Surgical Skin Preparation Resource from AORN Standards and

- Slides: 40

Surgical Skin Preparation Resource from AORN Standards and Recommended practices 2015
Skin Preparation Rationale Removes dirt and transient microbes from skin. Reduces resident microbial count in the shortest time, with the least amount of tissue irritation, which prevents rapid rebound growth of microbes. Skin can NEVER be sterilized.
Skin Preparation Factors considered: ◦ Condition of area involved. ◦ Number and kind of contaminants. ◦ Characteristics of the skin to be disinfected. ◦ General physical condition of patient.
Skin Prep—Control of Sources of Infection Goal is to lower the amount of bacteria on skin. Incision site, and area immediately surrounding, should be as FREE of microorganisms as possible.
Elements of Skin Preparation Pre-operative antiseptic showers. One night before and one in the morning before OR. Pre-operative hair removal. Remove as little as possible with clippers. Immediate surgical site preparation in the operating room with surgeon choice of prep solutions.
Elements of Skin Preparation Pre-operative showers: ◦ CDC (Center for Disease Control) “strongly recommends” that the facility require a patient to shower on the operative day, or night before, to reduce microbial colony counts on the skin. ◦ Chlorhexidine Gluconate showers have been shown to reduce skin microbial counts nine-fold. ◦ CMC has their patients take 2 showers with CHG 2%, one the night before and one the morning of surgery. ◦ CMC Inpatients will be instructed or assisted to take two preoperative showers, one the night before surgery and the second the morning of surgery, using chlorhexidine gluconate (CHG) liquid or sponge/brush or the Sage wipes (CHG) to reduce skin flora.
Elements of Skin Preparation Pre-operative hair removal: ◦ Clipping hair immediately before the surgery has shown a 1. 8% SSI (Surgical Site Infection) in comparison to 4. 0% SSI when clipping the night before. ◦ Using razors causes a higher incidence of skin irritation than clippers. ; SCIP measures require the use of clippers only in OR.
Elements of Skin Preparation Surgical Site Preparation: ◦ Should take place minutes before start of procedure. ◦ AORN states: “condition of skin at the surgical site should be assessed prior to preparation for rashes, skin eruptions and abrasions. ” ◦ Skin should be free of contamination (dirt, soil or other debris) before skin preparation is initiated.
Hair Removal If possible, hair is best left at the surgical site. Hair removal will depend on amount, location of incision and type of procedure to be performed. Pre-operative hair removal has been associated with an increased risk of surgical site infection. Assess for rashes, moles, warts, skin breaks, other conditions at surgical site that might increase the chance of infection. Report any findings to the surgeon.
Hair Removal Clippers are preferred method. ◦ Decrease potential for nicks. ◦ Decrease potential for infection. ◦ Clipping immediately before surgery (or as near as possible) is recommended. © 3 M Co. Used by Permission Depilatory—requires a pretest to make sure patient is not sensitive. Shave (not recommended)—studies have shown a direct relationship with increase of infections.
Hair Removal Should take place in a private place. Good lighting. Avoid scratching, nicking or cutting skin. As close to surgery as possible. To prevent dispersal of hair in the OR, hair removal should be performed OUTSIDE the OR. Follow policies established by facility Surgical Committee.
Properties of Antiseptic Skin Preparation Products Effectively cleans. Microbial count is reduced rapidly. Broad spectrum activity. Easy application. Non-irritating, non-toxic. © 3 M Co. Used by Permission Residual protection is provided.
Anti-microbial Agents Iodophors ◦ Betadine Scrub ◦ Betadine Solution ◦ Betadine Gel
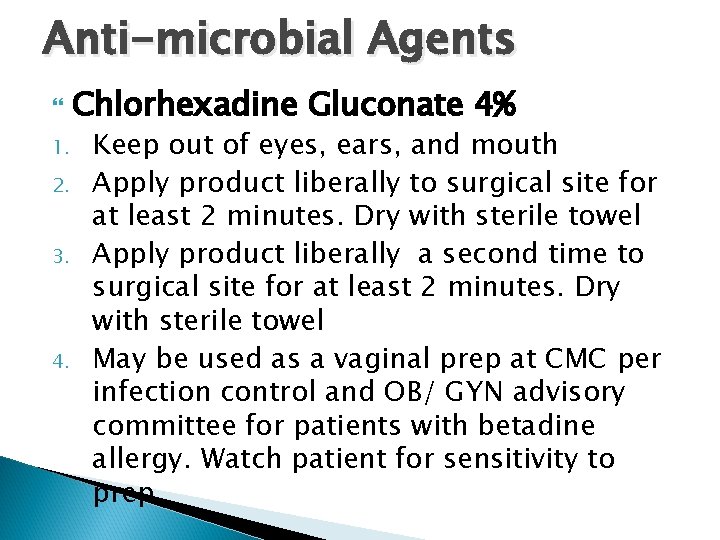
Anti-microbial Agents 1. 2. 3. 4. Chlorhexadine Gluconate 4% Keep out of eyes, ears, and mouth Apply product liberally to surgical site for at least 2 minutes. Dry with sterile towel Apply product liberally a second time to surgical site for at least 2 minutes. Dry with sterile towel May be used as a vaginal prep at CMC per infection control and OB/ GYN advisory committee for patients with betadine allergy. Watch patient for sensitivity to prep.
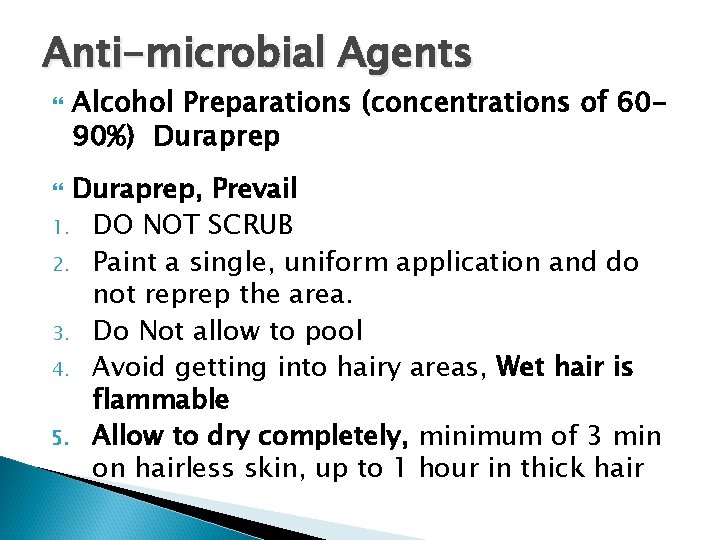
Anti-microbial Agents Alcohol Preparations (concentrations of 6090%) Duraprep, Prevail 1. DO NOT SCRUB 2. Paint a single, uniform application and do not reprep the area. 3. Do Not allow to pool 4. Avoid getting into hairy areas, Wet hair is flammable 5. Allow to dry completely, minimum of 3 min on hairless skin, up to 1 hour in thick hair
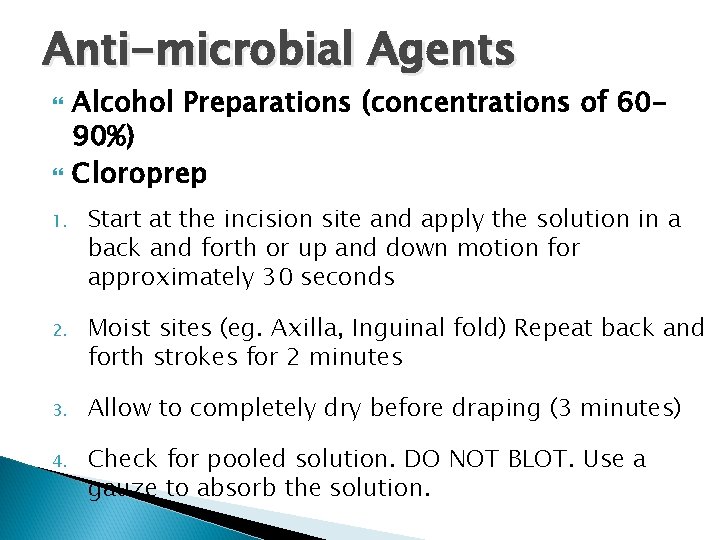
Anti-microbial Agents Alcohol Preparations (concentrations of 6090%) Cloroprep 1. Start at the incision site and apply the solution in a back and forth or up and down motion for approximately 30 seconds 2. Moist sites (eg. Axilla, Inguinal fold) Repeat back and forth strokes for 2 minutes 3. Allow to completely dry before draping (3 minutes) 4. Check for pooled solution. DO NOT BLOT. Use a gauze to absorb the solution.
Guidelines to Follow When Prepping Patient should be assessed for known allergies and sensitivities to prep solutions (alternate solution may be chosen, if allergic). If patient is awake, give explanation. Avoid unnecessary exposure. Prep should be performed using mechanical friction.
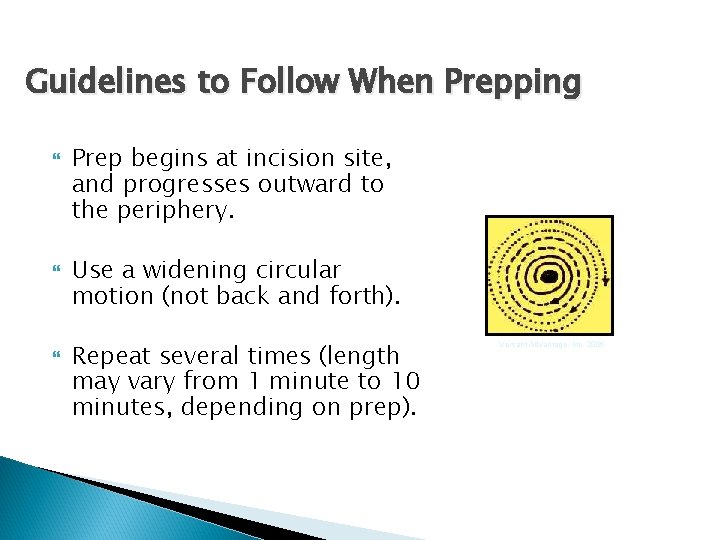
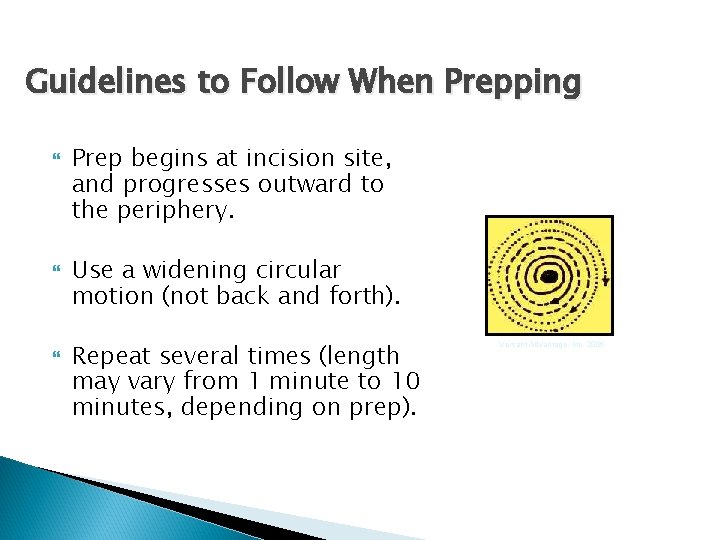
Guidelines to Follow When Prepping Prep begins at incision site, and progresses outward to the periphery. Use a widening circular motion (not back and forth). Repeat several times (length may vary from 1 minute to 10 minutes, depending on prep). Versant Advantage, Inc, 2006
Guidelines to Follow When Prepping If a scrub is used, the area is blotted with a sterile towel. The towel is pulled out and away from the prepped area. Do Not let the contaminated outer edges of the towel touch the prepped area. Apply antiseptic paint (betadine solution) over the prepped area. . Sterile gloves and prep kit should be used. Versant Advantage, Inc, 2006 Sponges or applicators used to prep an area are NEVER reapplied to area previously prepped.
Guidelines to Follow When Prepping Sponges or applicators should be discarded once the periphery of the prep area is reached. DO NOT allow prep solutions to pool under the patient, tourniquet cuff or ESU (electrocautery/ bovie grounding pad). Folded or disposable towels shall be placed at the periphery area of the prep to absorb the excess prep fluid, prevent pooling and saturation of drapes.
Guidelines to Follow When Prepping Dirtiest areas are always prepped LAST. ALWAYS move from CLEAN to DIRTY. Clean umbilicus separately with cotton-tip applicators. If an open wound or body orifice is not part of the area to be prepped, then begin at INCISION site. If contaminated areas are included in prep, begin at surrounding skin area.
Guidelines to Follow When Prepping If a colostomy is present, cover with gauze/sponge until surrounding area is prepped; prep LAST. Perineal area is prepped first with a separate prep kit so solution from a dirty area doesn’t splash onto the clean prep. Abdominal and perineal preps are to be done sequentially, not consecutively. Shoulder Prep—prep axilla last. Unusual Wounds/Incision Sites—use nursing judgment to decide process that results in least amount of microorganisms at the incision site.
Guidelines to Follow When Prepping If Betadine Gel is used—“paint” on, from cleanest to least clean, and let “dry” as much as possible. You only need a thin layer. Duraprep—“paint” on, from cleanest to least clean, and let “dry”; do not let pool; contains alcohol (several sponges are not provided in this type of prep; apply once, never going back to same area twice). Use a second applicator if you need to go back for a missed area. ©
Face/ Eye Preps Always prep both sides of the face for symmetry when doing the procedure Use cotton balls with a non-irritating solution. Begin at nose, continuing toward cheeks. images. MD, 2006 Use warm sterile water to rinse off solution. DO NOT allow solution to pool under patient’s eye.
Abdominal Prep Apply sterile gloves. Apply towels on periphery to prevent pooling. Use cotton tip applicators to clean umbilicus (dip in scrub solution prior to utilizing). Start at incision site with first sponge. Proceed to periphery. Repeat, if using a “scrub” solution (e. g. , Betadine Scrub). Blot with sterile towel, if using a paint after “scrub” (never reach over area); apply towel and remove toward you, blotting with gloved hand, using aseptic technique.
Abdominal Prep If applying a paint solution (e. g. , Betadine Solution), start at incision site and proceed to periphery. Remove sterile towels at periphery, being careful not to contaminate prepped site. Patient is now ready to be draped for procedure.
Extremity Prep An additional person or “apparatus” may be needed to hold the limb securely, so the entire limb can be prepped circumferentially (have person holding limb don sterile gloves). A scrub brush may be utilized for hands and feet (avoid irritating tender skin or scratching—portal of entry for bacteria). images. MD, 2006
Extremity Prep Scrub/ paint Don sterile gloves Start at incision line and prep circumferentially. Blot if a scrub is used. Paint with “solution” (usually betadine) starting at the incision line. Prep feet or hands last (if not site of incision) Do not get prep solution under the tourniquet Alcohol prep Don sterile gloves Start at incision line and prep circumferentially.
Documentation of Skin Prep Assessment of skin at operative site. Hair removal (if performed)—site, method, time and person performed. Patient allergies (if any). Site of prep. Prep agents utilized. Name of person performing prep. Allergic response (if any).
Implementation Issues Three “big” issues: ◦ Patient Preop preparation by the patient helps to reduce the risk of subsequent contamination of the surgical wound. ◦ Surgeon The surgeon needs to order the correct prep agent for a specific procedure. ◦ Staff Need to assess the patient and provide the best skin preparation to minimize contamination, prevent infection, keep the patient safe and free from injury. Microsoft clip art
Implementation Issues Patient Preop instructions for the day before surgery: ◦ Shower the night before with chlorhexadine gluconate (CHG) to reduce the number of microorganisms on the skin ◦ 4% CHG is more effective than Povidone iodine or soap ◦ No hair spray or alcohol based hair products should be used for head and neck procedures ◦ Instruct the patient not to shave or use a depilatory on the surgical site before surgery Mi
Inplementation Issues Staff: AORN (Association of peri. Operative Registered Nurses) suggests: Follow AORN recommended practices for skin preparation. Skin preparation is a core competency in orientation and ongoing education.
AORN Recommended Practices for Skin Preparation of Patients Recommended Practice I: Patients undergoing open Class I surgical procedures below the chin should have 2 preop showers with CHG before surgery. Recommended Practice II: Preoperative skin agents that have been FDA approved or cleared and approved by the health care organization’s infection control personnel should be used for all preop skin preparations. Recommended Practice III: The antiseptic agent used should be selected based on the patient assessment. The patient should be assessed for allergies.
AORN Recommended Practices for Skin Preparation of Patients Recommended Practice IV: Hair at the surgical site should be left in place whenever possible. Hair at the surgical site should not be removed with a razor Recommended Practice V: “The skin around the surgical site should be free of soil, debris, exudates, and transient microorganisms to minimize contamination of the surgical site before application of the skin prep.
AORN Recommended Practices for Skin Preparation of Patients 1. 2. 3. Recommended Practice VI: Protective measures should be implemented to prevent skin and tissue injury due to prolonged contact with skin prep agents. Sheets, padding, positioning equipment, and adhesive tape should be protected from dripping or pooling of prep agents beneath and around the patient. Electrodes and ESU pads should be protected from dripping or pooling of antiseptic agents. Skin and padding under the tourniquet cuff should be protected from contact with prep solutions.
AORN Recommended Practices for Skin Preparation of Patients 1. 2. 3. 4. Recommended Practice VII: The antiseptic agent should be applied to the skin over the surgical site and surrounding area in a manner to minimize the contamination, preserve the skin integrity, and prevent tissue damage. The prep should progress from the incision site to the periphery. If a dirty area is part of the prep, prep the cleanest area first instead of the incision site. When prepping the anus, sinus, ulcer, or open wound, the sponge should be applied once to that area and then discarded. Vaginal preps for procedures that include the abdomen should be performed in a manner to prevent splashing of prep agent expelled from the vagina onto the prepped abdomen.
AORN Recommended Practices for Skin Preparation of Patients Recommended Practice VII: 5. The prepared area of skin should extend to an area large enough to accommodate potential shifting of the drape fenestration, extension of the incision, the potential for additional incisions, and all potential drain sites. 6. The prep agent should remain in place for the full time suggested by the manufacturer’s written recommendations. (For example, Povidone iodine reaches maximum effectiveness only after it dries. )
AORN Recommended Practices for Skin Preparation of Patients Recommended Practice VIII: If a flammable prep agent is used, additional precautions should be taken to minimize the risk of a surgical fire and patient burn injury. 1. If pooling occurs, the excess solution should be wicked away. 2. The prep agent should be allowed to dry and vapors to dissipate before application of a drape or use of ESU or laser. 3. The use of flammable prep agent is to be discussed during the time out.
Recommended Practice VIII: Recommended Practice IX: Manufacturer’s written recommendations and MSDSs for handling, storing, and heating of all skin preparation agents should be readily available. 1. Heating of nonflammable skin preparation solutions should only be done in accordance with the manufacturer’s written instructions. 2. Skin prep should never be warmed in a microwave oven or autoclave.
AORN Recommended Practices for Skin Preparation of Patients Recommended Practice X: At the en of the surgical procedure, the skin prep agent should be thoroughly, removed from the skin unless otherwise indicated by the manufacturer’s written instructions. 1. Residual antiseptic prep agent should be removed before application of an occlusive dressing or tape. 2. Some manufacturers recommend that specific prep agents be left on the skin and allowed to wear off naturally.