Survey of CIC Program Participants Who Joined and













- Slides: 56
Survey of CIC Program Participants: Who Joined and How Did They Change Their Care-Seeking Behavior? Catherine Mc. Laughlin University of Michigan Erin Fries Taylor Mathematica Policy Research Web. Cast Presentation CIC programs June 23, 2004
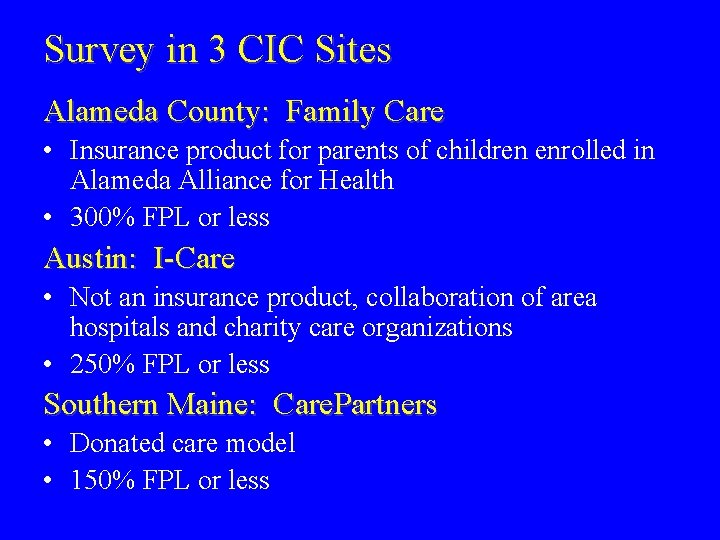
Survey in 3 CIC Sites Alameda County: Family Care • Insurance product for parents of children enrolled in Alameda Alliance for Health • 300% FPL or less Austin: I-Care • Not an insurance product, collaboration of area hospitals and charity care organizations • 250% FPL or less Southern Maine: Care. Partners • Donated care model • 150% FPL or less
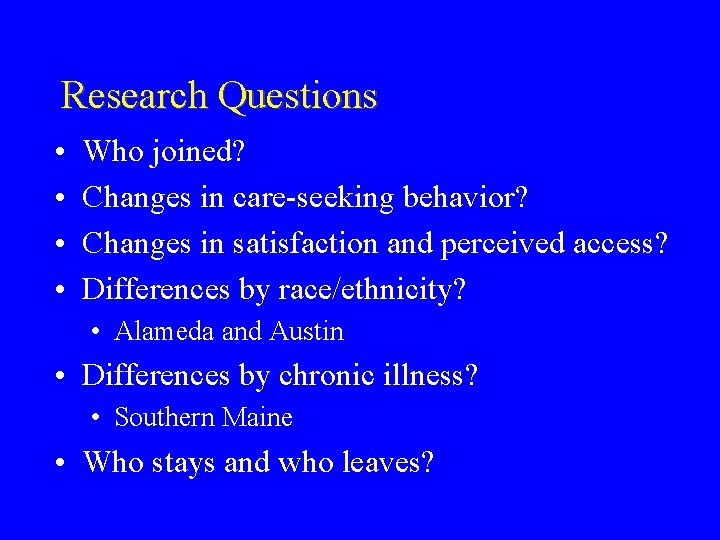
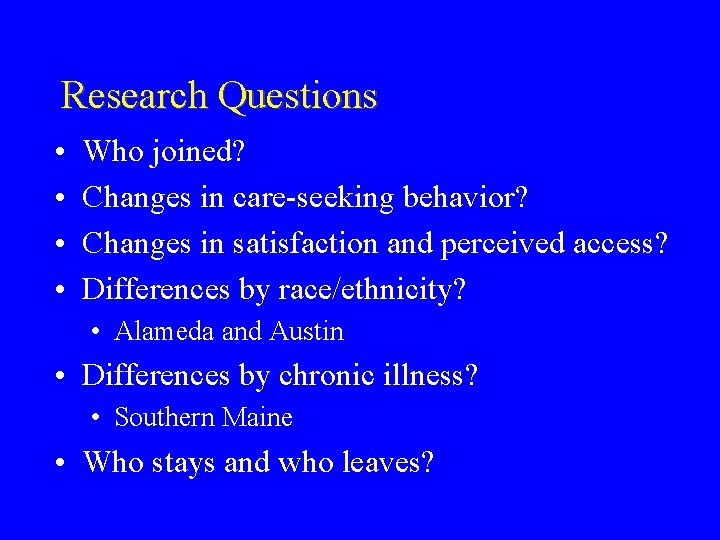
Research Questions • • Who joined? Changes in care-seeking behavior? Changes in satisfaction and perceived access? Differences by race/ethnicity? • Alameda and Austin • Differences by chronic illness? • Southern Maine • Who stays and who leaves?
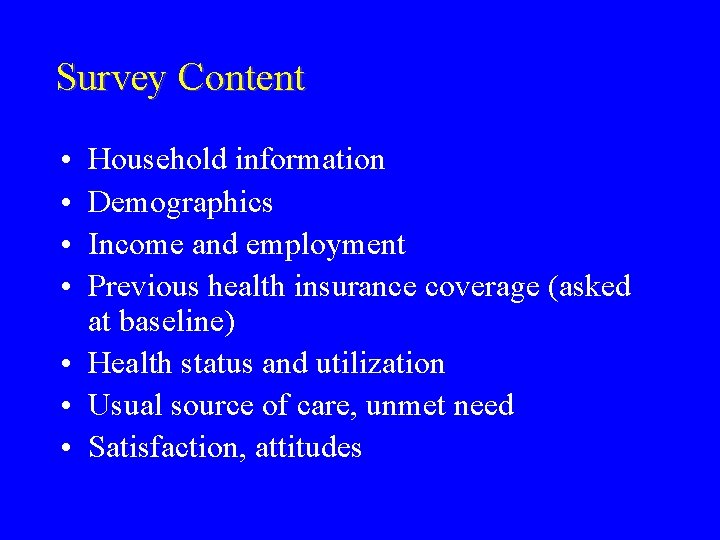
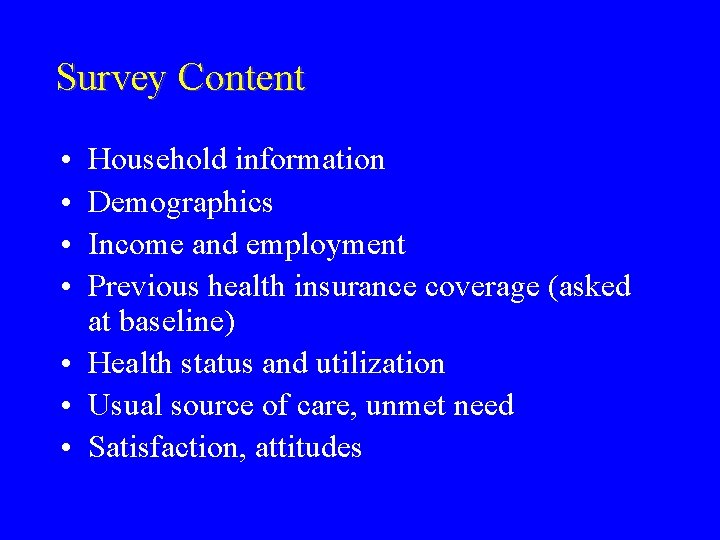
Survey Content • • Household information Demographics Income and employment Previous health insurance coverage (asked at baseline) • Health status and utilization • Usual source of care, unmet need • Satisfaction, attitudes

Wave 1 Details • Site provided contact information on all new enrollees over a period of 4 -6 months • Completed interviews in Wave 1 -Alameda: Alameda -Austin: Austin -S Maine: Maine 471 adults (Aug 01–Jan 02) 88% response rate 347 adults (Feb–Aug 02) 87% response rate 300 adults (Nov 01–June 02) 93% response rate
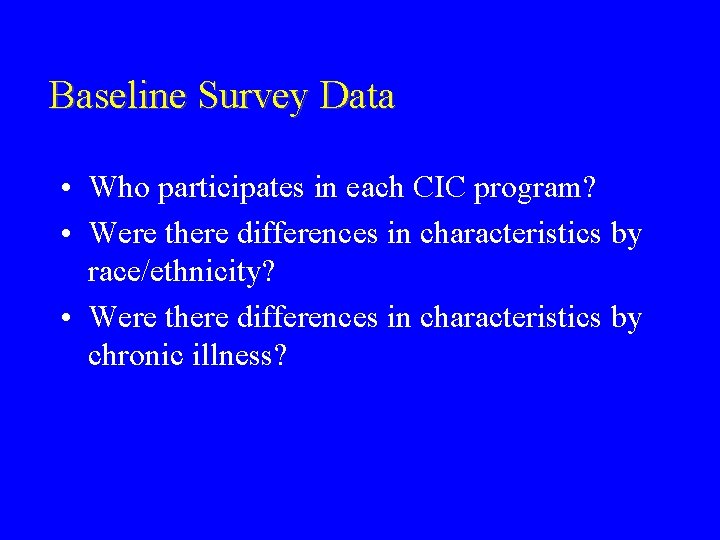
Baseline Survey Data • Who participates in each CIC program? • Were there differences in characteristics by race/ethnicity? • Were there differences in characteristics by chronic illness?
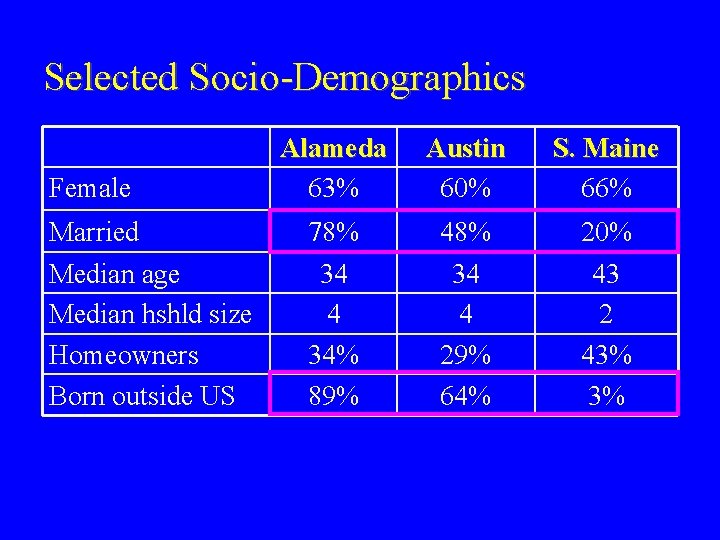
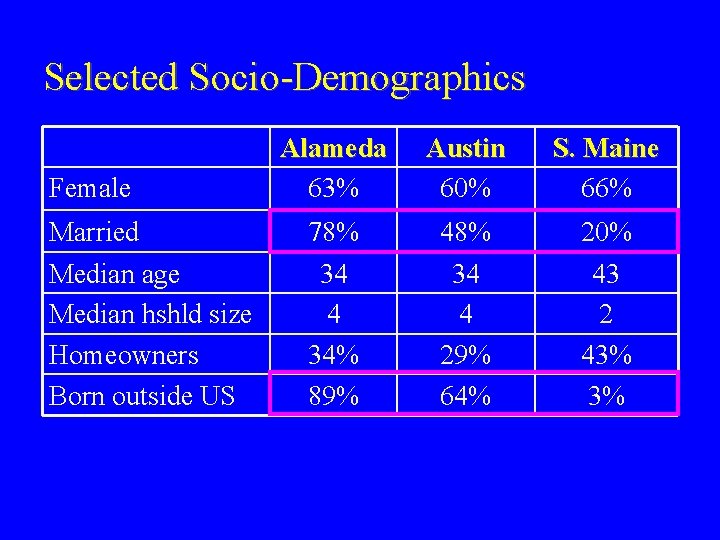
Selected Socio-Demographics Female Alameda 63% Austin 60% S. Maine 66% Married 78% 48% 20% Median age Median hshld size Homeowners Born outside US 34 4 34% 89% 34 4 29% 64% 43 2 43% 3%
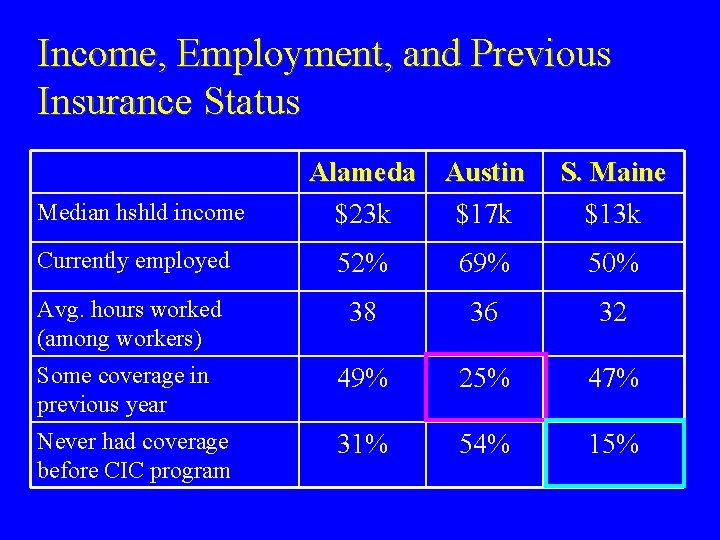
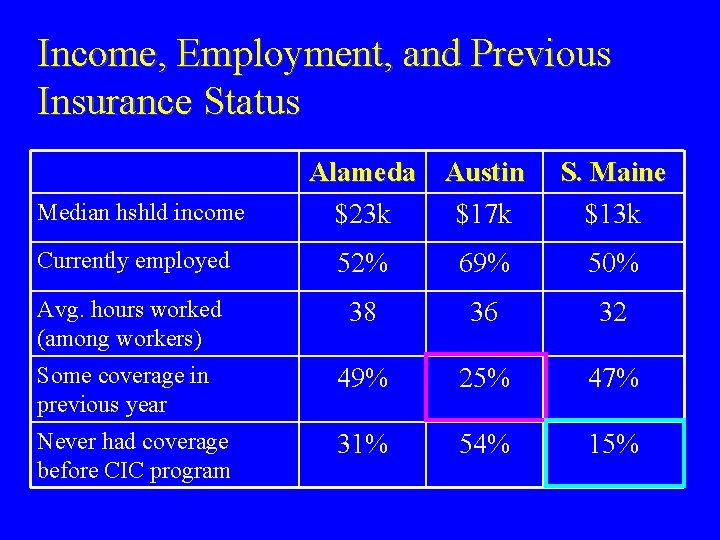
Income, Employment, and Previous Insurance Status Median hshld income Alameda Austin $23 k $17 k S. Maine $13 k Currently employed 52% 69% 50% Avg. hours worked (among workers) 38 36 32 Some coverage in previous year 49% 25% 47% Never had coverage before CIC program 31% 54% 15%
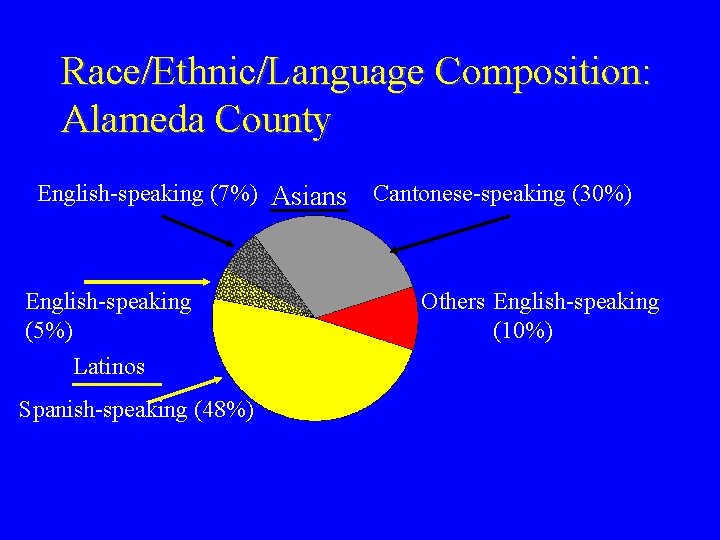
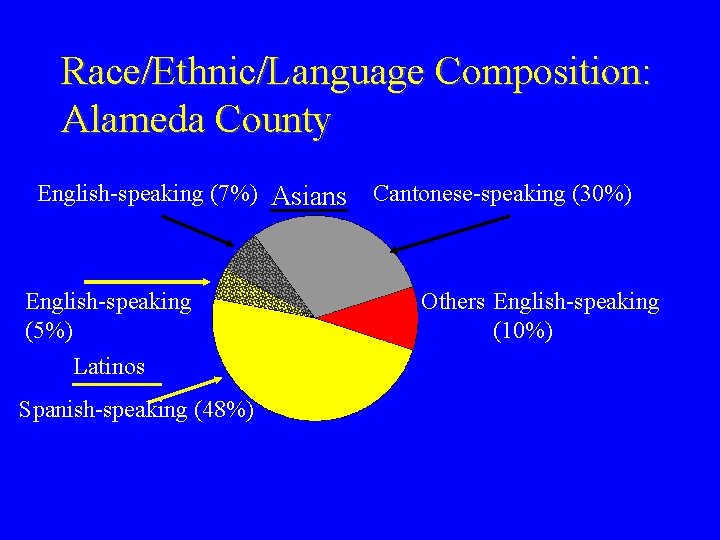
Race/Ethnic/Language Composition: Alameda County English-speaking (7%) Asians English-speaking (5%) Latinos Spanish-speaking (48%) Cantonese-speaking (30%) Others English-speaking (10%)
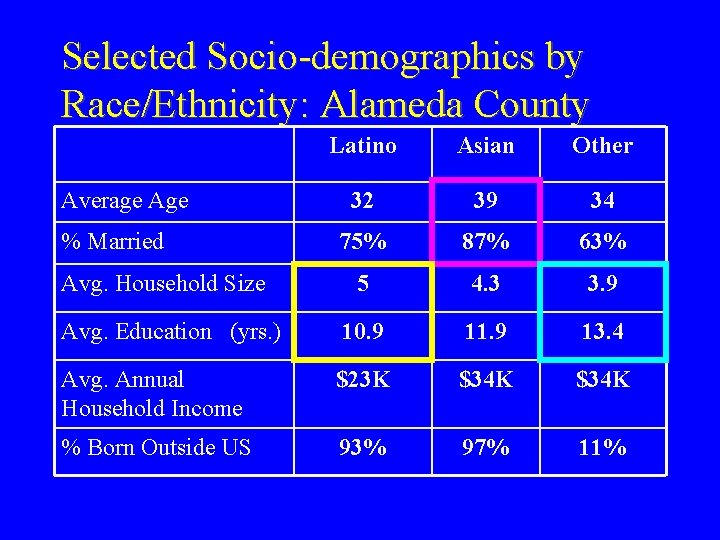
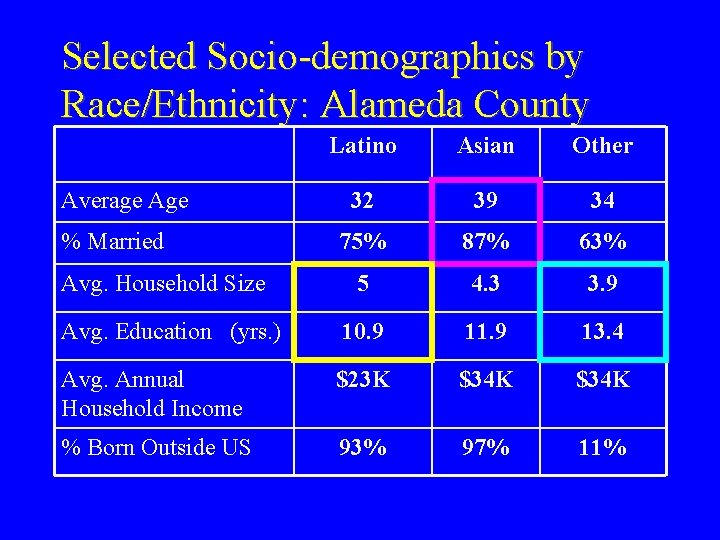
Selected Socio-demographics by Race/Ethnicity: Alameda County Latino Asian Other 32 39 34 75% 87% 63% 5 4. 3 3. 9 Avg. Education (yrs. ) 10. 9 11. 9 13. 4 Avg. Annual Household Income $23 K $34 K % Born Outside US 93% 97% 11% Average Age % Married Avg. Household Size
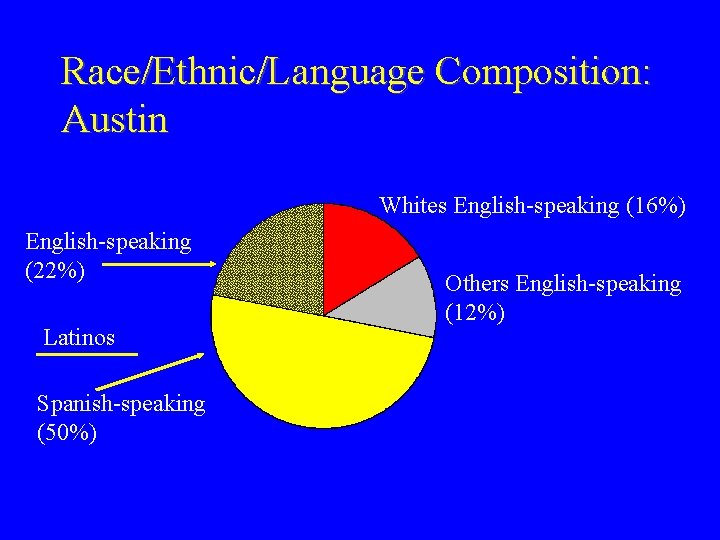
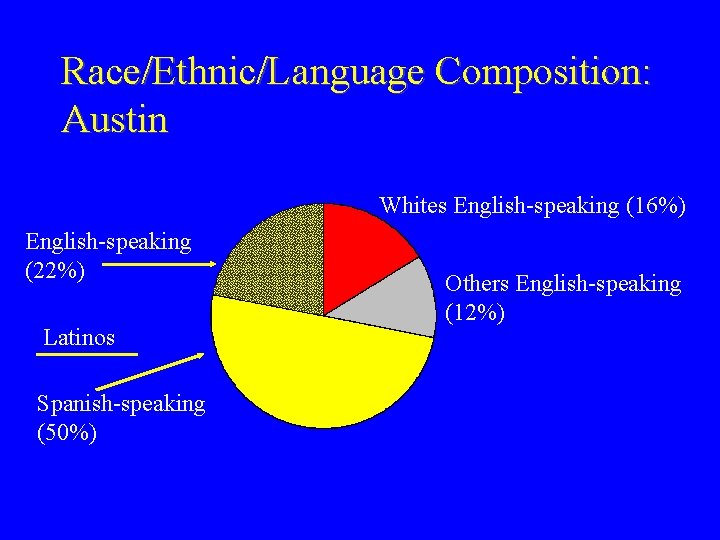
Race/Ethnic/Language Composition: Austin Whites English-speaking (16%) English-speaking (22%) Latinos Spanish-speaking (50%) Others English-speaking (12%)

Selected Socio-demographics by Race/Ethnicity: Austin Span-sp Latino (n=174) Eng-sp Latino (n=75) Other (n=42) White, NH (n=56) Avg. Age 35 35 41 38 % Married 63% 32% 50% 21% Avg. Household Size 4. 3 3. 6 3. 2 2. 4 Avg. Education (yrs. ) 10. 8 11. 8 13. 0 Avg. Annual Hshld. Income (2001) $17 K $18 K $25 K $18 K % Born Outside US 97% 33% 57% 7%

Baseline Health Status and Care. Seeking Behavior Alameda Austin S. Maine Fair or poor health status 22% 35% 30% Chronic or limiting condition 12% 22% 53% No health care utilization (previous 12 months) Median out-of-pocket costs (previous 12 months) 35% 32% 10% <$50 $100 -299 $300 -499

Preventive Services in Previous Year Alameda Austin S. Maine Physical Exam 38% 31% 53% Blood Pressure Check 59% 61% 84% Breast Exam (among women) 30% 22% Pap Smear (among women) 44% 34% 55% 50%
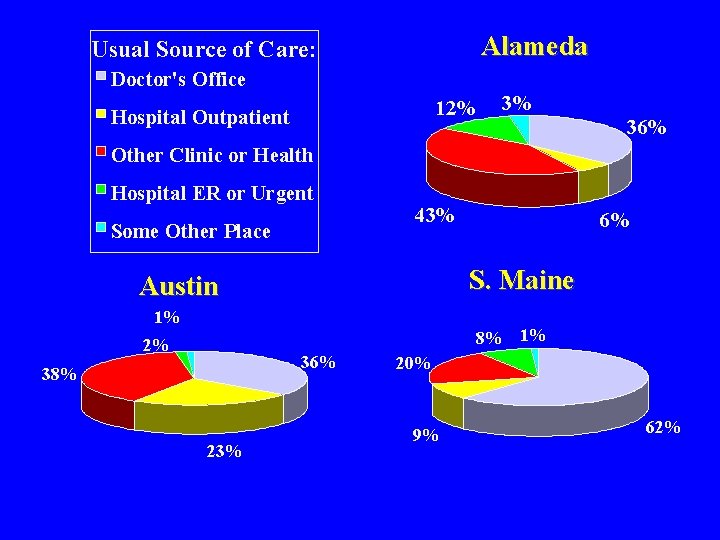
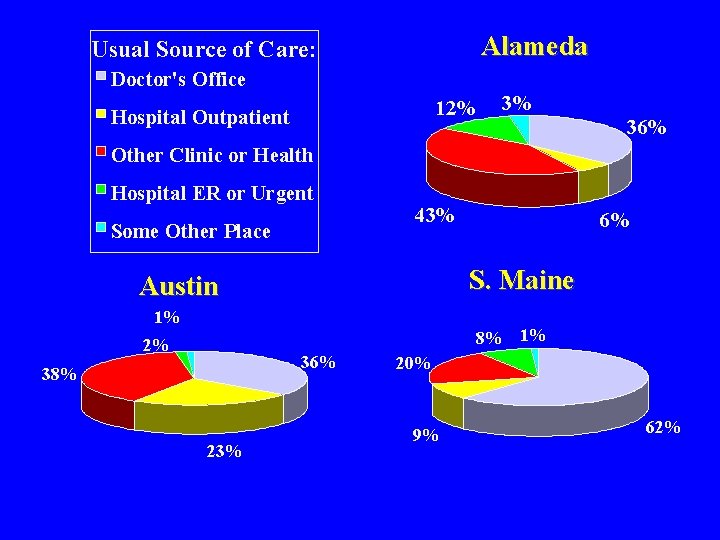
Alameda Usual Source of Care: Doctor's Office 12% Hospital Outpatient 3% 36% Other Clinic or Health Hospital ER or Urgent Some Other Place 43% 6% S. Maine Austin 1% 8% 1% 2% 36% 38% 23% 20% 9% 62%

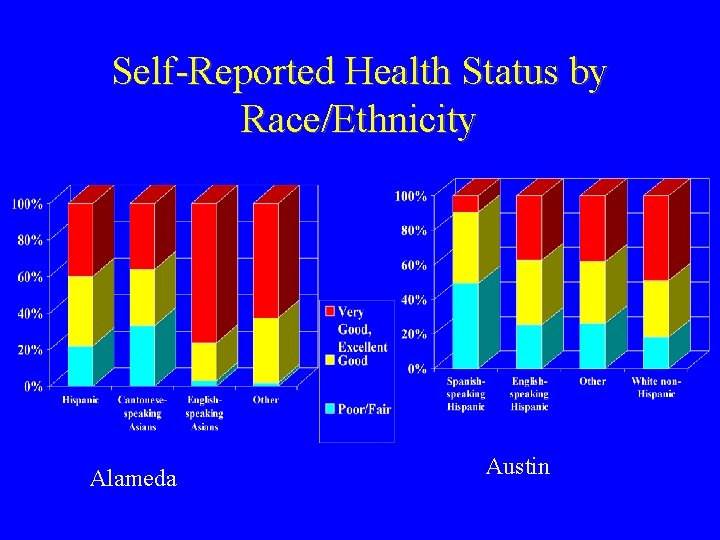
Alameda: Health and Care-Seeking Behaviors: Themes by Race/Ethnicity • Asians and Latinas reported worse health status, but fewer chronic conditions • Cantonese-speaking Asians rated health status lower than English-speaking Asians • Latinas and Other were more likely to have an ER visit or a doctor visit • Asians reported lowest out-of pocket costs and Other reported the highest

More on Baseline Health in Alameda: Themes by Race/Ethnicity • Cantonese-speaking Asians were most likely to have no health care utilization • Those in Other category were most likely to report unmet need

Austin: Utilization Rates By Race/Ethnicity White, Non. Latino English Speaking Latino Spanish Speaking Latino Other ER Visit 36% 39% 24% 36% Hospital Stay 9% 9% 6% 5% Doctor Visit 68% 61% 52% 62% No Utilization 18% 27% 39% 29% Median Out-of. Pocket Costs $200 $75 $200
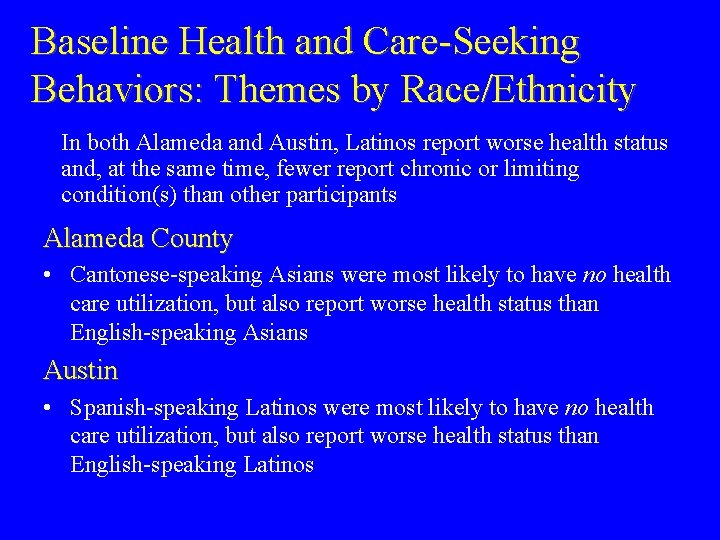
Baseline Health and Care-Seeking Behaviors: Themes by Race/Ethnicity In both Alameda and Austin, Latinos report worse health status and, at the same time, fewer report chronic or limiting condition(s) than other participants Alameda County • Cantonese-speaking Asians were most likely to have no health care utilization, but also report worse health status than English-speaking Asians Austin • Spanish-speaking Latinos were most likely to have no health care utilization, but also report worse health status than English-speaking Latinos
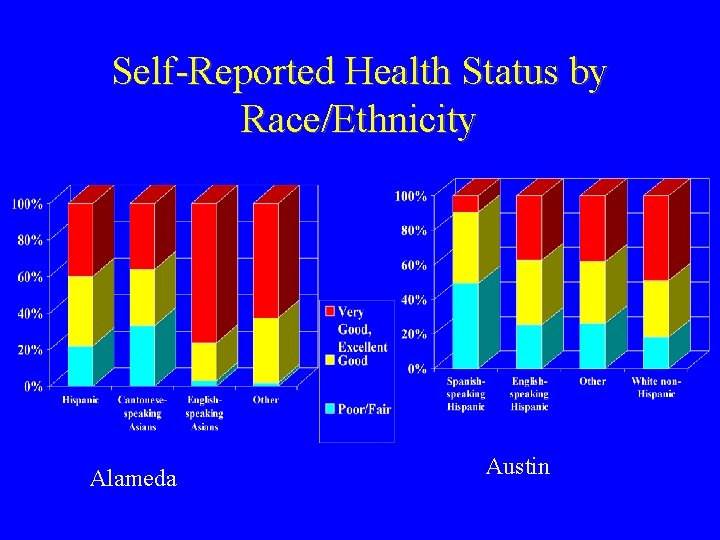
Self-Reported Health Status by Race/Ethnicity Alameda Austin
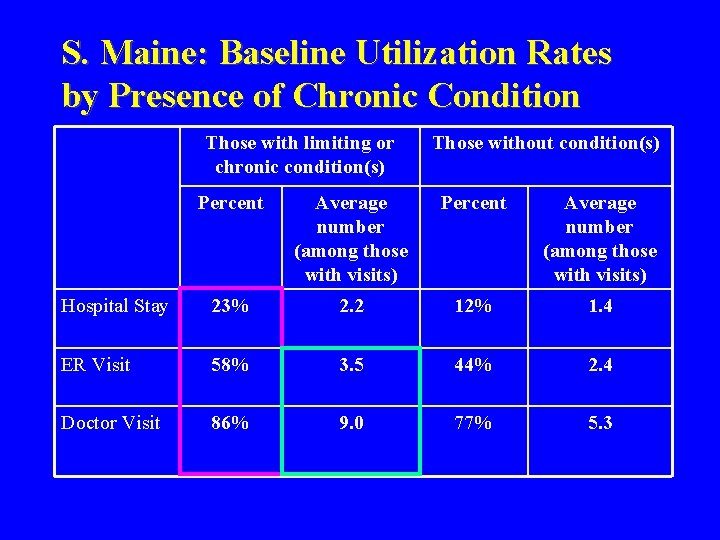
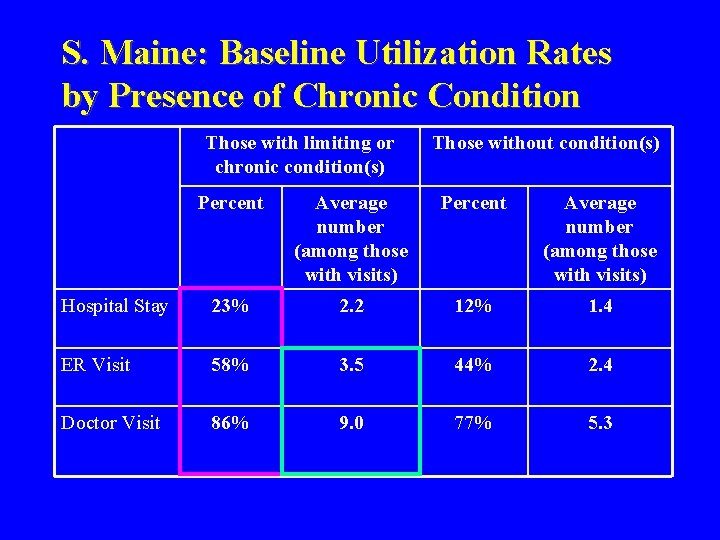
S. Maine: Baseline Utilization Rates by Presence of Chronic Condition Those with limiting or chronic condition(s) Those without condition(s) Percent Average number (among those with visits) Hospital Stay 23% 2. 2 12% 1. 4 ER Visit 58% 3. 5 44% 2. 4 Doctor Visit 86% 9. 0 77% 5. 3
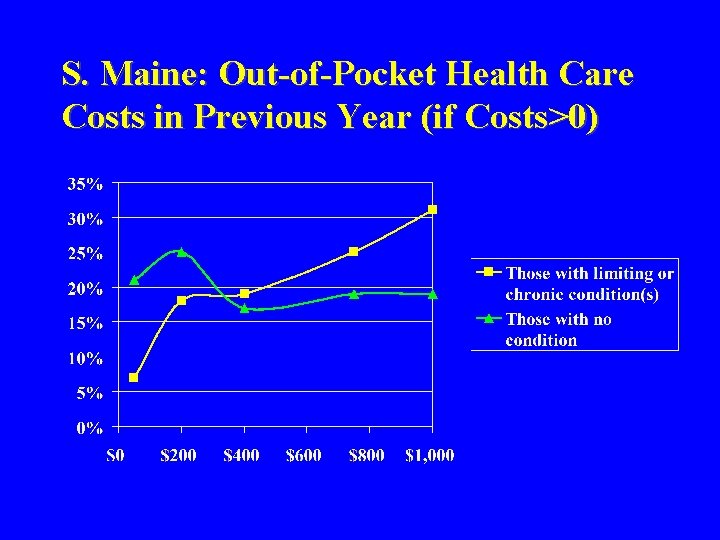
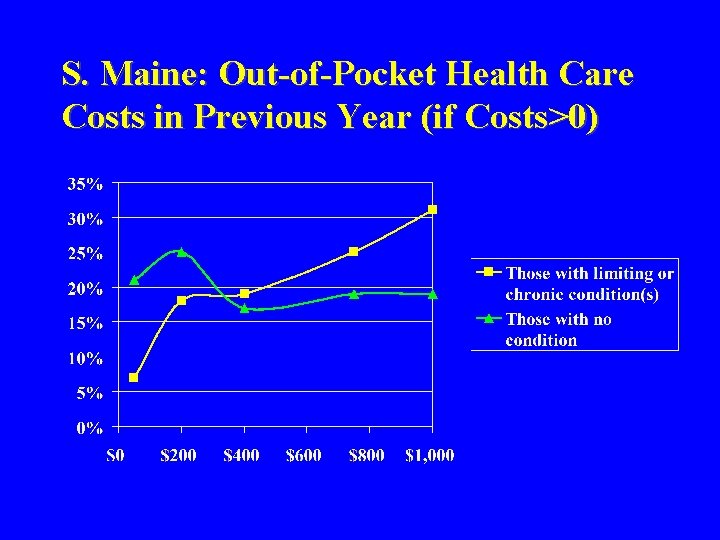
S. Maine: Out-of-Pocket Health Care Costs in Previous Year (if Costs>0)
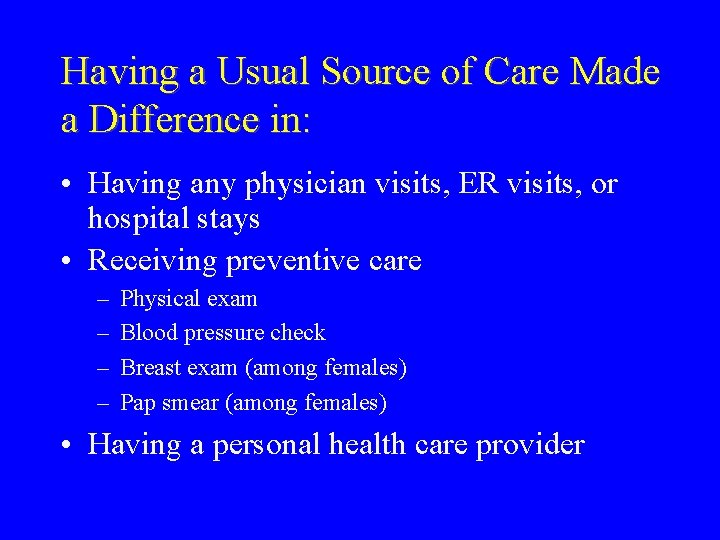
Having a Usual Source of Care Made a Difference in: • Having any physician visits, ER visits, or hospital stays • Receiving preventive care – – Physical exam Blood pressure check Breast exam (among females) Pap smear (among females) • Having a personal health care provider
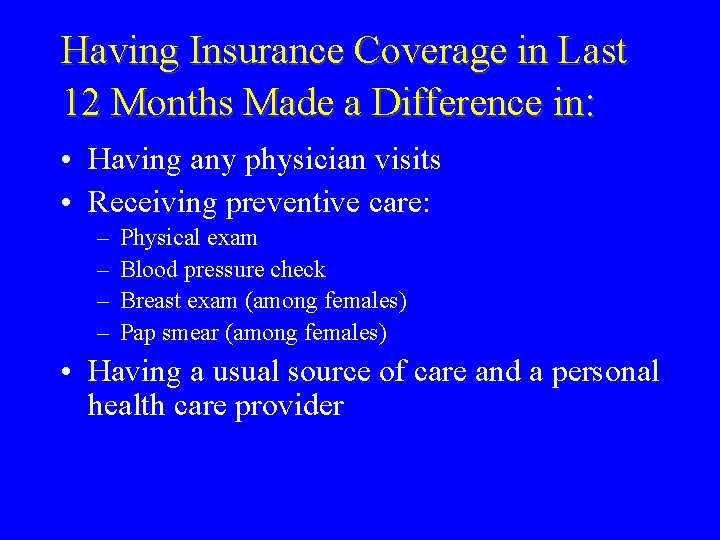
Having Insurance Coverage in Last 12 Months Made a Difference in: • Having any physician visits • Receiving preventive care: – – Physical exam Blood pressure check Breast exam (among females) Pap smear (among females) • Having a usual source of care and a personal health care provider
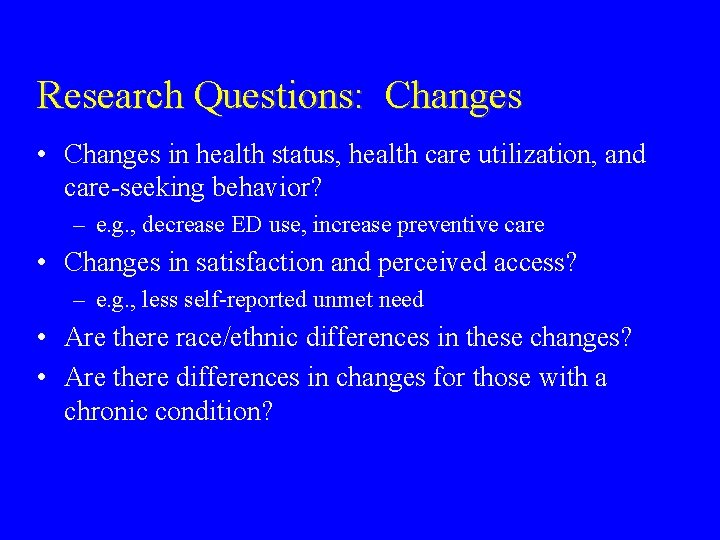
Research Questions: Changes • Changes in health status, health care utilization, and care-seeking behavior? – e. g. , decrease ED use, increase preventive care • Changes in satisfaction and perceived access? – e. g. , less self-reported unmet need • Are there race/ethnic differences in these changes? • Are there differences in changes for those with a chronic condition?
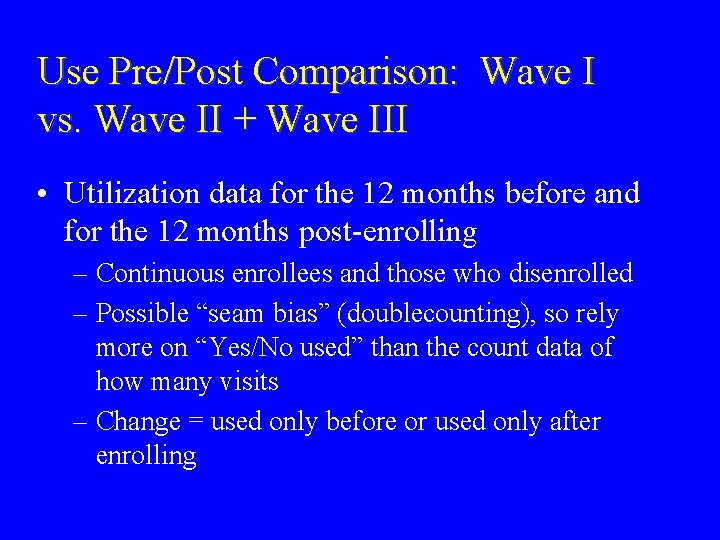
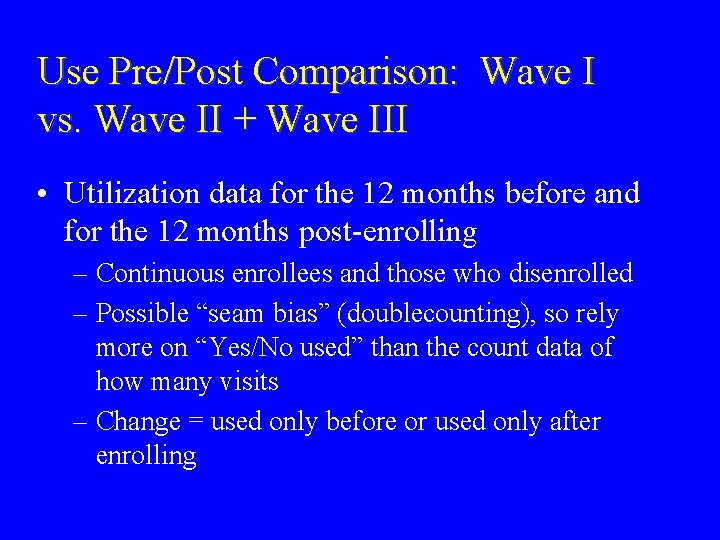
Use Pre/Post Comparison: Wave I vs. Wave II + Wave III • Utilization data for the 12 months before and for the 12 months post-enrolling – Continuous enrollees and those who disenrolled – Possible “seam bias” (doublecounting), so rely more on “Yes/No used” than the count data of how many visits – Change = used only before or used only after enrolling
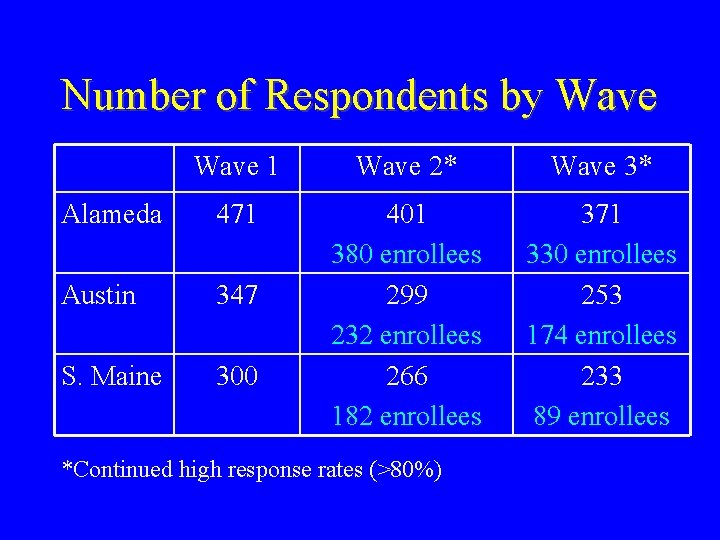
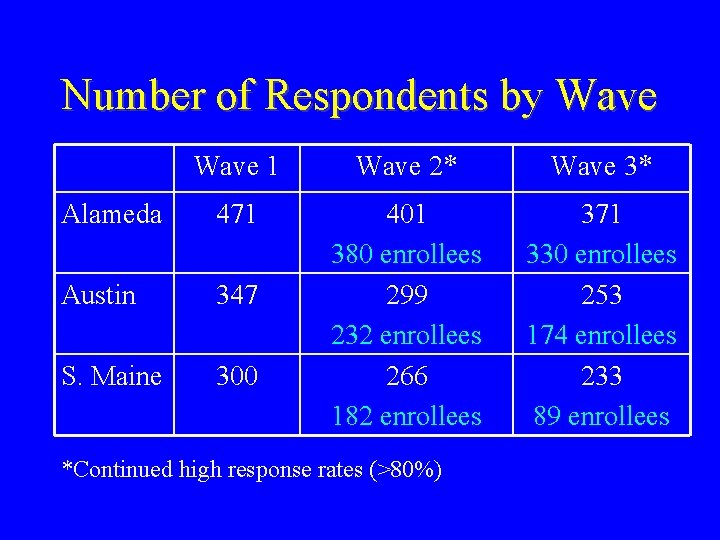
Number of Respondents by Wave 1 Wave 2* Wave 3* Alameda 471 Austin 347 S. Maine 300 401 380 enrollees 299 232 enrollees 266 182 enrollees 371 330 enrollees 253 174 enrollees 233 89 enrollees *Continued high response rates (>80%)
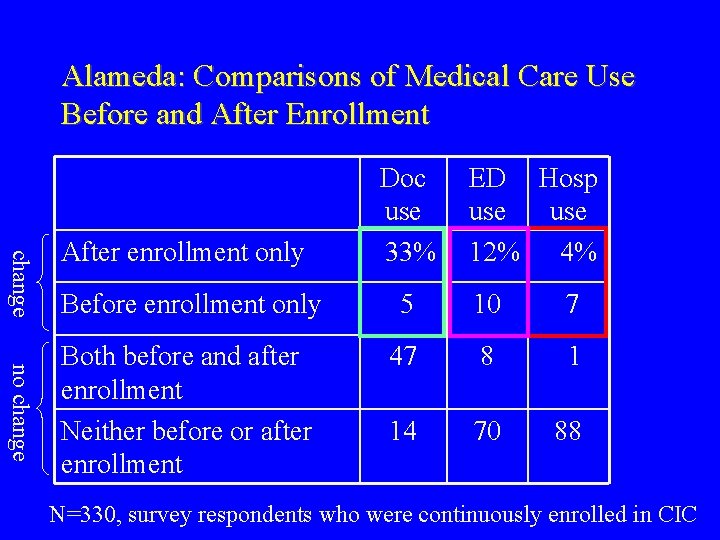
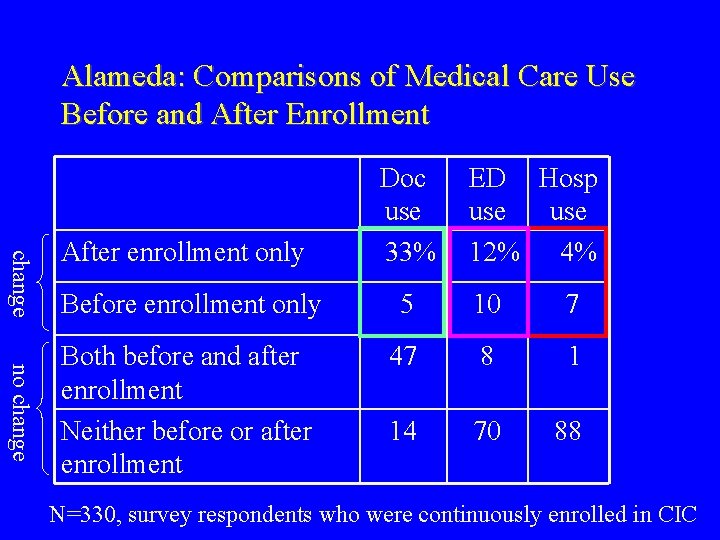
Alameda: Comparisons of Medical Care Use Before and After Enrollment change After enrollment only Doc use 33% ED Hosp use 12% 4% no change Before enrollment only 5 10 7 Both before and after enrollment Neither before or after enrollment 47 8 1 14 70 88 N=330, survey respondents who were continuously enrolled in CIC
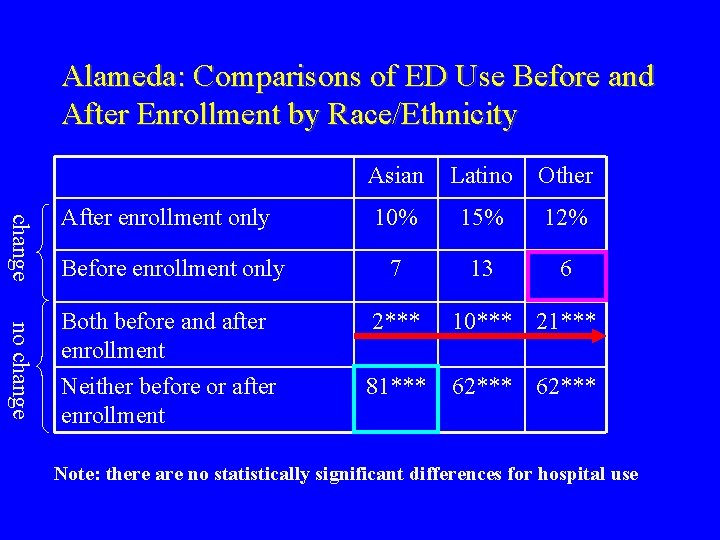
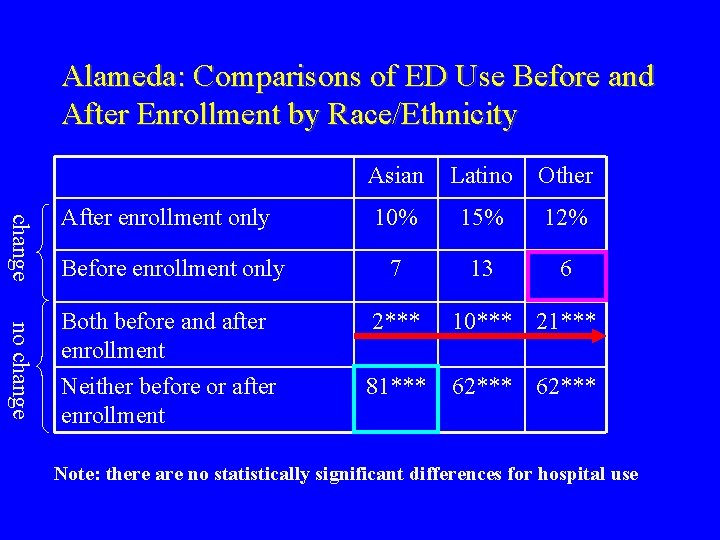
Alameda: Comparisons of ED Use Before and After Enrollment by Race/Ethnicity change no change Asian Latino Other 10% 15% 12% Before enrollment only 7 13 6 Both before and after enrollment Neither before or after enrollment 2*** 10*** 21*** 81*** 62*** After enrollment only Note: there are no statistically significant differences for hospital use

Austin: Comparisons of Medical Care Use Before and After Enrollment change After enrollment only Doc use 32% ED Hosp use 16% 9% no change Before enrollment only 3 16 6 Both before and after enrollment Neither before or after enrollment 52 15 0 13 52 85 N=164, survey respondents who were continuously enrolled in CIC
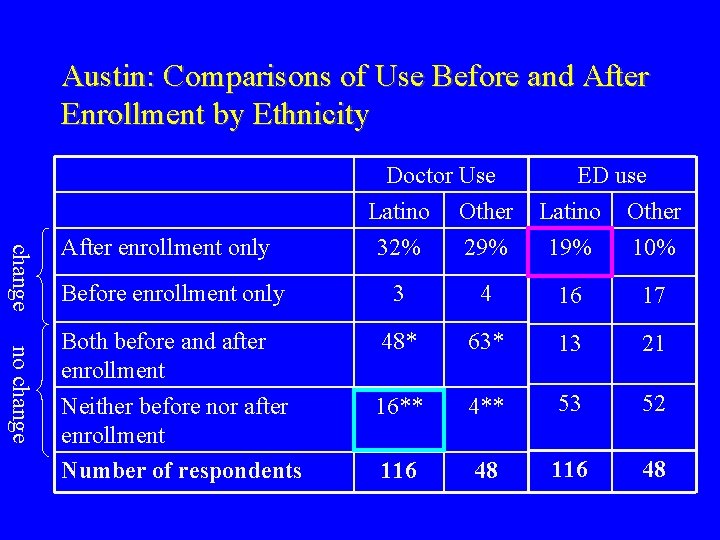
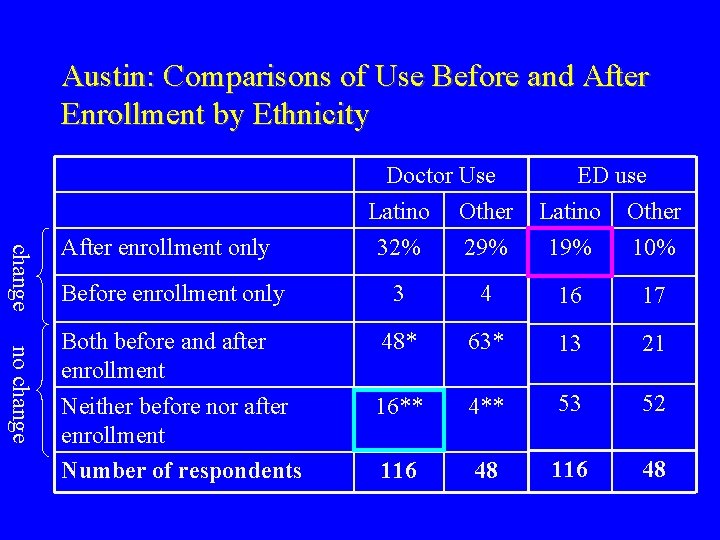
Austin: Comparisons of Use Before and After Enrollment by Ethnicity change After enrollment only Before enrollment only no change Both before and after enrollment Neither before nor after enrollment Number of respondents Doctor Use Latino Other 32% 29% ED use Latino Other 19% 10% 3 4 16 17 48* 63* 13 21 16** 4** 53 52 116 48
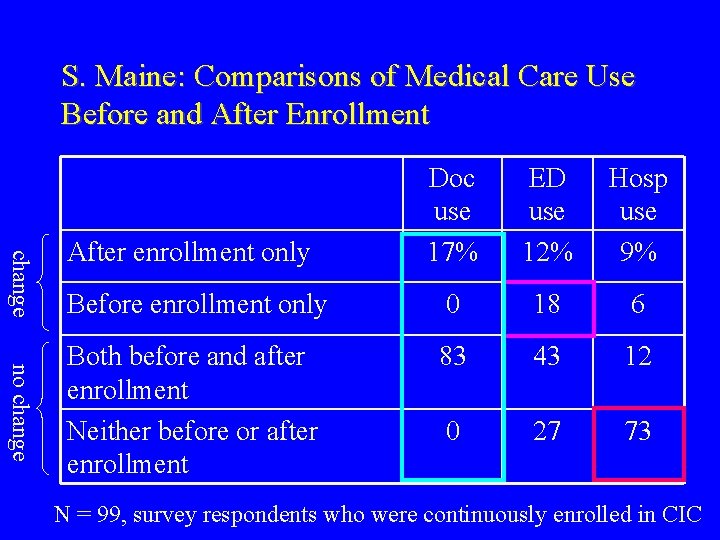
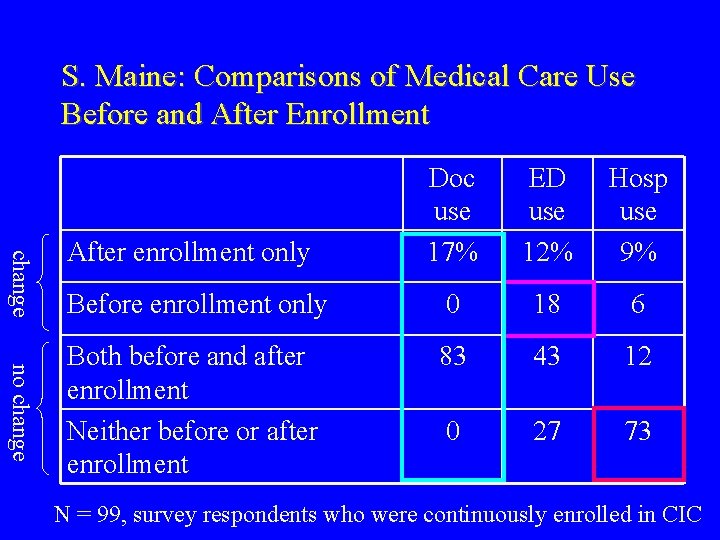
S. Maine: Comparisons of Medical Care Use Before and After Enrollment change no change Doc use 17% ED use 12% Hosp use 9% Before enrollment only 0 18 6 Both before and after enrollment Neither before or after enrollment 83 43 12 0 27 73 After enrollment only N = 99, survey respondents who were continuously enrolled in CIC
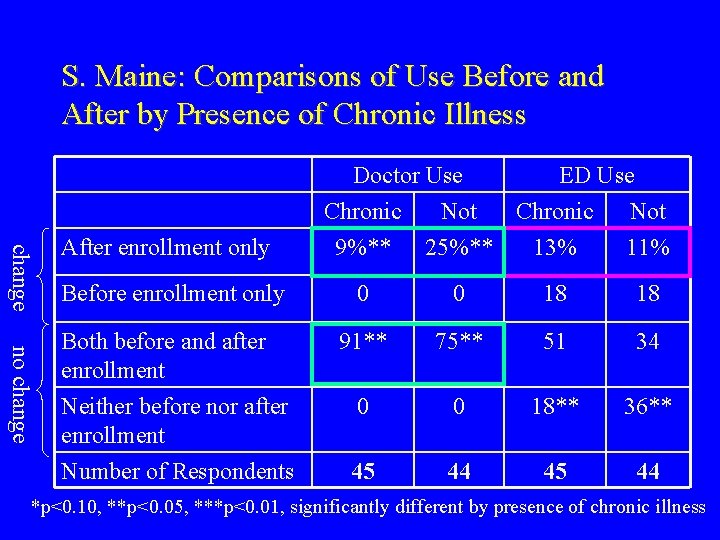
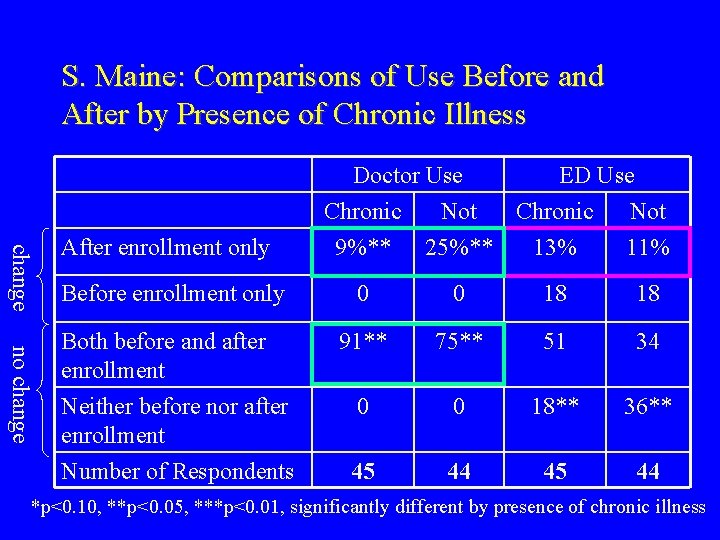
S. Maine: Comparisons of Use Before and After by Presence of Chronic Illness change After enrollment only Before enrollment only no change Both before and after enrollment Neither before nor after enrollment Number of Respondents Doctor Use ED Use Chronic Not 9%** 25%** 13% 11% 0 0 18 18 91** 75** 51 34 0 0 18** 36** 45 44 *p<0. 10, **p<0. 05, ***p<0. 01, significantly different by presence of chronic illness
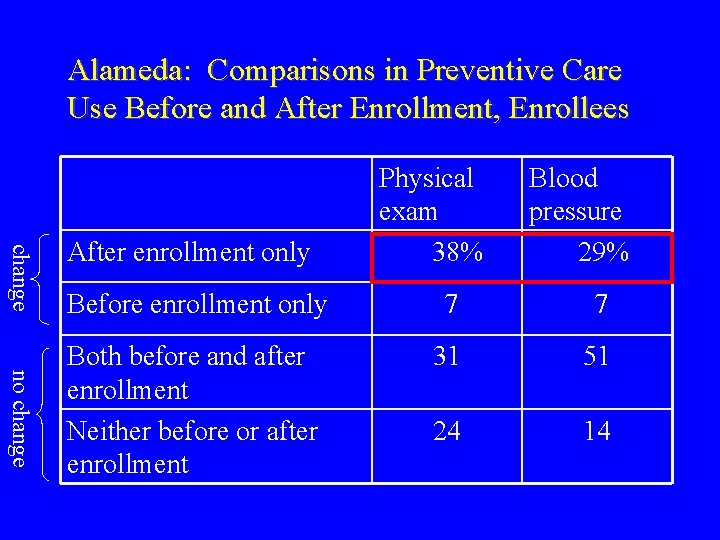
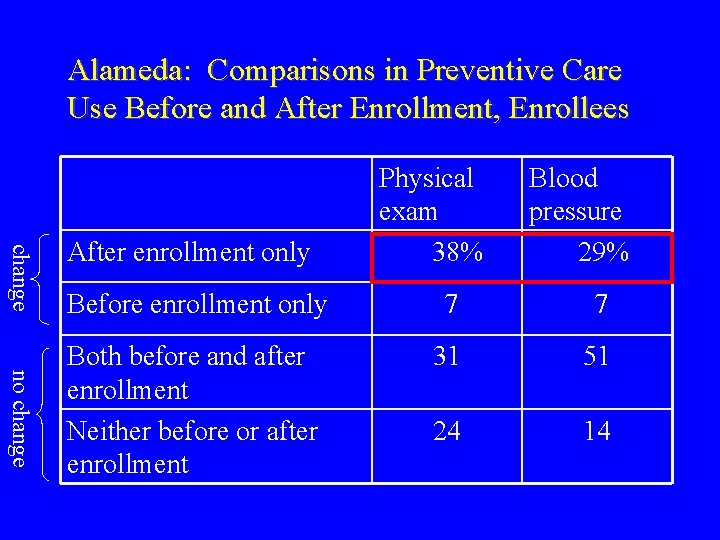
Alameda: Comparisons in Preventive Care Use Before and After Enrollment, Enrollees change After enrollment only Physical exam 38% Blood pressure 29% no change Before enrollment only 7 7 Both before and after enrollment Neither before or after enrollment 31 51 24 14
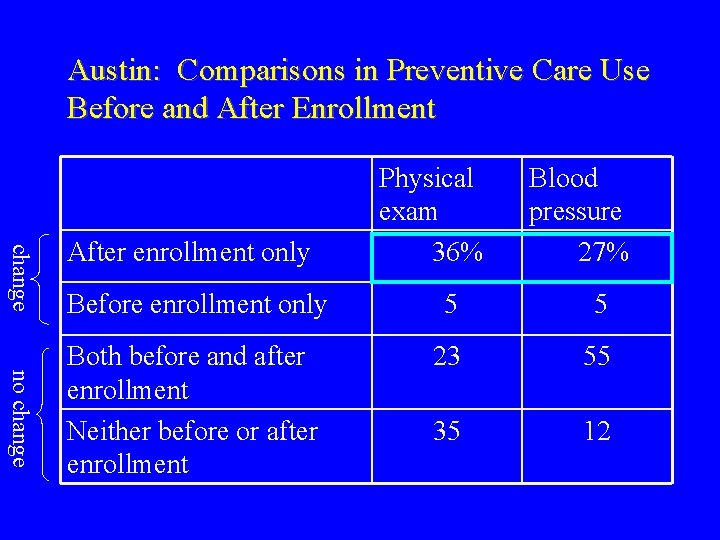
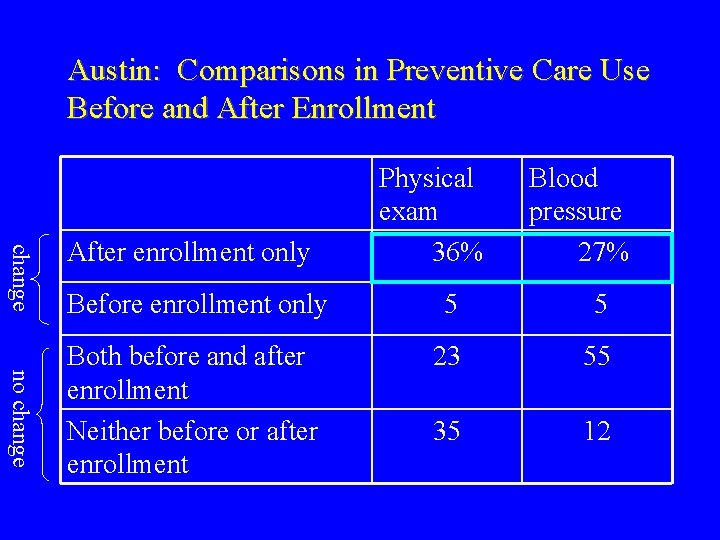
Austin: Comparisons in Preventive Care Use Before and After Enrollment change After enrollment only Physical exam 36% Blood pressure 27% no change Before enrollment only 5 5 Both before and after enrollment Neither before or after enrollment 23 55 35 12
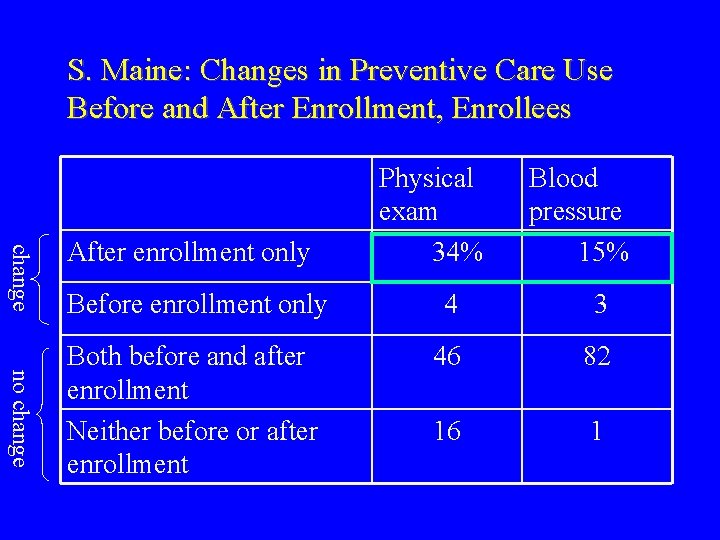
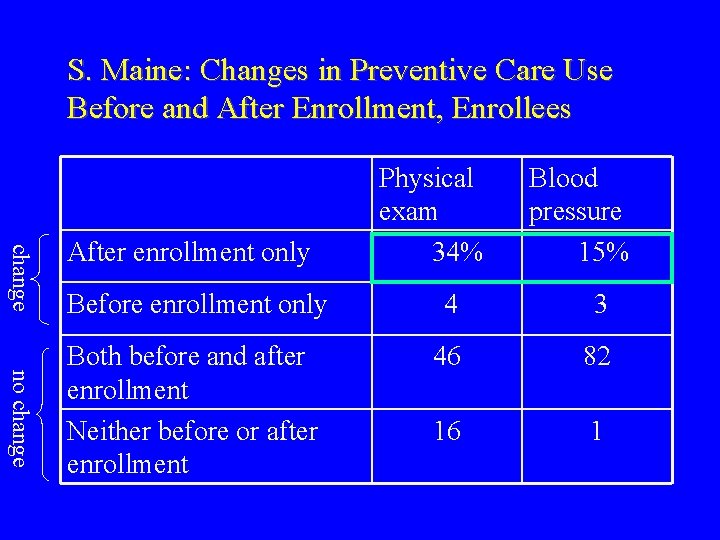
S. Maine: Changes in Preventive Care Use Before and After Enrollment, Enrollees change After enrollment only Physical exam 34% Blood pressure 15% no change Before enrollment only 4 3 Both before and after enrollment Neither before or after enrollment 46 82 16 1
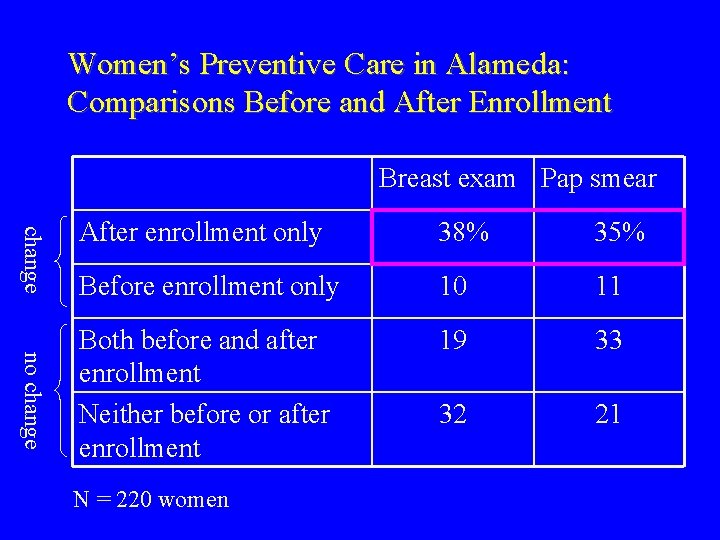
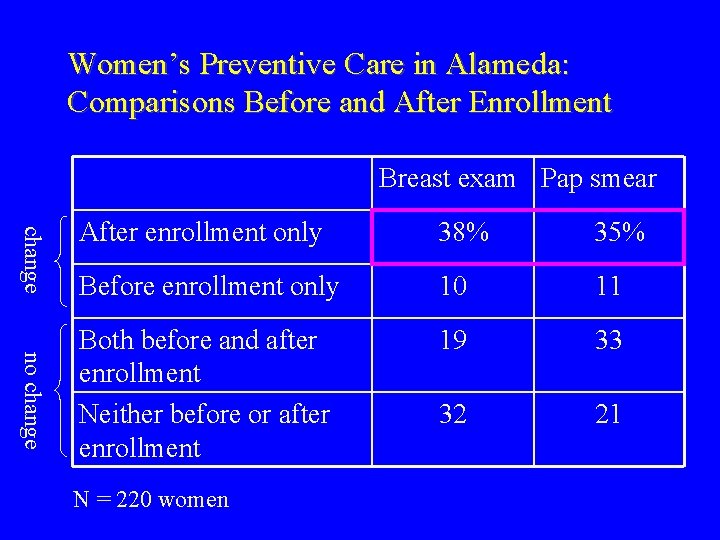
Women’s Preventive Care in Alameda: Comparisons Before and After Enrollment Breast exam Pap smear change no change After enrollment only 38% 35% Before enrollment only 10 11 Both before and after enrollment Neither before or after enrollment 19 33 32 21 N = 220 women
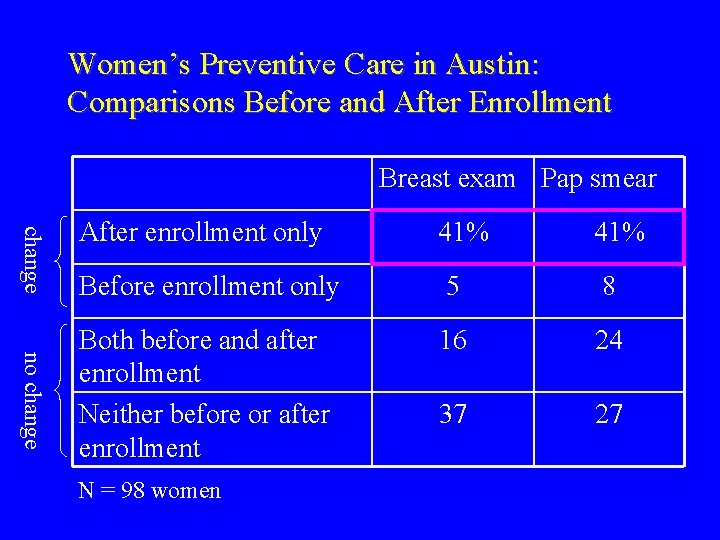
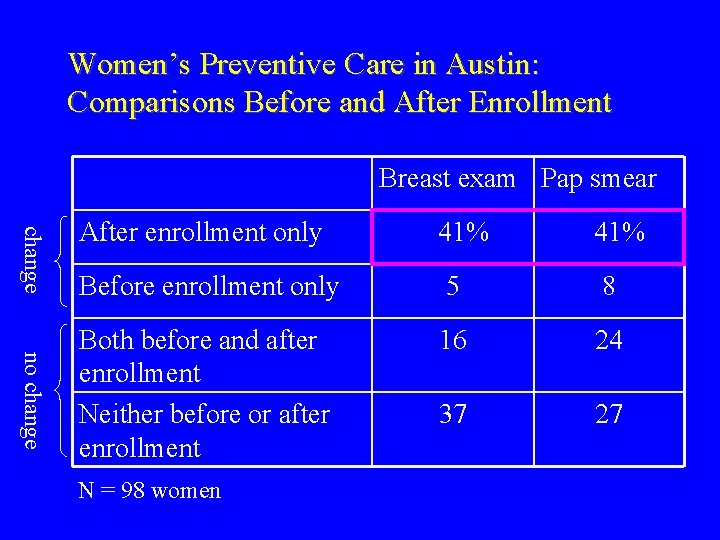
Women’s Preventive Care in Austin: Comparisons Before and After Enrollment Breast exam Pap smear change no change After enrollment only 41% Before enrollment only 5 8 Both before and after enrollment Neither before or after enrollment 16 24 37 27 N = 98 women
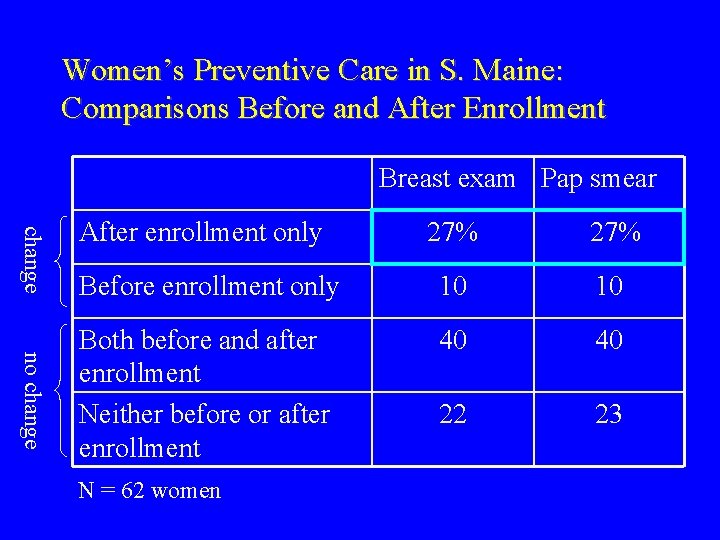
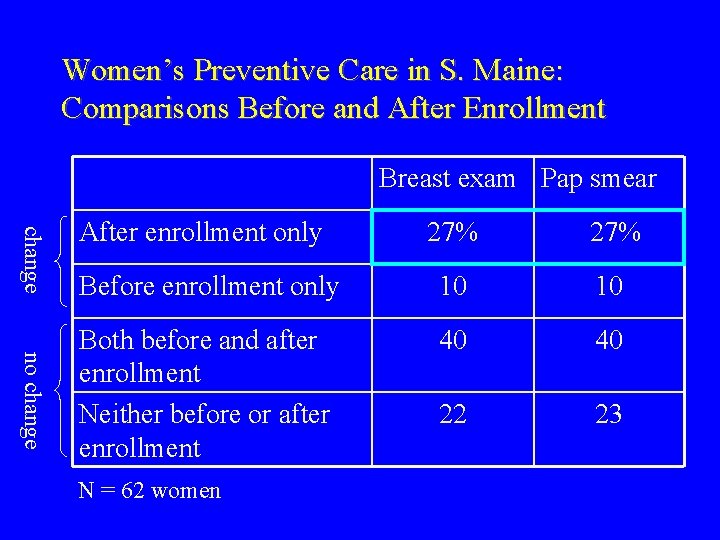
Women’s Preventive Care in S. Maine: Comparisons Before and After Enrollment Breast exam Pap smear change After enrollment only no change 27% Before enrollment only 10 10 Both before and after enrollment Neither before or after enrollment 40 40 22 23 N = 62 women
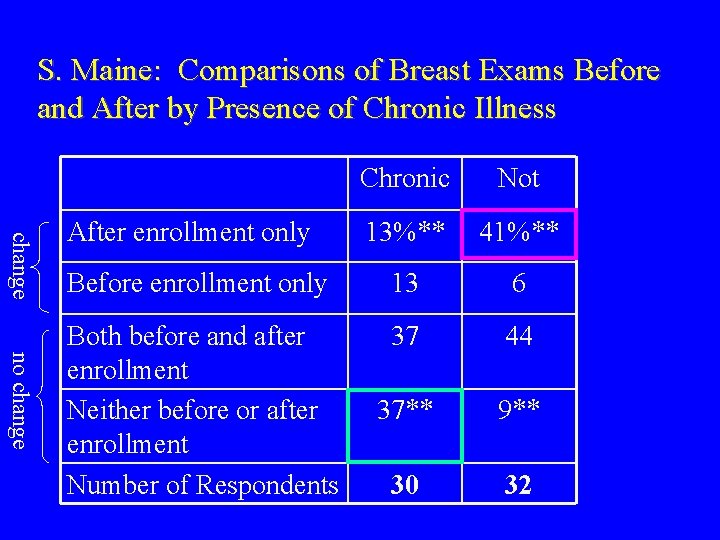
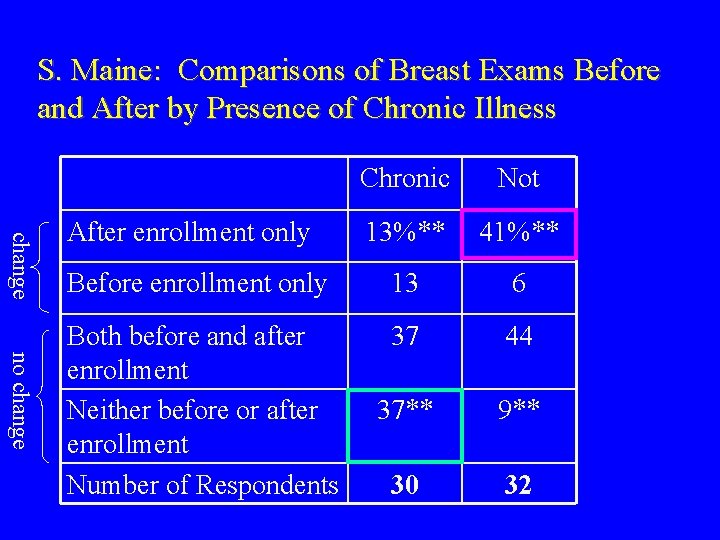
S. Maine: Comparisons of Breast Exams Before and After by Presence of Chronic Illness change no change Chronic Not 13%** 41%** Before enrollment only 13 6 Both before and after enrollment Neither before or after enrollment Number of Respondents 37 44 37** 9** 30 32 After enrollment only
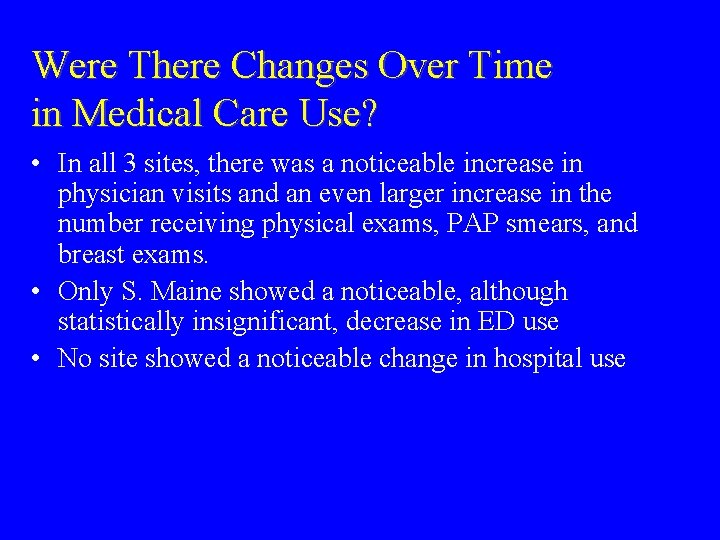
Were There Changes Over Time in Medical Care Use? • In all 3 sites, there was a noticeable increase in physician visits and an even larger increase in the number receiving physical exams, PAP smears, and breast exams. • Only S. Maine showed a noticeable, although statistically insignificant, decrease in ED use • No site showed a noticeable change in hospital use
Do Changes Over Time Differ in Different Populations? • In Alameda, changes in ED use varied significantly by race/ethnicity: Latinos were the most likely to go only before enrollment • In S. Maine, those without a chronic condition were more likely to increase use of physician services and to have a breast exam

Different Use by Different Populations • Most of the differences in utilization by race/ethnicity and by the presence of a chronic condition are differences in level of use, not change in use after enrolling – Asians were less likely to use physician, ED, and hospital services both before and after enrollment – Latinos were more likely than Asians, but less likely than “other” to use physician, ED, and hospital services both before and after – Those with a chronic condition were more likely to use ED and hospital services both before and after
Caveats • Results are based on self-reported utilization data -Utilization (e. g. , visits) tend to be underreported -Procedures (e. g. , pap smears) tend to be over-reported -Errors of omission increase with length of recall
Disenrollment • There were varying levels of disenrollment across the 3 sites, the highest in S. Maine • What were the reasons given for leaving? • Were disenrollees “different” from continuous enrollees? • What happened to disenrollees in terms of coverage, utilization, satisfaction?
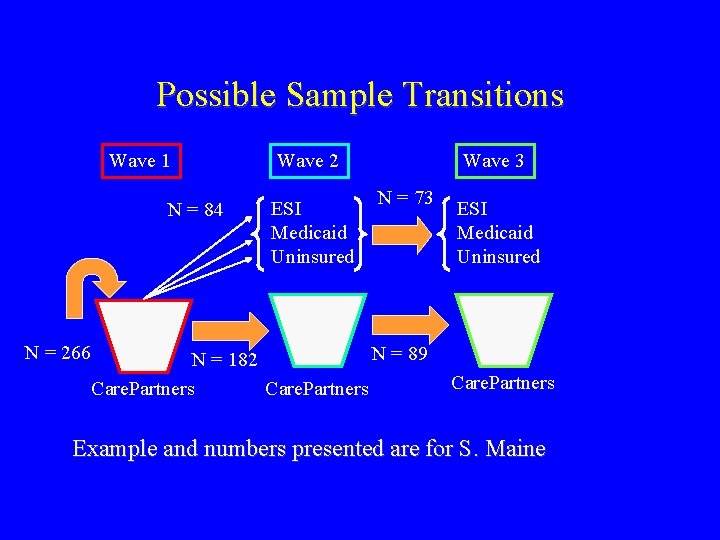
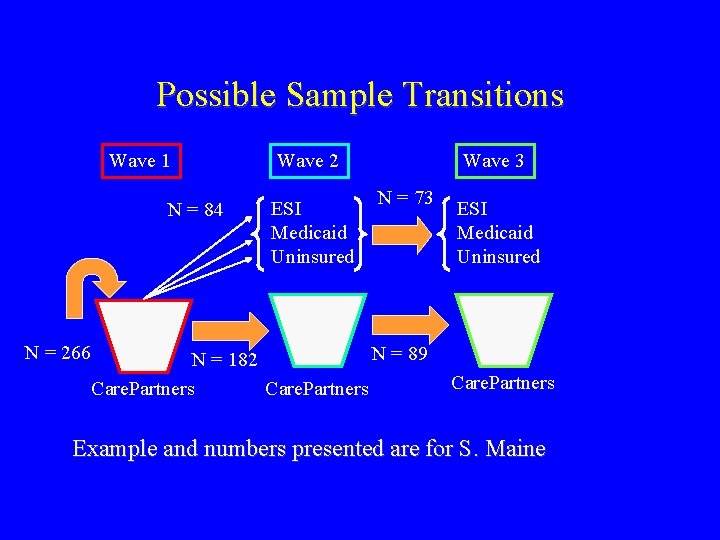
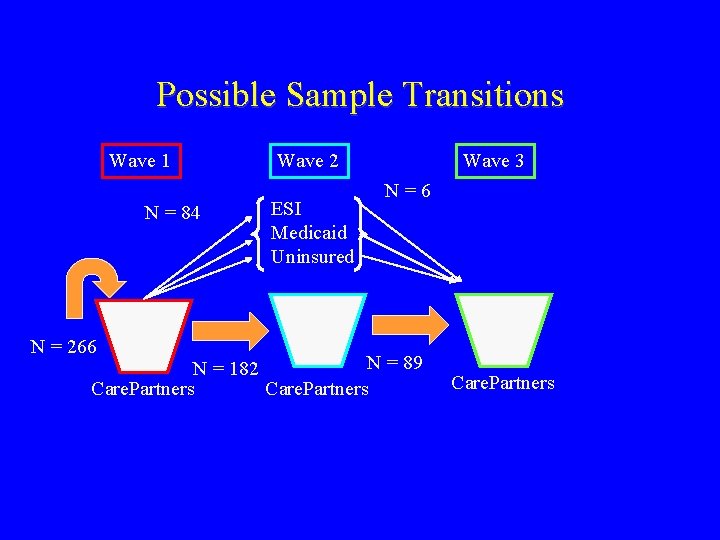
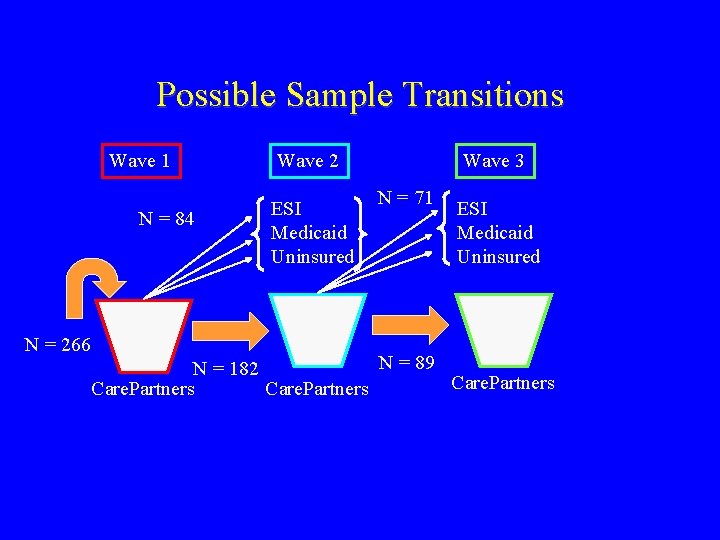
Possible Sample Transitions Wave 1 N = 84 N = 266 Wave 2 ESI Medicaid Uninsured Wave 3 N = 73 N = 89 N = 182 Care. Partners ESI Medicaid Uninsured Care. Partners Example and numbers presented are for S. Maine
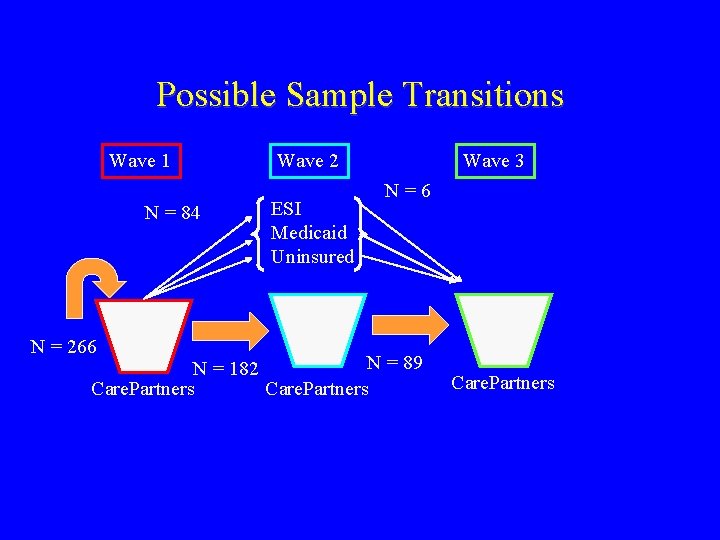
Possible Sample Transitions Wave 1 N = 84 Wave 2 ESI Medicaid Uninsured Wave 3 N=6 N = 266 N = 89 N = 182 Care. Partners
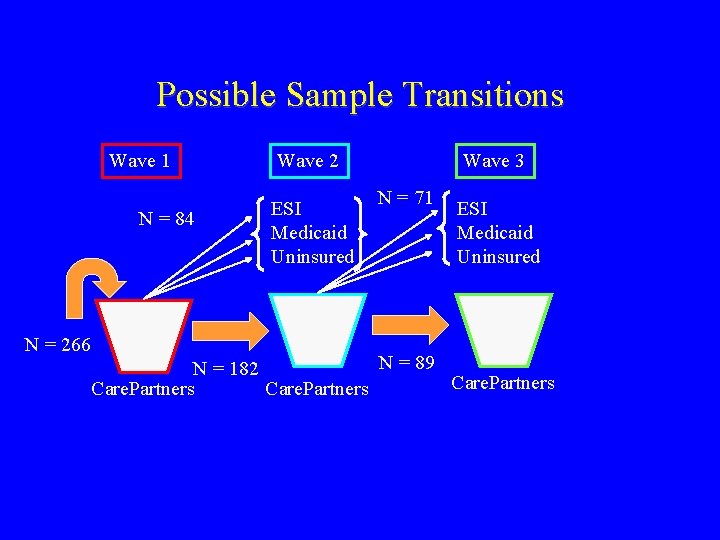
Possible Sample Transitions Wave 1 N = 84 N = 266 Wave 2 ESI Medicaid Uninsured Wave 3 N = 71 ESI Medicaid Uninsured N = 89 N = 182 Care. Partners
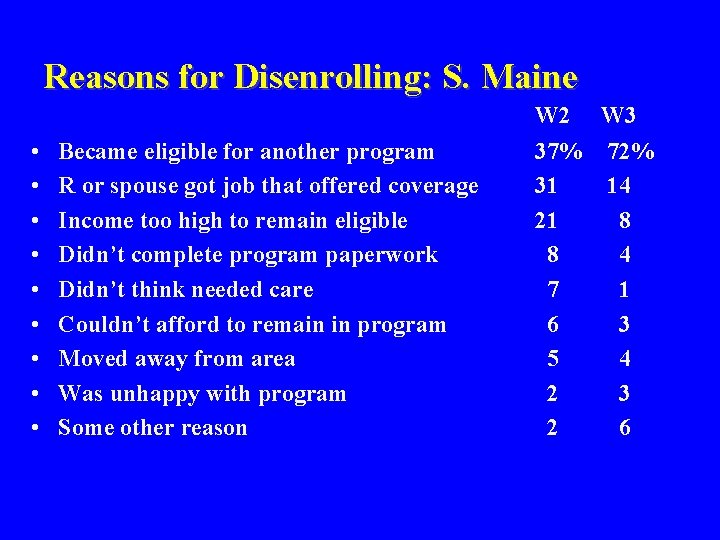
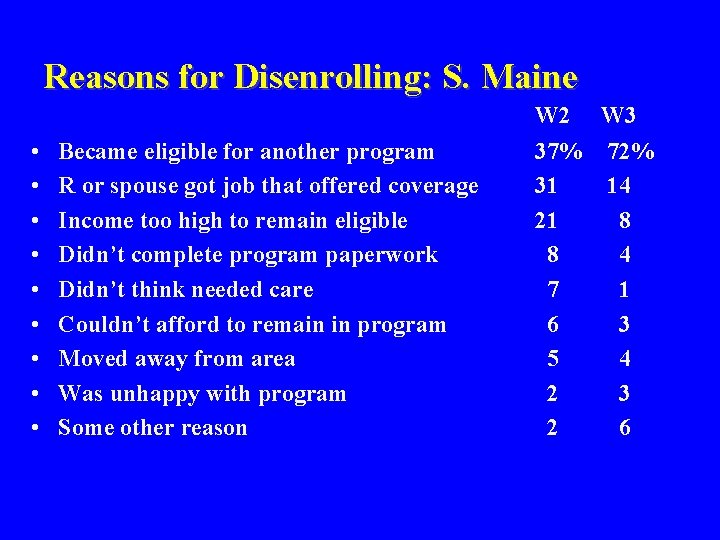
Reasons for Disenrolling: S. Maine • • • Became eligible for another program R or spouse got job that offered coverage Income too high to remain eligible Didn’t complete program paperwork Didn’t think needed care Couldn’t afford to remain in program Moved away from area Was unhappy with program Some other reason W 2 W 3 37% 31 21 8 7 6 5 2 2 72% 14 8 4 1 3 4 3 6

% of Participants by Insurance Status, Waves 2 and 3 Enrolled Disenrolled ESI Medicaid Uninsured • Wave 2 69 5 5 21 • Wave 3 69 4 8 18

Comparisons of Enrollees and Disenrollees by Insurance Status, Wave 2 Enrolled Disenrolled ESI Medicaid Uninsured • • • % Female % Married % Employed Hsehold Income % ESI before % Medicaid before 31 25 51 $15 k 24 10 25 8 100 32 k 75 0 43 36 21 13 k 57 36 37 25 57 19 k 43 4

Comparisons of Enrollees and Disenrollees by Health Status and Utilization, Wave 2 Enrolled Disenrolled ESI Medicaid Uninsured • • • % Fair or Poor HS % with Condition % Physician visit % Hospital stay % ED visit 33 49 93 15 2 0 42 100 8 2 21 79 93 23 3 22 37 91 14 3

Emerging Patterns • One group staying in program as long term source of coverage: – Part-time or self-employed workers who lack access to ESI
Emerging Patterns • Two groups tend to be using Care. Partners as stopgap measure: – Relatively healthy full-time workers who (re)gained access to ESI – Relatively sicker unemployed persons who became eligible for Medicaid
Emerging Patterns • Fourth group: – Those leaving the program who lost eligibility or failed to fill in the proper paperwork and remain uninsured
Next Steps • Investigate further how utilization changes across time (pent-up demand? ) • Continue to explore differences in use, access, and attitudes by race/ethnicity • Explore differences in use, access, and attitudes by presence of a chronic or limiting condition • Continue analysis of factors that predict retention in the program • Analyze changes in use and attitudes for disenrollees
 叫叫 abcd
叫叫 abcd Umanjenice primjeri
Umanjenice primjeri Cic certification
Cic certification What is cic certification
What is cic certification Cic portal zayed
Cic portal zayed Cic exam questions
Cic exam questions Fit 2 learn
Fit 2 learn Avaya vs customer interaction center cic
Avaya vs customer interaction center cic Cic annual report 2019
Cic annual report 2019 Apic certification study guide
Apic certification study guide Reporte crediticio sugef
Reporte crediticio sugef Cic certification requirements
Cic certification requirements Apic certification study guide
Apic certification study guide Cic
Cic Cic bim protocol
Cic bim protocol Shared future cic
Shared future cic Cic filter gain
Cic filter gain How to solve compound and absolute value inequalities
How to solve compound and absolute value inequalities Participants processes and circumstances
Participants processes and circumstances We are glad you are here
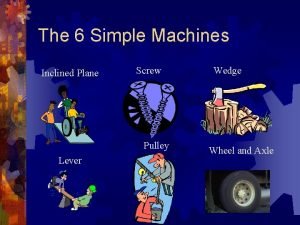
We are glad you are here Two inclined planes joined back to back
Two inclined planes joined back to back Two inclined planes joined back to back
Two inclined planes joined back to back I bar clasp indications
I bar clasp indications Single hem sheet metal
Single hem sheet metal Jay hummel
Jay hummel Examples of third class lever machines
Examples of third class lever machines An example of a solid
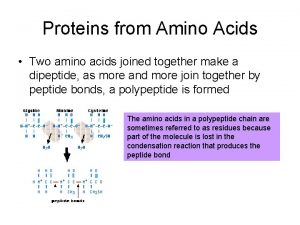
An example of a solid When two amino acids are joined together
When two amino acids are joined together What god has joined together let no man put asunder song
What god has joined together let no man put asunder song So glad you joined us
So glad you joined us Glad you joined us
Glad you joined us 4 semiquavers joined
4 semiquavers joined Inclined plane pyramids
Inclined plane pyramids Two inclined planes put together back to back
Two inclined planes put together back to back Welcome glad you are here
Welcome glad you are here Welcome glad you're here
Welcome glad you're here I newly joined the team
I newly joined the team Things that are joined together
Things that are joined together Welcome so glad you are here
Welcome so glad you are here We are glad you are here
We are glad you are here Welcome we are glad you are here
Welcome we are glad you are here Welcome we are so glad you are here
Welcome we are so glad you are here Montage editing definition
Montage editing definition Imagine that you just joined a development
Imagine that you just joined a development Amino acids are joined together in proteins by
Amino acids are joined together in proteins by Masters in survey methodology
Masters in survey methodology The big four ww1
The big four ww1 Challenge tournament example
Challenge tournament example Http://teachertech.rice.edu/participants/louviere/newton/
Http://teachertech.rice.edu/participants/louviere/newton/ Counterbalancing
Counterbalancing Financial markets and institutions jeff madura ppt
Financial markets and institutions jeff madura ppt Http://teachertech.rice.edu/participants/louviere/newton/
Http://teachertech.rice.edu/participants/louviere/newton/ Introduction of participants in training
Introduction of participants in training Gst ecosystem meaning
Gst ecosystem meaning Within subjects design
Within subjects design Participants in the business buying process
Participants in the business buying process Participants in the business buying process
Participants in the business buying process