Supporting our patients to become more activated and

Supporting our patients to become more activated and engaged 6 th December 2016 1

Welcome and setting the scene Alison Manson 2
“The definition of insanity is doing the same thing over and over again and expecting different results” Albert Einstein
4
In pairs discuss what you do on a daily basis that supports your patients to feel confident to self care 5
On a scale of 1 -10 how ‘activated’ are the majority of your patients currently? 6
Are we measuring what really matters? “People crave a life not a service” The care we provide is a means to this end
Outcomes for people not pathways
Another way to look at it 9

The ambition for Nottingham City Life Improver Score 10
There is something in human nature that resists being coerced and told what to do. Ironically, it is acknowledging the other’s right and freedom not to change that sometimes makes change possible. Rollnick S, Miller WR, Butler CC. Motivational interviewing in healthcare. Helping patients change behaviour. New York: Guilford Press (2008).
By the end of our session you will: • Understand why some patients are relatively easy to work with and others much more challenging • Have clearer insight that shows you where your patients are currently • Thought about how and where to use motivational interviewing and the stages of change • Know that ambivalence about changing is natural and develop some techniques on how to work with this • Started to think about how we can respond constructively when a person is 'resistant’ or ‘stuck’ – and know what to examine in our own practice when this happens • Thought about some ideas on how we might deliver care in a different way 12

It’s not WHAT we know it’s how we blend it all together 13
What is Motivational Interviewing (MI) ? “a goal directed, patient-centered counseling style for eliciting behavior change by helping people to explore and resolve ambivalence” (Miller & Rollnick, 2002) In pairs jot down on a post-it what this means to you 14
15
Motivational Interviewing • Model of skills and techniques to help patients take more control and change • Person centred, directive and non confrontational • Uses reframing and silence to reveal: – Individual personal strengths – Discrepancy between stated goals /values and behaviours 16
Benefits of MI • Minimises resistance • Creates discrepancy and builds on discrepancy between goals and current behaviour (from patient’s perspective) • Explores and resolves ambivalence • Elicits “change talk” • Sets in motion the patients change potential and activates change 17
Before we start a word about Ambivalence Me ambivalent ? …. Well yes and no 18

So what do we mean by Ambivalence • Having mixed (or opposite) feelings thoughts about the same thing • Simultaneous conflicting feelings • Being in two minds about something Need to change VERSUS the reality

Ambivalent? 20
Ambivalence Stuck in the middle • Having inconsistent beliefs is a normal process and we all have them • If ambivalence is being expressed there is something to work with • Resistance (arguing, interrupting, blaming others, ‘yes buts’, voting with feet) should be expected & part of the process 21
Techniques for resolving ambivalence • • Ask open ended questions Affirm patients autonomy Reflective listening Summarise conversation 22
23
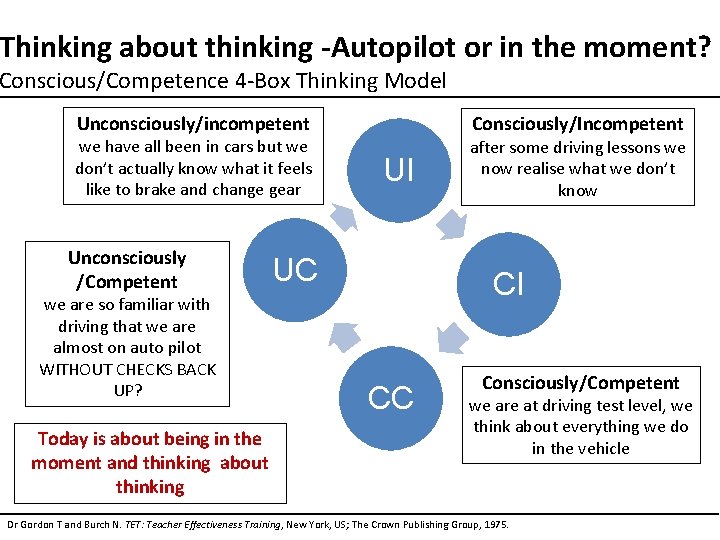
Thinking about thinking -Autopilot or in the moment? Conscious/Competence 4 -Box Thinking Model Unconsciously/incompetent we have all been in cars but we don’t actually know what it feels like to brake and change gear Unconsciously /Competent we are so familiar with driving that we are almost on auto pilot WITHOUT CHECKS BACK UP? Today is about being in the moment and thinking about thinking Consciously/Incompetent UI UC after some driving lessons we now realise what we don’t know CI CC Consciously/Competent we are at driving test level, we think about everything we do in the vehicle Dr Gordon T and Burch N. TET: Teacher Effectiveness Training, New York, US; The Crown Publishing Group, 1975.
Reflection exercise The ‘problem patient’ …. . Write about a behaviour/problem you’d like to consider making a change to…. & Please don’t share this just yet While writing answer these questions on your worksheet 1. What do you think about this behaviour/problem? 2. What do others thinks about it? 3. Do you want to change anything? 4. What do you want to change but don’t…. 25
Motivational Interviewing – a different approach Task led is what we will do – INPUTS Patient led - what are you trying to achieve – OUTCOMES Process led structured approach – you may already be doing this! 26
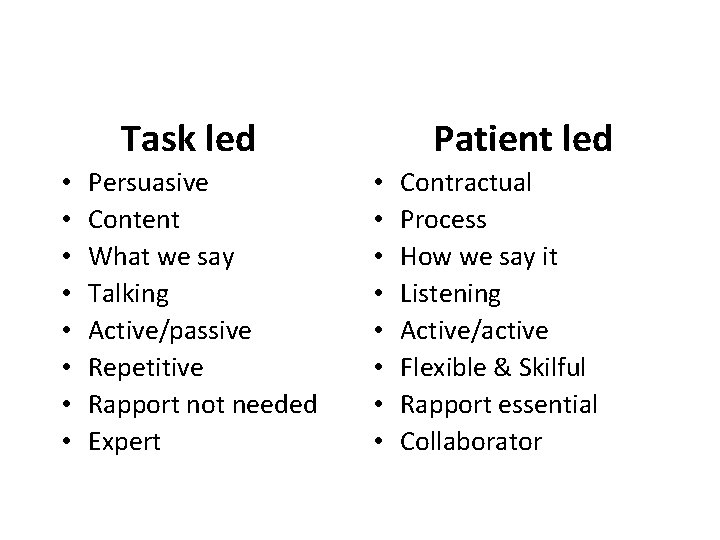
Task led • • Persuasive Content What we say Talking Active/passive Repetitive Rapport not needed Expert Patient led • • Contractual Process How we say it Listening Active/active Flexible & Skilful Rapport essential Collaborator
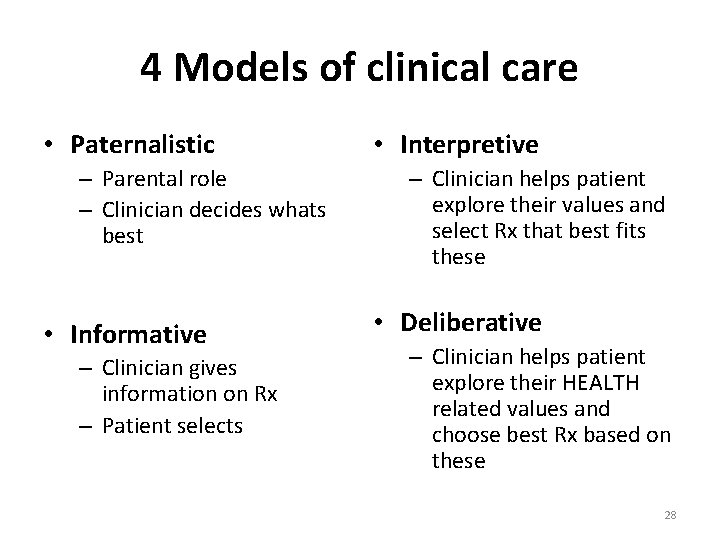
4 Models of clinical care • Paternalistic – Parental role – Clinician decides whats best • Informative – Clinician gives information on Rx – Patient selects • Interpretive – Clinician helps patient explore their values and select Rx that best fits these • Deliberative – Clinician helps patient explore their HEALTH related values and choose best Rx based on these 28
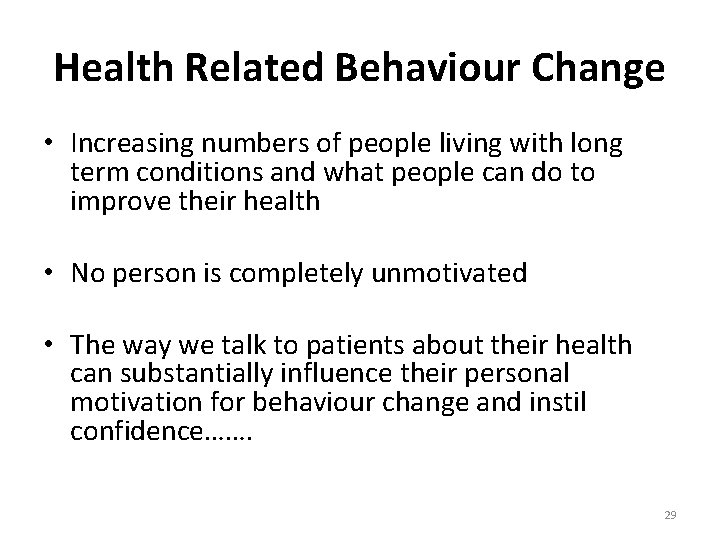
Health Related Behaviour Change • Increasing numbers of people living with long term conditions and what people can do to improve their health • No person is completely unmotivated • The way we talk to patients about their health can substantially influence their personal motivation for behaviour change and instil confidence……. 29
30
The process of change • People change behavior because they are: – Ready – Willing – Able • Change is not linear • Change is most persistent when it is internally motivated 31
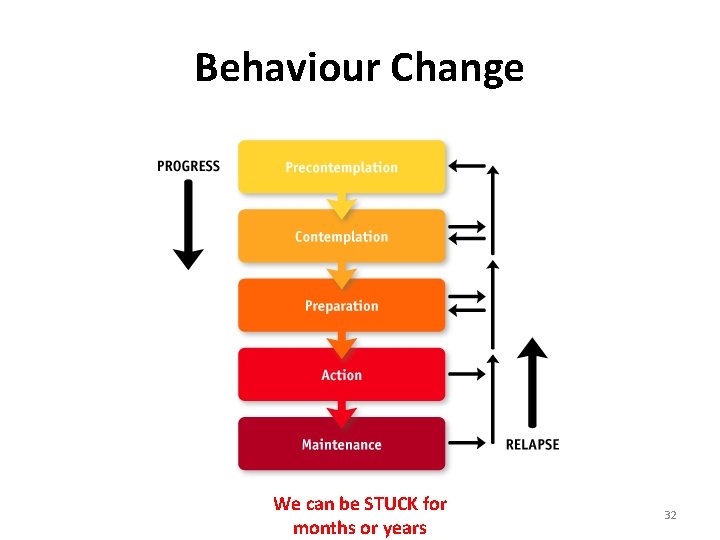
Behaviour Change We can be STUCK for months or years 32
Realities of Change • Change does not occur overnight • Change is a gradual process with occasional setbacks – not an outcome • Thinking and Doing components • Other positives/successes occur 33
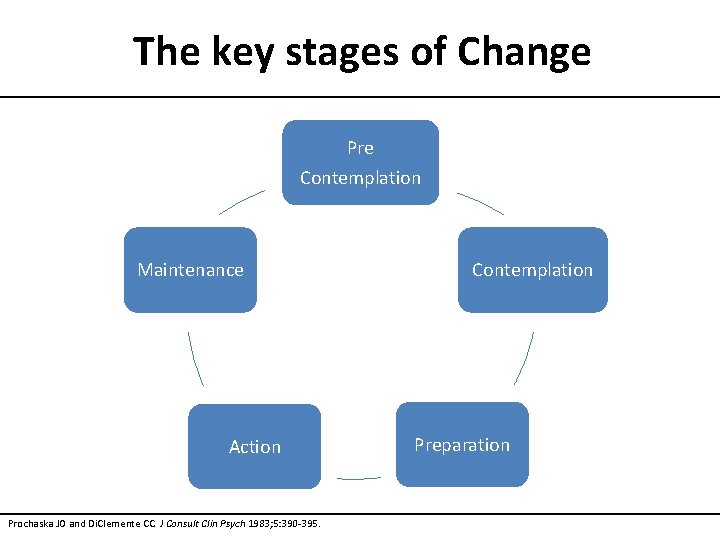
The key stages of Change Pre Contemplation Maintenance Action Prochaska JO and Di. Clemente CC. J Consult Clin Psych 1983; 5: 390 -395. Contemplation Preparation
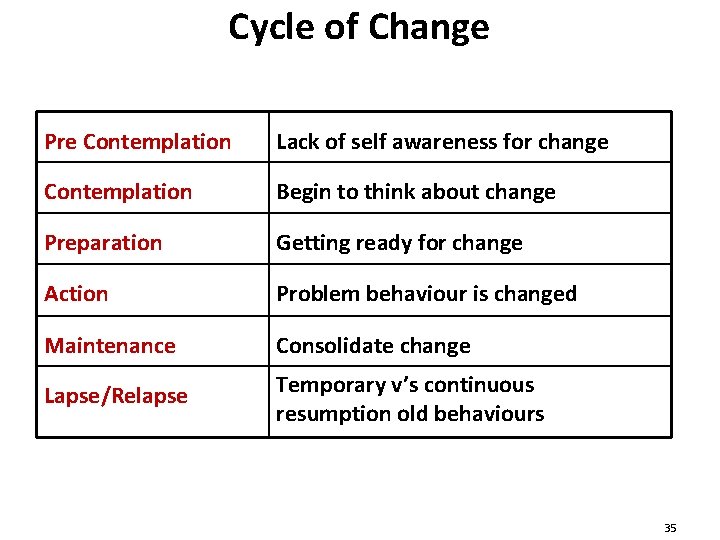
Cycle of Change Pre Contemplation Lack of self awareness for change Contemplation Begin to think about change Preparation Getting ready for change Action Problem behaviour is changed Maintenance Consolidate change Lapse/Relapse Temporary v’s continuous resumption old behaviours 35
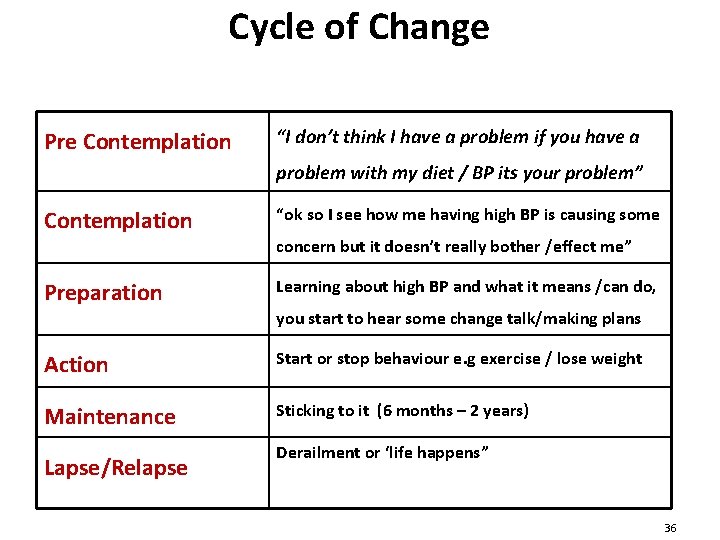
Cycle of Change Pre Contemplation “I don’t think I have a problem if you have a problem with my diet / BP its your problem” Contemplation “ok so I see how me having high BP is causing some concern but it doesn’t really bother /effect me” Preparation Learning about high BP and what it means /can do, you start to hear some change talk/making plans Action Start or stop behaviour e. g exercise / lose weight Maintenance Sticking to it (6 months – 2 years) Lapse/Relapse Derailment or ‘life happens” 36
Reflection exercise Go back to the behaviour/problem you wrote about earlier? Think about where do you consider yourself to be in the cycle of change with your behaviour/problem? Jot some thoughts down 37
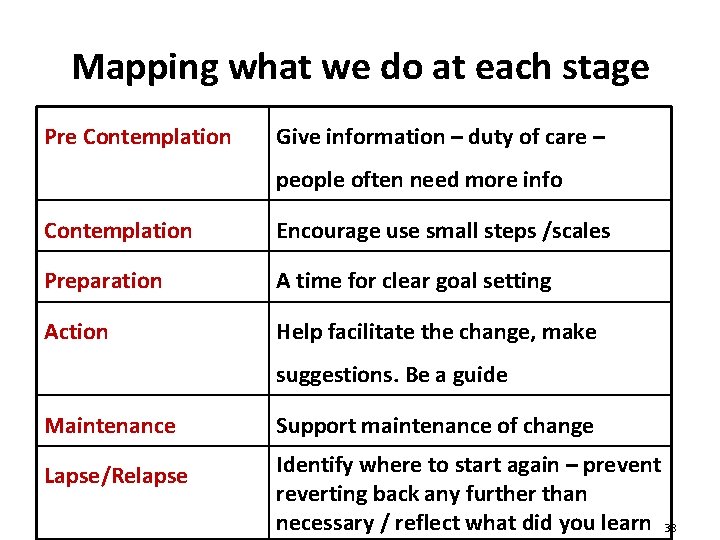
Mapping what we do at each stage Pre Contemplation Give information – duty of care – people often need more info Contemplation Encourage use small steps /scales Preparation A time for clear goal setting Action Help facilitate the change, make suggestions. Be a guide Maintenance Support maintenance of change Lapse/Relapse Identify where to start again – prevent reverting back any further than necessary / reflect what did you learn 38
Features of Stages of Change Model • People can present at any stage • People progress through stages of change • Movement may be forward and/or backward • The model normalises relapse – it is expected! 39
Techniques of MI • Rolling with Resistance - Avoid arguing Open-ended Questions Affirmations Summarise Develop Discrepancy Support Self-Efficacy Empathy 40
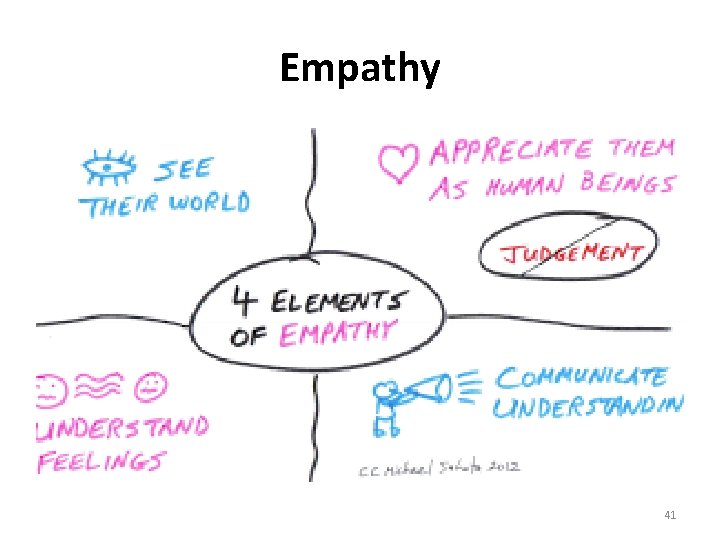
Empathy 41
Insert video Brené Brown on Empathy 42
ARGUMENT INCREASES RESISTANCE
AVOID ARGUMENT AT ALL COSTS • Arguments are counter-productive • MI is in itself challenging and confrontational in that it questions how much the patient wants to change • The goal of MI is to encourage the patient to hear themselves say WHY they want to change, not to keep repeating existing reasons for failing to change • If you don’t seem to be listening actively to the reasons why change for your client is problematic, they will work hard to convince you that these reasons are legitimate and that they are not being neglectful or difficult. This can consolidate their existing thinking and increase their resistance to change
ROLL WITH RESISTANCE When encountering resistance to change, do not confront it directly Reframe it and reflect it in a way that decreases resistance Avoid arguing for change Encountering resistance is a sign you should shift your approach 45
ROLL WITH RESISTANCE Dancing vs. Wrestling Guiding vs. Directing Tapping vs. Pulling Consulting vs. Instructing When you encounter resistance, step back, listen, and try to understand things from the patent’s perspective. 46
DEVELOP DISCREPANCY The patient needs to have goals to work towards and to realise that their current situation has consequences Goals should be generated by the patient and not imposed upon them (SMART goals? ) Check on how realistic these goals are. Can the patient think what might prevent them from being achieved? Can they prioritise them into a hierarchy? Identify the difference between the current and ideal situation. Consider aids such as metaphors to explain the nature of change
Change • Motivation – Why change? • Information – What to change? • Ability/Resources/Effort – How to change? DO WE AS HCP’S GIVE THE RIGHT INFORMATION AT THE RIGHT TIME? 48
CHANGE People say they want to change – yet continue with disruptive behaviour …. – “If you continue with x behaviours what might happen? ” – “How does this …. fit with being well? ” CHANGE EQUATION 49
The Spirit of MI • Collaboration versus Confrontation • Evocation versus Education • Autonomy versus Authority 50

BREAK 51
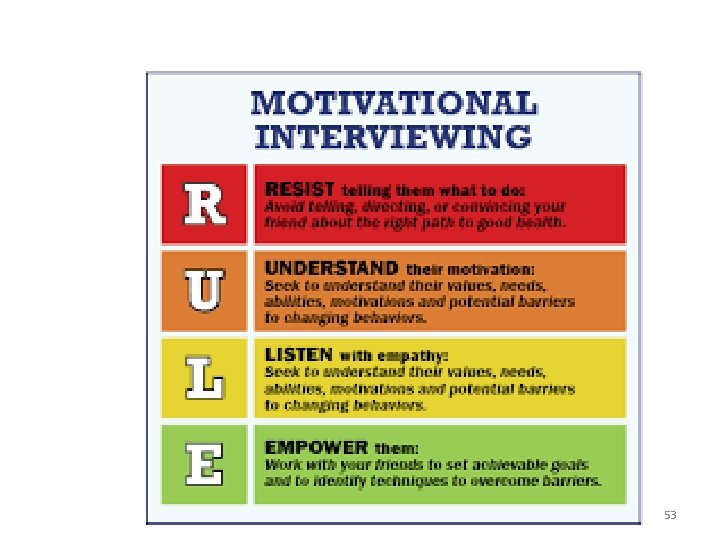
The 4 guiding Principles of Motivational Interviewing • Resist the righting reflex • To understand explore the patient’s own motivation • To listen with empathy • To empower the patient encouraging hope and optimism RULE – Resist, Understand, Listen & Empower 52
53
Principle 1: Resisting the Righting Reflex • We want to make things right • With MI we don’t try to change the patients behaviour • Change comes from the patients intrinsic motivation • To succeed at MI resist the righting reflex – No fixing! 54
Principle 2: Understand the patients motivation to change • Patient’s belief in the possibility of change is an important element of motivation • Client, not you, is responsible for choosing and carrying out change • The why THEY want to change and we must enhance their confidence to change NOTE: Your belief in client’s ability to change becomes a self-fulfilling prophecy 55
Principle 3: Listen to your patient • Listen as much as you inform • Resistance should not be directly opposed • Invite new perspectives but don’t impose them • When it comes to behaviour change, the answers usually always lie within the patient – finding them requires good listening skills 56
Principle 4: Empower your patients • Help patients EXPLORE how they can make difference • Support their hope that such change is possible and can make a difference • Facilitate the conversation – get the patient to think out loud – Change Talk 57
Time to practice Ones are Interviewees; Twos are Interviewers • Interviewee: Pick something in your life that is an issue or a challenge • Nothing will be disclosed about your exchange unless you do the disclosing • We want to know how you felt about the exchange/dialog • Interviewer : Try to solve your partner’s issue by giving pertinent information and advice addressing it. 58
2 nd time around Interviewee: Using the same challenge as before Interviewer: ◦ Assess your interviewee’s stage of change ◦ Listen and reflect without giving unsolicited advise 59
2 nd time around Was there a difference in how the 2 exchanges felt, as an interviewee and as the interviewer? 60

61
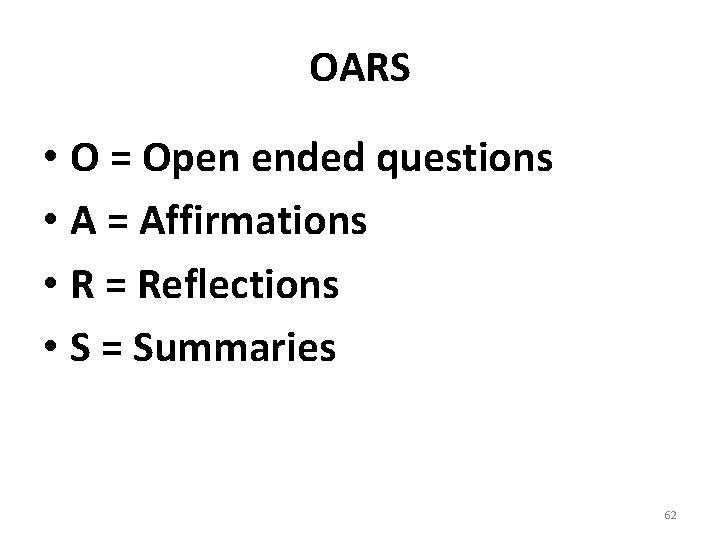
OARS • O = Open ended questions • A = Affirmations • R = Reflections • S = Summaries 62
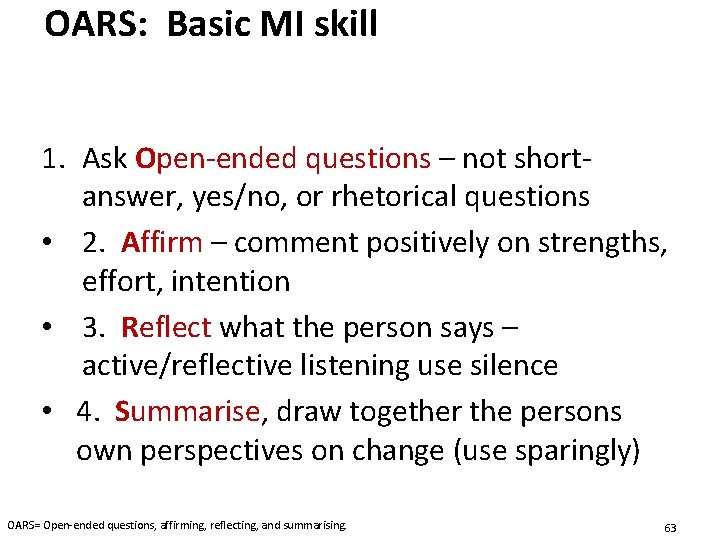
OARS: Basic MI skill 1. Ask Open-ended questions – not shortanswer, yes/no, or rhetorical questions • 2. Affirm – comment positively on strengths, effort, intention • 3. Reflect what the person says – active/reflective listening use silence • 4. Summarise, draw together the persons own perspectives on change (use sparingly) OARS= Open-ended questions, affirming, reflecting, and summarising. 63
Closed to open • • • Did it work as well as you thought it would? Do you think this is helpful? Have you tried this before? Is this easy/hard for you? Do you normally…? 64
Are People Ready to Change? Assessing readiness to change is about • Understanding how important this change is to a client • Understanding how confident this client feels about making a change • It is important that your patients express the arguments FOR change themselves. The technical term in this context is ‘Change Talk’ • 65
Change Talk! Represents movement towards change! Highly influenced by counseling style! A primary vehicle for resolving ambivalence and promoting behavior change! When you hear change talk, just don’t stand there! Reflect, Reinforce, Ask for more & Affirm! 66
Change Talk – Examples Desire: I want to get healthier and feel better Ability: I could lose weight / stop smoking Reasons: I should lose weight / stop smoking because. . Need: I've got to lose weight / stop smoking COMMITMENT to Change: “I will lose weight / stop smoking ” 67
Motivation • Assess: – How important is it for you to change right now? • Improve/Enhance: – Create context: patient’s life goals – Review prior efforts, including lessons from successes and failures – Recognise your lack of power – Acknowledge your lack of power – Identify your patient’s strengths – Promote your patient’s power
Scaling Questions 69
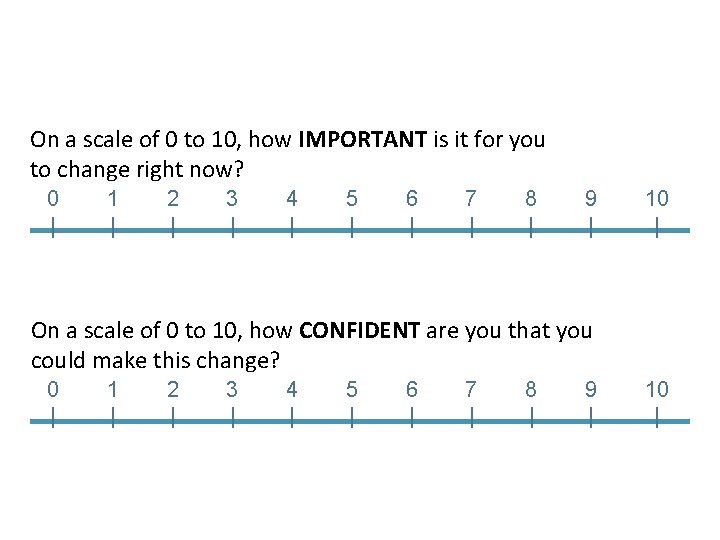
On a scale of 0 to 10, how IMPORTANT is it for you to change right now? 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | On a scale of 0 to 10, how CONFIDENT are you that you could make this change? 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
Building Confidence/Importance • • Do little else… Ask about the score… Brainstorm solutions Reviewing past successes and failure “when in your life have you made up your mind to do something and did it? ” • Review personal strengths and supports “What /who could help you make the change? How? ” • Hypothetical change – in the future “Suppose you did succeed , looking back now …. ” 71
Affirming Statements • Directly affirming a patient can help build rapport and increase confidence • Notice signs of patient’s strengths and efforts and reflect them back • “That seems like a good thing for you to start with as you know how to …” • “I appreciate you taking the big step and coming here” • “You’re clearly a resourceful person to deal with the difficulties you have / way you’ve been feeling for so long” 72
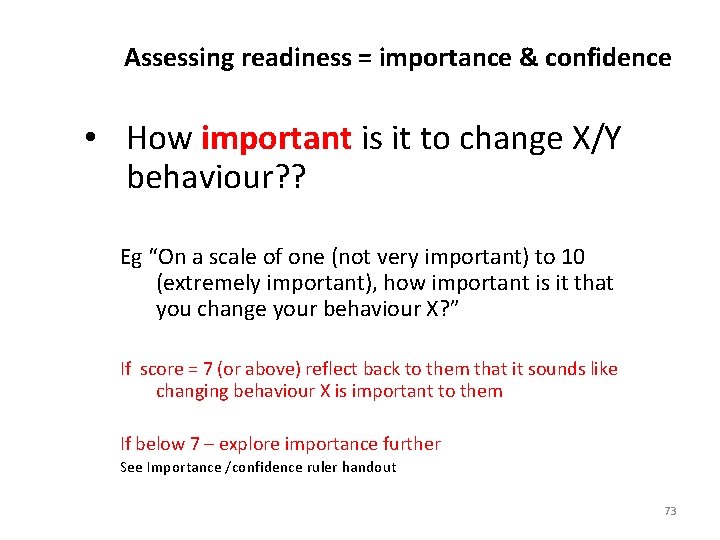
Assessing readiness = importance & confidence • How important is it to change X/Y behaviour? ? Eg “On a scale of one (not very important) to 10 (extremely important), how important is it that you change your behaviour X? ” If score = 7 (or above) reflect back to them that it sounds like changing behaviour X is important to them If below 7 – explore importance further See Importance /confidence ruler handout 73
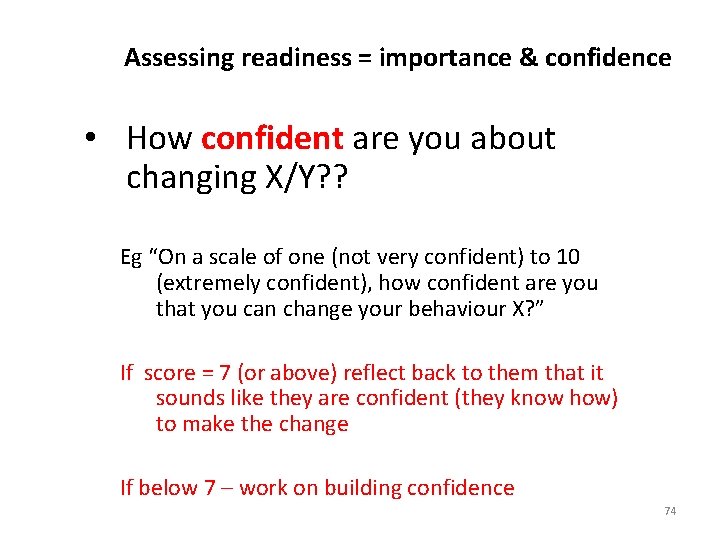
Assessing readiness = importance & confidence • How confident are you about changing X/Y? ? Eg “On a scale of one (not very confident) to 10 (extremely confident), how confident are you that you can change your behaviour X? ” If score = 7 (or above) reflect back to them that it sounds like they are confident (they know how) to make the change If below 7 – work on building confidence 74
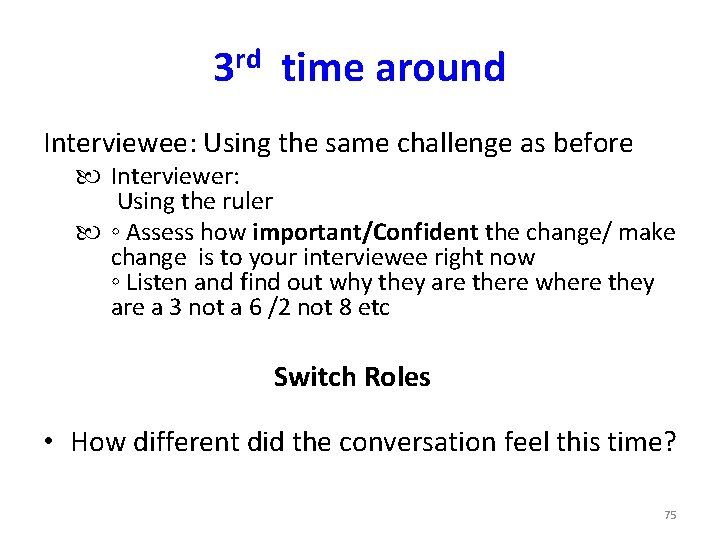
3 rd time around Interviewee: Using the same challenge as before Interviewer: Using the ruler ◦ Assess how important/Confident the change/ make change is to your interviewee right now ◦ Listen and find out why they are there where they are a 3 not a 6 /2 not 8 etc Switch Roles • How different did the conversation feel this time? 75

76

Motivational Interviewing ITS TRULY ABOUT: • CHANGING the nature of the RELATIONSHIP between professionals and patients • CHANGING the balance of POWER between professionals and patients • CHANGING and creating EXPECTATIONS between professionals and patients Write down 2 patients you will try this with in the next 2 weeks …. 77
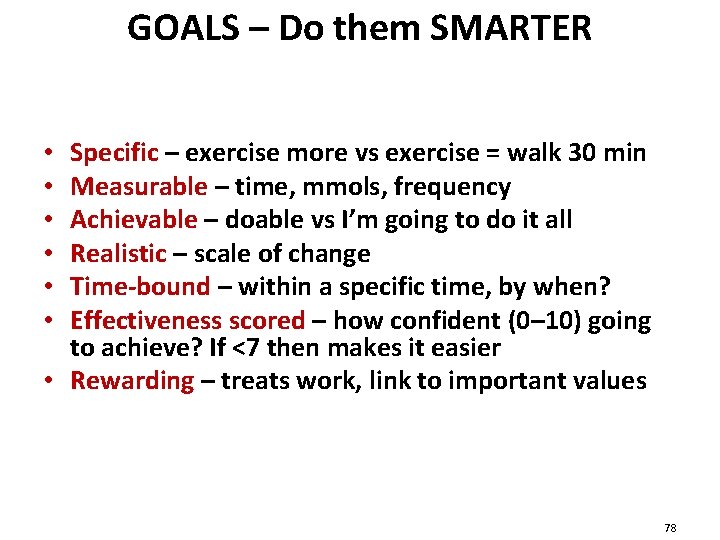
GOALS – Do them SMARTER Specific – exercise more vs exercise = walk 30 min Measurable – time, mmols, frequency Achievable – doable vs I’m going to do it all Realistic – scale of change Time-bound – within a specific time, by when? Effectiveness scored – how confident (0– 10) going to achieve? If <7 then makes it easier • Rewarding – treats work, link to important values • • • 78
This Session Has • Described the concept of motivational interviewing • Discussed interaction techniques and how these can apply to patients and groups • Summarised the potential benefits for healthcare professionals • It’s just the start ….
Further Resources Rollnick, S. , Miller, R. W. & Butler, C. (2008). Motivational interviewing in Health Care. London: Guildford Press Furze, G. , Donnison, J. & Lewin, R. J. P. (2008). The clinician’s guide to chronic disease mangement for long-term conditions: a cognitive behavioural approach. Keswick: M&K Publishing Dunn, C. & Rollnick, S. (2002). Lifestyle change. London: Elsevier Ltd Miller, W. R. , & Rollnick, S. (2002). Motivational interviewing: Preparing people for change. London: Guilford Press. Rollnick, S. , Mason, P. & Butler, C. (1999). Health Behaviour change: a guide for practitioners. London: Churchill Livingston Website: http: //www. motivationalinterview. org/ 80
Thank you for your hard work and interaction today Before you go Can you complete the evaluation form for the CCG 81

Contact details Alison Manson alison@elcworks. co. uk TEL: 07540969876 82
- Slides: 82