Stool Analysis What is the stool or feces
- Slides: 28
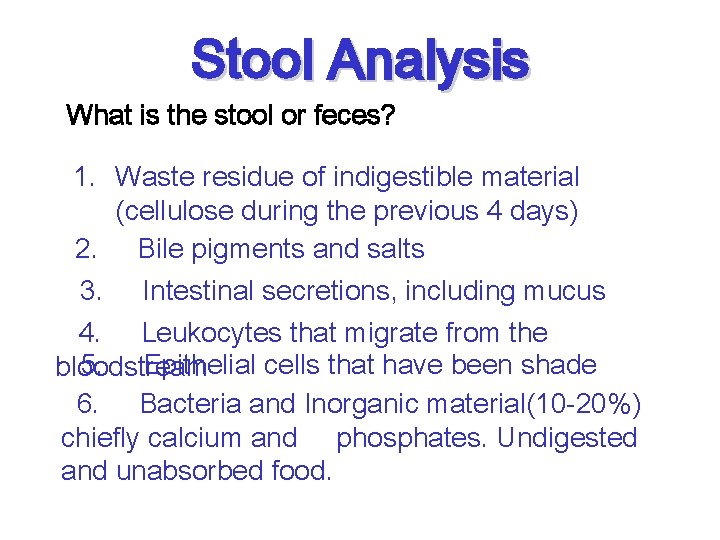
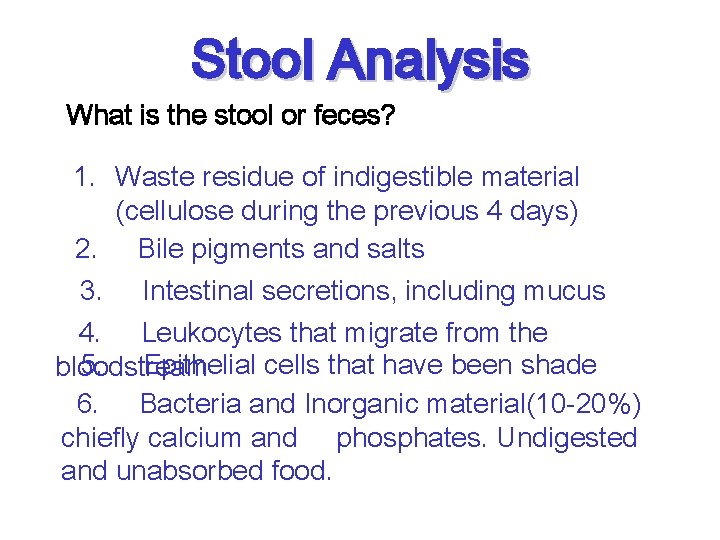
Stool Analysis What is the stool or feces? 1. Waste residue of indigestible material (cellulose during the previous 4 days) 2. Bile pigments and salts 3. Intestinal secretions, including mucus 4. Leukocytes that migrate from the 5. Epithelial cells that have been shade bloodstream 6. Bacteria and Inorganic material(10 -20%) chiefly calcium and phosphates. Undigested and unabsorbed food.
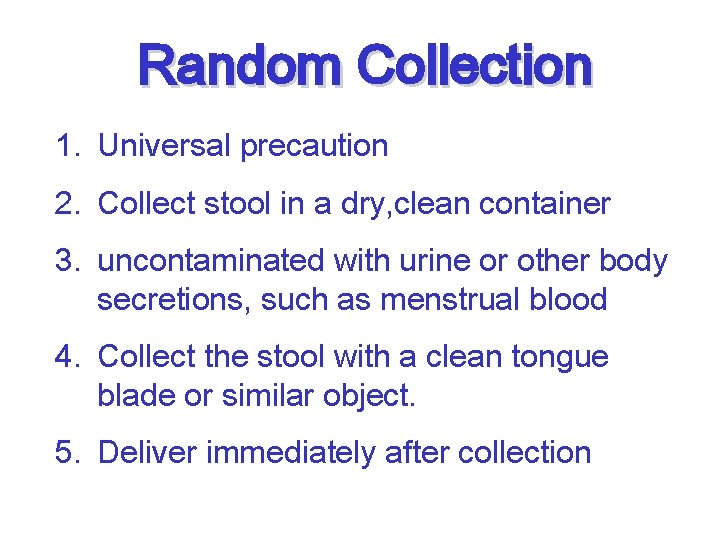
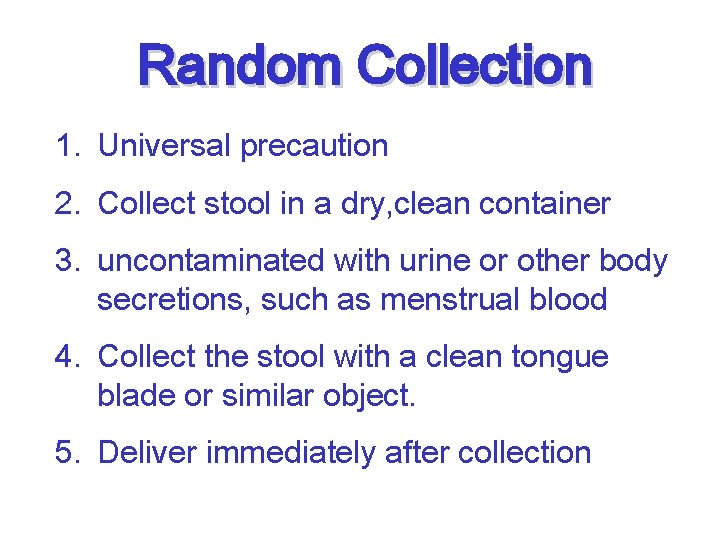
Random Collection 1. Universal precaution 2. Collect stool in a dry, clean container 3. uncontaminated with urine or other body secretions, such as menstrual blood 4. Collect the stool with a clean tongue blade or similar object. 5. Deliver immediately after collection
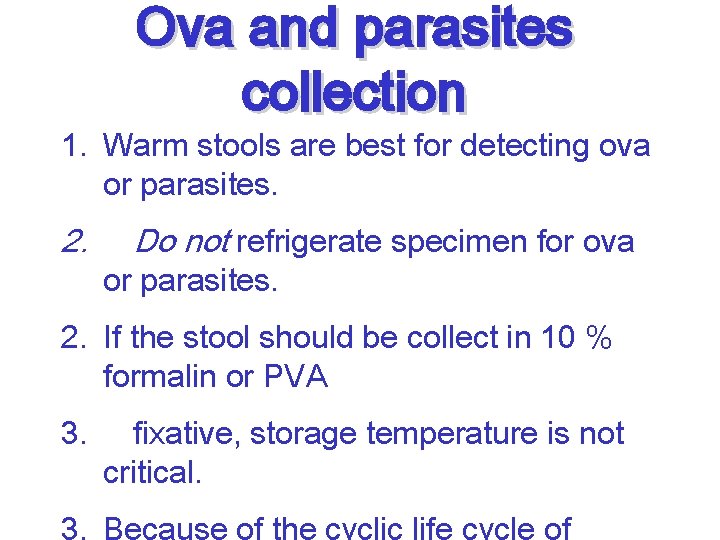
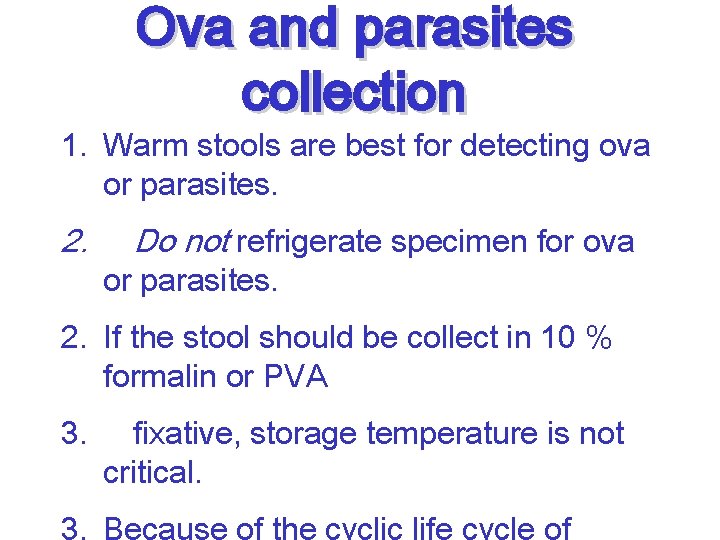
Ova and parasites collection 1. Warm stools are best for detecting ova or parasites. 2. Do not refrigerate specimen for ova or parasites. 2. If the stool should be collect in 10 % formalin or PVA 3. fixative, storage temperature is not critical.
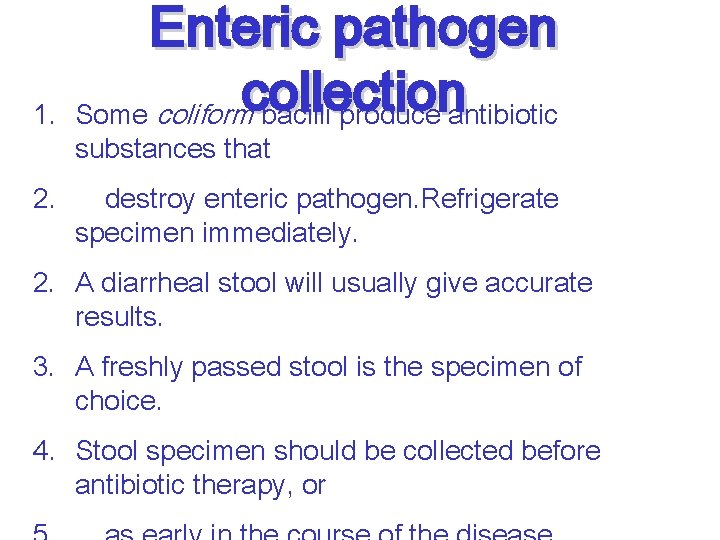
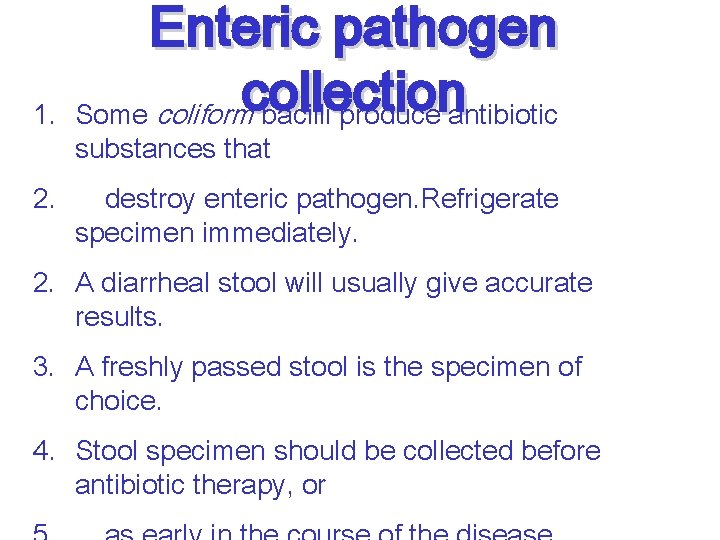
1. 2. Enteric pathogen collection Some coliform bacilli produce antibiotic substances that destroy enteric pathogen. Refrigerate specimen immediately. 2. A diarrheal stool will usually give accurate results. 3. A freshly passed stool is the specimen of choice. 4. Stool specimen should be collected before antibiotic therapy, or
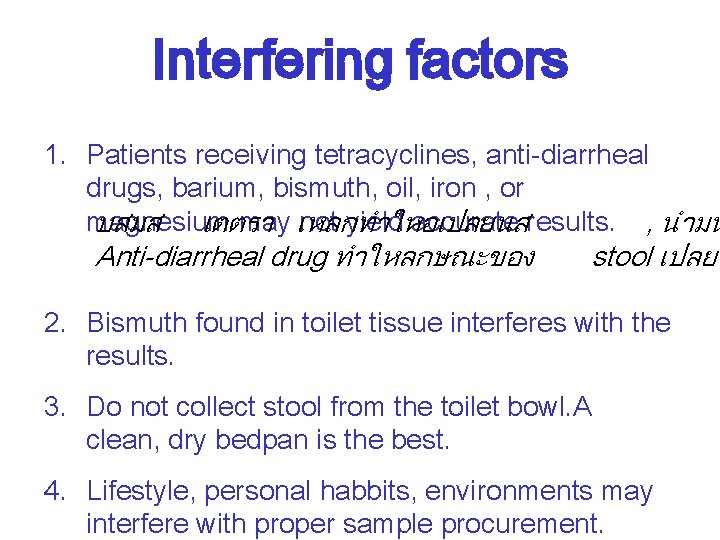
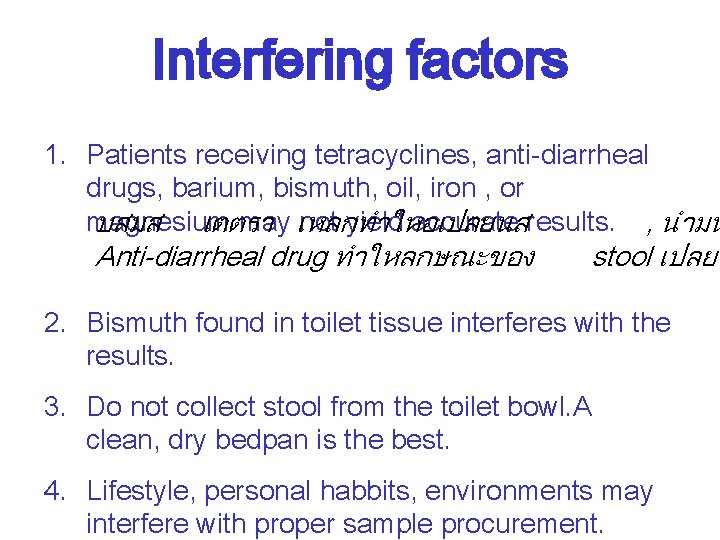
Interfering factors 1. Patients receiving tetracyclines, anti-diarrheal drugs, barium, bismuth, oil, iron , or magnesium may เหลกทำใหอเปลยนส not yield accurate results. , นำมน บสมส เตตรา Anti-diarrheal drug ทำใหลกษณะของ stool เปลยน 2. Bismuth found in toilet tissue interferes with the results. 3. Do not collect stool from the toilet bowl. A clean, dry bedpan is the best. 4. Lifestyle, personal habbits, environments may interfere with proper sample procurement.
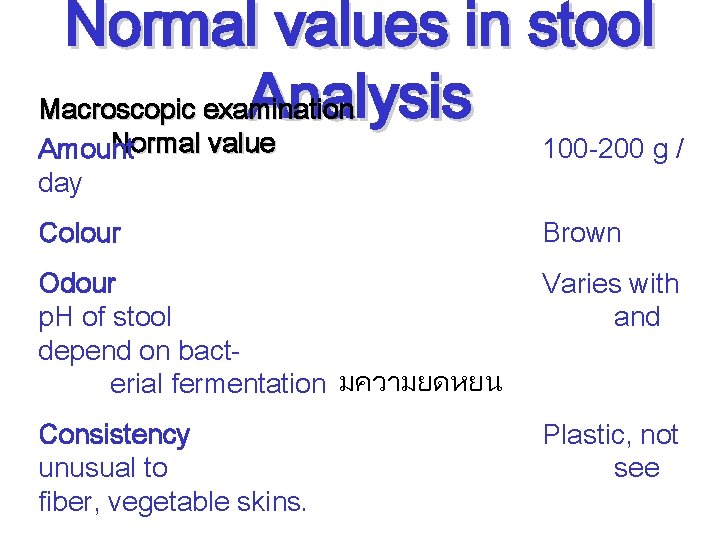
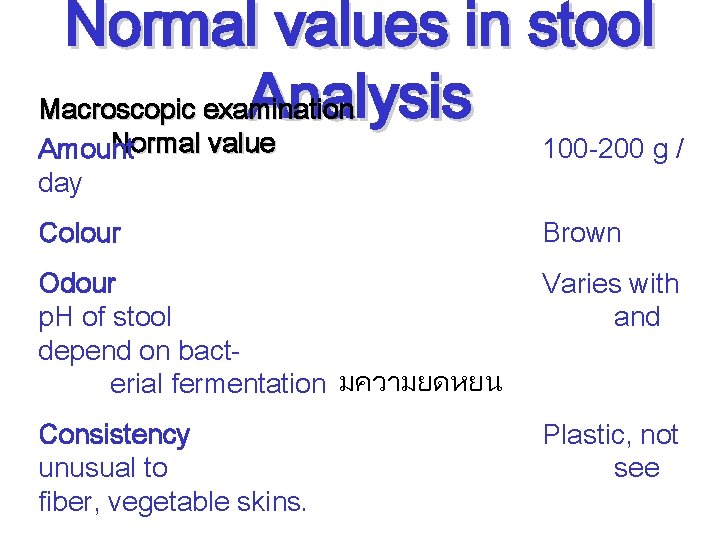
Normal values in stool Analysis Macroscopic examination Normal value Amount day 100 -200 g / Colour Brown Odour p. H of stool depend on bacterial fermentation มความยดหยน Varies with and Consistency unusual to fiber, vegetable skins. Plastic, not see
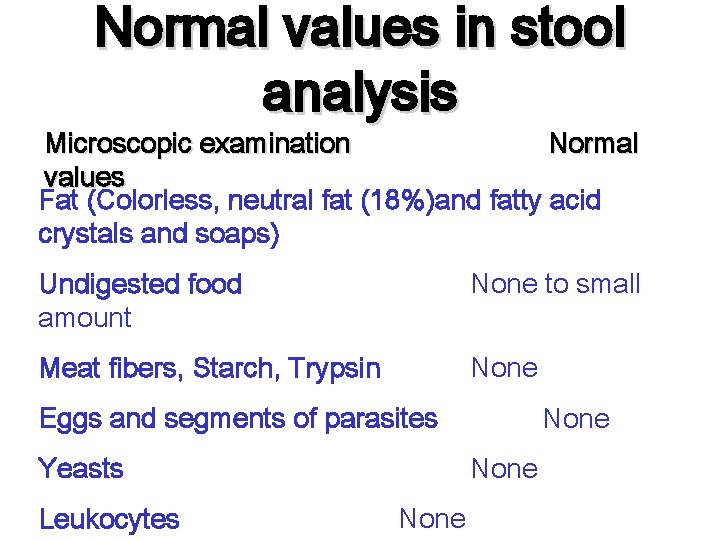
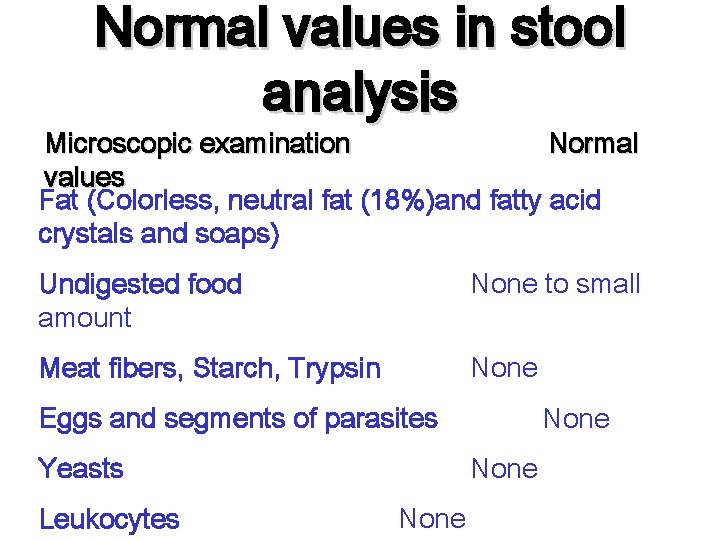
Normal values in stool analysis Microscopic examination Normal values Fat (Colorless, neutral fat (18%)and fatty acid crystals and soaps) Undigested food amount None to small Meat fibers, Starch, Trypsin None Eggs and segments of parasites Yeasts Leukocytes None
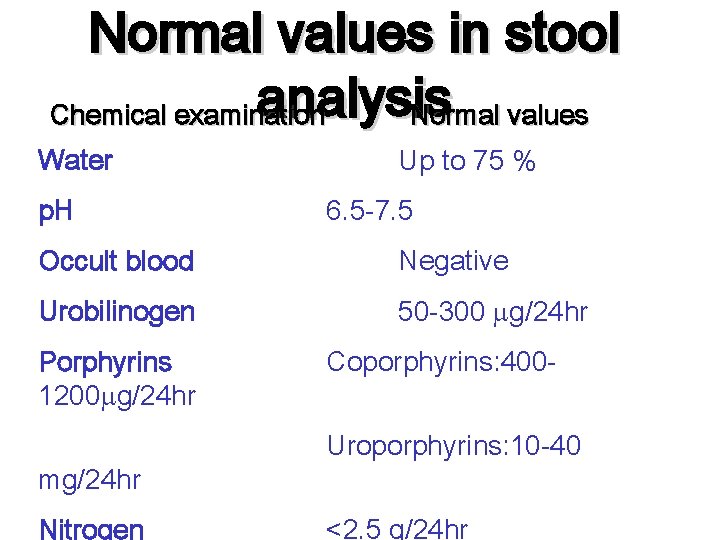
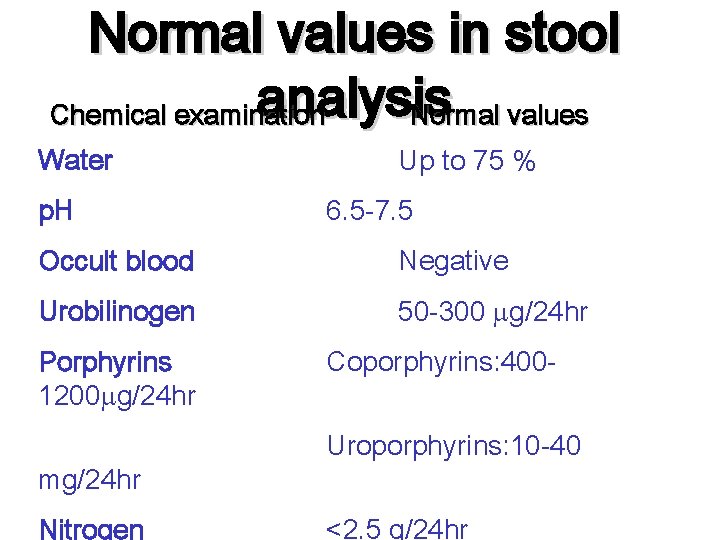
Normal values in stool analysis Chemical examination Normal values Water p. H Up to 75 % 6. 5 -7. 5 Occult blood Negative Urobilinogen 50 -300 g/24 hr Porphyrins 1200 g/24 hr mg/24 hr Nitrogen Coporphyrins: 400 Uroporphyrins: 10 -40 <2. 5 g/24 hr
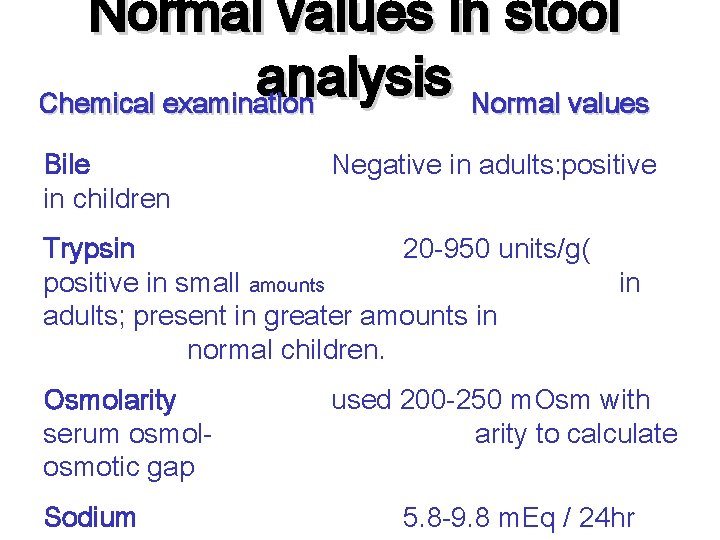
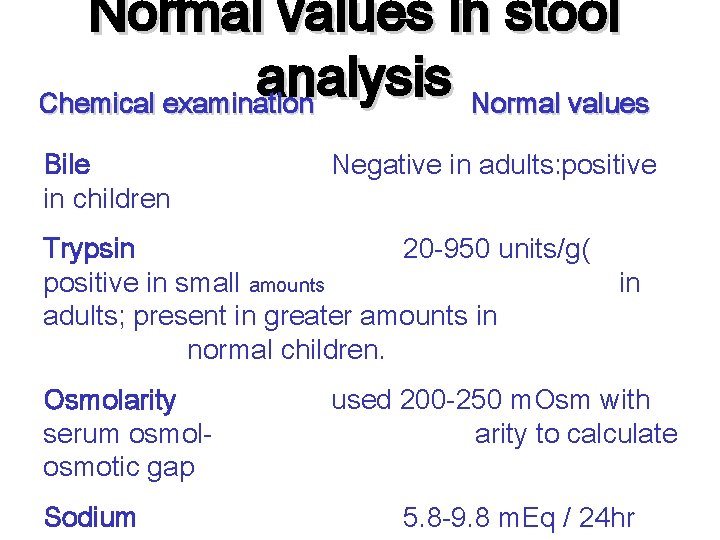
Normal values in stool analysis Chemical examination Normal values Bile in children Negative in adults: positive Trypsin 20 -950 units/g( positive in small amounts adults; present in greater amounts in normal children. Osmolarity serum osmolosmotic gap Sodium in used 200 -250 m. Osm with arity to calculate 5. 8 -9. 8 m. Eq / 24 hr
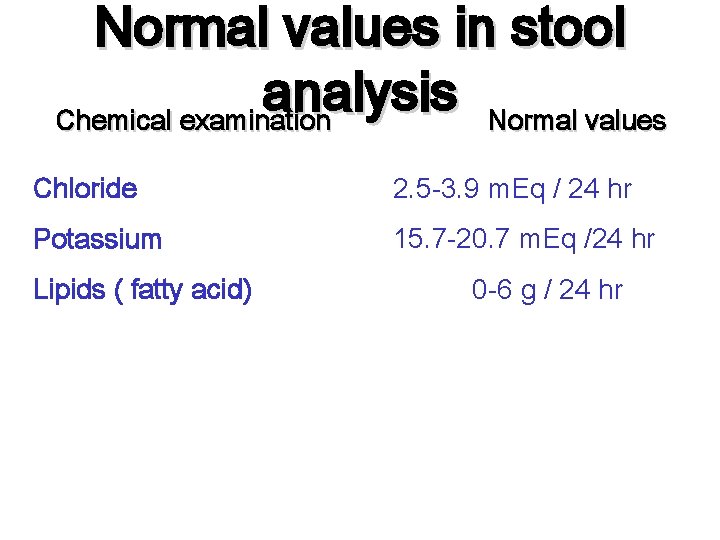
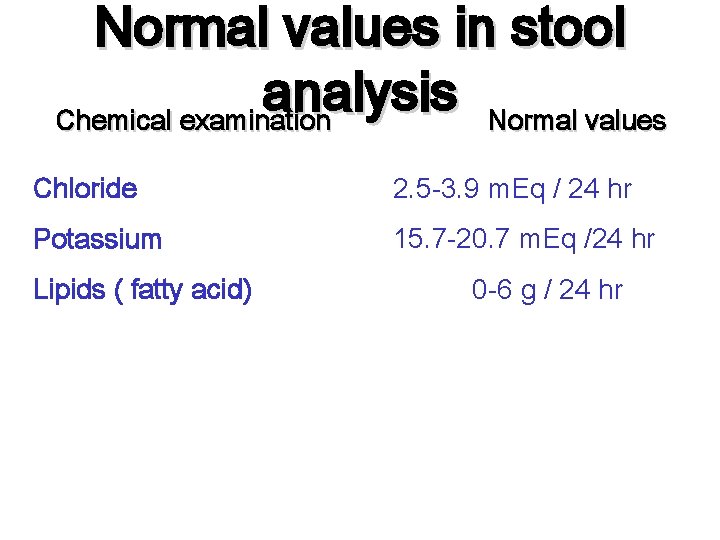
Normal values in stool analysis Chemical examination Normal values Chloride 2. 5 -3. 9 m. Eq / 24 hr Potassium 15. 7 -20. 7 m. Eq /24 hr Lipids ( fatty acid) 0 -6 g / 24 hr
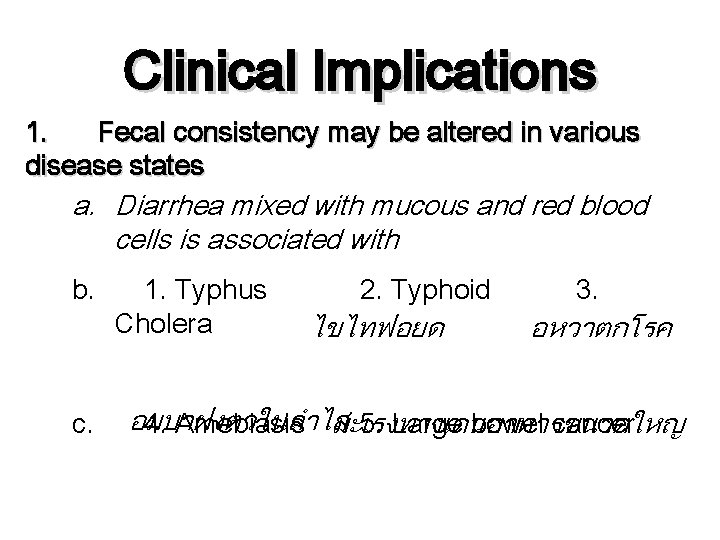
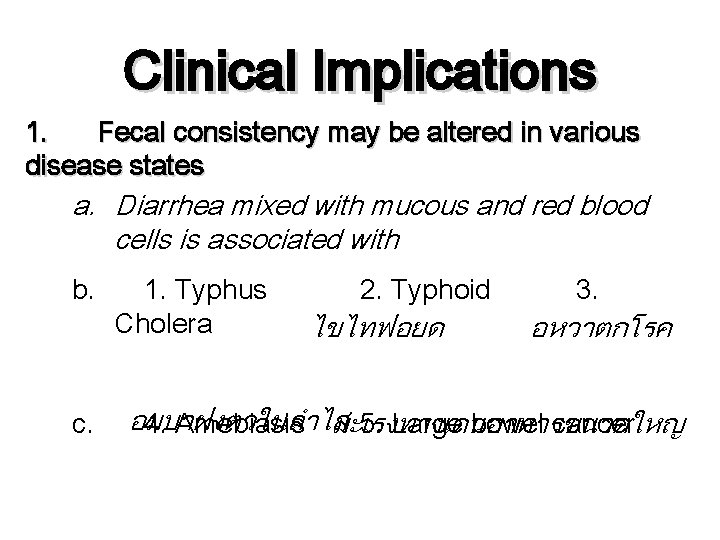
Clinical Implications 1. Fecal consistency may be altered in various disease states a. Diarrhea mixed with mucous and red blood cells is associated with b. c. 1. Typhus Cholera 2. Typhoid ไขไทฟอยด 3. อหวาตกโรค อมบาฝงตวในลำไส 4. Amebiasis มะเรงทางเดนอาหารขนาดใหญ 5. Large bowel cancer
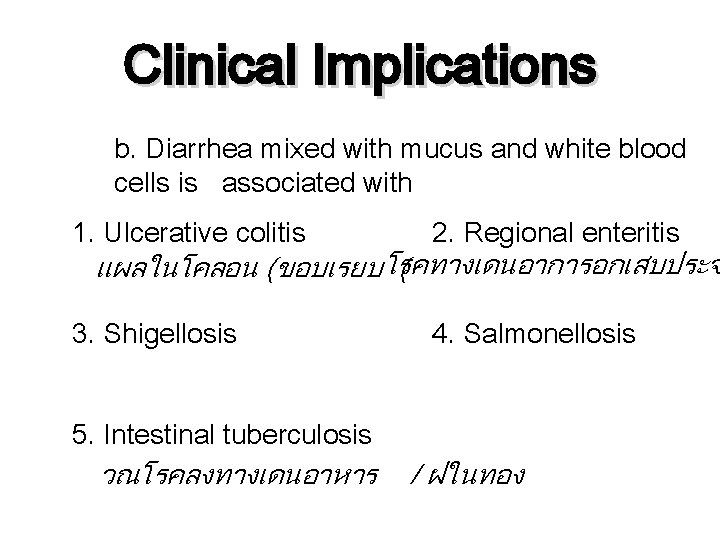
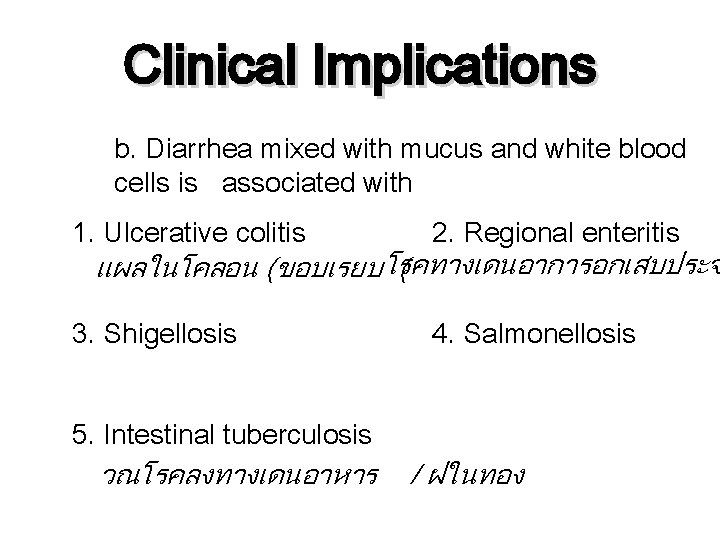
Clinical Implications b. Diarrhea mixed with mucus and white blood cells is associated with 1. Ulcerative colitis 2. Regional enteritis 3. Shigellosis 4. Salmonellosis แผลในโคลอน (ขอบเรยบ โรคทางเดนอาการอกเสบประจ ( 5. Intestinal tuberculosis วณโรคลงทางเดนอาหาร / ฝในทอง
Clinical Implications C. ”Pasty” stool is associated with a high fat content in the stool: 1. A significant increase of fat is usually detected on gross examination 2. With common bile duct obstruction, the fat gives the stool a putty- like appearance. 3. In cystic fibrosis, the increase of neutral fat gives มพงผดเกดขนในถงนำด a greasy, “butter stool” appearance.
Stool Odor Normal value Varies with p. H of stool and diet. Indole and sketole are the substances that produce normal odor formed by intestinal bacteria putrefaction and fermentation. Clinical implication. 1. A foul odor is caused by degradation of undigested protein. 2. A foul odor is produced by excessive carbohydrate ingestion. 3. A sickly sweet odor is produced by volatile
Stool color Normal value : Brown Clinical implication: 1. Yellow to yellow-green : severe diarrhea 2. Green : severe diarrhea เขยวเพราะนำดดดกลบไมทน ไมมเวลาใหแบคทเรยยอย bile Black: resulting from bleeding into the upper gastrointestinal tract (>100 ml blood) การบลอกทำใหไมมนำด การทมเลอดออกในทางเดนอาหารสวนบนเหล กจะถกกรดออกซไดซไดสดำ 3. Tan or Clay colored : blockage of the common แสดงถงการทไขมนไมถกยอย
Stool color(con( 4. Maroon-to-red-to-pink : possible result of bleeding from the lower gastrointestinal tract (eg. เนองอก , รดสดวง , รองตดแหก Tumors, hemorrhoids, fissures, inflammatory process) 5. Blood streak onรดสดวง the outer, surface of usually รกนผดปกต indicates hemorrhoids or anal abnormalities. 6. Blood in stool can arise from abnormalities higher in the colon. In some case the transit time is rapid blood from stomach or duodenum can appear as bright or dark red or maroon in stool.
Blood in Stool Normal value : Negative Clinical Implication : 1. Dark red to tarry black indicates a loss of 0. 50 to 0. 75 ml of blood from the upper GI tract. 2. Positive for occult blood may be caused by มะเรงของโคลอน colitis a. Carcinoma of colon แผลขอบเรยบทโคล b. Ulcerative ใสเลอนทกระบงลม ลำไสพนกนทำใหเน c. มะเรงกระเพาะอาการ Adenoma d. Diaphramatic hernia e. Gastric carcinoma g. Ulcers f. Diverticulitis
Mucous in Stool Normal value : Negative for mucous Clinical Implication: 1. Translucent gelatinous mucous clinging to the surface of formed stool occurs in เบงแรงๆ เมอกจากการอกเสบ a. Spastic constipation b. Mucous colitis อารมย c. Emotionally disturbed patients เกบอนานไป ไมชอบถาย d. Excessive straining at stool 2. Bloody mucous clinging to the surface suggests a. Neoplasm เนองอก rectal canal b. Inflammation of the ภาวะอกเสบทไสตรง
Mucous in Stool (con) 3. Mucous with pus and blood is associated with a. Ulcerative colitis dysentery ตดเชอแบซไล b. Bacilliary แผลทเกดจากมะเรงโคลอน c. Ulcerating cancer of colon diverticulitis e. Intestinal tuberculosis ลำไสพนก d. Acute
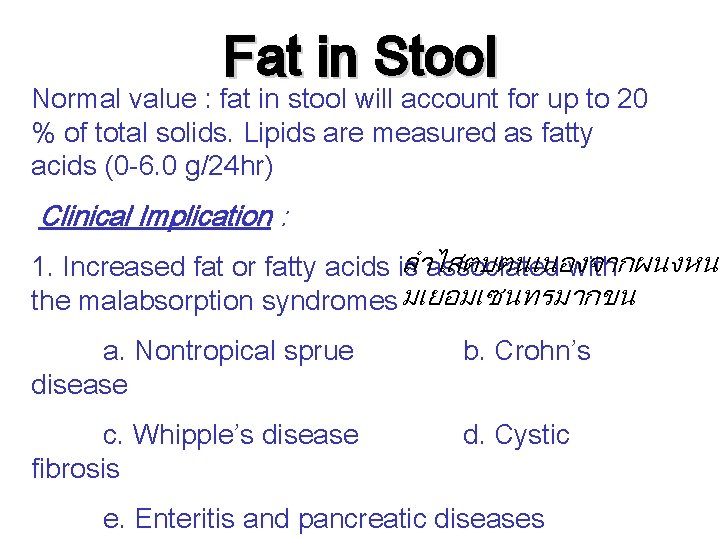
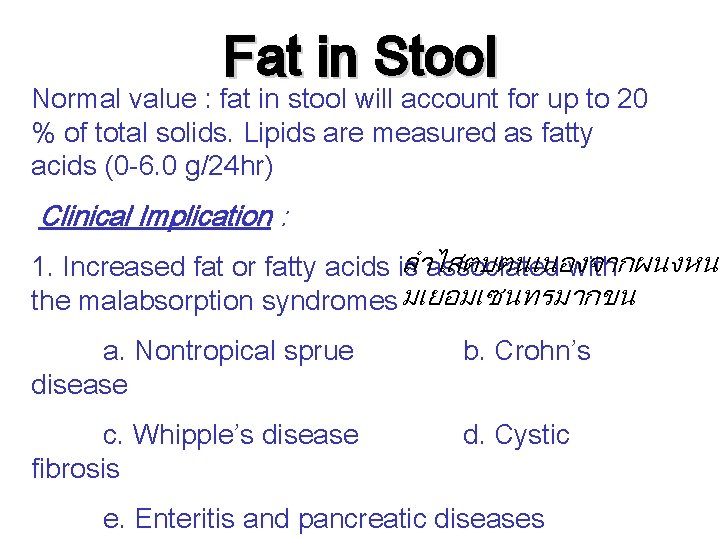
Fat in Stool Normal value : fat in stool will account for up to 20 % of total solids. Lipids are measured as fatty acids (0 -6. 0 g/24 hr) Clinical Implication : ลำไสตบตนเนองจากผนงหนา 1. Increased fat or fatty acids is associated with the malabsorption syndromes มเยอมเซนทรมากขน a. Nontropical sprue disease b. Crohn’s c. Whipple’s disease fibrosis d. Cystic e. Enteritis and pancreatic diseases
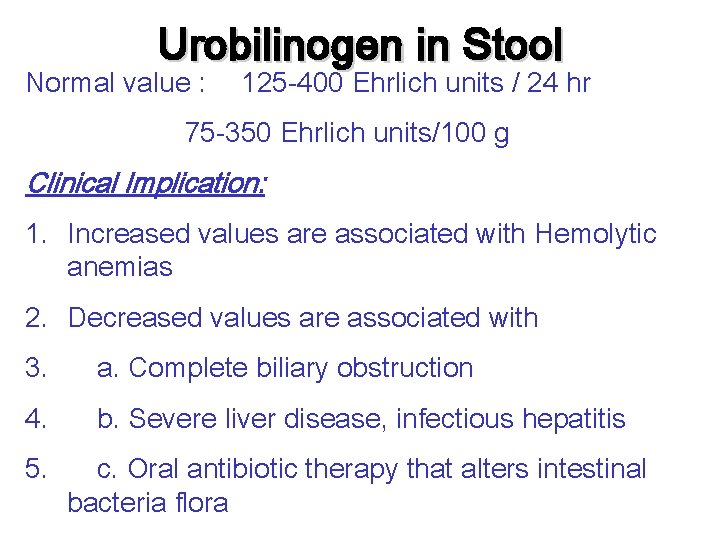
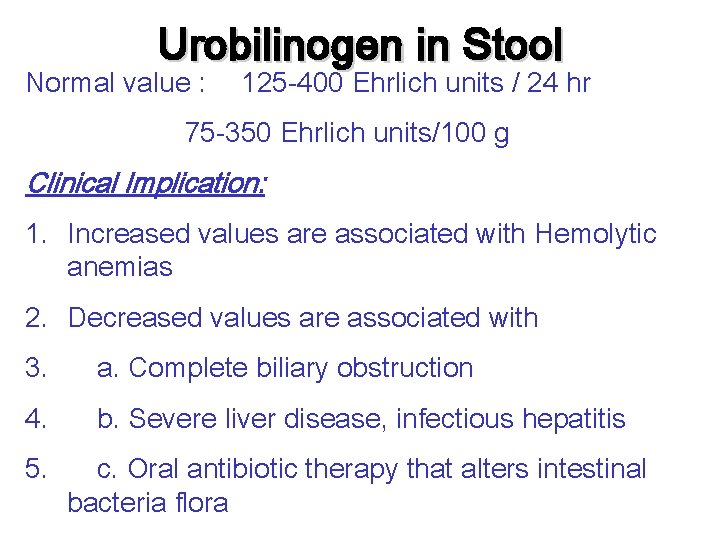
Urobilinogen in Stool Normal value : 125 -400 Ehrlich units / 24 hr 75 -350 Ehrlich units/100 g Clinical Implication: 1. Increased values are associated with Hemolytic anemias 2. Decreased values are associated with 3. a. Complete biliary obstruction 4. b. Severe liver disease, infectious hepatitis 5. c. Oral antibiotic therapy that alters intestinal bacteria flora
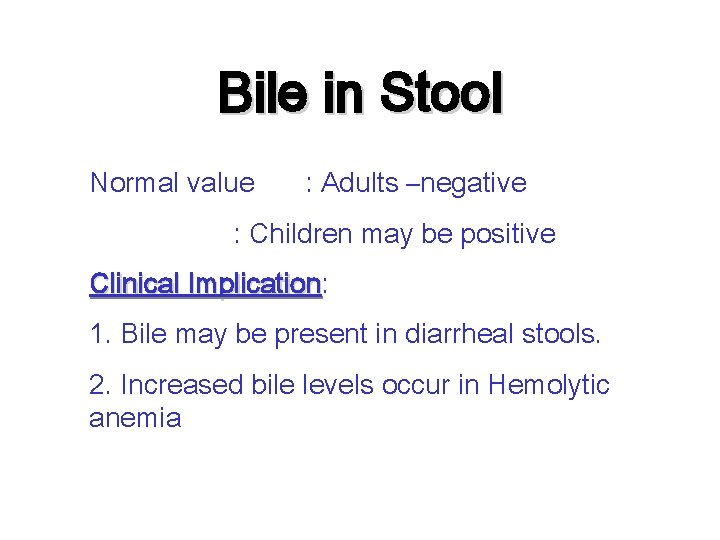
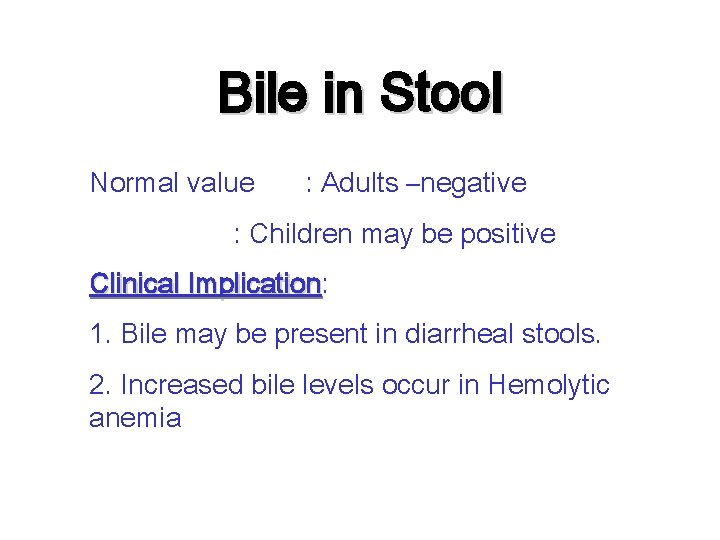
Bile in Stool Normal value : Adults –negative : Children may be positive Clinical Implication: Implication 1. Bile may be present in diarrheal stools. 2. Increased bile levels occur in Hemolytic anemia
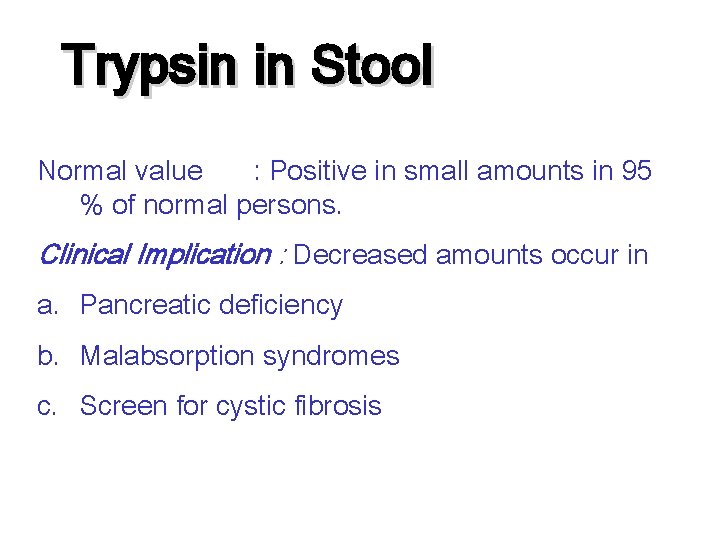
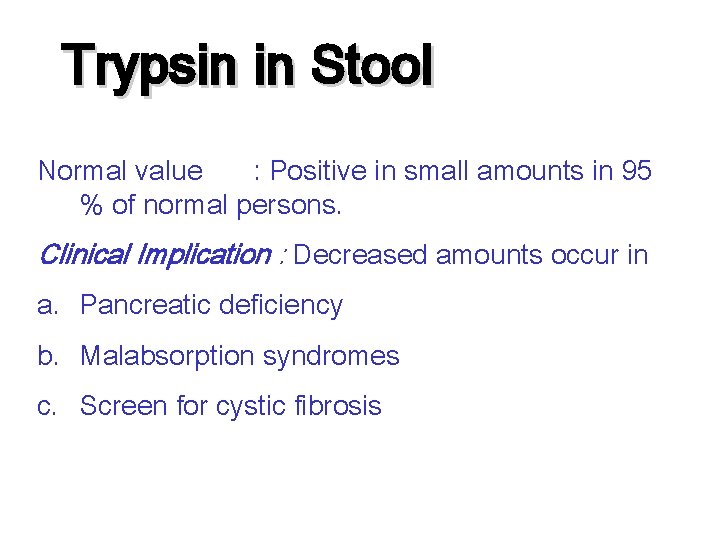
Trypsin in Stool Normal value : Positive in small amounts in 95 % of normal persons. Clinical Implication : Decreased amounts occur in a. Pancreatic deficiency b. Malabsorption syndromes c. Screen for cystic fibrosis
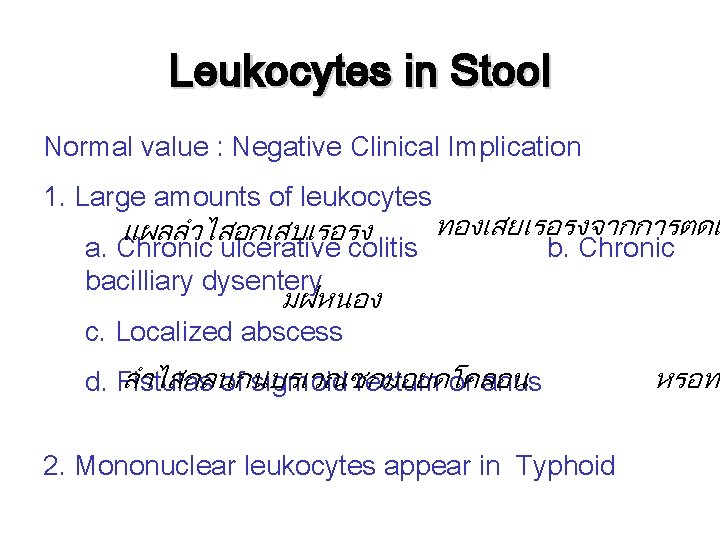
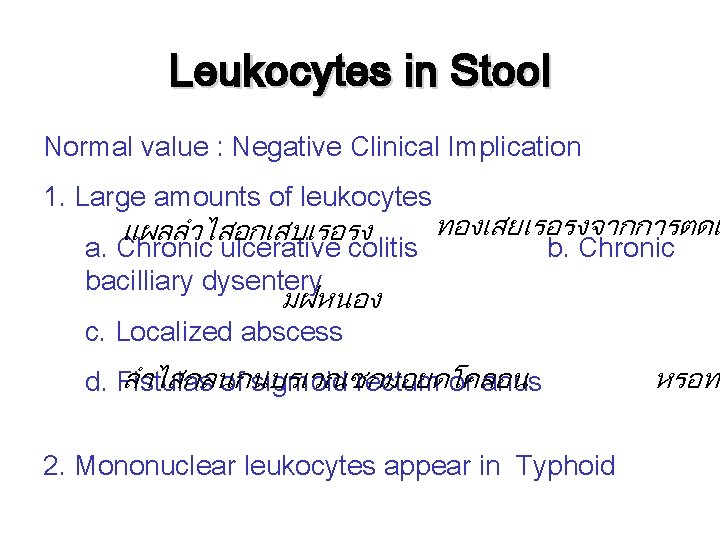
Leukocytes in Stool Normal value : Negative Clinical Implication 1. Large amounts of leukocytes แผลลำไสอกเสบเรอรง a. Chronic ulcerative colitis bacilliary dysentery ทองเสยเรอรงจากการตดแ b. Chronic มฝหนอง c. Localized abscess ลำไสกลนกนบรเวณซกมอยดโคลอน d. Fistulas of sigmoid rectum or anus 2. Mononuclear leukocytes appear in Typhoid หรอทท
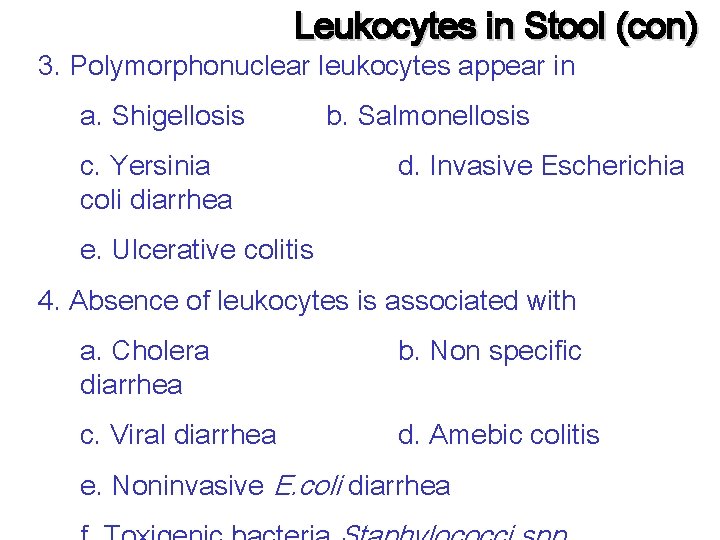
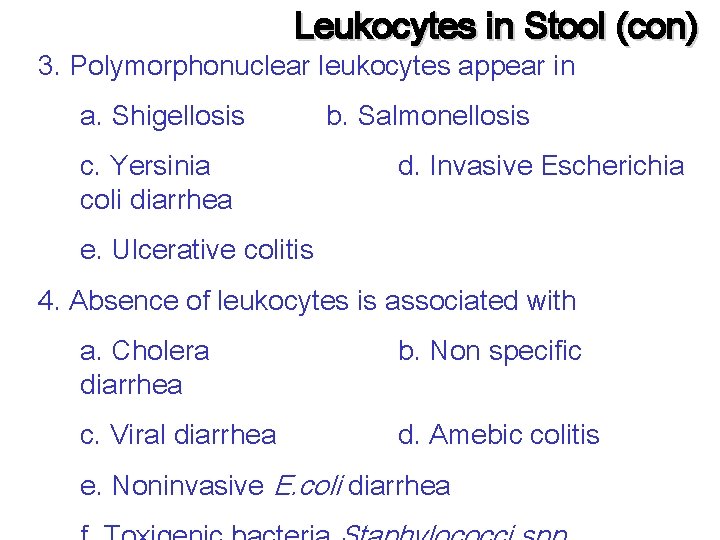
Leukocytes in Stool (con) 3. Polymorphonuclear leukocytes appear in a. Shigellosis c. Yersinia coli diarrhea b. Salmonellosis d. Invasive Escherichia e. Ulcerative colitis 4. Absence of leukocytes is associated with a. Cholera diarrhea b. Non specific c. Viral diarrhea d. Amebic colitis e. Noninvasive E. coli diarrhea
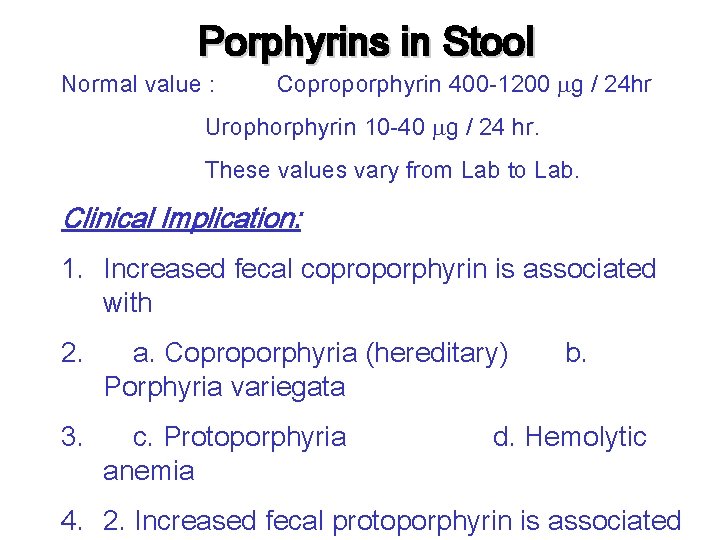
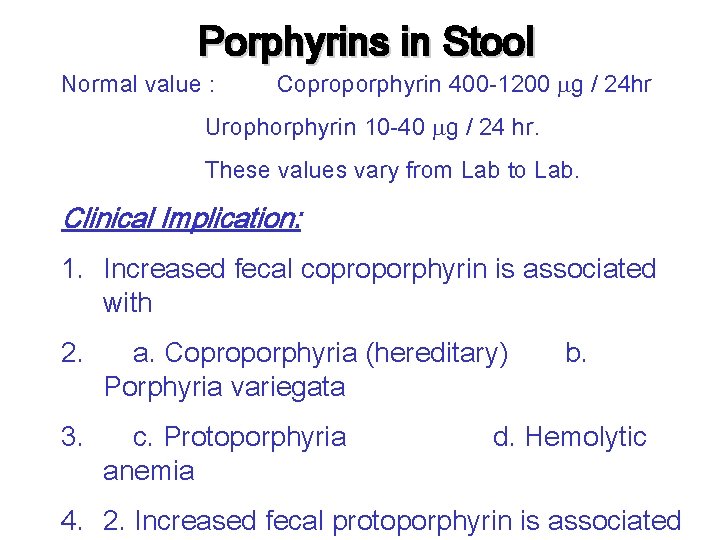
Porphyrins in Stool Normal value : Coproporphyrin 400 -1200 g / 24 hr Urophorphyrin 10 -40 g / 24 hr. These values vary from Lab to Lab. Clinical Implication: 1. Increased fecal coproporphyrin is associated with 2. a. Coproporphyria (hereditary) Porphyria variegata 3. c. Protoporphyria anemia b. d. Hemolytic 4. 2. Increased fecal protoporphyrin is associated
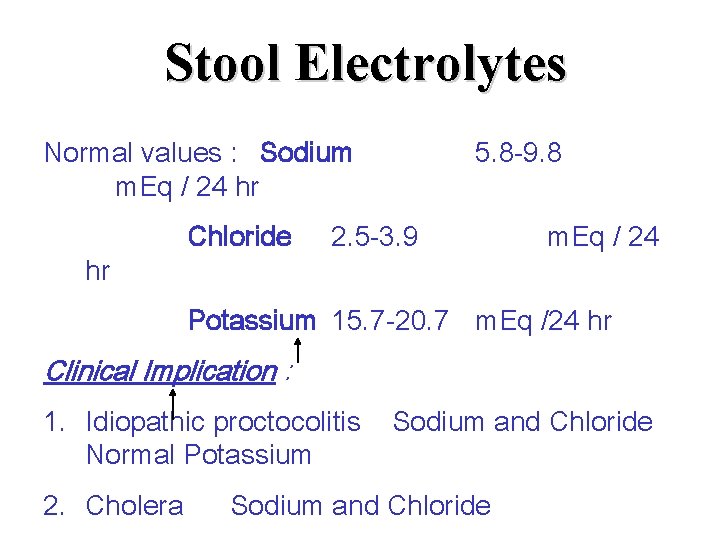
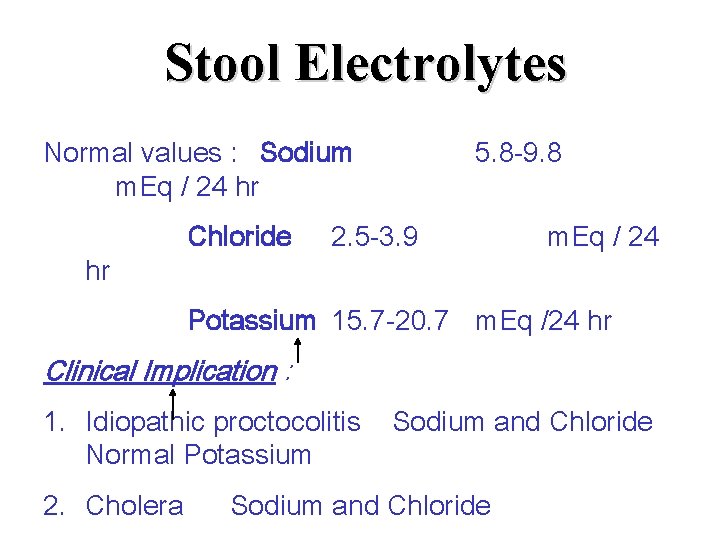
Stool Electrolytes Normal values : Sodium m. Eq / 24 hr hr Chloride 5. 8 -9. 8 2. 5 -3. 9 m. Eq / 24 Potassium 15. 7 -20. 7 m. Eq /24 hr Clinical Implication : 1. Idiopathic proctocolitis Normal Potassium 2. Cholera Sodium and Chloride