STRABISMUS WHY CANT WE WORK TOGETHER Kimberley Lovelace
STRABISMUS -WHY CAN’T WE WORK TOGETHER Kimberley Lovelace, MD Ophthalmology Update March 3, 2018
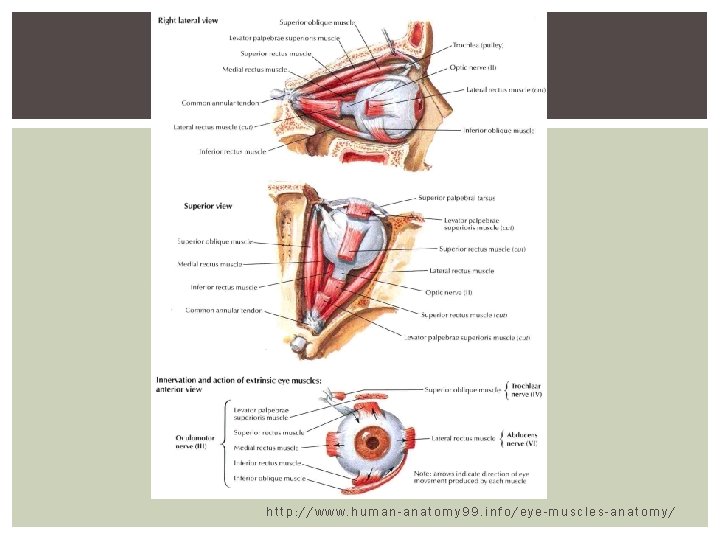
http: //www. human-anatomy 99. info/eye-muscles-anatomy/
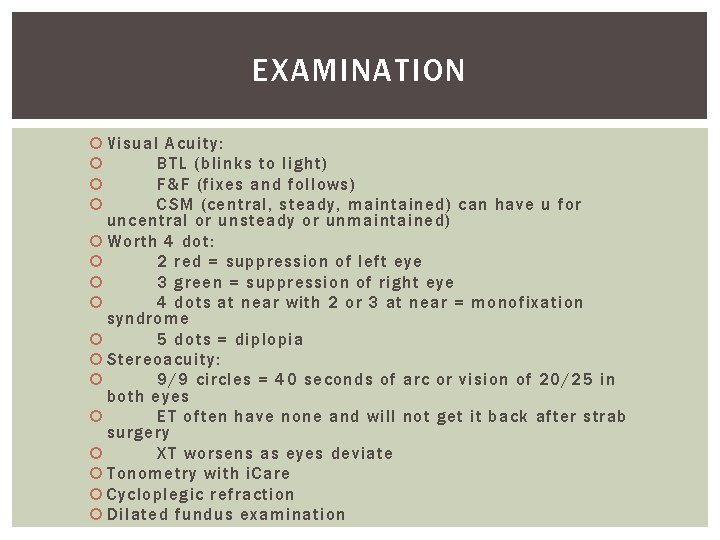
EXAMINATION Visual Acuity: BTL (blinks to light) F&F (fixes and follows) CSM (central, steady, maintained) can have u for uncentral or unsteady or unmaintained) Worth 4 dot: 2 red = suppression of left eye 3 green = suppression of right eye 4 dots at near with 2 or 3 at near = monofixation syndrome 5 dots = diplopia Stereoacuity: 9/9 circles = 40 seconds of arc or vision of 20/25 in both eyes ET often have none and will not get it back after strab surgery XT worsens as eyes deviate Tonometry with i. Care Cycloplegic refraction Dilated fundus examination
STRABISMUS EXAMINATION Light reflex Cover uncover Alternate cover Prism cover Hirshberg Krimsky Convergence/divergence Double Maddox Rod Red Filter 4 Base out prism
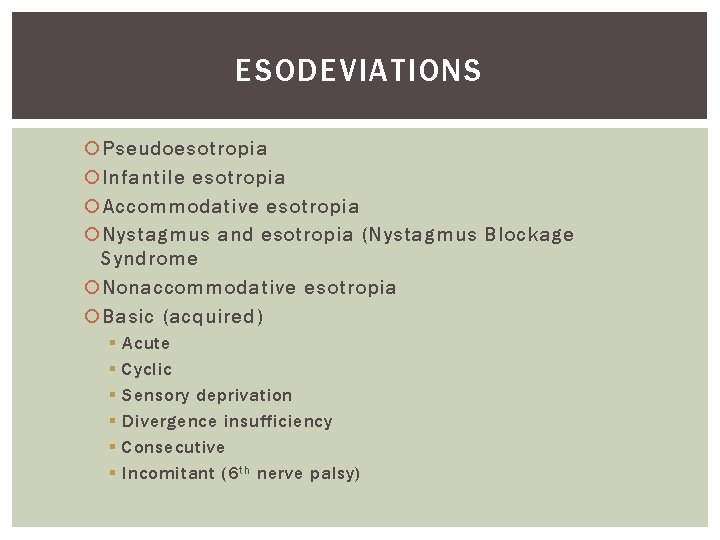
ESODEVIATIONS Pseudoesotropia Infantile esotropia Accommodative esotropia Nystagmus and esotropia (Nystagmus Blockage Syndrome Nonaccommodative esotropia Basic (acquired) § § § Acute Cyclic Sensory deprivation Divergence insufficiency Consecutive Incomitant (6 th nerve palsy)
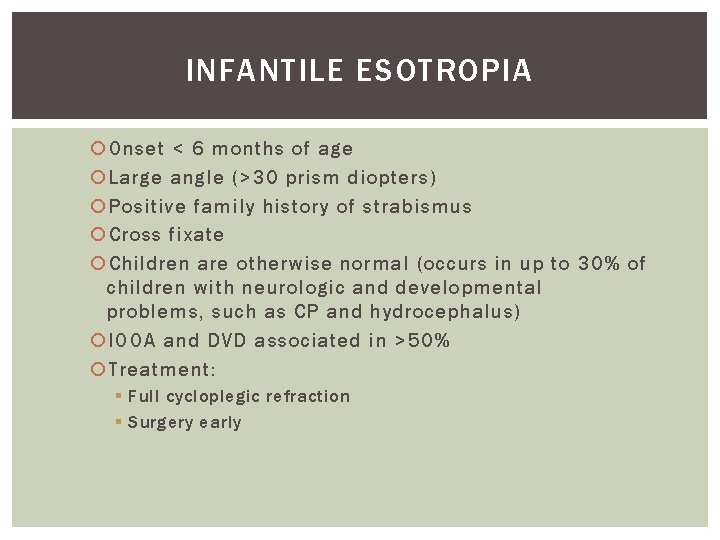
INFANTILE ESOTROPIA Onset < 6 months of age Large angle (>30 prism diopters) Positive family history of strabismus Cross fixate Children are otherwise normal (occurs in up to 30% of children with neurologic and developmental problems, such as CP and hydrocephalus) IOOA and DVD associated in >50% Treatment: § Full cycloplegic refraction § Surgery early
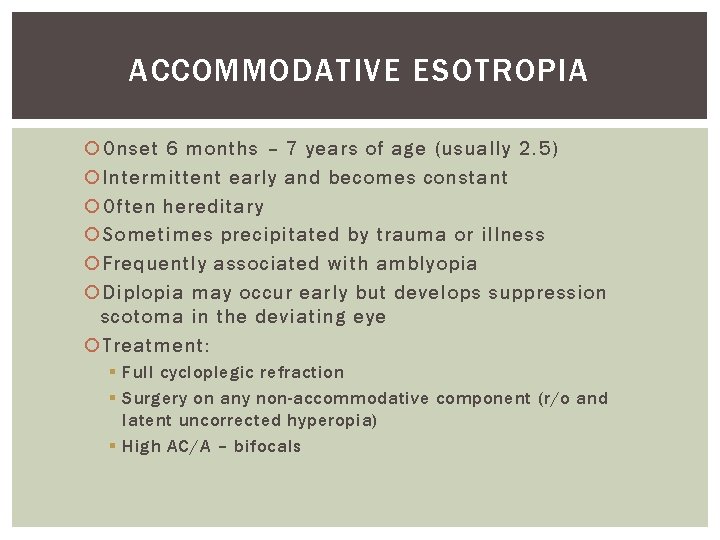
ACCOMMODATIVE ESOTROPIA Onset 6 months – 7 years of age (usually 2. 5) Intermittent early and becomes constant Often hereditary Sometimes precipitated by trauma or illness Frequently associated with amblyopia Diplopia may occur early but develops suppression scotoma in the deviating eye Treatment: § Full cycloplegic refraction § Surgery on any non-accommodative component (r/o and latent uncorrected hyperopia) § High AC/A – bifocals
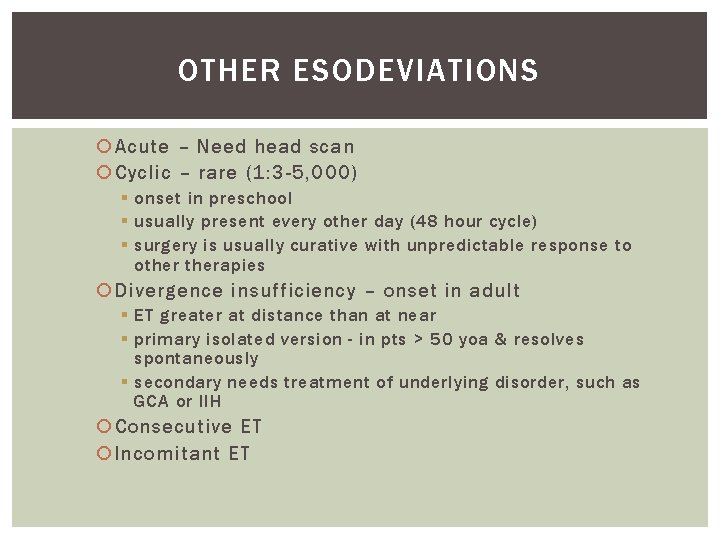
OTHER ESODEVIATIONS Acute – Need head scan Cyclic – rare (1: 3 -5, 000) § onset in preschool § usually present every other day (48 hour cycle) § surgery is usually curative with unpredictable response to otherapies Divergence insufficiency – onset in adult § ET greater at distance than at near § primary isolated version - in pts > 50 yoa & resolves spontaneously § secondary needs treatment of underlying disorder, such as GCA or IIH Consecutive ET Incomitant ET
EXODEVIATIONS Pseudo. XT Exophoria Intermittent XT Constant XT § Infantile § Sensory § Consecutive Dissociated Horizontal Deviation (DHD) Convergence insufficiency Convergence paralysis
INTERMITTENT XT Onset usually prior to 5 yoa Early on XT greater at distance than near Associated with IOOA Treatment: § Eventually need surgery § Myopic spectacle correction § Convergence exercises surgery when deviating 50% or more of time, stereoacuity decreasing, socially unacceptable
OTHER EXODEVIATIONS Infantile XT – associated with other neurologic abnormalities Sensory XT – common, treatment is surgical Convergence insufficiency Convergence paralysis – usually 2/2 intracranial lesion, normal adduction and accommodation with XT & diplopia, acute onset
VERTICAL DEVIATIONS Inferior oblique overaction – V pattern XT Superior oblique overaction – A pattern Dissociated vertical deviation Superior oblique palsy – head tilt Inferior oblique palsy Monocular elevation palsy – one eye cannot elevate Orbital floor fractures - restrictive
INFERIOR OBLIQUE OVERACTION/ SUPERIOR OBLIQUE PALSY Associated with V-pattern exotropia § Treatment: surgery to weaken the inferior oblique
SPECIAL FORMS OF STRABISMUS Duane Syndrome Brown Syndrome 3 r d nerve palsy 6 t h nerve palsy Thyroid eye disease Chronic progressive external ophthalmoplegia Myasthenia Gravis Congenital Fibrosis syndrome Mobius syndrome ET associated with high myopia
DUANE SYNDROME Can appear alone or in association with other systemic defects Caused by a defect in development occurring in 4 t h week of gestation Congenital cranial dysinnervation disorders (Mobius and congenital fibrosis syndrome) Sporadic (5 -10% AD) Females, left eye Nucleus of the 6 t h nerve is absent, aberrant branch of 3 r d innervates lateral rectus Type 1 – limitation of abduction Type 2 – limitation of adduction Type 3 – limitation of abduction and adduction Treatment: surgery reserved for primary position deviation, face turn, marked globe retraction, large upshoots or downshoots
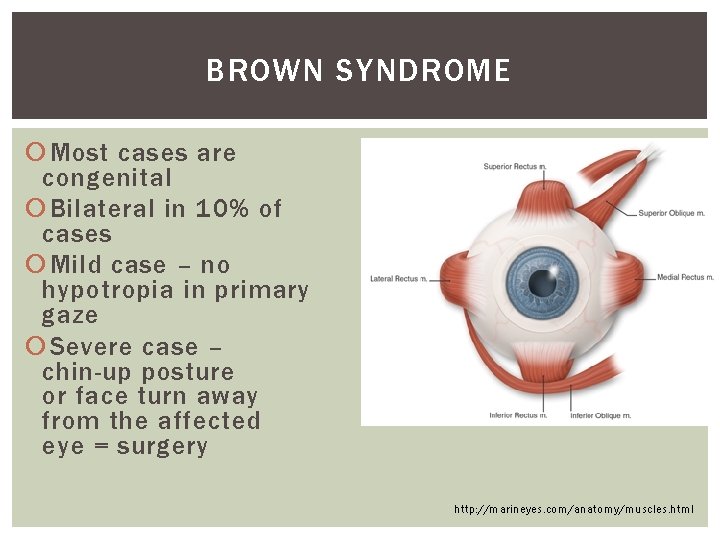
BROWN SYNDROME Most cases are congenital Bilateral in 10% of cases Mild case – no hypotropia in primary gaze Severe case – chin-up posture or face turn away from the affected eye = surgery http: //marineyes. com/anatomy/muscles. html
THIRD NERVE PALSY Causes: § Children: congenital 40 -50% of time, trauma, inflammation, viral infection, migraine, following inoculations, (rare) neoplastic lesions § Adults: intracranial aneurysm, microvascular infarction, vasculitis, diabetes, inflammation (sardoidosis), trauma, infection (meningitis), tumor/infilatration (lymphoma, carcinoma) A nontraumatic 3 r d nerve palsy with pupil involvement is caused by aneurysm until proven otherwise! Needs CTA/MRA.
THIRD NERVE PALSY Clinical signs: § Limited adduction, elevation and depression, eye is down & out § Ptosis § +/- Pupil involvement (complete results from loss of parasympathetic input = dilated pupil that responds poorly to light) Can be associated with pain Abherent regeneration confuses the picture
THIRD NERVE PALSY Isolated involvement of either superior or inferior division – usually from a lesion of the anterior cavernous sinus or possibly the posterior orbit – check MRI Aberrant regeneration: § Classic finding: eyelid retraction with adduction or pupillary miosis with elevation, adduction and depression § Common after trauma or compression by an aneurysm/tumor (not from microvascular infarct) § Primary aberrant regeneration – slowly expanding parasellar lesion, most commonly meningioma or carotid aneurysm within the cavernous sinus = neuroimaging
6 TH NERVE PALSY Most frequent cause of an isolated ocular motor palsy Isolated palsy in adults > 50 yoa § Usually ischemic § Resolve within 3 months § Neuroimaging is NOT required, unless persisting >3 months § Medical evaluation is appropriate Younger adults should have neuroimaging, think neuromuscular junction dz (MG), restricted MR (TED) Children: leukemia or brainstem glioma Adolescents & young adults: demyelination Lesions of the pontine angle usually involve 6 t h nerve plus other cranial nerves
THYROID EYE DISEASE Fibrosis of EOM due to lymphocytic infiltration Restricted motility Compressive optic neuropathy Surgical order: 1. Optic nerve decompression 2. Strabismus - Need stability of 6 months prior to sx 3. Eyelids
CHRONIC PROGRESSIVE EXTERNAL OPHTHALMOPLEGIA Slowly progressive to total paralysis of eyelids and EOMs Onset in childhood True pigmentary retinal dystrophy usually absent but constricted fields and ERG abnormalities Kearns-Sayre syndrome: retinal pigmentary changes, CPEO, cardiomyopathy Medical evaluation of cardiac status essential
MYASTHENIA GRAVIS Unusual in children 90% of ocular cases have both ptosis and limited ocular rotations Rapid fatigue of muscles Ptosis increases with looking upward for 30 seconds Sleep test: ptosis resolves after 20 -30 minutes in dark room with eyelids closed Cogan twitch: overshoot of eyelid when pt looks straight ahead after looking down for several minutes Ice test: 2 -5 minutes of ice improves levator function Tensilon test: edrophonium (neostigmine = alternative with prolonged effect) Tx: mestinon (physostigmine), surgery if stable strab measurements, needs medical evaluation
CONGENITAL FIBROSIS SYNDROME One of the congenital cranial dysinnervation disorders Treatment: Surgery to release fibrosis and place eyes in primary position
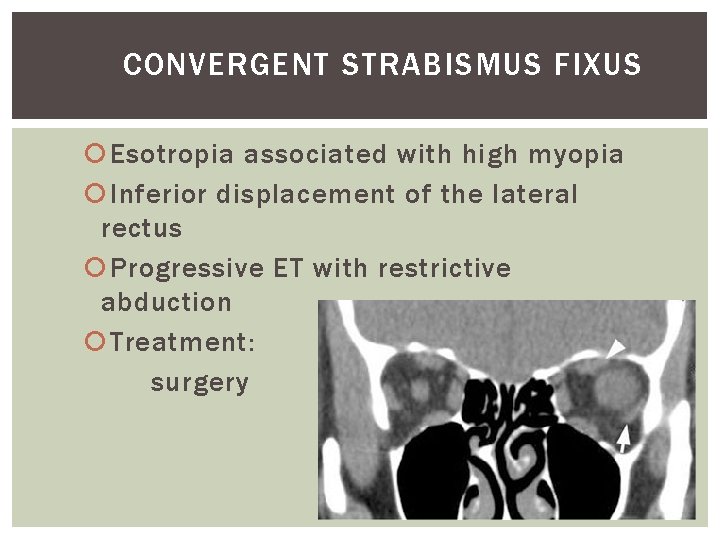
CONVERGENT STRABISMUS FIXUS Esotropia associated with high myopia Inferior displacement of the lateral rectus Progressive ET with restrictive abduction Treatment: surgery
NYSTAGMUS If null point causes abnormal head posture, then strabismus surgery is performed to set null point in primary position Kestenbaum-Anderson procedure
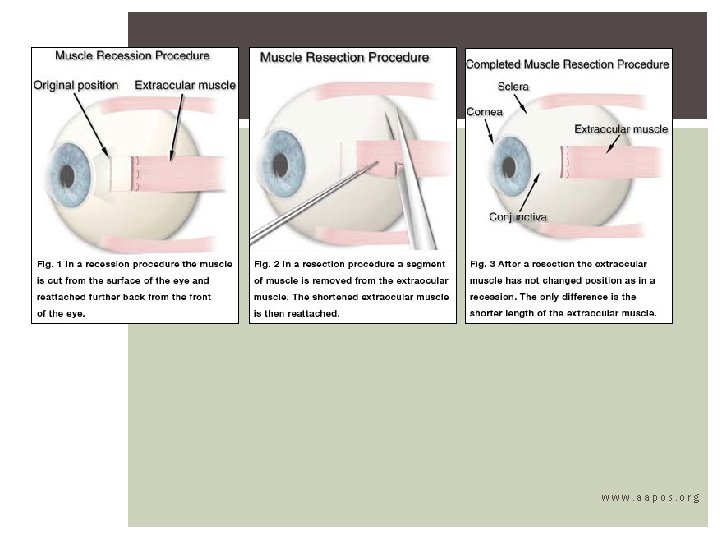
STRABISMUS SURGERY Recession – to weaken or loosen the muscle by moving it posteriorly Resection – to strengthen or tighten the muscle by shortening it Botox Superior oblique tendon spacer Inferior oblique recession and anteriorization
www. aapos. org
- Slides: 28