Sutter Care Coordination Program SCCP Supporting Patients and

- Slides: 19
Sutter Care Coordination Program (SCCP) Supporting Patients and Practitioners in Optimizing Health
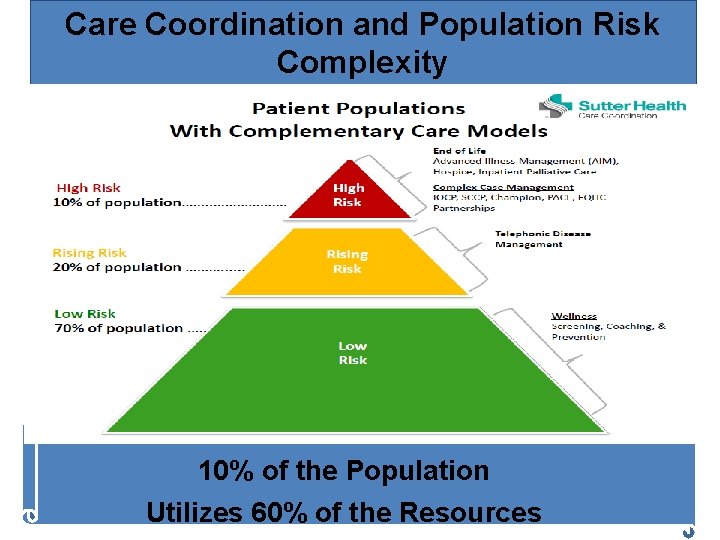
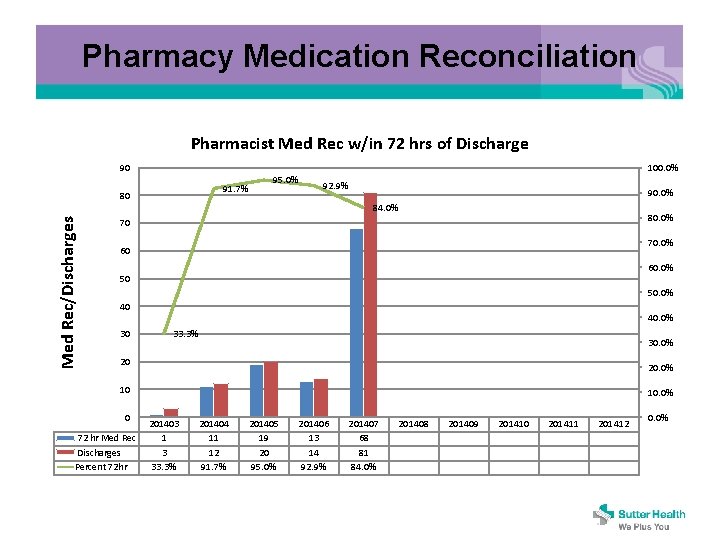
Care Coordination and Population Risk Complexity 2 10% of the Population Utilizes 60% of the Resources
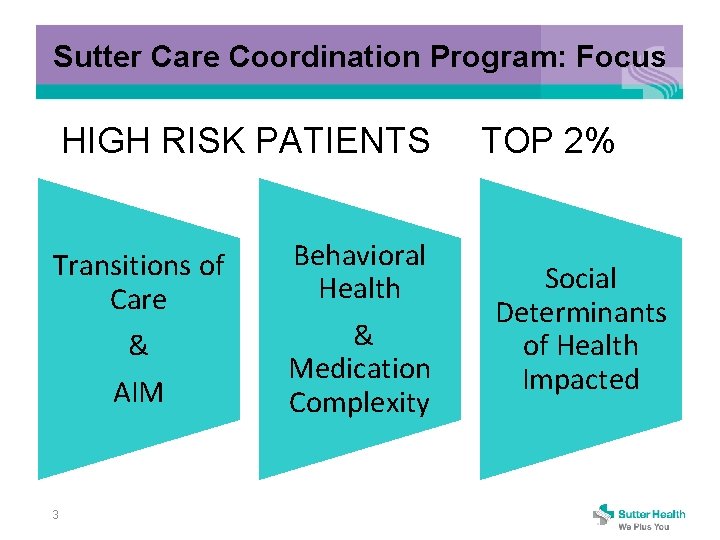
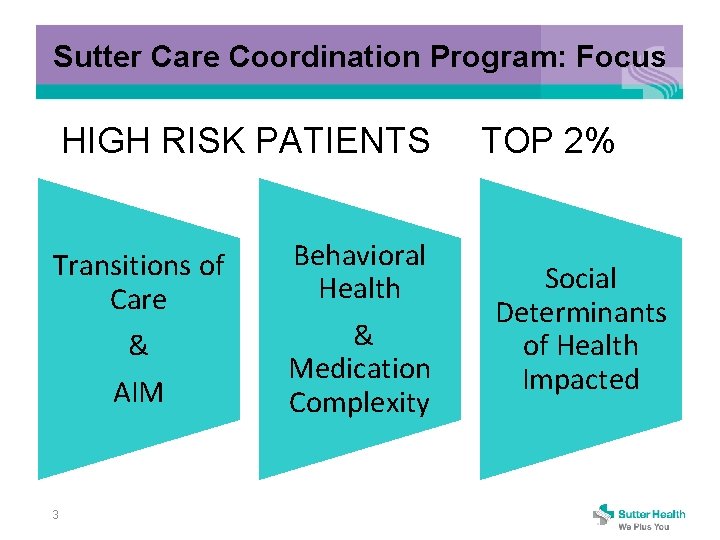
Sutter Care Coordination Program: Focus HIGH RISK PATIENTS TOP 2% Transitions of Care & AIM 3 Behavioral Health & Medication Complexity Social Determinants of Health Impacted
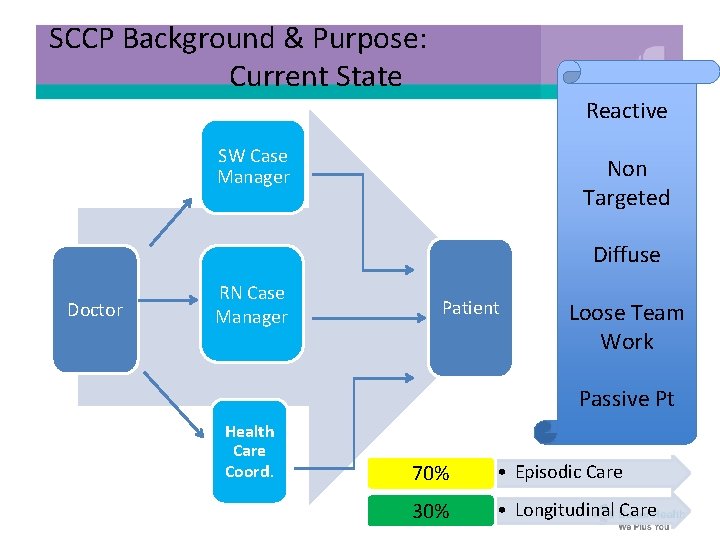
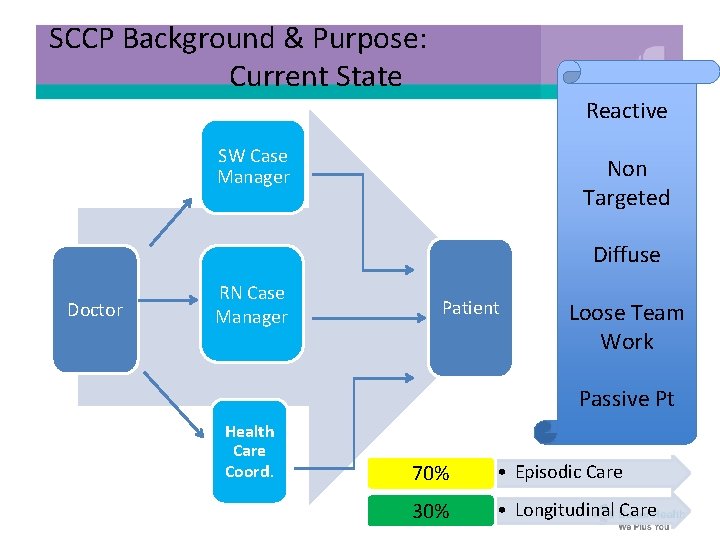
SCCP Background & Purpose: Current State Reactive SW Case Manager Non Targeted Diffuse Doctor RN Case Manager Patient Loose Team Work Passive Pt Health Care Coord. 70% • Episodic Care 30% • Longitudinal Care
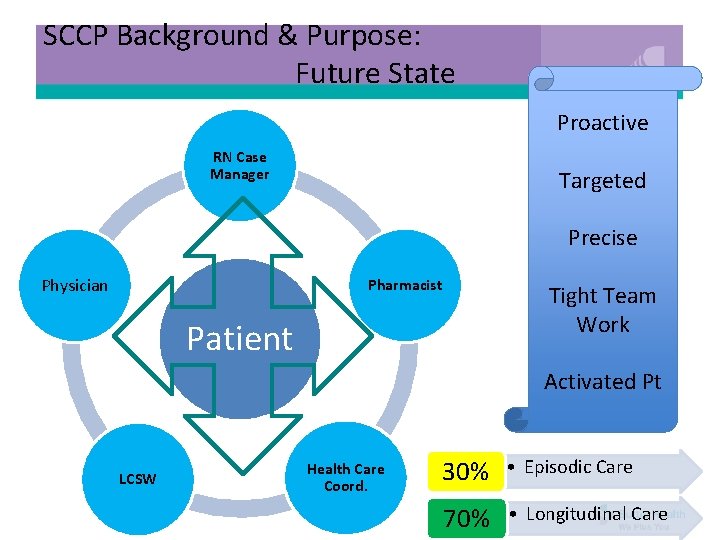
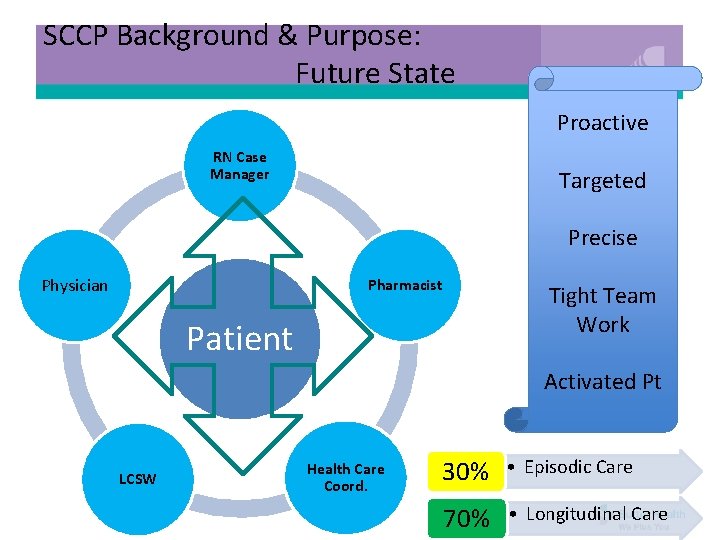
SCCP Background & Purpose: Future State Proactive RN Case Manager Targeted Precise Physician Pharmacist Tight Team Work Patient Activated Pt LCSW Health Care Coord. 30% • Episodic Care 70% • Longitudinal Care
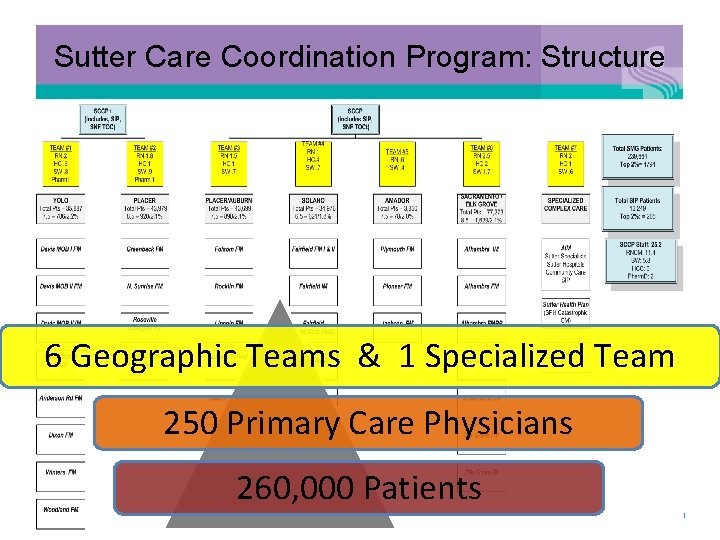
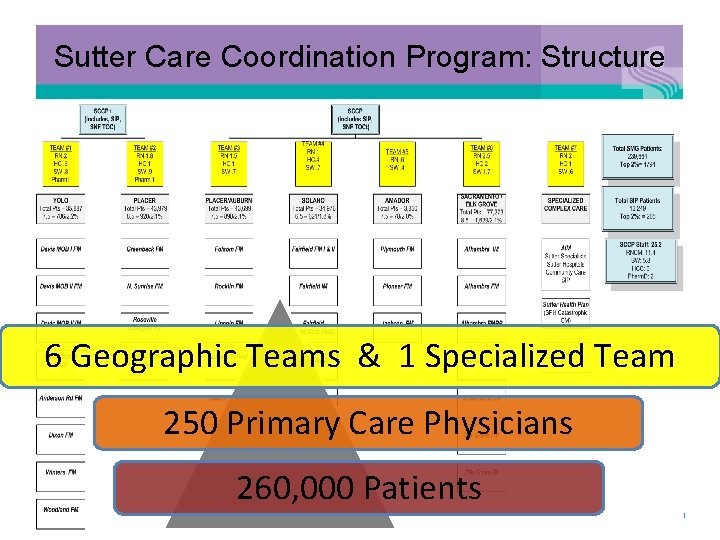
Sutter Care Coordination Program: Structure 6 Geographic Teams & 1 Specialized Team 250 Primary Care Physicians 260, 000 Patients 6
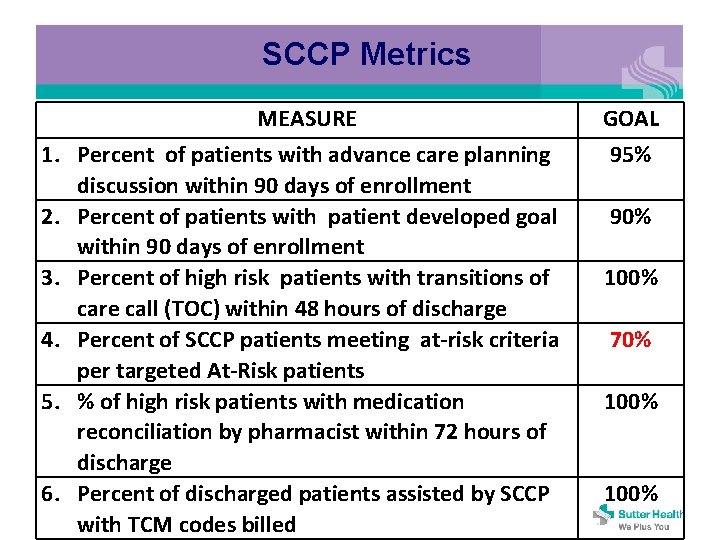
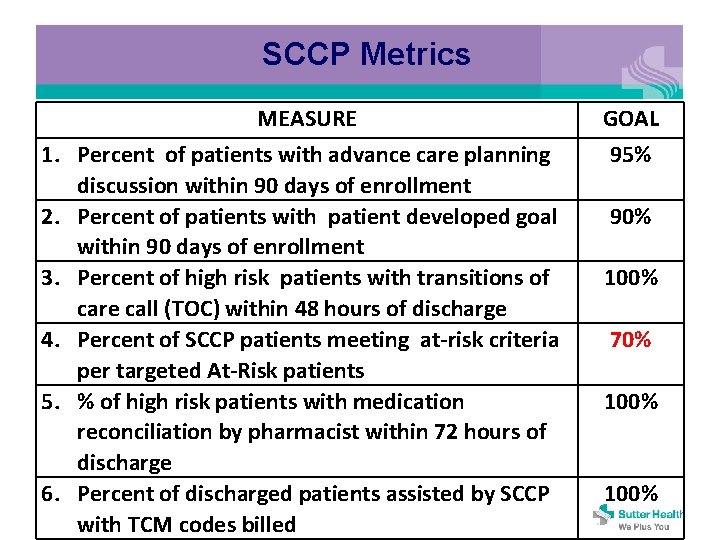
SCCP Metrics MEASURE GOAL 1. Percent of patients with advance care planning discussion within 90 days of enrollment 2. Percent of patients with patient developed goal within 90 days of enrollment 3. Percent of high risk patients with transitions of care call (TOC) within 48 hours of discharge 4. Percent of SCCP patients meeting at-risk criteria per targeted At-Risk patients 5. % of high risk patients with medication reconciliation by pharmacist within 72 hours of discharge 6. Percent of discharged patients assisted by SCCP with TCM codes billed 95% 90% 100% 70% 100%
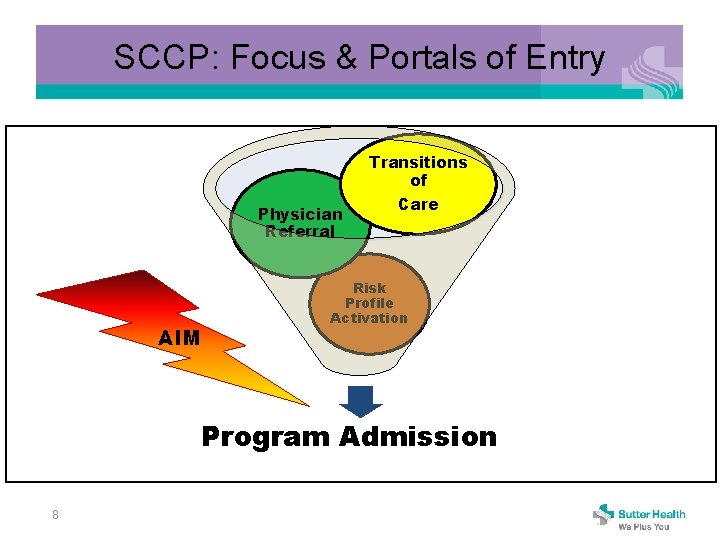
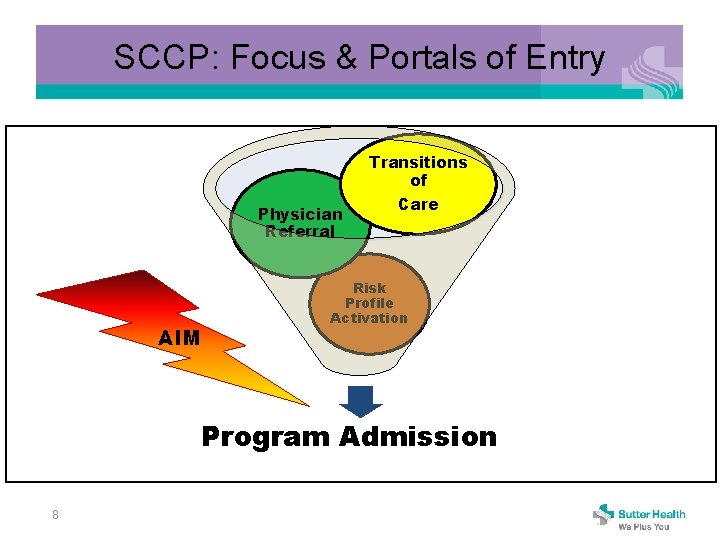
SCCP: Focus & Portals of Entry Transitions of Physician Referral AIM Care Risk Profile Activation Program Admission 8
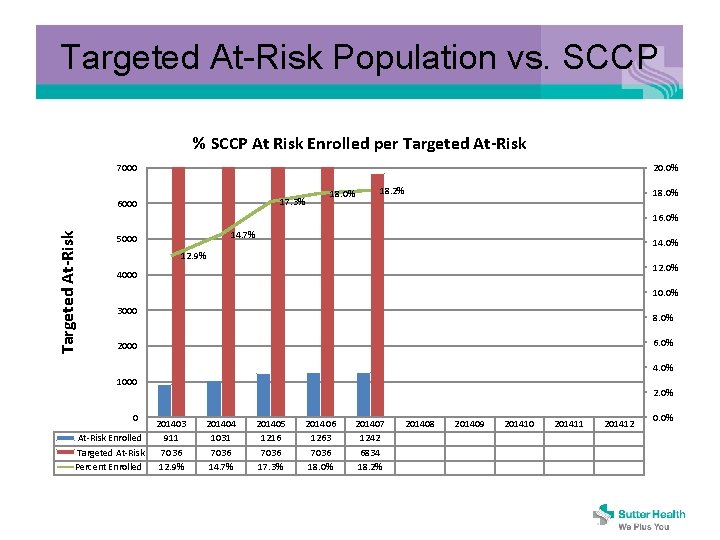
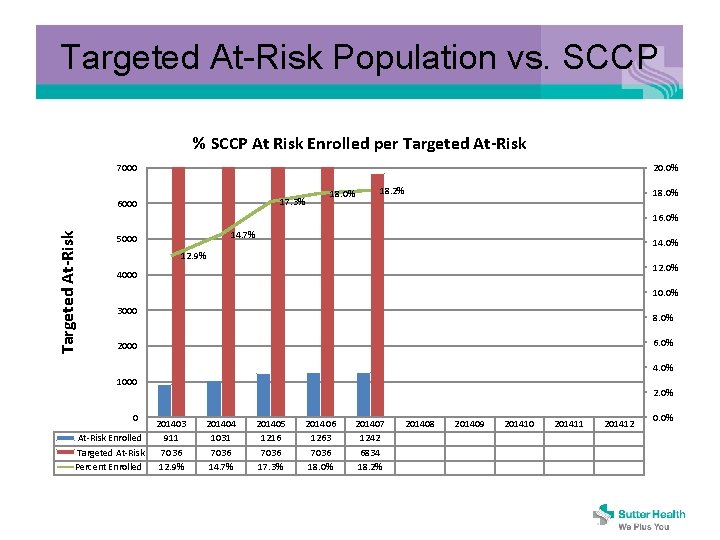
Targeted At-Risk Population vs. SCCP % SCCP At Risk Enrolled per Targeted At-Risk 7000 20. 0% 17. 3% 6000 18. 0% 18. 2% 18. 0% Targeted At-Risk 16. 0% 14. 7% 5000 14. 0% 12. 9% 12. 0% 4000 10. 0% 3000 8. 0% 6. 0% 2000 4. 0% 1000 0 At-Risk Enrolled Targeted At-Risk Percent Enrolled 2. 0% 201403 911 7036 12. 9% 201404 1031 7036 14. 7% 201405 1216 7036 17. 3% 201406 1263 7036 18. 0% 201407 1242 6834 18. 2% 201408 201409 201410 201411 201412 0. 0%
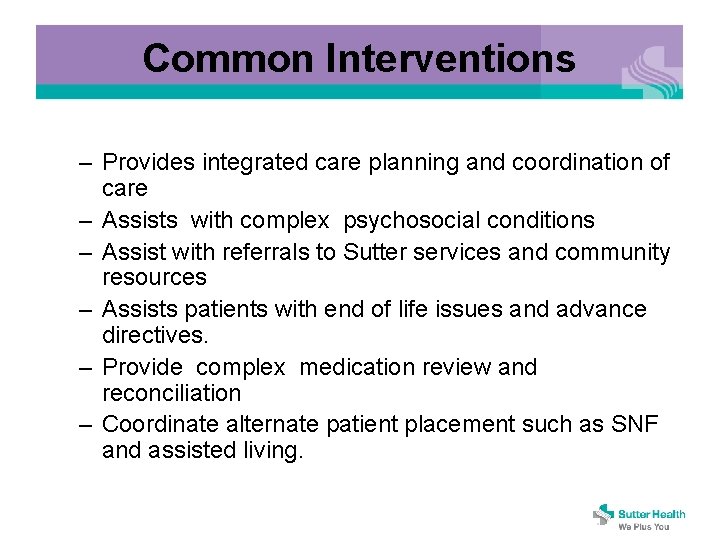
Common Interventions – Provides integrated care planning and coordination of care – Assists with complex psychosocial conditions – Assist with referrals to Sutter services and community resources – Assists patients with end of life issues and advance directives. – Provide complex medication review and reconciliation – Coordinate alternate patient placement such as SNF and assisted living.
Readmission Prevention • Management of patients at times of transitions – Discharge from Hospital setting – Discharge from SNF – Discharge from Home Health • Communication regarding shared patients – Acute case managers to Ambulatory case managers – Ambulatory case managers to Acute case managers • Phone • Midas
Daily Acute and SNF Census Review to Identify patients for follow-up • SMG or SIP physician • Discharge to home without home health • High Risk patients identified for follow up – Unplanned readmission within 30 days – ≥ 2 admissions/year – ≥ 2 ED visits/year – ≥ 3 Chronic Conditions – CMS Targeted Readmission diagnosis • COPD, pneumonia, stroke, AMI – Polypharmacy ≥ 7 medications
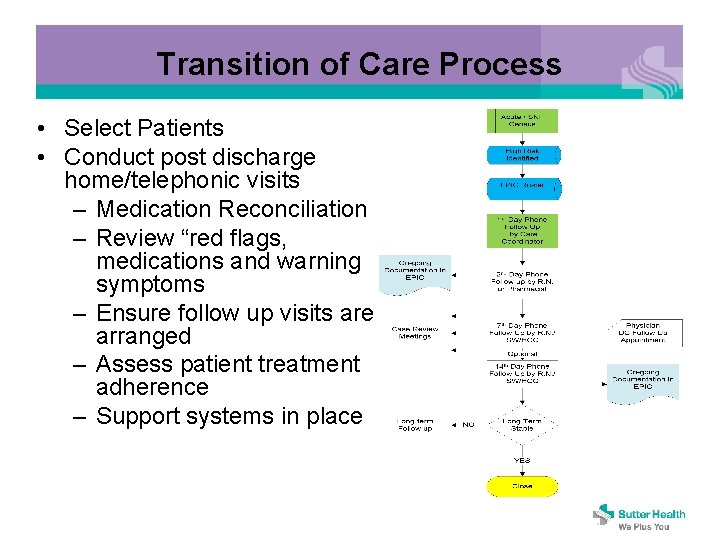
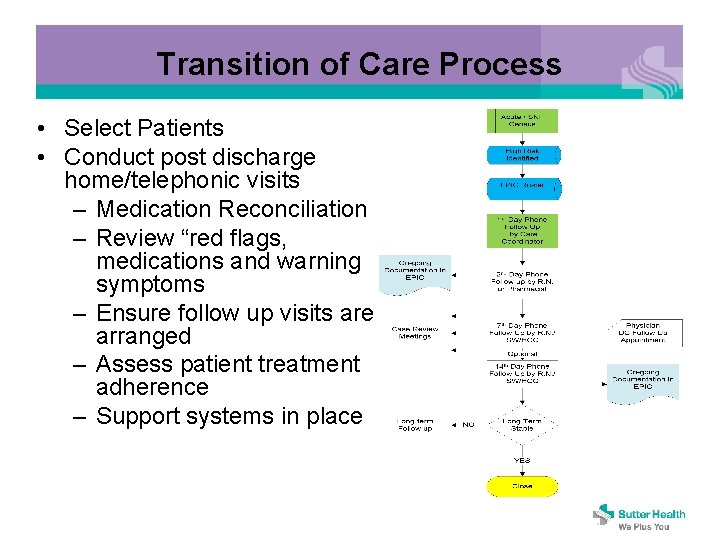
Transition of Care Process • Select Patients • Conduct post discharge home/telephonic visits – Medication Reconciliation – Review “red flags, medications and warning symptoms – Ensure follow up visits are arranged – Assess patient treatment adherence – Support systems in place
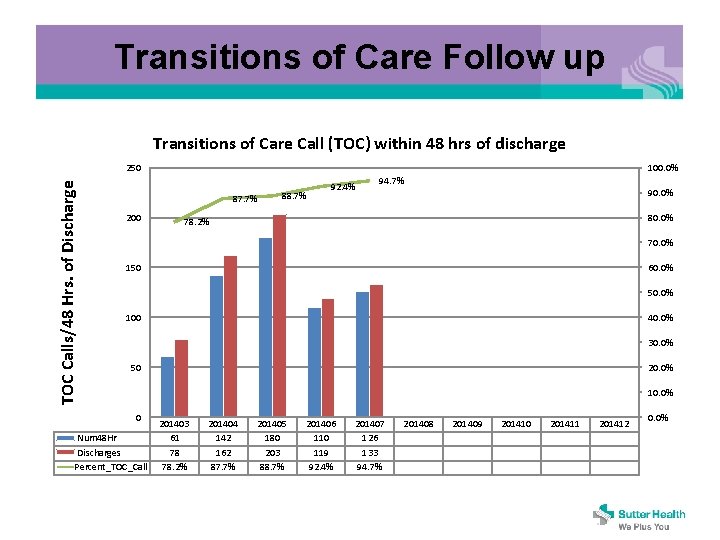
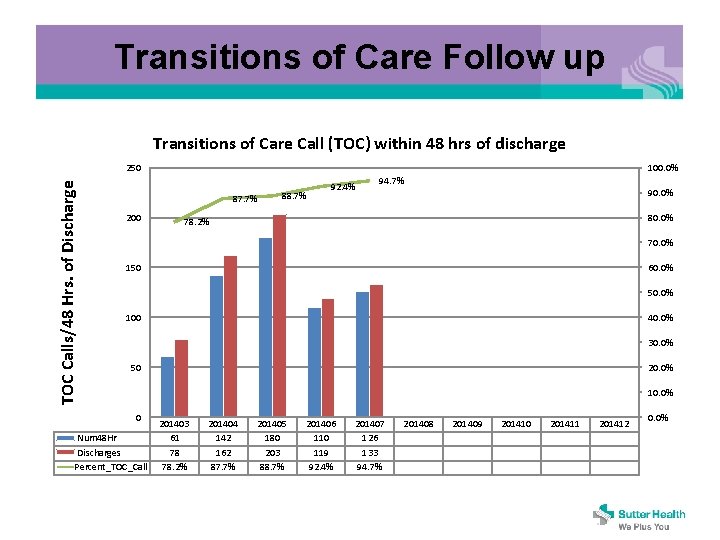
Transitions of Care Follow up Transitions of Care Call (TOC) within 48 hrs of discharge TOC Calls/48 Hrs. of Discharge 250 100. 0% 87. 7% 200 88. 7% 92. 4% 94. 7% 90. 0% 80. 0% 78. 2% 70. 0% 150 60. 0% 50. 0% 100 40. 0% 30. 0% 50 20. 0% 10. 0% 0 Num 48 Hr Discharges Percent_TOC_Call 201403 61 78 78. 2% 201404 142 162 87. 7% 201405 180 203 88. 7% 201406 110 119 92. 4% 201407 126 133 94. 7% 201408 201409 201410 201411 201412 0. 0%
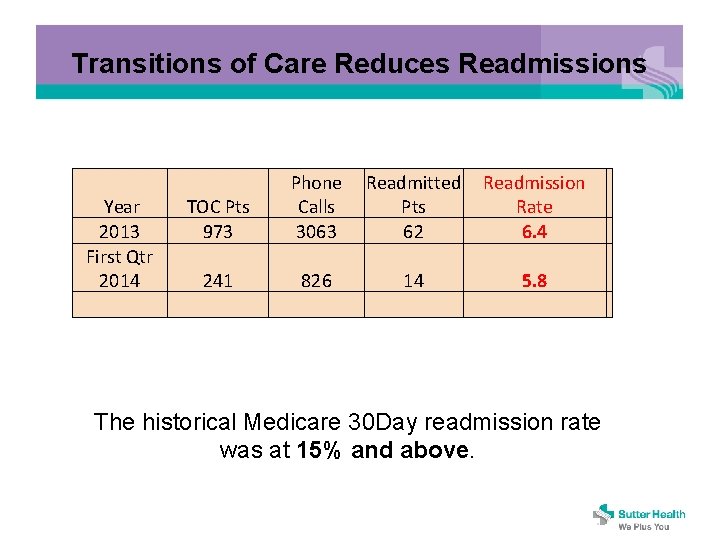
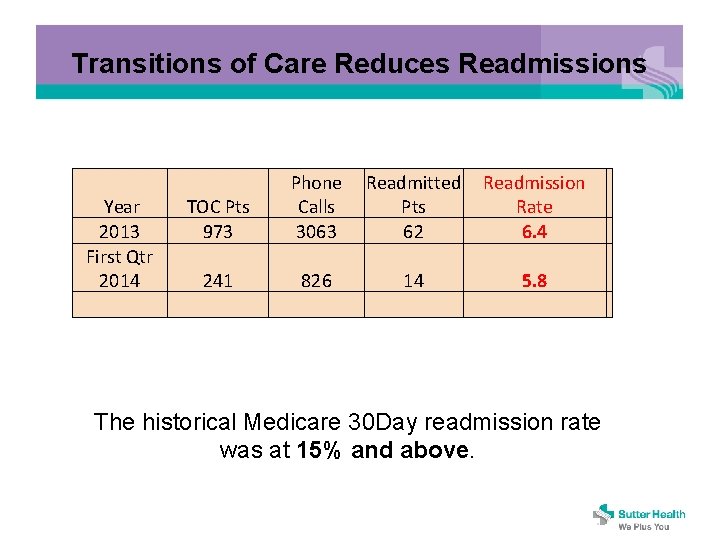
Transitions of Care Reduces Readmissions Year 2013 First Qtr 2014 TOC Pts 973 241 Phone Readmitted Readmission Calls Pts Rate 3063 62 6. 4 826 14 5. 8 The historical Medicare 30 Day readmission rate was at 15% and above.
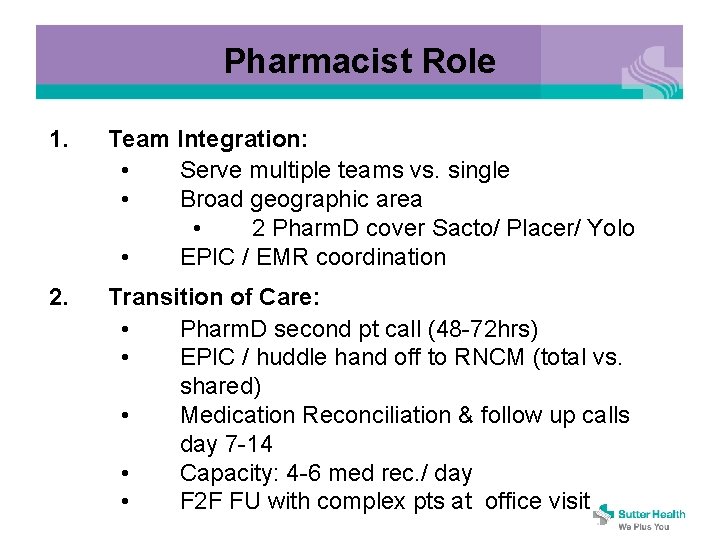
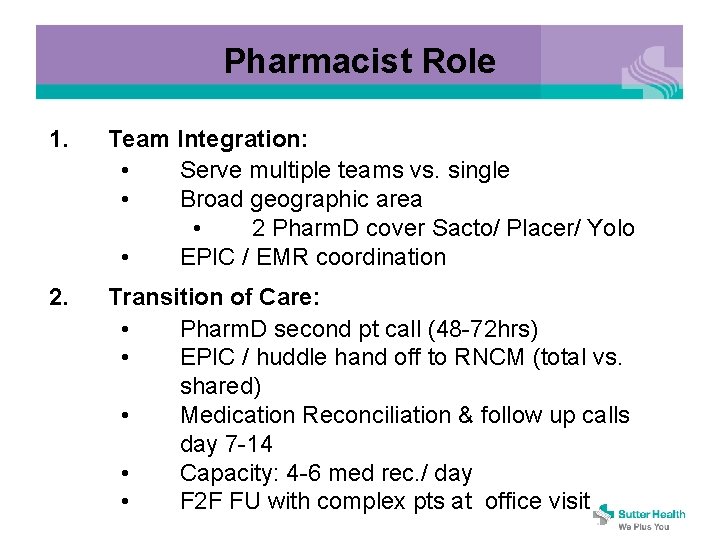
Pharmacist Role 1. Team Integration: • Serve multiple teams vs. single • Broad geographic area • 2 Pharm. D cover Sacto/ Placer/ Yolo • EPIC / EMR coordination 2. Transition of Care: • Pharm. D second pt call (48 -72 hrs) • EPIC / huddle hand off to RNCM (total vs. shared) • Medication Reconciliation & follow up calls day 7 -14 • Capacity: 4 -6 med rec. / day • F 2 F FU with complex pts at office visit
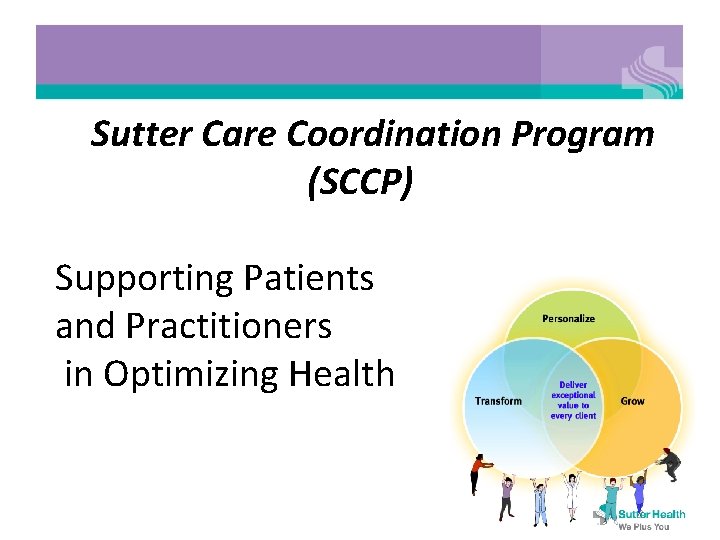
Pharmacist Role 3. Lessons Learned: • Benefit of LEAN to integrate • • • 4. Prior habits/ PCMH hangover (Pilot evolution) Complexity of med rec when done correctly = energy expended How to do telephonic work (cold call). Importance of provider relationships. MD & Pharm. D working in PCP practice Next Steps • • Continue program roll out Monitor & adjust
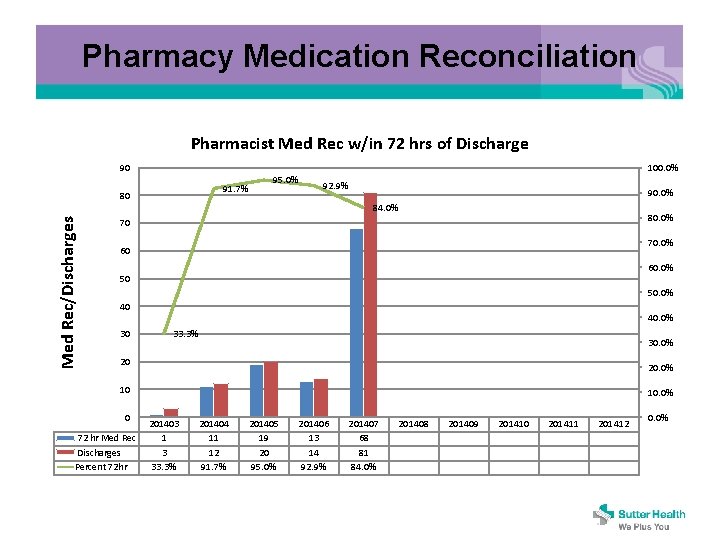
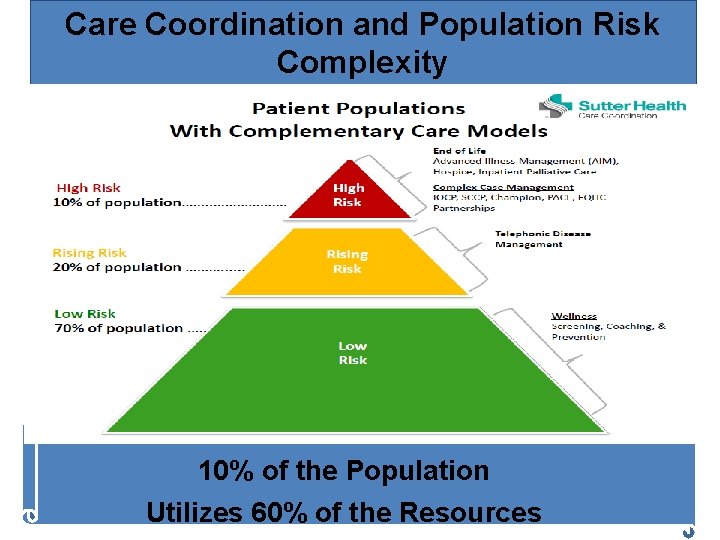
Pharmacy Medication Reconciliation Pharmacist Med Rec w/in 72 hrs of Discharge 90 100. 0% 91. 7% 80 95. 0% 92. 9% 90. 0% Med Rec/Discharges 84. 0% 80. 0% 70 70. 0% 60 60. 0% 50 50. 0% 40 30 40. 0% 33. 3% 30. 0% 20 20. 0% 10 0 72 hr Med Rec Discharges Percent 72 hr 10. 0% 201403 1 3 33. 3% 201404 11 12 91. 7% 201405 19 20 95. 0% 201406 13 14 92. 9% 201407 68 81 84. 0% 201408 201409 201410 201411 201412 0. 0%

19