STRUCTURE FUNCTION OF THE RENAL SYSTEM AND RENAL


- Slides: 37
STRUCTURE & FUNCTION OF THE RENAL SYSTEM AND RENAL DIAGNOSTIC PROCEDURES
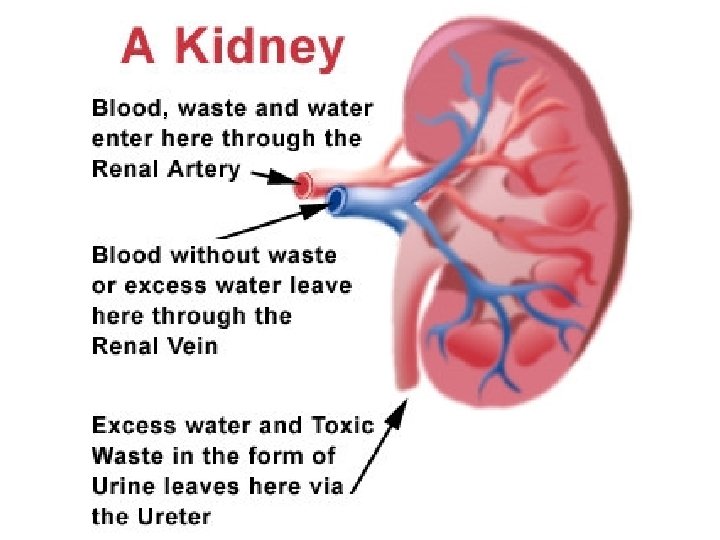
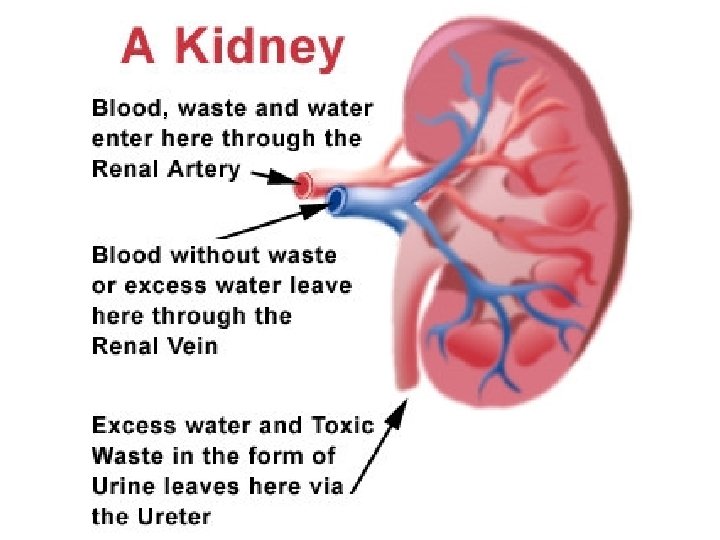
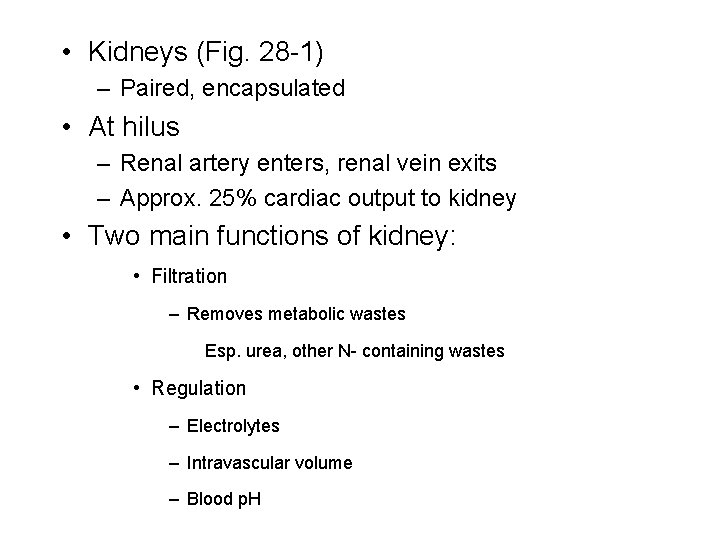
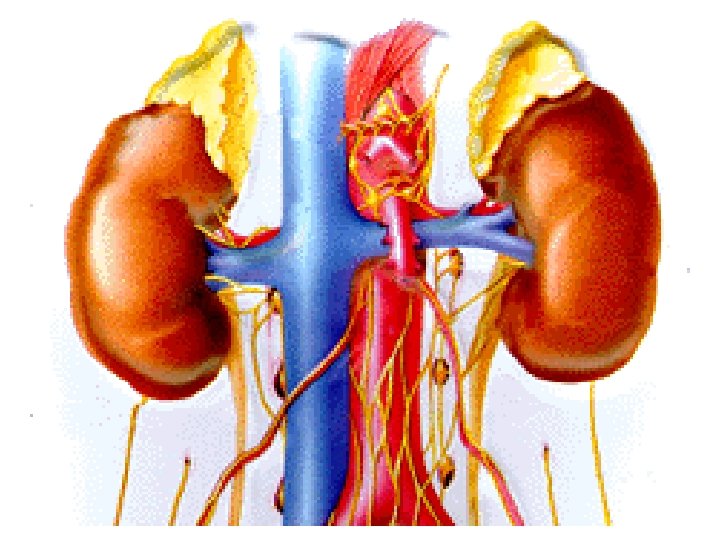
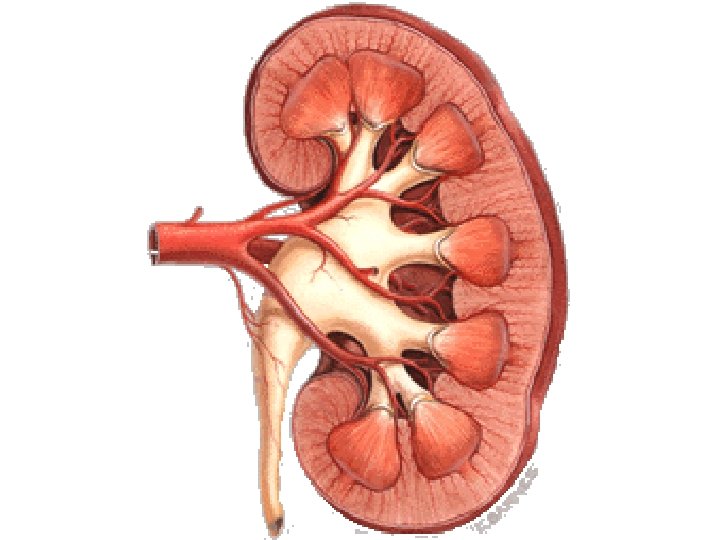
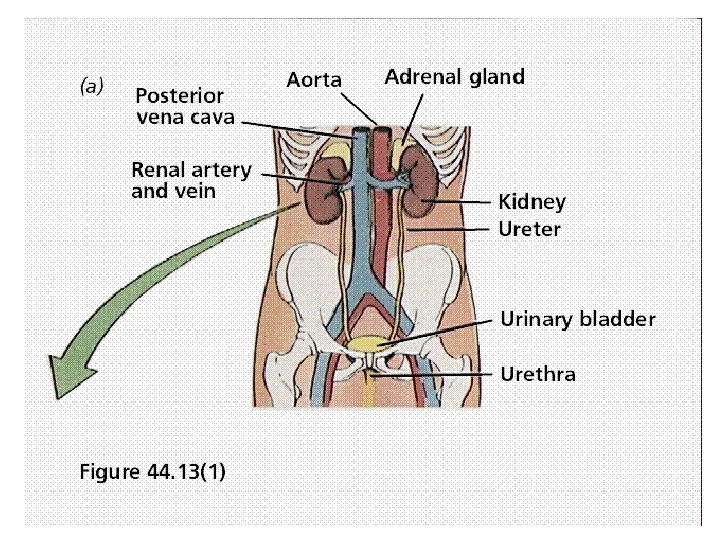
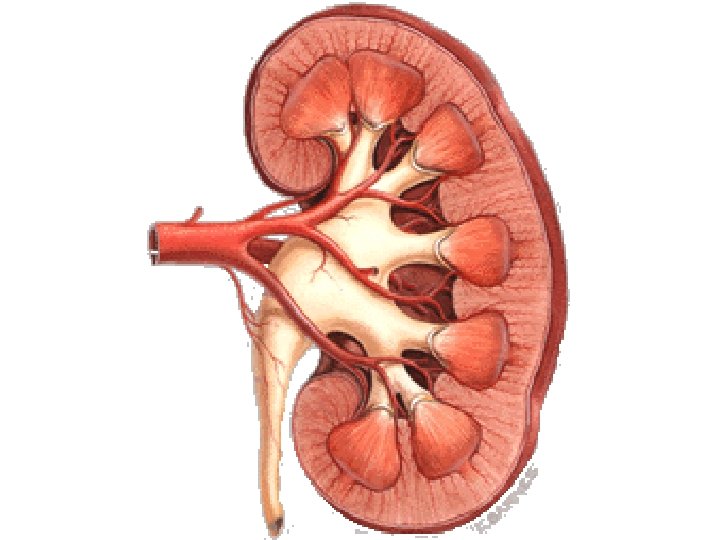
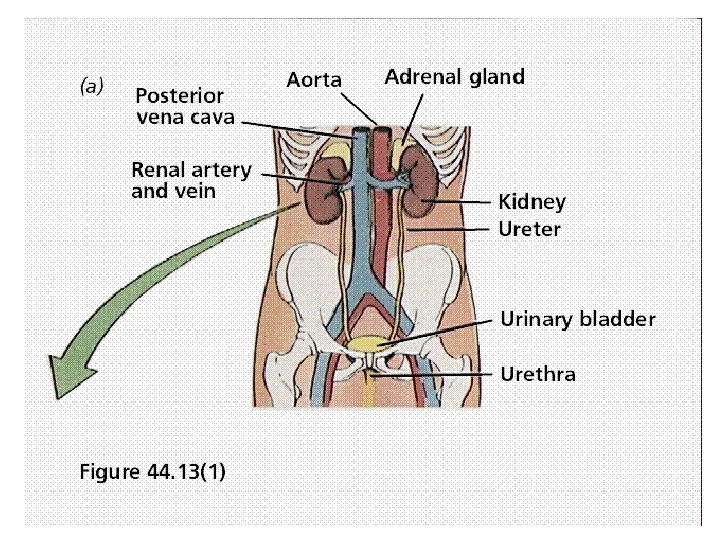
• Kidneys (Fig. 28 -1) – Paired, encapsulated • At hilus – Renal artery enters, renal vein exits – Approx. 25% cardiac output to kidney • Two main functions of kidney: • Filtration – Removes metabolic wastes Esp. urea, other N- containing wastes • Regulation – Electrolytes – Intravascular volume – Blood p. H
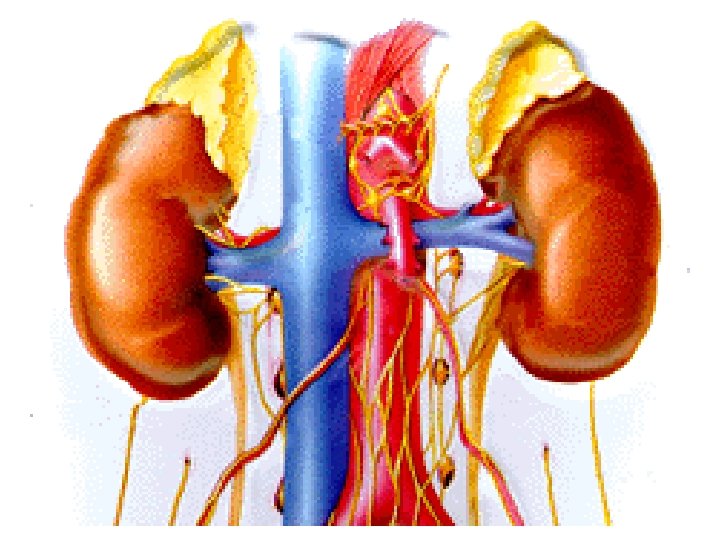
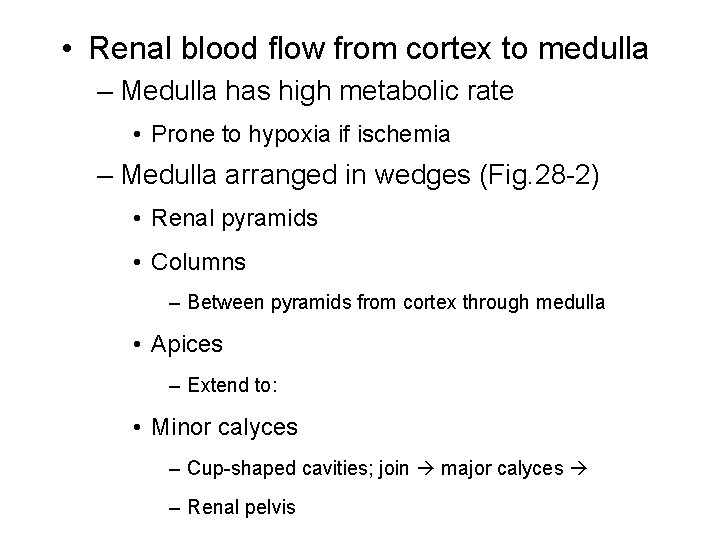
• Renal blood flow from cortex to medulla – Medulla has high metabolic rate • Prone to hypoxia if ischemia – Medulla arranged in wedges (Fig. 28 -2) • Renal pyramids • Columns – Between pyramids from cortex through medulla • Apices – Extend to: • Minor calyces – Cup-shaped cavities; join major calyces – Renal pelvis
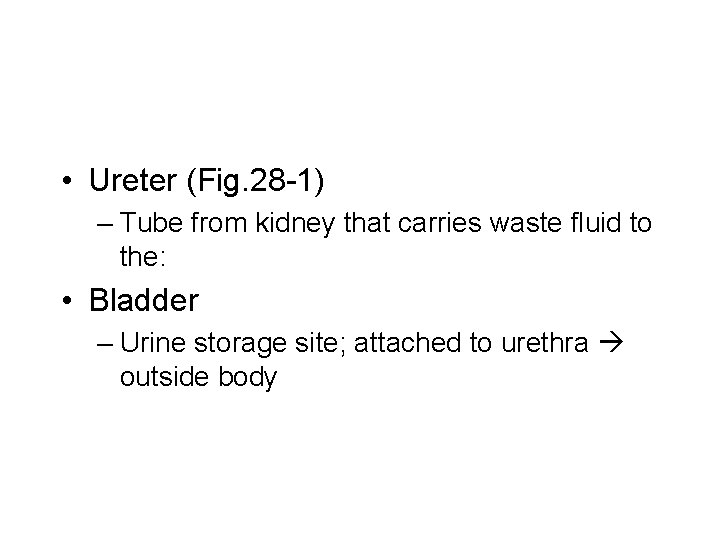
• Ureter (Fig. 28 -1) – Tube from kidney that carries waste fluid to the: • Bladder – Urine storage site; attached to urethra outside body
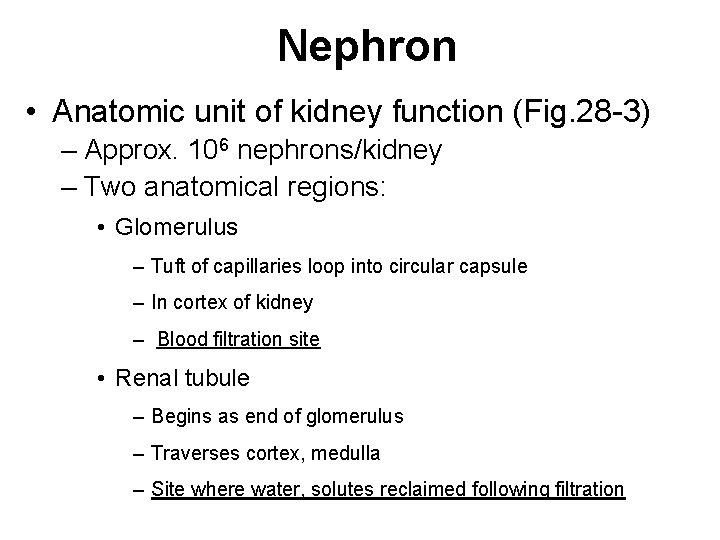
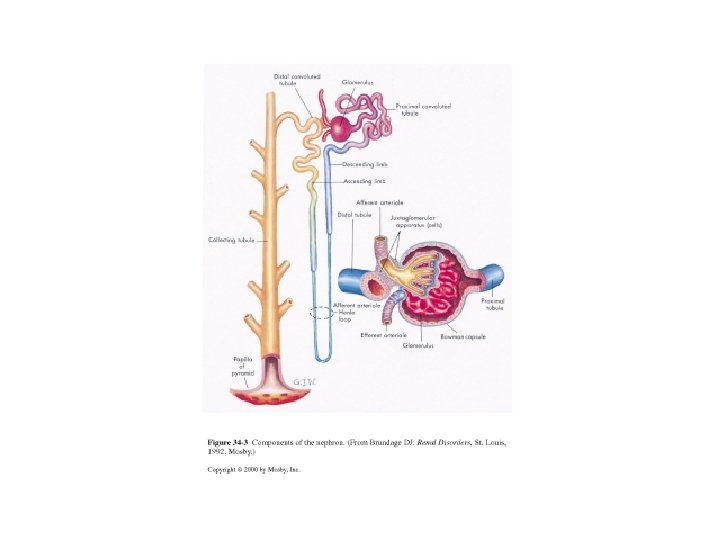
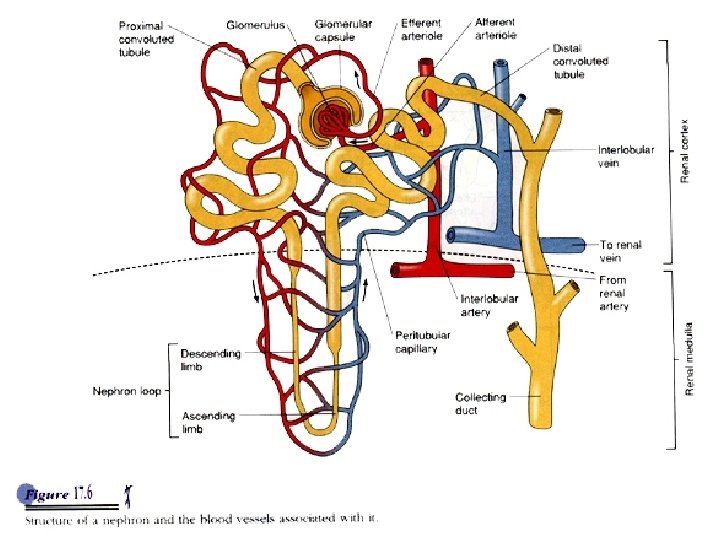
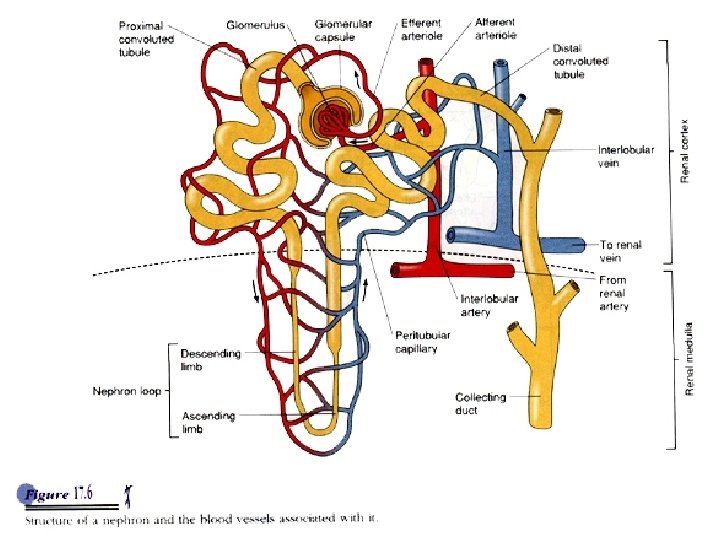
Nephron • Anatomic unit of kidney function (Fig. 28 -3) – Approx. 106 nephrons/kidney – Two anatomical regions: • Glomerulus – Tuft of capillaries loop into circular capsule – In cortex of kidney – Blood filtration site • Renal tubule – Begins as end of glomerulus – Traverses cortex, medulla – Site where water, solutes reclaimed following filtration
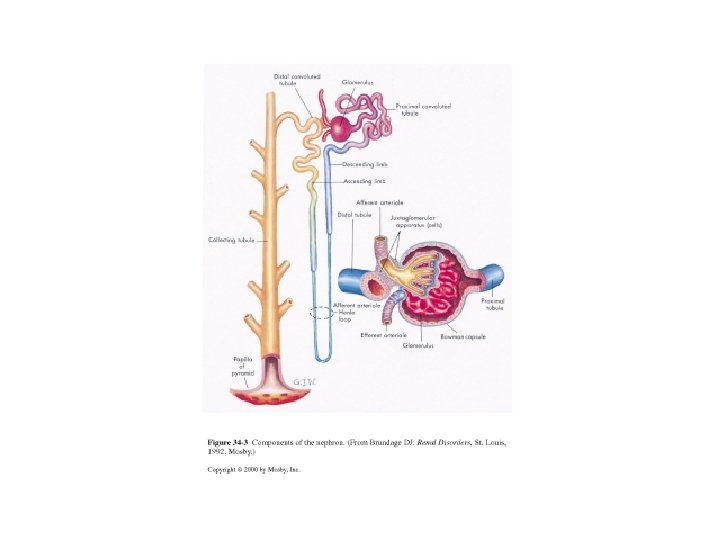

• Renal tubule – cont’d – Anatomical areas: – Proximal, convoluted tubule » Impt to reabsorption of water, electrolytes – Loop of Henle » Hairpin loop » Impt to urine concentration – Distal tubule » Both straight and convoluted » Impt to reabsorption in response to hormonal signals – Collecting ducts » Impt to Afine tuning@ of water, electrolytes
Renal Tubule Summary • Anatomical areas: – Proximal, convoluted tubule • Impt to reabsorption of water, electrolytes – Loop of Henle • Hairpin loop • Impt to urine concentration – Distal tubule • Both straight and convoluted • Impt to reabsorption responding to hormonal signals – Collecting ducts • Impt to fine tuning of water, electrolytes
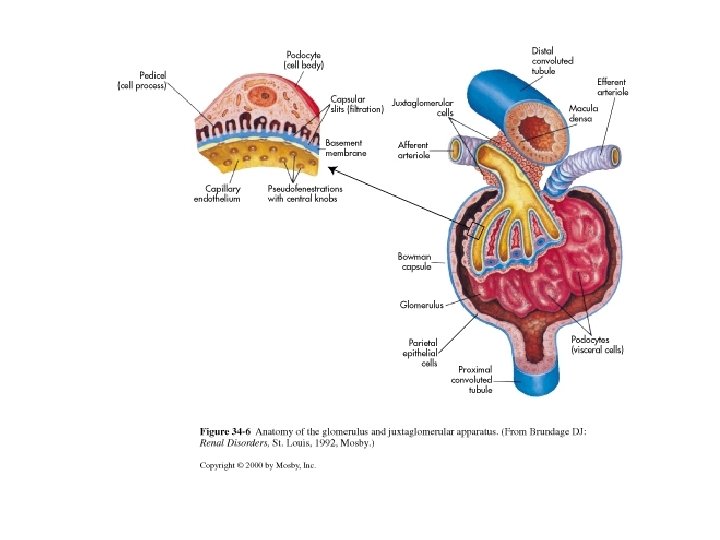
Renal corpuscle • Bowman's capsule + glomerular capillary tuft (Fig. 28 -6) • Bowman's capsule – Circular – Space inside = Bowman’s space – Narrows to form proximal tubule • Glomerular capillaries arranged in loops
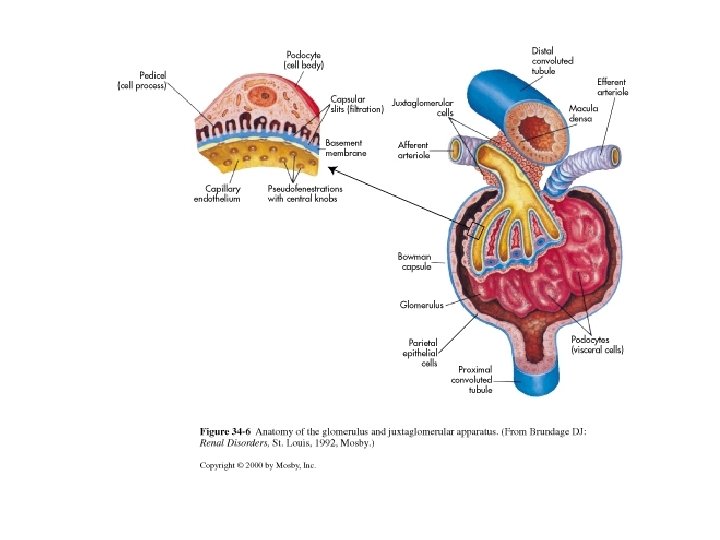
• Glomerular capillary membranes (Fig. 28 -6) – Blood components from artery filtered here – Glomerular capillary tuft -- three membrane layers • Different than most other capillaries in body – Cells of membrane layers -- unique w/ unique structures in each layer • Inner capillary endothelium • Basement membrane • Epithelium – Primary urine forms as result of filtration
• Glomerular filtration – Glomerulus permeable to • Water • Electrolytes • Small organic molecules (ex: glucose, urea, creatinine) – Not permeable to • Rbc’s • Wbc; s • Molecules w/ MW > 70, 000 (so most proteins) – Leave glomerulus (still in blood) through the efferent arteriole – Size and charge of molecules impt to whether molecule will be filtered or not
– Capillary pressures important (Fig. 28 -11, Table 28 -1) • Hydrostatic Pressure forces fluids through filter – What is the filter? • Forces opposing BHP: – Colloid osmotic P » Due to blood cells, proteins, as in “regular” capillaries – Hydrostatic P of fluid already in Bowman=s space • Net filtration P = (forces favoring filtration) ‑ (forces opposing filtration)(Table 28 -1) – Positive or negative net filtration in a healthy system?
– Glomerular filtration rate (GFR) • Volume of plasma filtered at glomerulus per unit time • Approx. 180 L/day = 120 m. L/min – BUT only 1 -2 L/day excreted » About 99% of filtrate reabs’d in tubule • GFR depends on factors affecting fluid pressures in nephron and vasculature – Arteriolar resistance changes capillary hydrostatic P in glomerulus – Decr’d blood flow to kidney from systemic circulation decr’s GFR – Obstruction to urine outflow may incr back pressure at Bowman’s capsule, so decr GFR – Loss of protein‑free fluid alters COP, so alters net filtration – Renal disease
Hormonal Regulation of GFR • Through renin • changes in renal blood flow, so changes in GFR – Occur and regulated locally (at kidney tissue) and systemically • Two impt hormones affect GFR: – Aldosterone (regulates Na+) – ADH (regulates water)
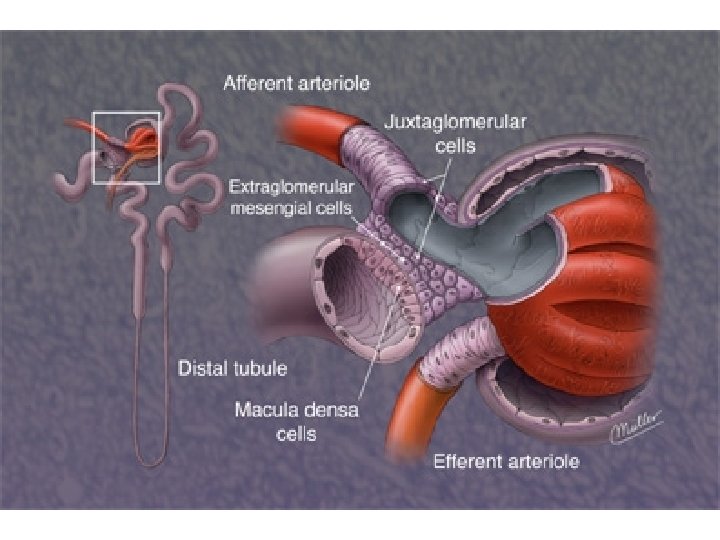
• Specialized cells sensitive to specific hormones – Juxtaglomerular aparatus • Juxtaglomerular cells – Lie around afferent arteriole • Macula densa – Portion of renal distal tubule » Loops back up toward Bowman’s capsule » Butts up against glomerulus – Located in space between afferent and efferent arterioles
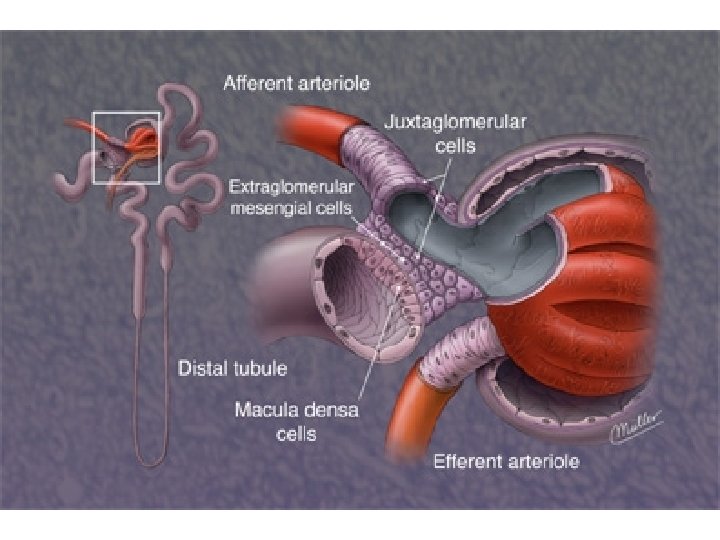
– Together juxtaglomerular cells + macula densa cells (or juxtaglomerular apparatus) control: • Blood flow into nephron at glomerulus, so – Glomerular filtration • Renal secretion – Because sensitive to hormones such as aldosterone and ADH

Renal Tubule Physiology • Extend from Bowman’s capsule • Receive and process filtrate from capsule • Processing of fluid by two major forces: tubular reabsorption and secretion – Reabsorption • Occurs through minute pores in tubules • Compounds reabsorbed from tubule peritubular capillaries (surround the tubules) blood
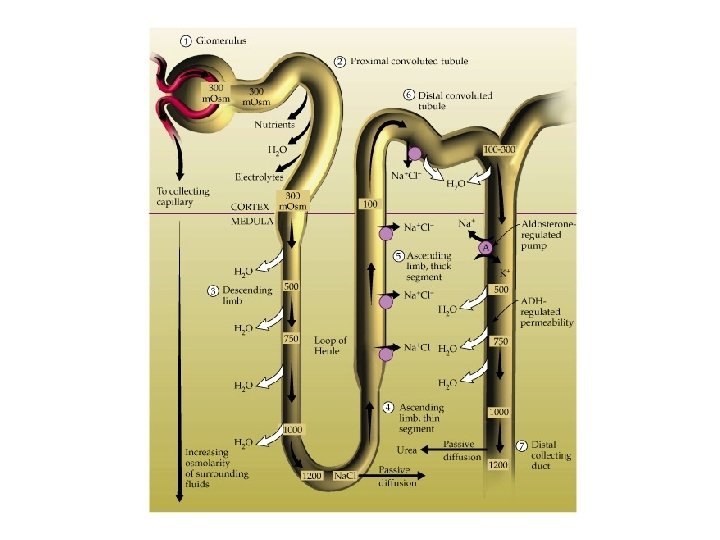
– Secretion • Opposite of reabsorption • Compounds secreted go from blood capillaries renal tubule filtrate – By the end of the proximal tubule • Water, Na+ – 60 -70% reabsorbed back into blood • K+, glucose, bicarb, Ca+2, amino acids, uric acid – Approx 90% reabsorbed back into blood
– Loop of Henle • Mostly Na+, Cl-, H 2 O move to adjust concentration of fluid in tubule • Loop has ascending, descending regions – Cells in some regions permeable to water » Here water can move out of tubule – Cells in other regions not permeable to water » Here water trapped in the tubule – Cells in some regions permeable to Na+ » Here Na+ can move out of the tubule – Cells in other regions not permeable to Na+ » Here Na+ is trapped in the tubule
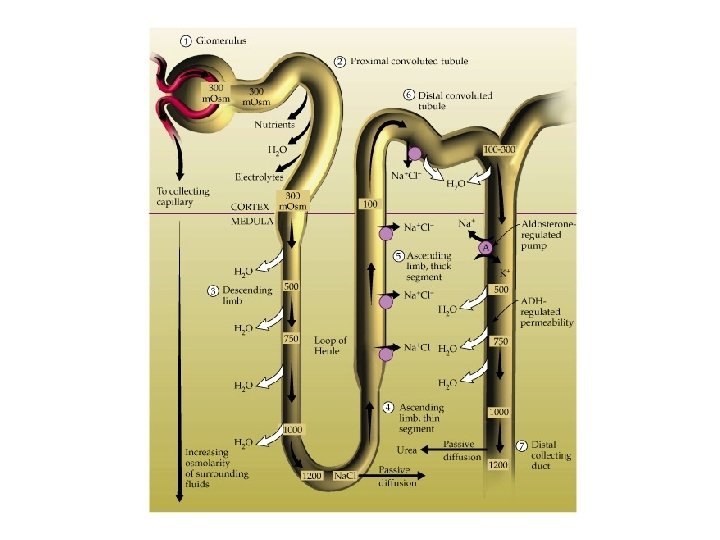
• Resulting fluid through loop goes from isotonic to hypertonic to hypotonic – Due to differences in kidney cells from cortex to medulla and different permeabilities of tubule to different molecules – As the fluid leaves loop of Henle, it is hypotonic (so dilute, compared to other body fluids)
– Distal tubule ‑ final regulation of water, and acid‑base balance • Water, Na+, bicarb – Reabsorbed here when ADH present • K+, urea, H+, ammonia – Secreted • Hormones important to regulation here – ADH (antidiuretic hormone) » incr’d water reabsorption – Aldosterone » incr’d Na+ reabsorption – Parathyroid hormone (PTH) » incr’d Ca+2 reabsorption
– Collecting duct • Final urine concentration adjusted • Final p. H balance adjusted • Final product = urine low in volume (compared to what was filtered), and high in osmotic concentration (the body rids itself of unwanted molecules)
Renal diagnostic procedures (Table 28 -3 p. 804) • Urinalysis – Non‑invasive, inexpensive – Normal urine properties well-known, easily measured • Specific gravity – – Solute concentration in urine Correlates w/ osmolality in normal urine Normal value: 1. 025 -1. 032 Usually describes ADH • Because ADH controls water reabsorption • What ADH problem might you expect if specific gravity were high? Low?
• Urine sediment can be examined microscopically – Red blood cells • Hematuria = large number rbcs in the urine – Should be few/none – Why? What keeps rbc’s in the body? – Casts • Precipitates from cells lining the renal tubules – Red cells suggest tubule bleeding – White cells suggest tubule inflammation – Epithelial cells suggest degeneration, necrosis of tubule cells
– Crystals • May form as urine cools • Observed microscopically • Indications – Inflammation – Infection – Stones – White blood cells (pyuria) • From urinary tract infection – Bacteria • Infection
• Clearance tests – Determine how much of substance can be cleared from blood by kidney per unit time • Indirect measure of GFR, tubular reabs’n/secr’n, renal blood flow – GFR • Best estimate of overall kidney health • Decreases w/ lost or damaged nephrons • Use creatinine clinically – Biochem prod’d by muscle, released to blood at constant rate – Freely filtered at the glomerulus – Neither reabs=d nor secr=d as it progresses through the tubule, so: • Amount creatinine excreted = amount creatinine filtered – Can be calculated: » Amount creatinine in urine over time = (vol. urine/time) x (urine concentration of creatinine)
• Blood tests – Plasma creatinine concentration (Pcr) • Normal levels = 0. 7 -1. 5 mg/d. L • Use same biochem described for clearance test, but measured in blood instead of in urine • Again, creatinine filtered at glomerulus; neither reabs’d nor secr’d; and amount creatinine filtered = amount excreted • Get increased Pcr if chronic disease affecting GFR – When GFR decr’d, get decr’d filtration of creatinine out of blood (and into urine), so – Blood (plasma) creatinine increases • Useful: – To monitor changes in chronic renal function • BUT Pcr increases with trauma, muscle tissue breakdown
– Blood Urea Nitrogen (BUN) • Urea prod’d constantly as cells metabolize proteins • Measurement of BUN reflects both GFR and urine concentrating ability • Normal levels 10 -20 mg/d. L • Urea filtered at glomerulus • Urea reabsorbed back into blood at tubules – If decr’d GFR, get incr’d BUN – OR if decr’d blood flow to kidney, get incr’d BUN – Incr’d BUN or Pcr = increase in nitrogenous substances in blood = azotemia