Surgical Shunts Causing Circular Shunt An Approach to


- Slides: 11
Surgical Shunts Causing Circular Shunt: An Approach to Management Manu Varma, DO Pediatric Cardiology Fellow University of Texas Health Science Center at Houston; Houston, TX

Disclosures None
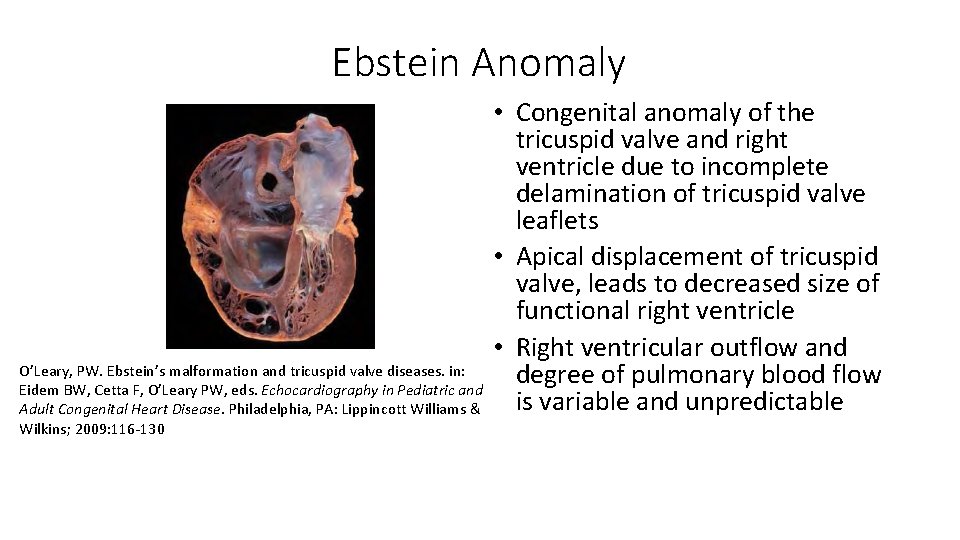
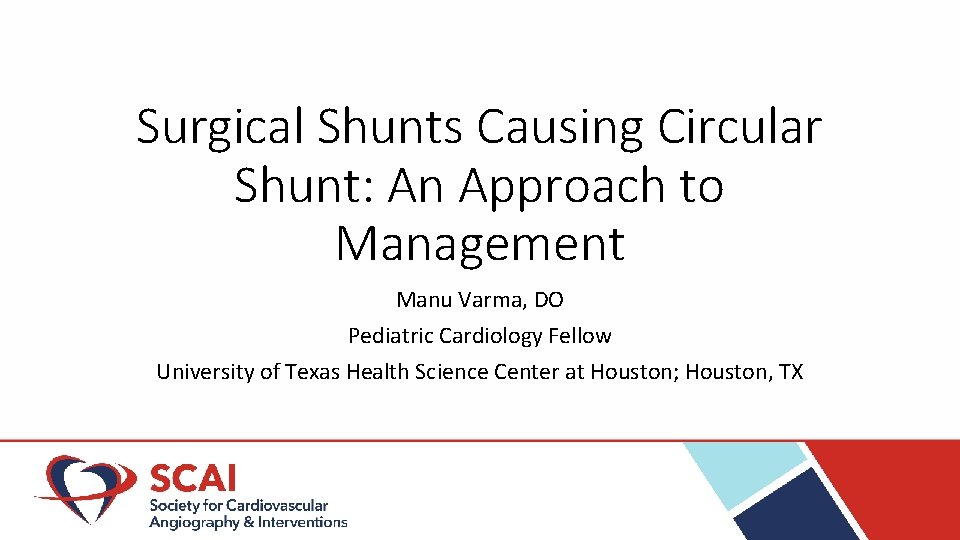
Ebstein Anomaly O’Leary, PW. Ebstein’s malformation and tricuspid valve diseases. in: Eidem BW, Cetta F, O’Leary PW, eds. Echocardiography in Pediatric and Adult Congenital Heart Disease. Philadelphia, PA: Lippincott Williams & Wilkins; 2009: 116 -130 • Congenital anomaly of the tricuspid valve and right ventricle due to incomplete delamination of tricuspid valve leaflets • Apical displacement of tricuspid valve, leads to decreased size of functional right ventricle • Right ventricular outflow and degree of pulmonary blood flow is variable and unpredictable
Patient History • Infant with Ebstein anomaly and pulmonary atresia • Initial surgical palliation with 8 mm valved femoral vein RV-PA conduit and 3 mm central shunt (added due to hypoxia coming off bypass) • Admitted at 3 months of age with increased work of breathing and cyanosis. Central shunt upsized to 3. 5 mm • Condition worsened postoperatively with hypoxia and increasing inotrope requirements • Echocardiogram showed free pulmonary insufficiency through conduit and tricuspid regurgitation
Initial Hemodynamics • Obtained on 100% Fi. O 2 and i. NO 20 ppm due to instability • Venous saturations: LINNV 12. 5%, SVC 15%, IVC 38% • Arterial saturations: LV 67%, a. AO 63%, d. AO 75. 2% • PVR 6. 05 WU/m 2 with m. PAP 23 mm. Hg
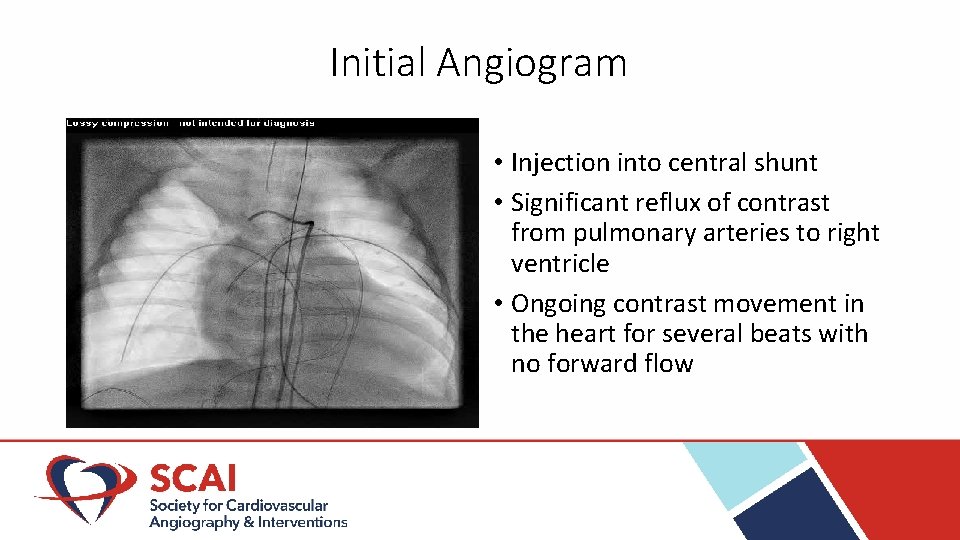
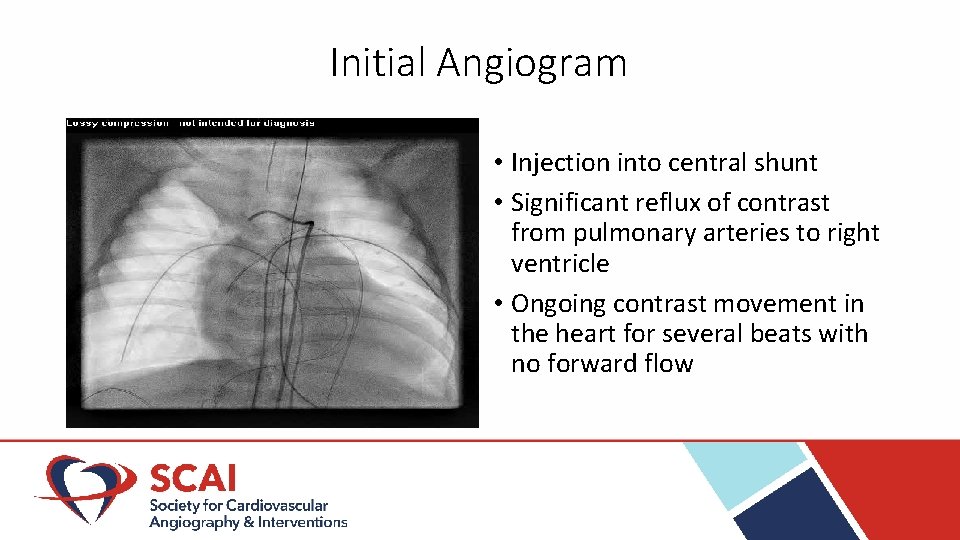
Initial Angiogram • Injection into central shunt • Significant reflux of contrast from pulmonary arteries to right ventricle • Ongoing contrast movement in the heart for several beats with no forward flow
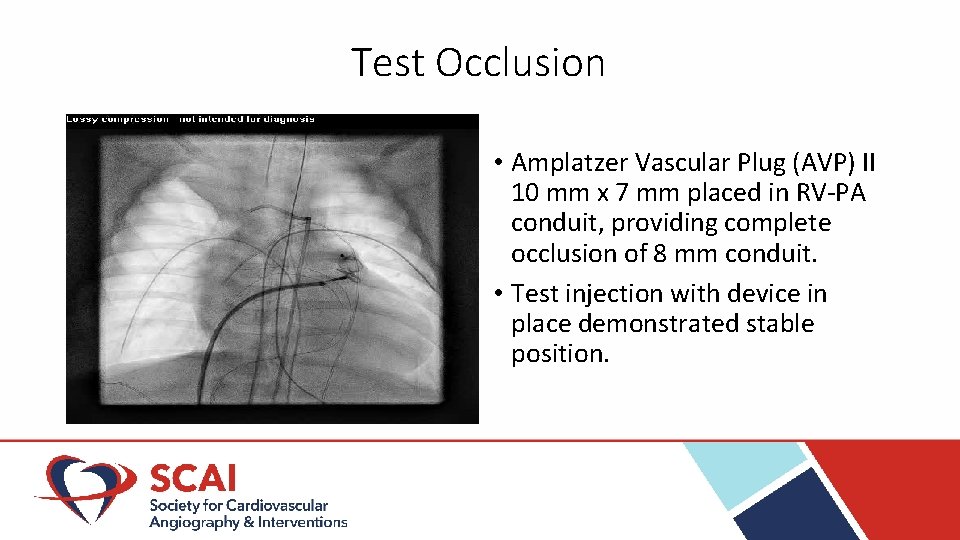
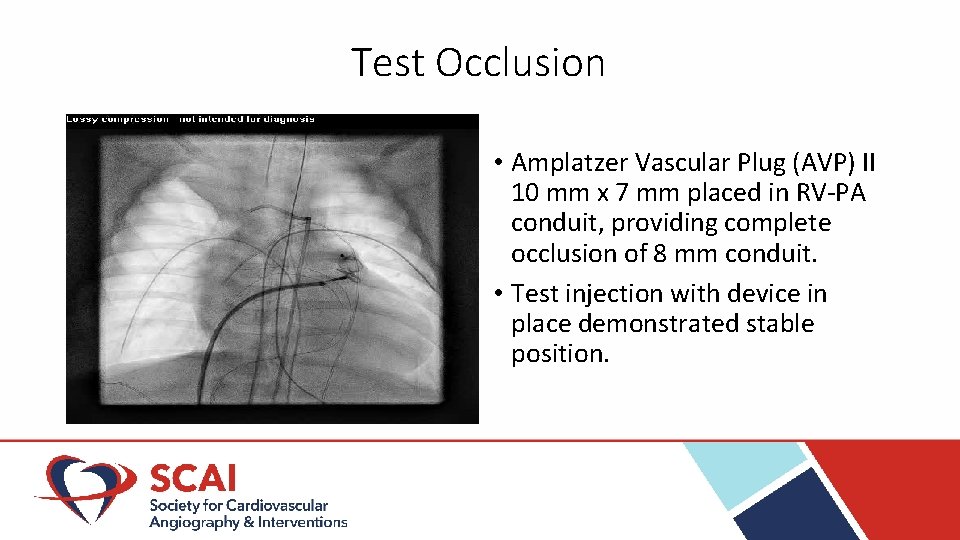
Test Occlusion • Amplatzer Vascular Plug (AVP) II 10 mm x 7 mm placed in RV-PA conduit, providing complete occlusion of 8 mm conduit. • Test injection with device in place demonstrated stable position.
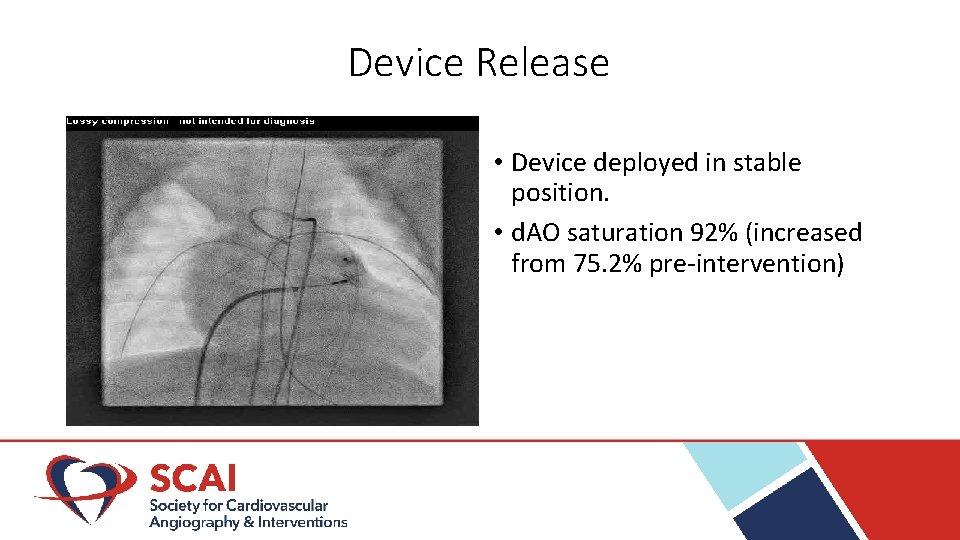
Device Release • Device deployed in stable position. • d. AO saturation 92% (increased from 75. 2% pre-intervention)
Patient Outcome • Patient’s condition improved in ICU with inotropes stopped and supplemental oxygen weaned. • Post-cath day 11: Repeat catheterization for pre-Glenn assessment showed PVR 0. 62 WU/m 2 with m. PAP 13 mm. Hg on room air. • Post-cath day 13: Bidirectional Glenn with RV-PA conduit replacement, central shunt takedown, and tricuspid valve replacement.
Discussion and Lessons • Pulmonary blood flow in Ebstein’s anomaly is unpredictable, both before and after surgical palliation • “Circular shunt” physiology can be a cause of hypoxia as a late complication after multiple surgical shunts are placed • Device occlusion of RV-PA conduit allowed resolution of critical illness from circular shunt and stabilization for surgical repair

Contact Information Manu. R. Varma@uth. tmc. edu