Stopping the Gaps Resident Driven OB Chart Audits
Stopping the Gaps: Resident -Driven OB Chart Audits Elizabeth Menzel, MD Kathryn Jacobe, MD Megan Everson, MD Kirsten Gierach, DO

Welcome: Who are we?
Who are you? • Are you currently doing any chart audits? • If so, of what types of charts? And for what purpose?
Disclosures • None
Objectives • On completion of this session, the participants should be able to… – Engage in reflective conversation concerning the challenges and barriers residents face in providing high quality, comprehensive evidence-based prenatal care. – Contemplate the unique benefits of a resident-driven audit process, particularly as it applies to resident learning, peer review process, and patient care. – Actively strategize the institution of a resident-driven chart auditing process in the attendees’ residency programs and leave with written materials to aid in this process.
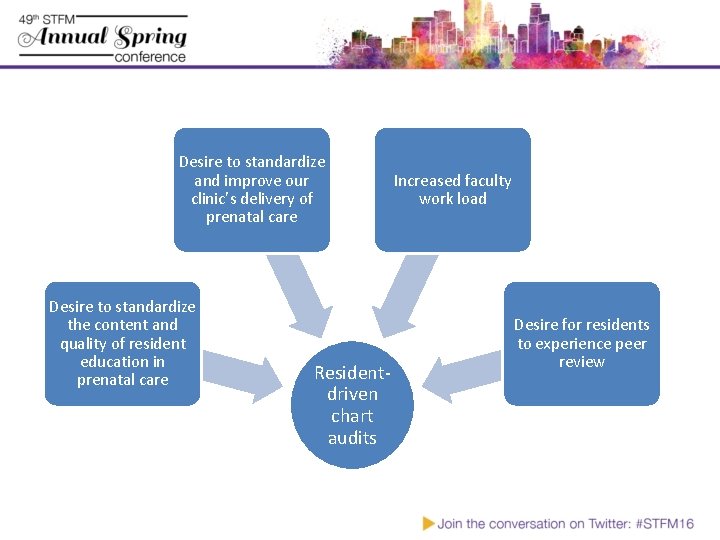
Desire to standardize and improve our clinic’s delivery of prenatal care Desire to standardize the content and quality of resident education in prenatal care Residentdriven chart audits Increased faculty work load Desire for residents to experience peer review
Standardize + Improve Resident Education • Identify/close gaps in knowledge • Standardize goals of care based on evidence-driven guidelines • PCP responsibility for all aspects of care (even delegated tasks) • Teach peer-review and professional practice improvement
Standardize + Improve Delivery of Prenatal Care • • Improve handoffs Identify/close gaps in patient care Increase supervision of patient care Ensure standardized high-quality, evidence-based care • Better manage a complex panel of patients
Self (or within program) Reflection • Currently Auditing – What are your current barriers and successes? • Not Auditing – In what context could you use auditing?
How did we develop our audits? – Found that a sister residency program (UW Verona FMR) was exploring chart audit process, but struggled with legal barriers of documentation – Explored their current materials – Reviewed evidence-based guidelines and made modifications to existing audits
How did we develop our audits? • Identified major goal-oriented milestones at which to do audits: 18 w, 28 w, 36 w • Adjusted audit structure/questions to correlate with milestones
How did we develop our audits? • Developed Epic templates and appropriate encounter-type to satisfy being in the chart but not discoverable • Started auditing – Initial “snapshot” – Then at 18, 28, 36 weeks • Auditing Gap
How did we develop our audits? • Residents missed the audits (!!) • Engaged resident leaders interested in reinvigorating audit process • Created new process
What is our current process? – Receptionist sends weekly message in EMR to residents who need to start audit – R 2 s on OB rotation create encounter/perform audit/review • Send to core OB faculty who review on rotating schedule (non-call week) • Send to primary OB doc (residents and/or faculty)
What is our current process? – Primary OB opens separate encounters/addend notes as needed to complete outstanding tasks. • Separate from audit encounter – When completed, residents cite chart location of completed tasks • Forward audit encounter to core OB faculty – Faculty review and close encounter if appropriate • Re-send/educate about any remaining tasks • Send to non-OB faculty who supervised care – Receptionist tracks timeliness/completion
Individual reflection. (2 minutes) • Currently auditing – What is something you may take away from our process that you can take to your own program – Write down the first step to incorporate that aspect. • Not auditing – What is the biggest barrier to starting audits? – Write down the first step to take to overcome that barrier.
Outcomes: Resident Feedback • Initial Complaints – Excessive, creates more work – Wish we would have started it sooner! • Later Reactions – Improves: • Quality of care • Resident knowledge • Documentation – Prioritizes future visit needs – Coordinates care between providers – Templates = intuitive, efficient
Outcomes • Identify/address knowledge gaps for all team members • Identify/address process failures • Improved post-dates planning • Helps close incomplete loops – Referrals/imaging/testing • Improved resident-resident professional communication • De-centralized workload
Discuss • What barriers did you identify and how have you/how do you plan to overcome them? • Benefits/concerns about residents driving this process?
Questions? Elizabeth Menzel, MD Katie Jacobe, MD Megan Everson, MD Kirsten Gierach, DO
Thank you! Please evaluate this presentation using the conference mobile app! Simply click on the "clipboard" icon on the presentation page.
- Slides: 22