Strabismus Terminology The term strabismus is derived from
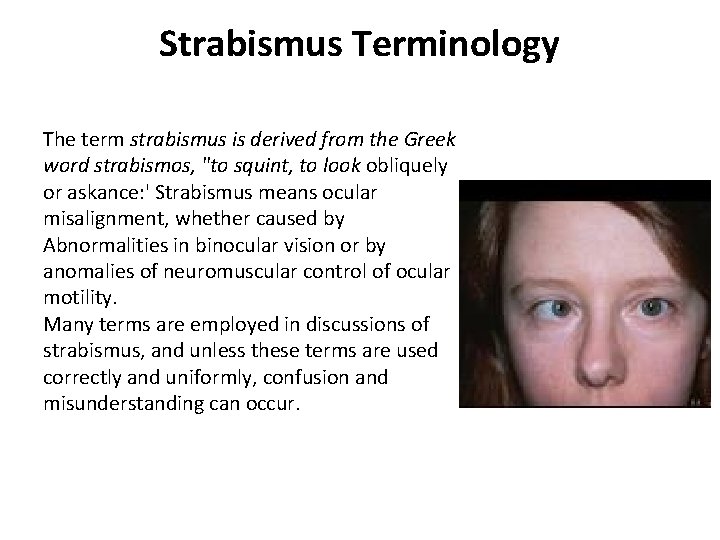
Strabismus Terminology The term strabismus is derived from the Greek word strabismos, "to squint, to look obliquely or askance: ' Strabismus means ocular misalignment, whether caused by Abnormalities in binocular vision or by anomalies of neuromuscular control of ocular motility. Many terms are employed in discussions of strabismus, and unless these terms are used correctly and uniformly, confusion and misunderstanding can occur.
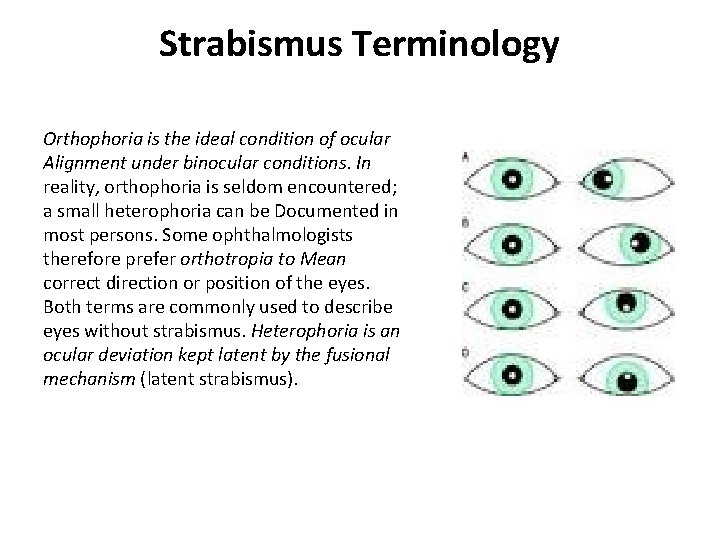
Strabismus Terminology Orthophoria is the ideal condition of ocular Alignment under binocular conditions. In reality, orthophoria is seldom encountered; a small heterophoria can be Documented in most persons. Some ophthalmologists therefore prefer orthotropia to Mean correct direction or position of the eyes. Both terms are commonly used to describe eyes without strabismus. Heterophoria is an ocular deviation kept latent by the fusional mechanism (latent strabismus).
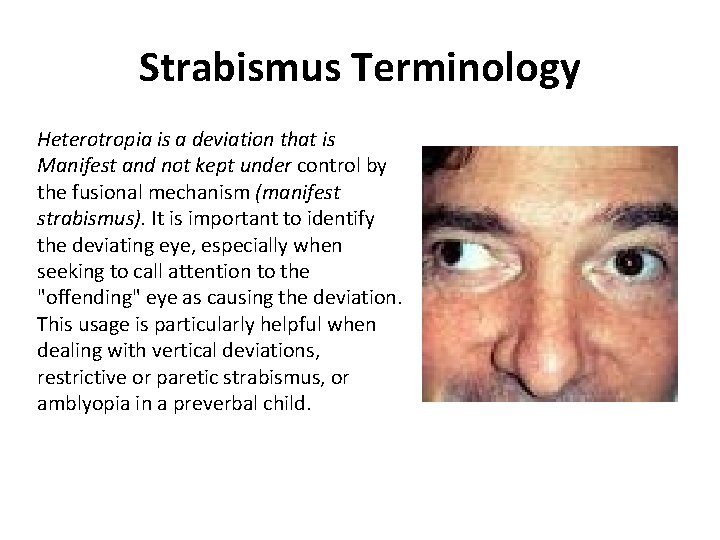
Strabismus Terminology Heterotropia is a deviation that is Manifest and not kept under control by the fusional mechanism (manifest strabismus). It is important to identify the deviating eye, especially when seeking to call attention to the "offending" eye as causing the deviation. This usage is particularly helpful when dealing with vertical deviations, restrictive or paretic strabismus, or amblyopia in a preverbal child.
Prefixes Eso- this is also known as convergent strabismus. Exo- this is also known as divergent strabismus. Hyper- This is also known as vertical strabismus. Hypo- This is also known as vertical strabismus. Incyclo- This is also known as intorsional strabismus. Excyclo- This is also known as extorsional strabismus.
Suffixes Phoria: A latent deviation (e. g. , esophoria, exophoria, right hyperphoria) that is controlled by the fusional mechanism so that The eyes remain aligned under normal binocular vision Tropia: A manifest deviation (eg, esotropia, exotropia, right hypertropia, excyclotropia) that exceeds the control of the fusional mechanism so that the eyes are not aligned under binocular conditions
Strabismus Classification Terms No classification is perfect or all-inclusive, and several methods of classifying eye alignment and motility disorders are used. Following are terms used in these classifications.
Fusional Status Phoria: A latent deviation in which fusional control is always present. Intermittent tropia: A deviation in which fusional control is present part of the time. Tropia: A manifest deviation in which fusional control is not present.
Variation Deviation With Gaze Position Comitant : (concomitant) The size of the deviation does not vary by more than a few prism diopters with direction of gaze or with the eye used for fixating. Incomitant : (noncomitant) The deviation varies in size with the direction of gaze or with the eye used for fixating. Most incomitant strabismus is paralytic or restrictive.
Fixation Alternating: Spontaneous alternation of fixation from one eye to the other. Monocular: Definite preference for fixation with one eye.
Age of onset Congenital: A deviation documented before age 6 months, presumably related to a defect present at birth; the term infantile might be more appropriate. Acquired: A deviation with later onset, after a period of apparently normal visual development.
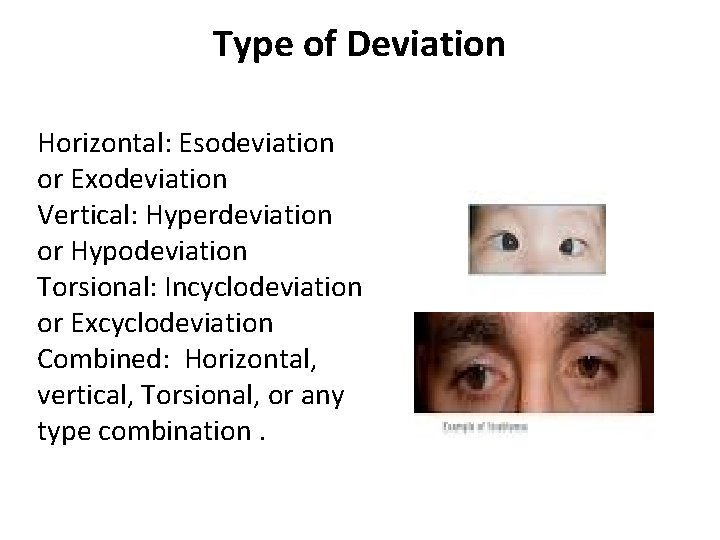
Type of Deviation Horizontal: Esodeviation or Exodeviation Vertical: Hyperdeviation or Hypodeviation Torsional: Incyclodeviation or Excyclodeviation Combined: Horizontal, vertical, Torsional, or any type combination.
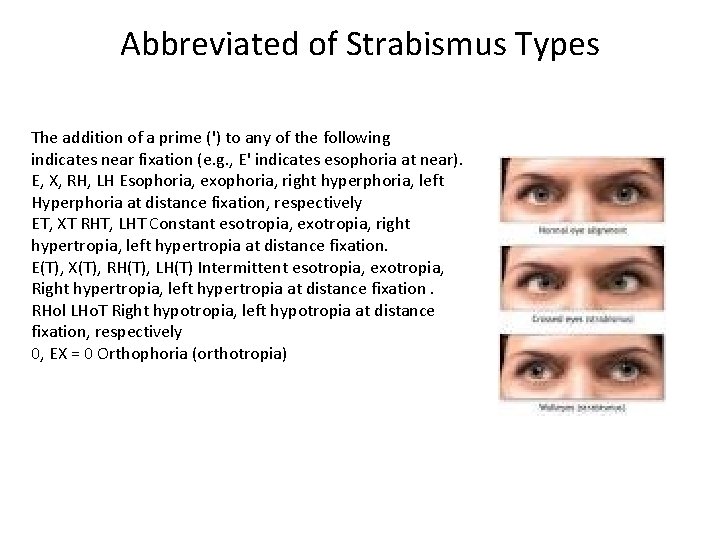
Abbreviated of Strabismus Types The addition of a prime (') to any of the following indicates near fixation (e. g. , E' indicates esophoria at near). E, X, RH, LH Esophoria, exophoria, right hyperphoria, left Hyperphoria at distance fixation, respectively ET, XT RHT, LHT Constant esotropia, exotropia, right hypertropia, left hypertropia at distance fixation. E(T), X(T), RH(T), LH(T) Intermittent esotropia, exotropia, Right hypertropia, left hypertropia at distance fixation. RHol LHo. T Right hypotropia, left hypotropia at distance fixation, respectively 0, EX = 0 Orthophoria (orthotropia)
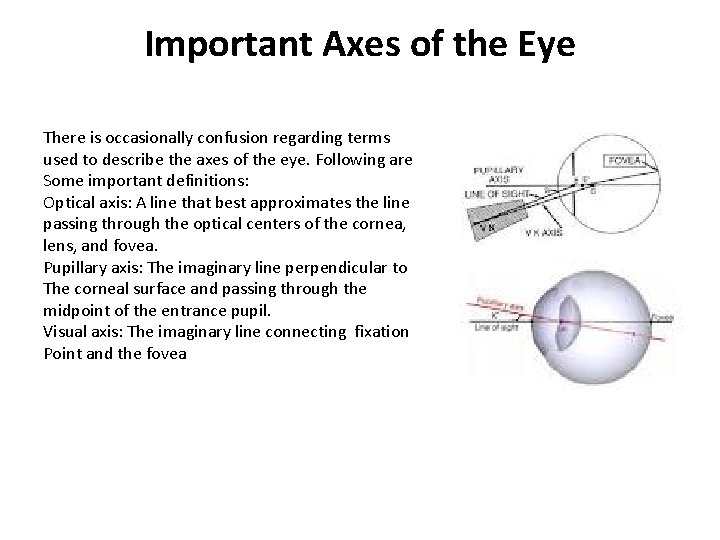
Important Axes of the Eye There is occasionally confusion regarding terms used to describe the axes of the eye. Following are Some important definitions: Optical axis: A line that best approximates the line passing through the optical centers of the cornea, lens, and fovea. Pupillary axis: The imaginary line perpendicular to The corneal surface and passing through the midpoint of the entrance pupil. Visual axis: The imaginary line connecting fixation Point and the fovea
Anatomy of the Extra ocular Muscles and Their Fascia
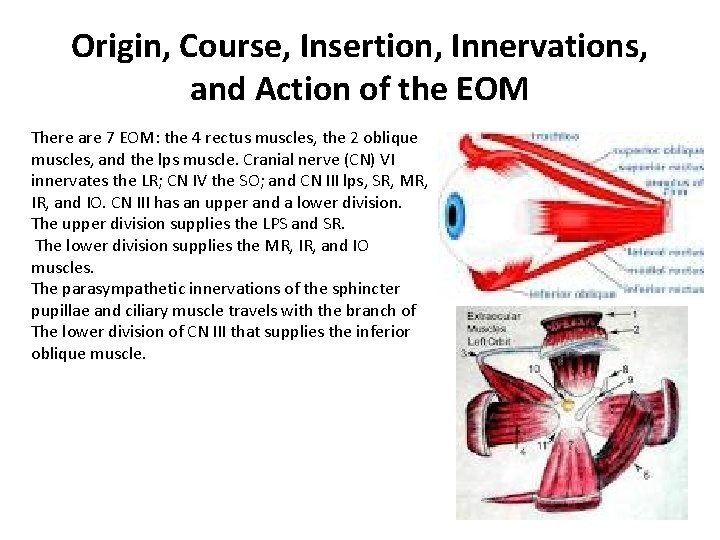
Origin, Course, Insertion, Innervations, and Action of the EOM There are 7 EOM: the 4 rectus muscles, the 2 oblique muscles, and the lps muscle. Cranial nerve (CN) VI innervates the LR; CN IV the SO; and CN III lps, SR, MR, IR, and IO. CN III has an upper and a lower division. The upper division supplies the LPS and SR. The lower division supplies the MR, IR, and IO muscles. The parasympathetic innervations of the sphincter pupillae and ciliary muscle travels with the branch of The lower division of CN III that supplies the inferior oblique muscle.
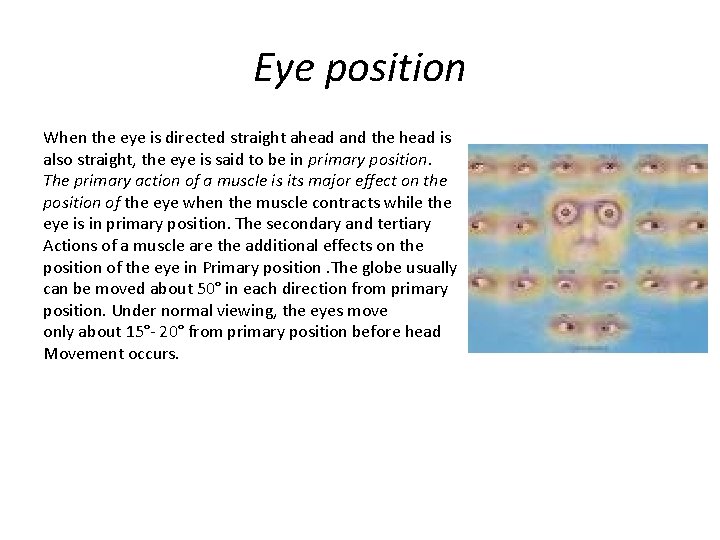
Eye position When the eye is directed straight ahead and the head is also straight, the eye is said to be in primary position. The primary action of a muscle is its major effect on the position of the eye when the muscle contracts while the eye is in primary position. The secondary and tertiary Actions of a muscle are the additional effects on the position of the eye in Primary position. The globe usually can be moved about 50° in each direction from primary position. Under normal viewing, the eyes move only about 15°- 20° from primary position before head Movement occurs.
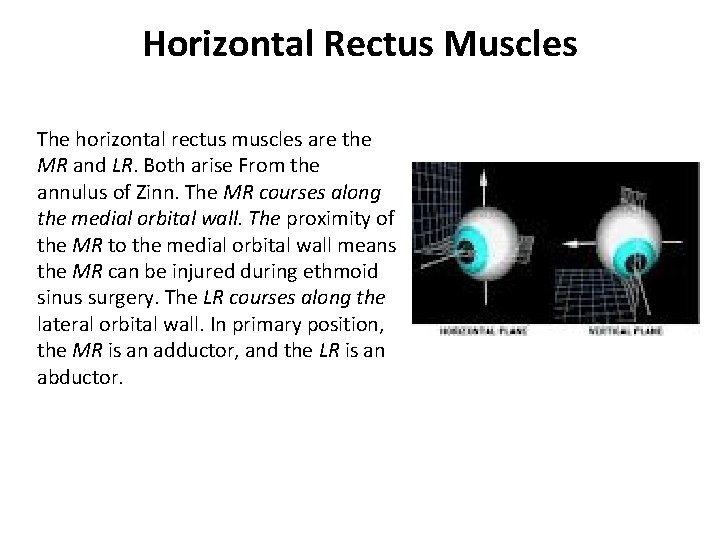
Horizontal Rectus Muscles The horizontal rectus muscles are the MR and LR. Both arise From the annulus of Zinn. The MR courses along the medial orbital wall. The proximity of the MR to the medial orbital wall means the MR can be injured during ethmoid sinus surgery. The LR courses along the lateral orbital wall. In primary position, the MR is an adductor, and the LR is an abductor.
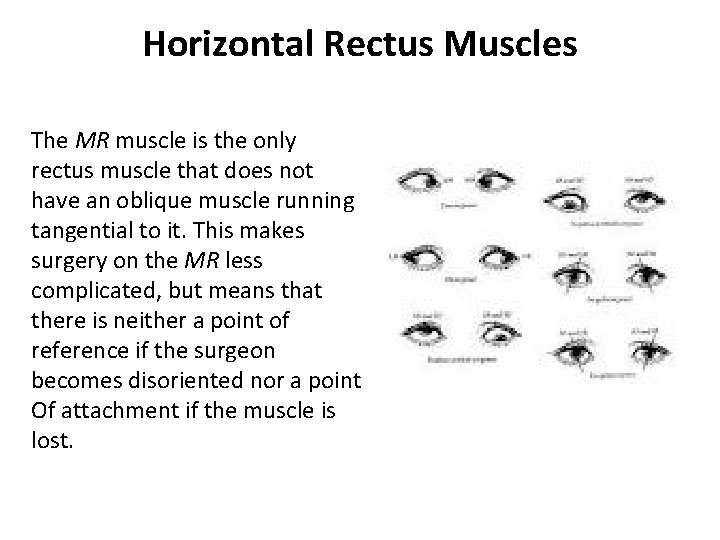
Horizontal Rectus Muscles The MR muscle is the only rectus muscle that does not have an oblique muscle running tangential to it. This makes surgery on the MR less complicated, but means that there is neither a point of reference if the surgeon becomes disoriented nor a point Of attachment if the muscle is lost.
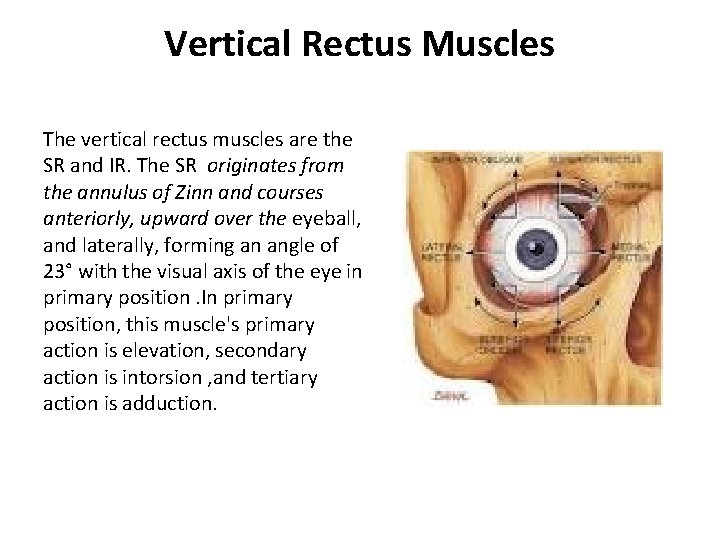
Vertical Rectus Muscles The vertical rectus muscles are the SR and IR. The SR originates from the annulus of Zinn and courses anteriorly, upward over the eyeball, and laterally, forming an angle of 23° with the visual axis of the eye in primary position. In primary position, this muscle's primary action is elevation, secondary action is intorsion , and tertiary action is adduction.
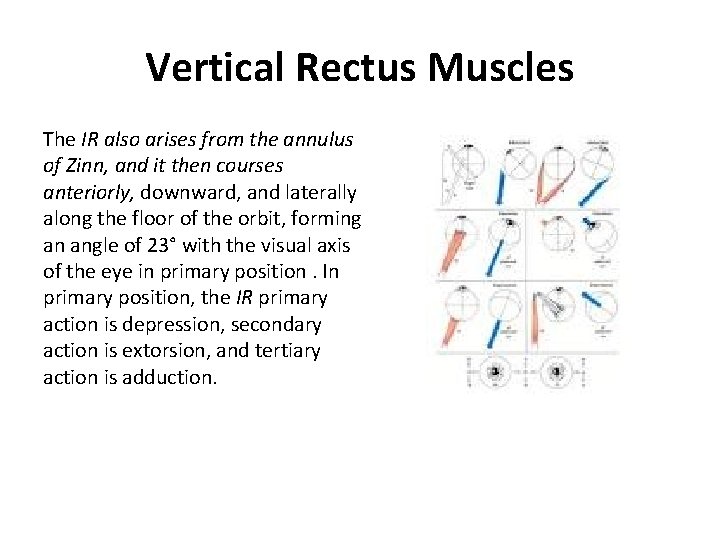
Vertical Rectus Muscles The IR also arises from the annulus of Zinn, and it then courses anteriorly, downward, and laterally along the floor of the orbit, forming an angle of 23° with the visual axis of the eye in primary position. In primary position, the IR primary action is depression, secondary action is extorsion, and tertiary action is adduction.
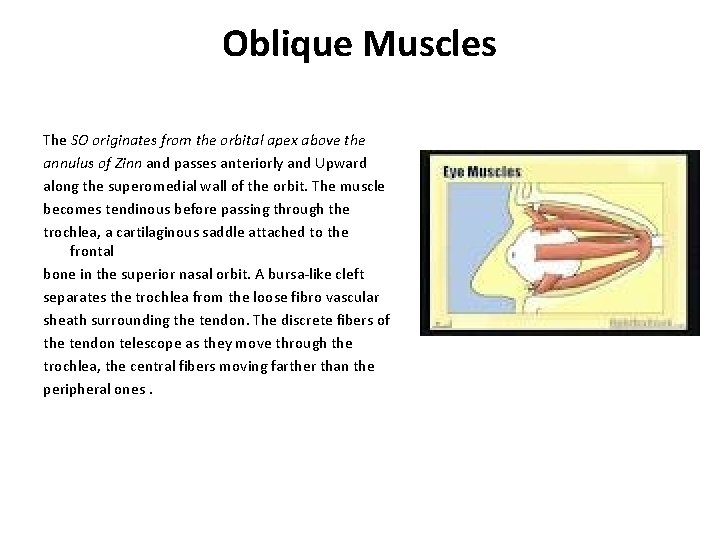
Oblique Muscles The SO originates from the orbital apex above the annulus of Zinn and passes anteriorly and Upward along the superomedial wall of the orbit. The muscle becomes tendinous before passing through the trochlea, a cartilaginous saddle attached to the frontal bone in the superior nasal orbit. A bursa-like cleft separates the trochlea from the loose fibro vascular sheath surrounding the tendon. The discrete fibers of the tendon telescope as they move through the trochlea, the central fibers moving farther than the peripheral ones.
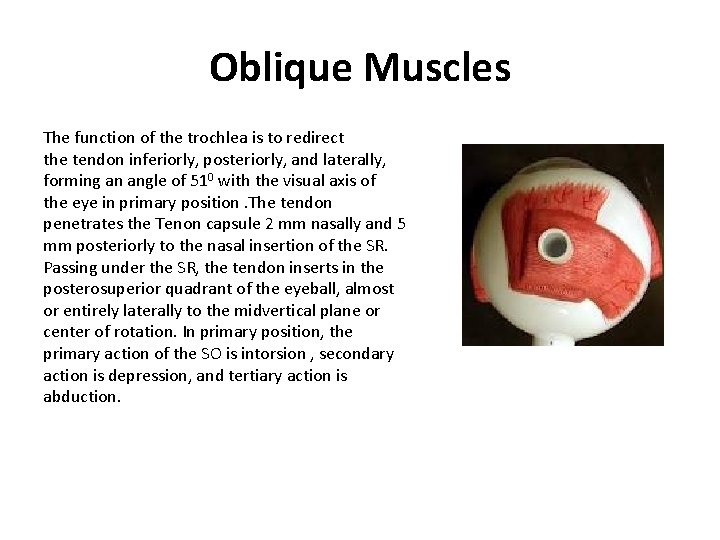
Oblique Muscles The function of the trochlea is to redirect the tendon inferiorly, posteriorly, and laterally, forming an angle of 510 with the visual axis of the eye in primary position. The tendon penetrates the Tenon capsule 2 mm nasally and 5 mm posteriorly to the nasal insertion of the SR. Passing under the SR, the tendon inserts in the posterosuperior quadrant of the eyeball, almost or entirely laterally to the midvertical plane or center of rotation. In primary position, the primary action of the SO is intorsion , secondary action is depression, and tertiary action is abduction.
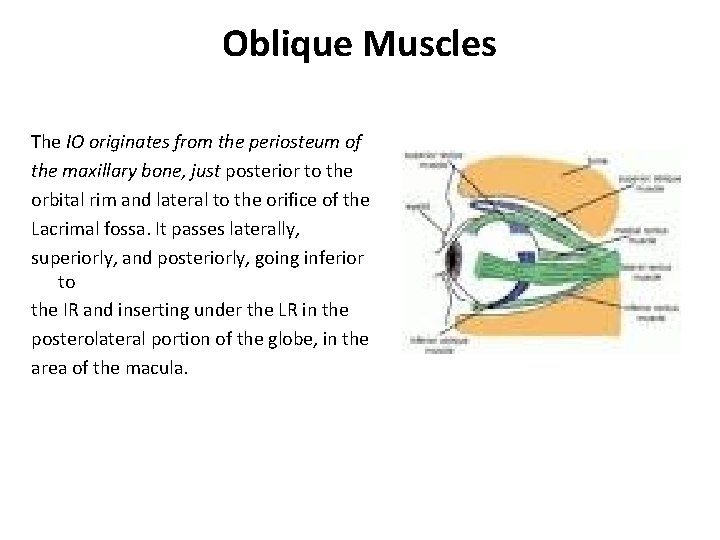
Oblique Muscles The IO originates from the periosteum of the maxillary bone, just posterior to the orbital rim and lateral to the orifice of the Lacrimal fossa. It passes laterally, superiorly, and posteriorly, going inferior to the IR and inserting under the LR in the posterolateral portion of the globe, in the area of the macula.
Oblique Muscles The IO forms an angle of 510 with the visual axis of the eye in primary position. In primary position, the muscle's primary action is extorsion , secondary action is elevation, and tertiary action is abduction.
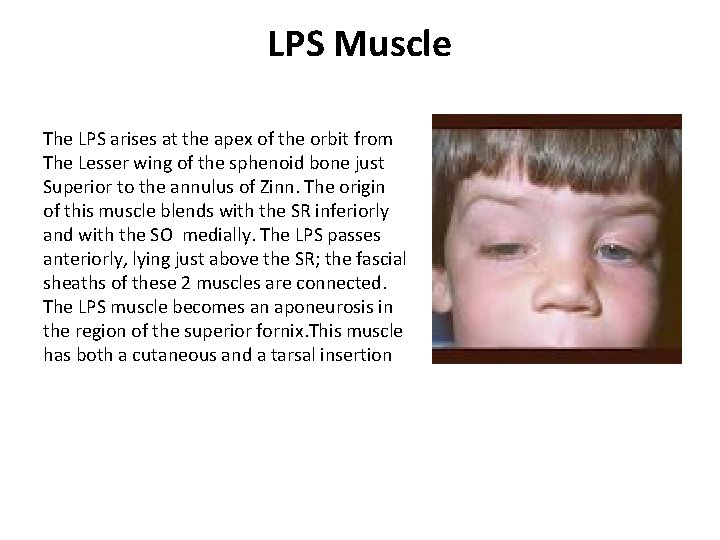
LPS Muscle The LPS arises at the apex of the orbit from The Lesser wing of the sphenoid bone just Superior to the annulus of Zinn. The origin of this muscle blends with the SR inferiorly and with the SO medially. The LPS passes anteriorly, lying just above the SR; the fascial sheaths of these 2 muscles are connected. The LPS muscle becomes an aponeurosis in the region of the superior fornix. This muscle has both a cutaneous and a tarsal insertion
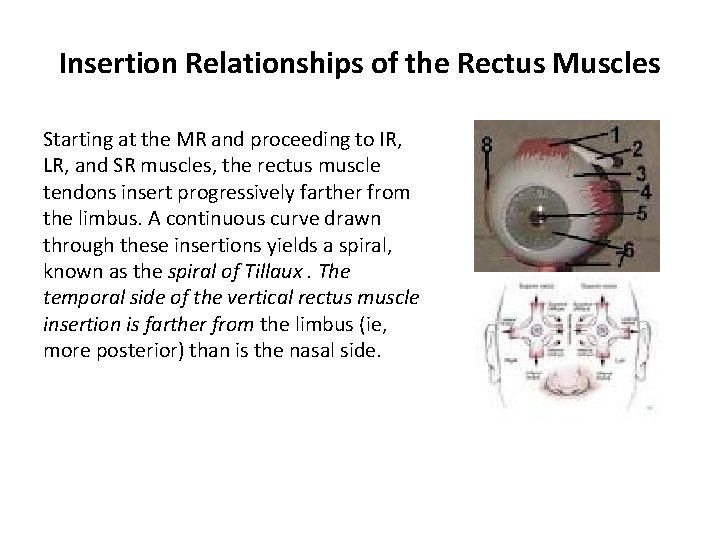
Insertion Relationships of the Rectus Muscles Starting at the MR and proceeding to IR, LR, and SR muscles, the rectus muscle tendons insert progressively farther from the limbus. A continuous curve drawn through these insertions yields a spiral, known as the spiral of Tillaux. The temporal side of the vertical rectus muscle insertion is farther from the limbus (ie, more posterior) than is the nasal side.
Blood Supply of the EOM Arterial System The muscular branches of the ophthalmic artery provide the most Important Blood Supply for the EOM. The lateral muscular branch supplies the LR, SO, and LPS muscles; the medial muscular branch, the larger of the 2, supplies the IR, MR, and IO muscles. The LR is partially supplied by the lacrimal artery; the infraorbital artery partially supplies the IO and IR muscles.
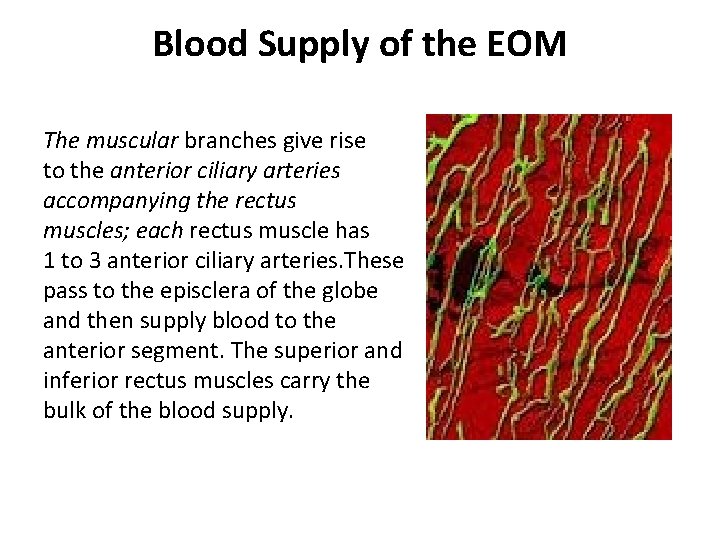
Blood Supply of the EOM The muscular branches give rise to the anterior ciliary arteries accompanying the rectus muscles; each rectus muscle has 1 to 3 anterior ciliary arteries. These pass to the episclera of the globe and then supply blood to the anterior segment. The superior and inferior rectus muscles carry the bulk of the blood supply.
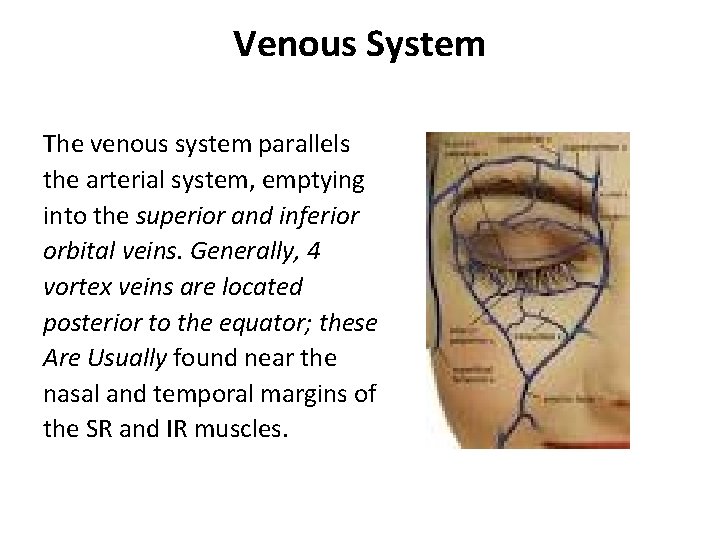
Venous System The venous system parallels the arterial system, emptying into the superior and inferior orbital veins. Generally, 4 vortex veins are located posterior to the equator; these Are Usually found near the nasal and temporal margins of the SR and IR muscles.
Structure of the EOM The important functional characteristics of muscle fibers are contraction speed and Fatigue resistance. The eye muscles participate in motor acts that are among the fastest (saccadic eye movements) in the body and in those that are among the most sustained (gaze fixation and vergence movements). Like skeletal muscle, EOM is Voluntary striated muscle. However, developmentally, biochemically, structurally, and functionally, it is different from typical skeletal muscle.
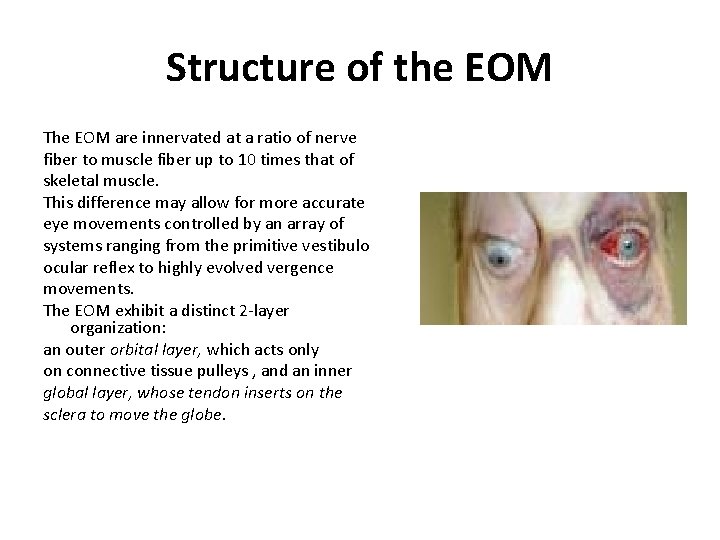
Structure of the EOM The EOM are innervated at a ratio of nerve fiber to muscle fiber up to 10 times that of skeletal muscle. This difference may allow for more accurate eye movements controlled by an array of systems ranging from the primitive vestibulo ocular reflex to highly evolved vergence movements. The EOM exhibit a distinct 2 -layer organization: an outer orbital layer, which acts only on connective tissue pulleys , and an inner global layer, whose tendon inserts on the sclera to move the globe.
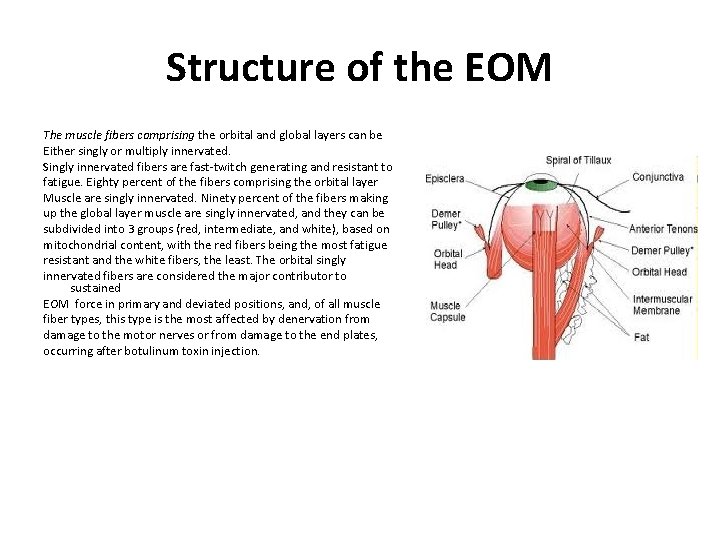
Structure of the EOM The muscle fibers comprising the orbital and global layers can be Either singly or multiply innervated. Singly innervated fibers are fast-twitch generating and resistant to fatigue. Eighty percent of the fibers comprising the orbital layer Muscle are singly innervated. Ninety percent of the fibers making up the global layer muscle are singly innervated, and they can be subdivided into 3 groups (red, intermediate, and white), based on mitochondrial content, with the red fibers being the most fatigue resistant and the white fibers, the least. The orbital singly innervated fibers are considered the major contributor to sustained EOM force in primary and deviated positions, and, of all muscle fiber types, this type is the most affected by denervation from damage to the motor nerves or from damage to the end plates, occurring after botulinum toxin injection.
Structure of the EOM The function of the multiply innervated fibers of the orbital and global layers is not clear. These fibers are not seen in the LPS, and it is thought that they are involved in the finer control of fixation and in the smooth and finely graded eye movements, particularly vergence control. These novel properties of eye muscles lead to differential responses to pharmaceuticals such as botulinum toxin, channel blockers, or local anesthetics, as well as disease processes such as myasthenia gravis and muscular dystrophy.
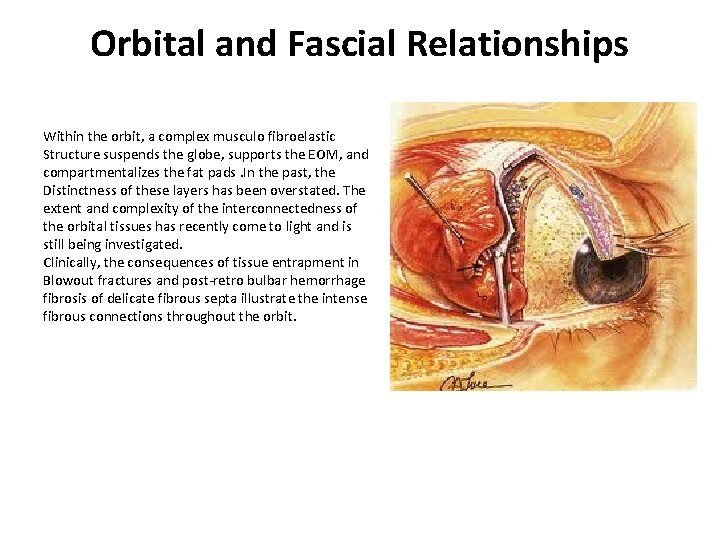
Orbital and Fascial Relationships Within the orbit, a complex musculo fibroelastic Structure suspends the globe, supports the EOM, and compartmentalizes the fat pads. In the past, the Distinctness of these layers has been overstated. The extent and complexity of the interconnectedness of the orbital tissues has recently come to light and is still being investigated. Clinically, the consequences of tissue entrapment in Blowout fractures and post-retro bulbar hemorrhage fibrosis of delicate fibrous septa illustrate the intense fibrous connections throughout the orbit.
Adipose Tissue The eye is supported and cushioned in the orbit by a large amount of fatty tissue. External to the muscle cone, fatty tissue comes forward with the rectus muscles, stopping About 10 mm from the limbus. Fatty tissue is also present inside the muscle cone, kept away from the sclera by the Tenon capsule.
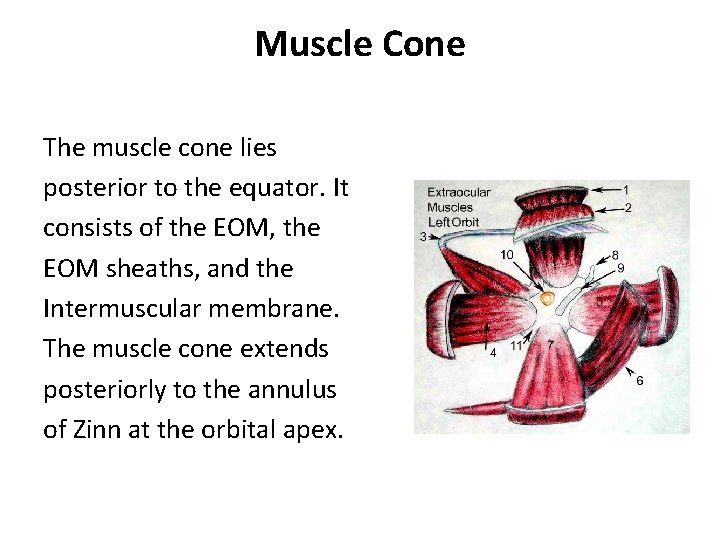
Muscle Cone The muscle cone lies posterior to the equator. It consists of the EOM, the EOM sheaths, and the Intermuscular membrane. The muscle cone extends posteriorly to the annulus of Zinn at the orbital apex.
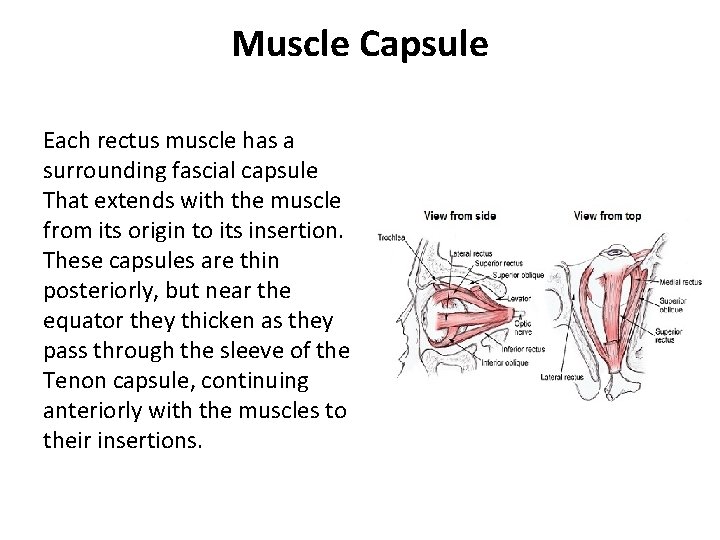
Muscle Capsule Each rectus muscle has a surrounding fascial capsule That extends with the muscle from its origin to its insertion. These capsules are thin posteriorly, but near the equator they thicken as they pass through the sleeve of the Tenon capsule, continuing anteriorly with the muscles to their insertions.
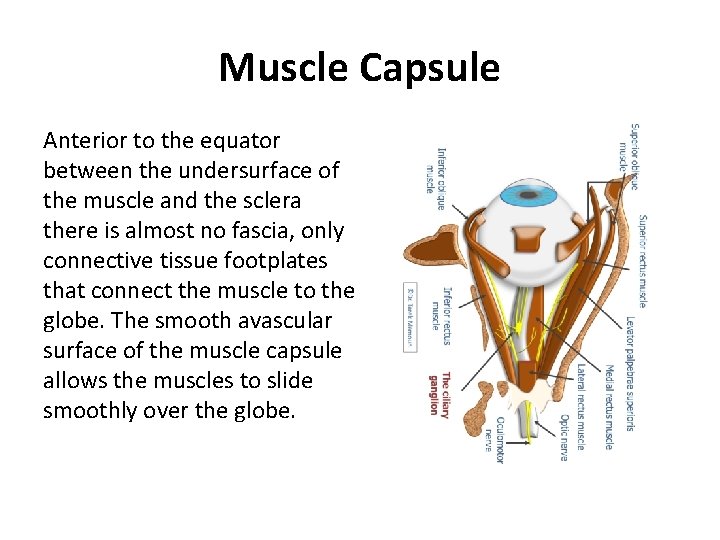
Muscle Capsule Anterior to the equator between the undersurface of the muscle and the sclera there is almost no fascia, only connective tissue footplates that connect the muscle to the globe. The smooth avascular surface of the muscle capsule allows the muscles to slide smoothly over the globe.
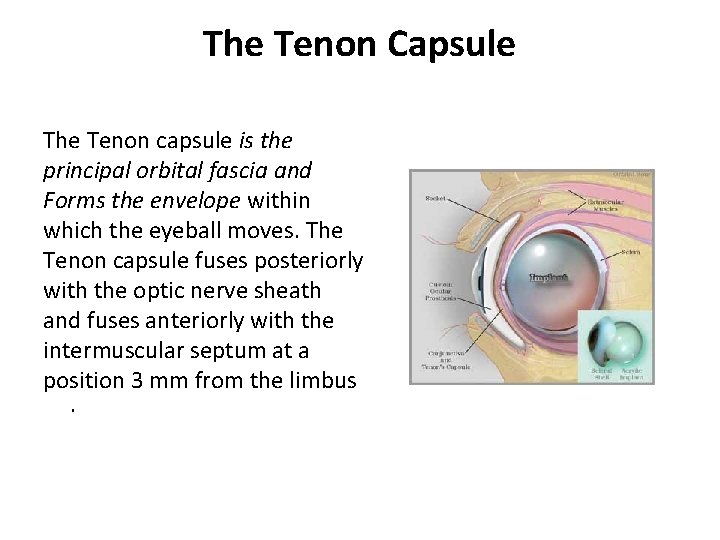
The Tenon Capsule The Tenon capsule is the principal orbital fascia and Forms the envelope within which the eyeball moves. The Tenon capsule fuses posteriorly with the optic nerve sheath and fuses anteriorly with the intermuscular septum at a position 3 mm from the limbus.
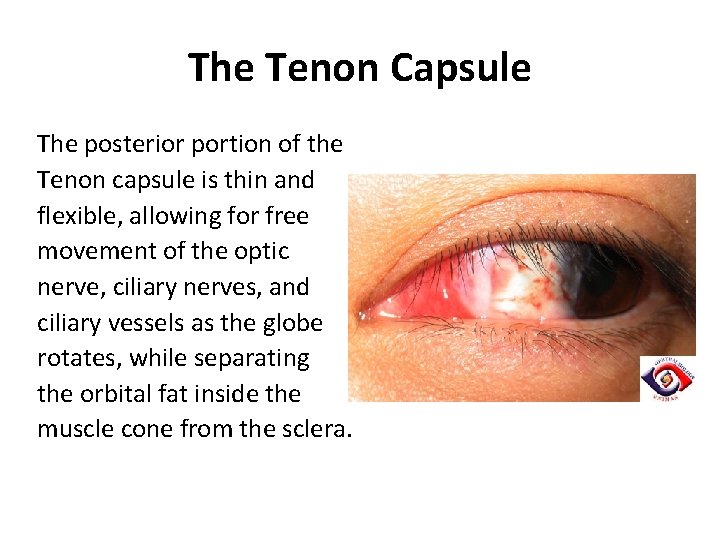
The Tenon Capsule The posterior portion of the Tenon capsule is thin and flexible, allowing for free movement of the optic nerve, ciliary nerves, and ciliary vessels as the globe rotates, while separating the orbital fat inside the muscle cone from the sclera.
The Tenon Capsule At and just posterior to the equator, the Tenon capsule is thick, suspending the globe like a Trampoline by means of connections to the periorbital tissues. The global layer of the 4 Rectus muscles penetrates thick Musculofibroelastic tissue approximately 10 mm posterior to their insertions. The oblique muscles penetrate the Tenon capsule anterior to the equator. The tenon capsule continues forward over these 6 extra ocular muscles and separates them from the orbital fat and structures lying outside the muscle cone.
Pulley System The 4 rectus muscles are surrounded by distinct fibroelastic pulleys. Though not as distinct as the trochlea of the SO, these pulleys maintain the position of the EOM relative to the orbit. They consist of collagen, elastin, and smooth muscle, which allows them to contract and relax. As the orbital muscle layer contracts, this pulley must be pulled back so that the distance between the location of the pulley and the insertion of the muscle on the globe remains approximately constant Just as the trochlea acts as the functional origin of the SO, these pulleys act mechanically as the Rectus muscle origins. The pulleys consist of discrete rings of dense collagen, which encircle the EOM, transitioning into less substantial but broader collagen sleeves both posteriorly and anteriorly.
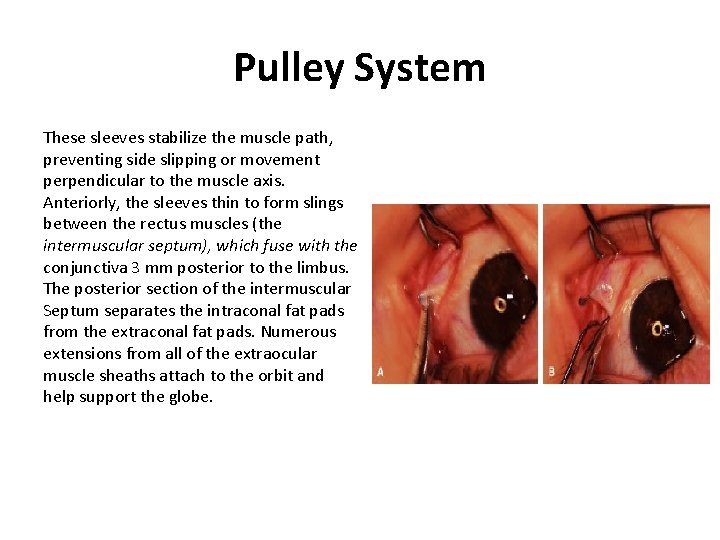
Pulley System These sleeves stabilize the muscle path, preventing side slipping or movement perpendicular to the muscle axis. Anteriorly, the sleeves thin to form slings between the rectus muscles (the intermuscular septum), which fuse with the conjunctiva 3 mm posterior to the limbus. The posterior section of the intermuscular Septum separates the intraconal fat pads from the extraconal fat pads. Numerous extensions from all of the extraocular muscle sheaths attach to the orbit and help support the globe.
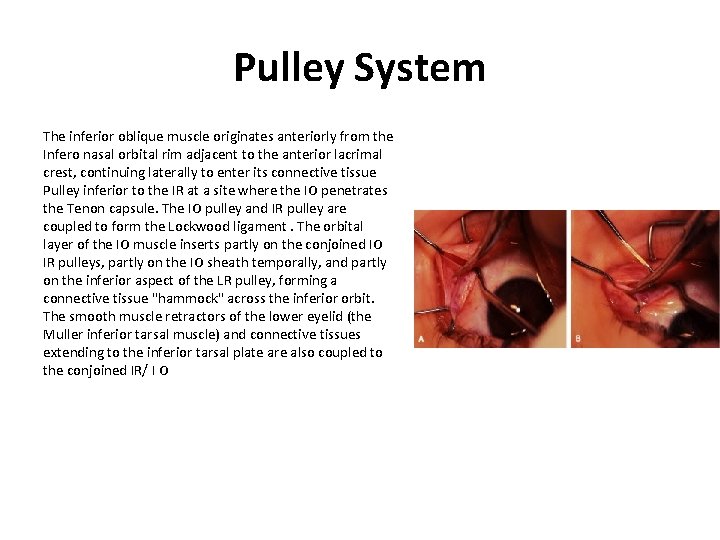
Pulley System The inferior oblique muscle originates anteriorly from the Infero nasal orbital rim adjacent to the anterior lacrimal crest, continuing laterally to enter its connective tissue Pulley inferior to the IR at a site where the IO penetrates the Tenon capsule. The IO pulley and IR pulley are coupled to form the Lockwood ligament. The orbital layer of the IO muscle inserts partly on the conjoined IO IR pulleys, partly on the IO sheath temporally, and partly on the inferior aspect of the LR pulley, forming a connective tissue "hammock" across the inferior orbit. The smooth muscle retractors of the lower eyelid (the Muller inferior tarsal muscle) and connective tissues extending to the inferior tarsal plate are also coupled to the conjoined IR/ I O
- Slides: 44