Structure and Function of Urinary System Urinary system
- Slides: 60
Structure and Function of Urinary System § Urinary system: § § Two kidneys Two ureters One urinary bladder One urethra § Infection prevented by: § Valves prevent backflow to kidneys § Acidity of urine § Mechanical flushing
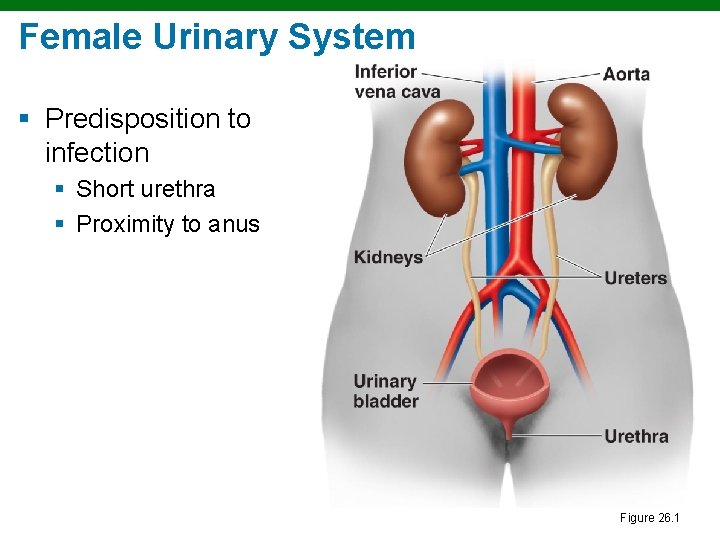
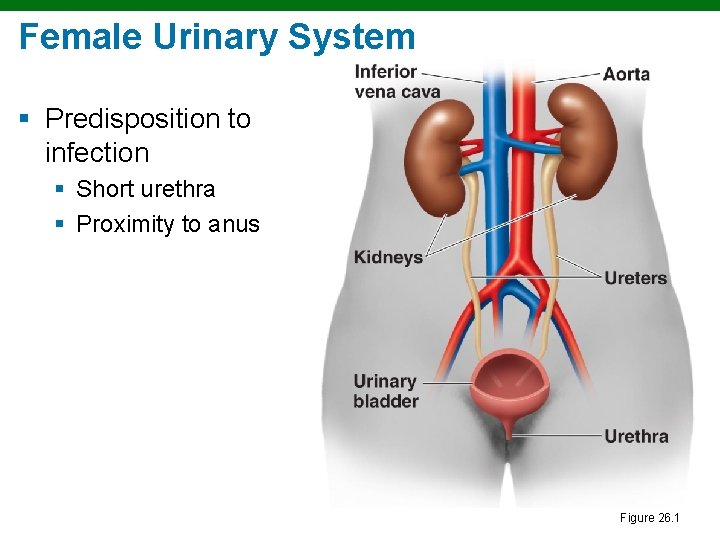
Female Urinary System § Predisposition to infection § Short urethra § Proximity to anus Figure 26. 1
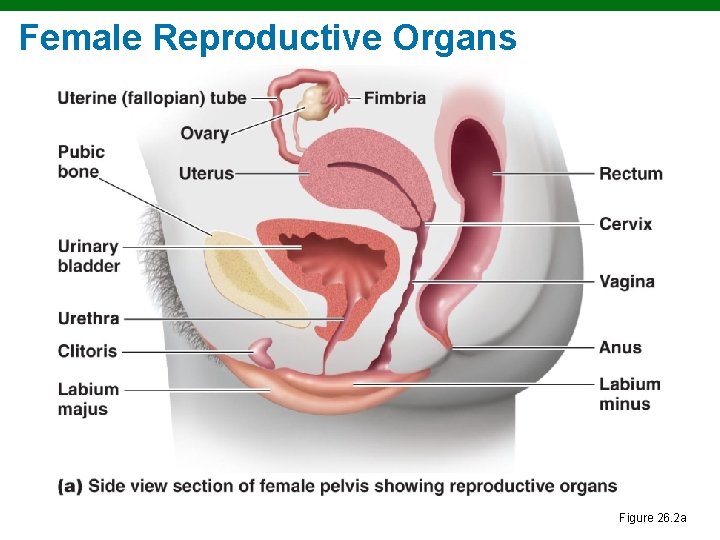
The Female Reproductive System § Female: § § Two ovaries Two uterine (fallopian) tubes The uterus, including the cervix; the vagina External genitals
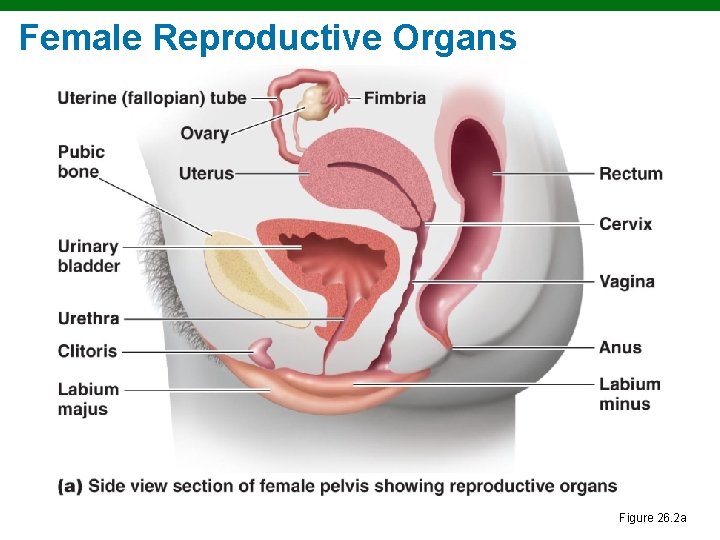
Female Reproductive Organs Figure 26. 2 a
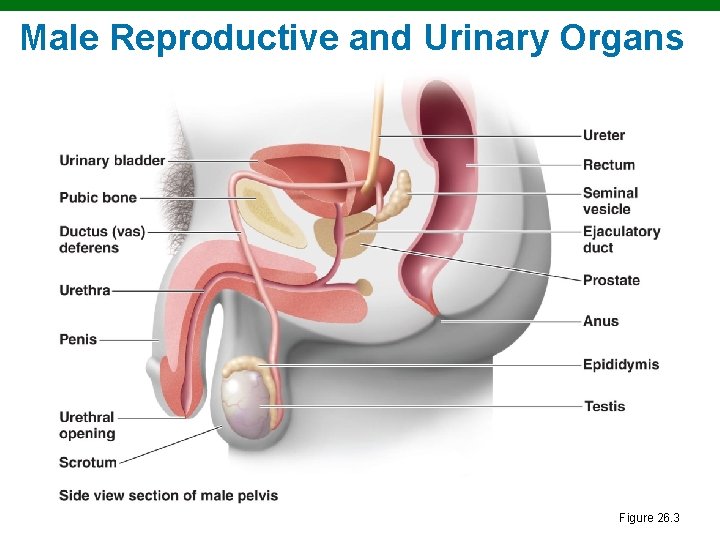
The Male Reproductive System § Male: § § § § Two testes Accessory glands Penis Epididymis Ductus (vas) deferens Ejaculatory duct Urethra
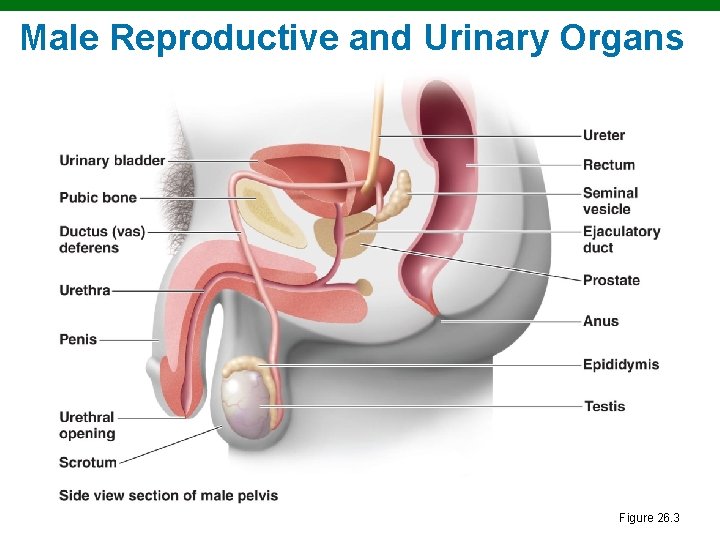
Male Reproductive and Urinary Organs Figure 26. 3
Normal Microbiota § Urinary bladder and upper urinary tract are sterile § Lactobacilli are predominant in the vagina § Produce H 2 O 2 § Grow on glycogen secretions § Infection is indicated by: § >10, 000 bacteria/ml § 100 coliforms/ml § Positive urine leukocyte esterase (LE) test
Urinary System Infections § Cystitis § An inflammation of the urinary bladder § Urethritis § An inflammation of the urethra § Pyelonephritis § An inflammation of one or both kidneys
Cystitis § Usual causative agents: § E. coli § S. saprophyticus § Symptoms: § Dysuria (difficult or painful urination) § Pyuria (pus in urine) § Diagnosis: >100 CFU/ml potential pathogens and + LE test § Treatment: Trimethoprim-sulfamethexazole
Pyelonephritis § § Causative agent: Usually E. coli Symptoms: Fever; back or flank pain Diagnosis: 104 CFUs/ml and + LE test Treatment: Cephalosporin
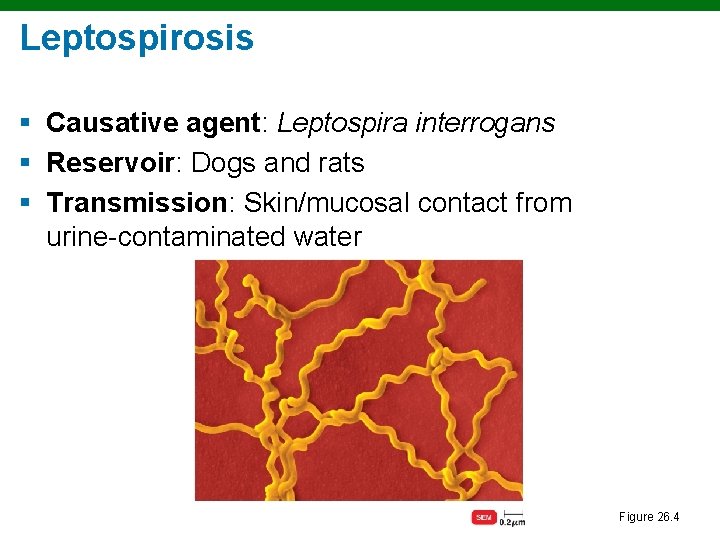
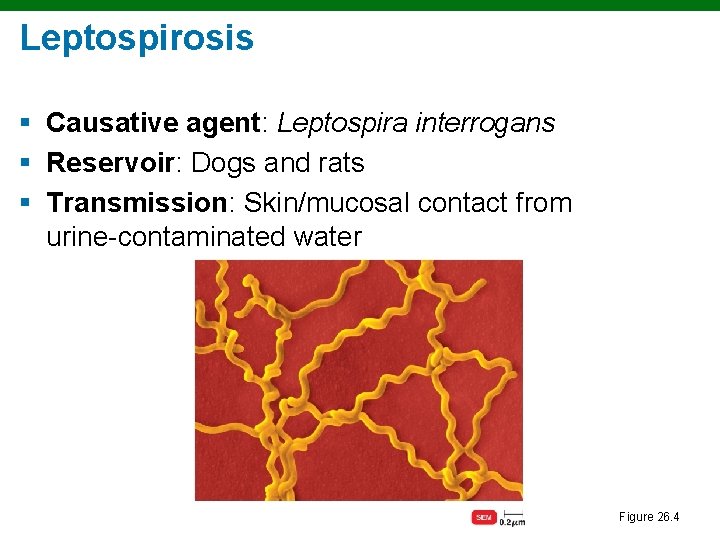
Leptospirosis § Causative agent: Leptospira interrogans § Reservoir: Dogs and rats § Transmission: Skin/mucosal contact from urine-contaminated water Figure 26. 4
Leptospirosis § Symptoms: Headaches, muscular aches, fever, kidney failure a possible complication § Diagnosis: Serological test § Treatment: Doxycycline
Sexually Transmitted Infections (STIs) § Prevented by condoms § Bacterial infections are treated with antibiotics
Sexually Transmitted Disease Surveillance 2010 Division of STD Prevention
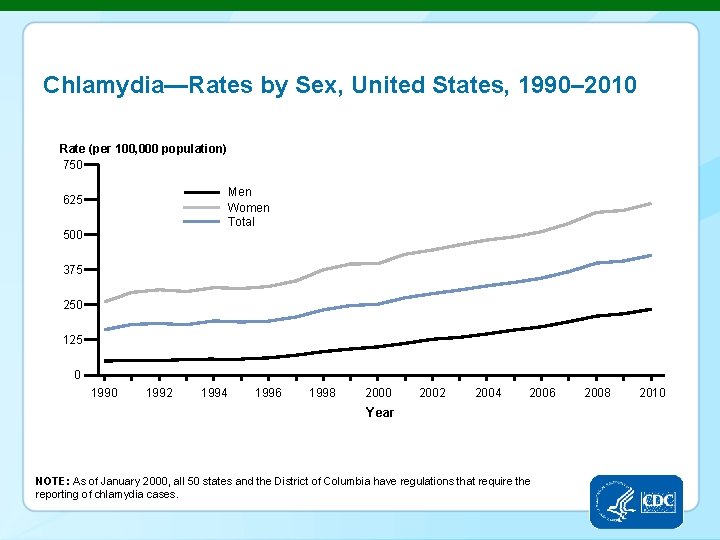
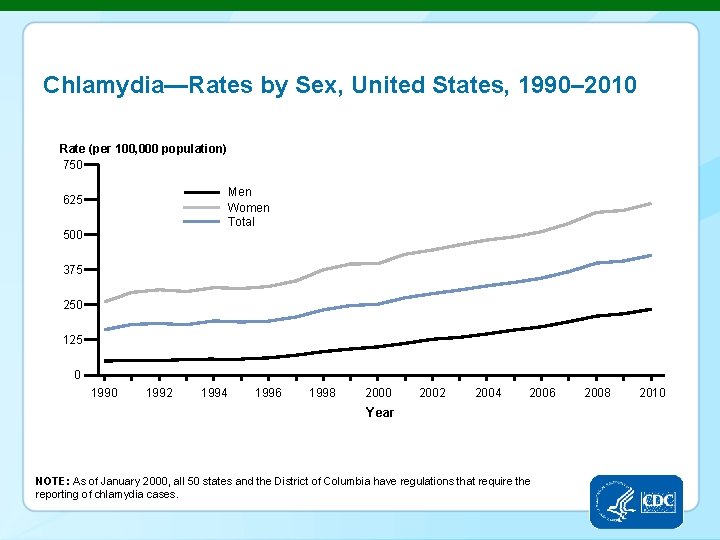
Chlamydia—Rates by Sex, United States, 1990– 2010 Rate (per 100, 000 population) 750 Men Women Total 625 500 375 250 125 0 1992 1994 1996 1998 2000 2002 2004 2006 Year NOTE: As of January 2000, all 50 states and the District of Columbia have regulations that require the reporting of chlamydia cases. 2008 2010
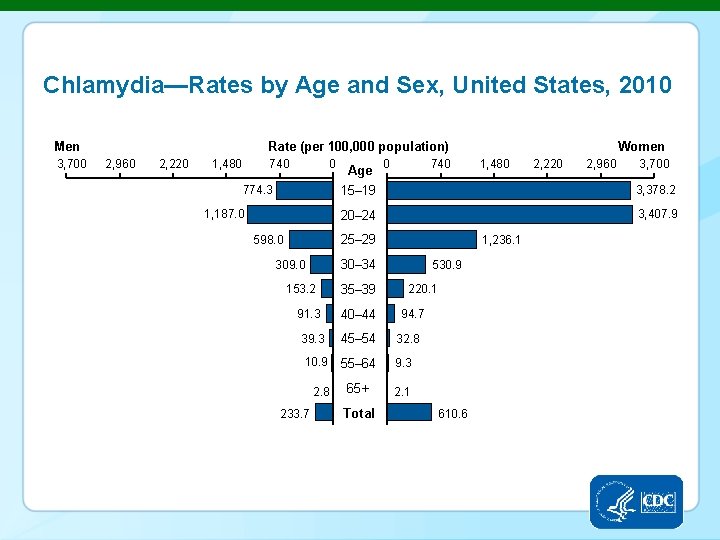
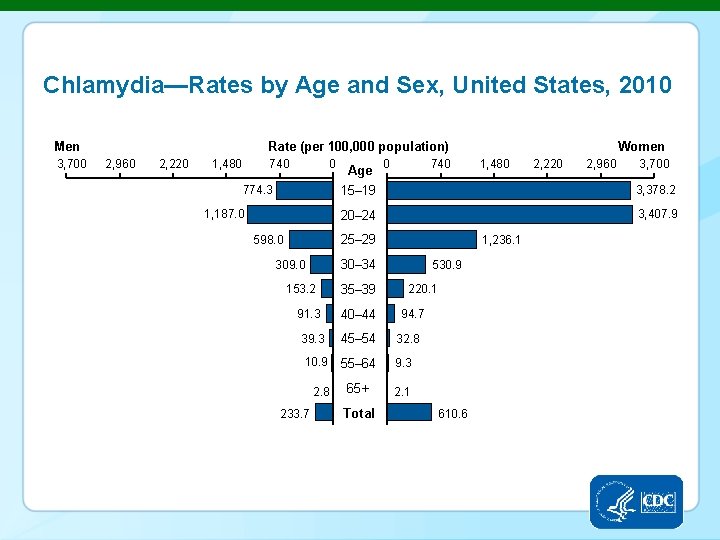
Chlamydia—Rates by Age and Sex, United States, 2010 Men 3, 700 Rate (per 100, 000 population) 2, 960 2, 220 1, 480 740 0 774. 3 1, 187. 0 Age 0 740 153. 2 91. 3 39. 3 10. 9 2. 8 233. 7 2, 220 2, 960 3, 700 3, 378. 2 20– 24 3, 407. 9 1, 236. 1 30– 34 309. 0 1, 480 15– 19 25– 29 598. 0 Women 35– 39 40– 44 530. 9 220. 1 94. 7 45– 54 32. 8 55– 64 9. 3 65+ 2. 1 Total 610. 6
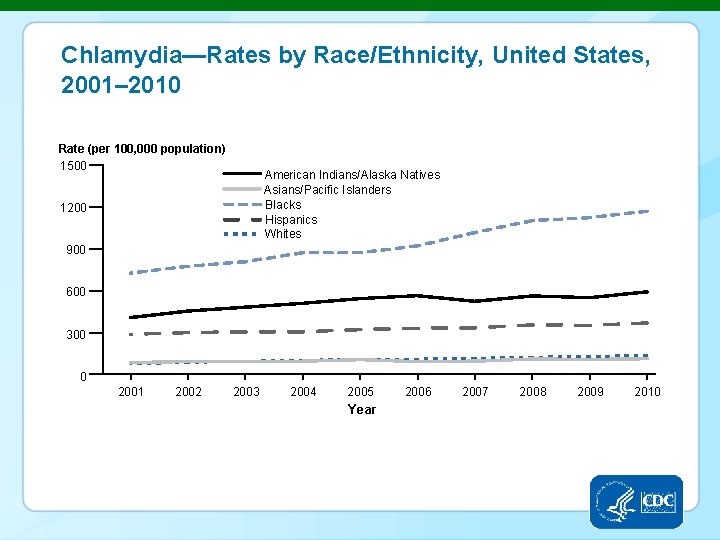
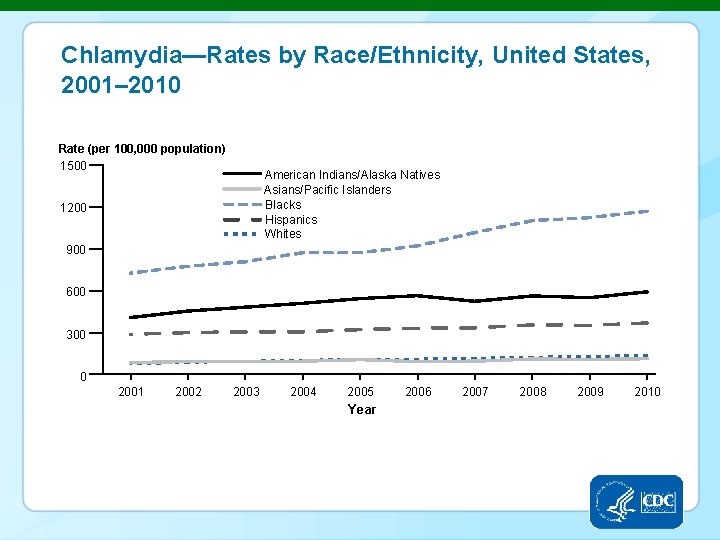
Chlamydia—Rates by Race/Ethnicity, United States, 2001– 2010 Rate (per 100, 000 population) 1500 American Indians/Alaska Natives Asians/Pacific Islanders Blacks Hispanics Whites 1200 900 600 300 0 2001 2002 2003 2004 2005 Year 2006 2007 2008 2009 2010
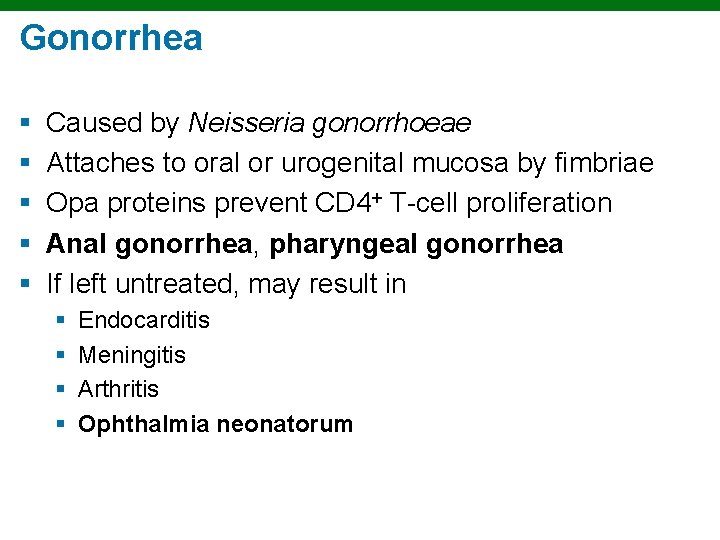
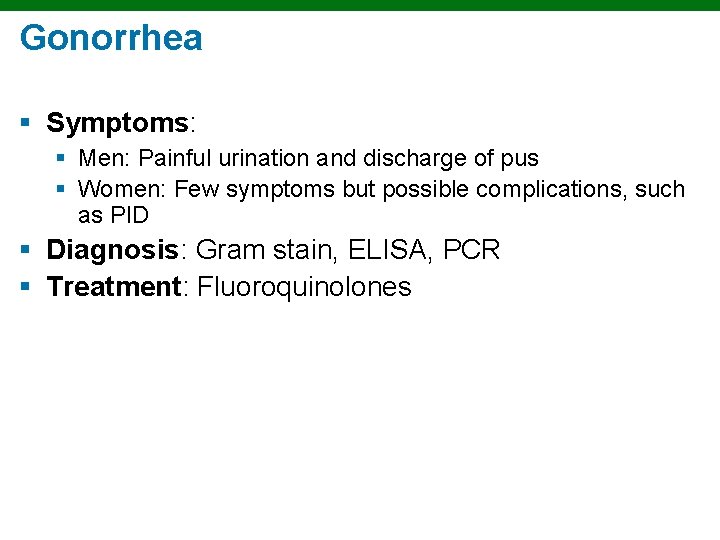
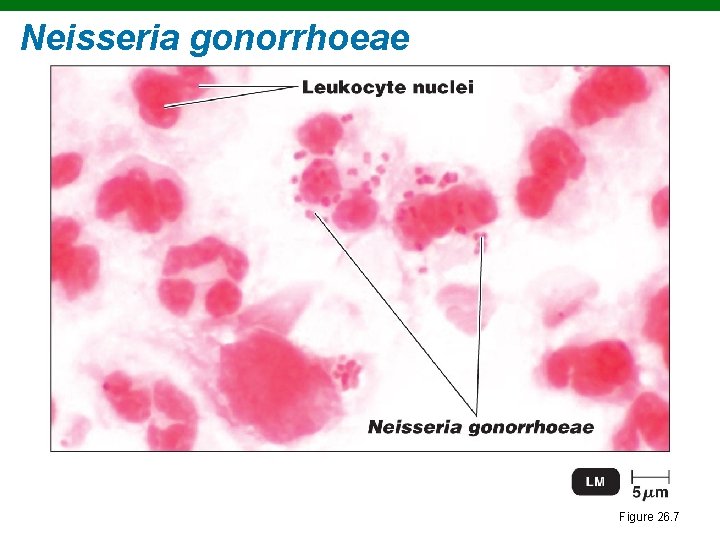
Gonorrhea § § § Caused by Neisseria gonorrhoeae Attaches to oral or urogenital mucosa by fimbriae Opa proteins prevent CD 4+ T-cell proliferation Anal gonorrhea, pharyngeal gonorrhea If left untreated, may result in § § Endocarditis Meningitis Arthritis Ophthalmia neonatorum
Gonorrhea § Symptoms: § Men: Painful urination and discharge of pus § Women: Few symptoms but possible complications, such as PID § Diagnosis: Gram stain, ELISA, PCR § Treatment: Fluoroquinolones
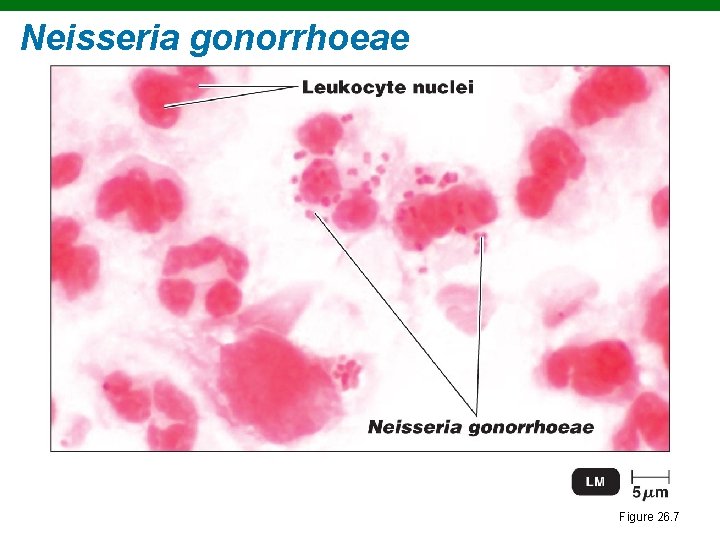
Neisseria gonorrhoeae Figure 26. 7
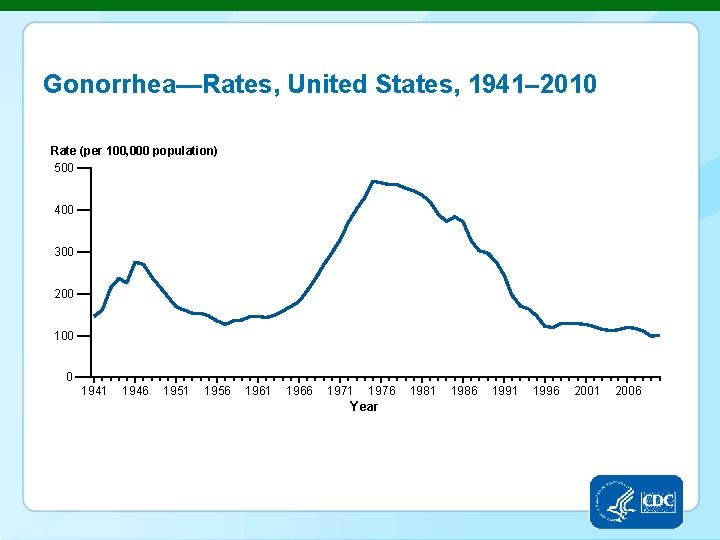
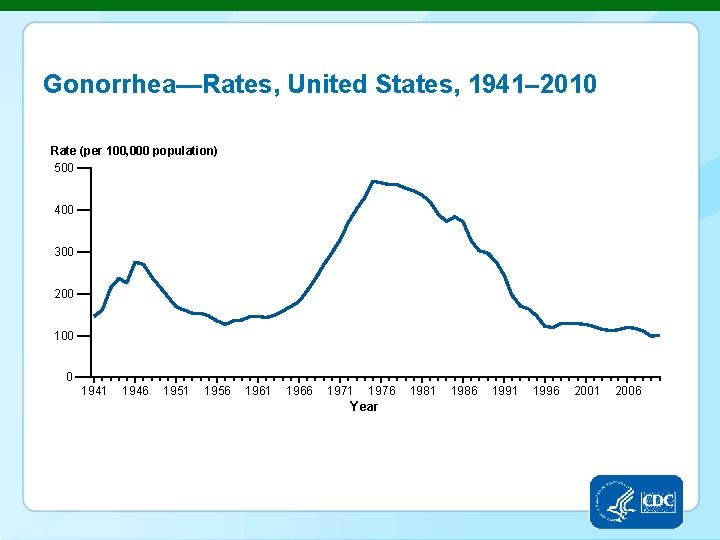
Gonorrhea—Rates, United States, 1941– 2010 Rate (per 100, 000 population) 500 400 300 200 100 0 1941 1946 1951 1956 1961 1966 1971 1976 Year 1981 1986 1991 1996 2001 2006
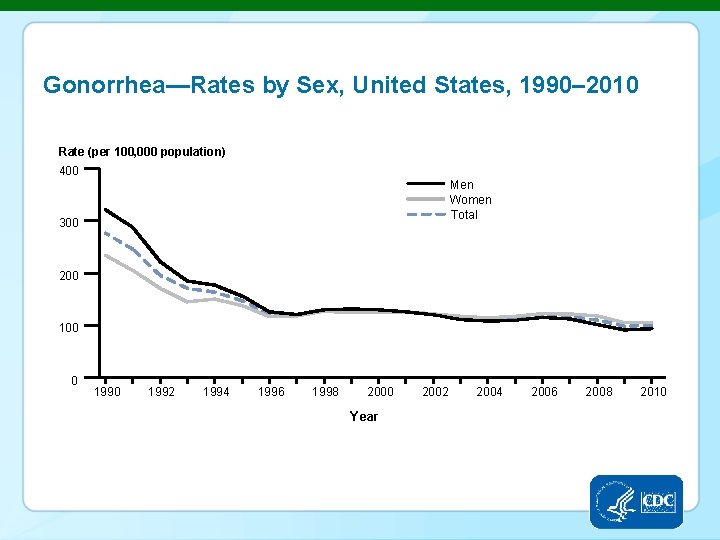
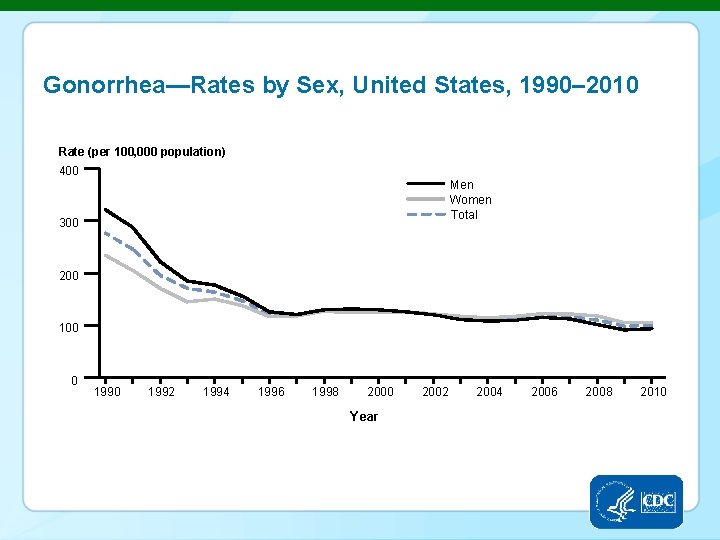
Gonorrhea—Rates by Sex, United States, 1990– 2010 Rate (per 100, 000 population) 400 Men Women Total 300 200 100 0 1992 1994 1996 1998 2000 Year 2002 2004 2006 2008 2010
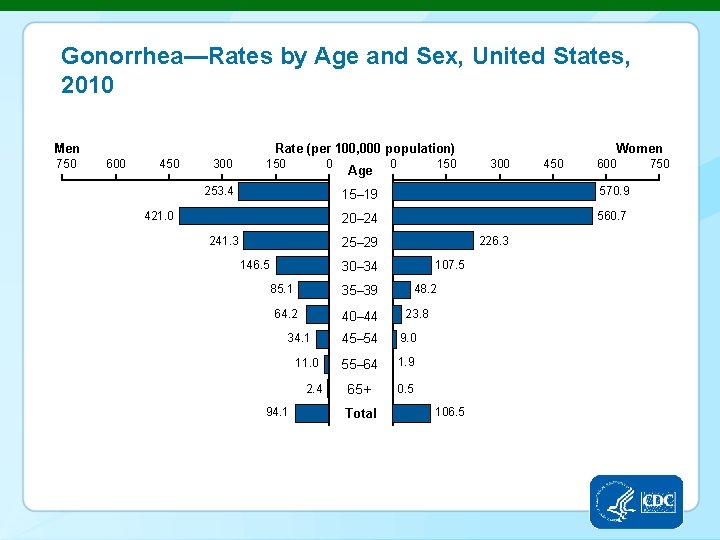
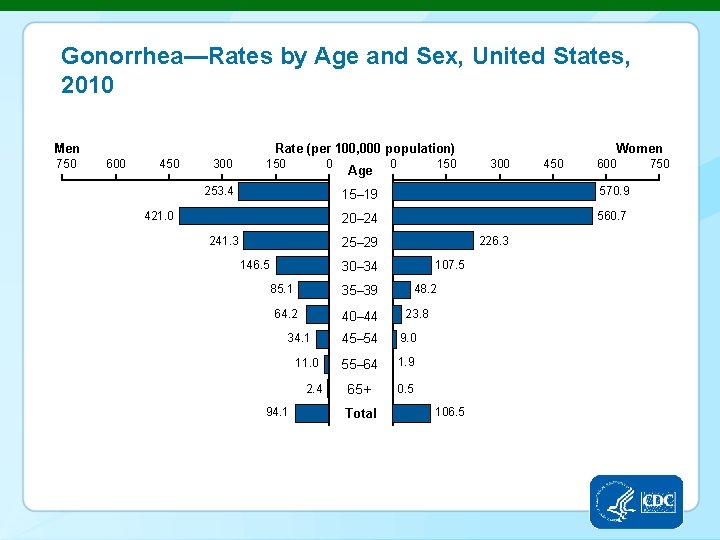
Gonorrhea—Rates by Age and Sex, United States, 2010 Men 750 Rate (per 100, 000 population) 600 450 300 150 0 253. 4 421. 0 241. 3 Age 0 150 20– 24 560. 7 35– 39 64. 2 40– 44 34. 1 11. 0 2. 4 94. 1 600 570. 9 226. 3 107. 5 30– 34 85. 1 450 15– 19 25– 29 146. 5 Women 300 48. 2 23. 8 45– 54 9. 0 55– 64 1. 9 65+ 0. 5 Total 106. 5 750
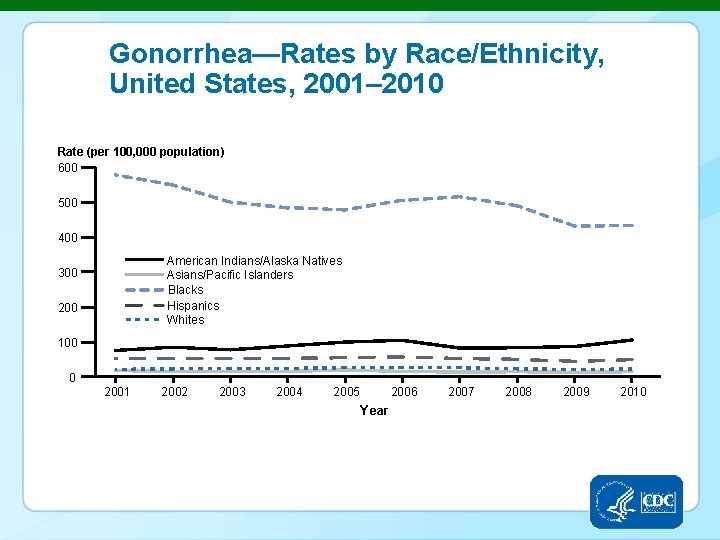
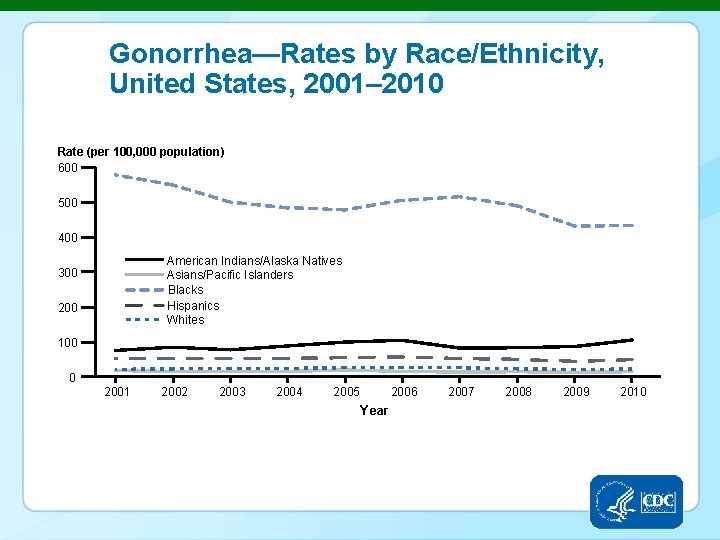
Gonorrhea—Rates by Race/Ethnicity, United States, 2001– 2010 Rate (per 100, 000 population) 600 500 400 American Indians/Alaska Natives Asians/Pacific Islanders Blacks Hispanics Whites 300 200 100 0 2001 2002 2003 2004 2005 Year 2006 2007 2008 2009 2010
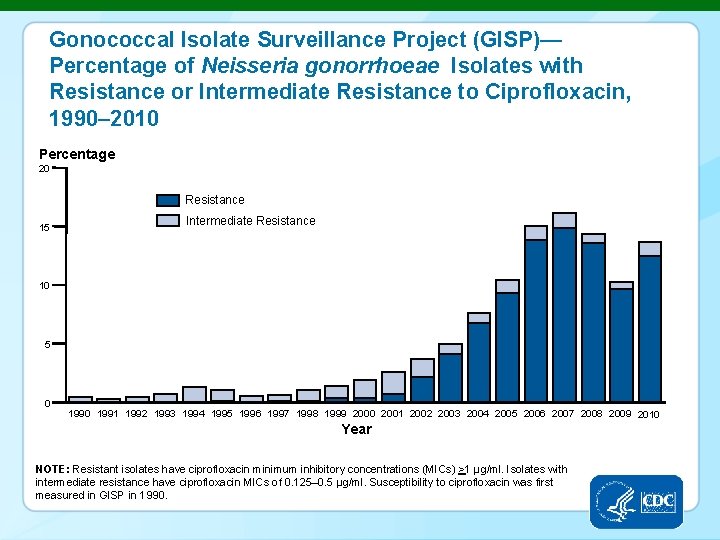
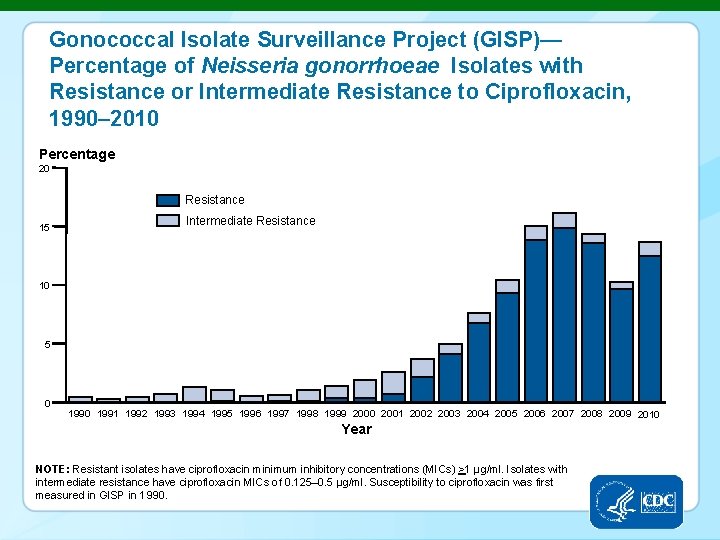
Gonococcal Isolate Surveillance Project (GISP)— Percentage of Neisseria gonorrhoeae Isolates with Resistance or Intermediate Resistance to Ciprofloxacin, 1990– 2010 Percentage 20 Resistance 15 Intermediate Resistance 10 5 0 1991 1992 1993 1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 Year NOTE: Resistant isolates have ciprofloxacin minimum inhibitory concentrations (MICs) >1 µg/ml. Isolates with intermediate resistance have ciprofloxacin MICs of 0. 125– 0. 5 µg/ml. Susceptibility to ciprofloxacin was first measured in GISP in 1990.
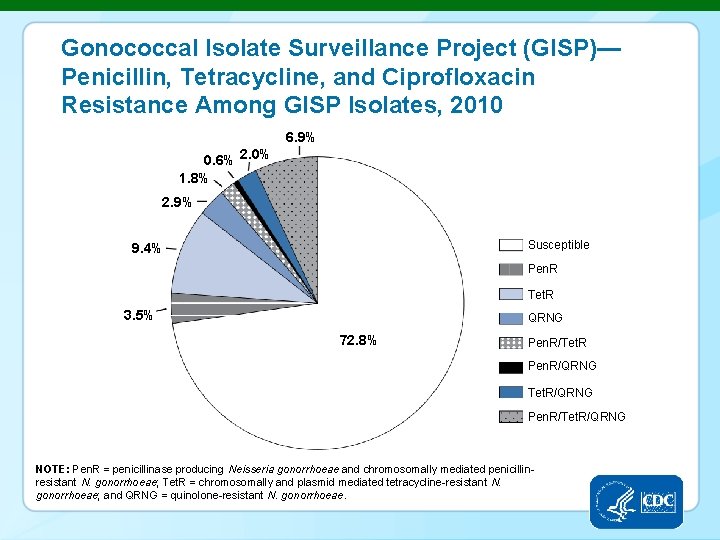
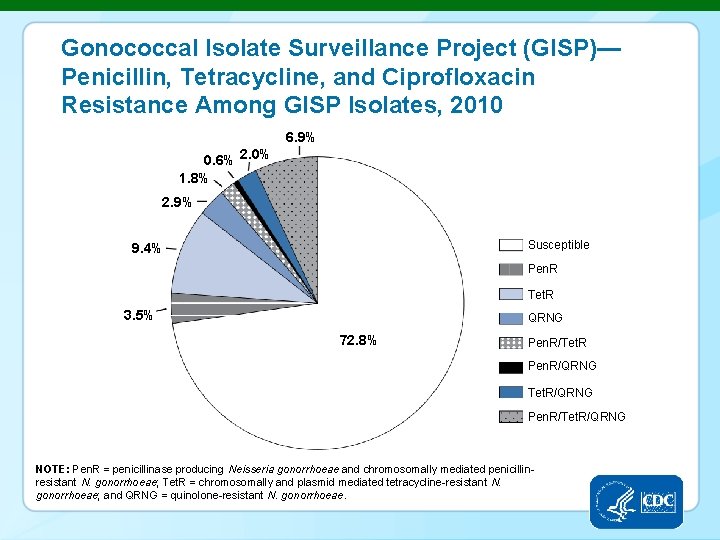
Gonococcal Isolate Surveillance Project (GISP)— Penicillin, Tetracycline, and Ciprofloxacin Resistance Among GISP Isolates, 2010 6. 9% 0. 6% 2. 0% 1. 8% 2. 9% Susceptible 9. 4% Pen. R Tet. R 3. 5% QRNG 72. 8% Pen. R/Tet. R Pen. R/QRNG Tet. R/QRNG Pen. R/Tet. R/QRNG NOTE: Pen. R = penicillinase producing Neisseria gonorrhoeae and chromosomally mediated penicillinresistant N. gonorrhoeae; Tet. R = chromosomally and plasmid mediated tetracycline-resistant N. gonorrhoeae; and QRNG = quinolone-resistant N. gonorrhoeae.
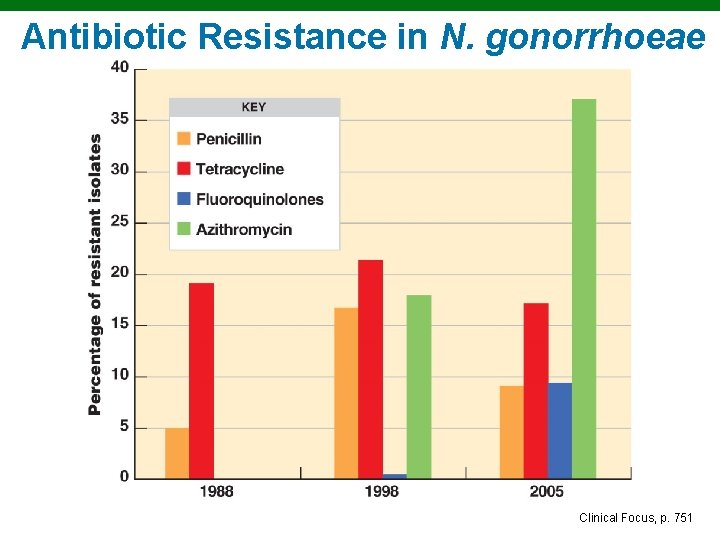
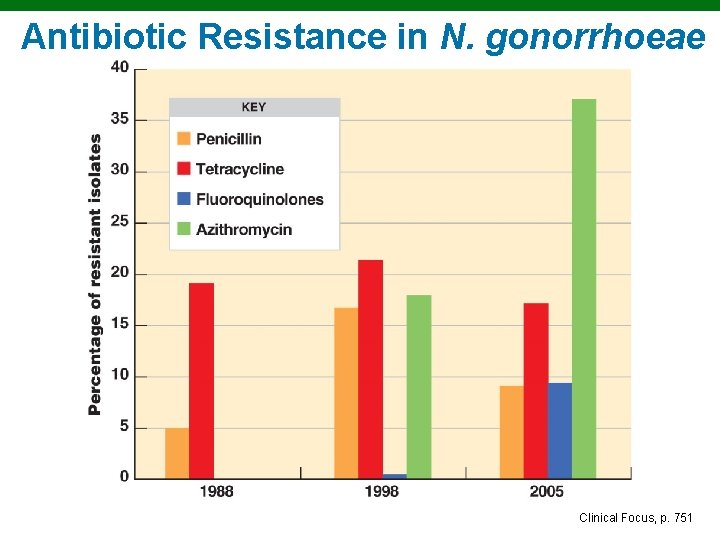
Antibiotic Resistance in N. gonorrhoeae Clinical Focus, p. 751
Nongonococcal Urethritis (NGU) § Nonspecific urethritis § Chlamydia trachomatis § Mycoplasma hominis § Ureaplasma urealyticum § Symptoms: Painful urination and watery discharge; in women, possible complications, such as PID § Diagnosis: Culturing, PCR § Treatment: Doxycycline, azithromycin
Pelvic Inflammatory Disease (PID) § Polymicrobic, usually § N. gonorrhoeae § C. trachomatis § Salpingitis (infection of uterine tubes) § Symptoms: Chronic abdominal pain § Treatment: Doxycycline and cefoxitin
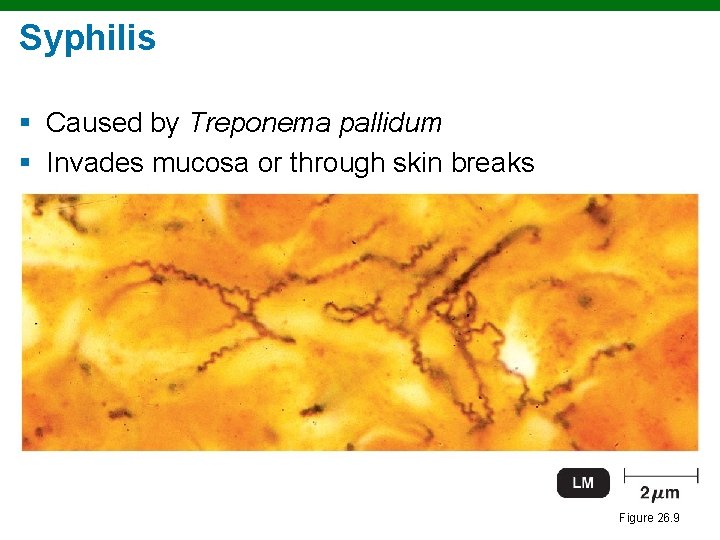
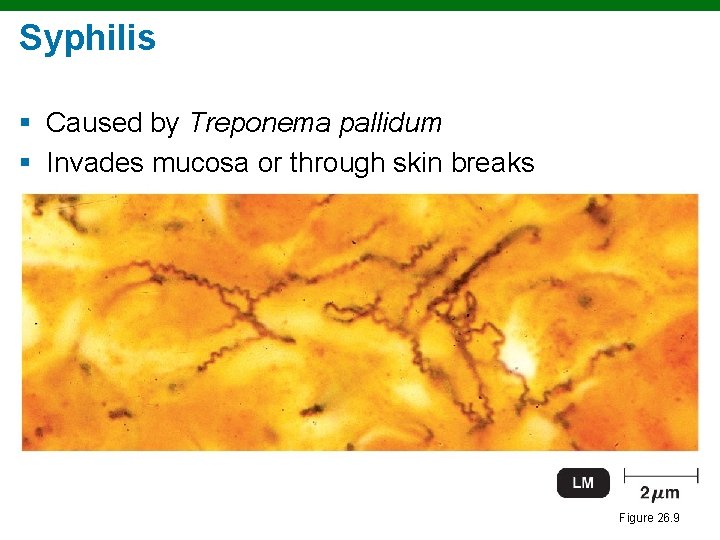
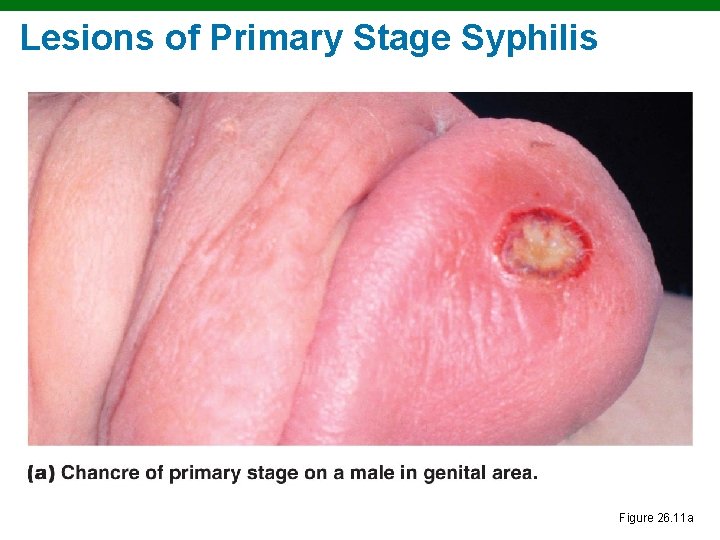
Syphilis § Caused by Treponema pallidum § Invades mucosa or through skin breaks Figure 26. 9
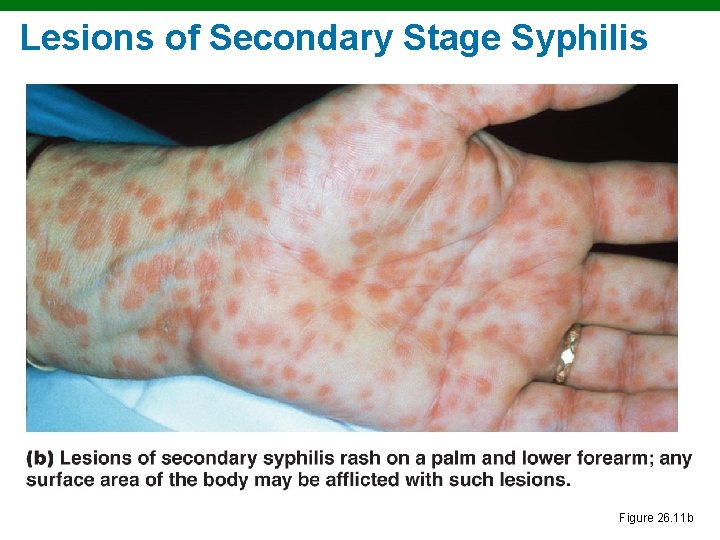
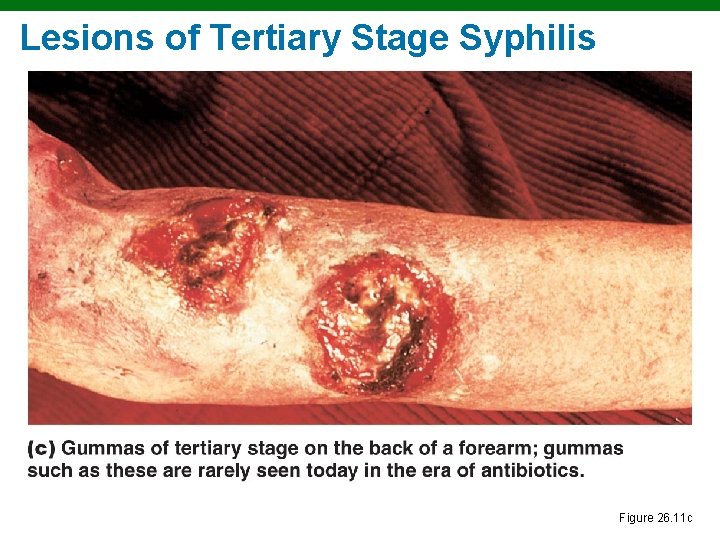
Syphilis § § § Primary stage: Chancre at site of infection Secondary stage: Skin and mucosal rashes Latent period: No symptoms Tertiary stage: Gummas on many organs Treatment: Benzathine penicillin Congenital: Neurological damage
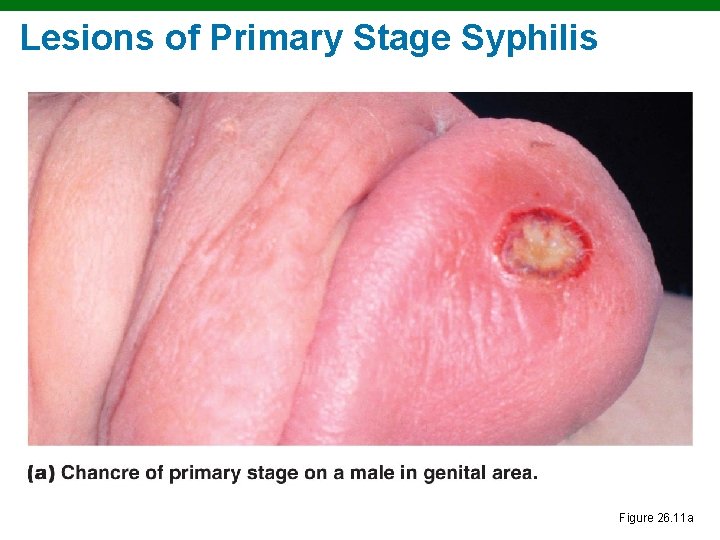
Lesions of Primary Stage Syphilis Figure 26. 11 a
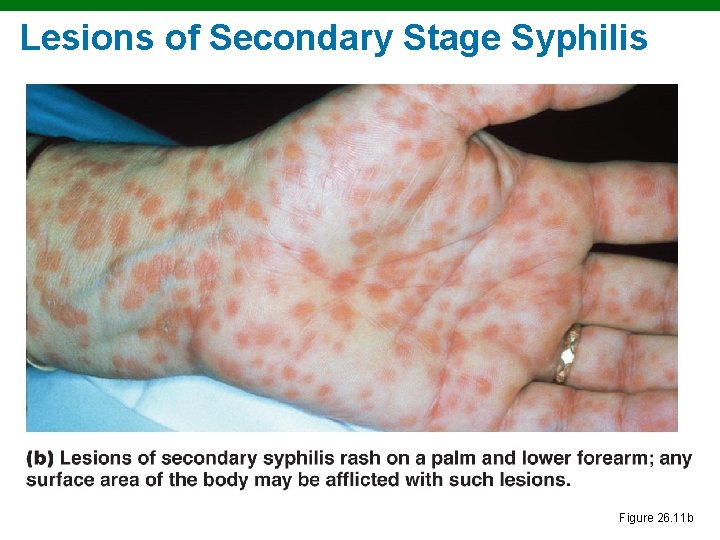
Lesions of Secondary Stage Syphilis Figure 26. 11 b
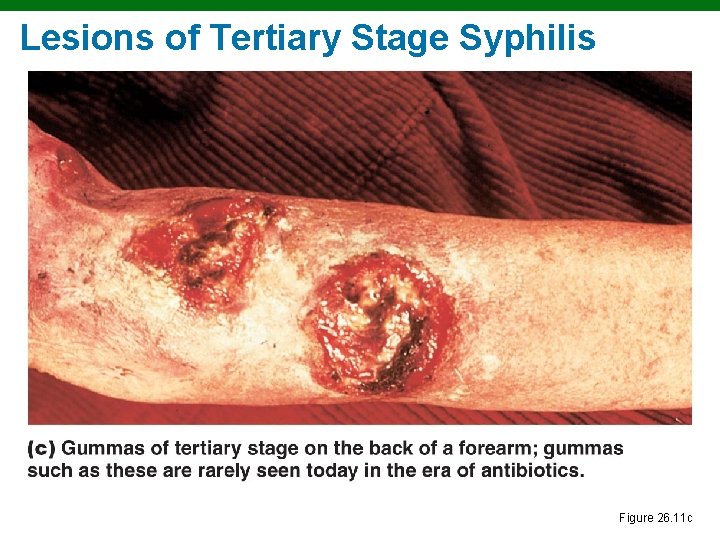
Lesions of Tertiary Stage Syphilis Figure 26. 11 c
Diagnosis of Syphilis § Direct diagnosis § Staining with fluorescent-labeled monoclonal antibodies § Indirect, rapid screening § VDRL, RPR, EIA § Confirming § FTA-ABS tests for anti-treponemal antibodies
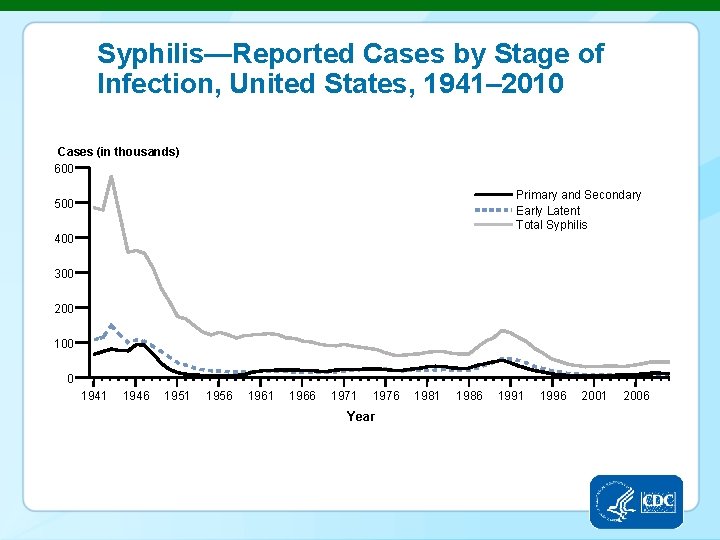
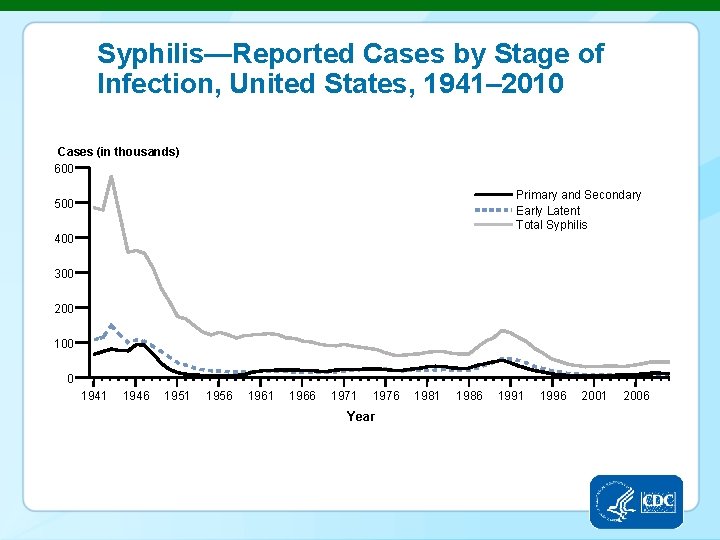
Syphilis—Reported Cases by Stage of Infection, United States, 1941– 2010 Cases (in thousands) 600 Primary and Secondary Early Latent Total Syphilis 500 400 300 200 100 0 1941 1946 1951 1956 1961 1966 1971 1976 Year 1981 1986 1991 1996 2001 2006
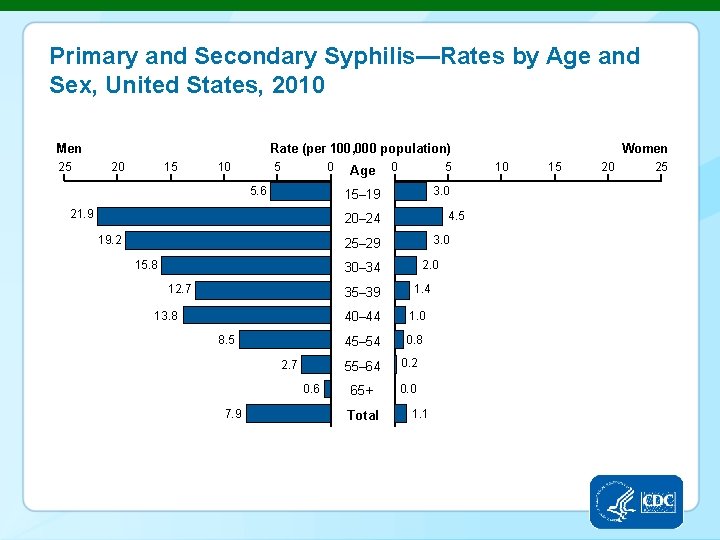
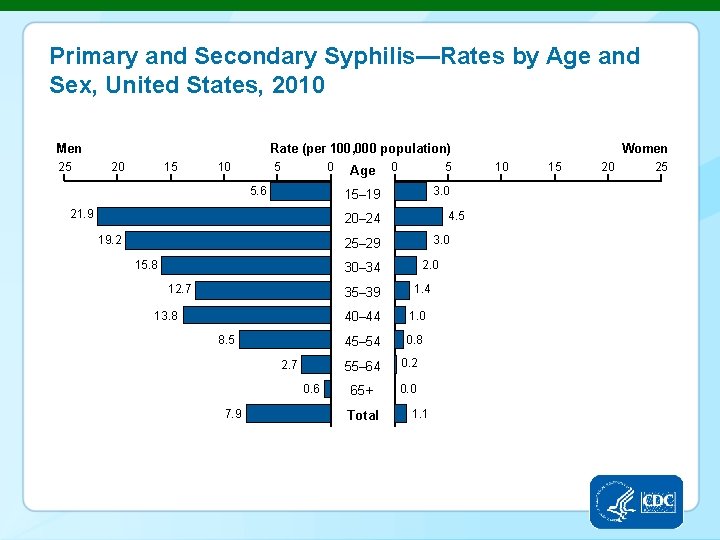
Primary and Secondary Syphilis—Rates by Age and Sex, United States, 2010 Men 25 Rate (per 100, 000 population) 20 15 10 5 0 5. 6 Age 0 5 3. 0 15– 19 21. 9 4. 5 20– 24 19. 2 3. 0 25– 29 15. 8 2. 0 30– 34 12. 7 35– 39 13. 8 8. 5 2. 7 0. 6 7. 9 1. 4 40– 44 1. 0 45– 54 0. 8 55– 64 0. 2 65+ 0. 0 Total 1. 1 Women 10 15 20 25
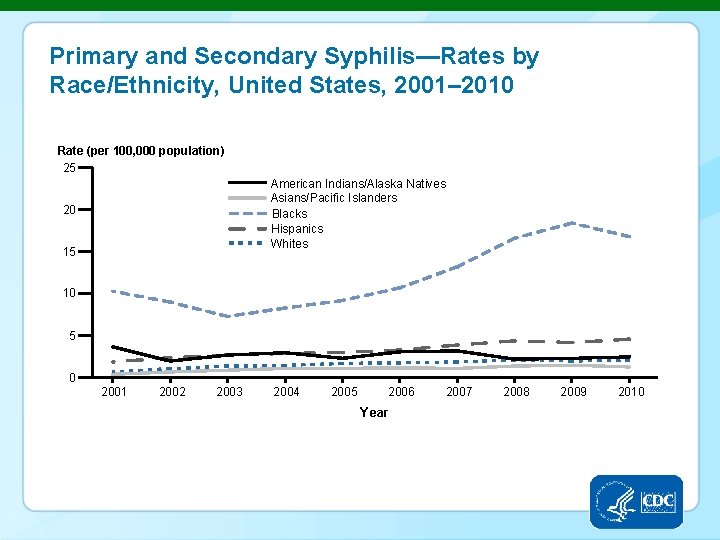
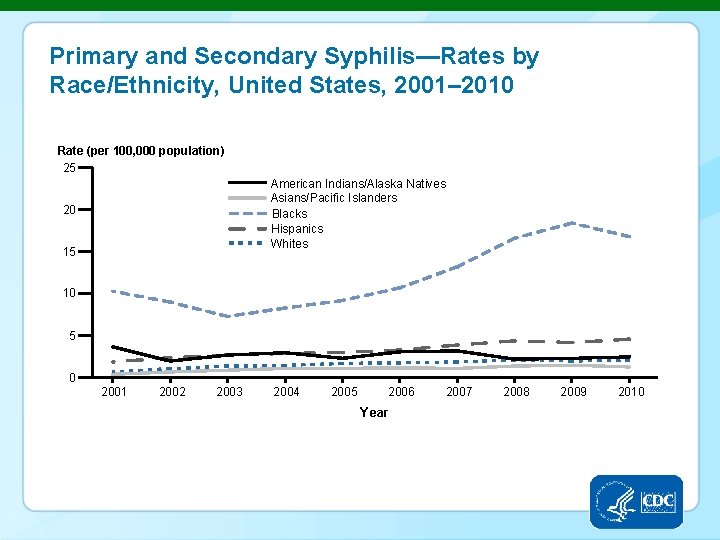
Primary and Secondary Syphilis—Rates by Race/Ethnicity, United States, 2001– 2010 Rate (per 100, 000 population) 25 American Indians/Alaska Natives Asians/Pacific Islanders Blacks Hispanics Whites 20 15 10 5 0 2001 2002 2003 2004 2005 2006 Year 2007 2008 2009 2010
Lymphogranuloma Venereum (LGV) § § § Causative agent: Chlamydia trachomatis Initial lesion on genitals heals Bacteria spread through lymph Symptoms: Swelling in lymph nodes in groin Diagnosis: Microscopic and culture Treatment: Doxycycline
Chancroid (Soft Chancre) § Causative agent: Haemophilus ducreyi § Symptoms: Painful ulcers of genitals swollen lymph nodes in groin § Diagnosis: Culture § Treatment: Erythromycin; cetriaxone
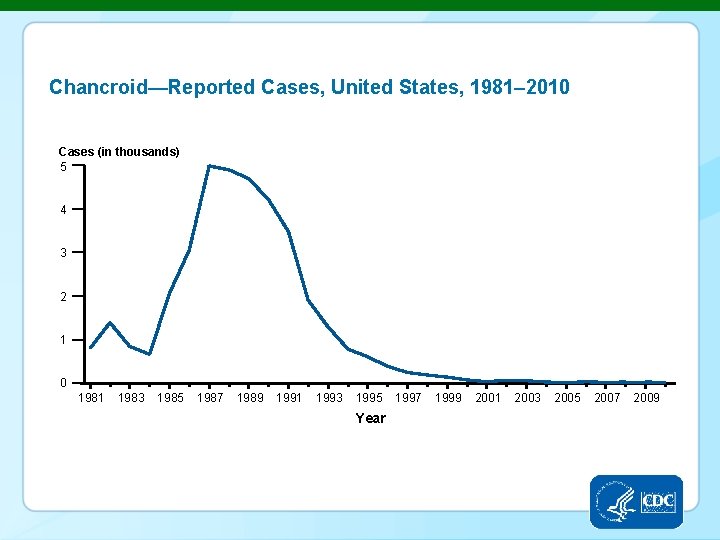
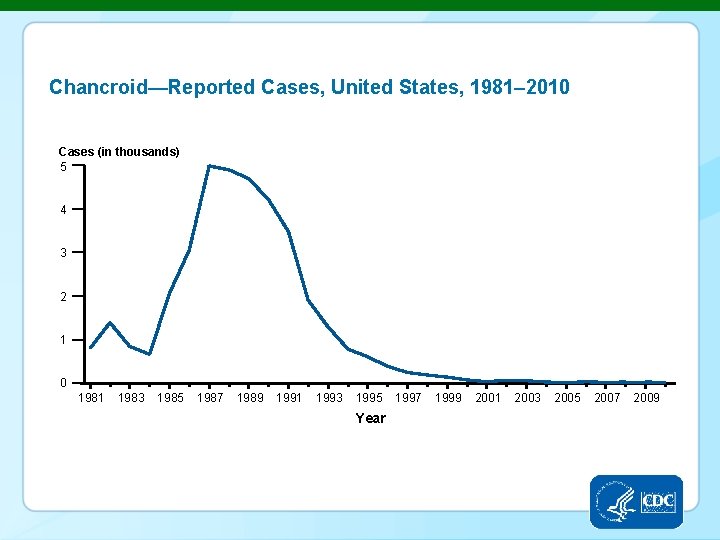
Chancroid—Reported Cases, United States, 1981– 2010 Cases (in thousands) 5 4 3 2 1 0 1981 1983 1985 1987 1989 1991 1993 1995 Year 1997 1999 2001 2003 2005 2007 2009
Bacterial Vaginosis § Causative agent: Gardnerella vaginalis § Symptoms: Copious fishy, gray-white, thin, frothy discharge § p. H: >4. 5 § Diagnosis: Clue cells § Treatment: Metronidazole
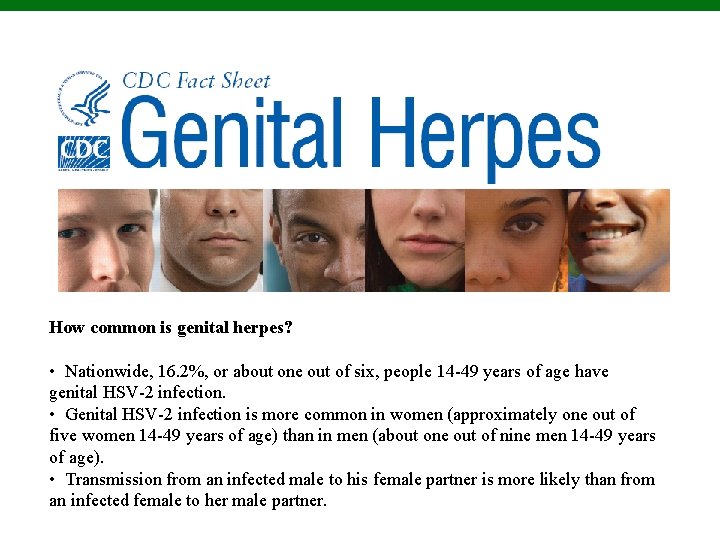
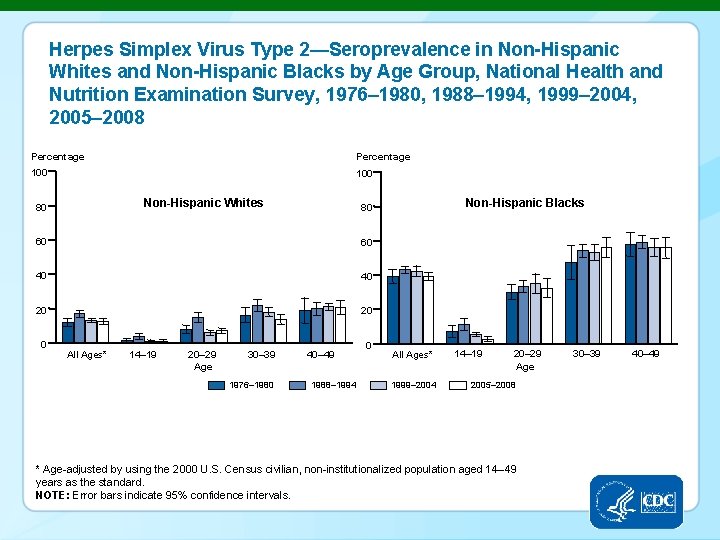
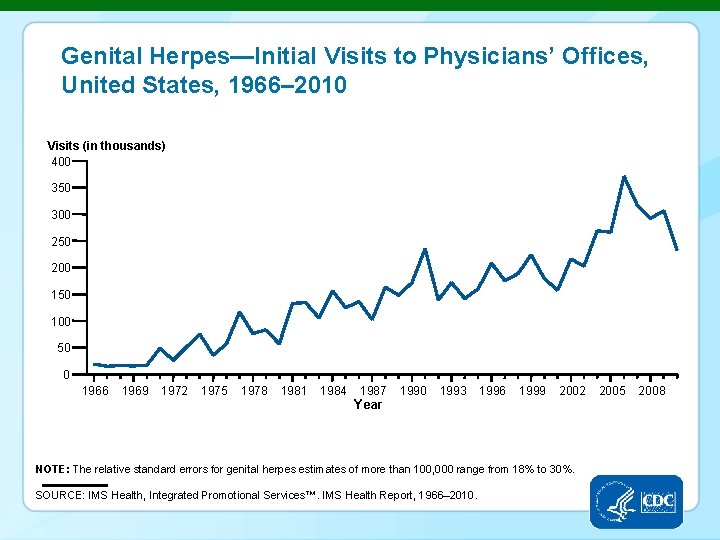
How common is genital herpes? • Nationwide, 16. 2%, or about one out of six, people 14 -49 years of age have genital HSV-2 infection. • Genital HSV-2 infection is more common in women (approximately one out of five women 14 -49 years of age) than in men (about one out of nine men 14 -49 years of age). • Transmission from an infected male to his female partner is more likely than from an infected female to her male partner.
Genital Herpes § Caused by herpes simplex virus 2 (human herpesvirus 2, or HSV– 2) § Painful vesicles on genitals § Neonatal herpes transmitted to fetus or newborns § Recurrences from viruses latent in nerves § Suppression: Acyclovir
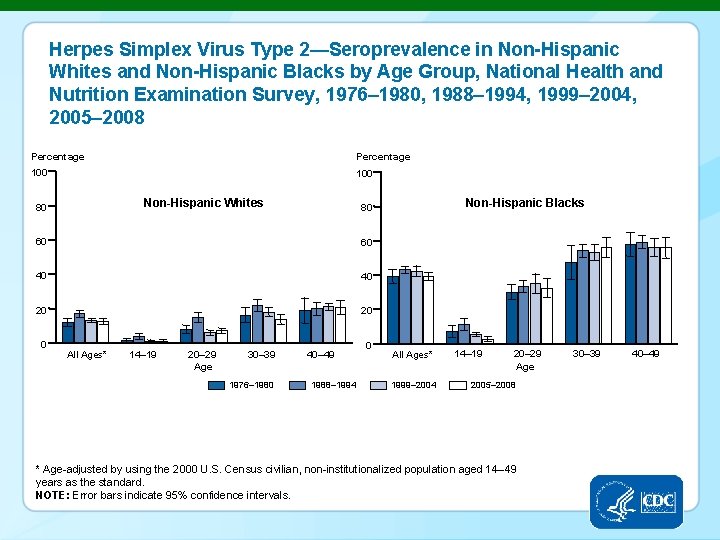
Herpes Simplex Virus Type 2—Seroprevalence in Non-Hispanic Whites and Non-Hispanic Blacks by Age Group, National Health and Nutrition Examination Survey, 1976– 1980, 1988– 1994, 1999– 2004, 2005– 2008 Percentage 100 Non-Hispanic Whites 80 60 60 40 40 20 20 0 All Ages* 14– 19 20– 29 Age 30– 39 1976– 1980 Non-Hispanic Blacks 80 40– 49 1988– 1994 0 All Ages* 1999– 2004 14– 19 20– 29 Age 2005– 2008 * Age-adjusted by using the 2000 U. S. Census civilian, non-institutionalized population aged 14– 49 years as the standard. NOTE: Error bars indicate 95% confidence intervals. 30– 39 40– 49
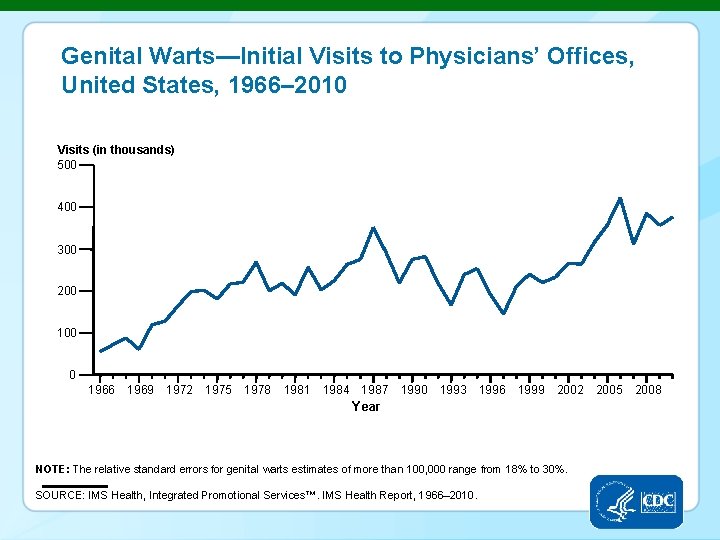
Genital Warts § Human papillomaviruses § Warts in genital area § HPV 16 causes cervical cancer and cancer of the penis § Treatment: Podofilox; imiquimod § Prevention: Vaccination against HPV strains
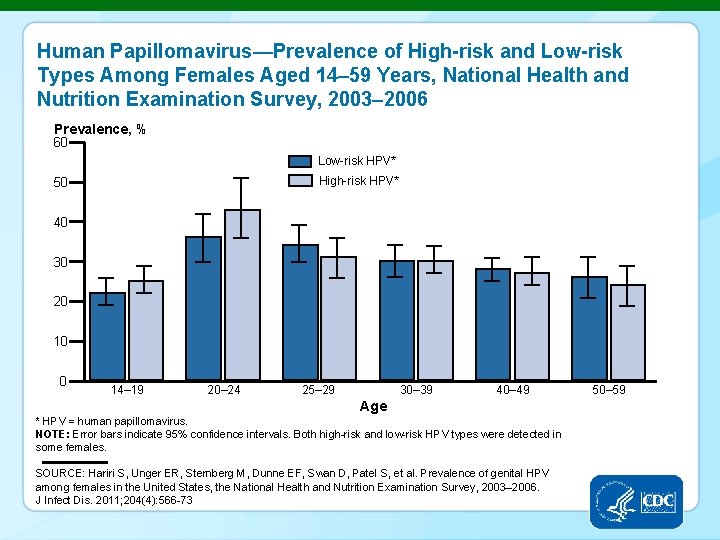
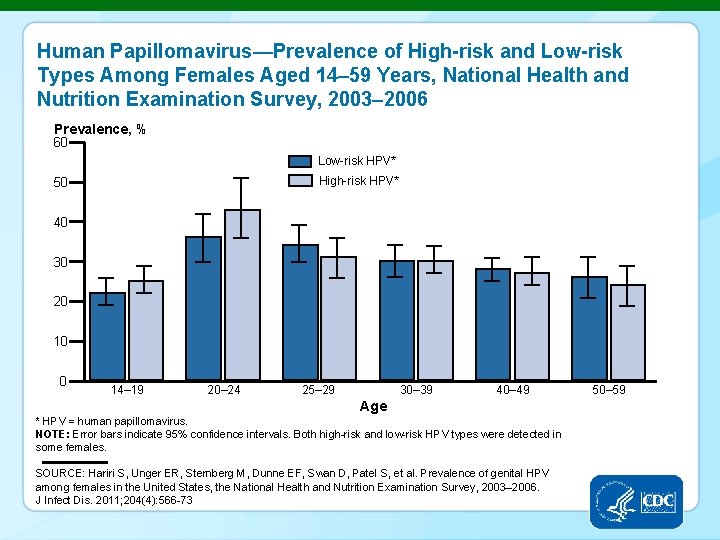
Human Papillomavirus—Prevalence of High-risk and Low-risk Types Among Females Aged 14– 59 Years, National Health and Nutrition Examination Survey, 2003– 2006 Prevalence, % 60 Low-risk HPV* High-risk HPV* 50 40 30 20 10 0 14– 19 20– 24 25– 29 30– 39 40– 49 Age * HPV = human papillomavirus. NOTE: Error bars indicate 95% confidence intervals. Both high-risk and low-risk HPV types were detected in some females. SOURCE: Hariri S, Unger ER, Sternberg M, Dunne EF, Swan D, Patel S, et al. Prevalence of genital HPV among females in the United States, the National Health and Nutrition Examination Survey, 2003– 2006. J Infect Dis. 2011; 204(4): 566 -73 50– 59
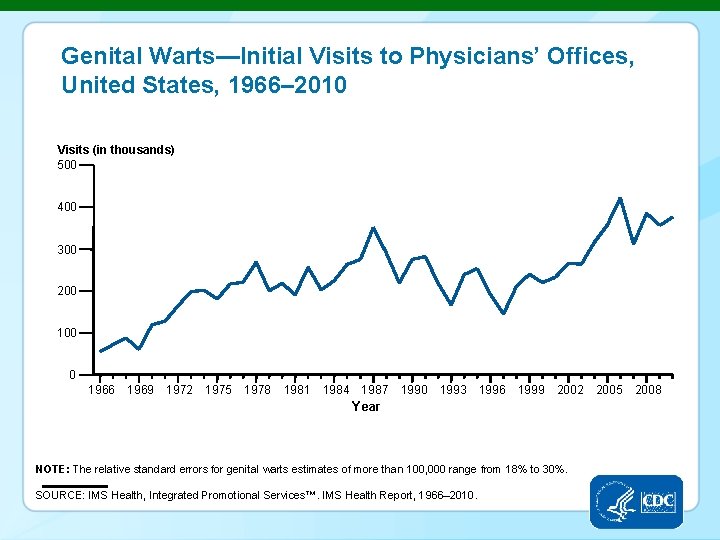
Genital Warts—Initial Visits to Physicians’ Offices, United States, 1966– 2010 Visits (in thousands) 500 400 300 200 100 0 1966 1969 1972 1975 1978 1981 1984 1987 1990 1993 1996 1999 2002 Year NOTE: The relative standard errors for genital warts estimates of more than 100, 000 range from 18% to 30%. SOURCE: IMS Health, Integrated Promotional Services™. IMS Health Report, 1966– 2010. 2005 2008
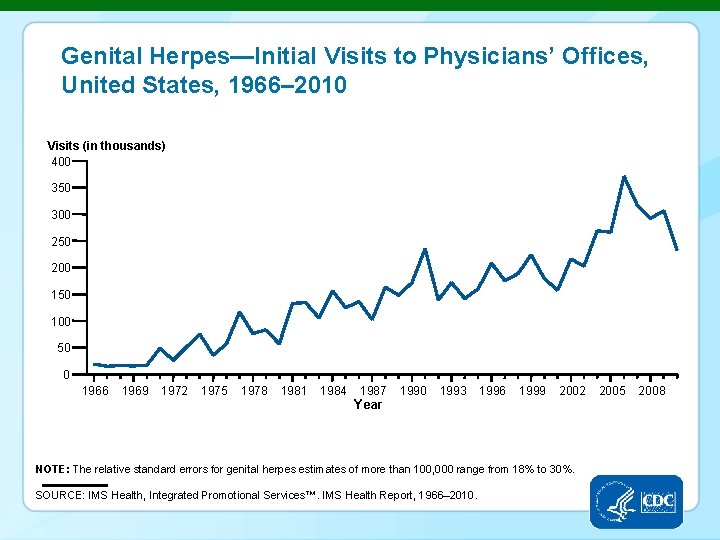
Genital Herpes—Initial Visits to Physicians’ Offices, United States, 1966– 2010 Visits (in thousands) 400 350 300 250 200 150 100 50 0 1966 1969 1972 1975 1978 1981 1984 1987 1990 1993 1996 1999 2002 Year NOTE: The relative standard errors for genital herpes estimates of more than 100, 000 range from 18% to 30%. SOURCE: IMS Health, Integrated Promotional Services™. IMS Health Report, 1966– 2010. 2005 2008
Candidiasis § Causative agent: Candida albicans § Grows on mucosa of mouth, intestinal tract, and genitourinary tract § NGU in males § Vulvovaginal candidiasis, yeasty discharge § p. H: <4 § Diagnosis: microscopic and culture § Treatment: Clotrimazole; fluconazole
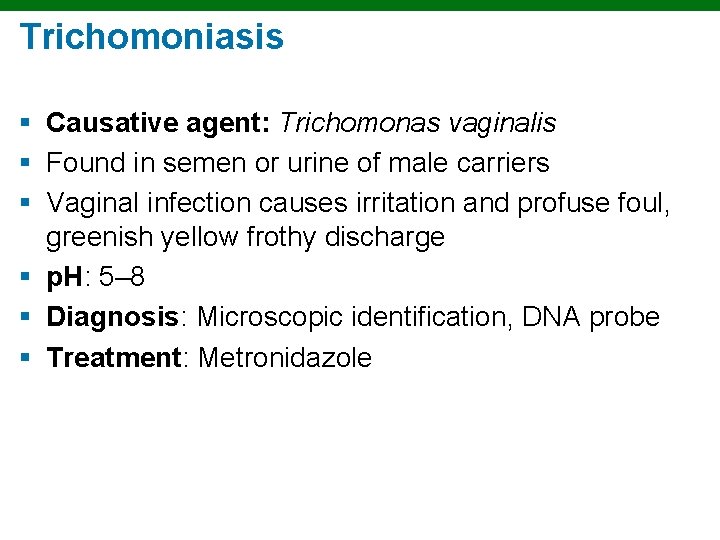
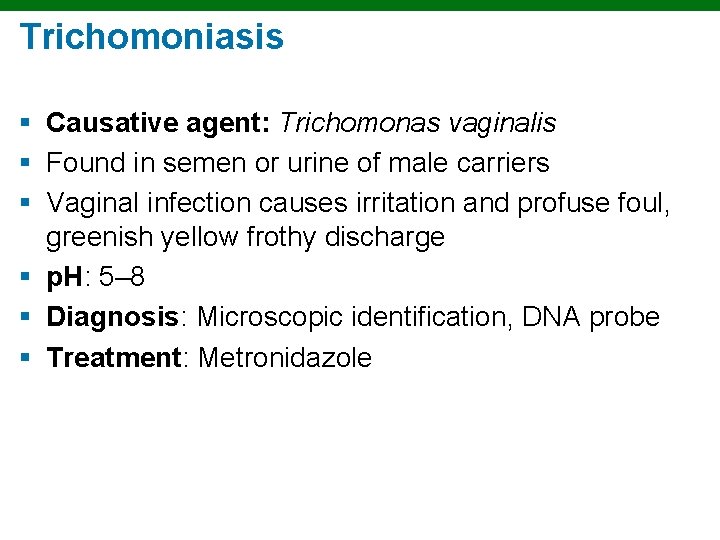
Trichomoniasis § Causative agent: Trichomonas vaginalis § Found in semen or urine of male carriers § Vaginal infection causes irritation and profuse foul, greenish yellow frothy discharge § p. H: 5– 8 § Diagnosis: Microscopic identification, DNA probe § Treatment: Metronidazole
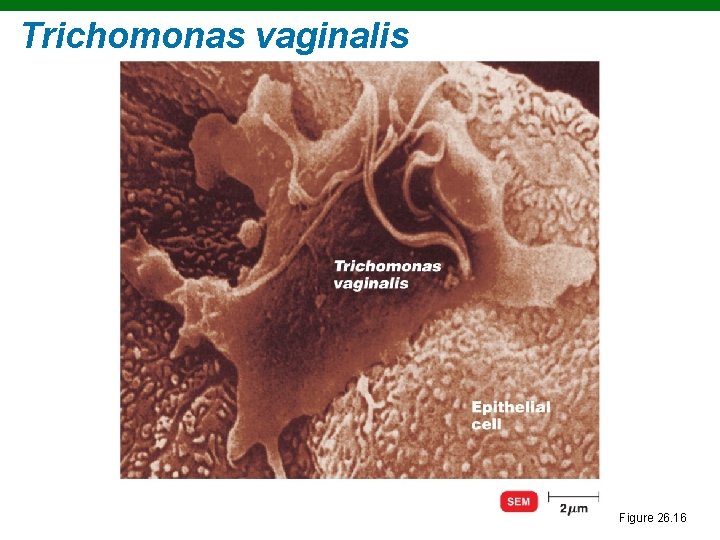
Trichomonas vaginalis Figure 26. 16
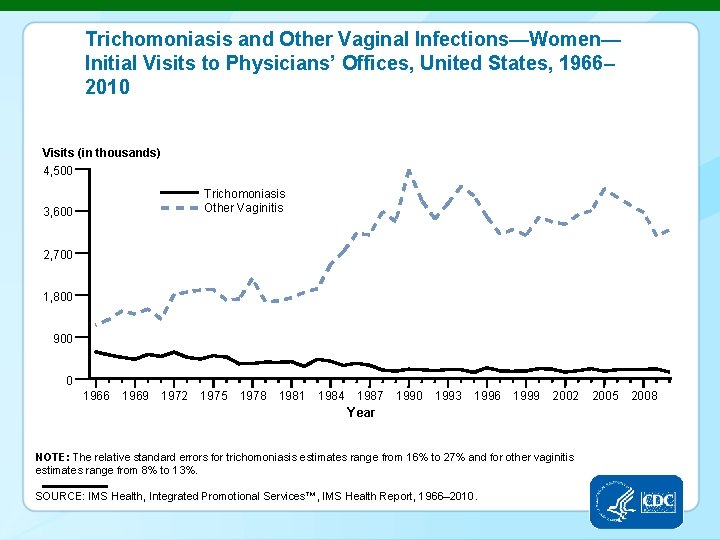
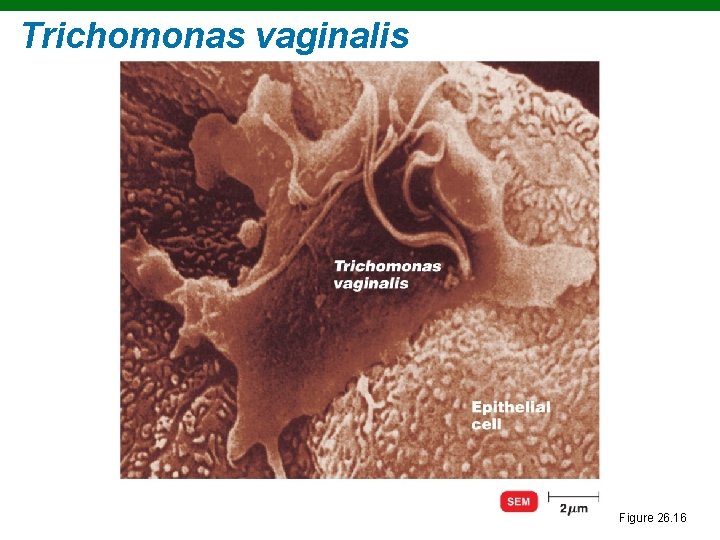
Trichomoniasis and Other Vaginal Infections—Women— Initial Visits to Physicians’ Offices, United States, 1966– 2010 Visits (in thousands) 4, 500 Trichomoniasis Other Vaginitis 3, 600 2, 700 1, 800 900 0 1966 1969 1972 1975 1978 1981 1984 1987 1990 1993 1996 1999 2002 Year NOTE: The relative standard errors for trichomoniasis estimates range from 16% to 27% and for other vaginitis estimates range from 8% to 13%. SOURCE: IMS Health, Integrated Promotional Services™, IMS Health Report, 1966– 2010. 2005 2008
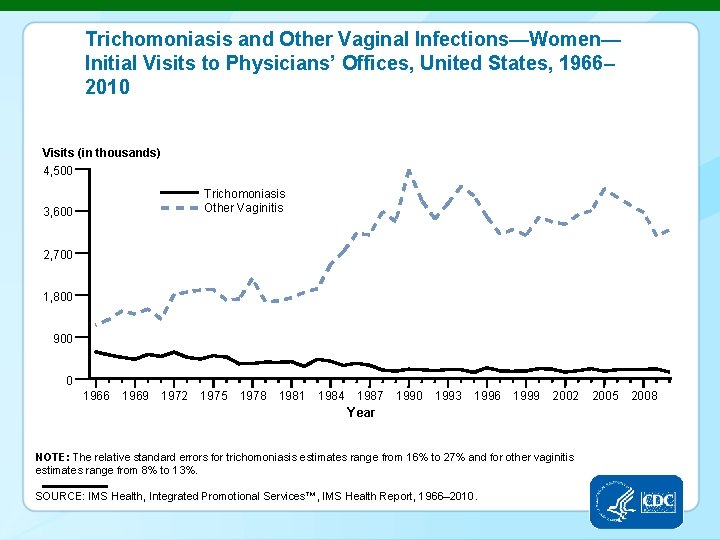
The TORCH Panel of Tests § Toxoplasmosis § Other (such as syphilis, hepatitis B, enterovirus, Epstein-Barr virus, varicella-zoster virus) § Rubella § Cytomegalovirus § Herpes simplex virus
STDS IN RACIAL AND ETHNIC MINORITIES Sexually Transmitted Disease Surveillance 2010 Division of STD Prevention
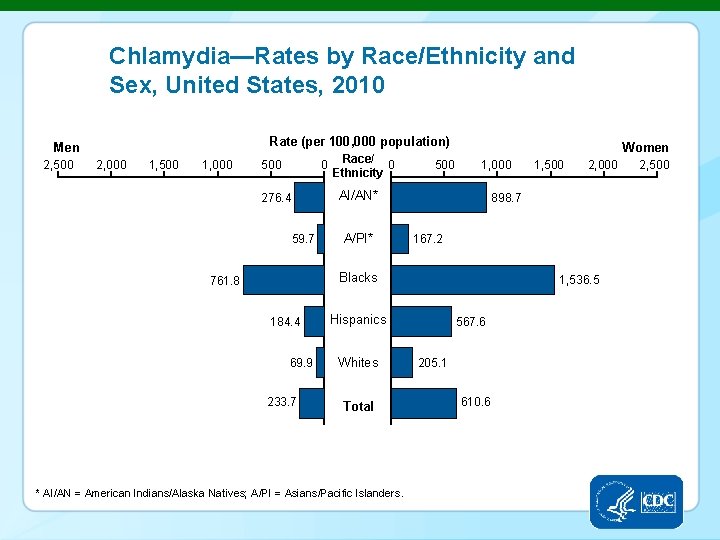
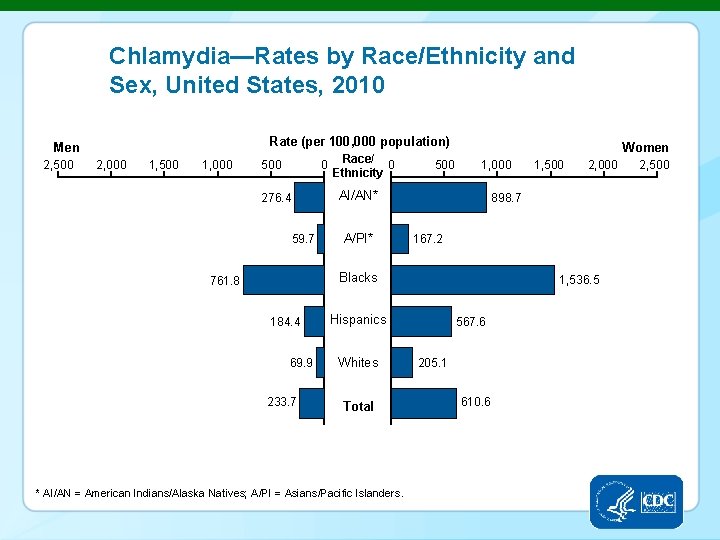
Chlamydia—Rates by Race/Ethnicity and Sex, United States, 2010 Rate (per 100, 000 population) Men 2, 500 2, 000 1, 500 1, 000 0 Race/ 0 Ethnicity 500 Women 1, 000 AI/AN* 276. 4 59. 7 A/PI* 184. 4 69. 9 167. 2 233. 7 1, 536. 5 Hispanics Whites Total * AI/AN = American Indians/Alaska Natives; A/PI = Asians/Pacific Islanders. 2, 000 898. 7 Blacks 761. 8 1, 500 567. 6 205. 1 610. 6 2, 500
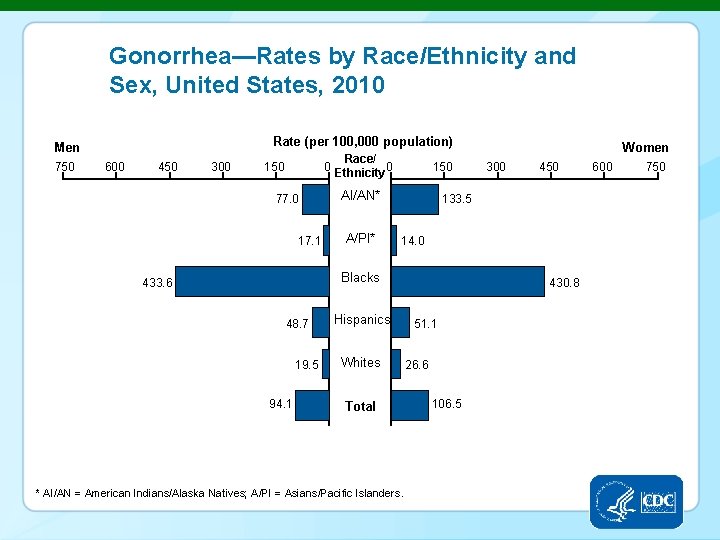
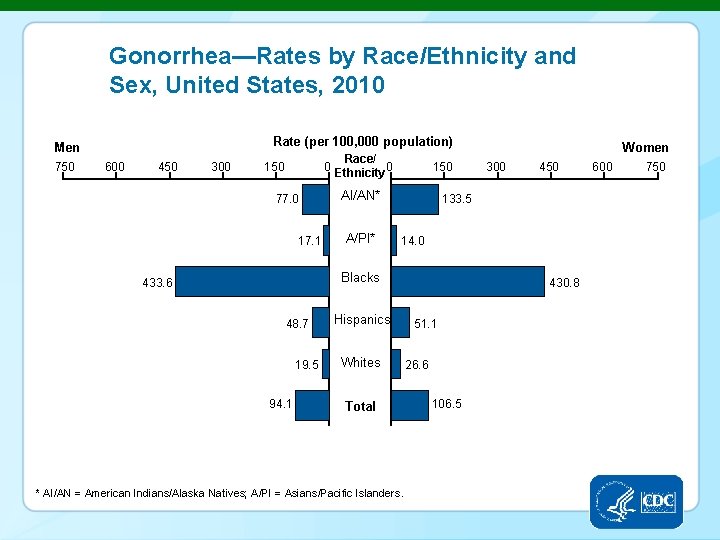
Gonorrhea—Rates by Race/Ethnicity and Sex, United States, 2010 Rate (per 100, 000 population) Men 750 600 450 300 Race/ 0 Ethnicity 0 150 77. 0 17. 1 150 AI/AN* A/PI* 48. 7 19. 5 94. 1 300 450 133. 5 14. 0 Blacks 433. 6 Women Hispanics Whites Total * AI/AN = American Indians/Alaska Natives; A/PI = Asians/Pacific Islanders. 430. 8 51. 1 26. 6 106. 5 600 750
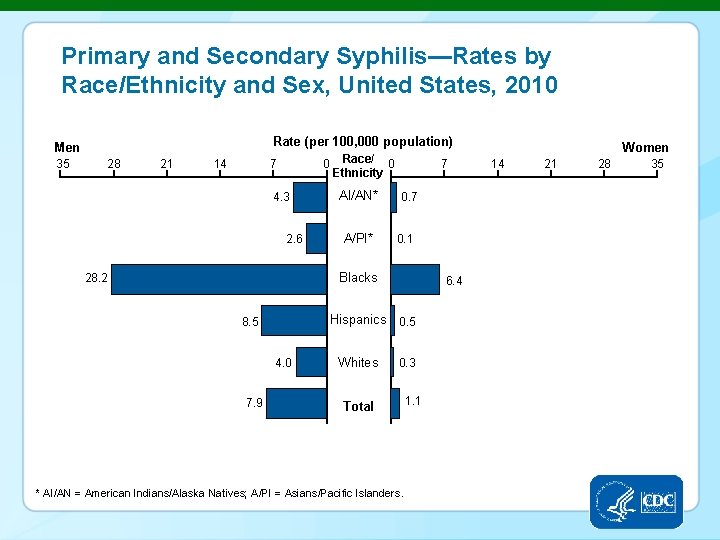
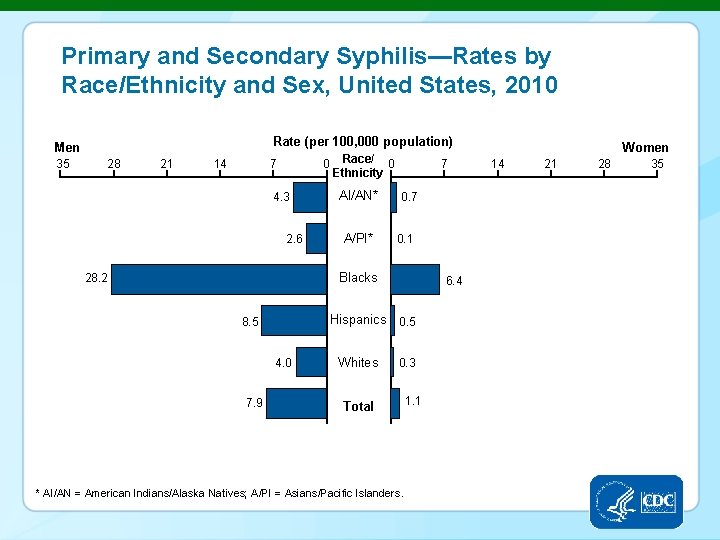
Primary and Secondary Syphilis—Rates by Race/Ethnicity and Sex, United States, 2010 Rate (per 100, 000 population) Men 35 28 21 14 0 Race/ 0 Ethnicity 7 4. 3 2. 6 28. 2 AI/AN* A/PI* 7 0. 1 Blacks Hispanics 0. 5 8. 5 4. 0 7. 9 6. 4 Whites 0. 3 Total * AI/AN = American Indians/Alaska Natives; A/PI = Asians/Pacific Islanders. 1. 1 Women 14 21 28 35