Surgical Treatment of Stress Urinary Incontinence Dr Cecilia



























- Slides: 68

Surgical Treatment of Stress Urinary Incontinence Dr Cecilia Cheon Consultant, Department of Obs. & Gyn. Queen Elizabeth Hospital, Hong Kong, China President, HK Urgynaecology Association
Definition of Urinary Incontinence Urinary incontinence is the complaint of any involuntary leakage of urine. Abram P et al. Neuro Urodyn 02
Terminology - Symptoms • Stress urinary incontinence (SUI) - Involuntary leakage on effort or exertion, or on sneezing or coughing
Urodynamic Terminology • Urodynamic stress incontinence (USI) - Involuntary leakage of urine during increased abdominal pressure, in the absence of a detrusor contraction - Old term: Genuine stress incontinence (GSI)
Impact on Quality of Life • Embarrassment • Reduced Self esteem • Impaired emotional & psychological wellbeing • Poorer sexual relationships • Impaired social activities and relationships
Economic Issues • USA – estimated to be $8. 1 billion (Hu, 1984) • Active evaluation and treatment of nursing home residents resulted in considerable cost savings • Indirect benefit : improve QOL of sufferers, difficult to quantify
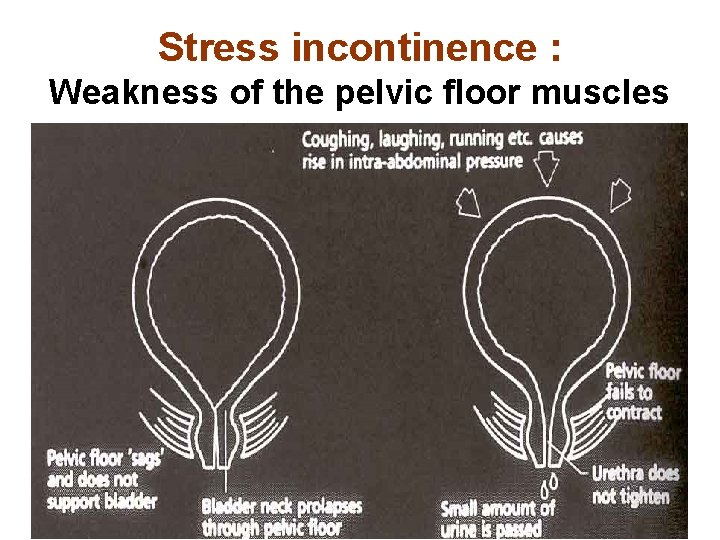
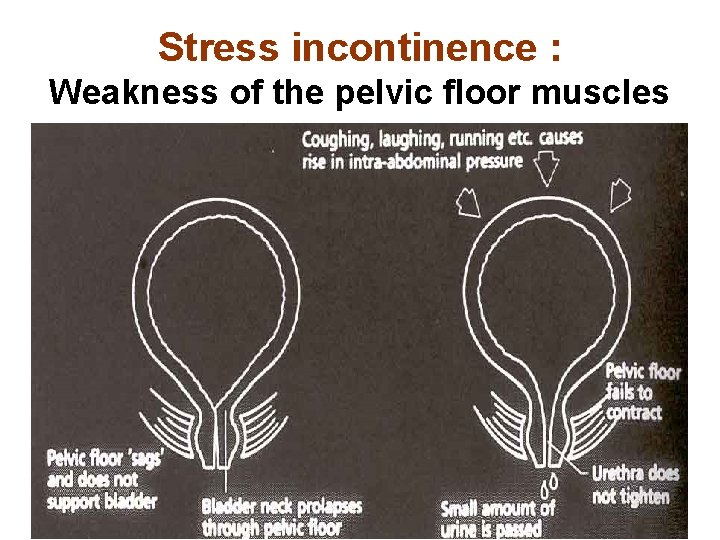
Stress incontinence : Weakness of the pelvic floor muscles
Treatment Strategy in women with USI / SUI Conservative treatment is the first line of treatment for women with SI International Consultation on Incontinence 01, Paris
Treatment for SUI 1. General measures 2. Pelvic floor exercises, PFEs 3. Biofeedback - perineometer, vaginal cones 4. Electrical stimulation treatment 5. Mechanical devices 6. Pharmacological treatment 7. Surgery
Surgical Treatment • Paravaginal repair • Bladder neck suspensions • Bladder Neck Slings / Midurethral slings • Periurethral injections • Artificial sphincter
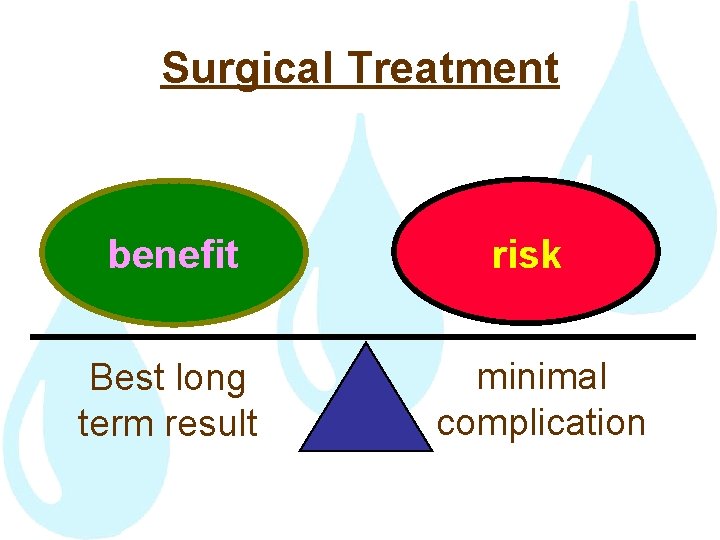
Surgical Treatment benefit Best long term result risk minimal complication

Bladder Neck Suspensions To use the anterior vagina as a hammock to elevate the bladder neck • Needle suspensions • Retropubic suspensions - abdominal - laparoscopic
Retropubic Suspensions • Burch’s • MMK
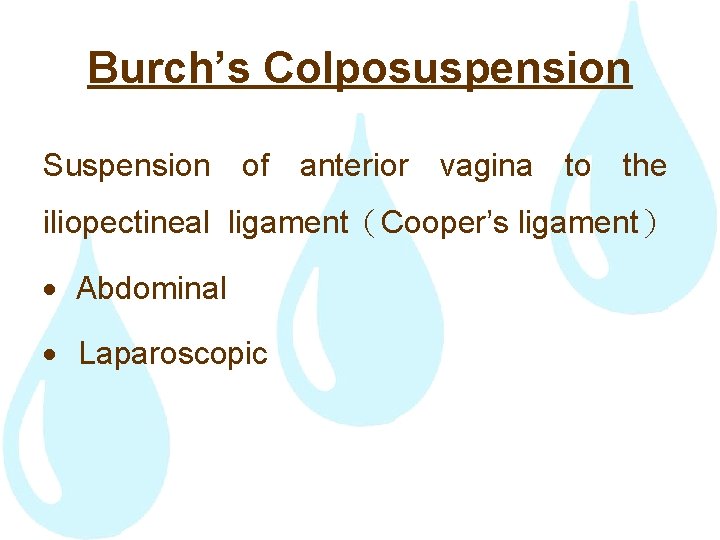
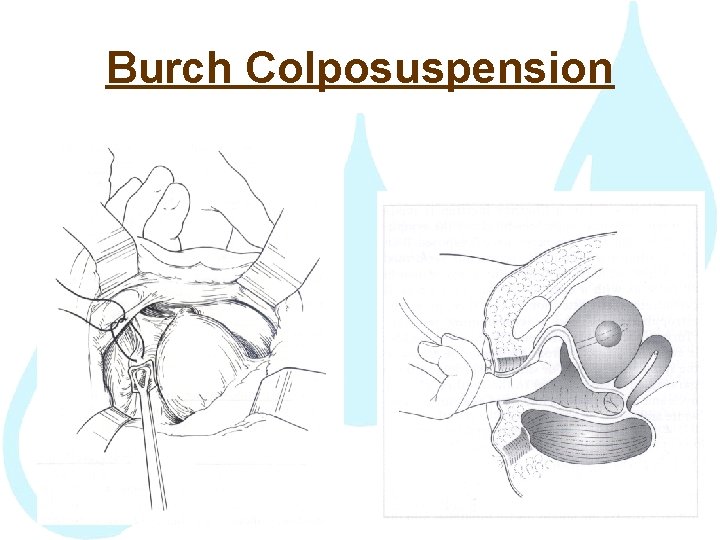
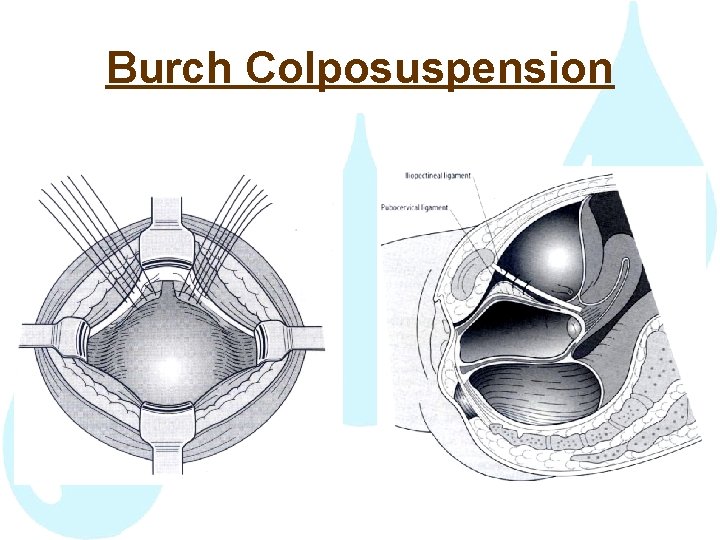
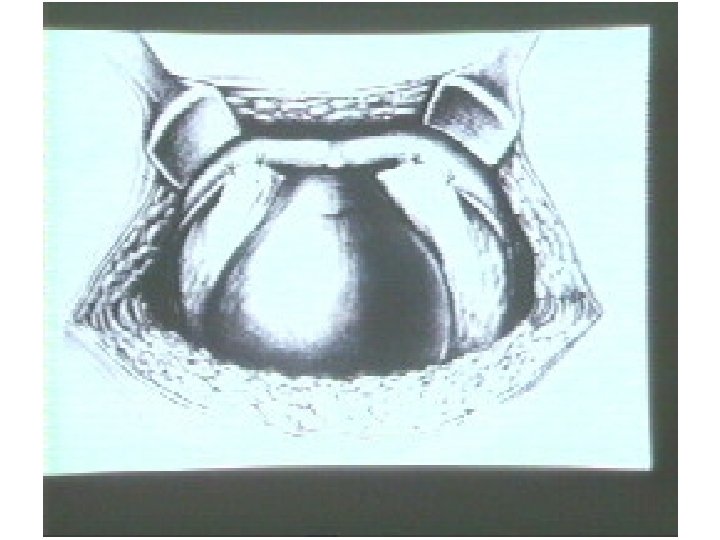
Burch’s Colposuspension Suspension of anterior vagina to the iliopectineal ligament(Cooper’s ligament) Abdominal Laparoscopic
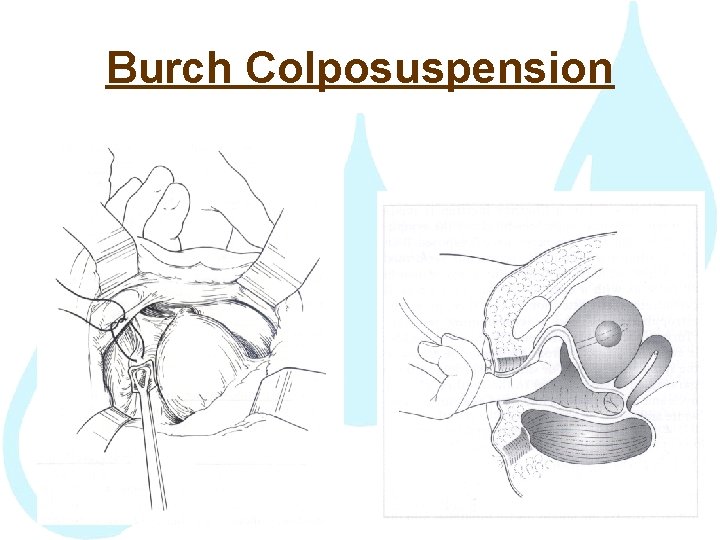
Burch Colposuspension
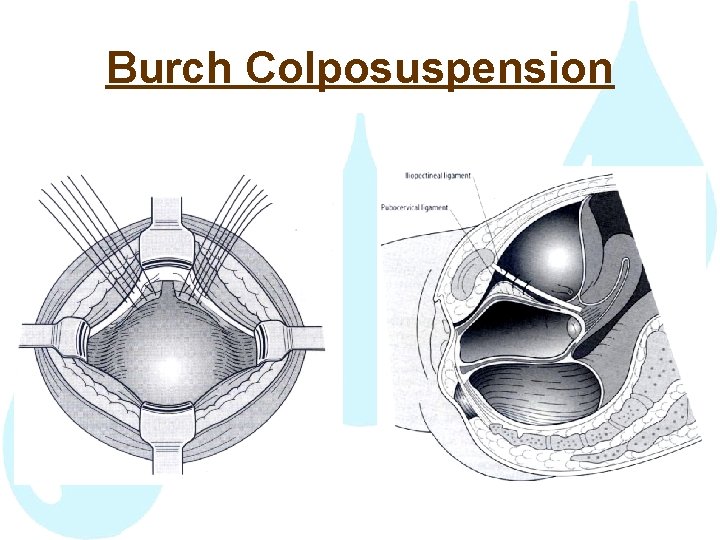
Burch Colposuspension

Subjective Cure Rate for Burch’s Operation
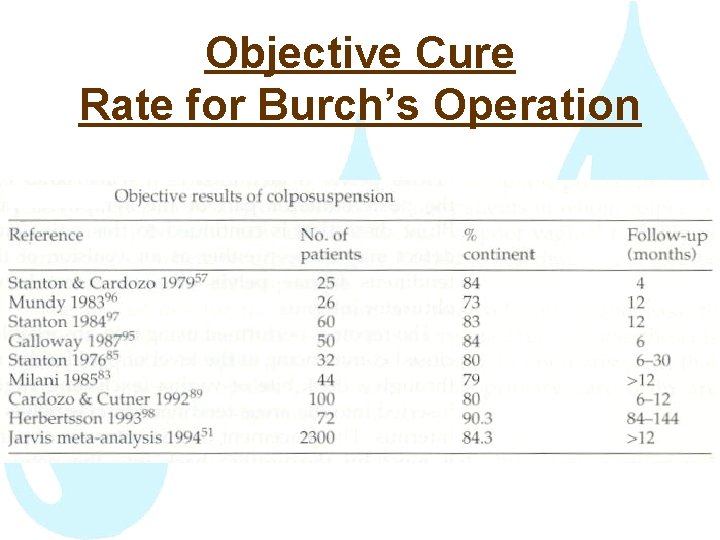
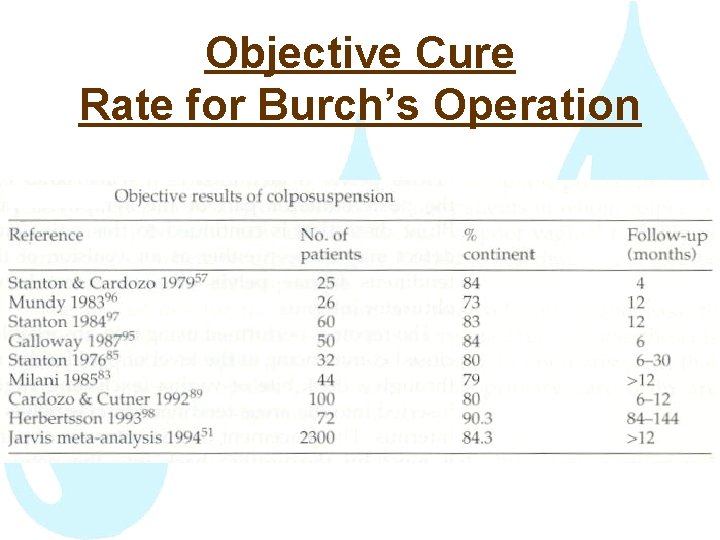
Objective Cure Rate for Burch’s Operation
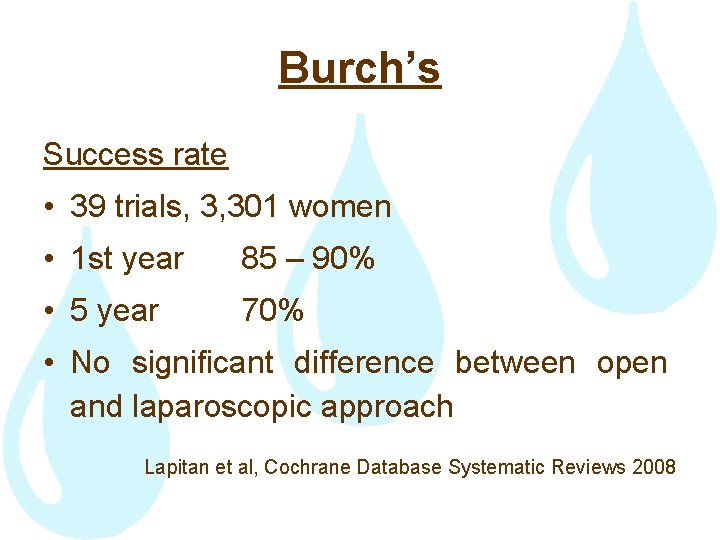
Burch’s Success rate • 39 trials, 3, 301 women • 1 st year 85 – 90% • 5 year 70% • No significant difference between open and laparoscopic approach Lapitan et al, Cochrane Database Systematic Reviews 2008
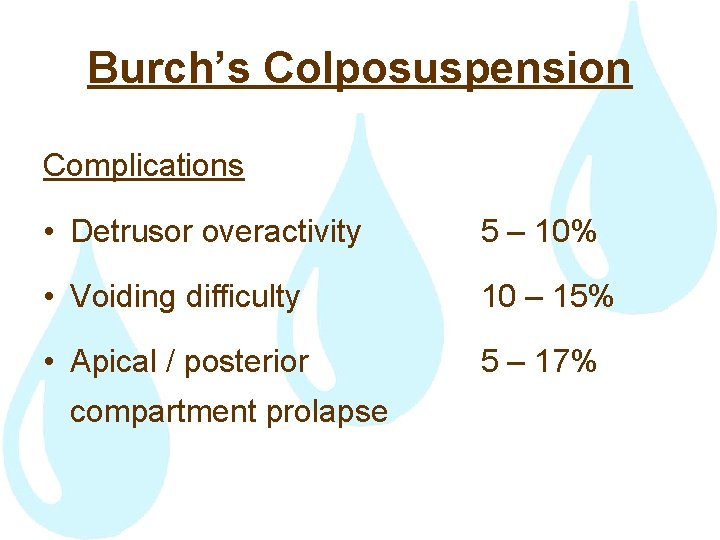
Burch’s Colposuspension Complications • Detrusor overactivity 5 – 10% • Voiding difficulty 10 – 15% • Apical / posterior 5 – 17% compartment prolapse
Slings Sling under the bladder neck or mid-urethra • Correct hypermobility • Increase sphincter closure pressure
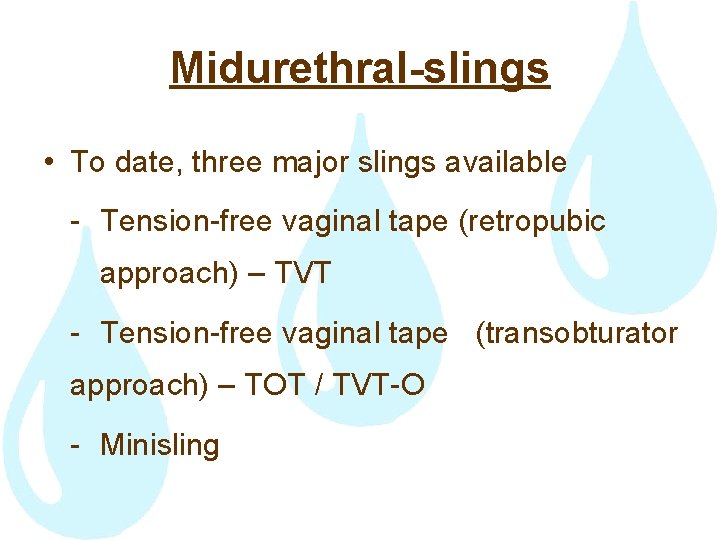
Midurethral-slings • To date, three major slings available - Tension-free vaginal tape (retropubic approach) – TVT - Tension-free vaginal tape (transobturator approach) – TOT / TVT-O - Minisling

The Integral Theory of Continence • Pelvic organ prolapse mainly caused by connective tissue laxity in the vagina or its supporting ligaments • Stress urinary incontinence is essentially due to pelvic floor muscle weakness

The pictorial diagnostic algorithm summarizes the relationships between structural damage in the three zones and urinary and fecal symptoms. Arrows represent directional muscle forces. Anterior zone: external urethral meatus to bladder neck; middle zone: bladder neck to cervix; posterior zone: vaginal apex, posterior vaginal wall, and perineal body. PRM = m. puborectalis; PCM = pubococcygeus; PUL = pubourethral ligament; ATFP = arcus tendineus fascia pelvis; N = bladder base stretch receptors
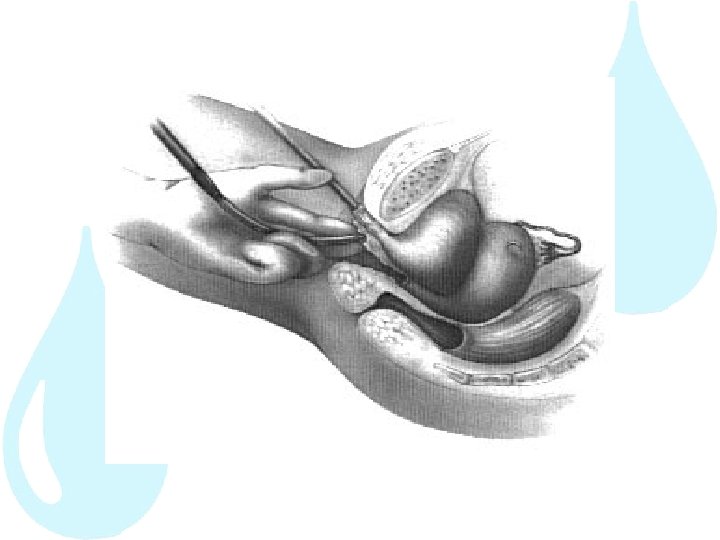
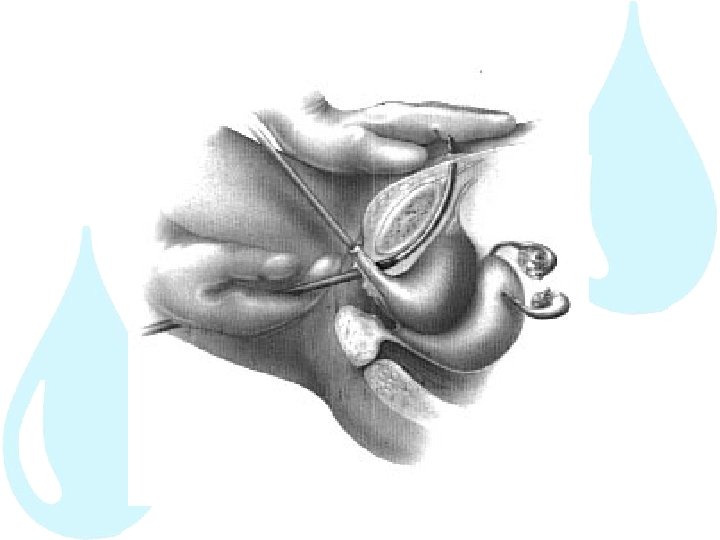
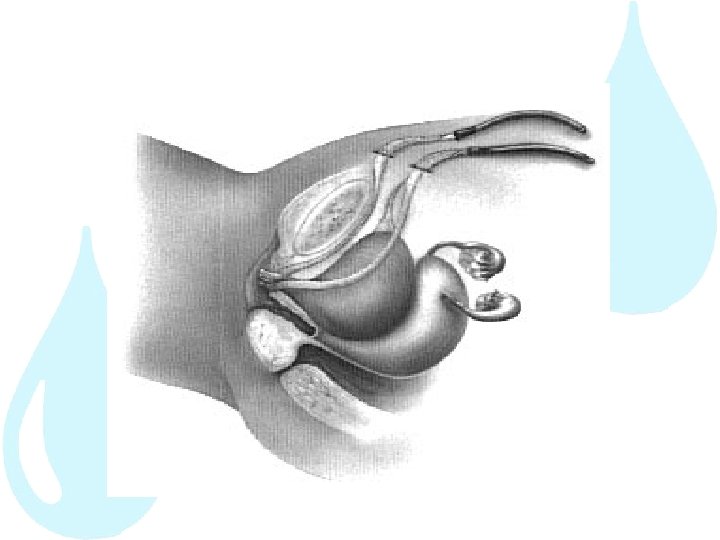
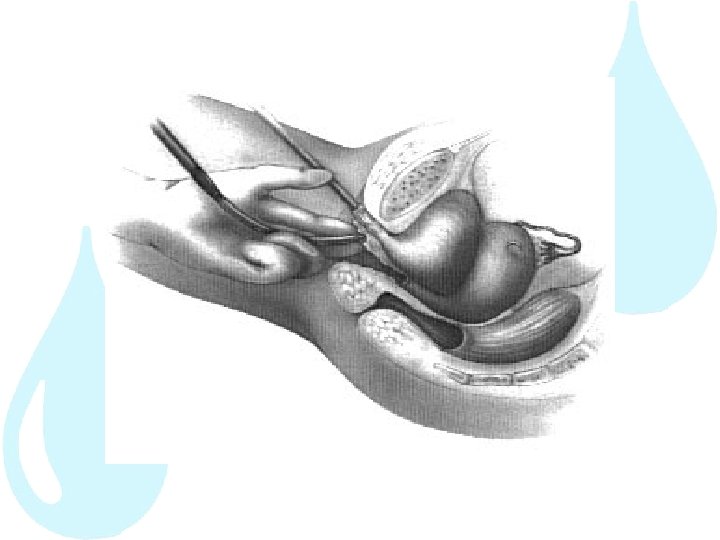
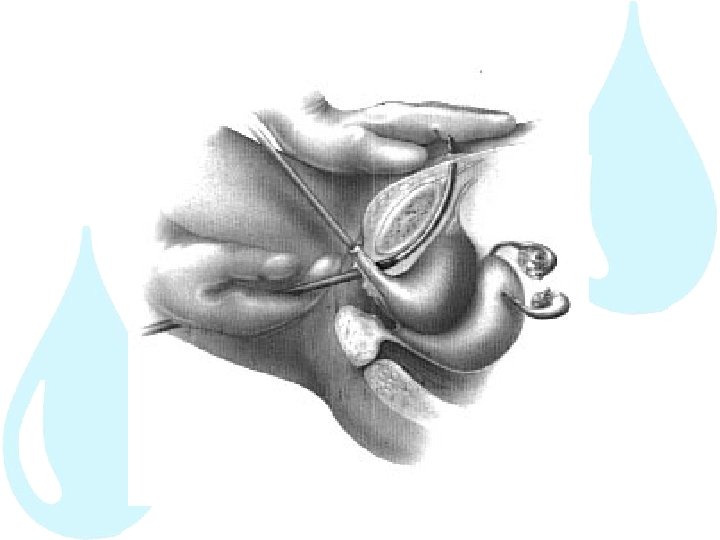
Tension-free Vaginal Tape (TVT) • Ulmsten et al in 1996 • Treats stress incontinence by positioning a polypropylene mesh tape underneath the urethra • Monofilament, macroporous, >75 microns • Free passage of marophages • In growth of fibroblast • Minimize erosion / infection

Tension-free vaginal Tape





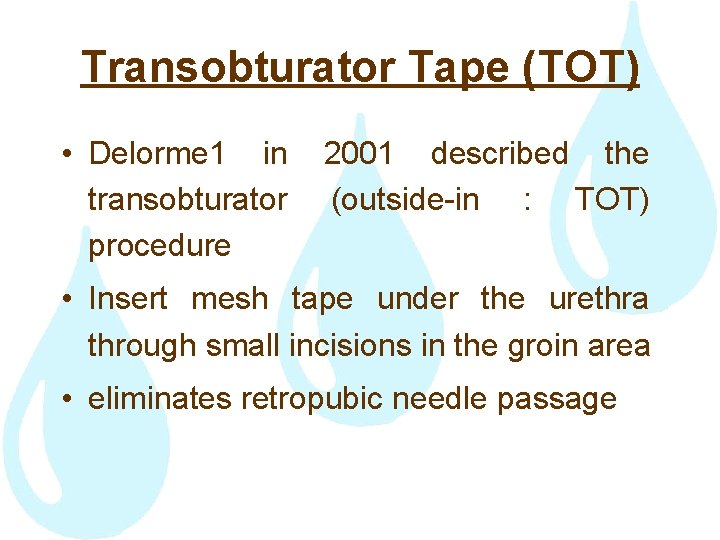
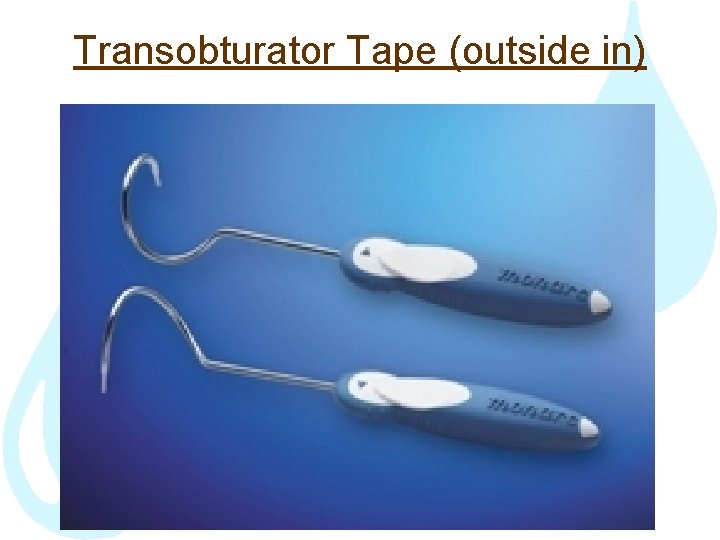
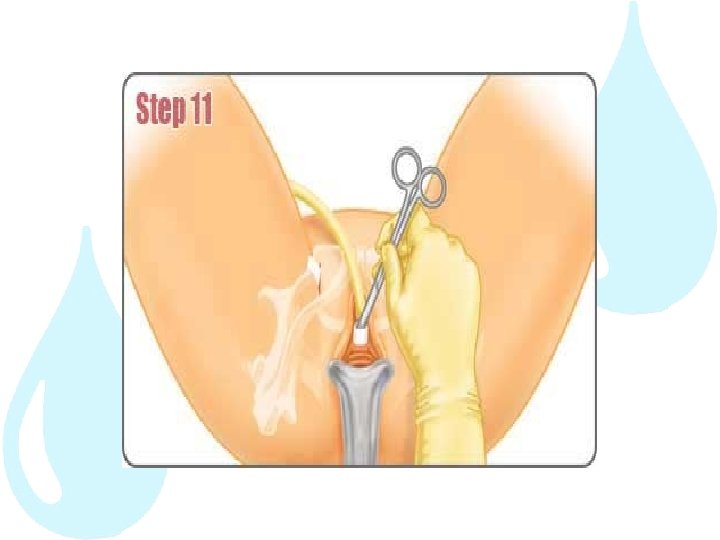
Transobturator Tape (TOT) • Delorme 1 in transobturator procedure 2001 described the (outside-in : TOT) • Insert mesh tape under the urethra through small incisions in the groin area • eliminates retropubic needle passage
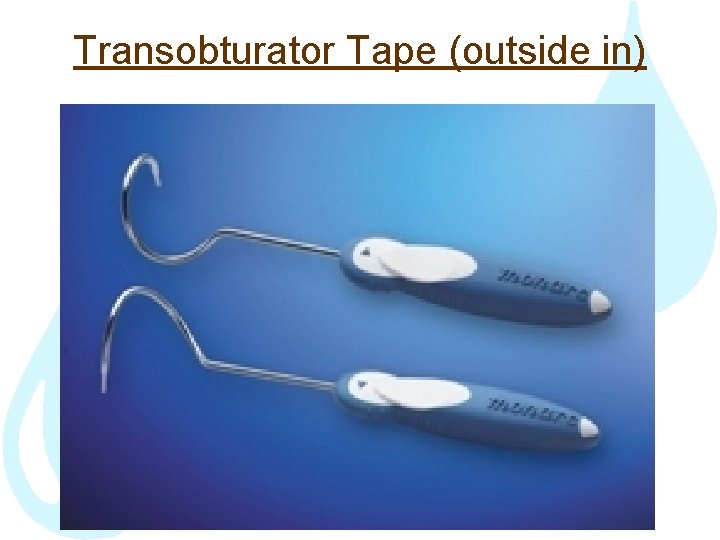
Transobturator Tape (outside in)









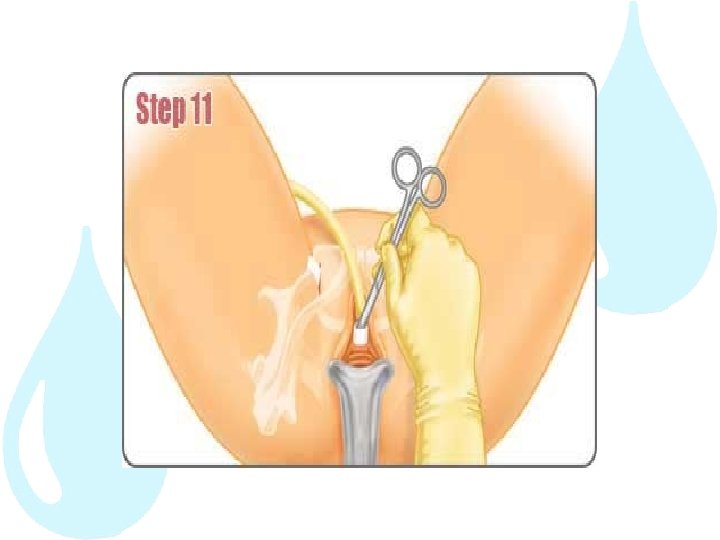

Transobturator Tape (TOT-O) • A variation of the technique has been described in 2003 by de Leval termed the TOT vaginal tape ‘‘inside-out’’ technique (TVT-O)

Transobturator Tape (inside out)

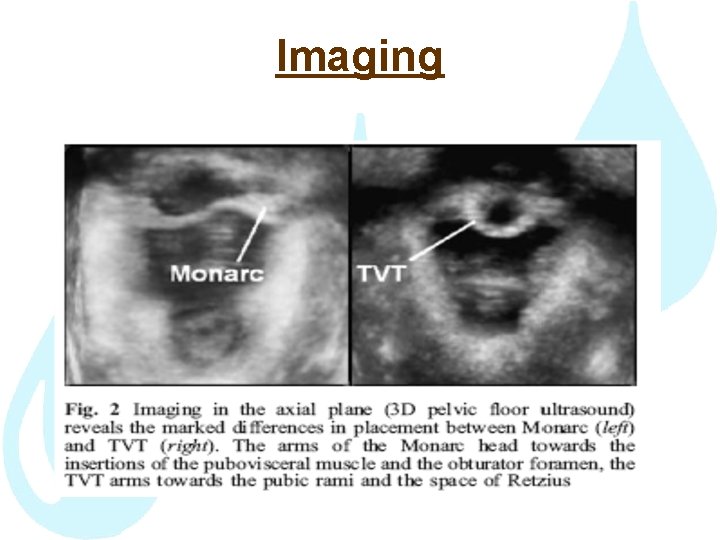
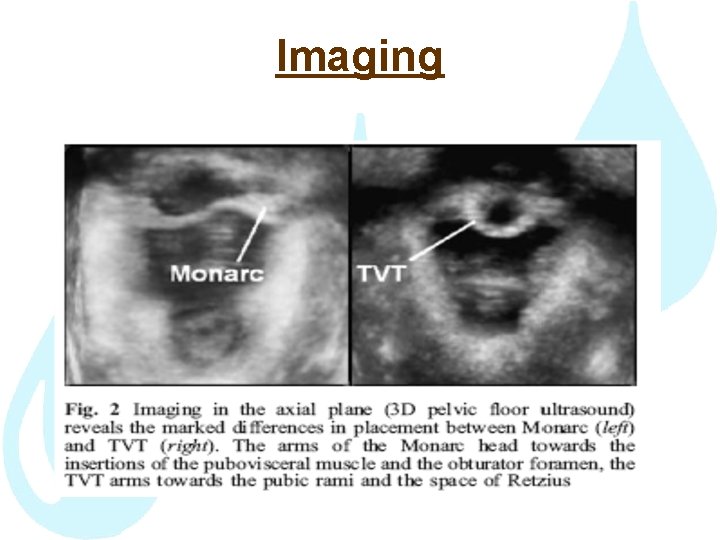
Imaging
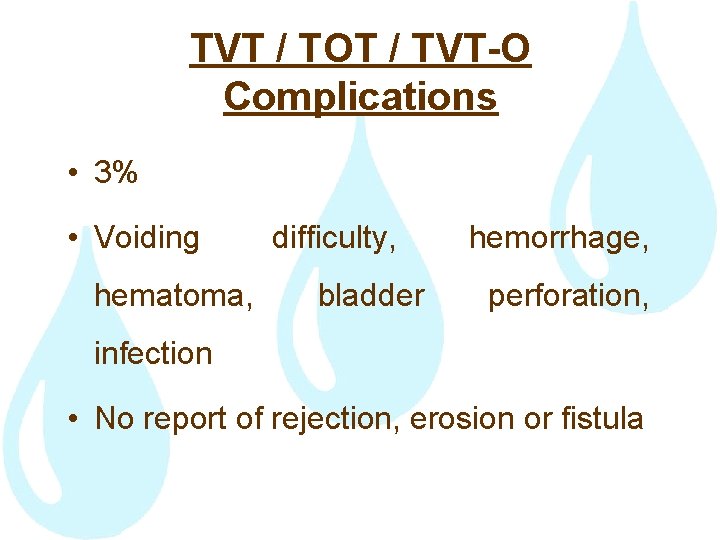
TVT / TOT / TVT-O Complications • 3% • Voiding hematoma, difficulty, bladder hemorrhage, perforation, infection • No report of rejection, erosion or fistula
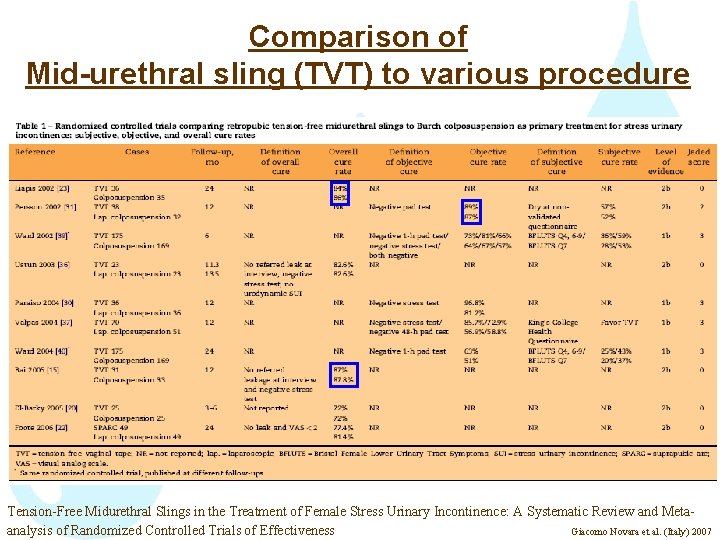
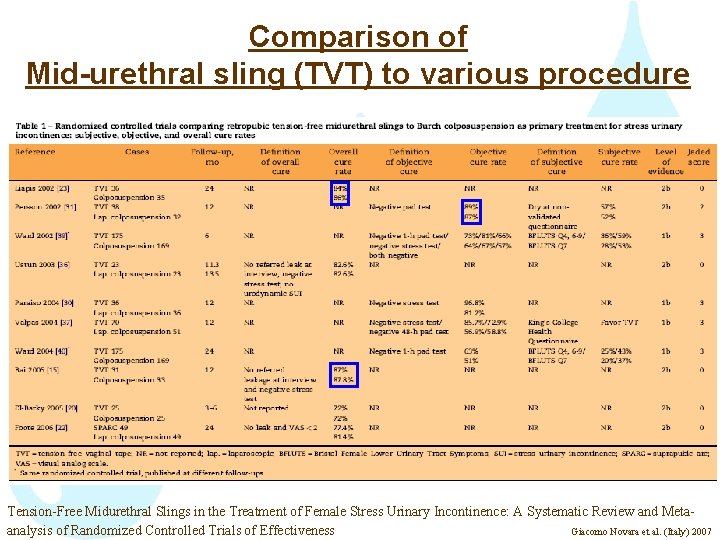
Comparison of Mid-urethral sling (TVT) to various procedure Tension-Free Midurethral Slings in the Treatment of Female Stress Urinary Incontinence: A Systematic Review and Metaanalysis of Randomized Controlled Trials of Effectiveness Giacomo Novara et al. (Italy) 2007
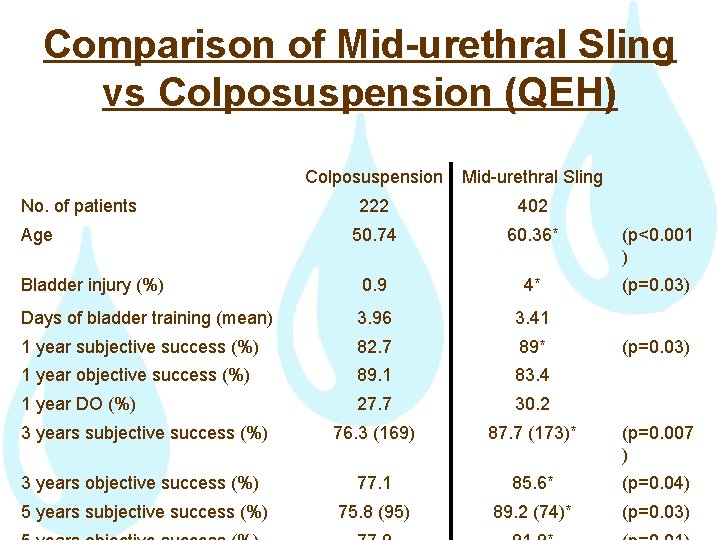
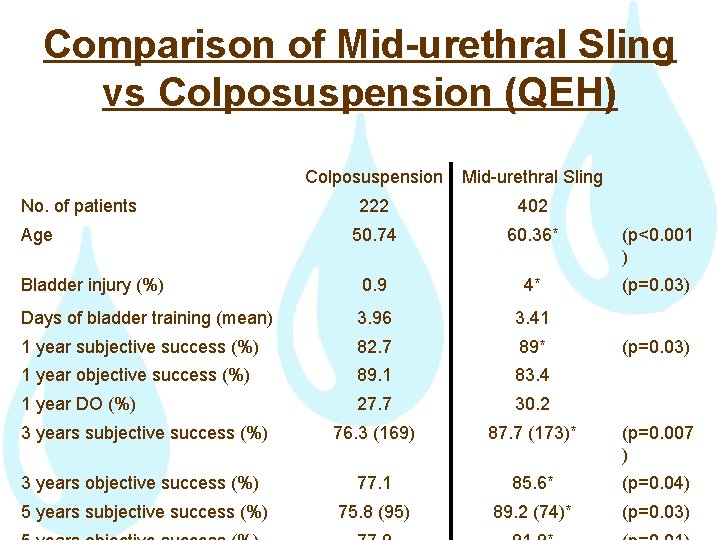
Comparison of Mid-urethral Sling vs Colposuspension (QEH) Colposuspension Mid-urethral Sling 222 402 50. 74 60. 36* (p<0. 001 ) Bladder injury (%) 0. 9 4* (p=0. 03) Days of bladder training (mean) 3. 96 3. 41 1 year subjective success (%) 82. 7 89* 1 year objective success (%) 89. 1 83. 4 1 year DO (%) 27. 7 30. 2 3 years subjective success (%) 76. 3 (169) 87. 7 (173)* (p=0. 007 ) 3 years objective success (%) 77. 1 85. 6* (p=0. 04) 5 years subjective success (%) 75. 8 (95) 89. 2 (74)* (p=0. 03) No. of patients Age (p=0. 03)
• Today, mid-urethral slings not only have replaced the Burch colposuspension as the gold standard in the treatment of SUI but also are even more often performed than colposuspension • Easy to perform, superior in terms of operation time, postoperative pain, and hospital stays • but similar cure rates
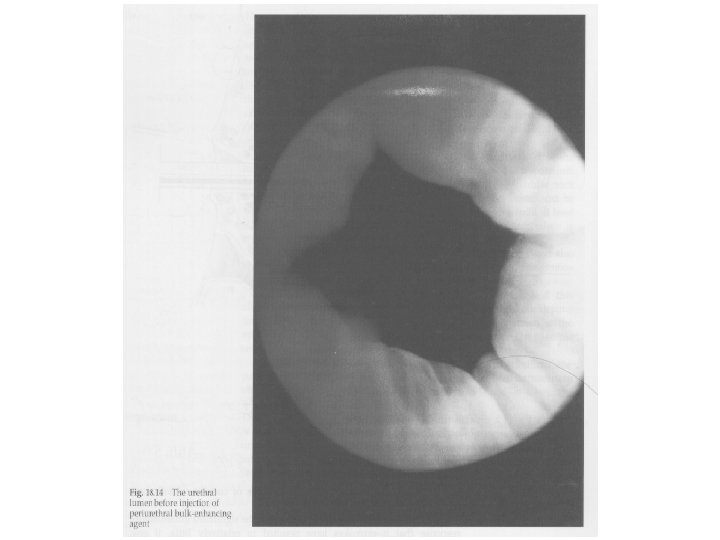
Peri-urethral Injection Use of injectable bulk forming agents to increase the urethral closure pressure
Peri-urethral Injection Material • Fat • Collagen • Silicone
Peri-urethral Injection Advantages • Safe Disadvantages • Low success rate 25 – 60% • Expensive • Need to be repeated every 1 -2 year


Artificial Sphincter • Last resort • Use when all the other operation have failed

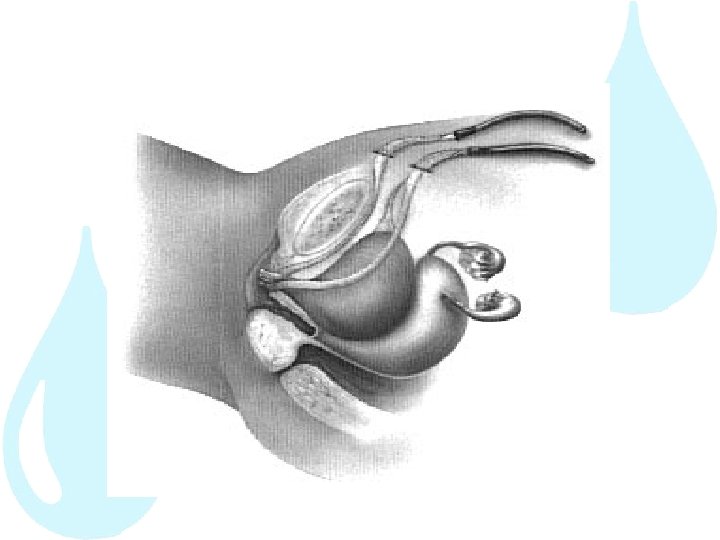
Artificial Sphincter
Conclusions • 1 in 2 women in HK has urinary symptoms 1 in 3 women has SUI • Much advances made in the care of female urinary incontinence • Effective treatment available which can significantly improve women’s Qo. L
Conclusion • The concept of the midurethral sling has revolutionized surgical treatment of SUI. Its minimally invasive approach and success rates have led to an increasing acceptance of the technique • TVT and TOT are both comparable in cure rate • The TOT approach is a potentially safer method owing to the avoidance of the retropubic space: bladder, vessels, bowel injury • Pregnancy is not contraindicated and cesarean is not abolute
• Long-term studies and RCTs are needed to identify the proper indications for the various types of slings and to assess efficacy and complication rates over time.

 Sacral reflex
Sacral reflex Coital incontinence
Coital incontinence Acfi appraisal pack
Acfi appraisal pack Acupuncture for incontinence
Acupuncture for incontinence Vaginal pessary
Vaginal pessary Chapter 10 stress responses and stress management
Chapter 10 stress responses and stress management True strain equation
True strain equation Axial normal stress
Axial normal stress Tres amigas ana beatriz y carmen
Tres amigas ana beatriz y carmen Cecilia gerber
Cecilia gerber Cecilia ventura
Cecilia ventura Chacn
Chacn Micropatia
Micropatia Dr varjú cecília
Dr varjú cecília Cecília meireles poemas curtos
Cecília meireles poemas curtos Cecilia bailliet
Cecilia bailliet Cecilia del toro
Cecilia del toro Amigdalitits
Amigdalitits Cecilia rose lap
Cecilia rose lap Cecilia lunardini
Cecilia lunardini Cecilia r aragon
Cecilia r aragon Gunnarsson fifa 19
Gunnarsson fifa 19 Alex liu cecilia liu
Alex liu cecilia liu Evidensbaserad metod
Evidensbaserad metod Colangiohepatitis en gatos
Colangiohepatitis en gatos Cecilia tinonin
Cecilia tinonin Cecilia espinola
Cecilia espinola Cecilia aversa
Cecilia aversa Luigi salvioni unipd
Luigi salvioni unipd Usenet messages maria
Usenet messages maria Cecilia taboada
Cecilia taboada Cecilia vargas abc
Cecilia vargas abc Cecilia gallego
Cecilia gallego Diagrama de flujo de como freir un huevo
Diagrama de flujo de como freir un huevo Cecilia brioni
Cecilia brioni Cecilia strand
Cecilia strand Maria cecilia luise
Maria cecilia luise Antonio skarmeta biografia
Antonio skarmeta biografia Fernando botero cecilia zambrano
Fernando botero cecilia zambrano O menino azul cecília meireles
O menino azul cecília meireles A song for st cecilia's day by john dryden
A song for st cecilia's day by john dryden Cecilia loyola
Cecilia loyola Cecilia gomez melendez
Cecilia gomez melendez Cecilia montana
Cecilia montana Gst 111 communication in english
Gst 111 communication in english Cecilia moraga
Cecilia moraga Cecilia velarde
Cecilia velarde Wat is die elemente van drama
Wat is die elemente van drama Cecilia lodi
Cecilia lodi Stanchi cecilia ig
Stanchi cecilia ig Cecilia sundberg
Cecilia sundberg Cecilia cunningham
Cecilia cunningham Cecilia he
Cecilia he Urinary bladder
Urinary bladder Cortical nephron
Cortical nephron Chapter 30 the urinary system workbook answers
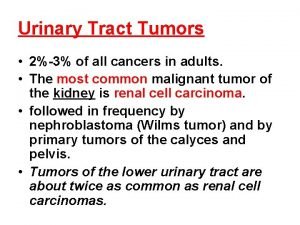
Chapter 30 the urinary system workbook answers Tumor in the urinary tract
Tumor in the urinary tract External anatomy of a rat
External anatomy of a rat Alteration in urinary elimination
Alteration in urinary elimination Physiology of urine formation
Physiology of urine formation Urinary system also known as
Urinary system also known as A combining form for calyx is
A combining form for calyx is _____ is difficulty in starting a urinary stream.
_____ is difficulty in starting a urinary stream. Where are the kidneys located in the body
Where are the kidneys located in the body Chapter 24 urinary elimination
Chapter 24 urinary elimination Spleen function
Spleen function ç
ç Figure 15-3 the urinary system
Figure 15-3 the urinary system Urinary system interesting facts
Urinary system interesting facts