Supra Ventricular Tachycardia Pathophysiology ECG features Management Authors


- Slides: 33
Supra. Ventricular Tachycardia : Pathophysiology, ECG features, Management Author(s): Geraldine Leong Level: Basic Academic Affiliation: Emergency Medicine Resident, Sing. Health Version No: 1. 0 Submitted: March 2012 Editors’ Review:
2 Disclaimer/Liability • The information provided in the VAP is made available in good faith and is derived from sources believed to be reliable and accurate at the time of release. • The materials presented on the VAP may include links to external Internet sites. These external information sources are outside the control of Duke-NUS. The user of the Internet links is responsible for making his or her own decision about the accuracy, reliability and correctness of the information found. • In no event shall Duke-NUS be liable for any indirect, special, incidental, or consequential damages arising out of any use of reliance of any information contained in the VAP. Nor does Duke-NUS assume any responsibility for failure or delay in updating or removing the information contained in the VAP. • Moreover, information provided on the VAP does not constitute medical advice or treatment nor should it be considered as a replacement of the patient/physician relationship or a physician’s professional judgment. Duke-NUS expressly disclaims all liability for treatment, diagnosis, decisions and actions taken or not taken in reliance upon information contained in the VAP. This work is licensed under a Creative Commons Attribution-Non. Commercial-No. Derivs 3. 0 Unported License To view a copy of this license, visit [http: //creativecommons. org/licenses/by-nc-nd/3. 0/]
3 Financial Disclosures (past 3 years) No Disclosures
4 Outline • Definition • Classification of tachyarrythmias • Pathophysiology • ECG features • Management principles in ED • Clinical scenario
5 Definition • Point of stimulation arises from above the bundle branches • 3 main features: – Regular – Narrow complex (QRS <120 ms) – Tachycardia

6 Classification Tachyarrythmias Narrow-complex Irregular Regular - fast atrial - sinus fibrillation tachycardia - atrial flutter with variable conduction - AVRT - multifocal atrial tachycardia - AVNRT - atrial flutter with 2: 1 conduction - junctional tachycardia Broad-complex • Ventricular Fibrillation • Ventricular Tachycardia • Any supraventricular tachycardias with aberrancy
7 Pathophysiology • 3 main mechanisms – Re-entrant dysrhythmias – Abnormal automaticity – Triggered dysrhythmias • Re-entrant dysrhythmias most commonly encountered mechanism
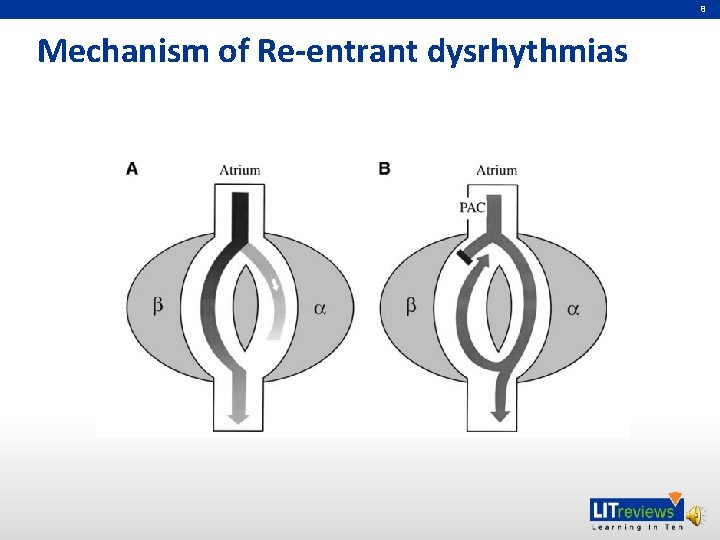
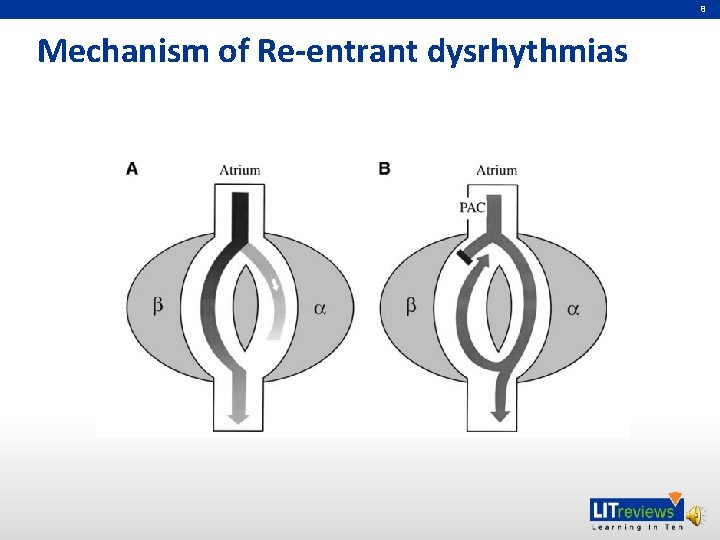
8 Mechanism of Re-entrant dysrhythmias
9 Paroxysmal SVTs Two types: • AVNRT (~60%) – AV nodal re-entrant tachycardia – Commonest type • AVRT (~30%) – AV re-entry tachycardia – A/w Accessory pathway – Eg. Wolf – Parkinson – White Syndrome
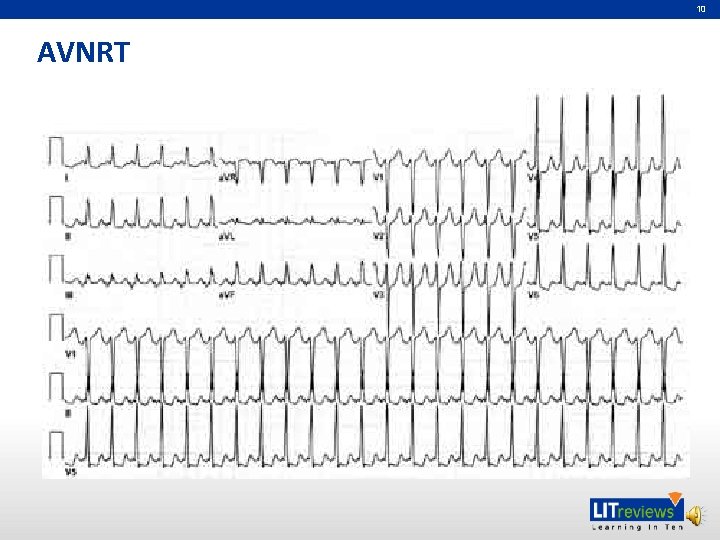
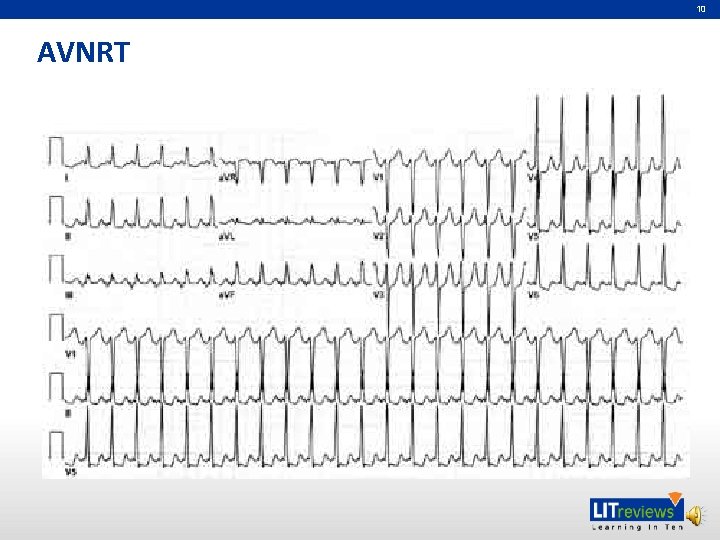
10 AVNRT
11 AVNRT: ECG features • Narrow complex, regular tachycardia • No P waves prior to QRS complexes • P waves are usually buried within QRS complex (but not always the case) • Rate is fixed – not like sinus tachycardia where rate demonstrates gradual variations over time in response to etiology and interventions
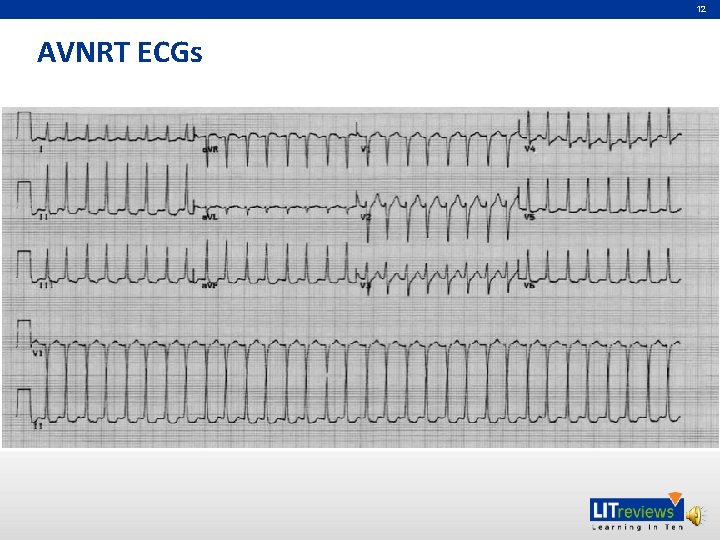
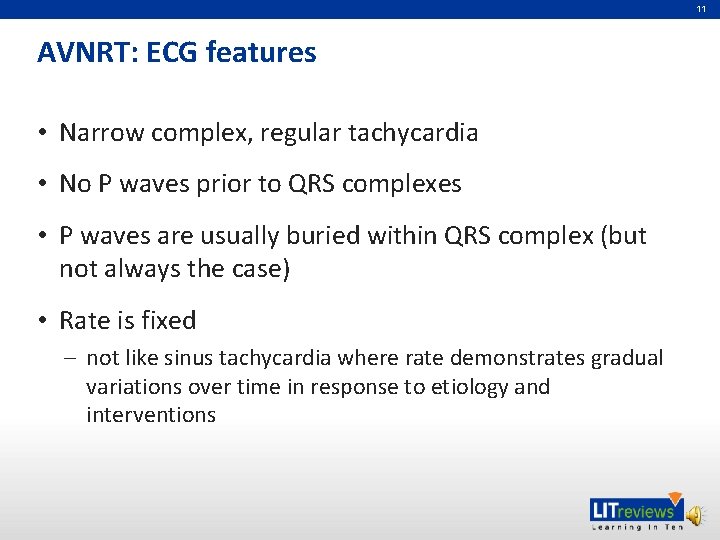
12 AVNRT ECGs
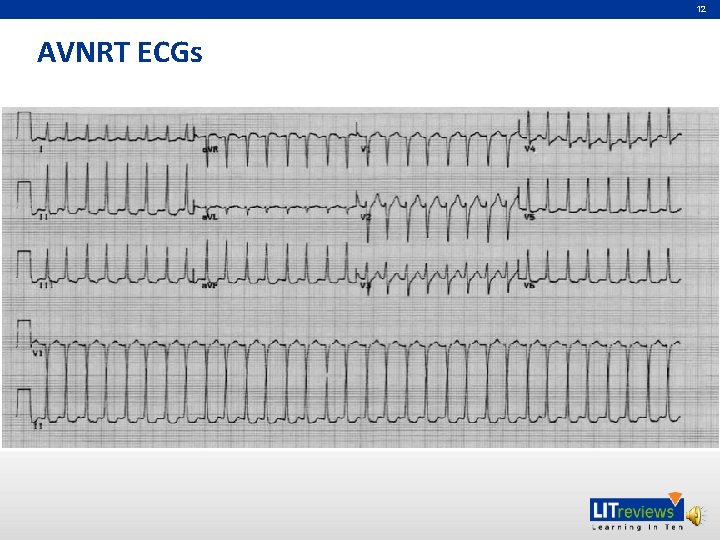
13 AVRT
14 AVRT: ECG features • Narrow complex, regular tachycardia • P wave likely visible on ECG and displaced/retrograde to QRS (may not be present all the time) • Otherwise features similar to AVNRT difficult to tell apart on ECG can only definitively diagnose with electrophysiology studies
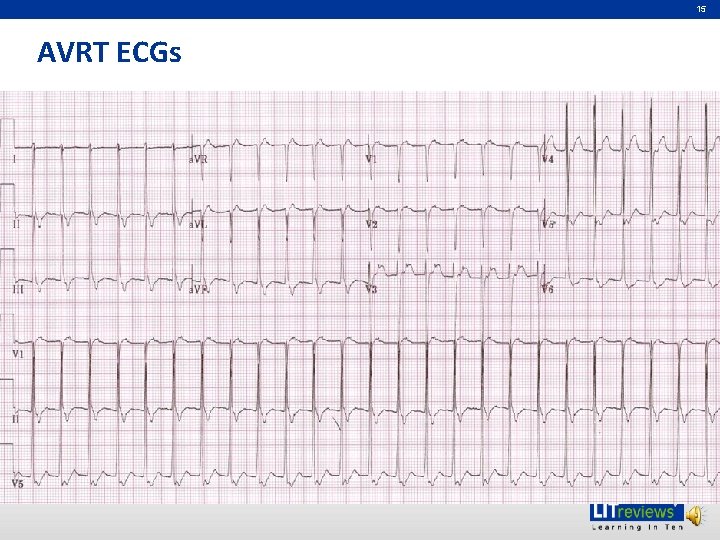
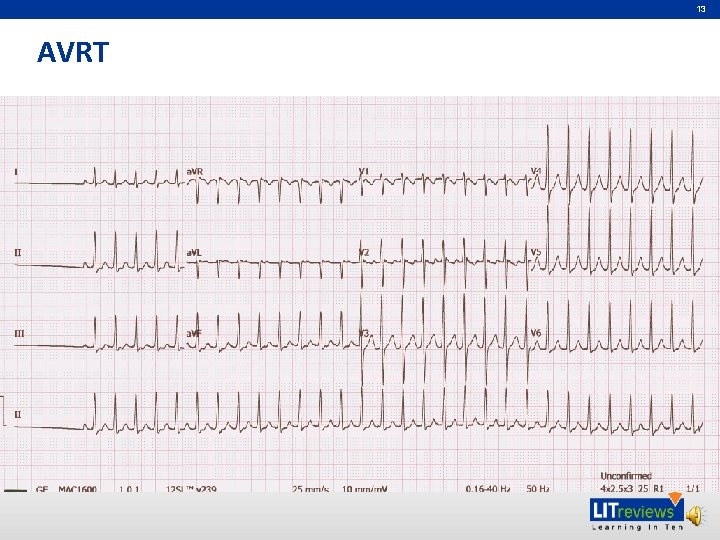
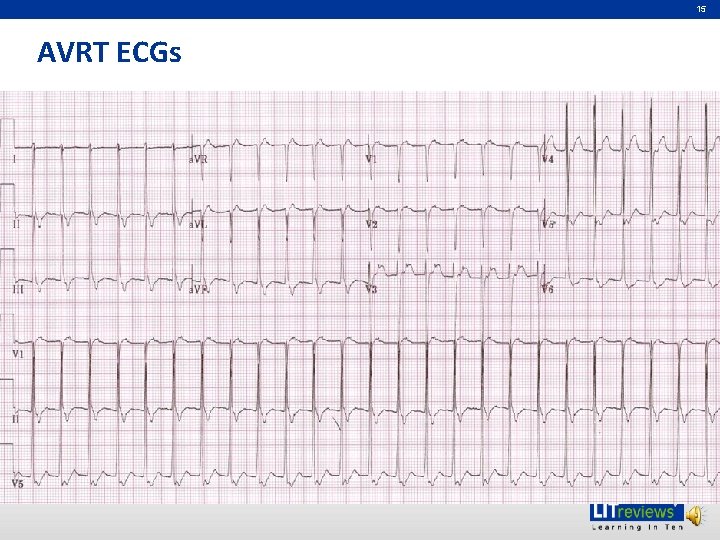
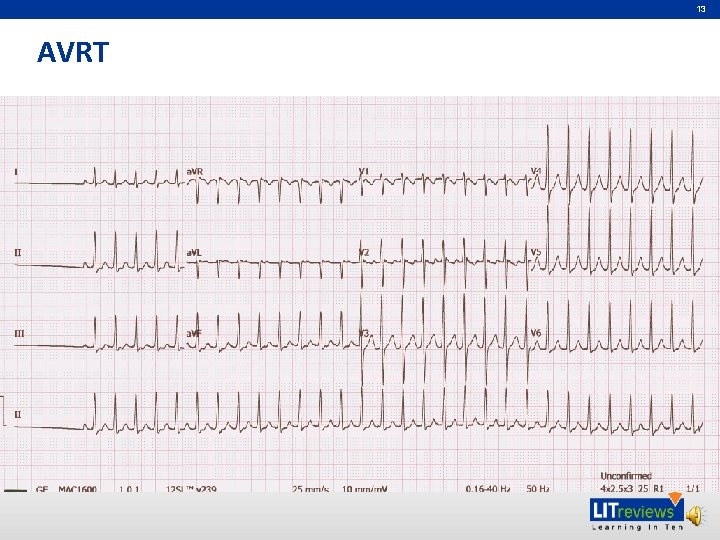
15 AVRT ECGs
16 Management Principles • Assessment of patient • Treating the rhythm • Disposition of patient
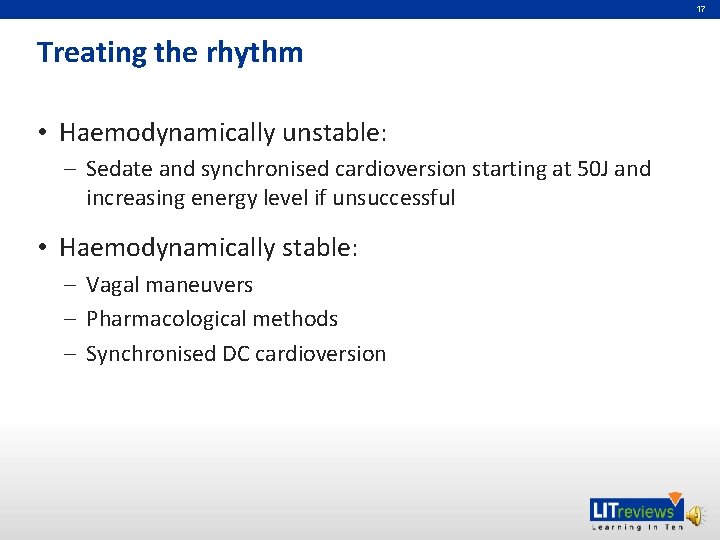
17 Treating the rhythm • Haemodynamically unstable: – Sedate and synchronised cardioversion starting at 50 J and increasing energy level if unsuccessful • Haemodynamically stable: – Vagal maneuvers – Pharmacological methods – Synchronised DC cardioversion
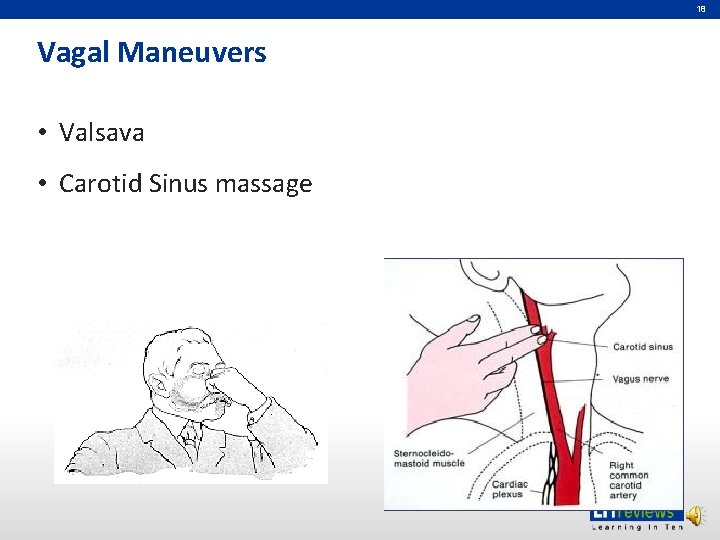
18 Vagal Maneuvers • Valsava • Carotid Sinus massage
19 Pharmacologic Methods • AV nodal blocking agents – Adenosine – Calcium channel blockers like verapamil or diltiazem • Asscessory pathway blocking agents – Procainamide • Other agents – Amiodarone
20 Brief note about Adenosine • Most commonly used drug to abort SVTs • Very short half-life < 10 seconds • Given as a fast bolus via a large peripheral cannular in the cubital fossa followed immediately by a saline flush • Start with IV 6 mg bolus followed by another 12 mg and another 12 mg bolus if unsuccessful • Can be both diagnostic and theraputic
21 Disposition • Observe in ED for period of about 2 -4 hours • Repeat ECG to ensure in NSR • Follow up with cardiology for further electrophysiology studies • Patient education
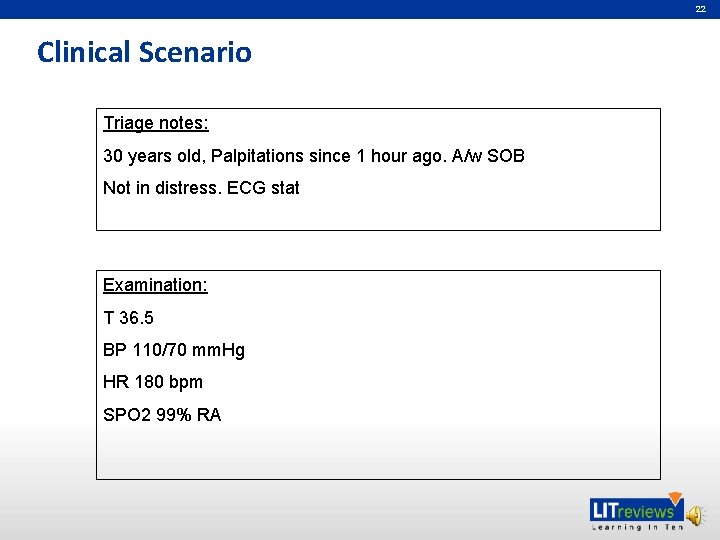
22 Clinical Scenario Triage notes: 30 years old, Palpitations since 1 hour ago. A/w SOB Not in distress. ECG stat Examination: T 36. 5 BP 110/70 mm. Hg HR 180 bpm SPO 2 99% RA
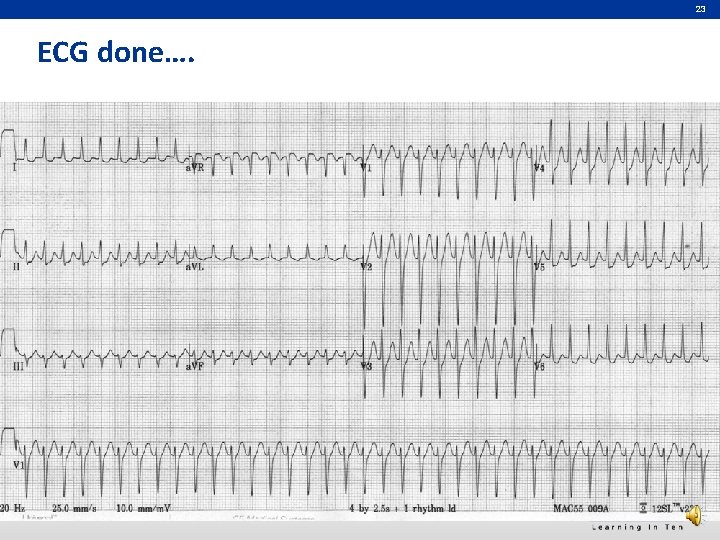
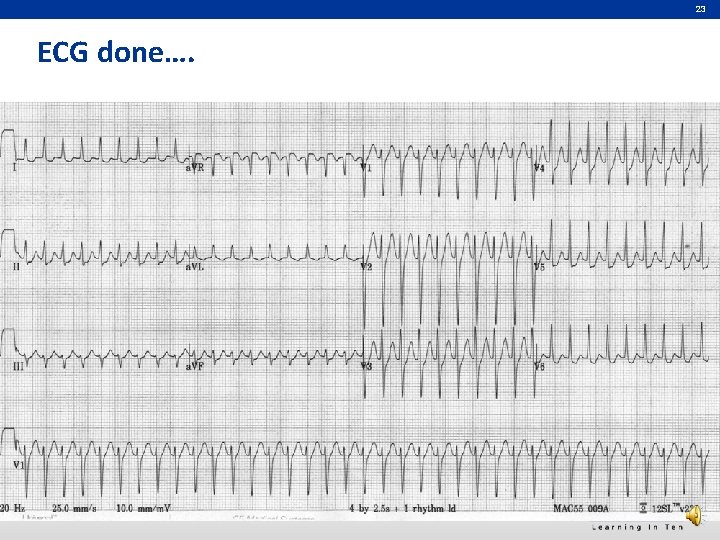
23 ECG done….
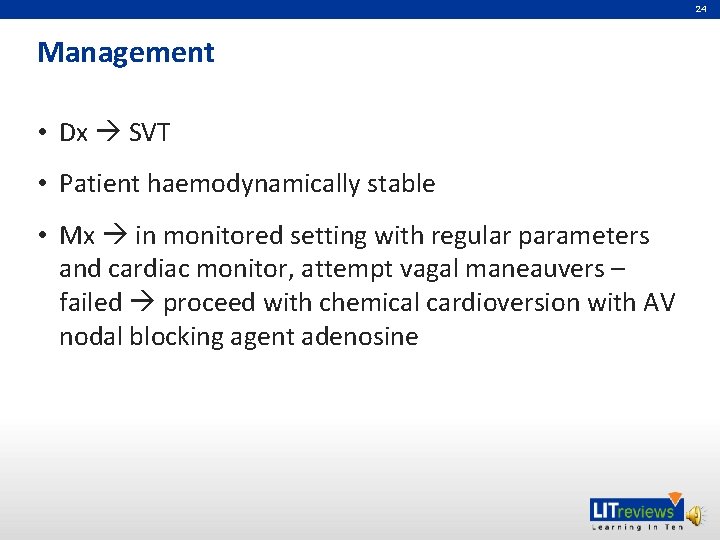
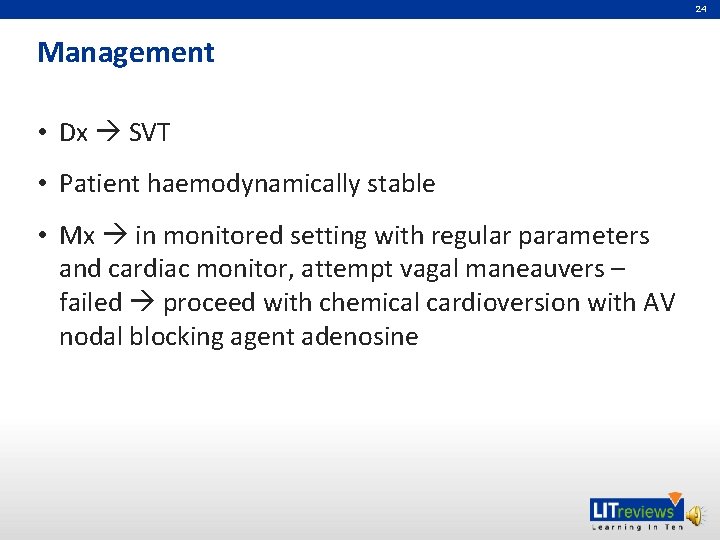
24 Management • Dx SVT • Patient haemodynamically stable • Mx in monitored setting with regular parameters and cardiac monitor, attempt vagal maneauvers – failed proceed with chemical cardioversion with AV nodal blocking agent adenosine
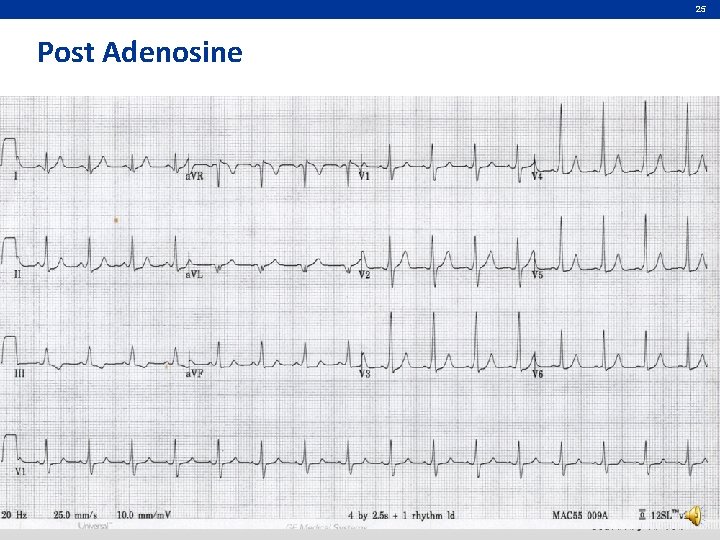
25 Post Adenosine
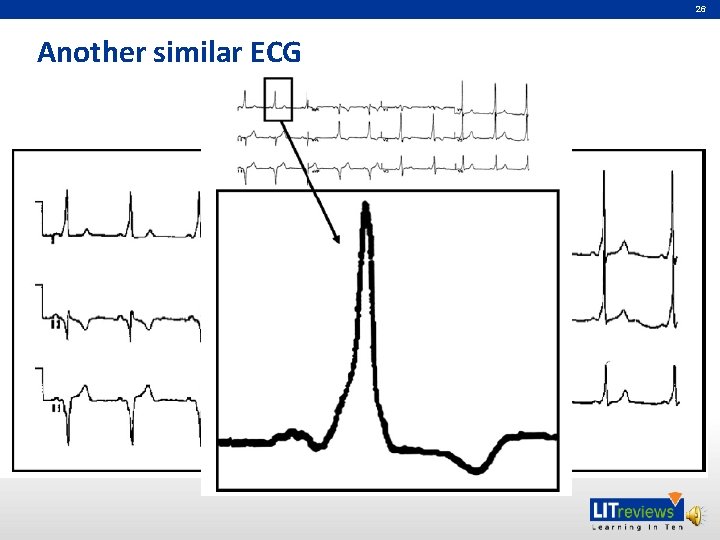
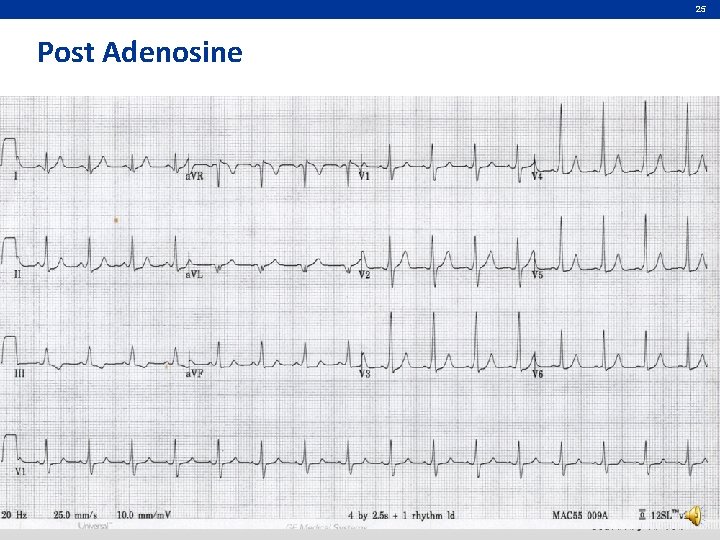
26 Another similar ECG
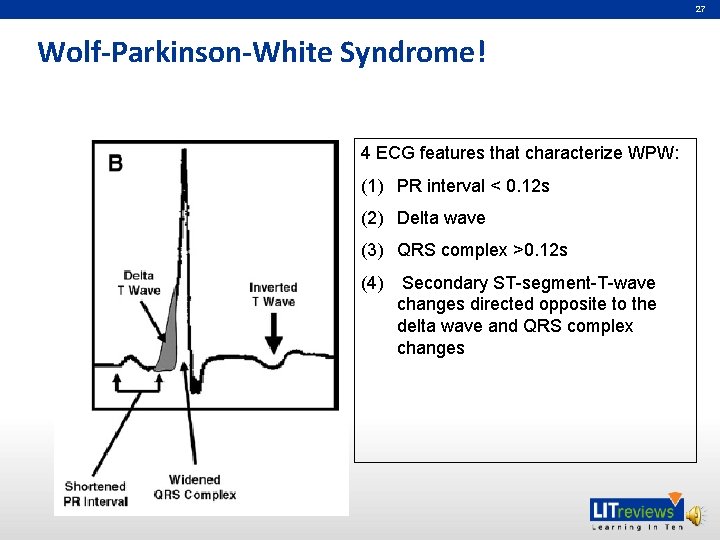
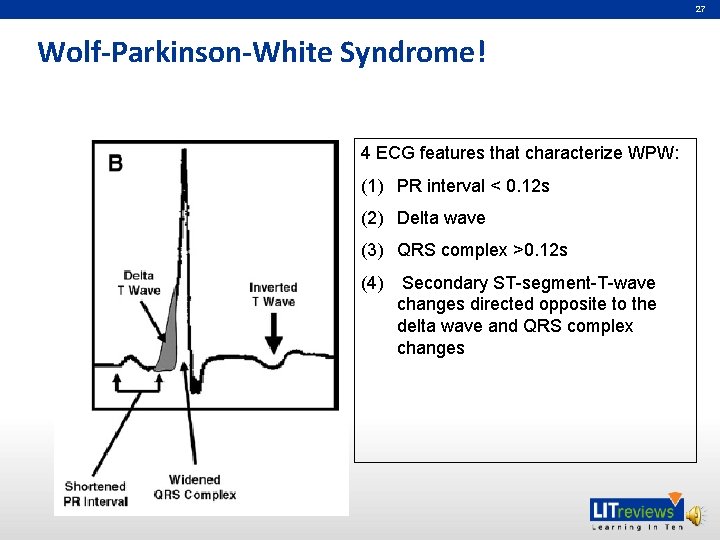
27 Wolf-Parkinson-White Syndrome! 4 ECG features that characterize WPW: (1) PR interval < 0. 12 s (2) Delta wave (3) QRS complex >0. 12 s (4) Secondary ST-segment-T-wave changes directed opposite to the delta wave and QRS complex changes
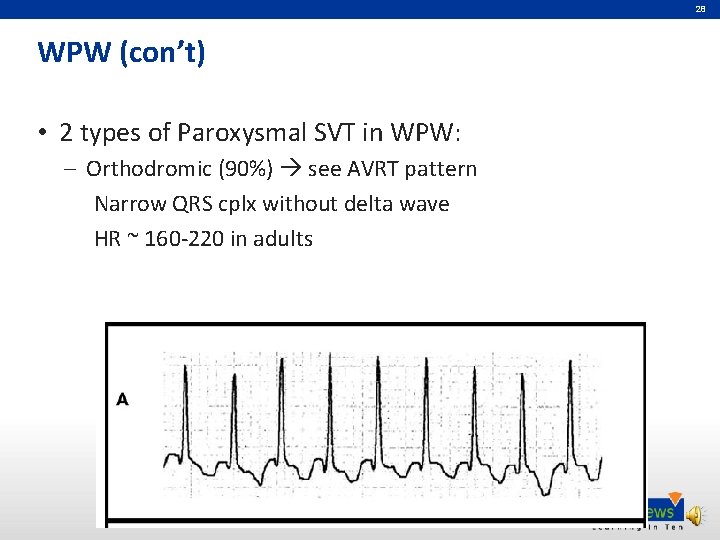
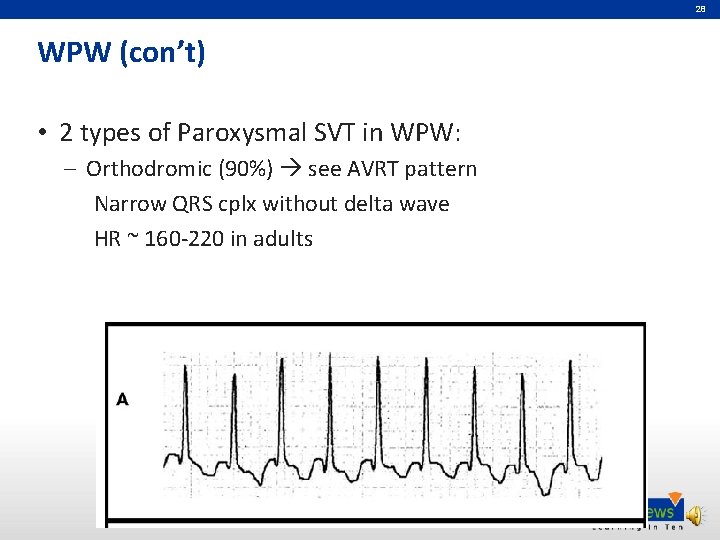
28 WPW (con’t) • 2 types of Paroxysmal SVT in WPW: – Orthodromic (90%) see AVRT pattern Narrow QRS cplx without delta wave HR ~ 160 -220 in adults
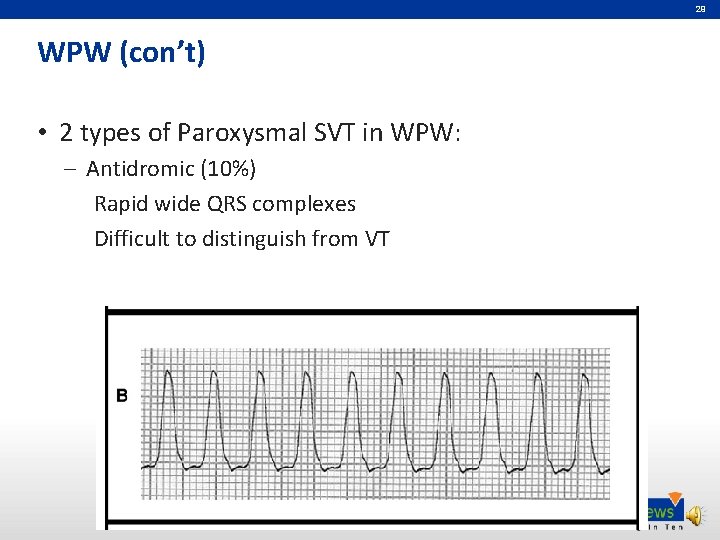
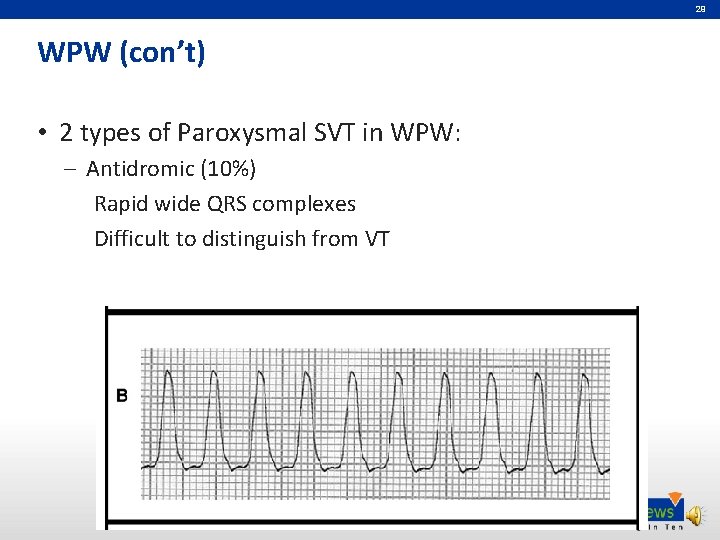
29 WPW (con’t) • 2 types of Paroxysmal SVT in WPW: – Antidromic (10%) Rapid wide QRS complexes Difficult to distinguish from VT
30 WPW (con’t) Back to the pt… • Electrophysiologic study showed accessory pathway with retrograde conduction properties • Underwent transcatheter radiofrequency ablation • Well on follow up
31 Take home messages • SYNCHRONISED CARDIOVERSION for all unstable patients with SVT • Refer patient cardiologist for electrophysiologic studies • Patient education is important!
32 References • Sarah AS, Robert C. Tachydysrhythmias, Emerg Med Cli N Am 24 (2006) 11 -40 • Jacqueline D, Christopher H, Amal M, William J. The electrocardiogram in the patient with syncope, American Journal of Emergency Medicine (2007) 25, 688– 701

Partners in Academic Medicine