Sum Scores Components Scores Chronic Scores Acute Rejection


















- Slides: 49
Sum Scores & Components’ Scores Chronic Scores Acute Rejection Scores Lillian W. Gaber University of Tennessee
Too Many or Less Features to Evaluate • Inclusive but in the mean time selective of the examined lesions • Weigh lesions according to their importance • Simplify the schema • less features to assess • Conspicuous lesions
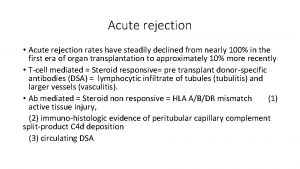
Definitions of Acute Rejection and Clinical Correlation • Mild AR: Mild cellular rejection • Moderate: Cellular rejection with glomerulitis or mild vasculitis • Severe: Extensive & diffuse cellular or vascular rejection and cases with thrombosis, RBC extravasation or necrosis • Irreversible: Extensive necrosis and infarction Banfi et al; 1981

Definitions of Acute Rejection and Clinical Correlation Mild rejection: Interstitial edema and minimal infiltrates Moderate rejection: More extensive infiltrate & evidence of glomerular or vascular changes Severe rejection: the above with necrosis or infarction Finkelstein et al, 1976

Early Studies with Semiquantitative Data • Hsu et al- University of Toronto (1976) – Chronic lesions, fibrinoid vascular deposits and obliterative endarteritis correlate with creatinine rise at 1 -3 mo post biopsy • Klaer et al- Aarhus Denmark (1980) – Glomeurlar or arterial thrombosis and infarction correlate with graft loss • Banfi et al- Milan (1981) – Glomerular necrosis, intimal arteritis, arterial fibrinoid necrosis and PTC congestion predicted elevation of the 2 -mo postbiopsy creatinine • Durand et al, France (1983) – Arterial and tubular lesions were the strongest predictors of adverse outcome • Parfrey et al, Mc. Gill University (1984) – Interstitial hemorrhage was the strongest predictor for graft failure. Intimal arteritis and glomerulitis strengthened the prognosis

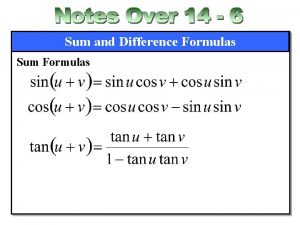
Acute Rejection Index (0 -36) • • • Glomerular endothelial swelling Endothelial and mesangial proliferation Glomerular Leukocytes Glomerular necrosis Interstitial edema Interstitial inflammation Swelling of the vascular endothelium and edema Mural vascular inflammation Mural vascular necrosis Finkelstein&Kashgarian 1976

Finkelstein et al, 1976
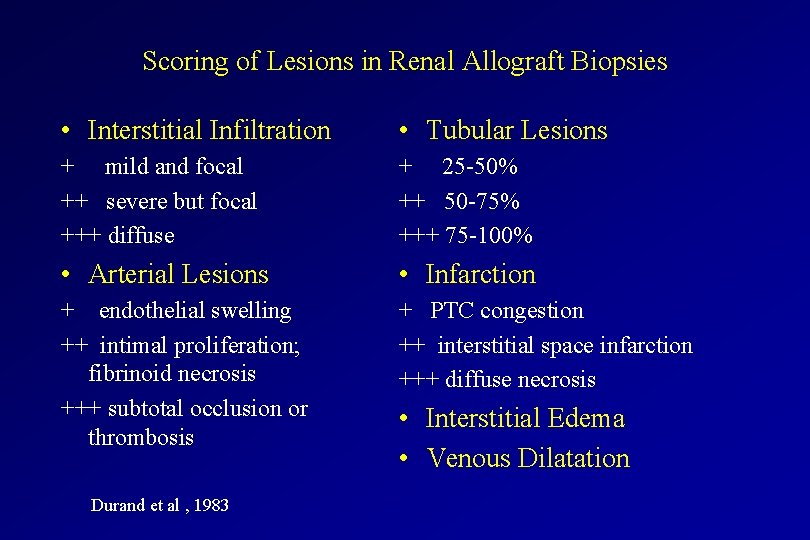
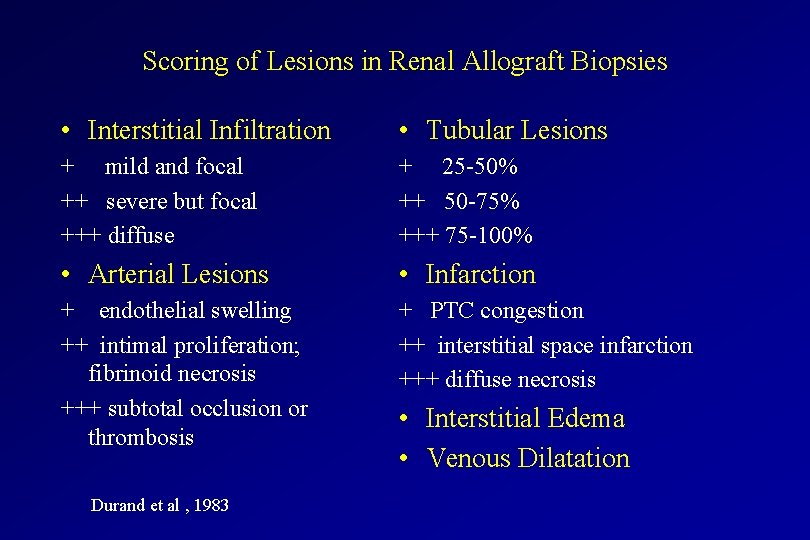
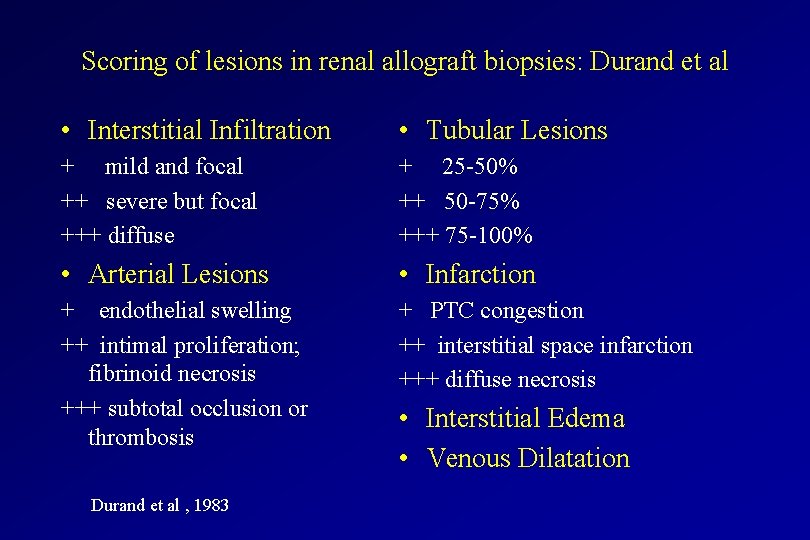
Scoring of Lesions in Renal Allograft Biopsies • Interstitial Infiltration • Tubular Lesions + mild and focal ++ severe but focal +++ diffuse + 25 -50% ++ 50 -75% +++ 75 -100% • Arterial Lesions • Infarction + endothelial swelling ++ intimal proliferation; fibrinoid necrosis +++ subtotal occlusion or thrombosis + PTC congestion ++ interstitial space infarction +++ diffuse necrosis Durand et al , 1983 • Interstitial Edema • Venous Dilatation

Semiquantitative Evaluation of Histologic Lesions and Outcome Durand et al , 1983

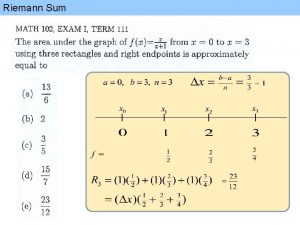
Scores Predicting Graft Outcome • Discriminative analysis of the major histologic features for their effect on prognosis & the generation of a linear combination • (0. 66 x infiltrate score) - (1. 98 arterial score) - (0. 42 edema score) - (1. 28 tubular score) - (0. 78 infarction score) + 3. 21 • When the combination was positive, the outcome was favorable in 83% of patients i. e. one year serum creatinine. • Durand et al , 1983
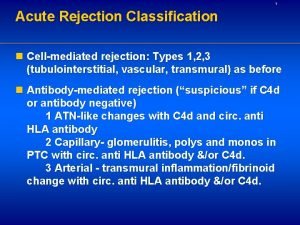
Banff ‘ 97/CCTT Grading of Acute Rejection * with at least i 1 and 2 or more of the following features: edema, activated lymphocytes or tubular injury
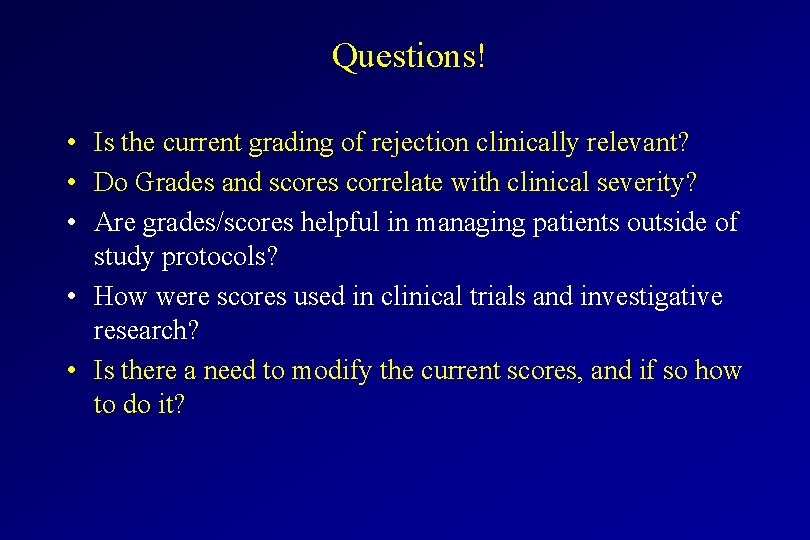
Questions! • Is the current grading of rejection clinically relevant? • Do Grades and scores correlate with clinical severity? • Are grades/scores helpful in managing patients outside of study protocols? • How were scores used in clinical trials and investigative research? • Is there a need to modify the current scores, and if so how to do it?
Did we do better with Banff Schema than descriptive terminology Dean, Cavallo et al; 1999
Interpretation by Standardized Banff Schema is Superior to conventional non-standardized diagnoses Over-read: lower scores were assigned by Banff than previous diagnosis Dean, Cavallo et al; 1999
Outcome of Patients Dean, Cavallo et al; 1999

CCTT Analysis of Morphologic Correlates to Clinical Severity of Acute Rejection • Morphologic features that significantly correlated with clinical severity of rejection – – – – Type II rejection Tubular injury Endothelialitis Interstitial hemorrhage Interstitial edema Glomerulitis Activated lymphocytes Tubulitis
Vascular Scores

Validity of Banff ‘ 93 Schema in Clinical Practice. University of Tennessee • Correlation between the sum scores and grades of acute rejection – – Borderline (Sum 1. 6 + 0. 5) Grade I (Sum 3. 3 + 0. 4) Grade II (Sum 4. 2 + 0. 3) Grade III (Sum 8. 5 + 0. 4) • Grades correlate with rejection reversal – Complete reversal occurred in 93% of Grade I – 47% of Grade III were irreversible* • Resistance to steroids and reversal of rejection correlate with the vascular scores
Impact of Vascular (Type II)/Cellular (Type I) Rejection in the First 3 months on Long Term Graft Survival Van Saase et al, 1995

Divergent graft survival between tubulointerstitial rejection and rejection with fibrinoid necrosis * P= 0. 03 versus Type I Nickeleit, Colvin et al, 1998
Av- Type of Vascular Pathology Nickelett & Colvin; 1998
Vascular Pathology and Rejection Outcome • Number of arteries with lesions did not correlate with steroid responsiveness or the 12 -month creatinine • Of the different types of lesions, reactive endothelium and sticking of mononuclear cells correlated with steroid resistance Nickelett & Colvin; 1998
Scores of Pathologic Features of Acute Rejection & the risk of graft failure Mueller et al; 2000
Vascular Scores • The most significant determinant of steroid response, rejection reversal and kidney function at one year • Vascular rejection is a predictor of chronic rejection • Number of arteries to be examined? • Isolated vascular rejection? • V 1 -2 rejection and severe tubulo-interstitial rejection? • Lumen compromise and severity of rejection? • Sticky mononuclear cells and endothelial edema? • Fibrinoid vascular necrosis! Rejection or no rejection?

Interstitial scores
Interstitial infiltrates Threshold for Acute Rejection • i 1 in Banff identified as 10 -25% of parenchyma involved • Type I rejection Banff requires at least i 1 • CCTT specified greater than 5% inflammation in the renal cortex

Extent of Interstitial Infiltrate & Rejection Grade Nickelett & Colvin; 1998

AI- Extent of interstitial infiltrates and outcome Nickelett & Colvin; 1998

Interstitial inflammation/infiltration Variables • Cell Types in the interstitial infiltrates – – Activated lymphocytes Monocytes Plasma cells Eosinophils • Surface area involved • Edema
Tubular Injury Scores
Acute tubular injury • CCTT group identified tubular injury as a significant parameter in determining severity of acute rejection • Tubulitis scores tended to be higher in patients with OKT 3 failure, and identified higher T scores for partially reversed and irreversible rejection compared to completely reversed rejection- UT • Mild or moderate tubulitis (Banff 97 IA) have better prognosis than acute cellular rejection with severe tubulitis (Banff 97 IB). No differences between acute rejection with t 3 (Banff IB) and rejection with mild vasculitis v 1(Banff IIA) in terms of rejection reversal, 12 -month creatinine or graft loss. Randhawa, AST 2000

Scores for Tubulitis • Post rejection biopsy scores • Severe tubulitis with very mild inflammation • Acute tubular necorsis + tubulitis

Acute Glomerulitis Scores
Glomerulitis • Kashgarian recognized the significance of endothelial swelling and glomerular inflammation alongside with vascular pathology • Scores for G were higher in the irreversible and partially reversible rejection, and in steroid resistant rejection. Higher glomerular scores for patients with recurrent rejections (NS). UT • Glomeruliits more in first rejection, patients with delayed graft function and has worse outcome than G 0 rejection. Racusen AST, 2000 • Glomerulitis distinguished patients with Bo that progressed to rejection
Glomerulitis Scores • Glomerulitis and Antibody-mediated rejection • Glomerular necorsis and thrombosis in TMA • Is it a sign of a unique or a severe rejection?
Scores and Sum Consensus
Sum scores in Clinical Practice • Excellent correlation between grades of rejection and response to therapy, outcome parameters • Although scores in most cases correlate the grade of rejection, they are not to be used for therapeutic decisions • Incorporation of scores in the reports is optional, but highly recommended for data accession and retrieval in academic centers • Inclusion of scores and sum of rejection is encouraged – Forces compulsive and methodical analysis of the morphologic features – Easy method to scan the pathology report for rejection severity in the different compartments
Sum Scores in Clinical Trials • It is strongly recommended for clinical trials for meaningful statistical analysis of morphologic features • Potential application in clinical trials – Fibrosis at 6 mo-2 years is an appropriate surrogate endpoint in chronic rejection trials – Not necessary for inclusion, but they may be important to thoroughly compare both arms in a study – Endpoint analysis – Control sample size and followup period
Vascular scores • Need 4 arteries to increase the sensitivity for the detected of intimal arteritis • Number of arteries affected by inflammation does not impact therapy response or graft survival • Adhesion of mononuclear cells to activated endothelium correlates with steroid failure. Should we add suspicious for acute vascular rejection or include it with Type IIA. Type IB and IIA act similarly!
Glomerulitis • Underdiagnosed entity • Highly associated with Ab-mediated rejection and feature of borderline progressing to acute rejection. May identify a subset of acute rejection. May be the predecessor for chronic transplant glomerulopathy • Should we use CD 68?
Tubulitis • Rejection with severe tubulitis acts similar to mild vascular rejection
Interstitial Inflammation • Continue to specify and flag cell types • Mononuclear cell score?

Chronicity scores • Interstitial fibrosis – Recommend evaluation by trichrome/sirius red – Morphometric assessment for studies is recommended • Chronic transplant vasculopathy – Types • Inactive sclerosing transplant vasculopathy • Proliferative sclerosing vasculopathy • Foam cell – Elastic stains or conventional stains adequate? • Chronic rejection with TV is more aggressive. Socres for RTV may need to be adjusted? • Glomerular pathology specify obsolescent/solidified/FSGS

C 4 D Staining • Do we need to incorporate in the sum? • What is the value to be assigned?
Sum Scores • Not ideal to represent the rejection severity or reflect on the pathogenesis of rejection. Linear parameter and does not take into account the varying relative strength of its components in the assessment of rejection severity • Design a more mathematically correct parameter? • Combined clinical and Morphological index?
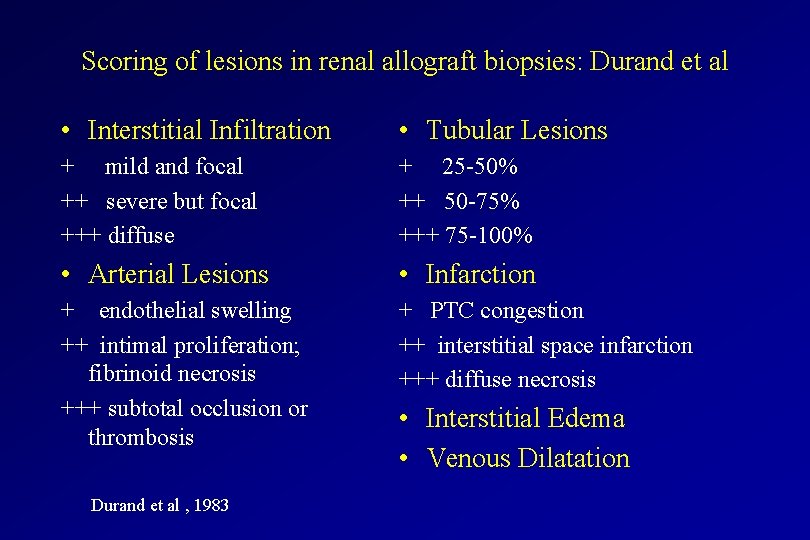
Scoring of lesions in renal allograft biopsies: Durand et al • Interstitial Infiltration • Tubular Lesions + mild and focal ++ severe but focal +++ diffuse + 25 -50% ++ 50 -75% +++ 75 -100% • Arterial Lesions • Infarction + endothelial swelling ++ intimal proliferation; fibrinoid necrosis +++ subtotal occlusion or thrombosis + PTC congestion ++ interstitial space infarction +++ diffuse necrosis Durand et al , 1983 • Interstitial Edema • Venous Dilatation
Frequency of Lesions and Outcome Durand et al , 1983
Semiquantitative Evaluation of Histologic Lesions and Outcome Durand et al , 1983

Scoring of lesions in renal allograft biopsies: Durand et al • Discriminative analysis of the major histologic features for their effect on prognosis lead to the generation of a linear combination • (0. 66 x infiltrate score) - (1. 98 arterial score) - (0. 42 edema score) - (1. 28 tubular score) - (0. 78 infarction score) + 3. 21 • when the combination was positive, the outcome was favorable in 83% of patients i. e. one year serum creatinine. • Durand et al , 1983
 Chronic rejection
Chronic rejection Refifs
Refifs Chronic rejection
Chronic rejection Basement membrane stain
Basement membrane stain Chronic rejection
Chronic rejection Chronic rejection
Chronic rejection Define periradicular disease
Define periradicular disease Acute cholecystitis vs chronic cholecystitis
Acute cholecystitis vs chronic cholecystitis Morphologic patterns of acute and chronic inflammation
Morphologic patterns of acute and chronic inflammation Acute subacute chronic
Acute subacute chronic Acute vs chronic heart failure
Acute vs chronic heart failure Hyperplasia
Hyperplasia Lll leukemia
Lll leukemia 5 signs of inflammation
5 signs of inflammation 18 common chronic and acute conditions
18 common chronic and acute conditions Indexes scales and typologies
Indexes scales and typologies Sum0
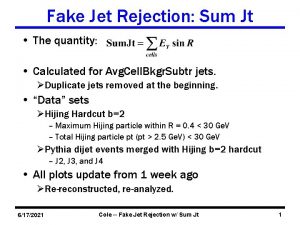
Sum0 Defect rejection ratio formula
Defect rejection ratio formula Sample rejection criteria
Sample rejection criteria Acceptance and rejection region
Acceptance and rejection region Reassurance dalam hubungan
Reassurance dalam hubungan Insulation coordination in high voltage engineering
Insulation coordination in high voltage engineering Cmrr op amp
Cmrr op amp Sample rejection criteria
Sample rejection criteria Can sugar gliders eat beets
Can sugar gliders eat beets Image frequency rejection ratio
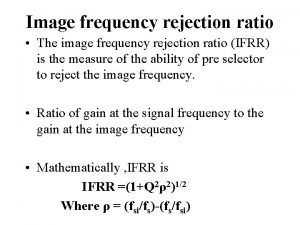
Image frequency rejection ratio Flop fashion cycle examples
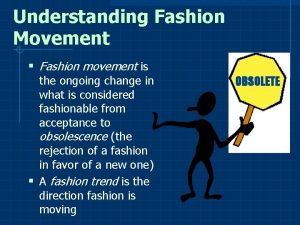
Flop fashion cycle examples Dependency rejection
Dependency rejection Rejection attachment
Rejection attachment Elisha prayers
Elisha prayers Luke 4 rejection at nazareth
Luke 4 rejection at nazareth Young heat exchangers
Young heat exchangers Sound beam ultrasound
Sound beam ultrasound Opposite rejection
Opposite rejection Rejection sensitive dysphoria
Rejection sensitive dysphoria Viral load sample collection
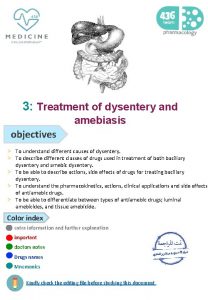
Viral load sample collection Chronic amebiasis
Chronic amebiasis Angioectasia icd 10
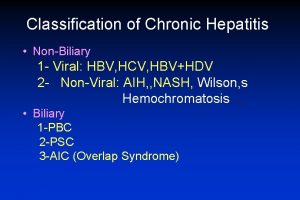
Angioectasia icd 10 Classification of chronic hepatitis
Classification of chronic hepatitis Dr ali azzam
Dr ali azzam Chronic inflammation
Chronic inflammation Labs for chronic pancreatitis
Labs for chronic pancreatitis Chronic addiction
Chronic addiction Carlee oakley
Carlee oakley Chronic insomnia
Chronic insomnia Chronic gout
Chronic gout Hemolytic anemia symptoms
Hemolytic anemia symptoms Chronic disease
Chronic disease Copd exacerbation nursing management
Copd exacerbation nursing management Improving chronic illness care model
Improving chronic illness care model