Structure Function of Immune System CELLS AND TISSUES



- Slides: 107
Structure & Function of Immune System
CELLS AND TISSUES OF THE IMMUNE SYSTEM Lympho – reticular system is a complex organization of cells of diverse morphology distributed widely in different organs and tissues of the body. The cells of the system are responsible for the development of specific immunity.
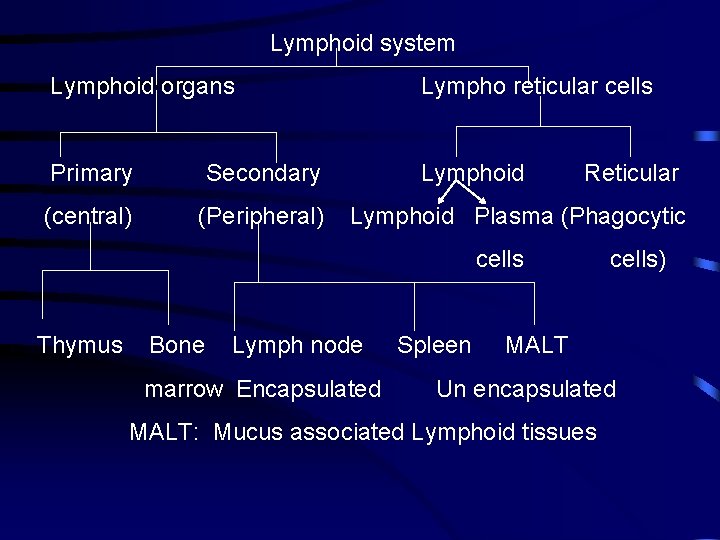
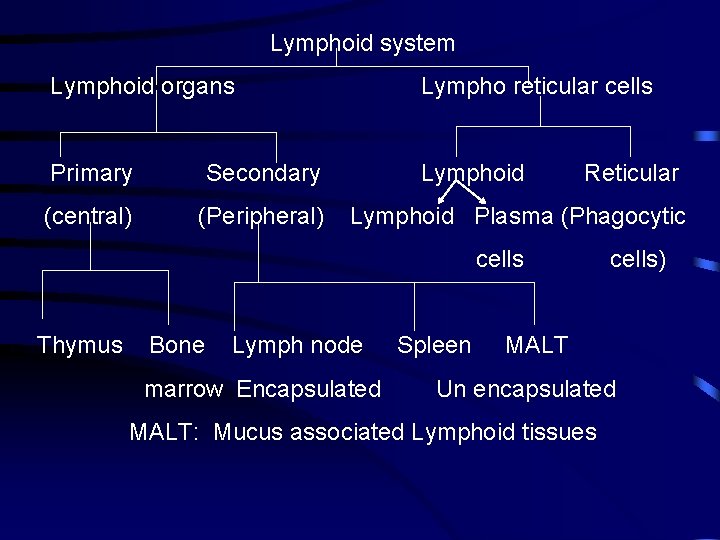
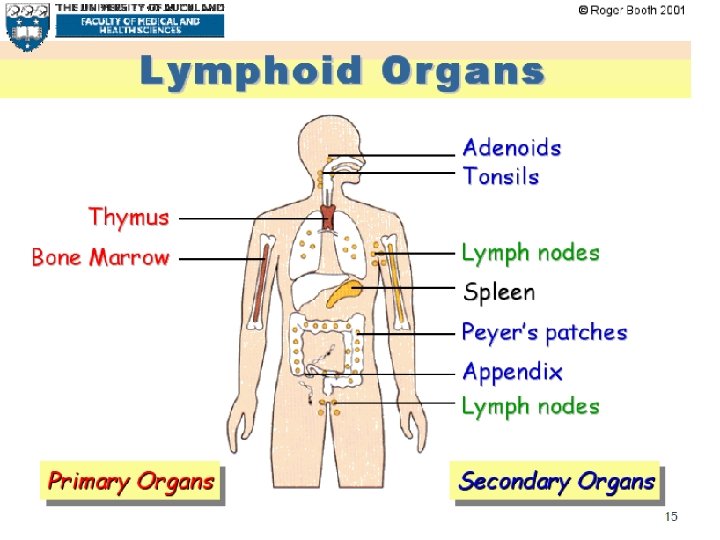
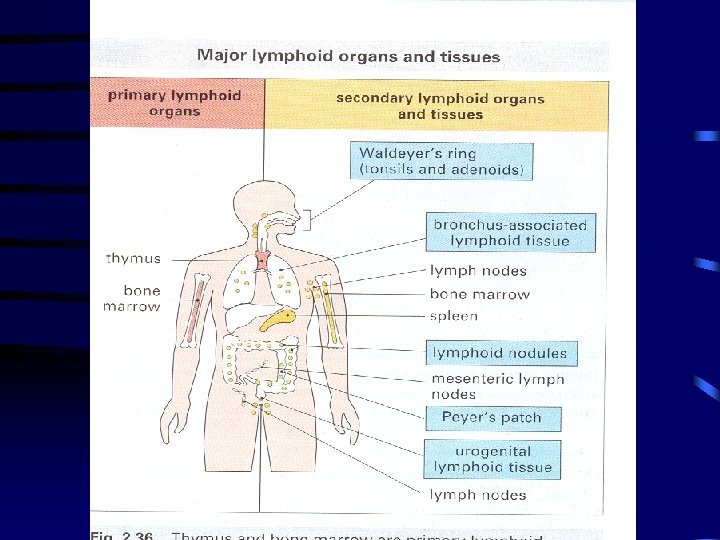
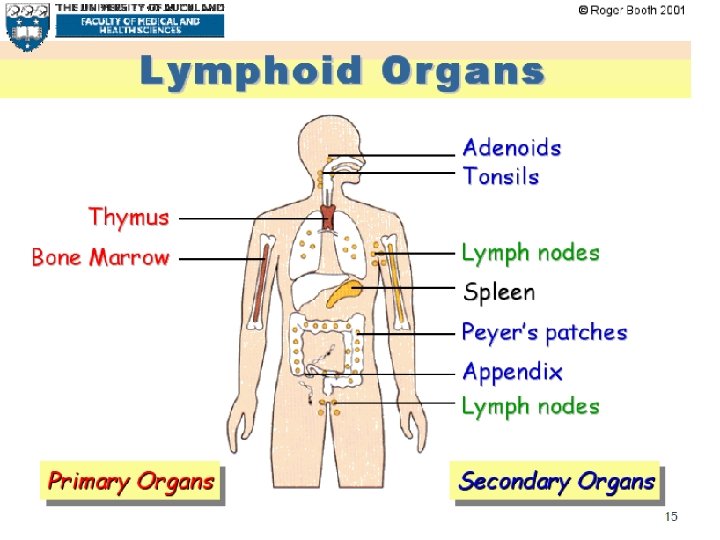
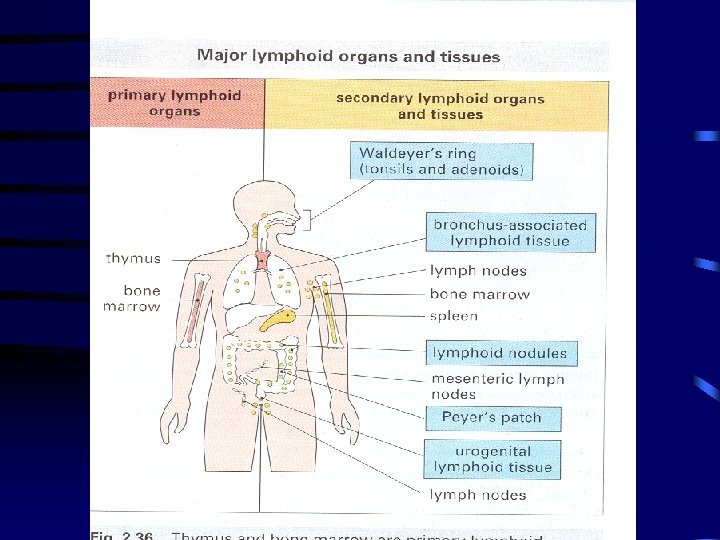
Lymphoid system Lymphoid organs Lympho reticular cells Primary Secondary Lymphoid (central) (Peripheral) Reticular Lymphoid Plasma (Phagocytic cells Thymus Bone Lymph node marrow Encapsulated Spleen cells) MALT Un encapsulated MALT: Mucus associated Lymphoid tissues
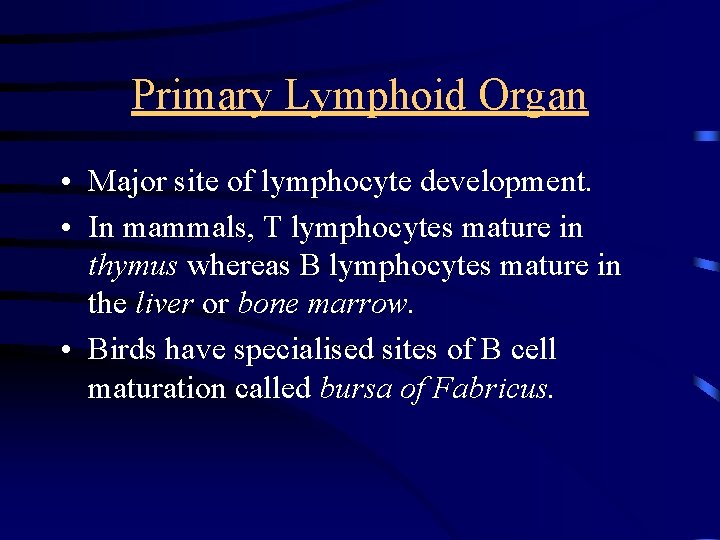
Primary Lymphoid organs (thymus and Bone marrow) Major sites for lymphopoiesis The lymphocytes, develop, differentiate proliferate and mature into functional cells. In mammals T cells mature in thymus and ‘B’ cells in fetal liver cells and Bone marrow. It is in the primary lymphoid organs the lymphocytes acquire the antigen receptors to fight with the antigenic challenge subsequently during life.
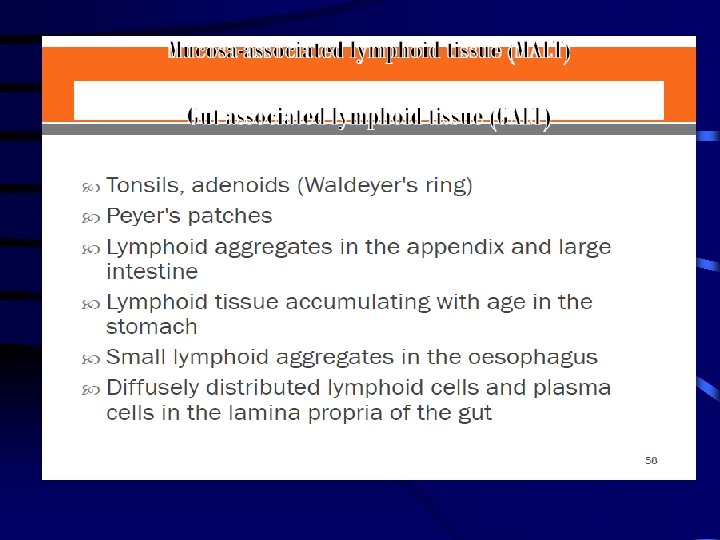
Secondary lymphoid organs Spleen, Lymph node, mucus associated lymphoid tissue (MALT) which include tonsils and payer's patches. Here the lymphocytes interact with lymphocytes and accessory cells (macrophage both phagocytic and antigen presenting) and also with antigen. The immune response is generated and disseminated in secondary lymphoid tissue.
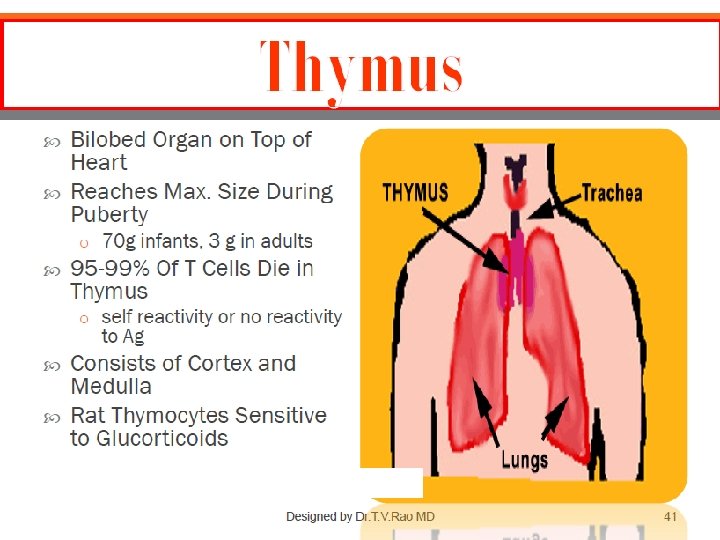
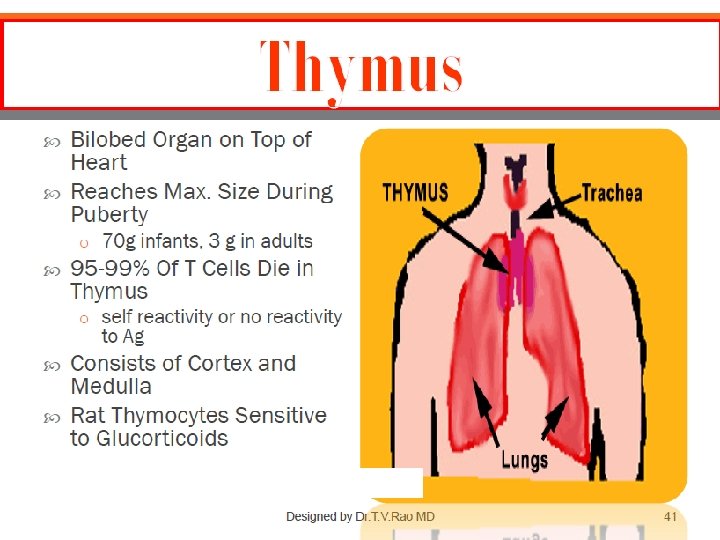
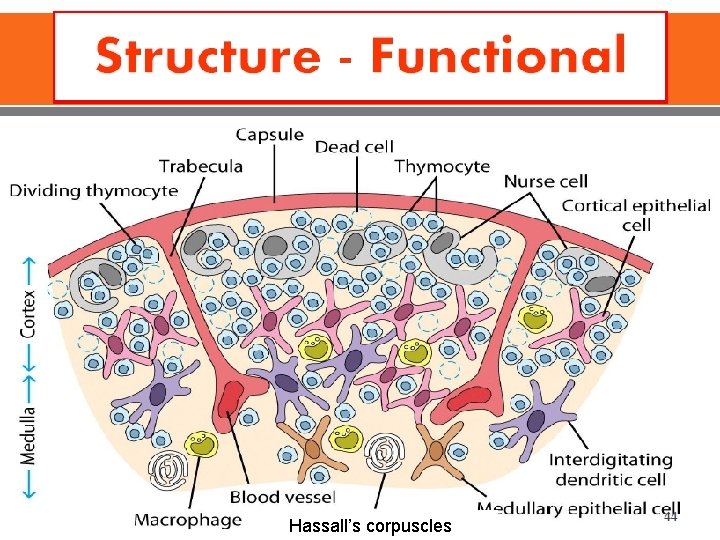
Structure • Two lobes surrounded by a fibrous capsule • Septa from capsule divide the gland into lobules • Outer Cortex and Inner Medulla • Cortex: Actively proliferating small lymphocytes • Medulla: Epithelial cells and mature lymphocytes
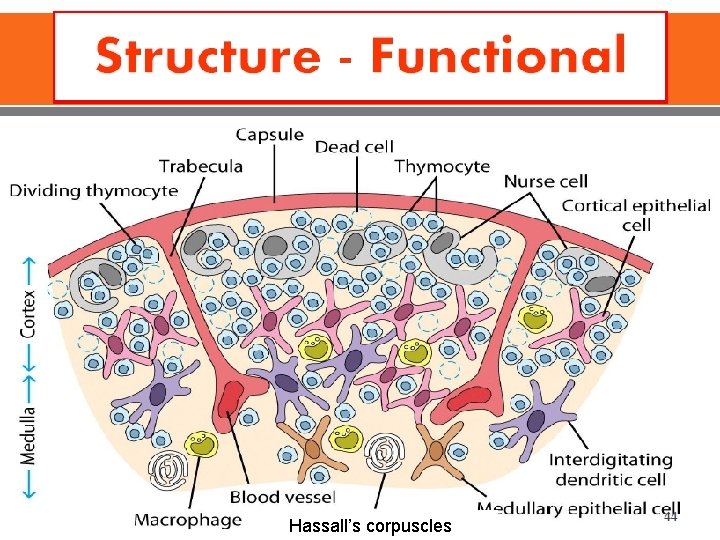
Hassall’s corpuscles
Functions • Production of thymic lymphocytes • Major site for Lymphocyte proliferation • Lymphocyte acquire new surface antigen (‘Thy’ Ag). Lymphocytes conditioned in thymus are called Thymus dependent or T cells. • Lymphocyte proliferation is not Ag dependent. • Immunological competence of lymphocytes • Prethymic lymphocytes are not immunocompetent.
Deficiency • Di. George syndrome: Congenital aplasia of thymus • Runt disease: Deficiency of CMI seen in neonatally thymectomised mice
Bone marrow • Site of origin of all lymphocytes • Site of ‘B-Cell’ origin & development • A Selection process – eliminates B cell with self reactive Ab Receptors
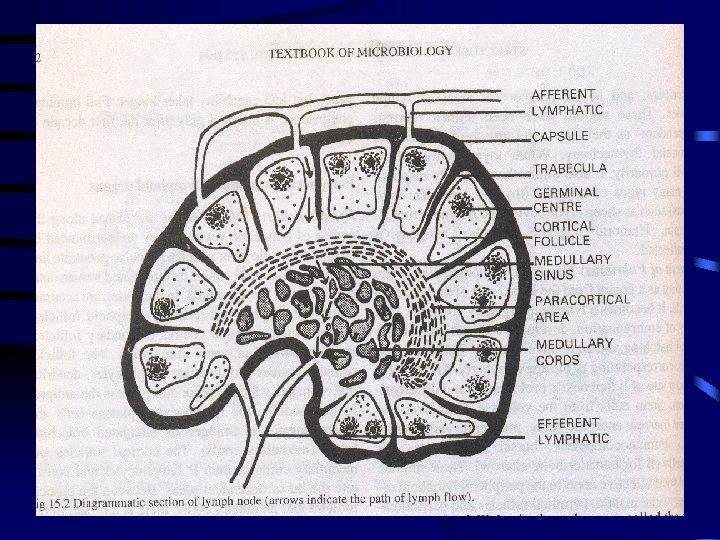
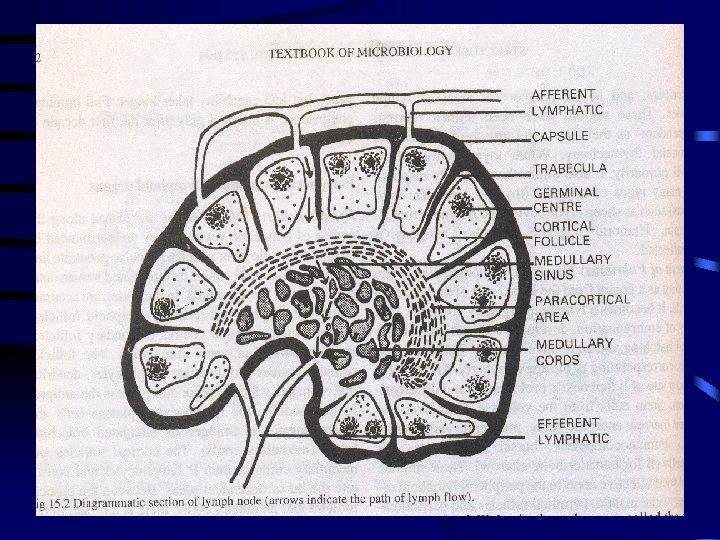
Lymph nodes • • Present along the course of lymphatic channels. Surrounded by a capsule. Consists of outer cortex & inner medulla. Cortex: primary lymphoid follicles (accumulation of lymphocytes) within which on antigenic stimulus, germinal centres develop, called secondary follicles. • Besides lymphocytes, follicles also contain dendritic macrophages which capture and process Ag.
• Medulla: Lymphocytes, Plasma cells, Macrophages are arranged as Medullary cords • Bursa dependent area: Cortical follicles and medullary cords containing B lymphocytes. • Thymus dependent area: Between cortical and medullary cords Paracortical area containing T lymphocytes.
Functions • Act as a filter for lymph. Each group of nodes draining a specific part of body. • Phagocytose foreign materials including microorganisms. • LNs help in proliferation & circulation of T & B cells. • LNs enlarge following local antigenic stimulus.
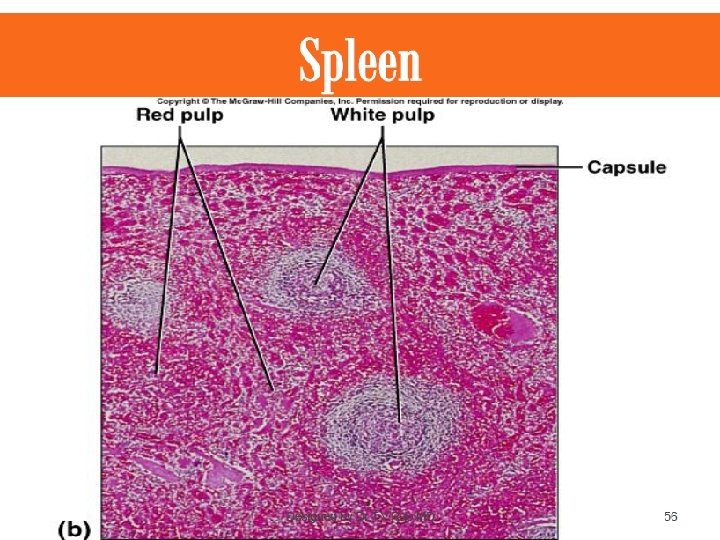
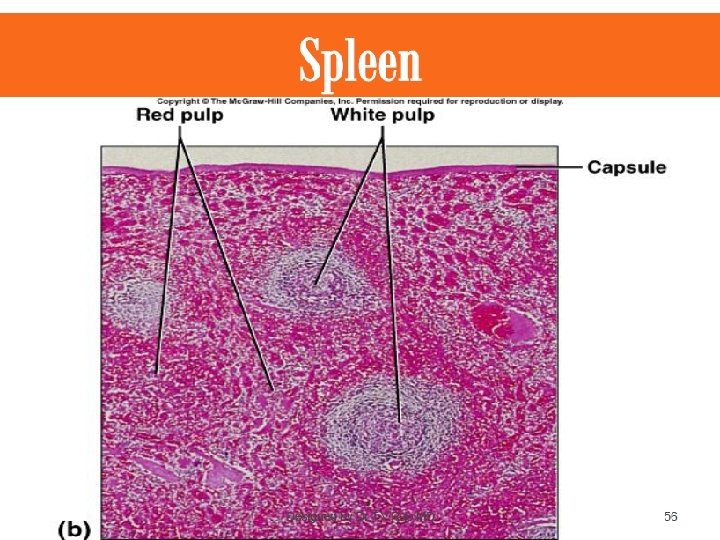
Spleen • Largest lymphoid organ. • Capsulated, trabeculae descend from it dividing spleen into interconnected compartments. • Branches of Splenic artery travel along trabeculae and branch again to form central arterioles. • These are surrounded by a sheath of lymphoid tissue and is called White pulp • The central arterioles proceed into red pulp rich in red blood cells
• Peri arterial lymphoid collection in white pulp is called Malpighian corpuscles or follicles. Rich in T cells • Germinal centres develop following antigenic stimulus. • Surrounding this is a mantle layer of lymphocytes. • Th lymphatic sheath just surrounding central arteriole is Thymus dependent. • Perifollicular region, germinal center and mantle layer: Thymus independent.
Functions • Graveyard for effete Red blood cells • Reserve tank and settling bed for blood and as a systemic filter for trapping blood borne foreign particles • Immunological function of the spleen is primarily directed against blood borne pathogens
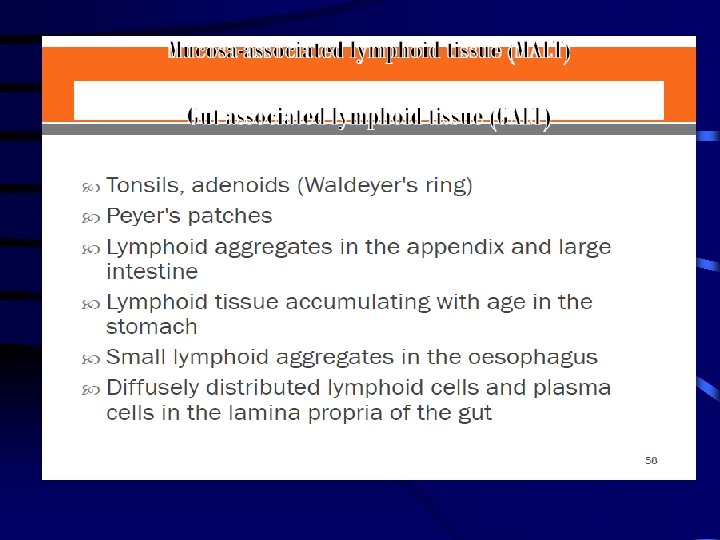
MALT • Mucosa lining the alimentary, respiratory, genitourinary and other Lumina. • Rich collection of lymphoid cells • MALT: Mucosa associated lymphoid tissue • GALT: Gut associated lymphoid tissue • BALT: Bronchus associated lymphoid tissue. • Lymphoid and phagocytic cells • Both B and T cells • Secretary Ig. A predominant

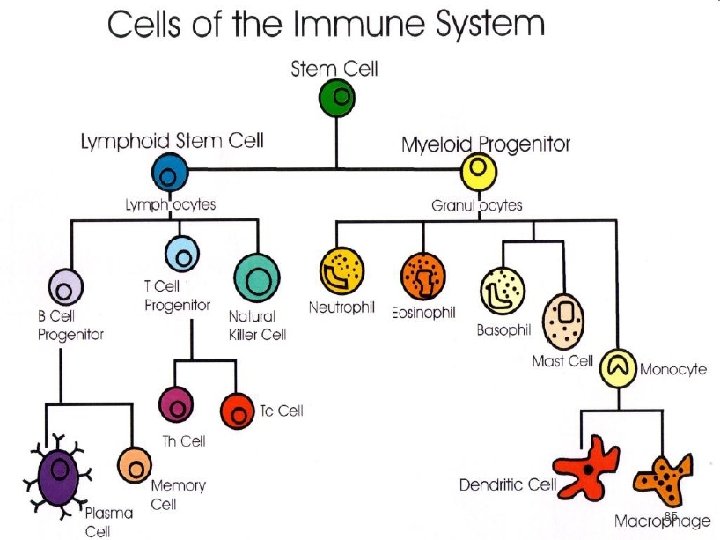
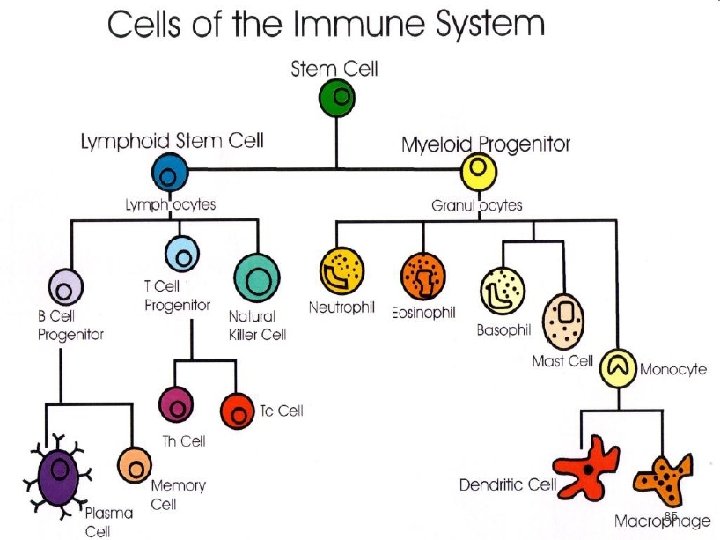
Cells of the Acquired Immune System • Lymphocytes • Antigen presenting cells (APCs)
Subsets of Lymphocytes • 2 subsets : T cells B cells • T cells are thymus derived. • B cells are bone marrow derived. • B cells : ability to synthesise proteins called Immunoglobulins (Igs). Each Ig can bind specifically & with high affinity to a particular Ag.
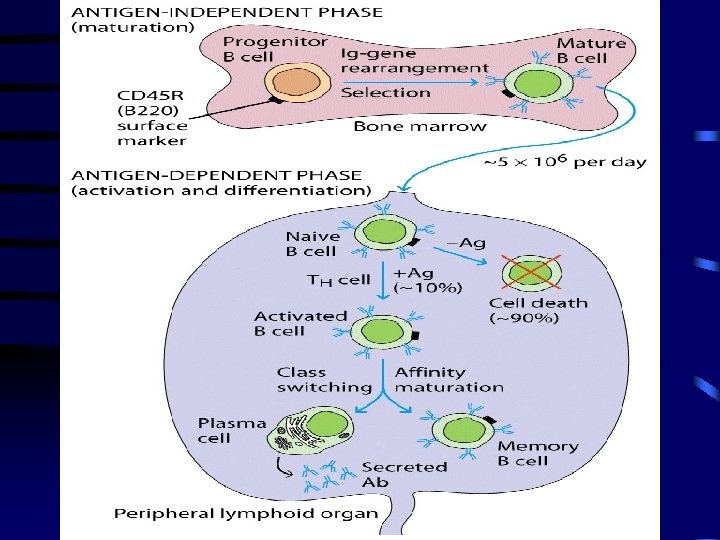
Lymphopoiesis • Occurs in yolk sac, fetal liver then bone marrow throughout rest of life • Mature, naïve B cells released into circulation • B cell production occurs throughout life; does not wane as does T cell production • About 5 million produced per day • Only 10% of B cells mature • Naïve B cells survive about one week • Undergo negative selection
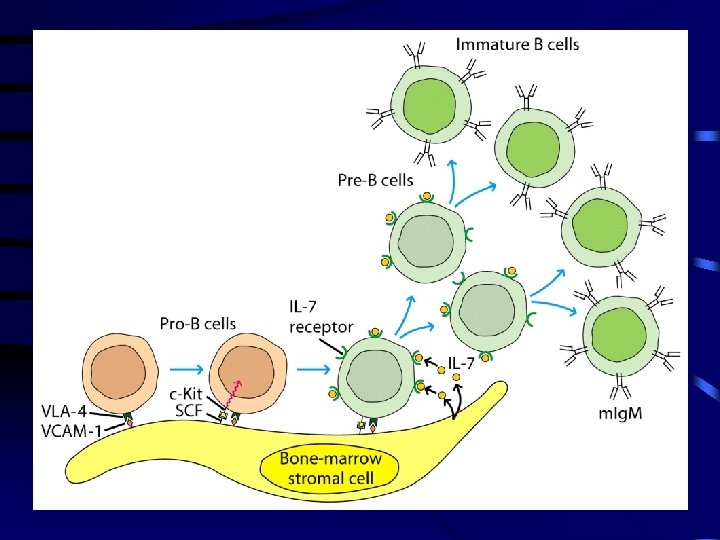
B Cell Development ü Maturation-Stem cells to mature, naïve B cells ü Activation-Ag binding; initiation of cell changes ü Differentiation-Cell division and changes into effector B cells (plasma cells) and memory B cells
B Cell Maturation • • Hematopoietic stem cells(HSC) Lymphoid stem cell (progenitor) B cell progenitor (pro-B cell) Pre-B cell Immature B cell naïve B cell Mature
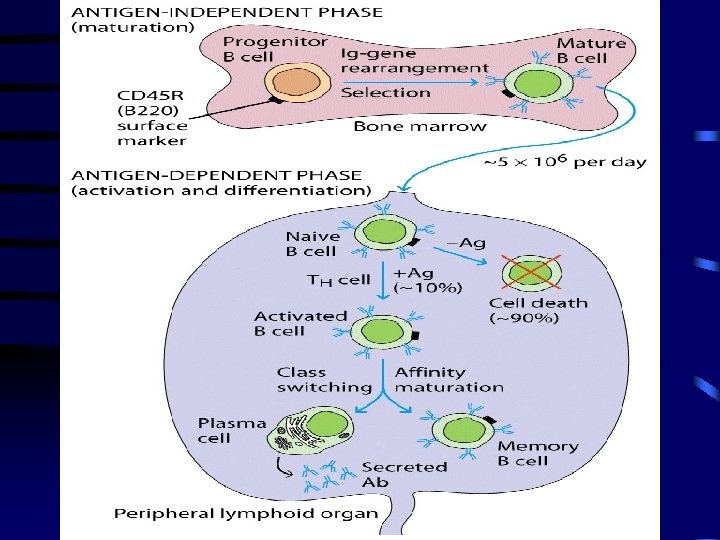
B Cell Changes • Pro B cells – Rearrangement of Ig heavy chain genes – Expression of CD 45 R and CD 19 – Further maturation is dependent on direct interaction with BM stromal cells
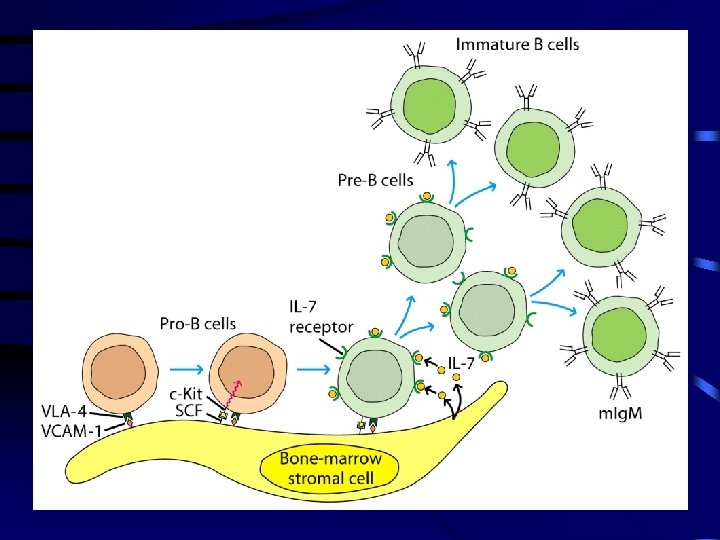
B Cell Changes • Pre B cells – Cell division occurs – Rearrangement of Ig light chain genes – Expression of IL 7 receptor – Expression of mu heavy chains – Shuts down further Ig gene rearrangement
B Cell Changes • Immature B cells – Ig. M expressed on surface – B cell receptor appears – Cells interact with self Ags – Negative selection (clonal deletion) occurs
B Cell Changes • Mature B cells – Migrate out of bone marrow – Both Ig. M and Ig. D expressed on surface – Cell division occurs
B Cell Activation • Triggered by combining with Ag – Two types of Ags that activate B cells • Thymus dependent Ag e. g. soluble proteins • Thymus independent Ag – Type 1, e. g. LPS – Type 2, e. g. capsular polysaccharides
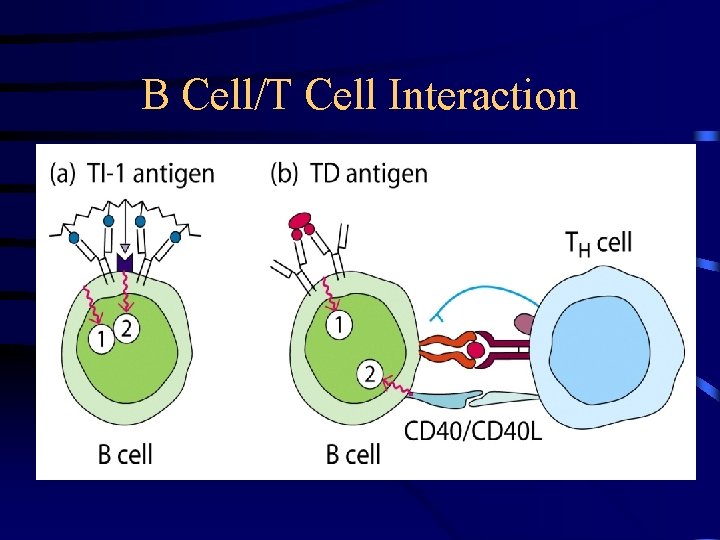
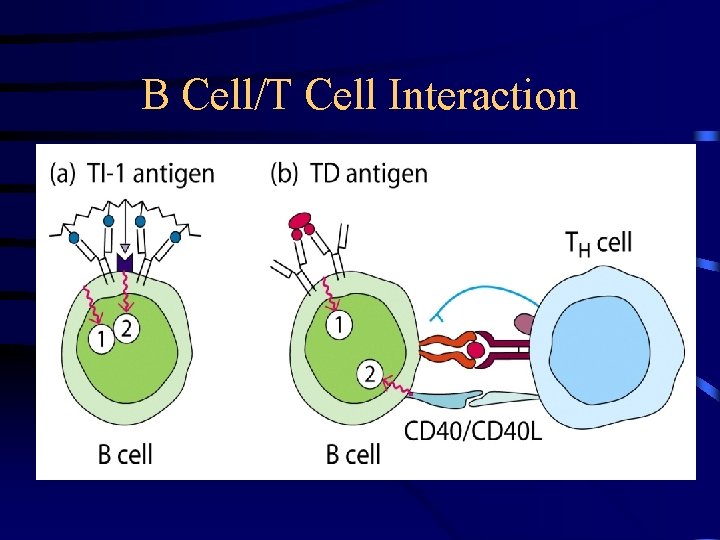
B Cell/T Cell Interaction
B Cell Subsets • B 1 – CD 5 marker – Seen in peritoneum IN NEONATES – Produce natural Ig. M antibacterial antibodies • B 2 – Most B cells (95%) – Drive the Ag response in secondary lymphoid organs
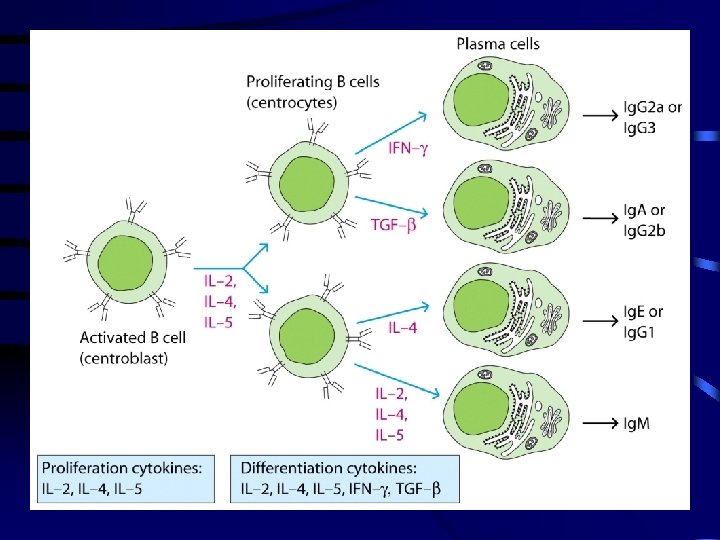
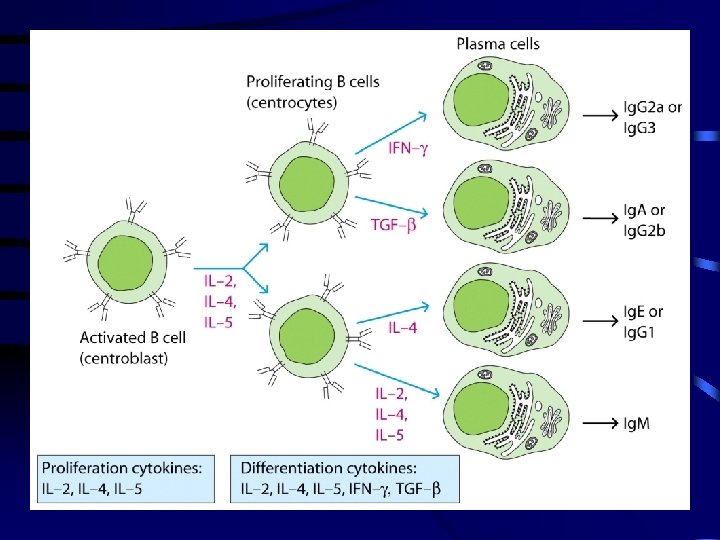
B cell development • Fetal liver & BM – precursor cells, pro B cells. • Pre B cells – rearrangement of immunoglobulin genes & synthesis of Ig. M in the cytoplasm • Immature B cells – Ig. M expressed on the cell surface. • Immature B cells migrate to the periphery & undergo Ig isotype switching.
B cell Activation & Differentiation • B cell activation & proliferation occurs in response to an appropriate Ag. • Forms plasma cells & memory B cells. • Plasma cells secrete Abs. • Mature B cell express Ig in 2 different forms. Membrane bound Ig in resting cells & secreted Ig by the plasma cells.
Functions of B cells • Chief cell type in humoral immunity. • Function as Ag Presenting Cells. • Secrete lymphokines & other factors that influence the growth and activities of other immunologically important cells.
LYMPHOCYTES • Small, round cells present in the peripheral blood, lymphoid organs and in many other tissues. • Constitute 20 -45% of leucocytes in the peripheral blood. • Major cell types in lymphoid organs. • 1012 lymphocytes in human body & only 1% of it is present in the blood.
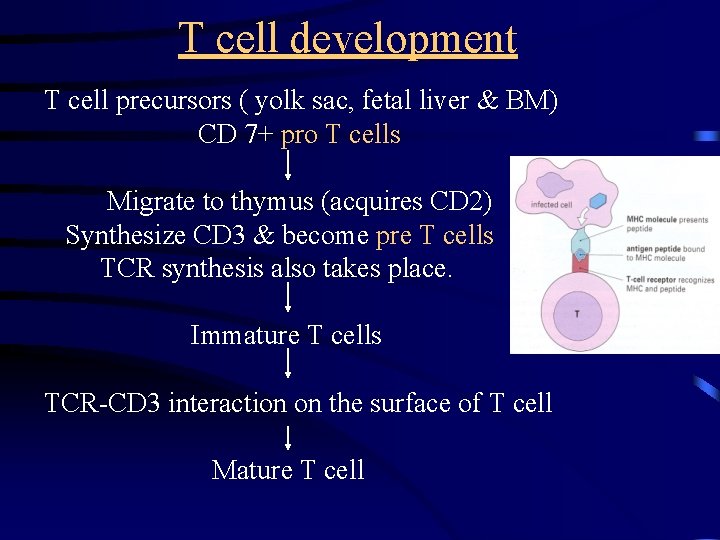
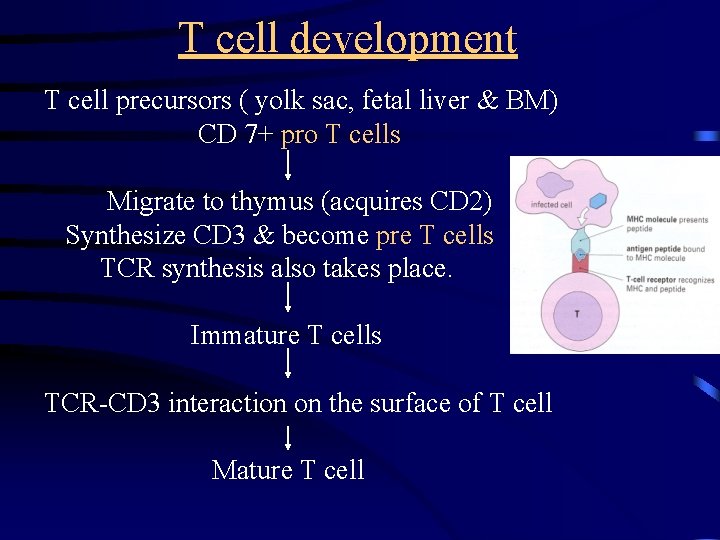
T cell development T cell precursors ( yolk sac, fetal liver & BM) CD 7+ pro T cells Migrate to thymus (acquires CD 2) Synthesize CD 3 & become pre T cells TCR synthesis also takes place. Immature T cells TCR-CD 3 interaction on the surface of T cell Mature T cell
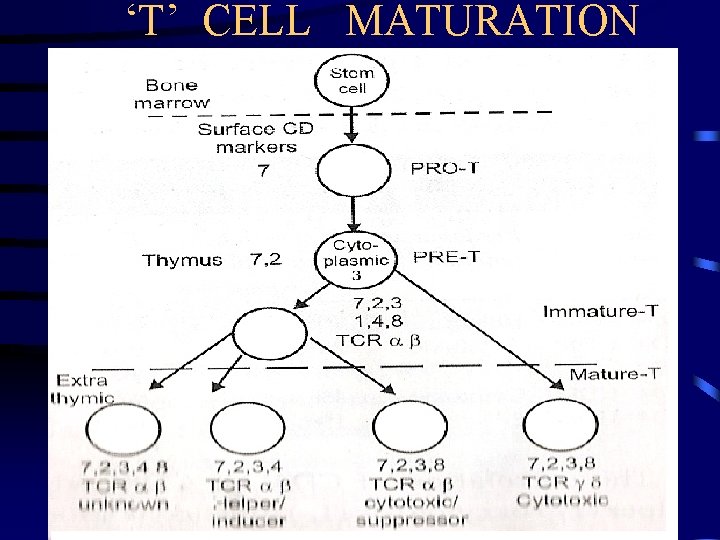
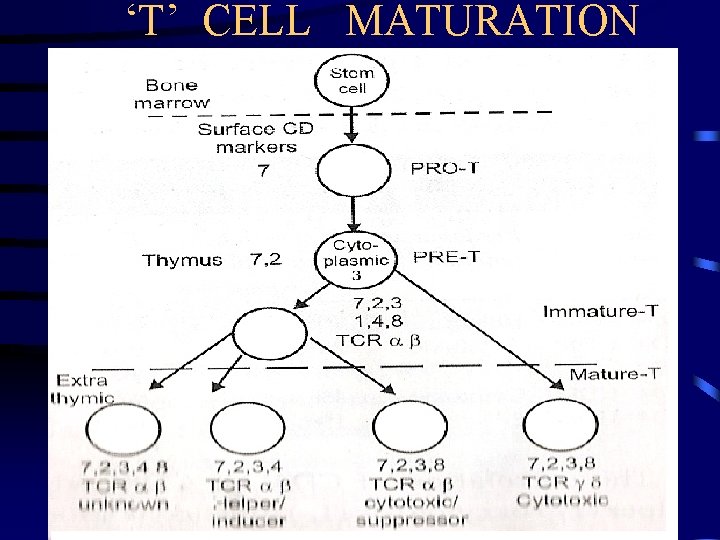
‘T’ CELL MATURATION
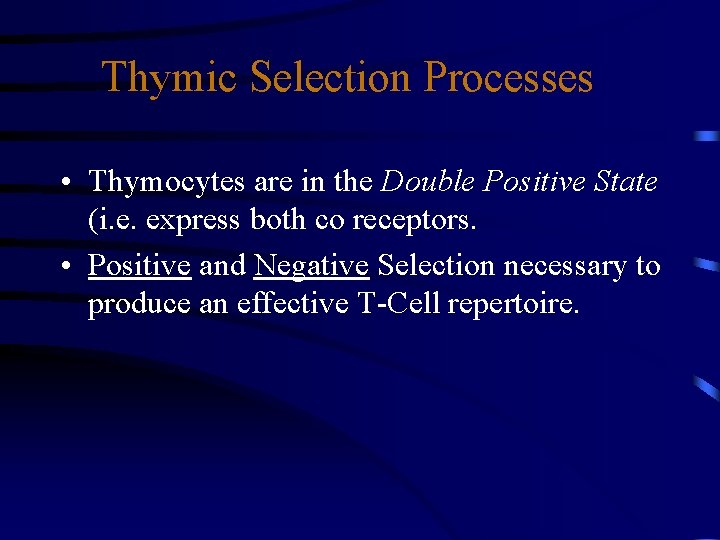
Thymic Selection Processes • Thymocytes are in the Double Positive State (i. e. express both co receptors. • Positive and Negative Selection necessary to produce an effective T-Cell repertoire.
• MHC Restriction - T cells responds to processed Ags on APC ONLY when they are presented along with the SELF- MHC Ag
Positive Selection • Results in MHC restriction • Mechanism: – Immature thymocytes cluster with MHC molecules on the cortical cells of the thymus • If TCR interacts with MHC protective signal results that prevents apoptosis. • If TCR does not interact with MHC no protective signal and apoptosis occurs.
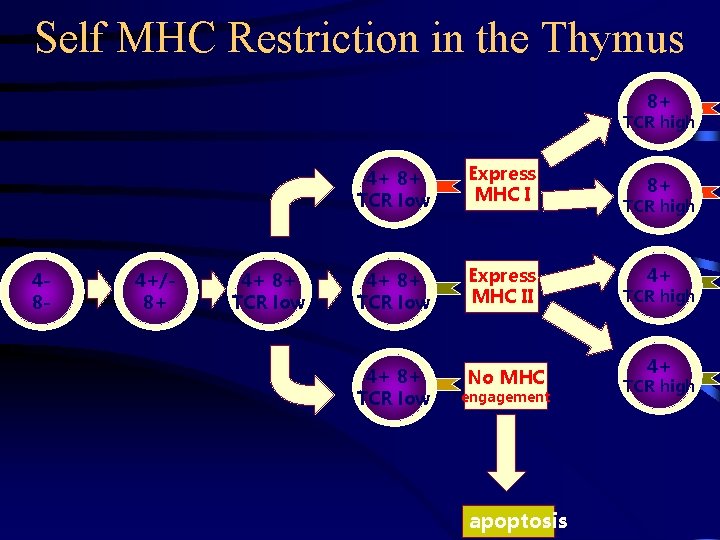
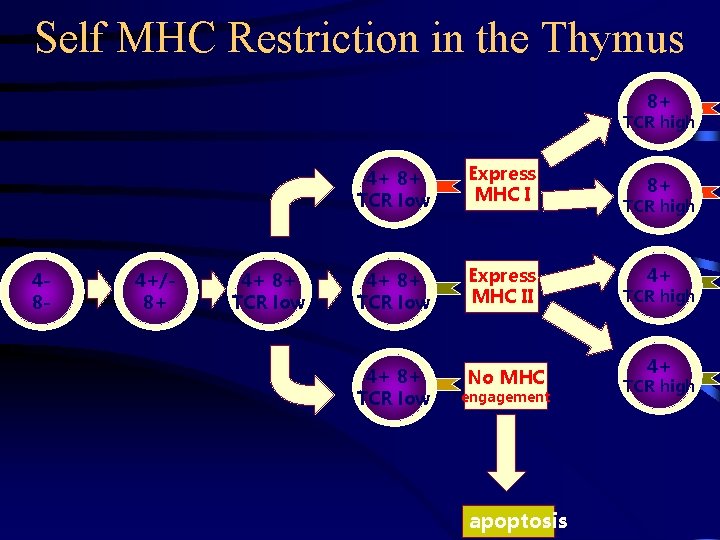
Self MHC Restriction in the Thymus 8+ TCR high 48 - 4+/8+ 4+ 8+ TCR low Express MHC II 4+ 8+ TCR low No MHC engagement apoptosis 8+ TCR high 4+ TCR high
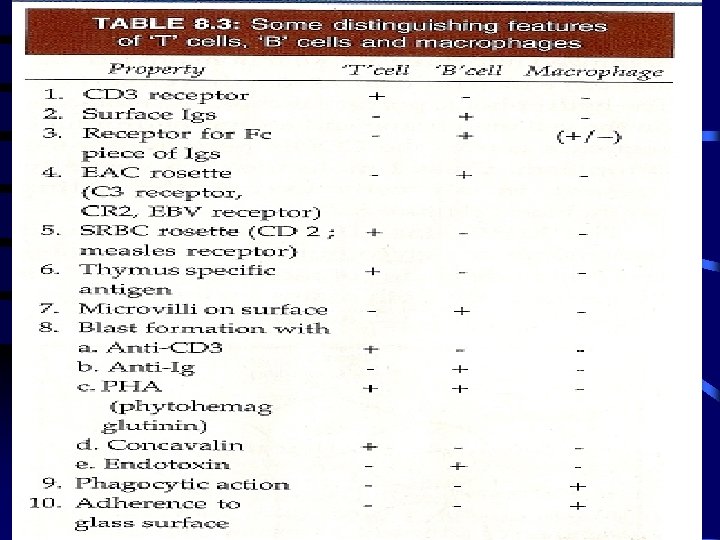
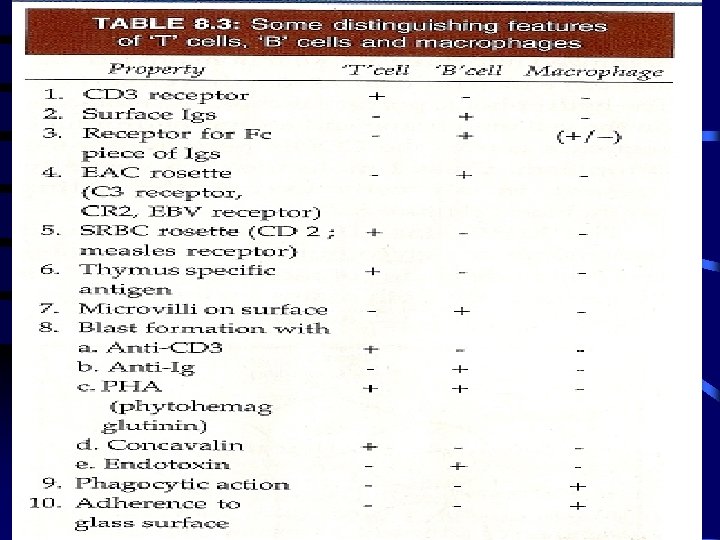
T cells • CD 2+CD 3 class of T cells in turn made up of distinct subpopulations called T cell subsets. • 2 most imp subsets are distinguished by the surface proteins CD 4 & CD 8. • A mature, functional T lymphocyte express only one of the 2 proteins & are designated as CD 4+CD 8 - or CD 4 -CD 8+. • CD 4+ Helper T cells: TH • CD 8+ Cyotoxic T cells: TC
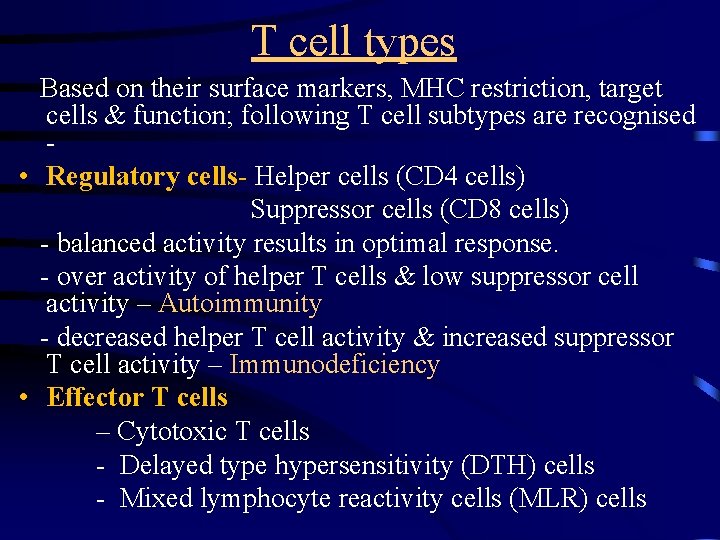
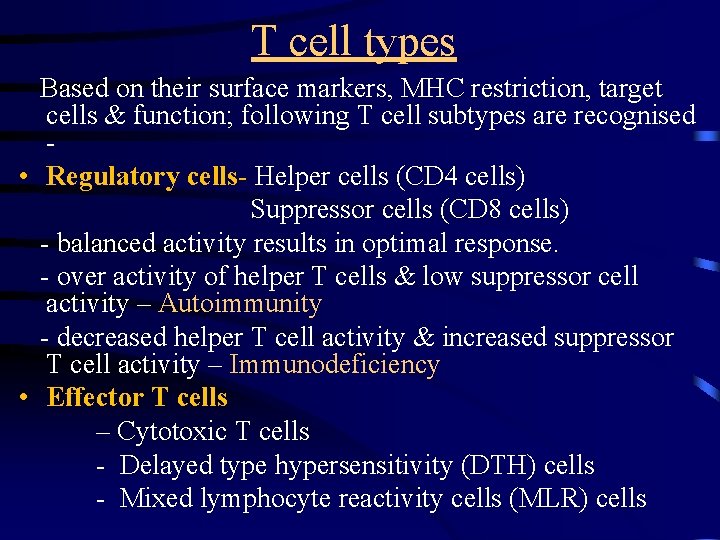
T cell types Based on their surface markers, MHC restriction, target cells & function; following T cell subtypes are recognised • Regulatory cells- Helper cells (CD 4 cells) Suppressor cells (CD 8 cells) - balanced activity results in optimal response. - over activity of helper T cells & low suppressor cell activity – Autoimmunity - decreased helper T cell activity & increased suppressor T cell activity – Immunodeficiency • Effector T cells – Cytotoxic T cells - Delayed type hypersensitivity (DTH) cells - Mixed lymphocyte reactivity cells (MLR) cells
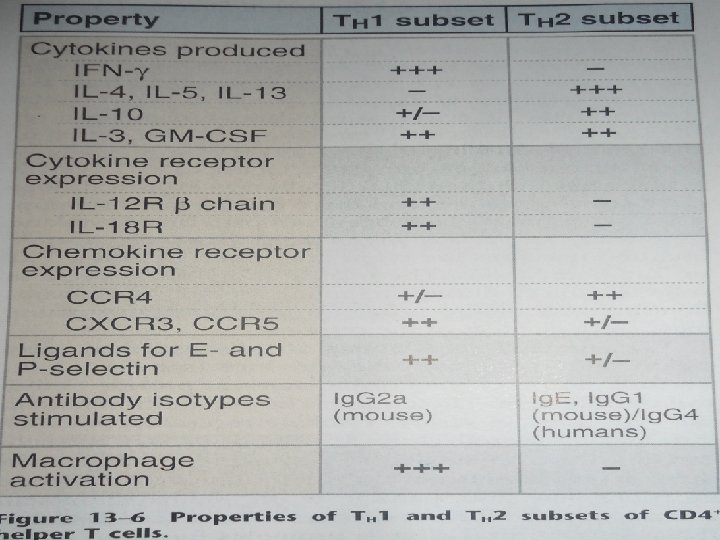
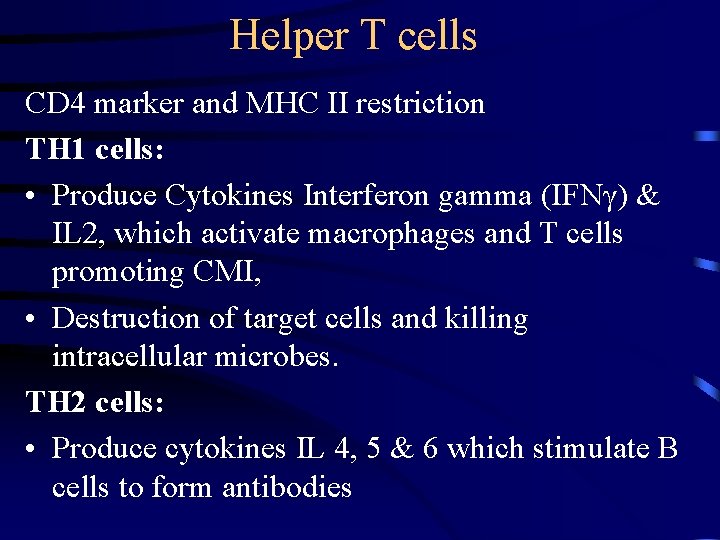
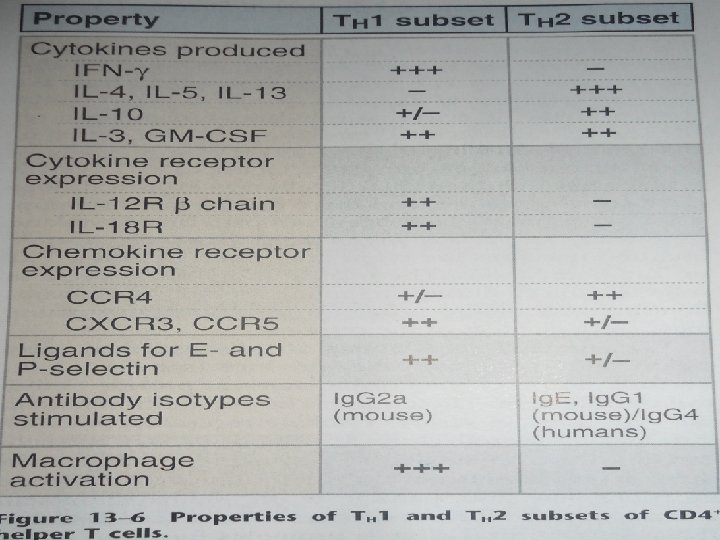
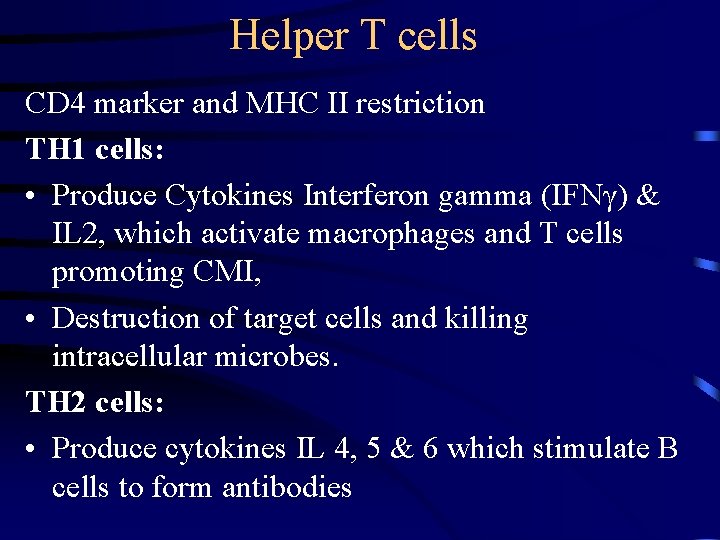
Helper T cells CD 4 marker and MHC II restriction TH 1 cells: • Produce Cytokines Interferon gamma (IFNγ) & IL 2, which activate macrophages and T cells promoting CMI, • Destruction of target cells and killing intracellular microbes. TH 2 cells: • Produce cytokines IL 4, 5 & 6 which stimulate B cells to form antibodies
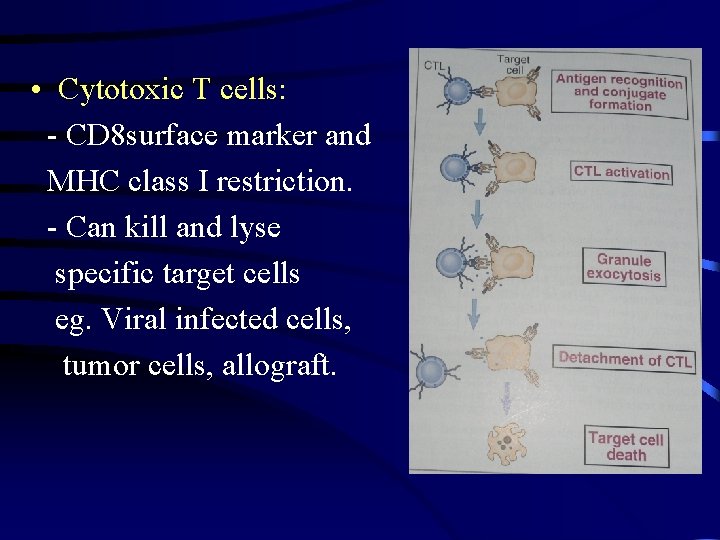
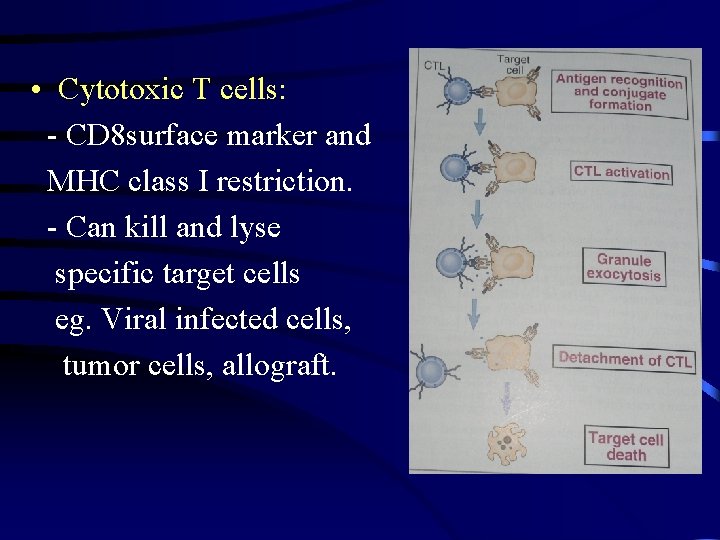
• Cytotoxic T cells: - CD 8 surface marker and MHC class I restriction. - Can kill and lyse specific target cells eg. Viral infected cells, tumor cells, allograft.
T supressor cells (Ts): CD 8 marker • block immune response by their action on Thelper or B-cells DTH cells: -Type of Th 1 cells - secretes different lymphokines (γ-interferon) - Responsible for Type IV hypersensitivity
Null cells • • Also called large granular lymhocytes (LGL) Double the size of small lymphocytes Indented nuclei & abundant cytoplasm Several azurophilic granules composed of mitochondria, ER, GA & ribosomes • Three types - Natural Killer cells (NK cells) - Ag dependent Cytotoxic cells (ADCC) - Lymphokines activated killer (LAK) cells
Natural killer cells • Cytotoxicity towards various target cells mainly tumor & virus infected • Cytotoxicity not Ab dependent or MHC restricted • Normally active in SCID • Their activity is augmented by interferon • Important in immune surveillance & natural defence against virus infected & malignant mutant cell
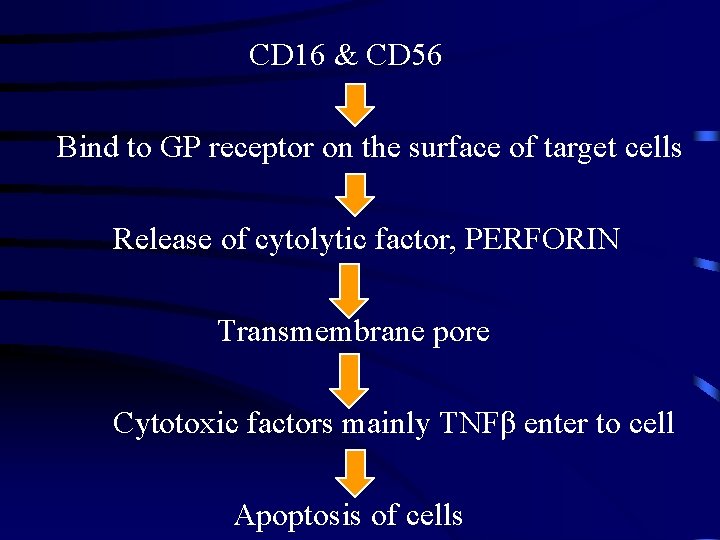
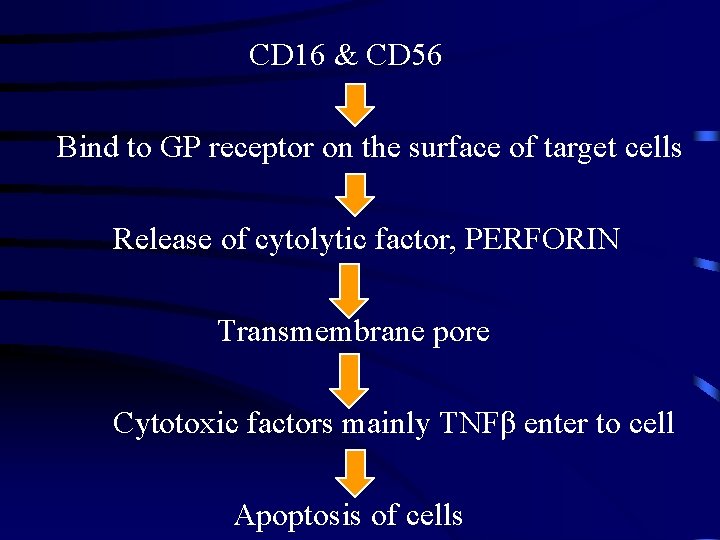
CD 16 & CD 56 Bind to GP receptor on the surface of target cells Release of cytolytic factor, PERFORIN Transmembrane pore Cytotoxic factors mainly TNFβ enter to cell Apoptosis of cells
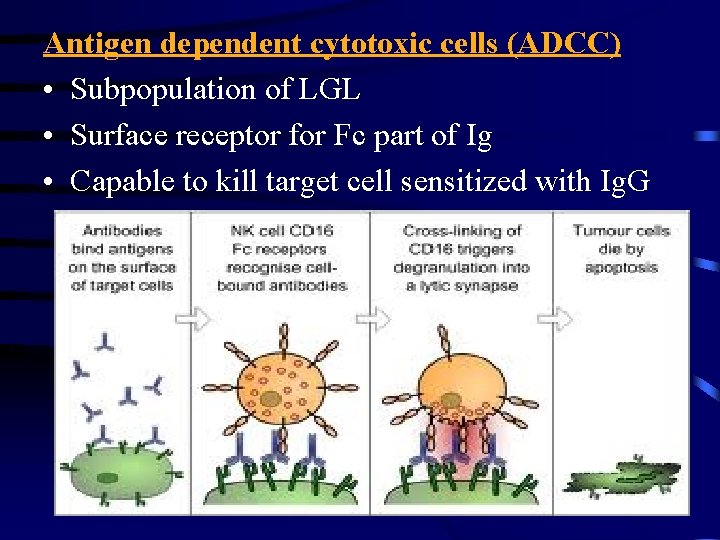
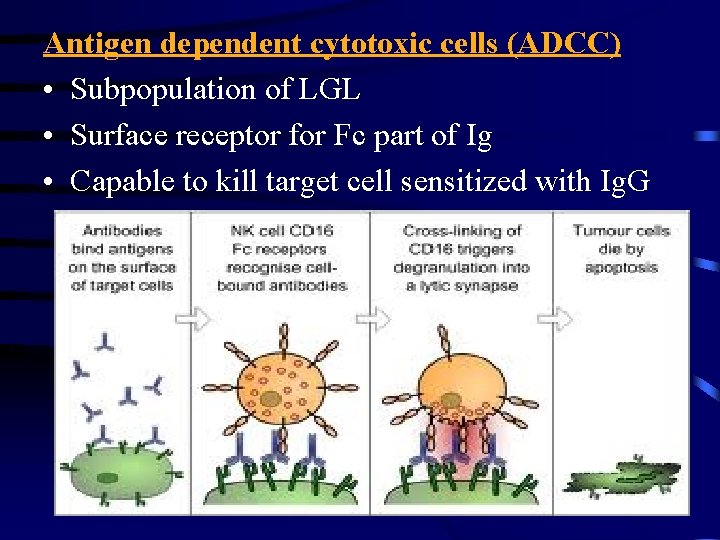
Antigen dependent cytotoxic cells (ADCC) • Subpopulation of LGL • Surface receptor for Fc part of Ig • Capable to kill target cell sensitized with Ig. G
Lymphokine activated killer cell (LAK) • NK lymphocytes treated with IL 2 • Cytotoxic to wide range of tumor cells without affecting normal cells
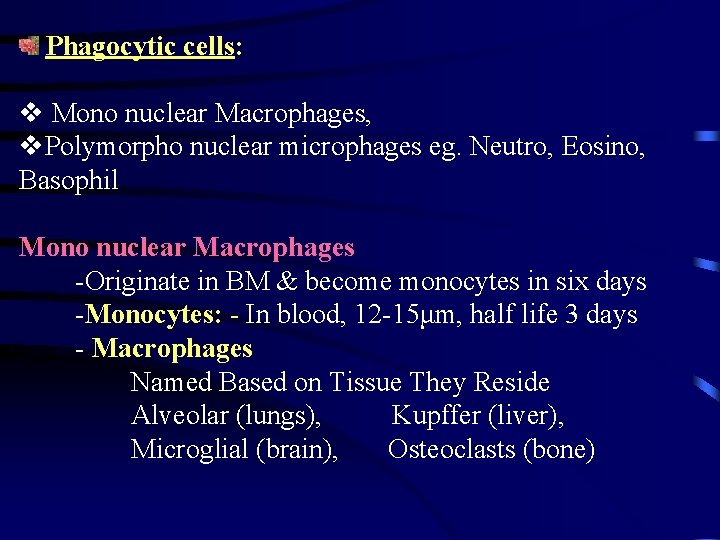
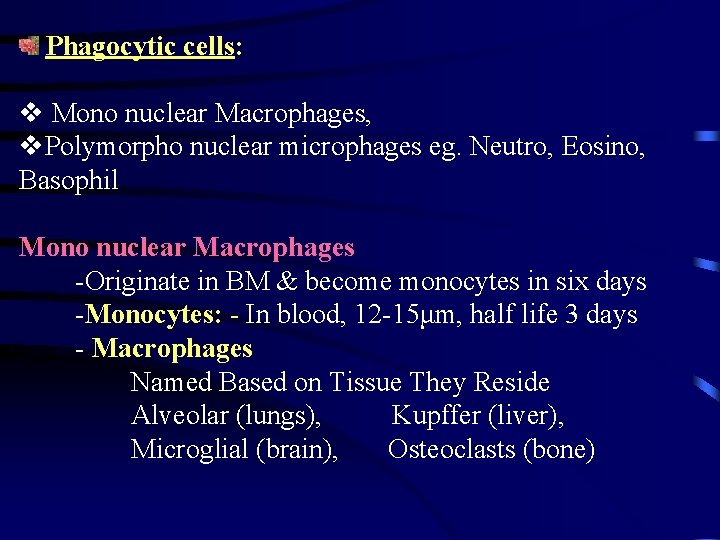
Phagocytic cells: v Mono nuclear Macrophages, v. Polymorpho nuclear microphages eg. Neutro, Eosino, Basophil Mono nuclear Macrophages -Originate in BM & become monocytes in six days -Monocytes: - In blood, 12 -15μm, half life 3 days - Macrophages Named Based on Tissue They Reside Alveolar (lungs), Kupffer (liver), Microglial (brain), Osteoclasts (bone)
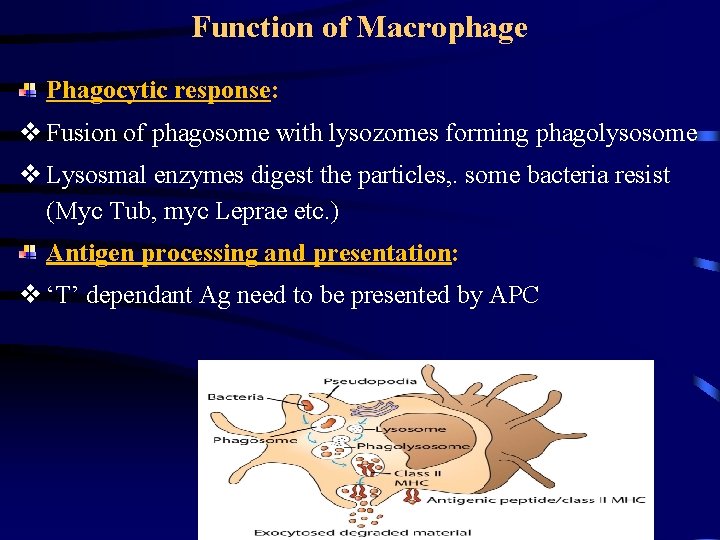
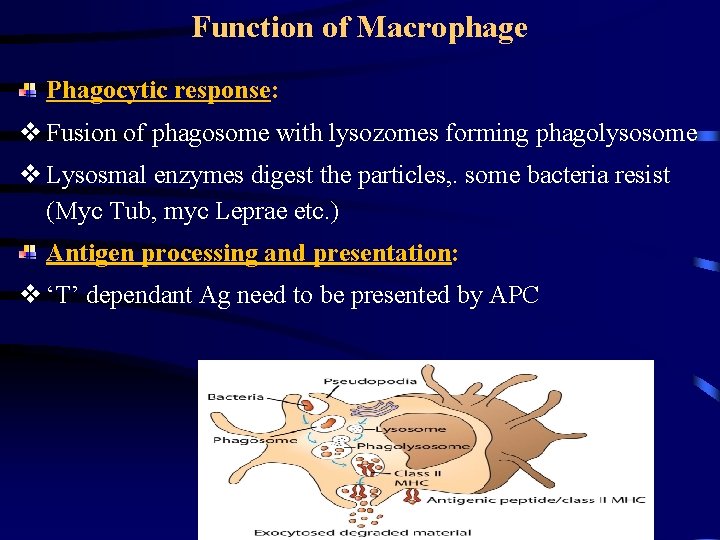
Function of Macrophage Phagocytic response: v Fusion of phagosome with lysozomes forming phagolysosome v Lysosmal enzymes digest the particles, . some bacteria resist (Myc Tub, myc Leprae etc. ) Antigen processing and presentation: v ‘T’ dependant Ag need to be presented by APC
Function of Macrophage (Contd. ) v Cleaved particles along with MHC Mol. (MHC I and II) attract ‘T’ cells with complementary receptor (MHC restricted) Cytokine Production: v Secrete a number of biologically active substances (IL-1, IL-6, CSF hydrolytic enzymes etc. ). Initiates inflammation (Pyrogen, prostaglandin, compliment, and clotting factors) Tissue repair (enzymes and growth factor)
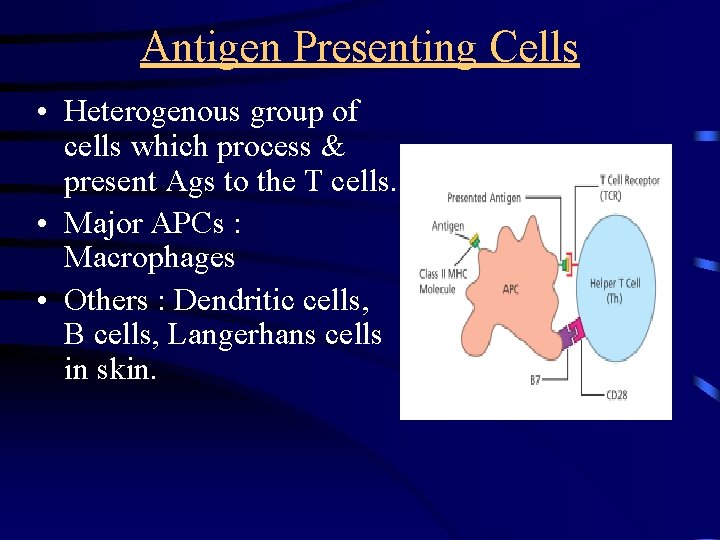
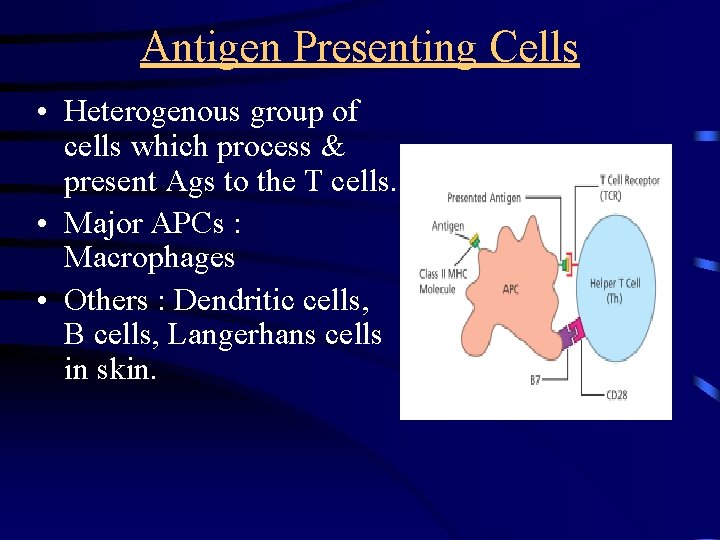
Antigen Presenting Cells • Heterogenous group of cells which process & present Ags to the T cells. • Major APCs : Macrophages • Others : Dendritic cells, B cells, Langerhans cells in skin.
MAJOR HISTOCOMPATIBILITY COMPLEX • Its discovery was based on transplantation experiments • First work done by GORER in 1930 on the Ag responsible for allograft rejection in inbreed mice • Snell, Dausset and Benacerraf was awarded the Nobel Prize for their work on MHC and the genetic control of immune system
• This is cell surface Ag that evoke immune response to an incompatible host resulting in allograft rejection • The H 2 Ag system are found to be the major histocompatibility Ag for mice • This Ag is coded for by a closely linked multiallelic cluster of genes called MHC
• These alloantigens are present on surface of leucocyte in man are called human leucocyte Ag (HLA) and set of genes coding for them is called the HLA complex
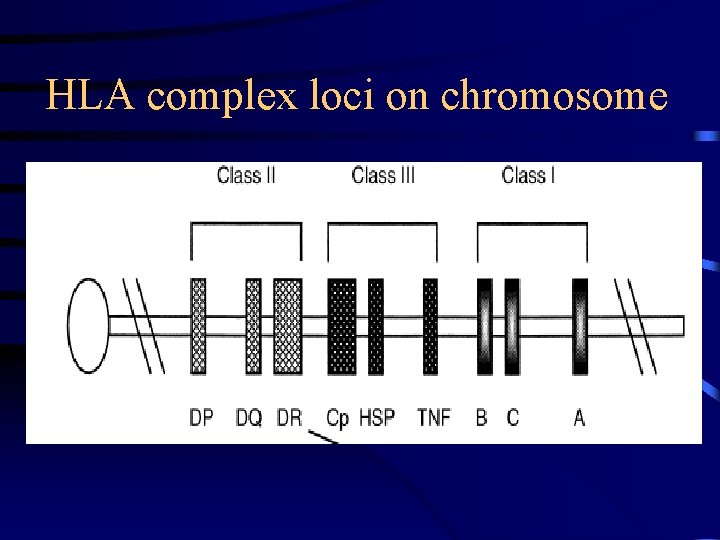
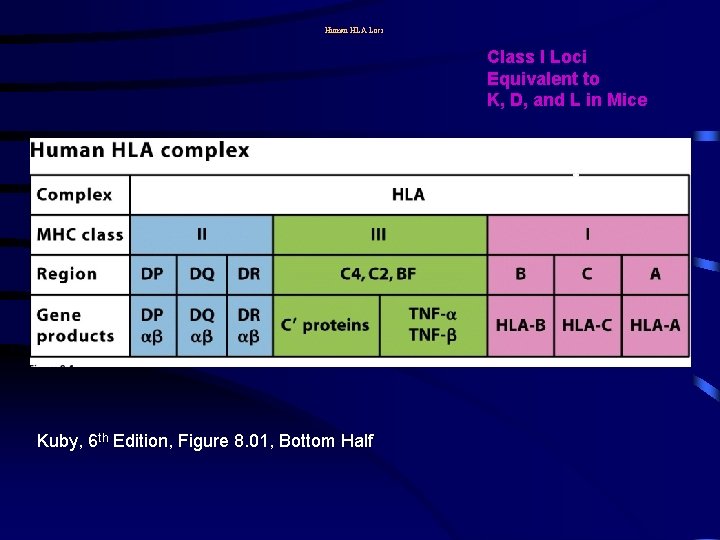
HLA COMPLEX • Gene for this complex are located on chromosome 6 • Pleomorphic • HLA loci are multiallelic • It consists of three separate cluster of gene - Class I: A, B & C loci - Class II: DR, DQ, & DP loci - Class III: Genes for C 2, C 4, Properdin factor B, Heat shock proteins & TNF α and β
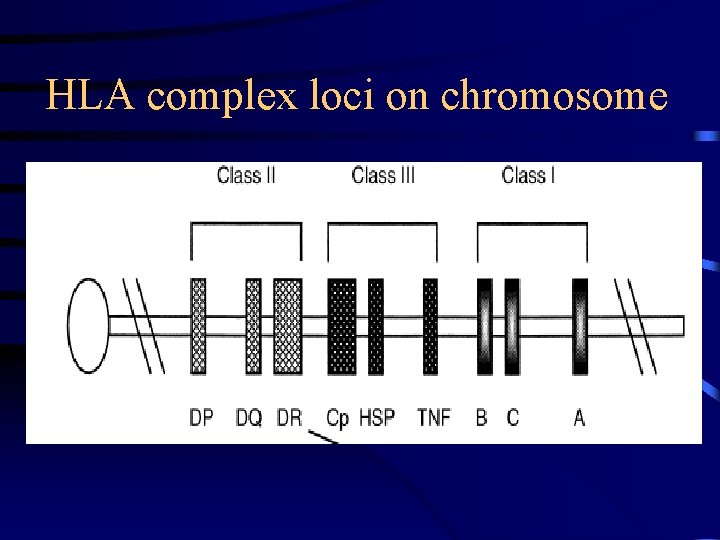
HLA complex loci on chromosome
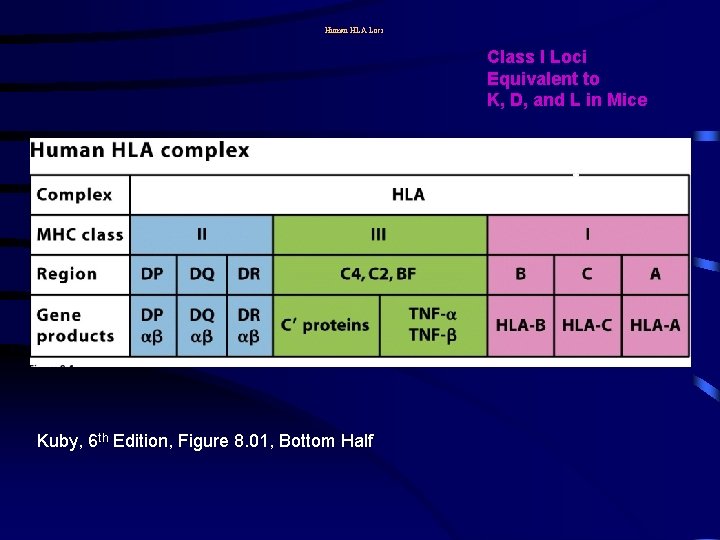
Human HLA Loci Class I Loci Equivalent to K, D, and L in Mice Kuby, 6 th Edition, Figure 8. 01, Bottom Half
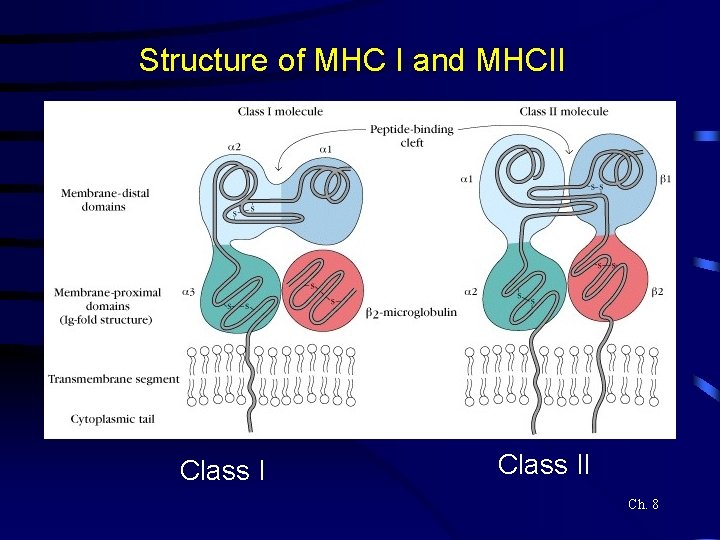
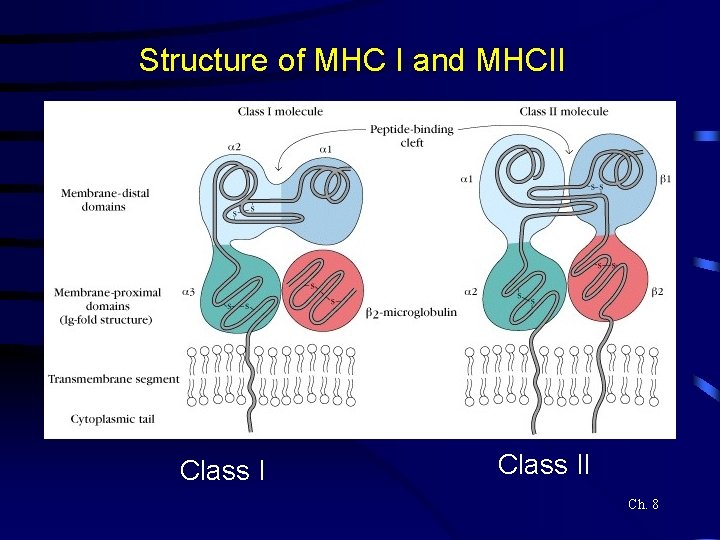
Structure of MHC I and MHCII Class II Ch. 8
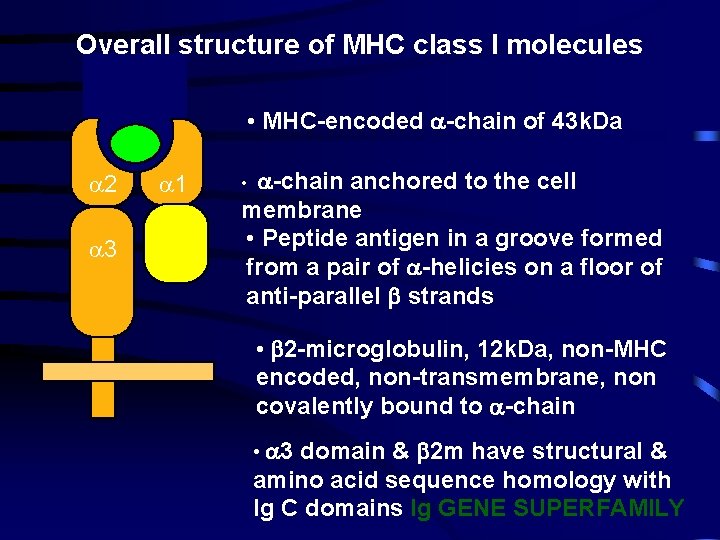
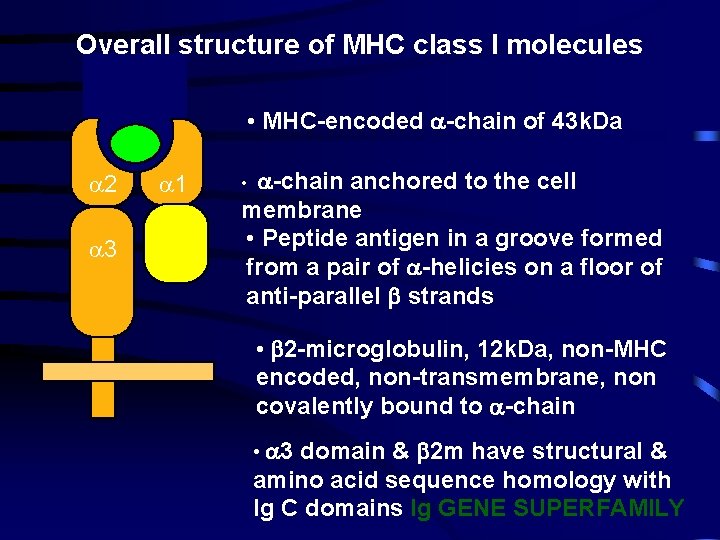
Overall structure of MHC class I molecules • MHC-encoded -chain of 43 k. Da 2 1 3 2 m -chain anchored to the cell membrane • Peptide antigen in a groove formed from a pair of -helicies on a floor of anti-parallel strands • • 2 -microglobulin, 12 k. Da, non-MHC encoded, non-transmembrane, non covalently bound to -chain • 3 domain & 2 m have structural & amino acid sequence homology with Ig C domains Ig GENE SUPERFAMILY
MHC I: Biological function 44
• HLA class I Ag present on surface of all nucleated cell. • Ags recognisation to CD 8 cell • Principal Ags involved in graft rejection & cell mediated cytolysis • May functions as component of hormone receptor
HLA II • More restricted in distribution being found only on macrophages, dendritic cells, activated T cells & B cells • Ags recognisation to CD 4 cell • Regulate the immune response • Responsible for graft Vs host reaction & mixed leucocyte reaction
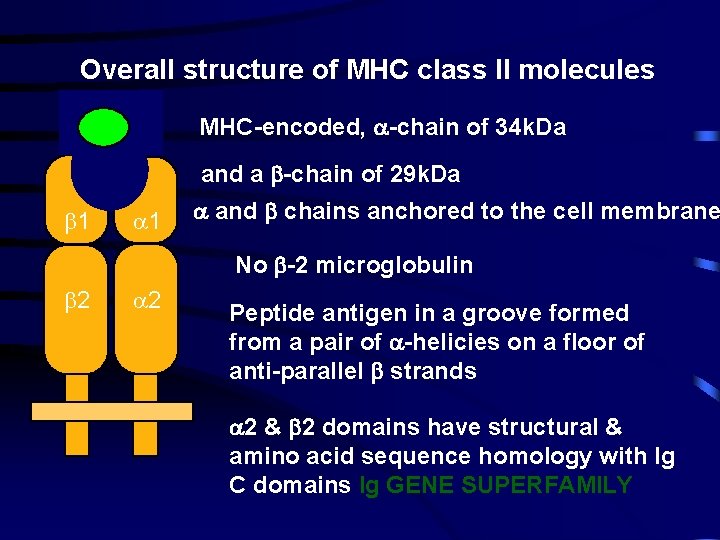
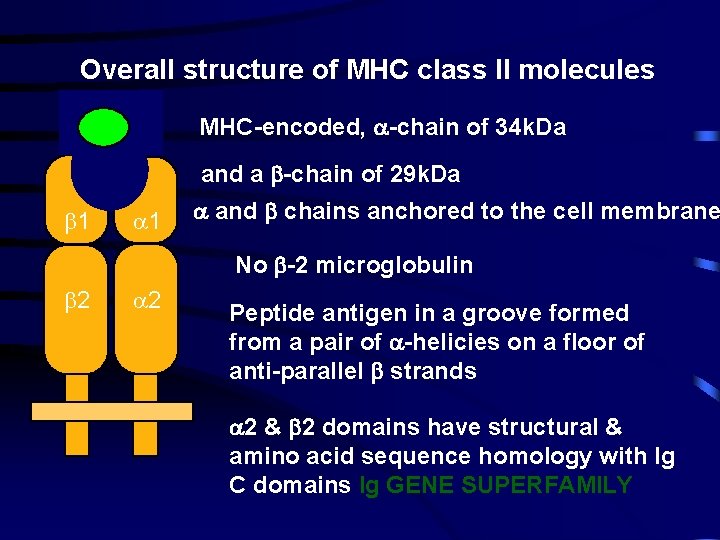
Overall structure of MHC class II molecules MHC-encoded, -chain of 34 k. Da and a -chain of 29 k. Da 1 1 and chains anchored to the cell membrane No -2 microglobulin 2 2 Peptide antigen in a groove formed from a pair of -helicies on a floor of anti-parallel strands 2 & 2 domains have structural & amino acid sequence homology with Ig C domains Ig GENE SUPERFAMILY
MHCII: Function 50
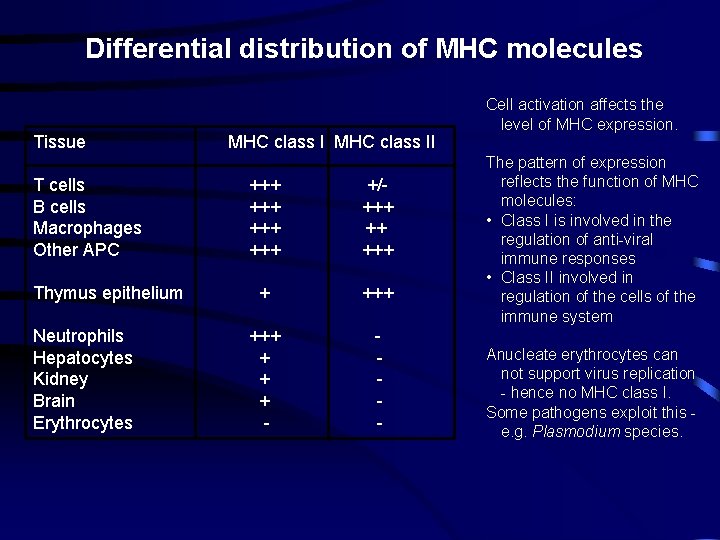
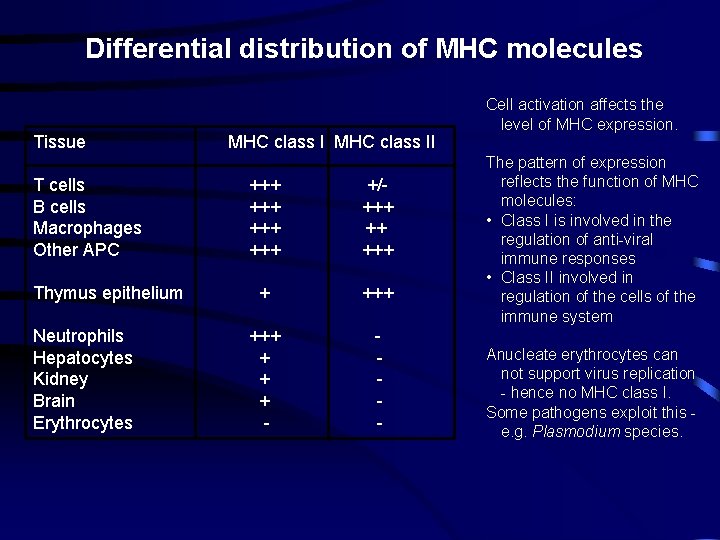
Differential distribution of MHC molecules Tissue T cells B cells Macrophages Other APC Thymus epithelium Neutrophils Hepatocytes Kidney Brain Erythrocytes MHC class II +++ +++ +/+++ ++ +++ + + + - - Cell activation affects the level of MHC expression. The pattern of expression reflects the function of MHC molecules: • Class I is involved in the regulation of anti-viral immune responses • Class II involved in regulation of the cells of the immune system Anucleate erythrocytes can not support virus replication - hence no MHC class I. Some pathogens exploit this e. g. Plasmodium species.
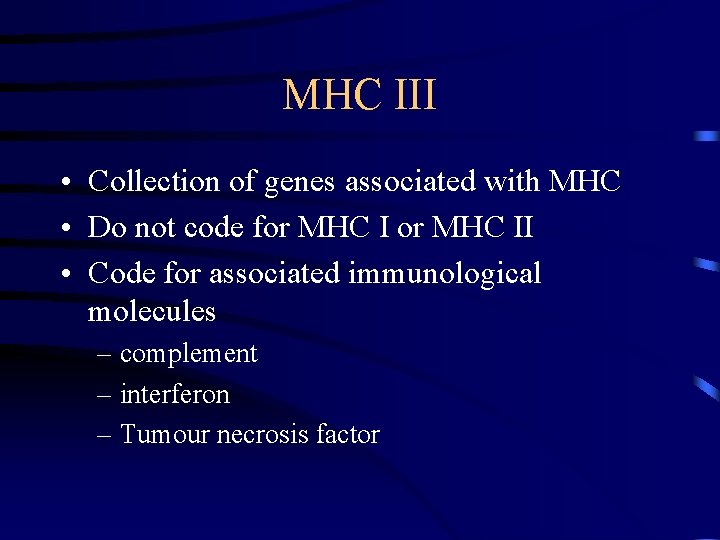
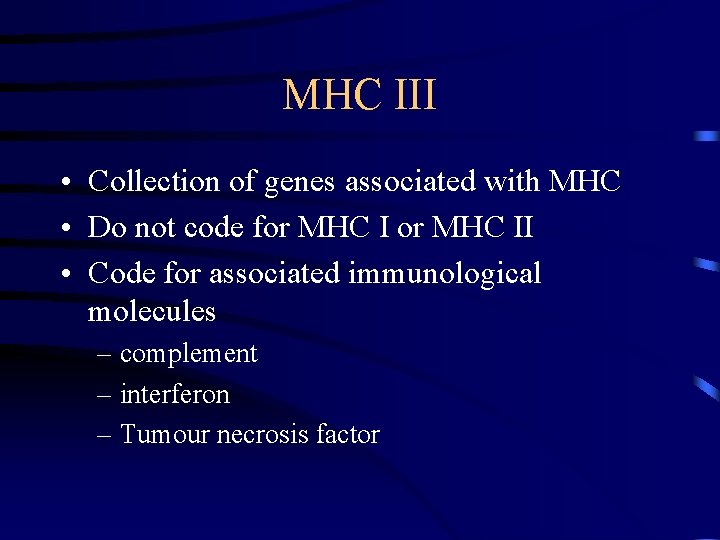
MHC III • Collection of genes associated with MHC • Do not code for MHC II • Code for associated immunological molecules – complement – interferon – Tumour necrosis factor
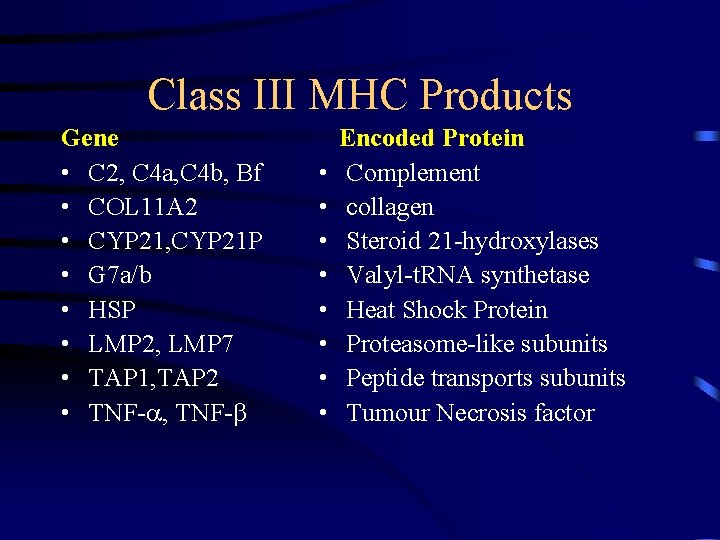
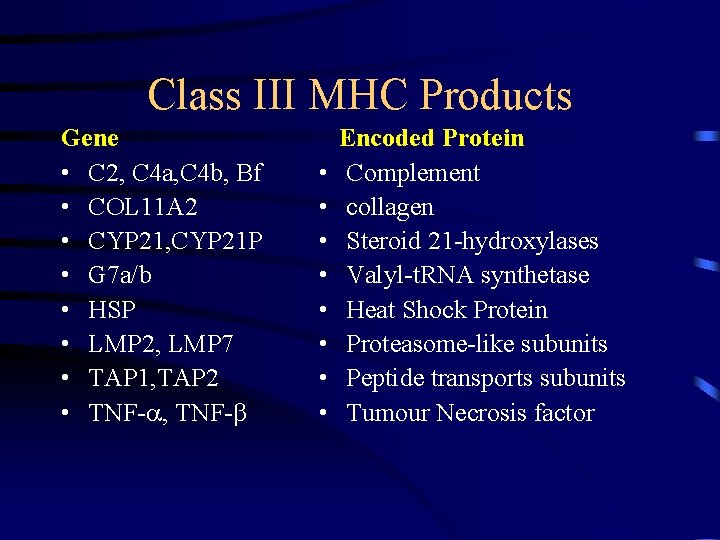
Class III MHC Products Gene • C 2, C 4 a, C 4 b, Bf • COL 11 A 2 • CYP 21, CYP 21 P • G 7 a/b • HSP • LMP 2, LMP 7 • TAP 1, TAP 2 • TNF- , TNF- • • Encoded Protein Complement collagen Steroid 21 -hydroxylases Valyl-t. RNA synthetase Heat Shock Protein Proteasome-like subunits Peptide transports subunits Tumour Necrosis factor
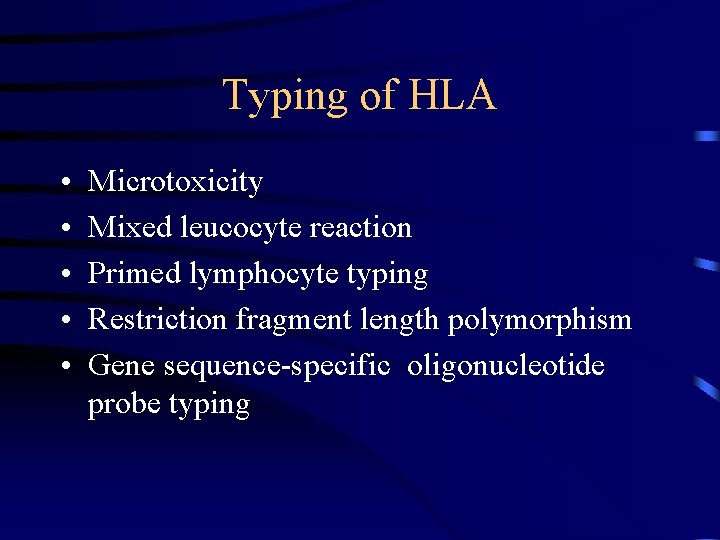
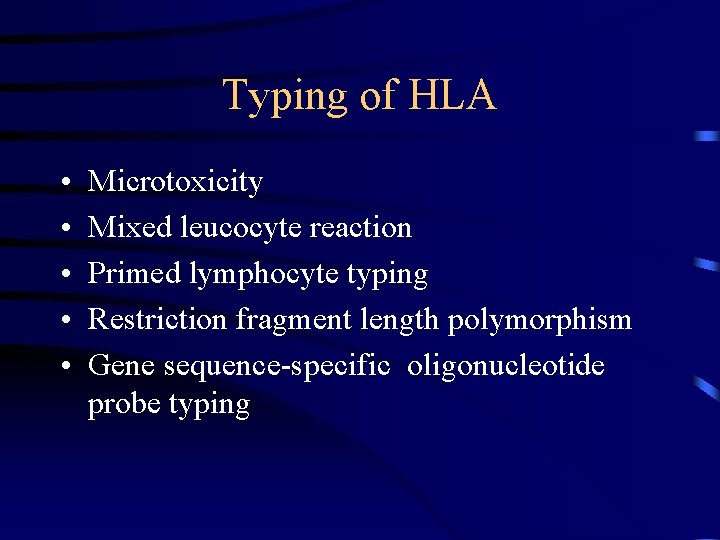
Typing of HLA • • • Microtoxicity Mixed leucocyte reaction Primed lymphocyte typing Restriction fragment length polymorphism Gene sequence-specific oligonucleotide probe typing
Application • Transplantation: used for testing compatibility between recipient and potential donor • Disputed Paternity • Anthropological studies • Genetic predisposition of disease
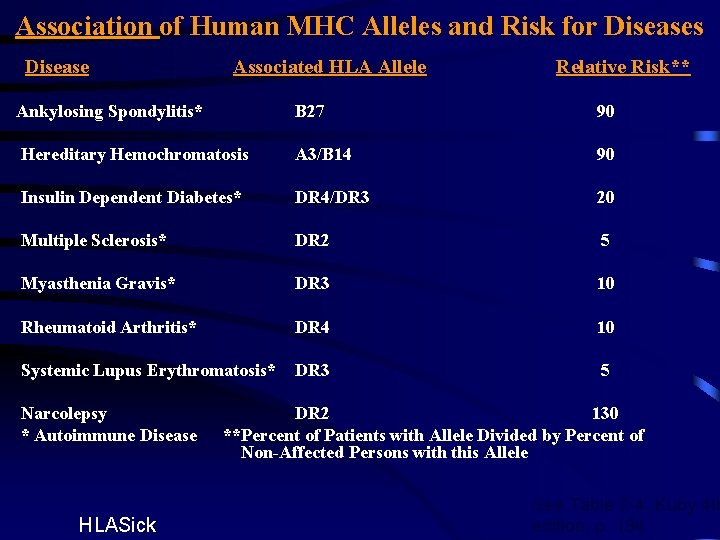
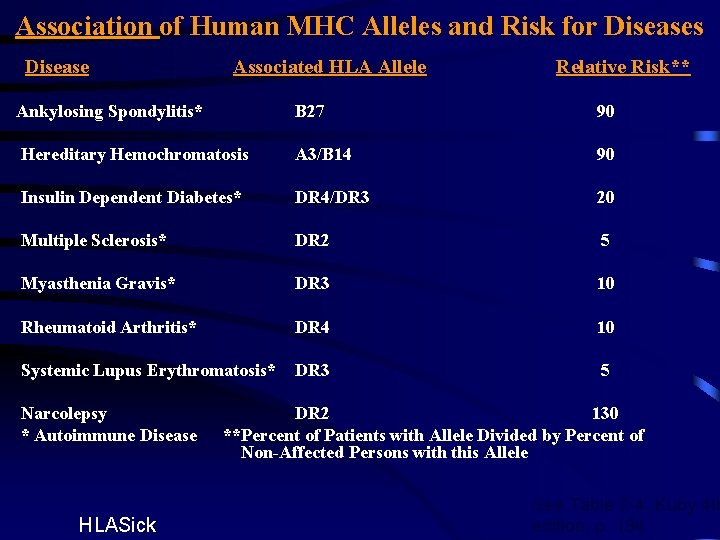
Association of Human MHC Alleles and Risk for Diseases Disease Associated HLA Allele Relative Risk** Ankylosing Spondylitis* B 27 90 Hereditary Hemochromatosis A 3/B 14 90 Insulin Dependent Diabetes* DR 4/DR 3 20 Multiple Sclerosis* DR 2 5 Myasthenia Gravis* DR 3 10 Rheumatoid Arthritis* DR 4 10 Systemic Lupus Erythromatosis* DR 3 5 Narcolepsy * Autoimmune Disease HLASick DR 2 130 **Percent of Patients with Allele Divided by Percent of Non-Affected Persons with this Allele See Table 7 -4, Kuby 4 th edition, p. 194

THANK YOU

Primary Lymphoid Organ • Major site of lymphocyte development. • In mammals, T lymphocytes mature in thymus whereas B lymphocytes mature in the liver or bone marrow. • Birds have specialised sites of B cell maturation called bursa of Fabricus.
THYMUS • By 8 th week of gestation, mesenchymal stem cells (precursors of lymphocytes) from the yolk sac, fetal liver & BM reach thymus & differentiate into thymic lymphoid cells, thymocytes. • Lymphocyte proliferation in thymus is not dependent on antigenic stimulus.
Secondary Lymphoid Organs • Lymph nodes • Spleen • Accumulation of lymphoid tissues like MALT (mucosa associated lymphoid tissue) GALT (gut associated lymphoid tissue) BALT (bronchus associated lymphoid tissue)
MALT • Contains lymphoid & phagocytic cells. • Both B & T cells present. • Secretory Ig. A is predominant.
Classification of Lymphocytes • According to the size: Small 5 -8µ Medium 8 -12µ Large 12 -15µ small lymphocytes are the most numerous. • Depending on the life span: Short lived – 2 wks - effector cells Long lived – 3 yrs or more or for life - immunological memory
Lymphopoiesis • Takes place in primary lymphoid organs • Enters circulation, peripheral lymphoid organs & tissues. • Constant movement of lymphocytes through the blood, lymphatic organs & tissues is called lymphocyte recirculation. • Ensures initiation of appropriate immune response at any site of entry of an Ag. • One cycle of recirculation is completed in 1 -2 days. Mainly consists of T cells.
The Immune System u Widely dispersed system u Review of structure and function ¶ bone marrow F located in marrow cavities of bones F yellow vs. red marrow F hematopoiesis
The Immune System u Review of structure and function · thymus gland F location F consists of lymphocytes and macrophages F “gives” immunocompetence to T lymphocytes via thymosins
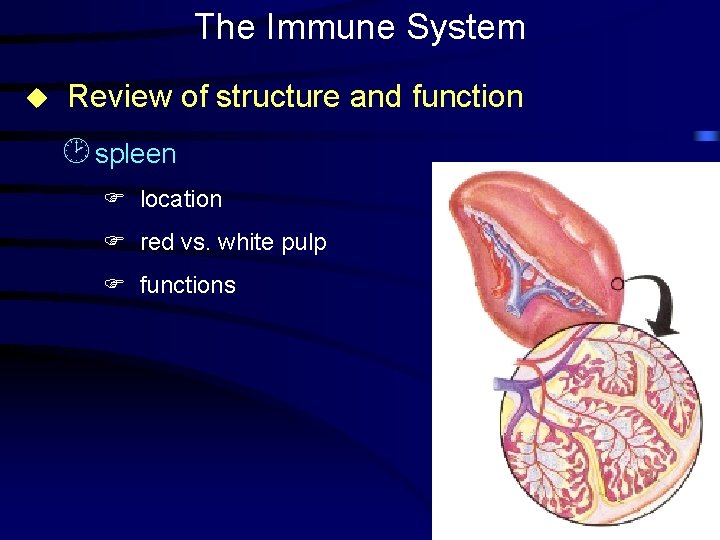
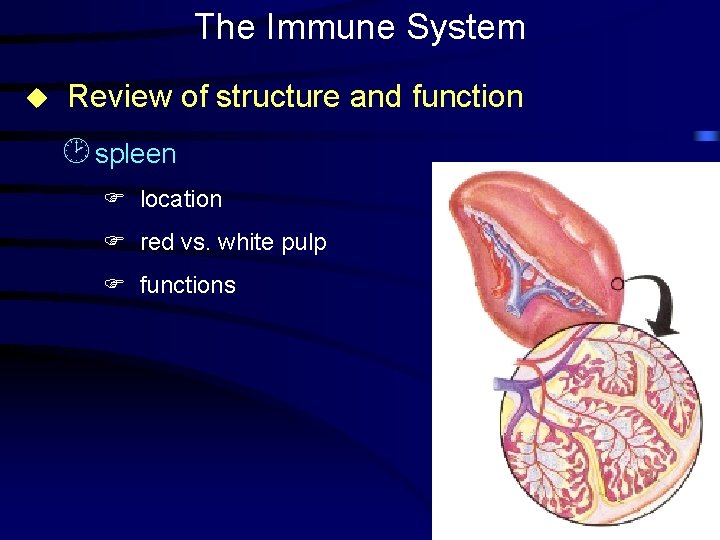
The Immune System u Review of structure and function ¸ spleen F location F red vs. white pulp F functions
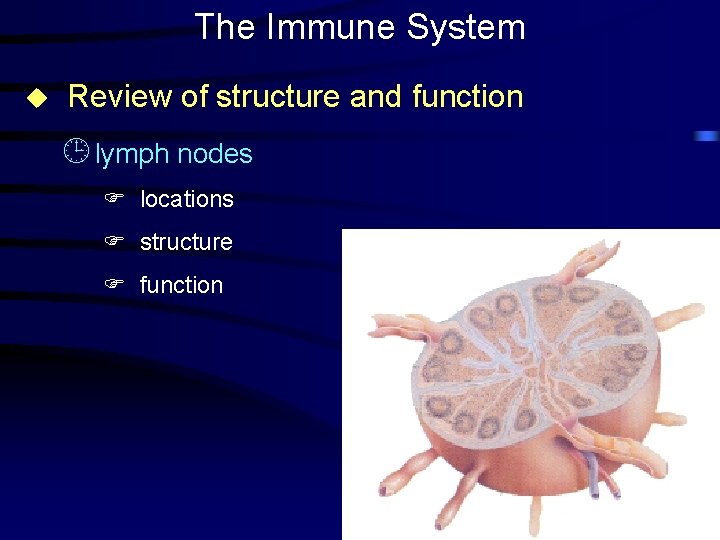
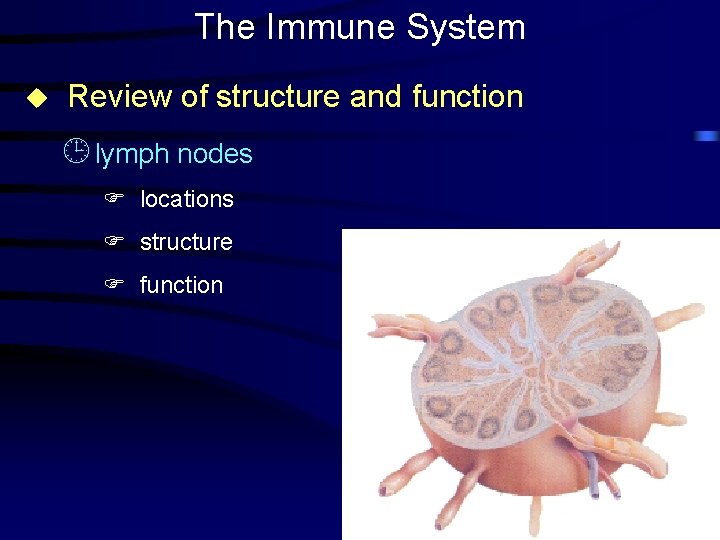
The Immune System u Review of structure and function ¹ lymph nodes F locations F structure F function
The Immune System u Review of structure and function º tonsils F locations F functions
The Immune System u Review of structure and function » lymphocytes and plasma cells F What is immunity? F origin and immunocompetence F T cells (cancer cells, transplants, bacteria, virus-laden cells) äcytotoxic T cells ä suppressor T cells ä helper T cells ä memory T cells F B cells (viruses, bacteria) äplasma cells ä memory B cells
The Immune System u Review of structure and function » lymphocytes and plasma cells F locations F primary immune response F secondary (anamnestic) response
Age-related changes in the immune system All lymphoid tissues decreases in mass and efficiency with age u u Bone marrow u Thymus gland ¶ puberty to 50, lose 90% of mass · loss of size = loss of thymosins ¸ new T cell immunocompetence decreases
Age-related changes in the immune system u B cells ¶ no decline with age · decreased responsiveness to antigens ¸ by 70, 85% reduction in antibody production ¸ B cell changes may be result of decreased helper T cell numbers
Age-related changes in the immune system u Spleen u Lymph nodes u Tonsils ¶ reach maximum size at 12 · palatine tonsils decrease gradually; pharyngeal tonsil (adenoid) atrophies completely ¸ unclear about functional losses
Age-related dysfunctions in the immune system u General decrease in immune responses ¶ decreased immune sensitivity · increased autoimmunity ¸ causes F decrease in precursor cells F decreased differentiation into T- and B-cells F increased suppressor T-cells F increased factors that inhibit immunity (? )
Age-related dysfunctions in the immune system u Age-associated T-lymphocyte defects ¶ T-cell numbers decrease with age · diseases normally held in check by T-cells are allowed to appear ¸ immunosuppressive treatment has same effect
Age-related dysfunctions in the immune system u Acquired immune deficiency syndrome ¶ HIV infects helper T-cells (CD 4 cells), ultimately killing them · alters ratio between helper T-cells and suppressor T-cells ¸ normal ratio is 2: 1 ¹ at ratio of 1: 1 AIDS symptoms begin to appear º at ratio of 0. 5: 1, full-blown disease u Lymphomas
Take home messages about immunity u decreased lymphoid tissue body-wide u general decline in immunity u decreased T cell number u decreased B cell activity increased incidences of autoimmune responses u