Structural Competency The Structural Determinants of Health PHASE



- Slides: 69
Structural Competency & The Structural Determinants of Health PHASE Convening November 29, 2018
Structural Competency Working Group Focused on integrating structural competency into training and practice of healthcare providers Comprised of health care providers, social scientists, health administrators, community health activists, and graduate and professional students. 2
Facilitator Introductions Ariana Thompson-Lastad, Ph. D Postdoctoral Research Fellow, UC San Francisco Ariana. Thompson-lastad@ucsf. edu Josh Neff, MS SCWG Co-founder and Co-coordinator Medical Student, UC San Francisco Joshua. Neff@ucsf. edu
Structural Competency Session Learning Objectives: 1. Develop shared vocabulary related to social structures and patient health 2. Analyze and discuss clinical case studies to gain tangible skills for identifying structural forces affecting particular patient populations 3. Explore the differences between social and structural determinants of health 4. Articulate strategies and plan concrete actions to respond to the influences of structures in and beyond healthcare settings
Structural Competency Session Positionality: • We all have specific areas of expertise • Privilege & blind spots • Feedback
Training Agenda • Shared language & workbook • Social structures and patient health • Origins and importance of Structural Competency • Key terms for this work • Practical steps for responding to harmful structures • Small group discussions: • Applying structures to a patient case study • How can we respond to harmful structures? Practical steps for our work
Why are people poor/sick? “No one has a right to work with poor people unless they have a real analysis of why people are poor. ” Barbara Major, Director, St. Thomas Health Clinic, New Orleans 7
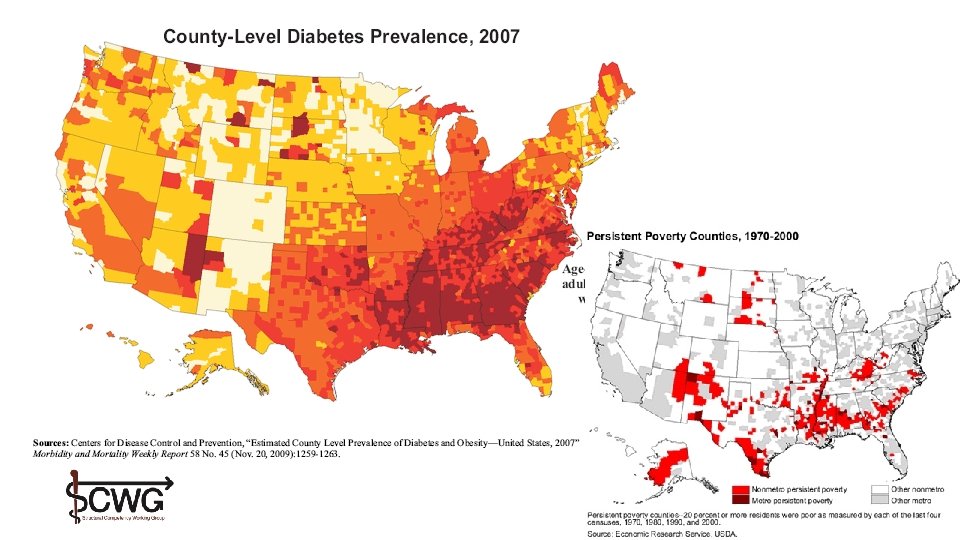
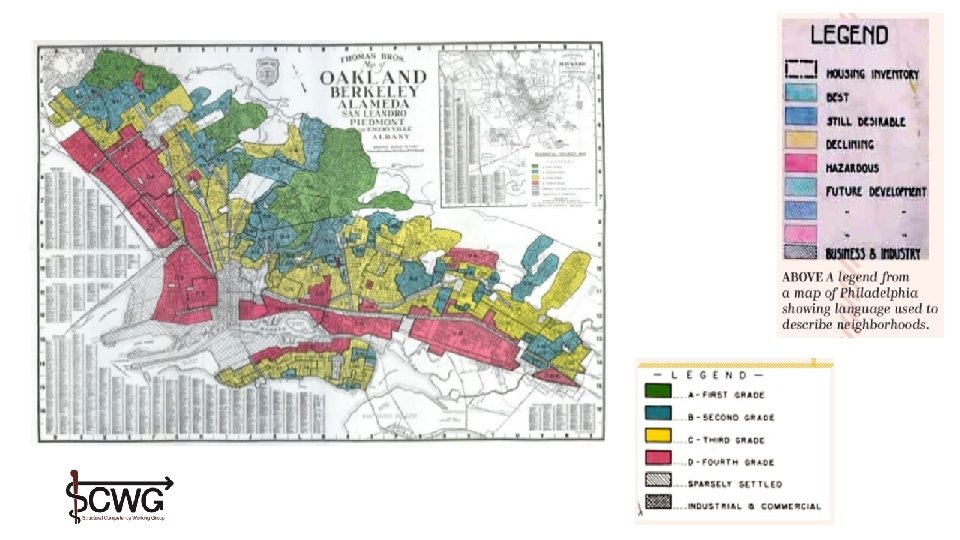
Examples of Structures and Patient Health
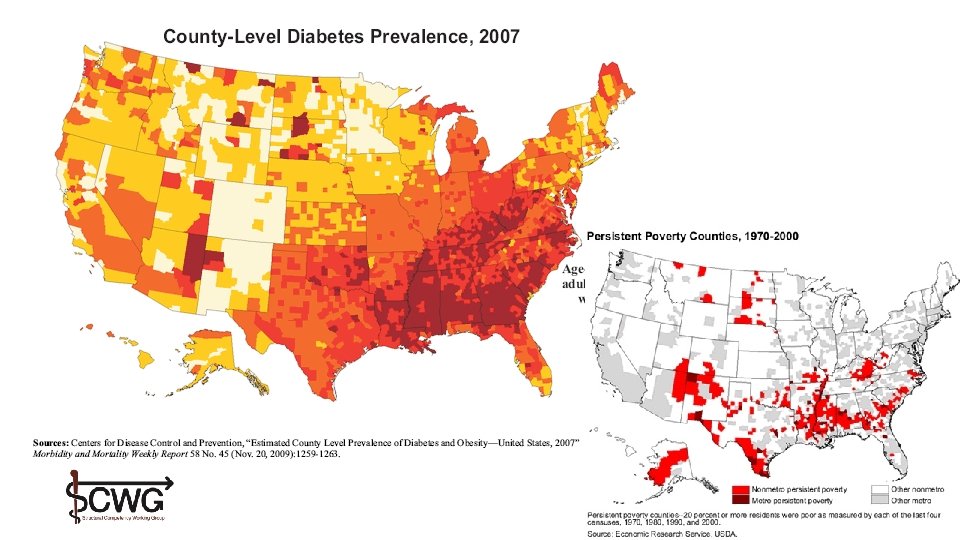
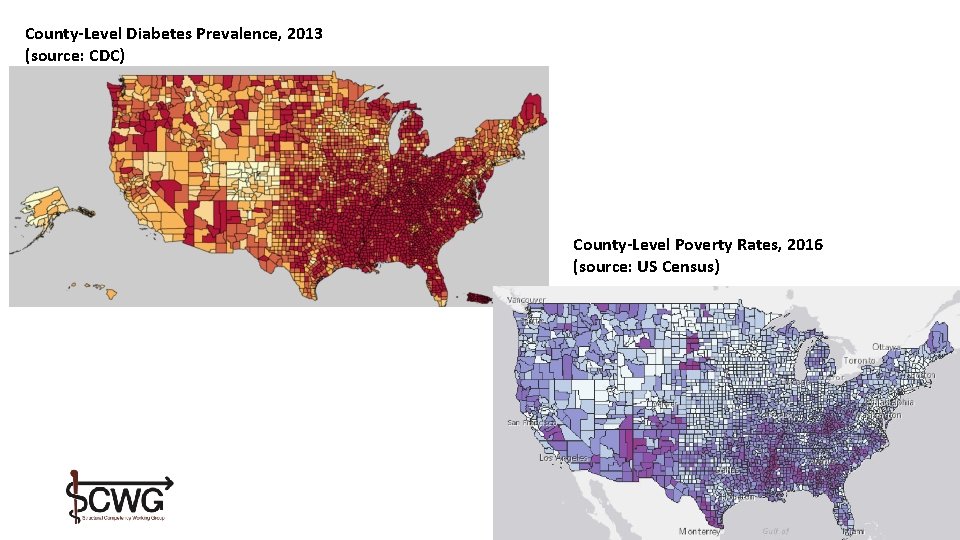
County-Level Diabetes Prevalence, 2013 (source: CDC) County-Level Poverty Rates, 2016 (source: US Census)
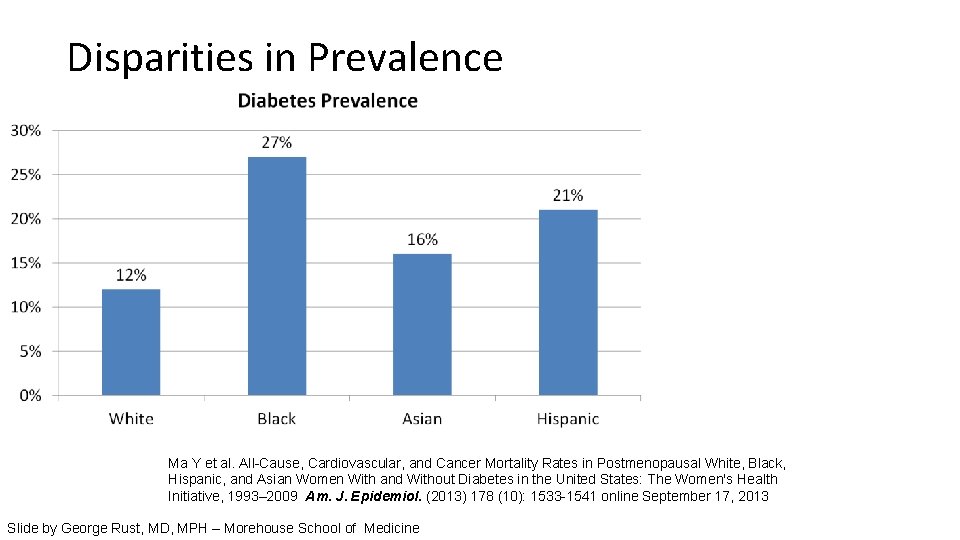
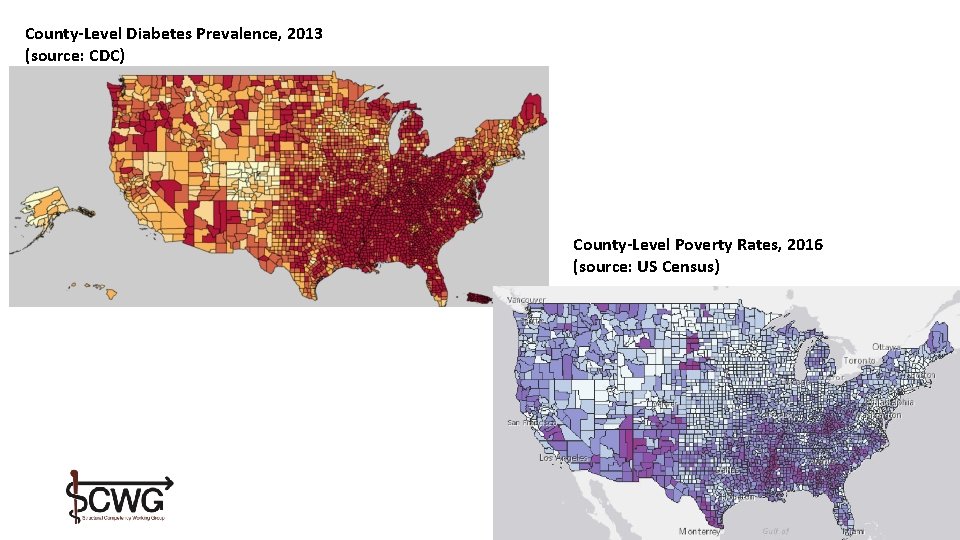
Disparities in Prevalence Ma Y et al. All-Cause, Cardiovascular, and Cancer Mortality Rates in Postmenopausal White, Black, Hispanic, and Asian Women With and Without Diabetes in the United States: The Women's Health Initiative, 1993– 2009 Am. J. Epidemiol. (2013) 178 (10): 1533 -1541 online September 17, 2013 Slide by George Rust, MD, MPH – Morehouse School of Medicine
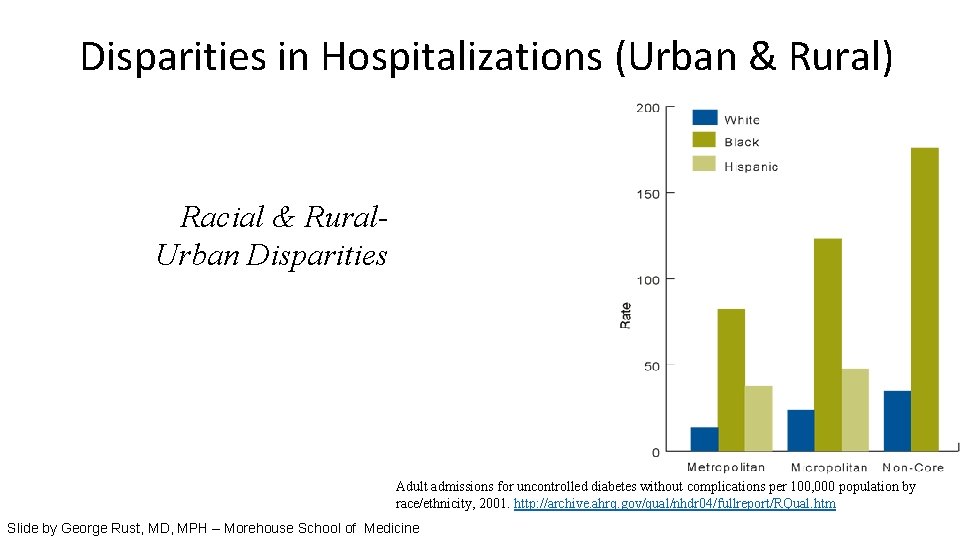
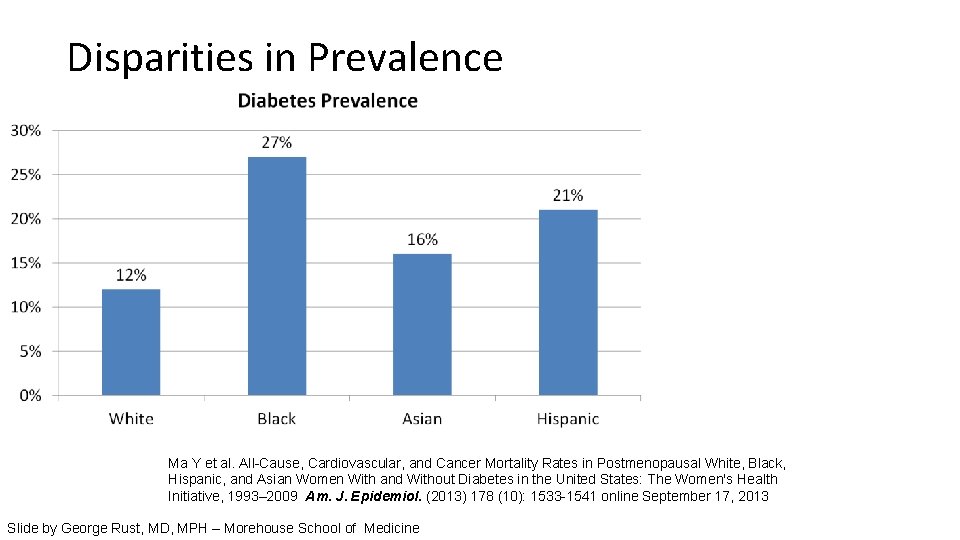
Disparities in Hospitalizations (Urban & Rural) Racial & Rural. Urban Disparities Adult admissions for uncontrolled diabetes without complications per 100, 000 population by race/ethnicity, 2001. http: //archive. ahrq. gov/qual/nhdr 04/fullreport/RQual. htm Slide by George Rust, MD, MPH – Morehouse School of Medicine
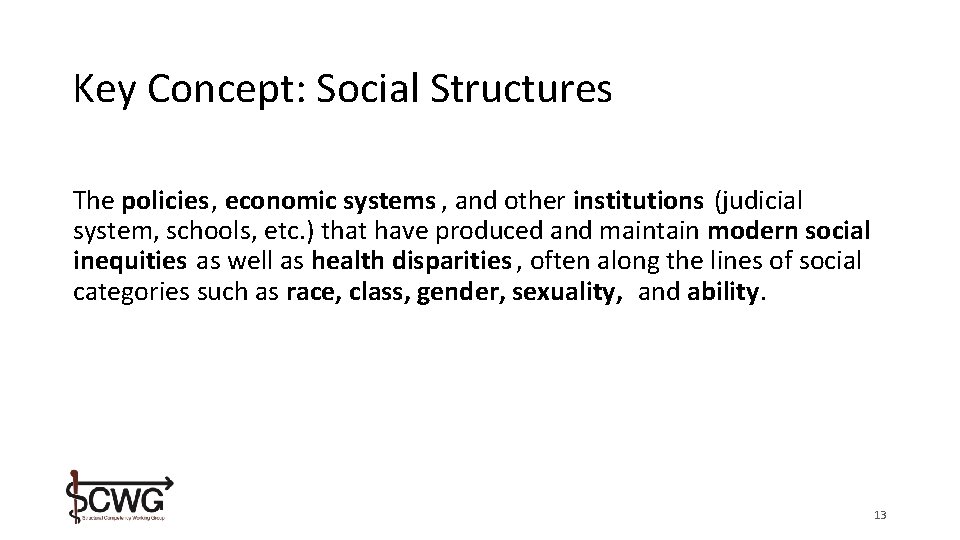
Key Concept: Social Structures The policies, economic systems , and other institutions (judicial system, schools, etc. ) that have produced and maintain modern social inequities as well as health disparities , often along the lines of social categories such as race, class, gender, sexuality, and ability. 13
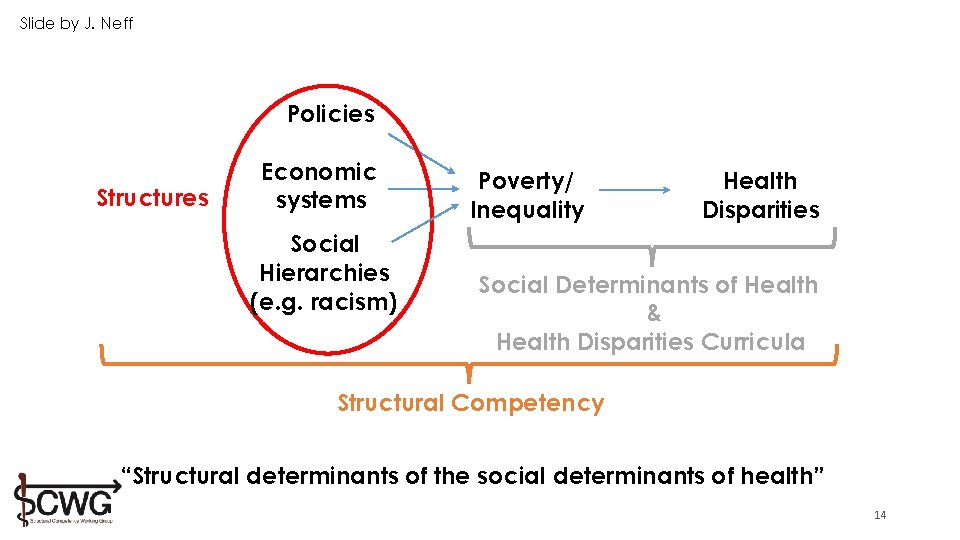
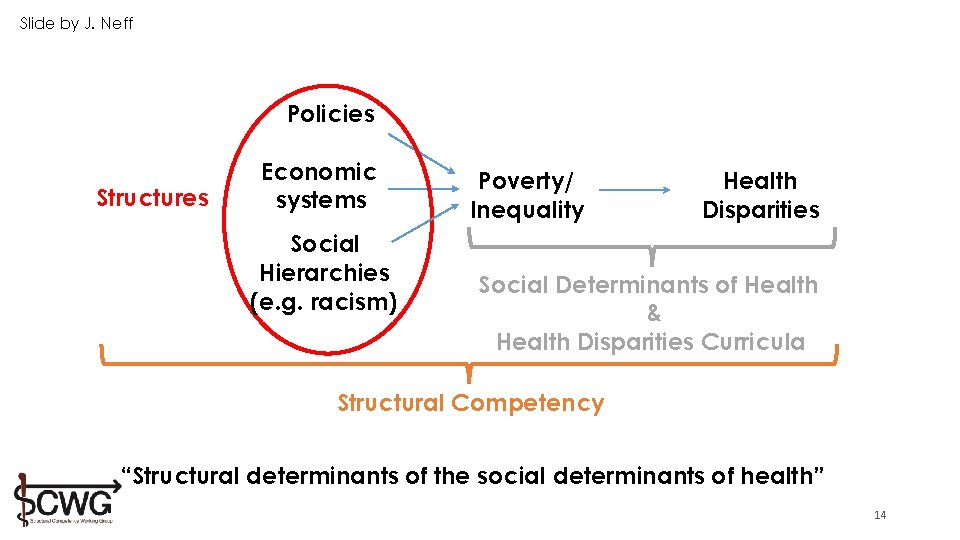
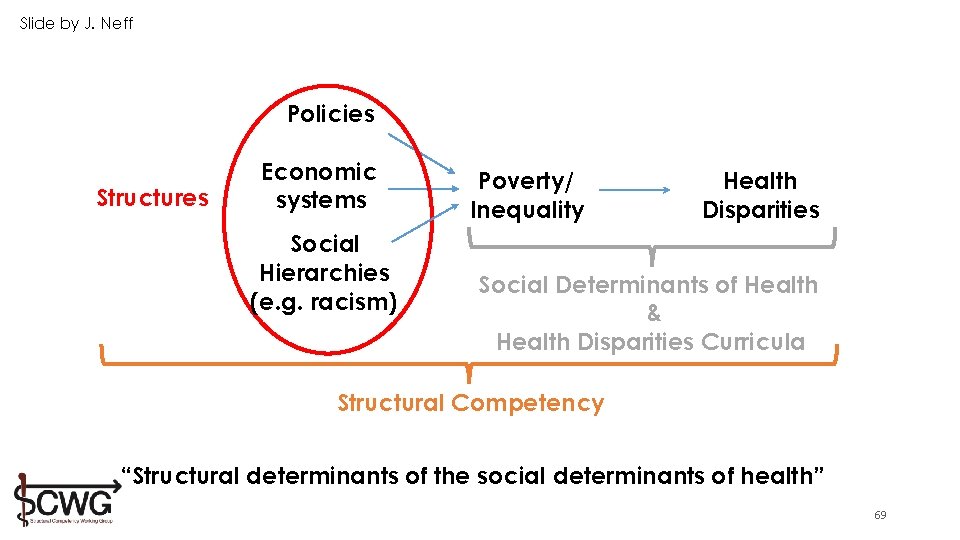
Slide by J. Neff Policies Structures Economic systems Social Hierarchies (e. g. racism) Poverty/ Inequality Health Disparities Social Determinants of Health & Health Disparities Curricula Structural Competency “Structural determinants of the social determinants of health” 14
If medicine is to fulfill her great task, then she must enter the political and social life. Do we not always find the diseases of the populace traceable to defects in society? —Rudolph Virchow, 1848
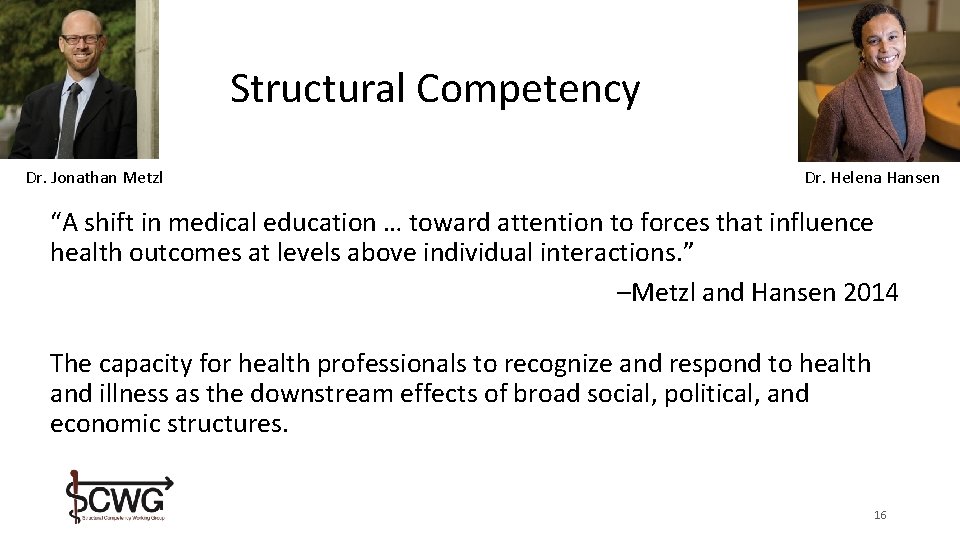
Structural Competency Dr. Jonathan Metzl Dr. Helena Hansen “A shift in medical education … toward attention to forces that influence health outcomes at levels above individual interactions. ” –Metzl and Hansen 2014 The capacity for health professionals to recognize and respond to health and illness as the downstream effects of broad social, political, and economic structures. 16
Structural Competency Develop trainees’ capacity in the following five areas: 1. Recognizing the influences of structures on patient health 2. Recognizing the influences of structures on the practice of healthcare 3. Responding to the influences of structures in the clinic 4. Responding to the influences of structures beyond the clinic 5. Approaching all of the above with structural humility -Neff, Knight, et al. 2017 17
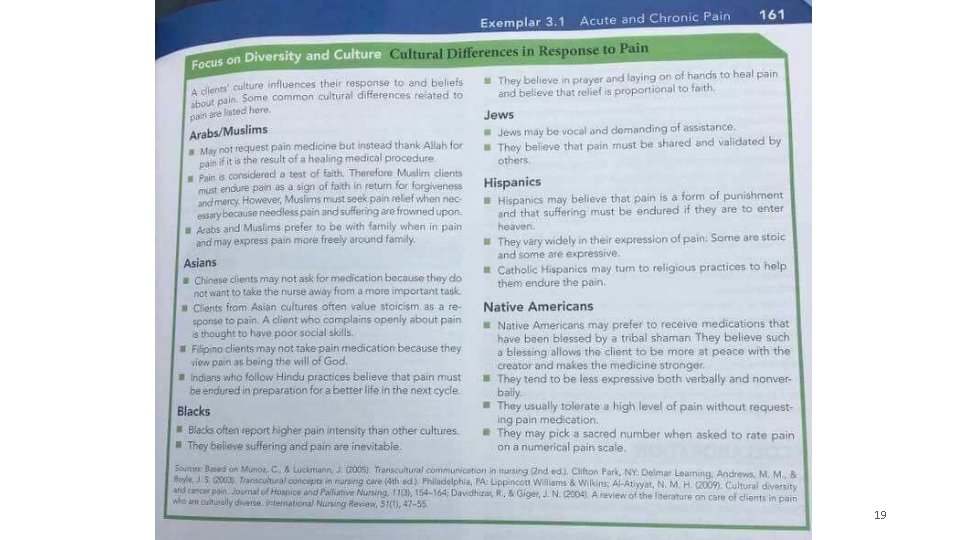
Cultural Competency • Motivation: Providers and patients can misunderstand one another if they have different understandings of illness and health • Cultural competency ideally helps providers to recognize that their own views are also culturally determined • But it often became “list of traits” to memorize about various cultural groups – but not about people of European descent/ white people 18
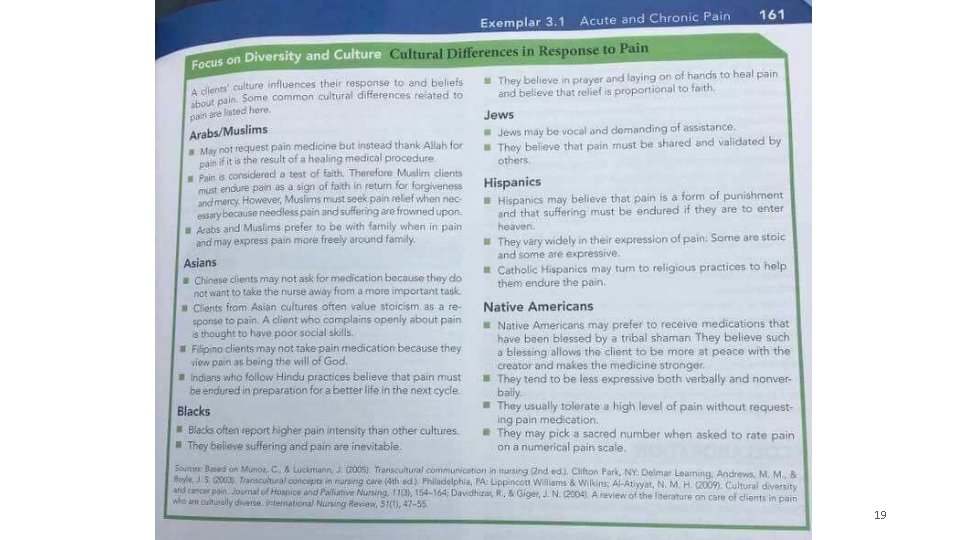
19
Cultural Humility • Developed out of a concern that some approaches to cultural competency were lists of stereotypes • “A commitment and active engagement in a lifelong process that individuals enter into on an ongoing basis with patients, communities, colleagues, and with themselves” —Tervalon and Murray-Garcia, 1998 • Emphasizes ongoing humility, self-reflection, self-critique, and lifelong learning
Structural Humility Structural humility cautions providers against making assumptions about the role of structures in patients' lives, instead encouraging collaboration with patients and communities in developing understanding of and responses to structural vulnerability. —Based on talk by Helena Hansen, April 2015 21
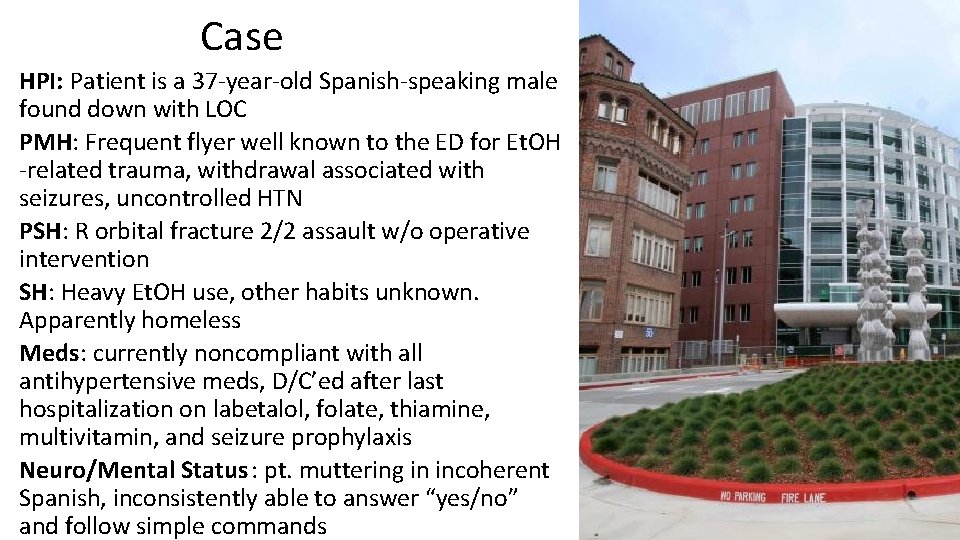
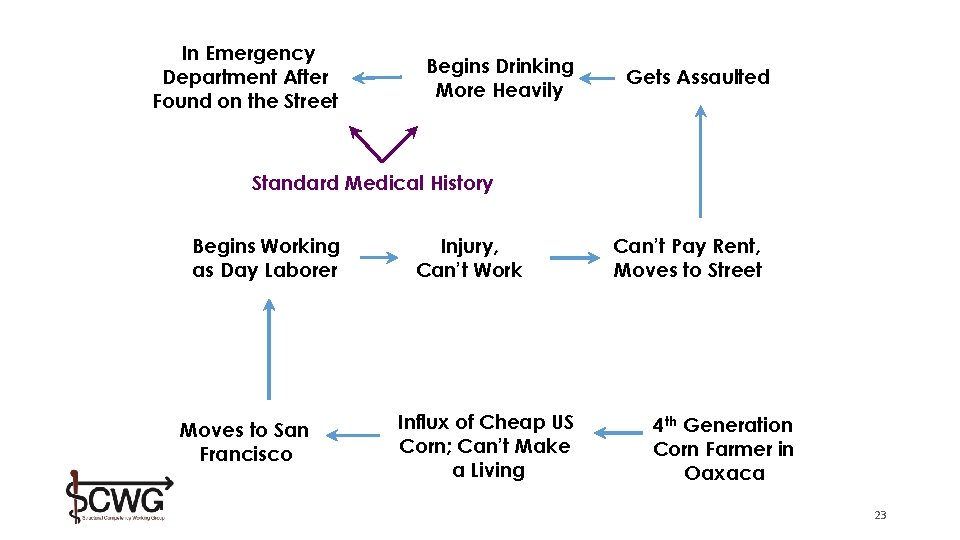
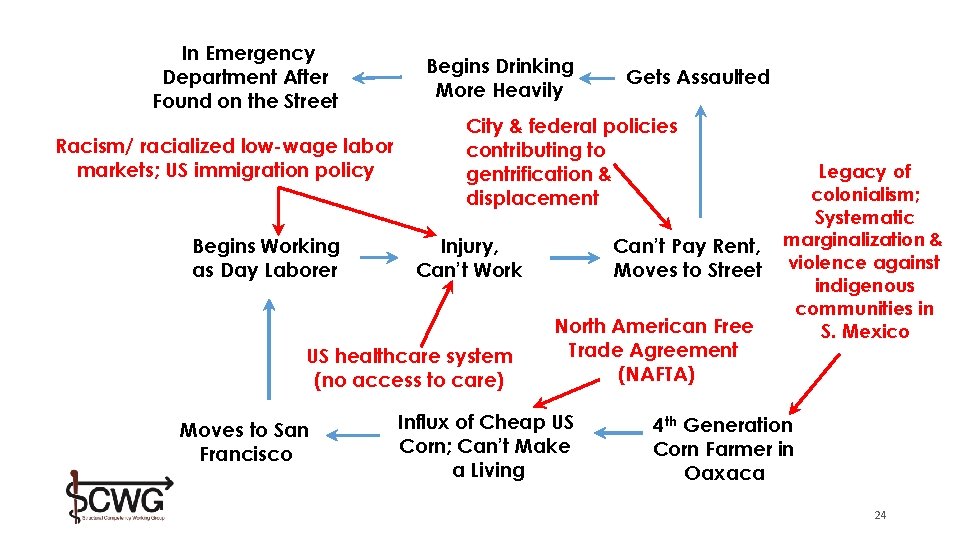
Case HPI: Patient is a 37 -year-old Spanish-speaking male found down with LOC PMH: Frequent flyer well known to the ED for Et. OH -related trauma, withdrawal associated with seizures, uncontrolled HTN PSH: R orbital fracture 2/2 assault w/o operative intervention SH: Heavy Et. OH use, other habits unknown. Apparently homeless Meds: currently noncompliant with all antihypertensive meds, D/C’ed after last hospitalization on labetalol, folate, thiamine, multivitamin, and seizure prophylaxis Neuro/Mental Status : pt. muttering in incoherent Spanish, inconsistently able to answer “yes/no” and follow simple commands 22
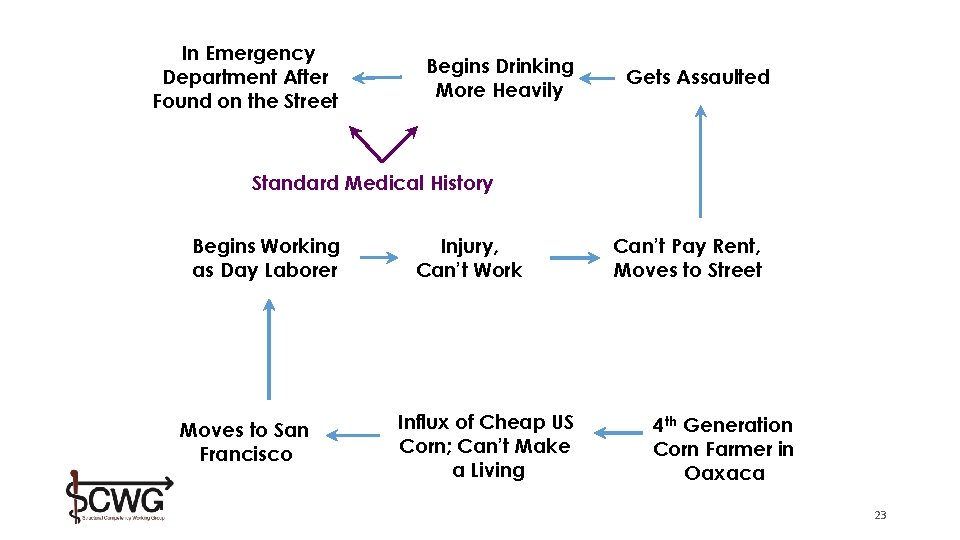
In Emergency Department After Found on the Street Begins Drinking More Heavily Gets Assaulted Standard Medical History Begins Working as Day Laborer Moves to San Francisco Injury, Can’t Work Influx of Cheap US Corn; Can’t Make a Living Can’t Pay Rent, Moves to Street 4 th Generation Corn Farmer in Oaxaca 23
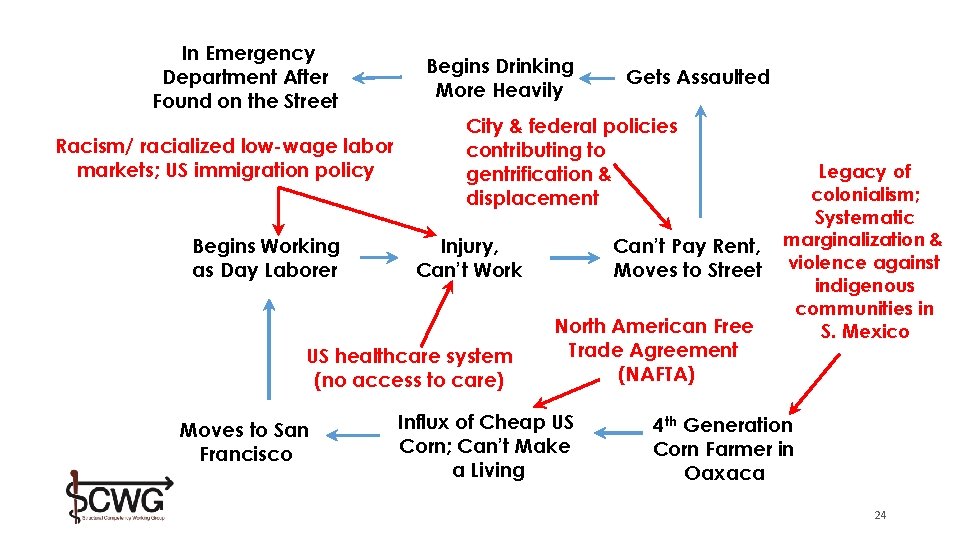
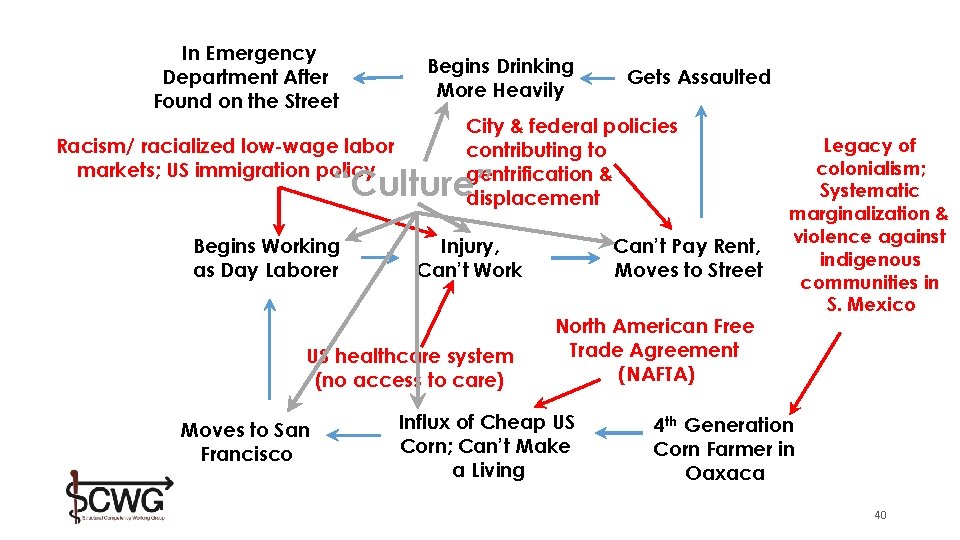
In Emergency Department After Found on the Street Racism/ racialized low-wage labor markets; US immigration policy Begins Working as Day Laborer Begins Drinking More Heavily City & federal policies contributing to gentrification & displacement Injury, Can’t Work US healthcare system (no access to care) Moves to San Francisco Gets Assaulted Can’t Pay Rent, Moves to Street North American Free Trade Agreement (NAFTA) Influx of Cheap US Corn; Can’t Make a Living Legacy of colonialism; Systematic marginalization & violence against indigenous communities in S. Mexico 4 th Generation Corn Farmer in Oaxaca 24
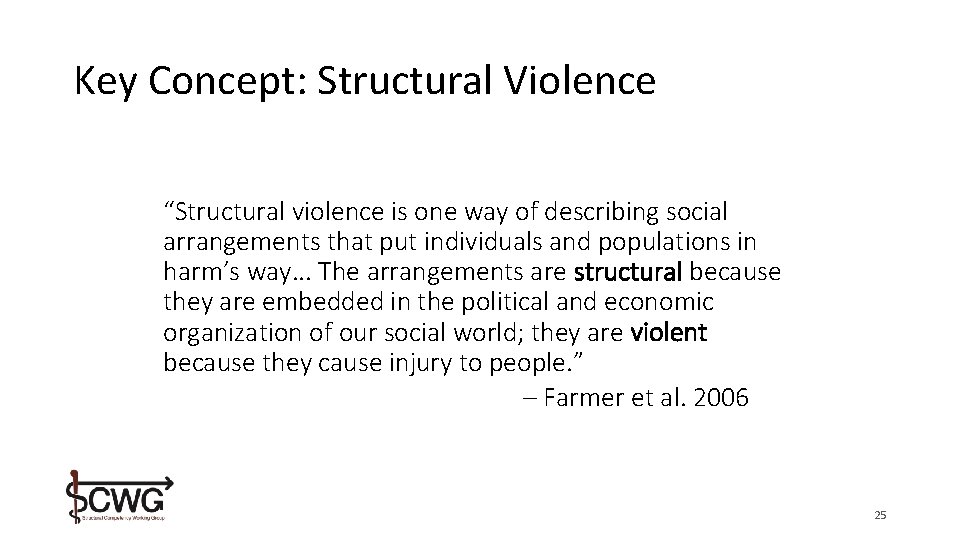
Key Concept: Structural Violence “Structural violence is one way of describing social arrangements that put individuals and populations in harm’s way. . . The arrangements are structural because they are embedded in the political and economic organization of our social world; they are violent because they cause injury to people. ” – Farmer et al. 2006 25
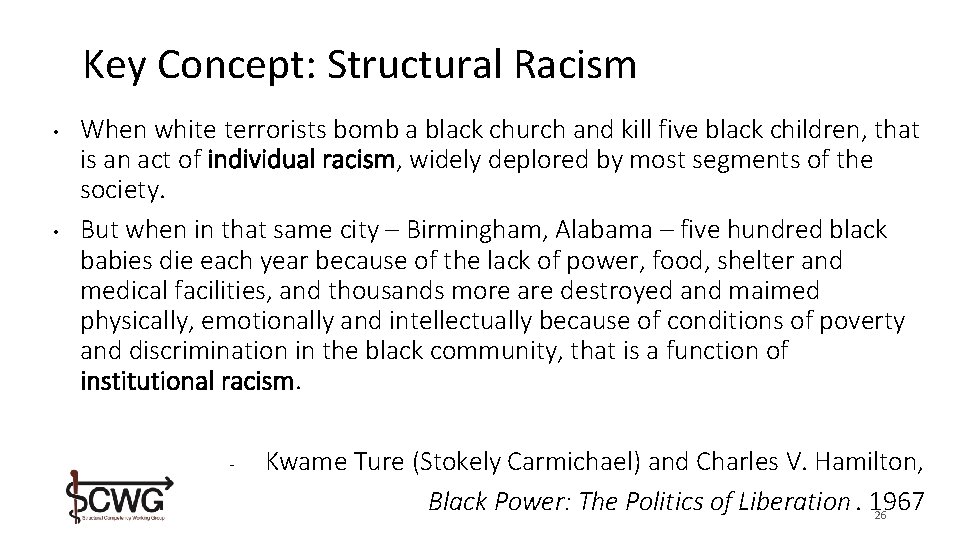
Key Concept: Structural Racism • • When white terrorists bomb a black church and kill five black children, that is an act of individual racism, widely deplored by most segments of the society. But when in that same city – Birmingham, Alabama – five hundred black babies die each year because of the lack of power, food, shelter and medical facilities, and thousands more are destroyed and maimed physically, emotionally and intellectually because of conditions of poverty and discrimination in the black community, that is a function of institutional racism. - Kwame Ture (Stokely Carmichael) and Charles V. Hamilton, Black Power: The Politics of Liberation. 1967 26
Key Concept: Structural Vulnerability The risk that an individual experiences as a result of structural violence – including their location in multiple socioeconomic hierarchies. Structural vulnerability is not caused by, nor can it be repaired solely by, individual agency or behaviors. 28
Structural Vulnerability • Framework for working and engaging with patients • Consider domains in which an individual is structurally vulnerable • Analogous to other health risk factors • Uses can be both: • Preventative medicine • Efficient, tailored and holistic treatment and healing
Assuming positive intent and giving the provider the benefit of the doubt: What are the factors that contributed to the provider seeing the patient in this way?
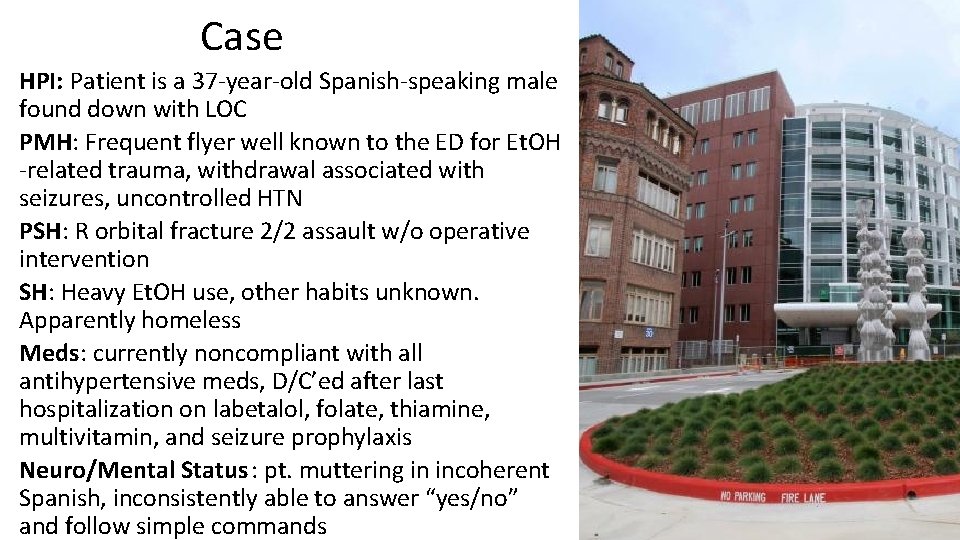
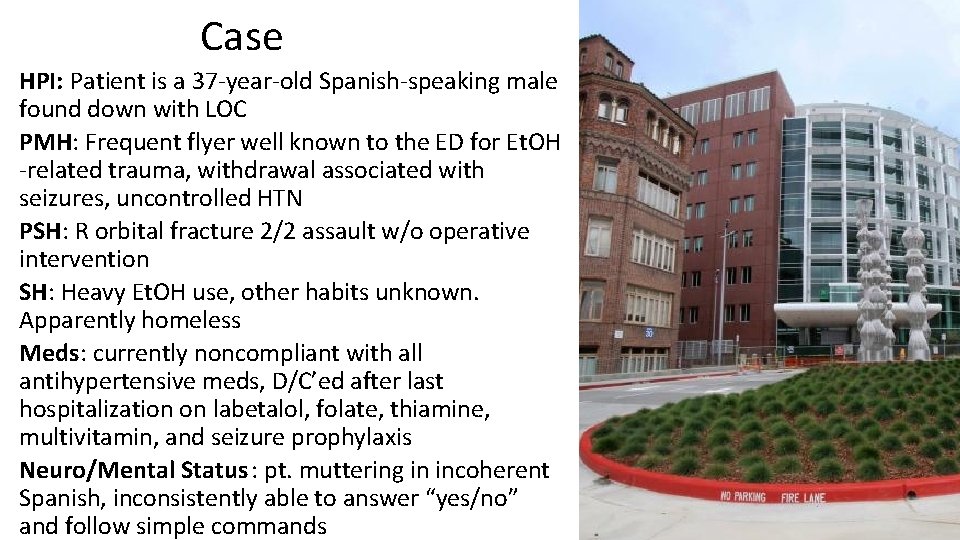
Case HPI: Patient is a 37 -year-old Spanish-speaking male found down with LOC PMH: Frequent flyer well known to the ED for Et. OH -related trauma, withdrawal associated with seizures, uncontrolled HTN PSH: R orbital fracture 2/2 assault w/o operative intervention SH: Heavy Et. OH use, other habits unknown. Apparently homeless Meds: currently noncompliant with all antihypertensive meds, D/C’ed after last hospitalization on labetalol, folate, thiamine, multivitamin, and seizure prophylaxis Neuro/Mental Status : pt. muttering in incoherent Spanish, inconsistently able to answer “yes/no” and follow simple commands 33
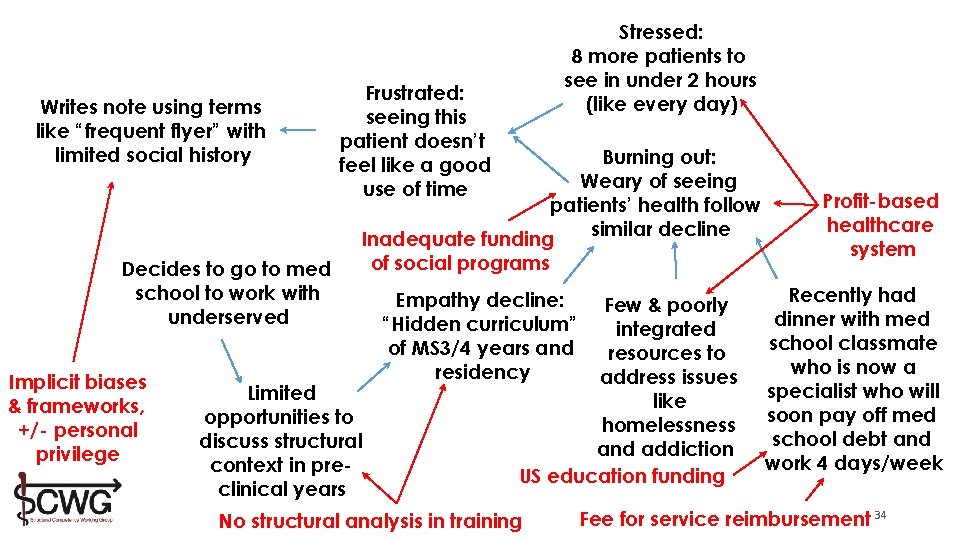
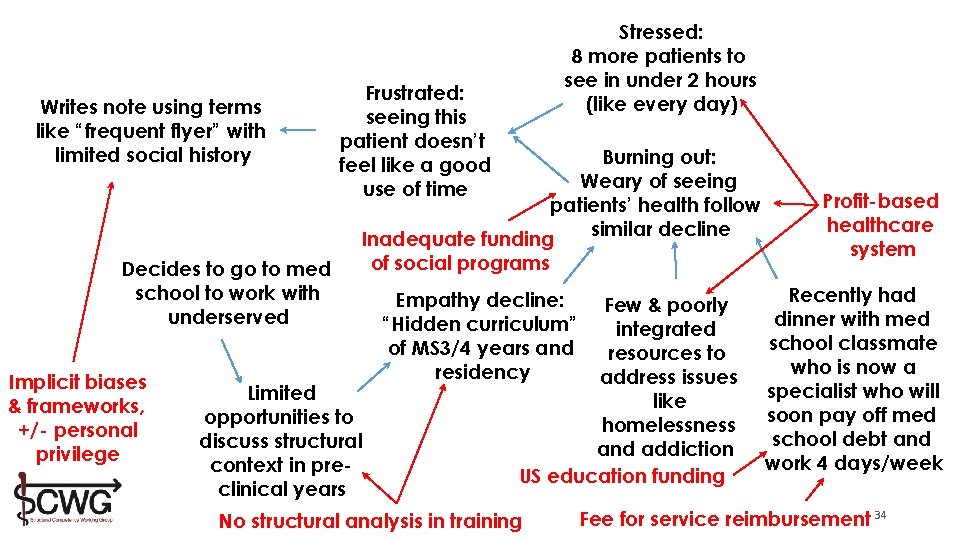
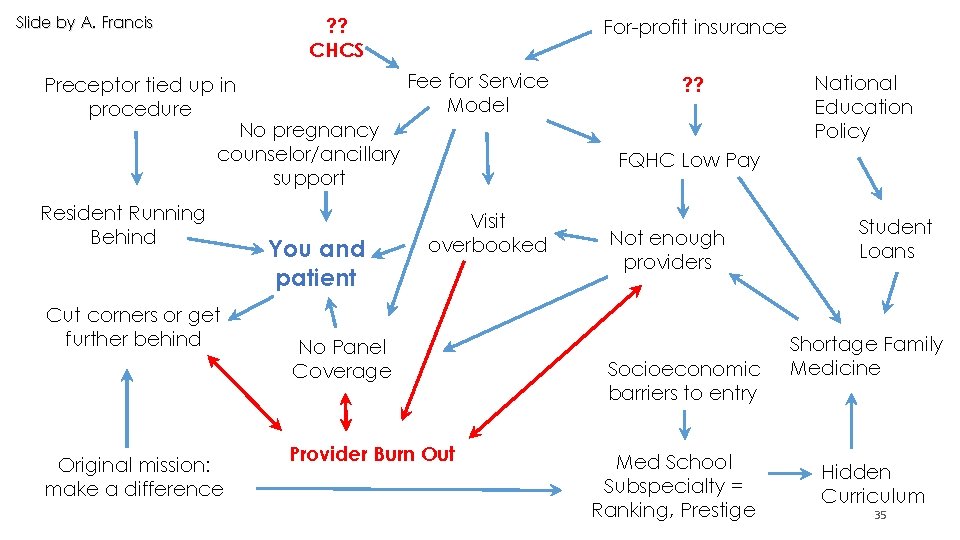
Writes note using terms like “frequent flyer” with limited social history Decides to go to med school to work with underserved Implicit biases & frameworks, +/- personal privilege Stressed: 8 more patients to see in under 2 hours (like every day) Frustrated: seeing this patient doesn’t feel like a good use of time Burning out: Weary of seeing patients’ health follow similar decline Inadequate funding of social programs Limited opportunities to discuss structural context in preclinical years Empathy decline: “Hidden curriculum” of MS 3/4 years and residency Few & poorly integrated resources to address issues like homelessness and addiction US education funding No structural analysis in training Profit-based healthcare system Recently had dinner with med school classmate who is now a specialist who will soon pay off med school debt and work 4 days/week Fee for service reimbursement 34
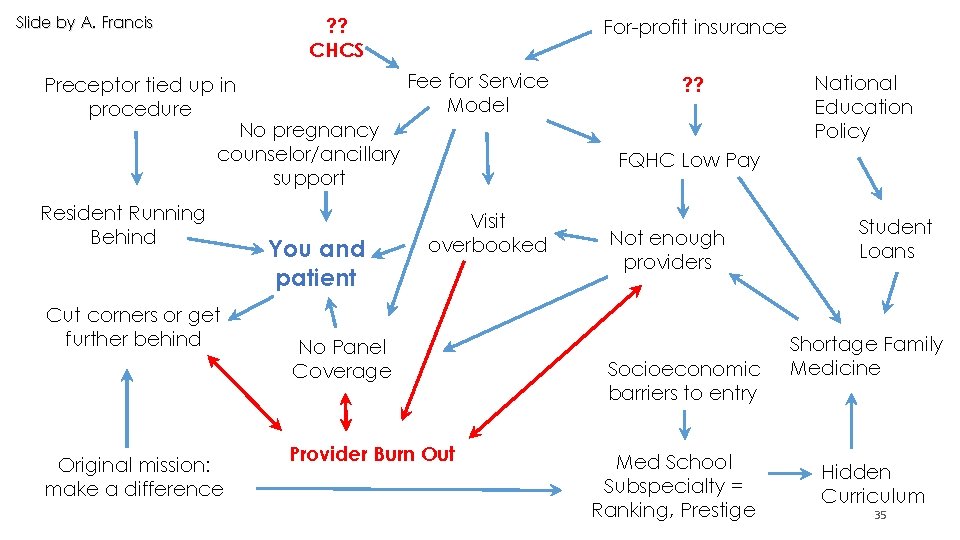
Slide by A. Francis ? ? CHCS For-profit insurance Fee for Service Model Preceptor tied up in procedure No pregnancy counselor/ancillary support Resident Running Behind Cut corners or get further behind Original mission: make a difference You and patient ? ? National Education Policy FQHC Low Pay Visit overbooked No Panel Coverage Provider Burn Out Not enough providers Socioeconomic barriers to entry Med School Subspecialty = Ranking, Prestige Student Loans Shortage Family Medicine Hidden Curriculum 35
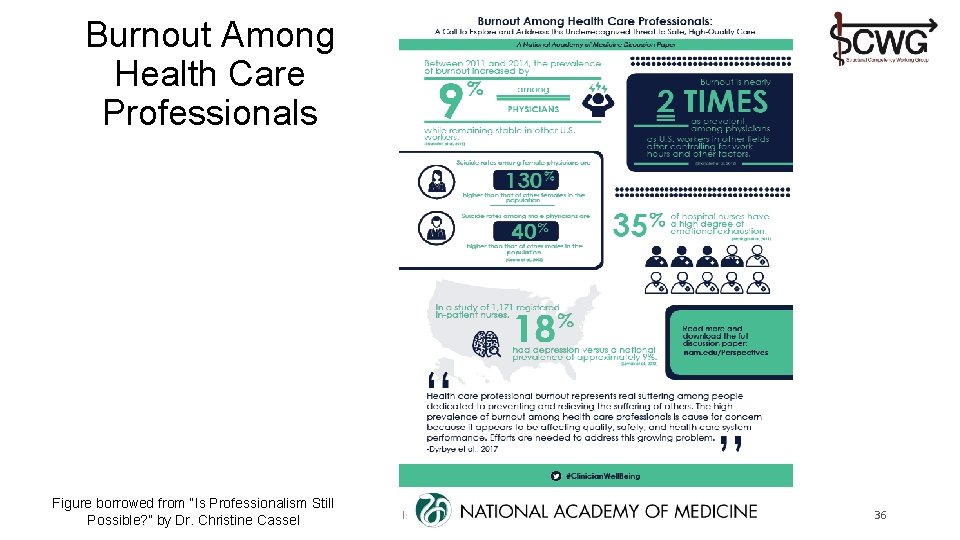
Burnout Among Health Care Professionals Figure borrowed from “Is Professionalism Still Possible? ” by Dr. Christine Cassel Is Professionalism Still Possible? 36
Why is there not more widespread discussion of structural violence and structural vulnerability in health and health care?
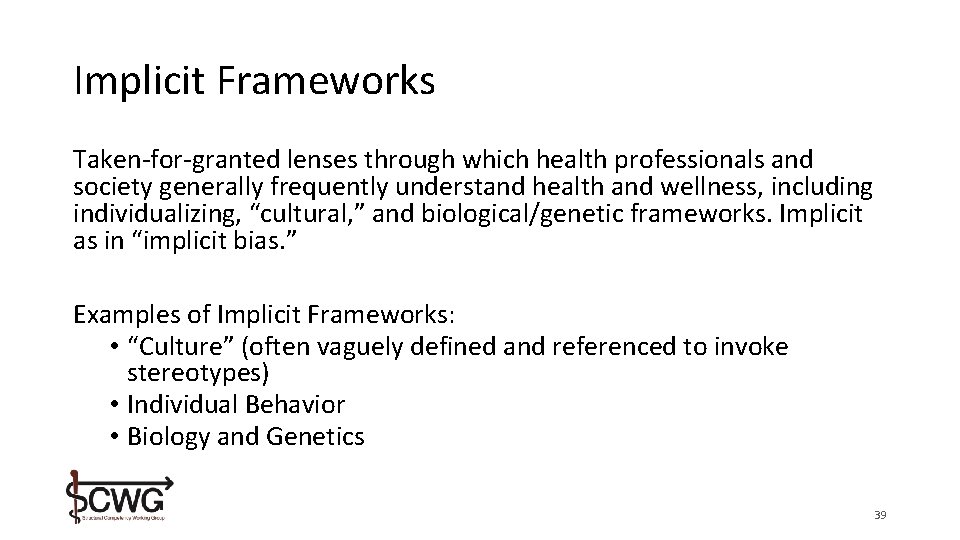
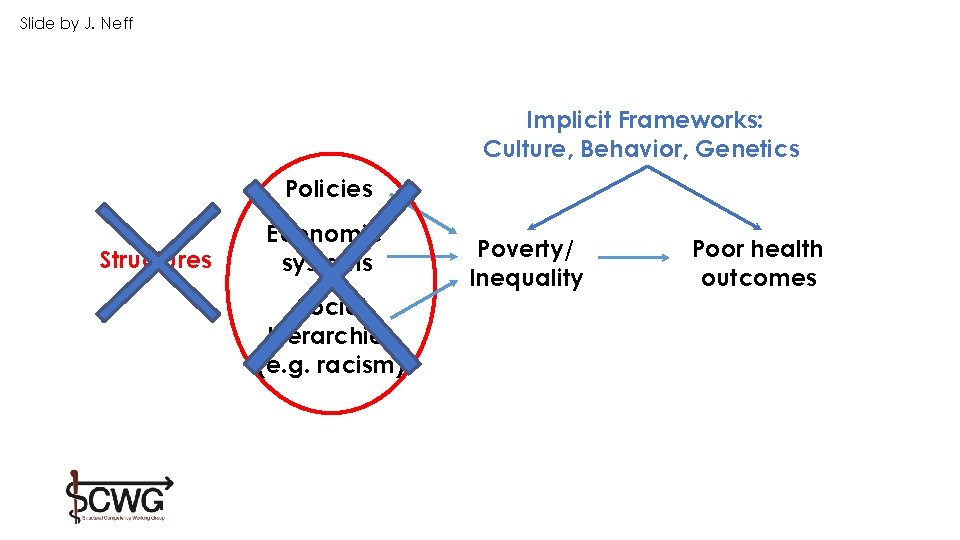
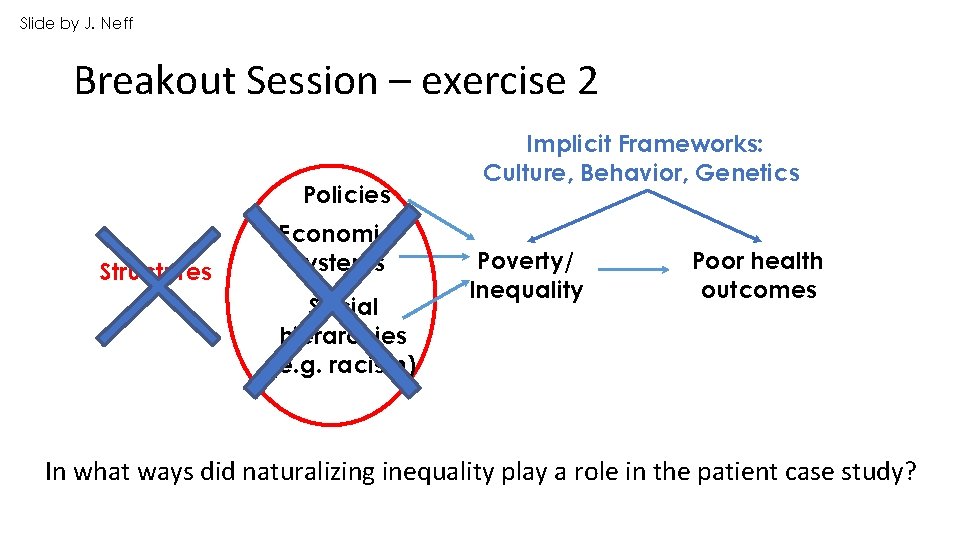
Naturalizing Inequality • The sometimes subtle, sometimes explicit, ways that structural violence is overlooked • Often through claims of cultural difference, behavioral shortcomings, or racial categories… which distract from the structural causes of harm • Operates through “Implicit Frameworks” 38
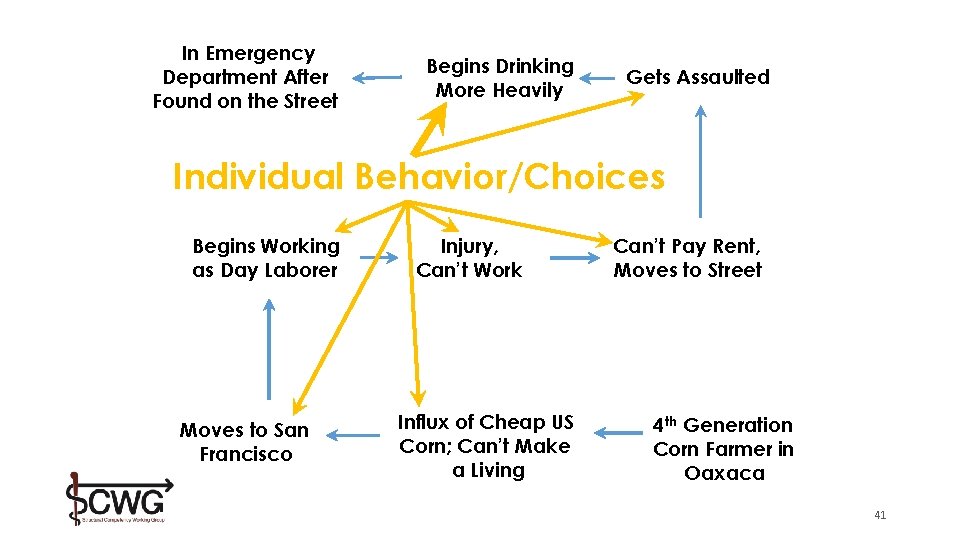
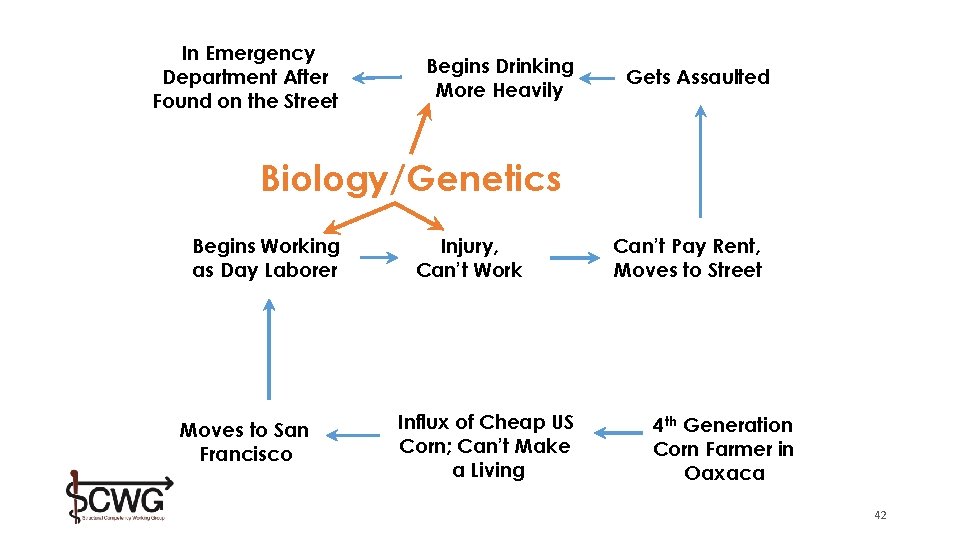
Implicit Frameworks Taken-for-granted lenses through which health professionals and society generally frequently understand health and wellness, including individualizing, “cultural, ” and biological/genetic frameworks. Implicit as in “implicit bias. ” Examples of Implicit Frameworks: • “Culture” (often vaguely defined and referenced to invoke stereotypes) • Individual Behavior • Biology and Genetics 39
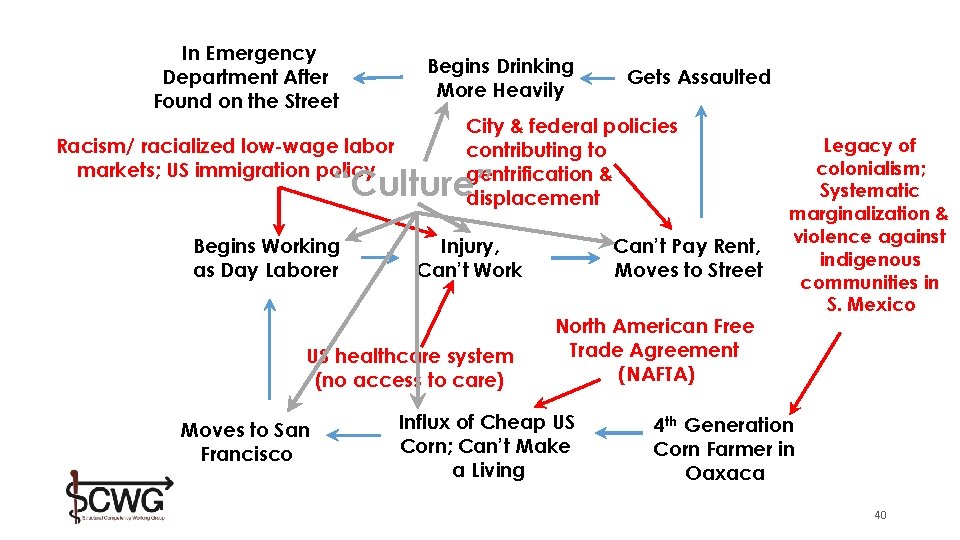
In Emergency Department After Found on the Street Racism/ racialized low-wage labor markets; US immigration policy Begins Drinking More Heavily Gets Assaulted City & federal policies contributing to gentrification & displacement “Culture” Begins Working as Day Laborer Injury, Can’t Work US healthcare system (no access to care) Moves to San Francisco Can’t Pay Rent, Moves to Street North American Free Trade Agreement (NAFTA) Influx of Cheap US Corn; Can’t Make a Living Legacy of colonialism; Systematic marginalization & violence against indigenous communities in S. Mexico 4 th Generation Corn Farmer in Oaxaca 40
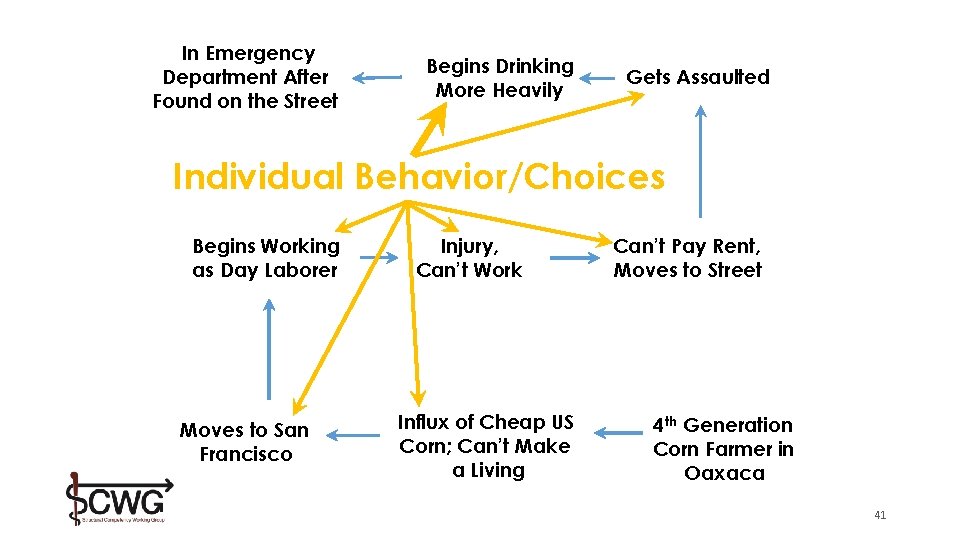
In Emergency Department After Found on the Street Begins Drinking More Heavily Gets Assaulted Individual Behavior/Choices Begins Working as Day Laborer Moves to San Francisco Injury, Can’t Work Influx of Cheap US Corn; Can’t Make a Living Can’t Pay Rent, Moves to Street 4 th Generation Corn Farmer in Oaxaca 41
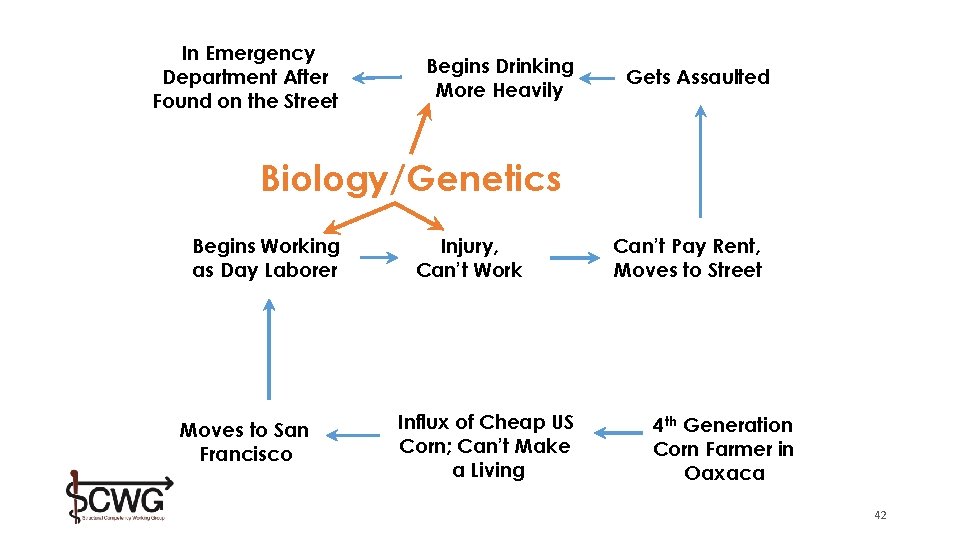
In Emergency Department After Found on the Street Begins Drinking More Heavily Gets Assaulted Biology/Genetics Begins Working as Day Laborer Moves to San Francisco Injury, Can’t Work Influx of Cheap US Corn; Can’t Make a Living Can’t Pay Rent, Moves to Street 4 th Generation Corn Farmer in Oaxaca 42
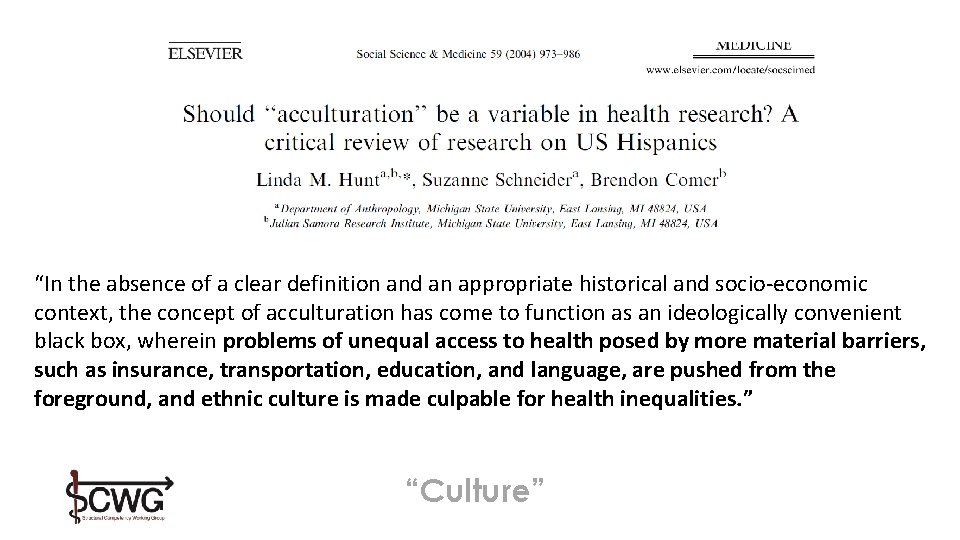
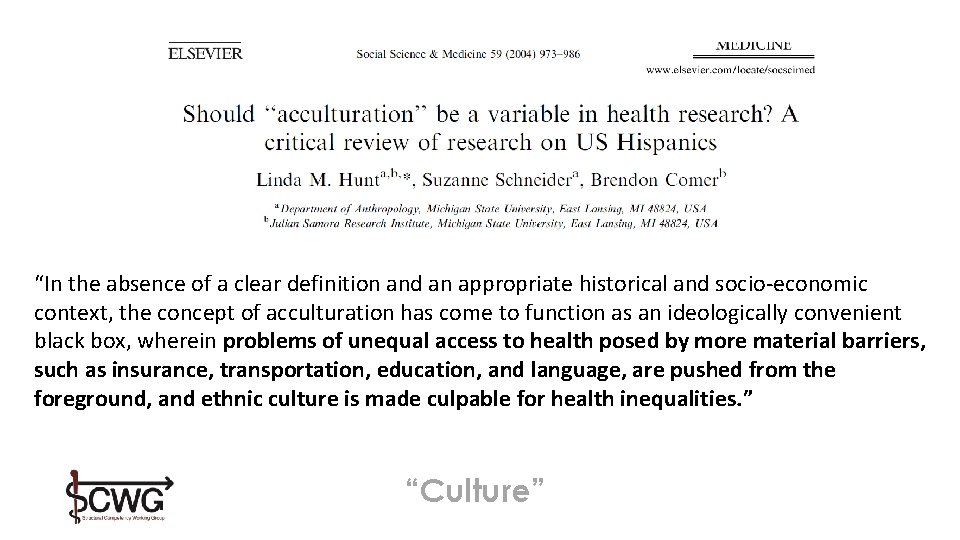
“In the absence of a clear definition and an appropriate historical and socio-economic context, the concept of acculturation has come to function as an ideologically convenient black box, wherein problems of unequal access to health posed by more material barriers, such as insurance, transportation, education, and language, are pushed from the foreground, and ethnic culture is made culpable for health inequalities. ” “Culture”
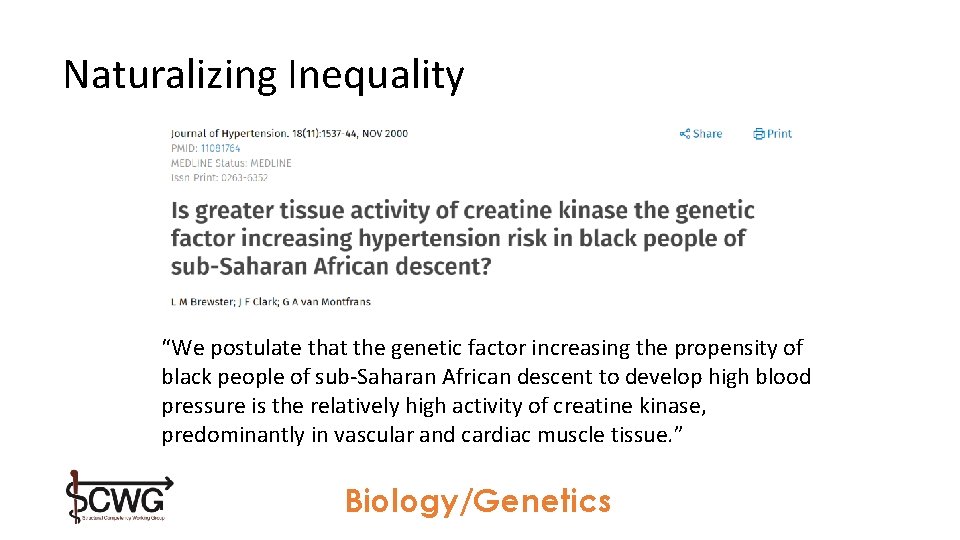
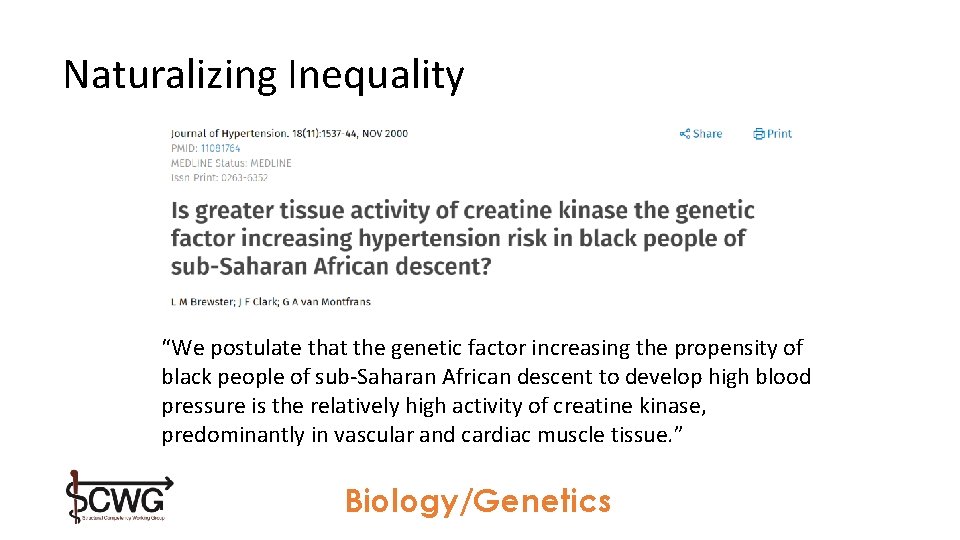
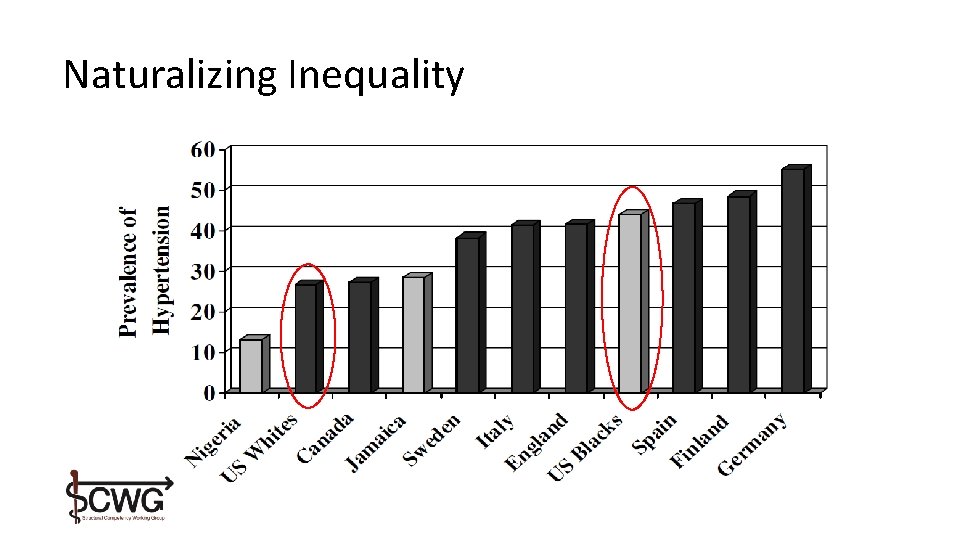
Naturalizing Inequality “We postulate that the genetic factor increasing the propensity of black people of sub-Saharan African descent to develop high blood pressure is the relatively high activity of creatine kinase, predominantly in vascular and cardiac muscle tissue. ” Biology/Genetics
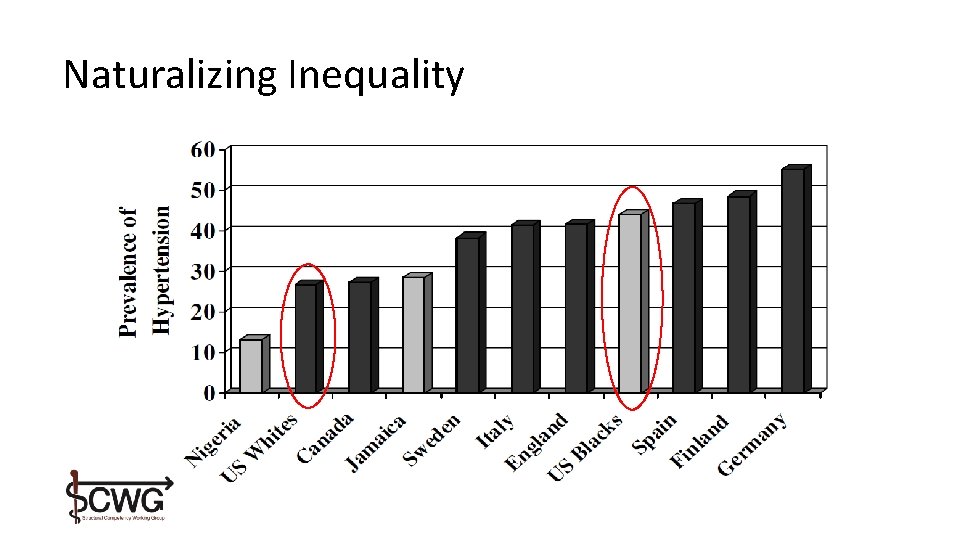
Naturalizing Inequality
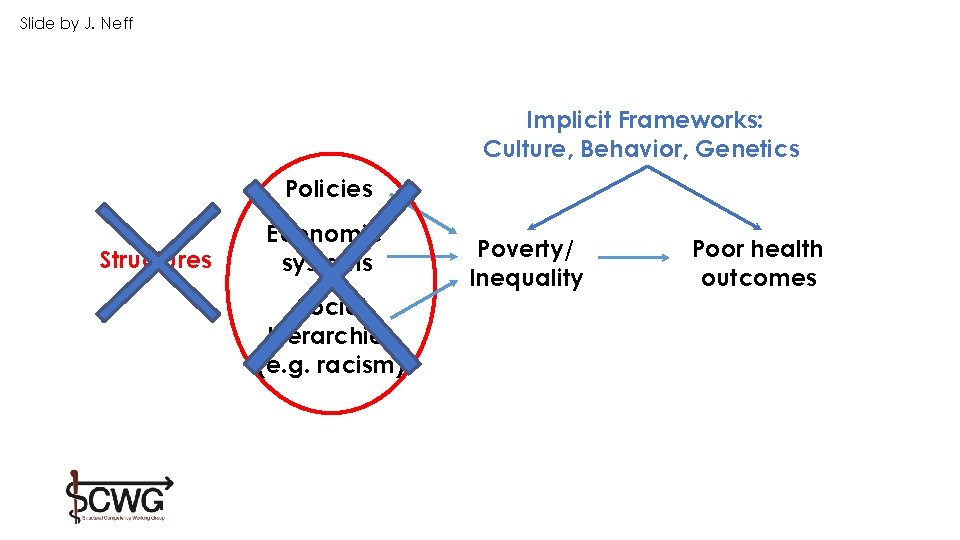
Slide by J. Neff Implicit Frameworks: Culture, Behavior, Genetics Policies Structures Economic systems Social hierarchies (e. g. racism) Poverty/ Inequality Poor health outcomes
Three principles of action (1) Improve the conditions of daily life (2) Tackle the inequitable distribution of power, money, and resources (3) Measure the problem, evaluate action, expand the knowledge base, develop a workforce trained in social [and structural] determinants of health Marmot, M. et al. (2008). Closing the gap in a generation: health equity through social action on the social determinants of health. Lancet, 372, 1661 -1669. 48
Breakout Session
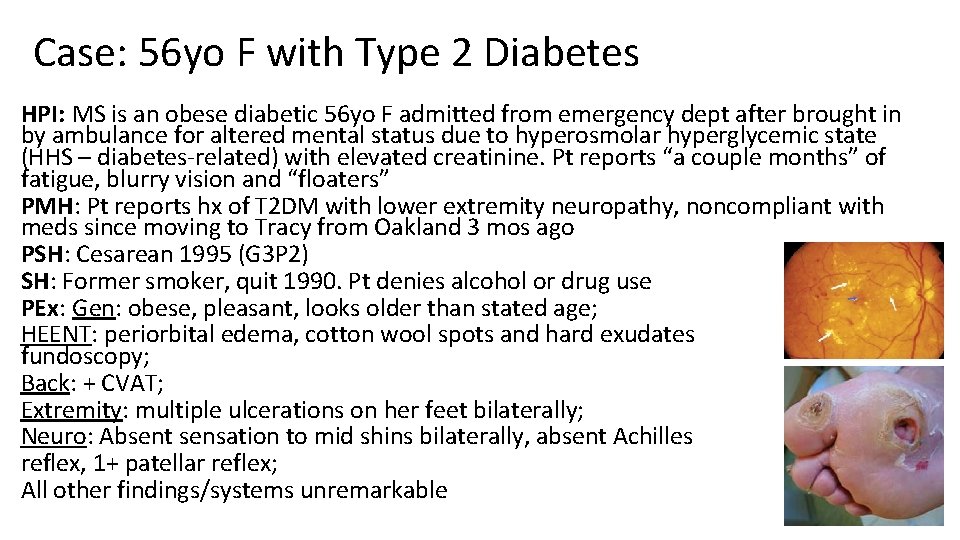
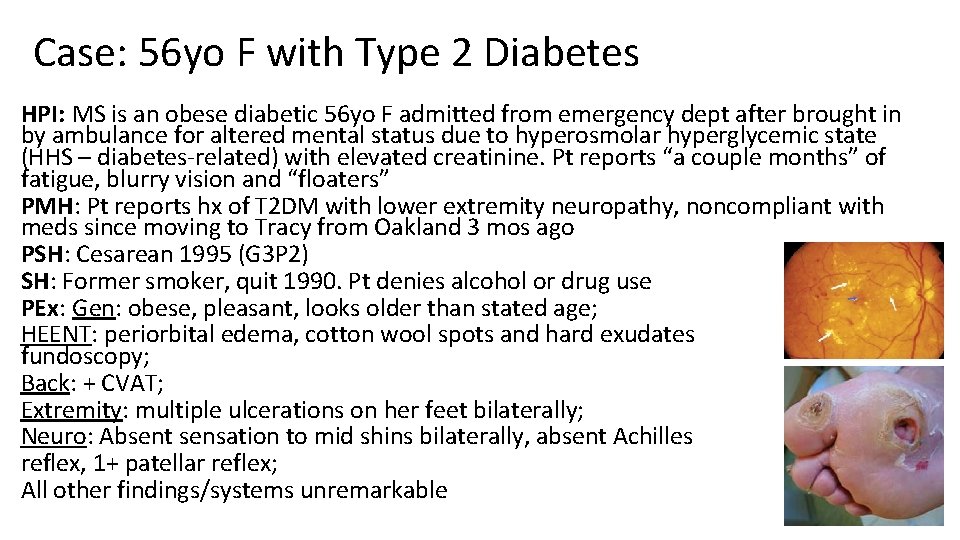
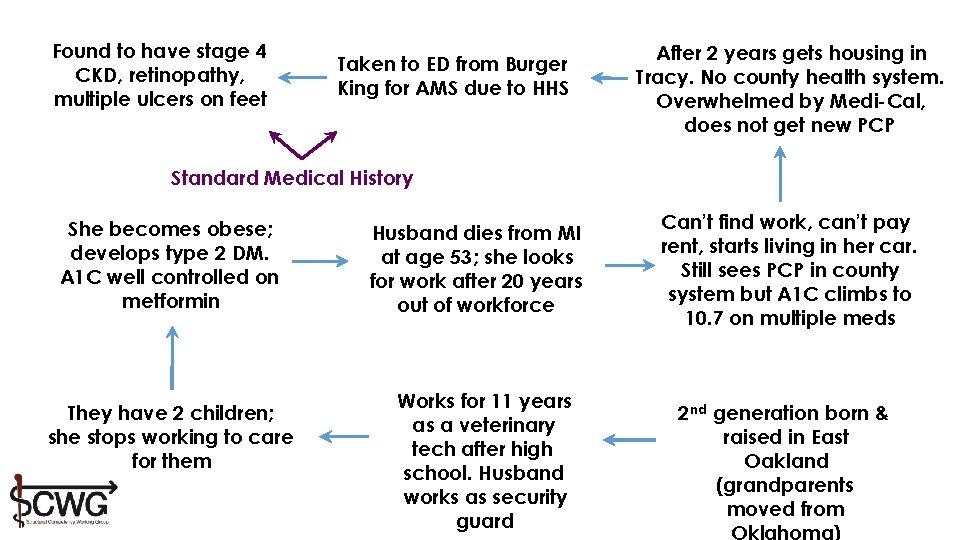
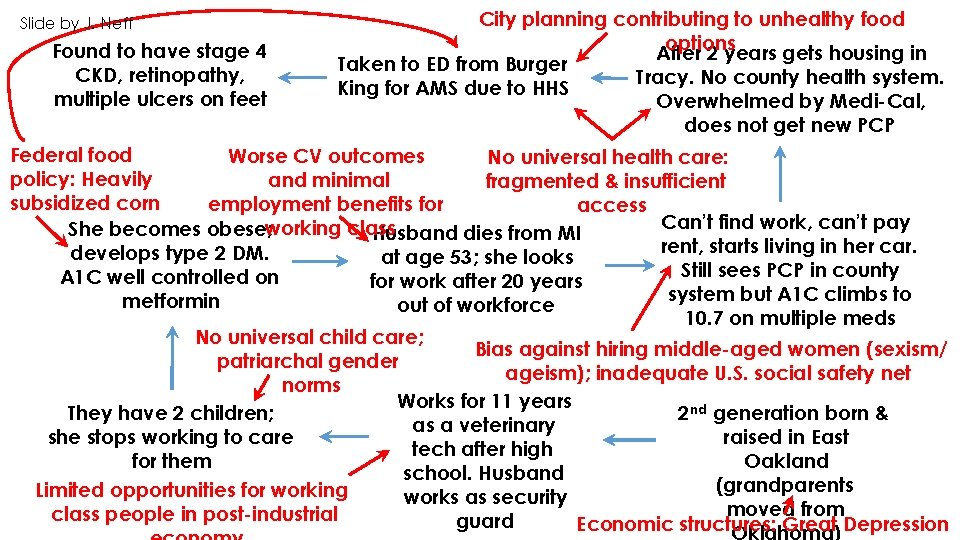
Case: 56 yo F with Type 2 Diabetes HPI: MS is an obese diabetic 56 yo F admitted from emergency dept after brought in by ambulance for altered mental status due to hyperosmolar hyperglycemic state (HHS – diabetes-related) with elevated creatinine. Pt reports “a couple months” of fatigue, blurry vision and “floaters” PMH: Pt reports hx of T 2 DM with lower extremity neuropathy, noncompliant with meds since moving to Tracy from Oakland 3 mos ago PSH: Cesarean 1995 (G 3 P 2) SH: Former smoker, quit 1990. Pt denies alcohol or drug use PEx: Gen: obese, pleasant, looks older than stated age; HEENT: periorbital edema, cotton wool spots and hard exudates on fundoscopy; Back: + CVAT; Extremity: multiple ulcerations on her feet bilaterally; Neuro: Absent sensation to mid shins bilaterally, absent Achilles reflex, 1+ patellar reflex; All other findings/systems unremarkable
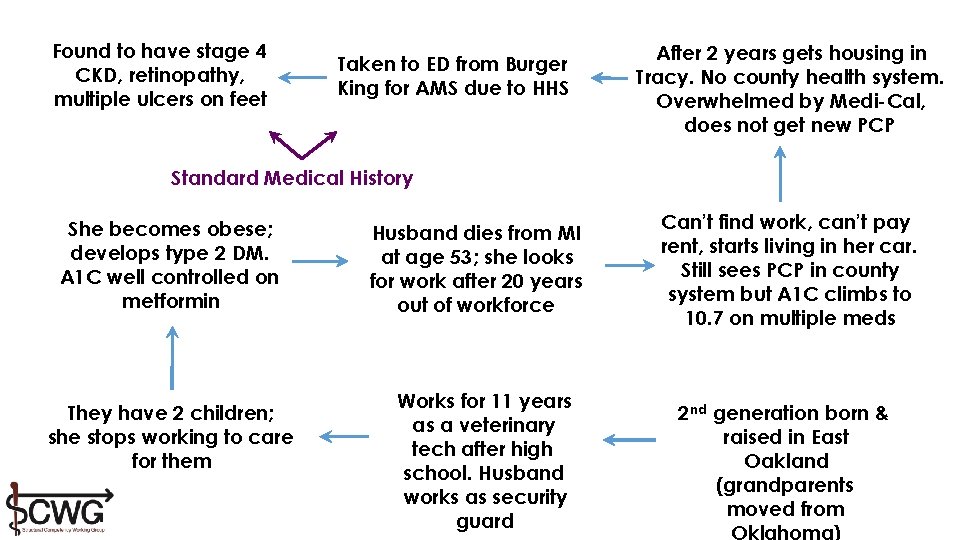
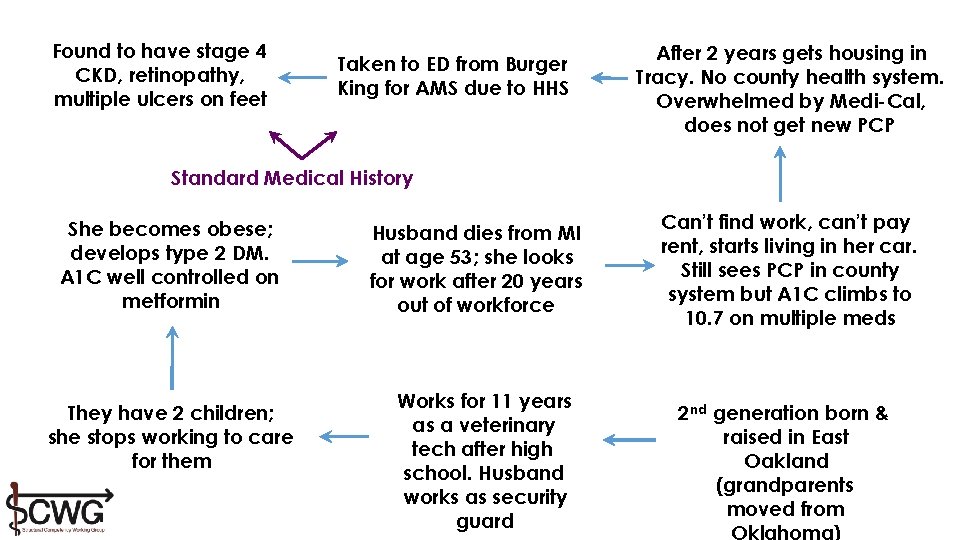
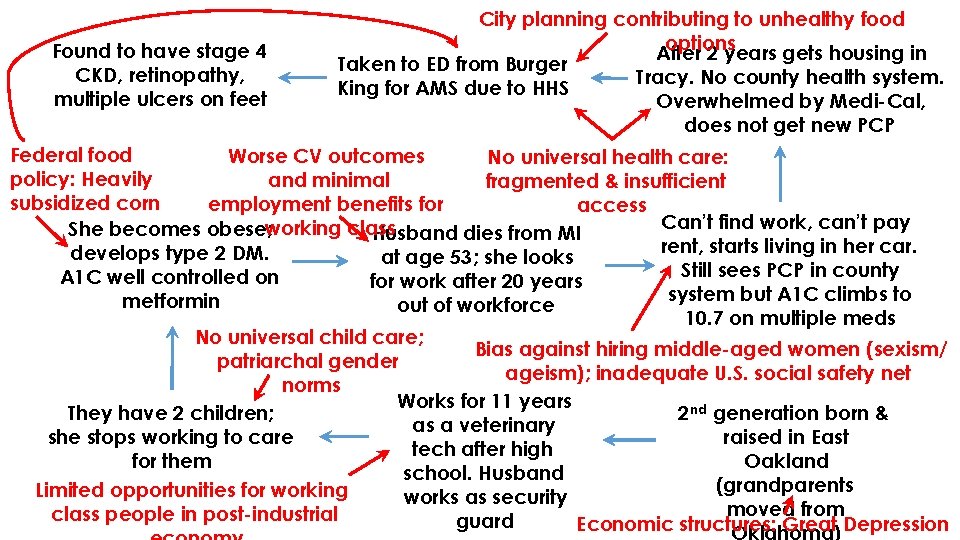
Found to have stage 4 CKD, retinopathy, multiple ulcers on feet Taken to ED from Burger King for AMS due to HHS After 2 years gets housing in Tracy. No county health system. Overwhelmed by Medi-Cal, does not get new PCP Standard Medical History She becomes obese; develops type 2 DM. A 1 C well controlled on metformin They have 2 children; she stops working to care for them Husband dies from MI at age 53; she looks for work after 20 years out of workforce Works for 11 years as a veterinary tech after high school. Husband works as security guard Can’t find work, can’t pay rent, starts living in her car. Still sees PCP in county system but A 1 C climbs to 10. 7 on multiple meds 2 nd generation born & raised in East Oakland (grandparents moved from
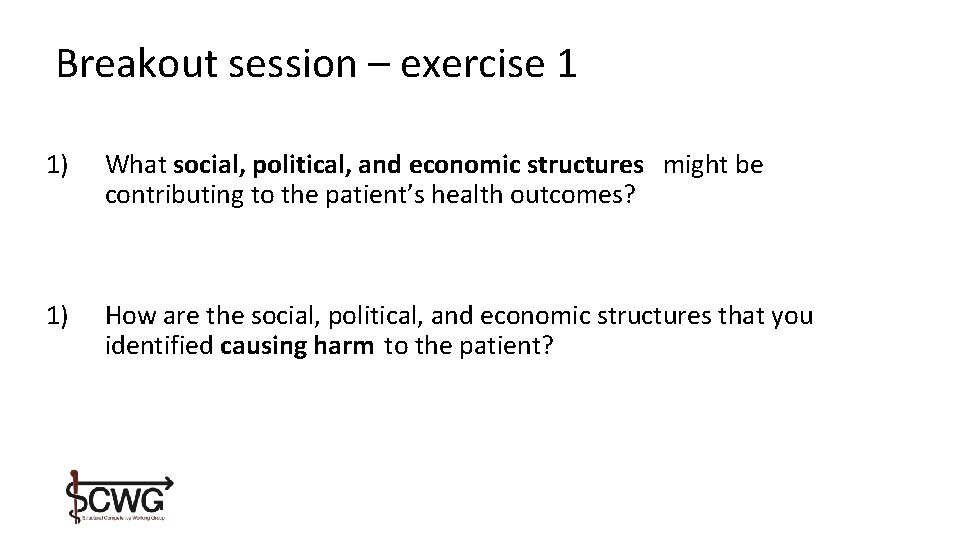
Breakout session – exercise 1 1) What social, political, and economic structures might be contributing to the patient’s health outcomes? 1) How are the social, political, and economic structures that you identified causing harm to the patient?
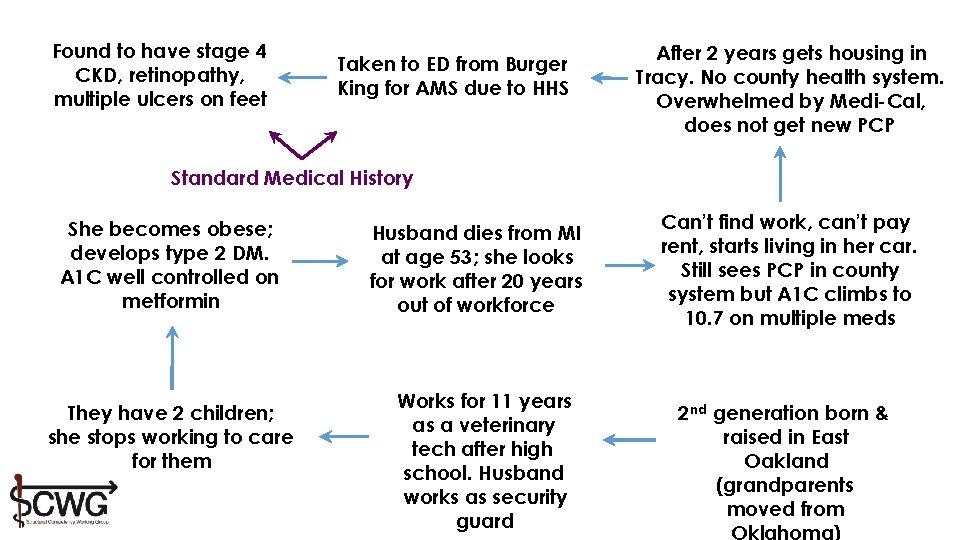
Found to have stage 4 CKD, retinopathy, multiple ulcers on feet Taken to ED from Burger King for AMS due to HHS After 2 years gets housing in Tracy. No county health system. Overwhelmed by Medi-Cal, does not get new PCP Standard Medical History She becomes obese; develops type 2 DM. A 1 C well controlled on metformin They have 2 children; she stops working to care for them Husband dies from MI at age 53; she looks for work after 20 years out of workforce Works for 11 years as a veterinary tech after high school. Husband works as security guard Can’t find work, can’t pay rent, starts living in her car. Still sees PCP in county system but A 1 C climbs to 10. 7 on multiple meds 2 nd generation born & raised in East Oakland (grandparents moved from
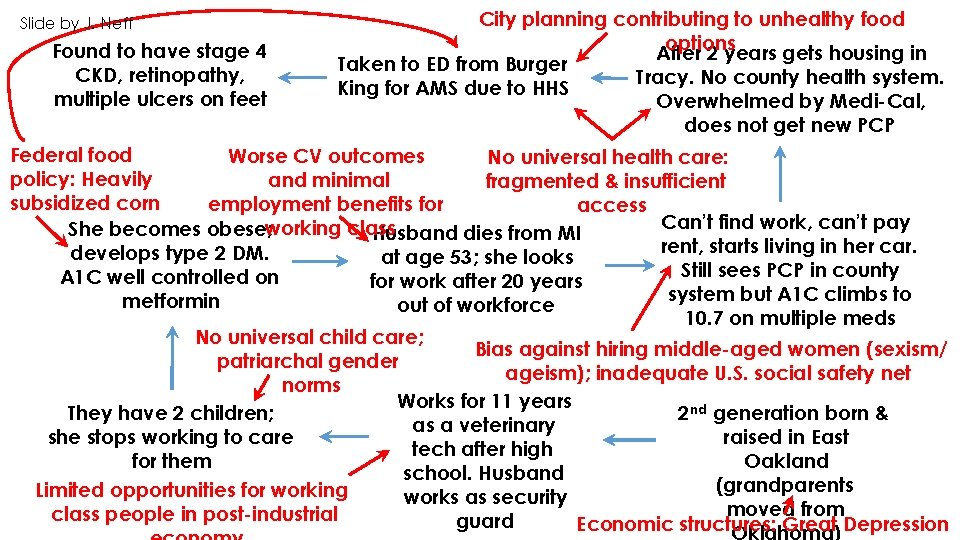
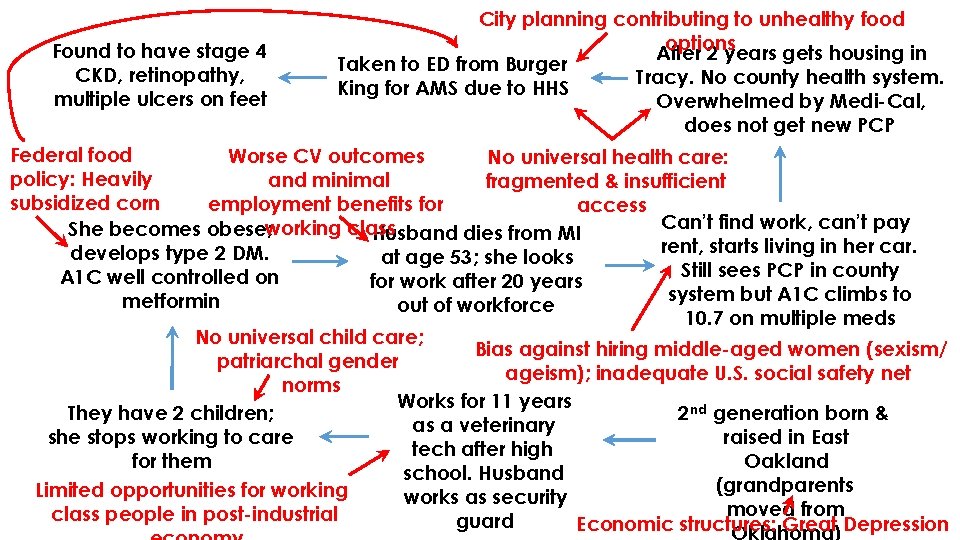
Slide by J. Neff Found to have stage 4 CKD, retinopathy, multiple ulcers on feet City planning contributing to unhealthy food options After 2 years gets housing in Taken to ED from Burger Tracy. No county health system. King for AMS due to HHS Overwhelmed by Medi-Cal, does not get new PCP Federal food Worse CV outcomes No universal health care: policy: Heavily and minimal fragmented & insufficient subsidized corn employment benefits for access Can’t find work, can’t pay She becomes obese; working class Husband dies from MI rent, starts living in her car. develops type 2 DM. at age 53; she looks Still sees PCP in county A 1 C well controlled on for work after 20 years system but A 1 C climbs to metformin out of workforce 10. 7 on multiple meds No universal child care; Bias against hiring middle-aged women (sexism/ patriarchal gender ageism); inadequate U. S. social safety net norms Works for 11 years 2 nd generation born & They have 2 children; as a veterinary raised in East she stops working to care tech after high Oakland for them school. Husband (grandparents Limited opportunities for working works as security moved from class people in post-industrial guard Economic structures: Great Depression
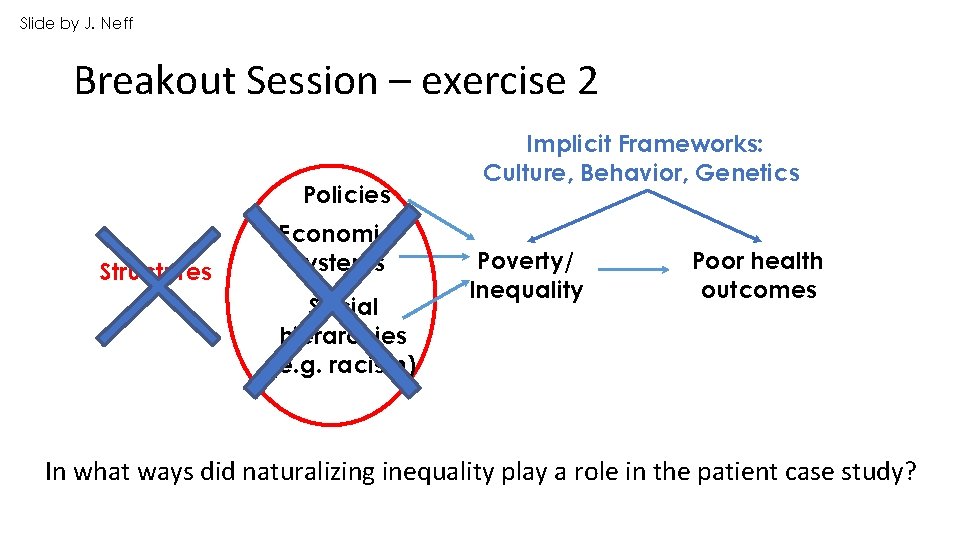
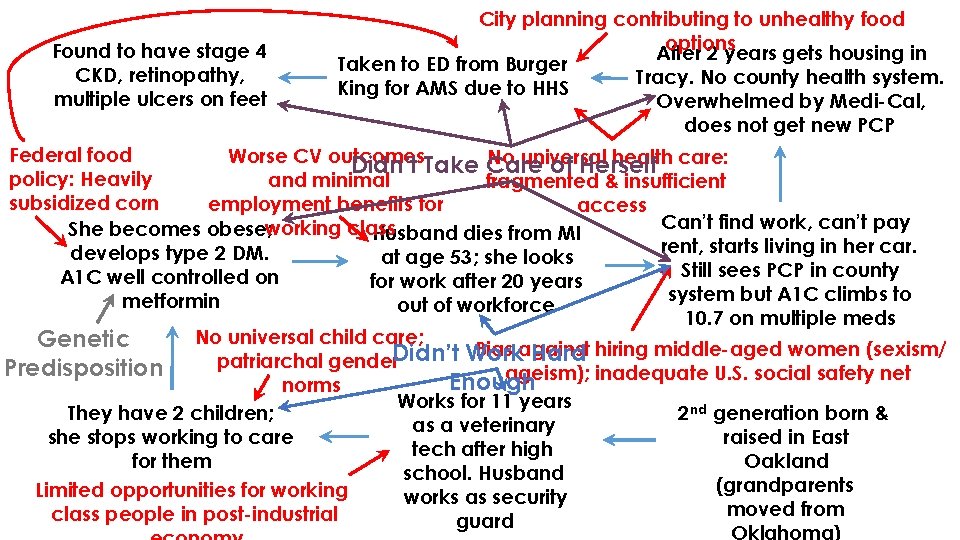
Slide by J. Neff Breakout Session – exercise 2 Policies Structures Economic systems Social hierarchies (e. g. racism) Implicit Frameworks: Culture, Behavior, Genetics Poverty/ Inequality Poor health outcomes In what ways did naturalizing inequality play a role in the patient case study?
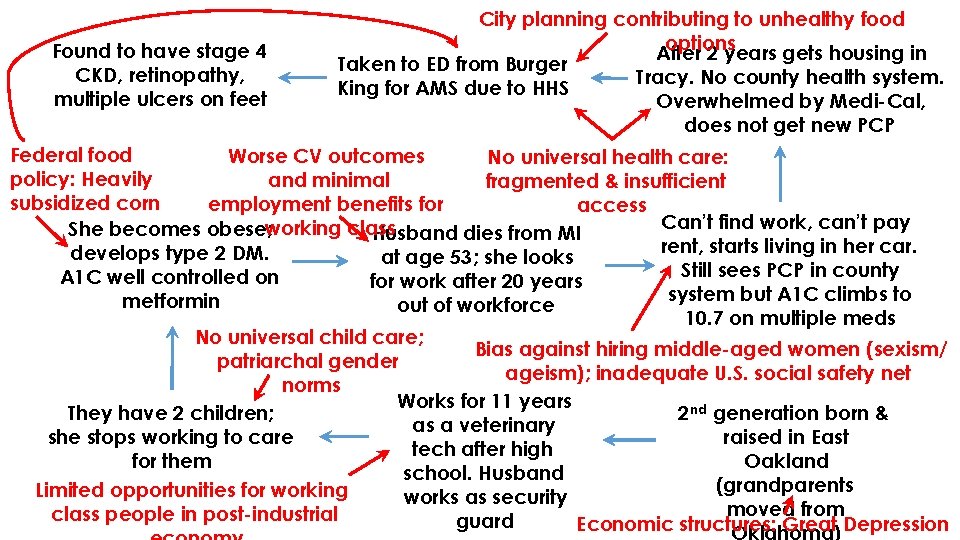
Found to have stage 4 CKD, retinopathy, multiple ulcers on feet City planning contributing to unhealthy food options After 2 years gets housing in Taken to ED from Burger Tracy. No county health system. King for AMS due to HHS Overwhelmed by Medi-Cal, does not get new PCP Federal food Worse CV outcomes No universal health care: policy: Heavily and minimal fragmented & insufficient subsidized corn employment benefits for access Can’t find work, can’t pay She becomes obese; working class Husband dies from MI rent, starts living in her car. develops type 2 DM. at age 53; she looks Still sees PCP in county A 1 C well controlled on for work after 20 years system but A 1 C climbs to metformin out of workforce 10. 7 on multiple meds No universal child care; Bias against hiring middle-aged women (sexism/ patriarchal gender ageism); inadequate U. S. social safety net norms Works for 11 years 2 nd generation born & They have 2 children; as a veterinary raised in East she stops working to care tech after high Oakland for them school. Husband (grandparents Limited opportunities for working works as security moved from class people in post-industrial guard Economic structures: Great Depression
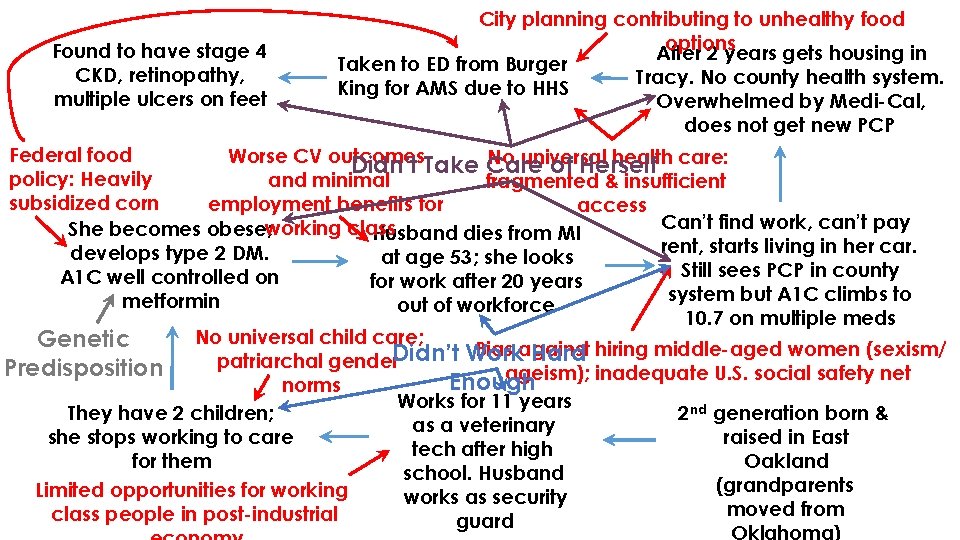
Found to have stage 4 CKD, retinopathy, multiple ulcers on feet City planning contributing to unhealthy food options After 2 years gets housing in Taken to ED from Burger Tracy. No county health system. King for AMS due to HHS Overwhelmed by Medi-Cal, does not get new PCP Federal food Worse CV outcomes No universal health care: Didn’t Take Care of Herself policy: Heavily and minimal fragmented & insufficient subsidized corn employment benefits for access Can’t find work, can’t pay She becomes obese; working class Husband dies from MI rent, starts living in her car. develops type 2 DM. at age 53; she looks Still sees PCP in county A 1 C well controlled on for work after 20 years system but A 1 C climbs to metformin out of workforce 10. 7 on multiple meds No universal child care; Genetic Bias against Didn’t Work Hard hiring middle-aged women (sexism/ patriarchal gender Predisposition ageism); inadequate U. S. social safety net Enough norms Works for 11 years 2 nd generation born & They have 2 children; as a veterinary raised in East she stops working to care tech after high Oakland for them school. Husband (grandparents Limited opportunities for working works as security moved from class people in post-industrial guard
Imagining and Implementing Structural Interventions
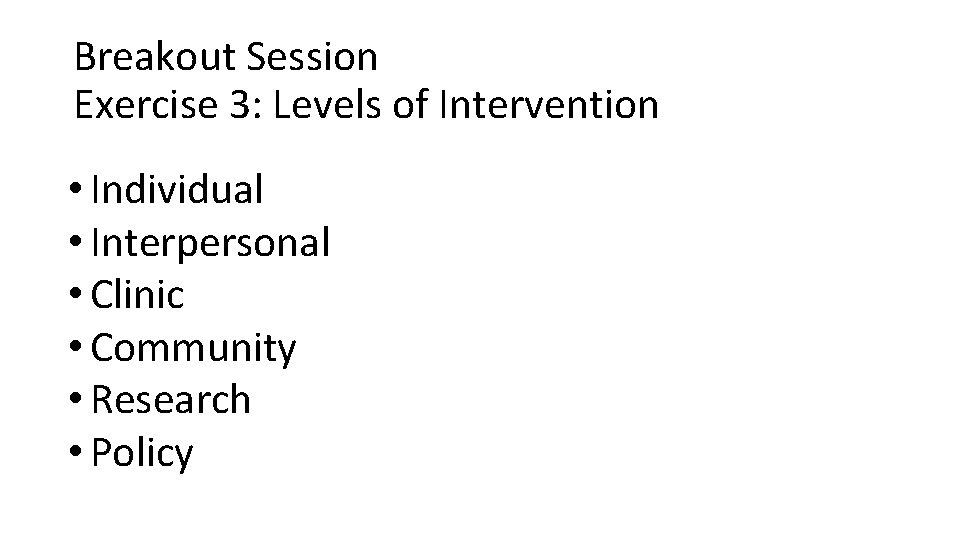
Levels of Intervention • Individual • Interpersonal • Clinic/Institutional • Community • Research • Policy 59
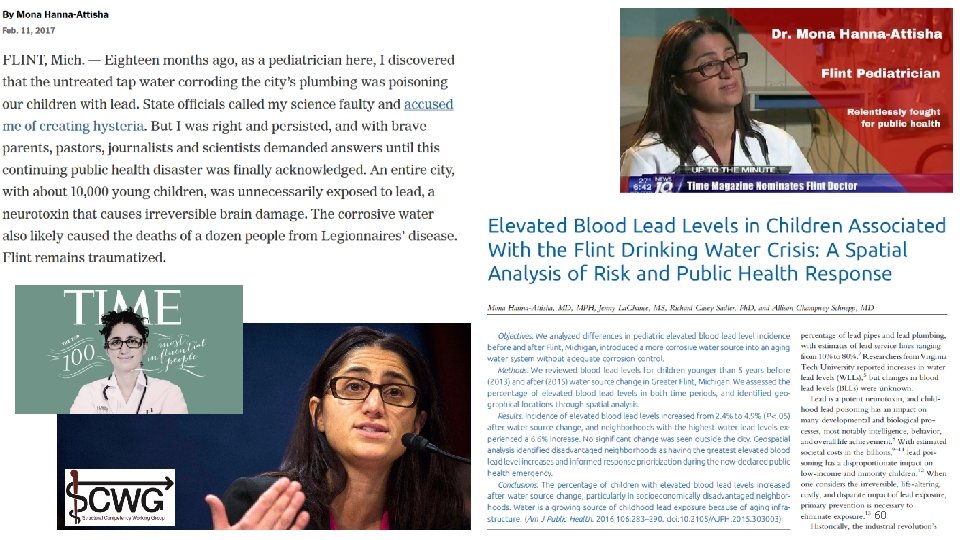
60
Black Panther Survival Programs Health Clinics (Berkeley Free Clinic, West Oakland Health Center) Breakfast Programs Food Giveaways Legal Clinics Free Busing to prisons for families Sickle Cell Testing
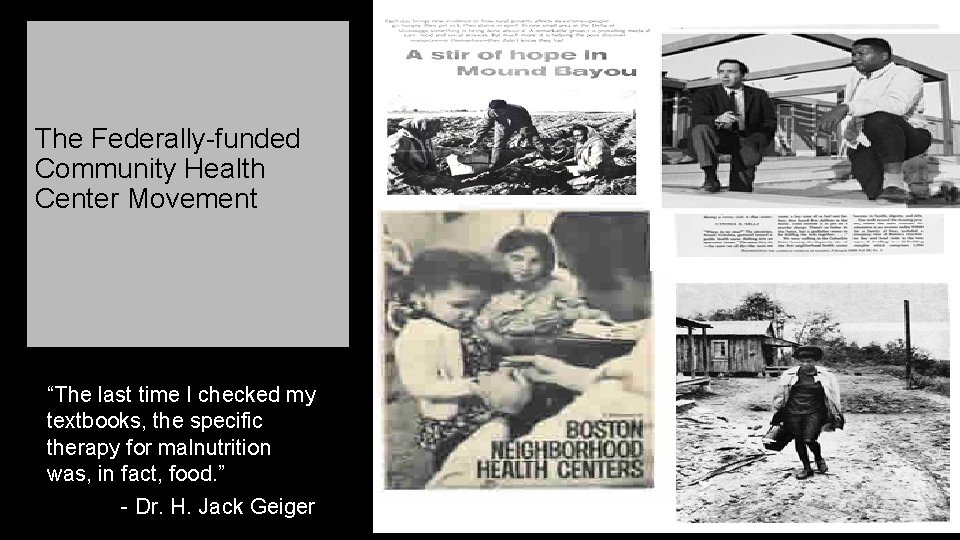
The Federally-funded Community Health Center Movement “The last time I checked my textbooks, the specific therapy for malnutrition was, in fact, food. ” - Dr. H. Jack Geiger


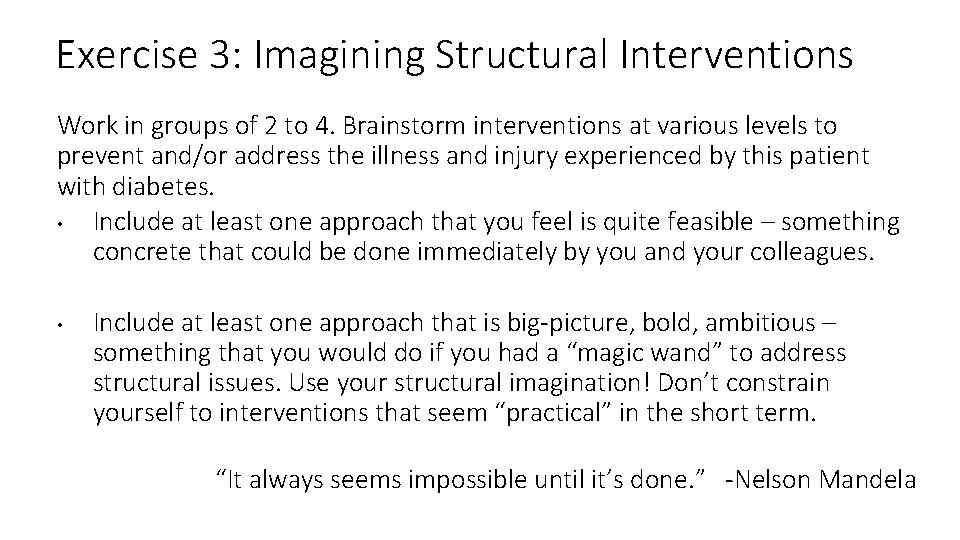
Exercise 3: Imagining Structural Interventions Work in groups of 2 to 4. Brainstorm interventions at various levels to prevent and/or address the illness and injury experienced by this patient with diabetes. • Include at least one approach that you feel is quite feasible – something concrete that could be done immediately by you and your colleagues. • Include at least one approach that is big-picture, bold, ambitious – something that you would do if you had a “magic wand” to address structural issues. Use your structural imagination! Don’t constrain yourself to interventions that seem “practical” in the short term. “It always seems impossible until it’s done. ” -Nelson Mandela
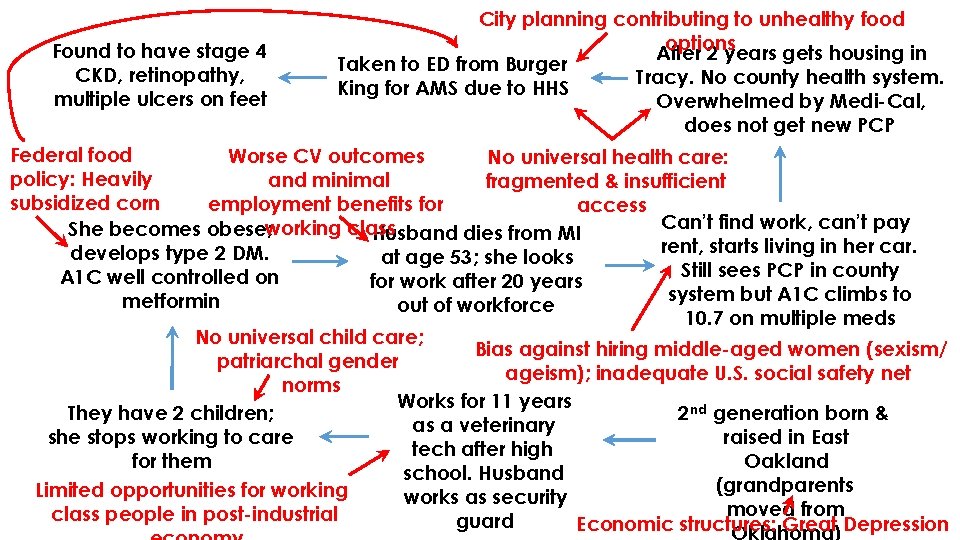
Found to have stage 4 CKD, retinopathy, multiple ulcers on feet City planning contributing to unhealthy food options After 2 years gets housing in Taken to ED from Burger Tracy. No county health system. King for AMS due to HHS Overwhelmed by Medi-Cal, does not get new PCP Federal food Worse CV outcomes No universal health care: policy: Heavily and minimal fragmented & insufficient subsidized corn employment benefits for access Can’t find work, can’t pay She becomes obese; working class Husband dies from MI rent, starts living in her car. develops type 2 DM. at age 53; she looks Still sees PCP in county A 1 C well controlled on for work after 20 years system but A 1 C climbs to metformin out of workforce 10. 7 on multiple meds No universal child care; Bias against hiring middle-aged women (sexism/ patriarchal gender ageism); inadequate U. S. social safety net norms Works for 11 years 2 nd generation born & They have 2 children; as a veterinary raised in East she stops working to care tech after high Oakland for them school. Husband (grandparents Limited opportunities for working works as security moved from class people in post-industrial guard Economic structures: Great Depression
Breakout Session Exercise 3: Levels of Intervention • Individual • Interpersonal • Clinic • Community • Research • Policy
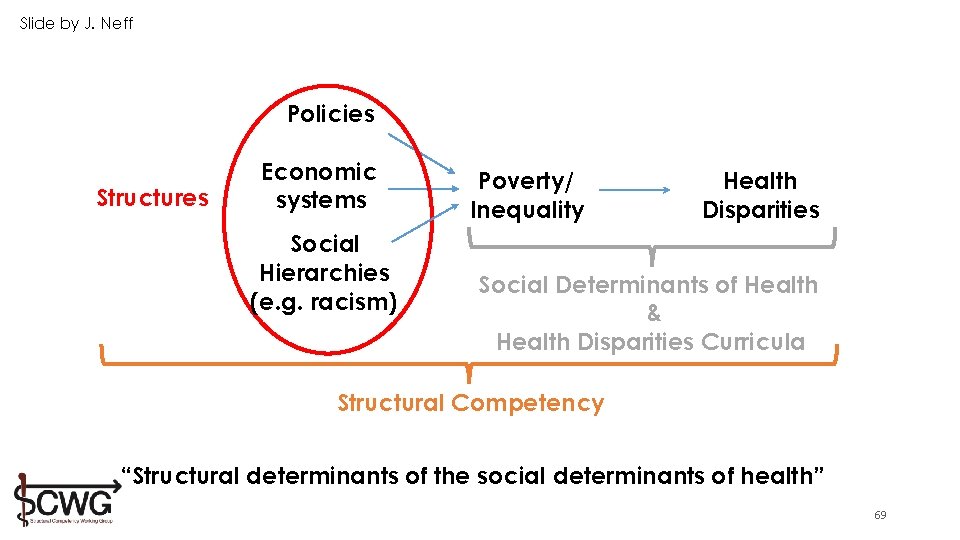
Slide by J. Neff Policies Structures Economic systems Social Hierarchies (e. g. racism) Poverty/ Inequality Health Disparities Social Determinants of Health & Health Disparities Curricula Structural Competency “Structural determinants of the social determinants of health” 69
What is your first step towards structural intervention? (tell the person next to you) 70

Questions? Contact us www. structcomp. org structuralcompetency@gmail. com
Go to www. menti. com and enter the code: 79 15 62 Please up to three words to describe your workshop experience. (For example: inspiring, practical, hands on, sobering, thought-provoking, etc. ). Your responses will build a Word Cloud in Nile Hall. 72 * | © 2011 Kaiser Foundation Health Plan, Inc. For internal use only.