Streptococcus pneumoniae pneumococcus Streptococcus pneumoniae Classic example of

- Slides: 29
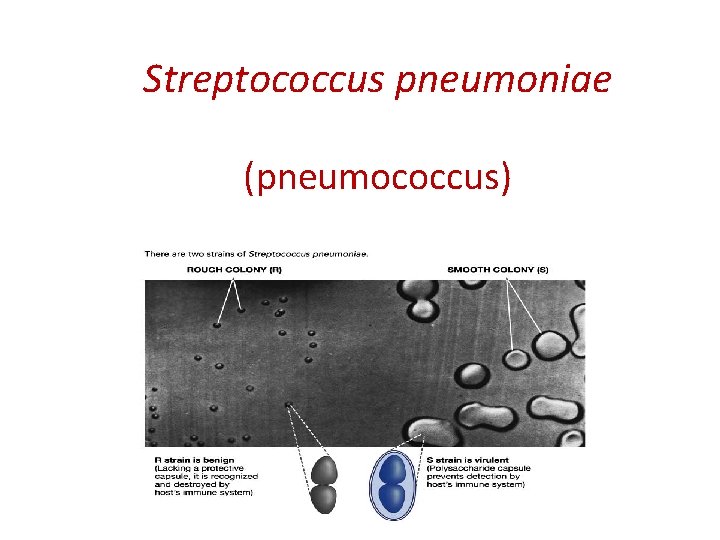
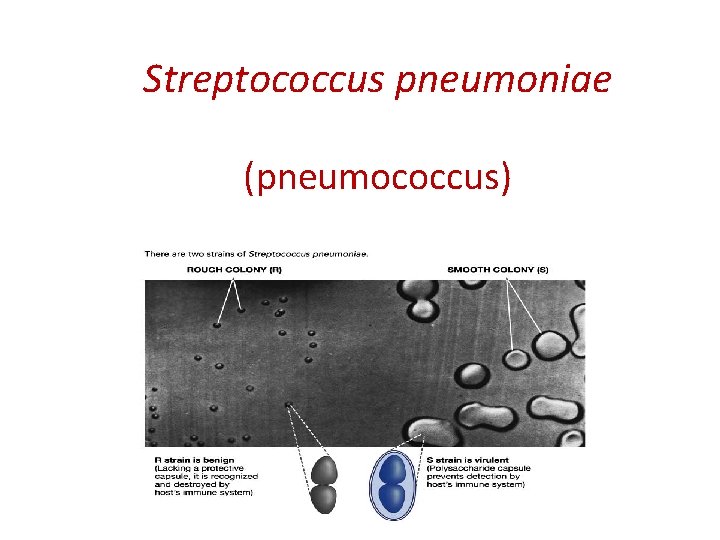
Streptococcus pneumoniae (pneumococcus)
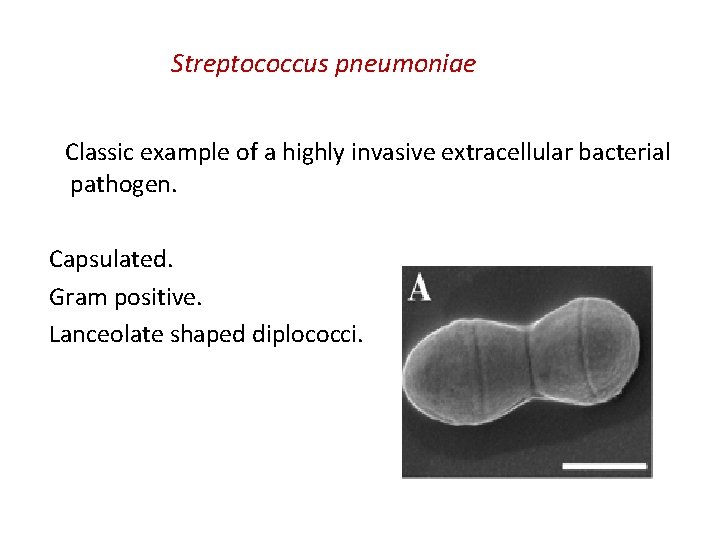
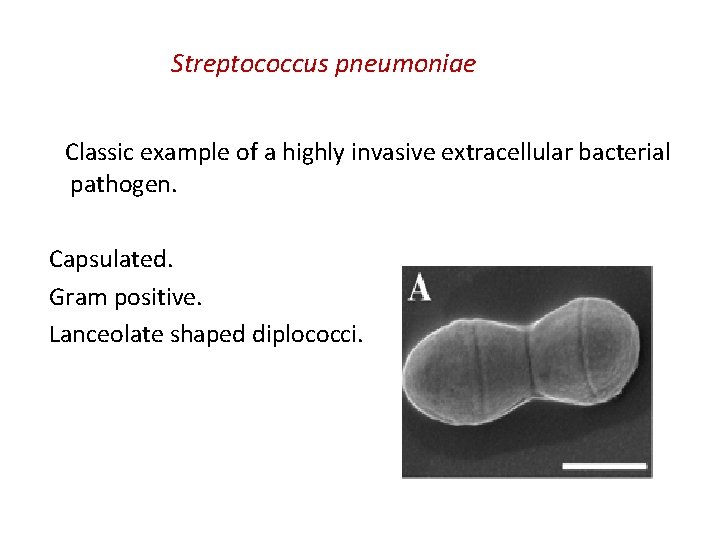
Streptococcus pneumoniae Classic example of a highly invasive extracellular bacterial pathogen. Capsulated. Gram positive. Lanceolate shaped diplococci.
It is a major cause of morbidity and mortality globally causing more deaths than any other infectious disease. Commonly a quiescent colonizer of the upper respiratory tract where up to 60% of small children may carry pneumococci in the nose asymptomatically. Diseases range from mild respiratory tract mucosal infections to more severe diseases.
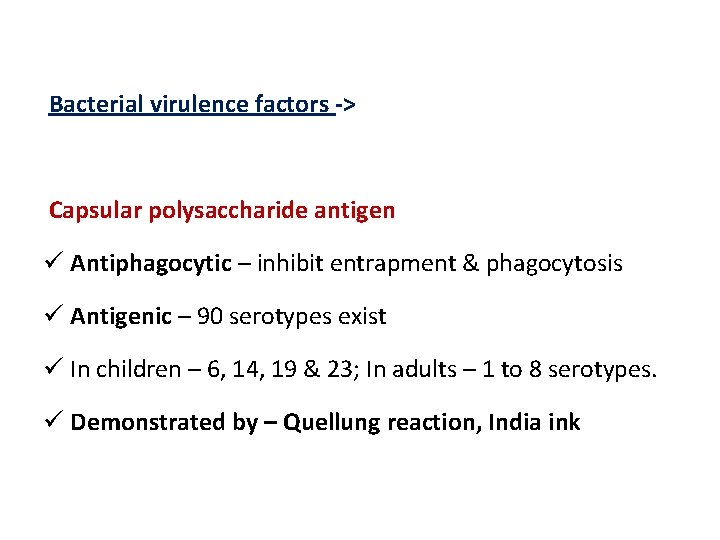
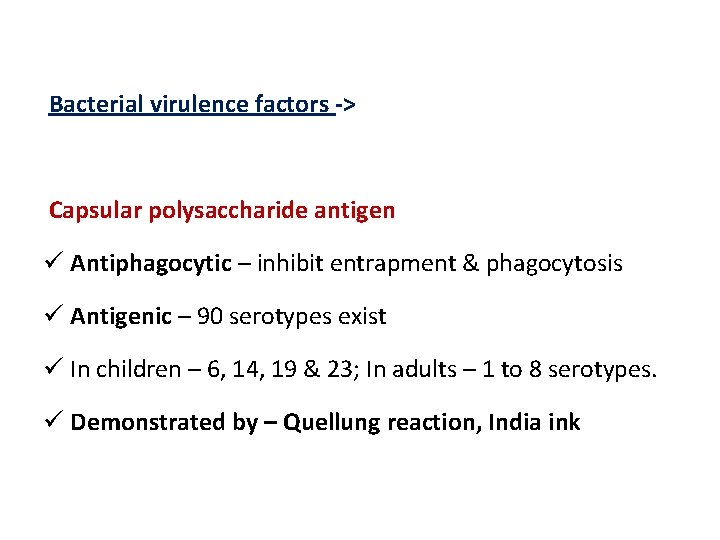
Bacterial virulence factors -> Capsular polysaccharide antigen ü Antiphagocytic – inhibit entrapment & phagocytosis ü Antigenic – 90 serotypes exist ü In children – 6, 14, 19 & 23; In adults – 1 to 8 serotypes. ü Demonstrated by – Quellung reaction, India ink
Lipoteichoic acid – activates complement and induces inflammatory cytokine production. Pneumolysin – a hemolysin causes α hemolysis & contributes to pathogenesis.
Pathogenesis -> 1. Source of infection: ü Exogenous – Patients / carriers -> shed organisms in their respiratory secretions. (40 – 70% of a population harbor pneumococci at some time during their lifetime). ü Endogenous – Part of the normal flora of URT. 2. Mode of infection – Inhalation of droplet nuclei or by direct / indirect contact.
3. Host predisposing factors Infection & carriage is common but disease occurs only under certain predisposing conditions. A. Abnormalities of the Respiratory tract a) Viral infections damaging surface cells. b) Abnormal accumulation of mucus – allergy. c) Bronchial obstruction – atelectasis. d) Respiratory tract injury due to irritants disturbing its muco-ciliary function.
B. Alcohol / Drug intoxication results in, i. Decreased phagocytic activity. ii. Decreased cough reflex. iii. Facilitates aspiration. C. Abnormal circulatory dynamics i. Pulmonary congestion. ii. Heart failure.
D. Other factors i. Malnutrition. ii. General debility. iii. Old age. iv. Sickle cell anemia. v. Hyposplenism. vi. Complement deficiency. vii. Convulsions.
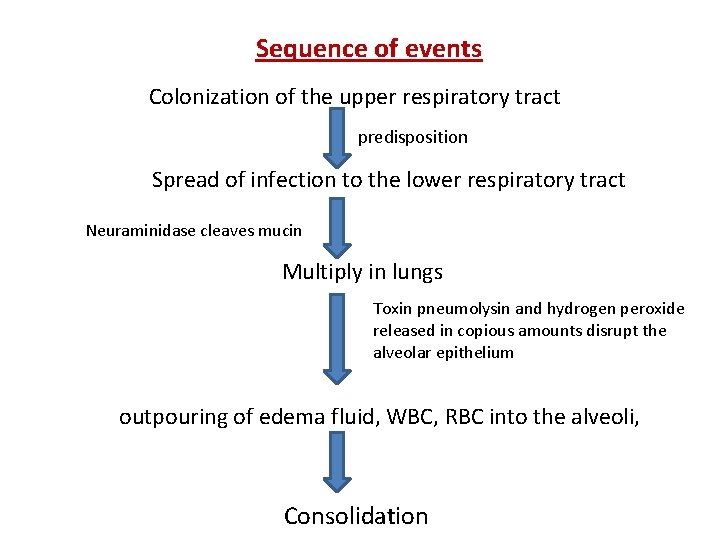
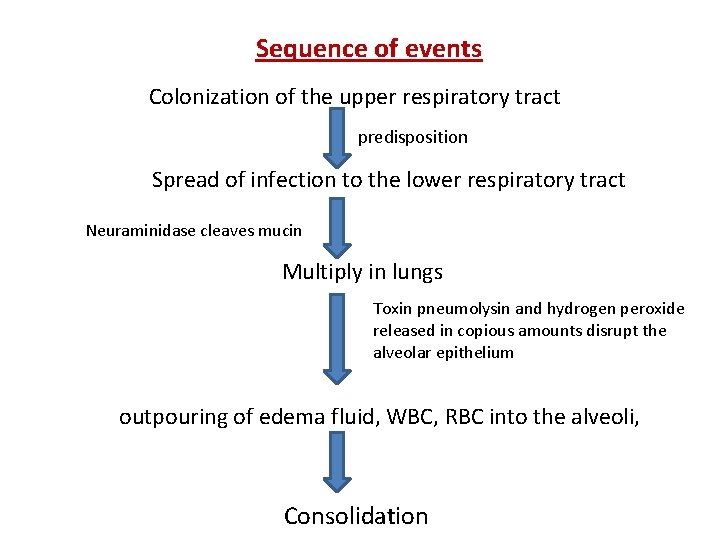
Sequence of events Colonization of the upper respiratory tract predisposition Spread of infection to the lower respiratory tract Neuraminidase cleaves mucin Multiply in lungs Toxin pneumolysin and hydrogen peroxide released in copious amounts disrupt the alveolar epithelium outpouring of edema fluid, WBC, RBC into the alveoli, Consolidation
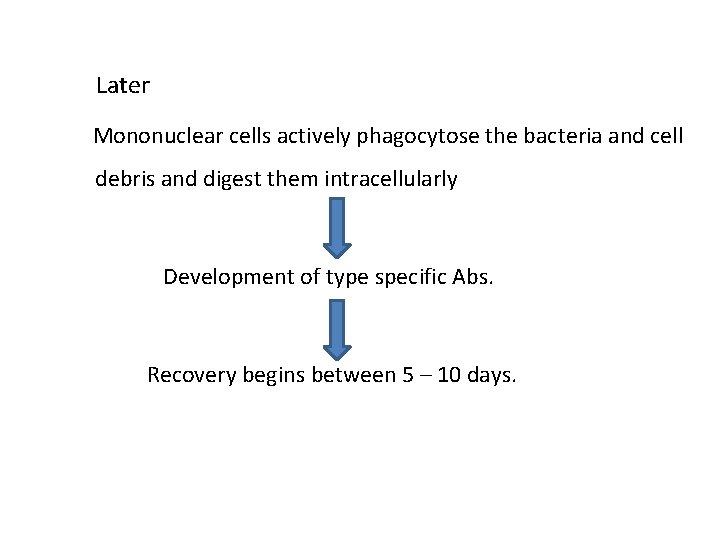
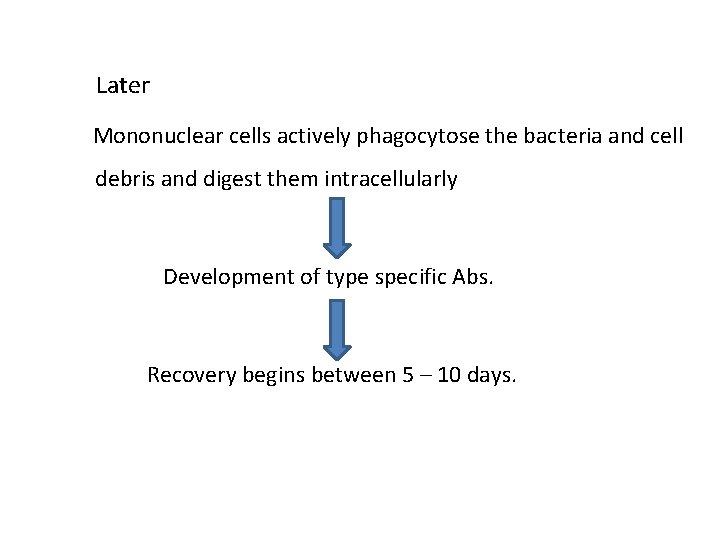
Later Mononuclear cells actively phagocytose the bacteria and cell debris and digest them intracellularly Development of type specific Abs. Recovery begins between 5 – 10 days.
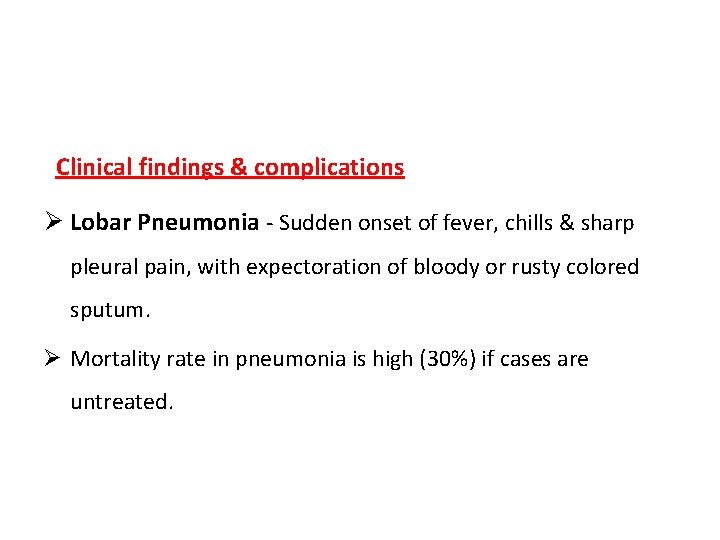
Clinical findings & complications Ø Lobar Pneumonia - Sudden onset of fever, chills & sharp pleural pain, with expectoration of bloody or rusty colored sputum. Ø Mortality rate in pneumonia is high (30%) if cases are untreated.
Ø Contiguous spread may result Middle ear infection (otitis). Mastoid (mastoiditis). Paranasal sinuses (sinusitis). Pus in pleural space (empyema) may require aspiration / drainage.
Ø bacteremia In 10 – 20% of patients occurs with metastatic involvement. Meninges (meningitis). joints (septic arthritis). Rarely, the endocardium (acute endocarditis).
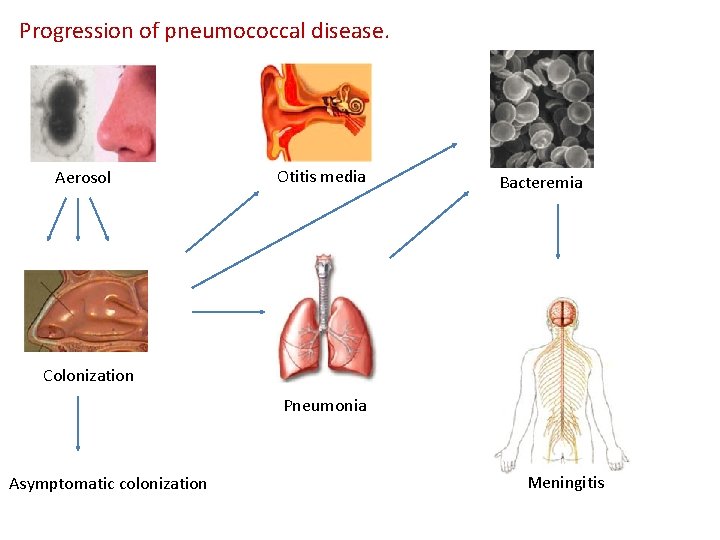
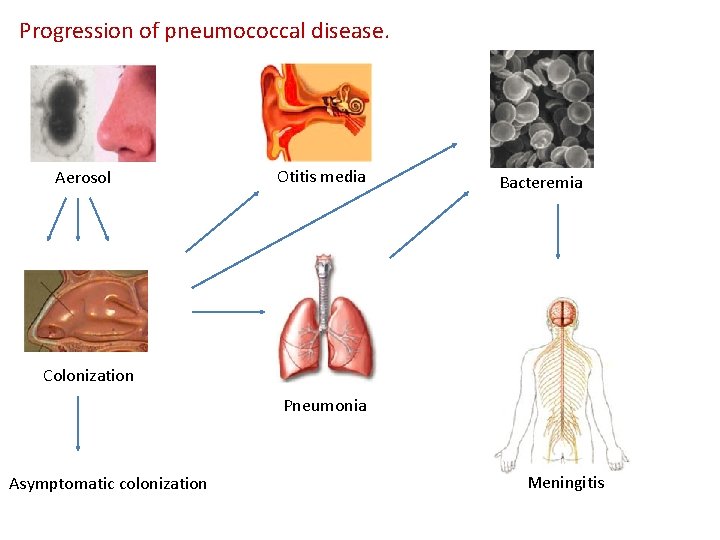
Progression of pneumococcal disease. Aerosol Otitis media Bacteremia Colonization Pneumonia Asymptomatic colonization Meningitis
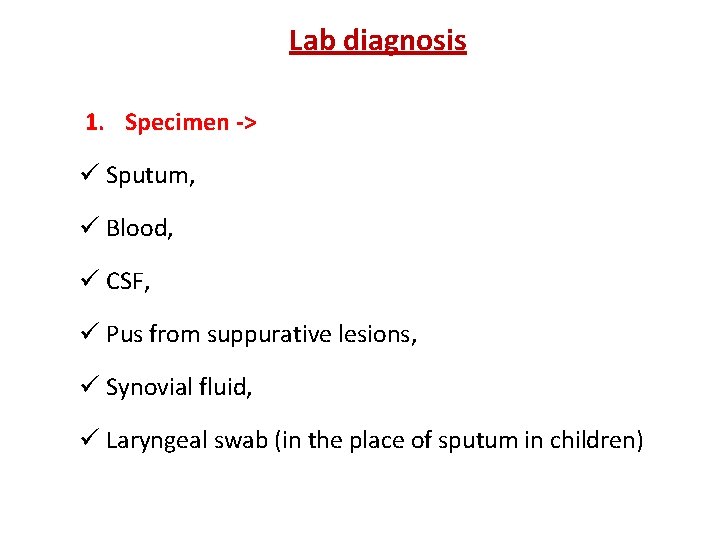
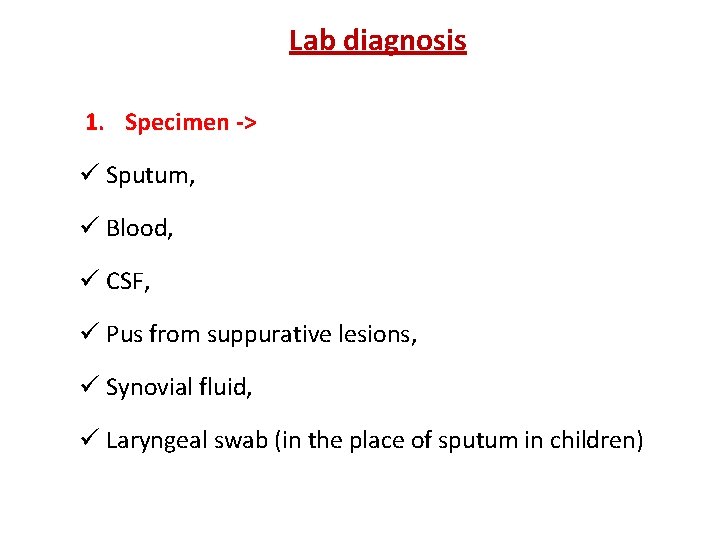
Lab diagnosis 1. Specimen -> ü Sputum, ü Blood, ü CSF, ü Pus from suppurative lesions, ü Synovial fluid, ü Laryngeal swab (in the place of sputum in children)
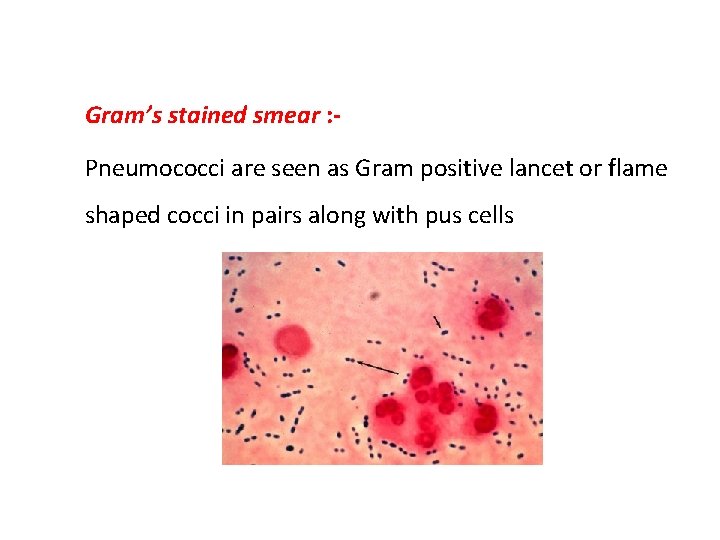
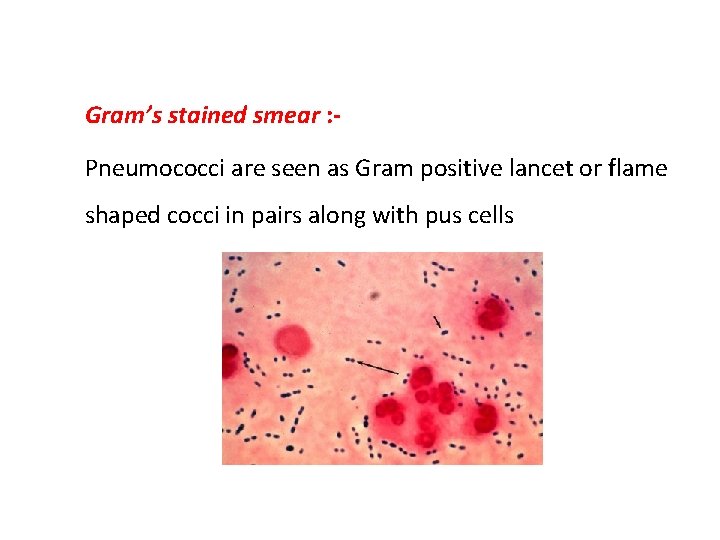
2. Microscopy -> Gram’s stained smear : Pneumococci are seen as Gram positive lancet or flame shaped cocci in pairs along with pus cells
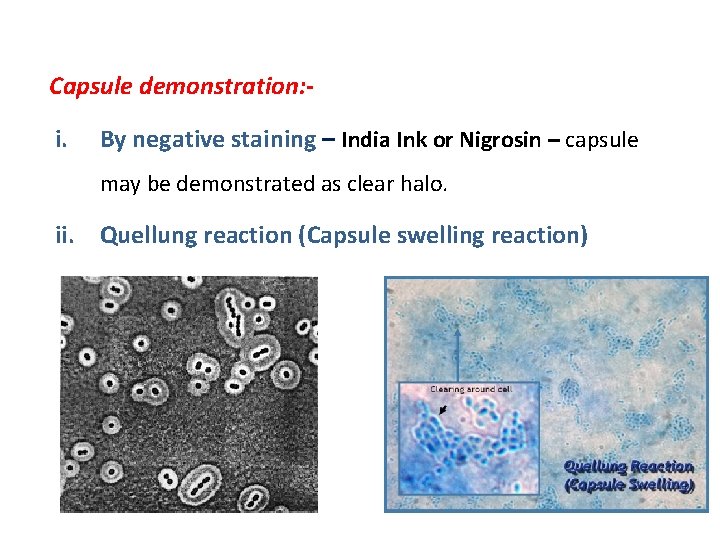
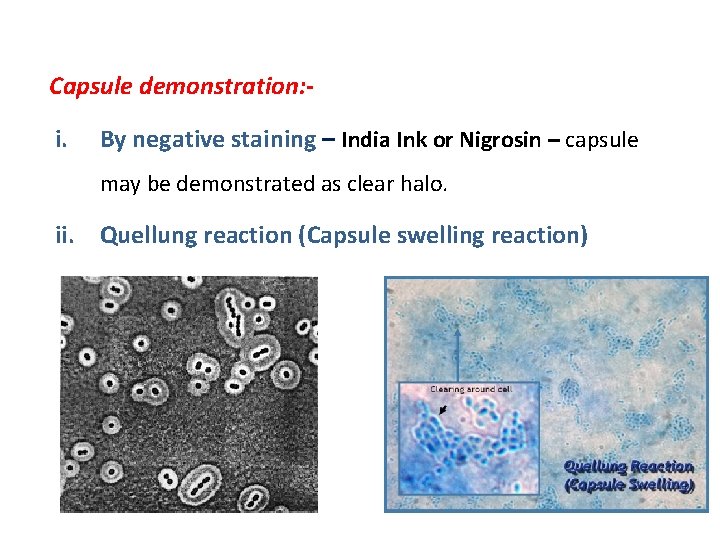
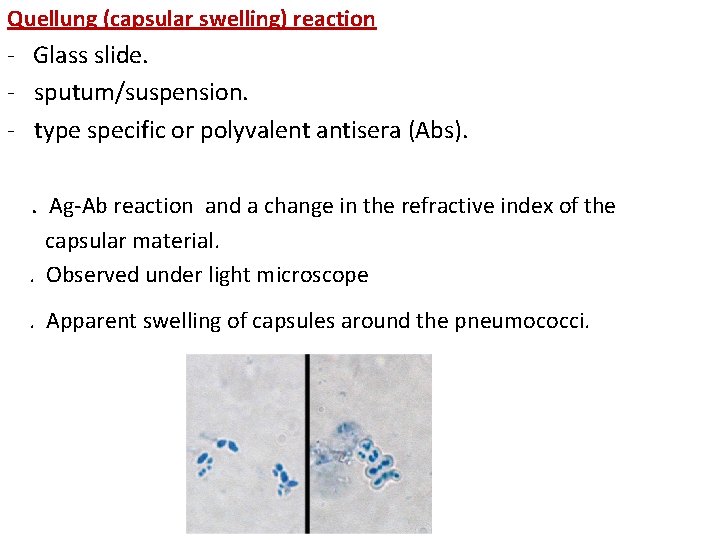
Capsule demonstration: - i. By negative staining – India Ink or Nigrosin – capsule may be demonstrated as clear halo. ii. Quellung reaction (Capsule swelling reaction)
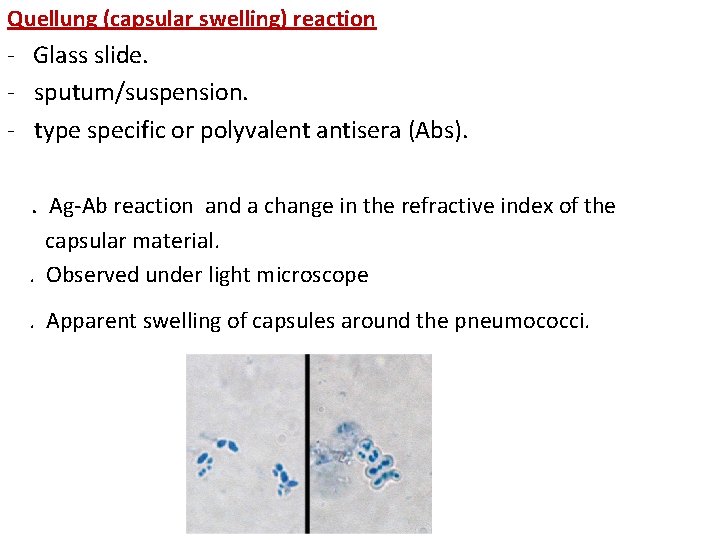
Quellung (capsular swelling) reaction - Glass slide. - sputum/suspension. - type specific or polyvalent antisera (Abs). . Ag-Ab reaction and a change in the refractive index of the capsular material. . Observed under light microscope. Apparent swelling of capsules around the pneumococci.
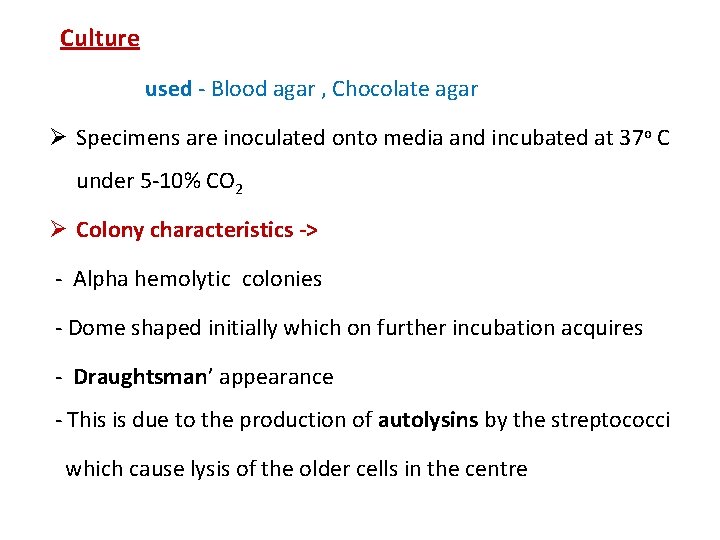
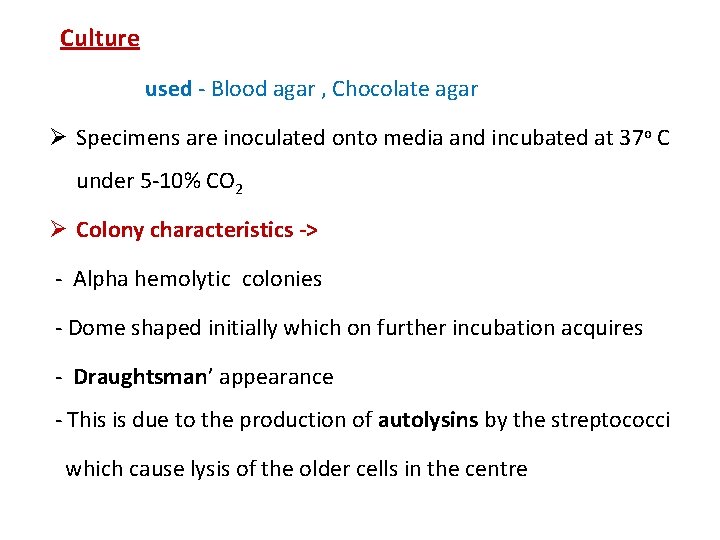
Culture Ø Media used - Blood agar , Chocolate agar Ø Specimens are inoculated onto media and incubated at 37 o C under 5 -10% CO 2 Ø Colony characteristics -> - Alpha hemolytic colonies - Dome shaped initially which on further incubation acquires - Draughtsman’ appearance - This is due to the production of autolysins by the streptococci which cause lysis of the older cells in the centre

Draughtsman’ colonies on blood agar
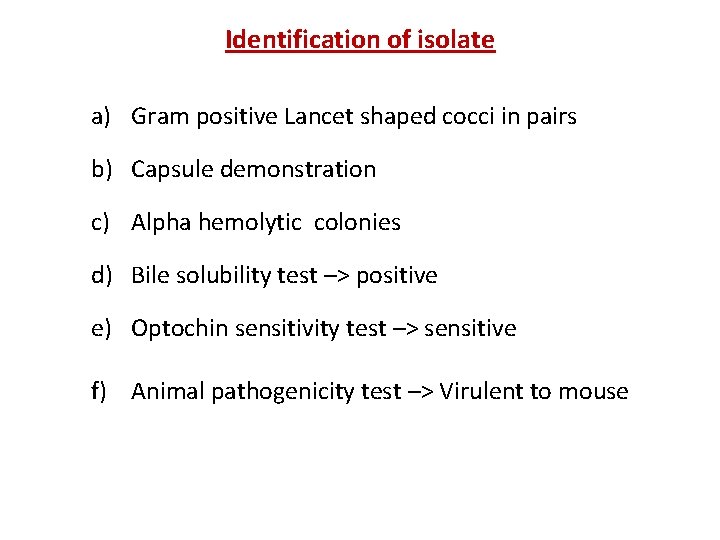
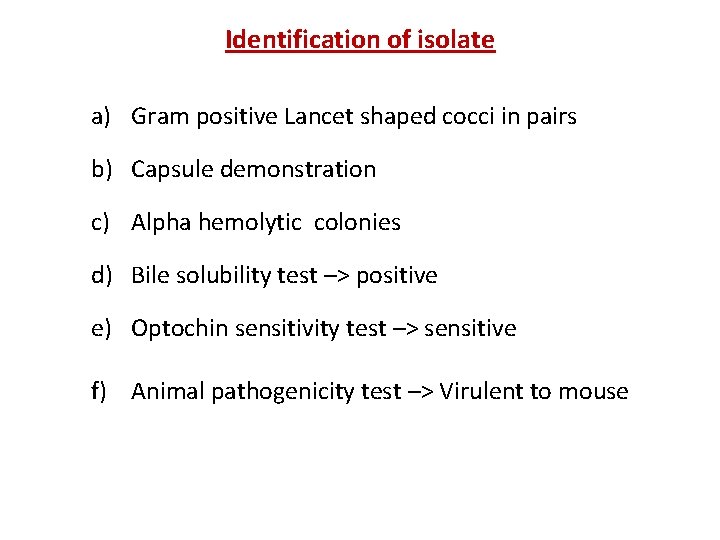
Identification of isolate a) Gram positive Lancet shaped cocci in pairs b) Capsule demonstration c) Alpha hemolytic colonies d) Bile solubility test –> positive e) Optochin sensitivity test –> sensitive f) Animal pathogenicity test –> Virulent to mouse
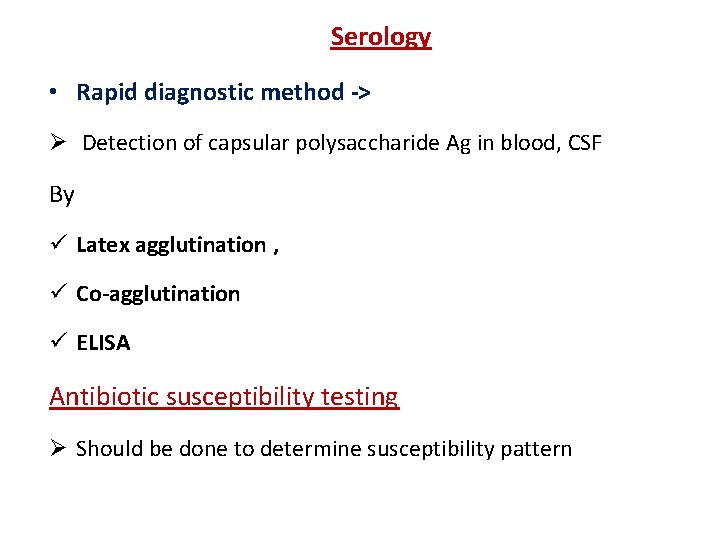
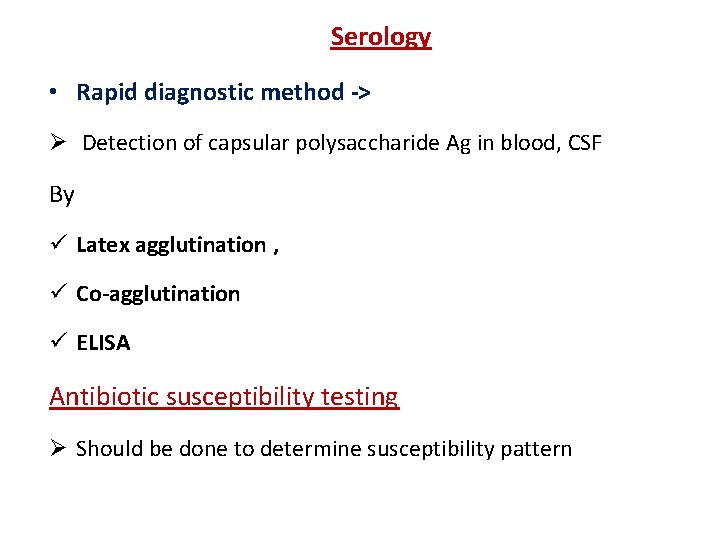
Serology • Rapid diagnostic method -> Ø Detection of capsular polysaccharide Ag in blood, CSF By ü Latex agglutination , ü Co-agglutination ü ELISA Antibiotic susceptibility testing Ø Should be done to determine susceptibility pattern
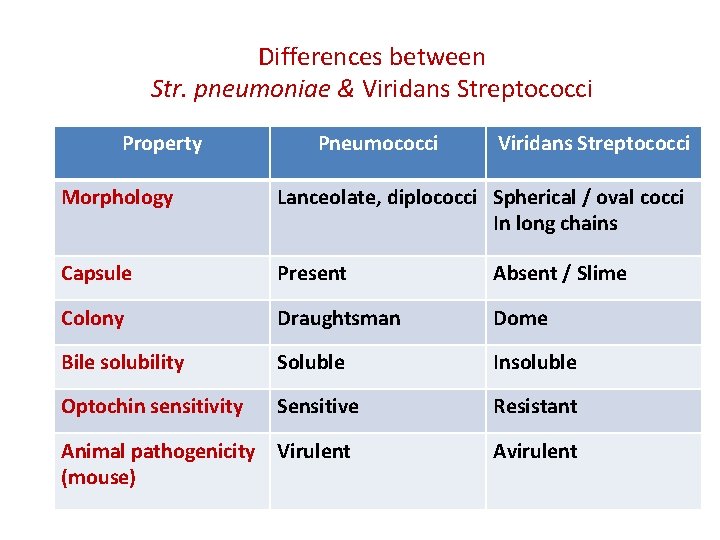
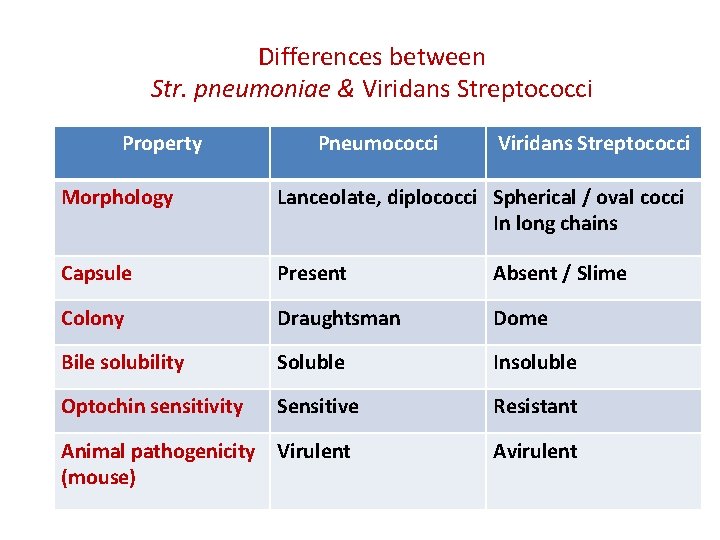
Differences between Str. pneumoniae & Viridans Streptococci Property Pneumococci Viridans Streptococci Morphology Lanceolate, diplococci Spherical / oval cocci In long chains Capsule Present Absent / Slime Colony Draughtsman Dome Bile solubility Soluble Insoluble Optochin sensitivity Sensitive Resistant Animal pathogenicity Virulent (mouse) Avirulent
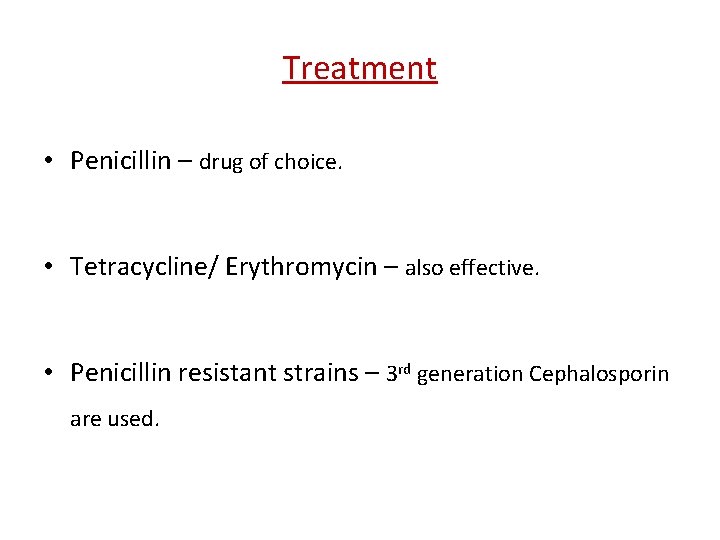
Treatment • Penicillin – drug of choice. • Tetracycline/ Erythromycin – also effective. • Penicillin resistant strains – 3 rd generation Cephalosporin are used.
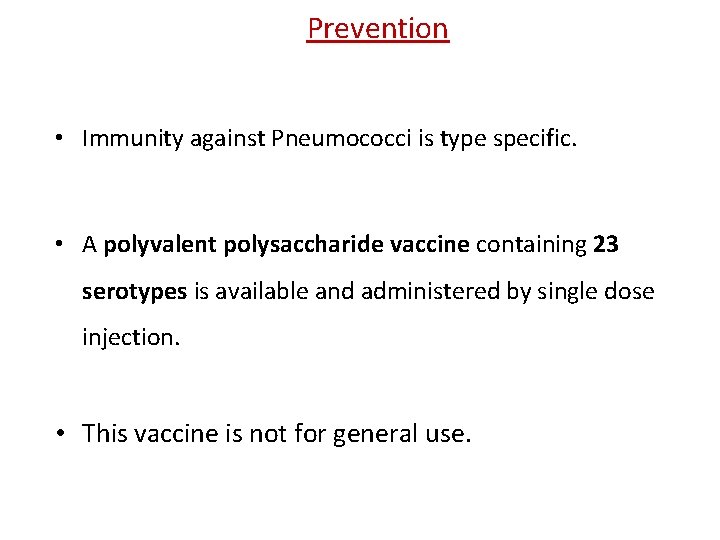
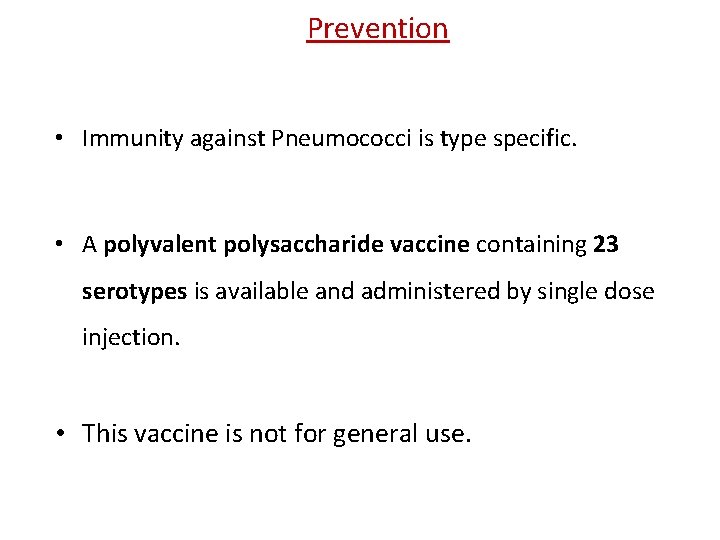
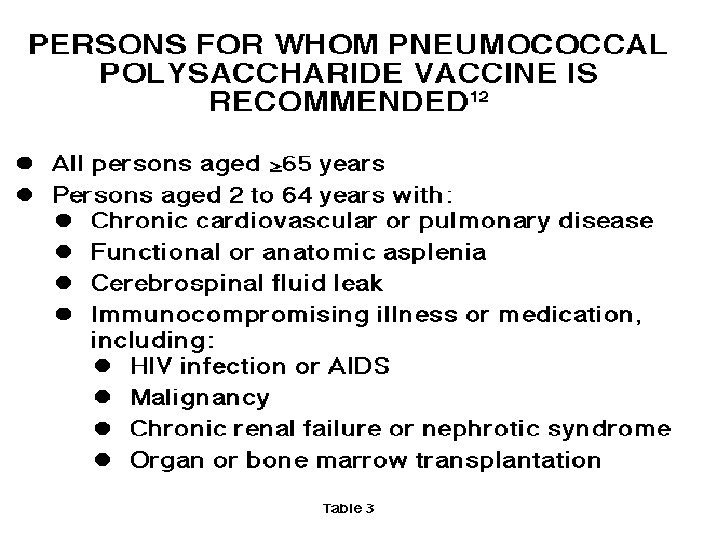
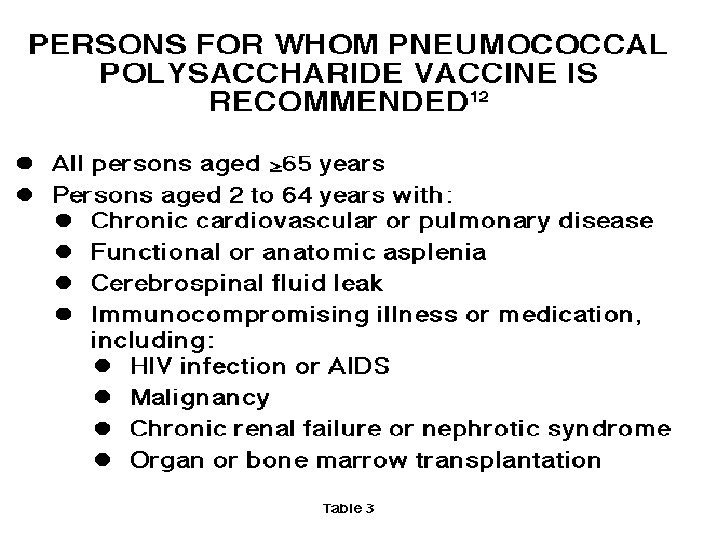
Prevention • Immunity against Pneumococci is type specific. • A polyvalent polysaccharide vaccine containing 23 serotypes is available and administered by single dose injection. • This vaccine is not for general use.
• Newer vaccines are now used (conjugate vaccines) • Proteins are coupled to the polysaccharides to get a more Tcell-dependent immune response. For technical reasons and because of high costs, only a limited number of polysaccharides have been included so far in the conjugate vaccines (7, 10, and recently 13 serotypes).
Thanks