Surgical Management of Obstructive Sleep Apnea Marilene B
Surgical Management of Obstructive Sleep Apnea Marilene B. Wang, MD Chief of Otolaryngology, VAGLAHS Professor UCLA Division of Head and Neck Surgery
Evaluation of Sleep n Polysomnography n n n n EMG Airflow EEG, EOG Oxygen Saturation Cardiac Rhythm Leg Movements AI, HI, AHI, RDI
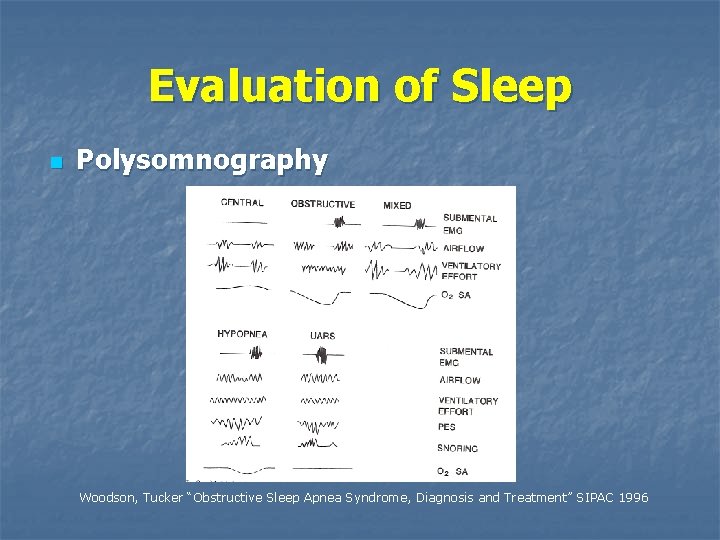
Evaluation of Sleep n Polysomnography Woodson, Tucker “Obstructive Sleep Apnea Syndrome, Diagnosis and Treatment” SIPAC 1996

Definition of OSA n n RDI>5 RDI > 20 increases risk of mortality RDI 20 -40=moderate, >40=severe Upper Airway Resistance Syndrome n n n Shares pathophysiology with OSA No desaturation, continuous ventilatory effort Snoring
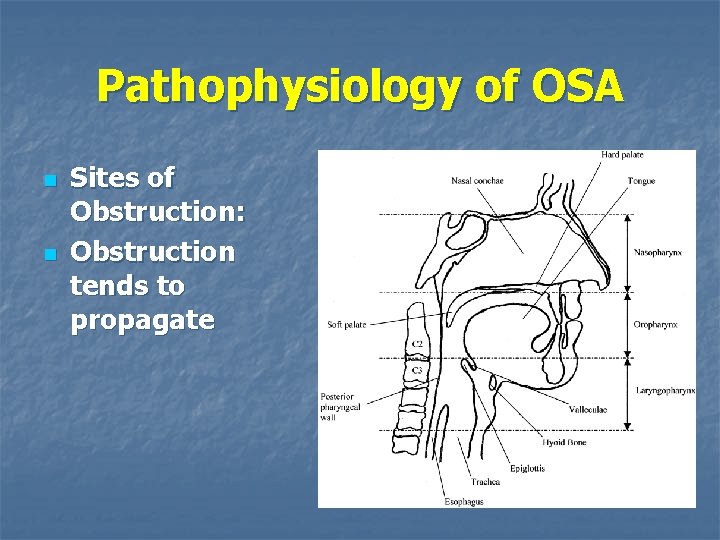
Pathophysiology of OSA n n Sites of Obstruction: Obstruction tends to propagate
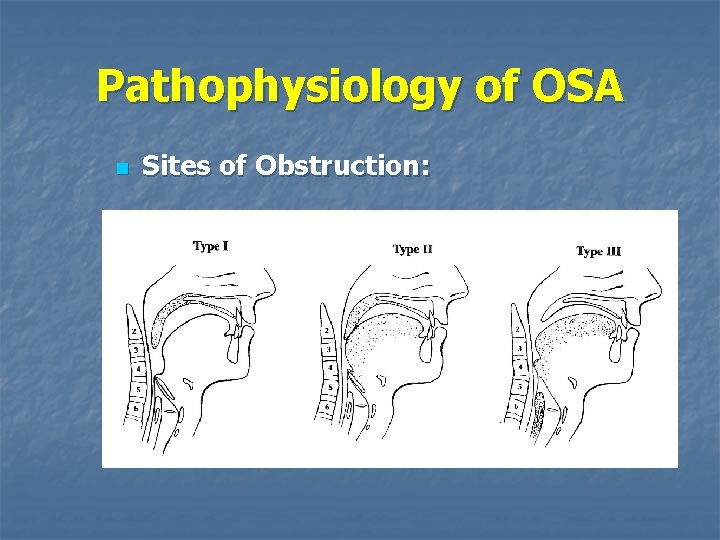
Pathophysiology of OSA n Sites of Obstruction:

Pathophysiology of OSA n Symptoms of OSA Snoring (most commonly noted complaint) n Daytime Sleepiness n Hypertension and Cardiovascular Disease are Associated n Pulmonary Disease n

Pathophysiology of OSA n Findings in Obstruction: Nasal Obstruction n Long, thick soft palate n Retrodisplaced Mandible n Narrowed oropharynx n Redundant pharyngeal tissues n Large lingual tonsil n Large tongue n Large or floppy Epiglottis n Retro-displaced hyoid complex n
Pathophysiology of OSA n Tests to determine site of obstruction: Muller’s Maneuver n Sleep endoscopy n Fluoroscopy n Manometry n Cephalometrics n Dynamic CT scanning and MRI scanning n
Medical Management n n n Weight Loss/Exercise Nasal Obstruction/Allergy Treatment Sedative Avoidance Smoking cessation Sleep hygiene Consistent sleep/wake times n Avoid alcohol, heavy meals before bedtime n Position on side n Avoid caffeine, TV, reading in bed n
Medical Management n CPAP n n Pressure must be individually titrated Compliance is as low as 50% n Air leakage, eustachian tube dysfunction, noise, mask discomfort, claustrophobia
Medical Management n Bi. PAP n n Useful when > 6 cm H 2 O difference in inspiratory and expiratory pressures No objective evidence demonstrates improved compliance over CPAP
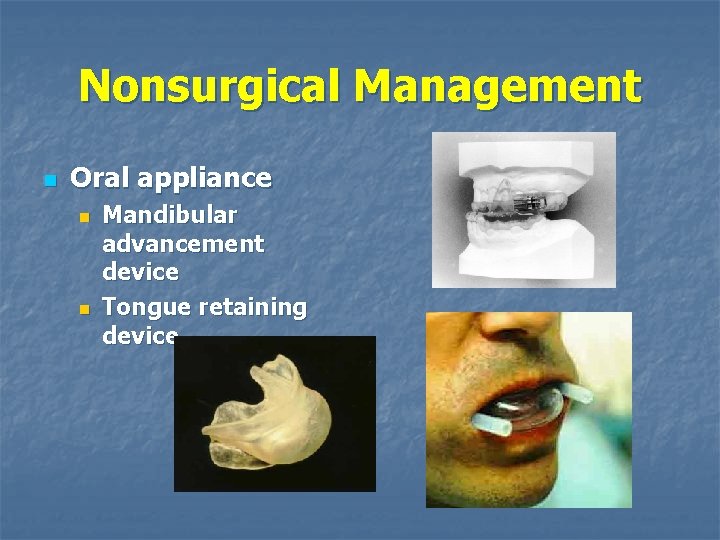
Nonsurgical Management n Oral appliance n n Mandibular advancement device Tongue retaining device
Nonsurgical Management n Oral Appliances May be as effective as surgical options, especially with sx worse on patient’s back n However low compliance rate of about 60% in study by Walker et al in 2002 rendered it a worse treatment modality than surgical procedures n Walker-Engstrom ML. Tegelberg A. Wilhelmsson B. Ringqvist I. 4 -year follow-up of treatment with dental appliance or uvulopalatopharyngoplasty in patients with obstructive sleep apnea: a randomized study. Chest. 121(3): 739 -46, 2002 Mar.
Surgical Management n Measures of success – No further need for medical or surgical therapy n Response = 50% reduction in RDI n Reduction of RDI to < 20 n Reduction in arousals and daytime sleepiness n

Surgical Management n Perioperative Issues High risk in patients with severe symptoms n Associated conditions of HTN, CVD n Nasal CPAP often required after surgery n Nasal CPAP before surgery improves postoperative course n Risk of pulmonary edema after relief of obstruction n
Surgical Management n Nasal Surgery Limited efficacy when used alone n Verse et al 2002 showed 15. 8% success rate when used alone in patients with OSA and day-time nasal congestion with snoring (RDI<20 and 50% reduction) n n Adenoidectomy (children)

Surgical Management n Uvulopalatopharyngoplasty The most commonly performed surgery for OSA n Severity of disease is poor outcome predictor n Levin and Becker (1994) up to 80% initial success decreased to 46% success rate at 12 months n Friedman et al showed a success rate of 80% at 6 months in carefully selected patients n Friedman M, Ibrahim H, Bass L. Clinical staging for sleep-disordered breathing. Otolaryngol Head Neck Surg 2002; 127: 13– 21.
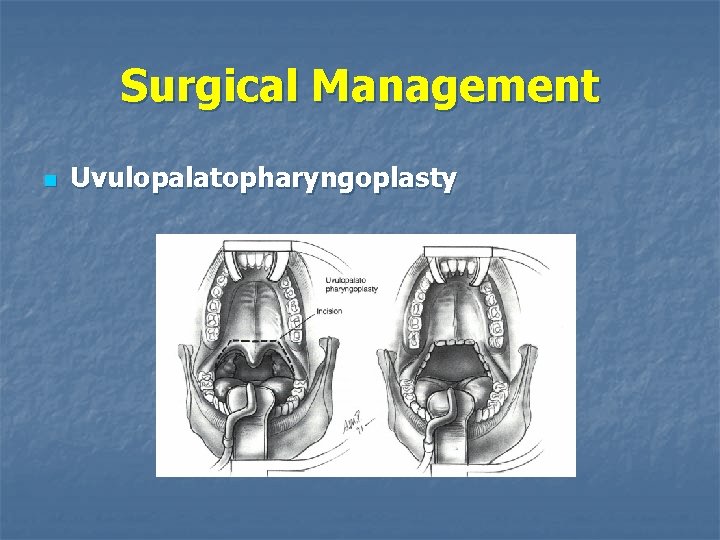
Surgical Management n Uvulopalatopharyngoplasty
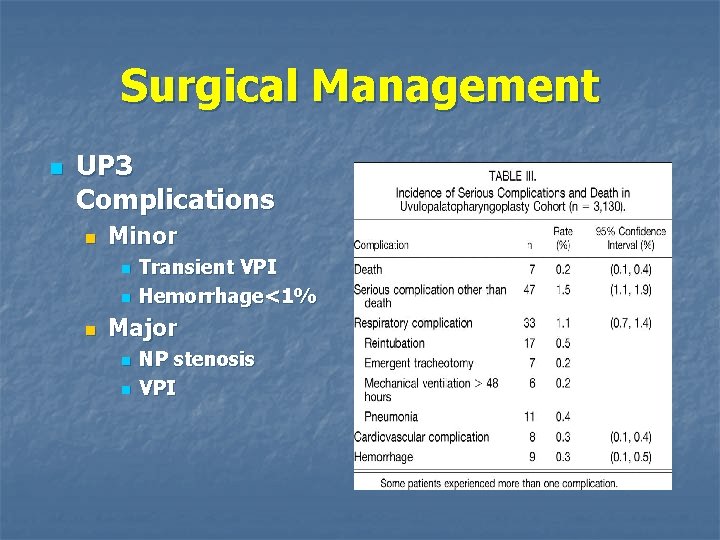
Surgical Management n UP 3 Complications n Minor n n n Transient VPI Hemorrhage<1% Major n n NP stenosis VPI
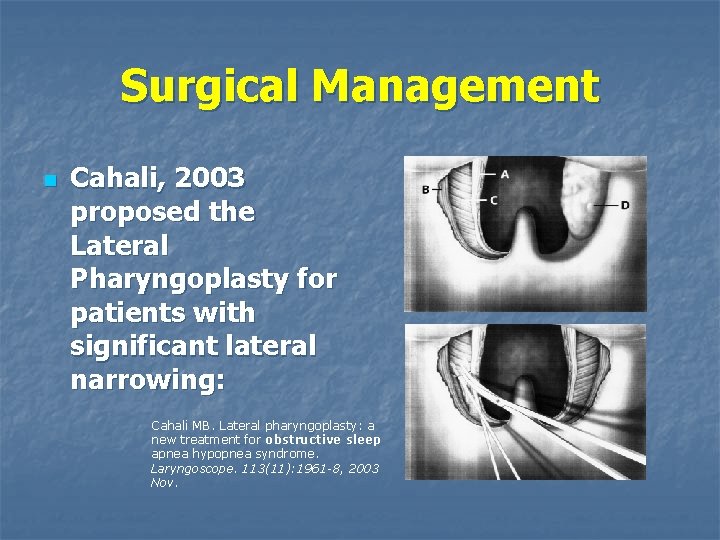
Surgical Management n Cahali, 2003 proposed the Lateral Pharyngoplasty for patients with significant lateral narrowing: Cahali MB. Lateral pharyngoplasty: a new treatment for obstructive sleep apnea hypopnea syndrome. Laryngoscope. 113(11): 1961 -8, 2003 Nov.
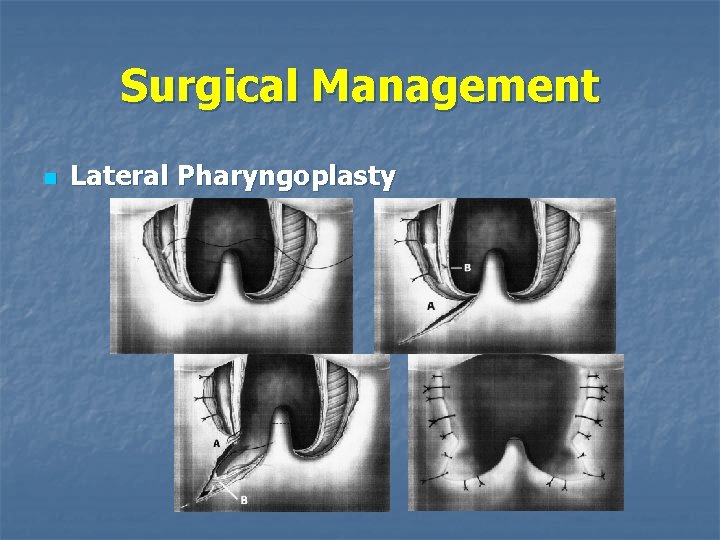
Surgical Management n Lateral Pharyngoplasty
Surgical Managment n Lateral Pharyngoplasty Median apnea-hypopnea index decreased from 41. 2 to 9. 5 (P =. 009) n No control group n No evaluation at 12 months n

Surgical Management n Laser Assisted Uvulopalatoplasty n n n High initial success rate for snoring Rates decrease, as for UP 3, at twelve months Performed awake
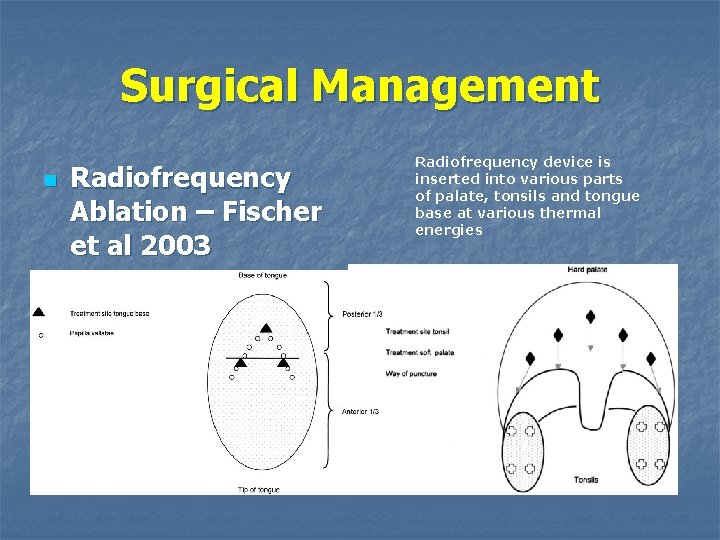
Surgical Management n Radiofrequency Ablation – Fischer et al 2003 Radiofrequency device is inserted into various parts of palate, tonsils and tongue base at various thermal energies
Surgical Management n Fischer et al 2003 n At 6 months Showed significant reduction of: n n n RDI (but not to below 20) Arousals Daytime sleepiness by the Epworth Sleepiness Scale
Pillar™ Palatal Implant System n n n n Three Implants Per Patient Implants are made of Dacron® Implants are 18 mm in length and 1. 8 mm in diameter Implants are meant to be Permanent Implants “can be removed” FDA Approved for SNORING FDA Approved for mild to moderate SLEEP APNEA - AHI UNDER 30
Anesthesia n n n n Antibiotic 1 hour pre-op or as directed Mouth Rinse (chlorhexidine gluconate or equivalent) Hurricane or Equivalent Topical Spray Ponticane or Equivalent Topical Jelly Anesthetic, optional. Local Anesthetic Infiltration: 2 to 3 cc. Beginning at the junction of the Hard and Soft Palate inject entire “Target Zone”. (lidocaine with epinephrine or equivalent) Have available: Flexible Scope, Angled Tonsil Forceps
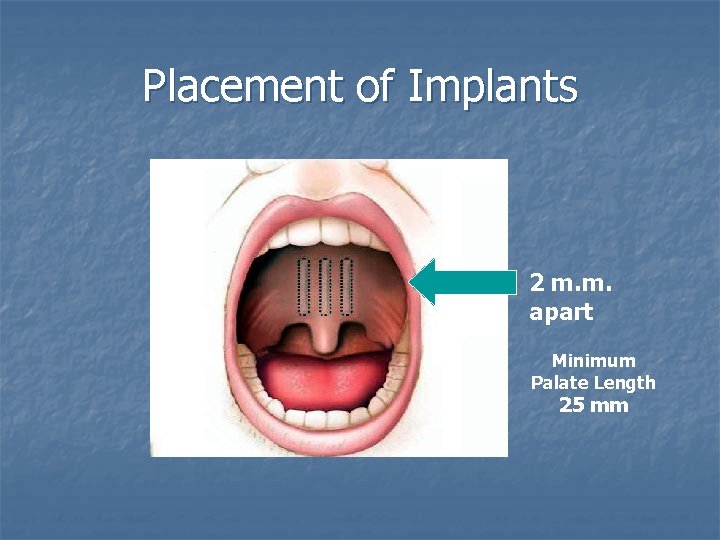
Placement of Implants 2 m. m. apart Minimum Palate Length 25 mm
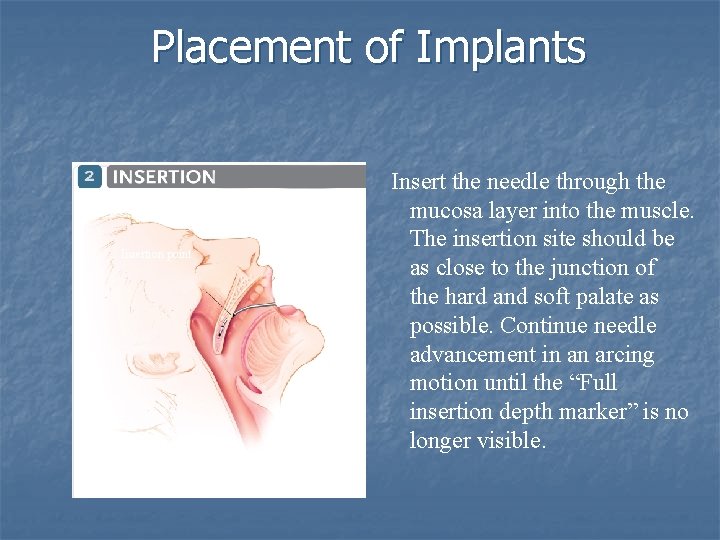
Placement of Implants Insertion point Insert the needle through the mucosa layer into the muscle. The insertion site should be as close to the junction of the hard and soft palate as possible. Continue needle advancement in an arcing motion until the “Full insertion depth marker” is no longer visible.
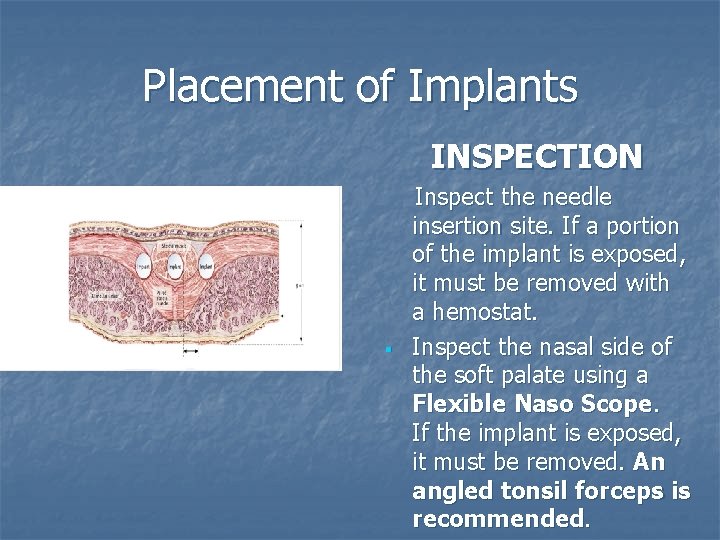
Placement of Implants INSPECTION Hard palate Muscle Implant Glandular tissue § Inspect the needle insertion site. If a portion of the implant is exposed, it must be removed with a hemostat. Inspect the nasal side of the soft palate using a Flexible Naso Scope. If the implant is exposed, it must be removed. An angled tonsil forceps is recommended.
Patient Selection “The Preferred Patient” n n n n BMI less than 32 AHI Less than 30 No Obvious Nasal Obstruction Small to Medium Sized Tonsils Mallampati Class І or Class ΙΙ Friedman Tongue Position I and II Minimum 25 mm Palate to treat
Surgical Management n Tongue Base Procedures n Lingual Tonsillectomy n may be useful in patients with hypertrophy, but usually in conjunction with other procedures
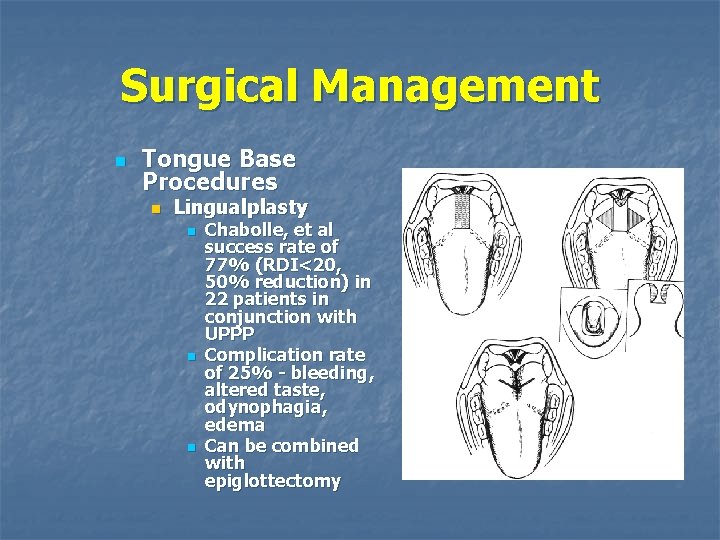
Surgical Management n Tongue Base Procedures n Lingualplasty n n n Chabolle, et al success rate of 77% (RDI<20, 50% reduction) in 22 patients in conjunction with UPPP Complication rate of 25% - bleeding, altered taste, odynophagia, edema Can be combined with epiglottectomy
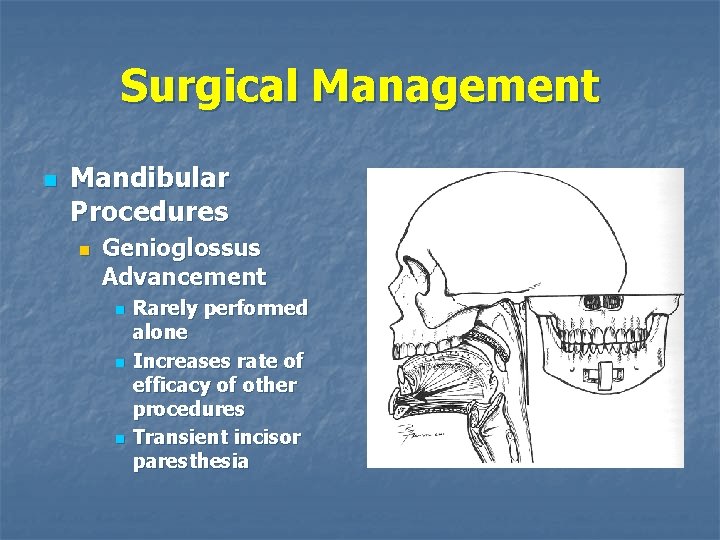
Surgical Management n Mandibular Procedures n Genioglossus Advancement n n n Rarely performed alone Increases rate of efficacy of other procedures Transient incisor paresthesia
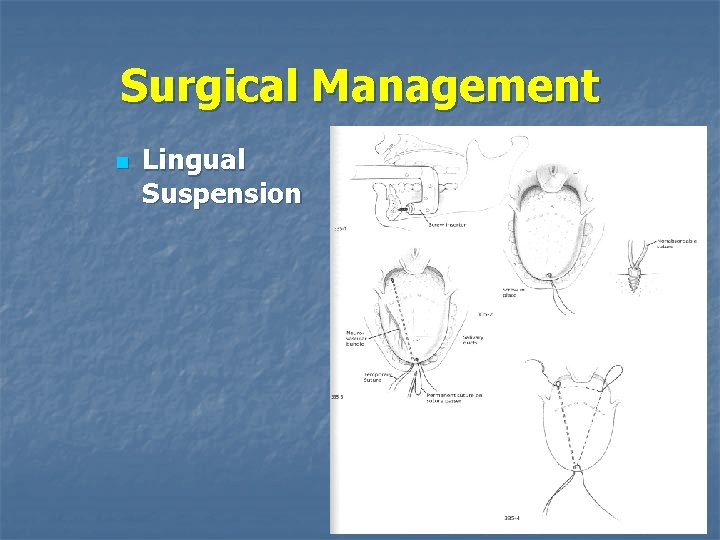
Surgical Management n Lingual Suspension
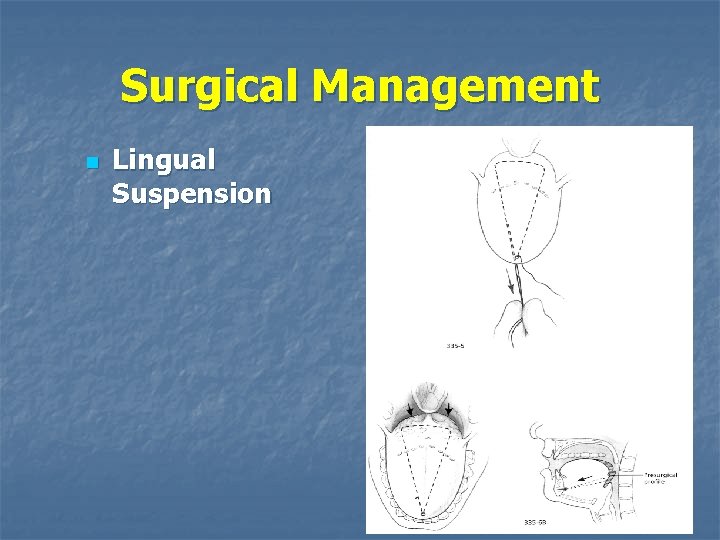
Surgical Management n Lingual Suspension
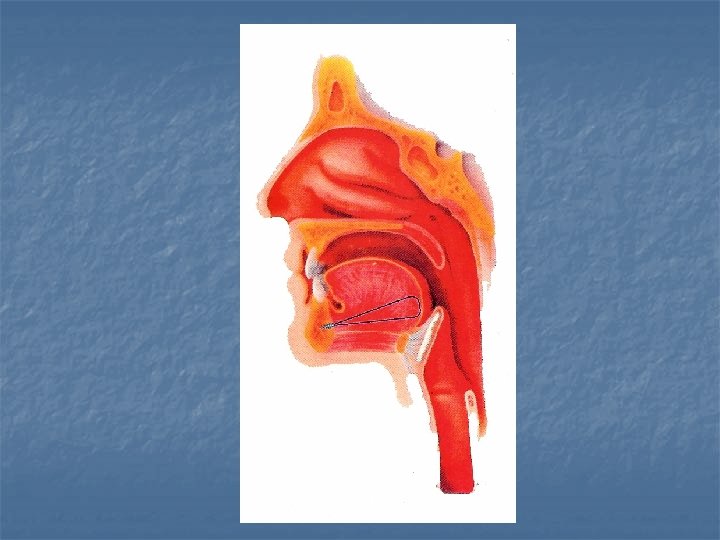

Surgical Management n Hyoid Myotomy and Suspension n n Advances hyoid bone anteriorly and inferiorly Advances epiglottis and base of tongue Performed in conjunction with other procedures Dysphagia may result

Surgical Management n Maxillary-Mandibular Advancement Severe disease n Failure with more conservative measures n Midface, palate, and mandible advanced anteriorly n Limited by ability to stabilize the segments and aesthetic facial changes n

Surgical Management n Maxillary. Mandibular Advancement n n n Performed in conjunction with oral surgeons Temporary or permanent paresthesia Change in facial structure
Surgical Management n Algorithms Studies efficacy of various algorithms n Therapy should be directed toward presumed site of obstruction n n This does not always guarantee results
Surgical Management n Algorithms n Riley et al 1992 n Studied 2 phase approach for multilevel site of obstruction (Stanford Protocol): n n n Phase 1: Genioglossal advancement, hyoid myotomy and advancement, UP 3 Phase 2: Maxillary-Mandibular advancement in 6 months if phase 1 failed Reported >90% success rate in patients who completed both phases Other studies have lowered this number Testing is done at 6 months

Surgical Management n Algorithms n Friedman et al developed a staging system for type of operation:

Surgical Management n n n Chance of success with surgical management decreases with increasing Friedman stage Stage I and II patients have good success with UPPP and tongue base procedures Stage III and IV patients have much lower rates of success following UPPP/tongue base
Ultimate Surgical Management n n n Tracheotomy Morbid obesity Significant anesthetic/surgical risks Obvious disadvantages Trach care Supplies, equipment n aesthetics n
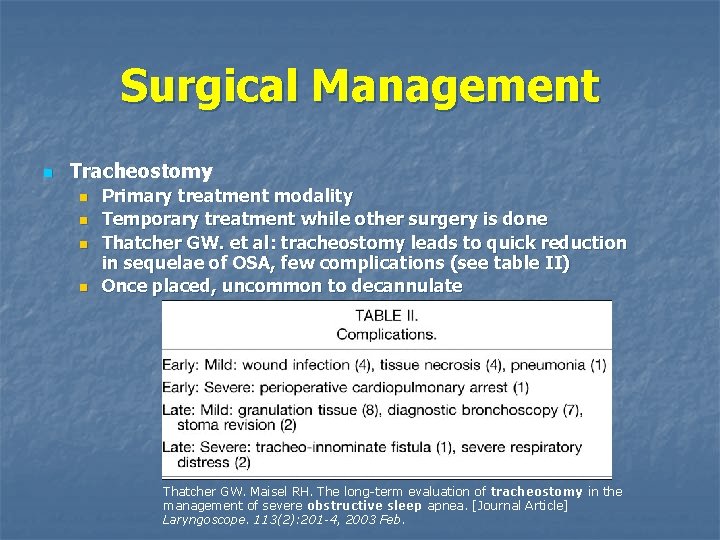
Surgical Management n Tracheostomy n n Primary treatment modality Temporary treatment while other surgery is done Thatcher GW. et al: tracheostomy leads to quick reduction in sequelae of OSA, few complications (see table II) Once placed, uncommon to decannulate Thatcher GW. Maisel RH. The long-term evaluation of tracheostomy in the management of severe obstructive sleep apnea. [Journal Article] Laryngoscope. 113(2): 201 -4, 2003 Feb.
CONCLUSIONS n n Surgical management provides effective management for OSA Can be safely performed in most patients with proper preoperative preparation Significant perioperative risks in some patients Surgery should be considered for patients unable to utilize nonsurgical management
- Slides: 49