Sudden visual loss a case based approach Michael
Sudden visual loss: a case based approach Michael Karampelas Clinical Lead Ophthalmology Department Watford General and St Albans City Hospitals Retinal specialist
Sudden visual loss definition • rapid onset • minutes up to days
Questions you need to ask • how long ago? • rapid or gradual onset? • course? • monocular or binocular? • transient or persistent? • painless or painful? • associated symptoms? • ophthalmic and medical history
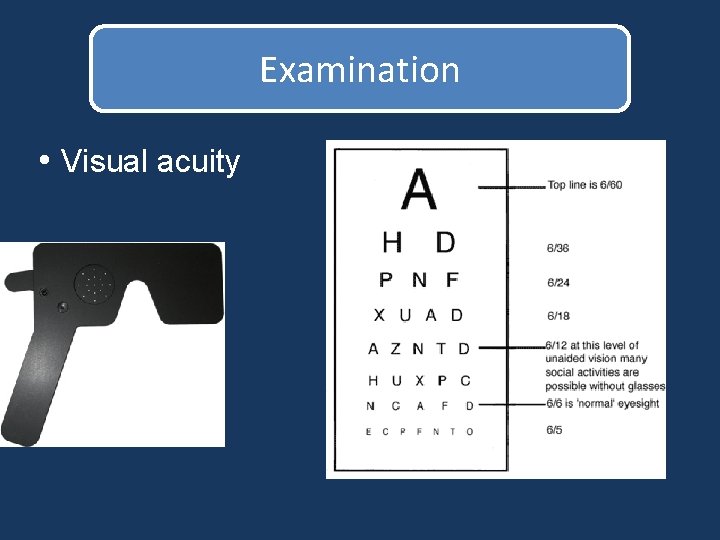
Examination • Visual acuity
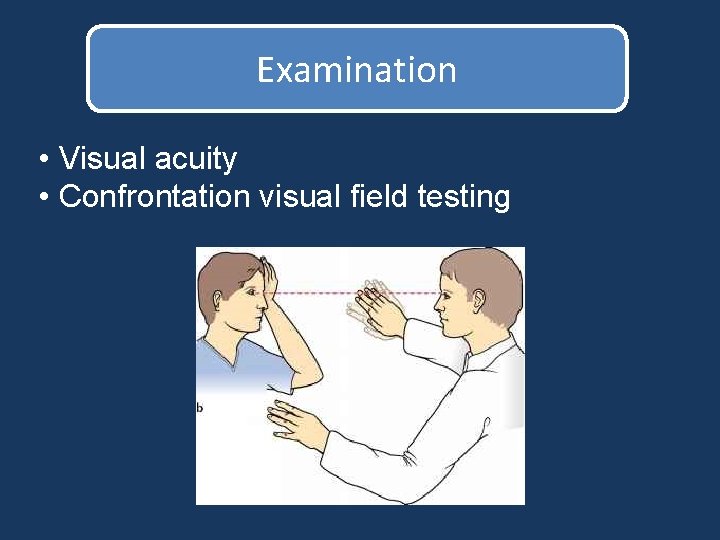
Examination • Visual acuity • Confrontation visual field testing
Examination • Visual acuity • Confrontation visual field testing With the patient looking at your nose, ask if your nose and other facial features are seen clearly Inability to clearly see your: Nose Eyes or lips Ears => central scotoma => paracentral scotoma => peripheral visual field defect
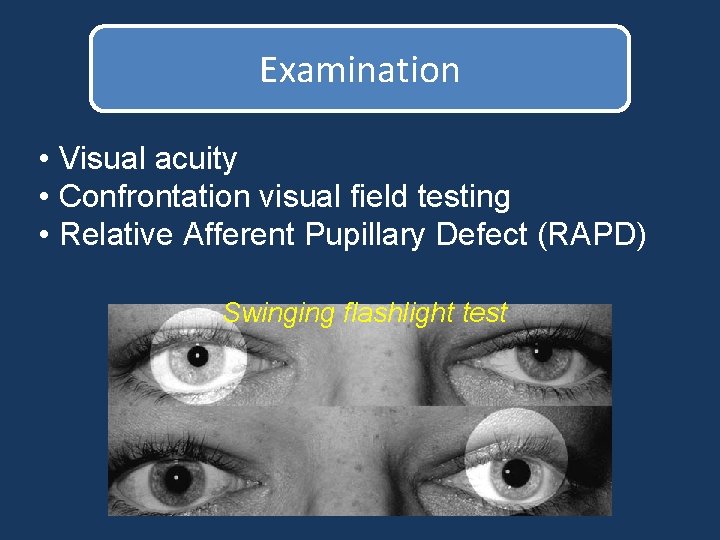
Examination • Visual acuity • Confrontation visual field testing • Relative Afferent Pupillary Defect (RAPD) Swinging flashlight test
Relative Afferent Pupillary Defect Significant retinal or optic nerve disease, in one eye more than the other
Examination • Visual acuity • Confrontation visual field testing • Relative Afferent Pupillary Defect (RAPD) • Direct ophthalmoscopy
Acute monocular visual loss Transient Persistent
Transient monocular acute visual loss • 74 year old man reports intermittent episodes of “fuzzy vision” lasting from 1 to 15 minutes. • unsure whether monocular or binocular • no other symptoms reported • p. MH: coronary artery disease, hypertension, hyperlipidemia • p. OH: previous cataract operations
Transient monocular acute visual loss • Visual acuity: 6/9 in both eyes • No RAPD • No gross visual field abnormality • No significant issue on retinoscopy
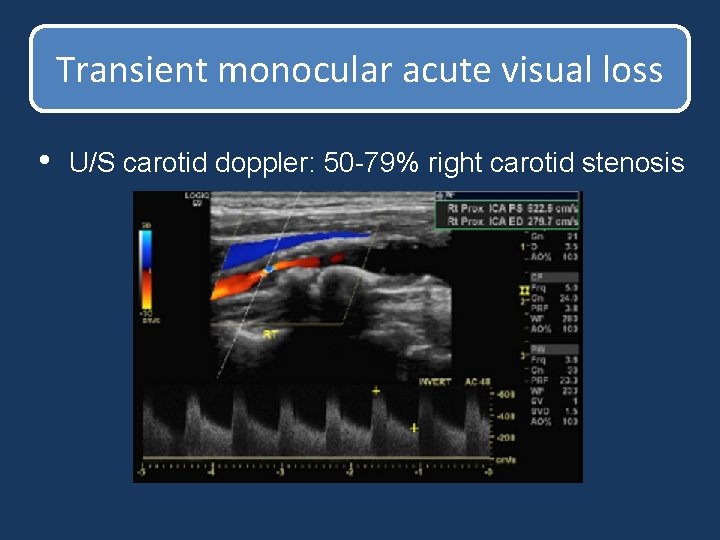
Transient monocular acute visual loss • U/S carotid doppler: 50 -79% right carotid stenosis
Amaurosis Fugax • Painless transient loss of vision, partial or complete, related to retinal arterial microembolization or hypoperfusion • If bilateral it may indicate Vertebrobasilar Insufficiency
Amaurosis Fugax • Visual disturbance: Dark, foggy, gray, white • Minutes (1 -5 minutes, occasionally longer); full resolution takes 10 -20 minutes • Painless • Usually occurs in isolation • Assessment of cardiovascular risk factors • U/S carotid doppler
Transient monocular acute visual loss • A 30 -year-old woman began to experience transient visual loss in the right eye 3 days before presentation • Episodes lasted from one to several minutes and consisted of flashing lights, grey-outs and episodes of reduced vision to her right eye • She did not experience headaches, diplopia or any other focal neurologic phenomena
Transient monocular acute visual loss • p. MH: Migraines • p. OH: free
Transient monocular acute visual loss • Visual acuity: 6/6 RE, 6/6 LE • no RAPD • normal visual fields
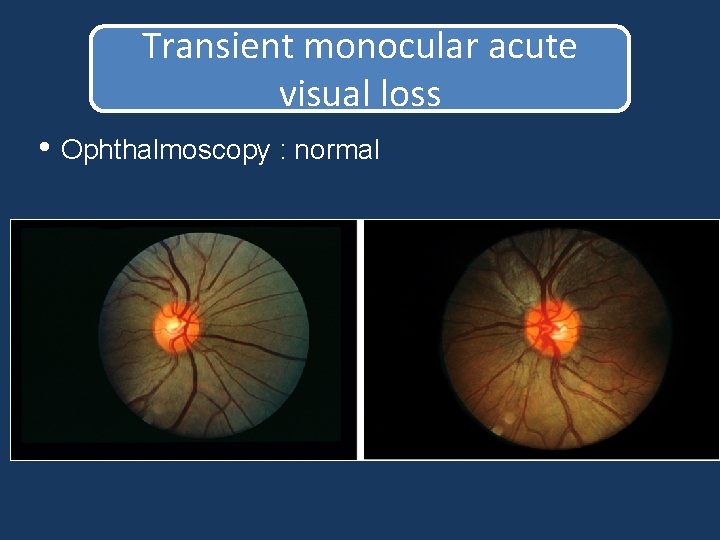
Transient monocular acute visual loss • Ophthalmoscopy : normal
Ocular migraine • Migraine with aura (“classic”) Jagged lines, fortification spectra, blind spots, flashing lights Generally start 5 -30 mins before headache and last for 20 -60 mins • Migraine without aura (“common”) • Ocular migraine: aura without headache
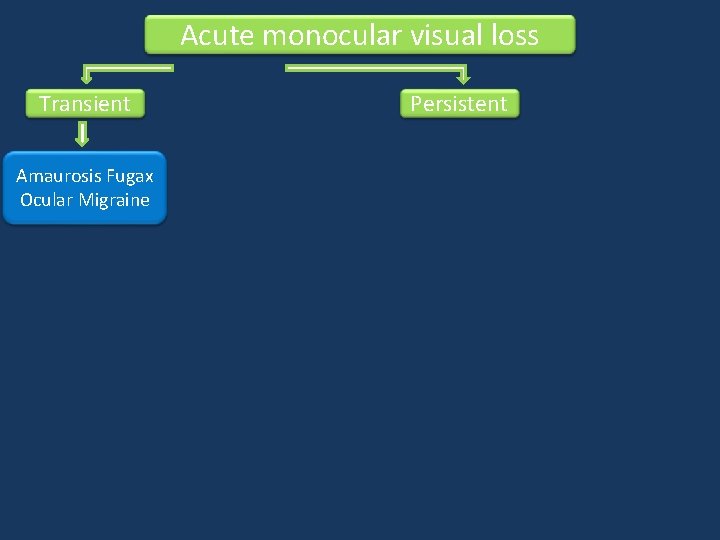
Acute monocular visual loss Transient Amaurosis Fugax Ocular Migraine Persistent
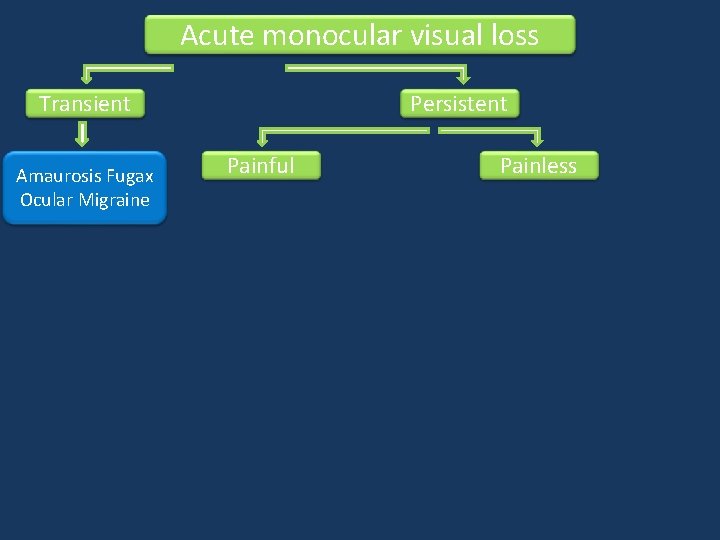
Acute monocular visual loss Transient Amaurosis Fugax Ocular Migraine Persistent Painful Painless
Persistent painful monocular acute visual loss • 64 year old woman reports severe pain in her right eye started suddenly 1 day ago • pain radiates to temple • hazy vision – haloes around lights • mild nausea • p. MH: hypertension, hyperlipidemia history of migraines • p. OH: hypermetropia
Persistent painful monocular acute visual loss • Visual acuity: RE: hand movements LE: 6/9 • no RAPD but RE pupil do not react to light • difficult to assess visual fields in RE. LE: normal • difficult to perform retinoscopy
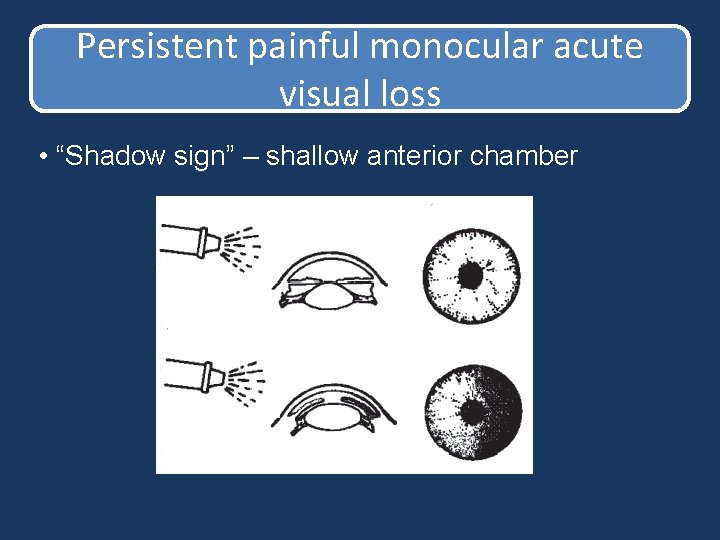
Persistent painful monocular acute visual loss • “Shadow sign” – shallow anterior chamber
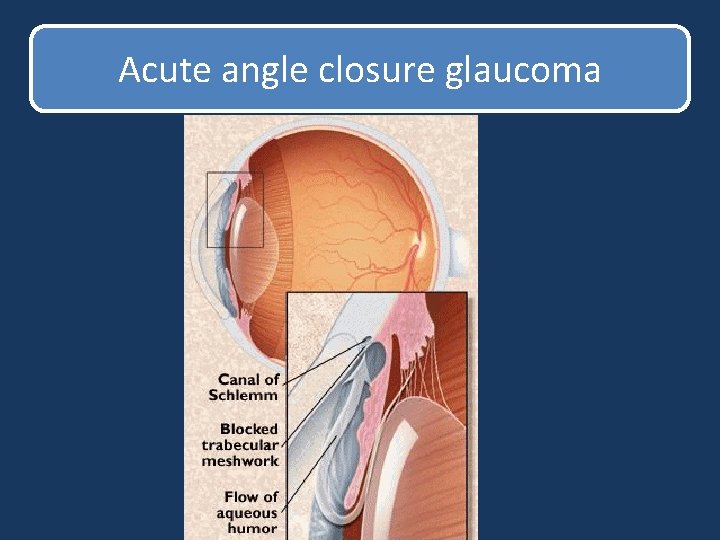
Acute angle closure glaucoma
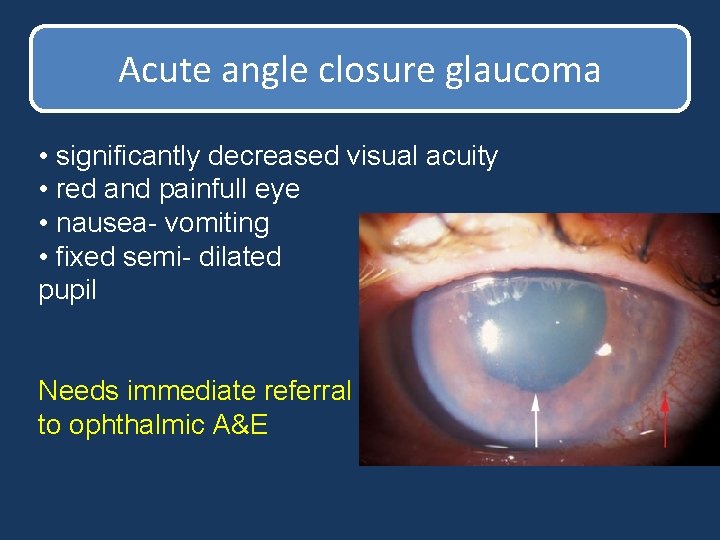
Acute angle closure glaucoma • significantly decreased visual acuity • red and painfull eye • nausea- vomiting • fixed semi- dilated pupil Needs immediate referral to ophthalmic A&E
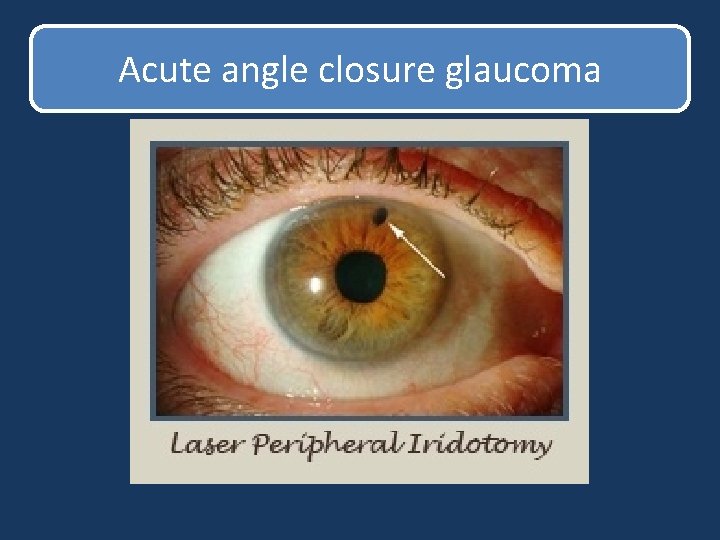
Acute angle closure glaucoma
Persistent painful monocular acute visual loss • 70 year old man reports gradual reduction in his RE vision of the last two days with some mild pain and redness • p. MH: hypertension, hyperlipidemia • p. OH: cataract operation in the RE 1 week ago
Persistent painful monocular acute visual loss • Visual acuity: RE: light perception LE: 6/6 • no RAPD • difficult to assess visual fields in RE. • difficult to perform retinoscopy
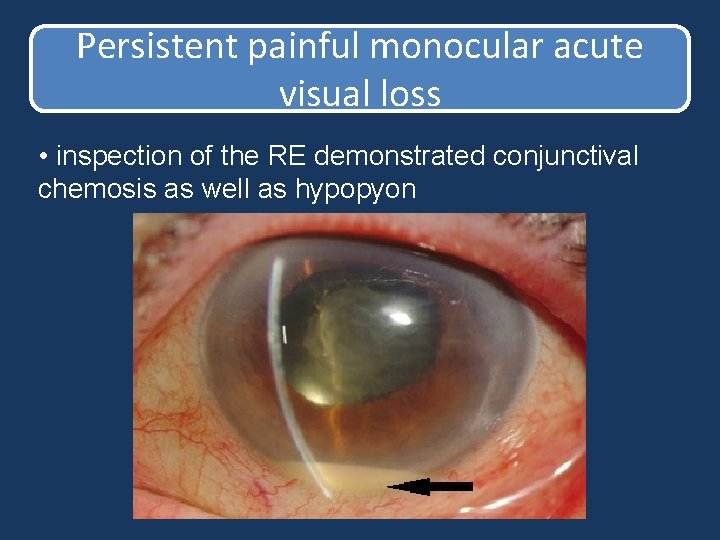
Persistent painful monocular acute visual loss • inspection of the RE demonstrated conjunctival chemosis as well as hypopyon
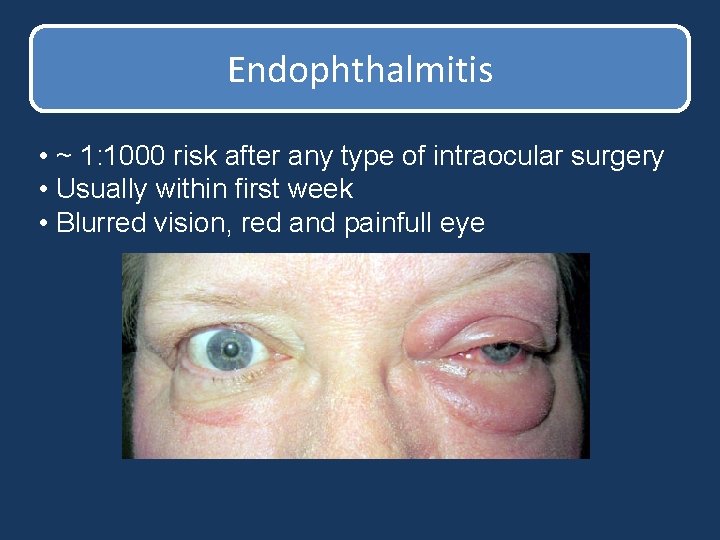
Endophthalmitis • ~ 1: 1000 risk after any type of intraocular surgery • Usually within first week • Blurred vision, red and painfull eye
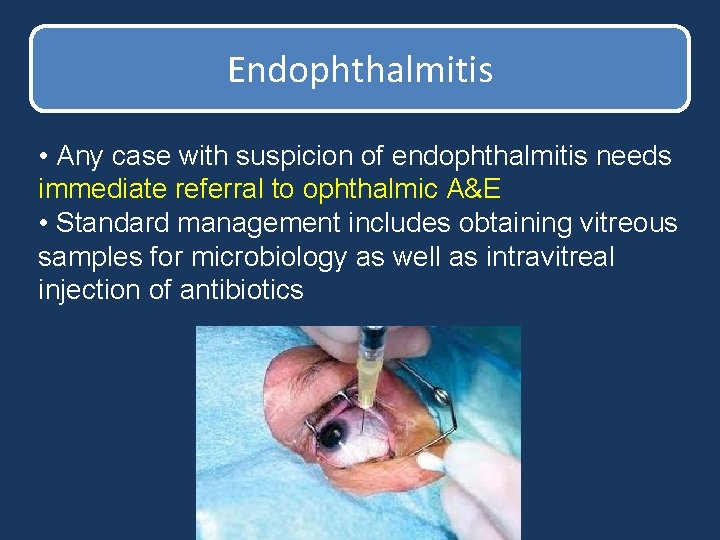
Endophthalmitis • Any case with suspicion of endophthalmitis needs immediate referral to ophthalmic A&E • Standard management includes obtaining vitreous samples for microbiology as well as intravitreal injection of antibiotics
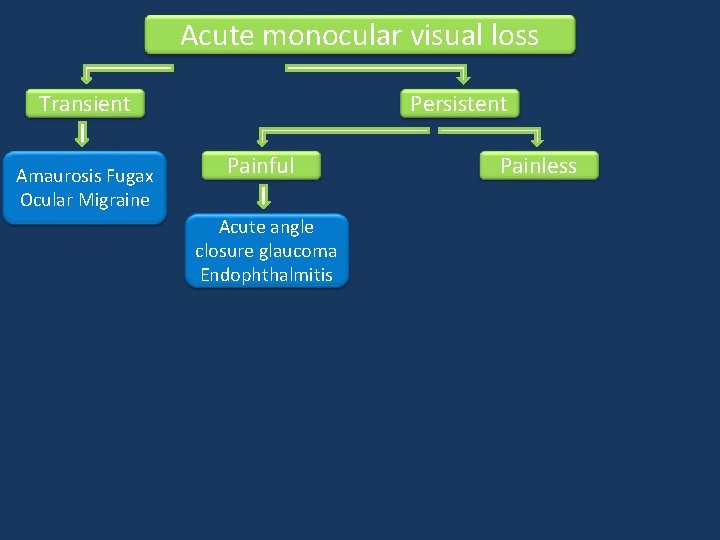
Acute monocular visual loss Transient Amaurosis Fugax Ocular Migraine Persistent Painful Acute angle closure glaucoma Endophthalmitis Painless
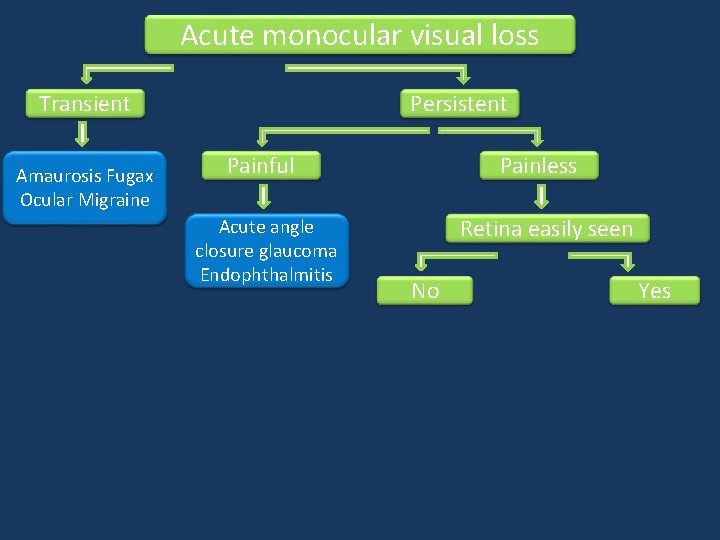
Acute monocular visual loss Transient Amaurosis Fugax Ocular Migraine Persistent Painful Acute angle closure glaucoma Endophthalmitis Painless Retina easily seen No Yes
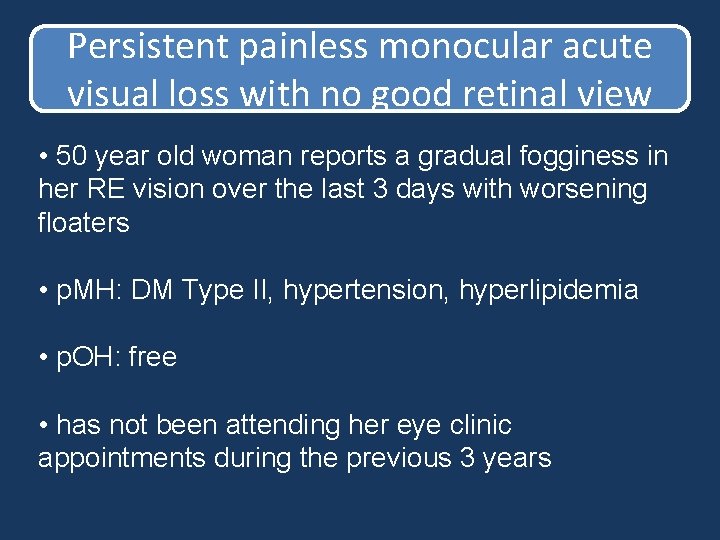
Persistent painless monocular acute visual loss with no good retinal view • 50 year old woman reports a gradual fogginess in her RE vision over the last 3 days with worsening floaters • p. MH: DM Type II, hypertension, hyperlipidemia • p. OH: free • has not been attending her eye clinic appointments during the previous 3 years
Persistent painless monocular acute visual loss with no good retinal view • Visual acuity: 6/60 RE, 6/6 LE • No RAPD • difficult to assess visual fields • difficult to obtain a retinal view. Diminished redreflex with direct ophthalmoscope
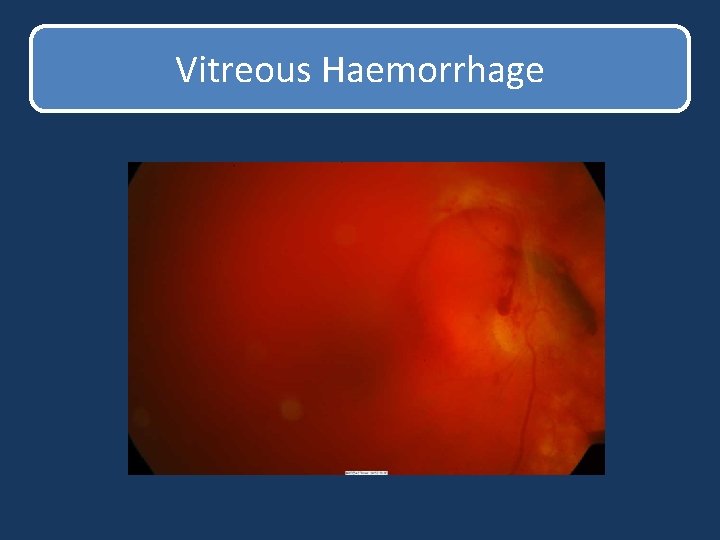
Vitreous Haemorrhage
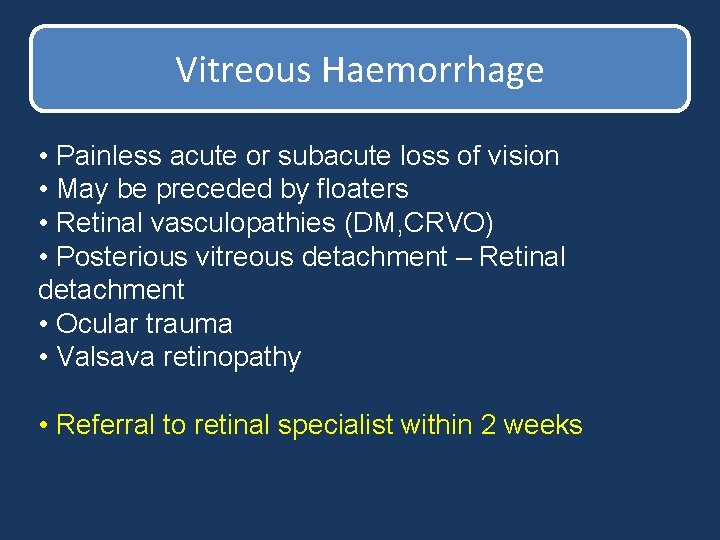
Vitreous Haemorrhage • Painless acute or subacute loss of vision • May be preceded by floaters • Retinal vasculopathies (DM, CRVO) • Posterious vitreous detachment – Retinal detachment • Ocular trauma • Valsava retinopathy • Referral to retinal specialist within 2 weeks
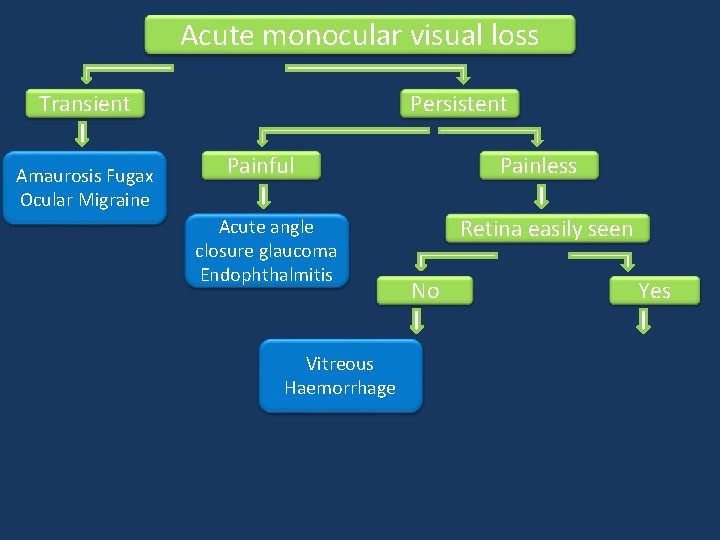
Acute monocular visual loss Transient Amaurosis Fugax Ocular Migraine Persistent Painful Acute angle closure glaucoma Endophthalmitis Vitreous Haemorrhage Painless Retina easily seen No Yes
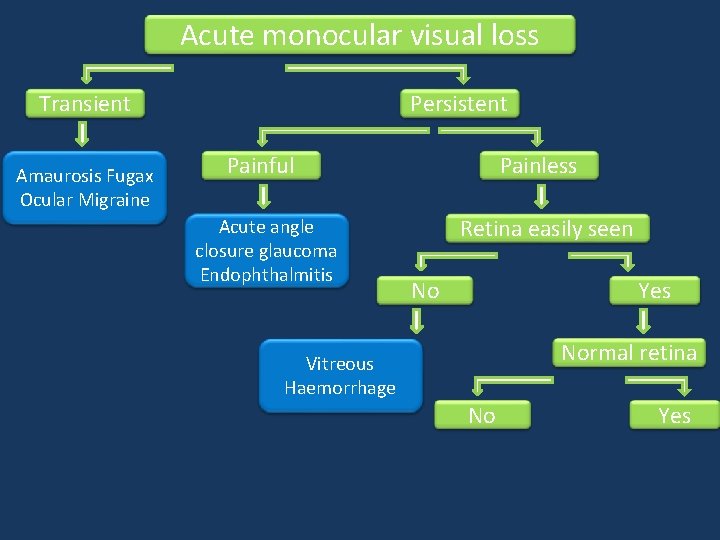
Acute monocular visual loss Transient Amaurosis Fugax Ocular Migraine Persistent Painful Acute angle closure glaucoma Endophthalmitis Painless Retina easily seen No Yes Normal retina Vitreous Haemorrhage No Yes
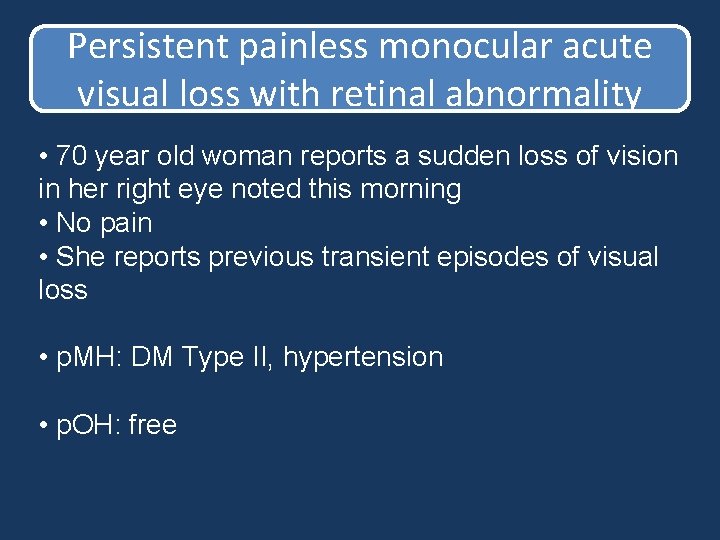
Persistent painless monocular acute visual loss with retinal abnormality • 70 year old woman reports a sudden loss of vision in her right eye noted this morning • No pain • She reports previous transient episodes of visual loss • p. MH: DM Type II, hypertension • p. OH: free
Persistent painless monocular acute visual loss with retinal abnormality • Visual acuity: CF RE, 6/6 LE • RAPD RE • Total loss of visual field RE
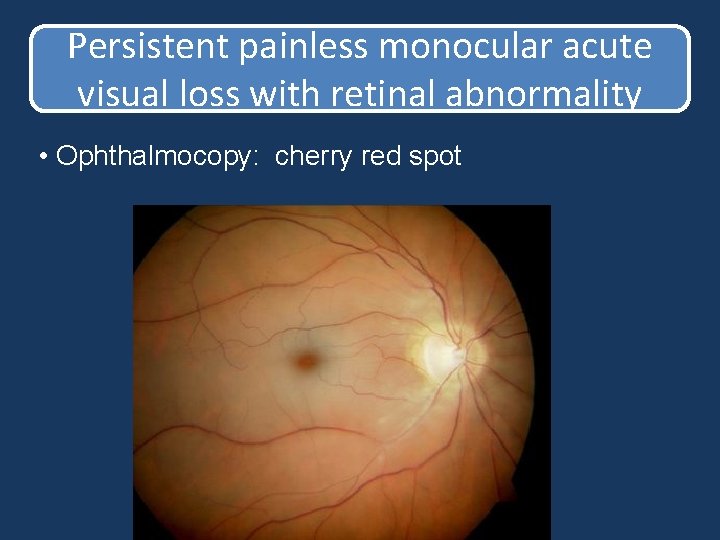
Persistent painless monocular acute visual loss with retinal abnormality • Ophthalmocopy: cherry red spot
Central retinal artery occlusion • Acute, painless, monocular, persistent and nearly complete loss of vision • Aetiology: Same as for any thromboembolic disease • 5 year mortality is 1/3 rd of age matched controls without CRAO • No standard treatment of proven benefit Need to exclude GCA
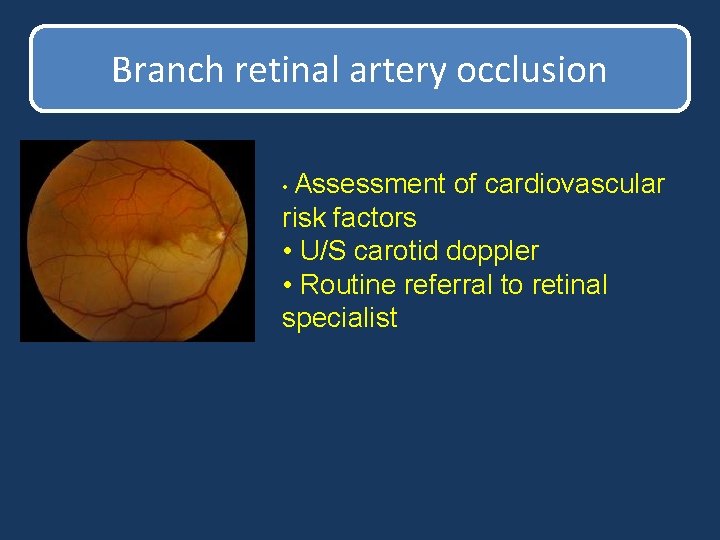
Branch retinal artery occlusion • Assessment of cardiovascular risk factors • U/S carotid doppler • Routine referral to retinal specialist
Persistent painless monocular acute visual loss with retinal abnormality • A 60 year old male complains of progressive loss of vision in left eye over the last 2 days. • No other symptoms • Painless uniform dulling of vision. • p. MH: DM Type II, hypertension • p. OH: free
Persistent painless monocular acute visual loss with retinal abnormality • Visual acuity is 6/6 RE – 6/60 LE • Mild RAPD LE • Constricted visual field LE
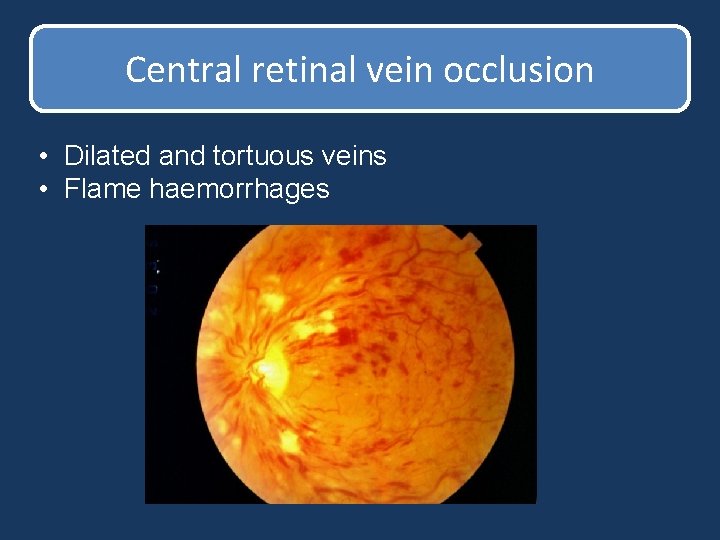
Central retinal vein occlusion • Dilated and tortuous veins • Flame haemorrhages
Central retinal vein occlusion • 10 times more common than CRAO • Most common risk factors: diabetes, hypertension, hyperlipidaemia • In patients <50 years old, haematologic and autoimmune disease should be excluded. • Lond term complications are macular oedema and retinal neovascularisation
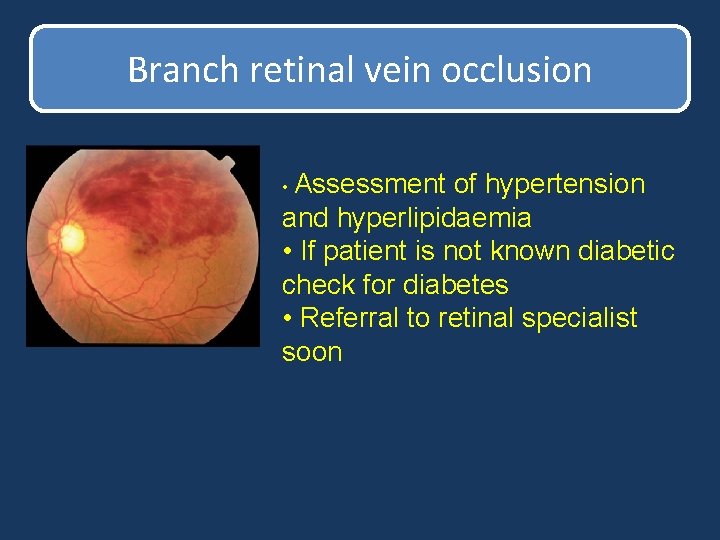
Branch retinal vein occlusion • Assessment of hypertension and hyperlipidaemia • If patient is not known diabetic check for diabetes • Referral to retinal specialist soon
Persistent painless monocular acute visual loss with retinal abnormality • 30 old year woman reports a “black shadow” in her inferior corner of her RE first noted yesterday getting progressively worse. Today her vision is blurry. No pain but had floaters and flashes during the last week. • p. MH: free • p. OH: Myopia
Persistent painless monocular acute visual loss with retinal abnormality • Visual acuity HM RE , 6/6 LE • RAPD RE • Inferior visual field defect
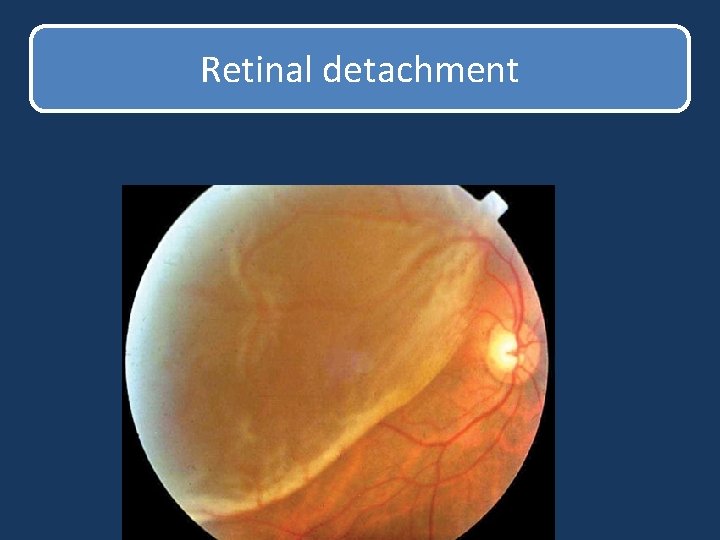
Retinal detachment
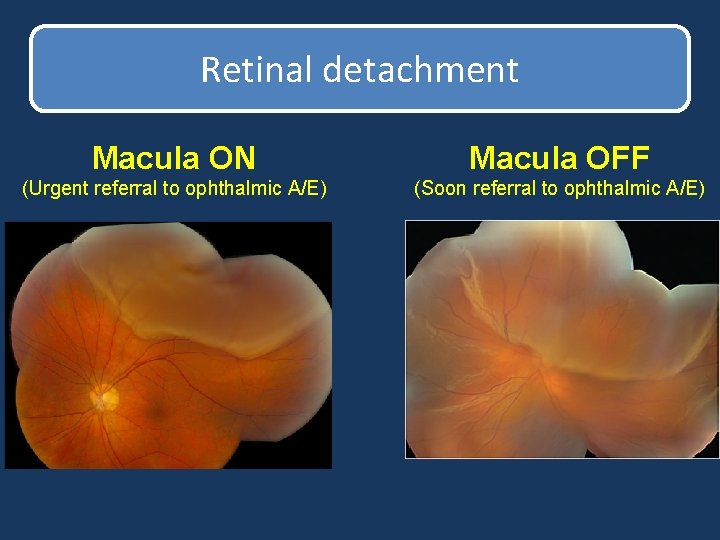
Retinal detachment Macula ON Macula OFF (Urgent referral to ophthalmic A/E) (Soon referral to ophthalmic A/E)
Retinal detachment • Risk Factors : myopia, previous cataract surgery, trauma
Persistent painless monocular acute visual loss with retinal abnormality • 76 old year woman reports a sudden onset of metamorphopsia and reduced vision in her right eye over a period of 3 days. No other symptoms • p. MH: hypertension • p. OH: dry AMD
Persistent painless monocular acute visual loss with retinal abnormality • Visual acuity is 6/36 RE and 6/12 LE • No RAPD • Central defect in visual field testing • Metamorphopsia in Amsler grid
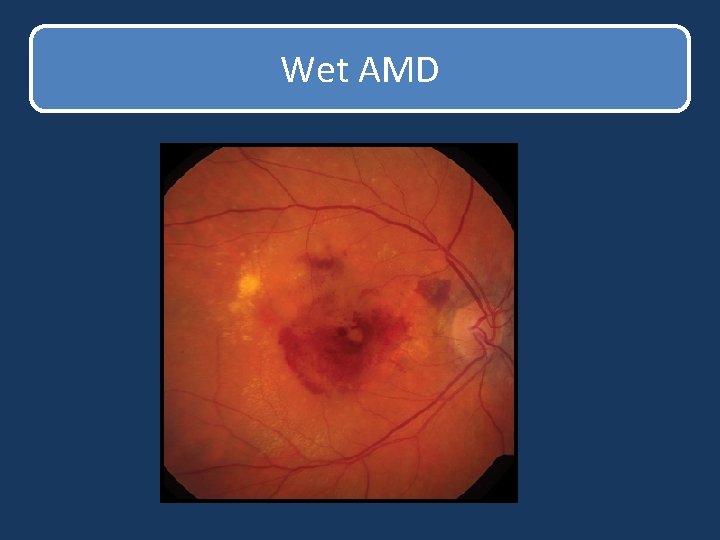
Wet AMD
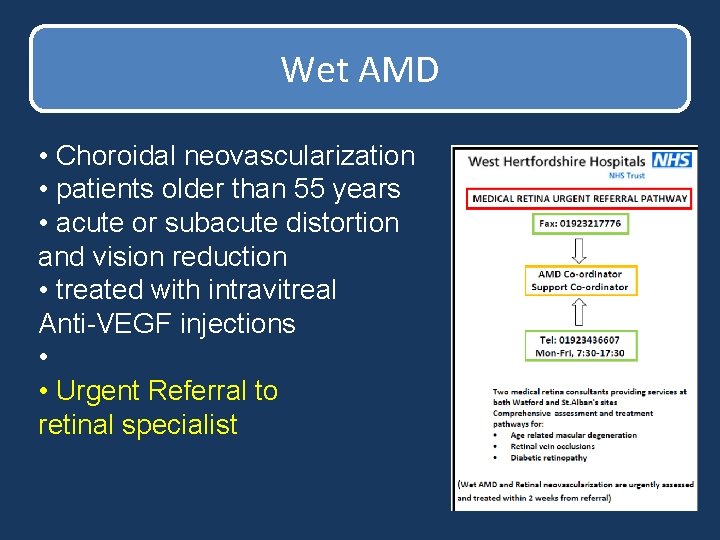
Wet AMD • Choroidal neovascularization • patients older than 55 years • acute or subacute distortion and vision reduction • treated with intravitreal Anti-VEGF injections • • Urgent Referral to retinal specialist
Persistent painless monocular acute visual loss with retinal abnormality • 68 year old man complains for blurred vision in his RE noted this morning upon waking up. No other symptoms • p. MH: hypertension, hyperlipaedimia • p. OH: free
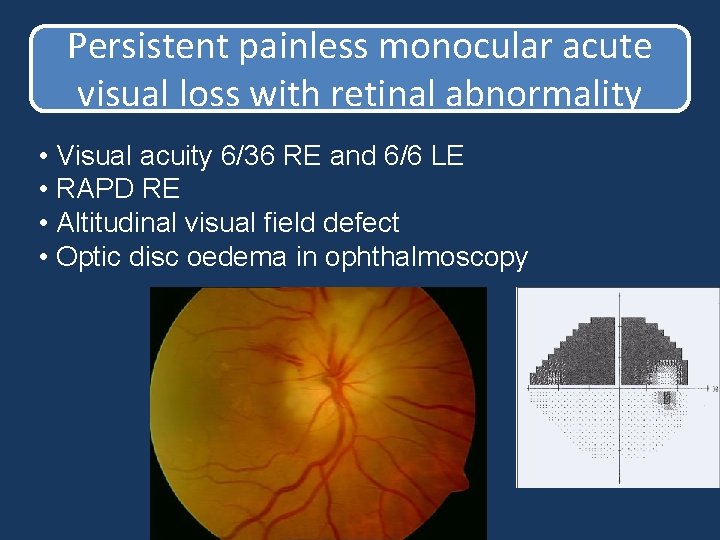
Persistent painless monocular acute visual loss with retinal abnormality • Visual acuity 6/36 RE and 6/6 LE • RAPD RE • Altitudinal visual field defect • Optic disc oedema in ophthalmoscopy
Anterior ischaemic optic neuropathy • Non-arteritic: Common cardiovascular risk factors Not much in terms of treatment • Arteritic: Autoimmune Chronic oral steroids to protect other eye
Giant cell arteritis • Factors suggestive of GCA: • Older than 50 years • Headache • Jaw pain or fatigue on chewing (claudication) • Scalp tenderness • Elevated ESR, CRP Start Prednisone (1 mg/kg) Temporal artery biopsy within 1 week
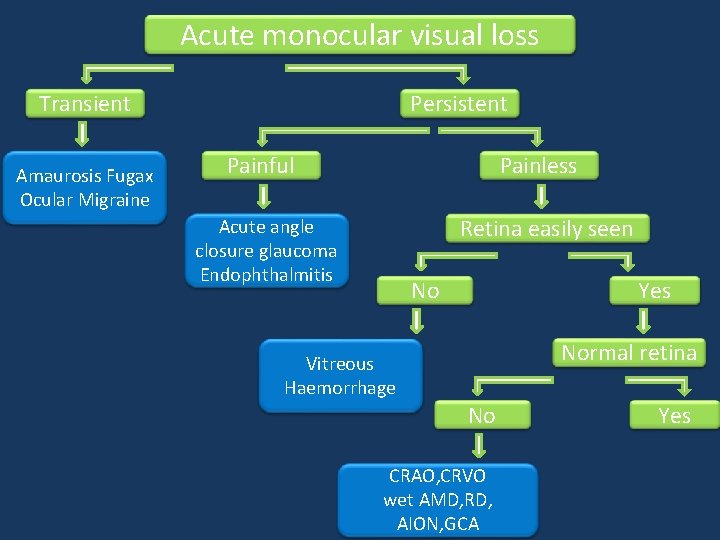
Acute monocular visual loss Transient Amaurosis Fugax Ocular Migraine Persistent Painful Painless Retina easily seen Acute angle closure glaucoma Endophthalmitis No Yes Normal retina Vitreous Haemorrhage No CRAO, CRVO wet AMD, RD, AION, GCA Yes
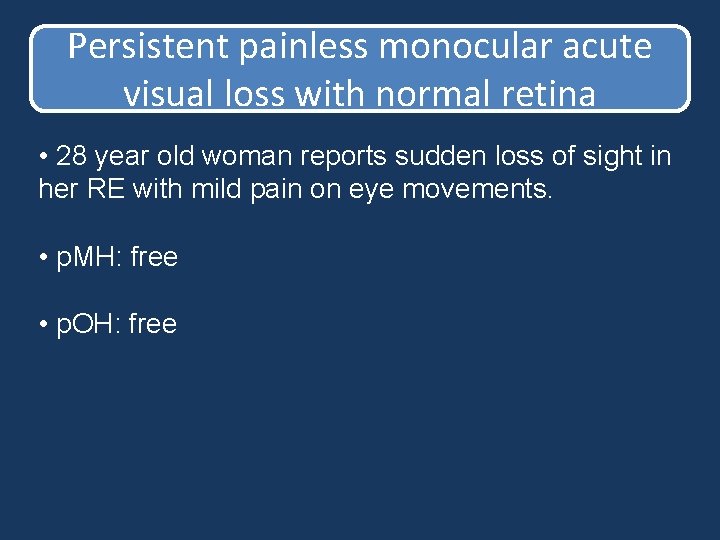
Persistent painless monocular acute visual loss with normal retina • 28 year old woman reports sudden loss of sight in her RE with mild pain on eye movements. • p. MH: free • p. OH: free
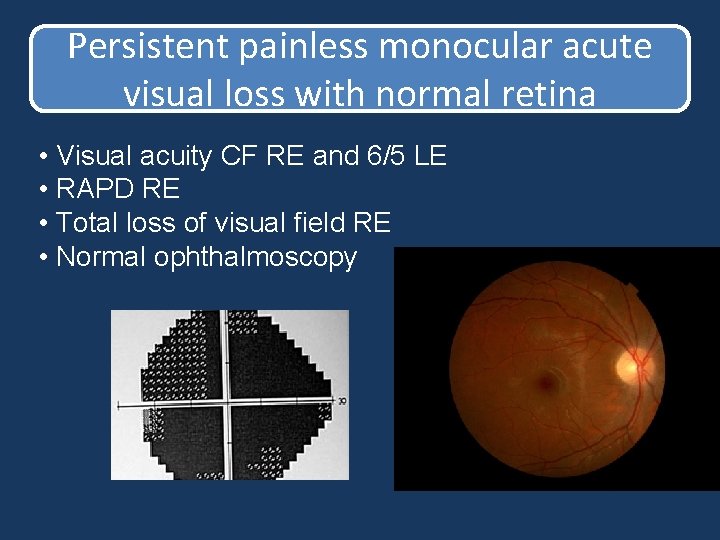
Persistent painless monocular acute visual loss with normal retina • Visual acuity CF RE and 6/5 LE • RAPD RE • Total loss of visual field RE • Normal ophthalmoscopy
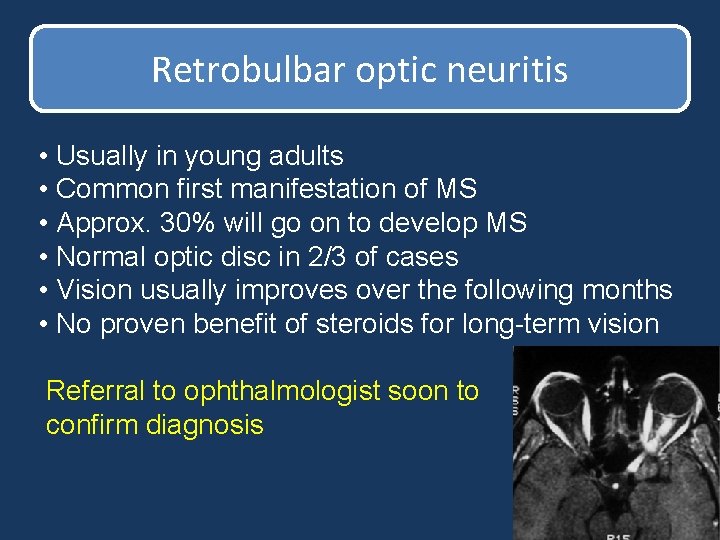
Retrobulbar optic neuritis • Usually in young adults • Common first manifestation of MS • Approx. 30% will go on to develop MS • Normal optic disc in 2/3 of cases • Vision usually improves over the following months • No proven benefit of steroids for long-term vision Referral to ophthalmologist soon to confirm diagnosis
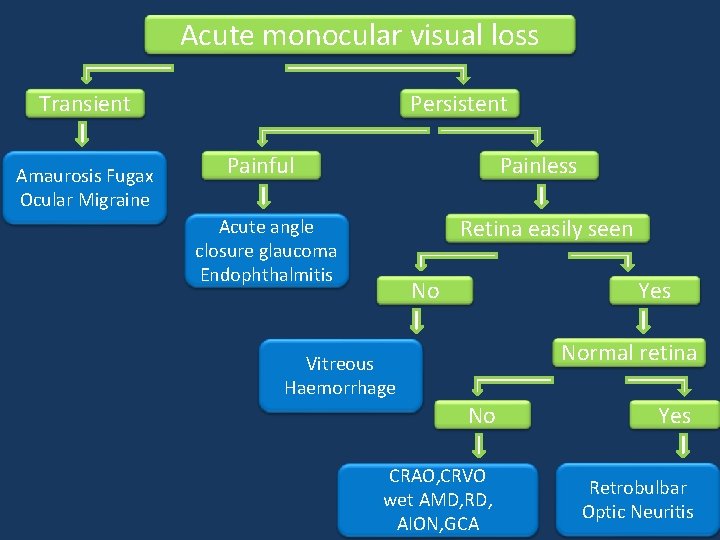
Acute monocular visual loss Transient Amaurosis Fugax Ocular Migraine Persistent Painful Painless Retina easily seen Acute angle closure glaucoma Endophthalmitis No Yes Normal retina Vitreous Haemorrhage No Yes CRAO, CRVO wet AMD, RD, AION, GCA Retrobulbar Optic Neuritis

Thank you
- Slides: 70