Surgical Nutrition TPN Enteral Feeds Jason D Sciarretta

- Slides: 31
Surgical Nutrition: TPN & Enteral Feeds Jason D. Sciarretta, M. D. Surgical Critical Care 2/2/11
History n Hippocrates: – “A slender and restricted diet is always dangerous in chronic and in acute diseases” n Cuthbertson 1976: – Extreme catabolism and negative nitrogen balance n Kinney 1980: – Catabolic response: lose 20% nl body wt. (3 wks) – Rapid wasting of large wt bearing muscle grps n Mc. Whirter & Pennington 1994: – 40% of pts are malnurished on admission

33
Nutritional Support Service n Optimal Organization: – Physician, Nurse, Pharmacist, Nutritionist, Respiratory therapist. n Recognize states n Ultimate mass risk of malnutrition & deficiency goal: minimize loss of lean body
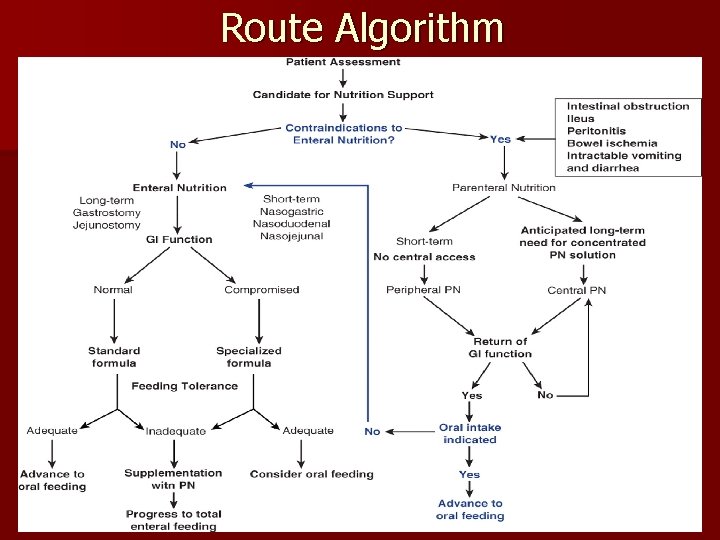
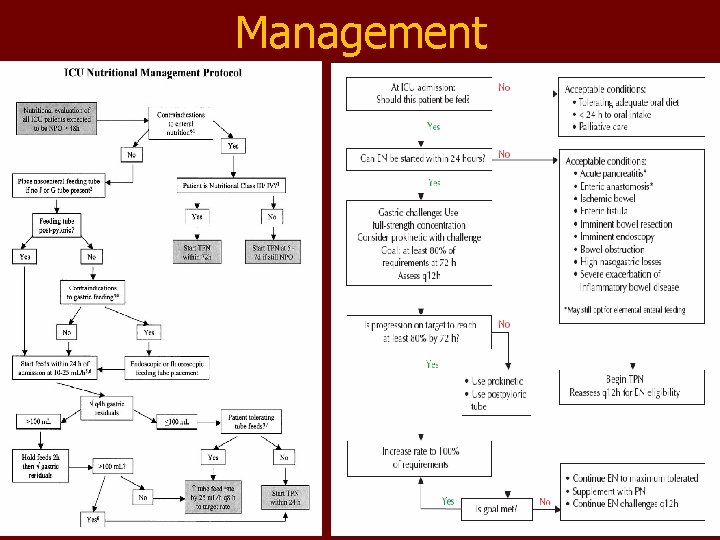
Route Algorithm
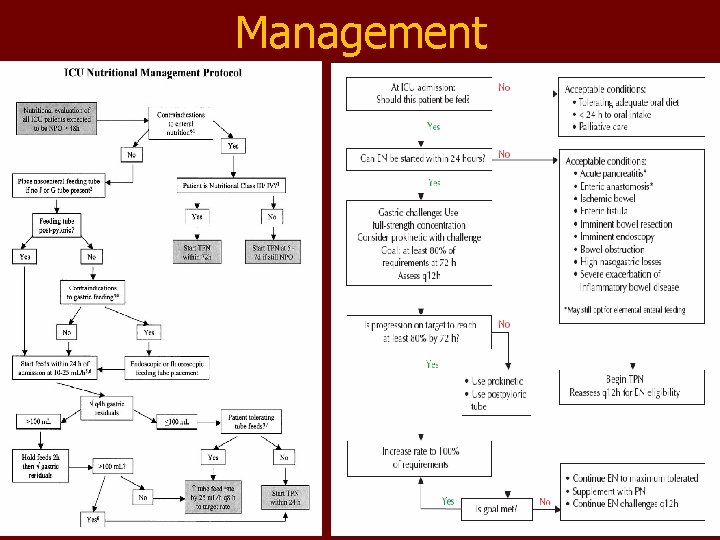
Management 12
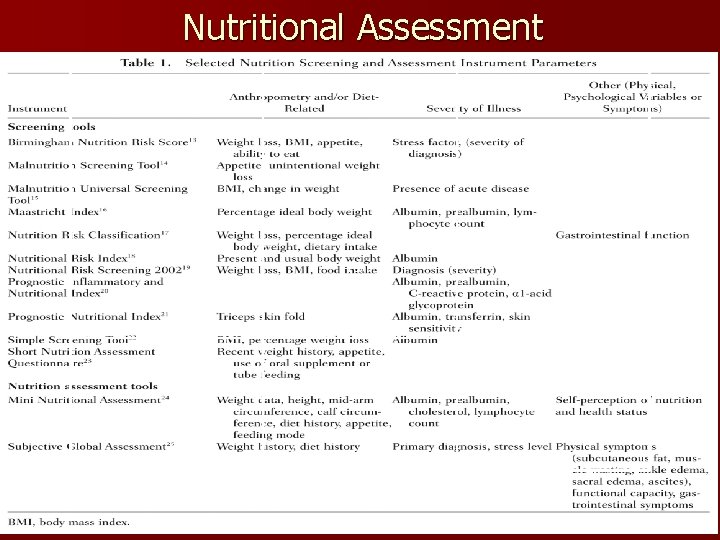
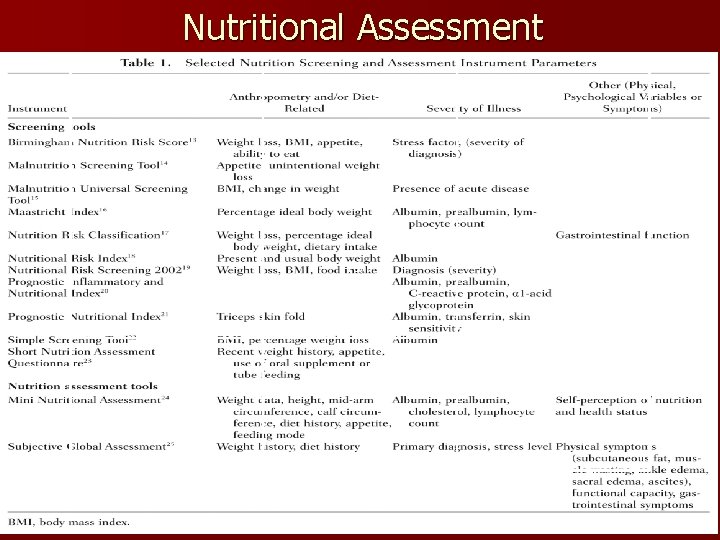
Nutritional Assessment Text
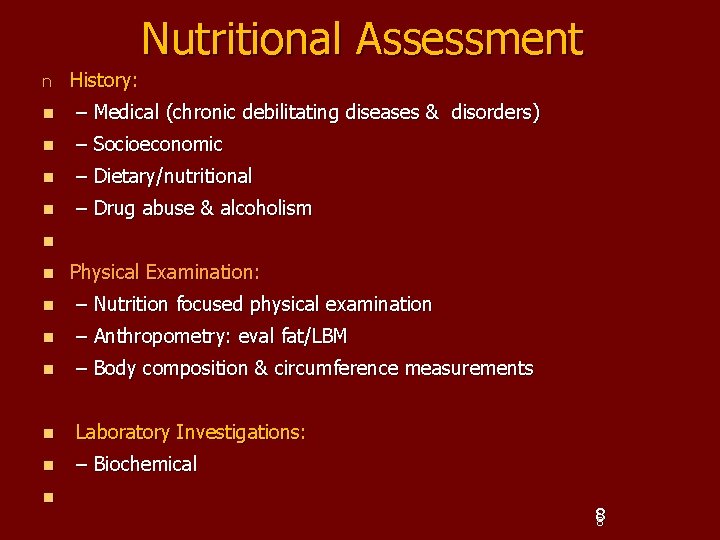
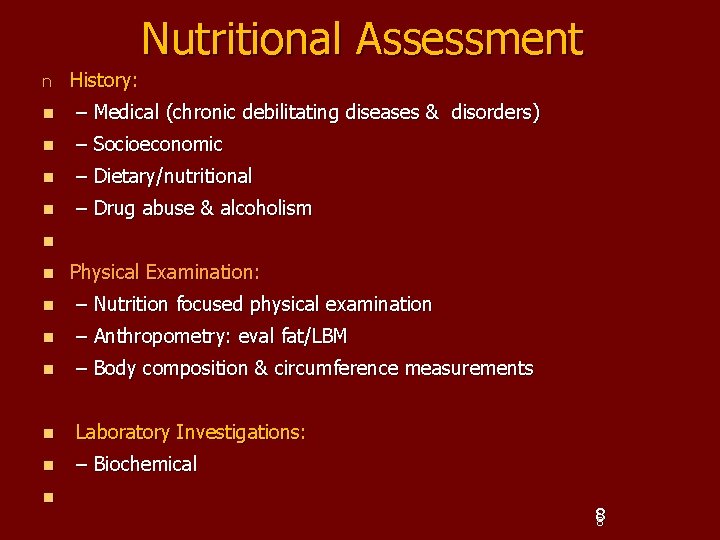
Nutritional Assessment n History: n – Medical (chronic debilitating diseases & disorders) n – Socioeconomic n – Dietary/nutritional n – Drug abuse & alcoholism n n Physical Examination: n – Nutrition focused physical examination n – Anthropometry: eval fat/LBM n – Body composition & circumference measurements n Laboratory Investigations: n – Biochemical n 88
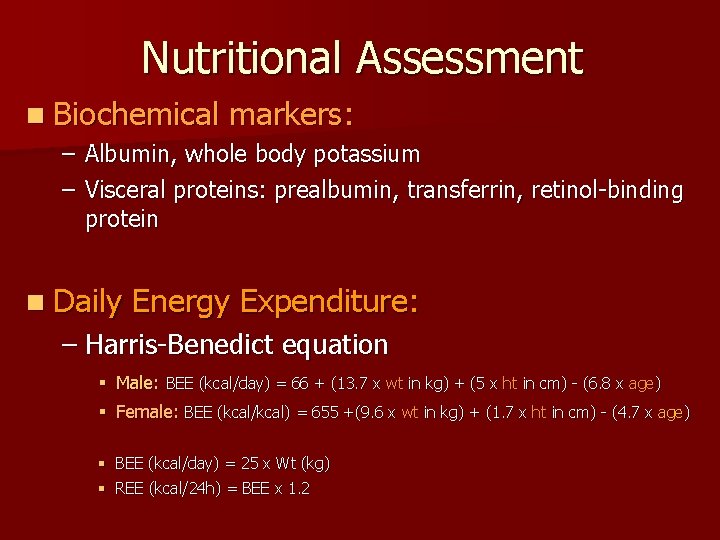
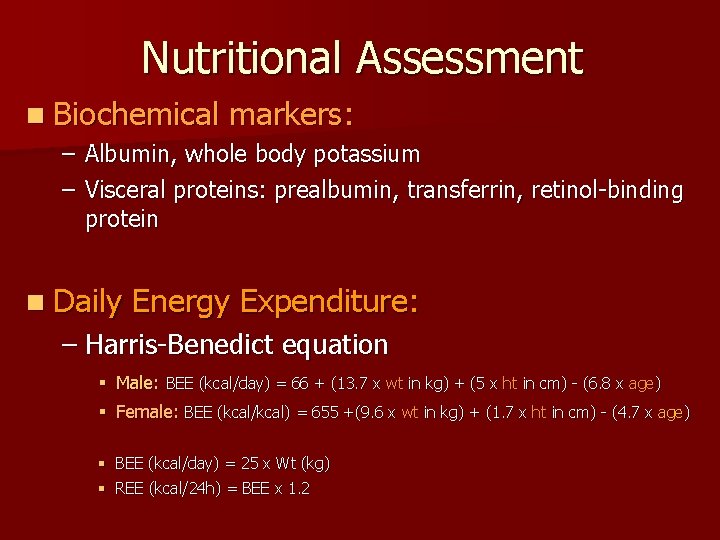
Nutritional Assessment n Biochemical markers: – Albumin, whole body potassium – Visceral proteins: prealbumin, transferrin, retinol-binding protein n Daily Energy Expenditure: – Harris-Benedict equation § Male: BEE (kcal/day) = 66 + (13. 7 x wt in kg) + (5 x ht in cm) - (6. 8 x age) § Female: BEE (kcal/kcal) = 655 +(9. 6 x wt in kg) + (1. 7 x ht in cm) - (4. 7 x age) § BEE (kcal/day) = 25 x Wt (kg) § REE (kcal/24 h) = BEE x 1. 2
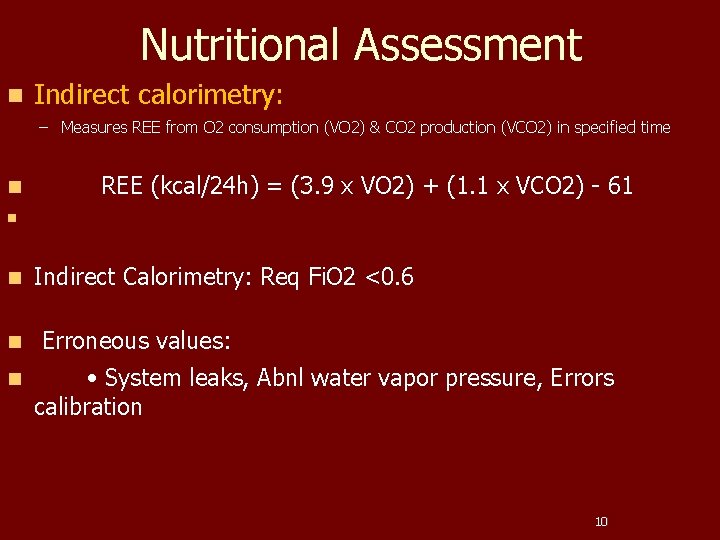
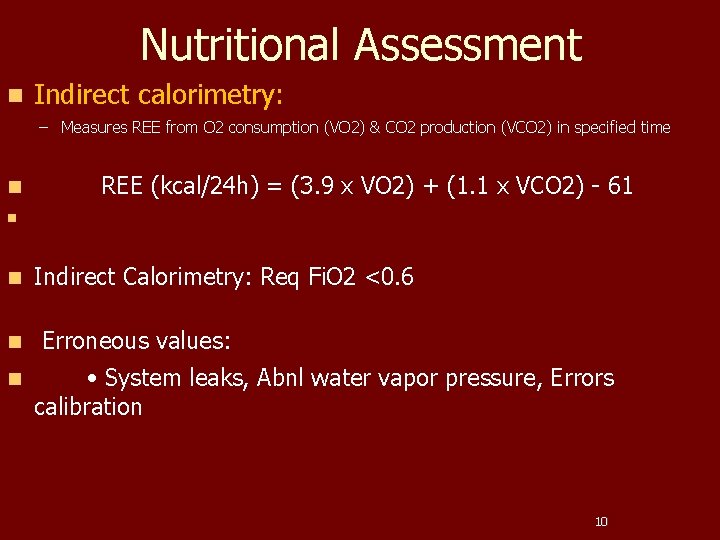
Nutritional Assessment n Indirect calorimetry: – Measures REE from O 2 consumption (VO 2) & CO 2 production (VCO 2) in specified time n REE (kcal/24 h) = (3. 9 x VO 2) + (1. 1 x VCO 2) - 61 n n Indirect Calorimetry: Req Fi. O 2 <0. 6 Erroneous values: • System leaks, Abnl water vapor pressure, Errors calibration 10
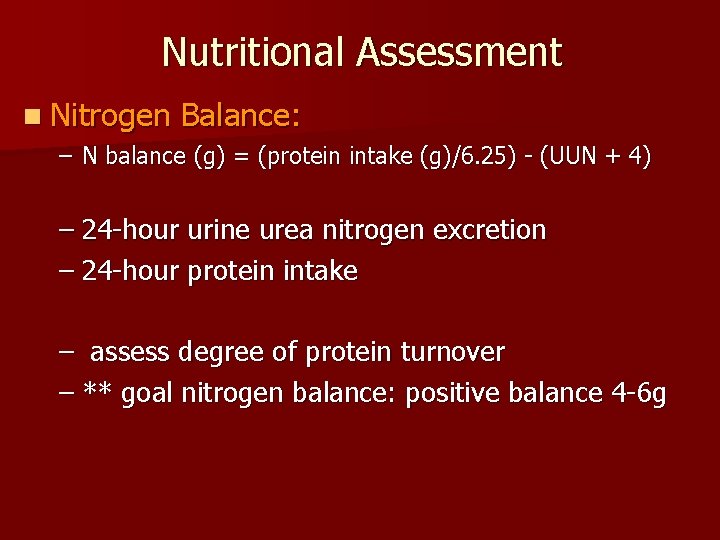
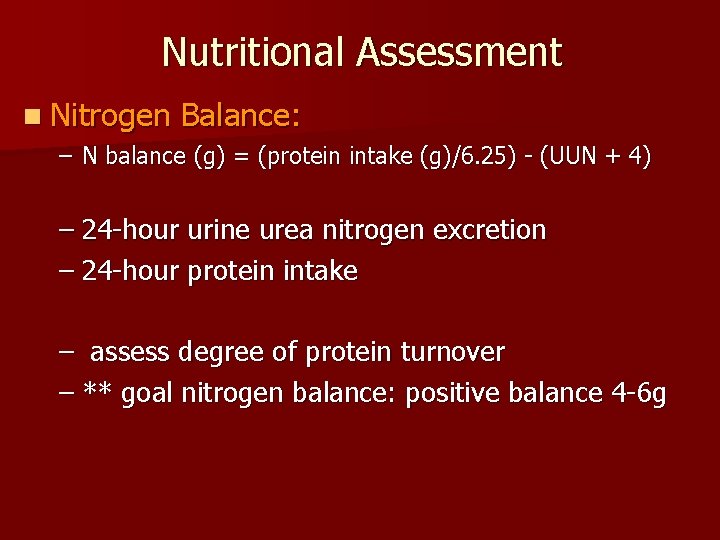
Nutritional Assessment n Nitrogen Balance: – N balance (g) = (protein intake (g)/6. 25) - (UUN + 4) – 24 -hour urine urea nitrogen excretion – 24 -hour protein intake – assess degree of protein turnover – ** goal nitrogen balance: positive balance 4 -6 g
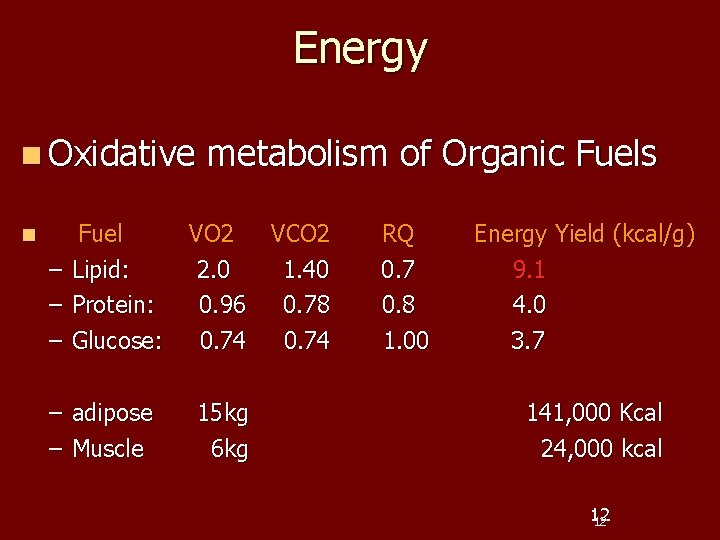
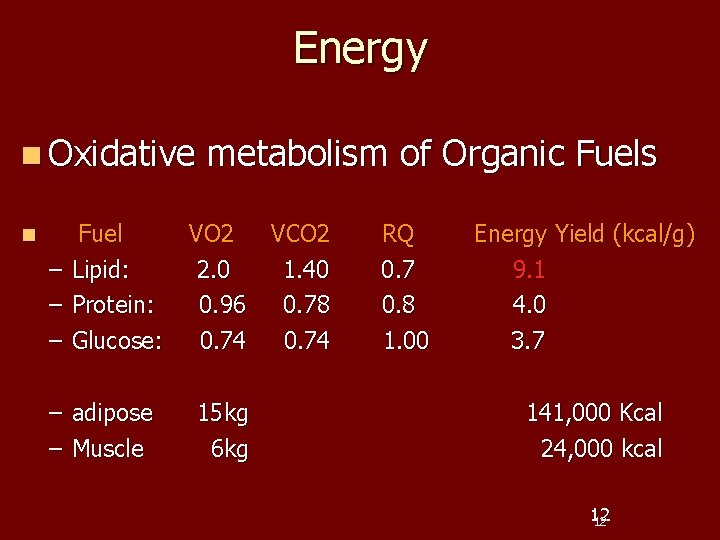
Energy n Oxidative n Fuel – Lipid: – Protein: – Glucose: – adipose – Muscle metabolism of Organic Fuels VO 2 VCO 2 2. 0 1. 40 0. 96 0. 78 0. 74 15 kg 6 kg RQ 0. 7 0. 8 1. 00 Energy Yield (kcal/g) 9. 1 4. 0 3. 7 141, 000 Kcal 24, 000 kcal 12 12
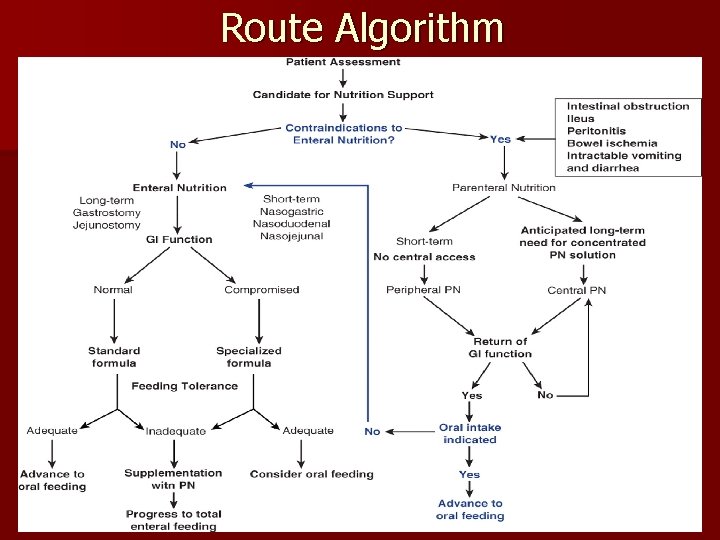
Nutrition n Routes of Nutrition: – Enteral – Parenteral: Central or Peripheral n Advantages & Disadvantage
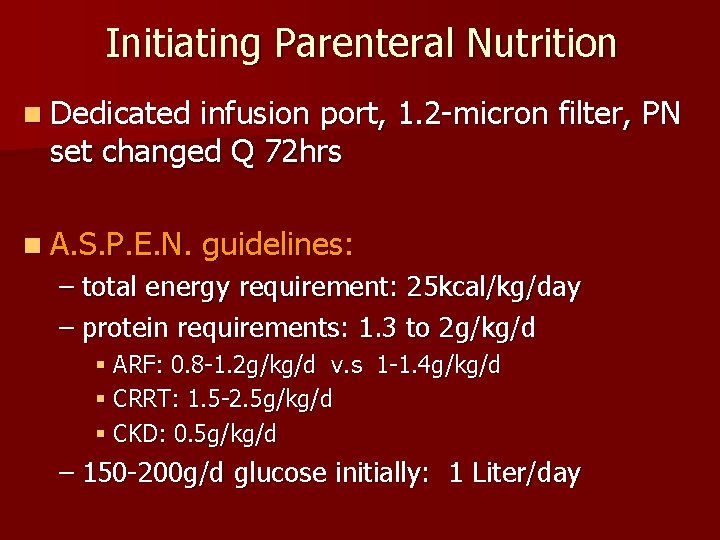
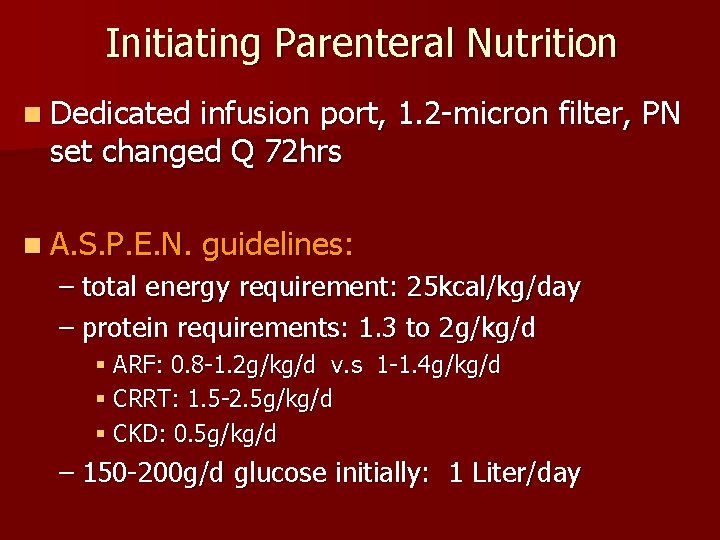
Initiating Parenteral Nutrition n Dedicated infusion port, 1. 2 -micron filter, PN set changed Q 72 hrs n A. S. P. E. N. guidelines: – total energy requirement: 25 kcal/kg/day – protein requirements: 1. 3 to 2 g/kg/d § ARF: 0. 8 -1. 2 g/kg/d v. s 1 -1. 4 g/kg/d § CRRT: 1. 5 -2. 5 g/kg/d § CKD: 0. 5 g/kg/d – 150 -200 g/d glucose initially: 1 Liter/day
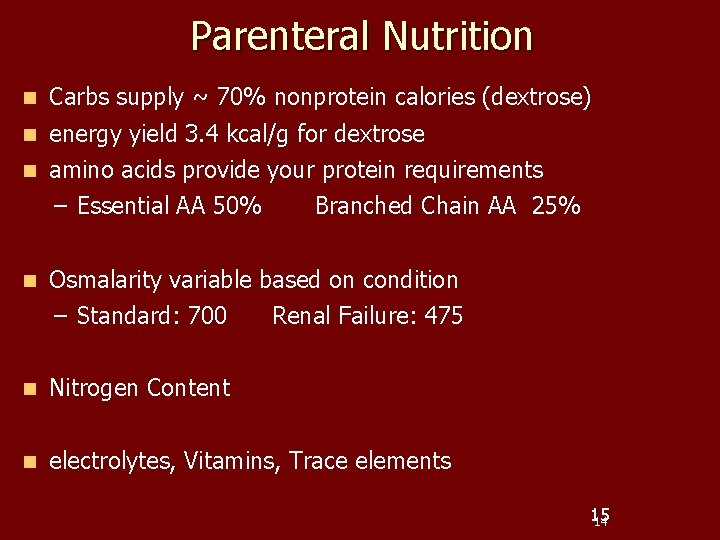
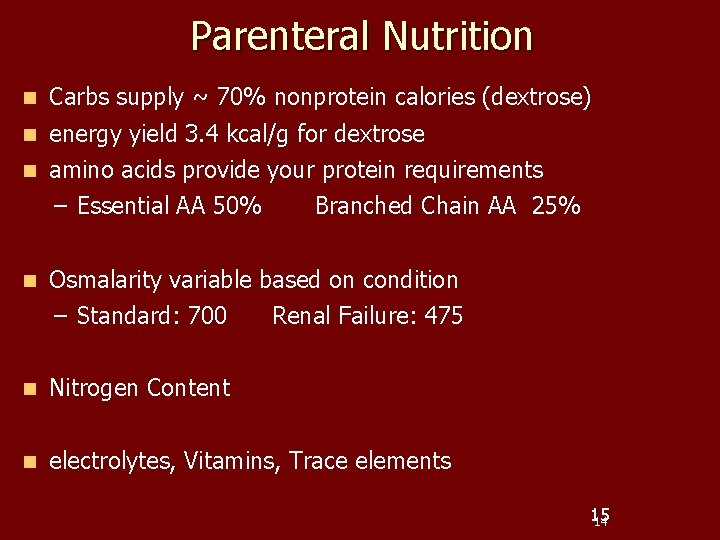
Parenteral Nutrition n Carbs supply ~ 70% nonprotein calories (dextrose) n energy yield 3. 4 kcal/g for dextrose n amino acids provide your protein requirements – Essential AA 50% Branched Chain AA 25% n Osmalarity variable based on condition – Standard: 700 Renal Failure: 475 n Nitrogen Content n electrolytes, Vitamins, Trace elements 15 14
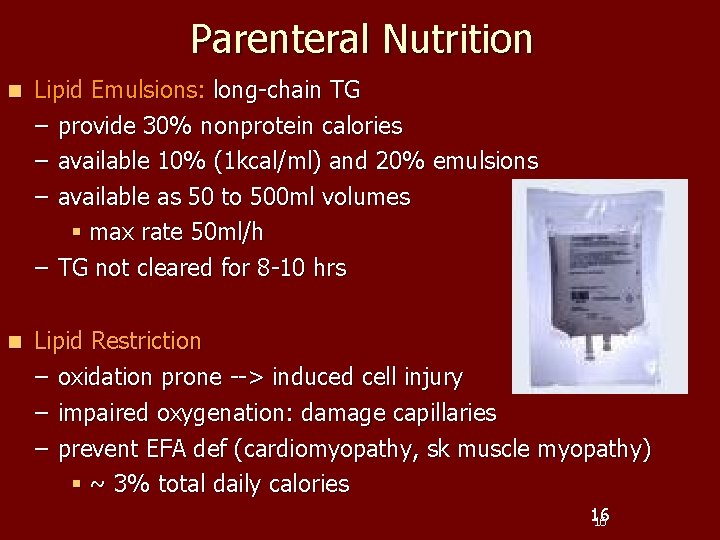
Parenteral Nutrition n Lipid Emulsions: long-chain TG – provide 30% nonprotein calories – available 10% (1 kcal/ml) and 20% emulsions – available as 50 to 500 ml volumes § max rate 50 ml/h – TG not cleared for 8 -10 hrs n Lipid Restriction – oxidation prone --> induced cell injury – impaired oxygenation: damage capillaries – prevent EFA def (cardiomyopathy, sk muscle myopathy) § ~ 3% total daily calories 16 16
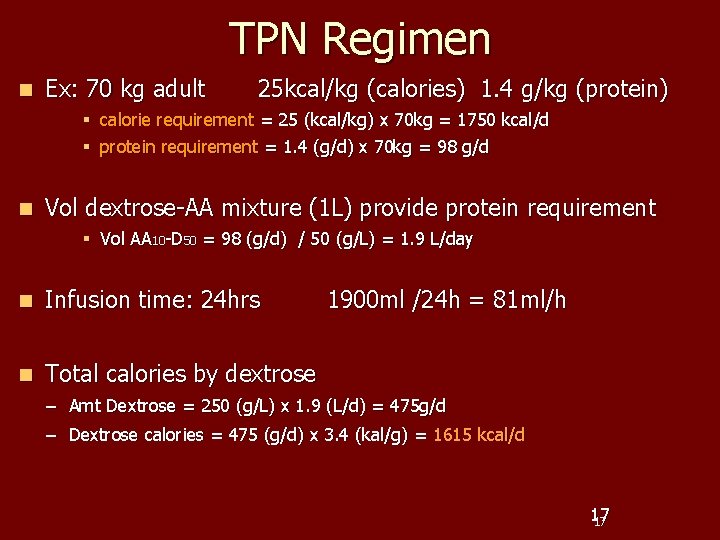
TPN Regimen n Ex: 70 kg adult 25 kcal/kg (calories) 1. 4 g/kg (protein) § calorie requirement = 25 (kcal/kg) x 70 kg = 1750 kcal/d § protein requirement = 1. 4 (g/d) x 70 kg = 98 g/d n Vol dextrose-AA mixture (1 L) provide protein requirement § Vol AA 10 -D 50 = 98 (g/d) / 50 (g/L) = 1. 9 L/day n Infusion time: 24 hrs n Total calories by dextrose 1900 ml /24 h = 81 ml/h – Amt Dextrose = 250 (g/L) x 1. 9 (L/d) = 475 g/d – Dextrose calories = 475 (g/d) x 3. 4 (kal/g) = 1615 kcal/d 17 17
Cyclic Parenteral Nutrition n Satiety center constantly stimulated – 25% of caloric needs n Advantages: – More mobility during day – Improved appetite – Less deterioration of liver function
Enteral Feeding n “Pharmacotherapy” – – for the gut Maintains gut integrity, improves mesenteric blood flow release endogenous agents n Early Feeding: with in 48 hrs § 20% decrease in ICU mortality § 25% decrease in hospital mortality n What formula to choose?
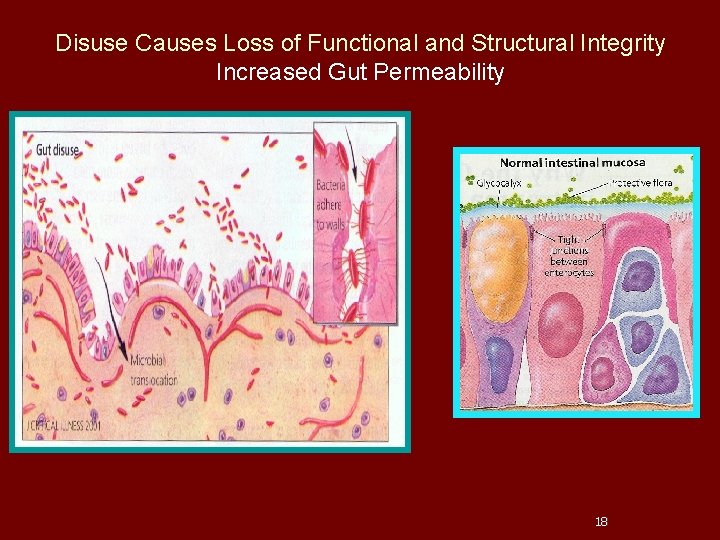
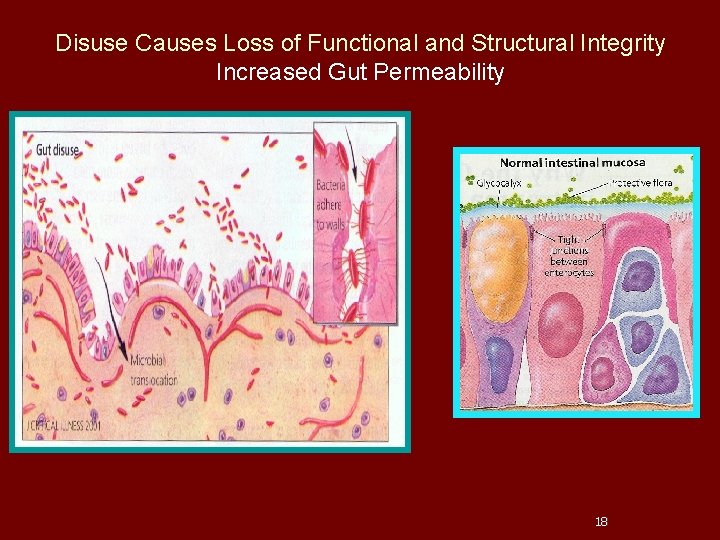
Disuse Causes Loss of Functional and Structural Integrity Increased Gut Permeability 18
n Enteral Orders Formula: – Monomeric v. s. polymeric § Most TF semi synthetic polymeric § Variable Caloric density § Amt of protein, fiber, Carb to Fat ratio n Polymeric: – Cost effective – digestive capability – high caloric density n Monomeric: – Malabsorption: short gut
Formula Selection n Suitability – – – evaluated based on: functional status of GI tract Macronutient ratios Digestion and absorption capabilities specific metabolic needs physical characteristics of formula cost effectiveness 22
Enteral Orders n Progression of Regimen: – 10 -20 ml/h and 10 -20 ml every 6 -8 h n Residuals: < 200 ml NG vs 100 ml gastrostomy n Transitions: bolus feeding regimens – More physiologic, sensations of hunger & satiety – 60% consumption n “closed systems”:
“Designer” Enteral Feeding n Specialized formulas with modified proteins specific patients stressed states n Formulas: – – Hepatic, Renal, Pulmonary, Metabolic stress, Glycemic (Nutri. Hep, Nepro, Pulmo. Car, Perative, Glucenra etc. )
“Hidden Kcals” n Inadvertent hypercaloric feeding: – Increase CO 2, hyperglycemia, hepatomegaly n Pay attention to medications – Dextrose in CRRT: daily caloric contribution § ~ 43 -45% absorbed across hemofilter § 123 -2, 388 kcal (dextrose concentration) – - Propofol: 10% intralipid § 1. 1 kcal/m. L Ex: 554 kcal/day
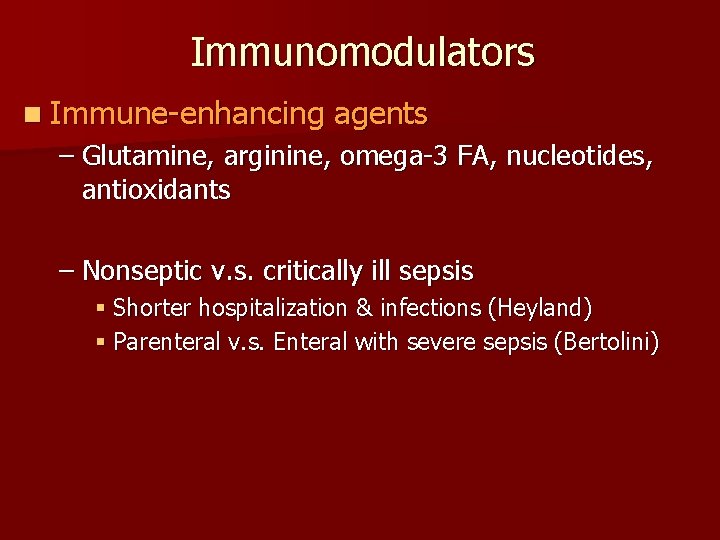
Immunomodulators n Immune-enhancing agents – Glutamine, arginine, omega-3 FA, nucleotides, antioxidants – Nonseptic v. s. critically ill sepsis § Shorter hospitalization & infections (Heyland) § Parenteral v. s. Enteral with severe sepsis (Bertolini)
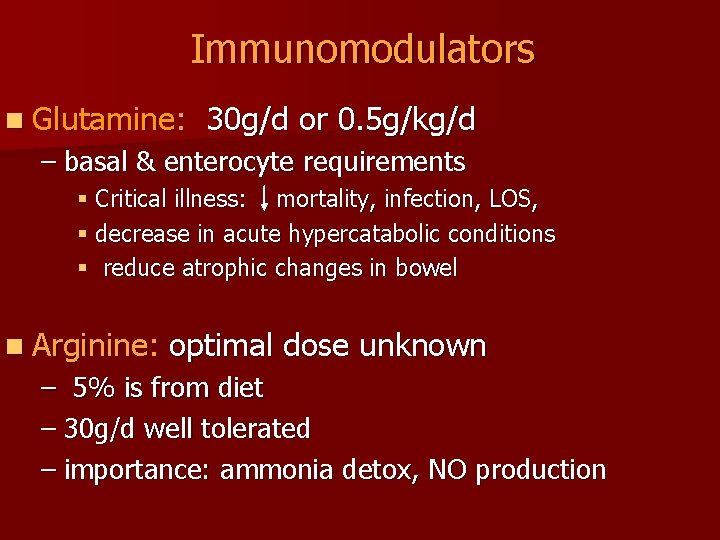
Immunomodulators n Glutamine: 30 g/d or 0. 5 g/kg/d – basal & enterocyte requirements § Critical illness: mortality, infection, LOS, § decrease in acute hypercatabolic conditions § reduce atrophic changes in bowel n Arginine: optimal dose unknown – 5% is from diet – 30 g/d well tolerated – importance: ammonia detox, NO production
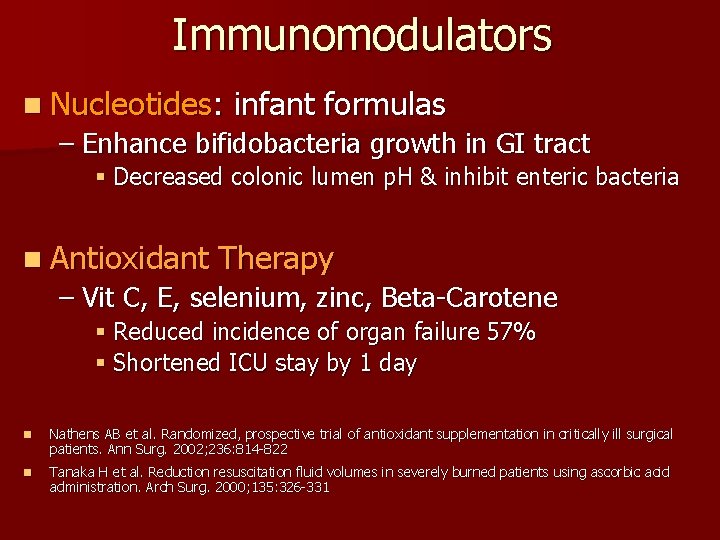
Immunomodulators n Nucleotides: infant formulas – Enhance bifidobacteria growth in GI tract § Decreased colonic lumen p. H & inhibit enteric bacteria n Antioxidant Therapy – Vit C, E, selenium, zinc, Beta-Carotene § Reduced incidence of organ failure 57% § Shortened ICU stay by 1 day n Nathens AB et al. Randomized, prospective trial of antioxidant supplementation in critically ill surgical patients. Ann Surg. 2002; 236: 814 -822 n Tanaka H et al. Reduction resuscitation fluid volumes in severely burned patients using ascorbic acid administration. Arch Surg. 2000; 135: 326 -331
29
Managing refeeding problems n n n n provide Thiamine/MVI/trace elements start nutrition support at 5 -10 kcal/kg/day increase levels slowly restore circulatory volume monitor fluid balance and clinical status replace PO 42 -, K+ and Mg 2+ Reduce feeding rate if problems arise 30
References n Marino P. The ICU book: 2 nd edition n Civetta. Critical Care 4 th Edition 2009 31 31