Student Induction Section 1 Clinical Governance Information Governance














- Slides: 102
Student Induction Section 1 Clinical Governance Information Governance Safeguarding Fire Safety Section 2 Infection Prevention & Control Datix Reporting Customer Service Medicines Management
Clinical Governance Section 1 Clinical Governance Information Governance Safeguarding Fire Safety

Clinical Governance COURSE OBJECTIVES o What Clinical Governance is; o History of Clinical Governance; o Service User involvement; o PALS involvement; o Use of clinical information; o NICE guidance; o Useful contacts. Definition of Clinical Governance “A framework through which NHS organisations are accountable for continuously improving the quality of their services and safeguarding high standards of care by creating an environment in which excellence in clinical care will flourish". Clinical Governance What is Clinical Governance? Clinical Governance is about providing a patient-centred, accountable, safe and high quality service in an open and questioning environment. Clinical Governance questions traditional structures and ways of doing things and creates a consistent and sustained approach to improving the quality of healthcare.
Definition of Quality There have been several definitions of quality care in the last 20 years. The definition below was adopted by the NHS in 2008. Quality treatment and care has three elements which must come together to ensure the delivery of HIGH QUALITY CARE: Effectiveness of the treatment and care provided to patients – measured by clinical outcomes and patient related outcomes The Safety of treatment and care provided to patients The experience patients have of the treatment and care they receive (Lord Darzi, NHS Next Stage Review, Leading Local Change, May 2008. ) The NHS Constitution (2010) enshrines the right of people to receive high quality care and treatment Clinical Governance
History of Clinical Governance 1997 : Labour Government in the White Paper ‘The New NHS’ – Modern & Dependable abandoned the internal market and introduced a statutory duty for quality improvement that was called CLINICAL GOVERNANCE. 1999: Trust Boards assumed a legal responsibility for quality of care that is equal in measure to their other statutory duties. Clinical governance is the mechanism by which that responsibility is discharged 2003: This “Duty of Quality” is a legal requirement and is found in the Health and Social Care (Community Health and Standards) Act 2003: 2004: Health Commission established to improve the quality of services in the NHS 2009: Department of Health. : A First Class Service 2009: Standards for Better Health Declaration 2009: Care Quality Commission to regulate National Standards across health and social care providers
Key Components of Clinical Governance Person centred care with service user involvement Visible Trust Board Level leadership Use of Clinical Information; o Patient safety and robust risk management; o Clinical Audit; o Research & Development o Clinical Effectiveness o Staffing & Management; Service User Involvement The Legislative Framework to ‘put patients at the centre of care’ was announced through the NHS Plan -Section 11 of the Health and Social Care Act 2001; This act came into force on 1 st January 2003 and states that all Trust’s must, as a matter of course, consult and involve patients and members of the public; Consult not just when a major change is proposed, but in the on going planning and development and the delivery of services day to day.
Feedback from Service Users Clinical Governance We must actively seek feedback from our service users and make sure that action and changes occur in response to this feedback. Feedback can come from a variety of sources: o o o o Sources of Feedback Complaints / compliments; comment cards National Surveys (including the National Patients Survey); Local Surveys; Advocacy services The Patient Advice and Liaison Service (PALS); Patient’s experience group (PEx). Involvement in the annual Business Planning cycle along with staff and other stakeholder groups Service user son recruitment panels Staff induction training for staff Take it to the Top Forums give direct access to the Chief Executive and Team Mystery Shoppers Focus Groups
Question Clinical Governance Continue Feedback can come from a variety of sources, including … Advocacy Services National Surveys Patient Experience Groups (Pex) Focus Group Everything Mentioned
Trust Board Leadership Clinical Governance Regular visits from executive and non-executive directors to clinical areas to discuss element of quality and safety: o Patient safety walk rounds o Director CQC spot checks o Improvement programmes led by directors and senior management. PALS Involvement Patients, relatives or carers may sometimes need help, advice or support; o PALS will provide confidential advice and support, helping with any concerns about the care provided by the Trust; o PALS can guide patients, relatives and carers through the different services available
Use of Clinical Information – Evidence Clinical Governance requires evidence of effective patient care and safe and appropriate services; Accurate, meaningful and reliable information provides a vital support to quality improvement processes; Information comes from many different sources including: o Routine monitoring and reports o Clinical Audit o Essence of Care Benchmarks o Productive Series outcomes o Patient & Carers surveys o Ward Dashboards

Question Clinical Governance Continue Clinical Governance requires evidence of effective patient care and safe and appropriate services. This evidence can come from: Clinical Audit Ward Dashboards Routine Monitoring & Reports Everything Mentioned
Risk Management Clinical Governance People Safety is about ensuring that people in our care receive high quality care and treatment by the right people at the right time in the right place. There are risks associated with all episodes of care. Risk Management is about minimising risks to patients and staff; It is a positive function and central to the quality of care we give to patients Risks need to be avoided or controlled; We do this by carrying out a Risk Assessment and agreeing the level of seriousness attached to each risk; o Actions are then taken on the result of the Risk Assessment to ensure everyone's safety. o Where risks cannot be completely removed we aim to minimise the harm caused by any adverse incidents. Risk Management is about "stopping bad things from happening“ o o o
Clinical Audit Clinical Governance As part of local arrangements for clinical governance, all NHS organisations are required to have a comprehensive programme of quality improvement activity that includes clinicians participating fully in audit; Clinical audit is the component of clinical governance that offers the greatest potential to assess the quality of care routinely provided for NHS users – audit should therefore be at the very heart of clinical governance systems; o National Institute for Health & Clinical Excellence (NICE). o Clinical Audit is part of the CQUIN and Quality Account work undertaken in local areas in partnership with commissioners Research & Effectiveness – Evidence Based Practice The work that we carry out daily should be based on accepted good practice. It should be proven to be appropriate and effective by people with knowledge and expertise. This is evidence based practice; The guidance provided by the National Institute for Health & Clinical Excellence (NICE) is a good example of evidence based practice.
NICE Guidance Clinical Governance NICE develop and distribute guidelines, technology appraisals (Drugs and equipment) and quality standards on a national level. These guidelines are all evidence based and well researched before distribution. Each Trust within the country is responsible for evidencing compliance with the NICE Guidance. The Head of Clinical Effectiveness has responsibility to ensure that we are applying all the NICE guidelines, where appropriate. Local NICE Groups have responsibility to ensure that where guidance is applicable there is an achievable action plan in place monitored within the service and progress sis reported to the Clinical Effectiveness Group (CEG) The Clinical Effectiveness Group (CEG) is responsible for ensuring that key decisions are made in relation to NICE guidelines.
Question Clinical Governance Continue Local NICE Groups have responsibility to ensure that where guidance is applicable there is an achievable action plan in place monitored within the service and progress is reported to the Clinical Effectiveness Group (CEG). True False
Staffing & Management Clinical Governance The Trust aims to: o have staff that are well trained and have appropriate skills to provide a high quality service through: Training; o Education; o Appraisal; o Clinical & Managerial Supervision Education & Training The Trust aims to: o Develop staff, at all levels, to their full potential, as a means of providing high quality, efficient and effective services and individual patient care; o Become a centre of excellence for The purpose of the Care Quality Commission is lifelong learning which is fundamental to to promote improvements in the quality of the continuous improvement of services healthcare and public health, through to patients and to fulfilling the local and independent, authoritative, patient-centred national objectives; assessments, of the performance of those who o Supporting personal growth, career provide services. development and employability, against a background of on going organisational From 1 April 2009 the Care Quality Commission change. brought together the Commission for Social Care Inspection, the Healthcare Commission and the MH Act Commission All Trusts are monitored by the Care Quality Commission
Information Governance Section 1 Clinical Governance Information Governance Safeguarding Fire Safety
Information Governance COURSE OBJECTIVES On completion of the Information Governance module, you will understand: • • Duty of Confidentiality Data Handling & Security Best Practice Guidelines Information Governance Toolkit Confidential/sensitive/corporate Information Sharing & Privacy Impact Assessments Consent Information Governance is the framework structures and processes that ensure the security, confidentiality and integrity of the Trust’s data information about it’s patients and employees, in particular personal sensitive and corporate information. It allows the Trust and individuals to: • Ensure that personal information is dealt with legally, securely, efficiently and effectively • Provides a framework to bring together all requirements, standards and best practices that apply to the handling of all information • Focus on settling standards and giving the Trust tools to achieve them • To be consistent in the way we handle personal/corporate information • Lead improvements in information handling, patient / public confidence in the Trust and employee training and development
Duty of Confidentiality Information Governance All employees of the Trust who record, handle, store or otherwise come across information, have a common law duty of confidence to patients and staff. We need to remember: • Keep personal information private. • Ensure confidential information is not unlawfully or inappropriately accessed. • Any confidentiality breaches need to be reported to your line manger and Information Governance. • Before disclosing information ensure you know who you are communicating with. • Comply with policies and procedures. • Do not leave manual records unattended. • Dispose of confidential information in the appropriate manner. • Ensure confidential information is held, stored and transported securely. Please note – this applies equally to those such as student and trainees, bank, agency and contracting staff, on temporary placements Information Governance helps all employees to manage person identifiable information so that all patients and staff know their records will not be disclosed inappropriately, which will: • Give individuals greater trust in our working practices. • Encourage individuals to be more open in sharing important personal details. • Ensure they will receive the best quality care.
Person Identifiable/sensitive & Corporate Information Person Identifiable Information: • Name • Address • Postcode • DOB • NHS number • NI number Sensitive Information: • Ethnic backgrounds • Political views • Sexual preferences • Gender • Criminal offences • Medical conditions Information Governance Corporate Information: Information that is not staff or patient related but could cause harm or damage to the organisation, this could be: • Set of minutes • Financial information • Tenders being agreed • Reports • Upcoming consultations
Information Governance Transferring Confidential Information Offsite – Paper • Confidential information should only be transferred, if absolutely necessary and with managers authorisation • Minimal amounts of data required • Where possible should be anonymised • Lockable carriers must be used when carrying confidential documentation (bus, walking, train, cycling etc) • Sealed medical records bags can also be used to transfer confidential information • Throughout transportation all information must be placed in the boot of the car and removed to a place of security at destination For further guidance please refer to the Records Management Procedure – Transportation of Records - Section 6. 3 Transferring Confidential Information Offsite – Electronic • Confidential information should only be transferred, if absolutely necessary • Minimal amount of data required • All devices must be encrypted and password protected • USBs, CDs, DVDs, mobile phones, laptops, digital Dictaphones etc should NOT be used to store any confidential information, only to transfer information if necessary and authorised • Once data has been transferred please ensure it is deleted and wiped as, per Trust policy states

Data Handling, Security and Best Practice Guidelines Information Governance Best Practice Guidelines – Confidential Waste • All confidential waste should be disposed either using a cross cut shredder or placing in the blue confidential waste bins • Never put confidential information in black refuse bags/recycling bins • Confidential waste paper should not be used as scrap paper • If you do not have the facility to dispose of confidential information securely at home, please bring back into the office for appropriate disposal. Best Practice Guidelines – Clear Desk Policy Operate a clear desk policy by ensuring all person identifiable/ sensitive/confidential information is locked away as appropriate, especially important when hot desking or working in an open plan office.
Data Handling, Security and Best Practice Guidelines Information Governance Best Practice Guidelines – Photocopying • Do not make excessive copies of confidential information; • Do not leave confidential information on the photocopying machine; • Regularly check/update your distribution list to ensure copies are not sent to staff who have left the Trust. Best Practice Guidelines – Post • PO box return labels to be displayed on external post • Ensure marked ‘Private & Confidential’ • Double check full postal address of recipient • Choose secure method of sending confidential information through external post (recorded delivery or private courier) • When necessary ask recipient to confirm receipt • Ensure incoming confidential post is handled appropriately. Best Practice Guidelines – Person Ensure you hold confidential conversations in an appropriate place. Inappropriate areas include: corridors, open plan offices etc Gain patient consent before sharing their personal information with relatives/friends.
Data Handling, Security and Best Practice Guidelines Information Governance Best Practice Guidelines – Email • No person identifiable/sensitive/ confidential information is to be detailed in the body or subject heading of the email • Confidential information is to be sent as a password protected attachment or transferred via NHS. net to NHS. net • Passwords to be sent by text or phone (wherever possible) or in a separate email (leave suitable time between emails) Best Practice Guidelines – Faxing Do not fax personal or confidential information unless absolutely necessary and ensure the Safe Haven Fax procedure is followed. • Call individual to make them aware you are sending a fax • Send cover sheet • Confirm this has been received • Continue to fax the information by pressing redial • Ask individual to confirm receipt once received.
Data Handling, Security and Best Practice Guidelines Information Governance Best Practice Guidelines – Voicemails for Clients • Only state forename and number • Do not state full name, team, service or organisation unless agreed • Consent needs to be obtained before leaving a voicemail Best Practice Guidelines – Telephone When receiving calls requesting personal information: • Verify the identity of the caller • Ask reason for request • If in doubt, call the individual back and seek advice from your line manager or the Information Governance Team / Data Protection Officer Best Practice Guidelines – Office • Remember to lock and secure the office when left unattended and at the end of the day • Close and lock all windows • Close any blinds/curtains • Set the intruder alarm system (if fitted) • Remember to wear your ID badge • Ensure clear desk policy is followed • Lock computer screens when left unattended (Ctrl, Alt, Delete)
Information sharing and Consent Information Governance Any confidential information that is going to be transferred needs to be shared in line with the Data Protection Act 1998 and Caldicott Principles as outlined below: Data Protection Act 1998 Principles: 1) Processed fairly and lawfully 2) Processed for specified purposes 3) Adequate, relevant and not excessive 4) Accurate and up to date 5) Not kept for longer than necessary 6) Processed in accordance with the rights of the data subject 7) Protected by appropriate security 8) Not transferred outside the EEA without adequate protection 9) The right to be forgotten (still being considered by the Government – seek guidance from the IG Team Caldicott Principles: 1) Justify the purpose of using confidential information 2) Only use it when absolutely necessary 3) Use the minimum required 4) Allow access on a strict need to know basis 5) Understand your responsibility 6) Understand comply with the law 7) Duty of confidentiality – in the best interest of the patient
Information Governance Information Sharing Agreements Where you are considering sharing information or are involved in arranging information sharing agreements you must include the Information Governance Team at the earliest opportunity, and an Information Sharing Agreement (ISA) will be distributed for completion. Privacy Impact Assessments Where a new system/process or change to an existing system/process has been identified it is necessary the Information Governance Team are informed to ensure a Privacy Impact Assessment has been completed. This will then allow the Information Governance Team to determine if there any confidentiality, consent, privacy, security or data protection issues related to the new/changed/system/process. Patients need to be informed how their information will be used and shared. It is therefore important consent is gained and understood. Consent for Children & Young People Children and young people must be assessed as Fraser or Gillick competent. When Consent Doesn’t Need to be Gained • Public interest • Court order
Human Rights Act & Computer Misuse Act Information Governance Human Rights Act: • Came into force in the UK in October 2000 • All public bodies (police, courts, hospitals, local governments) and others carrying out public functions have to comply with the convention rights. We work with article 8 of the Human Rights Act ‘Respect for your private and family life, home and correspondence’. Computer Misuse Act: Prior to 1990 there were no legislations in place to tackle the problems caused by hacking. Although it was known to be wrong and should be against the law, there was no framework in place to support this. As the problem grew, it became apparent that specific legislation was needed to enable individuals to be prosecuted under the law. So in 1990 the Computer Misuse Act was passed and recognised the following new offences. • Unauthorised access to computer systems • Unauthorised access with intent to commit or facilitate a crime • Unauthorised modification of computer material • Making, supplying or obtaining anything which can be used in computer misuse offences.
The Information Governance Toolkit Information Governance To help improve Information Governance / Security arrangements across the NHS, the Department of Health introduced a set of key standards called the IG Toolkit. • • • 45 mandatory requirements for NHS organisations Annual report stating improvements to Department of Health Provides assurance all processes and procedures meet national requirements Annual reports contribute to the Care Quality Commission audits Audits can be reviewed on public-facing websites (Health & Social Care Information Centre [HSCIS]) The Information Governance Team is responsible for the management of the toolkit and works closely with key staff to ensure compliance and collation of evidences to support the annual assessment. All staff need to be involved to improve Trust performance levels. This is can be achieved by: • • • Implementing guidance Completing required training Reporting incidents/breaches Complete Data Flow Mapping Assist with Information Governance spot check audits
Data Subject Access Requests Information Governance Subject Access Requests: The Data Protection Act 1998 gives an individual several rights in relation to the information held about them: • The right to seek access to their records held by the Trust • The right to obtain a copy of the record in permanent form or to view a record without obtaining a copy • The right to rectification, blocking, erasure (under very strict regulations) and destruction of information • For all staff related requests, access to records / information is required within 40 calendar days under the DPA Act • For all patient related access to health/medical records the Trust has to respond within 40 calendar days, unless the individual has been seen within 21 days in which case the information must be provided within 21 days of receipt of the application. When a request is made… there are two circumstances in which access can be denied and therefore the requestor may have the right to ask the Information Commissioner to assess: • If the record contains third party information and they have not consented to their information being disclosed • If access to all /part of the record will cause serious harm to the physical or mental wellbeing of the individual, or any other person. Publication Scheme The Publication Scheme is a guide to the information the Trust holds, and must be published on its website. It gives people access to some information without them having to make specific requests. The current publication scheme maybe found on the Trust’s internet site (www. sept. co. uk)
Freedom of Information Act 2000 Information Governance The Act allows any member of the public the right to view / receive copies of corporate information held by public bodies – it does not cover health or personal information. All such requests for information are managed by the Legal Department and should not be handled by teams locally. If you receive an external request for information you MUST ensure it is forwarded to the Legal Department immediately. REMEMBER: The Law requires that FOI requests are responded to strictly within 20 working days of receipt within the Trust. Applicants can choose to receive information in different formats: • Permanent form (hard copies) – paper or electronic • Summary form • Permission to inspect records containing the requested information Examples of Information that can be requested: • Executive Team reports • Emails • Handwritten notes on file • Financial information How should I respond to a request for information? EVERYONE is responsible for following these simple rules: • You should NOT respond directly to the applicant – other than to advise you have passed their request to the Legal Department • Send to the Legal Department FOI Lead (foi@sept. nhs. uk) immediately on receipt • Don’t forget ‘ 20’ day rule Application Requests: • All requests must be in writing (email/post/fax) • State clearly what information is required • State name of the applicant and address • Applicants do not need to mention the FOIA • Applicants do not have to give a reason for wanting the information • You are NOT allowed to ask the applicant their reasons for requesting.
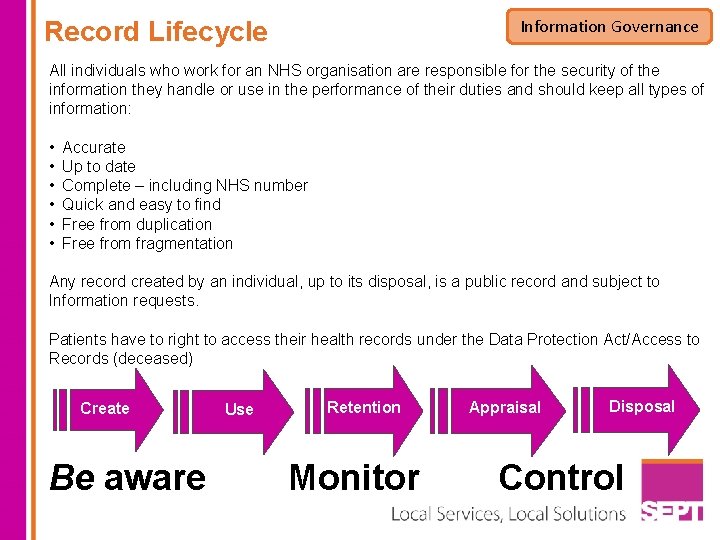
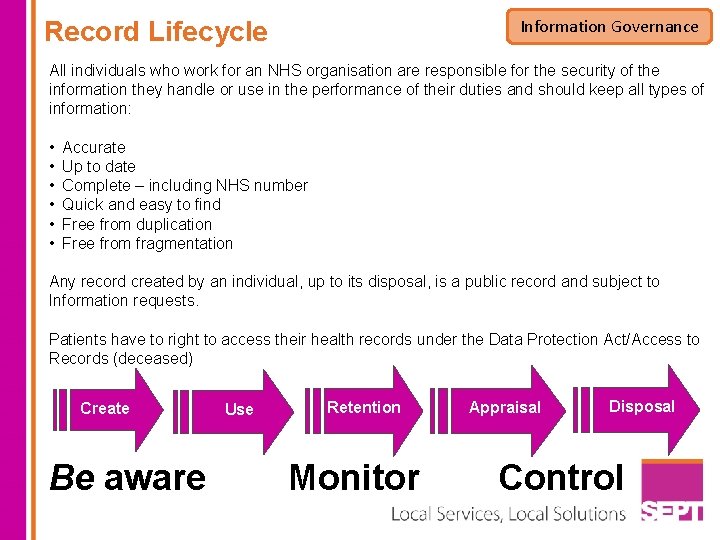
Information Governance Record Lifecycle All individuals who work for an NHS organisation are responsible for the security of the information they handle or use in the performance of their duties and should keep all types of information: • • • Accurate Up to date Complete – including NHS number Quick and easy to find Free from duplication Free from fragmentation Any record created by an individual, up to its disposal, is a public record and subject to Information requests. Patients have to right to access their health records under the Data Protection Act/Access to Records (deceased) Create Be aware Use Retention Monitor Appraisal Disposal Control
Record Management & Keeping Information Governance Records Disposal: The Trusts’ corporate procedural guideline CPG 9(g) Storage, Retention and Destruction of Records will tell you which records should be kept for how long, prior to disposal. • Please ensure records are destroyed in a secure way. Either in blue confidential waste bags or shed using a cross cut shredder. Do not place patient/staff identifiable information in waste paper bins. • Make note of how, when and where the record(s) were destroyed, together with any reference numbers. • If an applicant wants to see a record that is due to be destroyed, you must not destroy the record until the request has been answered or any complaint and appeals process has finished. • Destruction of all records should be completed in liaison with the Trusts’ Records Management Team. Records Management: Managing records effectively is essential for making access to information possible. Records management covers all aspects of a records life and should be: • • • Factual and correct Relevant and useful Clear and concise Up to date Complete They should not contain: • Unnecessary jargon • Personal opinions • Offensive language

Record Types: Records can be in physical or technical formats, including: Information Governance • In paper record keeping system • On computer, including emails • On film records, such as CCTV Also covers: • Information located in confidential waste • Information on computers • Information stored on computer internal drives, USB sticks, CD and disks. 1) Create – Use appropriate Trust folders and formats 2) Use – Enter information, use of templates, filing, discharge summaries, clinical coding processes 3) Track – Log the location/pathway 4) Missing – Report to the manager 5) Retain – Look after, manage multiple volumes, hold until not required 6) Disposal Methods – confidentiality using Trust procedures
Key Contacts Information Governance Overall responsibility for the Information Governance Agenda – Director of ITT (Senior Information Risk Owner) responsibility for public and non-health requests for information – Executive Director Corporate Affairs & Customer Services (Freedom of Information/ Data Subject Access Requests) Confidentiality / sharing of patient information – Executive Director Clinical Governance & Quality / Caldicott Guardian responsibility for the quality/accuracy of information – Assistant Director Systems Implementation & Data Quality (Community) Responsibility for the quality/accuracy of information, managing the IG agenda including the Toolkit and DPA – Assistant Director Systems Implementation & Data Quality (Mental Health) Responsibility for the implementation/security of records management and subject access requests (health) – Head of Records Management/Team Responsibility for legal processes (Data Subject Access Requests (non-health) / Freedom of Information Requests) and general advice and guidance – Legal Department
Safeguarding Introduction Section 1 Clinical Governance Information Governance Safeguarding Fire Safety
Aims and Objectives Safeguarding At the end of this training, you should be able to identify: • • • What abuse is and how different types of abuse might be identified Where abuse may take place Who abuses? Why abuse might occur and to whom What to do if you witness abuse Safeguarding is protecting adults and children from abuse, this online course is split into four distinct areas: Introduction to safeguarding: this covers safeguarding Adult and Child information Safeguarding Children: This covers abuse of children specifically All sections have to be completed for successful completion of the course. In total, the course should take roughly one hour to complete. Safeguarding Adults: This covers abuse of Adults who are at risk of abuse Questions: These confirm your learning
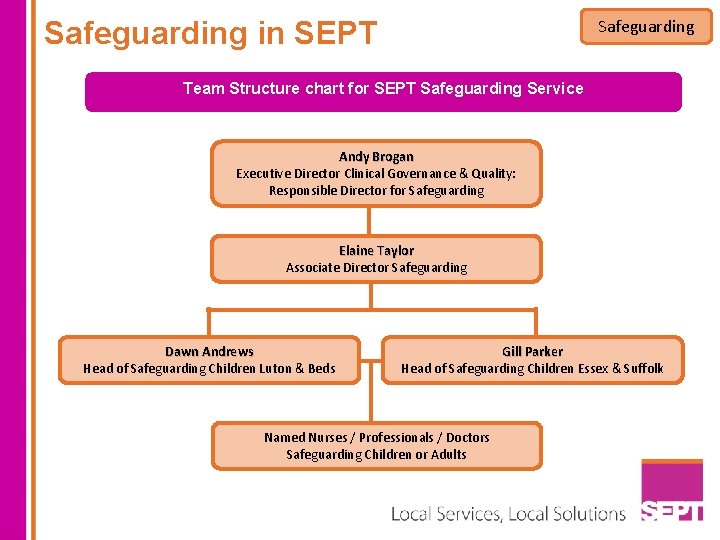
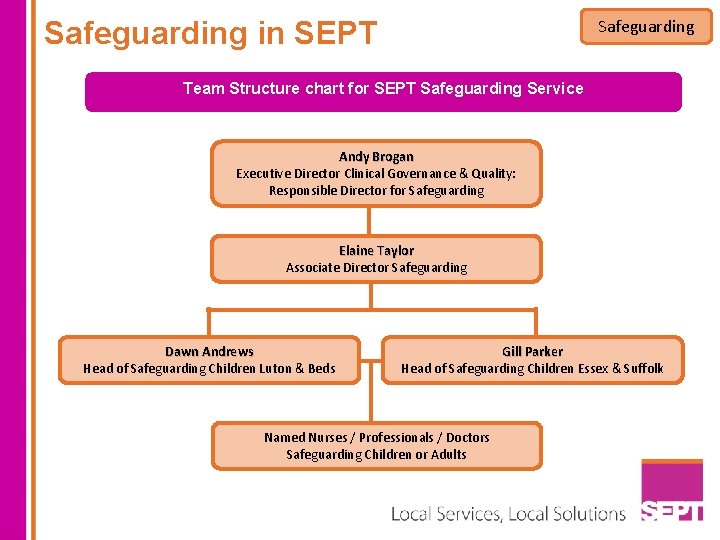
Safeguarding in SEPT Safeguarding Team Structure chart for SEPT Safeguarding Service. Andy Brogan Executive Director Clinical Governance & Quality: Responsible Director for Safeguarding Elaine Taylor Associate Director Safeguarding Dawn Andrews Head of Safeguarding Children Luton & Beds Gill Parker Head of Safeguarding Children Essex & Suffolk Named Nurses / Professionals / Doctors Safeguarding Children or Adults
Your Responsibility Safeguarding It is your responsibility to report any abuse wherever it is seen, suspected or reported and to take the necessary immediate actions to ensure the protection of any vulnerable person at risk. Remember to be clear on the form. Record what happened and provide information on why this is a situation of potential abuse
Access to further information You should be aware of how to access additional information via the Safeguarding site on the Trust Intranet. Polices Safeguarding Team Contact Details Referral Forms Information Sharing Guidance Whistle Blowing Policy Safeguarding
Prevention Safeguarding All teams must have in place systems that minimise the possibility of abuse. Effective Risk Assessment and Care Planning These Include: Provision of Information to Service Users on Protecting Themselves e. g. Staff Meetings where Safeguarding is Discussed Service User Meetings where Safety is Discussed Effective Training of Staff (including records of this) Leaflets and Posters etc.
Protection of Evidence Record all actions accurately. Any written evidence can be copied to preserve this. Safeguarding If there are items you think may be used as evidence do not handle them unless you have to. Ask for assistance as soon as possible if you think a criminal investigation may be required. The police will advise on preservation of evidence in each circumstance

Safeguarding Do Not stop someone who is freely recalling significant events Do Not be judgmental – have an open mind We do not want to be negative, but a few things to Avoid Do Not promise to keep secrets Do Not make promises you are unable to keep Do Not ask leading or closed questions or press for more details Do Not contact the alleged abuser
Whistleblowing Individual members of staff in the Trust have a legal right and a duty to raise with their Managers or the Trust Board any matters of concern they may have about safety, clinical practice, malpractice or wrong doing which may affect patients, the public, other staff or the organisation itself. Your concern may include • Unethical Practice, Clinical/Non-Clinical • Concerns regarding the professional conduct or performance of a member of staff • Criminal activity • Negligence Endangering of an individual’s health and safety • Bullying or Harassment • Damage to the environment • Abuse of position/authority Maladministration • A miscarriage of justice on matters which may be defined as gross misconduct The Trust encourages and supports you to report concerns Safeguarding Remember You do not need firm evidence to raise a concern Refer to the whistleblowing policy CPG 53

Safeguarding Children

Safeguarding children is everyone’s responsibility Safeguarding and promoting the welfare of children and young people A 'child' is anyone up to their eighteenth birthday. The Children Act 1989 defines a child in need; as children or young people who because of their vulnerability, will need the provision of services in order to reach or maintain a satisfactory level of health or development. Safeguarding and promoting the welfare of children is defined as protecting children from maltreatment, preventing impairment of children's health and development and ensuring children have optimum life chances All staff have a statutory duty to report concerns regarding a child's welfare to their Line Manager and/or the Safeguarding Children Team.
The Children Act 1989 (Section 17) The Children Act 1989 (section 17) defines a child in need; as children or young people who because of their vulnerability, will need the provision of services in order to reach or maintain a satisfactory level of health or development, this includes children with special needs Safeguarding Where a child in need is identified, practitioners working with the child will complete either: a Common Assessment Framework (CAF) or an Essex Request for Support Form (ERSF) for a co-ordinated response and delivery of services to the child/young person and their family. Consent from the parent and/or young person is central to this process.
The Children Act section 47 Safeguarding The Children Act (1989) introduced the concept of significant harm as a definition of abuse; harm means ill treatment or the impairment of health or development including impairment from seeing or hearing the ill treatment of another. Significant relates to the child’s health and development and the comparison with that which could reasonably be expected of a similar child. Where a child or young person has been identified as at risk of significant harm the Local Authority (Social Care) has a legal duty to make enquiries and take appropriate action to ensure the safety of the child/young person. Consent for these enquiries is not obligatory, but agencies will always seek to work with parents where this does not place the child or young person at increased risk.

Abusers come from all walks of life Children may be abused by: Someone the child knows well or more rarely a stranger. Safeguarding Abuse can occur within the family, an institution or community setting. Abuse can occur in all social groups regardless of age, gender, race, religion, culture, social class or financial position. By an Adult(s) By a child/young person All staff who work with children or adults from any service have a responsibility in safeguarding children when they become aware of or identify a child at risk of harm. This includes considering the implications for children of parents’ or users’ behaviours and the impact these may have on their parenting capacity.
Child abuse can take many forms, but is usually divided into four categories Safeguarding Signs that could indicate physical abuse Physical Abuse include: Involves a range of physical injuries including hitting, shaking, throwing, poisoning, burning, scalding, drowning or suffocating and also includes fabricated and/or induced illness and Female Genital Mutilation (FGM) Bruising on a non-mobile baby or child (maybe non mobile because of age or disability) On any fleshy, non-bony part of the body, for example: face, neck, buttocks or back Bruises are more likely to be accidental when found on the bony prominences of the body for example: forehead, chin, knees, shin, back of head Burns & Scalds Burns include scalds from hot liquids, contact burns from hot objects (such as an iron) burns caused by flames, chemical and electrical. Burns with a clear outline or uniform depth for example may be more indicative of non accidental injury. Fabricated or Induced Illness is classed as a physical abuse where a parent/carer fabricates or deliberately induces illness in a child Any injury which the child, parent, carer tries to hide or give several different or unlikely explanations, should raise concerns. In these circumstances advice should always be sought.
Sexual Abuse Safeguarding Sexual abuse involves forcing or enticing a child or young person to take part in sexual activities, including (CSE) child sexual exploitation. Free e-learning available: link on SEPT training bulletin keepthemsafeguardingchildrenea. co. uk/ This may involve sexual physical contact or non-contact activities including coercing or grooming children by the use of pornographic material or watching sexual activities including those via the internet, webcams, cameras, mobile phones, or encouraging children to behave in sexually inappropriate ways. Trust staff must report any known cases to their line manager and the Trust Safeguarding Team and a referral made to Children’s Social Care. It may also be appropriate to contact the Police if the situation is urgent. It is important to recognise that children & young people can be sexually abused by adult males, females and other children & young people.
Any sexual act with a child under 13 years is illegal and classed as statutory rape, as a child is not capable of consenting to sexual activity. Signs which could indicate sexual abuse include: Changes in behaviour such as withdrawn, or aggressive, risk taking such as running away or substance misuse Safeguarding If you are aware of a child that has contact with an adult with prior allegations or convictions of sexual abuse you must seek advice from the Safeguarding team and your line manager with a view to making a child protection referral. Children displaying inappropriate sexualised behaviour or language for their age and stage of development
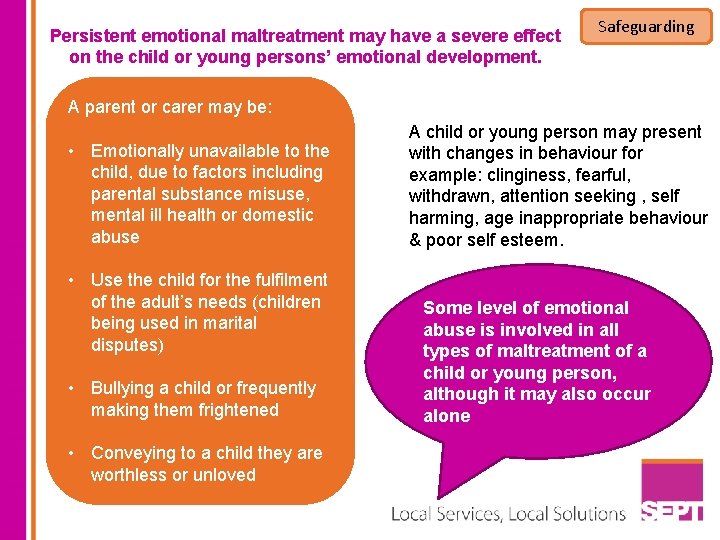
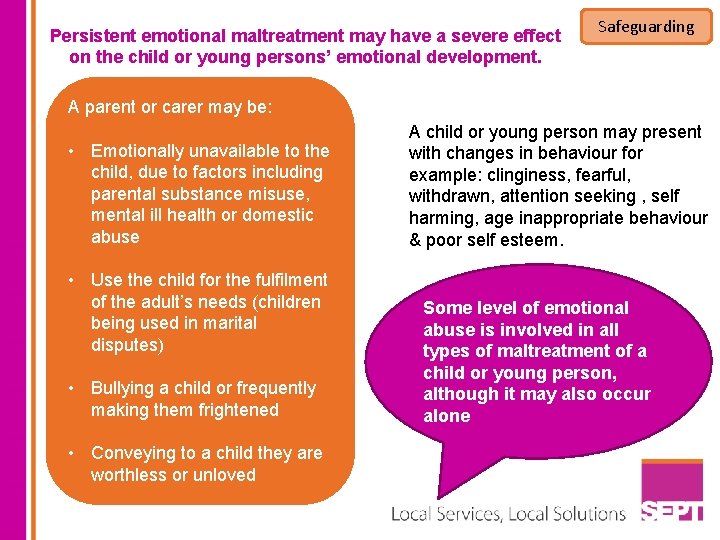
Persistent emotional maltreatment may have a severe effect on the child or young persons’ emotional development. Safeguarding A parent or carer may be: • Emotionally unavailable to the child, due to factors including parental substance misuse, mental ill health or domestic abuse • Use the child for the fulfilment of the adult’s needs (children being used in marital disputes) • Bullying a child or frequently making them frightened • Conveying to a child they are worthless or unloved A child or young person may present with changes in behaviour for example: clinginess, fearful, withdrawn, attention seeking , self harming, age inappropriate behaviour & poor self esteem. Some level of emotional abuse is involved in all types of maltreatment of a child or young person, although it may also occur alone
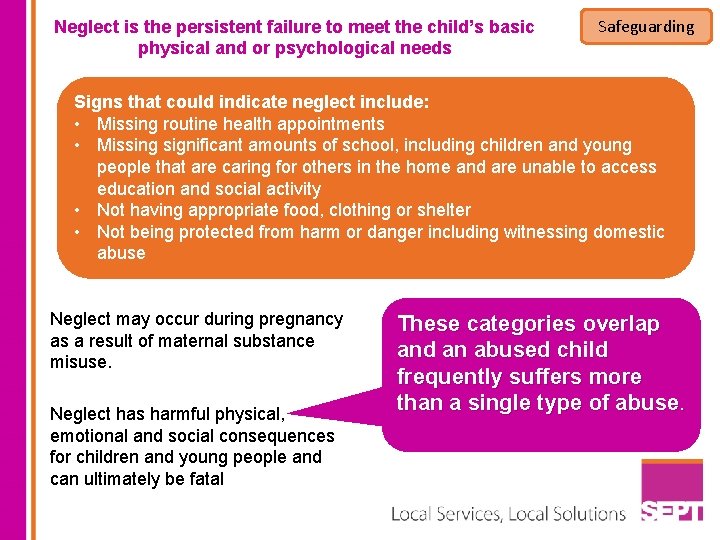
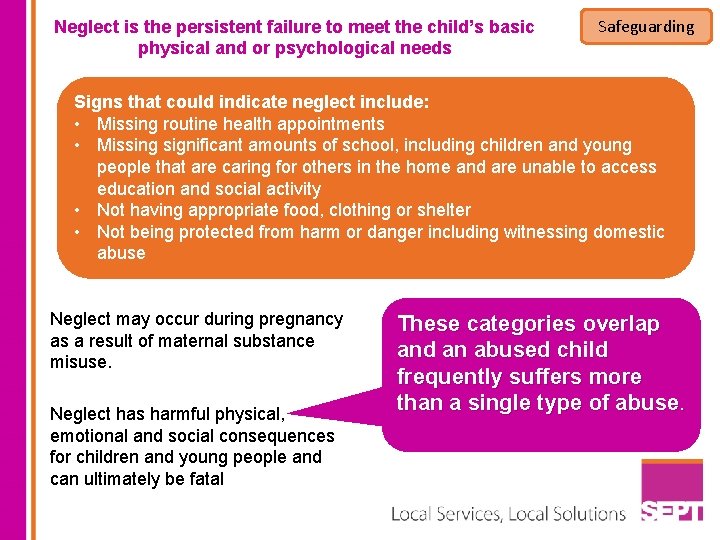
Neglect is the persistent failure to meet the child’s basic physical and or psychological needs Safeguarding Signs that could indicate neglect include: • Missing routine health appointments • Missing significant amounts of school, including children and young people that are caring for others in the home and are unable to access education and social activity • Not having appropriate food, clothing or shelter • Not being protected from harm or danger including witnessing domestic abuse Neglect may occur during pregnancy as a result of maternal substance misuse. Neglect has harmful physical, emotional and social consequences for children and young people and can ultimately be fatal These categories overlap and an abused child frequently suffers more than a single type of abuse.
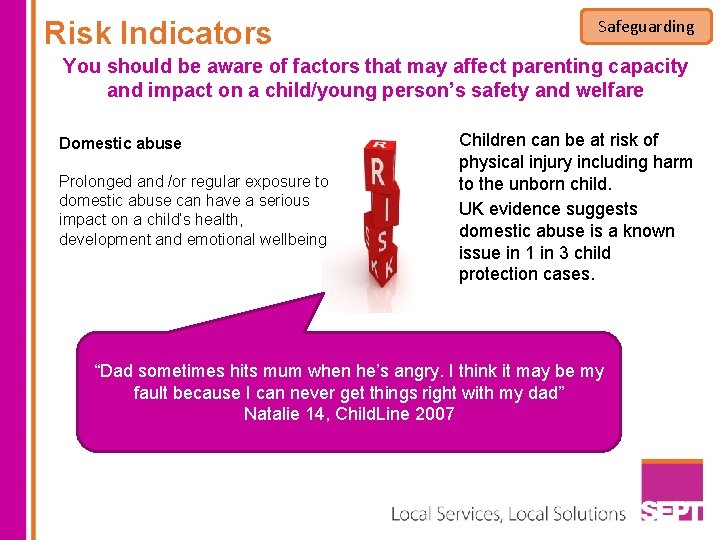
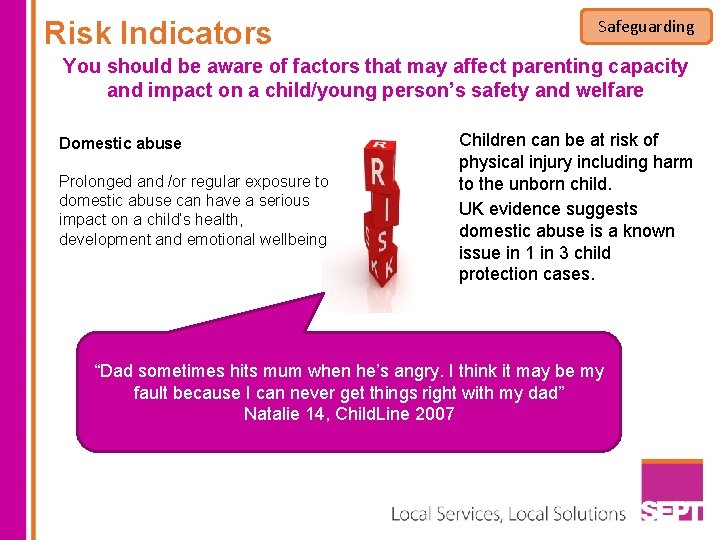
Risk Indicators Safeguarding You should be aware of factors that may affect parenting capacity and impact on a child/young person’s safety and welfare Domestic abuse Prolonged and /or regular exposure to domestic abuse can have a serious impact on a child’s health, development and emotional wellbeing Children can be at risk of physical injury including harm to the unborn child. UK evidence suggests domestic abuse is a known issue in 1 in 3 child protection cases. “Dad sometimes hits mum when he’s angry. I think it may be my fault because I can never get things right with my dad” Natalie 14, Child. Line 2007
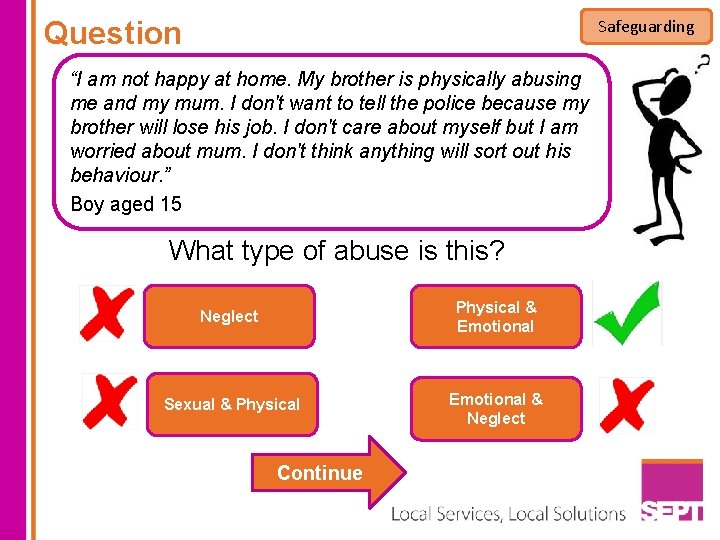
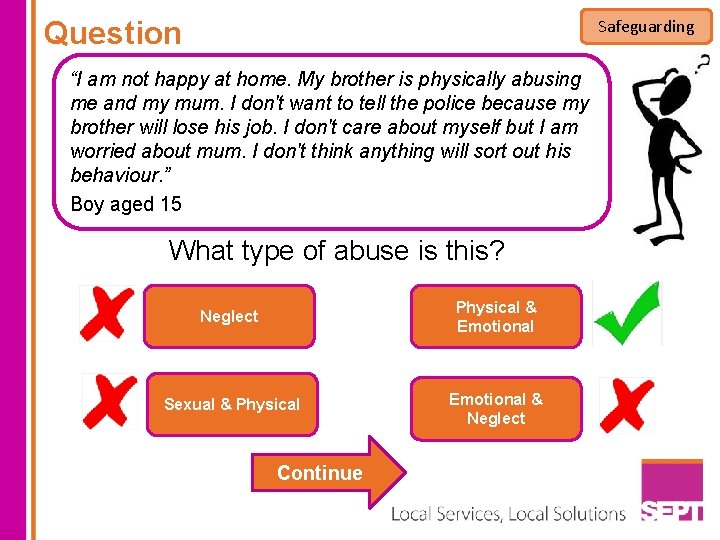
Question Safeguarding “I am not happy at home. My brother is physically abusing me and my mum. I don't want to tell the police because my brother will lose his job. I don't care about myself but I am worried about mum. I don't think anything will sort out his behaviour. ” Boy aged 15 What type of abuse is this? Neglect Physical & Emotional Sexual & Physical Emotional & Neglect Continue
Parental drug and alcohol misuse Misuse of drugs (prescribed or illegal) and or alcohol is strongly associated with significant harm to the unborn child, children and young people, especially when combined with other features such as domestic abuse and mental illness. “My dad broke my nose last year when he was drunk. My sister has left home. I feel empty and hurt” Milly 12 yrs (quote from Child. Line 2007) Safeguarding
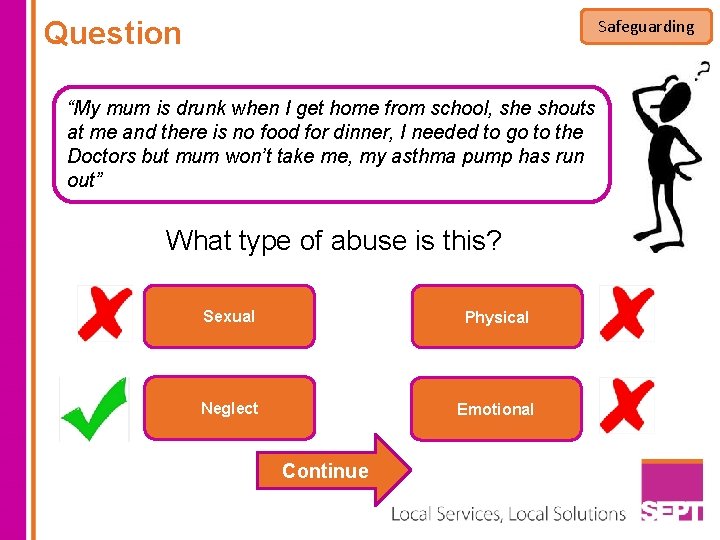
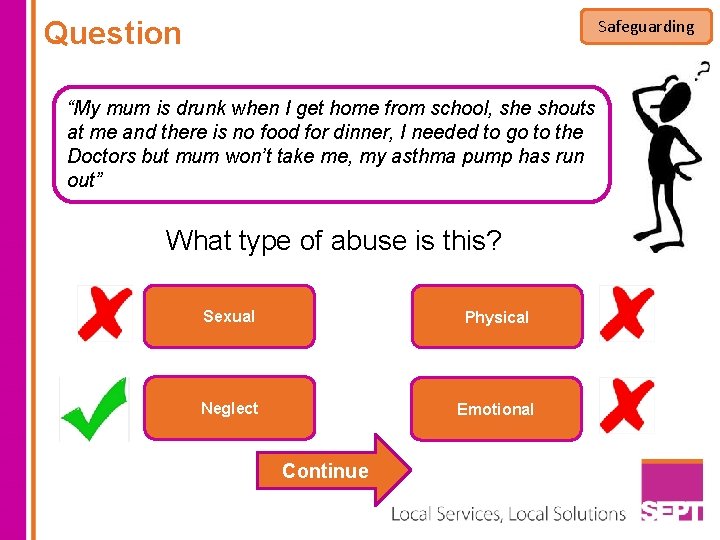
Question Safeguarding “My mum is drunk when I get home from school, she shouts at me and there is no food for dinner, I needed to go to the Doctors but mum won’t take me, my asthma pump has run out” What type of abuse is this? Sexual Physical Neglect Emotional Continue
Parental mental ill health Safeguarding The majority of parents who suffer mental illness are able to care for and safeguard their children, however nationally 25% of children who are subject to Child Protection Conferences have a parent with mental health problems. “Mum’s always miserable. She never asks me how I am. She just sits in front of the telly all day. I could be dead for all she cares” Wayne 13 years (quote from Child. Line 2007)
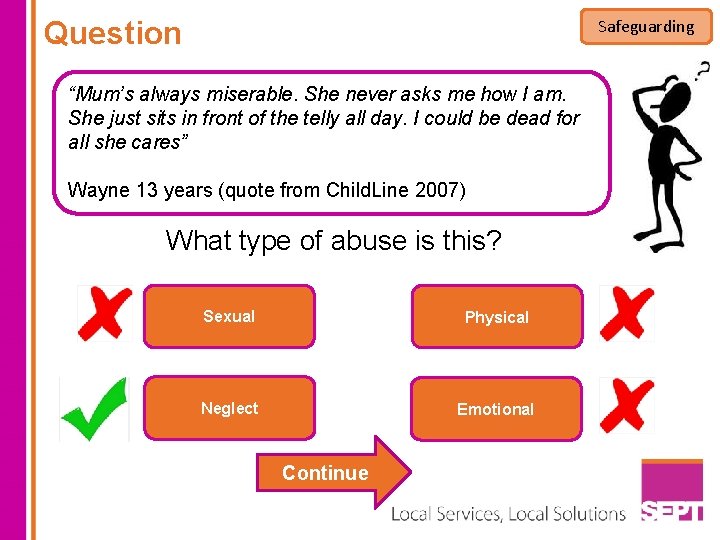
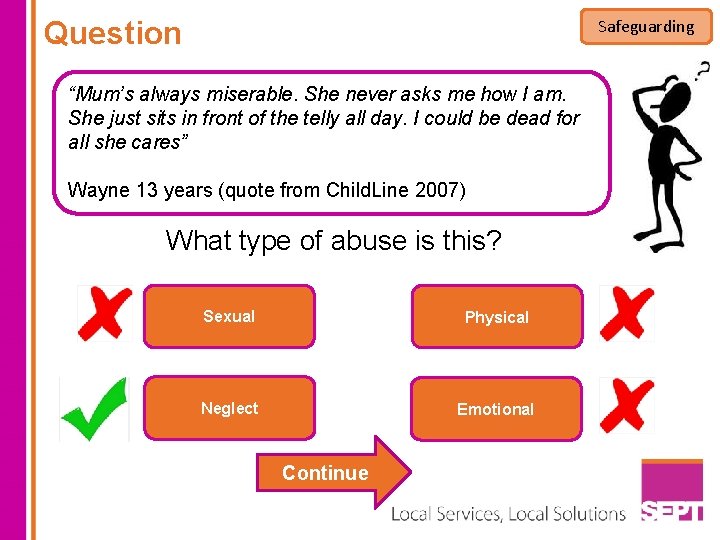
Question Safeguarding “Mum’s always miserable. She never asks me how I am. She just sits in front of the telly all day. I could be dead for all she cares” Wayne 13 years (quote from Child. Line 2007) What type of abuse is this? Sexual Physical Neglect Emotional Continue
Safeguarding Previous history of safeguarding concerns Where a previous child/young person has been subject to a child protection plan (formerly known as the child protection register) Where a previous child/young person has been removed from home Adults or young people known to be a Risk to a Child (formerly a Schedule 1 Offender) Child Factors Children under one year are more vulnerable to abuse and neglect as are: • Children and young people with any kind of disability • Looked after children/young people (LAC) those in private or local authority foster care or children’s homes
Safeguarding What do you do if you are concerned for the welfare of a child? All staff have a legal duty to report any concerns they may have for the safety and welfare of a child. If you are concerned about a child or young person you must seek advice from the Safeguarding team and your line manager with a view to making a However, You may need to child protection referral. ensure the child or young person’s immediate safety and access emergency assistance if necessary. You must then inform your Line Manager or the Trust Safeguarding Team. Outside normal working hours contact the Manager on call

Safeguarding What do you do if you are concerned for the welfare of a child? If you are unable to contact your line manager or a member of the safeguarding team you should seek advice directly from children’s social care. Referrals to children’s social care must be made within one day of identifying the concern and telephone contact must be followed up with a written referral within 48 hours. If the referrer has no contact from social care then they have a responsibility to follow up the outcome of the referral within 3 working days. You MUST record all information and actions clearly with your name, designation, signature and date.
Confidentiality and Consent Safeguarding Staff cannot give assurance of confidentiality where there are concerns about a child as information may need to be shared in order to protect the child. Consent to share information should always be sought where possible, except when; Permission has been refused but sufficient professional concern remains to justify disclosure Seeking permission is likely to impede a criminal investigation When gaining consent would place a child, young person or an adult at risk of significant harm If you are uncertain about when to share confidential information, always seek advice from the Trust Safeguarding Team or your line manager
Safeguarding Adults
What is safeguarding? Safeguarding The National Framework for Safeguarding Adults is called NO SECRETS 2000 No Secrets 2000 applies to those people over 18 years old who are dependant on others for their activities of daily living or care needs and who are or may be unable to protect themselves against significant harm or serious exploitation which may be caused by actions or inactions of other people’’.
Who Abused Adults? Safeguarding Anyone Who has POWER, over others, this can be by being a Social or Health Care Professional, a paid carer or an unpaid carer, a family member of friend. Think What have you seen in practice that has made you think Abuse may have taken place? Often it can be a feeling that things are not right, that service users are not getting treatment provided in a way we would accept, or that they are being exploited by others.

Physical Abuse Safeguarding Includes hitting, punching, slapping, kicking, Drowning, shaking, biting restraint, medication, lap belts, locked doors Possible Observed Signs and Symptoms • • Unexplained injuries, e. g. dislocations, fractures Unexplained bruising or abrasions Cowering and flinching Burns and scalds • • • There are 7 types of adult abuse Rough or inappropriate handling Hitting, Kicking, punching Force – feeding Misuse of medication Inappropriate use of restraint Inappropriate treatment regimes or sanctions, e. g. making someone sit in a corner Possible observed practices

Sexual Abuse Safeguarding Includes; rape, touching, innuendo, viewing sexual activity, or explicit materials, grooming to commit sexual acts • Possible Observed Signs and Symptoms • • Incontinence/bed wetting Difficulty walking Repeated urinary tract infections Bruising, bleeding or unexplained soreness around genital area Unexplained “love bites” Sexually Transmitted Infection or pregnancy Self neglect or risk taking behaviour • • • Sexual acts the person hasn’t consented to, was pressurised into consenting to Touching inappropriately Penetration Indecent exposure Taking photographs Using inappropriate language Possible observed practices
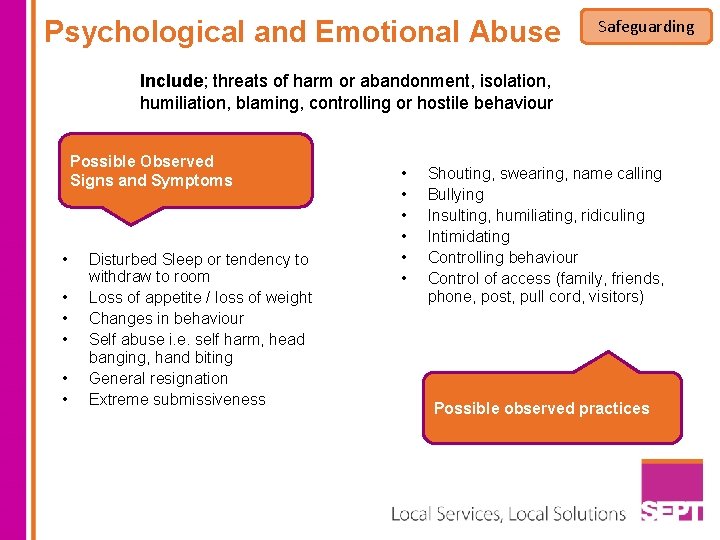
Psychological and Emotional Abuse Safeguarding Include; threats of harm or abandonment, isolation, humiliation, blaming, controlling or hostile behaviour Possible Observed Signs and Symptoms • • • Disturbed Sleep or tendency to withdraw to room Loss of appetite / loss of weight Changes in behaviour Self abuse i. e. self harm, head banging, hand biting General resignation Extreme submissiveness • • • Shouting, swearing, name calling Bullying Insulting, humiliating, ridiculing Intimidating Controlling behaviour Control of access (family, friends, phone, post, pull cord, visitors) Possible observed practices
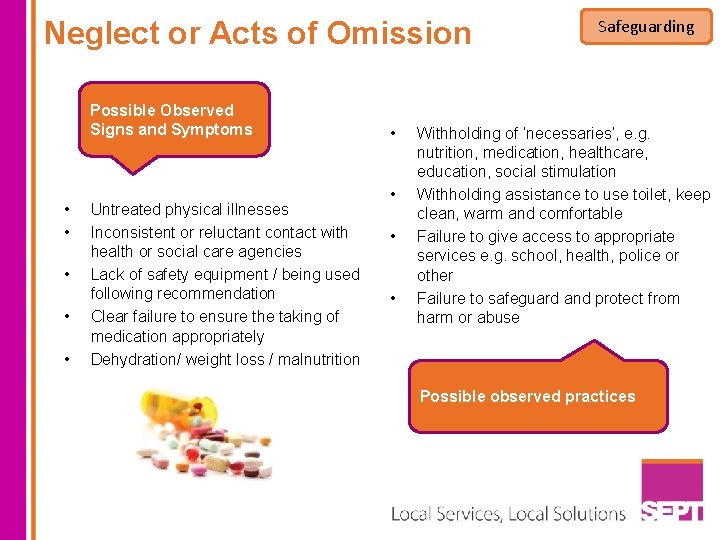
Neglect or Acts of Omission Possible Observed Signs and Symptoms • • • Untreated physical illnesses Inconsistent or reluctant contact with health or social care agencies Lack of safety equipment / being used following recommendation Clear failure to ensure the taking of medication appropriately Dehydration/ weight loss / malnutrition • • Safeguarding Withholding of ‘necessaries’, e. g. nutrition, medication, healthcare, education, social stimulation Withholding assistance to use toilet, keep clean, warm and comfortable Failure to give access to appropriate services e. g. school, health, police or other Failure to safeguard and protect from harm or abuse Possible observed practices
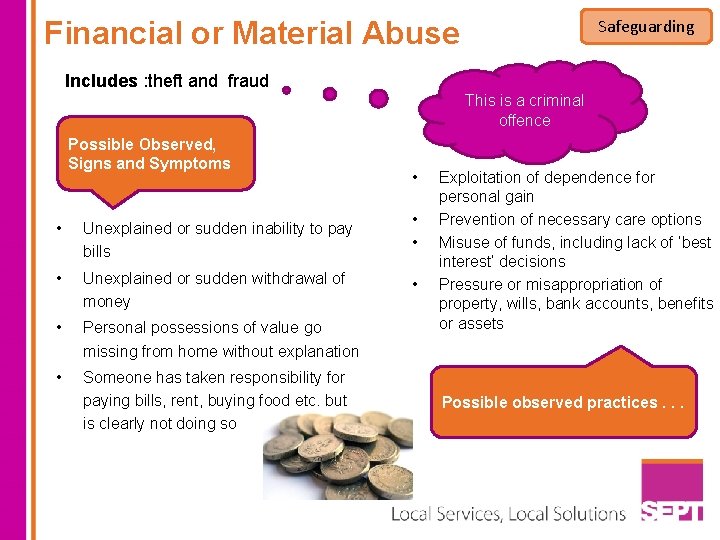
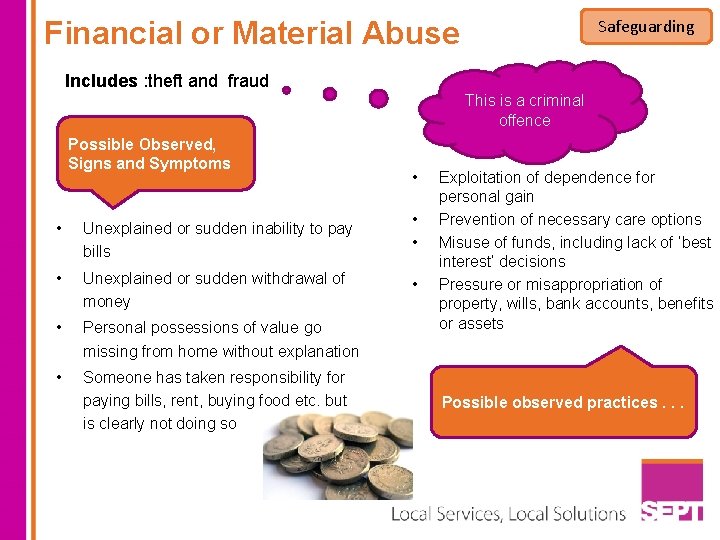
Financial or Material Abuse Safeguarding Includes : theft and fraud This is a criminal offence Possible Observed, Signs and Symptoms • Unexplained or sudden inability to pay bills • Unexplained or sudden withdrawal of money • Personal possessions of value go missing from home without explanation • Someone has taken responsibility for paying bills, rent, buying food etc. but is clearly not doing so • • Exploitation of dependence for personal gain Prevention of necessary care options Misuse of funds, including lack of ‘best interest’ decisions Pressure or misappropriation of property, wills, bank accounts, benefits or assets Possible observed practices. . .
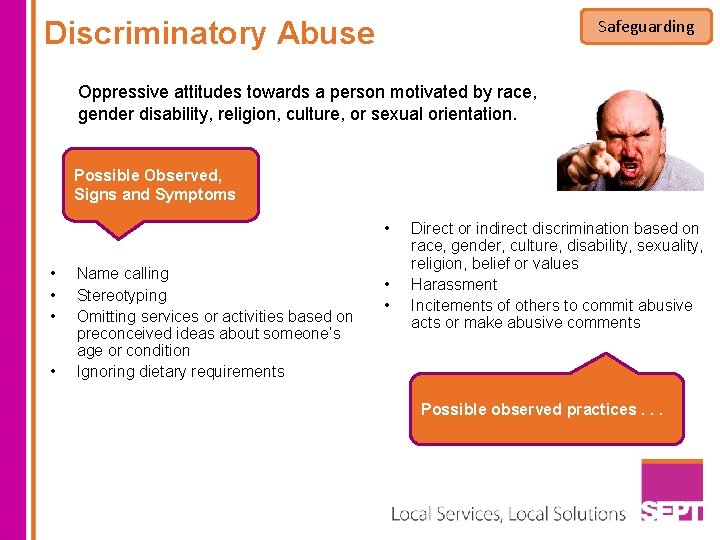
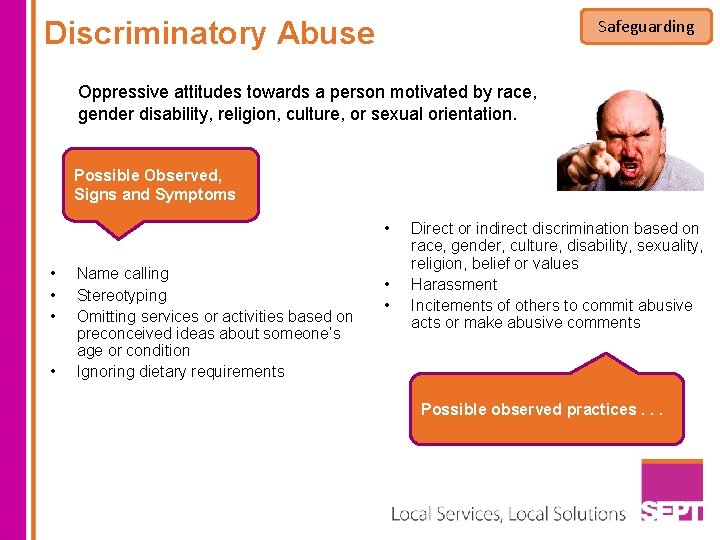
Discriminatory Abuse Safeguarding Oppressive attitudes towards a person motivated by race, gender disability, religion, culture, or sexual orientation. Possible Observed, Signs and Symptoms • • • Name calling Stereotyping Omitting services or activities based on preconceived ideas about someone’s age or condition Ignoring dietary requirements • • Direct or indirect discrimination based on race, gender, culture, disability, sexuality, religion, belief or values Harassment Incitements of others to commit abusive acts or make abusive comments Possible observed practices. . .
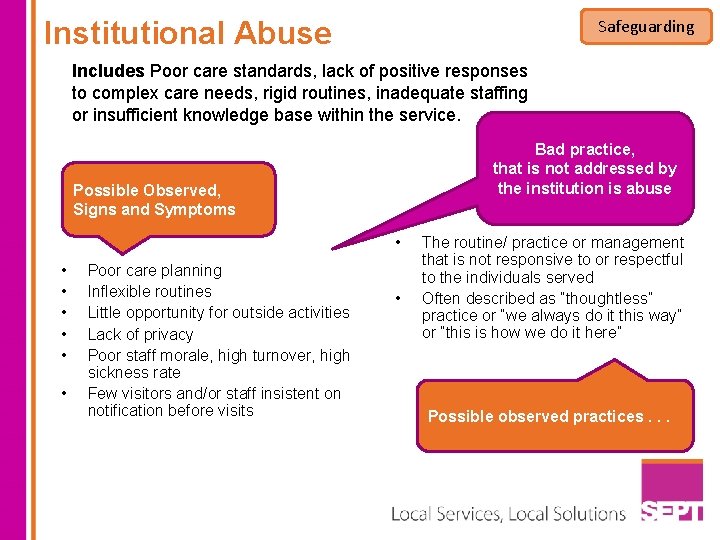
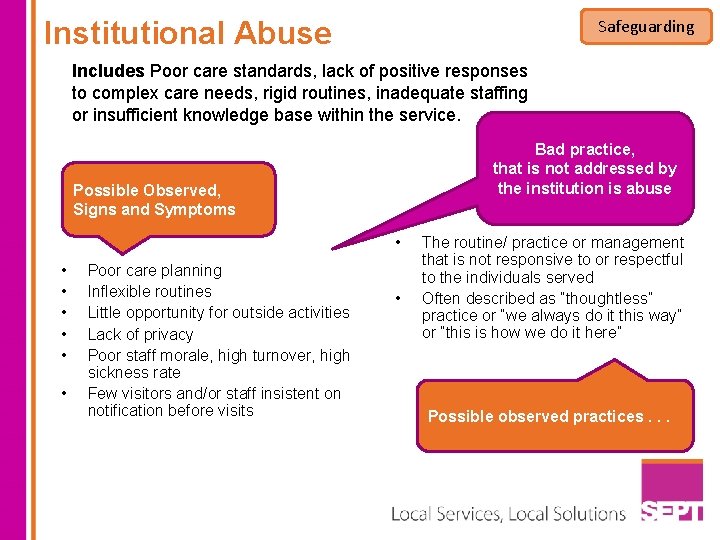
Institutional Abuse Safeguarding Includes Poor care standards, lack of positive responses to complex care needs, rigid routines, inadequate staffing or insufficient knowledge base within the service. Bad practice, that is not addressed by the institution is abuse Possible Observed, Signs and Symptoms • • Poor care planning Inflexible routines Little opportunity for outside activities Lack of privacy Poor staff morale, high turnover, high sickness rate Few visitors and/or staff insistent on notification before visits • The routine/ practice or management that is not responsive to or respectful to the individuals served Often described as “thoughtless” practice or “we always do it this way” or “this is how we do it here” Possible observed practices. . .
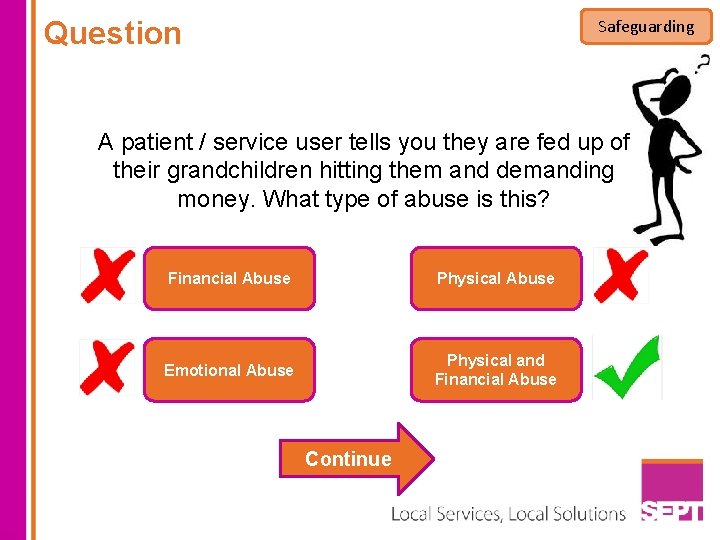
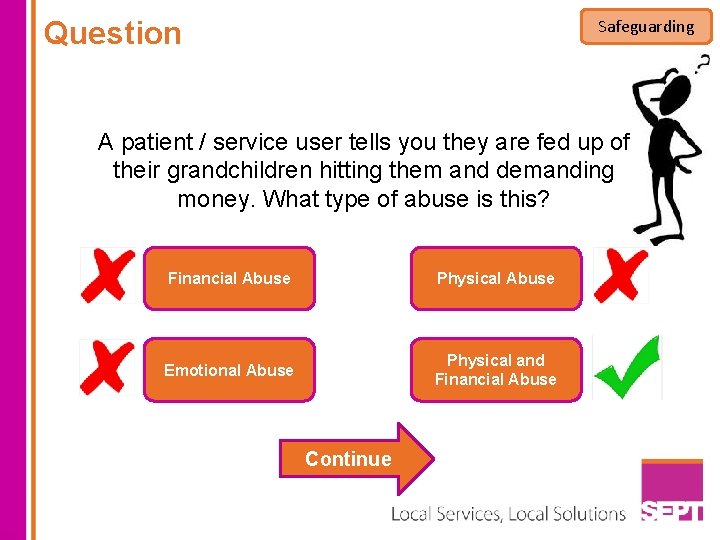
Question Safeguarding A patient / service user tells you they are fed up of their grandchildren hitting them and demanding money. What type of abuse is this? Financial Abuse Physical Abuse Emotional Abuse Physical and Financial Abuse Continue

Additional Safeguarding Concerns Safeguarding Some safeguarding issues apply to both children or adults as detailed below. Staff have a duty to seek advice and report any concerns. Honour Based Violence This is a violation of a persons Human Rights. It is a collection of violent and abusive practices, which are used to control behaviour within families or other social groups to protect perceived cultural and religious beliefs and/or honour Forced Marriage This is a marriage in which one or both spouses do not or (in the case of some adults with learning or physical disabilities) cannot consent to the marriage and duress is involved. Female Genital Mutilation Removal of part or all of the female genitalia for cultural or other non – therapeutic reasons If you suspect it report it !
Prevent and Safeguarding Violent Extremism PREVENT strategy Vulnerable adults and young people including those with mental health issues or learning disabilities may be susceptible to exploitation into violent extremism by radicalisers. Violent extremists often use persuasive rationale and charismatic individuals to attract people to their cause. The Trust Safeguarding Team should be contacted if staff are concerned that a service user may be exploited into extremism. PREVENT concerns can be reported under safeguarding as exploitation can be seen as abusive. . So if in doubt report under Safeguarding
Your Responsibility Safeguarding It is your responsibility to report any abuse wherever it is seen, suspected or reported and to take the necessary immediate actions to ensure the protection of any child or vulnerable person at risk. Remember to discuss with your line manager or safeguarding team. You may be asked to complete a DATIX form. Record clearly what happened and provide information on why this is a situation of potential abuse
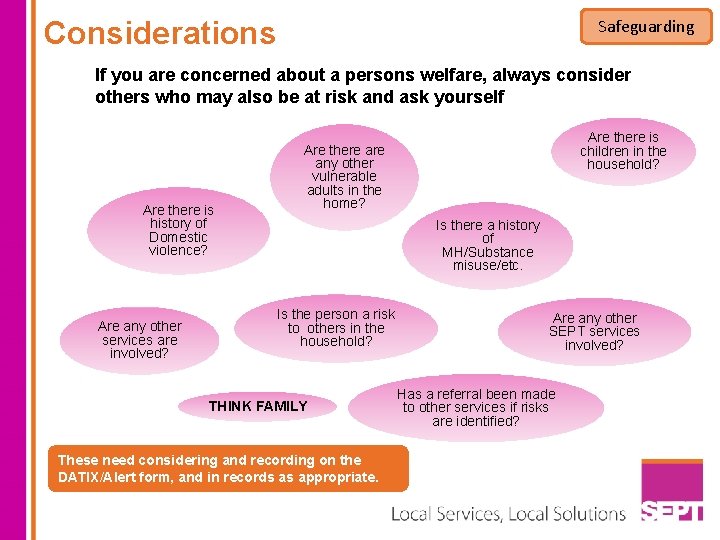
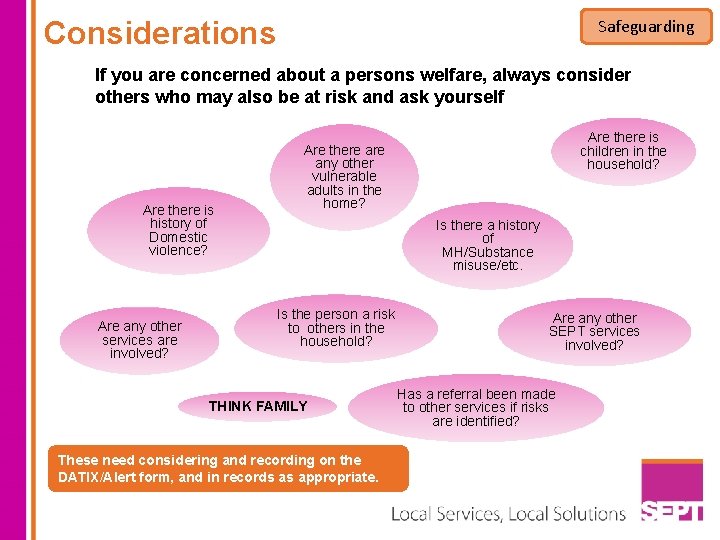
Considerations Safeguarding If you are concerned about a persons welfare, always consider others who may also be at risk and ask yourself Are there is history of Domestic violence? Are any other services are involved? Are there is children in the household? Are there any other vulnerable adults in the home? Is there a history of MH/Substance misuse/etc. Is the person a risk to others in the household? THINK FAMILY These need considering and recording on the DATIX/Alert form, and in records as appropriate. Are any other SEPT services involved? Has a referral been made to other services if risks are identified?
Safeguarding Finally – Remember…………… You must tell – YOU HAVE A DUTY TO Ignoring abuse is not an option We all have a responsibility to challenge abusive practice (Whistle blowing policies) ZERO TOLERANCE OF ABUSE You must record accurately
Fire Safety Section 1 Clinical Governance Information Governance Safeguarding Fire Safety
Learning Objectives Fire Safety Welcome to the Fire Safety Theory e-learning module This course forms part of your mandatory training and ensures that all staff are aware of your contribution to maintaining high standards of fire safety for yourself, your colleagues, visitors and any others. This training should be taken alternate years in conjunction with your face to face Fire training. v v v An introduction to fire safety Types of fire alarms Types of fire extinguishers Evacuation Policies and information Your part in fire safety
Introduction Fire Safety Fire safety responsibilities for employers and employees are put in place by Fire Safety Legislation, Health & Safety Legislation, and Health Technical Memorandum (HTM) guidance published by the Department of Health. The Trust has a range of Policies and Procedures that ensure that all employees, visitors and others are safe. However as an employee of the Trust you also have responsibilities, including: v Under the Regulatory Reform ( Fire Safety) Order 2005 and Trust’s Fire Safety Policy, all employees have a responsibility to assist in the maintenance of the fire precautions v Take reasonable care for the safety of yourself and other persons who may be affected by your acts or omissions at work v To co-operate with the Trust to enable any duty or requirement to be performed or complied with v Informing the Trust of any situation which you believe presents a serious and immediate danger or represents a shortcoming in the Trust’s arrangements for safety. v Ensure that a Fire evacuation drill is undertaken every six months

Question Fire Safety Fire evacuation drills are to be undertaken every 12 months. True False Continue
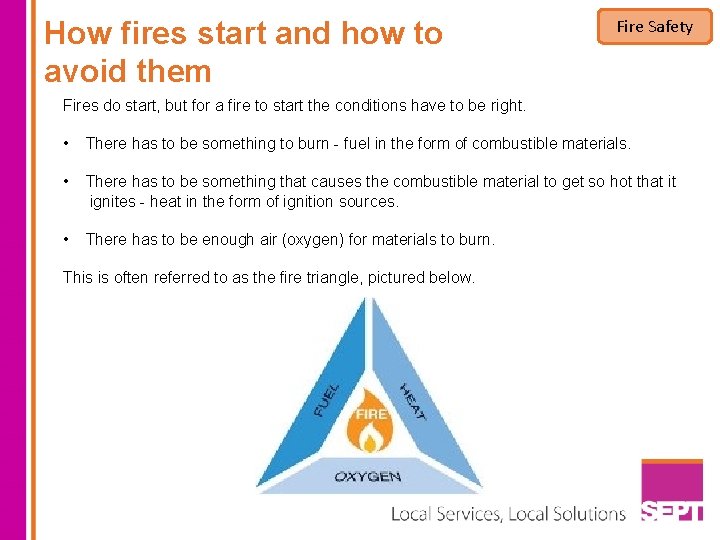
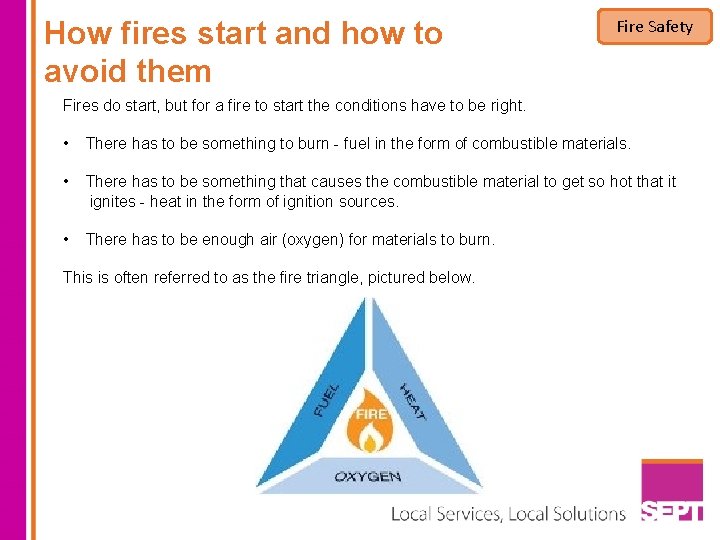
How fires start and how to avoid them Fire Safety Fires do start, but for a fire to start the conditions have to be right. • There has to be something to burn - fuel in the form of combustible materials. • There has to be something that causes the combustible material to get so hot that it ignites - heat in the form of ignition sources. • There has to be enough air (oxygen) for materials to burn. This is often referred to as the fire triangle, pictured below.
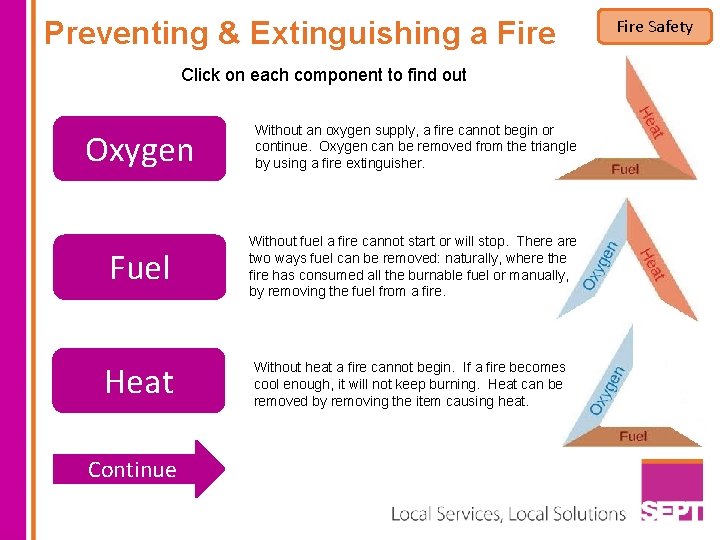
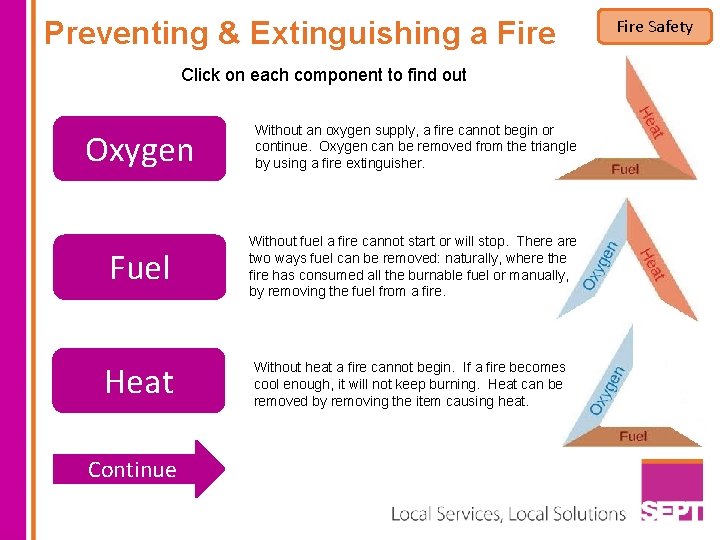
Preventing & Extinguishing a Fire Click on each component to find out Oxygen Without an oxygen supply, a fire cannot begin or continue. Oxygen can be removed from the triangle by using a fire extinguisher. Fuel Without fuel a fire cannot start or will stop. There are two ways fuel can be removed: naturally, where the fire has consumed all the burnable fuel or manually, by removing the fuel from a fire. Heat Without heat a fire cannot begin. If a fire becomes cool enough, it will not keep burning. Heat can be removed by removing the item causing heat. Continue Fire Safety
Basic Fire Safety Ignition sources in the workplace must be controlled. Faulty electrical equipment is a common source of ignition. The Trust regularly inspects and maintains its electrical equipment and services. It is a requirement that equipment is used correctly for its intended purpose and any faults reported promptly. You are responsible for the electrical equipment you use. There are particular danger signs you should look out for on all the electrical items you have in your workplace: v Hot plugs and sockets, fuses that blow frequently, flickering lights, scorch marks on sockets or plugs: these are all signs of problems that should be reported. v Overloaded sockets – too many electrical appliances plugged into one socket or the use of an adaptor can overload a circuit, which will lead to overheating – use only the adapters approved by the Trust v Do not allow visitors to use their own equipment unless it has been tested / authorised by the Estates Electrical department.
Question Fire Safety Which of the following is something you need to look out for with electrical items in the workplace Filing cabinet in front of electrical sockets Overloaded sockets Continue
Fire Safety No Smoking Some people are still tempted to smoke in Trust buildings or on Trust property. Remember it is both local Trust Policy and Department of Health NHS Policy, that you are not allowed to smoke on or in ANY NHS premises. Deliberate Ignition Arson is one of the reasons it is important to follow the Trust’s Security procedures, particularly ensuring that doors and windows are closed to prevent unauthorised access.
Fire Safety Other ignition sources include: Cooking Many fires are caused by toasters. Portable Heaters Should only be used as a last resort and be tested for electrical safety prior to use.
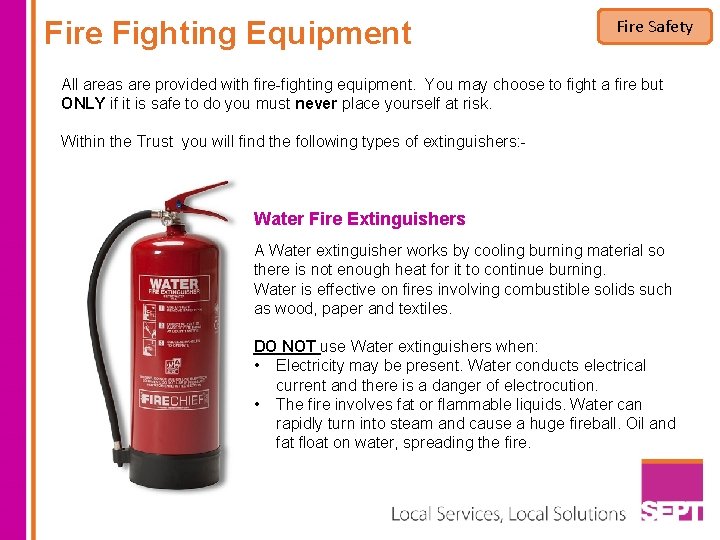
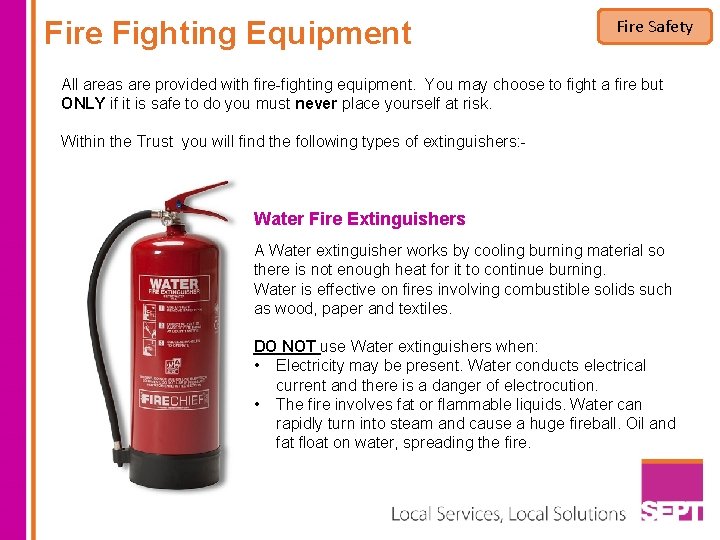
Fire Fighting Equipment Fire Safety All areas are provided with fire-fighting equipment. You may choose to fight a fire but ONLY if it is safe to do you must never place yourself at risk. Within the Trust you will find the following types of extinguishers: Water Fire Extinguishers A Water extinguisher works by cooling burning material so there is not enough heat for it to continue burning. Water is effective on fires involving combustible solids such as wood, paper and textiles. DO NOT use Water extinguishers when: • Electricity may be present. Water conducts electrical current and there is a danger of electrocution. • The fire involves fat or flammable liquids. Water can rapidly turn into steam and cause a huge fireball. Oil and fat float on water, spreading the fire.
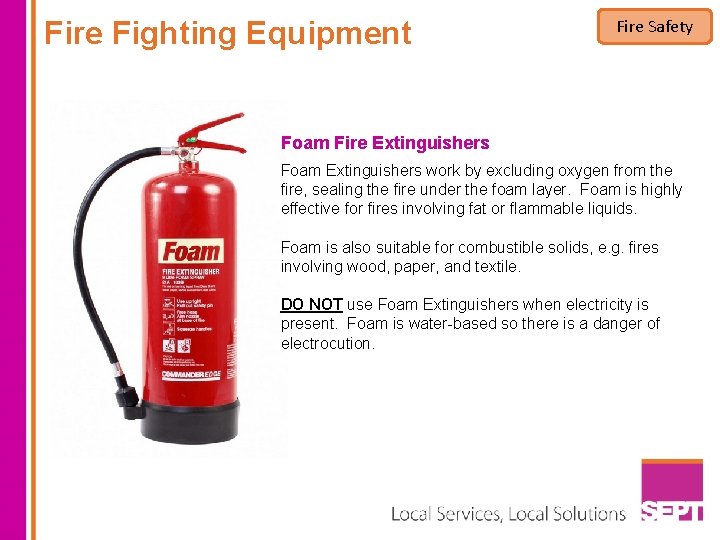
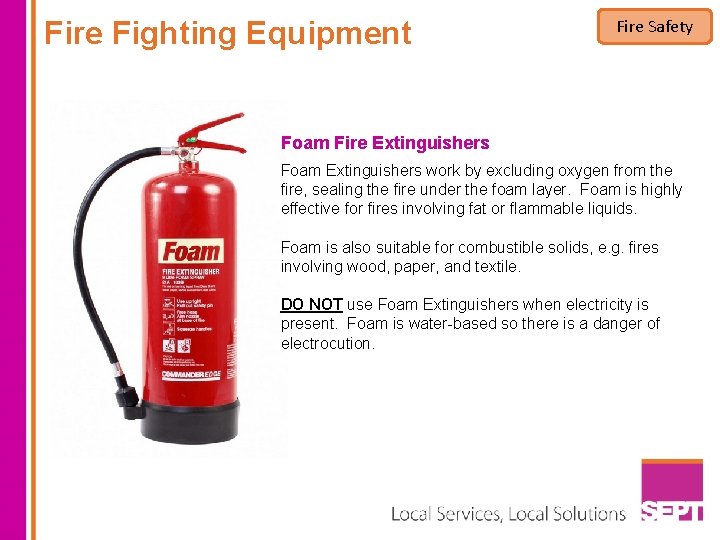
Fire Fighting Equipment Fire Safety Foam Fire Extinguishers Foam Extinguishers work by excluding oxygen from the fire, sealing the fire under the foam layer. Foam is highly effective for fires involving fat or flammable liquids. Foam is also suitable for combustible solids, e. g. fires involving wood, paper, and textile. DO NOT use Foam Extinguishers when electricity is present. Foam is water-based so there is a danger of electrocution.
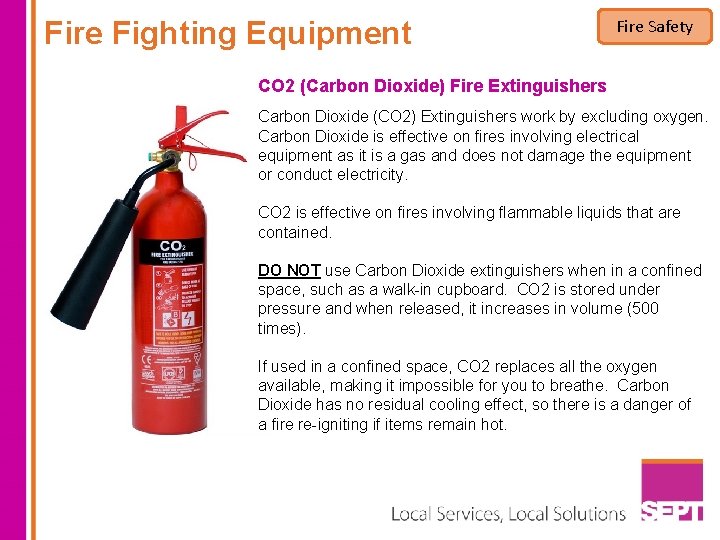
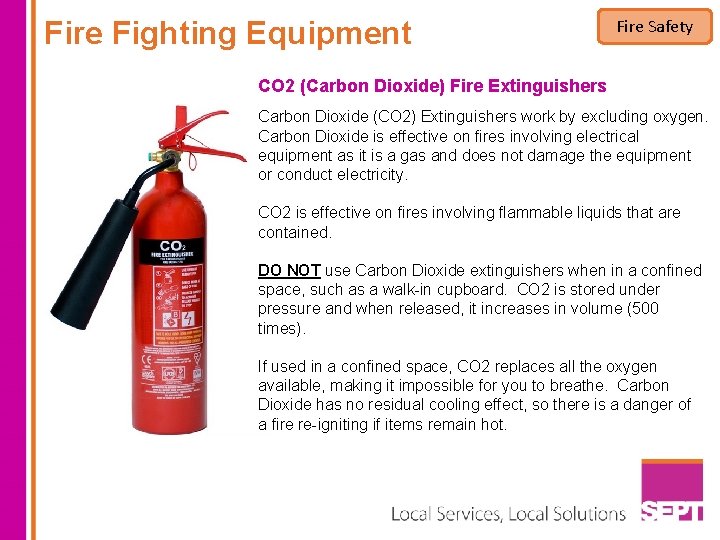
Fire Fighting Equipment Fire Safety CO 2 (Carbon Dioxide) Fire Extinguishers Carbon Dioxide (CO 2) Extinguishers work by excluding oxygen. Carbon Dioxide is effective on fires involving electrical equipment as it is a gas and does not damage the equipment or conduct electricity. CO 2 is effective on fires involving flammable liquids that are contained. DO NOT use Carbon Dioxide extinguishers when in a confined space, such as a walk-in cupboard. CO 2 is stored under pressure and when released, it increases in volume (500 times). If used in a confined space, CO 2 replaces all the oxygen available, making it impossible for you to breathe. Carbon Dioxide has no residual cooling effect, so there is a danger of a fire re-igniting if items remain hot.
Fire Fighting Equipment Fire Safety Fire Blankets are made of fire-resistant materials. They are particularly useful for smothering small fires or for wrapping around a person whose clothing is on fire. Fire Blankets are most often found in kitchen-like areas. It should not be located too close to any appliance (kettle, microwave, toaster) as you may not be able to reach it in the event of a fire.
Question Fire Safety Which type of fire extinguisher would you use to remove oxygen? Foam Water CO 2 Continue START FINISH
Raising the Alarm Fire Safety If you discover a fire YOU MUST: v Immediately activate the fire alarm by operating the nearest Call-point and shout to notify anyone in the vicinity. v Evacuate by the safest route following your local Fire Safety Procedures. v Close all windows and doors as you leave and area. v Call 999 to alert the Fire & Rescue Service. START FINISH
Raising the Alarm Fire Safety If you discover a fire DO NOT: v Panic, it can affect your ability to make safe decisions and can make others panic. v Risk being trapped. Never move to a position where the fire is between you and your exit. If the fire spreads suddenly, you may be cut off. v Put yourself in further danger. v Attempt to tackle a fire unless you are certain you can do so safely. If there is any doubt, GET OUT - leave it to the Fire Brigade. START FINISH

If the fire alarm is activated Fire Safety If the fire alarm is activated YOU MUST: v Calmly follow you local Fire Safety procedure. v If you're with a visitor, ask them to follow you. If the fire alarm is activated YOU MUST NOT: v Stop to collect your personal belongings. v Attempt to return to your own workstation or try to finish the work you are doing. v Use lifts or escalators (unless they have been specifically designed to allow for fire evacuation) as the power may be switched off and you may become trapped or have an accident. Remember Smoke is as dangerous as fire. Smoke also rises so, if you are evacuating from a smoke filled area, the safest breathing area is likely to be nearest to the floor. START FINISH
Question Fire Safety Elevators should be used as an escape route in the event of a fire TRUE FALSE Continue START FINISH
Review – Fire Procedures v When the fire alarm is activated, follow your Fire Safety Procedure immediately. v If you discover a fire, shout to notify those in the immediate danger area and activate the fire alarm. Follow your Fire Safety Procedure immediately. v When evacuating from a smoke filled room, the safest breathing area is nearest the floor. v Never place yourself in further danger. Only tackle a fire if you are certain that you can do so safely. v If you have evacuated from the building, go immediately to your Assembly Point. START FINISH Fire Safety
Good Housekeeping and Maintenance Fire Safety The prevention and control of fire is all about stopping heat, fuel and oxygen coming together. Good housekeeping habits and the maintenance of fire precautions are an important part of fire prevention and creates a safe workplace. Good housekeeping reduces risk by: v Limiting the amount of flammable and combustible materials in the workplace - quantities greater than the daily need should be kept in a secure store room. v Controlling ignition sources v Keeping work areas, aisles, sidewalks, stairways, and safety equipment should be kept clear of loose materials, scraps, etc. Keep all fire doors closed - Fire doors must never be held open with wedges; the Trust provides a number of fittings that allow doors to be held open, but will allow them to close on the operation of the fire alarm. Some fire doors do not have self-closing devices, and are normally kept locked shut. START FINISH
Summary Fire Safety Summary Prepare yourself by making sure you know the Fire Safety Procedures in your workplace. Ask yourself: v v Where is the nearest Fire Alarm? Where is the nearest Fire Exit and where does it lead? Where is the nearest Fire Extinguisher and do I know how to use it? What is the Evacuation Procedure, including for those who need help to leave? v Where is my Assembly Point? v Who is my Cascade Fire Safety Trainer and Fire Warden? If you don't know the answer to any of those questions, you should find out from your Line Manager! START FINISH