status n n 60 -70% of blood volume is in venous system Abnormalities are viewed in the context of SV/SI If high (>6) implies right ventricular dysfunction, especially if SV is low n If low (< 2) implies hypovolemia especially if SV is low n
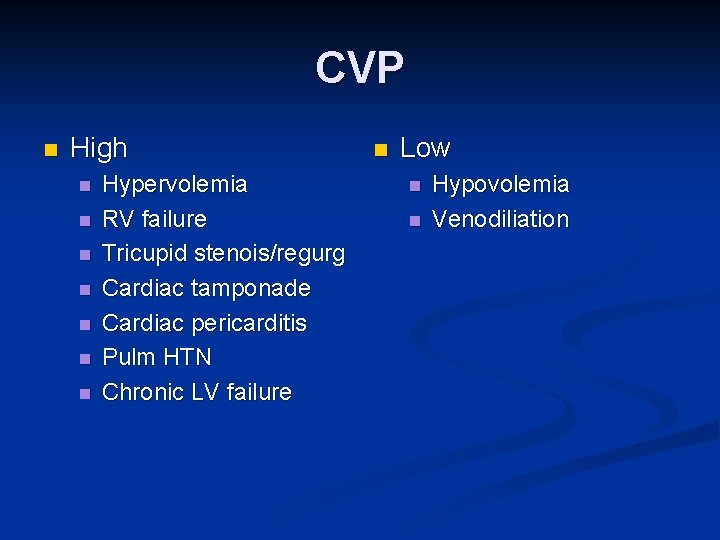
CVP n High n n n n Hypervolemia RV failure Tricupid stenois/regurg Cardiac tamponade Cardiac pericarditis Pulm HTN Chronic LV failure n Low n n Hypovolemia Venodiliation
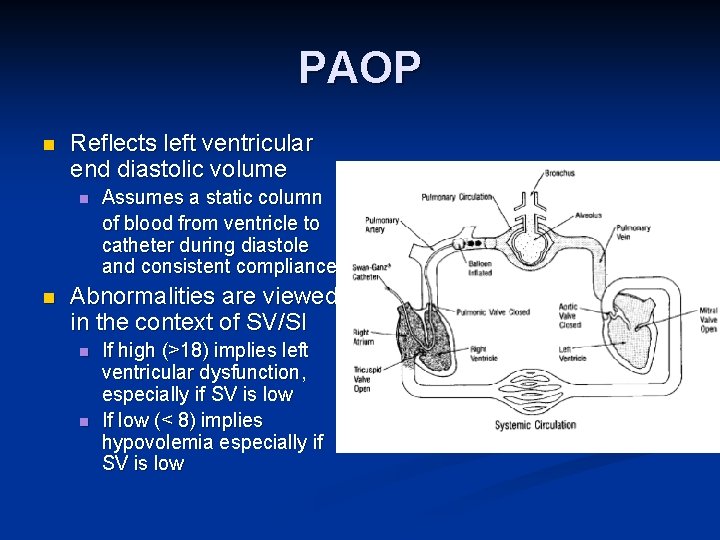
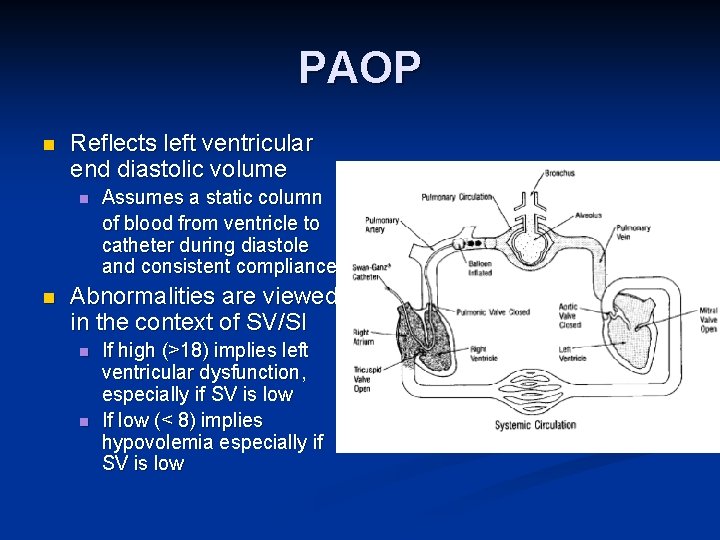
PAOP n Reflects left ventricular end diastolic volume n n Assumes a static column of blood from ventricle to catheter during diastole and consistent compliance Abnormalities are viewed in the context of SV/SI n n If high (>18) implies left ventricular dysfunction, especially if SV is low If low (< 8) implies hypovolemia especially if SV is low
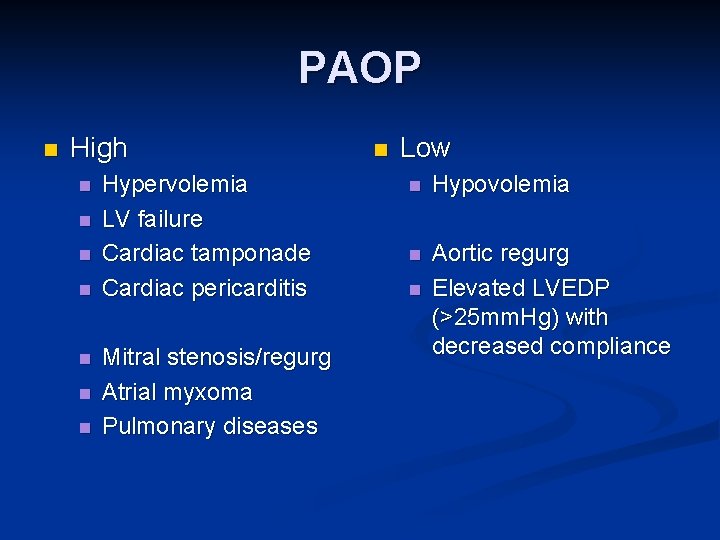
PAOP n High n n n n Hypervolemia LV failure Cardiac tamponade Cardiac pericarditis Mitral stenosis/regurg Atrial myxoma Pulmonary diseases n Low n Hypovolemia n Aortic regurg Elevated LVEDP (>25 mm. Hg) with decreased compliance n
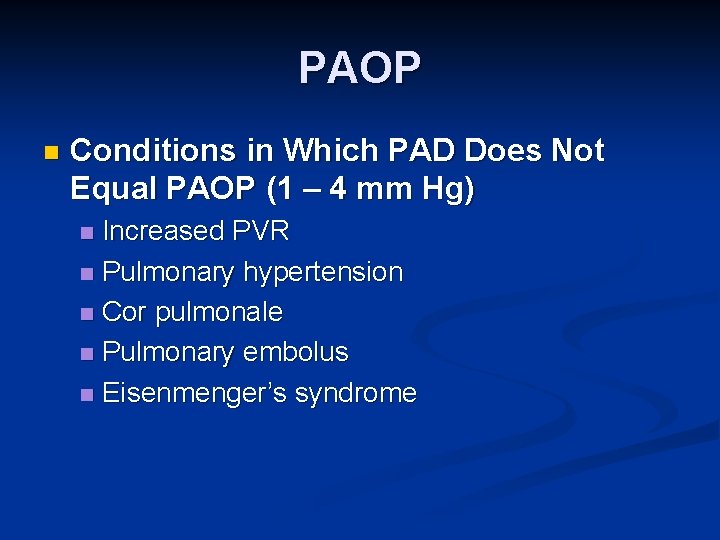
PAOP n Conditions in Which PAD Does Not Equal PAOP (1 – 4 mm Hg) Increased PVR n Pulmonary hypertension n Cor pulmonale n Pulmonary embolus n Eisenmenger’s syndrome n
Filling Pressures n If low, but other parameters are normal may only require observation If CO/CI are also low, treatment may be warranted n If Sv. O 2 and/or SV/SI are also low treatment is needed n Pulmonary congestion also warrants treatment n
S v. O 2 Reflects the balance between oxygen delivery and utilization n The larger the abnormality, the greater the risk of hypoxemia n Remember: a normal or high Sv. O 2 may represent a threat to tissue oxygenation n
S v. O 2 n A low Sv. O 2 usually warrants investigation n Evaluate: n SV/SI n May require treatment, even if CVP/PAOP are normal n Hb/Hct n Sa. O 2 (>90%) n Reasons for oxygen consumption to be elevated n Abnormally high Sv. O 2 may be indicative of a septal defect
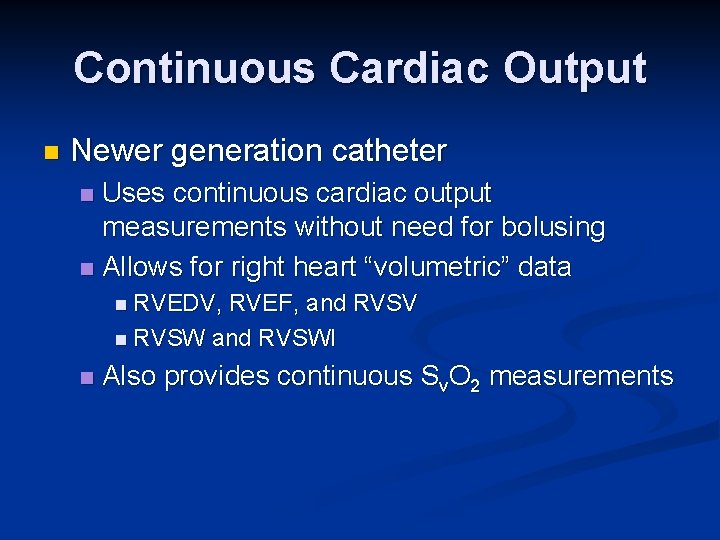
Continuous Cardiac Output n Newer generation catheter Uses continuous cardiac output measurements without need for bolusing n Allows for right heart “volumetric” data n n RVEDV, RVEF, and RVSV n RVSW and RVSWI n Also provides continuous Sv. O 2 measurements
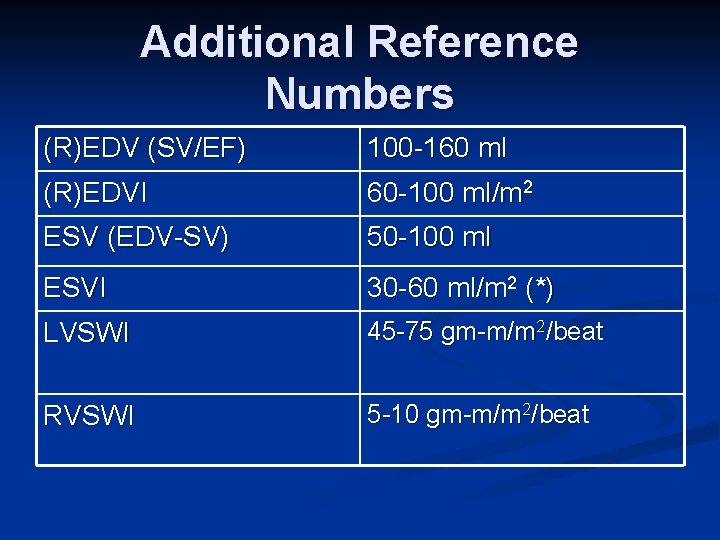
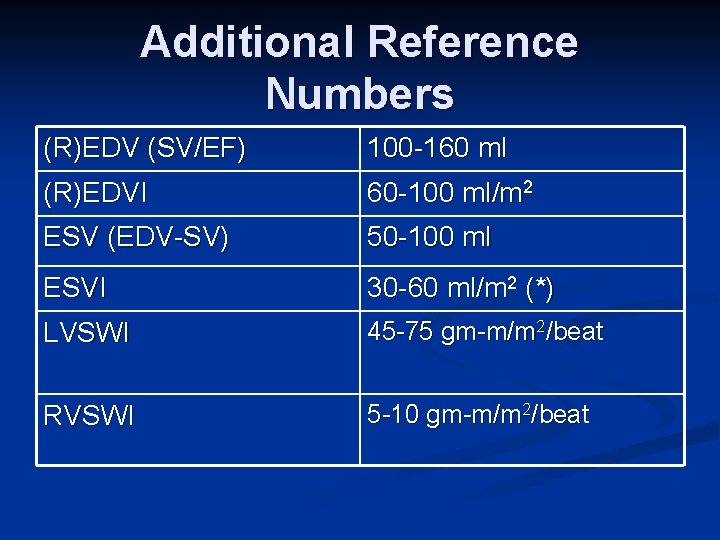
Additional Reference Numbers (R)EDV (SV/EF) 100 -160 ml (R)EDVI 60 -100 ml/m 2 ESV (EDV-SV) 50 -100 ml ESVI 30 -60 ml/m 2 (*) LVSWI 45 -75 gm-m/m 2/beat RVSWI 5 -10 gm-m/m 2/beat
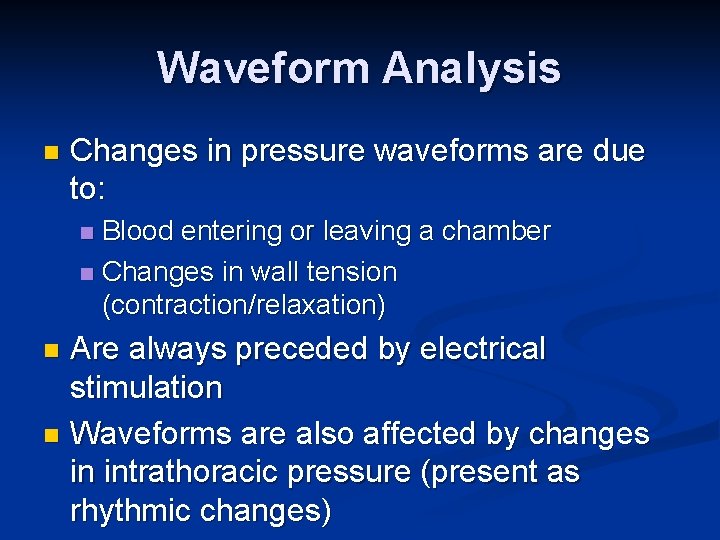
Waveform Analysis n Changes in pressure waveforms are due to: Blood entering or leaving a chamber n Changes in wall tension (contraction/relaxation) n Are always preceded by electrical stimulation n Waveforms are also affected by changes in intrathoracic pressure (present as rhythmic changes) n
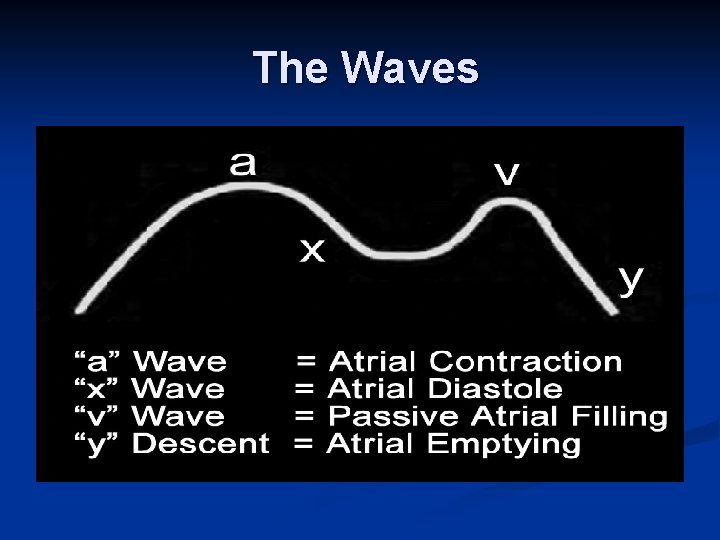
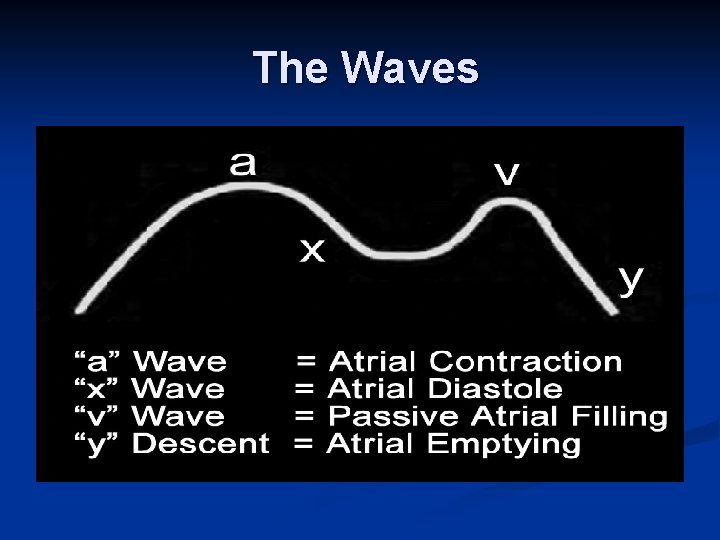
The Waves
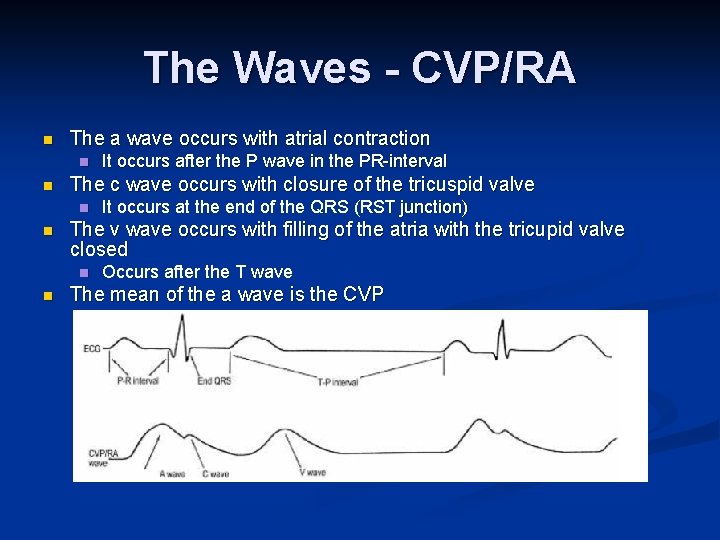
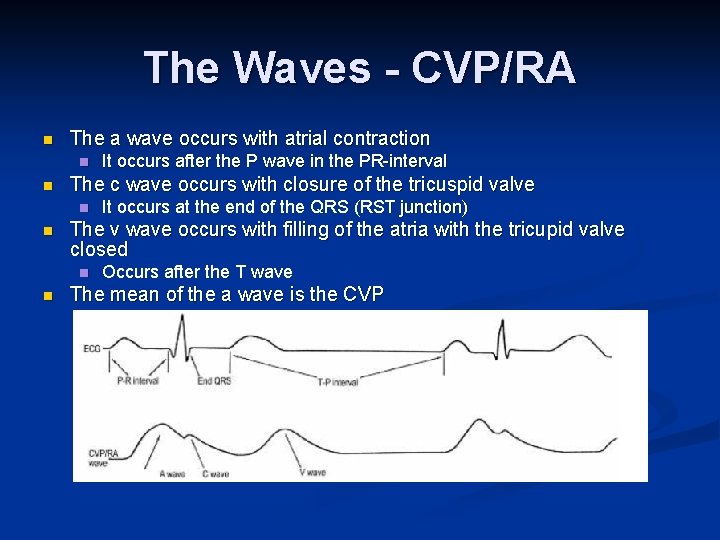
The Waves - CVP/RA n The a wave occurs with atrial contraction n n The c wave occurs with closure of the tricuspid valve n n It occurs at the end of the QRS (RST junction) The v wave occurs with filling of the atria with the tricupid valve closed n n It occurs after the P wave in the PR-interval Occurs after the T wave The mean of the a wave is the CVP
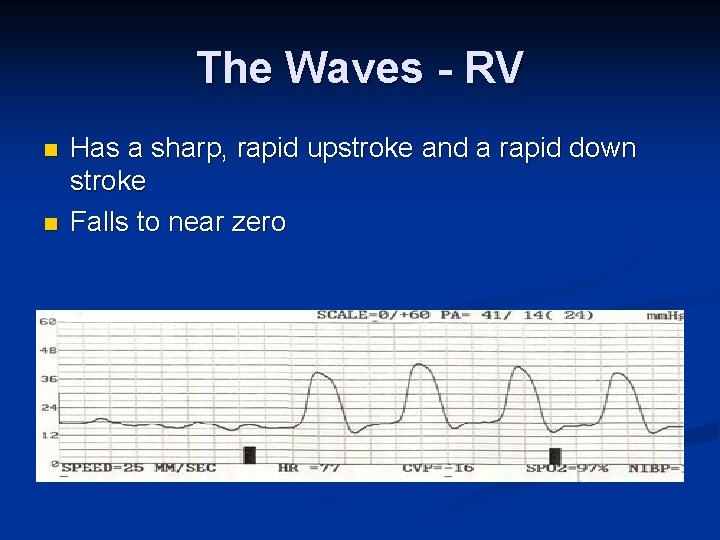
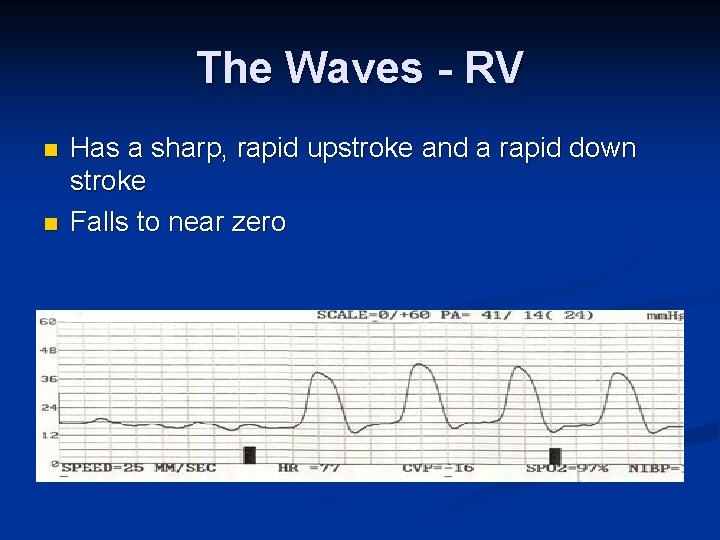
The Waves - RV n n Has a sharp, rapid upstroke and a rapid down stroke Falls to near zero
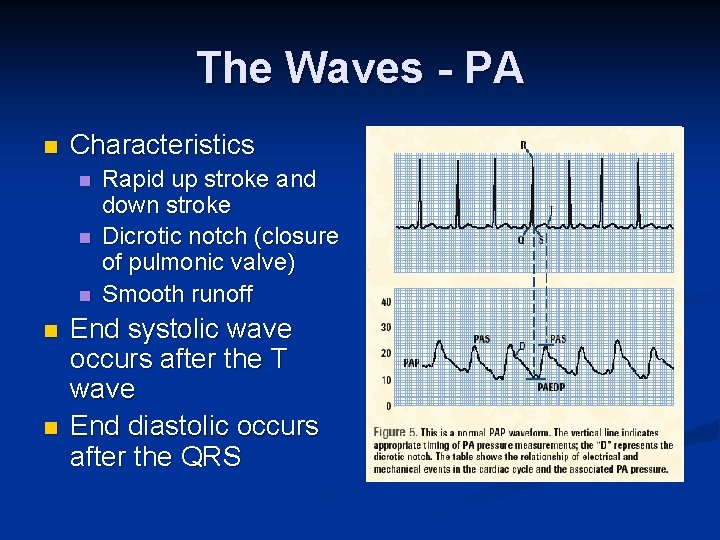
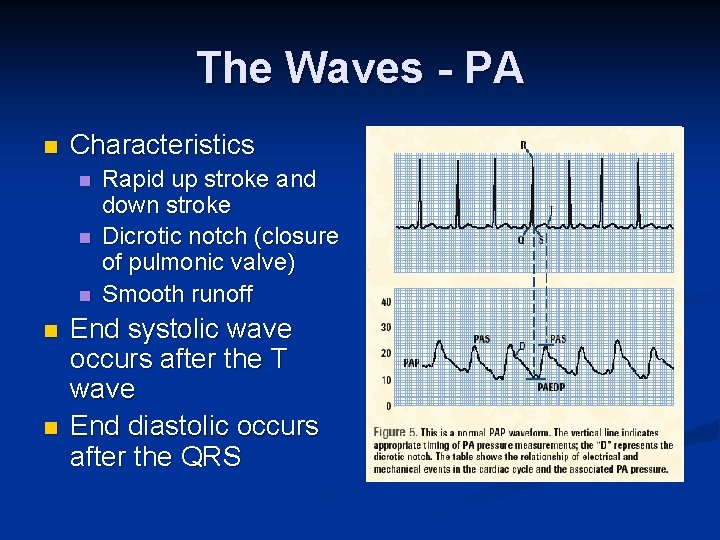
The Waves - PA n Characteristics n n n Rapid up stroke and down stroke Dicrotic notch (closure of pulmonic valve) Smooth runoff End systolic wave occurs after the T wave End diastolic occurs after the QRS
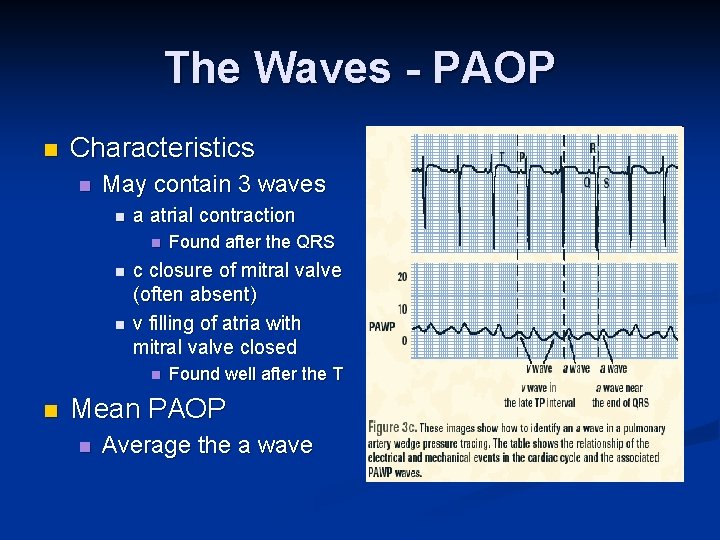
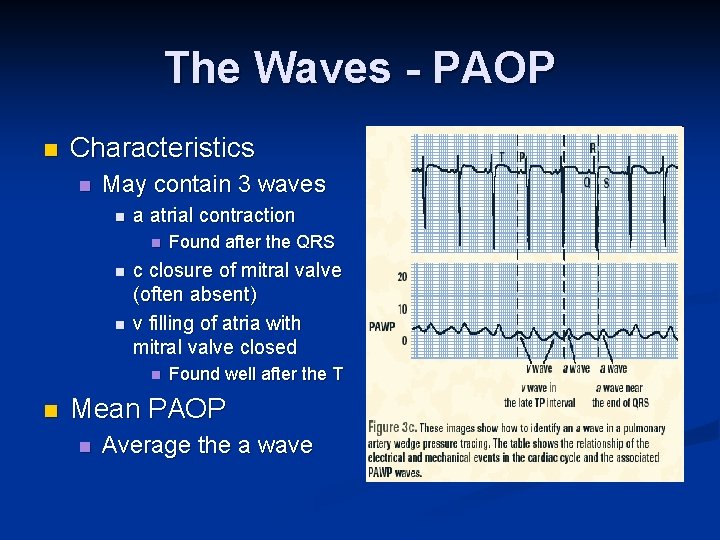
The Waves - PAOP n Characteristics n May contain 3 waves n a atrial contraction n c closure of mitral valve (often absent) v filling of atria with mitral valve closed n n Found after the QRS Found well after the T Mean PAOP n Average the a wave
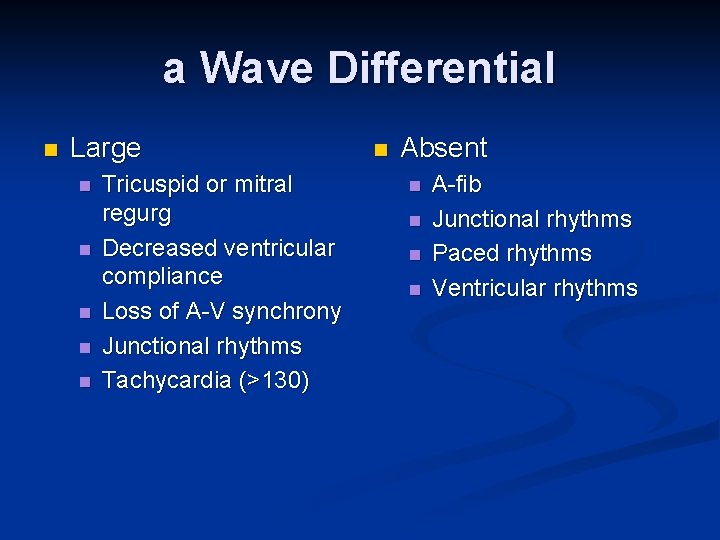
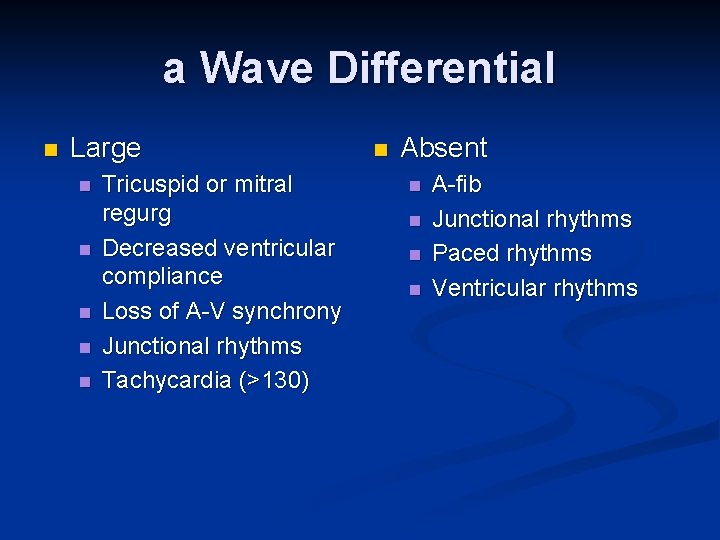
a Wave Differential n Large n n n Tricuspid or mitral regurg Decreased ventricular compliance Loss of A-V synchrony Junctional rhythms Tachycardia (>130) n Absent n n A-fib Junctional rhythms Paced rhythms Ventricular rhythms
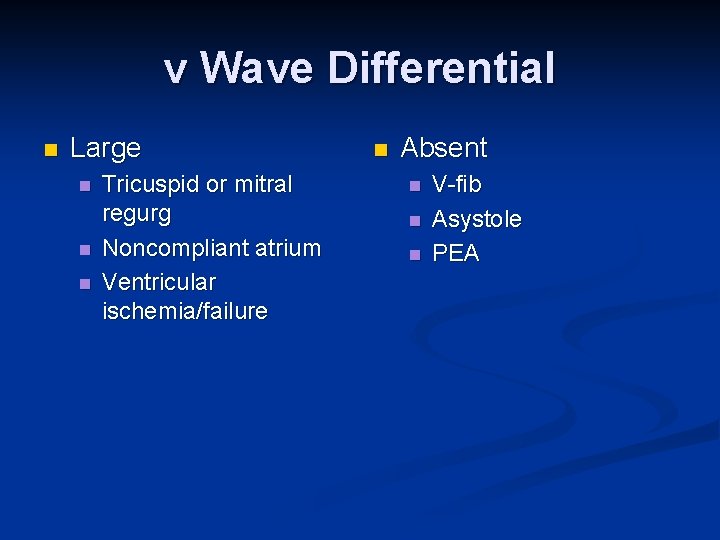
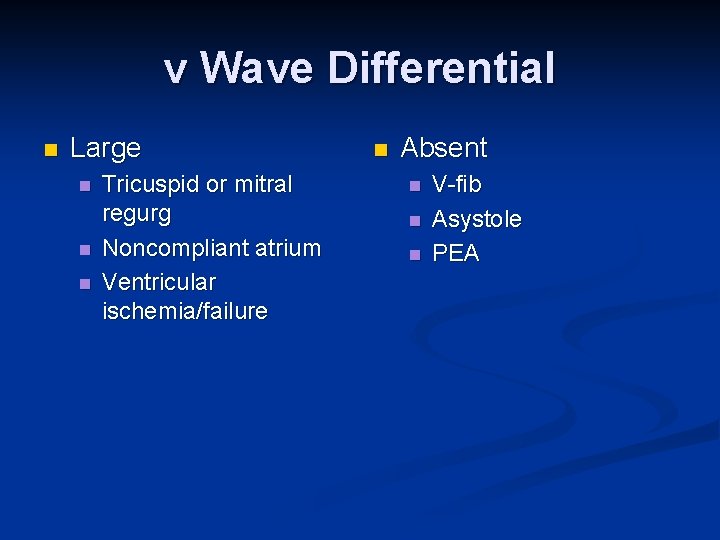
v Wave Differential n Large n n n Tricuspid or mitral regurg Noncompliant atrium Ventricular ischemia/failure n Absent n n n V-fib Asystole PEA
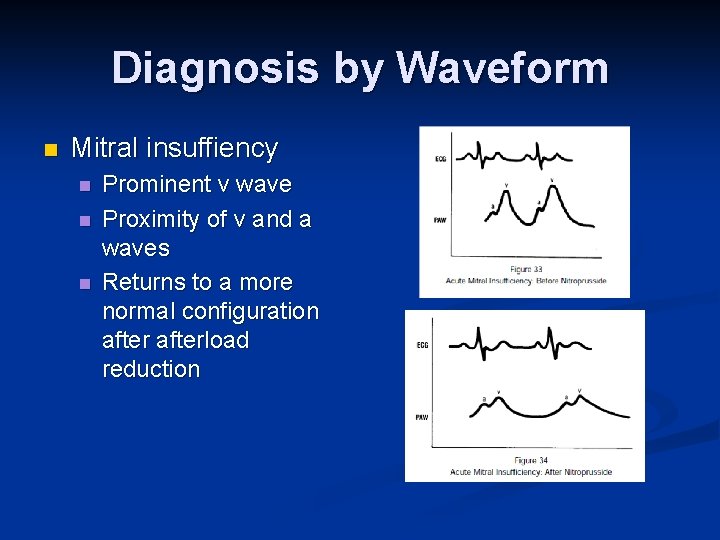
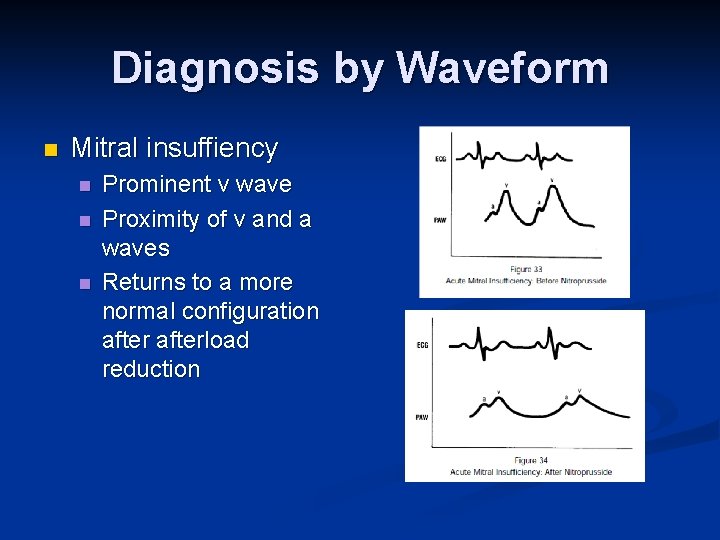
Diagnosis by Waveform n Mitral insuffiency n n n Prominent v wave Proximity of v and a waves Returns to a more normal configuration afterload reduction
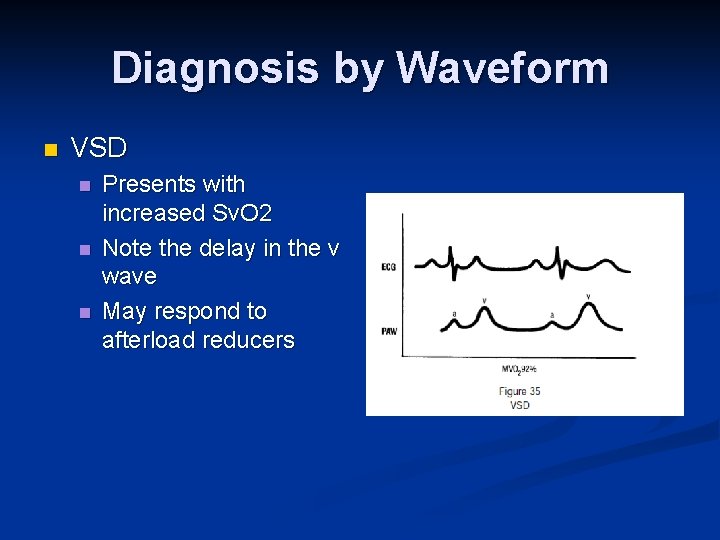
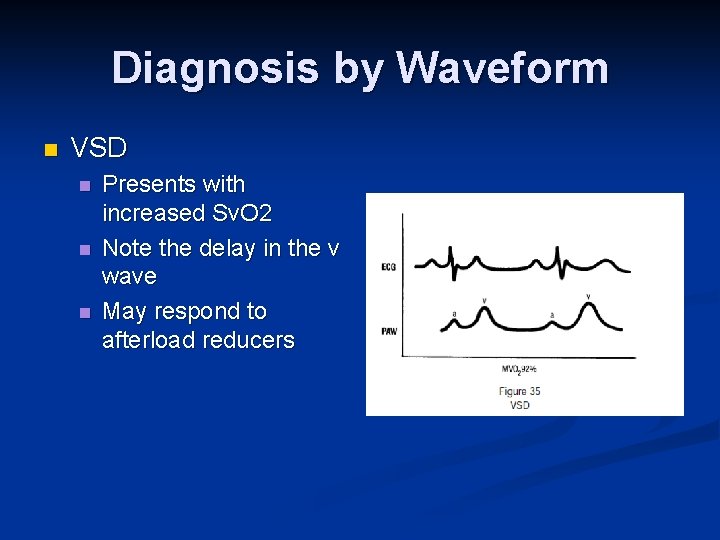
Diagnosis by Waveform n VSD n n n Presents with increased Sv. O 2 Note the delay in the v wave May respond to afterload reducers
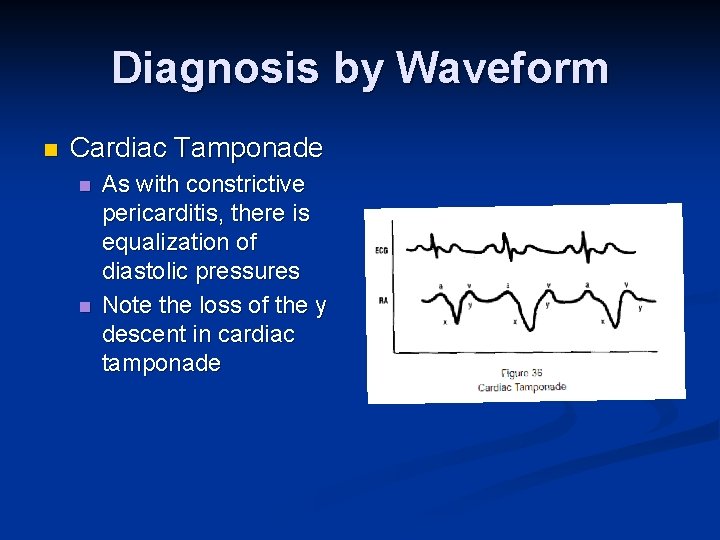
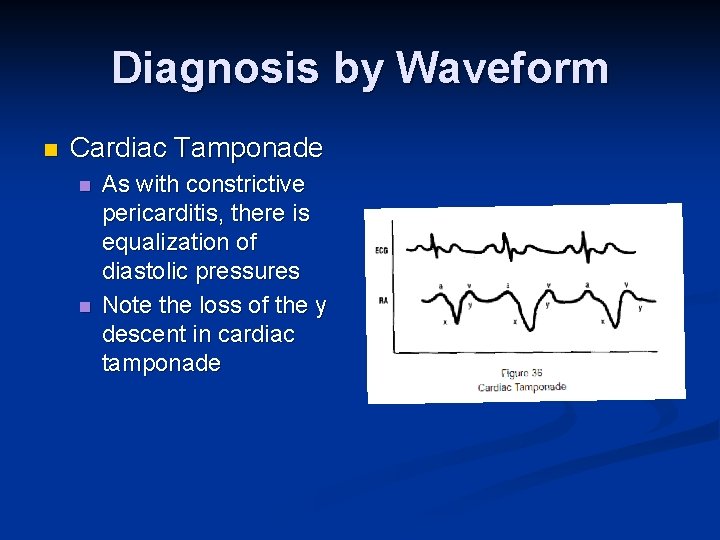
Diagnosis by Waveform n Cardiac Tamponade n n As with constrictive pericarditis, there is equalization of diastolic pressures Note the loss of the y descent in cardiac tamponade
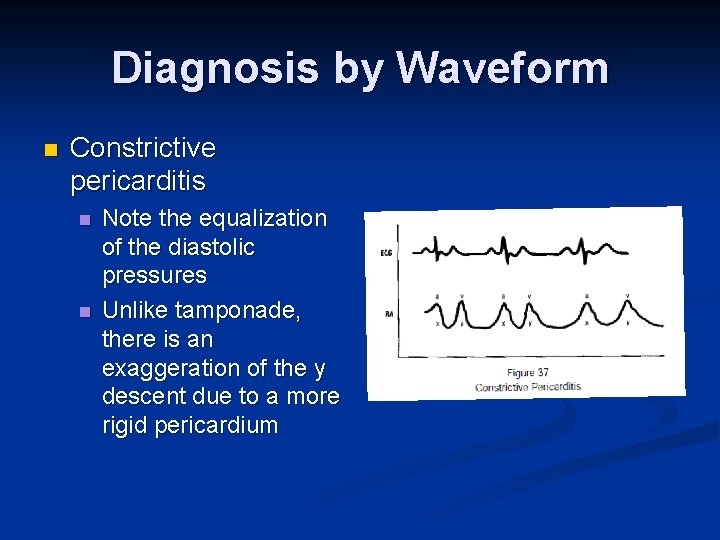
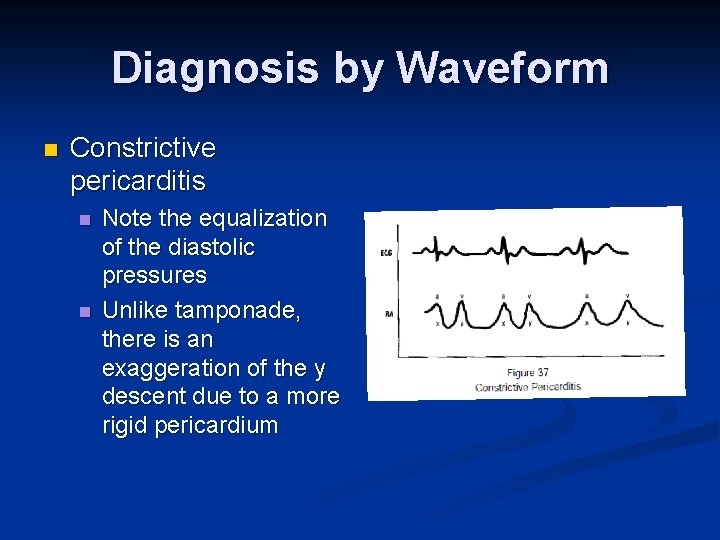
Diagnosis by Waveform n Constrictive pericarditis n n Note the equalization of the diastolic pressures Unlike tamponade, there is an exaggeration of the y descent due to a more rigid pericardium
Points to remember n Intrathoracic pressure during inhalation and exhalation cause pressures in the heart to vary n Therefore all pressures should be measured at end-expiration when intrathoracic pressure is closest to zero
Points to Remember n Limitations in hemodynamic monitoring n Ventricular filling pressures do not always accurately reflect ventricular filling volume n n n The PAOP is normally slightly (1 -5 mm Hg) less than the PAD pressure n n n The pressure-volume relationship depends upon ventricular compliance If compliance changes, the pressure-volume relationship changes This relationship stills exists with pulm hypertension due to LV failure However, with an ↑ PVR or tachycardia (>125 bpm) this relationship may breakdown and the PAD becomes significantly higher than the PAOP The PAOP may not equal LVEDP when n n there is high alveolar pressures when the catheter tip is above the left atrium severe hypovolemia tachycardia (130 bpm) in mitral stenosis.
Points to remember n Calculated variables (e. g. SVR, PVR & SV/SI) are limited in value due to assumptions made in their calculations
Complications n Air embolism n n n Arrhythmias n n n S&S: hypoxemia, cyanosis, hypotension/syncope, “machinery murmur”, elevated CVP, arrest Tx: place in left lateral trendelenburg, Fi. O 2 of 100%, attempt aspiration of air, CPR Prevention: keep balloon inflated, minimize insertion time Tx: removal of catheter, ACLS Heart blocks n n Typically RBBB occurs, so avoid PACs in LBBB Tx: transvenous/transcutaneous pacers, PACs with pacer
Complications n Knotting n n n Prevention: minimize insertion time, avoid pushing agaist resistance, verify RA to RV transition Tx: check CXR, attempt to unknot Pulmonary artery rupture n n n S&S: hypoxemia, hemoptysis, circ collapse Prevention: withdraw PAC if spontaneously wedges or wedges with < 1. 25 cc of air Tx: stop anti-coagulation, affected side down, selective bronchial intubation, PEEP, surgical repair (CPB or ECMO)
Complications n Pulmonary infarction n Prevention n n n Avoid distal positioning of catheter Check CXR Monitor PA EDP instead of PAOP Pull back if spontaneous wedge occurs Limit air in cuff (pull back if < 1. 25 cc) Tx n n n CXR Check cath position, deflate and withdraw Observe
Complications n Infection n Prevention! n n n n Aseptic technique Dead-end caps Sterile sleeve (swandom) Minimize entry into system Avoid glucose containing fluid Avoid over changing of tubing, etc (72 -96 hr) Remove catheter ASAP Thrombus n n Prevention – continuous flush +/- heparin Tx – lytic agent ; remove catheter
Emerging Technology n Devices exist that use arterial pressure waveform to continuously measure cardiac output n n n Variations of the arterial pressure are proportional to stroke volume Several studies demonstrate that SVV has a high sensitivity and specificity in determining if a patient will respond (increasing SV) when given volume (“preload responsiveness”) Limitations n n Only used in mechanically ventilated pts Wildly inaccurate when arrhythmias are present
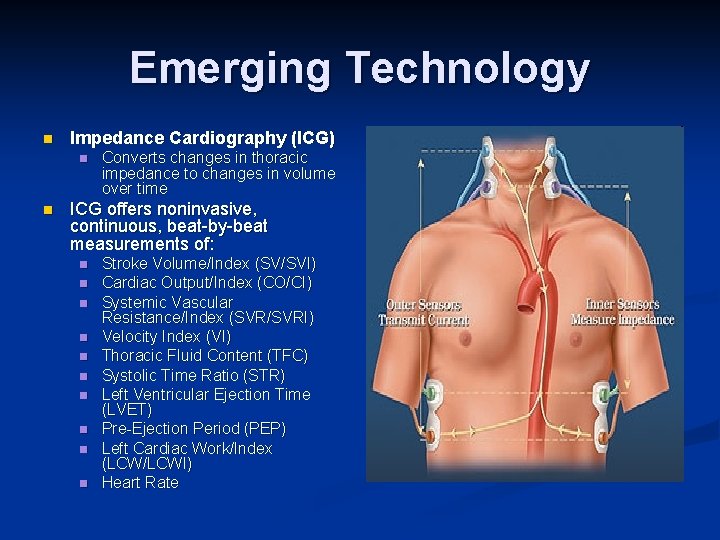
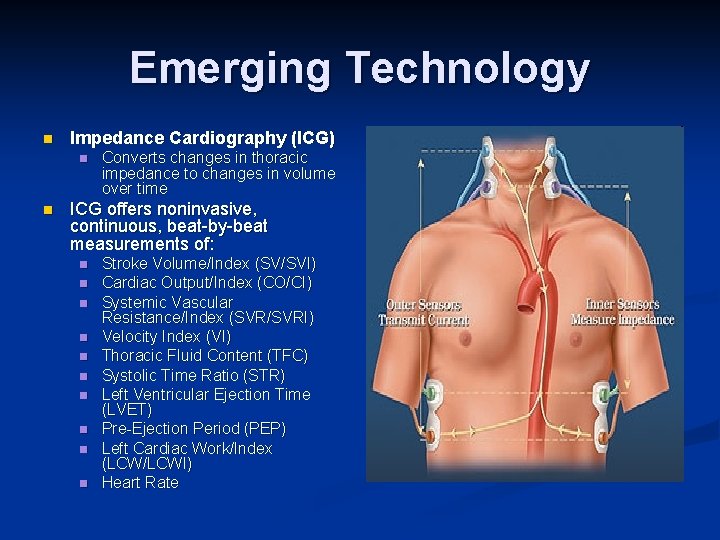
Emerging Technology n Impedance Cardiography (ICG) n n Converts changes in thoracic impedance to changes in volume over time ICG offers noninvasive, continuous, beat-by-beat measurements of: n n n n n Stroke Volume/Index (SV/SVI) Cardiac Output/Index (CO/CI) Systemic Vascular Resistance/Index (SVR/SVRI) Velocity Index (VI) Thoracic Fluid Content (TFC) Systolic Time Ratio (STR) Left Ventricular Ejection Time (LVET) Pre-Ejection Period (PEP) Left Cardiac Work/Index (LCW/LCWI) Heart Rate
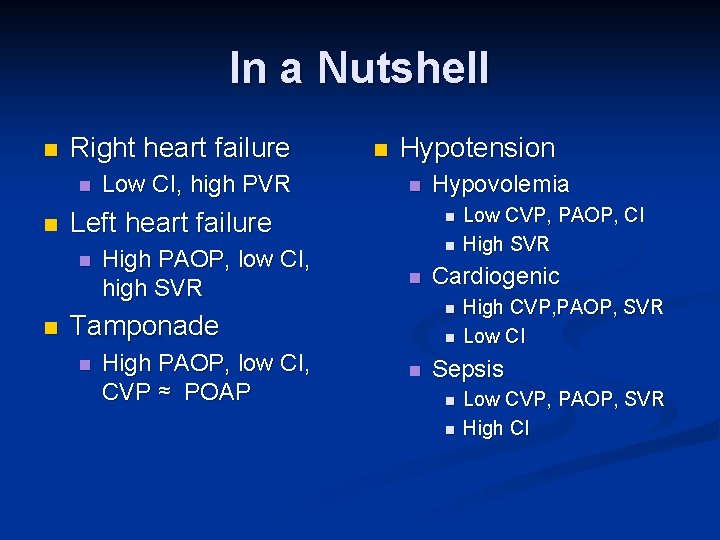
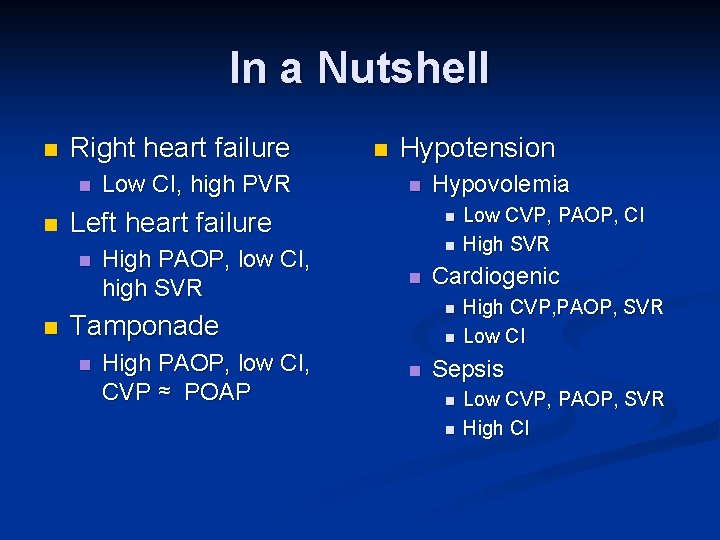
In a Nutshell n Right heart failure n n Hypotension n Left heart failure n n Low CI, high PVR n High PAOP, low CI, high SVR n n n High PAOP, low CI, CVP ≈ POAP n n Low CVP, PAOP, CI High SVR Cardiogenic n Tamponade n Hypovolemia High CVP, PAOP, SVR Low CI Sepsis n n Low CVP, PAOP, SVR High CI
References n Pulmonary Artery Catheter Education Project n http: //www. pacep. org n Chatterjee, The Swan-Ganz Catheters: Past, Present, and Future: A Viewpoint. Circulation 2009; 119; 147 -152 n Edwards Scientific n http: //ht. edwards. com/presentationvideos/powerpoint/strokevolumevaria tion/strokevolumevariation. pdf
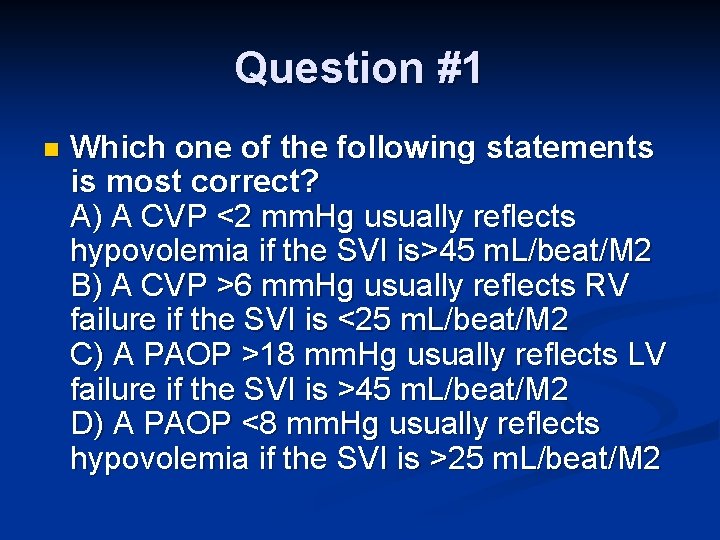
Question #1 n Which one of the following statements is most correct? A) A CVP <2 mm. Hg usually reflects hypovolemia if the SVI is>45 m. L/beat/M 2 B) A CVP >6 mm. Hg usually reflects RV failure if the SVI is <25 m. L/beat/M 2 C) A PAOP >18 mm. Hg usually reflects LV failure if the SVI is >45 m. L/beat/M 2 D) A PAOP <8 mm. Hg usually reflects hypovolemia if the SVI is >25 m. L/beat/M 2
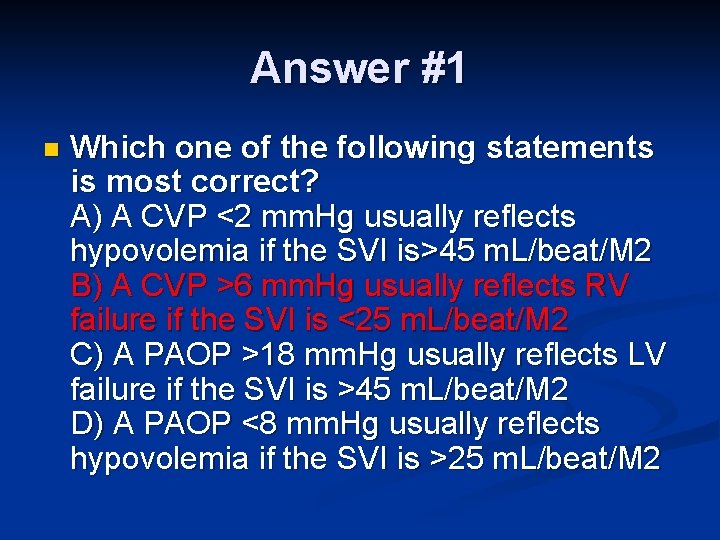
Answer #1 n Which one of the following statements is most correct? A) A CVP <2 mm. Hg usually reflects hypovolemia if the SVI is>45 m. L/beat/M 2 B) A CVP >6 mm. Hg usually reflects RV failure if the SVI is <25 m. L/beat/M 2 C) A PAOP >18 mm. Hg usually reflects LV failure if the SVI is >45 m. L/beat/M 2 D) A PAOP <8 mm. Hg usually reflects hypovolemia if the SVI is >25 m. L/beat/M 2
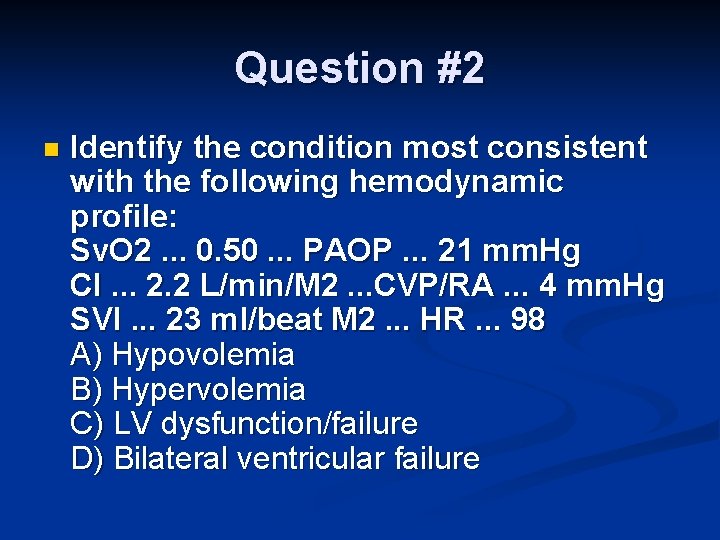
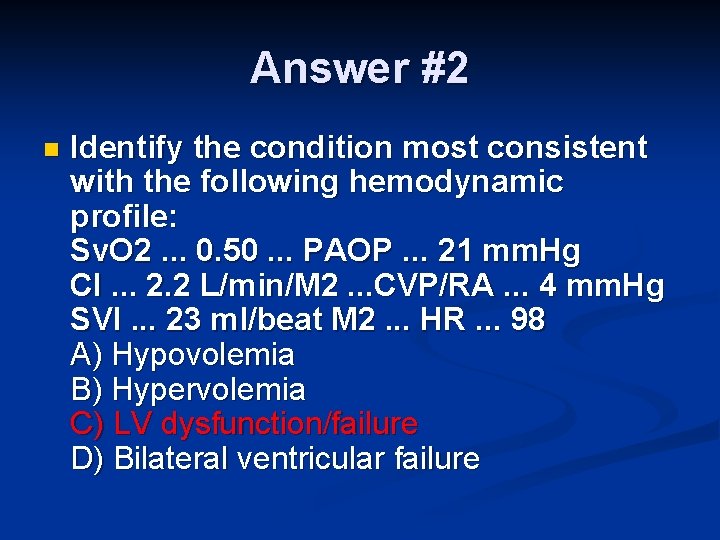
Question #2 n Identify the condition most consistent with the following hemodynamic profile: Sv. O 2. . . 0. 50. . . PAOP. . . 21 mm. Hg CI. . . 2. 2 L/min/M 2. . . CVP/RA. . . 4 mm. Hg SVI. . . 23 ml/beat M 2. . . HR. . . 98 A) Hypovolemia B) Hypervolemia C) LV dysfunction/failure D) Bilateral ventricular failure
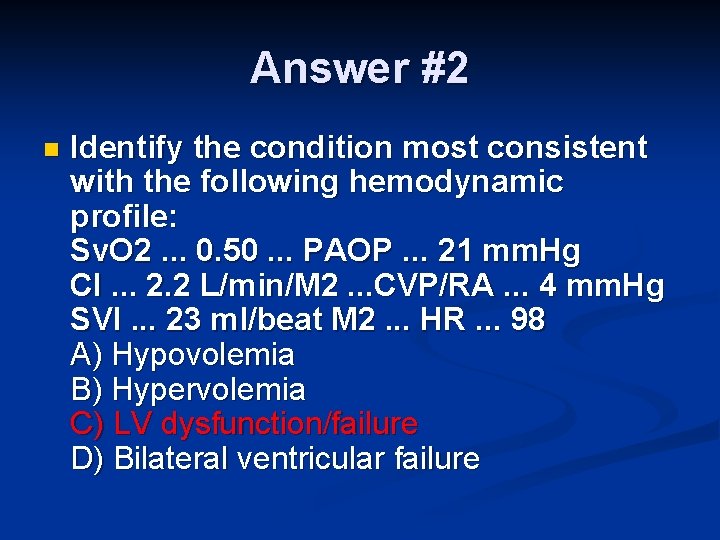
Answer #2 n Identify the condition most consistent with the following hemodynamic profile: Sv. O 2. . . 0. 50. . . PAOP. . . 21 mm. Hg CI. . . 2. 2 L/min/M 2. . . CVP/RA. . . 4 mm. Hg SVI. . . 23 ml/beat M 2. . . HR. . . 98 A) Hypovolemia B) Hypervolemia C) LV dysfunction/failure D) Bilateral ventricular failure
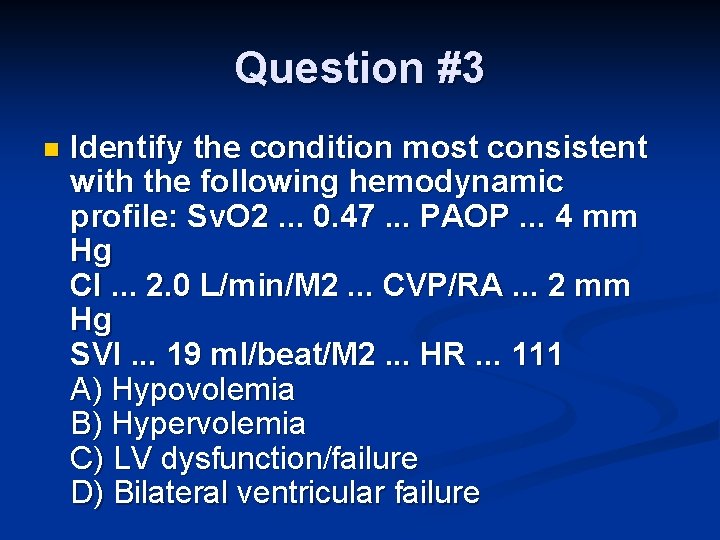
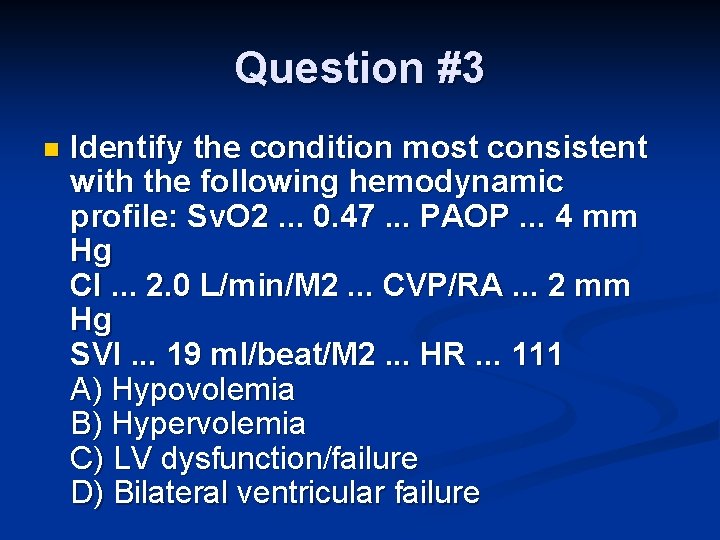
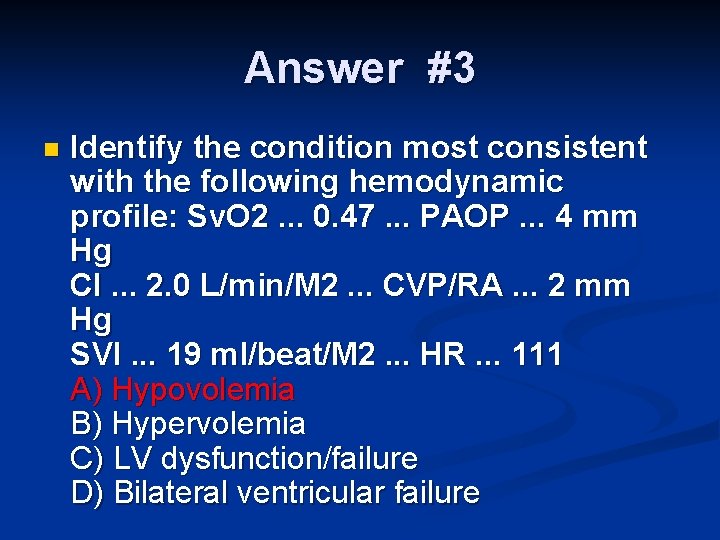
Question #3 n Identify the condition most consistent with the following hemodynamic profile: Sv. O 2. . . 0. 47. . . PAOP. . . 4 mm Hg CI. . . 2. 0 L/min/M 2. . . CVP/RA. . . 2 mm Hg SVI. . . 19 ml/beat/M 2. . . HR. . . 111 A) Hypovolemia B) Hypervolemia C) LV dysfunction/failure D) Bilateral ventricular failure
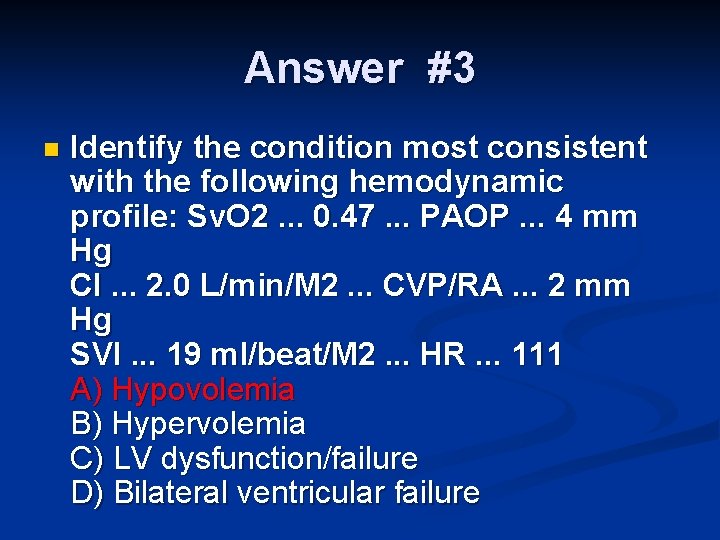
Answer #3 n Identify the condition most consistent with the following hemodynamic profile: Sv. O 2. . . 0. 47. . . PAOP. . . 4 mm Hg CI. . . 2. 0 L/min/M 2. . . CVP/RA. . . 2 mm Hg SVI. . . 19 ml/beat/M 2. . . HR. . . 111 A) Hypovolemia B) Hypervolemia C) LV dysfunction/failure D) Bilateral ventricular failure
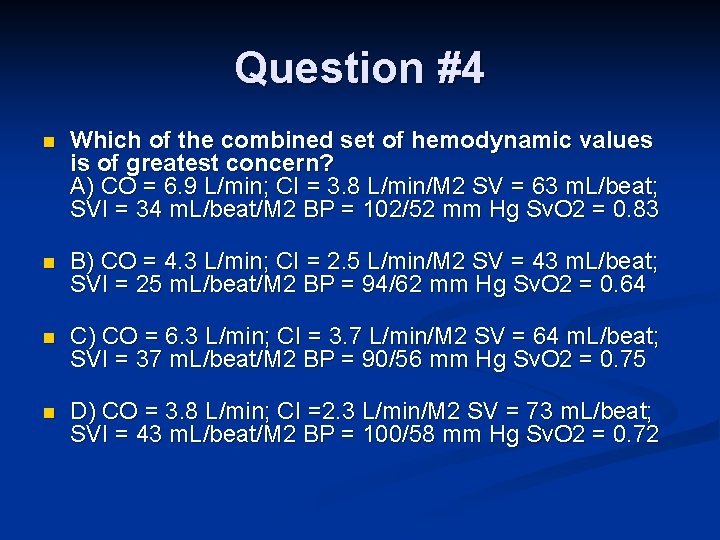
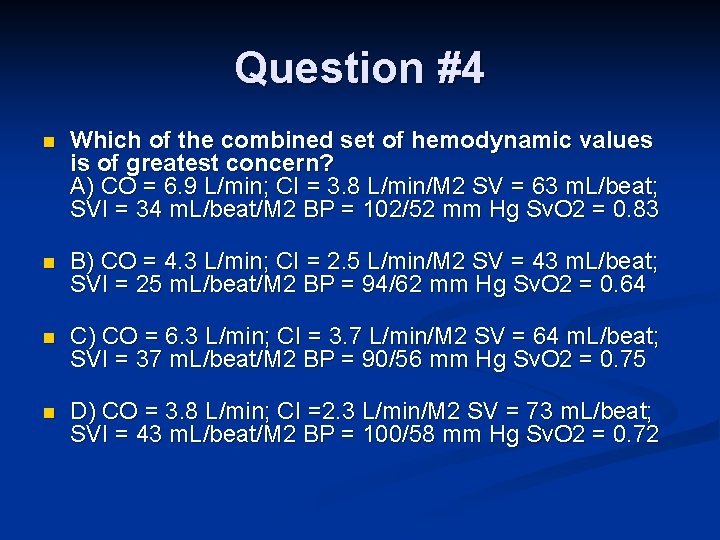
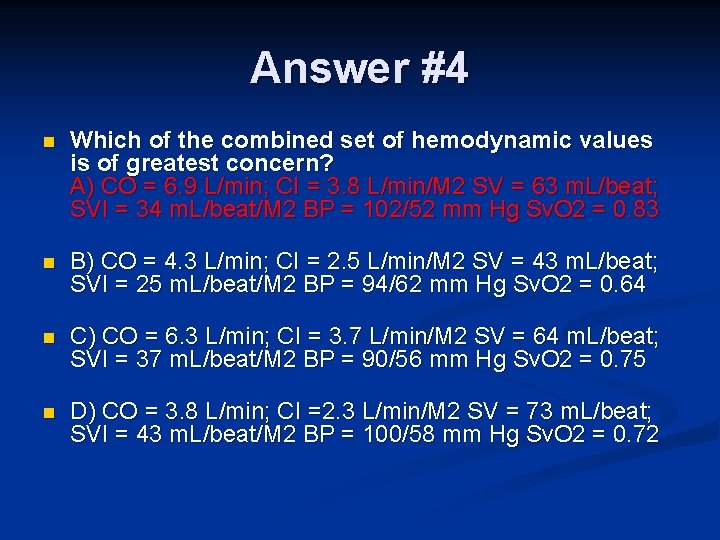
Question #4 n Which of the combined set of hemodynamic values is of greatest concern? A) CO = 6. 9 L/min; CI = 3. 8 L/min/M 2 SV = 63 m. L/beat; SVI = 34 m. L/beat/M 2 BP = 102/52 mm Hg Sv. O 2 = 0. 83 n B) CO = 4. 3 L/min; CI = 2. 5 L/min/M 2 SV = 43 m. L/beat; SVI = 25 m. L/beat/M 2 BP = 94/62 mm Hg Sv. O 2 = 0. 64 n C) CO = 6. 3 L/min; CI = 3. 7 L/min/M 2 SV = 64 m. L/beat; SVI = 37 m. L/beat/M 2 BP = 90/56 mm Hg Sv. O 2 = 0. 75 n D) CO = 3. 8 L/min; CI =2. 3 L/min/M 2 SV = 73 m. L/beat; SVI = 43 m. L/beat/M 2 BP = 100/58 mm Hg Sv. O 2 = 0. 72
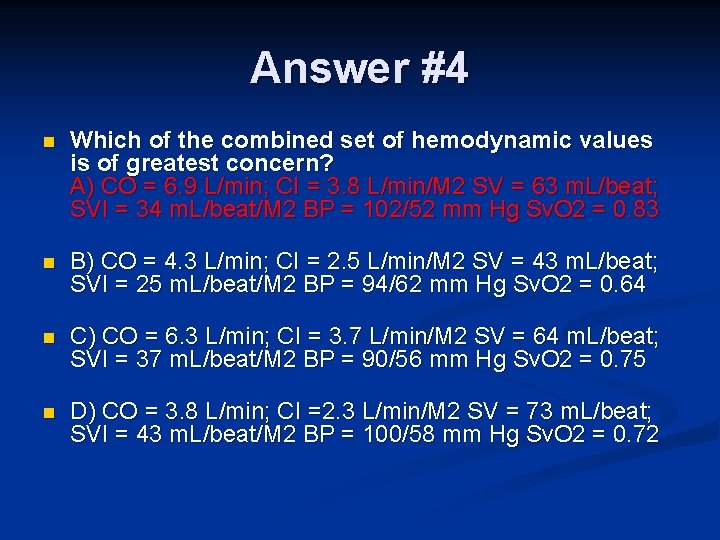
Answer #4 n Which of the combined set of hemodynamic values is of greatest concern? A) CO = 6. 9 L/min; CI = 3. 8 L/min/M 2 SV = 63 m. L/beat; SVI = 34 m. L/beat/M 2 BP = 102/52 mm Hg Sv. O 2 = 0. 83 n B) CO = 4. 3 L/min; CI = 2. 5 L/min/M 2 SV = 43 m. L/beat; SVI = 25 m. L/beat/M 2 BP = 94/62 mm Hg Sv. O 2 = 0. 64 n C) CO = 6. 3 L/min; CI = 3. 7 L/min/M 2 SV = 64 m. L/beat; SVI = 37 m. L/beat/M 2 BP = 90/56 mm Hg Sv. O 2 = 0. 75 n D) CO = 3. 8 L/min; CI =2. 3 L/min/M 2 SV = 73 m. L/beat; SVI = 43 m. L/beat/M 2 BP = 100/58 mm Hg Sv. O 2 = 0. 72
Question #5 n Immediate treatment of pulmonary artery rupture may include all of the following except: A) Discontinuation of anticoagulation B) Placing patient in lateral position with unaffected side down. C) Selective bronchial intubation D) PEEP
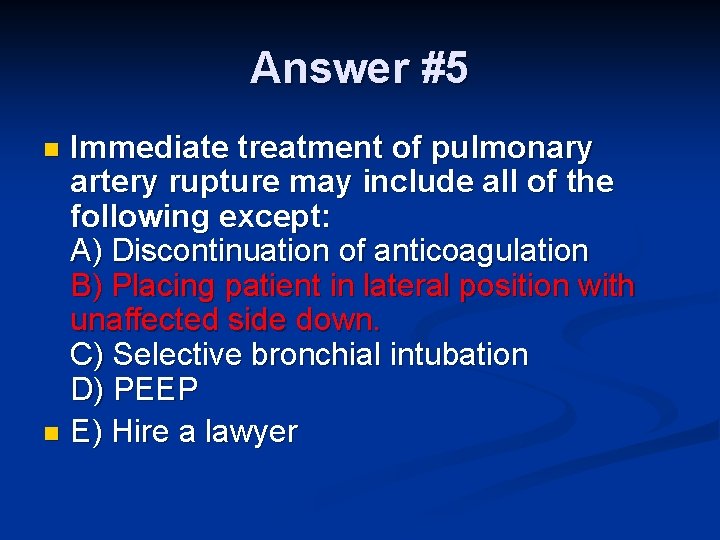
Answer #5 Immediate treatment of pulmonary artery rupture may include all of the following except: A) Discontinuation of anticoagulation B) Placing patient in lateral position with unaffected side down. C) Selective bronchial intubation D) PEEP n E) Hire a lawyer n