Sudden sensorineural hearing loss Dr Vishal Sharma Defining






- Slides: 49
Sudden sensori-neural hearing loss Dr. Vishal Sharma
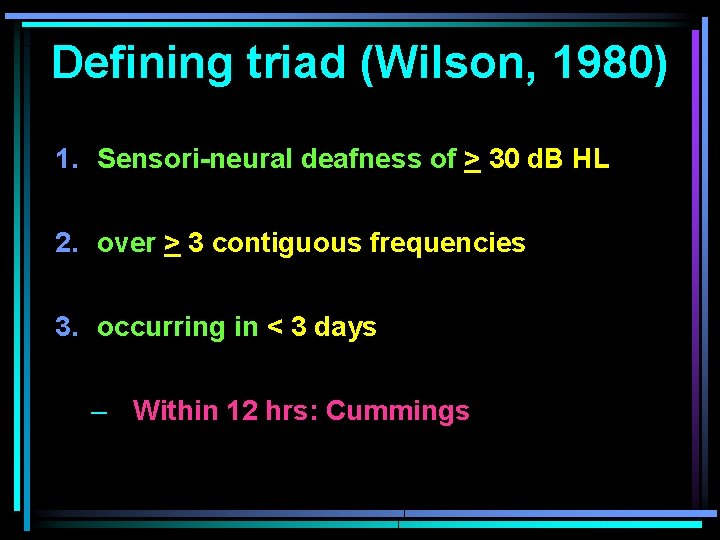
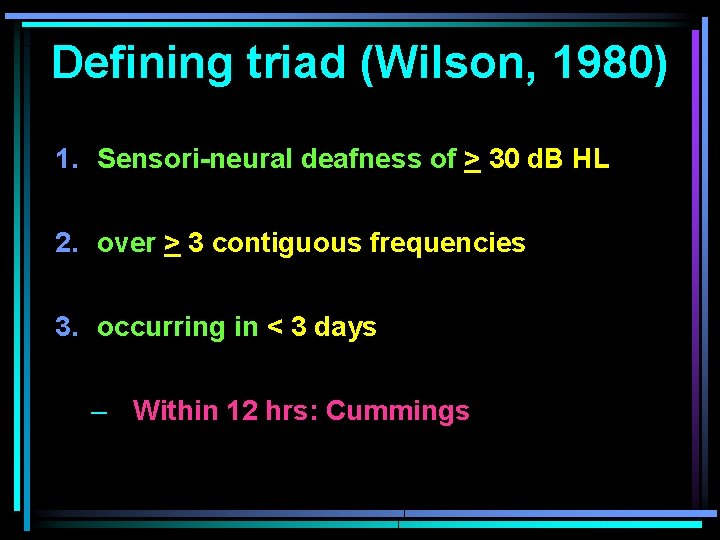
Defining triad (Wilson, 1980) 1. Sensori-neural deafness of > 30 d. B HL 2. over > 3 contiguous frequencies 3. occurring in < 3 days – Within 12 hrs: Cummings
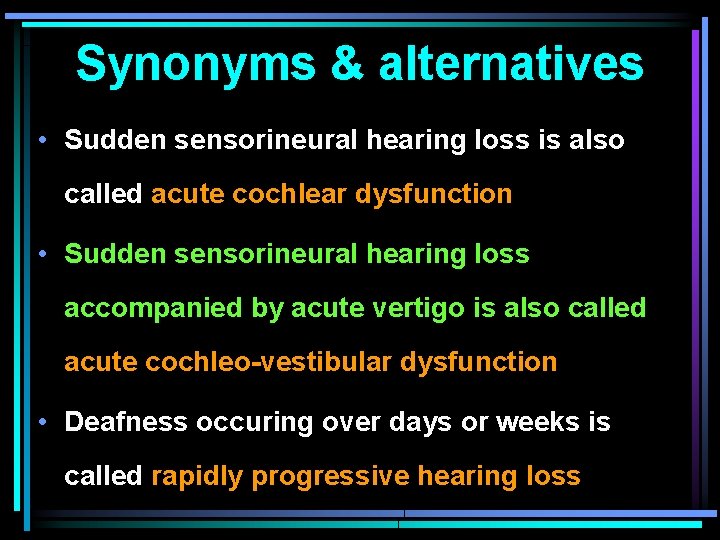
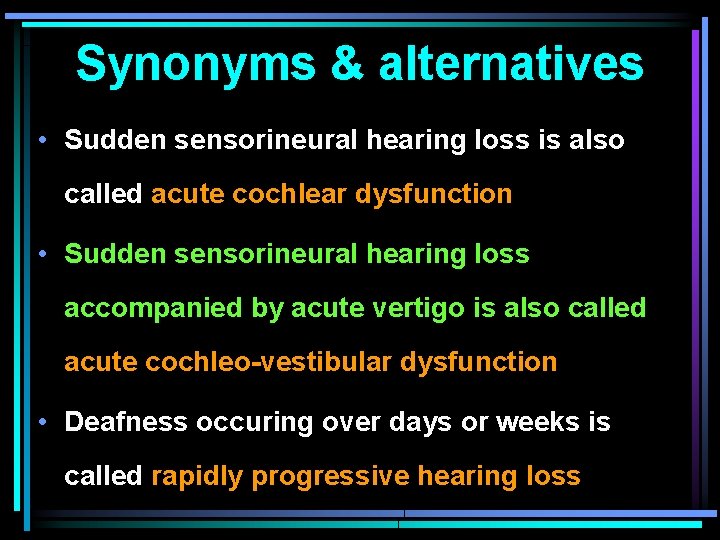
Synonyms & alternatives • Sudden sensorineural hearing loss is also called acute cochlear dysfunction • Sudden sensorineural hearing loss accompanied by acute vertigo is also called acute cochleo-vestibular dysfunction • Deafness occuring over days or weeks is called rapidly progressive hearing loss
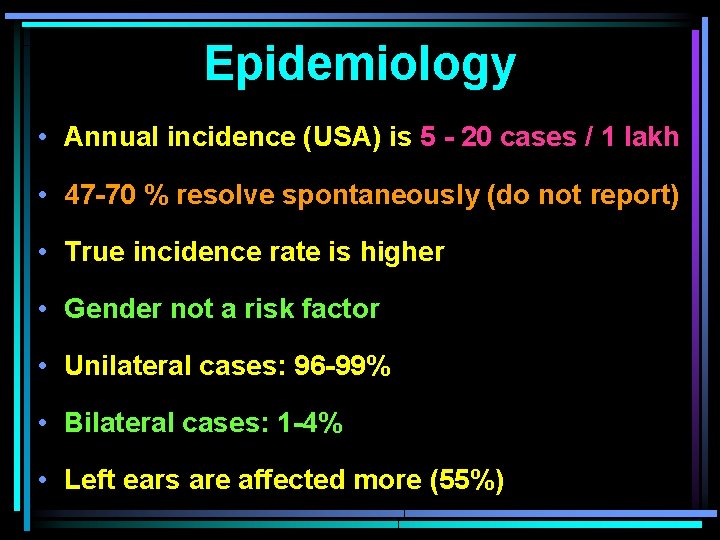
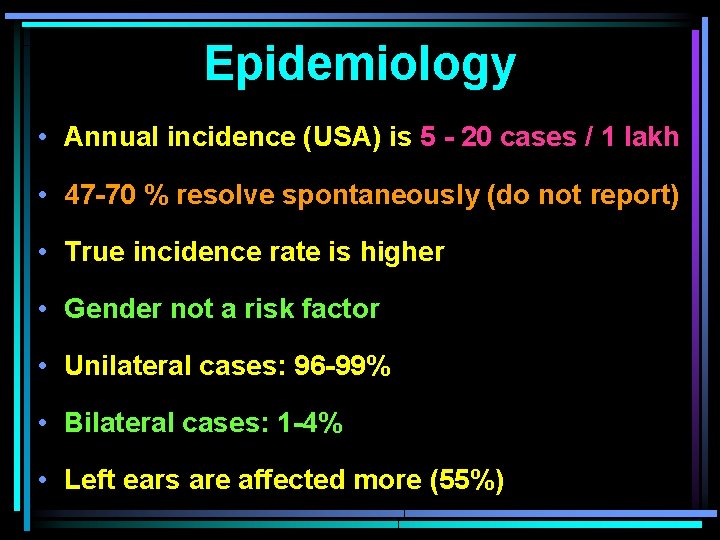
Epidemiology • Annual incidence (USA) is 5 - 20 cases / 1 lakh • 47 -70 % resolve spontaneously (do not report) • True incidence rate is higher • Gender not a risk factor • Unilateral cases: 96 -99% • Bilateral cases: 1 -4% • Left ears are affected more (55%)
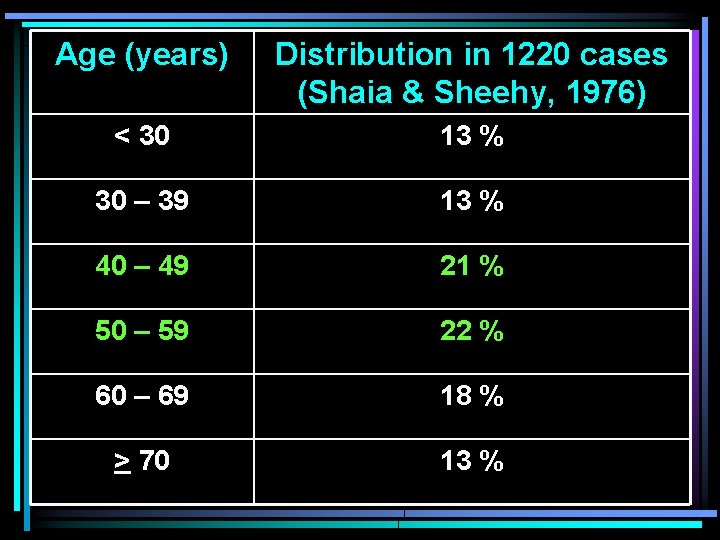
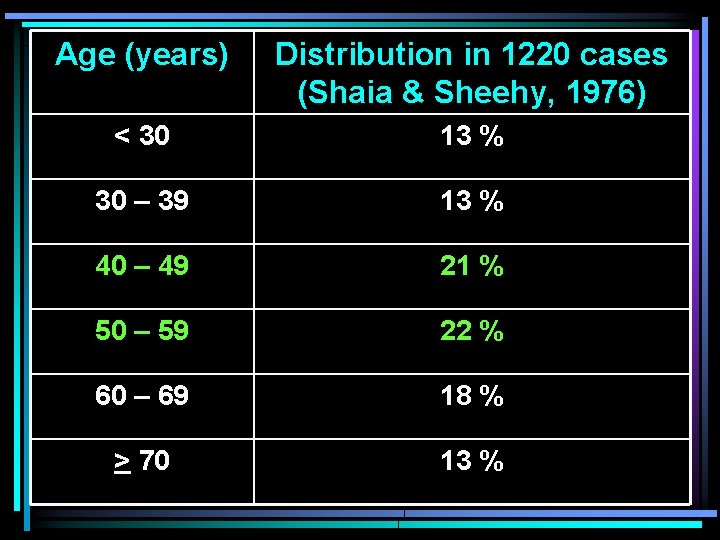
Age (years) Distribution in 1220 cases (Shaia & Sheehy, 1976) < 30 13 % 30 – 39 13 % 40 – 49 21 % 50 – 59 22 % 60 – 69 18 % > 70 13 %
Etiology 1. Idiopathic (single largest group: 90 - 95%) 2. Cochlear causes 3. Retro-cochlear causes 4. Miscellaneous • Psychogenic • Malingering
Criteria for idiopathic SSNHL • SSNHL present • No other cranial nerve involvement except eighth cranial nerve • No other etiology is known
Idiopathic SSNHL Various hypotheses are: 1. Labyrinthine viral infection (viral cochleitis) 2. Labyrinthine vascular compromise 3. Membrane rupture 4. Immune-mediated inner ear damage 5. Activation of cochlear nuclear factor kappa B
1. Labyrinthine viral Infection (20 – 40 %) • Herpes, mumps, measles, maternal rubella, cytomegalovirus, varicella zoster 2. Labyrinthine vascular compromise • caused by thrombosis, embolus, reduced blood flow, vasospasm • Western diet (rich in saturated fat), alcohol intake & tobacco smoking are predisposing factors
3. Membrane rupture (Simmons) • Pts hear pop sound before sudden deafness • Oval & round window perilymph fistulae leak perilymph into middle ear low perilymph pressure & relative endolymphatic hydrops • Rupture of intra-cochlear membranes mixing of perilymph & endolymph altering endo-cochlear potential
4. Immune-mediated inner ear damage • Antigen-antibody complex mediated destruction of cochlea • Cross-reacting circulating antibodies seen in 65 % pt of SSNHL. Associated conditions are: Cogan syndrome Relapsing polychondritis Systemic lupus erythematosus Polyarteritis nodosa Temporal arteritis
5. Activation of cochlear nuclear factor kappa B Merchant et al (2005) proposed this new theory Nuclear factor kappa B (NFҚ B) functions by: regulating inflammatory response + apoptosis regulating intracellular Ca & neuronal excito -toxicity NFҚ B activation is associated with destruction of spiral ganglion neurons & cochlear hair cells causing ISSNHL
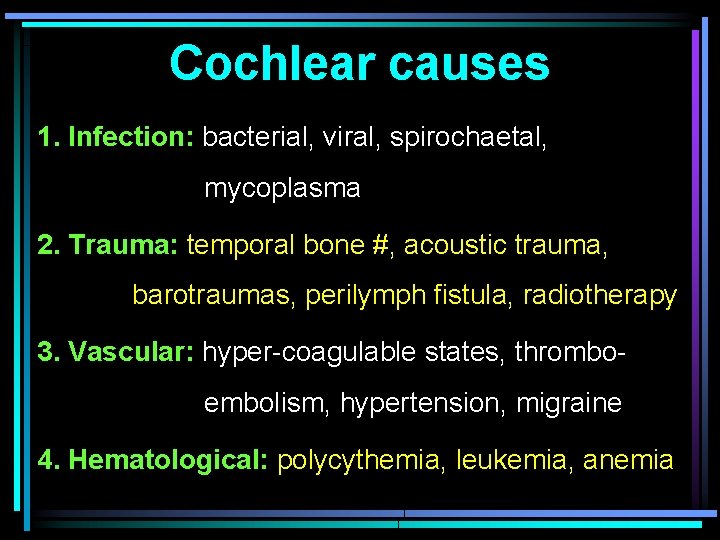
Cochlear causes 1. Infection: bacterial, viral, spirochaetal, mycoplasma 2. Trauma: temporal bone #, acoustic trauma, barotraumas, perilymph fistula, radiotherapy 3. Vascular: hyper-coagulable states, thrombo embolism, hypertension, migraine 4. Hematological: polycythemia, leukemia, anemia
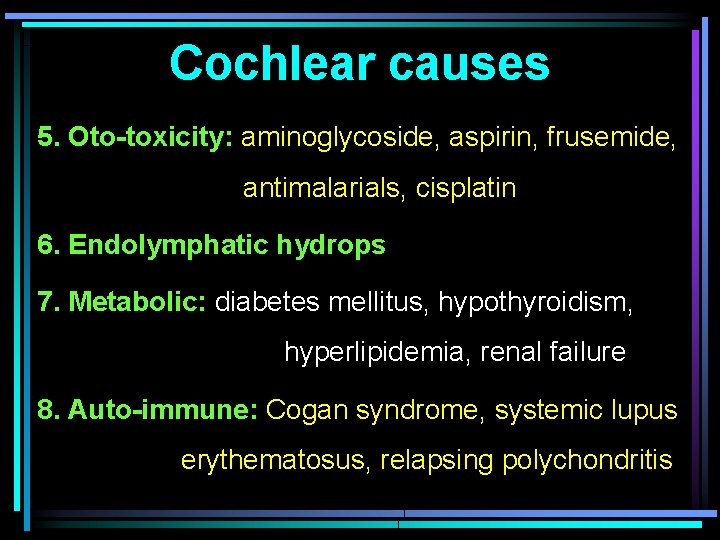
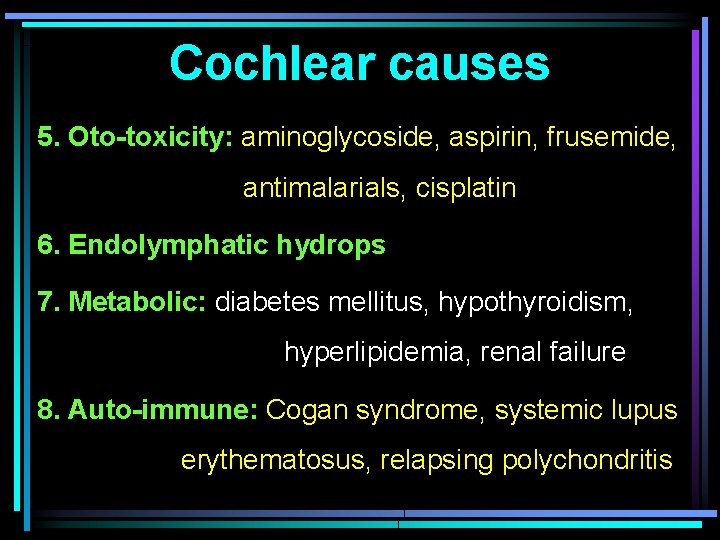
Cochlear causes 5. Oto-toxicity: aminoglycoside, aspirin, frusemide, antimalarials, cisplatin 6. Endolymphatic hydrops 7. Metabolic: diabetes mellitus, hypothyroidism, hyperlipidemia, renal failure 8. Auto-immune: Cogan syndrome, systemic lupus erythematosus, relapsing polychondritis
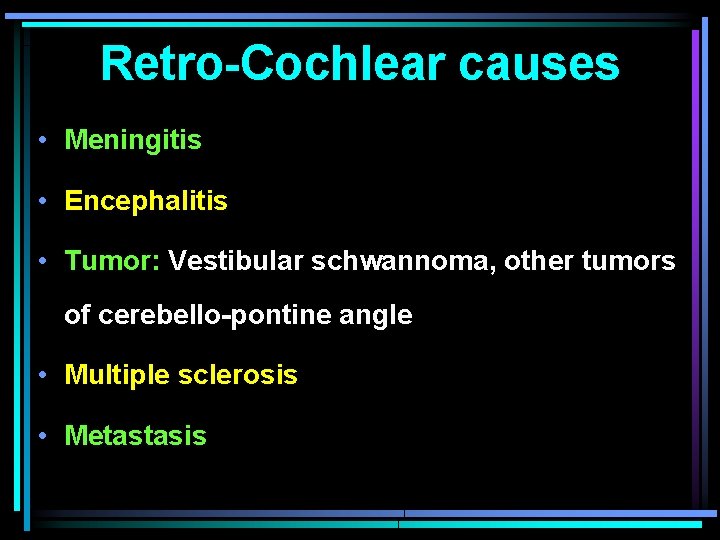
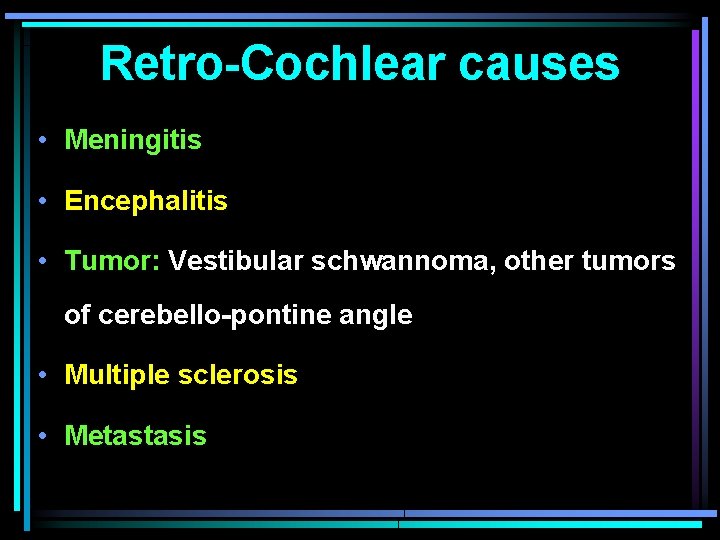
Retro-Cochlear causes • Meningitis • Encephalitis • Tumor: Vestibular schwannoma, other tumors of cerebello-pontine angle • Multiple sclerosis • Metastasis
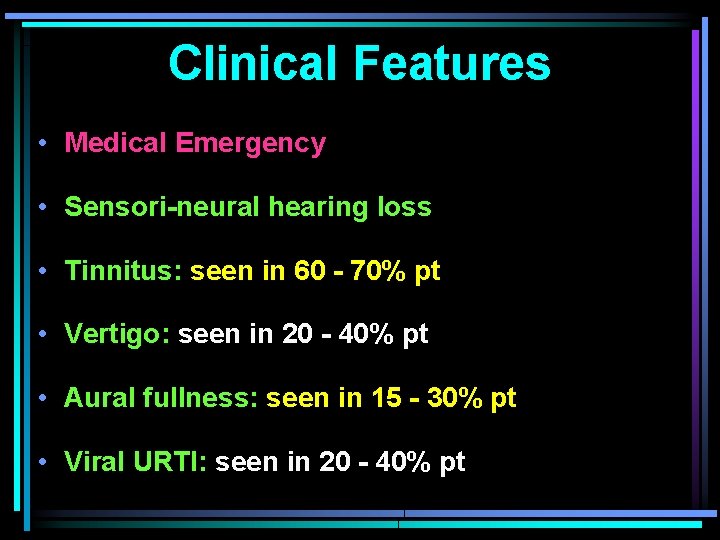
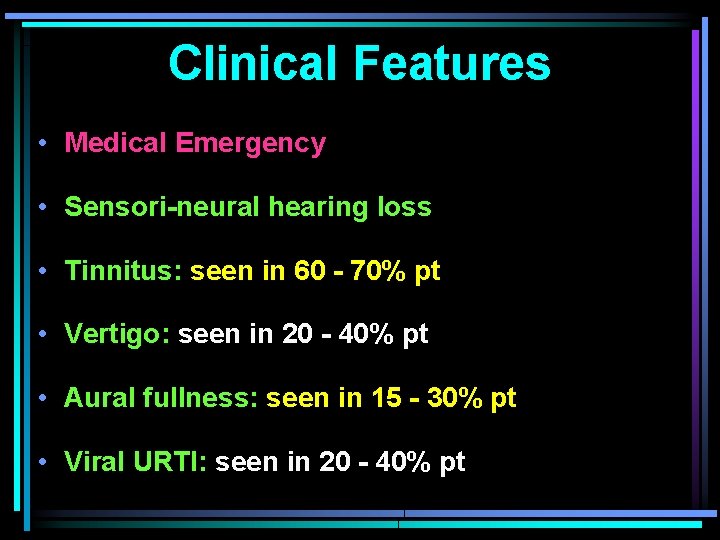
Clinical Features • Medical Emergency • Sensori-neural hearing loss • Tinnitus: seen in 60 - 70% pt • Vertigo: seen in 20 - 40% pt • Aural fullness: seen in 15 - 30% pt • Viral URTI: seen in 20 - 40% pt
Patient Evaluation
• Early diagnosis & Tx improves prognosis • Deafness: onset, duration, severity, previous HL • Associated vertigo / tinnitus / aural fullness • Exclude trauma (noise / baro / temporal bone #) • Exclude ototoxicity / DM / hypothyroidism / blood dyscrasia / hyperlipidemia / renal failure • Tuning fork tests & fistula test • Perform careful neurological examination

Basic Laboratory Investigations
1. Complete Blood Count + ESR: for infection 2. BT, CT, PT, a. PTT & INR: for bleeding disorder 3. VDRL, FTA-Abs, TPHA, TPI: for syphilis 4. ANA, Rh factor, other auto-antibody titre 5. T 3, T 4, TSH: for hypothyroidism 6. FBS & PPBS: for diabetes mellitus 7. Fasting lipid profile: for hyperlipidemia 8. Urea & Creatinine: for renal failure
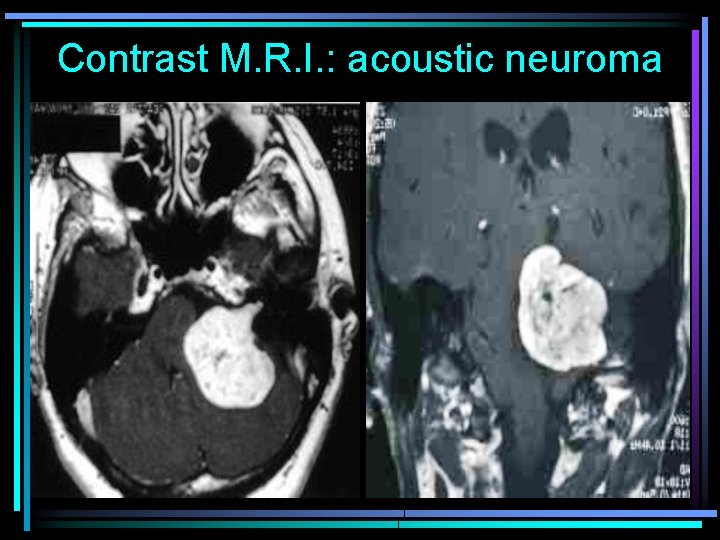
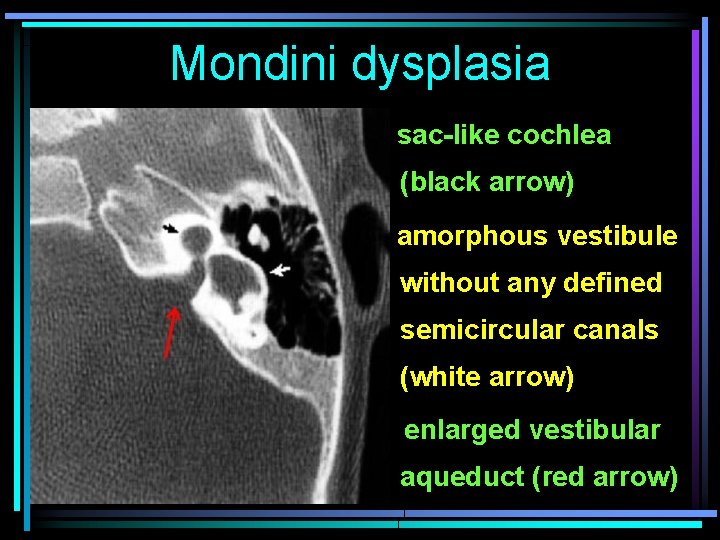
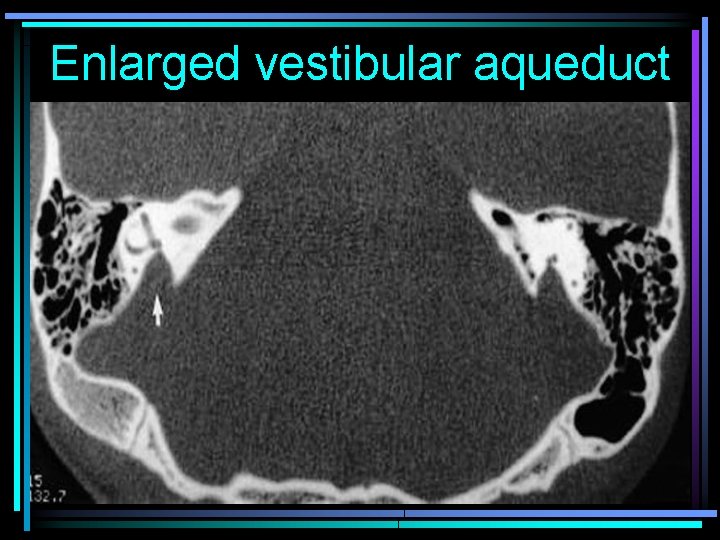
Imaging Studies 1. MRI with gadolinium contrast (gold standard): 1 -2% pt with ISSNHL have IAC or CPA tumors 3 -12% pt with acoustic neuroma have SSNHL 2. CT scan temporal bone + contrast • Detect anatomic defects (Mondini dysplasia or enlarged vestibular aqueduct syndrome)
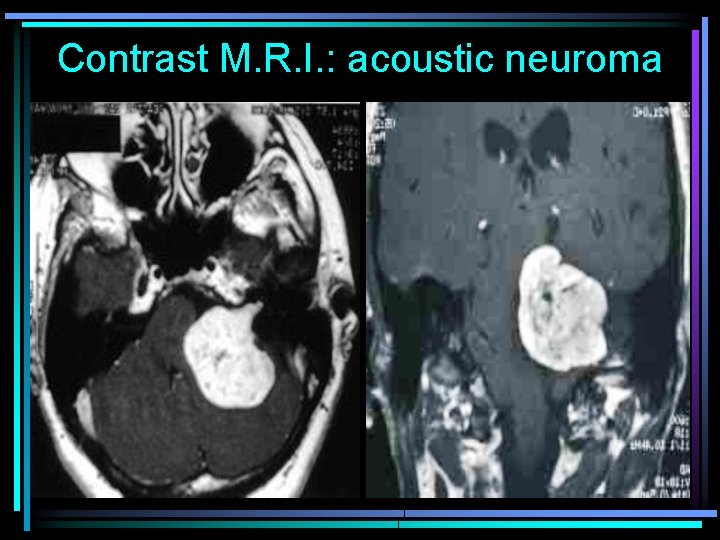
Contrast M. R. I. : acoustic neuroma
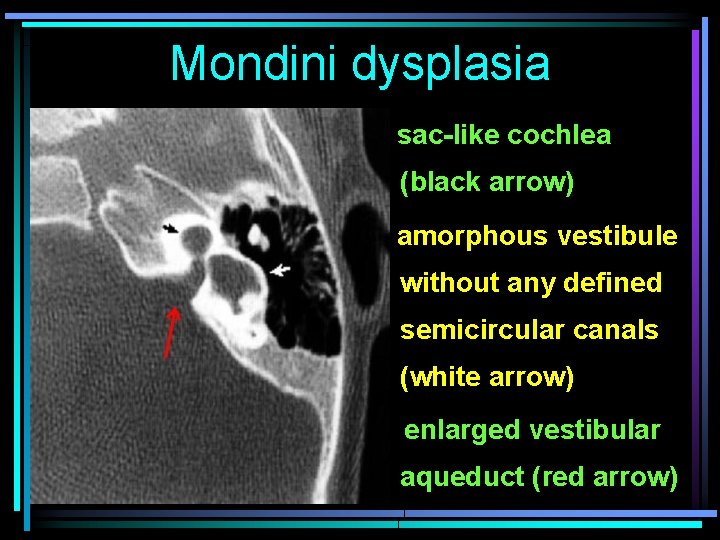
Mondini dysplasia sac-like cochlea (black arrow) amorphous vestibule without any defined semicircular canals (white arrow) enlarged vestibular aqueduct (red arrow)
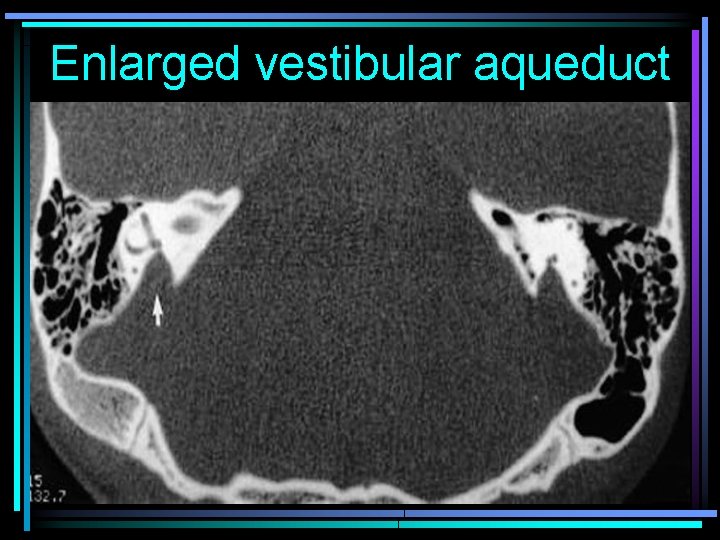
Enlarged vestibular aqueduct
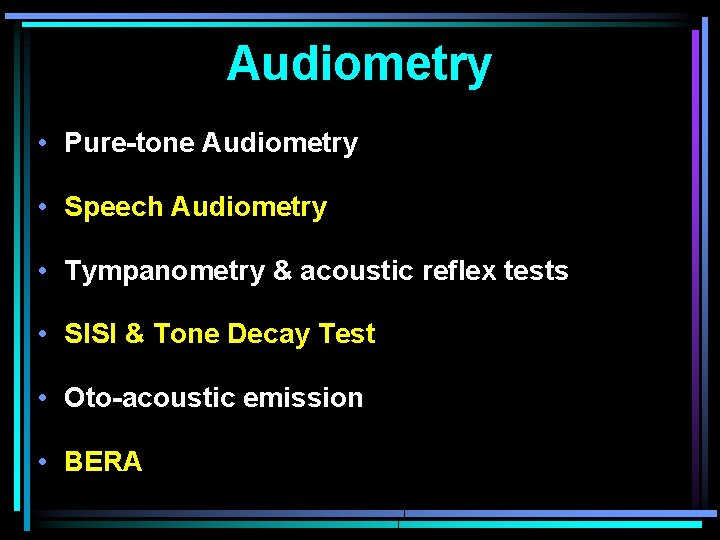
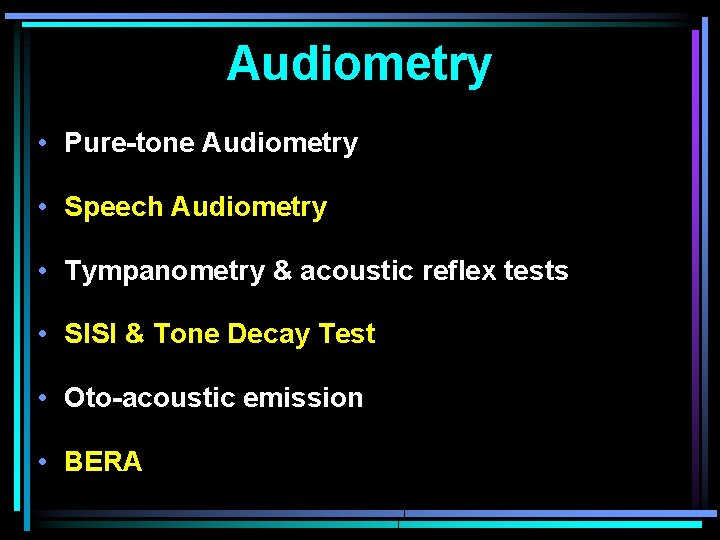
Audiometry • Pure-tone Audiometry • Speech Audiometry • Tympanometry & acoustic reflex tests • SISI & Tone Decay Test • Oto-acoustic emission • BERA
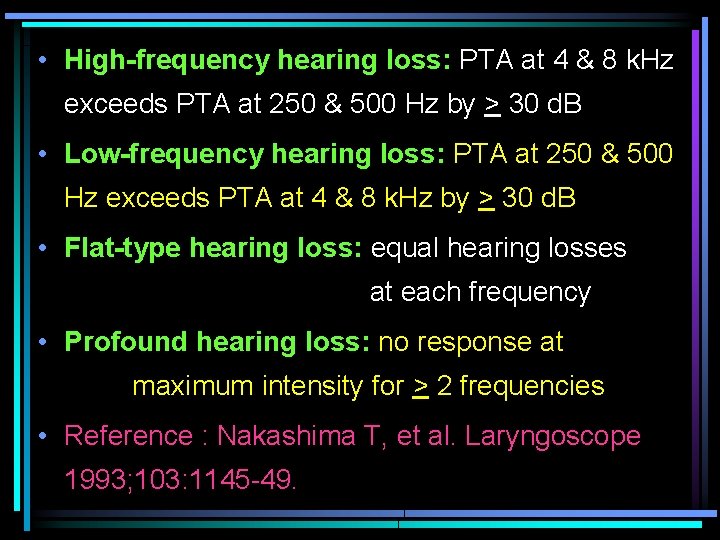
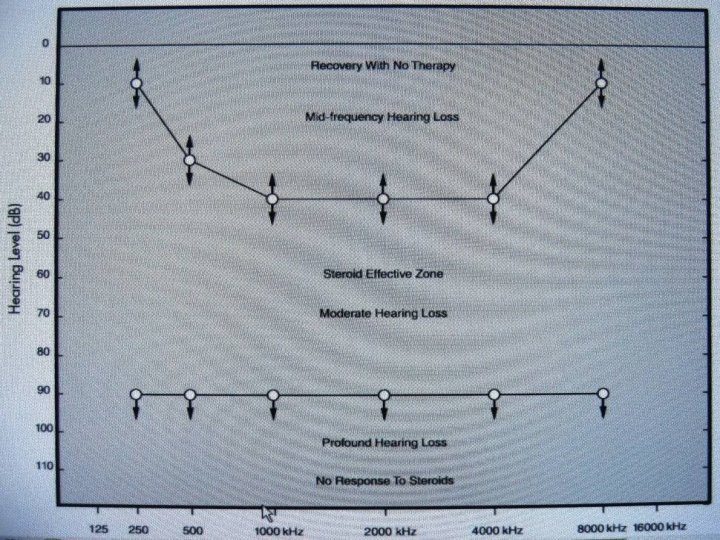
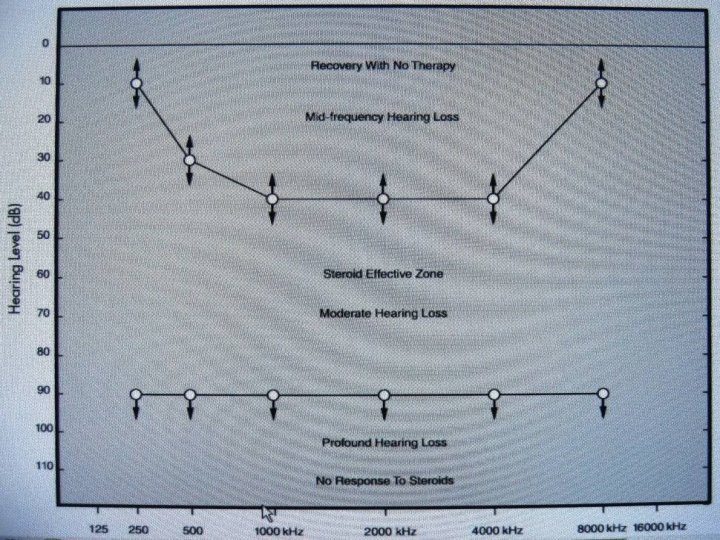
• High-frequency hearing loss: PTA at 4 & 8 k. Hz exceeds PTA at 250 & 500 Hz by > 30 d. B • Low-frequency hearing loss: PTA at 250 & 500 Hz exceeds PTA at 4 & 8 k. Hz by > 30 d. B • Flat-type hearing loss: equal hearing losses at each frequency • Profound hearing loss: no response at maximum intensity for > 2 frequencies • Reference : Nakashima T, et al. Laryngoscope 1993; 103: 1145 -49.
• Presence of OAE indicates preservation of some outer hair cell function • ABR reflects function of neural pathways • ABR & OAE results also assist in diagnosing psychogenic hearing loss & malingering • Vestibular tests are obtained when indicated by history & physical examination
Treatment
Treatment options (a) Vasodilators (b) Rheologic agents (c) Anti-inflammatory agents (Steroids) (d) Anti-viral agents (e) Diuretics (f) Hyperbaric oxygen (g) Surgery
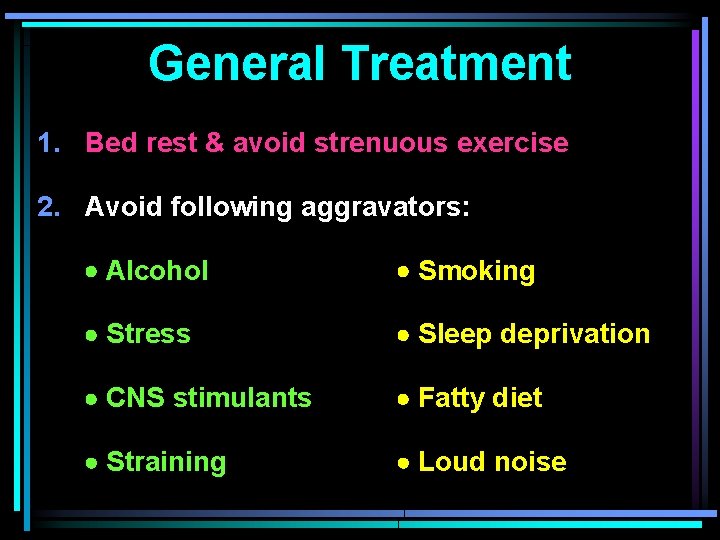
General Treatment 1. Bed rest & avoid strenuous exercise 2. Avoid following aggravators: Alcohol Smoking Stress Sleep deprivation CNS stimulants Fatty diet Straining Loud noise
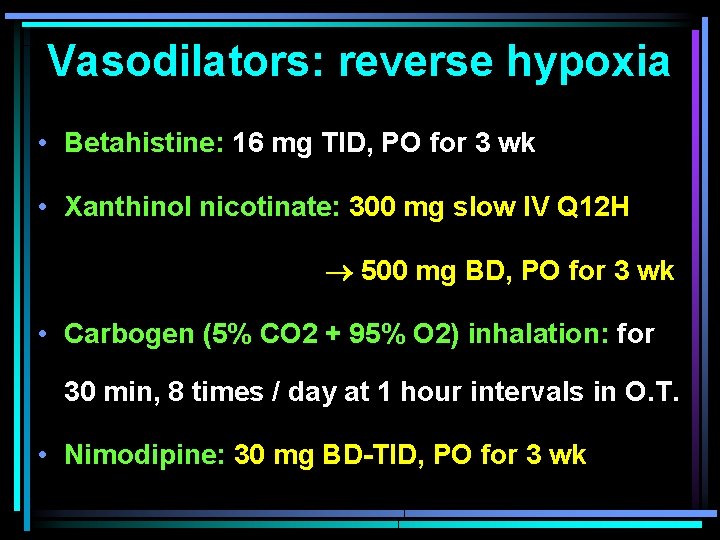
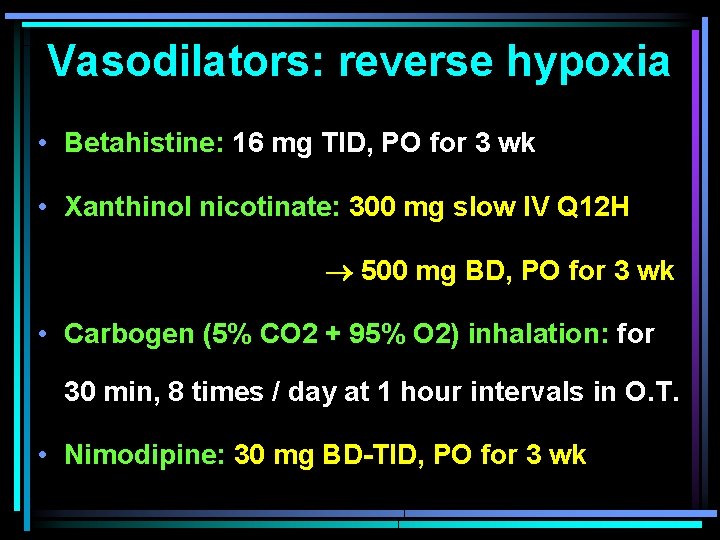
Vasodilators: reverse hypoxia • Betahistine: 16 mg TID, PO for 3 wk • Xanthinol nicotinate: 300 mg slow IV Q 12 H 500 mg BD, PO for 3 wk • Carbogen (5% CO 2 + 95% O 2) inhalation: for 30 min, 8 times / day at 1 hour intervals in O. T. • Nimodipine: 30 mg BD-TID, PO for 3 wk
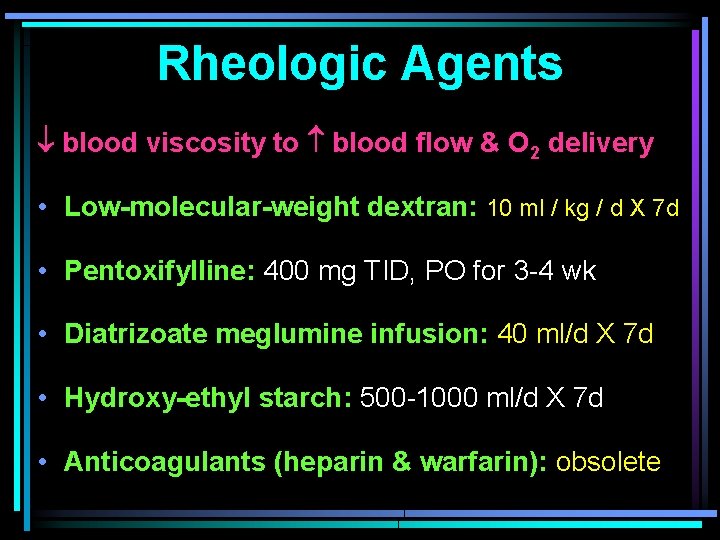
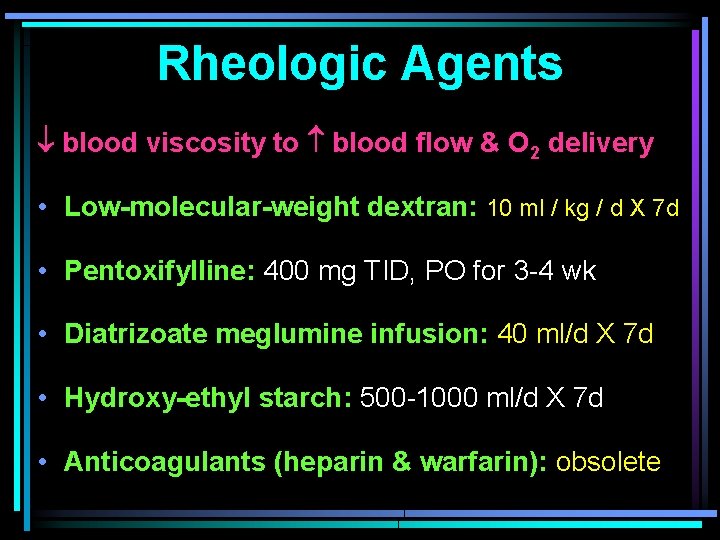
Rheologic Agents blood viscosity to blood flow & O 2 delivery • Low-molecular-weight dextran: 10 ml / kg / d X 7 d • Pentoxifylline: 400 mg TID, PO for 3 -4 wk • Diatrizoate meglumine infusion: 40 ml/d X 7 d • Hydroxy-ethyl starch: 500 -1000 ml/d X 7 d • Anticoagulants (heparin & warfarin): obsolete
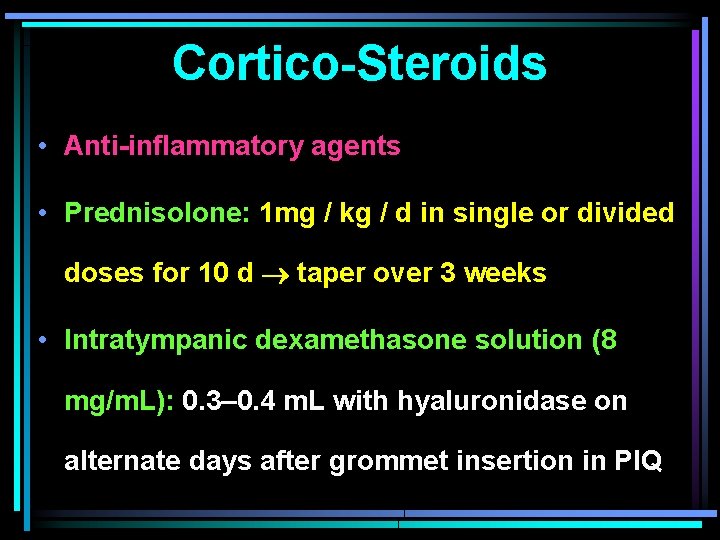
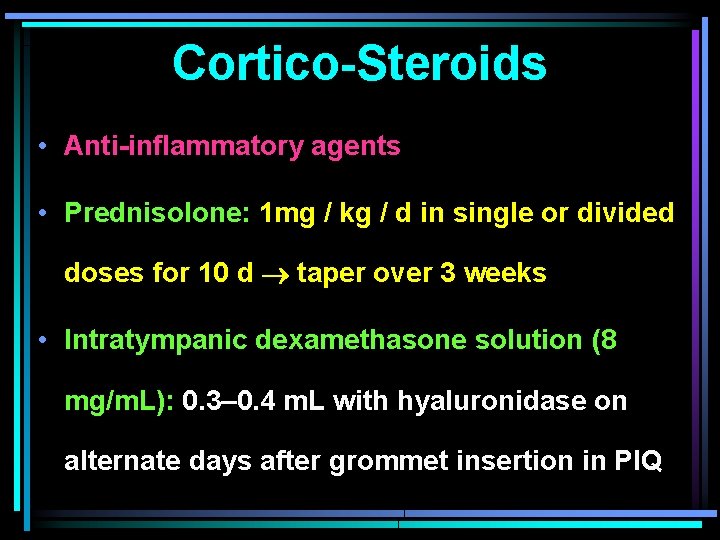
Cortico-Steroids • Anti-inflammatory agents • Prednisolone: 1 mg / kg / d in single or divided doses for 10 d taper over 3 weeks • Intratympanic dexamethasone solution (8 mg/m. L): 0. 3– 0. 4 m. L with hyaluronidase on alternate days after grommet insertion in PIQ

Grommet in P. I. Q.

Post-steroid recovery
Side-effects of Steroids • Hyperglycemia • Hypertension • Gastric ulceration • Osteoporosis • Flaring of infection & delayed wound healing • Psychiatric disturbance (insomnia, euphoria) • Weight gain & trunk obesity

Anti-virals & Diuretics • Anti-virals • Acyclovir: 800 mg PO, 5 times / day for 7 days • Famciclovir: 250 mg PO, TID for 7 days • Diuretics • Used in SSNHL due to endolymphatic hydrops • Hydrochlorothiazide: 25 mg PO, BD for 3 -4 wk
Hyperbaric oxygen • Consists of exposure to 100% oxygen at pressure of 250 k. Pa for 60 minutes in a multiplace hyperbaric chamber along with high doses of gluco-corticoids • Best results achieved if treatment started early
Surgery • Repair of oval & round window perilymph fistulae has been used in cases of ISSNHL associated with positive fistula test or history of recent trauma or barotrauma • No standard methods are detailed
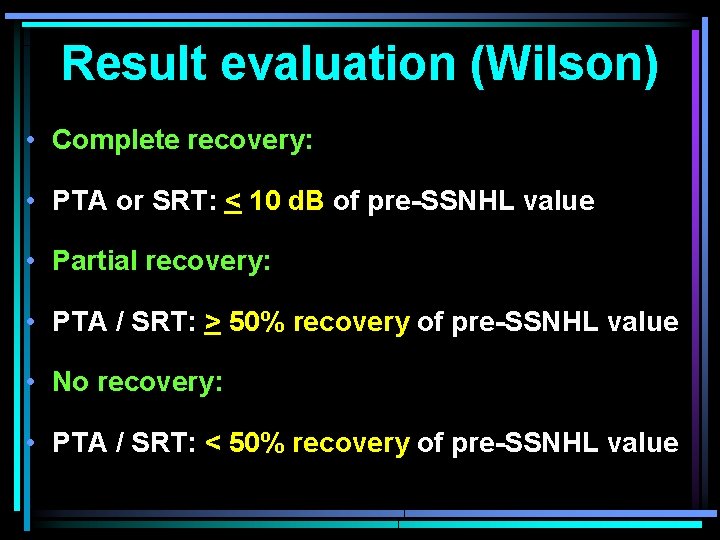
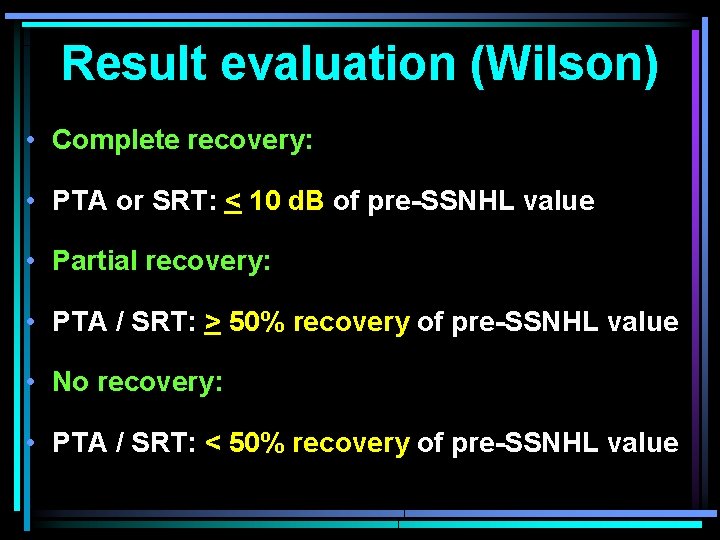
Result evaluation (Wilson) • Complete recovery: • PTA or SRT: < 10 d. B of pre-SSNHL value • Partial recovery: • PTA / SRT: > 50% recovery of pre-SSNHL value • No recovery: • PTA / SRT: < 50% recovery of pre-SSNHL value
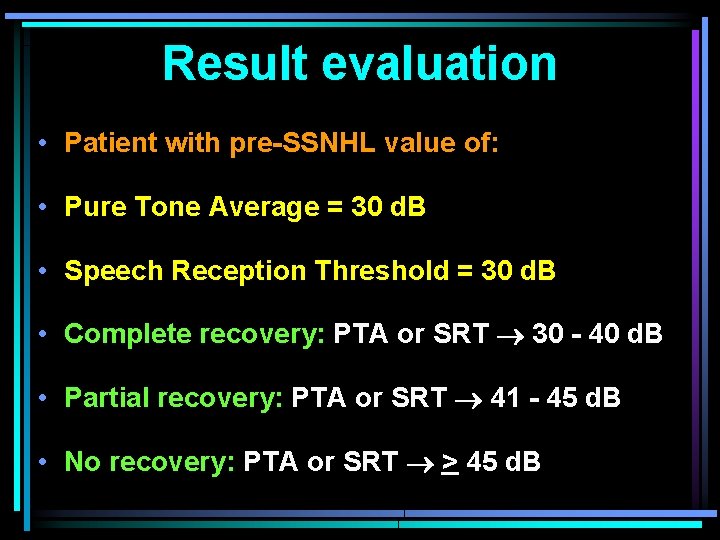
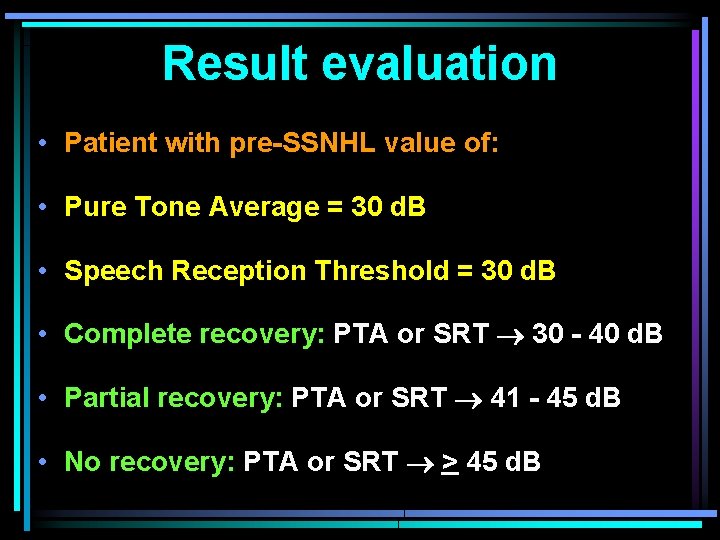
Result evaluation • Patient with pre-SSNHL value of: • Pure Tone Average = 30 d. B • Speech Reception Threshold = 30 d. B • Complete recovery: PTA or SRT 30 - 40 d. B • Partial recovery: PTA or SRT 41 - 45 d. B • No recovery: PTA or SRT > 45 d. B
Spontaneous Recovery • Spontaneous recovery rates for SSNHL range from 47 - 70%, combining categories of complete & partial recovery • Most spontaneous recoveries occur within 2 weeks
Results • No high-quality, randomized, controlled trial shows efficacy of any medical therapy • Most studies don't show significant beneficial effect of vasodilators, acyclovir, rheological agents, hyperbaric oxygen over placebo • Corticosteroid therapy is only accepted therapy for ISSNHL. Recovery rates = 40 - 60%
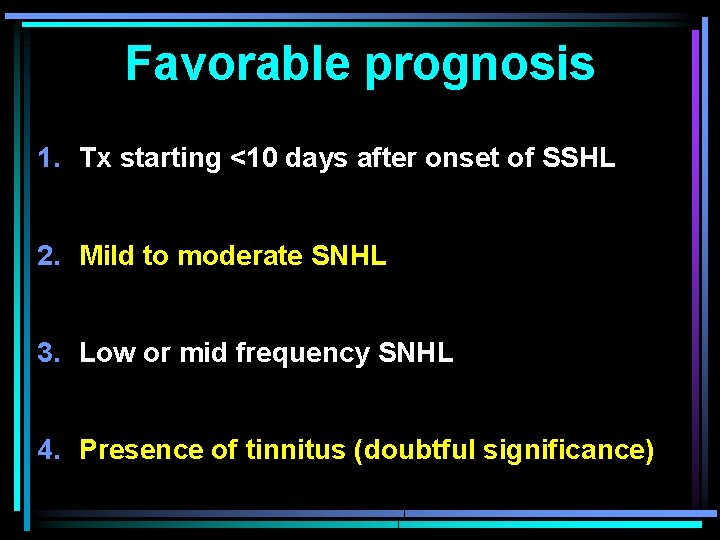
Favorable prognosis 1. Tx starting <10 days after onset of SSHL 2. Mild to moderate SNHL 3. Low or mid frequency SNHL 4. Presence of tinnitus (doubtful significance)
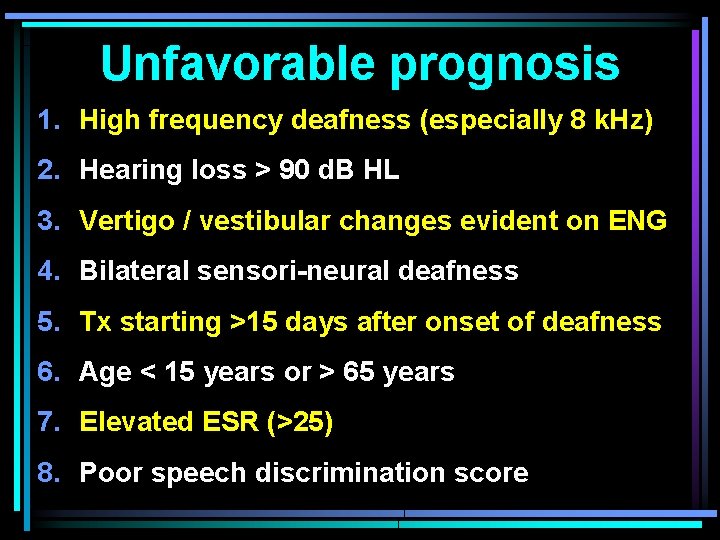
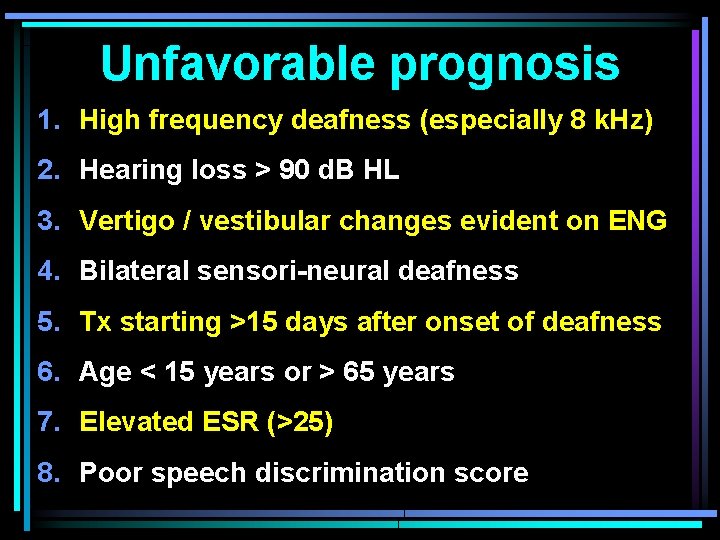
Unfavorable prognosis 1. High frequency deafness (especially 8 k. Hz) 2. Hearing loss > 90 d. B HL 3. Vertigo / vestibular changes evident on ENG 4. Bilateral sensori-neural deafness 5. Tx starting >15 days after onset of deafness 6. Age < 15 years or > 65 years 7. Elevated ESR (>25) 8. Poor speech discrimination score
Further Study

• Leong, A. C. et al. (2007). Sudden hearing loss - A 12 minute consultation. Clinical Otolaryngology. 32: 391– 394 • Xenellis J. et al. (2006). Idiopathic sudden sensorineural hearing loss: prognostic factors. J. L. O. 120, 718– 724 • Xenellis J. et al. (2006) Intra-tympanic steroid treatment in ISSNHL. Otolaryngol. Head Neck Surg. 134, 940– 945 • Aoki D. et al. (2006) Evaluation of superhigh-dose steroid for SSNHL. Otolaryngol. Head Neck Surg. 134, 783– 787 • Bennett M. et al. (2005) Hyperbaric oxygen therapy for ISSNHL & tinnitus: J. Laryngol. Otol. 119: 791 -798, • Wilson W. et al. (1980) The efficacy of steroids in the treatment of ISSNHL. Arch. Otolaryngol. 106, 772– 776

Thank You