Stroke Stroke n n n Second important cause


- Slides: 67

Stroke
Stroke n n n Second important cause of death Physical and pshychosocial handicap Lesions of brain parenchima due to pathology of cerebral circulatory system that leads to hemorrhageae or ichemic lesions
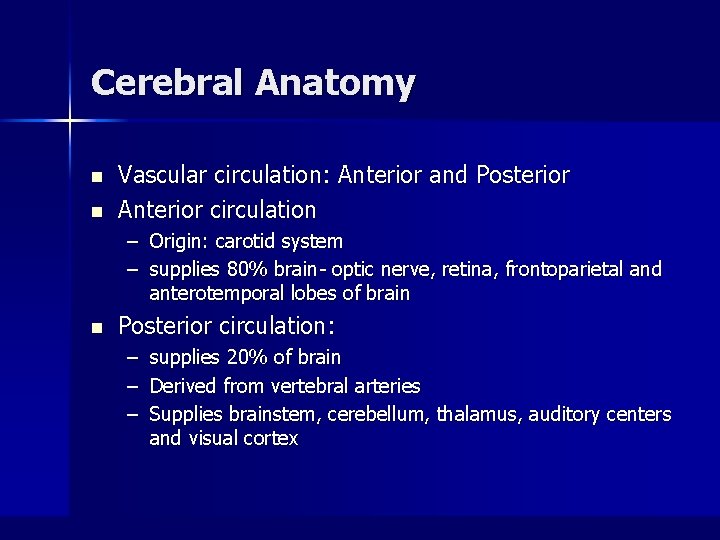
Cerebral Anatomy n n Vascular circulation: Anterior and Posterior Anterior circulation – Origin: carotid system – supplies 80% brain- optic nerve, retina, frontoparietal and anterotemporal lobes of brain n Posterior circulation: – – – supplies 20% of brain Derived from vertebral arteries Supplies brainstem, cerebellum, thalamus, auditory centers and visual cortex
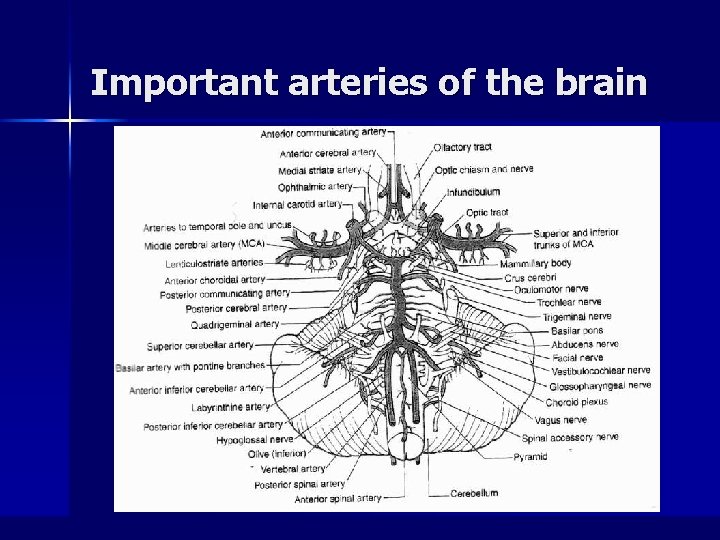
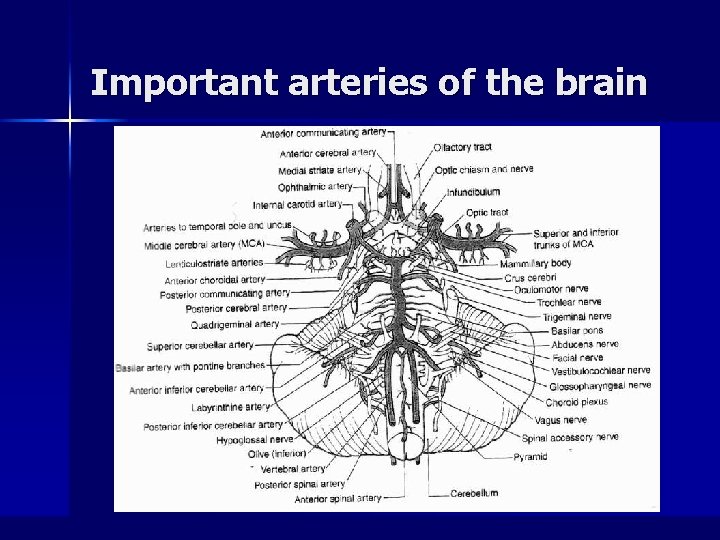
Important arteries of the brain
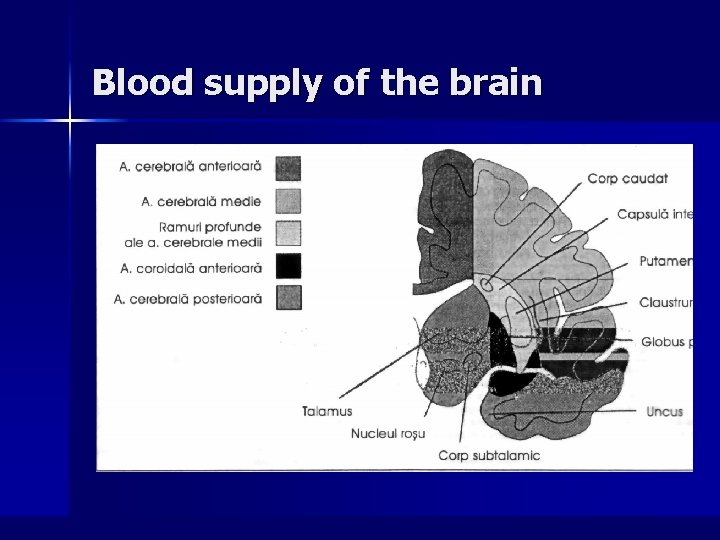
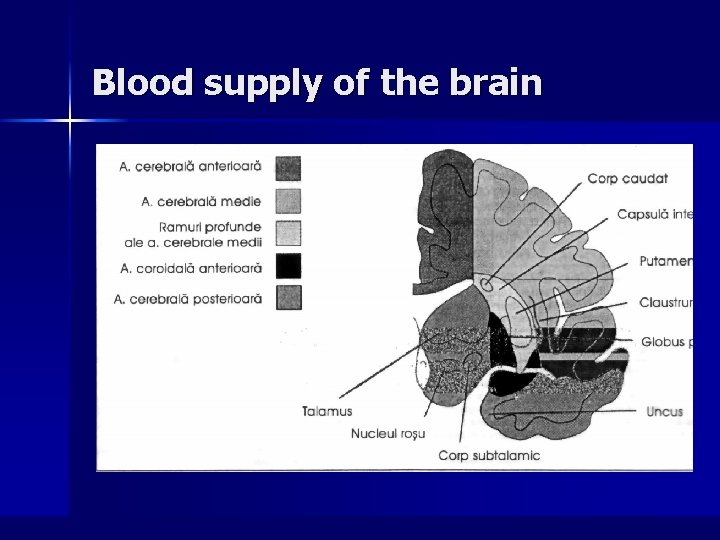
Blood supply of the brain
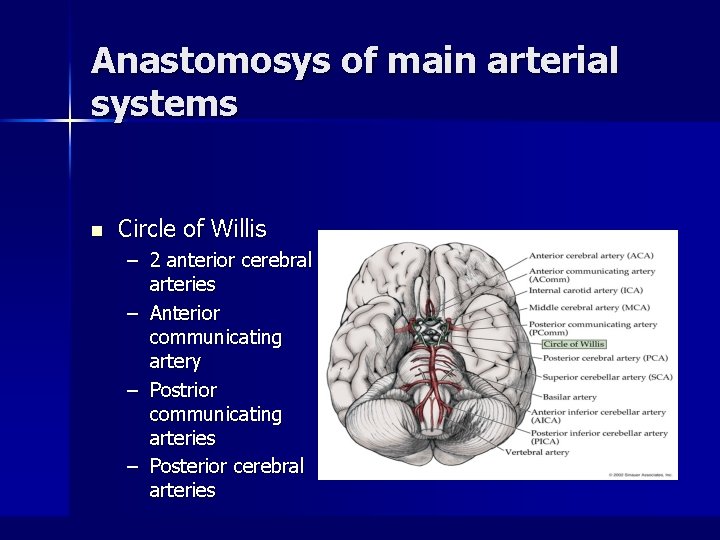
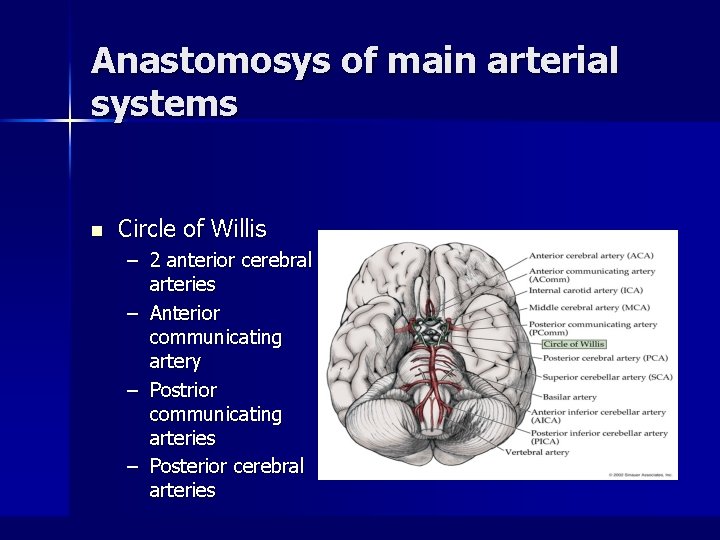
Anastomosys of main arterial systems n Circle of Willis – 2 anterior cerebral arteries – Anterior communicating artery – Postrior communicating arteries – Posterior cerebral arteries
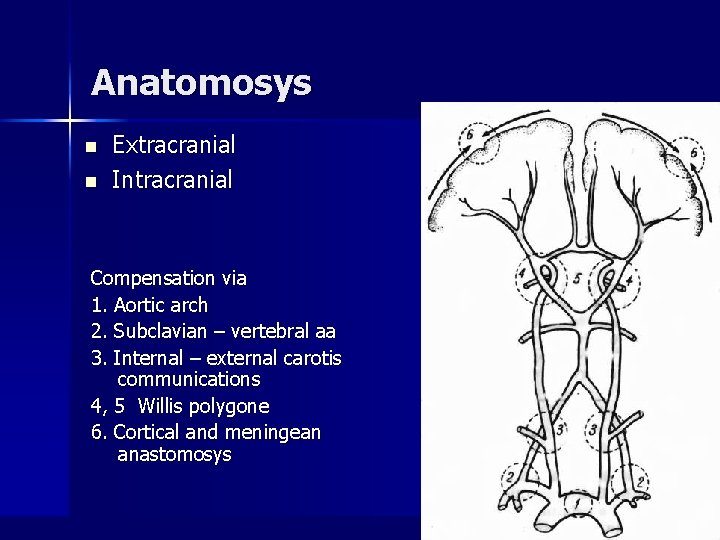
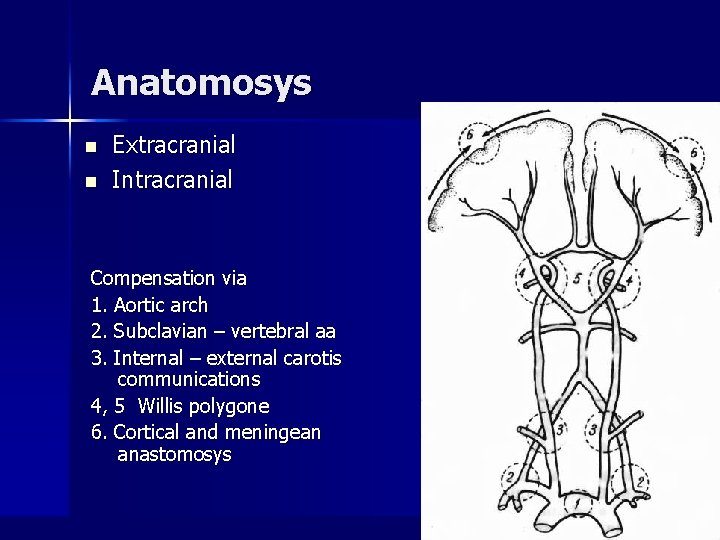
Anatomosys n n Extracranial Intracranial Compensation via 1. Aortic arch 2. Subclavian – vertebral aa 3. Internal – external carotis communications 4, 5 Willis polygone 6. Cortical and meningean anastomosys
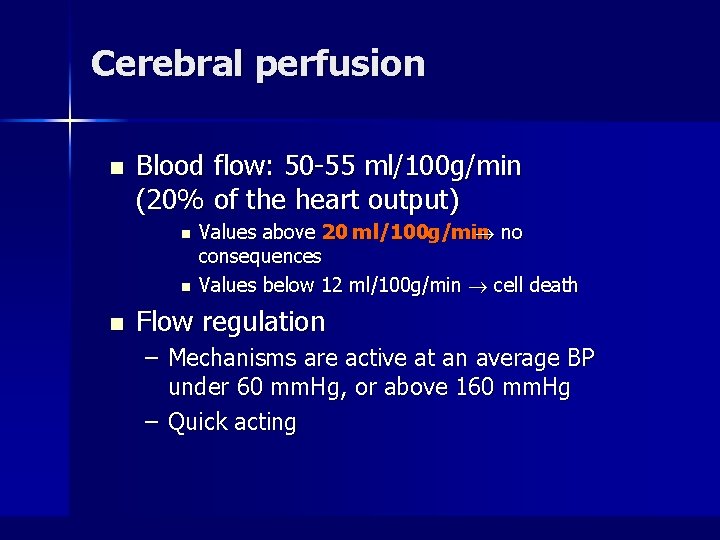
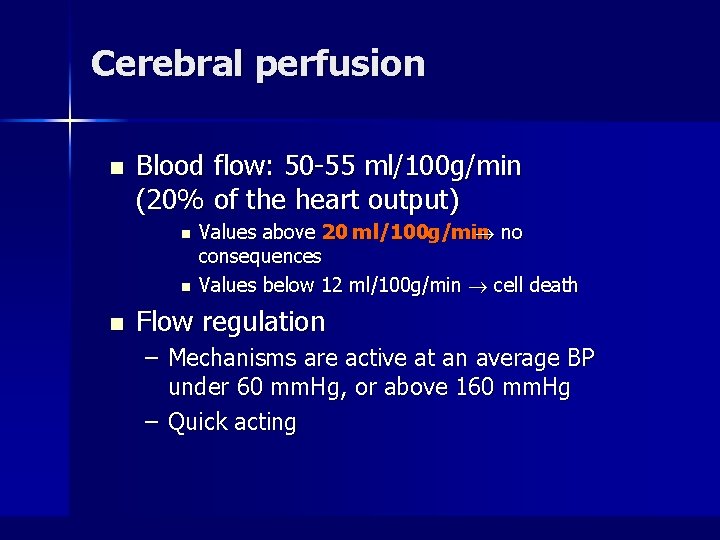
Cerebral perfusion n Blood flow: 50 -55 ml/100 g/min (20% of the heart output) n n n Values above 20 ml/100 g/min no consequences Values below 12 ml/100 g/min cell death Flow regulation – Mechanisms are active at an average BP under 60 mm. Hg, or above 160 mm. Hg – Quick acting
Stroke n n n Sudden onset (seconds- minutes, rarely 1 -2 days) of a focal neurological deficit Evolution towards stabilization or remission Risk factors for vascular disease: arterial hyoertension, embolic conditions, etc
Stroke Types n 80% ischemic – – – n Thrombosis Embolism Hypoperfusion 20% hemorrhagic – Intracerebral – Subarachnoid
Ischemic Strokes n n Thrombosis-most common cause Etiology – Atherosclerotic disease-most common – Vasculitis – Dissection – Polycythemia – Hypercoagulable states – Infectious Diseases-HIV, TB, syphilis n Evolution of mural thrombi: – Lysis – fragmentation (eventally emboli formation) or resorbtion – Fibrous evolution – Extension
Ischemic stroke – other type of vascular obstruction n n Inflamatory angeitis – Takayasu disease, Horton temporal arteritis, Lupus erithematosus, granulomatous angeitis) Infectious angeitis (lues, tuberculosys, AIDS) Arterial dissection Radiotherapy associated stenosys
Ischemic Strokes n n 1/5 th due to Embolism Etiology – Cardiac n n – – n n More often in the carotidian system Valvular Vegetations Mural thrombi- caused by A-fib, MI, or dysrhythmias Paradoxical emboli – from ASD, VSD Cardiac tumors-myxoma Arterial emboli (trombi, atheroma plaque fragments) Fat emboli Particulate emboli – IV drug injections Septic Emboli Spontaneous lysis and clinical remission may happen, depending of the nature of the embolus Usually multiple ischemic lesions of different ages More often secondary hemorrhageae
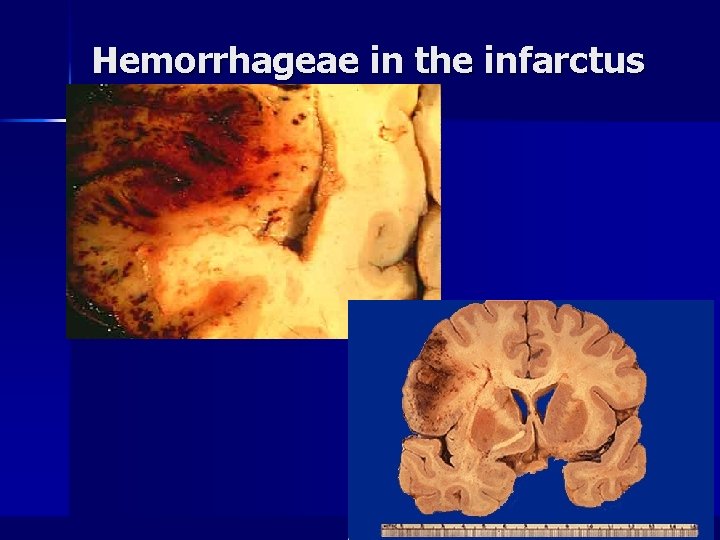
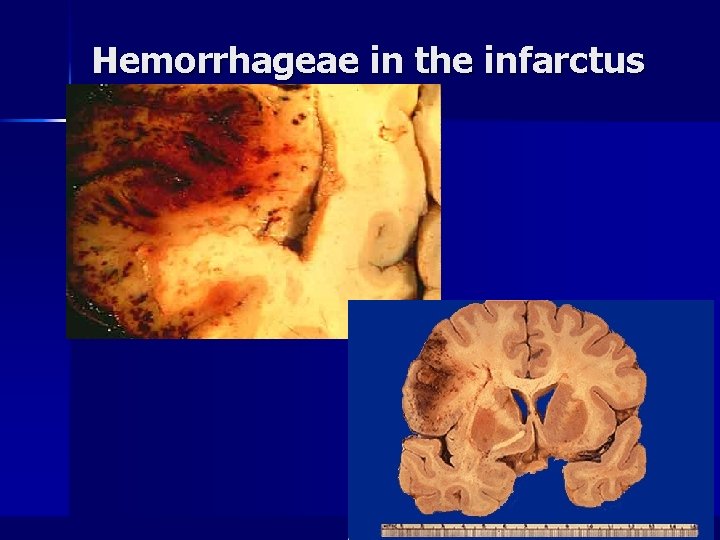
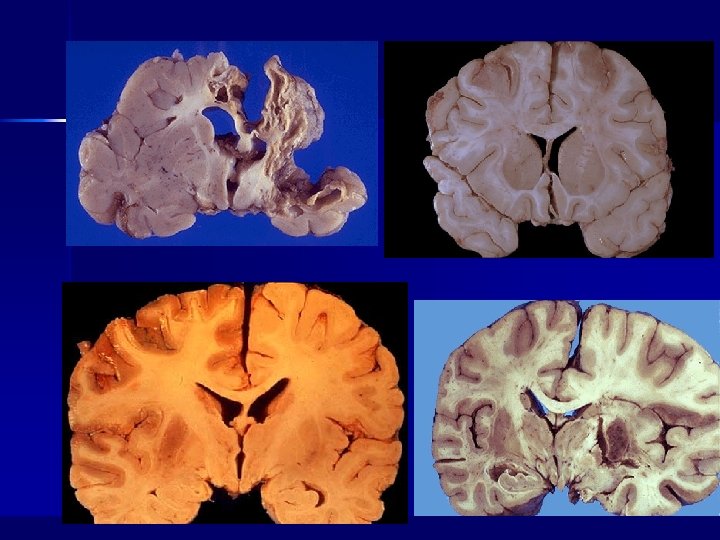
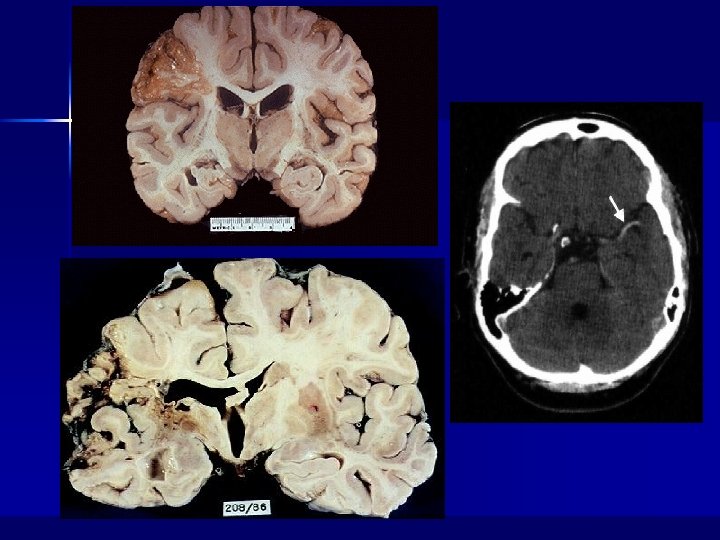
Hemorrhageae in the infarctus area
Ischemic Strokes n Hypoperfusion- less common mechanism – Typically caused by cardiac failure – More diffuse injury pattern vs thrombosis or embolism – Usually occur in watershed regions of brain – Focal hypoperfusion – arterial stenosis; collateral circulation may compensate – Global hypoperfusion – consequences depend on the dynamics of the flow reduction (duration, intensity) n n Systolic AT <7 mm. Hg Watershed infarct
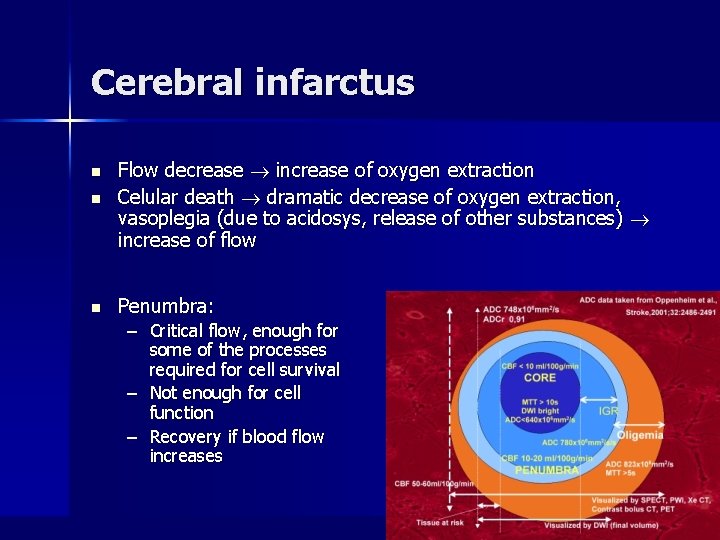
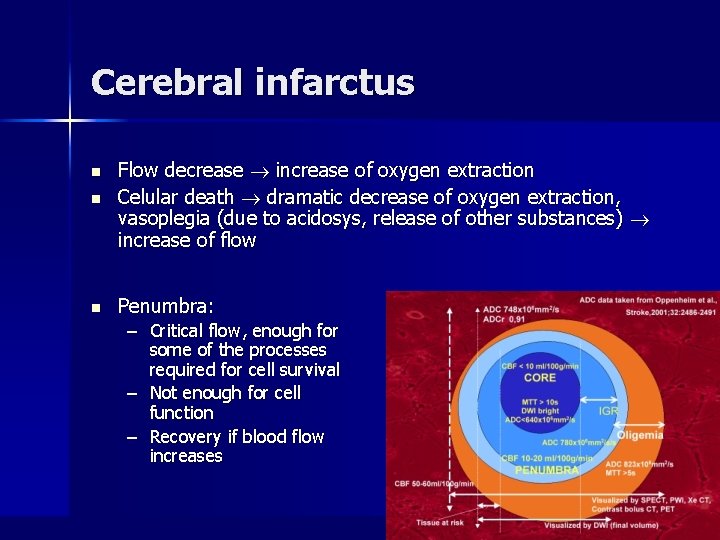
Cerebral infarctus n Flow decrease increase of oxygen extraction Celular death dramatic decrease of oxygen extraction, vasoplegia (due to acidosys, release of other substances) increase of flow n Penumbra: n – Critical flow, enough for some of the processes required for cell survival – Not enough for cell function – Recovery if blood flow increases
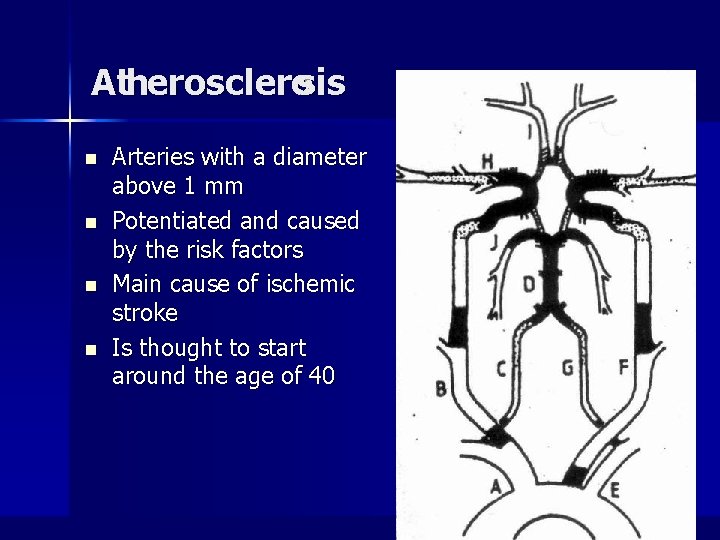
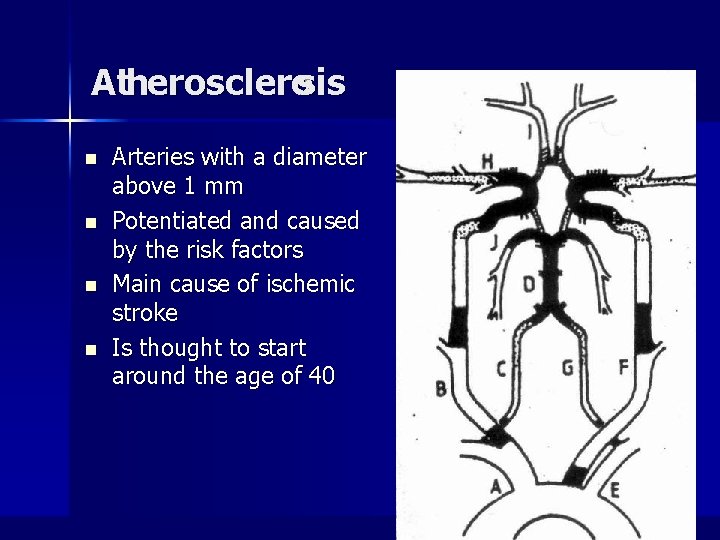
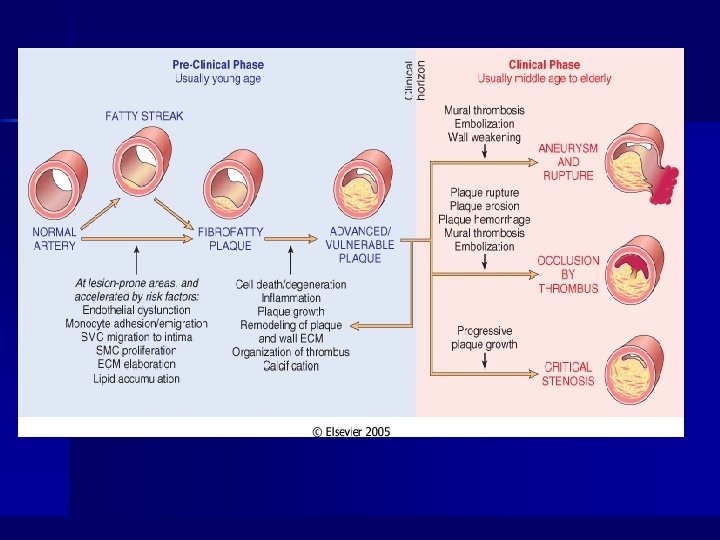
Atherosclerosis n n Arteries with a diameter above 1 mm Potentiated and caused by the risk factors Main cause of ischemic stroke Is thought to start around the age of 40
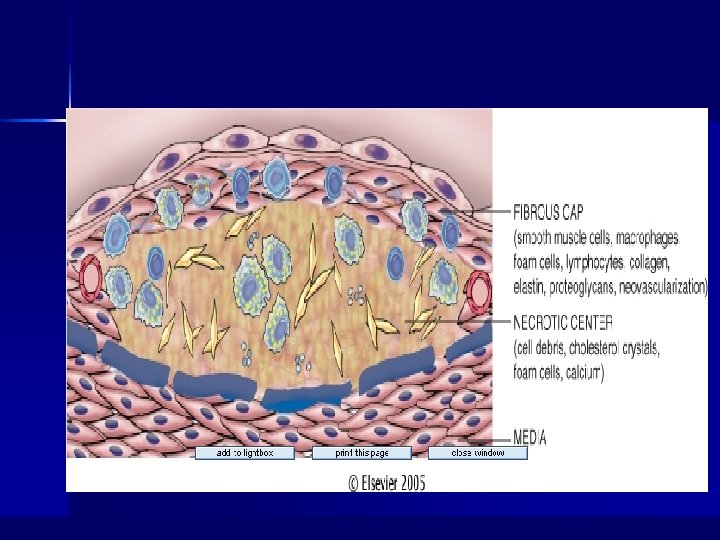
General Comments n Arteriosclerosis – Thickening and loss of elasticity of arterial walls – Hardening of the arteries – Greatest morbidity and mortality of all human diseases n Two major processes in plaque formation: – Intimal thickening – Lipid accumulation
Non-Modifiable Risk Factors n Age – A dominant influence – Atherosclerosis begins in the young, but does not precipitate organ injury until later in life n Gender – Men more prone than women, but by age 60 -70 about equal frequency n Family History – Familial cluster of risk factors – Genetic differences
Modifiable Risk Factors (potentially controllable) n n n n Hyperlipidemia Hypertension Cigarette smoking Diabetes Mellitus Elevated Homocysteine Factors that affect hemostasis and thrombosis Infections: Herpes virus; Chlamydia pneumoniae Obesity, sedentary lifestyle, stress
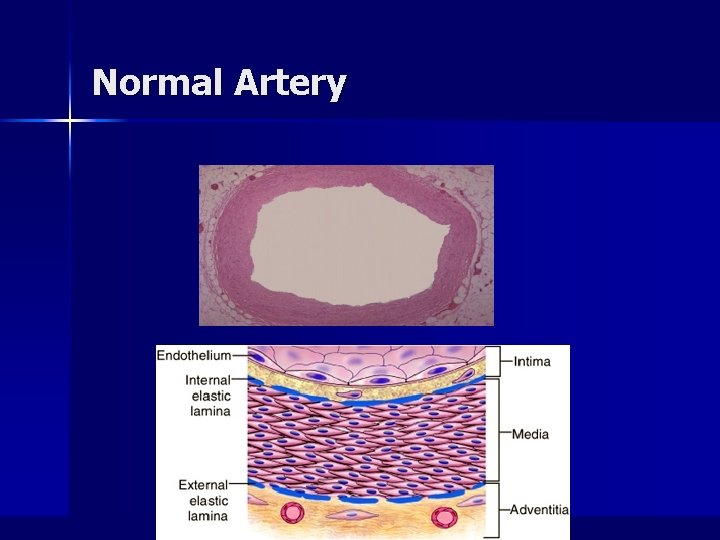
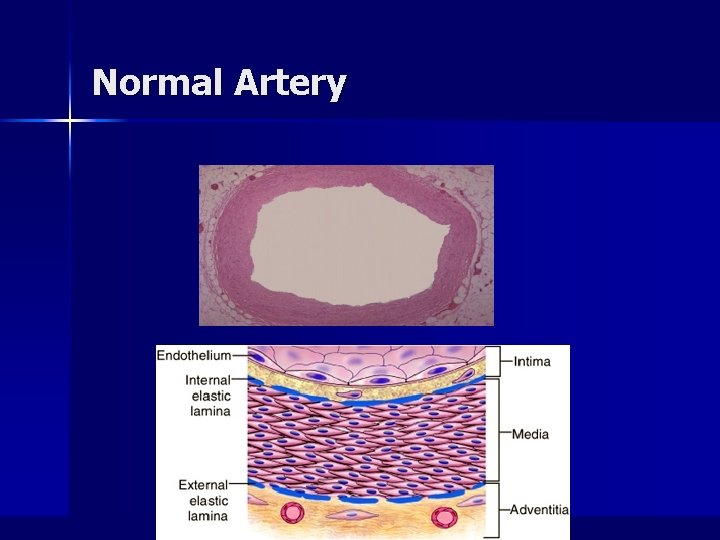
Normal Artery
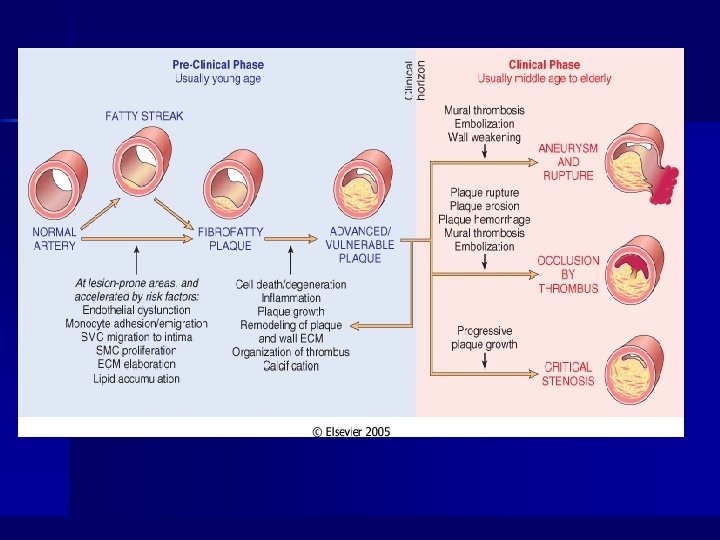
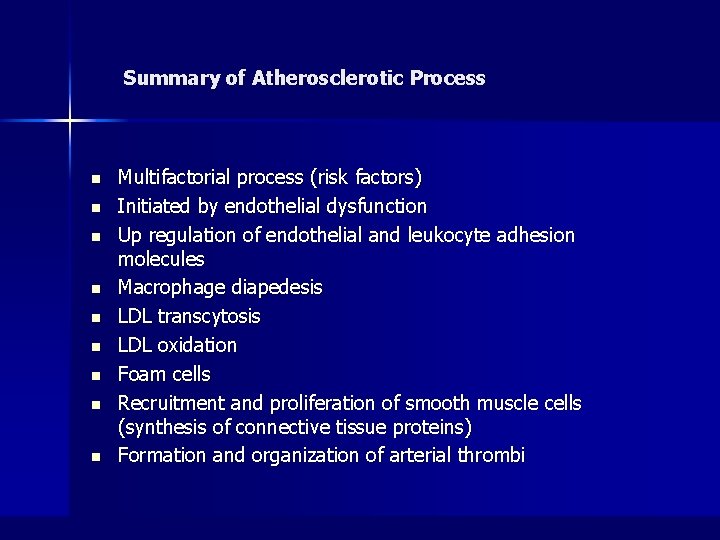
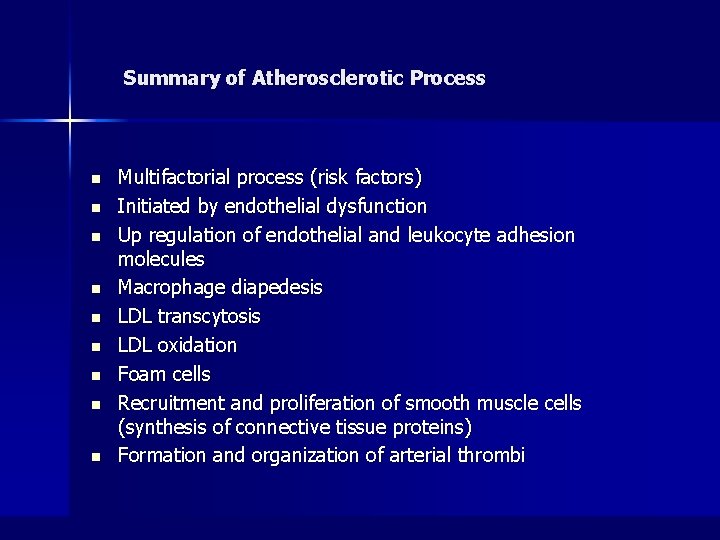
Summary of Atherosclerotic Process n n n n n Multifactorial process (risk factors) Initiated by endothelial dysfunction Up regulation of endothelial and leukocyte adhesion molecules Macrophage diapedesis LDL transcytosis LDL oxidation Foam cells Recruitment and proliferation of smooth muscle cells (synthesis of connective tissue proteins) Formation and organization of arterial thrombi
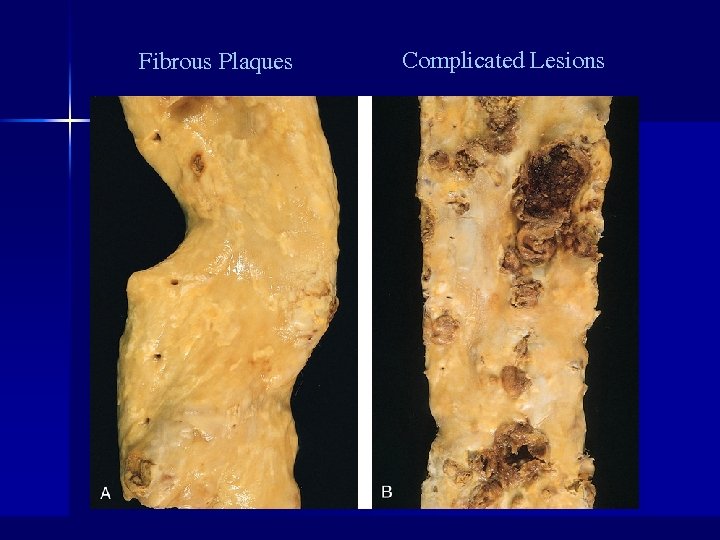
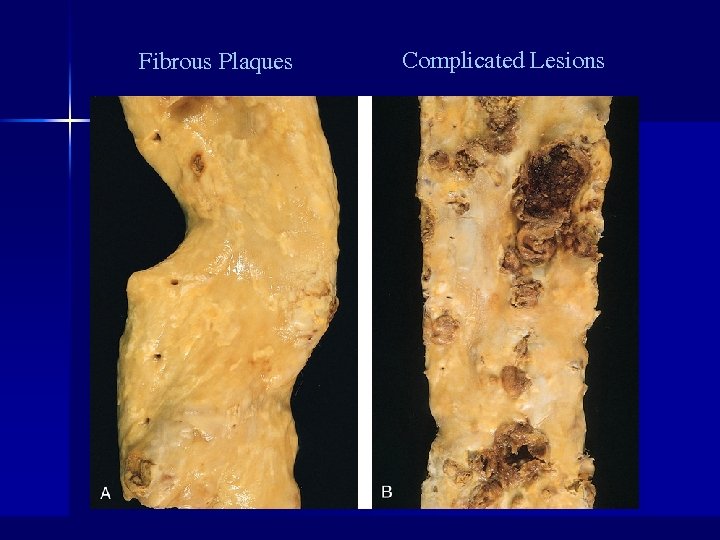
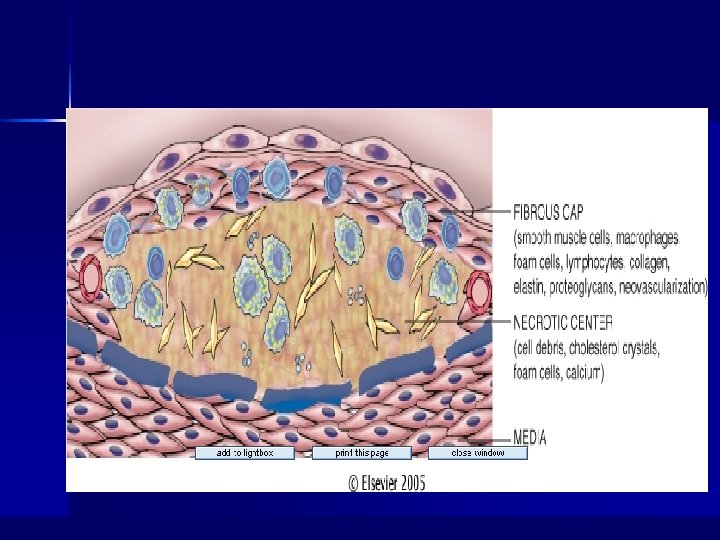
Fibrous Plaques Complicated Lesions

Complicated Lesions
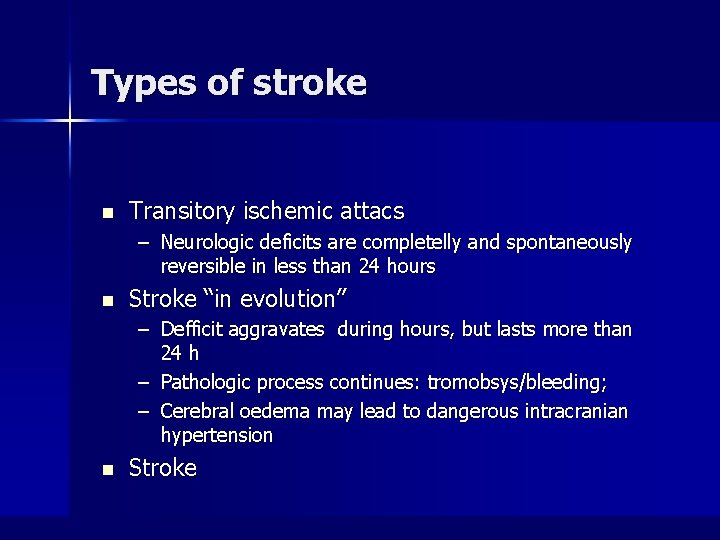
Types of stroke n Transitory ischemic attacs – Neurologic deficits are completelly and spontaneously reversible in less than 24 hours n Stroke “in evolution” – Defficit aggravates during hours, but lasts more than 24 h – Pathologic process continues: tromobsys/bleeding; – Cerebral oedema may lead to dangerous intracranian hypertension n Stroke
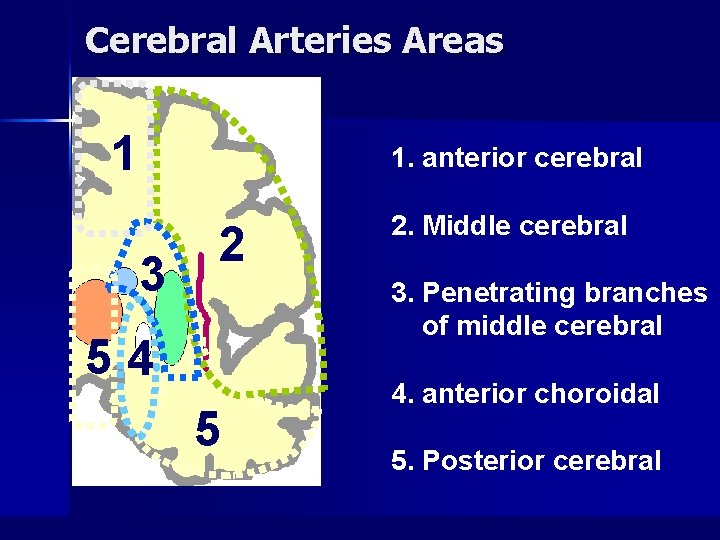
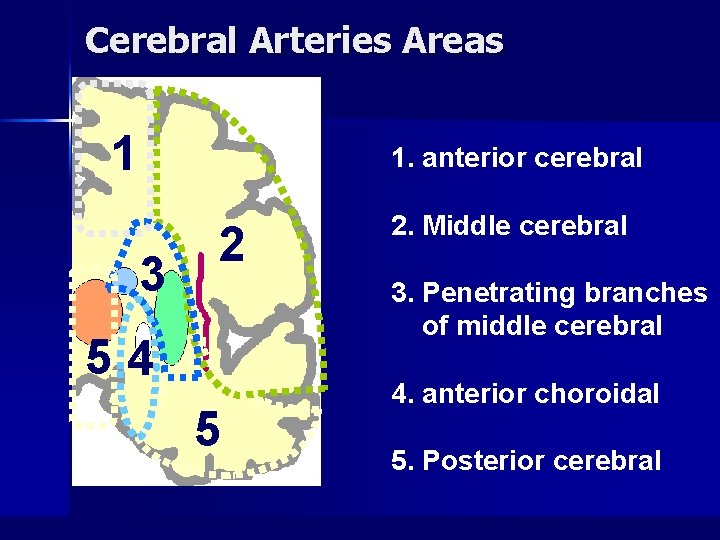
Cerebral Arteries Areas 1 1. anterior cerebral 3 2 2. Middle cerebral 3. Penetrating branches of middle cerebral 54 5 4. anterior choroidal 5. Posterior cerebral
Anterior cerebral artery syndrome
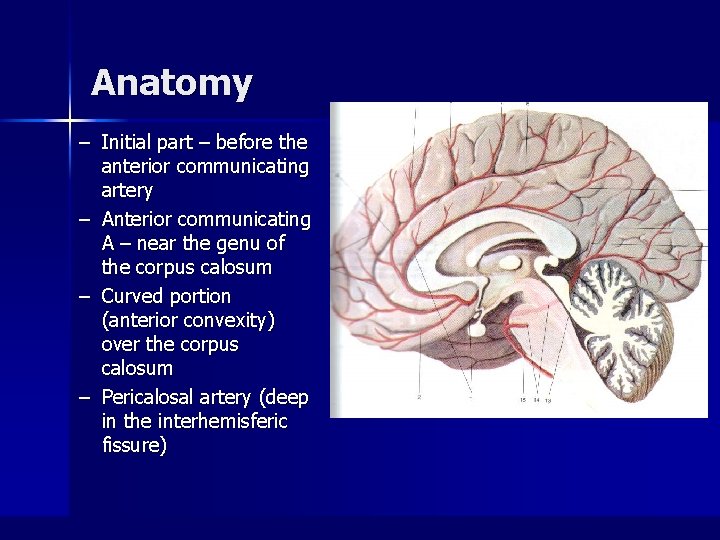
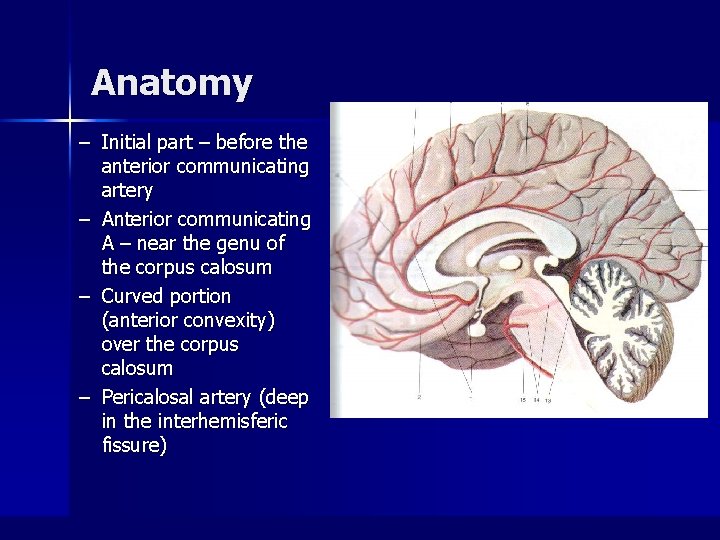
Anatomy – Initial part – before the anterior communicating artery – Anterior communicating A – near the genu of the corpus calosum – Curved portion (anterior convexity) over the corpus calosum – Pericalosal artery (deep in the interhemisferic fissure)
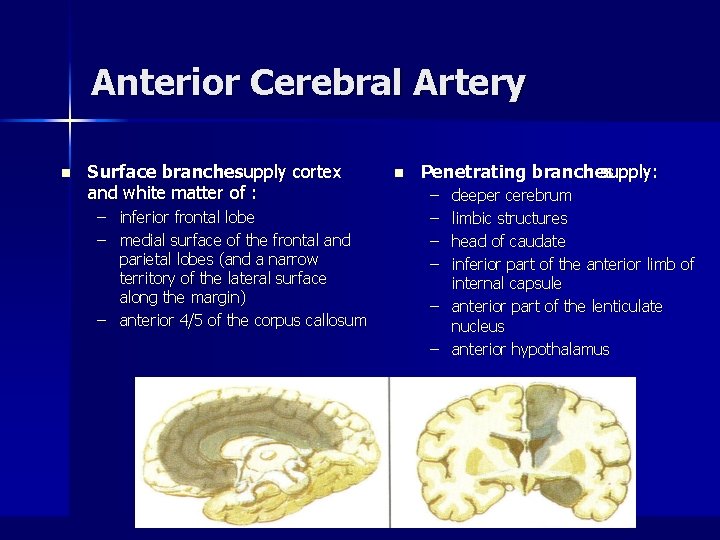
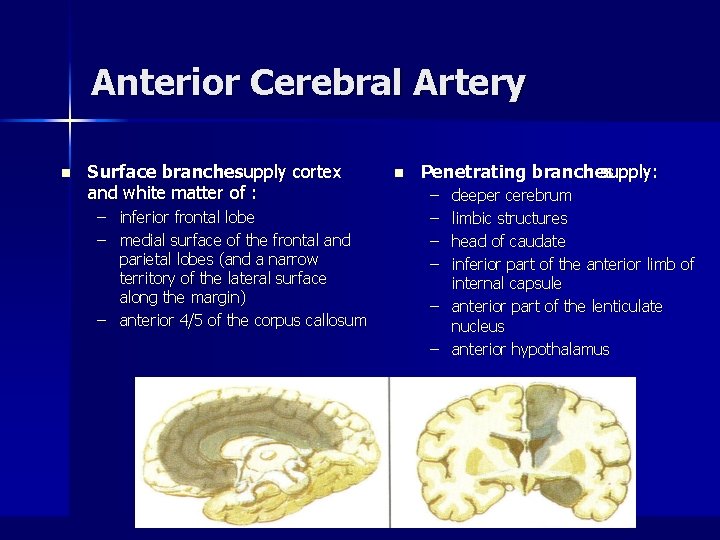
Anterior Cerebral Artery n Surface branchessupply cortex and white matter of : – inferior frontal lobe – medial surface of the frontal and parietal lobes (and a narrow territory of the lateral surface along the margin) – anterior 4/5 of the corpus callosum n Penetrating branches supply: – – deeper cerebrum limbic structures head of caudate inferior part of the anterior limb of internal capsule – anterior part of the lenticulate nucleus – anterior hypothalamus
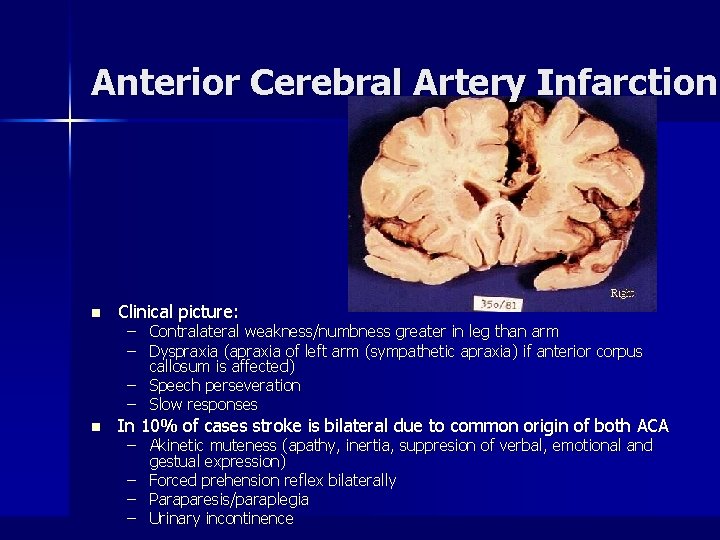
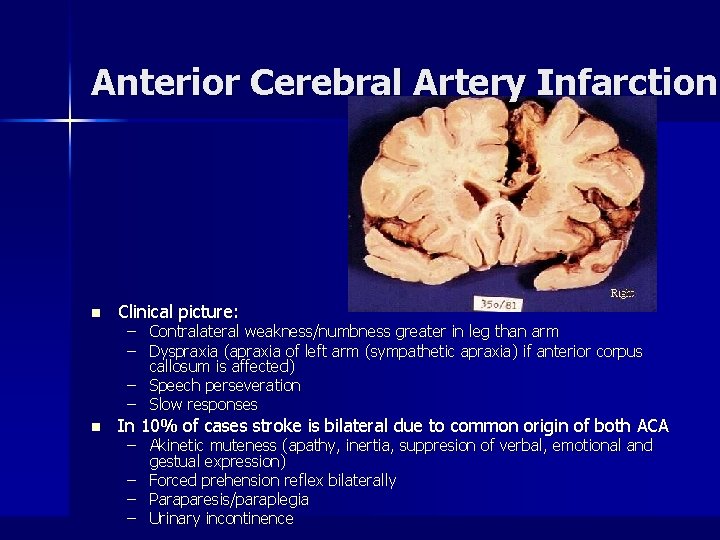
Anterior Cerebral Artery Infarction n Clinical picture: n In 10% of cases stroke is bilateral due to common origin of both ACA – Contralateral weakness/numbness greater in leg than arm – Dyspraxia (apraxia of left arm (sympathetic apraxia) if anterior corpus callosum is affected) – Speech perseveration – Slow responses – Akinetic muteness (apathy, inertia, suppresion of verbal, emotional and gestual expression) – Forced prehension reflex bilaterally – Paraparesis/paraplegia – Urinary incontinence
Middle cerebral artery syndrome
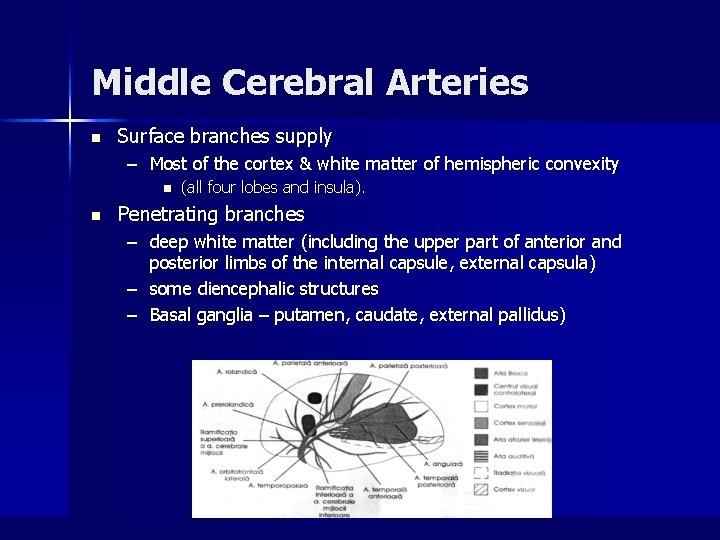
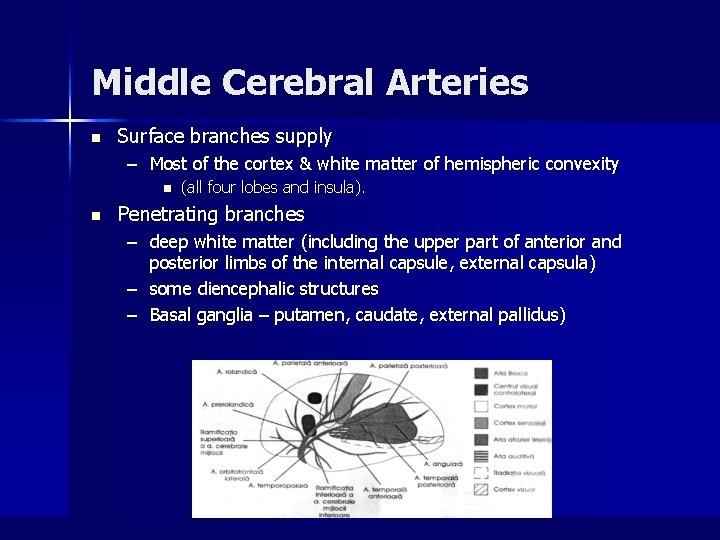
Middle Cerebral Arteries n Surface branches supply – Most of the cortex & white matter of hemispheric convexity n n (all four lobes and insula). Penetrating branches – deep white matter (including the upper part of anterior and posterior limbs of the internal capsule, external capsula) – some diencephalic structures – Basal ganglia – putamen, caudate, external pallidus)
Middle cerebral artery occlusion n contralateral motor and sensory deficits in the face and arm > leg, and aphasia in the dominant (left) hemisphere. (Netter, Part II, p. 58)
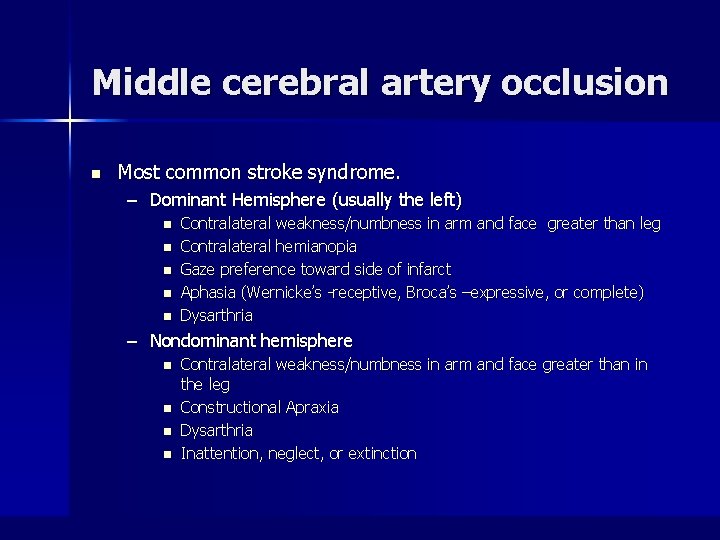
Middle cerebral artery occlusion n Most common stroke syndrome. – Dominant Hemisphere (usually the left) n n n Contralateral weakness/numbness in arm and face greater than leg Contralateral hemianopia Gaze preference toward side of infarct Aphasia (Wernicke’s -receptive, Broca’s –expressive, or complete) Dysarthria – Nondominant hemisphere n n Contralateral weakness/numbness in arm and face greater than in the leg Constructional Apraxia Dysarthria Inattention, neglect, or extinction
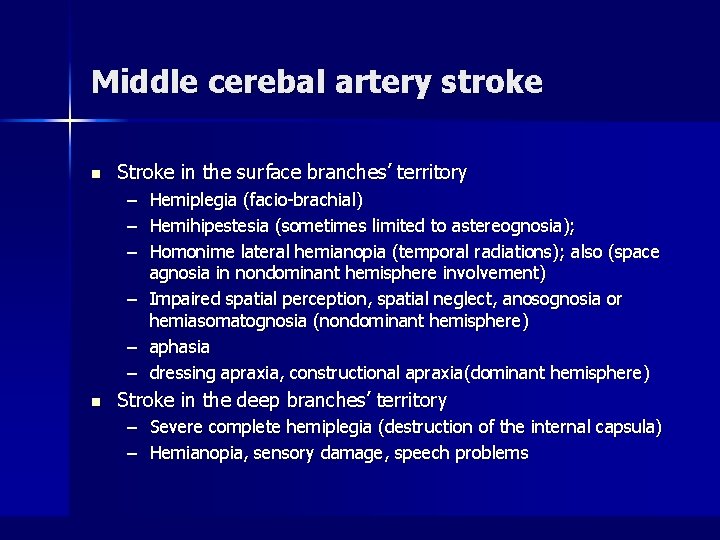
Middle cerebal artery stroke n Stroke in the surface branches’ territory – – – Hemiplegia (facio-brachial) Hemihipestesia (sometimes limited to astereognosia); Homonime lateral hemianopia (temporal radiations); also (space agnosia in nondominant hemisphere involvement) – Impaired spatial perception, spatial neglect, anosognosia or hemiasomatognosia (nondominant hemisphere) – aphasia – dressing apraxia, constructional apraxia(dominant hemisphere) n Stroke in the deep branches’ territory – Severe complete hemiplegia (destruction of the internal capsula) – Hemianopia, sensory damage, speech problems
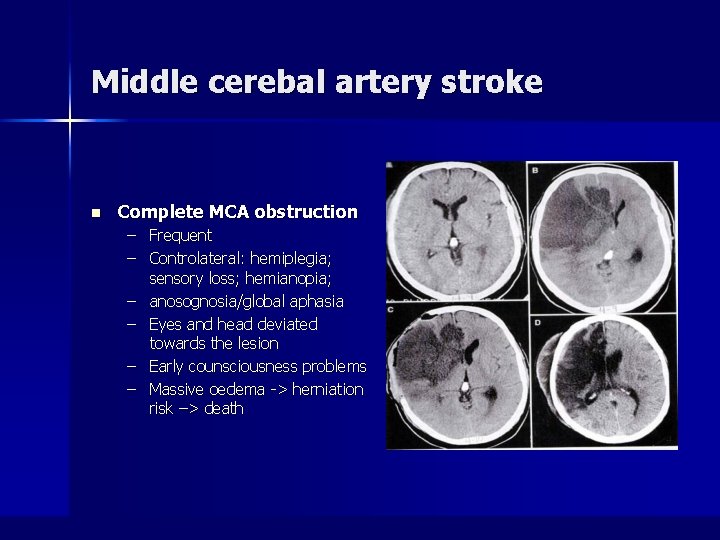
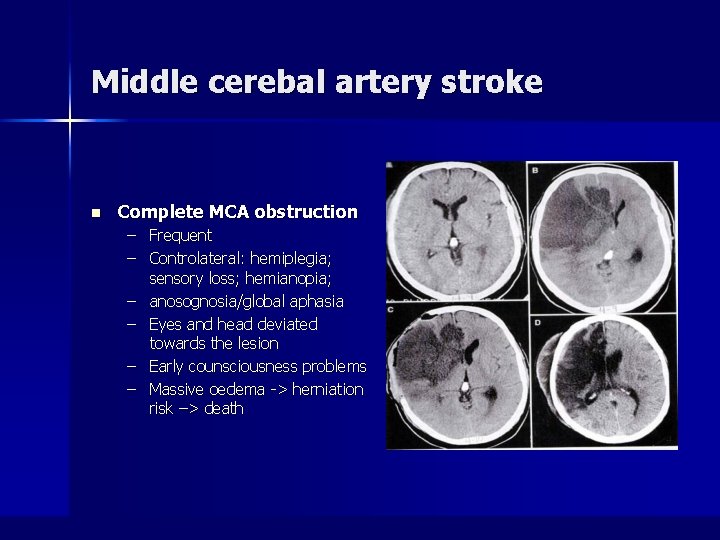
Middle cerebal artery stroke n Complete MCA obstruction – Frequent – Controlateral: hemiplegia; sensory loss; hemianopia; – anosognosia/global aphasia – Eyes and head deviated towards the lesion – Early counsciousness problems – Massive oedema -> herniation risk –> death
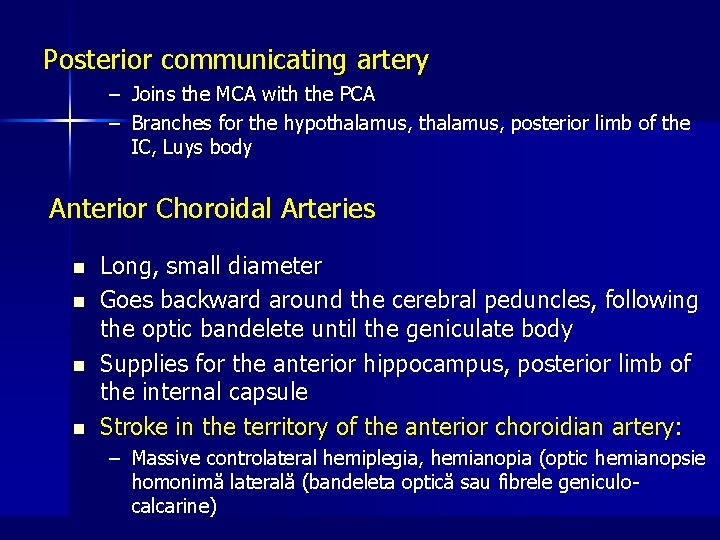
Posterior communicating artery – Joins the MCA with the PCA – Branches for the hypothalamus, posterior limb of the IC, Luys body Anterior Choroidal Arteries n n Long, small diameter Goes backward around the cerebral peduncles, following the optic bandelete until the geniculate body Supplies for the anterior hippocampus, posterior limb of the internal capsule Stroke in the territory of the anterior choroidian artery: – Massive controlateral hemiplegia, hemianopia (optic hemianopsie homonimă laterală (bandeleta optică sau fibrele geniculocalcarine)
Posterior cerebral artery syndrome
Vertebral Arteries n n Rise from subclavian artery Branches – anterior spinal arteries & – posterior inferior cerebellar arteries. n 2 vertebral arteries join at the junction of the pons and medulla – form basilar artery – basilar divides into 2 posterior cerebral arteries
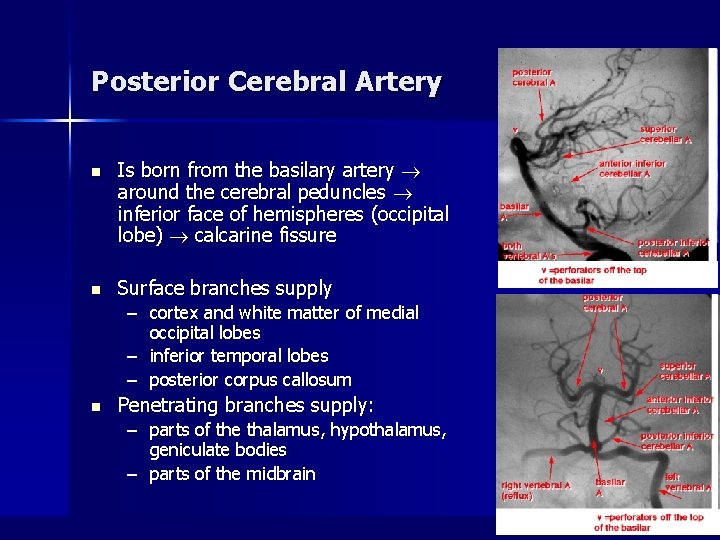
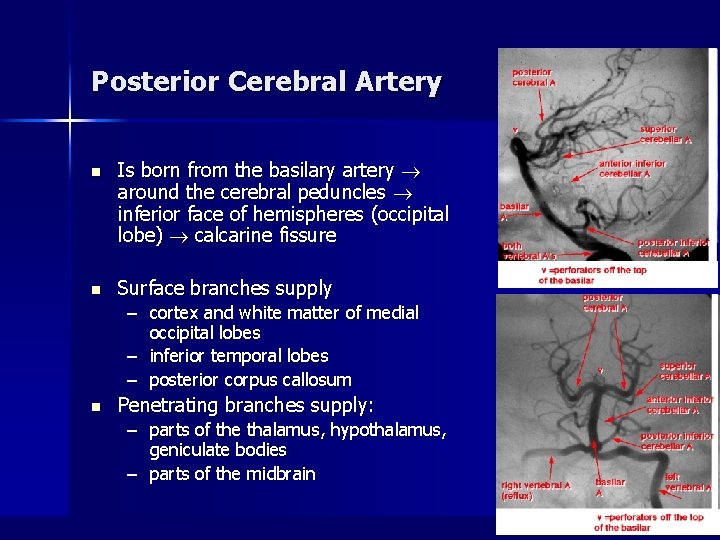
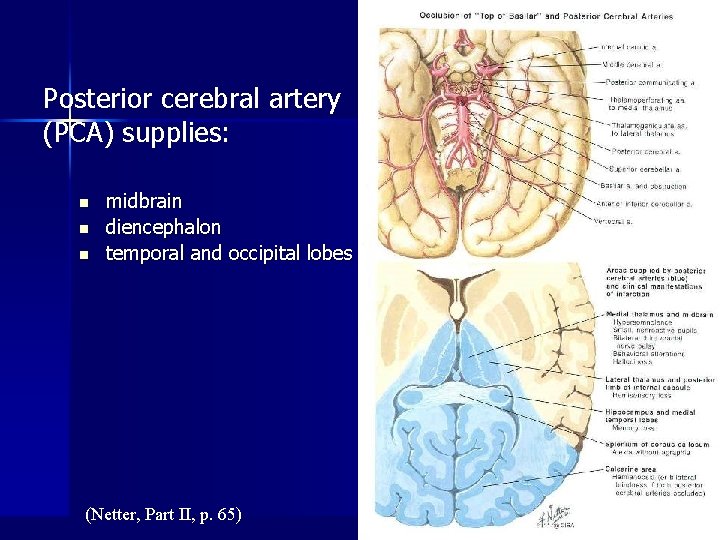
Posterior Cerebral Artery n Is born from the basilary artery around the cerebral peduncles inferior face of hemispheres (occipital lobe) calcarine fissure n Surface branches supply – cortex and white matter of medial occipital lobes – inferior temporal lobes – posterior corpus callosum n Penetrating branches supply: – parts of the thalamus, hypothalamus, geniculate bodies – parts of the midbrain
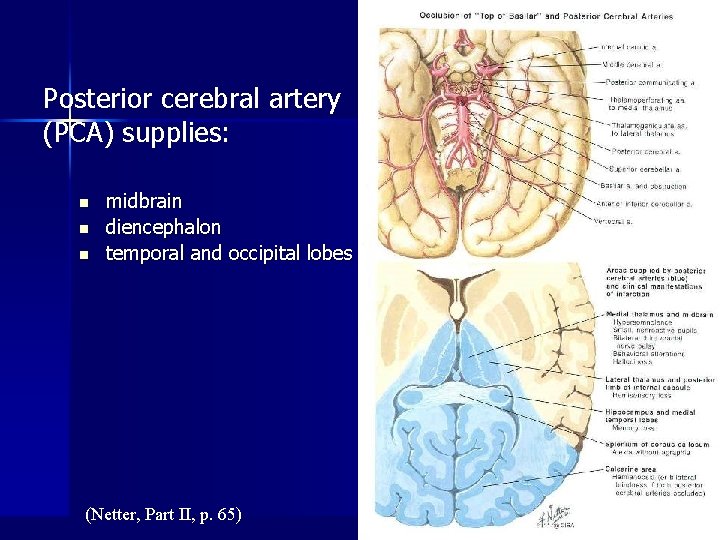
Posterior cerebral artery (PCA) supplies: n n n midbrain diencephalon temporal and occipital lobes (Netter, Part II, p. 65)
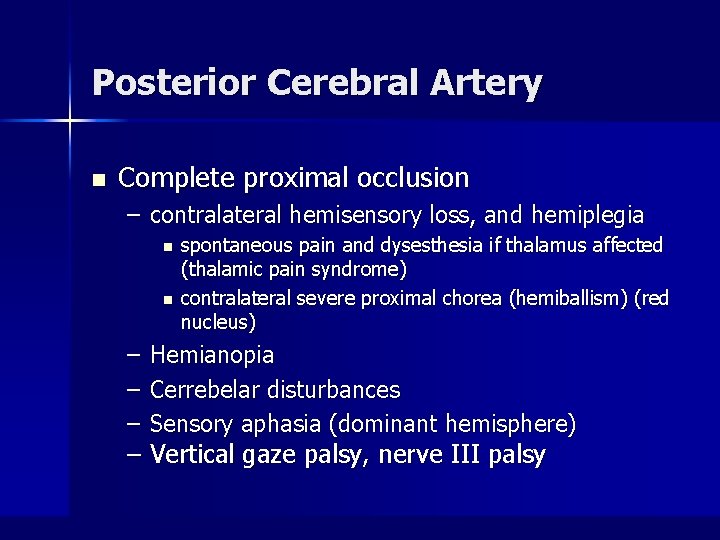
Posterior Cerebral Artery n Complete proximal occlusion – contralateral hemisensory loss, and hemiplegia n n – – – spontaneous pain and dysesthesia if thalamus affected (thalamic pain syndrome) contralateral severe proximal chorea (hemiballism) (red nucleus) Hemianopia Cerrebelar disturbances Sensory aphasia (dominant hemisphere) – Vertical gaze palsy, nerve III palsy
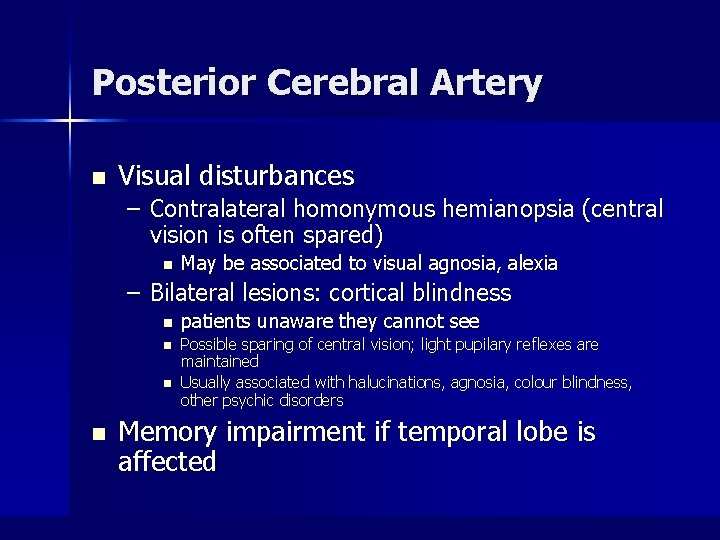
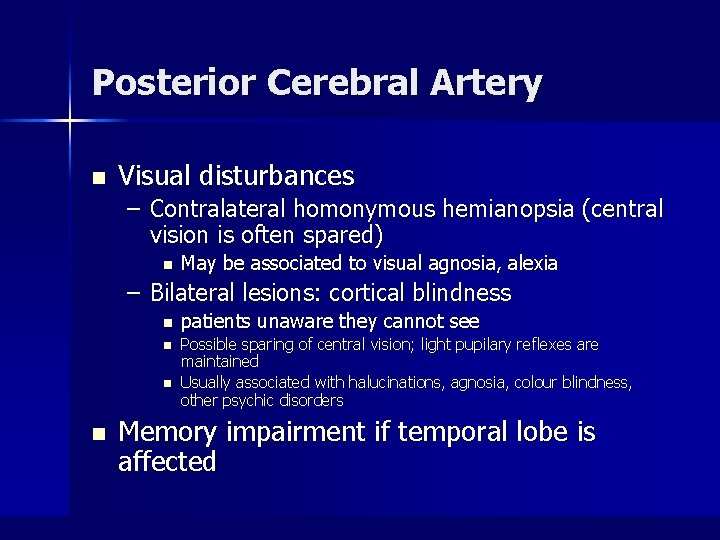
Posterior Cerebral Artery n Visual disturbances – Contralateral homonymous hemianopsia (central vision is often spared) n May be associated to visual agnosia, alexia – Bilateral lesions: cortical blindness n n patients unaware they cannot see Possible sparing of central vision; light pupilary reflexes are maintained Usually associated with halucinations, agnosia, colour blindness, other psychic disorders Memory impairment if temporal lobe is affected
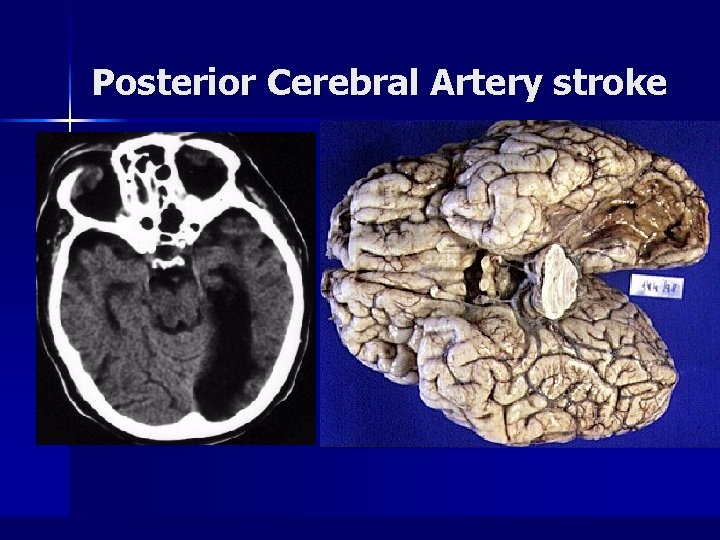
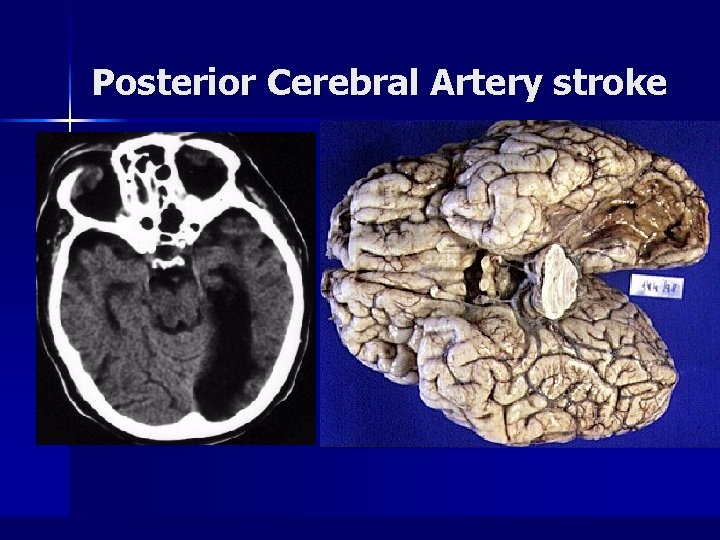
Posterior Cerebral Artery stroke
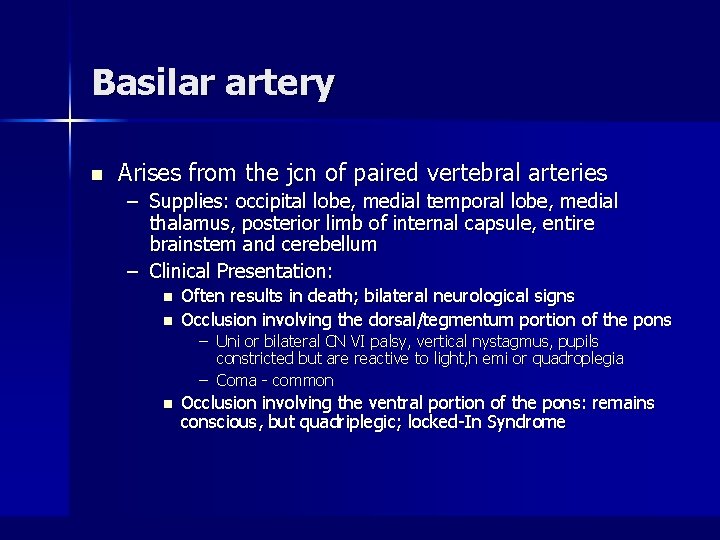
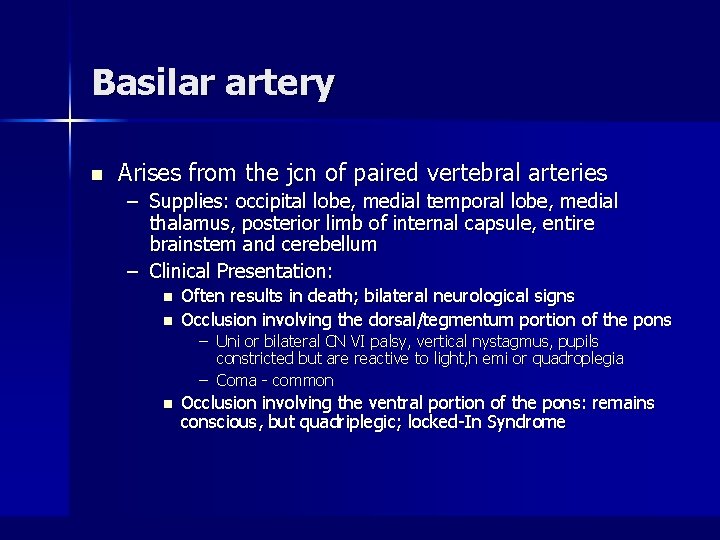
Basilar artery n Arises from the jcn of paired vertebral arteries – Supplies: occipital lobe, medial temporal lobe, medial thalamus, posterior limb of internal capsule, entire brainstem and cerebellum – Clinical Presentation: n n Often results in death; bilateral neurological signs Occlusion involving the dorsal/tegmentum portion of the pons – Uni or bilateral CN VI palsy, vertical nystagmus, pupils constricted but are reactive to light, h emi or quadroplegia – Coma - common n Occlusion involving the ventral portion of the pons: remains conscious, but quadriplegic; locked-In Syndrome
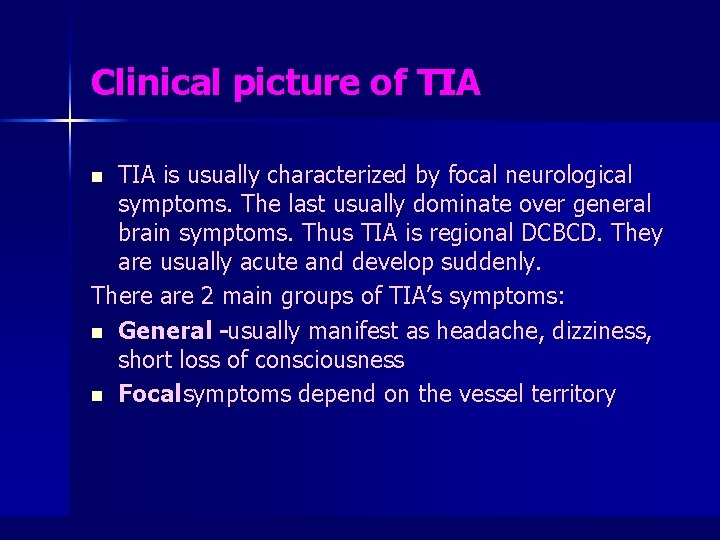
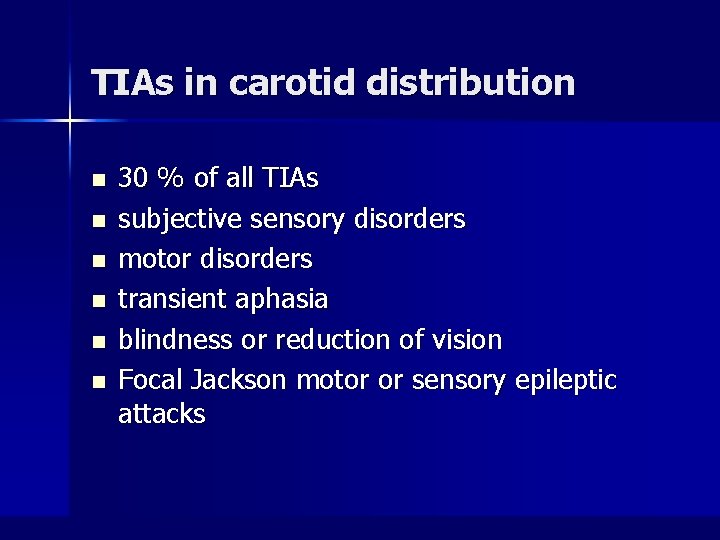
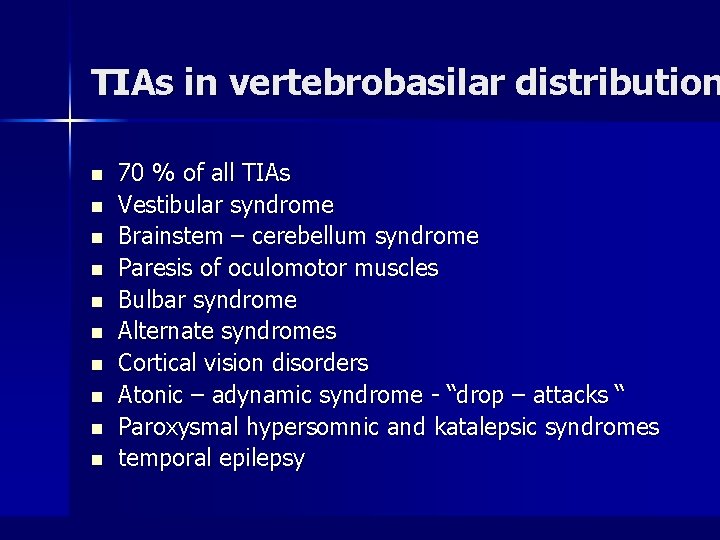
Clinical picture of TIA is usually characterized by focal neurological symptoms. The last usually dominate over general brain symptoms. Thus TIA is regional DCBCD. They are usually acute and develop suddenly. There are 2 main groups of TIA’s symptoms: n General -usually manifest as headache, dizziness, short loss of consciousness n Focal symptoms depend on the vessel territory n
TIAs in carotid distribution n n n 30 % of all TIAs subjective sensory disorders motor disorders transient aphasia blindness or reduction of vision Focal Jackson motor or sensory epileptic attacks
TIAs in vertebrobasilar distribution n n 70 % of all TIAs Vestibular syndrome Brainstem – cerebellum syndrome Paresis of oculomotor muscles Bulbar syndrome Alternate syndromes Cortical vision disorders Atonic – adynamic syndrome - “drop – attacks “ Paroxysmal hypersomnic and katalepsic syndromes temporal epilepsy
Diagnostic tests
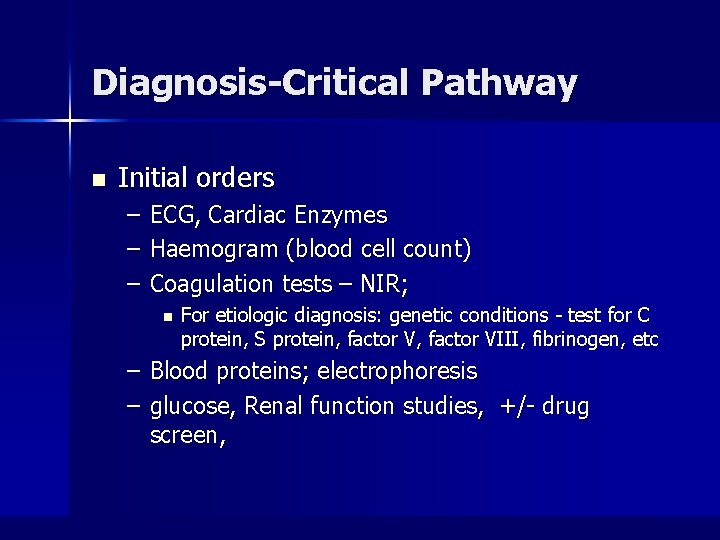
Diagnosis-Critical Pathway n Initial orders – – – ECG, Cardiac Enzymes Haemogram (blood cell count) Coagulation tests – NIR; n For etiologic diagnosis: genetic conditions - test for C protein, S protein, factor VIII, fibrinogen, etc – Blood proteins; electrophoresis – glucose, Renal function studies, +/- drug screen,
Diagnostic Tests n Noncontrast CT of head – Differentiate hemorrhage vs ischemia n MOST ischemic strokes are negative by CT for at least 6 hrs – Hypodensity indicating infarct seen 24 -48 hrs n n Can identify hemorrhage greater than 1 cm, and 95% of SAH If CT is negative, but still considering SAH may do lumbar punction
Diagnostic Tests n Depending on circumstances, other helpful tests – Echocardiogram – identifies mural thrombus, tumor, valvular vegetations in suspected cardioembolic stroke – Echography of arteries in the neck (Doppler, duplex) n n finds out the absence or presence of stenosis and occlusions of magistral arteries of head and neck. dissection
– Angiography – “gold standard” identifies occlusion or stenosis of large and small vessels of head/neck, dissections and aneurysms n Angio CT, MRA scan – identifies large vessel occlusions – may replace angiography in the future – MRI scan – identifies posterior circulation strokes better and ischemic strokes earlier than CT n Emergent MRI- considered for suspected brainstem lesion or dural sinus thrombosis – MRI techniques for recent ischemic stroke – allow rapid confirmation for thrombolysis
Additional methods of medical examination n Ultrasonic evaluation of carotids, verteral arteries – – – Absence or presence of stenosis and occlusions Degree of obstruction of the blood vessel Type of plaques, risk of emboli formations
Ischemic Stroke Management n General Management – General support measures n n n IV, oxygen, monitor, elevate head of bed slightly Treat dehydration and hypotension Avoid overhydration – cerebral edema Avoid IVF with glucose – except if hypoglycemic Fever – worsens neurologic deficits Hypertension – Treatment indicated for SBP > 220 mm Hg or mean arterial pressure > 130 mm Hg n n n Lowering BP too much reduces perfusion to penumbra converting reversible injury to infarction Use easily titratable Rx (labetalol or enalaprilat) SL Ca-channel blockers should be avoided
Management of HTN cont. n n Thrombolytic candidates- use NTG paste or Labetalol to reduce BP < 185/115 to allow tx Requirements for more aggressive treatment exclude the use of tissue plasminogen activator.
Thrombolysis Background n NIH/NINDS study – 624 patients, trial with I. V. t. PA vs placebo n Treatment w/in 3 hrs of onset – At 3 months, pts treated with t. PA were at least 30% more likely to have minimal/no disability; absolute favorable outcome in 11 -13 percent – 6. 4% of patients treated with t. PA developed symptomatic ICH compared with 0. 6% in placebo group – Mortality rate at 3 months not significantly different – t. PA group had significantly less disability – FDA approved in 1996
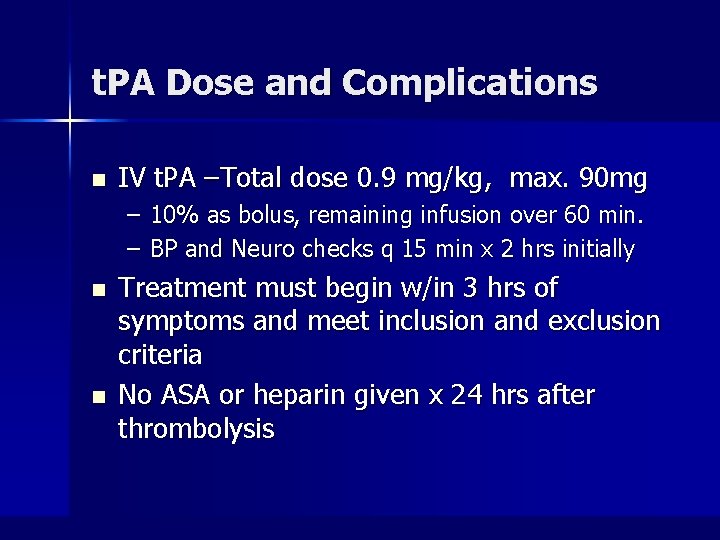
t. PA Dose and Complications n IV t. PA –Total dose 0. 9 mg/kg, max. 90 mg – 10% as bolus, remaining infusion over 60 min. – BP and Neuro checks q 15 min x 2 hrs initially n n Treatment must begin w/in 3 hrs of symptoms and meet inclusion and exclusion criteria No ASA or heparin given x 24 hrs after thrombolysis
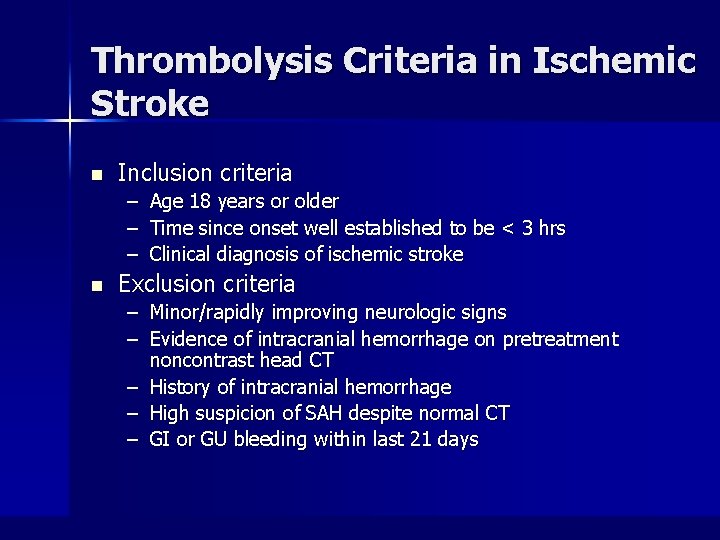
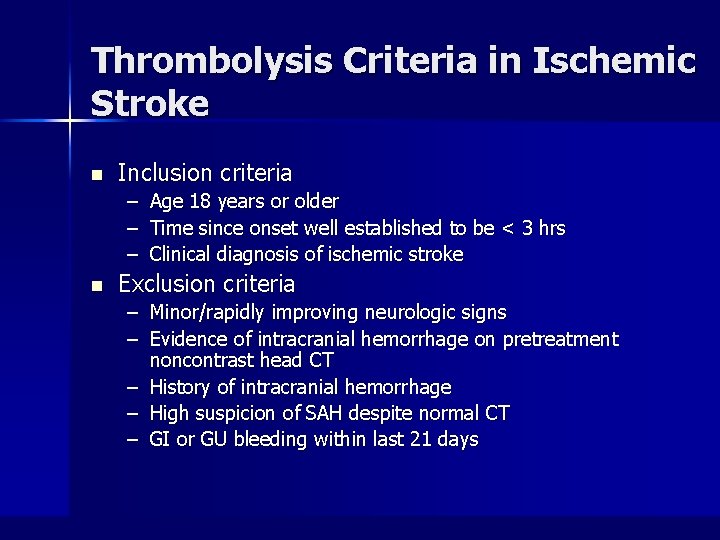
Thrombolysis Criteria in Ischemic Stroke n Inclusion criteria – Age 18 years or older – Time since onset well established to be < 3 hrs – Clinical diagnosis of ischemic stroke n Exclusion criteria – Minor/rapidly improving neurologic signs – Evidence of intracranial hemorrhage on pretreatment noncontrast head CT – History of intracranial hemorrhage – High suspicion of SAH despite normal CT – GI or GU bleeding within last 21 days
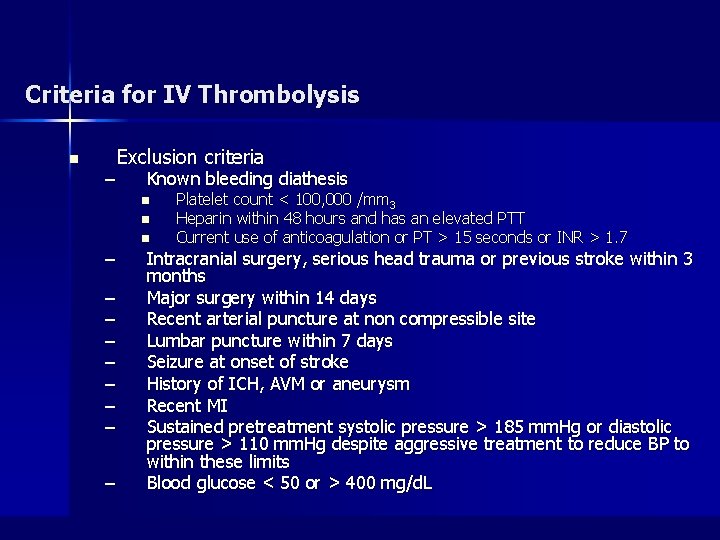
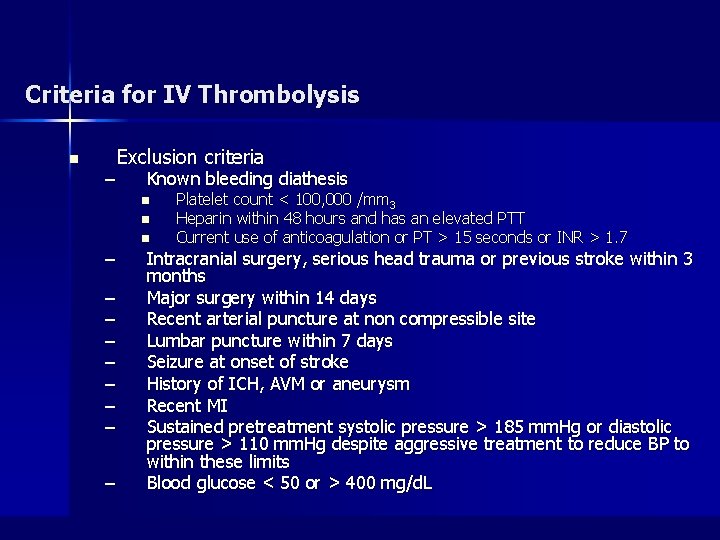
Criteria for IV Thrombolysis n – Exclusion criteria Known bleeding diathesis n n – – – – – n Platelet count < 100, 000 /mm 3 Heparin within 48 hours and has an elevated PTT Current use of anticoagulation or PT > 15 seconds or INR > 1. 7 Intracranial surgery, serious head trauma or previous stroke within 3 months Major surgery within 14 days Recent arterial puncture at non compressible site Lumbar puncture within 7 days Seizure at onset of stroke History of ICH, AVM or aneurysm Recent MI Sustained pretreatment systolic pressure > 185 mm. Hg or diastolic pressure > 110 mm. Hg despite aggressive treatment to reduce BP to within these limits Blood glucose < 50 or > 400 mg/d. L
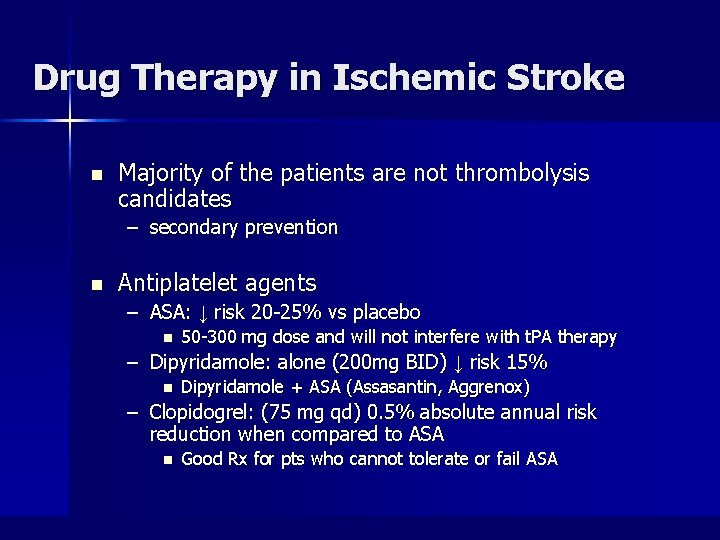
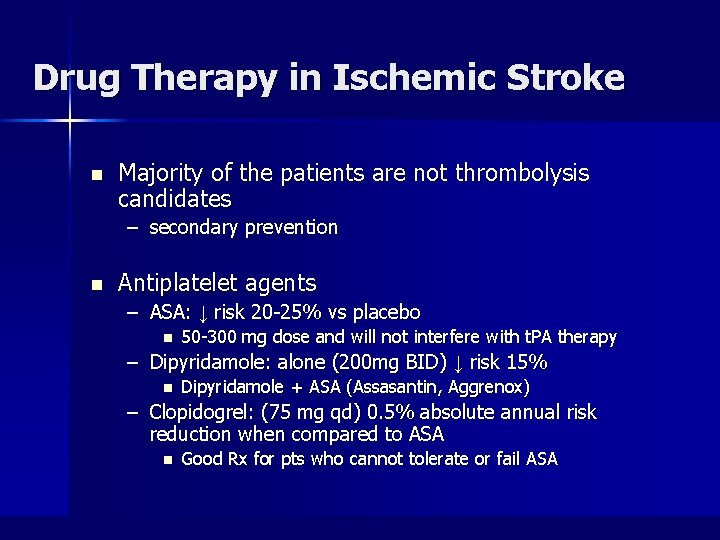
Drug Therapy in Ischemic Stroke n Majority of the patients are not thrombolysis candidates – secondary prevention n Antiplatelet agents – ASA: ↓ risk 20 -25% vs placebo n 50 -300 mg dose and will not interfere with t. PA therapy – Dipyridamole: alone (200 mg BID) ↓ risk 15% n Dipyridamole + ASA (Assasantin, Aggrenox) – Clopidogrel: (75 mg qd) 0. 5% absolute annual risk reduction when compared to ASA n Good Rx for pts who cannot tolerate or fail ASA
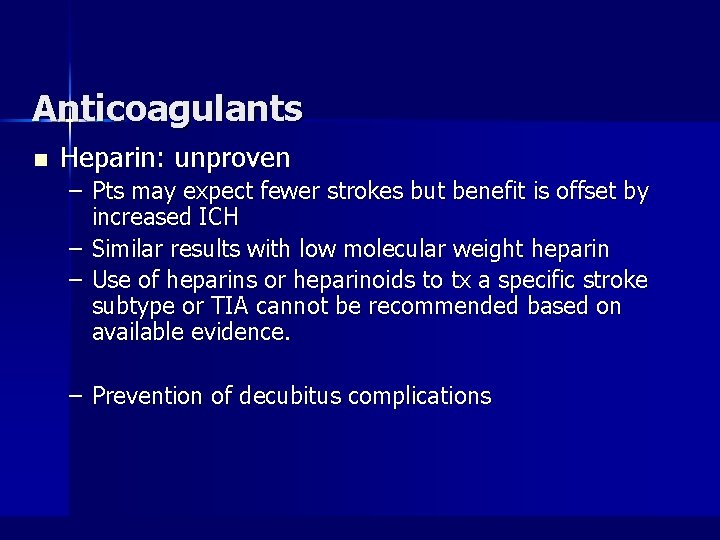
Anticoagulants n Heparin: unproven – Pts may expect fewer strokes but benefit is offset by increased ICH – Similar results with low molecular weight heparin – Use of heparins or heparinoids to tx a specific stroke subtype or TIA cannot be recommended based on available evidence. – Prevention of decubitus complications
Drug Therapy in Ischemic Stroke n Cerebral vasodilators: – vincamine, vinpocetine, nicergoline, pentoxifylline – Ginkgo biloba n Cerebral trophic agents – Pyracetam, pramiracetam – Cerebrolysin, Actovegin