SUR 122 OBSTETRICAL GYNECOLOGICAL SURGERY OBGYN Surgery Female
SUR 122 OBSTETRICAL & GYNECOLOGICAL SURGERY
OB-GYN Surgery Female ¡ From beginning of menses ¡
OB-GYN Specialists ¡ ¡ ¡ Obstetricians: pregnancy Gynecologists: Breast Surgery (non-reconstructive) Bladder Tac related Surgeries: pubovaginal Sling, TVT (tension vaginal tape, A & P Repair, etc. ) Can be both or one or the other Fertility Specialists Oncology Gynecologist
Obstetrical & Gynecological Surgery ¡ ¡ ¡ ¡ Reasons For: Diagnose abnormalities Treat abnormalities Pain relief Prevention of pregnancy Aide in conception for infertile couples Prevention of spontaneous abortion Cesarian delivery (abdominal) when vaginal delivery not possible
The Female Reproductive System ¡ ¡ ¡ ¡ Anatomy & Physiology Pathology Diagnostic & Pre-operative Testing Anesthesia & Medications Basic Supplies, Instrumentation, & Equipment Positioning, Prep, & Draping Dressings, Drains, & Post-operative Care
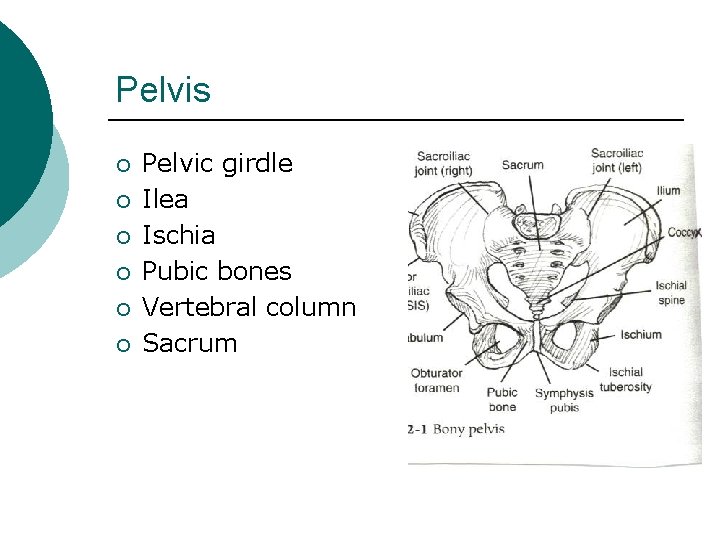
Pelvis ¡ ¡ ¡ Pelvic girdle Ilea Ischia Pubic bones Vertebral column Sacrum
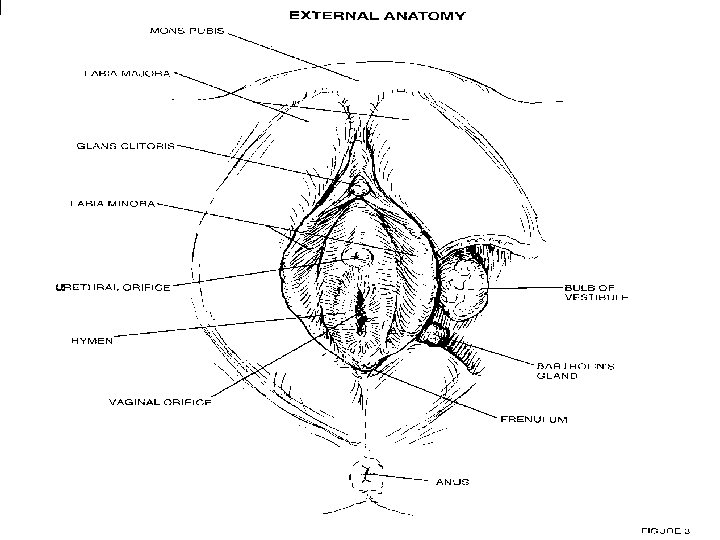
Anatomy & Physiology ¡ ¡ ¡ ¡ ¡ External Female Genitalia (Vulva) Mons pubis Labia majora Labia minora Urethral orifice Vaginal orifice Clitoris Hymen Perineum Anus
External genitalia ¡ Labia minora form the clitoris and contain sebaceous glands ¡ Vestibule is the cavity between the labia minora Contains urethral meatus and Bartholin’s (vestibular) glands ¡ ¡ ¡ Perineum is the area between vaginal opening and anus Can stretch with delivery however is frequently cut with an incision called episiotomy to prevent spontaneous tears during vaginal delivery
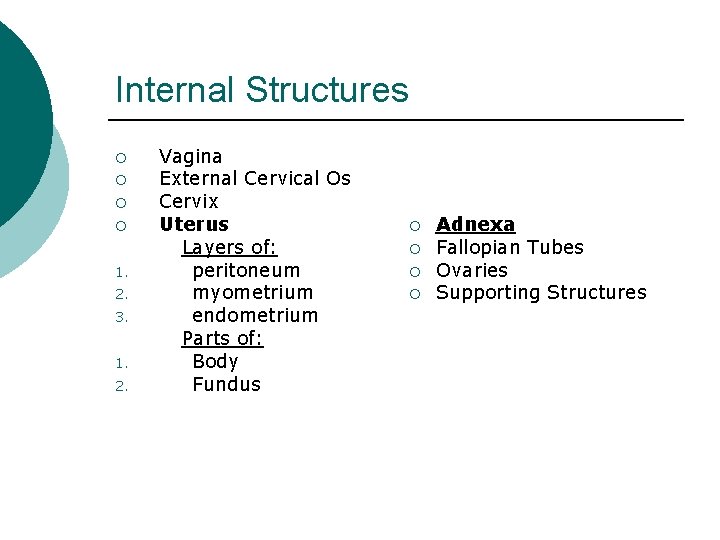
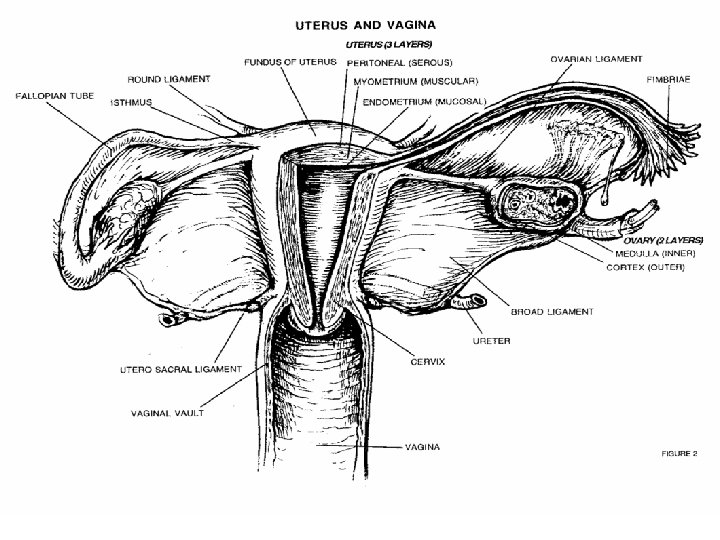
Internal Structures ¡ ¡ 1. 2. 3. 1. 2. Vagina External Cervical Os Cervix Uterus Layers of: peritoneum myometrium endometrium Parts of: Body Fundus ¡ ¡ Adnexa Fallopian Tubes Ovaries Supporting Structures
Vagina Receptacle to penis ¡ Passageway for menstrual flow ¡ Lower portion is the birth canal ¡
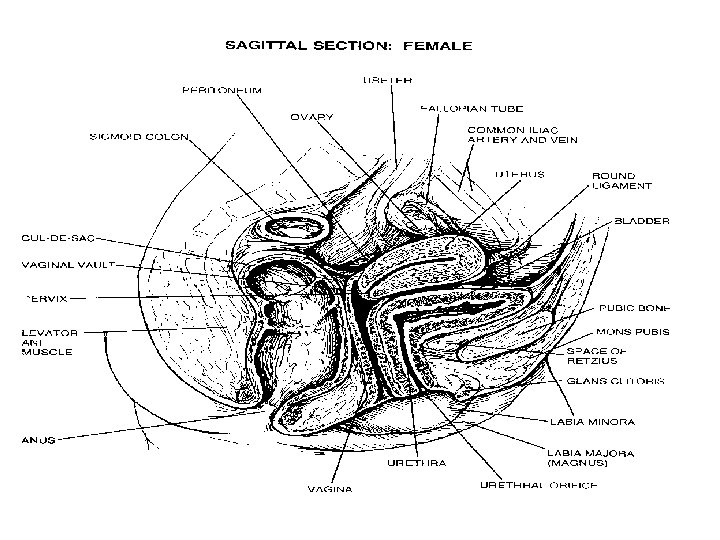
Uterus Function: ¡ Site of menstruation ¡ Or ¡ Site of implantation if implantation occurs then is the site of fetal development ¡
Uterus Parts of: ¡ Dome shaped portion=fundus ¡ Central portion=body ¡ Where narrows=cervix ¡ Internal cervical os=where uterus and cervix meet ¡ External os=where cervix meets vagina ¡
Uterus Lining of: 1. Perimetrium=outsi de of uterus covered in a this serous membrane lining 2. Myometrium= -smooth muscle lining -middle layer -fetal support -during labor expels fetus with assistance of hormone oxytocin ¡ 3. Endometrium=inner lining 2 parts: a. stratum basalis permanent layer thin b. Stratum functionalis -produced by s. basalis -temporary layer -shed w/menstruation -produces maternal portion of placenta
Uterus Blood supply: ¡ Uterine artery and uterine vein ¡
Ovaries ¡ ¡ ¡ Function: Production and expulsion of oocytes (ova or eggs) Release of hormones: estrogen and progesterone Are both endocrine and exocrine glands Exocrine produce eggs (ducts=fallopian tubes) Endocrine portion produces estrogen and progesterone
Ovaries Attachments: 1. Broad ligament -largest formed by a fold of peritoneum -contains fallopian tube, round and ovarian ligaments, blood vessels, lymphatics, and nerves ¡ Suspensory ligament ¡ Ovarian ligament ¡
Ovaries Suspensory ligament -small peritoneum fold -holds ovaries at upper end -contains blood vessels and nerves 3. Ovarian ligament -attaches ovaries at their lower end -is actually a thickening in the broad ligament 2.
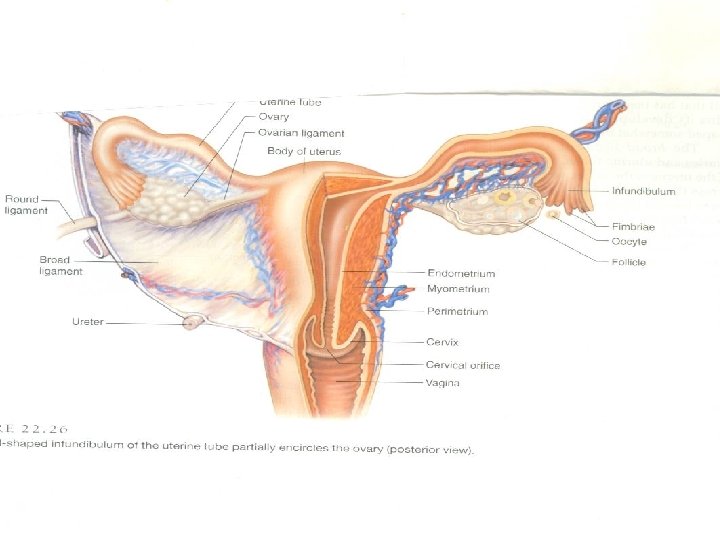
Fallopian tubes Egg is caught by finger-like projections called the fimbrae after it is released from the ovary ¡ Funnel shaped end prior to fimbrae=infundibulum ¡
Fallopian tubes 2 layers: 1. Mucous membrane innermost ¡ Is lined with ciliated columnar epithelial tissue ¡ Allows for movement of the egg ¡ Scarring from STDs can damage or scar this lining rendering a female sterile ¡
Fallopian tubes 2. Muscularis ¡ Smooth muscle ¡ Peristalsis or movement of the egg ¡ So… ¡ Egg movement through the fallopian tubes occurs by cilia and peristalsis ¡ Fertilization must occur in the distal 1/3 of the fallopian tubes for successful implantation into the uterus
Physiology ¡ ¡ ¡ Ovarian cycle caused by anterior pituitary gland which secretes: LH “ovulation hormone” FSH levels must be low to allow ovulation Causes secretion of estrogen Menses is caused by a sudden decrease in estrogen and progesterone triggered by no fertilization
Hormones 1. FSH ¡ Produced in anterior lobe pituitary ¡ Causes graafian follicular development ¡ Causes estrogen secretion
Hormones 2. ¡ ¡ LH Produced in anterior lobe pituitary Continues follicular development Stimulates estrogen and progesterone production Causes ovulation
Hormones 3. ¡ Estrogen Maintenance and development of reproductive organs and female sex characteristics
Hormones 4. ¡ ¡ ¡ Progesterone Primary cause of endometrial changes With Prolactin (hormone) influences mammary glands to develop and secrete milk Milk secretion and labor is stimulated by oxytocin (hormone)
Physiology In the ovary > the big 4 hormones are increasing which develops a follicle ¡ Follicle becomes a graafian follicle ¡ Graafian follicle rupture>egg released into fallopian tubes ¡ Outer rind of graafian follicle becomes corpus luteum ¡
Physiology ¡ ¡ ¡ 2 possibilities: No fertilization=corpus luteum degenerates and becomes corpus albicans and cycle starts over Fertilization=corpus luteum maintained four months to suppress egg production and menstruation with estrogen and progesterone Progesterone levels must be high enough to maintain endometrial lining to sustain pregnancy Corpus luteum acts as a temporary endocrine gland After four months placenta is developed and takes over
Obstetrics
Pregnancy (Obstetrics) Procedures ¡ ¡ 1. 2. ¡ ¡ Cerlage (Mac. Donald or Shirodkar) Deliveries: Vaginal Cesarian sections (C-sections) Tubal ligations (sterilization procedures) Emergent hysterectomy
Pregnancy Terminology ¡ ¡ 1. 2. 3. 4. Labor Four stages of: True labor onset Cervical dilation complete>birth Birth>placental delivery Placental delivery > stabilization of mother ¡ 1. 2. 3. 4. Primapara 6 -18 hours ½ - 3 hours (dilation 1 cm/hr) 0 -30 min 6 hours Multipara 2 -10 hours 5 -30 min (dilation 1. 2 cm/hr) 0 -30 min 6 hours
Pregnancy Terminology Braxton Hicks - “false labor” ¡ Bloody show – onset of labor ¡ Cervical dilation - cervical measurement (0 to 8 cm) ¡ Cervical Effacement – thinning of cervix ¡ Crowning - neonate head circumference at its largest point as it passes thru vulvar ring ¡
Pregnancy Terminology ¡ ¡ ¡ ¡ Descent – movement of fetus thru pelvis with contractions Expulsion – delivery of infant Gravida - how many times a woman has been pregnant Parity – number of time a woman has given birth Position – relationship between presenting infant part & pelvis of mother (OA) most common Presentation – fetal part overlying pelvic inlet Station – measurement of the descent of the infant’s presenting part thru the ischial spines
Presentation Breech - buttocks first ¡ Transverse – crosswise ¡ Footling – feet ¡ Vertex – upper back of head ¡
Obstetrical Complications Placenta previa – placental implantation over cervix ¡ Abruptio Placenta – premature placental separation ¡
Obstetrical Complications Abortions ¡ Missed ¡ Incomplete ¡ Imminent ¡ Spontaneous ¡ Voluntary ¡
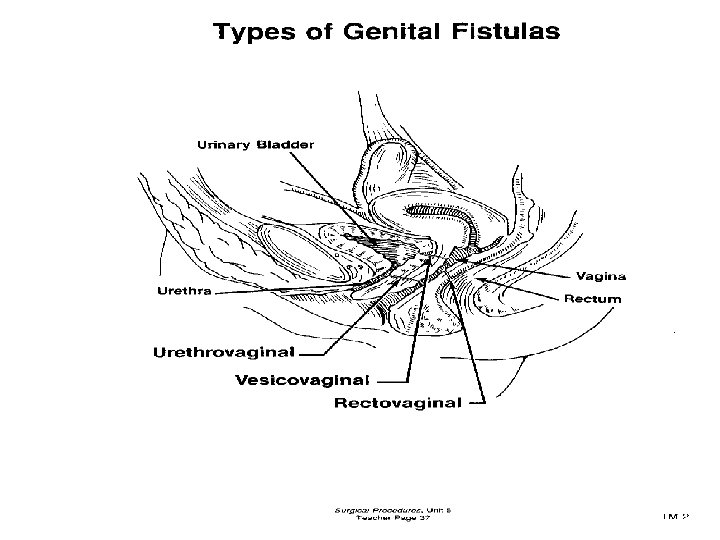
Pathology ¡ ¡ ¡ ¡ Benign Cysts Polyps (pedunculated lesion) Fistulas Dysplasia Leiomyoma/Myoma/Fibroid Fibroma ¡ ¡ ¡ ¡ Malignant Vulvar Vaginal Cervical Uterine Ovarian Other Endometriosis Cystocele Rectocele (posterior colporrhaphy) Enterocele Ectopic Pregnancy Incompetent Cervix (cerclage)
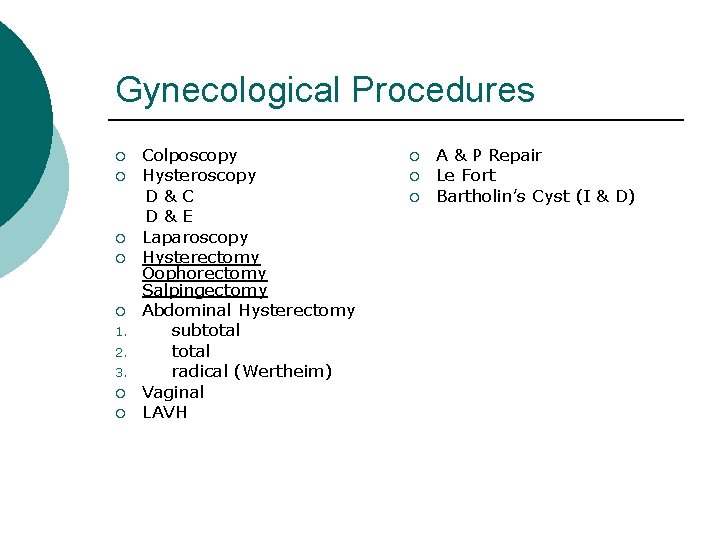
Gynecological Procedures ¡ ¡ ¡ 1. 2. 3. ¡ ¡ Colposcopy Hysteroscopy D&C D&E Laparoscopy Hysterectomy Oophorectomy Salpingectomy Abdominal Hysterectomy subtotal radical (Wertheim) Vaginal LAVH ¡ ¡ ¡ A & P Repair Le Fort Bartholin’s Cyst (I & D)
Patient symptoms: Abnormal bleeding ¡ Abdominal pain ¡ Absence of menses (amenorrhea) ¡ Excessive menses (menorrhagia) ¡ Painful menses (dysmenorrhea) ¡ Painful intercourse (dysparunia) ¡ Painful defication (dyschezia) ¡
Pre-Operative & Testing Diagnostic ¡ ¡ ¡ ¡ Physical exam UA, CBC, Blood Chemistry Pelvic exam Bi-manual exam Colposcopy PAP (papanicolaou smear) Schiller Test Biopsy Ultrasound MRI X-ray Laparoscopy D&C
Anesthesia General ¡ Spinal ¡ MAC with IV Sedation ¡
Medications Oxytocics: ¡ Stimulate uterine contraction to induce labor ¡ Post-delivery of baby and placental contents to induce uterine contraction allowing for expulsion of excess tissue and clots ¡ Post-delivery to prevent bleeding/hemorrhage ¡
Medications Lugol’s solution ¡ Iodine based ¡ Identification of abnormal vaginal and or cervical tissue ¡ Tissue that is abnormal will not stain ¡ Tissue that is normal will stain brown ¡ Schiller’s Test ¡
Medications ¡ ¡ ¡ ¡ 3% Acetic Acid Facilitates cervical visualization by removing cervical mucous Used during a colposcopy Methylene blue Dye Diluted with NS Direct > Checks for tubal patency (chromotubation) IV > excreted by the kidneys into the urine rules out ureteral injury as abdominal procedure concludes
Medications Antimicrobials ¡ Prophylactic ¡ IV ¡ ung (ointment) utilized with vaginal packing materials ¡
Medications ¡ ¡ ¡ ¡ Hysteroscopy solutions (for uterine distention) Dextrose 5% (D 5 W) Dextran 70% in dextrose Glycine Sorbitol Above may all be used with laser or cautery Hyskon (rarely used anymore due to ↑ laser use) No cautery or lasers may be used as would cause systemic absorption>systemic side effects
Instruments Major Tray ¡ Abdominal-Hysterectomy Tray ¡ D&C Tray ¡ Hysteroscopy Tray resectoscope & hysteroscope ¡ Laparoscopic Tray ¡ Camera/scope tray/scope warmer ¡
Specific Vaginal Instruments ¡ ¡ ¡ Auvard weighted speculum Graves speculum Sims vaginal speculum (single or double ended) Delivery forceps Goodell uterine dilator Sims uterine sound Bozeman uterine dressing forcep Hegar uterine dilators Heaney uterine dilators Emmett uterine tenaculum Sims uterine curettes (blunt/sharp)
Specific Abdominal Hysterectomy Instruments ¡ ¡ ¡ ¡ ¡ Abdominal retractor tray richardsons, deavers, malleables, Balfour w/bladder blade O’Sullivan-O’Connor abdominal Retractor Franz Abdominal Retractor Heaney Hysterectomy Forceps Heaney-Ballentine Hysterectomy Forceps Heaney Needleholder Jorgenson Curved Scissors Lister Bandage Scissors Pennington Forceps
Specific Laparoscopy Instruments ¡ ¡ ¡ ¡ ¡ Scope, Light cord (scope tray) Camera (camera sleeve if not sterile) Insufflation tubing (silastic tubing) Verres Needle (insufflation needle) Intrauterine cannula (chromotubation) Uterine manipulator Trocar Sleeves, Trocars Accessory Instruments: cautery adapted, graspers, scissors, loop applicators, suturing devices, resectoscopes Scope warmer Multi-fire laparoscopic staplers
Positioning ¡ ¡ ¡ ¡ Lithotomy Supine Trendelenburg OR table with foot-drop capacity Stirrups (candy cane, Allen, or Yellow Fins) Armboards Pillow/Headrest
Prep Likely do abdomen first if combined with vaginal approach ¡ Care to not allow pooling of prep solution in vagina especially if laser to be used ¡
Draping Impervious buttock drape (may have a port to attach to suction or just a “fluid-catch” bag ¡ Leggings ¡ Perineal drape with fenestration ¡ Laparotomy sheet ¡ Combination perineal/laparotomy drape ¡
Dressings Vaginal packing ¡ May be soaked in an antimicrobial solution ¡ May be pre-medicated packing (Iodophor) ¡ Perineal Pad ¡ Abdominal dressing surgeon choice ¡ Steri-strips, bandaids, telfa, xeroform, 4 x 4 s, ABD pad, primapore, tape (misc. ) ¡
Drains Penrose ¡ Closed Wound Drains: ¡ Jackson-Pratt ¡ Hemovac ¡
Post-operative Care ¡ ¡ ¡ Foley Catheter (placed pre-operatively by circulator or surgeon) Anti-embolic stockings Ted Hose Get OOB early to ambulate Performed in: physician offices, outpatient centers (ASC), hospital ORs May be discharged same day or have onethree day hospitalization depending on procedure
Post-Operative Complications ¡ ¡ ¡ ¡ Infection Nicking ureters, bladder, or urethra Hemorrhage (major blood vessel proximity) Adhesions Sciatic nerve damage due to spinal or epidural placement Blood clot (thrombosis) DVT PE (pulmonary embolus)
Summary ¡ ¡ ¡ ¡ Anatomy & Physiology Pathology Diagnostic & Pre-operative Testing Anesthesia & Medications Basic Supplies, Instrumentation, & Equipment Positioning, Prep, & Draping Dressings, Drains, & Post-operative Care
- Slides: 62