Supporting Psychological Well Being in Your Organisation Dr
Supporting Psychological Well. Being in Your Organisation Dr Petra Corr Clinical Director Psychological Services and Head of Occupational Health NHSCT

‘I don’t think we’re in Kansas anymore …’
Supporting the Well-being Needs of our Health and Social Care Staff during COVID-19: A Framework for Leaders and Managers
Leadership Framework • • • Value based Principles approach Phases of pandemic and staff response Helpful Organisational Responses Useful Resources
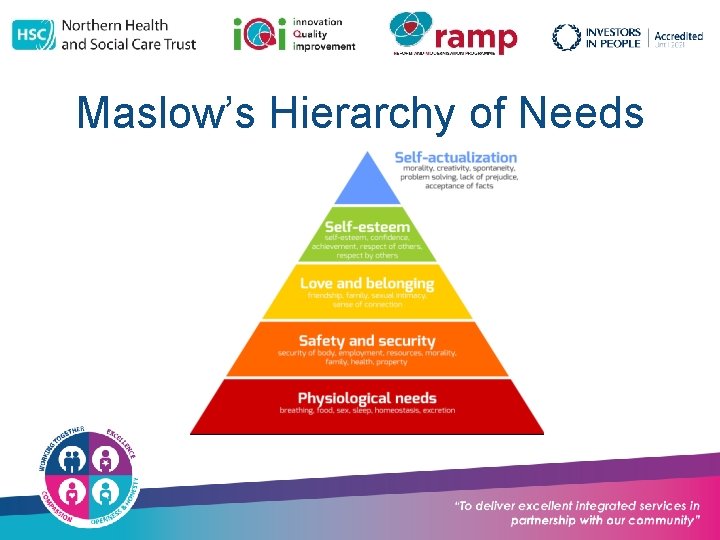
Maslow’s Hierarchy of Needs
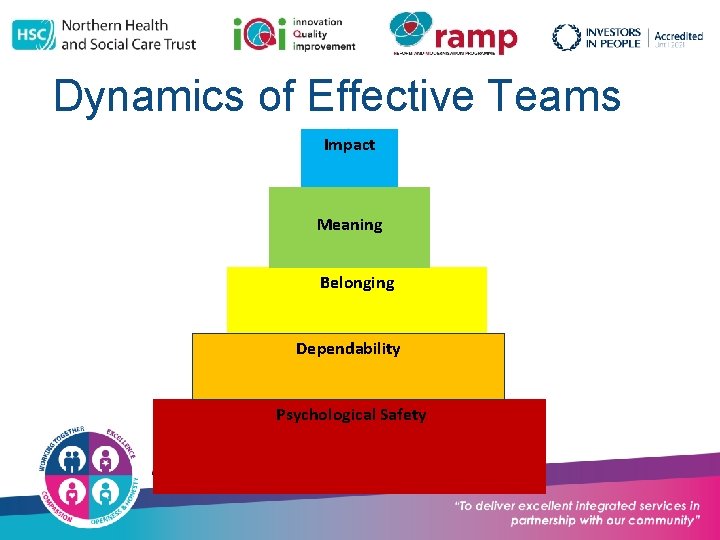
Dynamics of Effective Teams Impact Meaning Belonging Dependability Psychological Safety
Key Elements of Team Resilience • Psychological Safety and Dependability • Belonging • Meaning and Impact
Does Psychological Safety Matter? ‘As long as there is uncertainty and interdependence, psychological safety will be important. ’ (Edmondson, 2016)
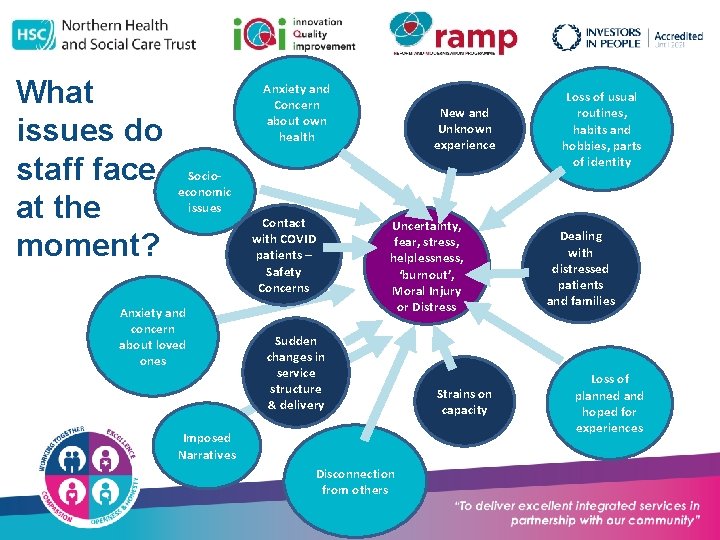
What issues do staff face at the moment? Anxiety and Concern about own health Socioeconomic issues Anxiety and concern about loved ones Contact with COVID patients – Safety Concerns New and Unknown experience Uncertainty, fear, stress, helplessness, ‘burnout’, Moral Injury or Distress Sudden changes in service structure & delivery Imposed Narratives Disconnection from others Strains on capacity Loss of usual routines, habits and hobbies, parts of identity Dealing with distressed patients and families Loss of planned and hoped for experiences
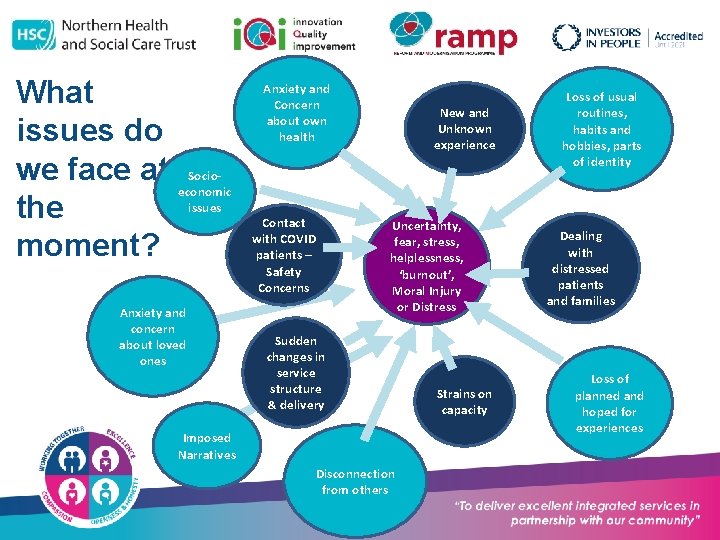
What issues do we face at Socioeconomic issues the moment? Anxiety and concern about loved ones Anxiety and Concern about own health Contact with COVID patients – Safety Concerns New and Unknown experience Uncertainty, fear, stress, helplessness, ‘burnout’, Moral Injury or Distress Sudden changes in service structure & delivery Imposed Narratives Disconnection from others Strains on capacity Loss of usual routines, habits and hobbies, parts of identity Dealing with distressed patients and families Loss of planned and hoped for experiences
What are you having to do (or not do) that is different for you? What are you finding most challenging? How is it for you to be managing this? How are you resourcing yourself?
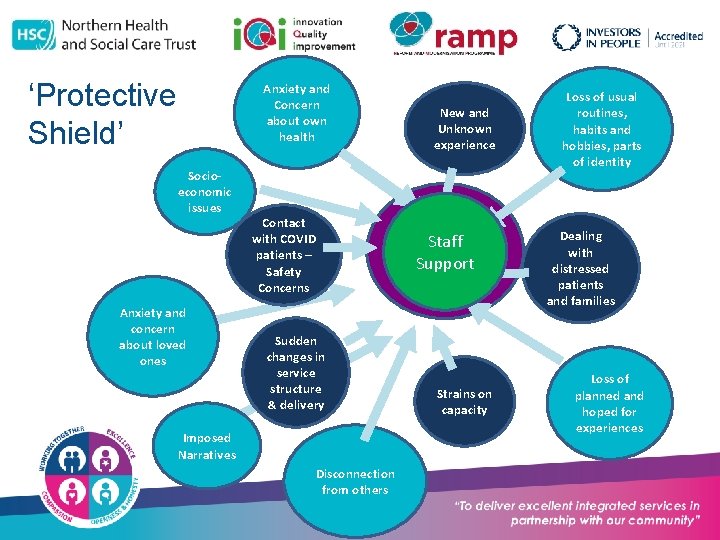
‘Protective Shield’ Anxiety and Concern about own health Socioeconomic issues Anxiety and concern about loved ones Contact with COVID patients – Safety Concerns Sudden changes in service structure & delivery Imposed Narratives Disconnection from others New and Unknown experience Uncertainty, fear, stress, Staff helplessness, Support ‘burnout’, Moral Injury or Distress Strains on capacity Loss of usual routines, habits and hobbies, parts of identity Dealing with distressed patients and families Loss of planned and hoped for experiences
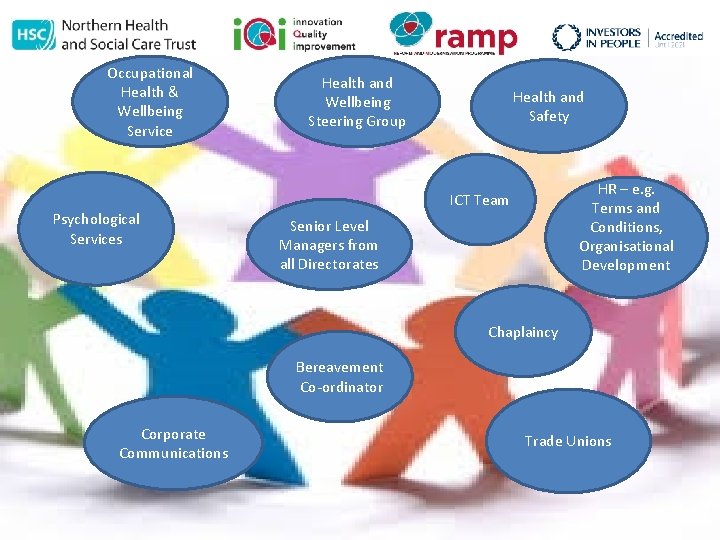
Occupational Health & Wellbeing Service Health and Wellbeing Steering Group Health and Safety HR – e. g. Terms and Conditions, Organisational Development ICT Team Psychological Services Senior Level Managers from all Directorates Chaplaincy Bereavement Co-ordinator Corporate Communications Trade Unions
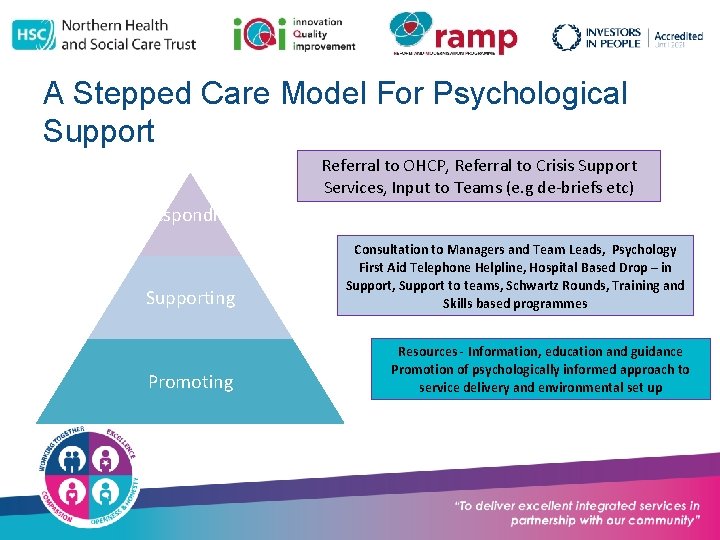
A Stepped Care Model For Psychological Support Referral to OHCP, Referral to Crisis Support Services, Input to Teams (e. g de-briefs etc) Responding Supporting Promoting Consultation to Managers and Team Leads, Psychology First Aid Telephone Helpline, Hospital Based Drop – in Support, Support to teams, Schwartz Rounds, Training and Skills based programmes Resources - Information, education and guidance Promotion of psychologically informed approach to service delivery and environmental set up
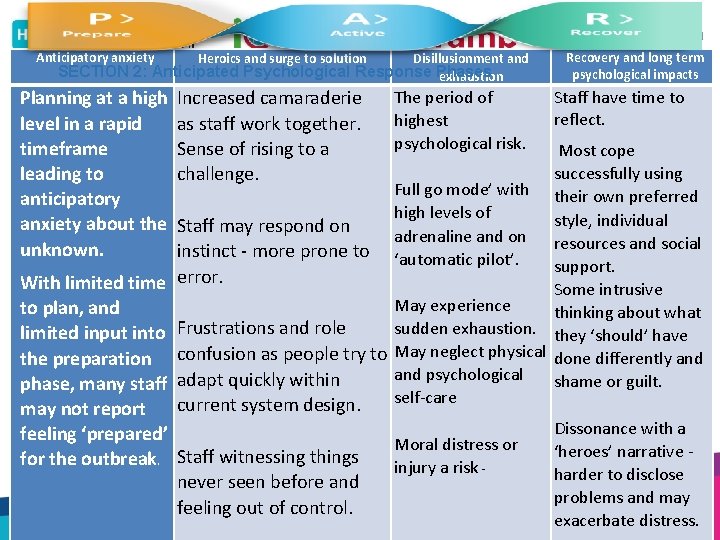
Anticipatory anxiety Disillusionment and SECTION 2: Anticipated Psychological Response Phases exhaustion Planning at a high level in a rapid timeframe leading to anticipatory anxiety about the unknown. With limited time to plan, and limited input into the preparation phase, many staff may not report feeling ‘prepared’ for the outbreak. Heroics and surge to solution Increased camaraderie as staff work together. Sense of rising to a challenge. The period of highest psychological risk. Recovery and long term psychological impacts Staff have time to reflect. Most cope successfully using Full go mode’ with their own preferred high levels of style, individual Staff may respond on adrenaline and on resources and social instinct - more prone to ‘automatic pilot’. support. error. Some intrusive May experience thinking about what sudden exhaustion. they ‘should’ have Frustrations and role confusion as people try to May neglect physical done differently and psychological adapt quickly within shame or guilt. self-care current system design. Dissonance with a Moral distress or ‘heroes’ narrative Staff witnessing things injury a risk harder to disclose never seen before and problems and may feeling out of control. exacerbate distress.
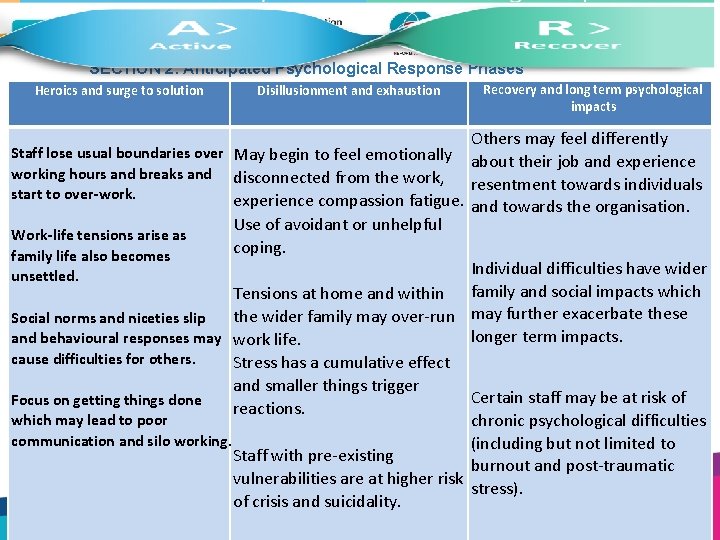
SECTION 2: Anticipated Psychological Response Phases Heroics and surge to solution Disillusionment and exhaustion Recovery and long term psychological impacts Others may feel differently Staff lose usual boundaries over May begin to feel emotionally about their job and experience working hours and breaks and disconnected from the work, resentment towards individuals start to over-work. experience compassion fatigue. Work-life tensions arise as family life also becomes unsettled. Use of avoidant or unhelpful coping. and towards the organisation. Individual difficulties have wider Tensions at home and within family and social impacts which the wider family may over-run may further exacerbate these Social norms and niceties slip longer term impacts. and behavioural responses may work life. cause difficulties for others. Stress has a cumulative effect and smaller things trigger Certain staff may be at risk of Focus on getting things done reactions. which may lead to poor chronic psychological difficulties communication and silo working. (including but not limited to Staff with pre-existing burnout and post-traumatic vulnerabilities are at higher risk stress). of crisis and suicidality.
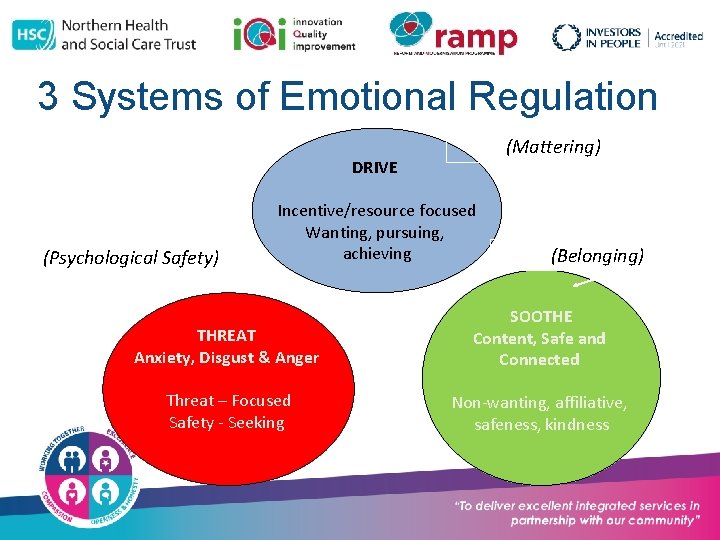
3 Systems of Emotional Regulation (Mattering) DRIVE (Psychological Safety) Incentive/resource focused Wanting, pursuing, achieving (Belonging) THREAT Anxiety, Disgust & Anger SOOTHE Content, Safe and Connected Threat – Focused Safety - Seeking Non-wanting, affiliative, safeness, kindness

What does this tell us? • At times of change and uncertainty, we are driven to try and feel safe – to survive • This drive to survive over-rides all other concerns • The way we (and others) behave often reflects this drive. • Safety – Belonging – Mattering become even more important

What You Can Do: Leadership Framework • • Visible Leadership Have a communication strategy Human connection and peer support Physical Safety Needs Normalise psychological reactions Support wellbeing in stepped ways Psychological care to patients and families Take care of yourself
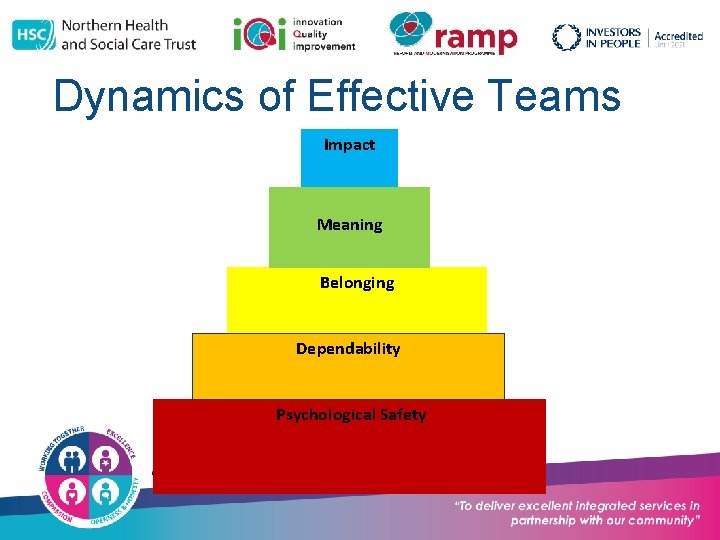
Dynamics of Effective Teams Impact Meaning Belonging Dependability Psychological Safety
Building Psychological Safety • Frame difficulties as challenges • Acknowledge own fallibility and uncertainties • Model curiosity and interest
Building Belonging ‘When front line employees feel a sense of ownership, results show a 70% success rate for transformation programmes. If they are allowed the initiative to drive the change that rate increases to 79%’ (Mc. Kinsey 2011)
Creating Meaning
LOOKING AFTER THE LEADER ‘Before you can start to lead others, you must first know how to lead yourself’
As a Leader … • Deal with complex and uncertain situations • While managing your own emotions and actions • Inspiring and motivating those around you • While managing emotions and actions of others • While appearing calm and in control • And remain authentic
When This Falls Apart • Risks for own health and well-being • Risks for performance • Risks for relationships with others • ALL OF WHICH ARE VITAL TO THE ROLE
Thriving as a Leader • Self – Awareness (recognising what’s there) • Self – Connection (recognising what matters) • Self – Compassion (recognising you’re human) • Self – Care (recognising what helps)
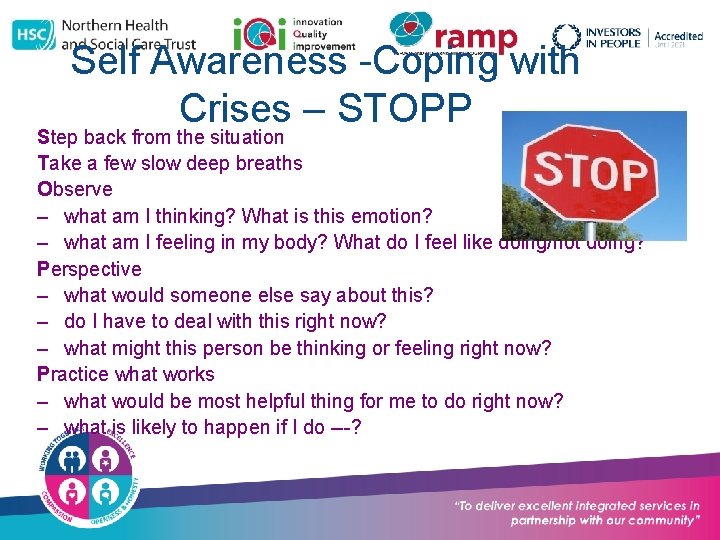
Self Awareness -Coping with Crises – STOPP Step back from the situation Take a few slow deep breaths Observe – what am I thinking? What is this emotion? – what am I feeling in my body? What do I feel like doing/not doing? Perspective – what would someone else say about this? – do I have to deal with this right now? – what might this person be thinking or feeling right now? Practice what works – what would be most helpful thing for me to do right now? – what is likely to happen if I do ---?
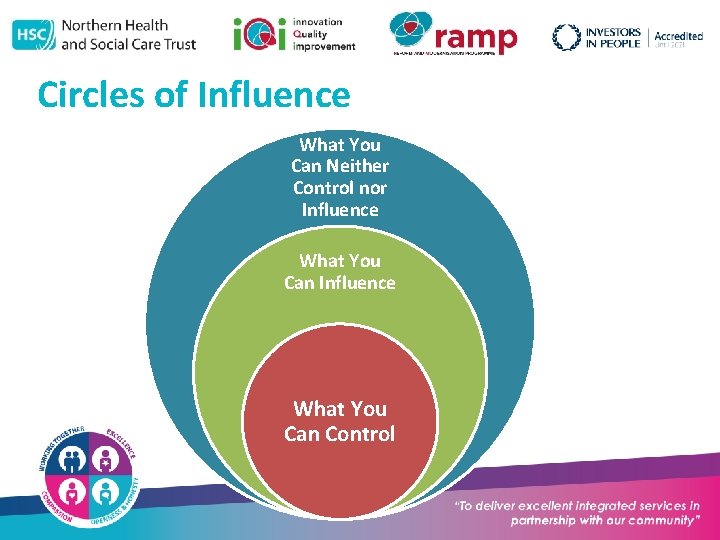
Circles of Influence What You Can Neither Control nor Influence What You Can Control
Self Connection • Connect to values • Connect to priorities
31 Self – Compassion ‘Be careful how you talk to yourself because you are listening’. Lisa M Hayes
Self - Care

The role of others • Be aware of support available Ø Talking with colleagues can alleviates stress, complaining reinforces it! Ø Formal support eg. Counselling Ø Informal support eg. friends, family, Ø groups
Useful Resources Link to PHA website and resources • www. publichealth. hscni. net/covid-19 coronavirus/guidance-hsc-staff/staff-health-andwellbeing Link to framework documents • www. publichealth. hscni. net/sites/default/files/202004/HSC_Regional%20 Staff%20 Wellbeing%20 Frame work. pdf •
- Slides: 35