Stroke Mark Sudlow Consultant and Senior Lecturer Stroke





- Slides: 35
Stroke Mark Sudlow Consultant and Senior Lecturer Stroke Northumbria/NHCT/University of Newcastle
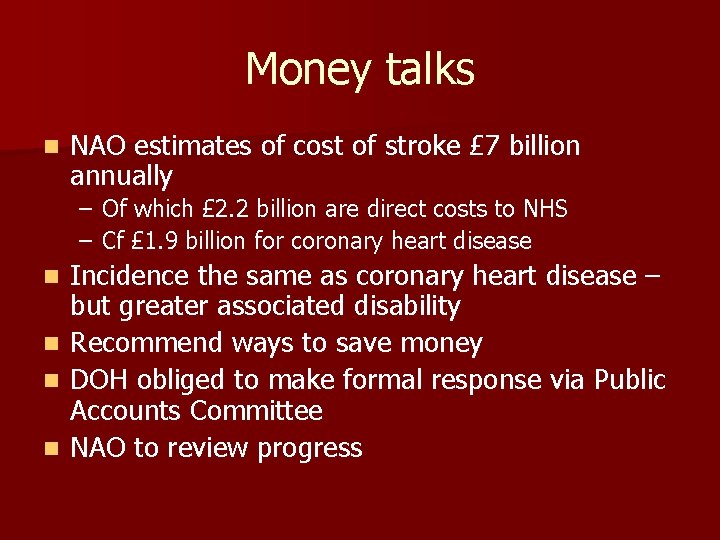
Money talks n NAO estimates of cost of stroke £ 7 billion annually – Of which £ 2. 2 billion are direct costs to NHS – Cf £ 1. 9 billion for coronary heart disease Incidence the same as coronary heart disease – but greater associated disability n Recommend ways to save money n DOH obliged to make formal response via Public Accounts Committee n NAO to review progress n
NAO Recommend n Faster access to specialist care for patients with TIA – High risk on same day – Lower risk within a week maximum n Faster access to specialist stroke care – Acute stroke units – Early scanning – 24 hours maximum – Thrombolysis - ? 10% target and timed benchmarks for onset to needle n Better long term care provision
Response from DOH n Stroke is no longer under Elderly or Long Term Conditions but under Vascular Disease n Working parties set up to look at recommendations on changing provision of care n NICE asked to fast track guidelines n Intercollegiate Acute Stroke and TIA Guidelines

Transient Ischaemic Attack High early risk and effective early treatment
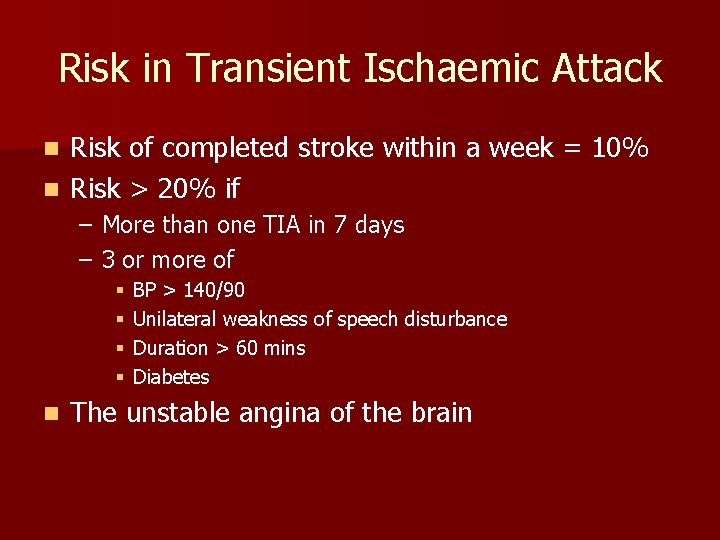
Risk in Transient Ischaemic Attack Risk of completed stroke within a week = 10% n Risk > 20% if n – More than one TIA in 7 days – 3 or more of § § n BP > 140/90 Unilateral weakness of speech disturbance Duration > 60 mins Diabetes The unstable angina of the brain
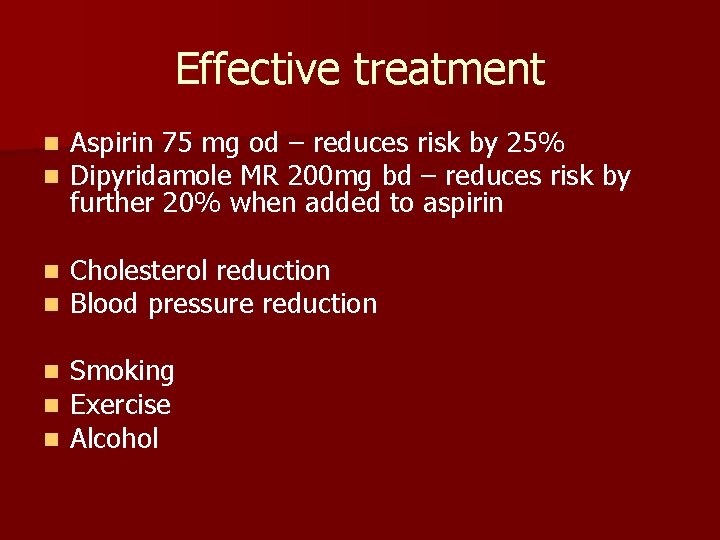
Effective treatment n n Aspirin 75 mg od – reduces risk by 25% Dipyridamole MR 200 mg bd – reduces risk by further 20% when added to aspirin n n Cholesterol reduction Blood pressure reduction n Smoking Exercise Alcohol
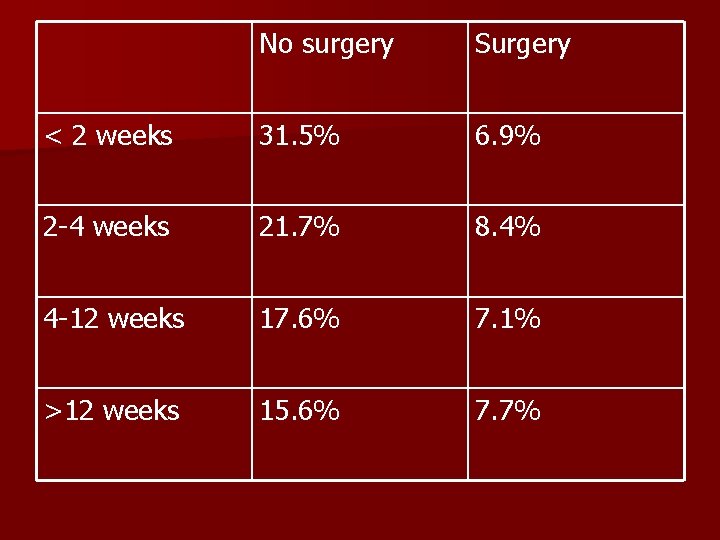
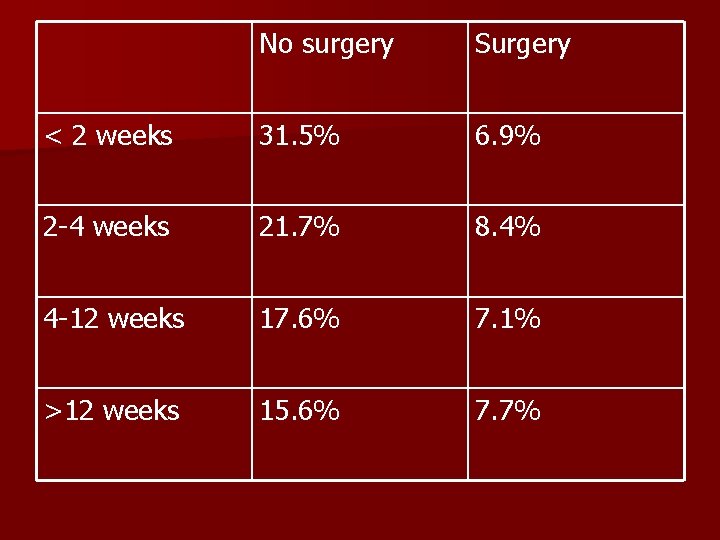
No surgery Surgery < 2 weeks 31. 5% 6. 9% 2 -4 weeks 21. 7% 8. 4% 4 -12 weeks 17. 6% 7. 1% >12 weeks 15. 6% 7. 7%
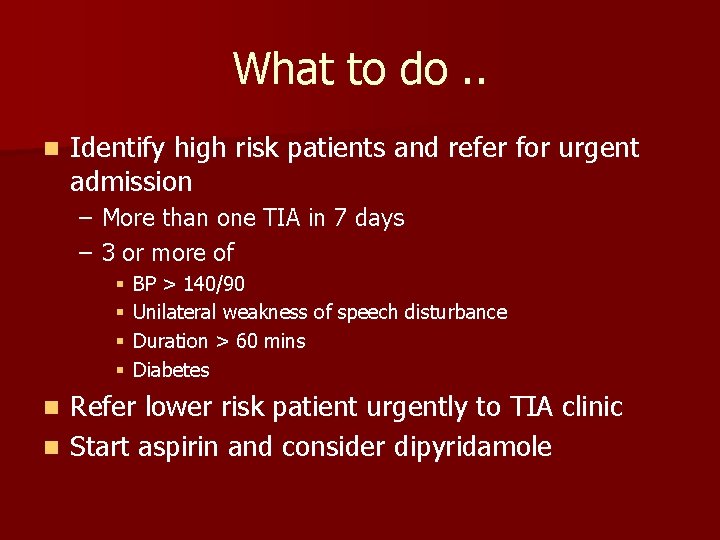
What to do. . n Identify high risk patients and refer for urgent admission – More than one TIA in 7 days – 3 or more of § § BP > 140/90 Unilateral weakness of speech disturbance Duration > 60 mins Diabetes Refer lower risk patient urgently to TIA clinic n Start aspirin and consider dipyridamole n
What we will do. . n Admit high risk patients n See lower risk patients within a week of referral – Start treatment – Arrange urgent imaging – Refer to vascular surgery – where they will be seen within a couple of days – – – Start treatment Information Lifestyle advice Arrange imaging Refer to vascular surgery – where they will be seen within two weeks
Acute Stroke FAST response allows life saving treatment
Evidence for specialist care n Clear evidence that hospitalisation and treatment by a coordinated specialist team improves mortality and outcome – Absolute improvement of 10% n Increasing evidence that early specialist care is the key

Evidence for early aspirin n 1% absolute reduction in recurrence and mortality if given within 24 hours n Requires CT scan to exclude haemorrhage
Evidence for thrombolysis n Within 3 hours of onset of symptoms n With CT scan showing no haemorrhage n 10% absolute improvement in number of patients with minimal disability
What to do. . n If a patient presents or calls with symptoms suggesting acute stroke n Call an ambulance
What we will do. . n If a patient presents with stroke within thrombolysis window – Immediate referral to stroke specialist – Immediate scanning – Thrombolysis n If a patient present outside that window – – – Admit to specialist stroke ward CT scan within 24 hours Preventative treatment started early Coordinated specialist assessment and rehabilitation Information Lifestyle advice
Secondary Prevention Need for risk reduction as for any high risk vascular disease With a few minor additions
n Risk of MI, cardiac death and further stroke is similar to after MI n Strategies are broadly similar

n Aspirin n Statin n Blood pressure – best evidence is for ACE and thiazide

Stroke specific Dipyridamole MR 200 mg bd for at least 2 years n Risk of further stroke is particularly high with atrial fibrillation n – 15% absolute per annum – Benefits of warfarin highest in this group n Risk of further stroke is particularly high with carotid stenosis – Carotid ultrasound and intervention if good recovery – Particularly important in partial anterior circulation strokes
What to do. . n Annual check – Antiplatelets – Blood pressure – Cholesterol – Lifestyle
What we will do. . n Arrange ongoing rehabilitation n Outpatient check at 6 weeks (as an inpatients if not discharged) n Outpatient check at six months
Life After Stroke Isolation and Dependency
n Information n Inclusion of function and mood in annual screening n Access to social services and rehabilitation review

How it should be
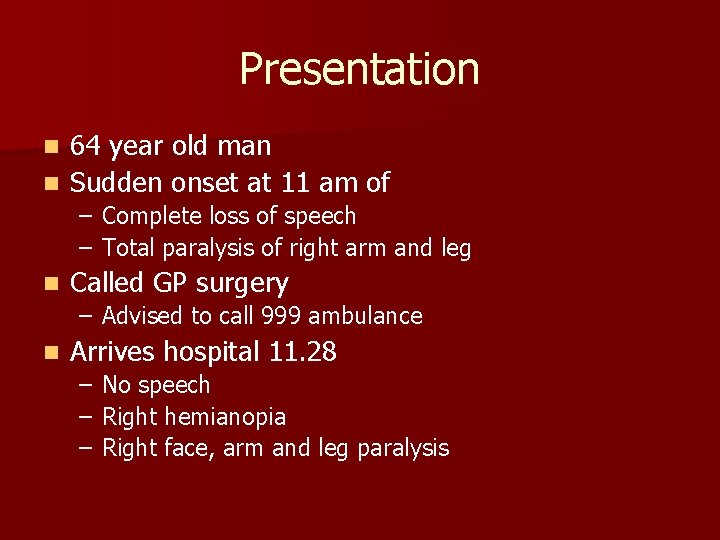
Presentation 64 year old man n Sudden onset at 11 am of n – Complete loss of speech – Total paralysis of right arm and leg n Called GP surgery – Advised to call 999 ambulance n Arrives hospital 11. 28 – No speech – Right hemianopia – Right face, arm and leg paralysis
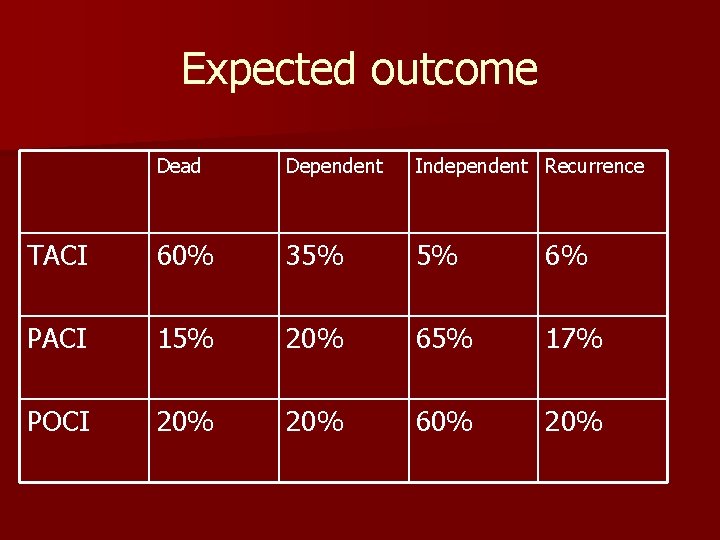
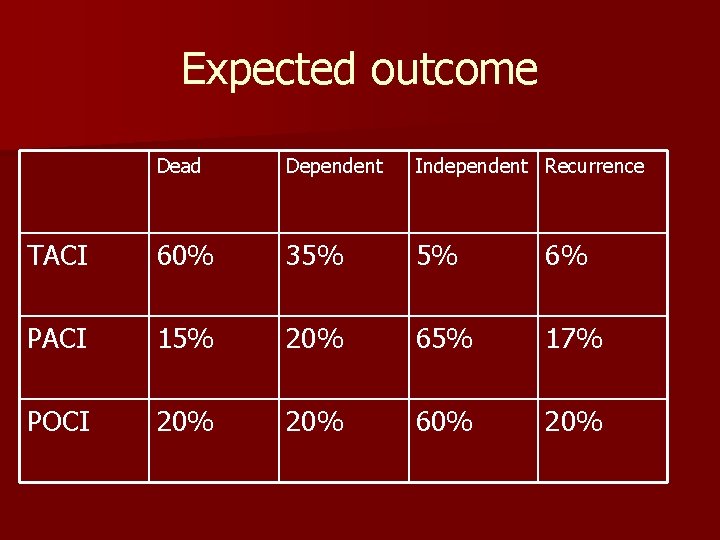
Expected outcome Dead Dependent Independent Recurrence TACI 60% 35% 5% 6% PACI 15% 20% 65% 17% POCI 20% 60% 20%
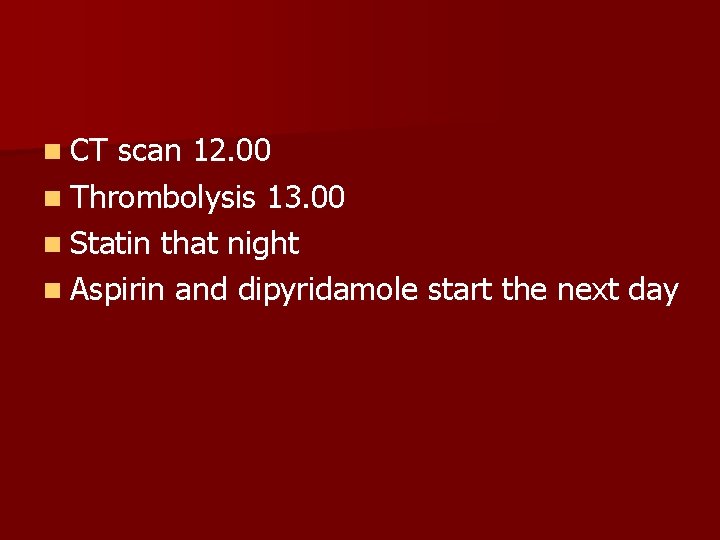
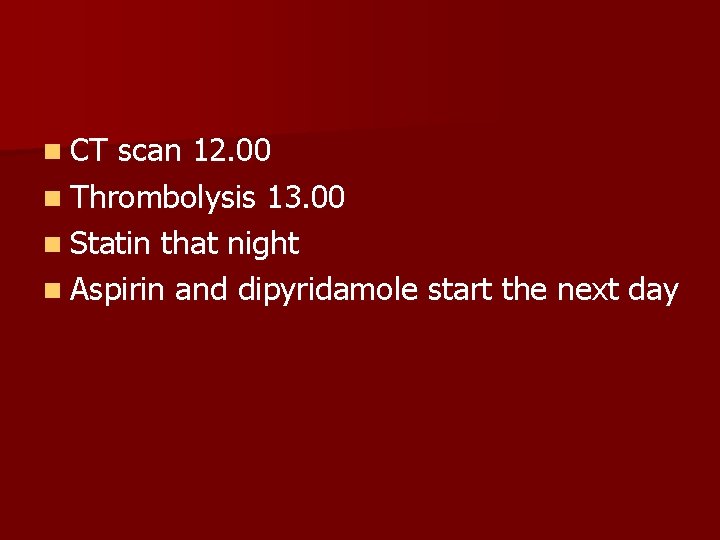
n CT scan 12. 00 n Thrombolysis 13. 00 n Statin that night n Aspirin and dipyridamole start the next day
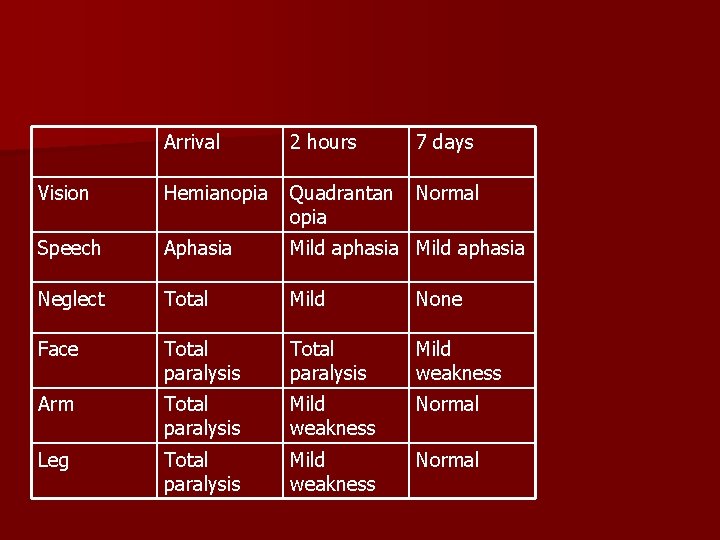
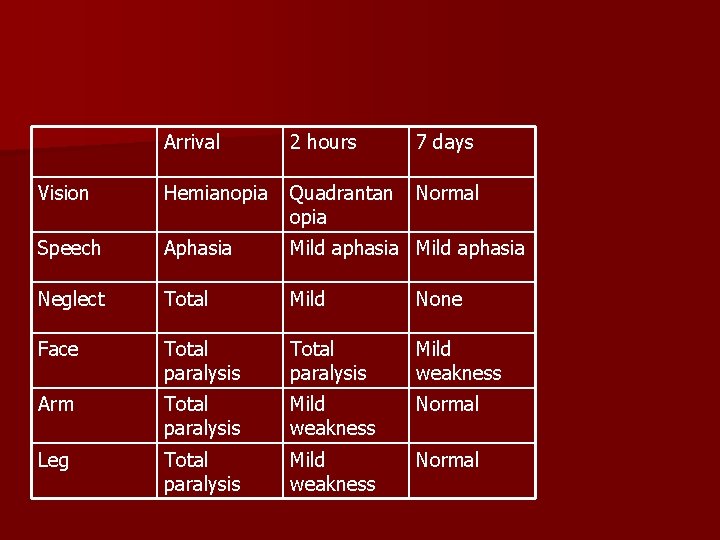
Arrival 2 hours 7 days Vision Hemianopia Quadrantan opia Normal Speech Aphasia Mild aphasia Neglect Total Mild None Face Total paralysis Mild weakness Arm Total paralysis Mild weakness Normal Leg Total paralysis Mild weakness Normal
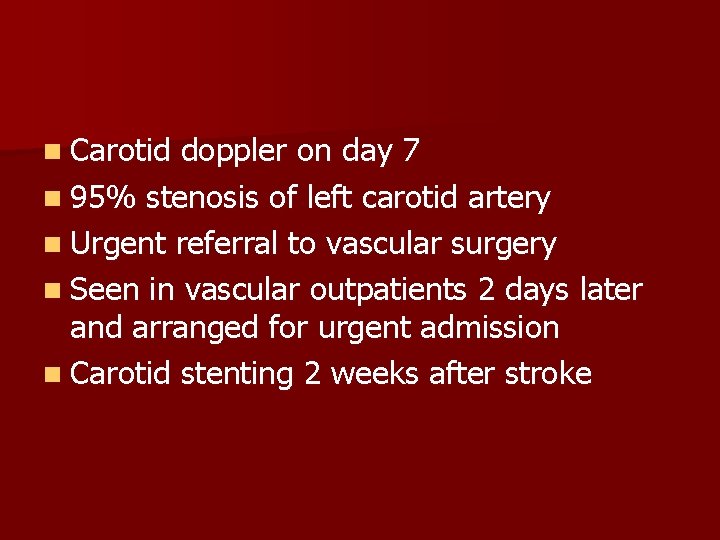
n Carotid doppler on day 7 n 95% stenosis of left carotid artery n Urgent referral to vascular surgery n Seen in vascular outpatients 2 days later and arranged for urgent admission n Carotid stenting 2 weeks after stroke
Out of stroke unit by 10 days n Out after carotid intervention by 2 weeks after stroke n n On treatment with – – – Aspirin Dipyridamole Simvastatin Perindopril Bendroflumethiazide
n Cholesterol 3. 2 n Blood pressure 128/76 n Stopped smoking n Complete recovery n Minimal ongoing risk
n With a coordinated approach from – – – n Ambulance service Primary care Emergency care Stroke service Vascular surgeons We can do this
n And save money