Streptococcus pneumoniae pneumococus Pneumonia Meningitis bacteraemia Description Grampositive
Streptococcus pneumoniae pneumococus Pneumonia Meningitis bacteraemia
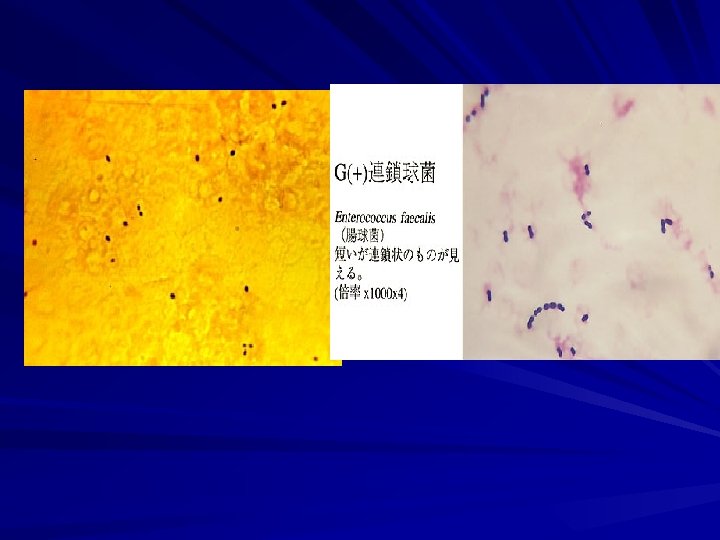
Description Gram-positive diplococci (in pairs) Encapsulated ovoid or lanceolate coccus Non-motile Fastidious (enriched media) – Blood or chocolate agar – 5 -10 % CO 2 Alpha haemolysis + draughtsman appearance Some strains are mucoid Soluble in bile Optochin sensitive
Pathogenesis Virulence factors – Capsular polysaccharide The major factor 84 serotypes Both antigenic and type specific Antiphagocytic Serotype 3 , 7 are most virulent 90% of cases of bacteraemic pneumococcal pneumonia and meningitis are caused by 23 serotypes Quellung reaction , india ink – Pneumolysin Membrane damaging toxin
Carrier rate – Oropharyngeal flora of 5 – 70% of the population – Significance in respiratory infection
Predisposing factors – Aspiration of upper airway secretions ( endogenous ) – No person-person spread – Disturbed consciousness , general anaesthesia , convulsions , CVA , epilepsy , head trauma – Prior LRT. VIRAL infection – Preexisting respiratory diseases , smoking Chronic bronchitis , bronchogenic malignancy – – – Chronic heart disease Chronic renal disease ( nephrotic syndrome ) Chronic liver disease ( cirrhosis) Diabetes mellitus Old age , (extreme of age ) Malnutrition , alcoholism
Specific deficiencies in host defence – Hypogamaglobulinaemia – Asplenia , hypospenism ( tuftsin ) – Homozygous sickle cell disease – Coeliac disease – Multiple myeloma , leukaemia , lymphomas – Neutropenia – HIV Relative or absolute deficiency of opsonic antibody or inadequate manufacture of type specific antibody
Diseases Respiratory tract infections – – – Lobar pneumonia ( commonest cause of CAP ) Empyema Otitis media (6 months – 3 yrs ) Mastoiditis Sinusitis Acute exacerbation of chronic bronchitis Meningitis Conjunctivitis Peritonitis ( primary ) Bacteraemia ( 15 % of pneumonia ) septicaemia
Clinical feature Lobar pneumonia – Sudden onset – Fever – rigor – Cough , rusty sputum – Pleural pain – Signs of lobar consolidation – Polymorphonuclear leucocytosis – Empyema , pericarditis
Meningitis – The most virulent pathogen of meningitis – Mortality ( 20% ) – Primary – Complicate infections at other site ( lung ) – Bacteraemia usually coexists – Bimodal incidence ( < 3 yr - > 45 yr )
Mortality Age (> 65 yr ) Preexisting disease Bacteraemia Serotype 3 , 7
Laboratory diagnosis Specimen – Sputum – CSF – Swabs – Pus – Blood culture – Aspirate
Microscopy – Gram stained smear Gram-positive diplococci + pus cells culture Blood agar , chocolate agar + 10 % CO 2 identification Alph-haemolytic colonies Optochin sensitive Bile soluble
Sensitivity testing – Penicillin – susceptible Sensitive – Nonsusceptible Intermediate Resistant – – – – Ampicillin , amoxicillin Erythromycin Ceftriaxone , cefuroxime Clindamycin Fluroquinolones tetracyclines Vancomycin
Treatment Meningitis – Parenteral ceftriaxone + vancomycin pneumonia – Outpatients Erythromycin Amoxacillin – clavulanic acid Cefuroxime or ceftriaxone (IV) + oral b- lactam – Inpatients Parenteral cefuroxime or ceftriaxone
Prevention 23 polysaccharide vaccine – Not effective in children < 2 yrs – >65 yrs – Functional or anatomical asplenia – SCD 7 -valent – protein- conjugated vaccine – Children < 3 yrs


- Slides: 18